Abstract
Background: Appropriate component sizing plays an important role in determining the functional outcome following total knee arthroplasty. Comparative studies of different populations have shown significant differences in the anthropometric parameters of knees in different race groups which negates the possibility of using a single sized implant system across different ethnic groups. This study evaluates the dimensions of femoral and tibial articular surfaces of Indian patients and compares the parameters with other ethnic groups and correlates the dimensions with five different commercially available knee systems.
Material & Methods: Computerized tomography (CT) scans of contralateral normal knees of patients who underwent the scan for various ailments of the knee were retrieved retrospectively from the hospital database and 3D reconstruction of the images was done. Mediolateral dimensions (fML,tML), Anteroposterior dimensions (fAP, tAP) and aspect ratio (fML/fAP, tML/tAP) of the femur and tibia respectively were calculated and compared with the dimensions of different ethnic groups as well as the femoral and tibial components of five different knee prosthesis systems.
Results
The average fML in the study group was less than that of Caucasian knees but was marginally larger than other ethnic groups. The fAP, tML and tAP was found to be smaller than all other ethnic groups but a larger femoral aspect ratio was reported than other ethnic groups. Among the implant systems, only NexGen LPS and Scorpio NRG implant femoral components closely matched the femoral dimensions in the study group whereas all implant systems showed significant mismatch with tibial component dimensions when compared to the study populations.
Conclusion
This study concludes that the dimensions of Indian knees are different from other ethnic groups and the use of commercially available knee Implants designed based on measurements in Caucasian populations can lead to significant mismatch between implant and resected bone surfaces.
Keywords: Component mismatch, Knee arthroplasty, Indian, Ethnic groups
1. Introduction
The successful functional recovery after total knee arthroplasty (TKA) depends on a lot of factors among which appropriate component sizing is significantly important1. Implant sizes that provide optimum coverage of the resected bone surfaces during TKA result in adequate flexion and extension gaps leading to adequate quadriceps strength and knee function2. It is important to note that mediolateral sizing of the resected surfaces is also important to allow for even stress distribution between the articulating surfaces and proper tracking of the patella in trochlear groove3. However, most of the implants have been designed based on the anthropometric parameters in Caucasian population which may not match the morphological parameters in Indian patients. Previously published studies on anthropometry of different races have shown significant differences in anthropometric parameters of Caucasian, African, Asian and Indian patients4.
Based on the preexisting studies about the racial differences, manufacturers have attempted to design implants specific to racial groups especially in Asian patients. However, relatively few implants have been designed catering to the anthropometric dimensions of Indian patients and most surgeons use implants designed for Caucasian patients in Indian patients due to lack of availability of customized implants. This study aims to study the mediolateral and anteroposterior dimensions of femoral and tibial articular surfaces of Indian patients using a three-dimensional (3D) Computerized Tomography (CT) study and compare the parameters with other ethnic groups and correlate the dimensions with existing five popular commercially available TKA systems available in India.
2. Materials and methods
This retrospective study was conducted between June 2017 to November 2017 in a high-volume arthroplasty center catering to a diverse range of regional and socioeconomic strata of people in India. All the CT scans of contralateral normal knees of patients who underwent CT scan of the knee joint for various ailments were retrieved from the hospital database and evaluated. Patients with preexisting gross articular deformity, inflammatory arthritis or erosions or previous history of surgery on knee joint or hip joint precluding proper positioning of the joint were excluded from the study.
All CT scans of knee were performed on a 64 sliced helical CT scan system (Seimans Healthineers, Erlangen Germany). All patients were placed supine on the scanner with both knees placed in an extended position. During the scan, 0.625 mm slices (resolution, 512 × 512 pixels) with a field of view of 360 × 360 mm were obtained from the hip joint to the ankle joint. All the images were retrieved on the workstation and copied in a DICOM file format and the region of interest of tibia and femur were formatted in the form of 3D reconstruction which were used for anthropometric assessment.
Femoral Morphology assessment: transThe femoral anteroposterior size (fAP) was taken perpendicular to the poterior condylar line wherein the reconstructed distal femur was rotated axially along its long axis to make the posterior condylar line horizontal and the total length of the lateral femoral condyle in anteroposterior direction was taken as the fAP. The femoral mediolateral (fML) size was taken as widest mediolateral distance of femoral condyle on posterior condylar line. In addition, the femoral aspect ratio (fML/fAP) as described by Bing Yue et al. was calculated5, (Fig. 1).
Fig. 1.
3D reconstructed image of proximal tibia and distal femur.
Tibial Morphology: The tibial long axis was passing through the middle of the tibial spines and oriented parallel to the posterior wall of the tibial shaft in the sagittal plane. In the coronal plane, it was angled equally with respect to the medial and lateral edges of the tibial shaft. The tibia was rotated about its long axis. The tML dimension was taken as the longest mediolateral length of the proximal tibial surface. The tAP dimension was taken as perpendicular to tML and passing through the midpoint of the tibial intercondylar eminence. Subsequently, the tibial aspect ratio (tML/tAP) was calculated [Fig. 1].
Comparison with different ethnic groups and knee systems: Data obtained from this study was compared to available data of Americans, Chinese, Japanese and Korean knees previously published in literature. Furthermore, the obtained data was compared with five commonly used knee implant systems at our center which included PFC Sigma Knee System (DePuy), NexGen LPS Flex Mobile Knee System (Zimmer), Scorpio NRG Knee System (Stryker), Freedom (MAXX) and Beuchel Pappas mobile bearing knee arthroplasty system.
3. Statistical analysis
Comparative statistical analyses between genders were made using the paired t-test for parametric continuous data. Linear regression analysis was performed to determine correlations of simulated bones and size-matched components among 5 total knee prosthetic systems. A p value of <0.05 was considered as statistically significant. All analysis was performed using SPSS 20.0 software.
4. Results
100 knees were included in the study, in which 49 were female and 51 were male. Mean age of male patients was 39 ± 10.5 years and of female patients was 38 ± 9.9 years.
5. Morphology of Indian knee
Mean fML was found to be 72.0 ± 5.7 mm in whole population under study while mean fAP was 61.1 ± 4.0 mm. Average femoral aspect ratio was 1.18 ± 0.6. Males had larger values of fML and fAP as compared to females (p < 0.001). In case of the femoral aspect ratio, statistically significant difference was found between males and females (p < 0.001). Femoral measurements for the study population have been compared across genders in Table 1.
Table 1.
Shows the measured dimensions of distal femur and proximal tibia on a three-dimensional CT scan.
| Distal femur and proximal tibia parameters | Total Mean ± SD (Range) |
Female Mean ± SD (Range) |
Male Mean ± SD (Range) |
P value |
|---|---|---|---|---|
| fML | 72.0 ± 5.7 (60.1–81.3) | 67.4 ± 3.7 (60.1–74.2) | 76.4 ± 3.2 (69.9–81.3) | <0.001 |
| fAP | 61.1 ± 4.0 (51.9–68.5) | 59.4 ± 4.1 (51.9–68.5) | 62.7 ± 3.2 (56.8–68.3) | <0.001 |
| fML/fAP | 1.18 ± 0.6 (1.03–1.29) | 1.13 ± 0.5 (1.03–1.28) | 1.21 ± 0.4 (1.14–1.29) | <0.001 |
| tML | 70.4 ± 5.8 (60.7–84.2) | 65.8 ± 3.9 (60.7–74.3) | 74.7 ± 3.6 (69.9–84.2) | <0.001 |
| tAP | 46.1 ± 4.0 (38.5–53.1) | 43.1 ± 3.0 (38.5–50.4) | 48.9 ± 2.6 (42.0–53.1) | <0.001 |
| tML/tAP | 1.52 ± 0.08 (1.40–1.79) | 1.52 ± 0.08 (1.42–1.79) | 1.52 ± 0.08 (1.40–1.78) | 0.78 |
The average tML length was 70.4 ± 5.8 mm and average tAP length was 46.1 ± 4.0 mm. The average tibial aspect ratio was 1.52 ± 0.08. Males had larger values of tML and tAP as compared to females (p < 0.001). In case of the tibial aspect ratio, no statistically significant difference was found between males and females (p = 0.78). Tibial measurements for the study population have been compared across genders in Table 1.
6. Comparison across ethnicities
A comparison of our data with previously published data of different ethnic groups revealed some differences. The average fML in our group is less than that of American knees but was marginally larger than other ethnic groups (Table 2). The fAP was found to be smaller than all other ethnic groups along with a larger femoral aspect ratio than other ethnic groups. Similarly, tML and tAP of the knees in our study group was found to be the least when compared to other ethnic groups (Table 3).
Table 2.
Distal Femoral morphometry of various ethnic groups. F – Female, M − Male, C - Combined.
| fML | fAP | fML/fAP | |
|---|---|---|---|
| Our Stud | 72.0 ± 5.7 (C) | 61.1 ± 4.0 (C) | 1.18 ± 0.6 (C) |
| 67.4 ± 3.7 (F) | 59.4 ± 4.1 (F) | 1.13 ± 0.5 (F) | |
| 76.4 ± 3.2 (M) | 62.7 ± 3.2 (M) | 1.21 ± 0.4 (M) | |
| Americans Berger et al.10 Griffin et al.12 |
75.4 ± 2.3(F) | 60.2 ± 2.0(F) | |
| 85.6 ± 5.1(M) | 68.1 ± 4.6(M) | ||
| 78.0 ± 6.7(C) | |||
| 74.1 ± 4.6(F) | |||
| 84.1 ± 4.4(M) | |||
| Chinese Cheng et al.13 |
71.0 ± 3.0(C) | 64.1 ± 2.7(C) | 1.11 ± 0.03(C) |
| 66.8 ± 3.1(F) | 61.0 ± 2.7(F) | 1.09 ± 0.04(F) | |
| 74.4 ± 2.9(M) | 66.6 ± 2.4(M) | 1.12 ± 0.03(M) | |
| Japanese Urabe et al.13 |
70.6 ± 4.5(C) | ||
| Koreans Lee et al.9 |
75(C) |
Table 3.
Proximal Tibial morphometry of various ethnic groups.
| tML | tAP | tML/tAP | |
|---|---|---|---|
| Indians (Our Study) | 70.4 ± 5.8 (C) | 46.1 ± 4.0 (C) | 1.52 ± 0.08 (C) |
| 65.8 ± 3.9 (F) | 43.1 ± 3.0 (F) | 1.52 ± 0.08 (F) | |
| 74.7 ± 3.6 (M) | 48.9 ± 2.6 (M) | 1.52 ± 0.08 (M) | |
| Americans Mensch et al.14 | 70.1 ± 2.8 (F) | 42.1 ± 1.7 (F) | |
| 80.3 ± 3.7 (M) | 48.9 ± 2.3 (M) | ||
| Chinese Cheng et al.13 | 73.0 ± 4.6 (C) | 48.8 ± 3.4 (C) | 1.49 ± 0.05 (C) |
| 68.8 ± 4.6 (F) | 45.7 ± 1.9 (F) | 1.51 ± 0.06 (F) | |
| 76.4 ± 2.8 (M) | 51.3 ± 2.0 (M) | 1.49 ± 0.06 (M) | |
| Japanese Uehara et al.15 | 74.3 ± 6.6 (C) | 48.3 ± 5.4 (C) | |
| 71.7 ± 4.0 (F) | 46.6 ± 3.6 (F) | ||
| 83.0 ± 6.2 (M) | 53.8 ± 6.6 (M) | ||
| Koreans Kwak et al.16 | 71.9 ± 5.6 (C) | 45.7 ± 3.8 (C) | 1.57 (C) |
| 67.6 ± 3.1 (F) | 43.2 ± 2.3 (F) | 1.56 (F) | |
| 76.1 ± 4.0 (M) | 48.2 ± 3.3 (M) | 1.58 (M) |
7. Comparison with conventional implants
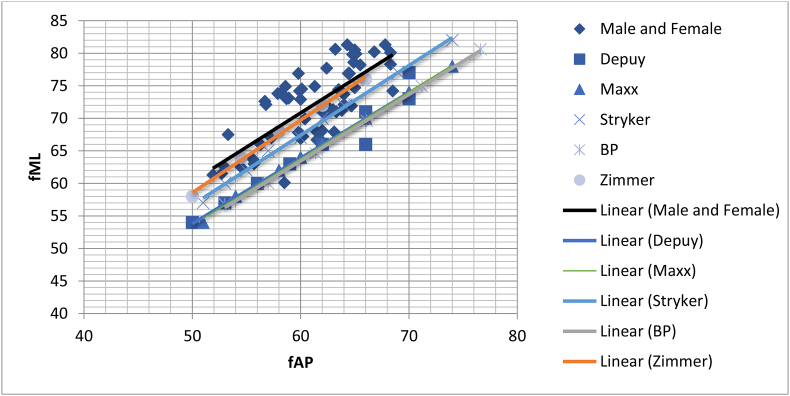
When the dimensions of the femoral components of different implants were compared with the femoral dimensions obtained in our study, only NexGen LPS and Scorpio NRG implant systems closely matched the data in our study (Fig. 2). Other implant systems showed significant mediolateral and anteroposterior mismatch of the femoral components explained by progressive decrease in the femoral aspect ratio with increase in fAP whereas the femoral aspect ratio of the implants has a constant femoral aspect ratio (Fig. 3). A sub group analysis of femoral components in female patients showed a significantly large for a given AP dimension with a larger overhand of the components in larger sizes (Fig. 4).
Fig. 2.
Comparison of fAP vs fML between study population and different knee systems.
Fig. 3.
Comparison of fAP vs fML/fAP between study population and different knee systems.
Fig. 4.
Comparison of fAP vs fML/fAP between female in study population and different knee systems.
When the tibial component dimensions were compared with the tibial anthropometry in our study, all implants systems showed significant mismatch between anteroposterior and mediolateral dimensions (Fig. 5). The implants showed that for smaller AP sizing, there was under-coverage of the implant in mediolateral dimension whereas in case of higher AP sizes, there was significant overhand of the tibial implant in mediolateral direction (Fig. 6).
Fig. 5.
Comparison of tML vs tAP between study population and various knee systems.
Fig. 6.
Comparison of tML vs tML/tAP between study population and various knee systems.
8. Discussion
This CT-scan based study of the morphological parameters of distal femur and proximal tibia performed in Indian patients shows that there is a significant difference in the dimensions of male and female patients in the studied patients suggesting the need for gender specific instrumentation and implants in this subset of population. Furthermore, it was observed that only two implant systems closely matched the dimensions of the femur and there was a possibility of significant over and under-coverage of the implant on the resected surfaces resulting in poor functional outcomes in patients undergoing total knee arthroplasty. This study also shows that none of the studied implants system showed appropriate matching of the tibial components to the resected tibial surface necessitating the need for the design of tibial components with appropriate dimensions.
Many previous studies have shown that for the long-term survival of implanted prosthesis following total knee arthroplasty, the dimensions of the prosthesis should match the resected surfaces of tibia and femur in the patients6. Maximal implant coverage on the resected bone surface minimizes the stress applied to the bone implant interface leading to better implant survival4. The anteroposterior diameter of the femoral component is important in determining the flexion-extension space, which in turn determines appropriate tension in the quadriceps mechanism of the knee joint. Any mismatch of the femoral component with the resected femoral surface in anteroposterior direction can result in flexion tightness or anterior knee pain postoperatively due to increased tension in quadriceps mechanism7. The mediolateral dimension of the femoral component is important in determining the adequate coverage of the resected bone surface, tension free wound closure and tension in the collateral ligaments. Mediolateral overhang of the implant can lead to soft tissue irritation and interfere with ligament balancing thereby causing pain and restriction of function8.
This study used a 3D CT image technique for morphological measurements of the tibia and femur in an Indian population. The measurements from the CT images strongly correlate to intraoperative measurements since the 3D CT image of the knee can undergo unconstrained rotation and the correct three-dimensional axis can be determined and maintained9. A comparison of femoral dimensions of our study group with other ethnic groups showed that knees of Indian patients had smaller mediolateral diameter compared to that of Caucasian knees but larger than that of Asian knees whereas the femoral anteroposterior diameter was the smallest among all the compared race groups10, 11, 12, 13. The tibial dimensions of the studied patients were smallest among all studied races suggesting a possibility for frequent femoral and tibial component overhang in Indian patients15,16. Our results are comparable to other studies performed in Indian patients measuring the anthropometry of distal femur and proximal tibia. Vaidya et al.4 performed CT scan based and dry bone measurements in 86 knees and concluded that there is significant mediolateral and anteroposterior mismatch in the dimensions of distal femur and advocated the need for manufacture of femoral component having an anteroposterior diameter of <50 mm and a mediolateral diameter of 54 cm which would suit most anthropometrically smaller Indian patients undergoing TKA. A study by Shah et al.17 using 3D models of the knee in Indian patients showed that Indian patients had similar anthropometric measurements to Asian patients but differed from Caucasian patients which is contrary to the observations in our study which showed a smaller tibial dimension in Indian patients.
This study reinforces the limitations of the use of commercially available implant systems, which have been designed based on the dimensions of Caucasian population and stress the need for the development of implants that suit the dimensions of Indian patients. Furthermore, gender specific designs catering to the female population is important based on the observation of significant differences in the dimensions of male and female knees in the studied population. This can lead to better anatomic conformity of implants leading to reduced stress and better biomechanics and functional outcome.
This study does have some limitations. The sample size of 100 knees is relatively small and a larger sample size involving different high volume centers across the country may result in a more reproducible and conclusive pattern of differences among the gender and ethnic groups. However, the studied patients show an equitable pattern of male and female sexes and decreases the possibility for deviation in the gender specific dimensions. The other limitation is the lack of inclusion of arthritic knees in studied population. However, since the goal of TKA is to reproduce a knee that closely mimics the native knee, the authors believe that the conclusions drawn from this study may help in designing a knee system suited to the needs of Indian patients.
This study concludes that the dimensions of Indian knees are different from other ethnic groups and the use of commercially available knee Implants designed based on measurements in Caucasian populations can lead to significant mismatch between implant and resected bone surfaces. This can lead to less than optimal functional outcomes and therefore there is a need to design ethnic group specific and gender specific knee systems that suit Indian patients.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Seil R., Pape D. Causes of failure and etiology of painful primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:1418–1432. doi: 10.1007/s00167-011-1631-9. [DOI] [PubMed] [Google Scholar]
- 2.Lo C.-S., Wang S.-J., Wu S.-S. Knee stiffness on extension caused by an oversized femoral component after total knee arthroplasty: a report of two cases and a review of the literature. J Arthroplast. 2003;18:804–808. doi: 10.1016/s0883-5403(03)00331-0. [DOI] [PubMed] [Google Scholar]
- 3.Bonnin M.P., Schmidt A., Basiglini L., Bossard N., Dantony E. Mediolateral oversizing influences pain, function, and flexion after TKA. Knee Surg Sports Traumatol Arthrosc. 2013;21:2314–2324. doi: 10.1007/s00167-013-2443-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaidya S.V., Ranawat C.S., Aroojis A., Laud N.S. Anthropometric measurements to design total knee prostheses for the Indian population. J Arthroplast. 2000;15:79–85x. doi: 10.1016/s0883-5403(00)91285-3. [DOI] [PubMed] [Google Scholar]
- 5.Yue Bing, Varadarajan Kartik M., Ai Songtao, Tang Tingting, Rubash Harry E., Li Guoan. Differences of knee anthropometry between Chinese and white men and women. J Arthroplast. 2011 January;26(1):124–130. doi: 10.1016/j.arth.2009.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Incavo S.J., Ronchetti P.J., Howe J.G., Tranowski J.P. Tibial plateau coverage in total knee arthroplasty. Clin Orthop Relat Res. 1994 Feb;(299):81–85. [PubMed] [Google Scholar]
- 7.Kawahara S., Matsuda S., Fukagawa S. Upsizing the femoral component increases patellofemoral contact force in total knee replacement. J Bone Joint Surg Br. 2012;94(1):56–61. doi: 10.1302/0301-620X.94B1.27514. [DOI] [PubMed] [Google Scholar]
- 8.Mahoney O.M., Kinsey T. Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am. 2010;92(5):1115–1121. doi: 10.2106/JBJS.H.00434. [DOI] [PubMed] [Google Scholar]
- 9.Lee I.S., Choi J.A., Kim T.K., Han I., Lee J.W., Kang H.S. Reliability analysis of 16-MDCT in preoperative evaluation of total knee arthroplasty and comparison with intraoperative measurements. AJR Am J Roentgenol. 2006 Jun;186(6):1778–1782. doi: 10.2214/AJR.05.1191. [DOI] [PubMed] [Google Scholar]
- 10.Berger R.A., Rubash H.E., Seel M.J., Thompson W.H., Crossett L.S. Determining therotational alignment of the femoral component in total knee arthroplasty using the epicondylar Axis. Clin Orthop Relat Res. 1993;286:40–47. [PubMed] [Google Scholar]
- 11.Griffin F.M., Math K., Scuderi G.R. Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees. J Arthroplast. 2000;115:354–359. doi: 10.1016/s0883-5403(00)90739-3. [DOI] [PubMed] [Google Scholar]
- 12.Cheng C.K., Lung C.Y., Lee Y.M., Huang C.H. A new approach of designing the tibial base plate of total knee prosthese. Clin Biomech. 1999;14:112–117. doi: 10.1016/s0268-0033(98)00054-0. [DOI] [PubMed] [Google Scholar]
- 13.Urabe K., Miura H., Kuwano T. Comparison between the shape of resected femoral sections and femoral prostheses used in total knee arthroplasty in Japanese patients-simulation using three-dimensional computed tomography. J Knee Surg. 2003;16:27–33. [PubMed] [Google Scholar]
- 14.Mensch J.S., Amstutz H.C. Knee morphology as a guide to knee replacement. Clin Orthop Relat Res. 1975 Oct;(112):231–241. [PubMed] [Google Scholar]
- 15.Uehara K., Kadoya Y., Kobayashi A., Ohashi H., Yamano Y. Anthropometry of the proximal tibia to design a total knee prosthesis for the Japanese population. J Arthroplast. 2002 Dec;17(8):1028–1032. doi: 10.1054/arth.2002.35790. [DOI] [PubMed] [Google Scholar]
- 16.Kwak D.S., Surendran S., Pengatteeri Y.H. Morphometry of the proximal tibia to design the tibial component of total knee arthroplasty for the Korean population. Knee. 2007 Aug;14(4):295–300. doi: 10.1016/j.knee.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Shah D.S., Ghyar R., Ravi B., Shetty V. 3D morphological study of the Indian arthritic knee: comparison with other ethnic groups and conformity of current TKA implant. Open J Rheumatol Autoimmune Dis. 2013;3:263. [Google Scholar]