Abstract
Background
Studies comparing cementless and cemented cups are lacking, especially for revision total hip arthroplasty (THA). The aim of this study was to investigate and compare the differences in implant accuracy between two fixation methods in revision THA.
Methods
We conducted a retrospective study of 85 hips in 70 patients who underwent revision THA using a computed tomography (CT)-based navigation system. Among these, 53 hips underwent cementless THA and 32 hips underwent cemented THA. We measured cup inclination and anteversion using the Kyocera two-dimensional-template with X-ray (Japan-Kyocera, Shiga, Japan) and stem anteversion with CT. We calculated the combined anteversion [cup anteversion+0.7×stem anteversion].
Results
There were no significant differences between the two groups with respect to definitive cup inclination and anteversion. The mean deviations in the inclination and anteversion angle were 40.3 ± 4.3 and 19.6 ± 6.2° in the cementless group and 40.5 ± 3.3 and 17.1 ± 5.1° in the cemented group. There were 11 outliers with respect to the Lewinnek safe zone in the cementless group and two in the cemented group (P = 0.072). Although there was no statistically significant difference, the number of safe zone outliers in the cemented group was less than that in the cementless group.
Conclusion
We conclude that when using a navigation system for revision THA, high precision can be obtained for the cup placement angle with or without cement. However, it seems that a major error in the installation angle of the cup is less likely to occur when using a cemented cup than when using a cementless cup in revision THA with a navigation system.
Keywords: Cemented cup, Cementless cup, CT-Based navigation, Revision THA
1. Introduction
Component malposition in total hip arthroplasty (THA) causes impingement and strains the edge of the bearing surface, potentially leading to dislocation, implant damage, increased abrasion of the bearing surface, and implant loosening.1, 2, 3 Optimal implant alignment is crucial for avoiding such complications; methods such as intraoperative x-ray and guide use have been applied to improve the accuracy of implants. Indexes used to position implants include Lewinnek “safe zone,” which is related to cup inclination,4 and Widmer's “combined anteversion,” which considers the stem.5
Computed tomography (CT)-based navigation is widely recognized as an effective tool for supporting optimal implant alignment. Many reports have examined alignment accuracy in primary THA; results have shown that the use of a navigation system allows accurate implant positioning.6,7 In comparison to primary THA, revision THA involves more factors, such as bone defects, bone fragility, and adhesion of soft tissues, which hinder the reconstruction of a stable hip joint. Furthermore, metal artifacts arising from implants disturb CT scans and make it difficult to accurately depict the bone surface, thus making detailed preoperative planning more challenging. Intraoperative anatomical orientation is also difficult due to factors such as bone defects. The rate of dislocation post revision THA is higher than that post primary THA owing to frequent technical difficulties in reconstruction, such as the adjustment of tension in the soft tissues.8 Navigation has been used to improve implantation accuracy and stability of reconstructed hip joints demonstrating the complications mentioned above. While the reported results have generally been favorable, most of these results were from cementless cups.6,9
Many cases of revision THA involve severe bone defects, which are difficult in terms of anatomical orientation and are also technically demanding. Even surgeons who use cementless cups for primary THA usually find it difficult to achieve stable initial fixation during revision THA; thus, many surgeons inevitably use cemented cups with reinforcement plates. It is more important for revision THA, compared to primary THA, that an appropriate cup be chosen (i.e., cementless or cemented) according to the patient's needs. To ensure accurate cup implantation, especially in revision THA where reconstruction is technically difficult owing to bone defects, the choice between the two major fixation methods (i.e., cementless versus cemented cup implantation) is often made in accordance with the characteristics of the individual case. We conducted revision THA using CT-based navigation and investigated and compared the differences in implant accuracy between the two fixation methods. We were interested to see whether there was a difference in the fixation accuracy of navigation between the two methods.
2. Materials and methods
From February 2010 to October 2016, 110 revision THAs were performed in our hospital. A navigation system was used during revision THAs in all hips (CT-based navigation system; Brain Lab, Japan). We used the navigation system for the cup revision alone. It was not used for femoral stem revisions. We excluded from this series all patients with femoral stem revision alone or those with less than a 1-year follow-up period after surgery. All patients in whom a navigation system was used for revision THA at our institute were targeted in this series. We performed preferential revision THAs using a cementless cup for moderate acetabular bone defects, such as those with an American Academy of Orthopaedic Surgeons [AAOS] Type II or lower acetabular bone defect classification, while preserving the acetabular posterior wall. On the other hand, we used a cemented cup when there were huge acetabular bone defects, which included the acetabular posterior wall such as a Type III or IV AAOS acetabular bone defect classification. The two fixation methods were selectively used during the same period. There were 20 cases of femoral stem revision alone and five cases of liner exchange revision. Therefore, 53 hips underwent cementless revision THA and 32 hips underwent cemented revision THA using a navigational system for cup setting. There were no crossovers between patients in each group. Patient demographics are shown in Table 1. The final diagnoses before revision THA in the cementless group were cup loosening in 39 hips, unknown pain in five hips, bipolar cup disassembly in four hips, infection in two hips, recurrent dislocation in two hips, and pseudotumor in one hip. The diagnoses in the cemented group were cup loosening in 29 hips, infection in two hips, and implant failure in one hip. In the cementless group, there were 44 hips with isolated acetabular component revisions and nine hips with both femoral and acetabular revisions. In the cemented group, there were 18 hips with isolated acetabular component revisions and 14 hips with both femoral and acetabular revisions.
Table 1.
Patient demographic data.
| Patient characteristics | Cementless group (n = 53) | Cemented group (n = 32) | p-value | Statistical power |
|---|---|---|---|---|
| Age | 69.0 ± 10.0 | 72.1 ± 9.8 | 0.448 | 0.27 |
| Sex (female/male) | 44/9 | 27/5 | 0.870 | 0.05 |
| Body mass index (kg/m2) | 25.0 ± 4.1 | 25.0 ± 3.7 | 0.685 | 0.05 |
| Follow-up period (month) | 34.0 ± 22.0 | 42.0 ± 26.0 | 0.774 | 0.31 |
Patients' age, sex, body mass index, and follow-up period were not significantly different between the cementless group and cemented group.
In the cementless group, SQRUM TT (Japan-Kyocera, Shiga, Japan) was used in 16 hips, AMS HA Shell (Japan-Kyocera, Shiga, Japan) in eight, Trident PSL (Stryker Orthopedics, Mahwah, NJ, US) in three, Titanium Acetabular System (Stryker Orthopedics, Mahwah, NJ, US) in five, Continuum Acetabular System (ZimmerBiomet, Warsaw, IN, US) in seven, Ringloc (ZimmerBiomet, Warsaw, IN, US) in six, Reflection SPM (Smith and Nephew, Inc, Memphis, TN, US) in three, Pinnacle (Depuy Synthes, Johnson and Johnson, Warsaw, IN, US) in two, Mallory Head Radial Shell (ZimmerBiomet, Warsaw, IN, US) in two, and Ranawat/Burstein Acetabular Shell (ZimmerBiomet, Warsaw, IN, US) in one hip. In the cemented group, the K-MAX KT plate S + Standard Socket CP (Japan-Kyocera, Shiga, Japan) was used in all hips. There were no patients lost to follow up at 1 year after the surgery; therefore, all patients were evaluated 1 year after surgery.
2.1. Preoperative planning
All patients underwent a CT scan of their hip joints from the iliac crest to the knee joint and through the distal femoral condyles using a 320-row multi-detector helical CT scanner (Aquilion ONE; Toshiba Medical Healthcare, Tochigi, Japan) (detector configuration 80 × 0.5, beam collimation 40 mm) with reconstructed slice widths of 1 mm and slice intervals of 1 mm. The CT data were transferred to the navigation system (VectorVision Compact Hip CT version 3.5.2; Brain Lab, Munich, Germany).
Our goal was to implant the acetabular component at the native acetabulum with an anatomical inclination of 40 ± 10° and an anteversion of 15 ± 10°. In isolated acetabular component revisions, cup anteversion was adjusted according to stem anteversion to prevent postoperative impingement and dislocation. In isolated acetabular component revisions, our goal for combined anteversion was 40–60°. The patients were blinded to the fixation method used for the cup.
2.2. Intraoperative procedures
All surgeries were performed by one senior hip surgeon using a posterolateral approach. We performed the registration process using a CT-based fluoro-matched navigational system prior to surgery. We inserted two screws and placed the antenna on the iliac crest while the patient was in the lateral decubitus position. Next, two fluoroscopic pelvic images taken from different angles of more than 20° were obtained using a mobile fluoroscopy system (Philips BV-29 C-Arm; Koninklijke Philips N.V, Eindhoven, the Netherlands) with the patient in the same position. The fluoroscopic anterior-posterior image included the pubic symphysis, the superior and inferior pubic ramus, and the ischium around the obturator foramen. Surface matching was performed by touching two points: the superior iliac spine and the iliac crest. The position of the pubic symphysis was finely adjusted and calibrated on a computer monitor; the accuracy of calibration was confirmed within 2 mm preoperatively. The cup was placed during surgery after calibration. We used the original cup holder for the cemented cup.
2.3. Postoperative procedures
Cephem antibiotics were usually administered by intravenous injection for 2 days postoperatively, and an antithrombotic drug was used for 10 days postoperatively. In all cases, postoperative X-ray and CT scan were performed 2 weeks after surgery. The cup inclination and anteversion were measured using the Kyocera 2D-template with X-ray, and stem anteversion was measured with a CT scan. The investigator was a medical doctor who had not participated in the treatment of any of the patients. We calculated the combined anteversion of the acetabular cup and femoral stem [cup anteversion+0.7×stem anteversion] at 2 weeks after surgery. Clinical data, such as postoperative complications, were collected up until 1 year after surgery.
2.4. Statistical analysis
Statistical analyses were performed using IBM SPSS® software (Version 25, IBM Corp., Armonk, NY, USA). An unpaired t-test was used to compare the accuracy of cup positioning. We used a χ2 test to compare the planned concordance rate. P < 0.05 indicated statistical significance in all analyses. In addition, we evaluated the statistical power calculation analysis of each result.
All procedures performed in studies involving human participants are in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This retrospective clinical study was approved by the Ethics Committee of XXX University (Approval No. XXX; 18 May 2018), and all patients provided written consent at their final follow-up.
3. Results
Table 2 presents the detailed results of the component-angle analysis. There were no significant differences between the two groups with respect to definitive cup inclination and anteversion. The mean deviations in inclination and anteversion in the cementless group were 40.3 ± 4.3 and 19.6 ± 6.2°, and 40.5 ± 3.3 and 17.1 ± 5.1° in the cemented group. The mean deviation in combined anteversion was 45.5 ± 15.6° in the cementless group and 43.0 ± 11.0° in the cemented group.
Table 2.
Comparison of cementless and cemented group.
| Cementless group (n = 53) | Cemented group (n = 32) | p-value | Statistical power | |
|---|---|---|---|---|
| Cup inclination (degrees) | 40.4 ± 4.3 | 40.5 ± 3.3 | 0.146 | 0.05 |
| Cup anteversion (degrees) | 19.6 ± 6.2 | 17.1 ± 5.1 | 0.202 | 0.49 |
| Combined anteversion (degrees) | 45.5 ± 15.6 | 43.0 ± 11.0 | 0.315 | 0.13 |
| Incidence of outliers | 20.75% (11/53) | 6.25% (2/32) | 0.072 | 0.43 |
| Postoperative dislocation rate | 3.8% (2/50) | 3.1% (1/32) | 0.875 | 0.05 |
Cup inclination or anteversion, combined anteversion, incidence of outliers, and dislocation rates after surgery were not significantly different between the cementless and cemented groups.
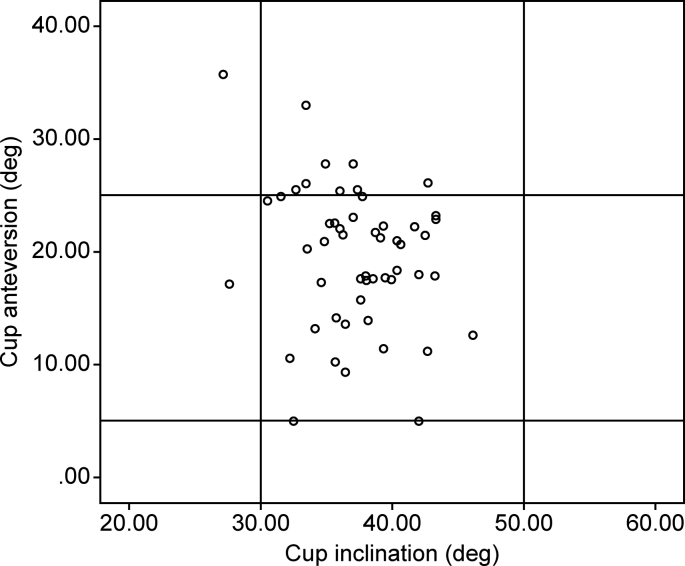
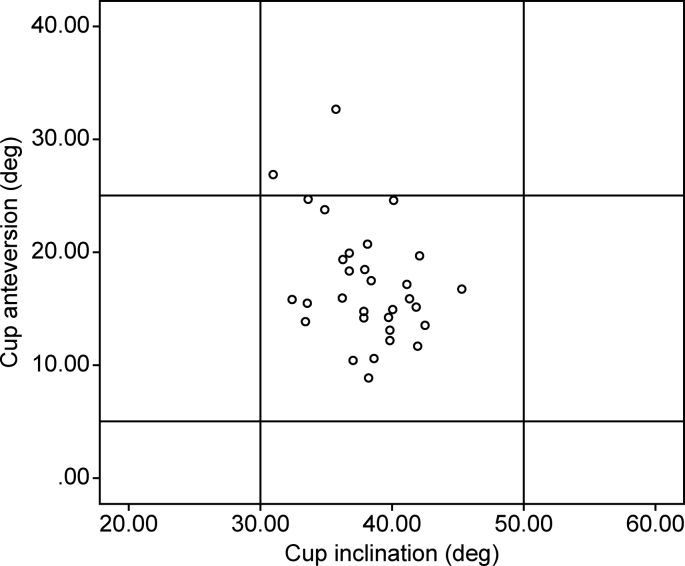
There were 11 outliers with respect to the safe zone in the cementless group (Fig. 1) and two outliers in the cemented group (Fig. 2) (P = 0.072). The incidence of outliers was 20.75% (11/53) in the cementless group and 6.25% (2/32) in the cemented group. The statistical power of the outliers was 0.43.
Fig. 1.
The mean deviations in inclination and anteversion in the cementless group were 40.3 ± 4.3° and 19.6 ± 6.2°. Outliers of the safe zone in the cementless group included 11 hips.
Fig. 2.
The mean deviations in inclination and anteversion in the cemented group were 40.5 ± 3.3° and 17.1 ± 5.1°. Outliers of the safe zone in the cemented group included two hips.
Postoperative dislocation occurred in two hips in the cementless group and in one hip in the cemented group. Since each dislocation was single, there were no cases of recurrent dislocation. One hip was infected in the cementless group; however, it subsided with debridement and irrigation while preserving the implants. There was no incidence of significant thrombosis with symptoms, re-revision surgery, or death after surgery in either group.
4. Discussion
Favorable implant accuracy in primary THA using CT-based navigation was reported by Kalteis et al.,9 who conducted a randomized controlled trial in which 90 primary THA patients were assigned to CT-based navigation, imageless navigation, or a freehand technique. In the CT-based navigation group, 25/30 acetabular components were within Lewinnek safe zone versus 28/30 in the imageless navigation group and 14/30 in the freehand group; the standard deviations for inclination and anteversion were optimal in the CT-based navigation group. However, this study was conducted with cementless cups only.
Only one study compared the implant accuracy between cementless and cemented cups in primary THA using navigation. Chawda et al.10 reported that with cementless cups, 4/20 cups deviated from the target inclination by ≥ 5°, while 7/20 cups deviated from the target version by ≥ 5°; however, none of the cemented cups deviated from the target inclination or version by ≥ 5°. Thus, cup position was more accurate with cemented cups. Although this study is significant in that it is the first study on the combination of cemented cups and navigation in THA, the study only involved primary THA, which features relatively few obstacles in implant positioning. In addition, the sample size was relatively small.
In the Japanese Arthroplasty Register for THA,11 cemented cups have been used in 19.0% of primary THA cases versus 43.4% of revision THA cases. Similar results are observed in the Italian THA registry where cemented cups have been used in 1.3% of primary THA cases versus 9.5% of revision THA cases.12 These results demonstrate that many surgeons, even those who prefer to use cementless cups in primary THA, tend to use cemented cups in revision THA. Chalmers et al.13 used cement to fix dual-mobility cups in 18 patients with recurrent dislocation of THA performed with cementless cups. In addition, Fink et al.14 used cementless cups for six joints and cemented cups for 29 joints requiring revision THA due to infection. Waddell et al.15 reported favorable outcomes for revision THA with impaction bone grafting and cementless cups for cases of major bone defects. On the other hand, Beckmann et al.16 demonstrated that cementless cups with 3D porous structures yielded more favorable outcomes for AAOS Type IV pelvic discontinuity with bone defects than cemented cups and reinforcement plates. In revision THA for dislocation or infection, particularly in revision THA cases with advanced bone defects, the choice between fixation with a cementless cup versus a cemented cup is often made depending on the characteristics of the individual case. Revision THA not only involves difficult surgical techniques but also sometimes features bone defects and soft tissue adhesion, which are rare in primary THA; therefore, it is especially important in revision THA to determine whether fixation with cementless cups versus cemented cups results in differences in navigation-assisted implant accuracy.
Few studies exist on the implant accuracy and dislocation rates in revision THA using navigation. Nakamura et al.17 and Kuroda et al.18 achieved registration accuracy in revision THA on par with that in primary THA using CT-based navigation. In addition, Chang et al.19 achieved cup inclination and combined anteversion in the safe zone in 100% of cases. Yun et al.20 also achieved a high target implant accuracy in all 12 cases in their study. In these studies, only cementless cups were used; no studies have demonstrated the differences in implant accuracy between the cementless and cemented cups.
The present study is the first study to compare cementless and cemented cups in revision THA using a navigation system with a large sample size. Favorable implant accuracy was achieved both with cementless cups and cemented cups. Since this study included revision THA with stem retention, the accuracy of combined anteversion was more valuable than that of cup anteversion. Although there was no significant difference between the two fixation methods, the p value was 0.072 and the statistical power was 0.43 when comparing the incidence of outliers in both groups. This meant that an increase in the number of cases might indicate a significant difference between the groups in the incidence of outliers, and cemented cups may be located more accurately in the safe zone. When implanting a cemented cup, there is a working time until the cement hardens. During this time, fine adjustments to the cup position can be made by checking the digital readout on the navigation screen. In contrast, cementless cups achieve favorable fixation with a press-fit; this press-fit is instantaneous, injures bone and soft tissue, may result in deviation from the desired position, and leaves almost no working time for micro adjustments. In revision THA, where acetabular bone defects are often observed, press-fitting sometimes fails to yield sufficient cup fixation. It is conceivable that the cup may slip out of position when turning the screw used to supplement fixing strength. Therefore, it is likely that we could more readily avoid accidental errors in cup installation when using cemented cups rather than cementless cups in revision THA with a navigation system.
It should be noted that there are some drawbacks to the CT-based navigation system for revision THA such as radiation exposure, increased preparation time, a skin incision for installation of an antenna at the registration before surgery, and the expense. The limitations of the present study include the following: it was not randomized and the sample sizes were different; both isolated acetabular revision and total (both femoral and acetabular) revision were included; and the follow-up period was short, thus precluding clinical assessment. The postoperative observation period was too short to evaluate the accuracy of cup placement and the risk of early dislocation. In consideration of the combination with femoral stem preservation, we were forced to use various kinds of cups in order to select a cup suitable for the preserved femoral stem. Conducting a randomized study is often difficult during treatment in the surgical field. This study included the largest number of cases reporting the use of a navigational system during revision THA. However, a greater number of cases are needed in the future to clarify the characteristics of the two groups with or without cement in revision THA using a navigation system.
5. Conclusion
This is the first study to compare cementless and cemented cups in revision THA using a navigation system with a large sample size. In the present study, we revealed that a favorable cup placement angle can be obtained with or without cement using a navigation system for revision THA, similar to that observed in primary THA. While there was no significant difference in the installation angle between cementless and cemented cups, cemented cups tended to yield more favorable outcomes in terms of the incidence of outliers. Therefore, it seems that a major error in the installation angle of the cup is less likely to occur when using a cemented cup than when using a cementless cup in revision THA with a navigation system.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations of interest
None.
Acknowledgments
None.
References
- 1.Shon W.Y., Baldini T., Peterson M.G., Wright T.M., Salvati E.A. Impingement in total hip arthroplasty a study of retrieved acetabular components. J Arthroplast. 2005;20:427–435. doi: 10.1016/j.arth.2004.09.058. [DOI] [PubMed] [Google Scholar]
- 2.Worblewski B.M., Siney P.D., Fleming P.A. Effect of reduced diameter neck stem on incidence of radiographic cup loosening and revision in Charnley low-frictional torque arthroplasty. J Arthroplast. 2009;24:10–14. doi: 10.1016/j.arth.2008.01.312. [DOI] [PubMed] [Google Scholar]
- 3.Barrack R.L., Burak C., Skinner H.B. Concerns about ceramics in THA. Clin Orthop Relat Res. 2004;429:73–79. doi: 10.1097/01.blo.0000150132.11142.d2. [DOI] [PubMed] [Google Scholar]
- 4.Lewinnek G.E., Lewis J.L., Tarr R., Compere C.L., Zimmerman J.R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 5.Widmer K.H., Majewski M. The impact of the CCD-angle on range of motion and cup positioning in total hip arthroplasty. Clin Biomech. 2005;20:723–728. doi: 10.1016/j.clinbiomech.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Kitada M., Nakamura N., Iwana D., Kakimoto A., Nishii T., Sugano N. Evaluation of the accuracy of computed tomography-based navigation for femoral stem orientation and leg length discrepancy. J Arthroplast. 2011;26:674–679. doi: 10.1016/j.arth.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Iwana D., Nakamura N., Miki H., Kitada M., Hananouchi T., Sugano N. Accuracy of angle and position of the cup using computed tomography-based navigation systems in total hip arthroplasty. Comput Aided Surg. 2013;18:187–194. doi: 10.3109/10929088.2013.818713. [DOI] [PubMed] [Google Scholar]
- 8.Lachiewics P.T., Soileau E., Ellis J. Modular revision for recurrent dislocation of primary or revision total hip arthroplasty. J Arthroplast. 2004;19:424–429. doi: 10.1016/j.arth.2003.12.077. [DOI] [PubMed] [Google Scholar]
- 9.Kalteis T., Handel M., Bäthis H., Perlick L., Tingart M., Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg Br. 2006;88:163–167. doi: 10.1302/0301-620X.88B2.17163. [DOI] [PubMed] [Google Scholar]
- 10.Chawda M., Hucker P., Whitehouse S.L., Crawford R.W., English H., Donnelly W.J. Comparison of cemented vs uncemented acetabular component positioning using an imageless navigation system. J Arthroplast. 2009;24:1170–1173. doi: 10.1016/j.arth.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Akiyama H., Hoshino A., Iida H. A pilot project for the Japan arthroplasty register. J Orthop Sci. 2012;17:358–369. doi: 10.1007/s00776-012-0229-5. [DOI] [PubMed] [Google Scholar]
- 12.Regional Register of Orthopaedic Prosthetic Implantology Hip, knee, and shoulder arthroplasty in Emilia-Romagna Region (Italy) 2017. https://ripo.cineca.it/
- 13.Chalmers B.P., Ledford C.K., Taunton M.J., Sierra R.J., Lewallen D.G., Trousdale R.T. Cementation of a dual mobility construct in recurrently dislocating and high-risk patients undergoing revision total arthroplasty. J Arthroplast. 2018;33:1501–1506. doi: 10.1016/j.arth.2017.11.055. [DOI] [PubMed] [Google Scholar]
- 14.Fink B., Schlumberger M., Oremek D. Single-stage acetabular revision during two-stage THA revision for infection is effective in selected patients. Clin Orthop Relat Res. 2017;475:2063–2070. doi: 10.1007/s11999-017-5334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waddell B.S., Della Valle A.G. Reconstruction of non-contained acetabular defects with impaction grafting, a reinforcement mesh and a cemented polyethylene acetabular component. Bone Joint Lett J. 2017;99-B(1 Supple A):25–30. doi: 10.1302/0301-620X.99B1.BJJ-2016-0322.R1. [DOI] [PubMed] [Google Scholar]
- 16.Beckmann N.A., Weiss S., Klotz M.C., Gondan M., Jaeger S., Bitsch R.G. Loosening after acetabular revision: comparison of trabecular metal and reinforcement rings. A systematic review. J Arthroplast. 2014;29:229–235. doi: 10.1016/j.arth.2013.04.035. [DOI] [PubMed] [Google Scholar]
- 17.Nakamura N., Nishii T., Kitada M., Iwana D., Sugano N. Application of computed tomography-based navigation for revision total hip arthroplasty. J Arthroplast. 2013;28:1806–1810. doi: 10.1016/j.arth.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 18.Kuroda K., Kabata T., Maeda T. The value of computed tomography-based navigation in revision total hip arthroplasty. Int Orthop. 2014;38:711–716. doi: 10.1007/s00264-013-2166-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang J.D., Kim I.S., Prabhakar S., Mansukhani S.A., Lee S.S., Yoo J.H. Revision total hip arthroplasty using imageless navigation with the concept of combined anteversion. J Arthroplast. 2017;32:1576–1580. doi: 10.1016/j.arth.2016.12.030. [DOI] [PubMed] [Google Scholar]
- 20.Yun H.H., Yoon J.R., Yu J.J., Seo H.S. Navigated acetabular cup fixation for acetabular deformity or revision total hip arthroplasty. Hip Pelvis. 2014;26:150–156. doi: 10.5371/hp.2014.26.3.150. [DOI] [PMC free article] [PubMed] [Google Scholar]