Abstract
Background
The aim of this study was to compare the functional outcome, the patient’s perception of the replaced hip joint with different bearing surfaces and to study the effect of femoral head size on joint perception as well.
Methods
One hundred and ten (110) patients, who underwent primary total hip replacement with an average follow-up of 48 months (12–156 months), were assessed for their functional outcome and joint perception. The functional outcome was calculated based on Oxford hip score (OHS) and SF-36. Joint perception was categorized as to whether the replaced joint was perceived like a natural joint or artificial joint with or without restriction of movements.
Results
There were 50 patients operated for ceramic on ceramic (CoC-hard-on-hard bearing), 60 patients for hard-on-soft bearing (Metal on Polyethelene-MoP 46, Ceramic on Polyethelene-CoP 14). Most of the patients with hard-on-hard bearings perceived their operated hip like a natural joint (p = 0.04) compared to hard-on-soft bearings. There was no significant difference in the functional outcome (OHS, SF-36) between the two bearing surface groups (p > 0.05). There were fifty patients with 28 mm size head while remaining 60 had larger heads (>32 mm). Patients with large heads felt like natural joint compared to small heads (p = 0.007).
Conclusion
The hard-on-hard bearing surfaces (CoC) and large femoral heads (32 mm, 36 mm) are perceived more like a natural joint. Different bearing surfaces do not affect the functional outcome after total hip replacement in a medium term follow up.
Keywords: Total hip arthroplasty, Bearing surface, Patient satisfaction, Functional outcome
1. Introduction
The bearing surfaces currently used for Total Hip Arthroplasty (THA) are Ceramic-on-ceramic (CoC), Ceramic-on-Polyethylene (CoP), Metal-on-Polyethylene (MoP) and Metal-on-metal (MoM). The success of the THA surgery depends on improvement in functional outcome and better patient satisfaction. Most of the design changes over the past two decades are focused on altering the bearing surface of the implant system for reducing wear and achieve better patient satisfaction. There are very few studies published until now comparing the functional outcomes of THA using different bearing surfaces. Most of the studies on bearing surfaces are concerned with wear of the implant, post-operative complications and the need for revision surgery.1,2 In all these studies the functional outcome is measured based on the standardized scoring systems. These scoring systems take into account the patient’s pain relief, level of activity and range of motion but do not consider the patient’s joint perception. Though the scoring system highlights most of the activity levels, the patient satisfaction outcome is not clear from their scores. Assessment of joint perception forms a major component of patient satisfaction after THA. The success of the surgery depends on the patient perception of the joint, so that he/she forgets the artificial joint to feel it like a natural joint. Though there are studies in literature comparing joint perception in total hip and knee replacements,3 no study compares the patient’s joint perception in total hip arthroplasty between the different bearing surfaces.
We have studied the effect of different bearing surfaces on patient’s functional outcome and tried to establish a correlation with joint perception after total hip replacement. We have also studied the effect of the head size on joint perception after total hip replacement.
2. Materials and methods
The patients who have undergone primary total hip replacement with minimum one-year follow-up were included in the study. Only those patients operated by primary author were included in the study. All patients had THA done via posterolateral approach in lateral position. Standard steps of total hip replacement procedure was followed. All uncemented cups were cluster hole porous coated cups. Screws were used as and when stability could not be achieved in any direction. All cementless stems were fully HA coated stems. Cemented stems were triple tapered polished stems and cemented cups were flanged all poly cups. Third generation cementing technique was followed. Full weight bearing walking with support was started 24 h after surgery in all cases irrespective of fixation. The support was gradually weaned of next few weeks as per patient’s recovery. Patients undergoing revision THA, with post-operative nerve palsy or infection and those with primary joint replacements other than hip were excluded from study. The information regarding bearing surface, head and cup size used was obtained from the hospital records and principal investigator records. Antero-posterior and lateral view of the hip was taken. The following parameters were looked for in the radiograph, 1) Inclination of the cup 2) Anteversion of cup, 3) Heterotopic ossification (Brooker grading4), 4) Peri-implant radiolucent lines and Osteolysis (Charnley zones,5 Gruen zones6). The functional outcome of the patient was assessed using 2 standardized scoring systems (a) Oxford Hip score7 and (b) SF-36 score. Based on the Oxford Hip Score outcome was classified as excellent, good, fair and poor.8
To assess the patient’s joint perception, the patient was asked to answer the following question. ‘How do you perceive your operated hip joint?’ and the response was graded as follows:
-
1.
Like a native or natural joint
-
2.
Like an artificial joint with no restriction
-
3.
Like an artificial joint with minimal restriction
-
4.
Like an artificial joint with major restriction
-
5.
Like a nonfunctional joint.
2.1. Statistical analysis
The outcome of our study was based on ordinal scale (joint perception) and rank (OHS, SF36 score). The outcomes had a clear limit of detection (OHS 0–48, SF-36 0–100). Non-parametric tests were applied to the data. P-Value < 0.05 was considered significant. The joint perception of each patient was compared between the groups using the Fischer Exact test. The SF-36 score (0–100) and Oxford hip score (0–48) were compared between the groups with Kruskal Wallis H test.
3. Results
The study population included 110 patients who were operated between 2004 and 2017, and included 78 males and 32 females after applying exclusion criteria. The average age was 47.33 years (25–78 years). Twenty-seven (24.5%) patients belonged to the young population group with age less than 35 years.9 The mean follow-up duration was 48 months (12–156 months). The primary diagnosis was avascular necrosis in 61 patients, inflammatory arthritis in 26 patients and dysplastic hip in 5 patients. The remaining 18 patients had THA done for hip fractures. 102 patients had uncemented hip replacements while only 8 patients had cemented hip replacements. The range of acetabulum inclination angle was 30–55°, while the version was between 10 and 25° in all cases.
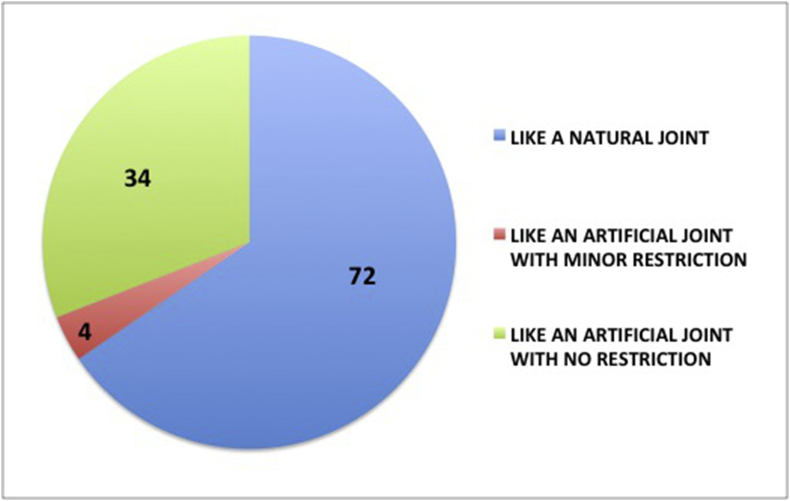
There were 50, 14 and 46 patients with CoC, CoP and MoP articulation respectively while there were no patients with MoM. To prevent skewing of data, CoP and MoP were grouped together as hard-on-soft bearings while CoC and MoM were grouped as hard-on-hard bearings. There were 50 patients with hard-on-hard bearing (CoC) whereas 60 with hard-on-soft (MoP, CoP). CoC group was dominated by younger patients (mean age 37.8 years) compared to MoP (mean age 55.7 years) and CoP (mean age 53.7 years). Fifty patients had 28 mm head size, while the remaining 60 patients had more than 32 mm (32, 36 or 40 mm). For statistical purposes 28 mm was taken as small head and 32 mm, 36 mm and 40 mm were grouped together as large heads. The patient’s perception of replaced joint is shown in Fig. 1.
Fig. 1.
Joint perception of all patients
3.1. Bearing surface and joint perception
Thirty-eight (76%) out of 50 patients with hard-on-hard bearing surface felt ‘like a natural joint’ while only 34 (56.7%) out of 60 patients with hard-on-soft bearing surface felt the same. The difference was found to be significant (p = 0.03), which shows hard-on-hard bearing surfaces are perceived more like a natural joint than hard-on-soft bearing surfaces (Table 1).
Table 1.
Comparision between bearing surface and joint perception.
| Bearing surface | Total | Joint perception |
|||||
|---|---|---|---|---|---|---|---|
| Like a native or natural joint | Like an artificial joint with no restriction of motion | Like an artificial joint with minimal restriction | |||||
| COC | 50 | Hard-on-hard | 50 | 38 (76%) | 12 (24%) | 0 | p value 0.03 |
| MOM | 0 | ||||||
| COP | 14 | Hard-on-soft | 60 | 34 (57%) | 22 (37%) | 4 (6%) | |
| MOP | 46 | ||||||
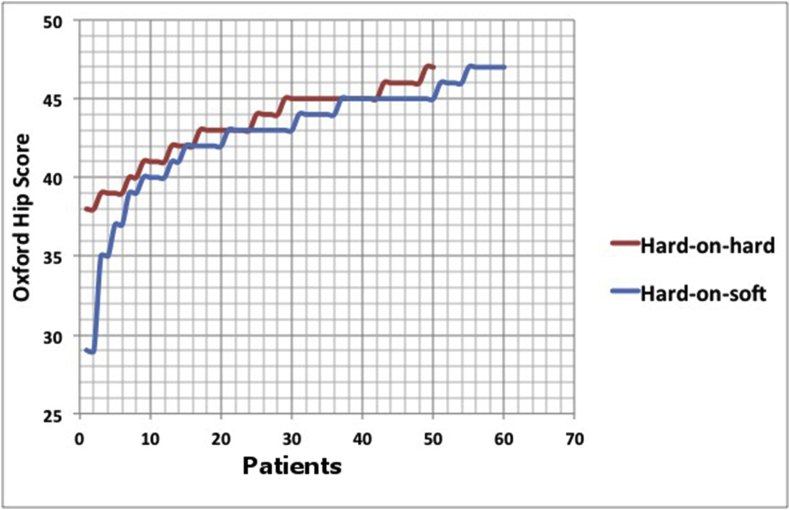
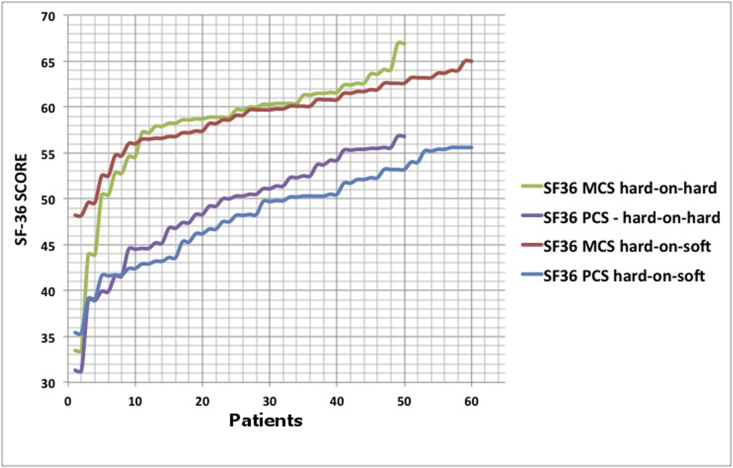
3.2. Functional outcome and bearing surfaces
Thirty eight (76%) patients with hard-on-hard bearing surface and 46 (77%) patients with hard-on-soft bearing surface had excellent outcomes with OHS score more than 418. There was no significant difference (p = 0.81) in the Oxford hip score between the 2 groups. The mean Physical component score (PCS) for the 2 groups were 48.89 and 48.37 (p = 0.31), while the mean Mental component score (MCS) was 57.93 and 59.06 (p = 0.78) respectively. Hence it was revealed that there was no significant difference in the SF-36 scores of both the groups as well. Thus for a short to mid-term follow-up period, there is no significant difference in functional outcome between the different bearing surfaces (Table 2) (Fig. 2, Fig. 3).
Table 2.
Functional outcome in different bearing surfaces.
|
Bearing surface |
Oxford hip score |
Sf 36 |
|||||
|---|---|---|---|---|---|---|---|
| 0–26 |
27–33 |
34–41 |
42–48 |
Mean | Mean PCS | Mean MCS | |
| Poor | Fair | Good | Excellent | ||||
| Hard-on-hard | 0 | 0 | 12 | 38 | 43.2 | 48.89 | 57.93 |
| Hard-on-soft | 0 | 2 | 12 | 46 | 42.73 | 48.37 | 59.06 |
| p-value | 0.8102 | 0.31 | 0.78 | ||||
Fig. 2.
Graph showing Oxford Hip Score of patients with Hard-on-hard and hard-on-soft bearings.
Fig. 3.
Graph showing SF36 scores of patients with hard-on-hard and hard-on-soft bearings.
3.3. Head size and joint perception
Twenty-six (52%) patients with smaller head (28 mm) felt like a natural joint, while 46 (76.7%) patients with large head (32 mm, 36 mm, 40 mm) felt like a natural joint. Hence there is a significant effect of head size on joint perception with larger heads being perceived more like natural joint than smaller heads (p = 0.007) (Table 3).
Table 3.
Effect of head size on joint perception.
| Size of head | Like a natural joint | Like an artificial joint with no restriction | Like an artificial joint with minimal restriction |
|---|---|---|---|
| 28 mm | 26 | 20 | 4 |
| ≥32 mm | 46 | 14 | 0 |
| p= 0.007 | |||
4. Discussion
The total sample size of our study was 110 patients with 78 males (70.1%) and 32 (29.1%) females. Indian Society of Hip and Knee Surgeons (ISHKS) joint registry report shows that 61% of the THA is done in males.10 The mean age of the patients in our study was 47.33 (±14.1) years, which is similar to the ISHKS registry data, which shows average age of patient undergoing THA in India is 52 years.10
Majority (65.5%) of the patients in our study felt that their operated joint was like a natural joint. No patient felt that the joint was like an artificial joint with major restriction or like a non-functional joint. These results are similar to that of Collins et al. (2012), which showed that hip arthroplasties are associated with better joint perception than knee arthroplasties.3 They developed a questionnaire evaluating patient’s joint perception after arthroplasty to determine whether they considered the joint as ‘natural’ or ‘artificial’. They also concluded that joint perception was strongly correlated with the functional outcome in all their study groups.
Patients with hard-on-hard bearing (CoC) perceived their joint more like a natural joint than hard-on-soft (CoP, MoP) group (p = 0.03). This could be attributed to the hydrodynamic lubrication seen in hard-on-hard bearings. The native hip joints (synovial joints) have full fluid film type of lubrication (hydrodynamic lubrication). Metal-on-polyethylene hip joints (hard-on-soft) articulate in the mixed film or boundary lubrication regime. It is not ideal and is more likely to occur in rough bearing surfaces, or as a result of third body formation or protein deposition. The longer the implants remain in situ the more likely these develop this type of lubrication. Hard-on-hard bearings primarily work in the elastohydrodynamic (fluid film) and mixed film lubrication regime, with increasing femoral head size (>28 mm), a shift toward full fluid film (hydrodynamic) lubrication is observed as well. The coefficient of friction is very less in full fluid film lubrication where the articulating surfaces are separated by the lubricant.11 Thus the hard-on-hard surfaces with lubrication regime similar to that of natural joint are perceived more like a natural joint.
The better joint perception for ceramic-on-ceramic could also be due to decreased wear and osteolysis. The potential for decreased wear is derived from the tribologic properties inherent to alumina. Alumina is highly polished, very hard, scratch resistant and has better wettability. The fluid film that develops on ceramic surfaces decreases frictional drag and adhesive wear. The low wear rates coupled with less alumina bioreactivity minimize the likelihood of osteolysis.
All the patients of our study had good functional outcome. The average Oxford hip score was 42.98, while the average for hard-on-hard bearings was 43.2 and for the hard-on-soft group was 42.7. Jafar et al. (2015) studied 60 patients undergoing primary THR, and showed that all patients had excellent improvements in functional outcome after the surgery.12 The average pre-operative Harris hip score was 23.77 while the average post-operative score was 87.90 after one-year follow-up. Ng CY et al. (2007) studied the functional outcome of 627 consecutive patients undergoing primary total hip replacement in terms of Harris hip score and SF-36 score.13 They showed that there was a significant improvement in both the scores in the post-operative period. All dimensions of the SF-36 except for mental health and general health improved significantly with the greatest improvement seen at six-month assessment.13
There was no significant difference in the functional outcome between the bearing surfaces as measured by the Oxford hip score and SF-36 in our study. Several studies have been done in the past, which show similar result. Parsons C et al. (2014) compared the clinical outcomes of three bearing surfaces (MoM, MoP, CoP).14 They studied the outcome of 81 primary THA patients with an average follow-up of 8.6 years. They concluded that the rates of pain, complications and need for revision secondary to articular wear are similar among the 3 bearing surfaces compared.14 Dongcai et al., in 2015 did a meta-analysis of randomized controlled trials to compare the outcome of ceramic-on-ceramic and metal-on-polyethylene bearing surfaces.2 There was no difference in functional outcome as measured by Harris hip score between the 2 groups. There was decreased rate of revision in the COC group (Table 4).
Table 4.
Studies comparing functional outcome in different bearing surfaces.
| Study | No of patients | Bearing surfaces | Variables | P value |
|---|---|---|---|---|
| D’Antonio et al.15 | 189 (216 hips) | CoC (144), MoP (72) | Osteolysis and revision rate (MoP > CoC) | <0.05 |
| Vendittoli et al.16 | 140 | CoC (71), MoP (69) | Functional outcome (WOMAC, PMA scale) | >0.05 |
| Osteolysis and revision (MoP > CoC) | <0.05 | |||
| Parsons C et al.14 | 81 | MoM (18), MoP (27), CoP (36) | Functional outcome (harris hip score) | >0.05 |
| Complication rate | >0.05 | |||
| Osteolysis | >0.05 | |||
| Dongcai et al.2 | 974 | CoC (601), MoP (373) | Harris hip score | 0.13 |
| Revision rates (MoP > CoC) | 0.01 | |||
| Implant fracture (CoC > MoP) | 0.04 | |||
| Osteolysis (MoP > CoC) | <0.01 | |||
| Wang et al.17 | 90 | COC | Functional outcome (harris hip score) | <0.05 |
| Present study | 110 | CoC (50), MoP (46), CoP (14) | Functional outcome (Oxford hip score, SF-36) | >0.05 |
No studies have been done previously to study the effect of femur head size on joint perception. Our study shows that larger heads (>32 mm) are perceived more like a natural joint (p: 0.007). The better joint perception for larger heads can be attributed to the better stability and impingement free range of motion.18,19 There is a clear kinematic advantage to larger femoral head bearings in THA. Increasing the femoral head size leads to an increased head–neck ratio, which results in increased amount of flexion and flexion with internal rotation of the hip. Even with some variability in acetabular component position, the range of motion before impingement is increased with larger femoral heads. The jump distance is increased by a head with a large diameter, reducing the risk of postoperative dislocation, even when utilizing a posterior approach to the hip. However, large diameter heads do have more volumetric wear, which may or may not cross the threshold for osteolysis.20
Our study has its limitations. The average follow-up of our study population is 48 months. Only the short to medium term results on functional outcome could be studied. Long-term follow-up is required to study further complications like osteolysis and loosening. The study population was 110 patients. Larger study group would further increase the power of the study. However our study is still significant as it is one of the first studies done to study the role of bearing surface on joint perception and patient satisfaction.
We conclude that bearing surface do play a role in patient satisfaction outcome after total hip replacement. Patients with hard-on-hard bearings (CoC) and large head diameters perceived their operated hip like a native joint. However the bearing surfaces did not affect the functional outcome of the patient.
Ethics statement
This study was conducted after approval by Institutional Ethics Committee. Informed written consent was obtained from all study participants.
Declaration of competing interest
All the authors declare no conflicts of interest.
Acknowledgement
Nil.
Contributor Information
Shubhranshu S. Mohanty, Email: drssmohanty@hotmail.com.
Hariharan Mohan, Email: hariharan274@gmail.com.
Tushar N. Rathod, Email: tnrathod@gmail.com.
Prashant Kamble, Email: dr.prashantkamble@gmail.com.
References
- 1.Mariconda Massimo, Galasso Olimpio, Costa Giovan Giuseppe, Recano Pasquale, Cerbasi Simone. Quality of life and functionality after total hip arthroplasty: a long-term follow-up study. BMC Muscoskelet Disord. 2011;12:222. doi: 10.1186/1471-2474-12-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hu Dongcai, Tie K., Yang X., Tan Y., Alaidaros M., Chen L. Comparison of ceramic-on-ceramic to metal-on-polyethylene bearing surfaces in total hip arthroplasty: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2015;10:22. doi: 10.1186/s13018-015-0163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collins M., Lavigne M., Girard J., Vendittoli P.A. Joint perception after hip or knee replacement surgery. Orthop Traumatol Surg Res. 2012;98:275–280. doi: 10.1016/j.otsr.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 4.Brooker A.F., Bowerman J.W., Robinson R.A., Riley L.H. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 5.Delee J.G., Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 6.Gruen T.A., Mcneice G.M., Amstutz H.C. Modes of failure of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 7.Dawson J., Fitzpatrick R., Carr A., Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996 Mar;78(2):185–190. [PubMed] [Google Scholar]
- 8.Murray D.W., Fitzpatrick R., Rogers K. The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007 Aug;89(8):1010–1014. doi: 10.1302/0301-620X.89B8.19424. PubMed PMID: 17785736. [DOI] [PubMed] [Google Scholar]
- 9.Petry N.M. A comparison of young, middle-aged, and older adult treatment-seeking pathological gamblers. Gerontol. 2002 Feb;42(1):92–99. doi: 10.1093/geront/42.1.92. PubMed PMID: 11815703. [DOI] [PubMed] [Google Scholar]
- 10.Pachore J.A., Vaidya S.V., Thakkar C.J., Bhalodia H.K., Wakankar H.M. ISHKS joint registry: a preliminary report. Indian J Orthop. 2013 Sept;47(5):505–509. doi: 10.4103/0019-5413.118208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hosseinzadeh Hamid Reza Seyyed, Eajazi Alireza, Shahi Ali Sina. The bearing surfaces in total hip arthroplasty – options, material characteristics and selection. In: Samo Fokter Dr., editor. Recent Advances in Arthroplasty. 2012. 978-953-307-990-5. [Google Scholar]
- 12.Jafar Osama, Aziz-ur-rehman, Kaleem shaukat M. vol. 6. July-September 2015. (Functional Outcome of Total Hip: JUMDC). Issue 3. [Google Scholar]
- 13.Ng C.Y., Ballantyne J.A., Brenkel I.J. Quality of life and functional outcome after primary total hip replacement. J Bone Jt Surg Br Vol. 2007;89-B:868–873. doi: 10.1302/0301-620X.89B7.18482. [DOI] [PubMed] [Google Scholar]
- 14.Parsons Christopher, Ryan Batson, Reighard Shane, Tanner Stephanie, Snider Becky, Pace Thomas B. Clinical outcomes assessment of three similar hip arthroplasty bearing surfaces. Orthop Rev. 2014;6:5334. doi: 10.4081/or.2014.5334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.D’Antonio J.A., Capello W.N., Naughton M. Ceramic bearings for total hip arthroplasty have high survivorship at 10 years. Clin Orthop Relat Res. 2012;470(2):373–381. doi: 10.1007/s11999-011-2076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vendittoli P.A., Rivière C., Lavigne M., Lavoie P., Alghamdi A., Duval N. Alumina on alumina versus metal on conventional polyethylene : a randomized clinical trial with 9 to 15 years follow-up. Acta Orthop Belg. 2013;79:181–190. [PubMed] [Google Scholar]
- 17.Wang Tao, Sun Jun-Ying, Zhao Xi-Jiang, Liu Yong, Yin Hai-bo. Ceramic-on-ceramic bearings total hip arthroplasty in young patients. Arthroplast Today. December 2016;2(4):205–209. doi: 10.1016/j.artd.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jameson S.S., Lees D., James P. Lower rates of dislocation with increased femoral head size after primary total hip replacement: a five-year analysis of NHS patients in England. J Bone Jt Surg Br Vol. 2011;93(7):876–880. doi: 10.1302/0301-620X.93B7.26657. [DOI] [PubMed] [Google Scholar]
- 19.Byström S., Espehaug B., Furnes O., Havelin L.I. Femoral head size is a risk factor for total hip luxation: a study of 42,987 primary hip arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop Scand. 2003 Oct;74(5):514–524. doi: 10.1080/00016470310017893. [DOI] [PubMed] [Google Scholar]
- 20.Barnes C.L. Wear performance of large-diameter differential-hardness hip bearings. J Arthroplast. 2008;23(6):56–60. doi: 10.1016/j.arth.2008.05.021. Suppl. 1. [DOI] [PubMed] [Google Scholar]