Abstract
Purpose
Periprosthetic fractures around total knee arthroplasty are relatively rare complication comprises to 0.3–2.5%. But these injuries are often complex and challenging for the surgeons due to ageing population in conjunction with severe osteoporosis. The management option varies from conservative to internal fixation or revision surgery. Thus this study was conducted to analyze the results of various methods of treatment of periprosthetic fractures following TKA and to form the optimal treatment guidelines for fixation or revision.
Material and methods
51 cases diagnosed with periprosthetic fracture were enrolled and underwent surgical intervention. Type of primary prosthesis, interval between TKA and periprosthetic fracture, type of fracture, prosthesis stability and mode of fixation of fracture, any revision surgery and complication were noted.
Results
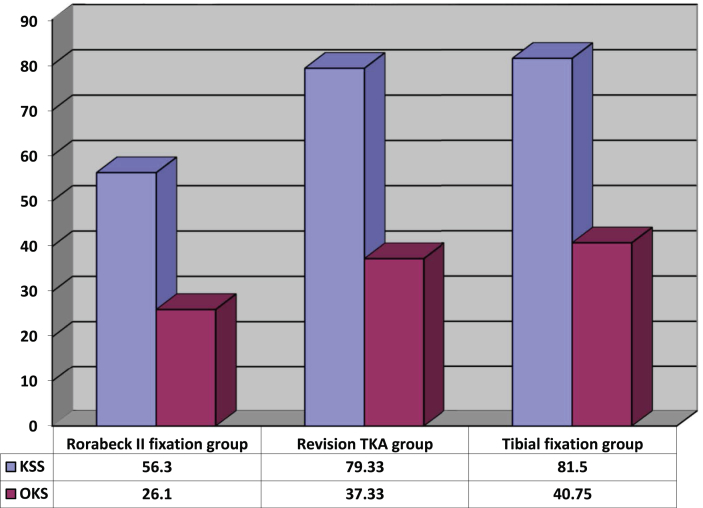
The mean age of all patients was 65.89 years. The mean interval between the index surgery and periprosthetic fracture was 6 years (Range 2 months to 10 years) in male and 18.5 months (Range 4 days to 7 years) in female. 44 (86%) fractures were femoral, 4 (8%) fractures were tibial and 3 (6%) fractures were of patella. The mean knee society score (KSS) & oxford knee score (OKS) were found to be good for revision group as compared to the fixation group at final follow up.
Conclusion
In presence of poor bone stock, far distal fracture configuration, comminution, severe osteoporosis, difficulty in achieving stability with plates & old age-revision TKA is a viable option with stemmed components.
Keywords: Periprosthetic fracture, Locking plates, Varus collapse, Revision TKA, Megaprosthesis
1. Introduction
Increase in the life expectancy and functional demands of the patients have resulted in substantial increase in the frequency of total knee arthroplasty (TKA). This further has increased the number of revision surgeries due to likelihood postoperative complications. Periprosthetic fractures around total knee arthroplasty are relatively rare complication comprises to 0.3–2.5%.1 But these injuries are often complex and challenging for the surgeons due to ageing population in conjunction with severe osteoporosis. It is often difficult to ascertain whether the prosthesis is well fixed or loose. Supracondylar fractures are the commonest periprosthetic fracture with incidence further increases to 1.6–38% after revision TKA.2 Tibial periprosthetic fractures are further less common with incidence of about 0.4% with primary TKA and a higher incidence after revision TKA.3 Patellar periprosthetic fractures are more common with patella resurfacing arthroplasties but overall incidence is 0.68%.4 Risk factors associated with periprosthetic fractures are patients related that include osteoporosis, rheumatoid arthritis, seizure disorder, Parkinson’s disease use of corticosteroids, old age and female sex. Iatrogenic factors include Anterior femoral notching & malalignment. Loosening of implant and osteolysis also predispose to these fractures.2,5, 6, 7
The management option varies from conservative to internal fixation or revision surgery. The most appropriate treatment to achieve a satisfactory outcome is dependent on a number of factors that include degree of displacement, adequacy of bone stock, stability of prosthesis and the medical fitness of the patient.2,5, 6, 7 Furthermore, it is often difficult to ascertain whether the prosthesis is well fixed or loose. These factors coupled with osteoporosis makes the success of internal fixation unpredictable. Similarly, revision surgery itself is a big challenge in the presence of periprosthetic fracture. So any form of treatment has a high rate of failure. Thus this study was conducted to analyze the results of various methods of treatment of periprosthetic fractures following TKA and to form the optimal treatment guidelines for fixation or revision.
2. Material and methods
It was a retrospective study which was conducted at high volume arthroplasty centre in northern part of India. Out of 7390 primary cemented TKAs performed during 2000–2018, 51 cases diagnosed with periprosthetic fracture were enrolled and underwent surgical intervention. The data was analysed in terms of clinical and functional outcome. All patients with periprosthetic fracture that occurred during intraoperative period & following primary or revision TKA were included in the study. Patients with incomplete records and those who died or did not come for follow up were excluded out. Diagnosis was made on the basis of clinical examination and radiographic evaluation of all the patients. Type of primary prosthesis, interval between TKA and periprosthetic fracture, type of fracture, prosthesis stability and mode of fixation of fracture, any revision surgery and complication were noted. The details of revision surgery were also recorded from the operative notes in terms of implant used or any additional procedure such as bone grafting, revision total knee arthroplasty with semiconstrained or fully constrained & distal femur replacement. Post operatively, Sequential x-rays of the knee were taken to asses union, malunion, nonunion and any sign of implant failure. The functional status of the patient before periprosthetic fracture was assessed from the records and compared with the latest follow-up using Knee Society Score (KSS) and Oxford Knee Score (OKS). All periprosthetic fractures were classified according to the prevalent classification system. Supracondylar femoral fractures after total knee arthroplasty were classified by Lewis and Rorabeck.8 While Felix3 and Goldberg9 classification systems were used to classify periprosthetic fracture around tibial and patellar site respectively. The goal of treatment was to obtain and maintain good postoperative fracture alignment and stability to allow early range of motion.
2.1. Statistical analysis
Statistical analysis was performed by the SPSS program for windows, version 17.0. Continuous variables are presented as mean and categorical variables are presented as absolute numbers and percentage. Data were checked for normality before statistical analysis. Normally distributed continuous variables were compared using the paired t-test whereas the Mann-Whitney U test was used for those variables that were not normally distributed. For all statistical tests, a p value less than 0.05 was taken to indicate a significant difference.
2.2. Observation and results
Demographic profile: This is a retrospective review of 51 cases of periprosthetic fractures following total knee arthroplasty treated from the year 2000–2018. There were 13 (25%) male patients and 38 (75%) female patients, 12 (23%) patients were of age <60 years, and 39 (77%) were >60 years old. The mean age of all patients was 65.89 years. All the cases were followed-up for a mean duration of 6.35 years (range 6months–15 years).
Cause of periprosthetic fracture & time interval: 13 (25%) fractures occurred intra-operatively, 36 (71%) fractures occurred after a trivial trauma and only 2 (4%) fractures occurred due to a road traffic accident. The mean interval between the index surgery and periprosthetic fracture was 6 years (Range 2 months to 10 years) in male and 18.5 months (Range 4 days to 7 years) in female. 44 (86%) fractures were femoral, 4 (8%) fractures were tibial and 3 (6%) fractures were of patella.
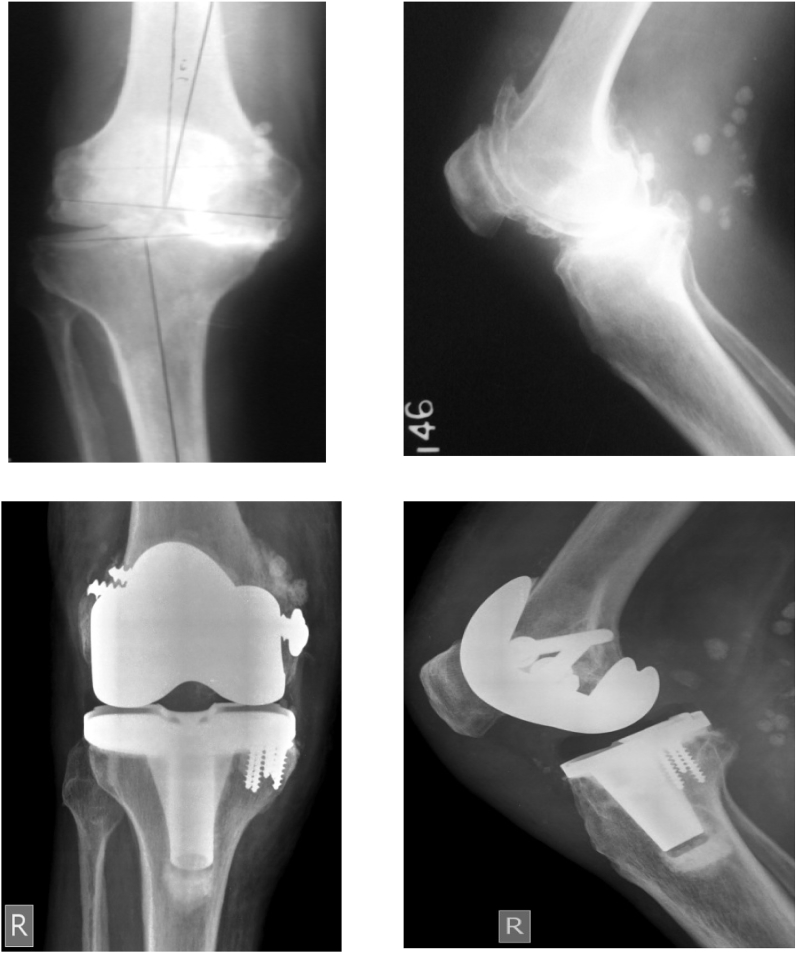
Intraoperative periprosthetic fractures: There were 13 intraoperative periprosthetic fractures recorded in the study, 11 were avulsion type fractures of medial epicondyle of femur and 2 were medial tibial plateau that occurred during tibial preparation. Out of 11 femoral fractures, 2 cases were managed with two cancellous screws due to good bone quality & other 2 were managed by transosseous suture technique repair method using ethibond no. 5-0 due to severe osteoporosis and poor purchase of screws. Rest 7 cases were stable type of injury thus managed conservatively with knee brace only. Both tibial site fractures were managed by cancellous screw fixation. Post op rehabilitation was done by long knee brace and patients were allowed to weight bear as tolerated with brace. Knee flexion was restricted to 30° for first three weeks. The check X-rays of one of the case at 9 months follow up showed no screws cut out of bone with no valgus instability and range of motion were comparable to opposite side knees (Fig. 1). Final mean knee society score of all intraoperative fractures was 80.8 (range 76–90) and oxford knee score was 40 (range 36–44). No complication was noticed in terms of valgus instability with loss of fixation, non union, infection or revision surgery.
Fig. 1.
Pre-op and Post-op radiograph of intra-op medial condyle avulsion fracture of femur, fixed by 2 cancellous screws.
2.3. Post-surgery periprosthetic fractures
Supracondylar femoral fractures: There were 31 post TKA supracondylar femur fractures. 1 case was undisplaced Rorabeck type I thus managed conservatively with above knee cast for 6 weeks followed by gradual mobilization and weight bearing was started. The fracture united well with good knee scores. 26 cases were Rorabeck type II managed with internal fixation and 4 cases were type III managed with revision arthroplasty (RHK) and distal femur replacement due to deficient distal femur bone stock, osteoporosis and ligament instability. Out of 26 cases, 18 (70%) fractures united after primary fixation. 2 (8%) fractures united after secondary fixation and 6 (22%) fractures did not unite even after multiple surgeries thus underwent revision arthroplasty & distal femur replacement. Mean union duration was 6 months after primary fixation with mean Knee Society Score 70.37 and mean Oxford Knee Score 32.87. 4 fractures out of 18 healed in 7.5 months with poor knee scores below 60(KSS) and 30(OKS). The poor score was because of stiffness and varus malalignment of knee. Rest 4 cases with Rorabeck type III were found to have excellent knee scores above 80(KSS) and 40(OKS) at their follow up.
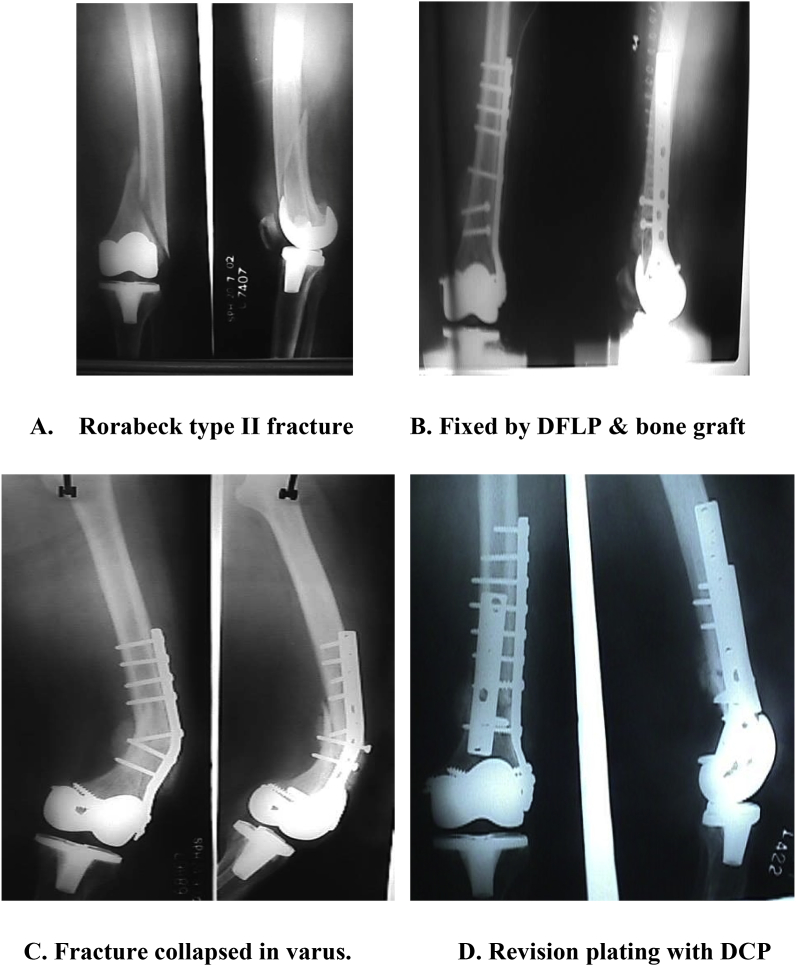
Fractures united after secondary fixation (revision fixation): 2 fractures collapsed in varus and thus required revision fixation with plating, one was managed with 4.5 mm Broad DCP on anterior aspect of femur with bone grafting (BG) (Fig. 2A–D). The other was fixed with locking compression plate and bone grafting on medial aspect of femur, both fractures were united in 9 months with poor knee scores below 50(KSS) and 30(OKS).
Fig. 2.
(A-D): Rorabeck type II fracture; varus collapse, managed with Revision plating.
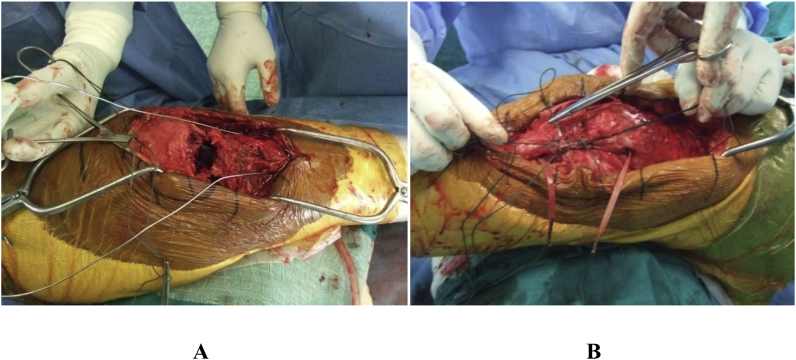
Complication: In this study, out of 26 Rorabeck type II fractures, 6 fractures needed Revision Arthroplasty because of nonunion. In one patient revision total knee replacement with semi-constrained LCCK implant (Legacy constained condyler knee-Zimmer) was done. Three patients revised with fully constrained RHK (Rotating Hinge Knee-Zimmer) implant. 2 patients with multiple implant failure and deficient distal half of femur were revised, one was with distal femur Megaprosthesis (LINK MEGASYSTEM-C) for distal femur and other was with total femur replacement (LINK MEGASYSTEM-C) (Fig. 3). Final mean KSS was 79.33 (64–90) and OKS was 37.33(28–42) (Table 1).
Fig. 3.
Showing rotating hinge knee with stemmed components, distal femur & total femur replacement.
Table 1.
Rorabeck type II fractures that required Revision total knee arthroplasty with RHK & distal femur replacement with Megaprosthesis after internal fixation.
| S.N | Age | Sex | Primary implant | Interval | Primary fixation | Secondary Surgery | Complication | Revision Arthroplasty | Final KSS | Final OKS |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 57 | F | LPS | 4 day | ORIF with IM nailing | DFLP + BG | Nonunion,implant failure | Revision tka (RHK) | 78 | 32 |
| 2 | 66 | M | LPS-flex | 2 years | ORIF with DFLP + BG | Debridement | Infected Non union | Revision tka (RHK) | 80 | 42 |
| 3 | 56 | M | LPS | 10 years | ORIF with DFLP + BG | Debridement, 1ststage revision | Infected nonunion | Revision tka (LCCK) | 90 | 40 |
| 4 | 62 | F | Gender | 2 months | ORIF with DFLP | Non union | Revision tkr (RHK) | 84 | 42 | |
| 5 | 54 | F | LPS | 4 months | ORIF with DCP + BG | IM nailing + BG,Revision with LCCK | non union, Multiple Implant failure | Revision tka (mega prosthesis) | 80 | 40 |
| 6 | 84 | F | LPS | 1 year | ORIF with DFLP + BG | Multiple plating + BG, Revision with RHK | non union, Multiple Implant failure | Total femur replacement | 64 | 28 |
Periprosthetic tibial fractures: There were 4 patients of Felix type III periprosthetic fracture noticed in the study. All four Felix type III tibial periprosthetic fractures were fixed with locking compression plate (LCP) system (Fig. 4). Three fractures were fixed after open reduction and one was plated by MIPPO technique. Bone grafting was done in 2 cases. All the fractures united with mean period of 6.255, 6, 7, 8 months with good to excellent knee score. The final mean KSS and OKS was 81.5 and 40.75 noted after fracture union.
Fig. 4.
Pre and Post op radiograph of Felix type III fracture, fixed by LCP.
Periprosthetic Patellar Fractures: There were 3 patients diagnosed with patella fractures. 1 case was of Goldberg type 1 and 2 patients with Goldberg type IIIa fracture were noticed. Type 1 case was managed conservatively with long knee brace for 6 weeks. Then gradual mobilization started & fracture united with good functional outcomes. In other 2 patients, the patellar tendon and inferior pole of patella were weaved through the intact superior pole of patella and securely knotted on superior part of patella by number 5 ethibond suture. In one patient the repair was protected by figure of eight stainless steel wire taken through the tibia (Fig. 5A &B). In the second patient the repair was augmented by semitendinous & gracilis (STG) harvested from same side with mersiline tape and passed horizontally through midpoint of patella and the tibial tubercle. Both the fractures united within mean duration of 5 months with good range of motion of 10–100°. The final mean KSS and OKS was 76 and 36 noted after fracture union. Overall mean KSS and OKS of all patients at the final follow up was 70.48 and 33.62. Mean KSS and OKS was highest for tibial periprosthetic fractures and lowest for Rorabeck type II fixation group (Fig. 6).
Fig. 5.
Goldberg type IIIa fracture managed by tendon repair, A. Repair protected by stainless steel wire B. Repair protected by STG graft and mersiline tape.
Fig. 6.
Higher Knee Society Score and Oxford Knee Score were observed for tibial fixation and revision TKA groups.
3. Discussion
3.1. Demography and age variations
There were 13 (25%) male patients and 38 (75%) female patients in our study. Scottish national database also showed that women are 2.3 times more likely to suffer a fracture than men(10). This is because more female patients undergo TKA than males & also more prone for osteoporosis therefore have higher incidence of fracture.10 The mean age of all patients was found to be 65.89 years in our study. Meek et al.11 reported that an age of more than 70 years was associated with higher risk of periprosthetic fractures. Scottish national database also reported that patients aged more than 70 years were 1.6 times more likely to have a fracture than younger patients.10 On the contrary, Jasvinder et al.12 in their study observed that younger age less than 60 years was associated with higher risk of postoperative periprosthetic fractures following primary TKA. A more active lifestyle with high demand in younger patients may put them at higher risk of trauma than older patients.
3.2. Incidence among subtype of periprosthtetic fractures
We found 13 (25%) intraoperative cases of periprosthetic fractures among 7390 primary TKAs performed at our centre. Periprosthetic distal femoral fracture during TKA is rare. Alex HF Pun et al. reviewed 1346 primary cemented TKAs with the NexGen LPS implants and reported 5 femoral avulsion fractures of the medial femoral condyles.13 In our study out of total postoperative periprosthetic fractures, 31(82%) fractures were supracondylar femoral fractures, 4(10%) tibial and 3(8%) were patellar. Supracondylar femoral periprosthetic fractures are by far the commonest reported in the literature.10 Periprosthetic tibial & patellar fractures after TKA are very uncommon.2,6,14
3.3. Risk factors and etiology
Osteoporosis is a significant risk factor for postoperative periprosthetic fractures. Paraschou et al.15 in their study showed that osteoporosis was associated with six patients out of a total of 15 & all fractures were due to low velocity trauma. In our study 71% periprosthetic fractures occurred following a trivial trauma. Due to osteoporosis these patients were more prone to develop periprosthetic fractures. Also these fractures are more common after revision Total Knee Arthroplasty having rotationally constrained implants that create increased torsional load transfer to bone.16 In our study no fracture occurred after revision Total Knee Arthroplasty till last follow up. Anterior femoral notching is anthor important risk factor for these fractures.2,5,6 It has been shown that 3 mm anterior femoral notching resulted in torsional load to failure by 55 Nm. These results however were based on mathematical and biomechanical studies. In literature many retrospective studies has demonstrated no difference in knees with or without notching & these observations were attributed to osseous remodeling and stress redistribution.7,16 In our study, out of 51 patients anterior notching was seen in only 2 patients & had fracture within 2 months of TKA. Anterior notching was not a decisive factor for periprosthetic fracture.
3.4. Intraoperative periprosthetic fractures
Patients with severe varus/valgus deformity requiring a semi-constrained implant are at higher risk of intra-operative fracture.17 In some implant designs, more than twice as much bone is resected from the intercondylar notch, and this results in a decreased segment of bone to bridge the femoral diaphysis and medial or lateral femoral condyle (Insall Burstein II: 12.7 cm3, Sigma: 13.5 cm3, Genesis II: 5.9 cm3, Legacy: 11.8 cm3, and Optitrack: 9.7 cm3). The relative risk for intra-operative distal femoral fracture is higher for posterior-stabilised implant than a cruciate-retaining implant. Intraoperative fractures most commonly occur during exposure and bone preparation or component trial testing.13,17 This study reviewed 13 intraoperative cases of periprosthetic fractures during TKA, in patients with posterior stabalised knee. Majority of femoral site fractures occurred during the trial phase when the tibia was reduced onto the femur while tibial site fractures occurred during tibia preparation. All fractures healed with good knee functional scores. We concluded these fractures are due to discrepancy between native bone and implant size, osteoporosis and inadequate soft tissue release.
3.5. Supracondylar peiprosthetic femoral fractures
Although displacement has been considered the major factor in determining nonsurgical or surgical management for supracondylar femoral fractures proximal to a total knee arthroplasty, sufficient evidence now supports surgical management in most cases. Nonsurgical management is reserved for undisplaced fracture and in patients who are medically unfit to tolerate surgery.16 Preoperative planning is important to establish the types and dimensions of existing total knee components and whether they are stable or loose. The choice of implant may be guided by the amount of bone available for distal fixation.16 Very distal comminuted fractures, severe osteoporosis and poor distal bone stock with implant loosening may require revision arthroplasty with a stemmed component or distal femur replacement and possibly a bulk allograft. The surgeon should be well prepared for revision surgery if intraoperative findings are more severe than indicated by preoperative radiography18. In our study, 4 cases with implant loosening were noticed and underwent revision arthroplasty or distal femur replacement.
Intramedullary nails and precontoured Distal Femoral locking plates are usually the best treatment for these fractures according to literature.2,19 Before planning a retrograde nail osteosynthesis, it has to be proven that the distal entry point between the condyles of a resurfacing total knee arthroplasty (TKA) is ‘open’. In prosthesis with a box (posteriorly stabilised) or with a stem, a plate should be preferred. According to a recent analysis of the literature, there seems to be no difference in clinical outcome using a nail or a plate.20 In our study one Rorabeck type II fracture was fixed by retrograde intramedullary nail went into nonunion with implant failure thus required revision TKA. Other Rorabeck type II fracture which was secondarily fixed with retrograde nail after failed primary plate fixation also did not unite and required revision with megaprosthesis (Table 1). We preferred to use periarticular locked compression plates for internal fixation, as using a retrograde intramedullary nail is limited by the narrow or closed intercondylar space of the TKA prosthesis. Enlargement of the notch is often required and may raise concern about 3rd body wear.21,22
Traditional plate fixation is prone to varus collapse.2,22 In our study one fracture fixed with dynamic compression plate collapsed in varus and needed revision. While 2 cases underwent dual plate construct due to distal fracture line with fixed prosthesis and united well with good functional knee scores. The locking plate is precontoured & angular stable implant so it helps in reducing the fracture fragments. Multiple screws are inserted at different angles thus prevents toggling of fracture fragments and varus collapse. Far distal fracture configuration sometimes limits the number of distal screws insertion thus we recommend anatomical reduction & augmentation with medial plating is to be done to prevent varus collapse & implant failure. This allows the surgeon to optimize stability while avoiding damage to in situ implant or interface. Using a minimally invasive technique, the locked compression plate can be inserted easily through a small incision into the sub muscular periosteal plane thus minimizing damage to the periosteal blood supply and promotes healing. In our study 10 fractures were managed with minimally invasive technique. All united in 4 months with good to excellent knee scores. Locking plates provide well stable fixation however complication rates of this technique nevertheless remain high with up to 29% failures.19 This may be attributed to following reasons: 1) Bone quality is poor due to pre-existing osteoporosis 2) Stable fixation is difficult to achieve in areas with an intramedullary implant and far distal fracture configuration 3) Fracture healing is significantly delayed in aged patients 4) Prosthesis loosening 5) Non anatomical reduction may facilitate the resulting fracture. Thus in such scenarios, we recommend revision arthroplasty as a viable option for better functional outcomes. If nonunion occurs either due to the deficiency of bone tissue that supports the femoral component in cases of severe comminution or bone loss or due to other internal fixation failure, distal femoral replacement using a tumor prosthesis can be considered as a limb salvage procedure to preserve minimum knee function and maintain the leg length.23,24 In our study, on comparison with fixation group, better knee function was observed in revision group (Fig. 6). In the literature many studies have suggested revision arthroplasty provides best results in terms of walking ability, range of motion and early rehabilitation.25
3.6. Periprosthetic tibial fractures
Tibial fractures are often accompanied by component loosening or instability and sometimes by component malalignment, malposition and joint instability thus requires revision arthroplasty with stemmed components.23 In this study, 4 Felix type III fractures were noticed with stable prosthesis, all were fixed by locking compression plate & bone grafting was done in 2 cases. All fractures healed in 6.25 months with excellent knee scores. Because of thin soft tissue layer we recommend minimally invasive techniques or percutaneous fixation of plates with direct or indirect reduction of the fracture thus preserving the local blood supply which prevents wound dehiscence and infection. For fracture with loose prosthesis, revision prosthesis with diaphyseal fixation which needs to be long enough to bypass the fracture site atleast by 2 cortical fixation is recommended for optimal results.
3.7. Periprosthetic Patellar Fractures
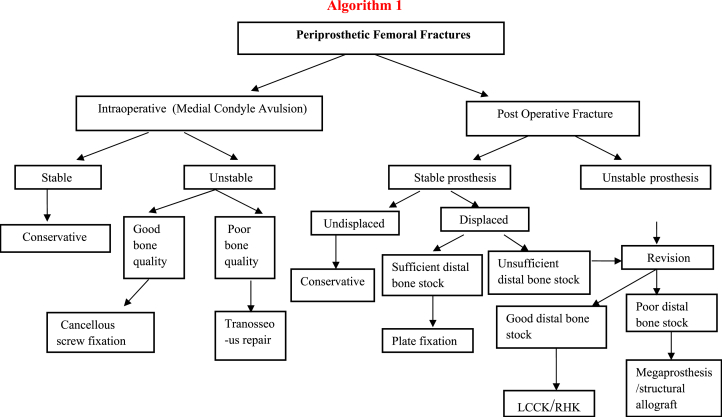
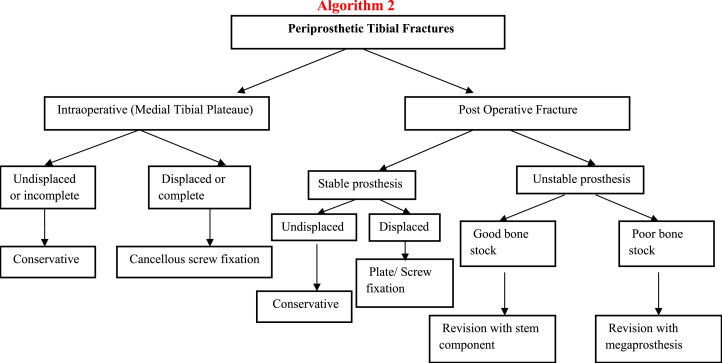
Technical factors such as implant and limb alignment, asymmetric resection or over resection of the patella and loss of blood supply leading to osteonecrosis undoubtedly place the patella at risk for fracture.6 Loosening of patellar component, maltracking of patella and disruption of extensor mechanisms are indicators of surgical intervention.1 In this study, no patella resurfacing was performed and out of 51, 3 cases of patellar periprosthetic fractures were noticed following trivial trauma. Due to disruption of extensor mechanism, 2 patients underwent surgical intervention as described earlier in the methodology. Good functional outcomes were noticed with the type of treatment given in all the cases. Thus we recommend surgical intervention in cases with extensor mechanism disruption. Augmentation with STG graft & mersiline tape further reinforce the fixation and allows early rehabilitation with predictive outcomes. Simple open reduction and internal fixation has high rates of non union and implant failure.1 Our study has few limitations. Small sample size and retrospective study with no comparison group were there to compare the type of treatment given for management of all periprosthetic fractures. Thus the fixed guidelines for management of periprosthetic fractures cannot be ascertained. However, our study prompts future studies to be performed on large cohort scales with large sample size and comparison groups. Our study showed the results with longest follow up (mean 6.5 yrs) with the type of treatment modalities given and suggested an algorithm of treatment options over management of these complex periprosthetic knee injuries (Algorithm 1&2).
4. Conclusion
Management of periprosthetic fractures after Total Knee Arthroplasty is difficult. In view of less healing capacity of osteoporotic bone in elderly patients with prosthesis in distal aspect union in supracondylar femoral fracture is challenging for surgeon. Our ultimate goal is to restore knee alignment and early range of motion. Although periarticular distal femoral locking plates have shown good results with minimal invasive technique but most of times plate or nail osteosynthesis leads to loss of fixation and varus angulation. Nonunion and implant failure are major complications in supracondylar femoral fractures. Multiple attempts to fix these fractures lead to deficient distal femur and unstable TKA implants results in flail knee. Revision TKA group did not have an increased complication rate and interestingly the recovery of patients was found to be quicker. Knee function (KSS & OKS) in revision group was better than fixation group and also revision patients were more satisfied as compared to fixation group. We conclude that in presence of poor bone stock, far distal fracture configuration, comminution, severe osteoporosis, difficulty in achieving stability with plates & old age-revision TKA is a viable option with stemmed components. If distal bone stock is deficient then we can choose megaprosthesis for distal femur. In cases with simple proximal fracture where indirect reduction with minimally invasive techniques are possible then precontoured distal femur locking plates should be preferred. For periprosthetic tibial fractures with fixed prosthesis, minimally invasive techniques with percutaneous plates fixation should be preferred.
Level of evidence
Level IV study.
Funding
There is no funding source for this study.
Ethical approval
This study does not contain any study with animals and all patients were included in the study only after their written consent.
Declaration of competing interest
The authors of the study have no conflict of interest.
Contributor Information
Nikhil Verma, Email: drnikhilucms@gmail.com.
Anuj Jain, Email: jain.doctor.anuj@gmail.com.
Chander Pal, Email: drnikhilucms@yahoo.com.
Simon Thomas, Email: simon_rac@yahoo.com.
Shekhar Agarwal, Email: shekhar1952@hotmail.com.
Prateek Garg, Email: gargprateek04@gmail.com.
References
- 1.Rayan F., Konan S. A review of periprosthetic fractures around total knee arthroplasties. Curr Orthop. 2008;22:52–61. [Google Scholar]
- 2.Whitehouse M., Mehendale S. Periprosthetic fractures around the knee: current concepts and advances in management. Curr Rev Musculoskelet Med. 2014;7:136–144. doi: 10.1007/s12178-014-9216-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Felix N.A., Stuart M.J., Hanssen A.D. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res. 1997;345:113–124. [PubMed] [Google Scholar]
- 4.Ortiguera C.J., Berry D.J. Patellar fracture after total knee arthroplasty. J Bone Joint Surg Am. 2002;84:532–540. doi: 10.2106/00004623-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 5.McGraw P., Kumar A. Periprosthetic fractures of the femur after total knee arthroplasty. J Orthop Traumatol: Off J Ital Soc Orthop Traumatol. 2010;11(3):135–141. doi: 10.1007/s10195-010-0099-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dennis D.A. Periprosthetic fractures following total knee arthroplasty. J Bone Joint Surg Am. 2001;83:120–130. [PubMed] [Google Scholar]
- 7.Gordon M.C., Khan W. Recent advances and developments in knee surgery: principles of periprosthetic knee fracture management. Open Orthop J. 2012;6(Suppl 2):301–304. doi: 10.2174/1874325001206010301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rorabeck C.H., Taylor J.W. Periprosthetic fractures of the femur complicating total knee arthroplasty. Orthop Clin N Am. 1999;30:265–277. doi: 10.1016/s0030-5898(05)70081-x. [DOI] [PubMed] [Google Scholar]
- 9.Goldberg V.M., Figgie H.E., Inglis A.E. Patellar fracture type and prognosis in condylar total knee arthroplasty. Clin Orthop Relat Res. 1988;236:115–222. [PubMed] [Google Scholar]
- 10.Sarmah S.S. Periprosthetic fractures around total knee arthroplasty. Ann R Coll Surg Engl. 2012;302–307 doi: 10.1308/10.1308/003588412X13171221592537. (PMC. Web. 14 Jan. 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meek R.M., Norwood T., Smith R., Brenkel I.J., Howie C.R. The risk of periprosthetic fracture after primary and revision total hip and knee replacement. J Bone Jt. Surg. 2011;93(1):96–101. doi: 10.1302/0301-620X.93B1.25087. [DOI] [PubMed] [Google Scholar]
- 12.Singh J.A., Jensen M., Lewallen D. Predictors of periprosthetic fracture after total knee replacement. Acta Orthop. 2013;84:170–177. doi: 10.3109/17453674.2013.788436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pun A.H.F. Intra-operative fracture in posterior-stabilised total knee arthroplasty. J Orthop Surg. 2015;23(2):205–208. doi: 10.1177/230949901502300219. [DOI] [PubMed] [Google Scholar]
- 14.Ebraheim N.A., Ray J.R., Wandtke M.E. Systematic review of periprosthetic tibia fracture after total knee arthroplasties. World J Orthop. 2015;6(8):649–654. doi: 10.5312/wjo.v6.i8.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paraschou S., Flegas P., Anastasopolus S., Dionellis P., Papanos A., Alexopolous J. vol. 61. 2010. pp. 59–64. (Results of Treatment of Periprosthetic Supracondylar Femoral Fractures above Total Knee Arthroplasty). [Google Scholar]
- 16.Su E.T., De Wal H., Di Cesare P.E. Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthop Surg. 2004;12:12–20. doi: 10.5435/00124635-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Delasotta L.A., Orozco F., Miller A.G. Distal femoral fracture during primary total knee arthroplasty. J Orthop Surg. 2015;23(2):202–204. doi: 10.1177/230949901502300218. [DOI] [PubMed] [Google Scholar]
- 18.Hagel A., Siekmann H., Delank K.-S. Periprosthetic femoral fracture—an interdisciplinary challenge. Dtsch Ärzteblatt Int. 2014;111(39):658–664. doi: 10.3238/arztebl.2014.0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruchholtz S., Tomás J. Periprosthetic fractures around the knee—the best way of treatment. Eur Orthop Traumatol. 2013;4:93–102. doi: 10.1007/s12570-012-0130-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herrera D.A., Kregor P.J., Cole P.A., Levy B.A., Jönsson A., Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty—systematic review of 415 cases (1981–2006) Acta Orthop. 2008;79:22–27. doi: 10.1080/17453670710014716. [DOI] [PubMed] [Google Scholar]
- 21.Kilicoglu O.I., Akgül T., Sağlam Y., Yazıcıoğlu O. Comparison of locked plating and intramedullary nailing for periprosthetic supracondylar femur fractures after knee arthroplasty. Acta Orthop Belg. 2013;79:417–421. [PubMed] [Google Scholar]
- 22.Agarwal S., Sharma R.K., Jain J.K. Periprosthetic fractures after total knee arthroplasty. J Orthop Surg. 2014;22(1):24–29. doi: 10.1177/230949901402200108. [DOI] [PubMed] [Google Scholar]
- 23.Yoo J.D., Kim N.K. Periprosthetic fractures following total knee arthroplasty. Knee Surg Relat Res. 2015;27(1):1–9. doi: 10.5792/ksrr.2015.27.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freedman E.L., Hak D.J., Johnson E.E., Eckardt J.J. Total knee replacement including a modular distal femoral component in elderly patients with acute fracture or nonunion. J Orthop Trauma. 1995;9:231–237. doi: 10.1097/00005131-199506000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Corideiro E.N. Periprosthetic fractures in patients with total knee arthroplasties. Clin Orthop Relat Res. 1990;252:182–189. [PubMed] [Google Scholar]