Abstract
Objective
Olecranon fractures are common injuries in patients of any age. The vast majority are treated with two operation techniques: a plate fixation (PF) or tension band wiring (TBW). The objective of this study is to compare the outcomes of surgically treated olecranon fractures with plate fixation or tension band wiring. We hypothesise that PF patients would show significantly inferior outcomes due to more complex injuries.
Patients and methods
Between 2010 and 2017, a total of 108 patients were treated with plate fixation and or tension band wiring. Clinical data of 40 surgically treated olecranon fractures were collected and analysed. Clinical and functional evaluations were performed using Mayo-Score, DASH-Score, Weseley -Score and subject elbow value (SEV). Furthermore, complication rates, time to return to work and operation duration were documented.
Results
The mean follow-up was 70.5 ± 45.6 months. Time of return to work was 6.5 ± 2.2 weeks in the TBW group and 10.9 ± 6,6 in the PF group (p = 0.372). The mean duration of surgery was 95.2 ± 47.0 min in the TBW group and 192.5 ± 113.0 min in the PF group (p = 0.001). In the TBW group, the mean hospitalisation period was 7.9 ± 10.1 days and 11.2 ± 9.8 days in the PF group. Revisions were required in 0.3 ± 0.6 of cases (0.2 ± 0.5 in TBE and 0.4 ± 0.7 in PF). The median DASH Score was 7.0 (3.6–13.7) in the TBW group and 12.1 (5.5–24.8) in the PF group (p = 0.948)
Conclusion
Tension band wiring and plate fixation are both practical treatment options with mostly positive outcomes, even though high complication rates can occur. There were no significant differences in either group concerning functional outcome or time back to work. The duration of surgery was significantly higher in the PF group, whereas the incidence of metalwork-associated complications was higher in the TBW group.
Keywords: Locking plate, Olecranon fixation, Olecranon fracture, Tension band wiring, Elbow fracture
1. Introduction
Up to 10% of all upper limb fractures involve the olecranon, and this type of fracture is the most common osseous injury of the elbow joint1,2 These show a bimodal distribution occurring in younger patients due to high-energy trauma and in elderly cohorts with low bone quality after low-energy falls.3 The fracture mechanism in most cases is a direct impact to the posterior aspect in the range 60°–110° flexion. The fracture pattern depends on bone quality, age and point of impact, with the most common accidents being simple falls and road traffic accidents.4,5 Due to tension of the triceps brachii muscle, most fractures are dislocated and not suitable for conservative treatment.6 Multiple classification systems for olecranon fractures exist, such as AO (Arbeitsgemeinschaft für Osteosynthesefragen), Mayo, Schatzker and Colton, but none are widely accepted or provide direct and reliable advice on operative strategies. Their low reproducibility rates also raise questions about their use in clinical and research contexts.7,8 While Schatzker and Colten divide the fractures in groups by quantity of fragments and fracture lines, the AO classification subsumes olecranon fractures to proximal forearm injuries.9,10
For outcome evaluation, multiple scoring systems such as the disabilities of the arm, shoulder and hand (DASH) questionnaire, Mayo Score and Weseley Score are used. The Mayo and M Weseley Score systems focus on motion, pain and stability, whereas the DASH is a subjective score including activities of daily life and covers functionality of the entire upper extremity.11,12
Numerous operative procedures are described, but most surgeons use tension band wiring (TBW) or plate fixation (PF), depending on the fracture pattern. In 1963, Weber and Vasey introduced a technique in which after reduction, two parallel Kirschner wires are introduced across the olecranon fracture for stabilisation. Another wire forming a figure-eight passes around the K-wires, and a drill hole in the ulna is used for compression on the fracture.13 TBW is a simple, approved, low-cost technique. Its disadvantages include the high number of symptomatic prominence of K-wires and the technique's limited capability in more complex fractures.14,15 Posterior plate fixation is considered for unstable, oblique and complex fractures but can be used in all fracture types. One-third tubular, reconstruction plates or pre-contoured LCPs are the most common implants. Pre-contoured plates are more often recommended and can prevent over-correction and loss of reduction. A common disadvantage is the higher cost of PF compared to TBW.2,16,17 A variety of alternative procedures such as percutaneous screw fixation, intramedullary nailing or cable pin systems are less utilised than TBW or PF.3,18,19
Outcomes of operative treatment of olecranon fractures are associated with positive clinical and functional results when no adverse events occur. Possible complications after surgery are proximal migration of K-wires, non-union, osteoarthritis and postoperative reduced range of motion, especially for extension.20
A stable and painless movable elbow joint is essential for daily activity, and patient recovery expectations may be high, especially in younger patients. Risk factors for posttraumatic elbow joint arthrosis are non-anatomical reconstruction of the joint surface, axial malalignment and untreated concomitant injuries.1
The main goal of this study is to present a comprehensive comparison of two common treatment strategies for olecranon fractures considering outcome factors such as range of motion, time back to work and complications in order to find the optimal solution in individual situations. The working hypothesis is that PF patients would show significantly inferior outcomes due to more complex injuries.
2. Patients and methods
A retrospective cohort study was conducted including 108 patients with isolated olecranon fractures who underwent operative therapy between 2007 and 2017. A total of 40 patients met the criteria to be included, of which 20 patients had been treated with TBW and 20 patients had been treated with PF. Pathologic fractures due to a malignant tumour, revisions after failed primary treatment in other hospitals and patients without epiphyseal fusion were excluded. No patients were excluded because of systemic or local risk factors. The minimum follow-up was 24 months. The institution in which all procedures took place is a certified, level I trauma centre, and all surgeons were experienced, board-certified orthopaedic and trauma surgeons.
All patients underwent physical examinations, laboratory tests and medical history analyses. An X-ray of the elbow joint in two planes (lateral and anterior-posterior projection) and a computed tomography scan were performed preoperatively. The fractures were graded with Schatzker, Mayo and AO classifications to accurately determine the fracture pattern and because the diversity of the systems makes none universally applicable. This study was approved by the local institutional review board (Ethics Committee No 056/16).
2.1. Operative technique
Each patient was placed in an abdominal position with a short arm board and a pneumatic tourniquet applied to the upper arm. The incision started at the proximal point of the olecranon and curved radially around the olecranon prominence to protect the ulnar nerve. A longitudinal posterior approach was adequate for most olecranon fractures, but in more complicated injuries, additional access to the medial or lateral elbow was required and the patient was then placed supine. If the bursa olecrani was damaged, a resection was performed to prevent infection.2,21
2.1.1. TBW
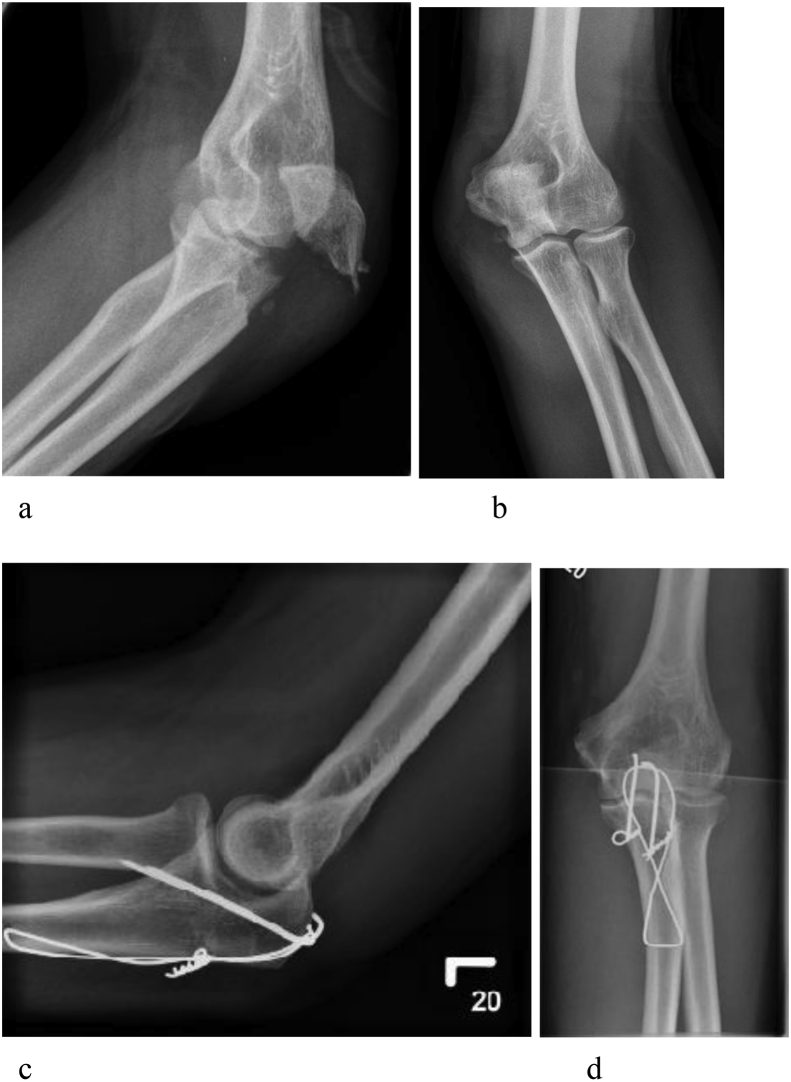
In simple and stable fractures (Mayo 1A, 2A, Schatzker A, B and AO B1, B3.1), TBW was the most customary procedure. The tension band converts tensile forces from the triceps muscles on the olecranon into compression forces at the joint line. After, positioning and surgical approach reduction was performed under radiographic control and temporary fixation with a tenaculum clamp. Two parallel 1.6-mm K-wires were introduced antegrade across the fracture site and penetrated the distal anterior cortex. This reduces the risk of proximal wire migration compared to intramedullary placement. The safe zone to avoid neurovascular injuries lies within 15 mm distal of the coronoid.22,23,24 The proximal end of the wire was bent 180° and should have been buried beneath the fibres of the triceps into the bone. Approximately 40 mm distal to the fracture line, a hole was drilled through the ulna using a 2-mm drill. A 1-mm wire was inserted through the drilled hole and passed in a figure-eight configuration around the ends of the K-wires. Both wire ends were then united with a twist and tightened with tongs. To achieve symmetric tension at the fracture site and a more rigid fixation, two knots (radial and ulnar) were placed and later bent down to the cortex. When tightened, the figure-eight wire loop acts as the tension band. Following fixation, full range of motion was tested intraoperatively and the implants were checked with plain radiographs (Fig. 1).
Fig. 1.
Fracture of a 52-year-old male patient after bicycle accident. a: X-ray in lateral view. b: AP view before surgery. c: Status after TBW in lateral X-ray. d: Status after TBW in AP view.
2.1.2. PF
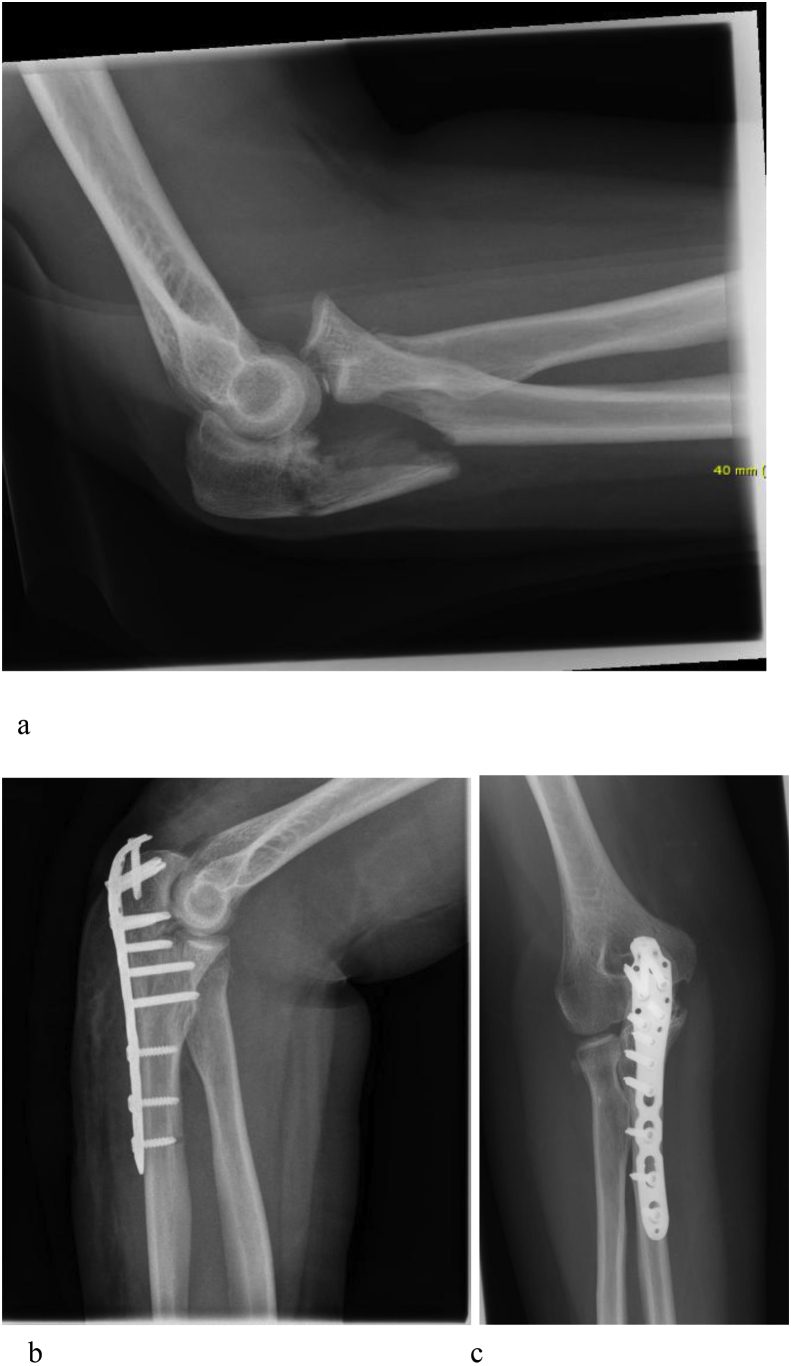
In unstable, oblique and multi-fragmentary fractures, Variable Olecranon Angle Locking Compression Plates (VA-LCP, DePuy Synthes, Solothurn, Switzerland) were used. The positioning and approach is similar to TBW. Temporary reduction was held by K-wires and confirmed by fluoroscopy. The plate was bent to fit the contour of the proximal ulna; to achieve bone contact, it may have been necessary to split the triceps attachment. Locking screws were then applied whenever possible bi-cortically and without protruding into the joint (Fig. 2). Interfragmentary compression or reduction of large coronoid fractures can sometimes be achieved by inserting additional lag screws through the plate.
Fig. 2.
X-ray of a Mayo IIIb fracture of a 49-year-old male patient after ladder accident. a: Lateral X-ray after injury. b: Lateral view after plate fixation. c: AP view after surgery.
2.1.3. Rehabilitation
After surgery, both patient groups were treated with the same structured aftercare algorithm. The affected extremity was placed in plaster for 2–3 days. Physiotherapy began on the first day after surgery for passive mobilisation in a painless range of motion. After wound-healing, active mobilisation for flexion, extension, pronation and supination was allowed as long as no pain occurred. For six weeks after surgery, no loading of the elbow was allowed.
2.2. Outcome evaluation
For outcome evaluation, data from follow-up visits in the outpatient clinic were used. All patients underwent physical and radiological examinations 6, 12 and 24 month after surgery. To measure pain intensity, the Visual Analogue Scale (VAS) was used. For functional outcome, the Weseley, Mayo and DASH Scores were determined. The Weseley Score is an objective functional grading score that collects data about pain and loss of function and rates the outcome in three categories from excellent to fair. The Mayo Elbow Performance Score (MEPS) is a mixed subjective and objective grading score including pain intensity, motion, stability and daily function. The outcome can be rated as poor (less than 60 points), fair (60–74 points), good (75–89 points) or excellent (90–100 points).25
The DASH questionnaire is a 30-item disability/symptom scale to measure upper extremity disorders and assess the upper extremity as a functional unit.11,12 The DASH asks about degree of difficulty in performing physical activities and includes questions about pain, weakness and social activities. The score for all items calculates a score ranging from 100 (most severe disability) to 0 (no disability). The DASH is validated for several languages, and in this study, we used the German version.26
The subjective elbow value (SEV) was also included in follow-up assessments. It consists of a single numeric value to assess the condition of the elbow with a maximum of 100%. Furthermore, the number of revisions, length of hospitalisation and duration of the procedure were documented. As a socioeconomic factor, the time to return to work after the injury was recorded.
2.3. Statistical analysis
Characteristics of the study patients are described as mean values (with standard deviation), median values (with IQR) or numbers (with percentages), as appropriate. The Mann–Whitney U test (for continuous variables) and Fisher's Exact test (for categorical variables) were used to compare the two therapy groups (PF versus TBW) w.r.t. patient characteristics.
The percentage and score variables of the Weseley, Mayo, DASH Score, SEV, extension and flexion were analysed using beta regression to account for the bounded range of the data; the beta distribution supports data ranging from zero to one while also accommodating right or left skewness.
The effect of the operation technique on the Wesley Score and occurrence of complications were assessed by Fisher's Exact test. The differences between the two therapy groups in time to return to work were analysed in a linear regression model.
All regression models were adjusted for age, gender and Schatzker classification.
Estimates obtained from the regression models are represented as coefficient estimates with 95% confidence intervals. P < 0.05 was considered significant. All analyses were carried out using the R Software for Statistical Computing Version 3.3.1.
3. Results
There were 20 patients in the TBW and 20 patients in the PF Group. Both cohorts showed no significant differences in age, sex or BMI at baseline. Table 1 summarises the data and shows details about patient characteristics, fracture classifications and lengths of surgery. The last follow-up examination took place after 66.5 ± 46.3 months in the TBW group and 74.5 ± 45.7 months in the PF group.
Table 1.
Characteristics of study population (n = 40).
| total | TBW | PF | p-Value | |
|---|---|---|---|---|
| Age (mean±sd) | 53.9 ± 20.2 | 53.2 ± 19.7 | 54.7 ± 21.2 | 0.824 |
| Sex (female) | 16 (40%) | 10 (50%) | 6 (30%) | 0.333 |
| BMI | 26.8 ± 5.3 | 26.7 ± 6.9 | 26.9 ± 4.8 | |
| Follow-up in months (30 days) | 70.5 ± 45.6 | 66.5 ± 46.3 | 74.5 ± 45.7 | 0.583 |
| Trauma | 0.819 | |||
| fall<3 m | 23 (57%) | 12 (60%) | 11 (55%) | |
| fall>3 m | 5 (12%) | 3 (15%) | 2 (10%) | |
| Traffic accident | 12 (30%) | 5 (25%) | 7 (35%) | |
| Mayo | 0.003 | |||
| 1a | 0 (0%) | 0 (0%) | 0 (0%) | |
| 1b | 0 (0%) | 0 (0%) | 0 (0%) | |
| 2a | 21 (52%) | 15 (75%) | 6 (30%) | |
| 2b | 16 (40%) | 3 (15%) | 13 (65%) | |
| 3a | 2 (5%) | 1 (5%) | 1 (5%) | |
| 3b | 1 (3%) | 1 (5%) | 0 (0%) | |
| Schatzker | 0.001 | |||
| A | 16 (40%) | 13 (65%) | 3 (15%) | |
| B | 9 (22%) | 5 (25%) | 4 (20%) | |
| C | 3 (8%) | 0 (0%) | 3 (15%) | |
| D | 10 (25%) | 1 (5%) | 9 (45%) | |
| E | 0 (0%) | 0 (0%) | 0 (0%) | |
| F | 2 (5%) | 1 (5%) | 1 (5%) | |
| AO | 0.014 | |||
| B1.1 | 20 (50%) | 14 (10%) | 6 (30%) | |
| B1.3 | 11 (28%) | 2 (10%) | 9 (45%) | |
| B3.3 | 1 (2.5%) | 0 (0%) | 1 (5%) | |
| C1.1 | 2 (5%) | 2 (10%) | 0 (0%) | |
| C2.1 | 2 (5%) | 1 (5%) | 1 (5%) | |
| C2.2 | 2 (5%) | 1 (5%) | 1 (5%) | |
| C3.2 | 1 (2.5%) | 0 (0%) | 1 (5%) | |
| C3.3 | 1 (2.5%) | 0 (0%) | 1 (5%) | |
| Revisions (mean±sd) | 0.3 ± 0.6 | 0.2 ± 0.5 | 0.4 ± 0.7 | 0.236 |
| Duration of surgery in min (mean±sd) | 143.8 ± 98.6 | 95.2 ± 47.0 | 192.5 ± 113.0 | <0.001 |
| Hospitalisation in days (mean±sd) | 9.5 ± 10.0 | 7.9 ± 10.1 | 11.2 ± 9.8 | 0.046 |
The mean follow-up was 70.5 ± 45.6 months. In both groups, a fall from less than 3 m was the most common cause of injury, reported in 23 fractures (57%), while high-energy trauma such as falling from a height (>3 m) or road traffic accident was reported in 17 fractures (32%). The most common fracture pattern using the Mayo classification was a 2a-type fracture in the TBW group (75%) and a 2b-type fracture in the PF group (65%). Using the Schatzker classification, an “A” fracture was most common in the TBW group (65%) and a “D” fracture was most common in the PF group (45%).
The mean duration of surgery was 95.2 ± 47.0 min in the TBW group and 192.5 ± 113.0 min in the PF group (p = 0.001). The mean time of hospital stay was 9.5 ± 10.0 days. The mean hospitalisation period was 7.9 ± 10.1 days in the TBW group and 11.2 ± 9.8 days in the PF group. Revisions were required in 0.3 ± 0.6 cases (0.2 ± 0.5 in TBE and 0.4 ± 0.7 in PF).
3.1. Outcome analysis
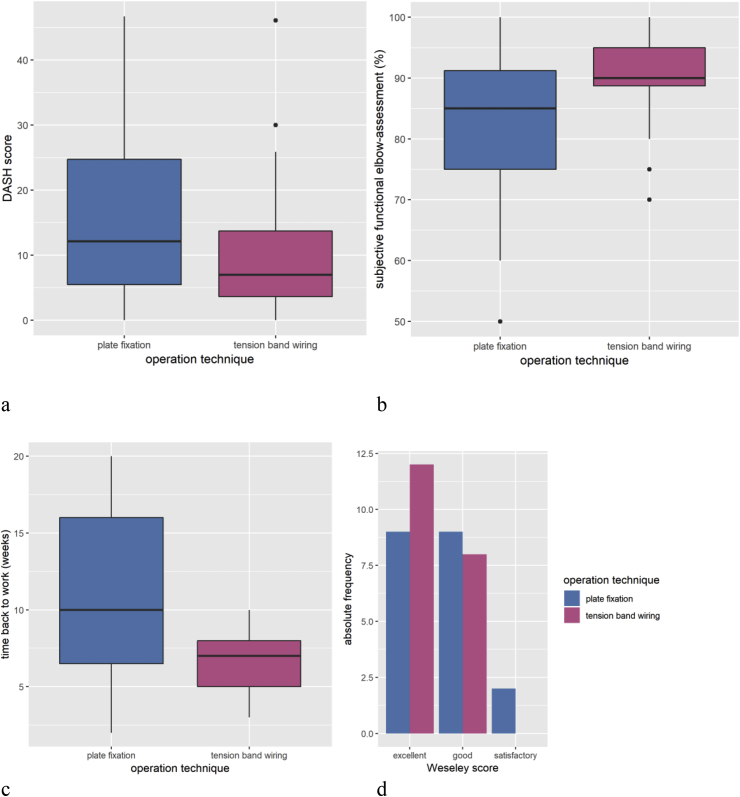
Table 2 shows the characteristics of the response variables in both groups. The median DASH Score was 7.0 (3.6–13.7) in the TBW and 12.1 (5.5–24.8) in the PF group (Fig. 3 a) The SEV showed a very similar pattern with a mean score of 90% in both groups (90 [88.9–95] in the TBW group and 90 [80–95] in the PF group (Fig. 3 b). The Wesley Score showed excellent results in 21 cases. 12 patients in the TBW group showed excellent results and eight showed good results, whereas nine cases in the PF group had excellent results and nine had good results.
Table 2.
Response variables.
| Total | TBW | PF | Effect estimate (TBW vs. PF) | p-value | |
|---|---|---|---|---|---|
| Weseley | 0.461 | ||||
| fair | 2 | 0 | 2 | ||
| good | 17 | 8 | 9 | ||
| excellent | 21 | 12 | 9 | ||
| Morrey (Median [IQR]) | 98 (92–100) | 99.5 (95–100) | 97 (91.5–99.3) | 0.05 (−0.54 - 0.64) | 0.867 |
| Mayo (Median [IQR]) | 100 (85–100) | 100 (92.5–100) | 100 (85–100) | 0.00 (−0.70 - 0.69) | 0.993 |
| DASH (Median [IQR]) | 9.9 (4.1–20.4) | 7.0 (3.6–13.7) | 12.1 (5.5–24.8) | −0.02 (−0.62 - 0.58) | 0.948 |
| SEV in % | 90 (80–95) | 90 (88.9–95) | 90 (80–95) | 0.00 (−0.61 - 0.61) | 0.995 |
| Time of return to work (mean ± sd) | 8.5 ± 5.2 | 6.5 ± 2.2 | 10.9 ± 6.6 | −2.07 (−6.81 - 2.67) | 0.372 |
| Extension deficit in % (Median [IQR]) | 5 (0–10) | 5 (0–10) | 10 (3.8–11.3) | −0.34 (−0.97 - 0.29) | 0.290 |
| Flexion in % (Median [IQR]) | 5 (0–15) | 5 (0–15) | 5 (0–20) | −0.12 (−0.80 - 0.56) | 0.735 |
| Complications | 13 (32.5%) | 8 (40%) | 5 (25%) | 0.0248 | |
Fig. 3.
Outcome analysis. a: DASH Score in TBW and PF group. b: Subjective elbow function according to operation technique. c: Time to return to work in weeks in both groups. d: Wesley score in three categories form fair to excellent in both operational groups.
(Fig. 3 d). The complication rate was 32.5% in all cases. The majority of complications in both groups were either implant-associated pain or mechanical blocking. The time to return to work was 6,5 ± 2,5 weeks in the TBW group and 10,9 ± 6,6 weeks in the PF group (p = 0.372) (Fig. 3 c).
4. Discussion
This paper focuses on two possible operative strategies for olecranon fractures. Compromised soft tissue, implant migration and high complication rates are some issues involved with restoring a pain-free and functional joint. A systematic review found that there is insufficient evidence for robust conclusions on the effects of different surgical treatment options. Studies comparing options in treatment, including patient-reported follow-up data on the effects of plates versus tension band wiring, are not numerous.27
In our cohort, both groups showed good to excellent outcomes regardless of which scoring system was used. There were no significant differences in complication rates, the period of hospitalisation or time to return to work. Also, the SEV was used as a simpler tool to measure functional outcome and satisfaction rates and showed high scores in both cohorts.
Recent clinical studies show mixed results concerning outcomes of TBW and PF. DelSole et al. found excellent functional outcomes after TBW and PF of olecranon fractures but slightly worse extension and time to union in patients undergoing PF. The authors stated that TBW outperformed plate osteosynthesis for patients with Mayo IA-IIIA fractures.28 Another study including 78 patients compared TBW and PF in simple and comminuted displaced fractures. The clinical outcome in both groups was described as excellent/good with low pain levels and minimal loss of functionality. Hardware removal was more frequently performed in the TBW group, and the complication rate was 29% in all patients.29 Both studies named an overlapping of the same fracture patterns that were treated either by TBW or PF, showing that no clear algorithm exists to determine when each technique is appropriate. A randomised trial involving 67 patients also showed no significant difference in DASH Score in a follow-up of one year. The complication rate was significantly higher in the TBW group due to symptomatic metalwork, while serious complications only occurred in the PF group.30
Some of these results match our findings, especially concerning the positive functional outcomes in both groups and the practicality of both techniques. Our findings showed a complication rate of 32.5% (n = 13) in all cases, although the rate was higher in the TBW group, with 40% compared to 25% in the PF group. Complications associated with metalwork were the most common (in 10 cases [25%]), of which most patients had been treated with TBW (n = 7). Infections occurred in two cases, both in the PF group. It is notable that the high complication rates do not appear to jeopardise a good or even excellent functional outcome for the patient.
The literature describes migration of K-wires, non-union, osteoarthritis and postoperative reduced range of motion, especially for extension, as the most common complications. The complication rates range between 19 and 82% with high rates of reoperation due to the subcutaneous position of the olecranon and prominent metalwork as common causes of patient discomfort after successful treatment.31,32 Edwards et al. reported an overall rate of implant removal after TBW or PF of 64.5% 19 months after surgery, with 39% of the patients without metal removal still describing functional impairment caused by the implant. 78% of patients who underwent removal had their metal removed by a surgeon other than the one who performed the original surgery, showing that removal rates may be much higher than expected.33 In conclusion, metal-related pain or loss of function is an expected reason for reoperation after TBW and PF after olecranon fractures without a verifiable negative impact on the long-term outcome.
Traditionally, simple fractures have been treated with tension band wiring, whereas plates are used in more complex or comminuted fractures. However, some data show positive clinical results using TBW in comminuted fractures and PF in non-comminuted fractures, so the choice of technique for operative therapy remains controversial.29,34 Biomechanical evaluations found greater interfragmentary compression and lower risk of secondary displacement in PF compared to TBW.35 Recent literature recommends pre-contoured locking plate systems for optimal fixation options even in poor-quality bone, whereas one-third tubular plates are thin and can fail under high-bending loads.36 Nevertheless, TBW is a widely-used option with lower material costs and, according to many reports, shorter surgery durations. However, no technique can yet be named the gold standard.
To evaluate functional outcome after elbow surgery, several tools are used, of which the DASH Score is most common. It is distinctive in its ability to detect changes in disability over time after elbow surgery and can be seen as a better endpoint for outcome evaluation than factors like reoperation or complications.11,28 As an alternative, the SEV is an easily administered score that shows a strong correlation to objective scoring systems like the Mayo elbow performance score.37 We found the SEV to be a fast, responsive and valid tool in daily clinical practice.
In some cases, a non-operative treatment can be an alternative to the examined techniques. This involves a cuff and collar sling or arm plaster in about 60° flexion of the elbow joint combined with supervised physiotherapy for mobilisation. A prospective randomised trial of non-operative versus operative management of olecranon fractures in elderly patients was stopped prematurely because of an unacceptably high complication rate of 82% in the operative treatment group. Nevertheless, the collected data showed no significant difference concerning the mean DASH score with general good results after one year.38 Other data showed increased numbers of cases of olecranon fractures that were managed under non-operative treatment and good outcomes even in younger patients.39,40 Considering our results and experience and the literature, we recommend a non-operative procedure only in individual cases like non-displaced fractures in elderly patients or patients with low expectations for functionality. Frequent radiological and clinical follow-up examinations are necessary to detect non-union or secondary displacement.
A main limitation of this study is the retrospective study design and the limited number of cases. Another limitation is the limited comparability of the two patient groups due to varying surgical interventions based on fracture pattern. There is furthermore no optimal and standardised questionnaire to evaluate follow-up results after operative treatment of isolated olecranon fractures.
Our goal was to compare two standard surgical procedures on olecranon fractures to find an optimal therapy concept in individual cases. Both procedures are technically challenging, and success is related to multiple factors including physical demands, bone quality and fracture patterns. Our hypothesis was that PF patients would show significant inferior functional outcomes due to more complex injuries and surgical procedures. The surgery for plate fixation took significantly longer, but no negative influence could be detected. Even though outside studies as well as our own data showed high complication rates in surgical therapy, the long-term outcomes and satisfaction rates are high. The results were inadequate to determine which technique would be more suitable for a particular case, and further investigation is needed for more distinct therapy algorithms.
Conflicts of interest
The authors declare no conflict of interest.
Funding
The authors received no funding for this work.
Footnotes
This study was approved by the local institutional review board (Ethics Committee No 056/16).
References
- 1.Nowak T.E., Dietz S.O., Burkhart K.J., Müller L.P., Rommens P.M. Frakturen des Ellenbogengelenkes. Chir. 2012, Feb 1;83(2):181–198. doi: 10.1007/s00104-011-2198-1. [DOI] [PubMed] [Google Scholar]
- 2.Powell A.J., Farhan-Alanie O.M., Bryceland J.K., Nunn T. The treatment of olecranon fractures in adults. Musculoskelet Surg. 2017, Apr 1;101(1):1–9. doi: 10.1007/s12306-016-0449-5. [DOI] [PubMed] [Google Scholar]
- 3.Wilkerson J.A., Rosenwasser M.P. Surgical techniques of olecranon fractures. J Hand Surg. 2014, Aug;39(8):1606–1614. doi: 10.1016/j.jhsa.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 4.Niéto H., Billaud A., Rochet S. Proximal ulnar fractures in adults: a review of 163 cases. Injury. 2015, Jan;46(Suppl 1):S18–S23. doi: 10.1016/S0020-1383(15)70006-9. [DOI] [PubMed] [Google Scholar]
- 5.Amis A.A., Miller J.H. The mechanisms of elbow fractures: an investigation using impact tests in vitro. Injury. 1995, Apr;26(3):163–168. doi: 10.1016/0020-1383(95)93494-3. [DOI] [PubMed] [Google Scholar]
- 6.Unger A.C., Renken F., Gille J., Schulz A.P., Faschingbauer M., Jürgens C. Klassifikation und Therapie von ellengelenknahen Verletzungen. Trauma Berufskrankh. 2010, Dec 1;12(4):247–254. [Google Scholar]
- 7.Benetton C.A., Cesa G., El-Kouba Junior G., Ferreira A.P.B., Vissoci J.R.N., Pietrobon R. Agreement of olecranon fractures before and after the exposure to four classification systems. J Shoulder Elb Surg. 2015, Mar;24(3):358–363. doi: 10.1016/j.jse.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 8.Tamaoki M.J.S., Matsunaga F.T., Silveira J.D., Balbachevsky D., Matsumoto M.H., Belloti J.C. Reproducibility of classifications for olecranon fractures. Injury. 2014, Nov;45(Suppl 5):S18–S20. doi: 10.1016/S0020-1383(14)70015-4. [DOI] [PubMed] [Google Scholar]
- 9.Uhlmann M., Barg A., Valderrabano V., Weber O., Wirtz D.C., Pagenstert G. Behandlung von isolierten Olekranonfrakturen. Der Unfallchirurg. 2014, Jul 1;117(7):614–623. doi: 10.1007/s00113-013-2389-y. [DOI] [PubMed] [Google Scholar]
- 10.Colton C.L. Fractures of the olecranon in adults: classification and management. Injury. 1973, Nov;5(2):121–129. doi: 10.1016/s0020-1383(73)80088-9. [DOI] [PubMed] [Google Scholar]
- 11.Gummesson C., Atroshi I., Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Muscoskelet Disord. 2003, Jun 16;4:11. doi: 10.1186/1471-2474-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hudak P.L., Amadio P.C., Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996, Jun;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 13.Deliyannis S.N. Comminuted fractures of the olecranon treated by the Weber- Vasey technique. Injury. 1973, Aug;5(1):19–24. doi: 10.1016/s0020-1383(73)80004-x. [DOI] [PubMed] [Google Scholar]
- 14.van der Linden S.C., van Kampen A., Jaarsma R.L. K-wire position in tension- band wiring technique affects stability of wires and long-term outcome in surgical treatment of olecranon fractures. J Shoulder Elb Surg. 2012, Mar;21(3):405–411. doi: 10.1016/j.jse.2011.07.022. [DOI] [PubMed] [Google Scholar]
- 15.Schneider M.M., Nowak T.E., Bastian L. Tension band wiring in olecranon fractures: the myth of technical simplicity and osteosynthetical perfection. Int Orthop. 2014, Apr;38(4):847–855. doi: 10.1007/s00264-013-2208-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schliemann B., Raschke M.J., Groene P. Comparison of tension band wiring and precontoured locking compression plate fixation in Mayo type IIA olecranon fractures. Acta Orthop Belg. 2014, Mar;80(1):106–111. [PubMed] [Google Scholar]
- 17.Hume M.C., Wiss D.A. Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation. Clin Orthop. 1992, Dec;(285):229–235. [PubMed] [Google Scholar]
- 18.Matar H.E., Ali A.A., Buckley S., Garlick N.I., Atkinson H.D. Surgical interventions for treating fractures of the olecranon in adults. Cochrane Database Syst Rev. 2014, Nov 26;(11):CD010144. doi: 10.1002/14651858.CD010144.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Larsen E., Lyndrup P. Netz or Kirschner pins in the treatment of olecranon fractures? J Trauma. 1987, Jun;27(6):664–666. doi: 10.1097/00005373-198706000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Macko D., Szabo R.M. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am. 1985, Dec;67(9):1396–1401. [PubMed] [Google Scholar]
- 21.Jung W., Schofer M., Kortmann H.-R. Differenzierte Therapie bei Olekranonfrakturen. Trauma Berufskrankh. 2003, Mar 1;5(1):13–20. [Google Scholar]
- 22.Buckley R.E., Moran C.G., Rüedi T. second ed. Thieme; Stuttgart: 2007. AO Principles of Fracture Management: Vol. 1: Principles, Vol. 2: Specific Fractures; p. 1112. [Google Scholar]
- 23.Hak D.J., Golladay G.J. Olecranon fractures: treatment options. J Am Acad Orthop Surg. 2000, Aug;8(4):266–275. doi: 10.5435/00124635-200007000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Prayson M.J., Iossi M.F., Buchalter D., Vogt M., Towers J. Safe zone for anterior cortical perforation of the ulna during tension-band wire fixation: a magnetic resonance imaging analysis. J Shoulder Elb Surg. 2008, Jan 1;17(1):121–125. doi: 10.1016/j.jse.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 25.Cusick M.C., Bonnaig N.S., Azar F.M., Mauck B.M., Smith R.A., Throckmorton T.W. Accuracy and reliability of the Mayo elbow performance score. J Hand Surg. 2014, Jun;39(6):1146–1150. doi: 10.1016/j.jhsa.2014.01.041. [DOI] [PubMed] [Google Scholar]
- 26.Offenbächer M., Ewert T., Sangha O., Stucki G. Validation of a German version of the “disabilities of arm, shoulder and hand” questionnaire (DASH-G) Z Rheumatol. 2003, Apr;62(2):168–177. doi: 10.1007/s00393-003-0461-7. [DOI] [PubMed] [Google Scholar]
- 27.Matar H.E., Ali A.A., Buckley S., Garlick N.I., Atkinson H.D. Surgical interventions for treating fractures of the olecranon in adults. Cochrane Database Syst Rev. 2014, Nov 26;(11):CD010144. doi: 10.1002/14651858.CD010144.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DelSole E.M., Pean C.A., Tejwani N.C., Egol K.A. Outcome after olecranon fracture repair: does construct type matter? Eur J Orthop Surg Traumatol Orthop Traumatol. 2016, Feb;26(2):153–159. doi: 10.1007/s00590-015-1724-0. [DOI] [PubMed] [Google Scholar]
- 29.Tarallo L., Mugnai R., Adani R., Capra F., Zambianchi F., Catani F. Simple and comminuted displaced olecranon fractures: a clinical comparison between tension band wiring and plate fixation techniques. Arch Orthop Trauma Surg. 2014, Aug;134(8):1107–1114. doi: 10.1007/s00402-014-2021-9. [DOI] [PubMed] [Google Scholar]
- 30.Duckworth A.D., Clement N.D., White T.O., Court-Brown C.M., McQueen M.M. Plate versus tension-band wire fixation for olecranon fractures: a prospective randomized trial. J Bone Joint Surg Am. 2017, Aug 2;99(15):1261–1273. doi: 10.2106/JBJS.16.00773. [DOI] [PubMed] [Google Scholar]
- 31.Naam N.H. CORR Insights(®): factors associated with reoperation after fixation of displaced olecranon fractures. Clin Orthop. 2016, Jan;474(1):201–203. doi: 10.1007/s11999-015-4554-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ren Y.M., Qiao H.Y., Wei Z.J. Efficacy and safety of tension band wiring versus plate fixation in olecranon fractures: a systematic review and meta-analysis. J Orthop Surg. 2016, Nov 14;11(1):137. doi: 10.1186/s13018-016-0465-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Edwards S.G., Cohen M.S., Lattanza L.L. Surgeon perceptions and patient outcomes regarding proximal ulna fixation: a multicenter experience. J Shoulder Elb Surg. 2012, Dec;21(12):1637–1643. doi: 10.1016/j.jse.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 34.Chalidis B.E., Sachinis N.C., Samoladas E.P., Dimitriou C.G., Pournaras J.D. Is tension band wiring technique the “gold standard” for the treatment of olecranon fractures? A long term functional outcome study. J Orthop Surg. 2008, Feb 22;3:9. doi: 10.1186/1749-799X-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilson J., Bajwa A., Kamath V., Rangan A. Biomechanical comparison of interfragmentary compression in transverse fractures of the olecranon. J Bone Joint Surg Br. 2011, Feb;93(2):245–250. doi: 10.1302/0301-620X.93B2.24613. [DOI] [PubMed] [Google Scholar]
- 36.Wagner F.C., Konstantinidis L., Hohloch N., Hohloch L., Suedkamp N.P., Reising K. Biomechanical evaluation of two innovative locking implants for comminuted olecranon fractures under high-cycle loading conditions. Injury. 2015;46(6):985–989. doi: 10.1016/j.injury.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 37.Schneeberger A.G., Kösters M.C., Steens W. Comparison of the subjective elbow value and the Mayo elbow performance score. J Shoulder Elb Surg. 2014, Mar;23(3):308–312. doi: 10.1016/j.jse.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 38.Duckworth A.D., Clement N.D., McEachan J.E., White T.O., Court-Brown C.M., McQueen M.M. Prospective randomised trial of non-operative versus operative management of olecranon fractures in the elderly. Bone Jt J. 2017, Jul;99– B(7):964–972. doi: 10.1302/0301-620X.99B7.BJJ-2016-1112.R2. [DOI] [PubMed] [Google Scholar]
- 39.Putnam M.D., Christophersen C.M., Adams J.E. Pilot report: non-operative treatment of Mayo Type II olecranon fractures in any-age adult patient. Shoulder Elb. 2017, Oct;9(4):285–291. doi: 10.1177/1758573217711889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Motisi M., Kurowicki J., Berglund D.D. Trends in management of radial head and olecranon fractures. Open Orthop J. 2017;11:239–247. doi: 10.2174/1874325001711010239. [DOI] [PMC free article] [PubMed] [Google Scholar]