Abstract
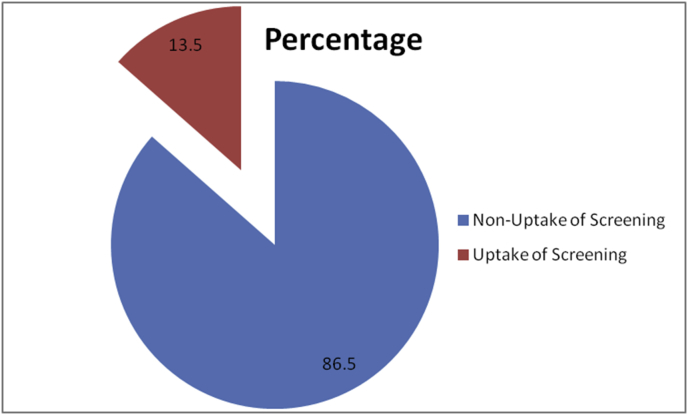
Despite the empirical evidence that cervical cancer screening has been a successful public health initiative to secondarily prevent the incidence and mortality from cervical cancer in developed nations, majority of women of sub-Saharan root, Nigeria inclusive, do not utilize this essential health service. This study/article contributes to the empirical literature on the drivers of cervical cancer screening utilization within Nigeria context. The paper investigates the determinants of cervical cancer screening utilization among both working class women and women involved in trading activities in Oyo state, Nigeria. The statistical estimations find strong support for attitudinal correlates, perceived seriousness and family history as drivers of utilization of cervical cancer screening. While only 13.5% of respondents reported to have ever utilized the screening test, majority had positive attitude towards the screening. The screening uptake among the women could improve, if necessary barriers are addressed. The paper highlights policy recommendations for enhancing organized screening guidelines in a developing country.
Keywords: Cancer research, Health sciences, Social sciences, Women, Screening, Nigeria, Cervical cancer
Cancer research; Health sciences; Social sciences; Women; Screening; Nigeria; Cervical cancer
1. Introduction
The Sustainable Development Goals (SDGs) clearly recognize the need to urgently address the incidence and mortality associated with Non-Communicable Diseases (NCDs), of which cancer contributes a great deal. Globally, there has a been steady increase of 12 million cases of cancer in 2008 to over 14 million cases in 2012; and a corresponding increasing mortality rate (Ahrens, Pohlabeln, Foraita, Nelis et al., 2014). Subsequently, Bray (2014) projects an estimate of over 20 million new cancer cases expected annually by 2025. Out of the numerous types of cancer, cervical cancer is the fourth-most common cancer among women globally and accounts for largest cause of female cancer deaths (World Cancer Report, 2014). According to Okunnu (2010), one woman dies of cervical cancer every two minutes worldwide, and 80% of these deaths occur in developing nations.
Cervical cancer has been a major public health menace to women of all age groups in Sub-Saharan Africa (Akinremi et al., 2005; Awodele et al., 2011). To further worsen the case in Sub-Saharan Africa, most cervical cancer cases are discovered in late stages due to low level of knowledge, unhealthy cultural beliefs and non-availability of preventive services (Kidanto et al., 2002). The disparities in cervical cancer incidence and mortality between the developed and developing countries are further evident in the recent global cancer statistics which reported steady increase in sub-Saharan Africa (IARC/WHO, 2013).
Nigeria, the most populous country in Africa with an estimated population above 166 million in 2012 (National Bureau of Statistics, 2013) and with an estimated total population of 40.43 million women aged between 15-49 years is rated tenth in cervical cancer mortality worldwide (Okoye, 2014). It has been reported as the second most common cancer among Nigerian women after breast cancer and it largely contribute to the burden of mortality from females cancers among women in their reproductive years (Adebamowo and Adekunle, 1999; Castellsague, et al., 2007). In Nigeria, 53.3 million women are estimated to be at risk of developing cervical cancer (IARC/ICO, 2017) with a national standardized prevalence rate of 33.0 per 100,000. The Yoruba speaking people of Southwest Nigeria describes cervical cancer as “Jejere enu ile omo” literally meaning cancer of the narrow opening of the womb. Empirical evidence suggests that cervical cancer is common in Nigeria partly due to some socio-cultural practices of early marriage and onset of sexual activities (Ezem, 2007; Ebughe et al., 2016).
The devastating situation of cervical cancer in Nigeria is not limited to the high incidence and mortality rate of the disease, but also of greater concern is low level of awareness of ways to prevent a woman from having cervical cancer which could be though primary prevention (Human Pappiloma Virus {HPV} vaccine) and secondary prevention (cervical cancer screening). This is quite critical because of limited infrastructure for effective treatment for invasive cervical cancer particularly when diagnosed in late stages. This is evident in Musa et al. (2016) whose study showed that majority of cancers in Nigeria are detected at advanced stages with low survival probability. In addition, the situation where majority of citizens have no health insurance coverage, even among the few with health insurance coverage, screening for cervical cancer and HPV vaccine are not covered by the National Health Insurance Scheme (NHIS) (Ewelukwa et al., 2013; Wright et al., 2011). Considering the high poverty level (48.4%) in Nigeria (World Bank, 2014), out-of-pocket payment for screening services which usually cost between 2,500 and 10,000 Naira (depending on the location of screening) is a great deal of money to part with (Obom-Egbulem, 2010). The cost for such life-saving preventive and therapeutic services, implicitly limits the utilization of cervical cancer services which could contribute to late presentation of abnormal changes and growth in the cervix with often little chance of survival (Musa, 2017).
Additionally, there are several related social, cultural and religious factors that negatively affect the attitude of individuals towards health preventive services. The cultural and religious beliefs of Nigerians include “confessing the positive” and “rejecting the negative” of any circumstance and projecting the occurrence of negative occurrence to their perceived “enemies”, thus, inhibiting positive health-seeking behaviour such as cervical cancer screening. It is within these existing knowledge gaps that this paper intends to contribute. Therefore, the concern of this article is to research into the drivers of uptake of cervical cancer screening among women in Nigeria with careful consideration of the attitudinal correlates and perceived seriousness of cervical cancer. The article further explores the mediating role of educational qualification of respondents, income level and family history of cervical cancer as factors determining the utilization of such an essential service. The article is structured as follows. The second section discusses the objectives of the study. Section 3 specifies the methodology adopted for the study. Section 4 reports the analysis of data and discussion of results. Section 5 concludes and suggests policy recommendations.
2. Materials and methods
2.1. Sample and sampling procedure
For the purpose of this study, a structured questionnaire to obtain information from Nigerian women was designed, validated and administered. The survey took place between November 2017 and January 2018 among 1004 respondents. The sampling of respondents used a multistage systematic random sampling technique. The sample size was determined using Charan and Biswas (2013)'s method for studies with unknown target population and variables of interest that can be classified into groups or levels. Where N = [Z2 x P (1-P)]/ε2. For this study, the sample size was calculated as N = 1.962 × 0.70 × 0.30/0.032 = 896. However, twelve percent of the calculated sample size was included to accommodate for attrition and incomplete responses, which is 12% of 896 = 104. Hence, 1004 copies of questionnaire were distributed on the field. However, after data collection, 852 questionnaires were found to be completely filled and suitable for data analysis. This study was carried out in Ibadan, one of the most populous cities in Nigeria with inhabitants of diverse backgrounds, socio-economic status and ethnic background. Ibadan has eleven local government areas, consisting of five urban local government areas in the city (Ibadan North, Ibadan North East, Ibadan North West, Ibadan South East and Ibadan South West) and six semi-urban local government areas (Akinyele, Egbeda, Ido, Lagelu, Ona Ara and Oluyole). The study employed the probability proportionate sampling technique and multi-stage random sampling technique in determining the number of women to participate from each local government area. This proportion is based on the size of each local government areas. Subsequently, government institutions and markets used were purposively selected across all the eleven local government areas. In order to ensure proportionate representation of study sample size, seven hundred (700) participants were systematically drawn from government institutions while 304 women were systematically drawn from market places.
The Institutional Ethical Review Committee of Obafemi Awolowo University, Ile-Ife, under the Institute of Public Health gave approval for the conduct of this study. The study was approved to be carried out with approval number IPH/OAU/879. In addition, verbal permission was obtained from the market leaders of the respective markets visited and permissions were also obtained from the Chairmen of the Local government secretariats where questionnaires were administered. Furthermore, verbal and signed informed consent was obtained from each respondent and anonymity was maintained.
2.2. Instruments
Uptake of Cervical Cancer Screening: The participant's uptake of cervical cancer screening was assessed by classification of the respondent's screening behaviour. Positive screening behaviour takes the value of 1 and 0 if otherwise. The items were adapted from Ndejjo et al. (2016) study that measured the uptake of cervical cancer screening associated factors among Women in Uganda and Ahmed et al. (2013) whose study assessed the knowledge, attitude and practice of cervical cancer screening among market women in Zaria, Nigeria. Those who reported ever screened even if once in their lifetime were regarded as having uptake of cervical cancer screening and those who had never screened were regarded as having no uptake of screening. In the analysis, a response of YES was represented with 1 while a response of NO was coded with 0. Participants were asked to rate the item based on their individual uptake of cervical cancer screening, likely barriers to non-participation, reasons for non-participation and frequency of uptake of the service.
Attitude towards Cervical Cancer Screening: The attitude towards cervical cancer screening was measured using an 11-item scale that contained both negatively and positively worded questions. The scale had 12 items with four Likert scale response categories with positive and negative responses with Likert scale response format: strongly agree, agree, disagree and strongly disagree. The following scoring system was used with respects to respondents’ responses: strongly agree 4, agree 3, disagree 2, strongly disagree 1. This scale is adapted from Ehiemere et al. (2015) whose study measured the attitude and practice of cervical cancer screening among female health workers in an hospital setting. The responses of the respondents were summed up and a total score obtained for each respondent. The mean score was calculated as 28.6. Respondents with a score above the mean of 29 were reported to have a positive attitude and scores below the mean of 29 was categorized as a negative attitude towards screening for cervical cancer screening. For data coding, the negative attitude was coded 0 while the positive attitude was coded 1.
Family History: This variable was measured by asking respondents if there has ever been a family member with history of cervical cancer, either living or dead. A positive response was coded as 1 while the alternative was coded as 0.
Educational Level: This served as a moderating variable in the study where the respondents were asked of their highest educational attainment. It was categorized as No formal education, secondary education and Tertiary Education.
Income Level: This also served as a moderating variable in the study where respondents were categorized into low income earners, lower middle income earners, upper middle income earners and upper income earners as adapted from Abdulraheem and Parakoyi (2009).
2.3. Estimation techniques
Descriptive analysis was used to discuss the women's family history of cervical cancer screening, income level and highest level of education. Also, the intention to go for screening using the theory of Planned Behaviour was explored. The dependent variable, Uptake of Screening takes the value of 1 if, in their lifetime and 0 otherwise. The drivers of screening uptake were analysed using binary logistic regression. It examined the relationship between multiple explanatory variables and a dichotomous dependent variable and estimates the probability of occurrence of an event (screening uptake) by fitting data to a logistic curve (seeTables 1 and 3).
Table 1.
Variables used in the study.
| Variable Name | Variable Description | N | Min | Max | Mean | SD |
|---|---|---|---|---|---|---|
| Dependent Variable | ||||||
| Uptake of Cervical Cancer Screening | 1 Ever gone for screening, 0 Never gone for screening |
852 | 0 | 1 | ||
| Independent Variables | ||||||
| Attitude | 1 Positive Attitude 0 Negative Attitude |
852 | 7 | 40 | 28.6 | 4.77 |
| Perceived Seriousness | 1 High 0 Low |
852 | 1 | 12 | 6.6 | 1.94 |
| Family History of Cervical Cancer | 1 Yes 0 No |
852 | 0 | 1 | ||
| Income Level | 1 Low income earners 2 Lower Middle Income earners 3 Upper Middle Income earners 4 High Income earners |
852 | 1 | 4 | 52,319 | 21,885 |
| Highest educational level | 0 No formal education 1 Secondary education 2 Tertiary Education |
852 | 0 | 2 | ||
Table 3.
Distribution of respondents on screening behaviour and barriers to screening.
| Variable | % |
|---|---|
| Screening Uptake | 13.5 |
| Reasons for uptake of screening | |
| Can afford it | 42.6 |
| My doctor recommends it | 44.4 |
| I don't want to die from cervical cancer | 42.4 |
| If detected early, it can be cured | 34.3 |
| My family encourages me to do it | 24.0 |
| I could have the disease | 16.2 |
| Lost a close relatives | 8.2 |
| Lost a close friend | 7.2 |
| Non-uptake of Screening | 86.5 |
| Reasons for non-uptake of cervical cancer screening | |
| I don't have the money | 38.1 |
| No centre around my house | 30.0 |
| My religion forbids it | 24.4 |
| Not aware it existed | 23.9 |
| Afraid of positive result | 19.0 |
| It is painful | 16.3 |
| I will if medical personnel is a female | 14.2 |
| It is embarrassing | 11.1 |
| My husband will not approve it | 5.7 |
| My culture forbids it | 2.2 |
| I'm not at risk | 2.2 |
| Because I have been vaccinated | .3 |
| I need more orientation | .3 |
∗Multiple responses. (Author's Survey, 2018)
3. Results and discussion
3.1. Analysis
The analysis in Table 2 shows the background information on both women who uptake screening and women with non-uptake of screening. Respondent's screening behaviour was compared with some determining factors; the analysis consistently indicates non-screening behaviour among the women despite high positive attitude, high level of education and high level of perceived seriousness of cervical cancer. This analysis illustrate that the level of uptake is low generally, even among women who reported positive attitude towards the screening. For instance, when comparing respondent's attitude to cervical cancer screening and their utilization of cervical cancer screening, it was reported that 83.9% of women with positive attitude do not uptake cervical cancer screening. However among women with negative attitude, 16.1% do not uptake the screening.
Table 2.
Comparative analysis of screening behaviour of respondents with independent variables.
| Variable | Non- Uptake N (%) |
Uptake N (%) |
|---|---|---|
| Attitude towards Screening | ||
| Negative Attitude | 108 (16.1) | 5 (4.9) |
| Positive Attitude | 561 (83.9) | 98 (95.1) |
| Perceived Seriousness | ||
| Low | 431 (65.5) | 52 (50.5) |
| High | 227 (34.5) | 51 (49.5) |
| Family History of Cervical Cancer | ||
| No | 626 (98.3) | 100 (97.1) |
| Yes | 11 (1.7) | 3 (2.9) |
| Monthly Earnings | ||
| Low Income earners | 80 (20.1) | 4 (5.4) |
| Lower Middle Earners | 221 (55.5) | 46 (62.2) |
| Upper Middle Earners | 77 (19.3) | 18 (24.3) |
| High Income earners | 20 (5.0) | 6 (8.1) |
Furthermore, the relationship between respondent's perception of how serious cervical cancer is and their uptake of cervical cancer screening were investigated. The analysis shows that among women who do not uptake cervical cancer screening, about 66% of them perceive cervical cancer to be less serious when compared to 34% of them who perceive it as highly serious.
Figure 1 describes the low percentage (13.5%) of women who has ever presented themselves for cervical cancer screening in the study area. This is consistent with studies across the country reporting an abysmal low rate of cervical cancer screening uptake. The study further examined the reasons why the screening services were not being utilized. Majority of the women reported barriers such as financial constraints, fear of positive result, as well as religious and cultural beliefs as prominent reasons for non-uptake of cervical cancer screening. For the women who uptake the screening, some of the motivators included doctor's recommendation, affordability and fear of death through cancer. This suggests that with intense awareness creation programmes in the hospital environment, the likelihood of future uptake could be enhanced.
Figure 1.
A display of respondent's Screening Behaviour.
3.2. Statistical analysis of the drivers of screening uptake
3.2.1. Attitudinal correlates
Results emerging from the analysis in Table 4 give a significant credence to the influence of attitudinal dispositions on screening uptake. The result implies that women with negative attitude towards cervical cancer screening as a preventive health services are 78% times less likely to uptake cervical cancer screening when compared with women with positive attitude (see Table 4). The results of this study support findings in similar studies such as (AlSairafi and Mohammed, 2009; Dormandy et al., 2005), where positive attitude is correlated with prompt and regular uptake of cervical cancer screening. It is also observed that the findings differ significantly from what was reported in Varadheswari, Dandekar & Sharanya (2015), possibly as a result of cultural differences. The discrepancies in findings could be as a result of cultural differences because culture, values and ways of life have strong influences on one's attitude and subsequently health seeking behaviour.
Table 4.
Binary logistic regression of the drivers of cervical cancer screening uptake among women in Nigeria.
| Variable | Odd Ratio | 95% C.I. | p-value |
|---|---|---|---|
| Attitude | |||
| Positive (RC) | 1 | 1 | 1 |
| Negative |
.219 |
.077–.625 |
.005 |
| Perceived Seriousness of cervical cancer | |||
| High (RC) | 1 | 1 | 1 |
| Low | .584 | .345–.988 | .045 |
| Family History | |||
| Yes (RC) | 1 | 1 | 1 |
| No |
.586 |
.161–2.136 |
.418 |
| Monthly Earnings | |||
| High Income Earners (RC) | 1 | 1 | 1 |
| Low I.E. | .214 | .054–.839 | .027 |
| Middle I.E. | .897 | .336–2.395 | .829 |
| Upper Middle I.E. | .993 | .341–2.892 | .989 |
∗Nagelkerke R square = .098, -2 Log likelihood = 369.245, Hosmer and Lemeshow Test = .850. (Author's Survey, 2018)
3.2.2. Perceived seriousness and screening uptake
Perceived seriousness, also known as perceived severity refers to the negative consequences an individual associates with an event or outcome, such as a diagnosis of cancer (National Cancer Institute). This study further extends the analysis to find out how much of an influence the perceived seriousness of cervical cancer by women could drive the uptake of cervical cancer screening. Analysis in binary logistic regression Table 4 shows that women who perceive cervical cancer as less serious are 41% less likely to uptake cervical cancer screening when compared with women who perceive cervical cancer as highly serious. This finding projects as another significant driver of screening uptake among the women. This supports the postulation of Health Belief Model (HBM) associating an individual's belief about the severity of a disease with his/her health seeking behaviour. According to the HBM, threat perception drives behaviour but the particular action taken is coupled with the beliefs about the behavioural options available to counter the threat. Similar to this present study's findings, Zewdie et al. (2012) in a qualitative study found high level of perceived severity of cervical cancer in the community and yet, low uptake of cervical cancer screening because of major beliefs in the disease being caused by a breach of social taboo.
3.2.3. Family history and screening uptake
In this study, a non-significant association was analyzed between family history of cervical cancer and uptake of cervical cancer screening. This can be interpreted as the history of cervical cancer in a woman's family did not predict the uptake of cervical cancer screening.
3.2.4. Monthly earnings and screening uptake
The study further examined the relationship between the monthly earnings of respondents and their screening uptake with the help of binary logistic analysis. The result shows a significant relationship between the two variables, that is women with low income earnings, lower middle income earners and upper middle income earners are less likely to go for screening of cervical cancer when compared to women that are high income earners. The cost of screening was reported as one of the significant barriers to screening by majority of the women in study area as screening costs between 2500naira and 7500naira. Many women however reported that they will be willing to screen if it is free or subsidized. This outcome is consistent with those in some studies carried out in India by Nene et al. (2007) and Gichangi et al. (2003) where it was reported that increased socio-economic status place the women population in a better position economically and knowledge-wise thus increasing the likelihood of them seeking for cervical screening. This situation is also similar to what obtains in the present study's area where most women struggle to earn a living; hence the cost of screening or perceived high cost might discourage some women from utilizing the screening. The present study also affirms the findings of Kritpetcharat et al. (2003) which found although a negative relationship between women's level of income and screening uptake, the study reported women with higher income levels were less likely to participate in the visual inspection based screening. The similarities in influence of income on uptake of screening in both studies could be as a result of similar level of economic development parameters in both Nigeria and India.
4. Conclusion
Health seeking behavior entails both primary and secondary prevention strategies which offer the opportunity for comprehensive prevention of illnesses such as cervical cancer. Cervical cancer screening has been proven to help in the early detection and prevention of cancer of cervix, yet it is underutilized among the study population. This study has shown that screening uptake was very low despite the reported high perception of seriousness of the disease and positive attitude towards screening. The study revealed that awareness of cancer, cervical cancer, and cervical cancer screening in terms of sheer awareness of the existence of the disease among the respondents was high. Reported major barriers to screening were fear of negative results, the perceived pain of the procedure as well as religious and cultural barriers, including being attended to by a male medical personnel. Few women were also of the opinion that they did not feel at risk of cervical cancer and others were afraid of being labeled as promiscuous.
This study therefore concludes that there is need for improved educative intervention programmes from health professionals to women at risk of having cervical cancer in order to eradicate false beliefs and subsequently reduce incidence and mortality accrued to cervical cancer in Nigeria.
Declarations
Author contribution statement
Ilevbare, Oluwatosin E.: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Adegoke, A.A.: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Adelowo, C.M.: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
Data associated with this study has been deposited at Obafemi Awolowo University, Ile-Ife, Library under the accession number SSP 13/14/H/0665.
References
- Abdulraheem I.S., Parakoyi D.B. Factors affecting mother’s healthcare-seeking behaviour for childhood illnesses in a rural Nigerian Setting. Early Child. Dev. Care. 2009;179(5):671–683. [Google Scholar]
- Adebamowo C., Adekunle O. Case controlled study of the epidemiological risk factors for breast cancer in Nigeria. Br. J. Surg. 1999;86:665–668. doi: 10.1046/j.1365-2168.1999.01117.x. [DOI] [PubMed] [Google Scholar]
- Ahmed S.A., Sabitu K., Idris S.H., Ahmed R. Knowledge, attitude and practice of cervical cancer screening among market women in Zaria, Nigeria. Niger. Med. J. 2013;54(5):316–319. doi: 10.4103/0300-1652.122337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinremi T.O., Nazeer S., Totsch M. Reduced alcohol use in the staining of Pap smears: a satisfactory low-cost protocol for cervical cancer screening. Acta Cytol. 2005;49(2):169–172. doi: 10.1159/000326127. [DOI] [PubMed] [Google Scholar]
- AlSairafi M, Mohammed F.A. Knowledge, attitudes, and practice related to cervical cancer screening among Kuwaiti women. Med. Princ. Pract. 2009;18(1):35–42. doi: 10.1159/000163044. [DOI] [PubMed] [Google Scholar]
- Awodele O., Adeyomoye A.A.A., Awodele D.F., Kwashi V., Awodele I.O., Dolapo D.C. A study on cervical cancer screening amongst nurses in Lagos university teaching hospital, Lagos, Nigeria. J. Canc. Educ. 2011;26(3):497–504. doi: 10.1007/s13187-010-0187-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray F. Transitions in human development and the global cancer burden. In: Wild C.P., Stewart B., editors. World Cancer Report 2014. International Agency for Research on Cancer; Lyon: 2014. [Google Scholar]
- Castellsague S. HPV and cervical cancer in the Report. Vaccine. 2007:C1–230. doi: 10.1016/S0264-410X(07)01183-8. [DOI] [PubMed] [Google Scholar]
- Charan J., Biswas T. How to calculate sample size for different study designs in medical research. Indian J. Psychol. Med. 2013;35(2):121–126. doi: 10.4103/0253-7176.116232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dormandy E, Michie S, Hooper R, Marteau T. Low Uptake of Prenatal screening for Down Syndrome in minority ethnic groups and socially deprived groups: a reflection of women’s attitudes or a failure to facilitate informed choices? Int. J. Epidemiol. 2005;34(2):346–352. doi: 10.1093/ije/dyi021. [DOI] [PubMed] [Google Scholar]
- Ebughe G.A., Ekanem I.A., Omoronyina O.E., Omotoso A.J., Ago B.U., Agan T.U., Ugbem T.I. Incidence of cervical cancer in Calabar, Nigeria. J. Canc. Tumor Int. 2016;3(2) [Google Scholar]
- Ehiemere I.O., Maureen D.F., Robinson-Bassey G.C. Attitude and practice of cervical cancer screening among female health workers in university of Port-Harcourt teaching hospital, Rivers State. J. Res. Nurs. Midwifery (JRNM) 2015;4(4):072–082. [Google Scholar]
- Ewelukwa O., Onoka C., Onwujekwe O. Viewing health expenditures, payment and coping mechanisms with an equity lens in Nigeria. BMC Health Serv. Res. 2013;13(1):87. doi: 10.1186/1472-6963-13-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezem B. Awareness and uptake of cervical cancer screening in Owerri, South-Eastern Nigeria. Ann. Afr. Med. 2007;6:94–98. doi: 10.4103/1596-3519.55727. [DOI] [PubMed] [Google Scholar]
- Gichangi P., Estambale B., Bwayo J. Knowledge and practice about cervical cancer and Pap smear among patients at Kenyatta National Hospital, Nairobi. Int. J. Gynecol. Canc. 2003;13:827–833. doi: 10.1111/j.1525-1438.2003.13612.x. [DOI] [PubMed] [Google Scholar]
- IARC/ICO Information Centre on HPV and Cancer . 2017. Human PappilomaVirus and Related Cancers, Fact Sheet 2017. [Google Scholar]
- IARC/World Health Organization . Global Cancer burden Rises to 14. 1 Million New Cases in 2012: Marked increase in breast cancers must be addressed. 2013. Latest world cancer statistics. press release. [Google Scholar]
- Kidanto H.L., Kilewo C.M, Moshiro C. Cancer of the cervix: knowledge and attitudes of female patients admitted at Mwuhimbili National Hospital, Dar es Salaam. East. Afr. Med. J. 2002;79:467–469. doi: 10.4314/eamj.v79i9.9118. [DOI] [PubMed] [Google Scholar]
- Kritpetcharat O., Suwanrungruang K., Sriamporn S., Kamsa-Ard S., Kritpetcharat P., Pengsaa P. The coverage of cervical cancer screening in Khon Kaen, Northeast Thailand. Asian Pac. J. Cancer Prev. APJCP. 2003;4(2):103–106. [PubMed] [Google Scholar]
- Musa J. The need for societal investment to improve cervical cancer outcomes in Nigeria: a commentary. Afr. J. Reprod. Health. 2017;21(4):17. doi: 10.29063/ajrh2017/v21i4.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musa J., Nankat J., Achenbach C.J., Shambe I.H., Taiwo B.O., Mandong B., Daru P.H., Murphy R.L., Sagay A.S. Cervical cancer survival in a resource-limited setting-North Central Nigeria. Infect. Agents Canc. 2016;11(1):15. doi: 10.1186/s13027-016-0062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndejjo R., Mukama T., Musabyyimana A., Musoke D. Uptake of cervical cancer screening and associated factors among women in rural Uganda: a cross sectional study. PloS One. 2016 doi: 10.1371/journal.pone.0149696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahrens W., Pohlabeln H., Foraita R., Nelis M., Lagiou P., Lagiou A. Oral health, dental care and mouthwash associated with upper aerodigestive tract cancer risk in Europe: the ARCAGE study. Oral Oncol. 2014;50(6):616–625. doi: 10.1016/j.oraloncology.2014.03.001. [DOI] [PubMed] [Google Scholar]
- Nene B., Jayant K., Arrossi S., Shastri S., Budukh A., Hingmire S., Muwonge R., Malvi S., Dinshaw K., Sankaranarayanan R. Determinants of women’s participation in cervical cancer screening trial, Maharashtra, India. Bull. World Health Organ. 2007;85(4):264–272. doi: 10.2471/BLT.06.031195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obom-Egbulem K. I’ll rather recharge my phone than test for cervical and breast cancer. Niger. Health J. 2010;8(3):45–49. [Google Scholar]
- Okoye C.A. Histopathological pattern of cervical cancer in Benin City, Nigeria. J. Med. Invest. Pract. 2014;9(4):147–150. [Google Scholar]
- Okunnu J. 2010. No woman needs to die from cervical cancer cynis and jenny limited 1st floor, Oaklan centre, 48 Aguiye Ironsi Street Maitama District Abuja.www.bwsinit.org [Google Scholar]
- 2014. http://data.worldbank.org/country/Nigeria
- Wright K.O., Faseru B., Kuyinu Y.A., Faduyile F.A. Awareness & uptake of the pap smear among market woman in Lagos. J. Publ. Health Afr. 2011;2(1) doi: 10.4081/jphia.2011.e14. eISSN 2038-9930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zewdie, Alemseged, Tefera, Amare, Hailemariam Health Seeking Behaviour for cervical cancer in Ethiopia: A Qualitative Study. Int. J. Equity Health. 2012;11(1) doi: 10.1186/1475-9276-11-83. [DOI] [PMC free article] [PubMed] [Google Scholar]