Abstract
Objective:
This study was conducted to assess the clinical usability of the zero-echo time (ZTE) technique of MRI for evaluating bone changes of the temporomandibular joint (TMJ) in comparison with CBCT.
Methods:
Twenty patients with TMJ disorder who underwent both CBCT and MRI were randomly selected. CBCT images were obtained with an Alphard 3030 device (Asahi Roentgen Ind., Co. Ltd, Kyoto, Japan). MRIs were obtained using a 3.0 T scanner (Pioneer; GE Healthcare, Waukesha, WI, USA) and a 21-channel head coil. An isotropic three-dimensional proton-density-weighted ZTE sequence was acquired. Two radiologists evaluated 40 joints of 20 patients for the presence of the following osseous changes: flattening, erosion, osteophyte and sclerosis of the condyle; and flattening, erosion and sclerosis of the articular fossa. CBCT and ZTE-MRI assessments were performed at a 2-month interval. The prevalence-adjusted and bias-adjusted κ statistic was used to analyse interexaminer and intraexaminer agreement and the agreement between ZTE-MRI and CBCT.
Results:
Intraexaminer and interexaminer agreement analyses of ZTE-MRI showed high reproducibility (κ>0.80), which was comparable to that of CBCT. Flattening, osteophyte and sclerosis of the condyle and all types of bone changes in the mandibular fossa showed nearly perfect agreement between CBCT and ZTE-MRI (κ = 0.80–0.90). Erosion of the condyle showed substantial agreement between both sets of images (κ = 0.65–0.70).
Conclusions:
It is suggested that ZTE-MRI provides clinically reliable images for bone assessment in TMJ disorder. MRI may become a beneficial diagnostic tool for patients with both TMJ disc and bone pathology, with advantages involving medical costs and radiation dose.
Keywords: magnetic resonance imaging, Temporomandibular joint disorders, Cone-beam computed tomography, digital radiography
Introduction
Magnetic resonance imaging (MRI) is a technique using non-ionizing radiation that generates images with high tissue contrast and resolution. Nonetheless, it is not actively applicable to dentomaxillofacial bone evaluation due to its relatively low imaging resolution with conventional sequences compared to computed tomography (CT). MRI depicts tissue structures, as it reflects the proton density of tissues. However, hard tissue structures contain relatively low proton density and those protons are attached to the tissue, making it difficult to obtain a signal from those structures using conventional MRI techniques.1 Nevertheless, techniques have been continually refined and advanced in response to an increasing clinical demand for the ability to use MRI to obtain bone structures. Techniques for capturing signals from protons in a very fast time frame, before they diminish, have been introduced; these are referred to as ultra-short echo time (UTE) and zero-echo time (ZTE) sequences. These techniques have shown the potential to enable useful MRI-based bone imaging.2
Conventional MRI has limitations in obtaining optimal bone images since the echo time (TE) for the spin-echo and gradient-echo pulse sequences is too slow (≈ 1–10 ms) to detect meaningful bone signals.1 With technological progression, the ZTE sequence has achieved a nearly zero TE for image acquisition by using radial k-space filling strategies, extrapolation of oversampling and algebraic reconstruction.3–5 This technique, with a TE close to zero, obtains sufficient data very rapidly, even for rapidly decaying bone signals. It provides high-resolution isotropic bone images with fast and silent scanning.6
To date, bone MRI using ZTE sequences has been most actively studied for positron emission tomography MRI. Attempts have also been made to utilize ZTE-MRI for conditions where both MRI and CT must be acquired for diagnosis, such as in cases of head trauma. Cho et al compared CT images and ZTE-MRI images of skull fractures due to head trauma and find the practicability of replacing CT with MRI.7 ZTE-MRI also has been applied to osseous imaging of the shoulder and spine, and its feasibility for replacing CT images has also been suggested. Those previous studies presented strong agreement between ZTE-MRI and CT images.6,8
MRI is the standard tool for diagnostic imaging for patients suffering from temporomandibular joint (TMJ) disorder and those in whom disc displacement or deformity is suspected.9 Disc evaluation has been attempted using other imaging modalities, such as ultrasonography, but MRI has long been accepted as an accurate diagnostic tool with high sensitivity and specificity.10 A pathological change of the disc is the initial sign of TMJ osteoarthritis, followed by or simultaneously with degenerative bony changes of the condyle and articular eminence, which progress and present as flattening, cortical bone erosion, sclerosis and osteophyte formation in the bone compartment.11 If it is possible to use ZTE-MRI to accurately detect bone changes in the TMJ, to the same standard as CT or cone-beam computed tomography (CBCT), the diagnosis of TMJ disorder with both bone and disc pathologies would become possible with MRI alone. However, ZTE-MRI has not been studied for clinical purposes in dentomaxillofacial bone pathology. This study aimed to assess the clinical usability of ZTE-MRI with CBCT for evaluating bone changes in TMJ.
Methods and materials
Subjects
Twenty patients who underwent both CBCT and MRI examinations at Yonsei University Dental Hospital due to TMJ disorder within 2 months were selected (13 females and seven males; mean age = 37.05 years). This study was approved by the Institutional Review Board of Yonsei University Dental Hospital.
CBCT image analysis
CBCT images were obtained with an Alphard 3030 device (Asahi Roentgen Ind., Co. Ltd, Kyoto, Japan) using the following parameters: tube voltage, 90 kVp; tube current, 8 mA; exposure time, 17 s; FOV, 15×15 cm. Image reconstruction was performed to obtain a true sagittal and coronal TMJ view with a slice thickness of 1.0 mm according to the long axis of the condylar head by a skilled radiographer using OnDemand 3D software (Cybermed, Seoul, Korea).
The imaging criteria defined by Alexiou et al and Hintze et al were utilized.11,12 All 40 joints were separately evaluated by two experienced radiologists. The observer evaluated each joint referring to both lateral and frontal cross-sectional view images. Each individual parameter was scored as absent or present. The evaluation procedure was performed once more after 2 months. The parameters were as follows:
-
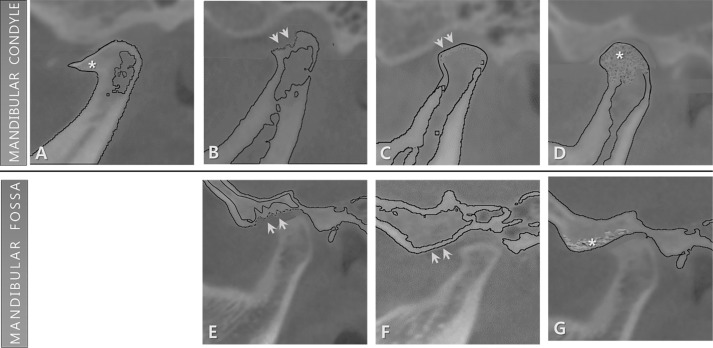
Osseous changes of the condyles ( Figure 1A–D )
Osteophyte: marginal bony deposition and bone outgrowth
Erosion: loss and irregular surface of cortical bone
Flattening: bony contour becomes flattened on the articular surface
Sclerosis: increased cortical bone area extending into the bone marrow
-
Osseous changes of the mandibular fossa (Figure 1E–G)
Erosion
Flattening
Sclerosis
Figure 1.
Schematic imaging features of osseous changes in the mandibular condyle (A-D) and fossa (E-G) for evaluation. Osteophyte (A): marginal bony deposition and bone outgrowth on the condyle are marked with an asterisk. Erosion: loss and irregular surface of cortical bone of the condyle (B) and fossa (E) are marked with arrows. Flattening: the bony contour becomes flattened on the articular surface of condyle (C) and fossa (F), as marked with arrows. Sclerosis: the increased cortical bone area extending into the bone marrow of the condyle (D) and fossa (G) is marked with an asterisk.
MR image analysis
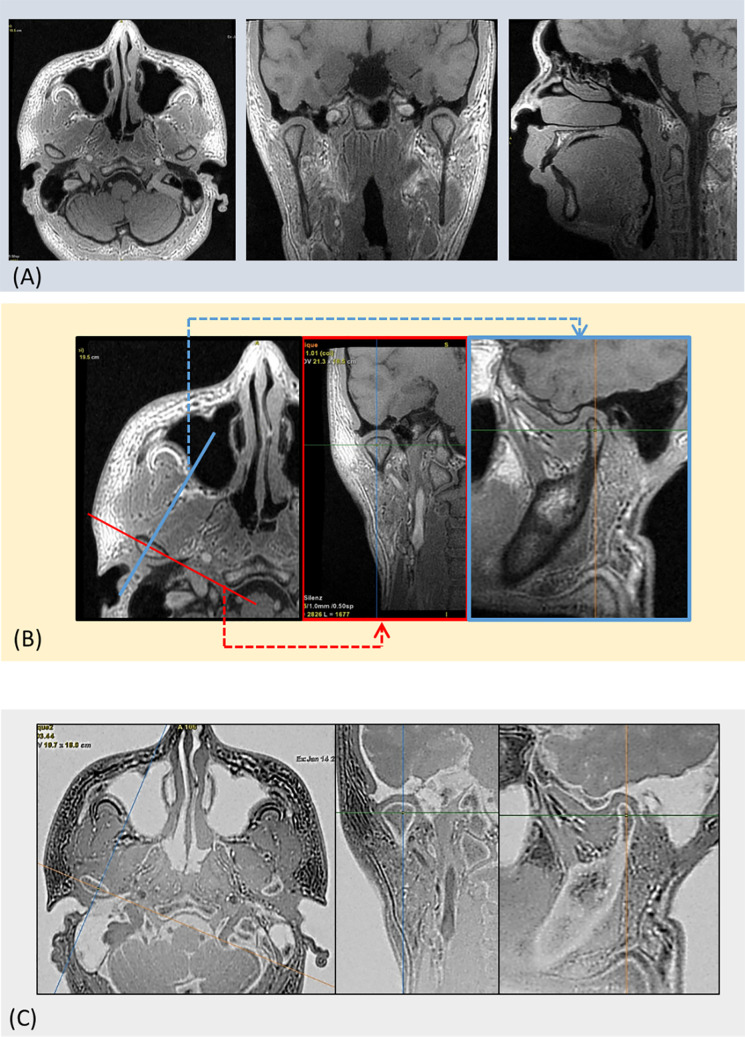
MRI examinations of the TMJ were acquired using a clinical 3.0 T scanner (Pioneer; GE Healthcare, Waukesha, WI, USA) with a 21-channel head coil. Isotropic three-dimensional proton-density weighted ZTE scans were acquired with the following parameters: TE/TR, 0/785 ms; flip angle, 4°; receiver bandwidth, 31.25 kHz; NEX, 2; FOV, 180 × 180 mm; acquisition matrix, 260 × 260, slice thickness, 1.0 mm; scan time,~5 min (Figure 2A). True sagittal and true coronal section views with a slice thickness of 1.0 mm, the same as on CBCT, were obtained as well (Figure 2B). The ZTE image settings were inverted to grayscale to follow CT-like contrast patterns (Figure 2C). This post-processing was performed using the AW server (GE Healthcare, Waukesha, WI, USA).
Figure 2.
Work flow of the image reconstruction and post-processing procedures of ZTE-MRI. (A) The original isotropic three-dimensional proton-density weighted ZTE image. (B) Image reconstruction according to the long axis of the condylar head to obtain true coronal and true sagittal views of the TMJ slice on the AW server (GE Healthcare, Waukesha, WI, USA). (C) Grayscale inversion was performed to obtain CT-like contrast patterns.
The ZTE image evaluation procedure was also performed by two radiologists, and the order of the given image set was random. The ZTE image evaluation was conducted 1 month after the CBCT image evaluation. The evaluation criteria were same as those used in the CBCT image analysis. Two observers scored each joint individually, and the evaluation was performed twice at a 2-month interval.
Statistical analysis
The prevalence-adjusted and bias-adjusted κ (PABAK) statistic was used to analyse interexaminer and intraexaminer agreement for CBCT and ZTE-MRI, respectively. Weighted-kappa values using PABAK statistics were also used to assess agreement between ZTE-MRI and CBCT regarding bony changes of the condyle and mandibular fossa in the TMJ. Kappa values were interpreted as follows: 0, no agreement; 0–0.19, poor agreement; 0.20–0.39, fair agreement; 0.40–0.59, moderate agreement; 0.60–0.79, substantial agreement; and 0.80–1.00, nearly perfect agreement.13
Results
The weighted-kappa values obtained from an analysis of intraexaminer and interexaminer agreement at a 2-month time interval showed a high level of measurement reproducibility for both CBCT and ZTE-MRI (κ > 0.80; Table 1). Both the intraexaminer and interexaminer agreement values of CBCT were slightly higher than those of ZTE-MRI.
Table 1.
Interobserver and intraobserver agreement for each imaging modality
| ZTE-MRI | CBCT | |
|---|---|---|
| Interobserver agreement (κ value) |
0.83 (0.65 ~ 1.00) |
0.84 (0.65 ~ 0.95) |
| Intraobserver agreement (κ value) |
0.90 (0.75 ~ 1.00) |
0.92 (0.75 ~ 1.00) |
CBCT, cone-beam computed tomography;ZTE, zero-echo time.
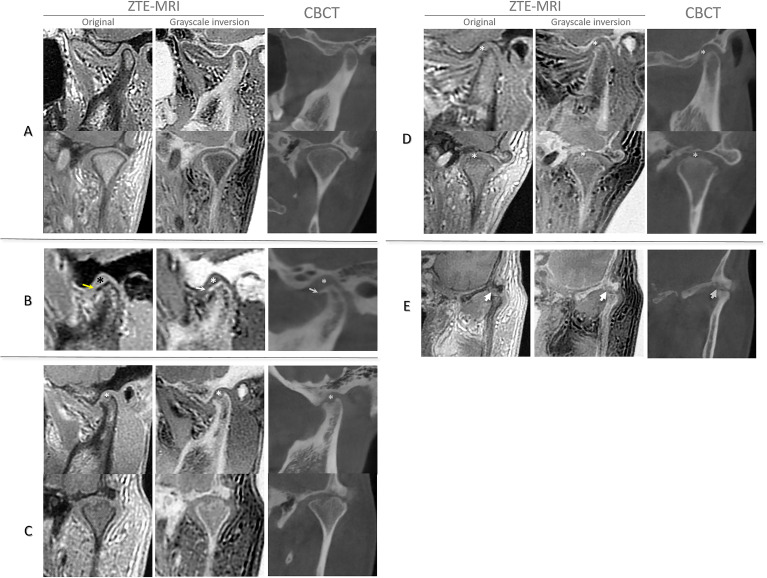
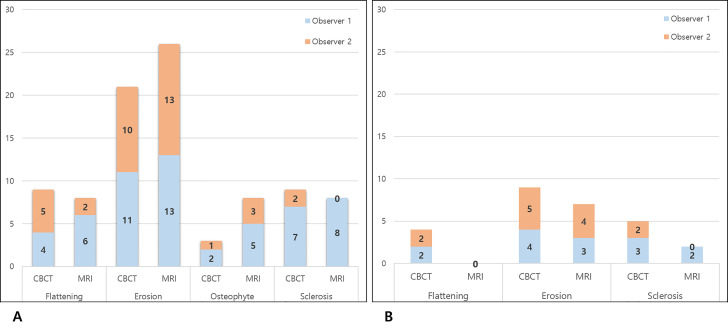
ZTE-MRI for all 40 joints presented clearly identifiable TMJ bone structure in image, similar to the CBCT images (Figure 3). Flattening, osteophyte and sclerosis of the condyle and all types of osseous changes in the mandibular fossa showed nearly perfect agreement between CBCT and ZTE-MRI (κ = 0.80–0.90). Erosion of the condyle showed substantial agreement between the two imaging modalities (κ = 0.65–0.70). The weighted κ values for each bone change parameter are presented in Table 2. Erosion was the most common bone change pattern recorded by both observers in both image modalities (Figure 4).
Figure 3.
ZTE-MRI and CBCT images of the TMJ with (A) normal cortical bone, (B) osteophyte formation (arrow) and flattening (asterisk) of condyle, (C) erosion (asterisk) of condyle, (D) subchondral sclerosis (asterisk) of condyle and (E) erosion (arrow) of mandibular fossa.
Table 2.
Agreement between CBCT and ZTE-MRI in evaluating TMJ osseous changes
| Condyle | Fossa | |||||||
|---|---|---|---|---|---|---|---|---|
| Flattening | Erosion | Osteophyte | Sclerosis | Flattening | Erosion | Sclerosis | ||
| Observer 1 (κ value) |
0.80 | 0.70 | 0.85 | 0.85 | 0.90 | 0.85 | 0.85 | |
| Observer 2 (κ value) |
0.85 | 0.65 | 0.90 | 0.90 | 0.90 | 0.95 | 0.90 | |
CBCT, cone-beam computed tomography; TMJ, temporomandibular joint; ZTE, zero-echo time.
Figure 4.
Frequency of bone change patterns evaluated by individual observers in ZTE-MRI and CBCT in condyle (A) and mandibular fossa (B). Note that erosion of the condyle was the most frequent feature among all joints evaluated.
Discussion
To the best of the authors’ knowledge, this is the first study to evaluate degenerative bone changes of the TMJ through ZTE-MRI sequences in comparison with CBCT. Substantial agreement was found between ZTE-MRI and the current clinical standard modality, CBCT, for assessing degenerative changes in TMJ bone structure.
Degenerative arthritis, or osteoarthritis, is the most common pathological condition of the TMJ. The initial stage is known to present as disc displacement. This condition then progresses into the late stage, showing osseous changes of the joint component, which is known as degenerative joint disease. 14 Degenerative bone changes of the TMJ are closely related to occlusion and may frequently require periodic follow-up imaging evaluations. 15 For such patients, the potential harmful effect of ionizing radiation cannot be ignored. Therefore, the ability to assess bone changes with MRI would be hugely beneficial for patients with TMJ disorder.
Until recently, MRI could not provide optimal bone images. The conventional TE is too long to detect signals from hydrogen atoms in cortical bone. The hydrogen atoms of cortical bone are excited and return back to their original status very quickly. Conventional MRI techniques cannot provide a short enough TE to capture the hydrogen atom signal of bone.1 Thus, in conventional MRI sequences (T 1-weighted, T 2-weighted and proton-density images), bone structure is mostly shown as black, which means that no signal has been detected for these structures.
Despite those limitations of conventional MRI for bone imaging, continuous demand for TMJ bone assessment through MRI has existed. In previous research, attempts have been made to detect abnormalities of TMJ cortical bone using conventional MRI, T 2-weighted and proton-density sequences, with the results compared to CBCT images.16 However, the sensitivity of MRI for detecting bone changes of the TMJ was relatively low.
Technical advances have made it feasible to use UTE and ZTE sequences to produce relatively optimal bone MRIs. Both UTE and ZTE pulse sequences begin data acquisition as soon as the radiofrequency (RF) pulse is completed. The difference is that UTE turns on the readout gradient soon after RF, while ZTE turns on the readout gradient prior to the RF pulse.17 Thus, there is a moment between the RF pulse and the signal readout in UTE sequences (although it is an ultra-short time), while there is no delay in signal acquisition in ZTE. The ZTE technique is known to yield images with a higher signal-to-noise ratio, and it is less sensitive to gradient fidelity than UTE sequences, while providing isotropic high-resolution images with multiplanar reconstruction.7,17,18
TMJ disorder frequently progress into degenerative bone changes of the condyle and the articular eminence of the mandibular fossa composing the TMJ, commonly manifesting as flattening, erosion, osteophyte, subchondral bone sclerosis and pseudocyst.11,12,19 The correct diagnosis of such bone changes is fundamental for identifying the stage of disease and planning appropriate treatment.19 CT and CBCT have been the standard imaging modality of choice for assessing degenerative bone changes of the TMJ.8 However, the ionizing radiation exposure from CT or CBCT constrains the degree to which serial imaging studies can be used to evaluate disease progression.
MRI is currently considered to be the reference imaging method for soft tissue pathology surrounding the TMJ, such as disc displacement or deformity or joint effusion.9 Currently, patients who require an evaluation of both the soft and hard tissue structures of the TMJ must undergo both CBCT (or CT) and MRI. Therefore, it is meaningful that ZTE-MRI yielded comparable results to those of CBCT for TMJ bone assessment in terms of both medical costs and the radiation dose.
In the current study, ZTE-MRI showed slightly lower intraobserver and interobserver agreement than CBCT. A previous study noted that a reason for discrepancies between the scores of CT and ZTE images is that observers are not familiar with evaluating bone using ZTE images, as ZTE-MRI is not currently a routine pulse sequence.8 Therefore, it is expected that TMJ evaluations based on ZTE images may improve, as radiologists become more acquainted with this sequence.
The agreement between CBCT and ZTE was the lowest for both evaluators in cases of erosive changes of the TMJ, which are assessed by detecting minute bone changes. It can be inferred that the ZTE-MRI sequence may not yet depict hard tissue in sufficient detail. In particular, considering the small size and complexity of the hard tissue of the dentomaxillofacial area, further technical development of the ZTE sequence is necessary.
This study has some limitations. A time interval existed between the CBCT and ZTE-MRI scans. However, this interval was less than 2 months, which is considered to be a relatively short time for bone changes to occur. Another limitation is that joints showing degenerative bone changes were outnumbered by those in a normal condition. In particular, there were too few cases of TMJ with sclerosis both on the condyle and the articular eminence of the mandibular fossa. Further research should investigate a larger number of joints showing bone changes, ranging from slight to severe.
Conclusions
The present study suggests that ZTE-MRI can provide clinically adequate images for the evaluation of degenerative bone changes of the TMJ. When the ZTE sequence is combined with conventional MRI sequences for the TMJ, MRI could become a valuable diagnostic tool for TMJ disorder patients with both disc and bone pathology, with advantages in both medical costs and the radiation dose.
Footnotes
Acknowledgment: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2019R1A2C1007508).
Chena Lee and Kug Jin Jeon contributed equally to this work
Contributor Information
Chena Lee, Email: CHENALEE@yuhs.ac.
Kug Jin Jeon, Email: dentjeon@yuhs.ac.
Sang-Sun Han, Email: sshan@yuhs.ac.
Young Hyun Kim, Email: yhkim0430@yuhs.ac.
Yoon Joo Choi, Email: yjchoi79@yuhs.ac.
Ari Lee, Email: ari0205@yuhs.ac.
Jong Hoon Choi, Email: JHCHOIJ@yuhs.ac.
REFERENCES
- 1. Du J , Carl M , Bydder M , Takahashi A , Chung CB , Bydder GM . Qualitative and quantitative ultrashort echo time ( Ute) imaging of cortical bone . J Magn Reson 2010. ; 207 : 304 – 11 . doi: 10.1016/j.jmr.2010.09.013 [DOI] [PubMed] [Google Scholar]
- 2. Eley KA , McIntyre AG , Watt-Smith SR , Golding SJ . "Black bone" MRI: a partial flip angle technique for radiation reduction in craniofacial imaging . Br J Radiol 2012. ; 85 : 272 – 8 . doi: 10.1259/bjr/95110289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Weiger M , Pruessmann KP . Mri with zero echo time . eMagRes 2012. ; 1 : 311 – 21 . [Google Scholar]
- 4. Kuethe DO , Caprihan A , Lowe IJ , Madio DP , Gach HM . Transforming NMR data despite missing points . Journal of Magnetic Resonance 1999. ; 139 : 18 – 25 . doi: 10.1006/jmre.1999.1767 [DOI] [PubMed] [Google Scholar]
- 5. Weiger M , Pruessmann KP , Bracher A-K , Köhler S , Lehmann V , Wolfram U , et al. . High-Resolution ZTE imaging of human teeth . NMR Biomed 2012. ; 25 : 1144 – 51 . doi: 10.1002/nbm.2783 [DOI] [PubMed] [Google Scholar]
- 6. Breighner RE , Endo Y , Konin GP , Gulotta LV , Koff MF , Potter HG . Technical developments: zero echo time imaging of the shoulder: enhanced osseous detail by using MR imaging . Radiology 2018. ; 286 : 960 – 6 . doi: 10.1148/radiol.2017170906 [DOI] [PubMed] [Google Scholar]
- 7. Cho SB , Baek HJ , Ryu KH , Choi BH , Moon JI , Kim TB , et al. . Clinical feasibility of zero te skull MRI in patients with head trauma in comparison with CT: a single-center study . AJNR Am J Neuroradiol 2019. ; 40 : 109 – 15 . doi: 10.3174/ajnr.A5916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Argentieri EC , Koff MF , Breighner RE , Endo Y , Shah PH , Sneag DB . Diagnostic accuracy of Zero-Echo time MRI for the evaluation of cervical neural Foraminal stenosis . Spine 2018. ; 43 : 928 – 33 . doi: 10.1097/BRS.0000000000002462 [DOI] [PubMed] [Google Scholar]
- 9. Talmaceanu D , Lenghel LM , Bolog N , Hedesiu M , Buduru S , Rotar H , et al. . Imaging modalities for temporomandibular joint disorders: an update . Clujul Med 2018. ; 91 : 280 – 7 . doi: 10.15386/cjmed-970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Abdel RA , BF A , Ahmed W , Haggag M . Assessment of articular disc displacement of temporomandibular joint with ultrasound . J Ultrasound 2015. ; 18 : 159 – 63 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hintze H , Wiese M , Wenzel A . Cone beam CT and conventional tomography for the detection of morphological temporomandibular joint changes . Dentomaxillofac Radiol 2007. ; 36 : 192 – 7 . doi: 10.1259/dmfr/25523853 [DOI] [PubMed] [Google Scholar]
- 12. Alexiou KE , Stamatakis HC , Tsiklakis K . Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography . Dentomaxillofac Radiol 2009. ; 38 : 141 – 7 . doi: 10.1259/dmfr/59263880 [DOI] [PubMed] [Google Scholar]
- 13. Landis JR , Koch GG . The measurement of observer agreement for categorical data . Biometrics 1977. ; 33 : 159 – 74 . doi: 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 14. Tanaka E , Detamore MS , Mercuri LG . Degenerative disorders of the temporomandibular joint: etiology, diagnosis, and treatment . J Dent Res 2008. ; 87 : 296 – 307 . doi: 10.1177/154405910808700406 [DOI] [PubMed] [Google Scholar]
- 15. Caldas W , CONTI ACdeCF , Janson G , CONTI PCR . Occlusal changes secondary to temporomandibular joint conditions: a critical review and implications for clinical practice . J. Appl. Oral Sci. 2016. ; 24 : 411 – 9 . doi: 10.1590/1678-775720150295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alkhader M , Ohbayashi N , Tetsumura A , Nakamura S , Okochi K , Momin MA , et al. . Diagnostic performance of magnetic resonance imaging for detecting osseous abnormalities of the temporomandibular joint and its correlation with cone beam computed tomography . Dentomaxillofac Radiol 2010. ; 39 : 270 – 6 . doi: 10.1259/dmfr/25151578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Larson PEZ , Han M , Krug R , Jakary A , Nelson SJ , Vigneron DB , et al. . Ultrashort echo time and zero echo time MRI at 7T . MAGMA 2016. ; 29 : 359 – 70 . doi: 10.1007/s10334-015-0509-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bae K , Jeon KN , Hwang MJ , Lee JS , Ha JY , Ryu KH , et al. . Comparison of lung imaging using three-dimensional ultrashort echo time and zero echo time sequences: preliminary study . Eur Radiol 2019. ; 29 : 2253 – 62 . doi: 10.1007/s00330-018-5889-x [DOI] [PubMed] [Google Scholar]
- 19. dos Anjos Pontual ML , Freire JSL , Barbosa JMN , Frazão MAG , dos Anjos Pontual A , Fonseca da Silveira MM . Evaluation of bone changes in the temporomandibular joint using cone beam CT . Dentomaxillofac Radiol 2012. ; 41 : 24 – 9 . doi: 10.1259/dmfr/17815139 [DOI] [PMC free article] [PubMed] [Google Scholar]