Abstract
Background
The proportion of the world's population aged over 60 years is increasing. Therefore, there is a need to examine different methods of healthcare provision for this population. Medical day hospitals provide multidisciplinary health services to older people in one location.
Objectives
To examine the effectiveness of medical day hospitals for older people in preventing death, disability, institutionalisation and improving subjective health status.
Search methods
Our search included the Cochrane Effective Practice and Organisation of Care (EPOC) Group Register of Studies, CENTRAL (2013, Issue 7), MEDLINE via Ovid (1950‐2013 ), EMBASE via Ovid (1947‐2013) and CINAHL via EbscoHost (1980‐2013). We also conducted cited reference searches, searched conference proceedings and trial registries, hand searched select journals, and contacted relevant authors and researchers to inquire about additional data.
Selection criteria
Randomised and quasi‐randomised trials comparing medical day hospitals with alternative care for older people (mean/median > 60 years of age).
Data collection and analysis
Two authors independently assessed trial eligibility and risk of bias and extracted data from included trials. We used standard methodological procedures expected by the Cochrane Collaboration. Trials were sub‐categorised as comprehensive care, domiciliary care or no comprehensive care.
Main results
Sixteen trials (3689 participants) compared day hospitals with comprehensive care (five trials), domiciliary care (seven trials) or no comprehensive care (four trials). Overall there was low quality evidence from these trials for the following results.
For the outcome of death, there was no strong evidence for or against day hospitals compared to other treatments overall (odds ratio (OR) 1.05; 95% CI 0.85 to 1.28; P = 0.66), or to comprehensive care (OR 1.26; 95% CI 0.87 to 1.82; P = 0.22), domiciliary care (OR 0.97; 95% CI 0.61 to 1.55; P = 0.89), or no comprehensive care (OR 0.88; 95% CI 0.63 to 1.22; P = 0.43).
For the outcome of death or deterioration in activities of daily living (ADL), there was no strong evidence for day hospital attendance compared to other treatments (OR 1.07; 95% CI 0.76 to 1.49; P = 0.70), or to comprehensive care (OR 1.18; 95% CI 0.63 to 2.18; P = 0.61), domiciliary care (OR 1.41; 95% CI 0.82 to 2.42; P = 0.21) or no comprehensive care (OR 0.76; 95% CI 0.56 to 1.05; P = 0.09).
For the outcome of death or poor outcome (institutional care, dependency, deterioration in physical function), there was no strong evidence for day hospitals compared to other treatments (OR 0.92; 95% CI 0.74 to 1.15; P = 0.49), or compared to comprehensive care (OR 1.05; 95% CI 0.79 to 1.40; P = 0.74) or domiciliary care (OR 1.08; 95% CI 0.67 to 1.74; P = 0.75). However, compared with no comprehensive care there was a difference in favour of day hospitals (OR 0.72; 95% CI 0.53 to 0.99; P = 0.04).
For the outcome of death or institutional care, there was no strong evidence for day hospitals compared to other treatments overall (OR 0.85; 95% CI 0.63 to 1.14; P = 0.28), or to comprehensive care (OR 1.00; 95% CI 0.69 to 1.44; P = 0.99), domiciliary care (OR 1.05; 95% CI 0.57 to1.92; P = 0. 88) or no comprehensive care (OR 0.63; 95% CI 0.40 to 1.00; P = 0.05).
For the outcome of deterioration in ADL, there was no strong evidence that day hospital attendance had a different effect than other treatments overall (OR 1.11; 95% CI 0.68 to 1.80; P = 0.67) or compared with comprehensive care (OR 1.21; 0.58 to 2.52; P = 0.61), or domiciliary care (OR 1.59; 95% CI 0.87 to 2.90; P = 0.13). However, day hospital patients showed a reduced odds of deterioration compared with those receiving no comprehensive care (OR 0.61; 95% CI 0.38 to 0.97; P = 0.04) and significant subgroup differences (P = 0.04).
For the outcome of requiring institutional care, there was no strong evidence for day hospitals compared to other treatments (OR 0.84; 95% CI 0.58 to 1.21; P = 0.35), or to comprehensive care (OR 0.91; 95% CI 0.70 to 1.19; P = 0.49), domiciliary care (OR 1.49; 95% CI 0.53 to 4.25; P = 0.45), or no comprehensive care (OR 0.58; 95% CI 0.28 to 1.20; P = 0.14).
Authors' conclusions
There is low quality evidence that medical day hospitals appear effective compared to no comprehensive care for the combined outcome of death or poor outcome, and for deterioration in ADL. There is no clear evidence for other outcomes, or an advantage over other medical care provision.
Keywords: Aged; Humans; Geriatrics; Activities of Daily Living; Day Care, Medical; Day Care, Medical/standards; Day Care, Medical/statistics & numerical data; Health Services Research; Health Services for the Aged; Health Services for the Aged/statistics & numerical data; Home Care Services; Home Care Services/standards; Randomized Controlled Trials as Topic; Treatment Outcome
Plain language summary
Medical day hospital care for the elderly versus alternative forms of care
Day hospitals are one way of delivering healthcare to older people. They are out‐patient facilities which older patients attend for a full or near full day and receive multidisciplinary health care ‘under one roof.’ Sixteen trials involving 3689 participants were included in this review and compared day hospitals with other comprehensive services (including inpatient and outpatient services), home based care and no comprehensive services. Attendance at a day hospital offers benefits compared to providing no treatment which include reducing the risk of needing more help with daily activities such as washing or dressing. Furthermore, patients are less likely to suffer one of the following: dying, being institutionalised or becoming more dependent on others. There is no apparent benefit when day hospitals are compared with other comprehensive services or home care. The economic value of day hospitals when compared with other health care services remains unclear.
Summary of findings
Summary of findings for the main comparison. Day hospitals compared to alternative care or no care for rehabilitation needs.
| Day hospitals compared to alternative or no care for rehabilitation | ||||||
| Patient or population: patients with rehabilitation needs Intervention: day hospitals Comparison: alternative care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Alternative or no care | Day hospitals | |||||
| Death by the end of follow up Follow‐up: median 12 months | Study population | OR 1.05 (0.85 to 1.28) | 3533 (16 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 127 per 1000 | 132 per 1000 (110 to 157) | |||||
| Moderate | ||||||
| 66 per 1000 | 69 per 1000 (57 to 83) | |||||
| Death or institutional care by the end of follow up Follow‐up: median 12 months | Study population | OR 0.85 (0.63 to 1.14) | 3030 (13 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 303 per 1000 | 270 per 1000 (215 to 331) | |||||
| Moderate | ||||||
| 221 per 1000 | 194 per 1000 (152 to 244) | |||||
| Death or deterioration in activities of daily living (ADL) Follow‐up: median 12 months | Study population | OR 1.07 (0.76 to 1.49) | 1268 (7 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 407 per 1000 | 423 per 1000 (343 to 506) | |||||
| Moderate | ||||||
| 430 per 1000 | 447 per 1000 (364 to 529) | |||||
| Death or poor outcome (institutional care, disability or deterioration) Follow‐up: median 12 months | Study population | OR 0.92 (0.74 to 1.15) | 2831 (13 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 365 per 1000 | 346 per 1000 (299 to 398) | |||||
| Moderate | ||||||
| 241 per 1000 | 226 per 1000 (190 to 267) | |||||
| Deterioration in ADL in survivors Various ADL measures | Study population | OR 1.11 (0.68 to 1.8) | 905 (7 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 251 per 1000 | 271 per 1000 (185 to 376) | |||||
| Moderate | ||||||
| 233 per 1000 | 252 per 1000 (171 to 354) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; ADL: activities of daily living | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Limitations for at least one risk of bias criterion, or some limitations for multiple criteria, sufficient to lower confidence in the estimate of effect 2 Whilst there was evidence of heterogeneity, this was anticipated due to the diversity of the populations and of the interventions 3 Wide CIs
Summary of findings 2. Day hospitals compared to no comprehensive care for rehabilitation needs.
| Day hospitals compared to no comprehensive care for rehabilitation needs | ||||||
| Patient or population: patients with rehabilitation needs Intervention: day hospitals Comparison: no comprehensive care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No comprehensive care | Day hospitals | |||||
| Death by the end of follow up Follow‐up: median 12 months | Study population | OR 0.88 (0.63 to 1.22) | 1345 (4 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 128 per 1000 | 114 per 1000 (85 to 152) | |||||
| Moderate | ||||||
| 131 per 1000 | 117 per 1000 (87 to 155) | |||||
| Death or institutional care by the end of follow up Follow‐up: median 12 months | Study population | OR 0.63 (0.4 to 1) | 1177 (4 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 248 per 1000 | 172 per 1000 (117 to 248) | |||||
| Moderate | ||||||
| 307 per 1000 | 218 per 1000 (151 to 307) | |||||
| Death or deterioration in ADL Follow‐up: median 9 months | Study population | OR 0.76 (0.56 to 1.05) | 651 (2 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 436 per 1000 | 370 per 1000 (302 to 448) | |||||
| Moderate | ||||||
| 446 per 1000 | 380 per 1000 (311 to 458) | |||||
| Death or poor outcome (institutional care, disability or deterioration) Follow‐up: median 12 months | Study population | OR 0.72 (0.53 to 0.99) | 982 (3 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 347 per 1000 | 277 per 1000 (220 to 345) | |||||
| Moderate | ||||||
| 400 per 1000 | 324 per 1000 (261 to 398) | |||||
| Deterioration in ADL in survivors Follow‐up: median 9 months | Study population | OR 0.61 (0.38 to 0.97) | 407 (2 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 277 per 1000 | 189 per 1000 (127 to 271) | |||||
| Moderate | ||||||
| 227 per 1000 | 152 per 1000 (100 to 222) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; ADL: activities of daily living | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Limitations for at least one risk of bias criterion or some limitations for multiple criteria, sufficient to lower confidence in the estimate of effect 2 Whilst there was evidence of heterogeneity, this was anticipated due to the diversity of the population and of the study design 3 Wide CIs
Summary of findings 3. Day hospitals compared to domiciliary care for rehabilitation needs.
| Day hospitals compared to domiciliary care for rehabilitation | ||||||
| Patient or population: patients with rehabilitation needs Intervention: day hospitals Comparison: domiciliary care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Domiciliary care | Day hospitals | |||||
| Death by the end of follow up Follow‐up: median 6 | Study population | OR 0.97 (0.61 to 1.55) | 901 (7 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 101 per 1000 | 98 per 1000 (64 to 148) | |||||
| Moderate | ||||||
| 64 per 1000 | 62 per 1000 (40 to 96) | |||||
| Death or institutional care by the end of follow up Follow‐up: median 6 months | Study population | OR 1.05 (0.57 to 1.92) | 672 (5 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 187 per 1000 | 194 per 1000 (116 to 306) | |||||
| Moderate | ||||||
| 69 per 1000 | 72 per 1000 (41 to 125) | |||||
| Death or deterioration in ADL Follow‐up: median 9 months | Study population | OR 1.41 (0.82 to 2.42) | 443 (4 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 392 per 1000 | 476 per 1000 (346 to 609) | |||||
| Moderate | ||||||
| 334 per 1000 | 414 per 1000 (291 to 548) | |||||
| Death or poor outcome (institutional care, disability or deterioration) Follow‐up: median 6 months | Study population | OR 1.08 (0.67 to 1.74) | 581 (5 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 297 per 1000 | 313 per 1000 (221 to 424) | |||||
| Moderate | ||||||
| 364 per 1000 | 382 per 1000 (277 to 499) | |||||
| Deterioration in ADL in survivors Follow‐up: median 9 months | Study population | OR 1.59 (0.87 to 2.9) | 349 (4 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 225 per 1000 | 315 per 1000 (201 to 457) | |||||
| Moderate | ||||||
| 188 per 1000 | 269 per 1000 (168 to 402) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; ADL: activities of daily living | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Limitations for at least one risk of bias criterion or some limitations for multiple criteria, sufficient to lower confidence in the estimate of effect 2 Whilst there was evidence of heterogeneity, this was anticipated due to the diversity of the population and the interventions 3 Wide CIs
Summary of findings 4. Day hospitals compared to comprehensive care for elderly persons requiring rehabilitation.
| Day hospitals compared to comprehensive care for older people requiring rehabilitation | ||||||
| Patient or population: older people requiring rehabilitation Intervention: day hospitals Comparison: comprehensive care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Comprehensive care | Day hospitals | |||||
| Death by the end of follow up Follow‐up: median 12 months | Study population | OR 1.26 (0.87 to 1.82) | 1287 (5 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 144 per 1000 | 175 per 1000 (128 to 234) | |||||
| Moderate | ||||||
| 69 per 1000 | 85 per 1000 (61 to 119) | |||||
| Death or institutional care by the end of follow up Follow‐up: median 12 months | Study population | OR 1 (0.69 to 1.44) | 1181 (4 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 426 per 1000 | 426 per 1000 (339 to 517) | |||||
| Moderate | ||||||
| 231 per 1000 | 231 per 1000 (172 to 302) | |||||
| Death or deterioration in ADL Follow‐up: median 12 months | Study population | OR 1.18 (0.63 to 2.18) | 174 (1 study) | ⊕⊕⊝⊝ low1,3 | ||
| 349 per 1000 | 387 per 1000 (252 to 539) | |||||
| Moderate | ||||||
| 349 per 1000 | 387 per 1000 (252 to 539) | |||||
| Death or poor outcome (institutional care, disability or deterioration) Follow‐up: median 12 months | Study population | OR 1.05 (0.79 to 1.4) | 1268 (5 studies) | ⊕⊕⊝⊝ low1,2,3 | ||
| 410 per 1000 | 422 per 1000 (355 to 493) | |||||
| Moderate | ||||||
| 221 per 1000 | 230 per 1000 (183 to 284) | |||||
| Deterioration in ADL in survivors Follow‐up: median 12 months | Study population | OR 1.21 (0.58 to 2.52) | 149 (1 study) | ⊕⊕⊝⊝ low1,3 | ||
| 243 per 1000 | 280 per 1000 (157 to 448) | |||||
| Moderate | ||||||
| 243 per 1000 | 280 per 1000 (157 to 447) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio; ADL: activities of daily living | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Limitations for at least one risk of bias criterion or some limitations for multiple criteria, sufficient to lower confidence in the estimate of effect 2 Whilst there was evidence of heterogeneity, this was anticipated due to the diversity of the population and of the study design 3 Wide CIs
Background
The first geriatric day hospital was opened in the UK in 1952 (Farndale 1961). Day hospitals developed rapidly in the United Kingdom in the 1960's as an important component of care provision for older people designed to complement in‐patient services (Black 2005). The model has since been widely applied in New Zealand, Australia, Canada, the USA and several European countries.
Geriatric day hospitals provide multi‐disciplinary rehabilitation in an outpatient setting and operate in a pivotal position between hospital and home‐based services (Ames 1995; Black 2005; Brocklehurst 1973; Petermans 2011). They provide specialist services for older people, which can include examinations and consultations, all concentrated in one location (Bussche 2010).
Although there is considerable descriptive literature on day hospital care (RCP 1994), concern has been expressed that evidence for effectiveness is equivocal (Brocklehurst 1980; Donaldson 1986) and that day hospital care is expensive (NAO 1994).
Concern is often expressed about the most appropriate health and social services required to address the needs of an aging population. In the UK, for example, the largest population increase is seen in the over 85 age group. A range of different services models, of which the day hospital is one, may be appropriate to address these needs. This review sets out to examine the effectiveness and resource implications of geriatric medical day hospital attendance for older people and to compare it with other models of healthcare delivery for an older population. This is an updated Cochrane review first published in Forster 1999a.
Description of the condition
Geriatric day hospitals are not usually specific to one condition. However, many will provide rehabilitation services appropriate to conditions such as stroke that are likely to be seen in an older population.
Description of the intervention
Geriatric day hospitals are out‐patient healthcare facilities for older people living in the community. They provide multi‐professional treatment on a full or part time basis (Beynon 2009).They serve several functions, including assessment, rehabilitation, and medical, nursing, maintenance, social and respite care (Brocklehurst 1980). Rehabilitation and maintenance comprise the main work of the day hospital: 42% and 23% respectively (RCP 1994), with rehabilitation regarded as the most important function (Brocklehurst 1980). The specific features and services offered by individual geriatric day hospitals are subject to considerable variation. However, they usually include a combination of medical assessment with support from nurses and allied health professionals, often including physiotherapists and occupational therapists. There is no consensus on what types of healthcare professionals should make up the multi‐disciplinary teams (Petermans 2011). Additional services such as chiropody, social work, exercise classes and assistance with bathing and hair washing are offered by some hospitals.
How the intervention might work
Geriatric day hospitals offer a multidisciplinary approach to assessment and rehabilitation, with provision of a variety of services in one location. As a result of assessment and treatment occurring 'under one roof,’ the health requirements of older people should be identified and responded to in an appropriate and timely manner. The day hospital can provide out‐patient delivery of a Comprehensive Geriatric Assessment (CGA) which has a robust evidence base for inpatient setting use (Ellis 2011). A CGA addresses medical, physical, psychological and social needs, and includes the formation of a plan of care and rehabilitation, with a clear method of implementation. Day hospital staff have specific skills, knowledge and experience related to working with older people. Furthermore, the day hospital environment has the advantage of providing social interaction between patients, a factor which domiciliary services and usual care cannot provide. These factors could result in better outcomes for patients through the provision of effective rehabilitation and other healthcare delivery for an older population.
Why it is important to do this review
Between 1985 and 2010 the proportion of the world's population that is aged over 65 years grew by approximately a quarter from 6.0% (291 million) to 7.6% (524 million), and is expected to increase to 13% by 2035, exceeding a billion people globally (UN 2011). As a result of this increase, providing health care that meets the diverse needs of an older population and is cost effective and efficient will be ever more important. Day hospitals are one way of delivering multidisciplinary rehabilitation to older people in an outpatient setting. This review is necessary to assess the effectiveness of day hospitals across a number of health, cost and resource outcomes.
Objectives
The primary question was whether older patients attending a geriatric medical day hospital would experience better outcomes (in terms of death, dependency or institutionalisation) than those receiving alternative forms of care.
Secondary questions concerned the impact of day hospital care on patient satisfaction and subjective health outcomes, carer distress and resource use and costs.
Methods
Criteria for considering studies for this review
Types of studies
We included studies that were of a prospective, controlled design in which there was random assignment of participants to alternative treatment groups (one of which involved day hospital care), not as part of a complex multi‐service intervention. Studies which utilised ‘quasi’ randomisation procedures (for example allocation to groups based on date of birth) were also included.
Types of participants
We included patients receiving medical care (mean/median age of >60 years for individual studies). We are aware that day hospital descriptive studies have indicated that day hospital attendance is determined more by needs than age and that younger patients do attend day hospitals. Our pre‐specified participant criterion of age 60 years and over was chosen to pragmatically capture this clinical practice. Studies which were specific to psychiatric patients were excluded.
Types of interventions
We defined a day hospital as an out‐patient facility where older patients attend for a full or near full day and receive multidisciplinary rehabilitation in a healthcare setting. This is consistent with previous definitions (Siu 1994) and excluded trials evaluating social day centres, or other types of day hospitals such as psychiatric day hospitals for patients with dementia or psychiatric conditions. We excluded studies on day hospitals that only provided services for single, specific conditions (for example, arthritis). We wanted to assess the effects of providing typical general assessment and rehabilitation services relevant to older people. The inclusion of disease‐specific trials would risk incorporating the effects of very specific therapies for specific conditions, which were not the focus of this review.
We anticipated considerable heterogeneity, particularly in the control services, and so pre‐specified key subgroup comparisons prior to reviewing the trials.
1) Day hospital care versus comprehensive care ‐ where control patients had access to a range of geriatric medical services (both inpatient and outpatient). 2) Day hospital care versus domiciliary care ‐ where control patients were provided an approximately equivalent rehabilitation program within their own home or social day centre. 3) Day hospital care versus no comprehensive care ‐ where control patients did not routinely have access to outpatient rehabilitation services.
Types of outcome measures
We wished to identify outcomes which reflected a previous definition of the purpose of day hospital care: to facilitate and prolong independent living for older people in the community (Donaldson 1987). Effective day hospital care would thus be expected to reduce death, to maintain older people in their own home and to reduce admissions to hospital. The following outcomes were therefore selected, all of which were recorded at the end of scheduled follow up.
Primary outcomes
Primary outcomes were:
death;
the need for institutional care;
dependency;
global 'poor outcome' comprising death or one of the following (in order of preference): resident in institutional care, severe dependency at end of follow up, or deterioration in physical function during follow up; this outcome was included in anticipation of incomplete data sets.
Secondary outcomes
Secondary outcomes included:
dependency, measured by activities of daily living (ADL) scores;
patient satisfaction;
subjective health status (including mood);
resource use (in hospital or institutional care) plus overall cost analyses;
carer distress.
We considered all studies that met the eligibility criteria for study design, participants and interventions regardless of whether the pre‐specified primary or secondary outcomes were reported.
Search methods for identification of studies
For this edition of the review, D Andre, University of Leeds Library, developed search strategies in consultation with the authors. They were peer reviewed by M Fiander, EPOC Trials Search Coordinator. We searched the databases listed below for relevant studies.
Electronic searches
Effective Practice and Organisation of Care (EPOC) group register of trials (August 2013);
Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Library, Issue 7, July 2013; Appendix 1);
MEDLINE (1996 to July 2013; Appendix 2);
Medline in Process (1996 to August 2013; Appendix 3);
EMBASE (1996 to August 2013; Appendix 4);
Cumulative Index to Nursing and Allied Health Literature (CINAHL; 1996 to August 2013; Appendix 5);
Allied and Complementary Medicine Database (AMED; 1996 to August 2013; Appendix 6);
Physiotherapy Evidence Database (PEDro; August 2008; Appendix 7);
Applied Social Science Index and Abstracts (ASSIA; 1996 to August 2013; Appendix 8);
International Bibliography of Social Sciences (IBSS; 1996 to August 2013; Appendix 9);
PsycINFO (1996 to August week 1, 2013; Appendix 10);
Health Management Information Consortium Database (HMIC; January 2008 to August 2013; Appendix 11);
NHS Economic Evaluation Database (NHS EED; searched October 2013; Appendix 12);
Health Technology Assessment (HTA) Database (searched October 2013; Appendix 12);
Web of Knowledge (1996 to August 2013; Appendix 13);
Web of Science, Conference Proceedings Citation Index ‐ Social Science (1990 to 2012; Appendix 14);
Google Scholar (searched August 2013; Appendix 15);
Index to Theses (1996 to August 2013; Appendix 16);
Proquest Dissertations and Theses (1996 to August 2013; Appendix 17);
Current Controlled Trials (searched August 2013; Appendix 18).
Search strategies were comprised of natural language (free text) terms and controlled vocabulary (index) terms. Language limits were not applied. Search strategies for this update have been revised in order to improve sensitivity and precision. Changes were made based on an analysis of indexing terms found on previously included studies and by testing terms from the original strategy for precision. Given these changes, searches have been run retrospectively. The results of this search have been de‐duplicated from searches we carried out for the previous update of this review in 2008. The reference list of reviews of potential relevance were also examined (Bours 1998; Mason 2007; Outpatient Service 2004; Prvu Bettger 2007; Petermans 2011).
Searching other resources
HSRProj (searched August 2013; Appendix 19);
National Research Register (searched September 2007);
Australian New Zealand Clinical Trials Registry (May 2008).
Data collection and analysis
Selection of studies
Two review authors independently assessed the titles and abstracts from the electronic searches and excluded obviously irrelevant studies. We obtained full text articles of the remaining studies and at least two review authors independently assessed these against pre‐specified inclusion criteria to determine which trials would be eligible for inclusion. Study authors were contacted for further details when necessary. Disagreements were resolved by discussion with other members of the review team.
Data extraction and management
At least two review authors extracted data independently. Disagreements were resolved through group consensus. When possible, we contacted study authors for additional information and data as required.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias in the included studies using the tool for assessing risk of bias in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We scored each study as being at ‘high risk of bias’, ‘low risk of bias’ or ‘unclear risk of bias’ for each of the following domains, and reported them in the 'Risk of bias' tables.
Random sequence generation (selection bias).
Allocation concealment (selection bias).
Blinding of participants and personnel (performance bias).
Blinding of outcome assessment (detection bias).
Incomplete outcome data (attrition bias).
Selective reporting (reporting bias).
Other possible bias.
Measures of treatment effect
We calculated odds ratios with 95% confidence intervals for the dichotomous outcomes using standard methods. We used a random effects model as the subjects and interventions would have differed in ways which we anticipated would affect results and we could not assume a common effect size (Borenstein 2009).
We calculated inpatient resource use as the average (mean) use of hospital beds (in days) per patient recruited to each trial group. This figure was calculated for individual trials, and groups of trials, by dividing the total number of bed days by the total number of patients.
Unit of analysis issues
In cross‐over trials, we only included data from the first period of the trial in meta‐analyses to guard against carry‐over effects. Where cluster randomised studies presented an estimate of effect that properly accounted for the cluster design, this was used. Where this was not the case, we assumed that the intra‐cluster correlation coefficient (ICC) was the same as for other studies included in the review for that outcome. We calculated an average ICC for the outcome and corrected the values for each unadjusted study by the design effect (Higgins 2011).
Dealing with missing data
Where possible, studies were analysed on an intention‐to‐treat basis. Patients who were lost to follow up or for whom outcome data were not available were excluded from the initial analysis. However, they were included in ‘best case’ (all missing data in favour of day hospital care), intermediate and ‘worst case’ (all missing data in favour of alternative care) sensitivity analyses.
Assessment of heterogeneity
We assessed heterogeneity using I² and the Q statistic, with P < 0.1 determining significant heterogeneity (Higgins 2011).
Assessment of reporting biases
We attempted to reduce the risk of reporting bias by undertaking comprehensive searches of multiple databases and trials registers, and contacting authors. Where sufficient studies were included for individual outcomes, we undertook visual inspection of funnel plots to identify any obvious sources of publication bias.
Data synthesis
For patient outcomes, we undertook meta‐analyses at the end of follow up for the domains of death, death or institutional care, death or deterioration in ADL, death or poor outcome (institutional care, disability or deterioration) and deterioration in ADL in survivors. Analyses were based on the published summary data rather than individual patient data. For other patient outcomes ‐ ADL, subjective health status and patient satisfaction ‐ we present a narrative summary and a summary of the data is provided in the Data and analyses section. A summary of carer outcomes is also presented in the Data and analyses section. To investigate resource use, we performed a meta‐analysis for the domain of requiring institutional care at the end of follow up. For hospital bed use during follow up and cost we present a narrative summary in the Data and analyses section. We assessed the quality of the evidence using the GRADE approach which results in a quality score of high, moderate, low or very low (GRADEpro 2014).
Results
Description of studies
This review update includes 16 randomised controlled trials of medical day hospital versus alternative forms of care for older people. This includes three new studies in addition to the 13 studies from the previous version of this review (Forster 2008).
Results of the search
We screened over 25,000 unique citations and reviewed the full text of 190. 153 full papers and 34 abstracts were obtained and reviewed by a minimum of two reviewers to assess eligibility. Of these, three were included; five are awaiting assessment pending translation or availability of a published report (Studies awaiting classification); the majority of studies were excluded for reasons described in Characteristics of excluded studies; a further 131 studies were excluded for this update but not reported, as they were excluded early in the selection process. A flow diagram of the review update process can be found in Figure 1.
1.

Included studies
Three new studies have been added to this review update (Crotty 2008; Masud 2006; Parker 2009). Five studies are currently awaiting assessment.
Interventions
The current analysis includes 16 trials comprising 37 individual day hospitals. In accordance with the definition of day hospital used, multidisciplinary outpatient rehabilitation was available at all sites. Several of the studies evaluated more than one day hospital; the pilot study undertaken by Vetter 1989 involved two, Masud 2006 and Crotty 2008 each involved three, while a further four trials (Hedrick 1993; Parker 2009; Weissert 1980; Young 1992) each evaluated four day hospitals and Roderick 2001 involved five. The studies were undertaken in various countries including the UK (Burch 1999; Gladman 1993; Masud 2006; Parker 2009; Roderick 2001; Vetter 1989; Woodford 1962; Young 1992), USA (Cummings 1985; Hedrick 1993; Weissert 1980), Australia (Crotty 2008), Canada (Eagle 1991), Hong Kong (Hui 1995), Finland (Pitkala 1991) and New Zealand (Tucker 1984). For further details see Characteristics of included studies.
Comparison groups
Attendance at a day hospital was evaluated against various comparison treatments which were grouped together in the following sub‐categories:
1) In five studies the comparison treatment was comprehensive care comprising a range of inpatient, outpatient and domiciliary geriatric medical services (Cummings 1985; Eagle 1991; Hedrick 1993; Pitkala 1991; Tucker 1984).
2) In seven trials the comparison treatment was domiciliary therapy. This was provided in the patient's home (Crotty 2008; Gladman 1993; Parker 2009; Roderick 2001; Vetter 1989; Young 1992) or day centre (Burch 1999). Three of these trials recruited stroke patients only (Gladman 1993; Roderick 2001; Young 1992) and a fourth was a pilot study (Vetter 1989). In the Nottingham trial patients were randomly allocated to domiciliary rehabilitation or hospital‐based rehabilitation in three strata according to discharge ward: health care of older people, general medical unit or stroke unit (Gladman 1993). Hospital‐based rehabilitation was provided during day hospital attendance for patients in the older people care stratum and only patients in this stratum have been included in our analysis.
3) Four trials compared day hospital attendance against a control group in which patients were eligible for, but not referred to, existing services (Hui 1995; Masud 2006; Weissert 1980; Woodford 1962). In Masud 2006 the control arm received information leaflets on falls prevention and usual care from the primary care service until outcome data was completed, after which time control participants were offered access to the day hospital intervention.
We initially allocated Cummings 1985 and Hui 1995 into their own individual sub‐categories according to their comparison group; day hospital versus inpatient care (Cummings 1985) and day hospital versus medical outpatient care (Hui 1995). However, in order to streamline the analysis, these two trials were incorporated into the above categorisation schemes prior to data analysis. The Cummings 1985 trial investigated a day hospital service designed to facilitate early hospital discharge. The service offered to the comparison group was equivalent to comprehensive care and the trial was re‐categorised accordingly. The Hong Kong trial (Hui 1995) recruited stroke patients admitted to the same ward and randomised to receive rehabilitation care led by a neurology team or by a geriatrician team. After discharge, patients assigned to a neurologist were followed up at a medical outpatient clinic and the geriatrician patients by day hospital attendance. There were no differences in length of inpatient stay or dependency at discharge and the main treatment difference at final follow up assessment was the type of supporting aftercare: day hospital or medical outpatients. Further discussion with the trialists indicated that this comparison group could best be categorised as 'no comprehensive care'.
Patient characteristics
This review includes studies with a total of 3689 participants. One trial (Hedrick 1993), which was run by the United States Department of Veterans Affairs, recruited largely (96%) male patients. The other trials had a mix of male and female patients. In all but one trial the mean patient age was over 70 years; the New York trial (Cummings 1985) had a mean patient age of 65 years. Four trials (Gladman 1993; Hui 1995; Roderick 2001; Young 1992) recruited only stroke patients. Masud 2006 specifically recruited participants considered at a high risk of falling. The remaining eleven studies recruited patients with a mixture of diagnoses (Burch 1999; Crotty 2008; Cummings 1985; Eagle 1991; Hedrick 1993; Parker 2009; Pitkala 1991; Tucker 1984; Vetter 1989; Weissert 1980; Woodford 1962). The participants usually had a degree of dependency at recruitment as judged by their ADL scores (for further details see Characteristics of included studies).
Excluded studies
The majority of studies were excluded for reasons including a lack of randomisation, intervention that did not meet our criteria for a day hospital, or participants who were not older patients receiving medical care. It should be noted that only those studies which initially appeared to meet the inclusion criteria, but on closer inspection did not, were reported in the Characteristics of excluded studies. For this update, a further 131 studies were excluded but not reported: 45 were not RCTs; in 45 the intervention did not meet our criteria; 29 were review, commentary or discussion papers; five were questionnaires or surveys; and in two the intervention was for a single condition.
Risk of bias in included studies
Ten studies had a low risk of selection bias (method of random sequence generation) of which four studies used a computer generated method (Burch 1999; Crotty 2008; Hedrick 1993; Roderick 2001), four used a random number table (Gladman 1993; Hui 1995; Tucker 1984; Woodford 1962) and two used external Internet/web based services (Masud 2006; Parker 2009). Pitkala 1991 had a high risk of bias as randomisation was by date of birth. In five studies, the method of random sequence generation was unreported or unclear (Cummings 1985; Eagle 1991; Vetter 1989; Weissert 1980; Young 1992). For review authors' judgements about each risk of bias item presented as percentages across all included studies see Figure 2, and for review authors' judgements about each risk of bias item for each included study see Figure 3.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Nine studies had an adequate method of allocation concealment (Burch 1999; Crotty 2008; Gladman 1993; Hedrick 1993; Hui 1995; Masud 2006; Parker 2009; Vetter 1989; Young 1992). Methods were unclear in 6 studies (Cummings 1985; Eagle 1991; Roderick 2001; Tucker 1984; Weissert 1980; Woodford 1962). Pitkala 1991 presented with a high risk of bias as their method of randomisation was by date of birth which meant allocation could have been foreseen.
Blinding
Performance bias was a feature of all studies as it was not possible to blind participants due to the nature of the intervention. As a result all studies had a high risk of bias in this domain. Six studies were considered at a low risk for detection bias (blinded outcome assessment; Burch 1999; Crotty 2008; Masud 2006; Roderick 2001; Tucker 1984; Young 1992). Masud 2006 stated that it was not possible to blind researchers to group allocation. However, the review authors considered that the relevant outcome measurements were unlikely to be influenced by a lack of blinding and therefore the risk remained low. The remaining studies were considered to have a high or unclear risk of bias (Cummings 1985; Eagle 1991; Gladman 1993; Hedrick 1993; Hui 1995; Parker 2009; Pitkala 1991; Vetter 1989; Weissert 1980; Woodford 1962).
Incomplete outcome data
Eight studies were considered to be at low risk of bias for attrition (Burch 1999; Crotty 2008; Eagle 1991; Gladman 1993; Hedrick 1993; Masud 2006; Roderick 2001; Young 1992). Three studies were judged to be at high risk of bias. For the Parker 2009 study, losses were similar across the groups but were in excess of 35% by final follow up. For Weissert 1980, 718 participants were excluded for missing data or due to non‐adherence. The numbers lost and reasons lost per group were not reported. For Woodford 1962, approximately a third of participants were lost and whilst numbers were balanced across groups, the reasons were not reported. The remaining studies were unclear regarding attrition (Cummings 1985; Hui 1995; Pitkala 1991; Tucker 1984; Vetter 1989).
Selective reporting
Two studies were judged to be at low risk for reporting bias (Masud 2006; Parker 2009). Crotty 2008 was considered at high risk as not all the proposed outcomes reported in the study protocol were included in the available publication. For the remaining studies it was unclear whether selective reporting occurred, or pre‐study protocols were unavailable (Burch 1999; Cummings 1985; Eagle 1991; Gladman 1993; Hedrick 1993; Hui 1995; Pitkala 1991; Roderick 2001; Tucker 1984; Vetter 1989; Weissert 1980; Woodford 1962; Young 1992).
Other potential sources of bias
The majority of studies were considered at low risk for other sources of bias (Crotty 2008; Eagle 1991; Gladman 1993; Hedrick 1993; Hui 1995; Masud 2006; Parker 2009; Roderick 2001; Tucker 1984; Vetter 1989; Weissert 1980; Woodford 1962; Young 1992).The Cummings 1985 study was judged as unclear as this was an ‘artificial’ day hospital established for the purpose of the study and the under‐utilisation of the facility may introduced bias. Pitkala 1991 was judged as unclear as 23% of the day hospital group refused the care. Burch 1999 was considered to be at a high risk as 10 of 55 patients transferred from day centre to day hospital.
Further details on how individual studies were scored across the different domains of bias are reported in the risk of bias tables in the Characteristics of included studies.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
The 16 trials included in the review recruited a total of 3689 patients.
Patient outcomes
Nine studies provided final outcome data at 12 months (Burch 1999; Eagle 1991; Gladman 1993; Hedrick 1993; Masud 2006; Parker 2009; Pitkala 1991; Weissert 1980; Woodford 1962), four studies at six months (Crotty 2008; Hui 1995; Roderick 2001; Young 1992), one study at five months (Tucker 1984), one study at three months (Cummings 1985) and one at two months (Vetter 1989).
Death
All 16 trials published data, or provided data on request, for the combined outcome of death at the end of follow up. The pooled OR for all the trials for death at the end of scheduled follow up shows no difference between the day hospital and comparison interventions (odds ratio (OR) 1.05; 95% confidence interval (CI) 0.85 to 1.28; P = 0.66). There was no evidence of a difference when day hospital attendance was compared with comprehensive care (OR 1.26; 95% CI 0.87 to 1.82; P = 0.22), domiciliary care (OR 0.97; 95% CI 0.61 to 1.55; P = 0.89) or no comprehensive care (OR 0.88; 95% CI 0.63 to 1.22; P = 0. 43). There was no significant heterogeneity overall (Chi² = 12.04; df = 14; P = 0.60) or for any of the subgroups (P > 0.05) (Analysis 1.1). Outcome data were missing for a total of 102 day hospital patients and 54 controls (representing 3.2% of patients in the comprehensive care subgroup, 0% in the domiciliary subgroup and 7.8% in the no comprehensive care subgroup). Best and worst case sensitivity analyses include the possibility of significant benefit (P < 0.001) or harm (P < 0.01) from day hospital attendance. Visual inspection of funnel plots did not identify any obvious signs of publication bias.
1.1. Analysis.

Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 1 Death by the end of follow up.
Death or institutional care
Thirteen trials published data, or provided data on request, for death or institutional care by the end of follow up (Burch 1999; Crotty 2008; Eagle 1991; Gladman 1993; Hedrick 1993; Hui 1995; Masud 2006; Pitkala 1991; Tucker 1984; Weissert 1980; Vetter 1989; Woodford 1962; Young 1992). The pooled OR for all the trials for death or institutional care at the end of scheduled follow up shows no difference between the day hospital and comparison interventions. (OR 0.85; 95% CI 0.63 to 1.14; P = 0.28). There was no significant difference between day hospital patients and those receiving comprehensive services (OR 1.00; 95% CI 0.69 to 1.44; P = 0.99), domiciliary care (OR 1.05; 95% CI 0.57 to 1.92; P = 0.88) or no comprehensive services (OR 0.63; 95% CI 0.40 to 1.00; P = 0.05). There were no significant subgroup differences (P = 0.26). There was significant heterogeneity overall for all studies (Chi² = 25.4, df =11, P = 0.01; I² = 57%; Analysis 1.2). Outcome data were missing for a total of 224 day hospital patients and 110 controls (representing 4.2% of patients in the comprehensive care subgroup, 0% in the domiciliary care subgroup and 19.3% in the no comprehensive care subgroup). Best and worst case sensitivity analyses include the possibility of significant benefit (P < 0.0001) or harm (P < 0.0001) from day hospital attendance. Visual inspection of funnel plots did not identify any obvious signs of publication bias.
1.2. Analysis.
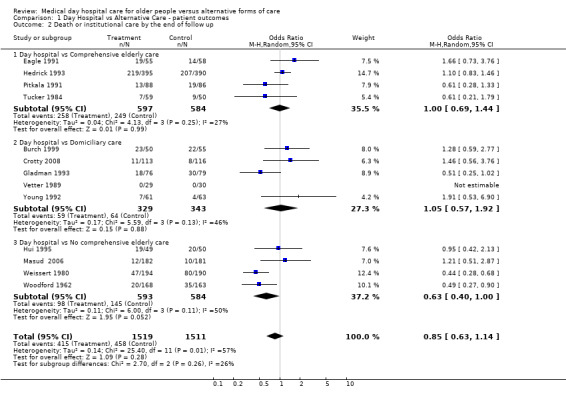
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 2 Death or institutional care by the end of follow up.
Death or deterioration in ADL
Seven trials published data on death or deterioration in ADL (Burch 1999; Gladman 1993; Hui 1995; Pitkala 1991; Vetter 1989; Weissert 1980; Young 1992). The pooled OR for all the trials at the end of scheduled follow up shows no difference between the day hospital and comparison interventions (OR 1.07; 95% CI 0.76 to 1.49; P = 0.70). Only Pitkala 1991 provided data for day hospital compared to comprehensive care and the difference was not significant (OR 1.18; 95% CI 0.63 to 2.18, P = 0.61). There was no difference between day hospital and domiciliary care (OR 1.41; 95% CI 0.82 to 2.42; P = 0.21) or no comprehensive care (OR 0.76; 95% CI 0.56 to 1.05; P = 0.09). There were no significant subgroup differences (P = 0.11) and no significant heterogeneity overall (Chi² = 10.25, df = 6, P = 0.11; I² = 41%; Analysis 1.3). Visual inspection of funnel plots did not identify any obvious signs of publication bias.
1.3. Analysis.
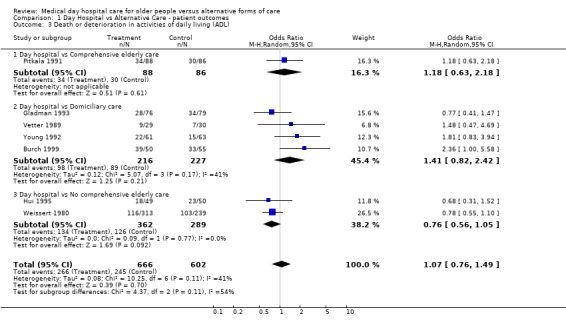
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 3 Death or deterioration in activities of daily living (ADL).
Death or poor outcome
Thirteen trials published data on death or poor outcome (Burch 1999; Cummings 1985; Eagle 1991; Gladman 1993; Hedrick 1993; Hui 1995; Pitkala 1991; Roderick 2001; Tucker 1984; Vetter 1989; Weissert 1980; Woodford 1962; Young 1992). Roderick 2001 reported data on poor outcome which they defined as "death, recurrent stroke and a six month Barthel score of < 14"; we determined that this was sufficiently similar to our own definition to include in the results. The pooled OR for all the trials at the end of scheduled follow up shows no significant difference between the day hospital and other interventions (OR 0.92; 95% CI 0.74 to 1.15; P = 0.49). There was no significant difference when day hospital was compared with comprehensive care (OR 1.05; 95% CI 0.79 to 1.40; P = 0.74) or domiciliary care (OR 1.08; 95% CI 0.67 to 1.74; P = 0.75). However, there was a significant difference in favour of the day hospital when compared with no comprehensive care (OR 0.72; 95% CI 0.53 to 0.99; P = 0.04), although subgroup results were not significantly different from each other (P = 0.17). There was no significant heterogeneity overall (Chi² = 17.27, df = 12, P = 0.14; I² = 31%; Analysis 1.4). Outcome data were missing for 55 day hospital patients and 121 controls (representing 4.6% of patients in the comprehensive care subgroup, 0.5% in the domiciliary care subgroup and 10.3% in the no comprehensive care subgroup). Best and worst case sensitivity analyses included the possibility of significant benefit (P < 0.0001) or harm (P < 0.05) from day hospital attendance. Visual inspection of funnel plots did not identify any obvious signs of publication bias.
1.4. Analysis.

Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 4 Death or poor outcome (institutional care, disability or deterioration).
Deterioration in ADL among survivors
We wished to examine the influence of day hospital attendance on the functional status of survivors. Although most trials described results in terms of ADL scores, seven different measures were used and reported in different ways. We therefore describe results in terms of recorded deterioration in ADL and the raw ADL results. Seven trials provided data on deterioration in ADL among survivors (Burch 1999; Gladman 1993; Hui 1995; Pitkala 1991; Vetter 1989; Weissert 1980; Young 1992). We judged the quality of the evidence for the following outcome as low (Table 1). Overall there was no difference between day hospital and alternative care in ADL scores (OR 1.11; 95% CI 0.68 to 1.80; P = 0.67). However, day hospital attenders appeared less likely to deteriorate than those receiving no comprehensive care (OR 0.61; 95% CI 0.38 to 0.97; P = 0.04). Differences were not significant when comparing day hospitals with comprehensive care (OR 1.21; 95% CI 0.58 to 2.52; P = 0.61) or domiciliary care (OR 1.59; 95% CI 0.87 to 2.90; P = 0.13). There were significant subgroup differences (P = 0.04) and evidence of heterogeneity (Chi² = 11.94, df = 6, P = 0.06; I² = 50%; Analysis 1.5). Visual inspection of funnel plots did not identify any obvious signs of publication bias.
1.5. Analysis.

Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 5 Deterioration in activities of daily living (ADL) in survivors.
ADL score
Fourteen trials reported a standardised measure of ADL among survivors. However, various measures were used and data were insufficient to allow a statistical summary of the results. Two trials demonstrated significant but small improvements in functional ability with day hospital attendance which was not sustained at six month follow up (Hui 1995; Tucker 1984). One trial (Young 1992) reported an improved functional outcome for the comparison group. The other 11 trials (Burch 1999; Cummings 1985; Eagle 1991; Gladman 1993; Hedrick 1993; Masud 2006; Parker 2009; Pitkala 1991; Roderick 2001; Vetter 1989; Weissert 1980) found no difference in disability scores between the day hospital and comparison groups (Analysis 1.6).
1.6. Analysis.
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 6 Activities of daily living (ADL) scores.
| Activities of daily living (ADL) scores | |
|---|---|
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | No significant difference in the Kenny ADL score ‐ Day hospital: 27.1 Control: 26 |
| Eagle 1991 | No significant difference in the Geriatric Quality of Life Questionnaire ADL score ‐ Day hospital: 4.01 Control: 4.43 |
| Hedrick 1993 | No significant in the physical dimension of the Sickness Impact Profile (NB high score indicates increased disability) ‐ Day hospital: 29.0 (SD 18.6) Control: 32.1 (18.8) |
| Pitkala 1991 | No data in this form |
| Tucker 1984 | No significant difference in the mean change in Northwick Park ADL score from baseline (NB high score indicates increased disability) Day hospital: 0.63 Control: ‐0.64 |
| Day hospital vs Domiciliary care | |
| Burch 1999 | No significant difference in Barthel index ‐ Day hospital: 14.5 (SD 4.9) Control: 15.7 (sd 4.5) |
| Gladman 1993 | No significant difference in median Barthel index ‐ Day hospital: 17 Control: 16 |
| Parker 2009 | No significant difference in mean (SD) Nottingham Extended Activities of Daily Living Scale Day hospital: 31.6 (15.4) Control: 28.1 (17.5) |
| Roderick 2001 | Significant improvement in Barthel score in both groups. No significant difference between groups. |
| Vetter 1989 | No significant difference in mean Barthel index ‐ Day hospital: 13.2 (SD 3.8) Control: 12.3 (SD 4.1) |
| Young 1992 | Significantly (P=0.01) lower Barthel ADL score ‐ Day hospital: 15 (IQR 12‐18) Control: 17 (IQR 15‐19) |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | No significant difference in mean Barthel index ‐ Day hospital: 17.1 (SD 3.6) Control: 15.6 (SD 5.6) |
| Masud 2006 | No significant difference in median (IQR) Barthel index scores
Day hospital: 19 (17‐20)
Control: 19 (17‐20) No significant difference in median (IQR) Nottingham Extended Activities of Daily Living (NEADL) scores Day hospital: 53 (43‐62) Control: 56 (43.8‐61) |
| Weissert 1980 | No comparable data |
| Woodford 1962 | No comparable data |
Subjective health status
A number of studies investigated subjective health status. However, various measures were used and we were unable to incorporate data into a meta‐analysis. Three studies investigating day hospital versus comprehensive care found no significant difference between the groups (Cummings 1985; Eagle 1991; Hedrick 1993). In Tucker 1984 there was a significant improvement in mood measured by the Zung index in the day hospital group compared to the comprehensive care group at final follow up (P = 0.01). Pitkala 1991 provided no comparable data. There were no significant differences in any of the studies investigating day hospital versus domiciliary care (Burch 1999; Gladman 1993; Parker 2009; Roderick 2001; Vetter 1989; Young 1992). For day hospital versus no comprehensive care, Hui 1995 found no significant differences. Weissert 1980 and Woodford 1962 did not provide comparable data (Analysis 1.7).
1.7. Analysis.
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 7 Subjective health status.
| Subjective health status | |
|---|---|
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | No significant difference in the modified Dupay assessment ‐ Day hospital: 30.4 Control: 25.9 |
| Eagle 1991 | No significant difference in the General Health Questionnaire ‐ Day hospital: 3.85 Control: 4.33 |
| Hedrick 1993 | No significant difference in the Sickness Impact Profile ‐ Day hospital: 34.1 Control: 34.5 |
| Pitkala 1991 | No comparable data |
| Tucker 1984 | There was a statistically significant improvement in mood measured by the Zung index in the Day hospital group compared to the Comprehensive elderly care group at final follow up (P = 0.01) |
| Day hospital vs Domiciliary care | |
| Burch 1999 | No significant difference in the change in the Philidelphia Geriatric Morale scale during follow up ‐ Day hospital: 1.80 Control: 0.92 |
| Gladman 1993 | No significant difference in the number of patients with distress (Nottingham Health Profile >30) ‐ Day hospital: 17 (33%) Control: 25 (48%) |
| Parker 2009 | There was no significant difference in the EuroQol index (difference in means 0.147, P = 0.141) or the EuroQol VAS (difference in means 0. 6.315, P = 0.187) |
| Roderick 2001 | No between groups significant difference for SF‐36 physical or mental health scales. The Philadelphia Geriatric Morale Scale scores fell in both groups (indicating lower morale) but less so in the domiciliary group. |
| Vetter 1989 | No significant difference in the Sickness Impact Profile |
| Young 1992 | No significant difference in the number of patients with distress (Nottingham Health Profile >30) ‐ Day hospital: 19 (41%) Control: 20 (39%) |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | No significant difference in the Geriatric Depression Scale |
| Weissert 1980 | No comparable data |
| Woodford 1962 | No comparable data |
Patient satisfaction
Data on patient satisfaction were only available from one study. Hui 1995 found no significant difference between the day hospital and no comprehensive care (Analysis 1.8).
1.8. Analysis.
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 8 Patient satisfaction.
| Patient satisfaction | |
|---|---|
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | No available data |
| Eagle 1991 | No available data |
| Hedrick 1993 | No comparable data |
| Pitkala 1991 | No comparable data |
| Tucker 1984 | No available data |
| Day hospital vs Domiciliary care | |
| Burch 1999 | No available data |
| Gladman 1993 | No available data |
| Roderick 2001 | No available data |
| Vetter 1989 | No available data |
| Young 1992 | No available data |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | No significant difference in the level of satisfaction |
| Weissert 1980 | No available data |
| Woodford 1962 | No available data |
Carer outcomes
Distress
There were no available or comparable data for day hospital versus comprehensive care or day hospital versus no comprehensive care. Data were available from three studies comparing day hospital with domiciliary care. Crotty 2008 and Gladman 1993 found no significant difference at follow up; Burch 1999 found a significant difference in the mean change between baseline and three months in the Caregiver Strain Index in both groups but no significant difference between groups. (Analysis 1.9).
1.9. Analysis.
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 9 Carer Distress.
| Carer Distress | |
|---|---|
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | No comparable data |
| Eagle 1991 | No available data |
| Hedrick 1993 | No comparable data |
| Pitkala 1991 | No comparable data |
| Tucker 1984 | No data available |
| Day hospital vs Domiciliary care | |
| Burch 1999 | There was a significant difference in the mean change between baseline and 3 months in the Caregiver Strain Index in both groups
Day hospital: ‐1.45 (95% CI ‐0.41, ‐2.49)
Control: ‐1.59 (‐0.62, ‐2.56) There was no significant difference between between groups |
| Crotty 2008 | No significant difference at 3 months in the Carer Strain Index Day hospital: 4.9 (3.9) Control: 4.3 (3.1) |
| Gladman 1993 | No significant difference at 6 months in the median Life Satisfaction Index ‐ Day hospital: 18 (IQR 11‐22) Control: 15 (IQR 10‐19) |
| Roderick 2001 | No available data |
| Vetter 1989 | No data available |
| Young 1992 | Proportion of carers showing distress (General Health Questionnaire 28 score > 5) ‐
Day hospital: 14 of 33 scored >5 (42%)
Control: 8 of 30 scored >5 (27%) Differences were not significant |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | No available data |
| Weissert 1980 | No available data |
| Woodford 1962 | No available data |
Resource use
Requiring Institutional care at the end of follow up
Thirteen trials provided information about the number of patients requiring institutional care at the end of follow up (Burch 1999; Crotty 2008; Eagle 1991; Gladman 1993; Hedrick 1993; Hui 1995; Masud 2006; Pitkala 1991; Tucker 1984; Vetter 1989; Weissert 1980; Woodford 1962; Young 1992). In one trial (Weissert 1980) these data were available only for a subgroup of patients (384 patients of 552 recruited to the main study). There was no difference between day hospital and all other services (OR 0.84; 95% CI 0.58 to 1.21; P = 0.35), or for any of the subgroups: day hospital versus comprehensive care (OR 0.91; 95% CI 0.70 to 1.19; P = 0.49), day hospital versus domiciliary care (OR 1.49; 95% CI 0.53 to 4.25; P = 0.45) or day hospital versus no comprehensive care (OR 0.58; 95% CI 0.28 to 1.20; P = 0.14). Overall there was significant heterogeneity (Chi² = 20.03, df = 11, P = 0.04; I² = 45%; Analysis 2.1). On the basis of these data (95% CI 10 to 34) 21 patients (95% CI 12.3 to 70.9) would need to attend day hospital (as opposed to receiving no comprehensive service) to prevent one admission to long term institutional care. Visual inspection of funnel plots did not identify any obvious signs of publication bias.
2.1. Analysis.

Comparison 2 Day Hospital vs Alternative Care ‐ resource outcomes, Outcome 1 Requiring institutional care at the end of follow up.
Hospital bed use
Although hospital use was described in several ways in the trials, it proved possible to obtain a standardised measure for 14 trials of average (mean) hospital bed use per patient recruited (Burch 1999; Cummings 1985; Eagle 1991; Gladman 1993; Hedrick 1993; Hui 1995; Masud 2006; Pitkala 1991; Roderick 2001; Tucker 1984; Vetter 1989; Weissert 1980; Woodford 1962; Young 1992; Analysis 2.2). A measure of variance was not possible for this analysis and therefore confidence limits cannot be reported. The results show a small reduction in bed use by the day hospital patients compared to other treatment across all trials: 13.6 versus 14.6 (Analysis 2.2), with subgroup results as follows:
2.2. Analysis.
Comparison 2 Day Hospital vs Alternative Care ‐ resource outcomes, Outcome 2 Hospital bed use during follow up.
| Hospital bed use during follow up | |
|---|---|
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | Day hospital: 206 bed days for 48 patients (4.3 days per patient) Control: 274 bed days for 48 patients (5.7 days per patient) |
| Eagle 1991 | Day hospital: 1388 bed days for 55 patients (25.2 days per patient) Control: 1351 bed days for 58 patients (23.3 days per patient) |
| Hedrick 1993 | Day hospital: 8020 bed days for 411 patients (19.5 days per patient) Control: 8067 bed days for 415 patients (19.4 days per patient) |
| Pitkala 1991 | Day hospital: 3538 bed days for 88 patients (40.2 days per patient) Control: 3713 bed days for 86 patients (43.2 days per patient) |
| Tucker 1984 | Day hospital: 472 bed days for 62 patients (7.6 days per patient) Control: 800 bed days for 58 patients (13.8 bed days per patient) |
| Day hospital vs Domiciliary care | |
| Burch 1999 | Day hospital: 923 bed days for 50 patients (18.5 per patient) Control: 1438 bed days for 55 patients (26.1 per patient) |
| Gladman 1993 | Day hospital: 436 bed days for 76 patients (5.7 days per patient) Control: 766 bed days for 79 patients (9.7 days per patient) |
| Roderick 2001 | Day hospital: 296 bed days for 74 patients ( 4 days per patient) Control:203 bed days for 66 patients (3 bed days per patient) |
| Vetter 1989 | No bed days used in either group |
| Young 1992 | Day hospital: 311 bed days for 61 patients (5.1 days per patient) Control: 278 bed days for 63 patients (4.4 days per patient) |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | Day hospital: 81 bed days for 59 patients (1.4 days per patient) Control: 165 bed days for 61 patients (2.7 days per patient) |
| Masud 2006 | Day hospital: 552 bed days for 172 patients (3.2 days per patient) Control: 529 bed days for 171 patients (3.1 days per patient) |
| Weissert 1980 | Day hospital: 3443 bed days for 313 patients (11.0 days per patient) Control: 2868 bed days for 239 patients (12.0 days per patient) |
| Woodford 1962 | Day hospital: 2534 bed days for 168 patients (15.1 days per patient) Control: 2375 bed days for 163 patients (14.6 days per patient) |
Day hospital versus comprehensive care ‐ 20.5 versus 21.5.
Day hospital versus domiciliary care ‐ 6.8 versus 9.2.
Day hospital versus no comprehensive care ‐ 9.3 versus 9.4.
Data from Parker 2009 was in a format that did not allow us to incorporate it into the above analysis. However, they reported the mean total length of stay in hospital for patients which was higher in the day hospital group compared to the home rehabilitation group (mean difference 9.3 days; 95% CI 12.5 to 31.1; P > 0.05).
Costs
A number of studies reported a comparison of treatment costs (Analysis 2.3), but methods for reporting data were not consistent and therefore the data could not be incorporated into a meta‐analysis. Seven studies reported that day hospital attendance was more expensive than the comparison treatment (Burch 1999; Gladman 1993; Hedrick 1993; Masud 2006; Tucker 1984; Weissert 1980; Young 1992). Three trials reported that the costs were similar (Hui 1995; Cummings 1985; Roderick 2001). Woodford 1962 reported that day hospital attendance was considerably less expensive than inpatient care (8% of weekly inpatient costs) but made no comparison of other costs incurred specifically by the comparison group. Parker 2009 reported that there was insufficient evidence to support the hypothesis that rehabilitation is less expensive in a home based setting.
2.3. Analysis.
Comparison 2 Day Hospital vs Alternative Care ‐ resource outcomes, Outcome 3 Resource use.
| Resource use | |
|---|---|
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | Average treatment cost per patient to 3 months post discharge ‐ Day hospital: $ 16,966 Control: $ 14,082 |
| Eagle 1991 | No cost data |
| Hedrick 1993 | Mean total costs over 12 months ‐ Day hospital: $ 28,709 Control: $ 26, 204 |
| Pitkala 1991 | No costing data |
| Tucker 1984 | Average cost for 5 months care ‐ Day hospital: NZ$ 3052 Control: NZ$ 2083 |
| Day hospital vs Domiciliary care | |
| Burch 1999 | Total annual cost per attendance ‐ Day hospital: £ 77.39 Control: £ 59.46 |
| Gladman 1993 | Mean total health service cost per patient ‐ Day hospital: £ 456.90 Control: £ 362.60 |
| Parker 2009 | (entries) Mean total cost at 213 days: Day hospital (21) £10,102; Home based rehab (25) £14,330 (note SDs not reported) (entries) Mean total cost at 395 days: Day hospital (13) £23,812; Home based rehab (23) £26,105 (note SDs not reported) (entries) Median total cost at 213 days: Day hospital (21) £5958; Home based rehab (25) £7679 (note IQRs not reported) (entries) Median total cost at 395 days: Day hospital (13) £9842; Home based rehab (23) £18,432 (note IQRs not reported) |
| Roderick 2001 | Median costs per patient: Rehabilitation costs: Day hospital:£1090 (IQR 513‐1475), Control group: 933 (IQR 339‐2010). Median Total health and social service costs: Day hospital 1568 (IQR 982‐3130), Control £2208 (IQR 694‐3849) |
| Vetter 1989 | No cost data |
| Young 1992 | Mean total costs for 8 weeks treatment ‐ Day hospital: £ 620 (IQR 555‐730) Control: £385 (IQR 240‐510) |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | Mean cost of treatment to the health service over 6 months ‐ Day hospital: $ 58,168 (SEM 25,898) Control: $ 51, 809 (SEM 30,480) |
| Masud 2006 | The mean falls programme cost was £349 per person. With additional health‐care costs, this resulted in a mean incremental cost of £578 for the intervention Health service resource use and costs. Total cost per participant mean (SD): Day hospital £2,238 (4957) Control £1,659 (5100) |
| Weissert 1980 | Average cost for 1 year ‐ Day hospital: $ 5813 Control: $ 3815 |
| Woodford 1962 | No formal costing |
For the sub category comparing mean treatment costs between day hospital care and other comprehensive care services, Cummings 1985, Hedrick 1993 and Tucker 1984 reported higher costs for the day hospital. The Cummings 1985 and Hedrick 1993 trials included the cost of nursing home care. There was no information from two trials for this comparison (Eagle 1991; Pitkala 1991). For the sub category comparing treatment costs between day hospital care and domiciliary care the Burch 1999; Gladman 1993 and Young 1992 trials found that day hospital was more expensive. In the Roderick 2001 trial, the day hospital was more expensive for rehabilitations costs but was less so when considering total health and social services costs. There was no information from three trials for this comparison (Crotty 2008; Parker 2009; Vetter 1989). For the sub category comparing treatment costs between day hospital care and no comprehensive care, day hospital was more expensive than no comprehensive care in Hui 1995, Masud 2006 and Weissert 1980. No formal costing data were provided by Woodford 1962.
Assessments of the quality of the body of evidence
Using the GRADE approach we judged the quality of the body of evidence to be low for the patient outcomes of death, death or institutional care, death or deterioration in ADL, death or poor outcome, and deterioration in ADL (Table 1; Table 2; Table 3; Table 4; Appendix 20). For each outcome the body of evidence was from randomised controlled trials but we reduced the quality rating because of a high likelihood of bias in the included studies and imprecision in the effect estimates (wide CIs). We did not reduce the quality rating despite evidence of heterogeneity because this was anticipated due to the diversity of the populations and of the interventions.
Discussion
Summary of main results
The majority of included studies have compared day hospital care with other services. Only four trials employed a comparison group of patients who received neither comprehensive care nor domiciliary rehabilitation (Masud 2006; Woodford 1962; Hui 1995; Weissert 1980). The results from this group were the most favourable to day hospital care, but these four trials are now quite old. Overall the quality of the evidence was low, therefore further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
For the outcome of death, there was no difference between day hospitals and other services, including when day hospitals were compared with any of the subcategories individually. For the combined outcome of death or institutional care there was no significant difference between the day hospital and all other services. For the combined outcome of death or deterioration in ADL, there was no significant difference between the day hospital and other services although there was a trend in favour of the day hospital compared with no comprehensive care. For the combined outcome of death or poor outcome, there was a significant difference in favour of the day hospital when compared with no comprehensive services. For the outcome of deterioration in ADL, there was a significant difference between attending day hospital and no comprehensive care. However, there was no difference between the day hospital and other services.
When considering resource implications among those requiring institutional care, there was no difference at the end of follow up between day hospital and other services. There was a slight reduction in hospital bed use overall for day hospital patients and particularly when day hospitals were compared with domiciliary services; however, whilst a summary statistic was not possible for hospital bed use or cost, individual studies suggest that day hospitals are predominantly as expensive or more expensive than others services.
Overall completeness and applicability of evidence
The day hospital trials included in this systematic review have predominantly employed a pragmatic design and have attempted to address broad questions of overall day hospital effectiveness. This review included 16 studies with 3689 participants, although within the analyses of specific outcomes these numbers were reduced as each study only contributed data for some comparisons. It is unfortunate that data was not available, or in a suitable format, to undertake statistical analyses for the patient outcomes of activities of daily living, subjective health status, patient satisfaction or carer distress, or for the resource outcome of cost. It also proved impossible to determine a summary statistic for disability because, although included as an outcome measure in 11 trials, different measurement instruments were used and variance data were not available. The outcome of death was reported by all studies, however other adverse events and effects were not reported consistently by all studies, thus compromising the overall completeness of findings.
We have based the systematic review on a broad comparison of day hospital care versus alternative services. We wanted to be able to generalise to a range of scenarios and not defined populations. As we anticipated considerable variations in the comparison services, these were identified and categorised prior to data collection and analysis. We have ensured that the treatment schedules described matched our pre‐determined definition of day hospital care. Thus, whilst the study by Weissert and colleagues (Weissert 1980) refers to ‘day care’ services, the intervention provided fitted our definition of day hospital care and was therefore included. A lack of consensus in terminology related to day hospitals has also been noted elsewhere (Petermans 2011).
The applicability of the findings from this review to various regions will depend on current health care provision and populations. As comprehensive care, in one form or another, is likely to be available to many older patients who require rehabilitation, the relevance of some comparisons may be limited in certain countries and populations; specifically the findings from the comparison between day hospitals and no comprehensive care (which was favourable for the day hospital on the combined measure of death or poor outcome, with a trend in favour of the day hospital for the combined measure of death or institutional care). This review found little evidence that day hospitals were better than alternative types of comprehensive service. However, the diversity in the content of alternative services and the populations being served (studies originated from seven different counties) means the external validity of this finding may be compromised. Furthermore, 10 of the studies were at least 20 years old and the types of health service and the populations being served may not reflect current practice or requirements. Services may need to be considered on a case by case basis regarding their applicability against current health provision.
Two main limitations of our review lie in the multinational settings of the studies and in the forty year time span of study publication, during which time health and social care policies inevitably changed. It is disappointing that there have been only four further evaluations of the effectiveness of day hospital care since this review was first published (Forster 1999a). Nonetheless, the data presented here probably represent the best evidence currently available upon which to base a judgment of day hospital effectiveness.
Quality of the evidence
There are limitations due to the lack of statistical power resulting from small, heterogeneous trials. As a result there is a danger of both false‐positive and false‐negative results being generated. Furthermore, the data was from a series of studies performed by researchers operating independently and the studies were therefore not functionally equivalent. This resulted in significant heterogeneity through variations in participants and in the interventions employed in the various day hospitals and comparison treatments. Participants and interventions likely differed in ways that impacted the results. Consequently, we cannot assume a common effect size (Borenstein 2009). A frequently encountered issue with pragmatic rehabilitation trials is that the methods to record subject characteristics, which might influence prognosis and treatment processes, are poorly developed. Considerable detail was recorded in the USA (Hedrick 1993) trial; it is important that any future trials also address this issue. Data were missing for a number of outcomes which could theoretically alter the scale and direction of the results. All of our conclusions must be qualified by this condition.
It is possible that biases have resulted in the overestimation or underestimation of the effects of the intervention. All studies were at a high risk of bias for blinding of participants and personnel; this is typical of such an intervention and effective blinding would be challenging to implement in view of ethical considerations which require participants to have prior knowledge of potential interventions. However, a lack of blinding of outcome assessment was also problematic and only half the studies were considered to have a low risk in this domain. Contamination can result in the underestimation of treatment effects and whilst not all studies were judged to be of high risk, contamination and deviation from the protocol (switching between interventions) did feature in some studies comparing day hospitals with other comprehensive services and domiciliary care. In addition, the risk of selective reporting was often unclear. Only the three studies which were reported in the last eight years had available protocols against which their reports could be assessed to determine if all outcomes had been reported. Finally, half of the studies were considered to have a low risk of bias for the domain of incomplete outcome data. This should be considered positive, taking into account the nature of the intervention and participants, post intervention follow up periods, and the age of the studies where attrition was less frequently reported.
Potential biases in the review process
The search strategy was extensive, taking into account multiple databases and sources, and this is reflected in the large number of titles identified. Two authors extracted all data, discussions were undertaken to achieve consensus, and a third person was utilised where disagreements remained. As a result, we are confident in the quality of the review. It was unfortunate, however, that we could not quantitatively combine data for a number of outcomes, due to the diversity of measures used (for example, ADL, subjective health status, patient satisfaction, carer distress, bed use and resource use).
Publication bias (Egger 1997) remains a possibility in any review process. However, our search strategy was extensive and included contacting the authors of papers relating to day hospital care around the world.
We were fortunate that many of the authors of the published papers or abstracts were able to provide additional information which has not been published previously.
Agreements and disagreements with other studies or reviews
Another systematic review drew similar conclusions to our review (Petermans 2011). They found that geriatric day hospitals were better for patients undergoing assessment and intervention than no comprehensive care. However, they found little benefit when compared to treatment in a geriatric ward or other geriatric services. They also found few studies reporting on the outcome of patient satisfaction. The authors did not include meta‐analysis and they did not report on any cost‐benefit outcomes; their conclusions were drawn from various sources including RCTs and cohort studies. Another systematic review, with meta‐analysis, found that comprehensive geriatric assessments linking geriatric evaluation with long term management are effective in improving survival and function in older people (Stuck 1993).
Individual results from the included studies suggest that day hospitals are probably as expensive or more expensive than other comprehensive or domiciliary services. Several costing studies have drawn attention to the expense of day hospital services (Eagle 1987; Gerard 1988; Gladman 1994; MacFarlane 1979; Young 1993).
Authors' conclusions
Implications for practice.
Any conclusions are limited by the relatively small amount of data available and the low quality of the data contributing to a number of important outcomes. Day hospital care appears to be an effective outpatient service for older people, but no more effective (at least for the outcomes examined in this review), and possibly more expensive, than other forms of comprehensive care. These findings do not support the closure of day hospital services but do support the exploration of alternative systems for delivering an equivalent or superior form of comprehensive care. Our findings support the view that day hospital attendance needs to be carefully monitored (George 1989) and the staff and facilities used as flexibly and efficiently as possible (Brocklehurst 1995).
Implications for research.
The findings are limited by the relatively small amount of data available and overall low quality of the evidence; further research is likely to impact on our confidence in the estimate of effect. Further randomised trials are justifiable and should focus on comparing services which aim to provide an equivalent intervention to day hospital care (e.g. domiciliary care). Given the diversity of patients attending day hospitals and the corresponding diversity of day hospital interventions employed, future trials should be large, multi‐centre trials or should examine more focused questions. Outcomes should include subjective health status and carer well being. There is concern that commonly used measures of disability lack sensitivity to change in the outpatient setting of a day hospital due to their ceiling effect (Parker 1994). Future trials should incorporate measures of instrumental activities of daily living as a more relevant and potentially more sensitive outcome. Furthermore, future trials should incorporate adequate methods of randomisation and allocation concealment, and undertake blinded outcome assessment where possible, as well as ensuring that methods are adequately reported.
What's new
| Date | Event | Description |
|---|---|---|
| 24 April 2014 | New search has been performed | New searches performed and three new trials identified |
| 24 April 2014 | New citation required but conclusions have not changed | Three new trials have been identified, five studies are awaiting classification |
History
Review first published: Issue 3, 1999
| Date | Event | Description |
|---|---|---|
| 12 November 2008 | Amended | Minor changes |
| 14 August 2008 | New search has been performed | New search |
| 10 July 2008 | Amended | Converted to new review format. |
| 22 June 2008 | New citation required but conclusions have not changed | This review is an update of the review first published in 1999. The total number of studies included is 16. |
Acknowledgements
The Day Hospital Group is formed from the authors of this systematic review and the authors of the original trials. We are very pleased to acknowledge the help and support given by the Day Hospital trialists who provided additional information about trial procedures and data and are members of the Day Hospital Group. They are as follows: S Burch, J Longbottom, M Mackay, C Borland, T Prevost (Burch 1999); K Pitkala (Pitkala 1991); J Gladman (Gladman 1993); S Hedrick, ML Rothman, MK Chapko, JL Ehreth, P Diehr, TS Inui, RT Connis, PL Grover, JR Kelly (Hedrick 1993); E Hui, C Lum, RLC Kay, J Woo, KH Or (Hui 1995); N Vetter (Vetter 1989).
V Cummings, J Eagle and SJ Ogle also expressed support for the review. J Baskett provided additional information and TK Kong identified a relevant trial. For this edition, we wish to thank the authors of the included trials (Crotty 2008; Masud 2006; Parker 2009) who provided additional information. A thanks to S Ozer from the Academic Unit of Elderly Care, Bradford Teaching Hospital NHS Foundation Trust, who contributed to data extraction for risk of bias tables for the original included studies. We wish to thank D Andre from the University of Leeds for conducting the literature searches and P Spoor and colleagues for undertaking previous literature searches. We also wish to thank R Lambley who was a co‐author on the original review.
Appendices
Appendix 1. Cochrane Central search strategy
2012 to Aug 2013 Last Saved: 13/08/2013 14:32:36.502 Description: DA 11.10.12 ID Search #1 MeSH descriptor: [Day Care] this term only #2 (daycare or day care) .ti,ab. #3 (child* daycare or child* day care) .ti,ab. #4 #2 not #3 #5 (day N2 (hospital* or clinic* or unit* or service*)) tw. #6 (day healthcare or day health care) .tw. #7 #1 or #4 or #5 or #6 #8 MeSH descriptor: [Outpatient Clinics, Hospital] this term only #9 MeSH descriptor: [Outpatients] this term only #10 (outpatient* or out‐patient*) .tw. #11 MeSH descriptor: [Ambulatory Care Facilities] this term only #12 MeSH descriptor: [Ambulatory Care] this term only #13 #8 or #9 or #10 or #11 or #12 #14 MeSH descriptor: [Rehabilitation Centers] this term only #15 #13 or #14 #16 MeSH descriptor: [Aged] explode all trees #17 MeSH descriptor: [Geriatrics] this term only #18 MeSH descriptor: [Geriatric Nursing] this term only #19 MeSH descriptor: [Geriatric Assessment] this term only #20 MeSH descriptor: [Medicare] explode all trees #21 MeSH descriptor: [Health Services for the Aged] this term only #22 (geriatr* or elder* or gerontol* or seniors or senior citizen* or older adult* or older person* or older people) .ti,ab. #23 (over N2 ("60" or "61" or "62" or "63" or "64" or "65" or "66" or "67" or "68" or "69" or "70" or "71" or "72" or "73" or "74" or "75" or "76" or "77" or "78" or "79" or "80" or "81" or "82" or "83" or "84" or "85" or "86" or "87" or "88" or "89" or "90" or "91" or "92" or "93" or "94" or "95" or "96" or "97" or "98" or "99" or "100") N years) .ti,ab. #24 #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 #25 #15 and #24 from 2012 to 2013, in Trials
Appendix 2. Medline search strategy
Database: Ovid MEDLINE(R) <1946 to September Week 4 2012> Search Strategy: 1 Day Care/ (4533) 2 (daycare or day care).ti,ab. not (child* daycare or child* day care).ti,hw. (4034) 3 (day adj2 (hospital* or clinic* or unit* or service*)).tw. (10712) 4 (day healthcare or day health care).tw. (103) 5 or/1‐4 [day care] (16542) 6 Outpatient Clinics, Hospital/ (13890) 7 Outpatients/ (7739) 8 (outpatient* or out‐patient*).tw. (105361) 9 ambulatory care facilities/ (11057) 10 ambulatory care/ (34113) 11 or/6‐10 [outpatients or ambulatory care] (143564) 12 Rehabilitation Centers/ (6387) 13 5 or 11 or 12 [day care or outpatients or ambulatory care or rehabilitation centers] (163835) 14 exp Aged/ (2156773) 15 Geriatrics/ (25947) 16 Geriatric Nursing/ (11831) 17 Geriatric Assessment/ (16544) 18 exp medicare/ (33506) 19 Health Services for the Aged/ (14224) 20 (geriatr* or elder* or gerontol* or seniors or senior citizen* or older adult* or older person* or older people).ti,ab. (212717) 21 (over adj2 ("60" or "61" or "62" or "63" or "64" or "65" or "66" or "67" or "68" or "69" or "70" or "71" or "72" or "73" or "74" or "75" or "76" or "77" or "78" or "79" or "80" or "81" or "82" or "83" or "84" or "85" or "86" or "87" or "88" or "89" or "90" or "91" or "92" or "93" or "94" or "95" or "96" or "97" or "98" or "99" or "100") adj years).ti,ab. (11511) 22 or/14‐21 [aged] (2235474) 23 13 and 22 [day care or outpatients or rehabilitation centers and aged terms] (50773) 24 randomized controlled trial.pt. (338627) 25 controlled clinical trial.pt. (85346) 26 randomized.ab. (241408) 27 clinical trials as topic.sh. (162900) 28 randomly.ab. (173245) 29 trial.ab. (250145) 30 or/24‐29 (831491) 31 exp animals/ not humans.sh. (3791651) 32 30 not 31 [RCT Filter] (762874) 33 23 and 32 [Search strategy and RCT filter] (8372) 34 limit 33 to yr="1996‐ 2012" (6212)
Appendix 3. Medline in Process search strategy
Search Strategy: 1 (daycare or day care).ti,ab. not (child* daycare or child* day care).ti,hw. (185) 2 (day adj2 (hospital* or clinic* or unit* or service*)).tw. (429) 3 (day healthcare or day health care).tw. (4) 4 or/1‐3 [day care] (603) 5 (outpatient* or out‐patient*).tw. (4842) 6 ambulatory care.tw. (143) 7 or/5‐6 [outpatients or ambulatory care] (4961) 8 Rehabilitation Centers.tw. (39) 9 3 or 7 or 8 [day care or outpatients or ambulatory care or rehabilitation centers] (4993) 10 (geriatr* or elder* or gerontol* or seniors or senior citizen* or older adult* or older person* or older people).ti,ab. (10162) 11 (over adj2 ("60" or "61" or "62" or "63" or "64" or "65" or "66" or "67" or "68" or "69" or "70" or "71" or "72" or "73" or "74" or "75" or "76" or "77" or "78" or "79" or "80" or "81" or "82" or "83" or "84" or "85" or "86" or "87" or "88" or "89" or "90" or "91" or "92" or "93" or "94" or "95" or "96" or "97" or "98" or "99" or "100") adj years).ti,ab. (548) 12 or/10‐11 [aged] (10502) 13 9 and 12 [day care or outpatients or rehabilitation centers and aged terms] (201) 14 limit 13 to yr="1996 ‐Current" (191)
Appendix 4. Embase search strategy
1 *day care/ (4925) 2 (daycare or day care).ti,ab. not (child* daycare or child* day care).ti,hw. (8090) 3 (day adj2 (hospital* or clinic* or unit* or service*)).tw. (18818) 4 (day healthcare or day health care).tw. (133) 5 or/1‐4 [day care] (28159) 6 *outpatient department/ (14428) 7 *outpatient/ (7212) 8 (outpatient* or out‐patient*).tw. (172022) 9 *ambulatory care/ (12390) 10 or/6‐9 [outpatients or ambulatory care] (191843) 11 *rehabilitation center/ (3505) 12 5 or 10 or 11 [day care or outpatients or ambulatory care or rehabilitation centers] (220802) 13 *aged/ (45020) 14 *geriatrics/ (29516) 15 *geriatric nursing/ (8307) 16 *geriatric assessment/ (3843) 17 *medicare/ (20657) 18 *elderly care/ (17857) 19 (geriatr* or elder* or gerontol* or seniors or senior citizen* or older adult* or older person* or older people).ti,ab. (329006) 20 (over adj2 ("60" or "61" or "62" or "63" or "64" or "65" or "66" or "67" or "68" or "69" or "70" or "71" or "72" or "73" or "74" or "75" or "76" or "77" or "78" or "79" or "80" or "81" or "82" or "83" or "84" or "85" or "86" or "87" or "88" or "89" or "90" or "91" or "92" or "93" or "94" or "95" or "96" or "97" or "98" or "99" or "100") adj years).ti,ab. (18155) 21 or/13‐20 [aged] (400729) 22 12 and 21 [day care or outpatients or rehab centers and aged terms] (11545) 23 Clinical trial/ (896532) 24 Randomized controlled trial/ (356334) 25 Randomization/ (63384) 26 Single blind procedure/ (18110) 27 Double blind procedure/ (121701) 28 Crossover procedure/ (38424) 29 Randomi?ed controlled trial$.tw. (92881) 30 Rct.tw. (12449) 31 Random allocation.tw. (1368) 32 Randomly allocated.tw. (19792) 33 Allocated randomly.tw. (1952) 34 (allocated adj2 random).tw. (887) 35 Single blind$.tw. (14138) 36 Double blind$.tw. (149363) 37 ((treble or triple) adj blind$).tw. (368) 38 Prospective study/ (247788) 39 or/23‐38 (1293655) 40 Case study/ (29938) 41 Case report.tw. (276189) 42 Abstract report/ or letter/ (900527) 43 or/40‐42 (1201339) 44 39 not 43 [RCT Filter] (1261174) 45 22 and 44 [day care or outpatients or rehab centers and aged terms with RCT filter] (1434)
Appendix 5. Cinahl search strategy
# Query Limiters/Expanders Last Run Via Results Action S34 (S23 and S33) Limiters ‐ Published Date: 20121001‐20130831 Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 103 S33 (S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32) Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 159,352 S32 allocat* random* Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 3,266 S31 MH quantitative studies Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 8,934 S30 random* allocat* Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 3,266 S29 MH random assignment Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 29,624 S28 randomi?ed control* trial* Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 41,208 S27 singl* n1 blind* or doubl* blind* or trebl* n1 blind* or tripl* n1 blind* or singl* n1 mask* or doubl* n1 mask* or trebl* n1 mask* or tripl* n1 mask* Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 28,645 S26 clinic* n1 trial* Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 96,650 S25 PT clinical trial Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 50,625 S24 MH clinical trials+ Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 116,409 S23 S13 and S22 Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 17,212 S22 S14 or S15 or S16 or S17 or S18 or S19 or S21 Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 336,036 S21 TI ( over N2 "60 years" or over N2 "61 years" or over N2 "62 years" or "over N2 63 years" or "over N2 64 years" or over N2 “65 years" or "over N2 "66 years" or over N2 "67 years" or over N2 "68 years" or over N2 "69 years" or over N2 "70 years" or over N2 "71 years" or over N2 "72 years" or over N2 "73 years" or "over N2 "74 years" or over N2 "75 years" or over N2 "76 years" or over N2 "77 years" or over N2 "78 years" or over N2 "79 years" or over N2 "80 years" or over N2 "81 years" or over N2 "82 years" or over N2 "83 years" or over N2 "84 years" or over N2 "85 years" or over N2 "86 years" or over N2 "87 years" or over N2 "88 years" or over N2 "89 years" or over N2 "90 years" or over N2 "91 years" or over N2 "92 years" or over N2 "93 years" or over N2 "94 years" or over N2 "95 years" or over N2 "96 years" or over N2 "97 years" or over N2 "98 years" or over N2 "99 years" or over N2 "100 years" ) OR AB ( over N2 "60 years" or over N2 "61 years" or over N2 "62 years" or "over N2 63 years" or "over N2 64 years" or over N2 “65 years" or "over N2 "66 years" or over N2 "67 years" or over N2 "68 years" or over N2 "69 years" or over N2 "70 years" or over N2 "71 years" or over N2 "72 years" or over N2 "73 years" or "over N2 "74 years" or over N2 "75 years" or over N2 "76 years" or over N2 "77 years" or over N2 "78 years" or over N2 "79 years" or over N2 "80 years" or over N2 "81 years" or over N2 "82 years" or over N2 "83 years" or over N2 "84 years" or over N2 "85 years" or over N2 "86 years" or over N2 "87 years" or over N2 "88 years" or over N2 "89 years" or over N2 "90 years" or over N2 "91 years" or over N2 "92 years" or over N2 "93 years" or over N2 "94 years" or over N2 "95 years" or over N2 "96 years" or over N2 "97 years" or over N2 "98 years" or over N2 "99 years" or over N2 "100 years" ) Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 1,959 S20 TI ( geriatr* or elder* or gerontol* or seniors or "senior citizen*" or "older adult*" or "older person*" or "older people" ) OR AB ( geriatr* or elder* or gerontol* or seniors or "senior citizen*" or "older adult*" or "older person*" or "older people" ) Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 79,409 S19 MH health services for the aged Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 4,142 S18 MH medicare+ Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 20,935 S17 MH geriatric assessment Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 5,669 S16 MH Gerontologic Nursing Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 9,478 S15 MH geriatrics Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 2,281 S14 MH aged+ Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 313,321 S13 S5 or S11 or S12 Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 62,380 S12 MH rehabilitation centers Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 5,020 S11 S6 or S7 or S8 or S9 or S10 Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 52,172 S10 MH ambulatory care Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 5,740 S9 MH ambulatory care facilities Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 3,064 S8 outpatient* or "out patient*" Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 46,426 S7 MH outpatients Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 29,211 S6 MH outpatient service Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 3,231 S5 S1 or S2 or S3 or S4 Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 6,565 S4 day healthcare or day health care Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 378 S3 day N2 hospital* or day N2 clinic* or day N2 unit* or day N2 service* Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 3,023 S2 TI ( daycare or day care ) OR AB ( daycare or day care ) NOT TI ( child* daycare or child* day care ) NOT MW ( child* daycare or child* day care ) Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 3,013 S1 MH day care Search modes ‐ Boolean/Phrase Interface ‐ EBSCOhost Research Databases Search Screen ‐ Advanced Search Database ‐ CINAHL 1,722
Appendix 6. AMED search strategy
Database: AMED (Allied and Complementary Medicine) <1985 to August 2013> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 Day care/ (255) 2 (daycare or day care).ti,ab. not (child* daycare or child* day care).ti,hw. (206) 3 (day adj2 (hospital* or clinic* or unit* or service*)).tw. (358) 4 (day healthcare or day health care).tw. (6) 5 or/1‐4 [day care] (641) 6 outpatient clinics hospital/ (75) 7 Outpatients/ (243) 8 (outpatient* or out‐patient*).tw. (59166) 9 ambulatory care facilities/ (36) 10 Ambulatory care/ (359) 11 or/6‐10 [outpatients or ambulatory care] (59262) 12 Rehabilitation centers/ (295) 13 5 or 11 or 12 [day care or outpatients or ambulatory care or rehabilitation centers] (59841) 14 exp Aged/ (10822) 15 Geriatrics/ (325) 16 Geriatric Nursing/ (92) 17 Geriatric Assessment/ (219) 18 exp medicare/ (212) 19 Health Services for the Aged/ (758) 20 (geriatr* or elder* or gerontol* or seniors or senior citizen* or older adult* or older person* or older people).ti,ab. (9559) 21 (over adj2 ("60" or "61" or "62" or "63" or "64" or "65" or "66" or "67" or "68" or "69" or "70" or "71" or "72" or "73" or "74" or "75" or "76" or "77" or "78" or "79" or "80" or "81" or "82" or "83" or "84" or "85" or "86" or "87" or "88" or "89" or "90" or "91" or "92" or "93" or "94" or "95" or "96" or "97" or "98" or "99" or "100") adj years).ti,ab. (251) 22 or/14‐21 [aged] (14194) 23 13 and 22 [day care or outpatients or rehabilitation centers and aged terms] (4477) 24 limit 23 to yr="2012 ‐Current" (210) 25 remove duplicates from 24 (210)
Appendix 7. PeDRO search strategy
Database: PeDRO, Platform: Centre for Evidence‐Based Physiotherapy, Dates searched: Oct 2012 to 14 Aug 2013
Searched in Title 1. Day hospital 2. Day care 3. Daycare as using broader terms brought back irrelevant results.
No results found
Appendix 8. ASSIA search strategy
ASSIA Day care search update Oct 2012 to Aug 2013 DA all((daycare OR "day care") OR (outpatient* OR out patient* OR "ambulatory care*" OR "rehab* center*" OR "rehab* centre*") AND (geriatric* OR elder* OR gerontol* OR seniors OR "senior citizen*" OR "older adult*" OR "older person*" OR "older people") AND (RCT OR Random*) NOT (child* OR young* OR boy* OR girl*)) Limited to 11th Oct 2012 to 14th August 2013
Appendix 9. IBSS search strategy
Day Hospitals Search Strategy 2012 to 2013 IBSS all(daycare OR "day care") OR all((outpatient* OR out patient* OR "ambulatory care*" OR "rehab* center*" OR "rehab* centre*")) AND all(geriatric* OR elder* OR gerontol* OR seniors OR "senior citizen*" OR "older adult*" OR "older person*" OR "older people") NOT all(child* OR young*) Limited to 11th Oct 2012 to 14th Aug 2013
Appendix 10. PsycINFO search strategy
Database: PsycINFO <1806 to August Week 1 2013> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 Adult Day Care/ (264) 2 day care centers/ not (child* daycare or child* day care).ti,hw. (667) 3 (daycare or day care).ti,ab. not (child* daycare or child* day care).ti,hw. (3001) 4 (day adj2 (hospital* or clinic* or unit* or service*)).tw. (3327) 5 (day healthcare or day health care).tw. (41) 6 or/1‐5 [day care] (6249) 7 outpatients/ (5177) 8 (outpatient* or out‐patient*).tw. (41880) 9 Outpatient Treatment/ (5069) 10 or/6‐9 [outpatients or ambulatory care] (48380) 11 Rehabilitation Centers/ (511) 12 6 or 10 or 11 [day care or outpatients or ambulatory care or rehabilitation centers] (48858) 13 exp Aging/ (35456) 14 Geriatrics/ (6518) 15 Geriatric Assessment/ (723) 16 exp Medicare/ (1239) 17 (geriatr* or elder* or gerontol* or seniors or senior citizen* or older adult* or older person* or older people).ti,ab. (88922) 18 (over adj2 ("60" or "61" or "62" or "63" or "64" or "65" or "66" or "67" or "68" or "69" or "70" or "71" or "72" or "73" or "74" or "75" or "76" or "77" or "78" or "79" or "80" or "81" or "82" or "83" or "84" or "85" or "86" or "87" or "88" or "89" or "90" or "91" or "92" or "93" or "94" or "95" or "96" or "97" or "98" or "99" or "100") adj years).ti,ab. (1178) 19 or/13‐18 [aged] (106221) 20 12 and 19 [day care or outpatients or rehabilitation centers and aged terms] (2853) 21 limit 20 to yr="2012‐Current" (218) 22 remove duplicates from 21 (218)
Appendix 11. HMIC search strategy
Database: HMIC Health Management Information Consortium <1983 ‐ present> Search Strategy: ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐ 1 Day care/ (766) 2 (daycare or day care).ti,ab. not (child* daycare or child* day care).ti,hw. (1083) 3 (day adj2 (hospital* or clinic* or unit* or service*)).tw. (1265) 4 (day healthcare or day health care).tw. (12) 5 or/1‐4 [day care] (2317) 6 Out patient departments/ (488) 7 Out patients/ (700) 8 (outpatient* or out‐patient*).tw. (3986) 9 ambulatory care/ (205) 10 Ambulatory care services/ (39) 11 out patient care/ (181) 12 or/6‐11 [outpatients or ambulatory care] (4400) 13 Rehabilitation centres/ (60) 14 5 or 12 or 13 [day care or outpatients or ambulatory care or rehabilitation centers] (6658) 15 exp older people/ (15816) 16 Geriatrics/ (114) 17 Geriatric Nursing/ (140) 18 exp medicare/ (280) 19 (geriatr* or elder* or gerontol* or seniors or senior citizen* or older adult* or older person* or older people).ti,ab. (15287) 20 (over adj2 ("60" or "61" or "62" or "63" or "64" or "65" or "66" or "67" or "68" or "69" or "70" or "71" or "72" or "73" or "74" or "75" or "76" or "77" or "78" or "79" or "80" or "81" or "82" or "83" or "84" or "85" or "86" or "87" or "88" or "89" or "90" or "91" or "92" or "93" or "94" or "95" or "96" or "97" or "98" or "99" or "100") adj years).ti,ab. (364) 21 or/15‐20 [aged] (20814) 22 14 and 21 [day care or outpatients or rehabilitation centers and aged terms] (774) 23 limit 22 to yr="2012 ‐Current" (21) 24 remove duplicates from 23 (21)
Appendix 12. NHS EED and HTA search strategy
1996 to 2013 HTA NHSEED DA 7.10.13 Last Saved: 08/10/2013 09:07:26.578 Description: DA 11.10.12 ID Search #1 MeSH descriptor: [Day Care] this term only #2 (daycare or day care) .ti,ab. #3 (child* daycare or child* day care) .ti,ab. #4 #2 not #3 #5 (day N2 (hospital* or clinic* or unit* or service*)) tw. #6 (day healthcare or day health care) .tw. #7 #1 or #4 or #5 or #6 #8 MeSH descriptor: [Outpatient Clinics, Hospital] this term only #9 MeSH descriptor: [Outpatients] this term only #10 (outpatient* or out‐patient*) .tw. #11 MeSH descriptor: [Ambulatory Care Facilities] this term only #12 MeSH descriptor: [Ambulatory Care] this term only #13 #8 or #9 or #10 or #11 or #12 #14 MeSH descriptor: [Rehabilitation Centers] this term only #15 #13 or #14 #16 MeSH descriptor: [Aged] explode all trees #17 MeSH descriptor: [Geriatrics] this term only #18 MeSH descriptor: [Geriatric Nursing] this term only #19 MeSH descriptor: [Geriatric Assessment] this term only #20 MeSH descriptor: [Medicare] explode all trees #21 MeSH descriptor: [Health Services for the Aged] this term only #22 (geriatr* or elder* or gerontol* or seniors or senior citizen* or older adult* or older person* or older people) .ti,ab. #23 (over N2 ("60" or "61" or "62" or "63" or "64" or "65" or "66" or "67" or "68" or "69" or "70" or "71" or "72" or "73" or "74" or "75" or "76" or "77" or "78" or "79" or "80" or "81" or "82" or "83" or "84" or "85" or "86" or "87" or "88" or "89" or "90" or "91" or "92" or "93" or "94" or "95" or "96" or "97" or "98" or "99" or "100") N years) .ti,ab. #24 #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 #25 #15 and #24 from 1996 to 2013, in Technology Assessments and Economic Evaluations
Appendix 13. Web of Knowledge search strategy
ISI Web of Knowledge Search Strategy Set Results # 13 1,109 #12 AND #11 Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 12 850,044 Topic=(rct* or random*) Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 11 5,788 #10 AND #9 Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 10 217,332 Topic=(geriatr* or elder* or gerontol* or seniors or "senior citizen*" or "older adult*" or "older person*" or "older people") Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 9 86,609 #8 OR #7 OR #4 Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 8 2,361 Topic=("rehab* center*" or "rehab* centre*") Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 7 78,177 #6 OR #5 Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 6 3,768 Topic=("ambulatory care") Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 5 75,216 Topic=(outpatient* or "out patient* ") Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 4 6,970 #3 OR #2 OR #1 Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 3 48 Topic=("day healthcare" OR "day health care") Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 2 2,412 Topic=("day unit*" or "day hospital*" or "day clinic*" or "day centre*" or "day center*") Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On # 1 4,608 Topic=((daycare or "day care")) NOT Topic=(("child* daycare" or "child* day care")) Databases=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH Timespan=1996‐01‐01 ‐ 2012‐10‐11 Lemmatization=On
Appendix 14. Web of Science search strategy
Still to add
Appendix 15. Google search strategy
Not possible to search for full range of terms due to limited search capabilities of Scholar so search limited to "day hospitals" OR "day hospital") AND (geriatric* OR "older adult*" OR "older person*" OR "older people" OR elderly ) AND (random* OR rct*) 2012 to 2013 (all languages)
Appendix 16. Index to Theses search strategy
Index to Theses Day Hospital Update Oct 2012 to Aug 2012 DA Search Strategy Note: limited search to day hospital or day hospital in title as a broader search brought back irrelevant results Your query was: (ti contains day hospital) OR (ti contains day hospitals ) AND (yr contains 2012 or 2013) Search Results 0 document(s) retrieved
Appendix 17. Proquest Dissertations and Theses search strategy
Day Hospitals Update Oct 2012 to Aug 2013 DA Search Strategy Proquest Dis and Abs all((daycare OR "day care") OR (outpatient* OR out patient* OR "ambulatory care*" OR "rehab* center*" OR "rehab* centre*") AND (geriatric* OR elder* OR gerontol* OR seniors OR "senior citizen*" OR "older adult*" OR "older person*" OR "older people") AND (RCT OR Random*) NOT (child* OR young* OR boy* OR girl*)) Limited to 10th Oct 2012 to 14th Aug 2013
Appendix 18. Current Controlled trials search strategy
Searched Current Controlled Trials ISRCTN (trials registered with a unique identifier) Search 1: “Day Hospital” or “day hospitals”
Appendix 19. HSRProj search strategy
HSR Proj Day Hospital Search Strategy and results 1996 to 2012 Searched 15/10/12 Found 1 Projects with search of: ("day hospital" OR "day hospitals" or "adult day care") Advanced Search on : Project status = All : Initial Year Range =2012 ‐ 2012 : Final Year Range =2012 ‐ 2022
Appendix 20. Assessing the relative importance of outcomes and deciding which ones to include in the 'Summary of findings' table
Review: Medical day hospital care for the elderly versus alternative forms of care
Assessed by: LB, AB, TC
Date:
Rate the relative importance for each outcome on a 9 point scale ranging from 1 (not important) to 9 (critical).
1‐3: Not important and not included in the 'Summary of findings' (SoF) table
4‐6: Important but not critical for making a decision (inclusion in the SoF table may depend on how many other important outcomes there are)
7‐9: Critical for making a decision and should definitely be included in the SoF table
Include potential undesirable effects (harms) and resource use (costs), as well as desirable effects (benefits)
| Outcome | Initials of people assessing the relative importance of the outcomes | Consensus | |||
| LB | AB | TC | All (finals score) | ||
| Relative importance (1‐9) | |||||
| a) Death by the end of follow up | 9 | 7 | 7 | 7 | Include following discussion |
| b) Death or institutional care by the end of follow up | 9 | 8 | 6 | 5 | Include following discussion |
| c) Death or deterioration in activities of daily living (ADL) |
9 | 7 | 5 | 6 | Include following discussion |
| d) Death or poor outcome (institutional care, disability or deterioration) |
9 | 7 | 5 | 6 | Include following discussion |
| e) Deterioration in activities of daily living (ADL) in survivors |
9 | 8 | 4 | 8 | Include following discussion |
| f) Activities of daily living (ADL) scores |
7 | 8 | 4 | 5 | |
| g) Subjective health status | 7 | 5 | 5 | 5 | |
| h) Patient satisfaction | 5 | 4 | 4 | 4 | |
| i) Carer distress | 4 | 5 | 5 | 5 | |
| j) Requiring institutional care at the end of follow up |
7 | 7 | 5 | 5 | |
| k) Hospital bed use during follow up |
6 | 6 | 4 | 5 | |
| l) Cost‐benefit analysis (added by TC) | 9 | No available data | |||
Data and analyses
Comparison 1. Day Hospital vs Alternative Care ‐ patient outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Death by the end of follow up | 16 | 3533 | Odds Ratio (M‐H, Random, 95% CI) | 1.05 [0.85, 1.28] |
| 1.1 Day Hospital vs Comprehensive elderly care | 5 | 1287 | Odds Ratio (M‐H, Random, 95% CI) | 1.26 [0.87, 1.82] |
| 1.2 Day hospital vs Domiciliary care | 7 | 901 | Odds Ratio (M‐H, Random, 95% CI) | 0.97 [0.61, 1.55] |
| 1.3 Day hospital vs No comprehensive elderly care | 4 | 1345 | Odds Ratio (M‐H, Random, 95% CI) | 0.88 [0.63, 1.22] |
| 2 Death or institutional care by the end of follow up | 13 | 3030 | Odds Ratio (M‐H, Random, 95% CI) | 0.85 [0.63, 1.14] |
| 2.1 Day hospital vs Comprehensive elderly care | 4 | 1181 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.69, 1.44] |
| 2.2 Day hospital vs Domiciliary care | 5 | 672 | Odds Ratio (M‐H, Random, 95% CI) | 1.05 [0.57, 1.92] |
| 2.3 Day hospital vs No comprehensive elderly care | 4 | 1177 | Odds Ratio (M‐H, Random, 95% CI) | 0.63 [0.40, 1.00] |
| 3 Death or deterioration in activities of daily living (ADL) | 7 | 1268 | Odds Ratio (M‐H, Random, 95% CI) | 1.07 [0.76, 1.49] |
| 3.1 Day hospital vs Comprehensive elderly care | 1 | 174 | Odds Ratio (M‐H, Random, 95% CI) | 1.18 [0.63, 2.18] |
| 3.2 Day hospital vs Domiciliary care | 4 | 443 | Odds Ratio (M‐H, Random, 95% CI) | 1.41 [0.82, 2.42] |
| 3.3 Day hospital vs No comprehensive elderly care | 2 | 651 | Odds Ratio (M‐H, Random, 95% CI) | 0.76 [0.56, 1.05] |
| 4 Death or poor outcome (institutional care, disability or deterioration) | 13 | 2831 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.74, 1.15] |
| 4.1 Day hospital vs Comprehensive elderly care | 5 | 1268 | Odds Ratio (M‐H, Random, 95% CI) | 1.05 [0.79, 1.40] |
| 4.2 Day hospital vs Domiciliary care | 5 | 581 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.67, 1.74] |
| 4.3 Day hospital vs No comprehensive elderly care | 3 | 982 | Odds Ratio (M‐H, Random, 95% CI) | 0.72 [0.53, 0.99] |
| 5 Deterioration in activities of daily living (ADL) in survivors | 7 | 905 | Odds Ratio (M‐H, Random, 95% CI) | 1.11 [0.68, 1.80] |
| 5.1 Day hospital vs Comprehensive elderly care | 1 | 149 | Odds Ratio (M‐H, Random, 95% CI) | 1.21 [0.58, 2.52] |
| 5.2 Day hospital vs Domiciliary care | 4 | 349 | Odds Ratio (M‐H, Random, 95% CI) | 1.59 [0.87, 2.90] |
| 5.3 Day hospital vs No comprehensive elderly care | 2 | 407 | Odds Ratio (M‐H, Random, 95% CI) | 0.61 [0.38, 0.97] |
| 6 Activities of daily living (ADL) scores | Other data | No numeric data | ||
| 6.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 6.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 6.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||
| 7 Subjective health status | Other data | No numeric data | ||
| 7.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 7.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 7.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||
| 8 Patient satisfaction | Other data | No numeric data | ||
| 8.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 8.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 8.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||
| 9 Carer Distress | Other data | No numeric data | ||
| 9.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 9.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 9.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data |
Comparison 2. Day Hospital vs Alternative Care ‐ resource outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Requiring institutional care at the end of follow up | 13 | 3003 | Odds Ratio (M‐H, Random, 95% CI) | 0.84 [0.58, 1.21] |
| 1.1 Day hospital vs Comprehensive elderly care | 4 | 1181 | Odds Ratio (M‐H, Random, 95% CI) | 0.91 [0.70, 1.19] |
| 1.2 Day hospital vs Domiciliary care | 5 | 672 | Odds Ratio (M‐H, Random, 95% CI) | 1.49 [0.53, 4.25] |
| 1.3 Day hospital vs No comprehensive elderly care | 4 | 1150 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.28, 1.20] |
| 2 Hospital bed use during follow up | Other data | No numeric data | ||
| 2.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 2.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 2.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||
| 3 Resource use | Other data | No numeric data | ||
| 3.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 3.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 3.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Burch 1999.
| Methods | Randomised controlled trial Method of randomisation: computer generated Concealment of allocation: sealed envelopes Outcome assessor blinding: blinded research sociologist |
|
| Participants | Country: UK Patients referred to day hospital Exclusion criteria: dysphasic, required nursing or occupational therapy > twice per week 163 patients eligible (28 needed day hospital treatment, 21 refused consent, 9 operational problems at day centre) Participants randomised = 105 Baseline function: Median (IQR) Barthel Index 15 (12‐17) and 15 (11‐17) Male: 36% Age: mean (SD) 80.4 (7.6) years |
|
| Interventions | Day hospital: care by multidisciplinary rehabilitation team, principally nursing assessment, occupational therapy and physiotherapy. Median number of treatments (interquartile range) 11.5 (5–20.5). Day centre: rehabilitation provided by a physiotherapist and two support workers. Median number of treatments (interquartile range) 10 (5–14). |
|
| Outcomes | 12 month follow up Death Institutional care Barthel Index Caregiver Strain Index Philadelphia Geriatric Morale scale Costs | |
| Notes | Total of 105 patients of whom 23 had a stroke diagnosis, 14 osteoarthritis, 13 fracture, 9 Parkinsonism Of the 55 patients randomised to day centre attendance, 10 transferred to day hospital | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Low risk | Quote: "Immediately after consent, subjects were randomly allocated to day hospital or day centre by a sequence of labelled tickets in sealed, opaque envelopes securely kept and opened by a senior ward clerk unattached to the trial team....computer generated blocks of 20." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Reported as single blind which appears to have been the assessor, not participants or personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessments were undertaken by a blinded research sociologist Quote: "The interviewer correctly identified 38/55 as day hospital and 20/38 as day centre, yielding kappa = 0.22 indicating poor agreement/successful blinding." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar losses per group (˜30%), moderately high but similar reasons reported for both groups |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | High risk | 18% of participants randomised to day centre attendance transferred to the day hospital leading to possibility of contamination (the experiment and control groups becoming mixed) |
Crotty 2008.
| Methods | Randomised controlled trial Method of randomisation: computer generated Concealment of allocation: sealed envelopes Outcome assessor blinding: blinded research occupational therapist |
|
| Participants | Country: Australia Hospitalised patients referred for ambulatory rehabilitation Inclusion criteria; medically stable; ready for hospital discharge; rehabilitation which required at least 12 therapy sessions Exclusion criteria: lived out of the health region; if referring clinician felt they were unsuitable to receive one of the programmes 301 patients assessed for study inclusion (34 patients did not meet the eligibility criteria, 38 patients declined to participate or were not approached on the request of the physician) Participants randomised = 229 Modified Bartel Index mean (SD): 92.4 (6.5) Mini‐Mental State Examination mean (SD): 26.9 (3.1) Male: 48% Age: mean (SD) 71.7 (14.1) years |
|
| Interventions | Day hospital: Interdisciplinary programme providing 4–6 weeks of high intensity rehabilitation in either individual or group sessions with the option of extending the programme. Each visit lasted 3 hours. Participants had access to physiotherapy, occupational therapy, social work, psychology, dietetics and nursing and rehabilitation medicine. Home based rehabilitation: One to one rehabilitation programme delivered by an interdisciplinary team to participants in their homes. This included physiotherapy, occupational therapy, speech therapy, social work, dietetics, nursing and rehabilitation medicine. Three to five session per week usually delivered for between 4 and 6 weeks. |
|
| Outcomes | Primary outcome: Assessment of Motor and Process Skills, bioelectrical impedance Secondary outcomes: depression, Mini Nutritional Assessment, Assessment of Appetite, Mini Mental State Exam, Timed Up and Go, and Short Form 36 (patient and carer), patient satisfaction and carer/family satisfaction, Carer Strain Index, mortality and place of residence, cost and readmissions. Outcomes assessed at baseline, discharge, three and six months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Low risk | Quote: "statistician external to the study generated the randomisation sequence using the random number generator in Microsoft Excel and created sequentially numbered, opaque, sealed envelopes containing group allocation for participants" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The same doctor provided medical services to both groups. Furthermore, participants could not have been blinded to the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assesments were undertaken by a research occupational therapist blinded to the group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced across groups and with similar reasons reported |
| Selective reporting (reporting bias) | High risk | Some outcome measures reported in study protocol (Australian New Zealand Clinical Trials Registry) not reported in current publications |
| Other bias | Low risk | No other obvious sources of bias |
Cummings 1985.
| Methods | Randomised controlled trial Method of randomisation: not reported Concealment of allocation: not reported Outcome assessor blinding: unclear for some outcomes |
|
| Participants | Country: USA Patients referred for inpatient rehabilitation Inclusion criteria: age over 15 years, disabled (not spinal injuries or head injuries), living with someone, fit to travel, 24 hour telephone contact, suitable residence, medicare eligible 556 patients screened (8 patient/carers refused consent, 452 rejected from study sample) Participants randomised = 96 Baseline function: Kenny ADL index 21.8 and 22.1 Male: 54% Age: not reported |
|
| Interventions | Day hospital attendance 5 days a week with emphasis on rehabilitation with greater patient and carer involvement. Complete range of medical and therapeutic services available. Rehabilitation as an inpatient. | |
| Outcomes | 3 month follow up Death Institutional care ADL: i) modified Kenny, ii) subjective rating Instrumental ADL Checklists to measure indoor and outdoor leisure activity Medical status Mental state Psychological well‐being (Kahn Mental Status Questionnaire) Patient satisfaction Family impact questionnaire Costs | |
| Notes | 96 patients were recruited, of whom 55 had a stroke diagnosis and 26 were amputees Day hospital tested as an alternative to inpatient care | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information reported |
| Allocation concealment (selection bias) | Unclear risk | No information reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No information reported but would have been obvious to participants |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was reported that medical status was assessed by a physician who did not know the patient. However, it was unclear if this was the case for other outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not all outcomes were reported in the publication (Cummings 1985). However, some additional information was provided by the authors on request |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Unclear risk | This was an ‘artificial' day hospital designed specifically for the purpose of the study and may have been affected by some environmental factors and under‐utilisation of the hospital |
Eagle 1991.
| Methods | Randomised controlled trial, stratified by conventional service Method of randomisation: not reported Concealment of allocation: not reported Outcome assessor blinding: not undertaken |
|
| Participants | Country: Canada Patients referred from the community to 2 geriatricians or about to be discharged from hospital Inclusion criteria: age over 65 years, reduced function with rehabilitation potential 128 patients asked to participate (15 refused) Participants randomised = 113 Baseline function: Geriatric Quality of Life Questionnaire (ADL) 4.49 and 4.46 Male: 40% Age: mean (SD) 78.9 (7.2) years |
|
| Interventions | Day hospital: Attendance 2 days a week. Treatment included multidisciplinary team assessment, programme of rehabilitation provided by physiotherapists and occupational therapists. Usual care: Management in inpatient geriatric assessment unit for comprehensive assessment and treatment, management in the outpatient geriatric clinic, with limited diagnostic and rehabilitative opportunities, or early discharge from a medical‐surgical inpatient unit and appropriate community follow‐up services. The same professionals provided treatment to both groups |
|
| Outcomes | 12 month follow up Death Institutional care Mental status Geriatric Quality of Life Questionnaire Barthel Index Rand questionnaire Global Health Question (GHQ) Family rating of Barthel Index, GHQ, Rand Questionnaire Patient rating of Barthel Index Resource use | |
| Notes | 113 patients were recruited, of whom 26 had a stroke diagnosis, 32 a diagnosis of depression and 19 a diagnosis of degenerative joint disease Patients were stratified according to the type of conventional care specified by the participating geriatrician prior to randomisation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information reported |
| Allocation concealment (selection bias) | Unclear risk | No information reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: “We were unable to blind the patients, caregivers and study personnel administering the questionnaires and instruments for measuring functional status to the study groups” |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: “We were unable to blind the patients, caregivers and study personnel administering the questionnaires and instruments for measuring functional status to the study groups” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data fairly balanced in numbers across groups |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Low risk | No other obvious sources of bias |
Gladman 1993.
| Methods | Randomised controlled trial Method of randomisation: random number table Concealment of allocation: sealed envelopes Outcome assessor blinding: blinded assessment at 6 months and 1 year |
|
| Participants | Country: UK Patients discharged home from hospital after acute stroke Exclusion criteria: discharged to residential or nursing homes, requiring respite or terminal care, receiving outpatient rehabilitation prior to the stroke, no significant disability, in hospital < 7 days Patients discharged from older care, general medical wards and stroke unit were randomised separately Participants = 155 Baseline function: Median Barthel Index (IQR) 17 (14‐17) and 16 (13‐17) Male: 48% Age: mean 70 years |
|
| Interventions | Domiciliary rehabilitation intervention: 2 half time physiotherapists, 1 occupational therapist and treatment for up to 6 months (75% received treatment). Day hospital intervention: multidisciplinary rehabilitation provided (54% received treatment). |
|
| Outcomes | 12 month follow up Death Institutional care Extended ADL score Barthel Index Nottingham Health Profile Brief Assessment of Social Engagement Life Satisfaction Index (Nottingham version) Costs | |
| Notes | All stroke patients (155) Previous stroke in day hospital group 42 (27%), domiciliary group 19 (31%) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "consecutive sealed envelopes which contained cards marked either “DRS” or “HRS" which had been prepared before the start of the study by reference to a table of random numbers." |
| Allocation concealment (selection bias) | Low risk | Quote: "consecutive sealed envelopes which contained cards marked either “DRS” or “HRS which had been prepared before the start of the study by reference to a table of random numbers." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No information reported. However, participants would have been aware of allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded assessment at 6 months and 1 year, however unclear if baseline data were collected by a blinded assessor |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Some imbalance in missing outcome data but losses relatively low in both groups |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Low risk | No other obvious sources of bias |
Hedrick 1993.
| Methods | Randomised controlled trial Method of randomisation: computerised random Concealment of allocation: assignment from central site Outcome assessor blinding: not reported |
|
| Participants | Country: USA To be eligible, Veterans Aaffairs service patients had one of the following: at risk of nursing home placement, 'Service connected disability', hospital inpatient, in home care programme, in a Veterans Affaris domiciliary service Inclusion criteria (one of the following): living in a nursing home, need help for ADL activities, bowel incontinence, significant cognitive impairment, acceptable to day care staff 1236 patients screened (252 not eligible, 158 refused consent) Patients randomised = 826 Baseline status: Sickness Impact Profile (Physical) Mean (SD) 31.7 (18.8) and 33.8 (18.4) Male: 96% Age: mean 71.1 years |
|
| Interventions | Medical Day Hospital: therapeutically orientated programme providing health maintenance and rehabilitation services. Staff included nurses, rehabilitation therapists, recreation therapists and social worker. Mean attendance over 6 months: 28 days. Usual care: Nursing home, inpatient care, clinic visits, home care etc. | |
| Outcomes | 12 month follow up Death Institutional care Mini Mental state Sickness Impact Profile Survival Satisfaction Questionnaire Self‐rated health Social support scale Katz Instrumental ADL Psychological Distress Scale Caregiver Burden Scale Satisfaction Questionnaire Service use and costs | |
| Notes | No accurate information on patient diagnosis given Evaluation of adult day health care | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator |
| Allocation concealment (selection bias) | Low risk | Assignment from central site |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No reported blinding of participants or personnel. However, it would have been obvious to participants |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No reported blinded outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Low risk | No other obvious sources of bias |
Hui 1995.
| Methods | Randomised controlled trial
Stratified by disability Method of randomisation: random number table Concealment of allocation: sealed envelopes Outcome assessor blinding: unclear |
|
| Participants | Country: Hong Kong Patients admitted to a rehabilitation ward one week after acute stroke Exclusion criteria: age < 65 yrs, previous stroke, dementia, live outside catchment area, Barthel index of 20 Participants randomized = 120 Baseline function: mean (SD) Barthel index 9.9 (4.9) and 10.4 (5.3) Male: 44% Age: mean (SD) 73.6 (5.7) years |
|
| Interventions | Medical day hospital: care under the geriatrician with early discharge, as able, with continued care in the day hospital. Duration of intervention not reported for day hospital or inpatient rehabilitation. Conventional inpatient rehabilitation: delivered by a neurology team with medical clinic follow up. |
|
| Outcomes | 6 month follow up Death Institutional care Abbreviated mental test score Barthel index Self‐rated health scale score Geriatric Depression Scale Subjective satisfaction with services Use of hospital and community services Costs | |
| Notes | Stroke patients only All patients initially treated on same rehabilitation ward | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table (information obtained from follow up correspondence) |
| Allocation concealment (selection bias) | Low risk | Quote (from letter): "The codes were sealed in envelopes and placed at an office in Shatin Hospital. When the patient is deemed suitable to be discharged, an envelope would be withdrawn and patient assigned into the specific group (Day Hospital or Conventional Management)." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No report of blinding but would have been obvious to participants |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Follow up assessment was carried out by a research nurse. However, not reported if assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Losses relatively similar across the groups. However, reasons for participants defaulting not reported |
| Selective reporting (reporting bias) | Unclear risk | Reported that "patient well‐being...use of community services and financial support were all comparable between the two treatment groups at each follow‐up (data not shown)." No numerical data reported |
| Other bias | Low risk | No other obvious sources of bias |
Masud 2006.
| Methods | Randomised controlled trial Method of randomisation: Internet based randomisation service Concealment of allocation: Internet based randomisation service Outcome assessor blinding: not undertaken |
|
| Participants | Country: UK Inclusion criteria: the study population was comprised of men and women aged 70 and over identified as being at high risk of falling by a postal screening questionnaire, registered with the participating general practices in Nottinghamshire and Derbyshire. Exclusion criteria: patients already attending one of the day hospitals; under follow‐up with an existing primary care based falls prevention scheme; in nursing or residential homes; patients with terminal illnesses; unwilling or unable to travel to the day hospital (using transport as provided); unable to provide informed consent or assent. 6113 assessed for study inclusion (844 potential participants did not meet the eligibility criteria, 4925 declined to participate) Participants randomised = 364 Male: 40% Age: mean (SD) 78.8 (5.7) years |
|
| Interventions | Medical day hospital: screening questionnaire, information leaflet, leaflet on falls prevention and invitation to attend the day hospital for assessment and any subsequent intervention. Control intervention: screening questionnaire, information leaflet, leaflet on falls prevention and usual care from primary care service until outcome data collected, then offer of day hospital intervention. Duration of intervention not reported for day hospital or control intervention |
|
| Outcomes | Primary outcome: Rate of falls over the 12 month follow‐up period Secondary Outcomes Proportion of people with single or recurrent falls and fall‐related injuries: fracture, serious sprain requiring immobilisation in plaster, joint dislocations, head injury requiring hospitalisation, and lacerations requiring suturing Disability: Nottingham Extended Activities of Daily Living Scale; Barthel index of daily living; Quality of life: Falls Efficacy Scale and EuroQoL‐5 Institutionalisation and use of health services: residency and diary information Cost analysis Deaths checked from PCT records and measured as proportions |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An Internet based randomisation service provided by the hosts institution's clinical trials unit |
| Allocation concealment (selection bias) | Low risk | An Internet based randomisation service provided by the hosts institution's clinical trials unit |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to the nature of the intervention It would not be possible to blind participants |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "it was not possible to blind participants or researchers to allocation." However, the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding. GP recording of death or institutionalisation are unlikely to be biased by the participation in either arm of the study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Misisng data balanced across groups with similar reasons |
| Selective reporting (reporting bias) | Low risk | Study protocol available and additional information provided on request |
| Other bias | Low risk | No other obvious sources of bias |
Parker 2009.
| Methods | Randomised controlled trial Method of randomisation: external web based randomisation service Concealment of allocation: external web based randomisation service Outcome assessor blinding: unclear |
|
| Participants | Country: UK Participants were older people referred for rehabilitation for various conditions including stroke, orthopaedic rehabilitation, movement disorder, mobility assessment and falls assessment. Inclusion criteria: referred for multidisciplinary rehabilitation, a permanent address in the catchment area, able to give informed consent (with the help of a career or advocate if necessary). Exclusion criteria: local exclusion criteria meant that patients were excluded from randomisation if they had a specific clinical need that could only be addressed at one centre (sites provided specific services). Participants randomised = 89 Baseline function: mean (SD) Nottingham Extended Activities of Daily Living 29.9 (15.2) Males: 55% Age: mean (SD) 75 (11) years |
|
| Interventions | Medical day hospital (4 sites): Some variation in the services provided between the four day hospitals. However, all sites were multidisciplinary and patients could access a hospital doctor, nursing care, physiotherapy and occupation therapy services. Some sites provided access to a social worker. Number of rehabilitation episodes: mean 17.7, median 18. Rehabilitation at home: Some variation in the services offered by the 4 participating home rehabilitations teams. However, all provided physiotherapy services and the majority provided occupational therapy. Some services provided access to a doctor and a social worker. Number of rehabilitation episodes: mean 9.4; median 8.5. Reported in the study protocol that the length of the interventions would be determined by the local clinical team with the expectation that 95% of participants would be discharged within 16 weeks. |
|
| Outcomes | 12 month follow up Patient outcomes: Hospital anxiety and depression scale Euro‐qol 5D Nottingham Extended Activities of Daily Living Socio‐economic data, survival Therapy outcome measures Views of treatment by qualitative interview Carer outcomes: General health questionnaire Socio‐economic data Views of treatment |
|
| Notes | http://www.controlled‐trials.com/ISRCTN71801032 https://portal.nihr.ac.uk/Profiles/NRR.aspx?Publication_ID=N0071140216 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | External web based randomisation service |
| Allocation concealment (selection bias) | Low risk | External web based randomisation service and investigators were not involved in the allocation to groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "the nature of the treatments was such that it was not possible for the patients or their health‐care professionals to be blinded to the treatment allocation, or to guarantee that the local researchers remained unaware of allocation for the duration of follow‐up" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "the nature of the treatments was such that it was not possible for the patients or their health‐care professionals to be blinded to the treatment allocation, or to guarantee that the local researchers remained unaware of allocation for the duration of follow‐up" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Whilst the reasons for losses were relatively similar across both groups, losses were > 35% by final follow up |
| Selective reporting (reporting bias) | Low risk | Protocol available (Current Controlled Trials ISRCTN71801032) |
| Other bias | Low risk | No other obvious sources of bias |
Pitkala 1991.
| Methods | Randomised controlled trial Method of randomisation: randomised according to date of birth Concealment of allocation: date of birth, therefore could have been foreseen Outcome assessor blinding: not reported |
|
| Participants | Country: Finland Patients receiving home care in a rural community in Finland All 177 chronically ill patients receiving home care screened (3 refused consent) Participants randomised = 174 Male: 34% Age: mean (range) 77 (43‐91) years |
|
| Interventions | Day hospital: new 10‐place day hospital provided medical and nursing assessment and care. Intensive physiotherapy and occupational therapy provided according to individual need. Patients attended 2‐3 days a week from 8.30am‐ 4.30pm. On average 20 days treatment over 2 months. Usual care: included mixture of home health care and referral to a hospital or outpatient care. |
|
| Outcomes | 12 month follow up Death Institutional care Katz ADL Subjective health assessment Mood Resource use, hospital admissions, outpatients visits, GP visits Number of symptoms Number of medications | |
| Notes | Total of 174 patients of whom 40 had a stroke diagnosis, 54 a diagnosis of coronary heart disease, 53 arthrosis, 33 'moderate' or 'severe' dementia | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "were randomised into two groups according to their date of birth." |
| Allocation concealment (selection bias) | High risk | Allocation based on date of birth, therefore could have been foreseen |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No report of blinding and would have been obvious to participants which group they were in |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No reported blinded outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Similar numbers of losses but reasons for losses not reported so cannot determine risk |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Unclear risk | Nearly one quarter of the day hospital group refused the care |
Roderick 2001.
| Methods | Randomised controlled trial
Stratified by sex, age and disability (Barthel index <10; 10‐14; >15) and catchment areas of day hospitals. Method of randomisation: computer generated Concealment of allocation: unclear Outcome assessor blinding: blinded research nurse |
|
| Participants | Country: UK Inclusion criteria: patients with newly diagnosed stroke admitted to a Poole Hospital NHS Trust hospital, or community referrals. Confirmed diagnosis of stroke Aged over 55 years Residents of East Dorset Needed rehabilitation for stroke related disability Were able to attend day hospital No previous disability which would prevent rehabilitation No signs of advanced dementia Exclusion criteria: terminal illness, needing day hospital care for social or medical reasons. 180 eligible Patients randomised = 140 Baseline function: Median (IQR) Barthel Index: Day Hospital 14 (9‐17), Control 14 (9‐16). Male: 46% Age: mean (range) 78.95 (60‐95) years |
|
| Interventions | Day hospital: 5 day hospitals with coordinated care from multidisciplinary teams, both individual and group therapies. Median number of visits to the day hospital 17. Domiciliary care: domiciliary stroke team comprising 1 full time physiotherapist and a half time physiotherapist and consultant geriatrician, who met with each other fortnightly to review patients. Out patient speech and language therapy provided. Median number of domicilliary visits 17. In both interventions, therapy was provided until maximum potential for recovery was reached. Patients were then placed on review, and if no further therapy required, discharged. |
|
| Outcomes | 6 month follow‐up
Primary outcome: Barthel index Secondary outcomes: Rivermead Mobility Index Philadelphia Geriatric Center Morale Scale Frenchay Activities Index Perceived Quality of Life (SF‐36) Health and local authority social service costs |
|
| Notes | All stroke patients, previous stroke in the day hospital group 23 (32%) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was attempted. Quote: "...by calling a centralised office where closed lists ... were kept" , the sample was stratified by sex (2 groups), disability (3 groups), age and day hospital catchment area. Minimum 2x3x2x5 = 60 groups. There were 5 day hospitals so potentially 60 groups. The approach to stratification is not described but is likely to be a permuted‐block design, with small block size and therefore allocation could have been predicted for some of the patients |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not reported but would have been obvious to participants |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assesments were carried out by a research nurse blind to allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar losses in each group with similar reasons |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Low risk | There was contamination: 5 switched from domiciliary to day hospital and two the other way. One other ‘incorrect placement’ (unexplained). Appears these were analysed in original groups (correctly (ITT) but therefore contaminating the result). However, because the contamination involved so few participants we judged it unlikely to have significantly altered the estimate of effect. |
Tucker 1984.
| Methods | Randomised controlled trial
Stratified by stroke or non‐stroke diagnosis Method of randomisation: random number table Concealment of allocation: unclear Outcome assessor blinding: research occupational therapist |
|
| Participants | Country: New Zealand Patients over 55 years Patients needing assessment and rehabilitation but not 24 hour institutional care Referrals from hospital and GPs Excluded: dementia, patients needing social care Baseline function: 17.6 (12‐31) and 16.3 (12‐25) on Northwick Park ADL score Male: 43% Age: mean (range) 72 (55‐92) years |
|
| Interventions | Day hospital: intensive physiotherapy, occupational therapy, speech therapy and medical and nursing assessment and supervision. Patients attended 2‐3 days per week, Monday to Friday from 8.30 a.m. ‐ 2.00 p.m. for 6 ‐ 8 weeks. Usual care: inpatient, outpatient follow‐up with or without outpatient physiotherapy, by referral for domiciliary services, by referral to the sole care of their GP, or by referral to a day centre as decided before randomisation |
|
| Outcomes | 5 months follow up Death Institutional care Northwick Park ADL Zung Depression Index Service use Costs | |
| Notes | No information on number of patients screened for inclusion Stroke patients randomised separately from other diagnoses (65 of 120) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients with and without strokes were randomised separately into day hospital and control groups with standard tables of random numbers." |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported. Therefore, insufficient information to determine risk |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No report of blinding. However, it would have been obvious to participants which group they were in |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "In an attempt to preserve blindness of assessment she [research occupational therapist] was not concerned in the rehabilitation of these patients and worked in another occupational therapy department." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Some lost to follow up (5% from experimental group, 14% from control). Some differences in reasons for losses |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Low risk | No other obvious sources of bias |
Vetter 1989.
| Methods | Randomised controlled trial (pilot study) Method of randomisation: not reported Concealment of allocation: sealed envelopes Outcome assessor blinding: not reported |
|
| Participants | Country: UK Consecutive patients attending 2 day hospitals were eligible for trial if: Required rehabilitation Had not attended day hospital in previous year Did not require medical investigations only provided in day hospital Not confused 270 patients screened (83 needing maintenance ‐ had attended the day hospital in the previous year, 41 needed medical investigation, 28 confused, 10 required respite, 5 attended only once, 4 refused and 40 not recruited due to administrative problems) Participants randomised = 59 Baseline function: Barthel index of approximately 13 Male: 32% Age: 98% over 65 years |
|
| Interventions | Day hospitals (2 sites): medical and nursing support and physiotherapy, occupational therapy, speech therapy, chiropody, dietary, pharmaceutical and opthalmic services.
Home rehabilitation: a newly established service, comprising two part‐time physiotherapists, three part‐time occupational therapists, speech therapist, dietician, clinical psychologist available for referrals as appropriate. Regular team meetings, attempt to equalise amount of therapy given to both groups, the duration of the interventions were not reported. |
|
| Outcomes | 2 month follow up Death Institutional care Barthel index Sickness Impact Profile | |
| Notes | Total of 59 patients of whom 16 had a stroke diagnosis, 12 fractured neck or femur, 5 osteo‐arthritis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation not reported |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes opened after participants had been included |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No report of blinded outcome assessment. However, it would have been obvious to participants |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No report of blinded outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The outcomes were not reported in the original report (Vetter 1989), although some additional information was provided on request |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Low risk | No other obvious sources of bias |
Weissert 1980.
| Methods | Randomised controlled trial Method of randomisation: no information reported Concealment of allocation: no information reported Outcome assessor blinding: no information reported |
|
| Participants | Country: UK New service established and advertised Referral from a number of sources (hospital, community, etc) Patients screened for eligibility for day care service 63% of eligible referred patients agreed to participate Participants randomised = 644 Male: 39% Age: 50% ≥ 75 years |
|
| Interventions | Day hospital: a programme of services including nursing, physiotherapy, patient activities provided under health leadership with physical rehabilitation as the treatment goal. Four different sites available. Patients attended for an average of 51 days per year. Control group: all patients continued to be eligible for existing services, which included hospital and skilled nursing inpatient and outpatient care, home health visits. | |
| Outcomes | 12 month follow up Death Institutional care Katz ADL index Kahn Mental Status Questionniare Contentment scale Social activity Resource use Costs | |
| Notes | Little information on patient diagnosis (only circulatory disorders (225, 41%) and injuries (55, 10%)) Alternative to institutional care | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information reported |
| Allocation concealment (selection bias) | Unclear risk | No information reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No information reported. However, it would have been obvious to participants |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing data and numbers/reasons for drop outs per group not reported |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Low risk | No other obvious sources of bias |
Woodford 1962.
| Methods | Randomised controlled trial
Stratified by age and sex Method of randomisation: random number table Concealment of allocation: not reported Outcome assessor blinding: not reported |
|
| Participants | Country: UK Patients (N = 331) from a consecutive series of 500 former geriatric unit inpatients (169 had died, left area, or were not traced) Inclusion criteria: patients over 60 years without psychiatric disorders |
|
| Interventions | Day hospital: patients received a medical assessment, occupational therapy and group exercises
Individual physiotherapy provided as required. Chiropody, bathing and hair washing also available. Attended 1 day a week 9am ‐ 5pm. Control: usual care with limited resources available. |
|
| Outcomes | 12 month follow up Death Institutional care Hospital readmission Subjective health assessment by doctor and patient | |
| Notes | No information on patient diagnosis Aimed to reduce demand for hospital admission | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No report of blinding and the nature of the intervention would make it unlikely that blinding had been undertaken |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No report of blinded assessment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 26% of the original 500 participants lost at the outset, numbers relatively balanced across groups but reasons not reported. Some exclusions due to contamination of controls |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | High risk | No other obvious sources of bias |
Young 1992.
| Methods | Randomised controlled trial
Stratified by disability and time since stroke Method of randomisation: unclear Concealment of allocation: unclear Outcome assessor blinding: researcher |
|
| Participants | Country: UK Inclusion criteria: Patients discharged home from hospital after new stroke event Fit to travel Age > 60 yrs Barthel index < 20 Exclusion criteria: patients who had to attend day hospital for respite care (n = 9) 516 screened for inclusion (143 patients discharged to residential care, 160 patients Barthel score of 20, 40 patients no change in Barthel index score, 25 lived out of area, 9 needed respite care, non‐consent 15) Participants radomised = 124 Baseline function: Median (IQR) Barthel index 15 (range 4‐19) and 16 (1‐19) Male: 56% Age: Median (range) day hospital 72 years (60‐88), domiciliary group 70 years (60‐89) |
|
| Interventions | Day hospital attendance: focus on physical rehabilitation, staffed by a multidisciplinary team of nurses, physiotherapists and occupational therapists. 2 days a week for 8 weeks 9.30am ‐ 3.45pm. Home physiotherapy: to a maximum of 20 hours in 8 weeks. | |
| Outcomes | 6 months follow up Death Institutional care Barthel index Functional Ambulatory Catagories Motor Club Assessment Frenchay Activities Index Nottingham Health Profile Carers GHQ‐28 Service use Costs (first eight weeks only) | |
| Notes | Stroke patients only (124) Previous stroke 36 29% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomisation to one of the two treatment groups was by an independent worker." However, the specific method of randomisation was not reported |
| Allocation concealment (selection bias) | Low risk | Quote: that "randomisation to one of the two treatment groups was by an independent worker" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No report of blinding of participants or personnel. However, it would have been obvious to participants which group they were in. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "by a research worker who was not involved with the randomisation or with the patient’s treatment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar numbers lost from each group for similar reasons ˜20% |
| Selective reporting (reporting bias) | Unclear risk | We were unable to obtain the pre‐study protocol so cannot determine risk of reporting bias |
| Other bias | Low risk | Some contamination from participants changing intervention group. However, this was only 4% |
ADL: activities of daily living GP: general practitioner
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adamowski 2009 | Psychiatric patients. |
| Aimonino Ricauda 2008 | General medical ward versus care at home. |
| Bartak 2011 | Psychiatric patients. |
| Baskett 1999 | Patients were randomised to treatment at home or to outpatient/day hospital attendance, patients attending day hospital not reported separately. |
| Baumgarten 2002 | Evaluation of adult day care rather than day hospital. |
| Bjokdahl 2006 | Median age of patients was 53 years. |
| Bussche 2010 | Not a randomised controlled trial. This is a qualitative study. |
| Canuto 2008 | Not a randomised controlled trial. This is a longitudinal study. |
| Capomolla 2002 | Patients with heart failure, mean age 56 years. |
| Chau 2013 | Not a randomised controlled trial. Patients were free to choose which service they attended. |
| Chiu 2009 | Psychiatric patients. |
| Close 1999 | The day hospital was part of a more complex intervention. |
| Coleman 1999 | Not an evaluation of a medical day hospital; patients attended a chronic care clinic for half‐day visits every 3‐4 months. |
| Comans 2010 | The intervention took place in a hospital gym and did not meet the criteria for a medical day hospital. |
| Crilly 2005 | Not a randomised controlled trial. |
| Dasgupta 2005 | Retrospective review of patients; not a randomised controlled trial. |
| de Oliveira 2010 | The intervention was specific to patients with Chronic Obstructive Pulmonary Disease (COPD). Studies of single, specific conditions were excluded (see methods‐types of interventions). Appears to be an out‐patient intervention rather than day hospital. |
| Del Giudice 2009 | Not a randomised controlled trial. |
| Desrosiers 2004 | Not a randomised controlled trial. |
| Edelman 2010 | The intervention facility was a clinic specific to treating patients with both diabetes and hypertension, with a specific tailored intervention. Studies of single, specific conditions were excluded (see methods‐types of interventions). |
| Evans 1998 | Hospital‐based rehabilitative care versus outpatient services. |
| Famadas 2008 | Not a randomised controlled trial. |
| Foley 2009 | Not a randomised controlled trial. |
| Gitlin 2006 | Not a randomised controlled trial. |
| Glaesmer 2003 | Not a randomised controlled trial. |
| Hershkovitz 2003 | Observational study. |
| Hershkovitz 2007 | Not a randomised controlled trial. |
| Horgan 2009 | The study took part in a day hospital but this was not the intervention. |
| Jacob 2007 | Not a randomised controlled trial. |
| Juhani 2011 | The outpatient programme was specific to patients with coronary heart disease. |
| Kallert 2007 | Psychiatric patients. |
| Kneebone 2010 | Not a randomised controlled trial. |
| Lariviere 2010 | Psychiatric patients. |
| Lariviere 2011 | Psychiatric patients. |
| Leveille 1998 | Evaluated the effect of a chronic illness self‐managment programme delivered in a senior centre. All participants attended the senior centre. |
| Luk 2011 | Not a randomised controlled trial. |
| Luk 2011a | Not a randomised controlled trial. |
| Malone 2002 | Prospective study; not a randomised controlled trial. |
| Manckoundia 2007 | Not a randomised controlled trial. |
| Marsden 2010 | The intervention was only for 2.5 hours a week, therefore it does not meet our criteria for a near full day, or full day. The intervention appeared to be more social care rather than rehabilitation (group sessions rather than individualised). |
| Masuda 2006 | Not a randomised controlled trial. |
| Meinck 2002 | Not a randomised controlled trial. |
| Olsson 2007 | Not a randomised controlled trial. |
| Pereira 2010 | Not a randomised controlled trial. |
| Priebe 2011 | Psychiatric patients aged 18‐65. |
| Richardson 2000 | Evaluation of different treatment approaches; all patient attended the day hospital. |
| Sato 2007 | Patients were in receipt of day services and were randomised to attend a water exercise program once or twice a week or to a social activity control group. The intervention was a swimming intervention, as part of a day service, and not a day hospital. |
| Schweikert 2009 | Quote: "As randomization was chosen by only 2.5% of participants, the study had to be analyzed as an observational study." |
| Scott 2004 | Not day hospital intervention, group meeting for 90 minutes once a month. |
| Sherwood 1986 | Not a randomised controlled trial. |
| Skellie 1982 | The day hospital arm of the study included data from two other interventions, including home services, and it was not possible to extract the data specific to the day hospital. |
| Spice 2009 | Participants only attended day hospital for up to two hours a day. |
| Velghe 2011 | Not a randomised controlled trial. |
| Wade 2003 | Evaluation of treatment for patients with Parkinsons disease. Intervention provided by a specialist multidisciplinary team to patients with Parkinson's disease in a day hospital setting. Studies of single, specific conditions were excluded (see methods‐types of interventions). |
| Weiler 1976 | Not a randomised or quasi‐randomised study. |
| Wong 1998 | Not a randomised controlled trial. |
| Zank 2002 | Not a randomised controlled trial. |
Characteristics of studies awaiting assessment [ordered by study ID]
ISRCTN53696600.
| Methods | |
| Participants | Stroke patients |
| Interventions | Physiotherapy versus standard care |
| Outcomes | Timed 10 metre walk, questionnaire to establish if there is an improvement in function |
| Notes | http://www.controlled‐trials.com/ISRCTN53696600/53696600 |
Matzen 2007.
| Methods | Randomised controlled trial |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes |
Moe 2010.
| Methods | |
| Participants | |
| Interventions | Multidisciplinary and multifaceted outpatient management of patients with osteoarthritis |
| Outcomes | |
| Notes | Protocol for a randomised controlled trial |
NCT00785746.
| Methods | Randomised controlled trial |
| Participants | Older people attending the geriatric day hospital |
| Interventions | Core‐Strength training program in comparison to a Stretch & Strength program. |
| Outcomes | Berg balance scale, Functional walking capacity 6 minute walk test, Gait speed, Bridge Test, Activities‐Specific Balance Confidence Scale, International Consultation on Urinary Incontinence Questionnaire |
| Notes | ClinicalTrials.gov identifier: NCT00785746 |
Yamada 2005.
| Methods | |
| Participants | Older patients with dementia |
| Interventions | |
| Outcomes | |
| Notes |
Differences between protocol and review
Methods to account for unit of analysis issues were added in the methods section.
Contributions of authors
AF, JY and PL planned and initiated the original review, assessed trials, drafted the final report and were guarantors of the initial review. AF oversaw literature searching and PL provided methodological support.
For this edition, LB, AF, TC and AB screened titles and abstracts for study inclusion. LB and AB extracted data and LB drafted the final report.
Sources of support
Internal sources
Bradford Teaching Hospitals NHS Foundation Trust, UK.
University of Glasgow, UK.
-
Raithby Bequest, UK.
University of Leeds, School of Medicine
External sources
Northern and Yorkshire Region NHS Executive, UK.
Department of Health Cochrane Review Incentive Scheme 2007, UK.
Declarations of interest
Two of the authors of this review, JY and AF, were involved in one of the included studies (Young 1992).
The Day Hospital Group is formed from the authors of this systematic review and the authors of the original trials.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Burch 1999 {published and unpublished data}
- Burch S, Borland C. Collaboration, facilities and communities in day care services for older people. Health and Social Care in the Community 2001;1:19‐30. [DOI] [PubMed] [Google Scholar]
- Burch S, Longbottom J, MacKay M, Borland C, Prevost T. A randomised controlled trial of day hospital and day centre therapy. Clinical Rehabilitation 1999;2:105‐12. [DOI] [PubMed] [Google Scholar]
- Burch S, Longbottom J, McKay M, Borland C, Prevost T. The Huntingdon Day Hospital Trial: secondary outcome measures. Clinical Rehabilitation 2000;4:447‐53. [DOI] [PubMed] [Google Scholar]
Crotty 2008 {published and unpublished data}
- Crotty M. Post acute rehabilitation: a randomised controlled trial of day hospital and domiciliary care versus rehabilitation in the home for deconditioned patients following hospitalisation to improve functional and nutritional status. Australian New Zealand Clinical Trials Registry 13/10/2005. [ACTRN12605000638639]
- Crotty M, Giles L C, Halbert J, Harding J, Miller M. Home versus day rehabilitation: a randomised controlled trial. Age and ageing 2008;36(6):628‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cummings 1985 {published data only}
- Cummings V, Kerner JF, Arones S, Steinbock C. An evaluation of a day hospital service in rehabilitation medicine. National Centre for Health Services Research Grant HS 01043 1980.
- Cummings V, Kerner JF, Arones S, Steinbock C. Day hospital service in rehabilitation medicine: an evaluation. Archives of Physical Medicine and Rehabilitation 1985;66(2):86‐91. [MEDLINE: ] [PubMed] [Google Scholar]
Eagle 1991 {published data only}
- Eagle DJ, Guyatt GH, Patterson C, Turpie I, Sackett B, Singer J. Effectiveness of a geriatric day hospital. CMAJ 1991;144(6):699‐704. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Gladman 1993 {published and unpublished data}
- Gladman J, Whynes D, Lincoln N. Cost comparison of domiciliary and hospital‐based stroke rehabilitation. DOMINO Study Group. Age and Ageing 1994;23(3):241‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Gladman JR, Lincoln NB. Follow‐up of a controlled trial of domiciliary stroke rehabilitation (DOMINO Study). Age and Ageing 1994;23(1):9‐13. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Gladman JR, Lincoln NB, Barer DH. A randomised controlled trial of domiciliary and hospital‐based rehabilitation for stroke patients after discharge from hospital. Journal of Neurology, Neurosurgery, and Psychiatry 1993;56(9):960‐6. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hedrick 1993 {published and unpublished data}
- Hedrick SC, Branch LG (eds). Adult day health care evaluation study. Medical Care 1993;31(9 suppl):SS1‐124. [MEDLINE: ] [PubMed] [Google Scholar]
Hui 1995 {published and unpublished data}
- Hui E, Lum CM, Woo J, Or KH, Kay RL. Outcomes of elderly stroke patients. Day hospital versus conventional medical management. Stroke 1995;26(9):1616‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Masud 2006 {published and unpublished data}
- Conroy S, Kendrick D, Harwood R, Gladman J, Coupland C, Sach T, et al. A multicentre randomised controlled trial of day hospital‐based falls prevention programme for a screened population of community‐dwelling older people at high risk of falls. Age and Ageing 2010;39:704‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvine L, Conroy SP, Sach T, Gladman JRF, Harwood RH, Kendrick D, et al. Cost‐effectiveness of a day hospital falls prevention programme for screened community‐dwelling older people at high risk of falls. Age and Ageing 2010;39:710‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masud T, Coupland C, Drummond A, Gladman J, Kendrick D, Sach T, et al. Multifactorial day hospital intervention to reduce falls in high risk older people in primary care: A multi‐centre randomised controlled trial. Current Controlled Trials in Cardiovascular Medicine 2006;7:5. [MEDLINE: ; ISRCTN46584556] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parker 2009 {published and unpublished data}
- Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby P, et al. Rehabilitation of older patients: day hospital compared with rehabilitation at home. Clinical outcomes. Age and Ageing 2011;40(5):557‐62. [DOI] [PubMed] [Google Scholar]
- Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al. Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial. Health Technology Assessment 2009;13(39):1‐143. [DOI] [PubMed] [Google Scholar]
Pitkala 1991 {published and unpublished data}
- Pitkala K. The effectiveness of day hospital care on home care patients. Journal of the American Geriatrics Society 1998;46(9):1086‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Pitkala K, Winell K, Tilvis RS. Effects of day hospital care for home patients. Archives of Gerontology and Geriatrics 1991;Suppl 2:51‐4. [Google Scholar]
Roderick 2001 {published data only}
- Roderick P, Low J, Day R, Peasgood T, Mullee MA, Turnbull JC, et al. Stroke rehabilitation after hospital discharge: a randomized trial comparing domiciliary and day‐hospital care. Age and Ageing 2001;30:303‐10. [DOI] [PubMed] [Google Scholar]
Tucker 1984 {published data only}
- Tucker MA, Davison JG, Ogle SJ. Day hospital rehabilitation‐effectiveness and cost in the elderly: a randomised controlled trial. British Medical Journal (Clinical Research Ed) 1984;289(6453):1209‐12. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vetter 1989 {published and unpublished data}
- Vetter NJ, Smith A, Sastry D, Tinker G. Day hospital: pilot study report. St Davids Hospital, Department of Geriatrics, 1989. [Google Scholar]
Weissert 1980 {published data only}
- Wan TT, Weissert WG, Liviertos BB. Geriatric day care and homemaker services: an experimental study. Journal of Gerontology 1980;35(2):256‐74. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Weissert W, Wan T, Liviertos B, Katz S. Effects and costs of day‐care services for the chronically ill: a randomized experiment. Medical Care 1980;18(6):567‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Weissert WG, Wan TH, Liviertos B. Effects and costs of day care and homemaker services for the chronically ill: a randomized experiment. National Center for Health Services Research February 1980. [DOI] [PubMed]
Woodford 1962 {published data only}
- Woodford‐Williams E, McKeon JA, Trotter IS, Watson D, Bushby C. The day hospital in the community care of the elderly. Gerontology Clinic 1962;4:241‐56. [DOI] [PubMed] [Google Scholar]
Young 1992 {published and unpublished data}
- Young J, Forster A. Day hospital and home physiotherapy for stroke patients: a comparative cost‐effectiveness study. Journal of the Royal College of Physicians of London 1993;27(3):252‐7. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
- Young JB, Forster A. The Bradford community stroke trial: results at six months. BMJ 1992;304(6834):1085‐9. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Adamowski 2009 {published data only}
- Adamowski T, Hadrys T, Kiejna A. Comparison between day‐care ward and inpatient ward in terms of treatment effectiveness based on the analysis of psychopathologic symptoms, subjective quality of life and number of rehospitalisations after discharge. Archives of Psychiatry and Psychotherapy 2009;11(3):67‐73. [PubMed] [Google Scholar]
Aimonino Ricauda 2008 {published data only}
- Aimonino Ricauda N, Tibaldi V, Leff B, Scarafiotti C, Marinello R, Zanocchi M, Molaschi M. Substitutive "hospital at home" versus inpatient care for elderly patients with exacerbations of chronic obstructive pulmonary disease: a prospective randomized, controlled trial. Journal of the American Geriatrics Society 2008;56(3):493‐500. [DOI] [PubMed] [Google Scholar]
Bartak 2011 {published data only}
- Bartak A, Andrea H, Spreeuwenberg MD, Ziegler UM, Dekker J, Rossum BV, et al. Effectiveness of outpatient, day hospital, and inpatient psychotherapeutic treatment for patients with cluster B personality disorders. Psychotherapy and Psychosomatics 2011;80(1):26‐38. [DOI] [PubMed] [Google Scholar]
Baskett 1999 {unpublished data only}
- Baskett JJ, Broad JB, Reekie G, Hocking C, Green G. Shared responsibility for ongoing rehabilitation: a new approach to home‐based therapy after stroke. Clinical Rehabilitation 1999;13(1):23‐33. [DOI] [PubMed] [Google Scholar]
Baumgarten 2002 {published data only}
- Baumgarten M, Lebel P, Laprise H, Leclerc C, Quinn C. Adult day care for the frail elderly: outcomes, satisfaction, and cost. Journal of Aging and Health 2002;14(2):237‐59. [DOI] [PubMed] [Google Scholar]
Bjokdahl 2006 {published data only}
- Bjorkdahl A, Nilsson AL, Grimby G, Sunnerhagen KS. Does a short period of rehabilitation in the home setting facilitate functioning after stroke?. Clinical Rehabilitation 2006;20:1038‐49. [DOI] [PubMed] [Google Scholar]
Bussche 2010 {published data only}
- Bussche PV, Desmyter F, Duchesnes C, Massart V, Giet D, Petermans J, et al. Geriatric day hospital: opportunity or threat? A qualitative exploratory study of the referral behaviour of Belgian general practitioners. BMC Health Services Research 2010;10(1):202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Canuto 2008 {published data only}
- Canuto A, Meiler‐Mititelu C, Herrmann FR, Delaloye C, Giannakopoulos P, Weber K. Longitudinal assessment of psychotherapeutic day hospital treatment for elderly patients with depression. International Journal of Geriatric Psychiatry 2008;23(9):949‐56. [DOI] [PubMed] [Google Scholar]
Capomolla 2002 {published data only}
- Capomolla S, Febo O, Ceresa M, Caporotondi A, Guazzotti G, Rovere MT, et al. Cost/utility ratio in chronic heart failure: comparison between heart failure management program delivered by day‐hospital and usual care. Journal of the American College of Cardiology 2002;40(7):1259‐66. [DOI] [PubMed] [Google Scholar]
Chau 2013 {published data only}
- Chau PH, Yeung F, Chan TW, Woo J. A quasi‐experimental study on a new service option for short‐term residential care of older stroke patients. Clinical interventions in aging 2013;8:1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chiu 2009 {published data only}
- Chiu L, Lam W, Lin W, Wong M, Lee H. Retrospective Study on the Outcome of Patients Attending Psychogeriatric Day Hospital (PGDH). Medical Diary 2009;14(2):11. [Google Scholar]
Close 1999 {published data only}
- Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet 1999;353(9147):93‐7. [DOI] [PubMed] [Google Scholar]
Coleman 1999 {published data only}
- Coleman EA, Grothaus LC, Sandhu N, Wagner EH. Chronic care clinics: a randomized controlled trial of a new model of primary care for frail older adults. Journal of the American Geriatrics Society 1999;47:775‐83. [DOI] [PubMed] [Google Scholar]
Comans 2010 {published data only}
- Comans TA, Brauer SG, Haines, Terry P. Randomized trial of domiciliary versus center‐based rehabilitation: which is more effective in reducing falls and improving quality of life in older fallers?. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2010;65(6):672‐9. [DOI] [PubMed] [Google Scholar]
Crilly 2005 {published data only}
- Crilly RG, Lytwynec S, Kloseck M, Smith JM, Olsen T, Gold B, et al. Patient Outcomes after Discharge from a Geriatric Day Hospital. Cadadian Journal on Aging 2005;24(3):305‐10. [DOI] [PubMed] [Google Scholar]
Dasgupta 2005 {published data only}
- Dasgupta M, Clarke NCT, Brymer CD. Characteristics of patients who made gains at a geriatric day hospital. Archives of Gerontology and Geriatrics 2005;40:173‐84. [DOI] [PubMed] [Google Scholar]
Del Giudice 2009 {published data only}
- Giudice E, Ferretti E, Omiciuolo C, Sceusa R, Zanata C, Manganaro D, et al. The hospital‐based, post‐acute geriatric evaluation and management unit: the experience of the acute geriatric unit in Trieste . Archives of Gerontology and Geriatrics 2009;49:49‐60. [DOI] [PubMed] [Google Scholar]
de Oliveira 2010 {published data only}
- Oliveira JCM, Leitão Filho FSS, Sampaio LMM, Oliveira ACN, Hirata RP, Costa D, et al. Outpatient vs. home‐based pulmonary rehabilitation in COPD: a randomized controlled trial. Multidisciplinary respiratory medicine 2010;5(6):401‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Desrosiers 2004 {published data only}
- Desrosiers J, Hebert R, Payette H, Roy P, Tousignant M, Cote S, et al. Geriatric Day Hospital: Who Improves the Most?. Canadian Journal on Aging 2005;23(3):217‐29. [DOI] [PubMed] [Google Scholar]
Edelman 2010 {published data only}
- Edelman D, Fredrickson SK, Melnyk SD, Coffman CJ, Jeffreys AS, Datta S, et al. Medical Clinics Versus Usual Care for Patients With Both Diabetes and Hypertension. A Randomized Trial. Annals of Internal Medicine 2010;152(11):689‐96. [DOI] [PubMed] [Google Scholar]
Evans 1998 {published data only}
- Evans R L, Connis RT, Haselkorn J K. Hospital‐based rehabilitative care versus outpatient services: effects on functioning and health status. Disability & Rehabilitation 1998;20(8):298‐307. [DOI] [PubMed] [Google Scholar]
Famadas 2008 {published data only}
- Famadas JC, Frick KD, Haydar ZR, Nicewander D, Ballard D, Boult C. The effects of interdisciplinary outpatient geriatrics on the use, costs and quality of health services in the fee‐for‐service environment. Aging ‐ Clinical and Experimental Research 2008;20(6):556‐61. [DOI] [PubMed] [Google Scholar]
Foley 2009 {published data only}
- Foley A, Hillier S, Barnard R. Evaluation of a geriatric day rehabilitation centre: Subjective and objective outcomes in community‐dwelling older adults. Australian Journal of Primary Health 2009;15(2):117‐22. [Google Scholar]
Gitlin 2006 {published data only}
- Gitlin LN, Reever K, Dennis MP, Mathieu E, Hauck WW. Enhancing Quality of Life of Families Who Use Adult Day Services: Short‐ and Long‐Term Effects of the Adult Day Services Plus Program. The Gerontologist 2006;46(5):630‐9. [DOI] [PubMed] [Google Scholar]
Glaesmer 2003 {published data only}
- Glaesmer H, Kunstler J, Reuter W. Improvement of functional deficits, physical mobility and cognitive function by treatment in a geriatric day hospital. Zeitschrift fur Gerontologie und Geriatrie 2003;6:475‐83. [DOI] [PubMed] [Google Scholar]
Hershkovitz 2003 {published data only}
- Hershkovitz A, Gottieb D, Beloosesky Y, Brill S. Programme evaluation of a geriatric rehabilitation day hospital. Clinical Rehabilitation 2003;17:750‐5. [DOI] [PubMed] [Google Scholar]
Hershkovitz 2007 {published data only}
- Hershkovitz A, Brill S. The association between patients' cognitive status and rehabilitation outcome in a geriatric day hospital. Disability & Rehabilitation 2007;29(4):333‐7. [DOI] [PubMed] [Google Scholar]
Horgan 2009 {published data only}
- Horgan NF, Crehan F, Bartlett E, Keogan F, O'Grady AM, Moore AR, et al. The effects of usual footwear on balance amongst elderly women attending a day hospital. Age and Ageing 2009;38(1):62‐7. [DOI] [PubMed] [Google Scholar]
Jacob 2007 {published data only}
- Jacob M E, Abraham V J, Abraham S, Jacob KS. The effect of community based daycare on mental health and quality of life of elderly in rural south India: a community intervention study. International Journal of Geriatric Psychiatry 2007;22(5):445‐7. [DOI] [PubMed] [Google Scholar]
Juhani 2011 {published data only}
- Juhani J, Mila G‐L, Hannu T. Results of a multidisciplinary out‐patient rehabilitation programme for senior coronary patients‐A randomised controlled trial. Psychology & Health 2011;26:35. [Google Scholar]
Kallert 2007 {published data only}
- Kallert TW, Priebe S, McCabe R, Kiejna A, Rymaszewska J, Nawka P, et al. Are day hospitals effective for acutely ill psychiatric patients? A European multicenter randomized controlled trial. Journal of Clinical Psychiatry 2007;68(2):278‐87. [DOI] [PubMed] [Google Scholar]
Kneebone 2010 {published data only}
- Kneebone II, Hurn JS, Raisbeck E, Cropley M, Khoshnaw H, Milton JE. The Validity of Goal Achievement as an Outcome Measure in Physical Rehabilitation Day Hospitals for Older People. International Journal of Disability, Development and Education 57;2:145‐153. [Google Scholar]
Lariviere 2010 {published data only}
- Lariviere N, Desrosiers J, Tousignant M, Boyer R. Who benefits the most from psychiatric day hospitals? A comparison of three clinical groups. Journal of Psychiatric Practice 2010;16(2):93‐102. [DOI] [PubMed] [Google Scholar]
Lariviere 2011 {published data only}
- Lariviere N, Desrosiers J, Tousignant M, Boyer R. Multifaceted impact evaluation of a day hospital compared to hospitalization on symptoms, social participation, service satisfaction and costs associated to service use. International Journal of Psychiatry in Clinical Practice 2011;15(3):228‐40. [DOI] [PubMed] [Google Scholar]
Leveille 1998 {published data only}
- Leveille SG, Wagner EH, Davis C, Grothaus L, Wallace J, LoGerfo M, et al. Preventing disability and managing chronic illness in frail older adults: a randomized trial of community‐based partnership with primary care. Journal of the American Geriatric Society 1998;46(10):1191‐8. [DOI] [PubMed] [Google Scholar]
Luk 2011 {published data only}
- Luk JKH, Chan CF. Rehabilitation outcomes of older patients at 6 months follow‐up after discharged from a geriatric day hospital (GDH). Archives of Gerontology and Geriatrics 2011;52(3):327‐30. [DOI] [PubMed] [Google Scholar]
Luk 2011a {published data only}
- Luk JKH, Chan CF, Chan FHW, Chu LW. Rehabilitation outcomes of older Chinese patients with different cognitive function in a geriatric day hospital. Archives of Gerontology & Geriatrics 2011;53(2):e144‐8. [DOI] [PubMed] [Google Scholar]
Malone 2002 {published data only}
- Malone M, Hill A, Smith G. Three‐month follow up of patients discharged from a geriatric day hospital. Age and Ageing 2002;31:471‐5. [DOI] [PubMed] [Google Scholar]
Manckoundia 2007 {published data only}
- Manckoundia P, Gerbault N, Mourey F, d' Athis P, Nourdin C, Monin M‐P, et al. Multidisciplinary management in geriatric day‐hospital is beneficial for elderly fallers: a prospective study of 28 cases. Archives of gerontology and geriatrics 2007;44(1):61‐70. [DOI] [PubMed] [Google Scholar]
Marsden 2010 {published data only}
- Marsden D, Quinn R, Pond N, Golledge R, Neilson C, White J. multidisciplinary group programme in rural settings for community‐dwelling chronic stroke survivors and their carers: a pilot randomized controlled trial. Clinical Rehabilitation 2010;24(4):328‐41. [DOI] [PubMed] [Google Scholar]
Masuda 2006 {published data only}
- Masuda Y, Noguchi H, Kuzuya M, Inoue A, Hirakawa Y, Iguchi A, et al. Comparison of medical treatments for the dying in a hospice and a geriatric hospital in Japan. Journal of palliative medicine 2006;9(1):152‐60. [DOI] [PubMed] [Google Scholar]
Meinck 2002 {published data only}
- Meinck M, Freigang K, John B, Keitel C, Puls E, Robra B. Outpatient geriatric rehabilitation: an evaluation of two models assessing trends of medical outcomes. Die Rehabilitation 2003;42(1):45‐51. [DOI] [PubMed] [Google Scholar]
- Meinck M, Freigang K, John B, Keitel C, Puls R, Robra BP. Outpatient geriatric rehabilitation ‐ the structural and process quality of a geriatric mobile service team and a community‐based outpatient center. Zeitschrift fur Gerontologie und Geriatrie 2002;35:463‐73. [DOI] [PubMed] [Google Scholar]
Olsson 2007 {published data only}
- Olsson BG, Sunnerhagen KS. Functional and Cognitive Capacity and Health‐Related Quality of Life 2 Years After Day Hospital Rehabilitation for Stroke: A Prospective Study. Journal of Stroke and Cerebrovascular Diseases 2007;16(5):208‐15. [DOI] [PubMed] [Google Scholar]
Pereira 2010 {published data only}
- Pereira SR, Chiu W, Turner A, Chevalier S, Joseph L, Huang AR. How can we improve targeting of frail elderly patients to a geriatric day‐hospital rehabilitation program?. BMC Geriatrics 2010;10:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Priebe 2011 {published data only}
- Priebe S, Barnicot K, McCabe R, Kiejna A, Nawka P, Raboch J, et al. Patients' subjective initial response and the outcome of inpatient and day hospital treatment. European Psychiatry 2011;26(7):408‐13. [DOI] [PubMed] [Google Scholar]
- Priebe S, McCabe R, Schutzwohl M, Kiejna A, Nawka P, Raboch J, et al. Patient characteristics predicting better treatment outcomes in day hospitals compared with inpatient wards. Psychiatric Services 2011;62(3):278‐84. [DOI] [PubMed] [Google Scholar]
Richardson 2000 {published data only}
- Richardson J, Law M, Wishart L, Guyatt G. The use of a simulated environment (easy street) to retrain independent living skills in elderly persons: a randomized controlled trial. Journals of Gerontology Series A‐Biological Sciences and Medical Sciences 2000;55(10):M578‐84. [DOI] [PubMed] [Google Scholar]
Sato 2007 {published data only}
- Sato D, Kaneda K, Wakabayashi H, Nomura T. Comparison two‐year effects of once‐weekly and twice‐weekly water exercise on health‐related quality of life of community‐dwelling frail elderly people at a day‐service facility. Disability & Rehabilitation 2009;31(2):84‐93. [DOI] [PubMed] [Google Scholar]
- Sato D, Kaneda K, Wakabayashi H, Nomura T. The water exercise improves health‐related quality of life of frail elderly people at day service facility. Quality Life Research 2007;16:1577‐85. [DOI] [PubMed] [Google Scholar]
Schweikert 2009 {published data only}
- Schweikert B, Hahmann H, Steinacker JM, Imhof A, Muche R, Koenig W, et al. Intervention study shows outpatient cardiac rehabilitation to be economically at least as attractive as inpatient rehabilitation. Clinical research in cardiology 2009;98(12):787‐95. [DOI] [PubMed] [Google Scholar]
Scott 2004 {published data only}
- Scott JC, Conner DA, Venohr RN, Gate G, McKenzie M, Kramer AM, et al. Effectiveness of a Group Outpatient Visit Model for Chronically Ill Older Health Maintenance Organization Members: A 2‐Year Randomized Trial of the Cooperative Health Care Clinic. Journal of the American Geriatrics Society 2004;52:1463‐70. [DOI] [PubMed] [Google Scholar]
Sherwood 1986 {published data only}
- Sherwood S, Morris JN, Ruchlin HS. Alternative paths to long‐term care: nursing home, geriatric day hospital, senior center, and domiciliary care options. American Journal of Public Health 1986;76(1):38‐44. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Skellie 1982 {published data only}
- Skellie FA, Mobley GM, Coan RE. Cost‐effectiveness of community‐based long‐term care: current findings of Georgia's alternative health services project. American Journal of Public Health 1982;72(4):353‐8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spice 2009 {published and unpublished data}
- Spice CL, Morotti W, George S, Dent TH, Rose J, Harris S, et al. The Winchester falls project: a randomised controlled trial of secondary prevention of falls in older people. Age and Ageing 2009;38(1):33‐40. [DOI] [PubMed] [Google Scholar]
Velghe 2011 {published data only}
- Velghe A, Kohn L, Petermans J, Gillain D, Petrovic M, Noortgate N. The Belgian geriatric day hospitals as part of a care program for the geriatric patient: first results of the implementation at the national level. Acta clinica belgica 2011;66(3):186‐90. [DOI] [PubMed] [Google Scholar]
Wade 2003 {published data only}
- Wade DT, Gage H, Owen C, Trend P, Grossmith C, Kaye J. Multidisciplinary rehabilitation for people with Parkinson's disease: A randomised controlled study. Journal of Neurology, Neurosurgery and Psychiatry 2003;74(2):158‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weiler 1976 {published data only}
- Weiler PG, Kim P, Pickard LS. Health care for elderly Americans: evaluation of an adult day health care model. Medical Care 1976;14(8):700‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wong 1998 {published data only}
- Wong SF, Yap KB, Chan KM. Day hospital rehabilitation for the elderly: a retrospective study. Annals of the Academy of Medicine, Singapore 1998;27(4):468‐73. [PubMed] [Google Scholar]
Zank 2002 {published data only}
- Zank S, Schacke C. Evaluation of geriatric day care units: effects on patients and caregivers. Journals of Gerontology Series B‐Psychological Sciences and Social Sciences 2002;57B(4):348‐57. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
ISRCTN53696600 {published data only}
- ISRCTN53696600. Can assistance by carers during walking in the home be reduced by increasing physiotherapy input for stroke patients attending a day hospital once a week?. http://www.controlled‐trials.com/ISRCTN53696600/53696600 (accessed December 2013).
Matzen 2007 {published data only}
- Matzen L E, Foged L, Pedersen P, Wengler K, Andersen‐Ranberg K. Primary visitation of elective referred geriatric patients‐‐a randomised study of home visits compared to day hospital visits. Ugeskrift for laeger 2007;169(22):2109‐13. [PubMed] [Google Scholar]
Moe 2010 {published data only}
- Moe R H, Uhlig T, Kjeken I, Hagen K B, Kvien T K, Grotle M. Multidisciplinary and multifaceted outpatient management of patients with osteoarthritis: protocol for a randomised, controlled trial [BMC musculoskeletal disorders]. BMC musculoskeletal disorders 2010;11(1):253. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT00785746 {published data only}
- NCT00785746. Improving Balance in Frail Elderly. http://clinicaltrials.gov/show/NCT00785746 (accessed December 2013).
Yamada 2005 {published data only}
- Yamada S, Toba K. A prospective comparison of day care and freely chosen occupational therapy for elderly patients with dementia. Nihon Ronen Igakkai zasshi. Japanese journal of geriatrics 2004;42(1):83. [DOI] [PubMed] [Google Scholar]
Additional references
Ames 1995
- Ames D, Hastie IR. Geriatric day hospitals ‐ the future?. Postgraduate Medical Journal 1995;71(835):260‐1. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beynon 2009
- Beynon JH, Padiachy D. The past and future of geriatric day hospitals. Reviews in Clinical Gerontology 2009;19(01):45‐51. [Google Scholar]
Black 2005
- Black D. The geriatric day hospital. Age and ageing 2005;34 427‐429(5):427‐429. [DOI] [PubMed] [Google Scholar]
Borenstein 2009
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Fixed‐Effect versus Random‐Effects Models. Introduction to Meta‐Analysis. Chichester: Wiley, 2009:77‐86. [Google Scholar]
Bours 1998
- Bours GJJW, Ketelaars CAJ, Frederiks CMA, Abu‐Saad HH, Wouters EFM. The effects of aftercare on chronic patients and frail elderly patients when discharged from hospital: a systematic review. Journal of Advanced Nursing May 1998;27(5):1076‐86. [DOI] [PubMed] [Google Scholar]
Brocklehurst 1973
- Brocklehurst JC. Role of hospital day care. British Medical Journal 1973;4(886):223‐5. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brocklehurst 1980
- Brocklehurst JC, Tucker J. Progress in geriatric day care. London: King's Fund 1980.
Brocklehurst 1995
- Brocklehurst J. Geriatric day hospitals. Age and Ageing 1995;24(2):89‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Donaldson 1986
- Donaldson C, Wright K, Maynard A. Determining value for money in day hospital care for the elderly. Age and Ageing 1986;15(1):1‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Donaldson 1987
- Donaldson C, Wright KG, Maynard AK, Hamill JD, Sutcliffe E. Day hospitals for the elderly: utilisation and performance. Community Medicine 1987;9(1):55‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Eagle 1987
- Eagle DJ, Guyatt G, Patterson C, Turpie I. Day hospitals' cost and effectiveness: a summary. Gerontologist 1987;27(6):735‐40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith S, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ellis 2011
- Ellis G, Whitehead MA, O'Neill D, Langhorne P, Robinson, D. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD006211.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Farndale 1961
- Farndale J. The day hospital movement in Great Britain. Oxford: Pergamon Press, 1961. [Google Scholar]
George 1989
- George J, Young J. Community referrals to the day hospital. Health Trends 1989;21:24‐5. [PubMed] [Google Scholar]
Gerard 1988
- Gerard K. An appraisal of the cost‐effectiveness of alternative day care settings for frail elderly people. Age and Ageing 1988;17(5):311‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gladman 1994
- Gladman J, Whynes D, Lincoln N. Cost comparison of domiciliary and hospital‐based stroke rehabilitation. DOMINO Study Group. Age and Ageing 1994;23(3):241‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
GRADEpro 2014 [Computer program]
- McMaster University. GRADEpro. Version 2014. McMaster University, 2014.
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
MacFarlane 1979
- MacFarlane JP, Collings T, Graham K, MacIntosh JC. Day hospitals in modern clinical practice‐cost benefit. Age and Ageing 1979;8(Suppl):80‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mason 2007
- Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al. A systematic review of the effectiveness and cost‐effectiveness of different models of community‐based respite care for frail older people and their carers. Health Technology Assessment 2007;11(15):1‐176. [DOI] [PubMed] [Google Scholar]
NAO 1994
- National Audit Office. National health service day hospitals for elderly people in England. HMSO 1994.
Outpatient Service 2004
- Legg L, Langhorne P, Outpatient Service Trialists. Rehabilitation therapy services for stroke patients living at home: systematic review of randomised trials. The Lancet 2004;363:352‐6. [DOI] [PubMed] [Google Scholar]
Parker 1994
- Parker SG, Du X, Bardsley MJ, Goodfellow J, Cooper RG, Cleary R, et al. Measuring outcomes in care of the elderly. Journal of the Royal College of Physicians of London 1994;28(5):428‐33. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Petermans 2011
- Petermans J, Velghe A, Gillain D, Boman X, Noortgate N. Geriatric day hospital: What evidence? A systematic review [L’hôpital de jour gériatrique: quels objectifs, quelle organisation, quelle efficience?]. Gériatrie et Psychologie Neuropsychiatrie du Vieillissement 2011;9(3):295‐303. [DOI] [PubMed] [Google Scholar]
Prvu Bettger 2007
- Prvu Bettger JA, Stineman MG. Effectiveness of Multidisciplinary Rehabilitation Services in Postacute Care: State‐of‐the‐Science. A Review. Archives of Physical Medicine and Rehabilitation November 2007;88:1526‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
RCP 1994
- Research Unit of the Royal College of Physicians and British Geriatric Society. Geriatric day hospitals: their role and guidelines for good practice. Royal College of Physicians of London 1994.
Siu 1994
- Siu AL, Morishita L, Blaustein J. Comprehensive geriatric assessment in a day hospital. Journal of the American Geriatrics Society 1994;42(10):1094‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Stuck 1993
- Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta‐analysis of controlled trials. The Lancet 1993;342(8878):1032‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
UN 2011
- United Nations Department of Economic & Social Affairs. Population Division. World Population Prospects: The 2010 Revision. United Nations, 2011. [Google Scholar]
Young 1993
- Young J, Forster A. Day hospital and home physiotherapy for stroke patients: a comparative cost‐effectiveness study. Journal of the Royal College of Physicians of London 1993;27(3):252‐7. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Forster 1999
- Forster A, Young J, Langhorne P, on behalf of the Day Hospital Group. Systematic review of day hospital care for elderly people. British Medical Journal 1999;318:837‐41. [PUBMED: 10092260] [DOI] [PMC free article] [PubMed] [Google Scholar]
Forster 1999a
- Forster A, Young J, Langhorne P. Day Hospital Group. Medical day hospital care for the elderly versus alternative forms of care. Cochrane Database of Systematic Reviews 1999, Issue 3. [DOI: 10.1002/14651858.CD001730.pub2] [DOI] [PubMed] [Google Scholar]
Forster 2008
- Forster A, Young J, Lambley R, Langhorne P. Medical day hospital care for the elderly versus alternative forms of care. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD001730.pub2; PUBMED: 18843620] [DOI] [PubMed] [Google Scholar]


