Abstract
Background
Isolated fractures of the shaft of the ulna, which are often sustained when the forearm is raised to shield against a blow, are generally treated on an outpatient basis. This is an update of a Cochrane review first published in 1998 and last updated in 2009.
Objectives
To assess the effects of various forms of treatment for isolated fractures of the ulnar shaft in adults.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (April 2012), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2012, Issue 3), MEDLINE (1966 to April week 1 2012), EMBASE (1981 to week 15 2012), CINAHL (1982 to 16 April 2012), various trial registers, various conference proceedings and bibliographies of relevant articles.
Selection criteria
Randomised or quasi‐randomised trials of conservative and surgical treatment of isolated fractures of the ulnar shaft in adults. Excluded were fractures of the proximal ulna and Monteggia fracture dislocations.
Data collection and analysis
We performed independent assessment of risk of bias and data extraction. We contacted trialists for more information. There was no pooling of data.
Main results
The updated search resulted in the identification of one ongoing trial comparing surgery versus conservative treatment.
Four trials, involving a total of 237 participants, were included. All four trials were methodologically flawed and potentially biased.
Three trials tested conservative treatment interventions. One trial, which compared short arm (below elbow) pre‐fabricated functional braces with long arm (elbow included) plaster casts, found there was no significant difference in the time it took for fracture union. Patient satisfaction and return to work during treatment were significantly better in the brace group. The other two trials, both quasi‐randomised, had three treatment groups. One trial compared Ace Wrap elastic bandage versus short arm plaster cast versus long arm plaster cast. The large loss to follow‐up in this trial makes any data analysis tentative. However, the need for replacement of the Ace wrap by other methods due to pain indicates the potential for a serious problem with this intervention. The other trial, which compared immediate mobilisation versus short arm plaster cast versus long arm plaster cast for minimally displaced fractures, found no significant differences in outcome between these three interventions.
The fourth trial, which compared two types of plates for surgical fixation, found no significant differences in functional or anatomical outcomes nor complications between the two groups.
Authors' conclusions
There is insufficient evidence from randomised trials to determine which method of treatment is the most appropriate for isolated fractures of the ulnar shaft in adults. Well designed and reported randomised trials of current forms of conservative treatment are recommended.
Plain language summary
Interventions for treating adults with an isolated fracture of the ulnar shaft
The ulna is one of the two bones of the forearm. Isolated fractures of the shaft of the ulna, without other fractures, often result when the forearm is raised to fend off a blow. Such fractures are fairly rare, but can result in significant disability. Most people are treated in outpatients with plaster casts or arm braces. Some are treated surgically. Surgery generally involves the re‐alignment and fixation of the broken ends of the bone.
Four trials, involving a total of 237 participants, were included in the review. These trials had methodological weaknesses that could have resulted in serious bias. One trial compared 'short arm' (splintage stopping below the elbow) pre‐fabricated functional braces with 'long arm' (splintage includes the elbow) plaster casts. It found no clear difference between the two groups in the time taken for the fracture to heal. However, significantly more people in the brace group were satisfied with their treatment and significantly more returned to work during their treatment. One trial compared Ace Wrap elastic bandage, short arm plaster cast and long arm plaster cast. The large loss to follow‐up in this trial makes any findings tentative. However, the need for replacement of the Ace wrap by other methods due to pain does indicate the potential for a serious problem with this intervention. The third trial, which compared immediate mobilisation versus short arm plaster cast versus long arm plaster cast for minimally displaced fractures, found no clear differences in outcome between these three interventions. The fourth trial found no significant differences in functional or anatomical outcomes nor complications between the two types of plates used for surgical fixation of the fracture.
Overall, there was not enough evidence from randomised controlled trials to show which methods of treatment are better for these injuries.
Background
Description of the condition
Isolated fractures of the shaft of the ulna are often sustained when the forearm is raised to shield against a blow. The energy is then absorbed by the subcutaneous ulna resulting in the characteristic 'nightstick' type fracture (Atkin 1995a). (A nightstick is an American policeman's truncheon.) This type of fracture frequently occurs in young males involved in violent activities (Du Toit 1979).
Epidemiological data on the incidence of this injury is difficult to locate, probably as most of these fractures are treated on an outpatient basis. Initially in the absence of accessible general information, one of us (Pearce) examined his local hospital database at the time and found that the Friarage Hospital, Northallerton, a small District General Hospital in rural Northern England which serves a population of 122,000, had a total of 26 cases of isolated fracture of the ulna in 1997. Most of these injuries were a result of direct violent or high energy impact and many involved incidents with cattle or horses. This figure gives a local incidence rate of 0.2 per 1000 population. This agrees with the general impression of low incidence but it is not known how this figure compares nationally or internationally. Subsequently, we located a report of an epidemiological study of people over 14 years of age with fractures of the radius and ulna presenting to the Orthopaedic Trauma Unit of the Royal Infirmary of Edinburgh, UK, over a three year period starting January 1990 (McQueen 2000). This unit, which serves a population of around 650,000 meeting the above age criterion, treated a total of 72 cases of isolated fractures of the ulna over the three year period. This gives an annual incidence of approximately 0.04 per 1,000 population, which is a fifth of the rate in Northallerton. Nonetheless, we still anticipate that the incidence is likely to be higher in bigger cities and other areas where violence is more common. McQueen 2000 reported that 38% of the injuries resulted from a direct blow, 31% from a simple fall and 14% from pedestrian road traffic accidents; the mechanism of injury was not stated for the other 17% but none involved sport. Nearly two thirds of the study population was male (63%). The mean age of patients was 43 years; range 18 to 94 years. There was a bimodal distribution of annual age and sex specific incidence; the incidence in males was highest in the youngest age group and tapered off with age, whereas that in females increased gradually for the first few decades and then, reflecting underlying osteoporosis, more dramatically in the elderly.
Although not common, the fracture appears to have a high complication rate, principally non‐union, malunion, reduction in the range of wrist and elbow movements, pain and deformity. For instance, Grace 1980 reported a fracture non‐union rate of 14%. In a brief review of the results of seven studies of people treated for ulna fracture, Pollock 1983 reported non‐union rates ranging from 1% to 12%, impairment of forearm rotation between 18% to 32% of patients and, for four studies, significant reductions in elbow flexion and extension. A similar picture was conveyed in a review of 33 "series" by Mackay 2000. Such complications may have an effect upon a person's ability to perform their activities of daily living and can prevent them from returning to their previous employment (Atkin 1995a).
Description of the intervention
The most suitable method of management of this injury has not been established. The choice of treatment will be influenced by the mechanism of injury, fracture pattern, degree of displacement, angulation and location, associated injuries, as well as patient preferences. The treatment options are:
-
Conservative treatment with:
above elbow plaster cast;
below elbow plaster cast;
functional brace;
Ace wrap elastic bandage (Pollock 1983);
sling (De Jong 1989).
-
Open reduction and internal fixation with:
plates;
intramedullary nails/devices.
The evaluation of treatment has been traditionally based on either anatomical accuracy of reduction and/or functional outcomes based on range of movement, pain, grip strength, residual soft tissue swelling, local complications, cosmetic appearance, patient satisfaction with treatment, and activities of daily living.
Why it is important to do this review
Though isolated ulnar shaft fractures are comparatively rare, there remains a need to establish the best methods to manage these fractures which are often associated with a high rate of complications and, for some, serious limitations in function. This update of a Cochrane review, first published in 1998 and last updated in 2009 (Handoll 2009), continues the review of evidence for treatment interventions as it accrues, albeit slowly.
Objectives
We aimed to compare the relative effects (benefits and harms) of the following for adults with displaced or non‐displaced isolated fractures of the ulnar shaft.
Any method of conservative treatment versus any other method of conservative treatment.
Any method of surgical treatment versus any method of conservative treatment.
Any method of surgical treatment versus any other method of surgical treatment.
Methods
Criteria for considering studies for this review
Types of studies
Any randomised or quasi‐randomised (methods of allocating participants to a treatment which are not strictly random e.g. by date of birth, hospital record number, alternation) clinical trials of interventions listed below were considered.
Types of participants
Adults of either gender with an isolated fracture of the mid and lower third of the ulna above the distal radio‐ulnar joint. Studies which focus solely on ulnar shaft fractures in children or Monteggia fractures were to be excluded.
Types of interventions
Conservative treatment using above or below elbow plaster casts or functional braces, or surgical treatment involving open reduction and internal fixation.
Types of outcome measures
Data for the following outcomes were sought.
Primary outcomes
Subjective functional outcomes, preferable validated self‐reported assessment of upper‐limb function and activities of daily living, such as Disabilities of the Arm, Shoulder and Hand (DASH: Beaton 2001), or overall function, e.g. Short Musculoskeletal Function Assessment (SMFA: Swiontkowski 1999), and SF‐36 physical component scale.
Non or delayed union, preferably confirmed radiologically.
Secondary outcomes
Health related quality of life outcomes, e.g. SF‐36
Patient satisfaction with outcome
Pain
Clinical outcomes: residual soft tissue swelling, local and other complications, cosmetic appearance, non or delayed union, time to recover.
Range of movement
Radiographic results: non‐union and deformity
Economic outcomes
Surgical intervention, hospital stay, physiotherapy, return to work and time off work.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (April 2012), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2012, Issue 3), MEDLINE (1966 to April week 1 2012), EMBASE (1981 to week 15 2012) and the Cumulative Index to Nursing and Allied Health Literature ‐CINAHL (1982 to 16 April 2012). We also searched Current Controlled Trials (accessed April 2012), the UK National Research Register archives (covers up to September 2007), and the WHO International Clinical Trials Registry Platform (accessed April 2012) for ongoing and recently completed trials.
The search strategies used in the current update for MEDLINE (OVID WEB), EMBASE (OVID WEB), CINAHL (EBSCO), The Cochrane Library (Wiley InterScience) together with other electronic searches are shown in Appendix 1. In MEDLINE, the search strategy was combined with the first two sections of optimal MEDLINE search strategy for randomised trials (Higgins 2006).
Searching other resources
We handsearched the British Volume of the Journal of Bone and Joint Surgery supplements (1996 to 2006), abstracts of the American Society for Surgery of the Hand annual meetings (2000 to 2011) and abstracts of the American Orthopaedic Trauma Association annual meetings (up to 2011). We electronically searched the British Volume of the Journal of Bone and Joint Surgery and conference proceedings from 2006 onwards (April 2012). Previously, we searched the following conference proceedings on the Acta Orthopaedica Scandinavica web page: Danish Orthopedic Society, Arhus, May 2001; Danish Orthopedic Society, Copenhagen, October 2000; Danish Orthopedic Society, Odense, May 2000; Netherlands Orthopedic Society, Groningen, May 2001; Netherlands Orthopaedic Association, Utrecht, September 2000; Netherlands Orthopaedic Association, Rotterdam, January 2000; Nordic Orthopaedic Federation, Tampere, Finland, June 2000; Norwegian Orthopedic Society, Oslo, October 1999; Swedish Orthopaedic Association, Vaxjo, September 2000.
Up to December 2008, we scrutinised weekly downloads of "Fracture" articles in new issues of 17 journals (Acta Orthop Scand; Am J Orthop; Arch Orthop Trauma Surg; Clin J Sport Med; Clin Orthop; Emerg Med Clin North Am; Foot Ankle Int; Injury; J Accid Emerg Med; J Am Acad Orthop Surg; J Arthroplasty; J Bone Joint Surg Am; J Bone Joint Surg Br; J Foot Ankle Surg; J Orthop Trauma; J Trauma; Orthopedics) from AMEDEO.
We checked reference lists of all identified articles and reviews.
No language restriction was applied.
The search concluded in April 2012.
Data collection and analysis
Selection of studies
All identified trials were independently assessed for inclusion by both review authors using the above criteria.
Data extraction and management
Data were independently extracted by both review authors using a pre‐derived data extraction form and entered into RevMan. Trialists were contacted for further details of their trials.
Assessment of risk of bias in included studies
Methodological quality and risk of bias was independently assessed, without masking of the source and authorship of the trial reports, by both review authors. Any disagreement was resolved by discussion. For our last update (Handoll 2009), we had continued to use our subject‐specific modification of the former generic evaluation tool developed by the Cochrane Bone, Joint and Muscle Trauma Group. We had modified this by replacing the scores 2, 1, 0 respectively by Y (yes, criterion satisfied), ? (unclear or criterion partially satisfied), and N (no, criterion not satisfied). Table 4 shows the grading scheme based on 11 aspects of trial validity, plus brief notes of coding guidelines including the specific scores for items 9, 10 and 11 for the outcome of fracture non‐union. Additionally, we independently assessed risk of bias using the tool outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). This tool incorporates assessment of randomisation (sequence generation and allocation concealment), blinding (of participants, treatment providers and outcome assessors), completeness of outcome data, selection of outcomes reported and other sources of bias. We considered patient‐rated and clinician‐rated outcomes separately in our assessment of blinding and completeness of outcome data. We assessed two additional sources of bias: selection bias resulting from imbalances in key baseline characteristics (age, sex, fracture location, pattern and displacement, and associated soft tissue); and performance bias resulting from lack of comparability in the experience of care providers and provision of treatment interventions such as advice on activity, exercises undertaken, timing of intervention.
1. Methodological quality assessment scheme.
| Items | Grades | Notes |
| 1. Was the assigned treatment adequately concealed prior to allocation? | Y = method did not allow disclosure of assignment. ? = small but possible chance of disclosure of assignment or unclear. N = quasi‐randomised or open list/tables. | Cochrane code: Clearly yes = A; Not sure = B; Clearly no = C |
| 2. Were the outcomes of participants who withdrew described and included in the analysis (intention to treat)? | Y = withdrawals well described and accounted for in analysis. ? = withdrawals described and analysis not possible. N = no mention, inadequate mention, or obvious differences and no adjustment. | |
| 3. Were the outcome assessors blinded to treatment status? | Y = effective action taken to blind assessors. ? = small or moderate chance of unblinding of assessors. N = not mentioned or not possible. | |
| 4. Were the treatment and control group comparable at entry? | Y = good comparability of groups. ? = confounding small; mentioned. N = large potential for confounding, or not discussed. | The principle confounders were considered to be: age, sex, fracture location, pattern and displacement, and associated soft tissue injury. |
| 5. Were the participants blind to assignment status after allocation? | Y = effective action taken to blind participants. ? = small or moderate chance of unblinding of participants. N = not possible, or not mentioned (unless double‐blind), or possible but not done. | |
| 6. Were the treatment providers blind to assignment status? | Y = effective action taken to blind treatment providers. ? = small or moderate chance of unblinding of treatment providers. N = not possible, or not mentioned (unless double‐blind), or possible but not done. | |
| 7. Were care programmes, other than the trial options, identical? | Y = care programmes clearly identical. ? = clear but trivial differences. N = not mentioned or clear and important differences in care programmes. | Examples of clinically important differences in other interventions which could act as active measures for treatment of ulna fractures were considered to be: advice on activity, exercises undertaken, timing of intervention etc. |
| 8. Were the inclusion and exclusion criteria clearly defined? | Y = clearly defined. ? = inadequately defined. N = not defined. | |
| 9. Were the outcome measures used clearly defined? (by outcome measure) | Y = clearly defined. ? = inadequately defined. N = not defined. | For fracture non‐union: Was the algorithm for detection clearly described? |
| 10. Were diagnostic tests used in outcome assessment clinically useful? (by outcome) | Y = optimal. N = adequate. ? = not defined, not adequate. | For fracture union (non‐union): 2 = full bridging of external callus determined radiographically, and no pain on forearm movement. 1 = as above but no associated test for pain. 0 = no mention of criteria. |
| 11. Was the duration of surveillance clinically appropriate? (by outcome measure) | Y = optimal. ? = adequate. N = not defined, not adequate. | For fracture union (non‐union): 2 = 26 weeks or more post injury. 1 = 10‐26 weeks. 0 = under 10 weeks. |
Data synthesis
Where available, discrete outcome data were tested for statistical significance using risk ratios and 95% confidence intervals. No data pooling was appropriate and no sensitivity or subgroup analyses were undertaken.
Results
Description of studies
Results of the search
For this update (search completed April 2012), we screened a total of 69 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (0 records); Cochrane Central Register of Controlled Trials (19), MEDLINE (12), EMBASE (16), CINAHL (13), the WHO International Clinical Trials Registry Platform (8) and Current Controlled Trials (1). We also identified one potentially eligible study from the American Orthopaedic Trauma Association conference proceedings.
The updating of the search from December 2008 to April 2012 resulted in the identification of one ongoing trial (NCT01123447) and one study reported in a conference abstract (Coulibaly 2010), which was excluded.
Overall, there are now four included trials, eight excluded studies and one ongoing trial.
Table 5 is a compilation of our reports of the products of the search strategies and study selection decisions from the previous nine versions of the review.
2. History of search results and study selection decisions.
| Version | Date searched up to | Report |
| 1st version Issue 3, 1998 | July 1997 | "The specific MEDLINE search, run from 1976 to 1997, in conjunction with the first two levels of the optimal RCT specific search (see 'Search strategy for identification of studies') produced 32 reports of which 13 focused on the management of isolated ulnar fractures, and only two of which were controlled studies and put forward for inclusion. The EMBASE search run from 1981 to 1997 produced 26 studies, of which seven focused on the management of isolated fractures of the ulna, but as none of these were controlled, none were put forward for inclusion. A further two comparative studies (Labbe 1996; Skinner 1989), both published as abstracts, were identified but were excluded since they were not randomised or quasi‐randomised trials (see the 'Characteristics of excluded studies'). In their recent response stating that Labbe 1996 was a retrospective study, the trialists added that they were working on an randomised controlled trial investigating the same comparison (percutaneous intramedullary nailing versus plate fixation). A request for further details of this trial will be sent." |
| 2nd version Issue 2, 2000 | August 1999 | "There was no response from Dr Labbe to our request sent September 1998 for further details on the randomised controlled trial which he mentioned in his first response. Neither were there details given in the full report of Labbe 1996 published in 1998 (see Footnote). Correspondence in October 1998 with Dr Lisa Wood, then an orthopaedic registrar based in the Princess Margaret Hospital, Swindon, UK, alerted one of the review authors, Helen Handoll, to the possibility that a comparative study by Goel et al (Goel 1991) could be a randomised trial. However, since there was no response from the trialists to our inquiries, we have placed this study in the excluded studies category." |
| 3rd version Issue 2, 2001 | December 2000 | "The newly identified trial (Collinge 2000), located via handsearching, involved a randomised comparison of open reduction and plating with intramedullary nailing in 36 patients with 37 diaphyseal forearm fractures. Separate data were not presented for the six patients (three in each group) with only an ulnar fracture. Some of these may have been among the 10 patients who were not included in the results. We considered that the sample size was too small to pursue the data for these patients and thus have excluded this trial." |
| 4th version Issue 2, 2002 | November 2001 | "The updating of the search strategy to November 2001 resulted in the identification of no new studies." |
| 5th version Issue 2, 2003 | November 2002 | "The updating of the search strategy from November 2001 to November 2002 resulted in the identification of three new studies. Two of these, published in German, were located via CENTRAL and the other via MEDLINE. Upon obtaining translation or through enquiry with the trial investigator, all three were excluded for reasons given in the 'Characteristics of excluded studies' table." |
| 6th version Issue 2, 2004 | December 2003 | "The updating of the search strategy from November 2002 to December 2003 resulted in the identification of one new study, which compared two types of plates used for the surgical fixation of forearm diaphyseal (shaft) fractures (Leung 2003). This study was included upon obtaining separate data for patients with isolated ulnar fractures." |
| 7th version Issue 2, 2005 | January 2005 | "The updating of the search strategy from December 2003 to January 2005 resulted in the identification of a letter and reply (Rajasekhar 2004) regarding one of the included trials (Leung 2003). We found no new studies." |
| 8th version Issue 1, 2007 | September 2006 | "The updating of the search from January 2005 to September 2006 resulted in the identification of no new studies." |
| 9th version Issue 3, 2009 | December 2008 | "The updating of the search from September 2006 to December 2008 resulted in the identification of one new trial (Van Leemput 2007)." |
Labbe JL, Peres O, Leclair O, Goulon R, Bertrou V, Saintlanne S. La fracture isolee de la diaphyse ulnaire, de l'osteosynthese par plaque a l'embrochage centro‐medullaire [Fixation of isolated ulnar shaft fracture by open reduction and internal fixation with plate or percutaneous intramedullary nailing]. Revue de Chirurgie Orthopedique et Reparatrice de l'Appareil Moteur 1998;84(6):515‐22.
Included studies
Four trials (Atkin 1995; Gebuhr 1992; Leung 2003; Van Leemput 2007), involving a total of 237 participants, are included in this review. The majority of the participants were male in two trials (Atkin 1995: 71%; Leung 2003: 90%), but not in Gebuhr 1992 (49%) or Van Leemput 2007 (42%). The potential bimodal distribution of age for these fractures has been described in the 'Background' and the age range of the pooled population for this review is 12 to 85 years of age. It is very unlikely that there were more than a very few children in the two trials (Gebuhr 1992; Leung 2003), but there were no data to confirm this.
Three trials (Atkin 1995; Gebuhr 1992; Van Leemput 2007) included people with closed isolated fractures of the mid and distal ulnar shaft and excluded those of the proximal shaft. Three of the 29 isolated ulnar shaft fractures in Leung 2003 were open fractures.
Three trials compared conservative treatment options. Atkin 1995 compared three treatment groups: Ace wrap elastic bandages, short arm plaster casts and long arm plaster casts. Gebuhr 1992 compared the use of short arm pre‐fabricated functional braces and long arm plaster casts. Van Leemput 2007 compared three treatment groups: immediate mobilisation, below elbow (short arm) plaster casts and above elbow (long arm) plaster casts.
We failed to locate any completed randomised trials comparing surgical with conservative treatment.
Leung 2003 compared two types of plates used in open reduction and internal fixation of fractures: the point contact fixator (Pc‐Fix) versus the limited contact dynamic compression plate (LC‐DCP).
Further details of these four trials are given in the Characteristics of included studies.
Excluded studies
Details of the reasons for excluding eight other studies are given in the Characteristics of excluded studies.
Ongoing studies
Details of the ongoing study (NCT01123447) are provided in the Characteristics of ongoing studies.
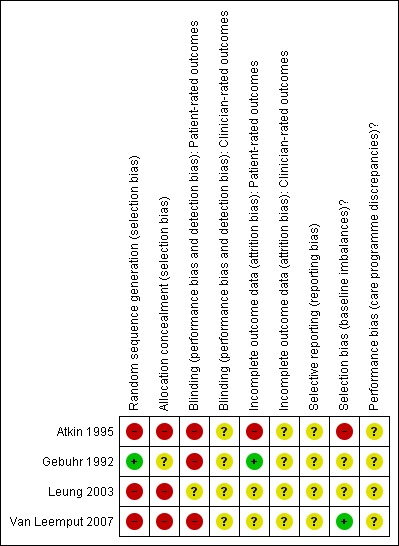
Risk of bias in included studies
All four trials were methodologically flawed and were at risk of serious bias. Table 6 shows the grades obtained by each of the four trials for the 11 items defined in Table 4. As well as the 'Risk of bias' table entries for individual trials in the Characteristics of included studies, an overall summary is available in Figure 1.
3. Methodological quality assessment results for individual trials.
| Items / Trials | Atkin 1995 | Gebuhr 1992 | Leung 2003 | Van Leemput 2007 |
| 1. Allocation concealment | N | ? | N | N |
| 2. Intention‐to‐treat analysis | N | N | ? | N |
| 3. Assessor blinding | N | N | N | N |
| 4. Baseline characteristics comparability | N | N | ? | Y |
| 5. Participant blinding | N | N | N | N |
| 6. Treatment provider blinding | N | N | N | N |
| 7. Care programme comparability | N | N | ? | ? |
| 8. Inclusion and exclusion criteria | ? | Y | Y | Y |
| 9. Well defined outcome measures | Y | Y | Y | Y |
| 10. Clinically useful diagnostic tests | Y | Y | Y | ? |
| 11. Adequate duration of follow‐up | ? | ? | Y | ? |
Y = yes; ? = partial/unknown; N = no
* Assessments for items 9, 10 and 11 relate to the outcome of fracture non‐union.
1.
Risk of bias summary
Allocation
Neither Atkin 1995 nor Gebuhr 1992 reported the method of randomisation adequately, but Atkin 1995 was quasi‐randomised being based on the order of hospital admission. In response to a request for further information, Gebuhr 1992 reported using a computer program to generate random numbers but gave no assurance of allocation concealment. Leung 2003 changed their method from open randomisation lists to "strict" alternation around a third way through the trial; allocation was clearly not concealed at any stage of this trial. Treament allocation in Van Leemput 2007 was also not concealed; even if "strictly randomised" according to the date of presentation at the hospital. We judged there was a high risk of selection bias in all three quasi‐randomised trials (Atkin 1995; Leung 2003; Van Leemput 2007).
Blinding
No mention of assessor blinding was made in any of the trial reports; there was, however, independent assessment of anatomical reduction in Leung 2003. Aside from the comparison of surgical devices in Leung 2003, we decided that there was a risk of bias for patient‐rated outcomes for comparisons of conservative interventions but that clinician‐rated outcomes, based on objective criteria, were probably less susceptible to bias.
Incomplete outcome data
The loss to follow‐up (48%) was severe in Atkin 1995. Though the trialists acknowledged this and stated that last attended clinic visits and X‐rays before loss to follow‐up revealed that the outcomes for these trial participants were not significantly different to those followed up to fracture union, the problem of bias remains. Atkin 1995 considered such large losses were a function of the indigent population and often violent cause of this injury. Gebuhr 1992 lost seven people (15%) to follow‐up. There appeared to be no loss to follow‐up at 12 months in Leung 2003; though losses did occur subsequently. Similarly, there appeared to be no loss to follow‐up from Van Leemput 2007, but this has not been confirmed.
Selective reporting
While there was insufficient information to permit judgement, we considered that this was not an issue for any of the included trials, all of which report on a typical set of outcomes for these fractures.
Other potential sources of bias
Selection bias
Incomplete information was provided for baseline characteristics in both Atkin 1995 and Gebuhr 1992. However, in both these trials, the distribution of fracture types (location, displacement and pattern) for those followed up was comparable between treatment groups. Aside from open and closed fractures, no specific information on fracture type was provided by Leung 2003; however, other patient characteristics were roughly comparable in the two groups in this trial. Assuming no loss to follow‐up in Van Leemput 2007, baseline characteristics were similar in the three groups and thus this trial was probably free from confounding due to baseline differences.
Performance bias
There were insufficient details of the care provided to trial participants other than the trial interventions. Differences between the trial groups in the scheduling of follow‐up could affect trial outcome but we decided the risk of performance bias was 'unclear' for all four trials.
Detection bias
While not explicitly assessed via the 'Risk of bias' tool, ascertainment bias could result from difference in the follow‐up assessments for the trial groups (this could occur through lack of active and systematic follow‐up).
There was clearly active surveillance in Leung 2003 and Van Leemput 2007. While surveillance also appeared active for Atkin 1995 and Gebuhr 1992, neither reported a satisfactory systematic approach with set follow‐up times. Atkin 1995 did not provide details of the frequency or timing of follow‐up visits. Trial participants were seen at two to four week intervals in Gebuhr 1992; this variation in the times of assessment could potentially distort the findings of this trial.
In Atkin 1995 and Gebuhr 1992, the length of follow‐up was based on the time for radiographically evident union and lack of pain. In Atkin 1995, the mean follow‐up time was 20 weeks, whereas 20 weeks was the maximum follow‐up in Gebuhr 1992. After a set follow up of 12 months in Leung 2003, the final follow‐up ranged from 14 to 40 months and was partly dependent on whether the implant was removed. Follow‐up in Van Leemput 2007 was 12 weeks.
Effects of interventions
The outcomes reported by the four studies are listed in the Characteristics of included studies. The small number of people involved, inadequate data and problems resulting from large losses to follow‐up meant that graphical presentation of the trial results was considered inappropriate for Atkin 1995 and Gebuhr 1992. However, where possible the data were tested for statistical significance, partly to check the claims within the trial reports. The data for Leung 2003 are presented, in part because these would not be available otherwise. Few data were available for presentation in Van Leemput 2007, which is reported under two comparisons below: immediate mobilisation versus plaster cast immobilisation; and short arm plaster cast versus long arm plaster cast immobilisation.
Immediate mobilisation versus plaster cast immobilisation
Van Leemput 2007 found no differences in outcome between immediate mobilisation (compression bandage supplied) versus cast immobilisation (short arm or long arm plaster casts) in adults with minimally displaced isolated ulnar shaft fractures. Specifically, there was no difference in the incidence of delayed union (Analysis 1.1. 4/34 versus 9/68; risk ratio (RR) 0.89, 95% confidence interval (CI) 0.29 to 2.68); nor in the time to union in the remaining trial participants (10.4 weeks versus 10.6 weeks). There were also no differences between the two groups in mean pain scores (8.62 versus 8.67; scale 0 = worst pain, 10 = no pain); mean loss of rotation arc (5.53° versus 6.29°) and mean loss of flexion/extension arc (4.33° versus 4.58°).
1.1. Analysis.
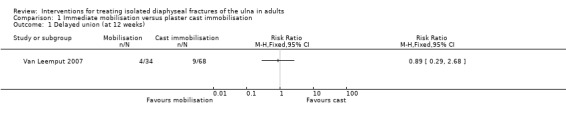
Comparison 1 Immediate mobilisation versus plaster cast immobilisation, Outcome 1 Delayed union (at 12 weeks).
Short arm pre‐fabricated functional brace versus long arm plaster cast
Gebuhr 1992 reported a median time of fracture healing of 56 days for the pre‐fabricated functional brace group compared with 50 days for the long arm plaster cast group. This small difference was reported as not being statistically different and all fractures had healed by 20 weeks. Data for range of motion outcomes were not available for analysis but the wrist extension/flexion results for the brace group were reported to be significantly better (P < 0.004). Significantly more people returned to work while using the brace than the cast (non return to work: 1/14 versus 12/13; RR 0.08, 95% CI 0.01 to 0.51). Patient satisfaction with the device was also significantly greater in the brace group: an excellent grade being given for 14 out of 20 in the brace group compared with only one out of 19 in the cast group.
Short arm plaster cast versus long arm plaster cast immobilisation
Atkin 1995 reported a mean fracture union time of 7.9 weeks (14 people) for the short arm plaster cast group compared with 7.2 weeks (8 people) for the long arm cast group. A "significant" loss of motion was reported in two people in the short arm cast group. No or inadequate data were available for range of motion or anatomical outcomes. Patient assessment based on interviews of pain, cosmetic deformity and overall evaluation were not significantly different in either group (pain: 6/13 versus 2/5; cosmetic deformity: 2/11 versus 0/5; poor or fair result: 2/10 versus 1/5). Three people removed their cast prematurely (before union was confirmed) in the short arm cast but none in the long arm cast. Two people in each group were unable to return to their previous employment (2/14 versus 2/9; RR 0.64, 95% CI 0.11 to 3.78).
Van Leemput 2007 found no differences in outcome between short arm plaster cast immobilisation versus long arm plaster cast immobilisation in adults with minimally displaced isolated ulnar shaft fractures. Specifically, there was no difference in the incidence of delayed union (Analysis 2.1 5/36 versus 4/32; RR 1.11, 95% CI 0.33 to 3.78); nor in the time to union in the remaining trial participants (10.5 weeks versus 10.7 weeks). There were also no differences between the two groups in mean pain scores (8.69 versus 8.62; scale 0 = worst pain, 10 = no pain); mean loss of rotation arc (5.86° versus 6.66°) and mean loss of flexion/extension arc (4.50° versus 4.68°).
2.1. Analysis.
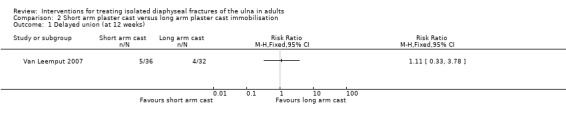
Comparison 2 Short arm plaster cast versus long arm plaster cast immobilisation, Outcome 1 Delayed union (at 12 weeks).
Ace Wrap elastic bandage
Six out of the eight people allocated Ace wrap and followed up in Atkin 1995, changed to another treatment due to pain. Three were given short arm casts and the other three long arm casts. Although intention‐to‐treat results were provided for this group, this failure of treatment is the primary outcome.
Point contact fixator (PC‐Fix) versus the limited contact dynamic compression plate (LC‐DCP)
Twenty‐nine out of the 93 people with forearm fractures recruited into Leung 2003 had isolated fracture of the ulna. The two surgeons performing the operations, both of whom were experienced in using both implants, reported similar amounts of ease or difficulty with both implants. The mean operating time was lower in the PC‐Fix group (64 versus 78 minutes); this parallels the results for all forearm fractures (78 versus 92 minutes): the latter difference was reported not to be statistically significant. All fractures united but one person in the PC‐Fix group and two people in the LC‐DCP group had delayed union; all three had had closed fractures (Analysis 3.1). Precise anatomical reduction of fracture fragments was not achieved in 10 PC‐Fix group participants and five LC‐DCP group participants (Analysis 3.2). Two people in the PC‐Fix group had pain at follow‐up. All participants had "full" range of motion; defined as less than 10% loss of dorsiflexion‐palmar flexion of the wrist and less than 25% loss of pronation‐supination. Three participants had complications: a deep infection occurred in one person in the LC‐DCP group (implant removal was not required); one person in the PC‐Fix group had a superficial infection; and one person in the LC‐DCP group developed compartment syndrome (Analysis 3.3). There was no nerve injury and none of the people who had had their implant removed at a later date sustained a refracture. As can be seen from the analyses, none of the differences reached statistical significance.
3.1. Analysis.
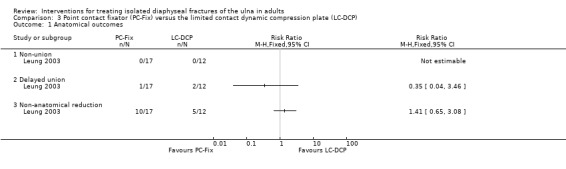
Comparison 3 Point contact fixator (PC‐Fix) versus the limited contact dynamic compression plate (LC‐DCP), Outcome 1 Anatomical outcomes.
3.2. Analysis.
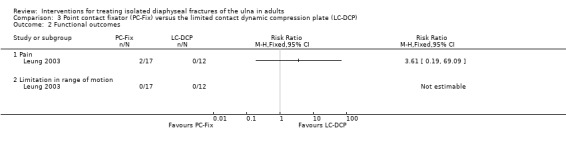
Comparison 3 Point contact fixator (PC‐Fix) versus the limited contact dynamic compression plate (LC‐DCP), Outcome 2 Functional outcomes.
3.3. Analysis.
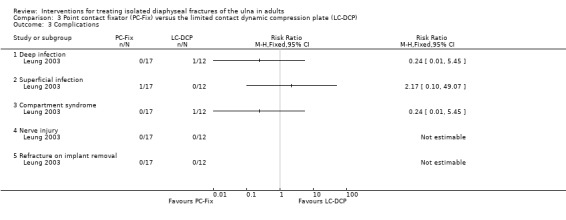
Comparison 3 Point contact fixator (PC‐Fix) versus the limited contact dynamic compression plate (LC‐DCP), Outcome 3 Complications.
Discussion
Summary of main results
Although the absence of strictly comparable interventions and fracture types precluded pooling of data, we found no evidence that cast immobilisation of the elbow offers a short‐term advantage in respect of pain relief or fracture union compared with the use of casts or braces which immobilise only the forearm. Participants allocated to a functional forearm brace in Gebuhr 1992 returned to work significantly sooner than those wearing an above elbow cast. The efficacy of an elastic forearm wrap rather than forearm cast immobilisation remains unclear. We found no completed randomised trial comparing surgical versus conservative treatment. Where surgical fixation is considered appropriate, there is no evidence to support any particular implant type.
Overall completeness and applicability of evidence
The most common mechanism for these fractures is a direct hit on the forearm and these fractures are often sustained when the forearm is raised to fend off blows or when trying to protect the head. Forty‐six per cent of the injuries in Gebuhr 1992 were attributed to violence and the large loss to follow‐up in Atkin 1995 was considered to be a function of the often violent cause of this injury. However, an osteoporotic basis for those fractures that result from a simple fall in older females is also indicated in McQueen 2000. The majority of fractures in Leung 2003 and Van Leemput 2007 were reported as resulting from low trauma, the latter trial attributing all fractures as resulting from a direct hit on the forearm. Despite the differences in location and clear variation in the populations of the included trials, their results are likely to apply more generally.
However, in all three conservative treatment trials, interventions were poorly defined and the absence of strictly comparable interventions and fracture types precluded pooling of data. Two trials, Atkin 1995 and Van Leemput 2007, reported pain outcomes when comparing a forearm elastic wrap (or compression bandage) with a cast, and came to different conclusions. In Atkin 1995, the majority of participants allocated to an Ace wrap requested a change to another treatment because of pain. In Van Leemput 2007, pain scores showed no significant difference between groups. It is unclear why this should be, but it may reflect the impact of differences in the context in which each study was conducted (Hawe 2004). More data on this comparison would be useful.
While we have not found any randomised trial comparing surgical versus conservative treatment, and thus are unable to define when surgical intervention is indicated, we were able to include a trial comparing two types of plate fixation. Leung 2003, however, was underpowered and the results of both the main trial and those of the subgroup of isolated ulnar shaft fractures, presented in this review, do not reveal statistically significant differences between the two implants. The two plates, both made of titanium, under comparison in this trial are manufactured by the same company and represent interim stages in a sequence of technological developments by the associated AO Research Institute (Perren 1995; Perren 2003). Further developments in plating technology may preclude the use of these two specific plates in the future (Smith 2004), a point discussed in subsequent correspondence on this trial (Rajasekhar 2004).
Quality of the evidence
All four trials included in this review had methodological weaknesses that makes them highly susceptible to bias. Three were quasi‐randomised, and there was no assurance of allocation concealment for the only trial that had adequate sequence generation. There was no blinding of outcome assessment, and in Atkin 1995, almost half the participants were lost to follow‐up. The absence of information on loss to follow‐up in Van Leemput 2007 is a concern.
Potential biases in the review process
We think that it is unlikely that the review process itself has introduced bias. We did not conduct a meta‐analysis, and have reported the potential biases associated with the studies themselves. We believe that publication bias is unlikely; the search was comprehensive, and included the bibliography of a large narrative review (Mackay 2000).
Agreements and disagreements with other studies or reviews
We found two relevant reviews. Mackay 2000 provided an useful compilation of the literature and summary of the treatment methods used in studies from the 1950s onwards, and included data from 33 mainly retrospective case reporting the outcomes from 1876 people. Methods used in Mackay 2000 for combining the results of groups of people who were given the same treatment were not optimal; for instance, confidence limits were not provided for estimated effects. In addition, although study design and some aspects of study methodology were noted in their appraisal of individual studies, the potential for systematic bias arising from flawed study methodology was not explored or discussed. A formal critique of Mackay 2000 may be found in DARE (Database of Abstracts of Reviews of Effects) (DARE 2006). The quantitative results of Mackay 2000 should be viewed with caution and should not be taken as the basis for comparisons of effectiveness of the various treatments covered in the review.
A more recent review (Bhandari 2004), which reviewed evidence from randomised studies only, found the same three randomised trials published before 2004 as included in the concurrent version of this review, and reached similar conclusions.
Authors' conclusions
Implications for practice.
Overall, there is insufficient evidence from randomised controlled trials to determine which method of treatment is the most appropriate for the treatment of isolated fractures of the ulnar shaft in adults. There is, however, weak evidence that in people with minimally displaced isolated fracture of the ulna, cast immobilisation of the elbow may offer no short‐term advantage in respect of pain relief or fracture union, and may be associated with longer delay in return to work, when compared with the use of a cast or brace that immobilises only the forearm.
Implications for research.
Though isolated ulnar shaft fractures are comparatively uncommon there remains a need to establish the best methods to manage these fractures, which are often associated with a high rate of complications and, for some people, significant life changes. The limited information on incidence, and choice, cost, and outcome of treatment, hampers an appraisal of what priority needs to be given to research in this area. However, given that most fractures are treated conservatively and the availability of only weak evidence, the use of splintage and the inclusion or not of the elbow in splintage for minimally displaced fractures appear to be suitable candidates for future randomised trials. All future research should meet robust contemporary standards of design conduct, and reporting, including the use of randomisation methods involving stratification, to ensure baseline equivalence between treatment groups in respect of fracture pattern, location of the fracture, and bone quality.
What's new
| Date | Event | Description |
|---|---|---|
| 26 April 2012 | New search has been performed | For this update (published in Issue 6, 2012), the search for trials was updated to April 2012. There were no new included trials but one ongoing trial comparing surgery with conservative treatment was identified. A conference abstract reporting a retrospective comparison was excluded. |
| 26 April 2012 | New citation required but conclusions have not changed | For clarification purposes, the title has been changed from 'Interventions for isolated diaphyseal fractures of the ulna in adults'. |
History
Protocol first published: Issue 4, 1997 Review first published: Issue 3, 1998
| Date | Event | Description |
|---|---|---|
| 6 May 2009 | New search has been performed | In this issue (Issue 3, 2009) the search for trials was updated to December 2008. One new trial evaluating conservative treatment options was identified and included. Outcomes were grouped into primary and secondary outcomes. Risk of bias was assessed. There were changes to the conclusions of the review. |
| 6 May 2009 | New citation required and conclusions have changed | Some changes were made to the conclusions as a result of the addition of evidence from a newly included trial. |
| 12 January 2009 | New search has been performed | Substantive changes made (January 2009) for Issue 3, 2009 1. Literature search extended to December 2008. 2. Addition of new included conservative treatment trial. 3. Restructuring of outcomes into primary and secondary outcomes 4. Risk of bias implemented. |
| 5 August 2008 | Amended | Converted to new review format. |
| 3 October 2006 | New search has been performed | In Issue 1, 2007, the search for trials was updated to September 2006. No new trials or associated data were identified. The 'Synopsis' was amended to a 'Plain language summary'. The 'Objectives' were reworded but remained as before. Methodological quality scores of individual criteria were no longer summed. There was no change to the conclusions of the review. For details of all updates, please see 'Published notes'. |
| 2 October 2006 | New search has been performed | Non substantive changes made (October 2006) for Issue 1, 2007 1. Literature search extended to September 2006. 2. Synopsis modified to a Plain language summary. 3. Objectives were reworded. 4. Overall methodological quality scores removed. |
| 10 January 2005 | New search has been performed | Non substantive changes made (January 2005) for Issue 2, 2005. 1. Literature search extended to January 2005. 2. Correspondence on one trial added and some other changes made to conform to Cochrane Style Guide. |
| 5 January 2004 | New search has been performed | Substantive changes made (January 2004) for Issue 2, 2004 1. Literature search extended to December 2003. 2. Addition of new included surgical trial evaluating two types of plates. |
| 11 November 2002 | New search has been performed | Non substantive changes made (November 2002) for Issue 2, 2003. 1. Literature search extended to November 2002. 2. Three more excluded studies. |
| 5 November 2001 | New search has been performed | Non substantive changes made (November 2001) for Issue 2, 2002. 1. Literature search extended to November 2001. 2. Some epidemiological information was added. |
| 11 December 2000 | New search has been performed | Non substantive changes made (December 2000) for Issue 2, 2001. 1. Literature search extended to December 2000. 2. One more excluded study. 3. Active follow‐up rated in methodological quality. 4. Relative risks presented instead of Peto odds ratios. 5. Some comments made on a recently published systematic review. |
| 3 January 2000 | New search has been performed | Non substantive changes made (January 2000) for Issue 2, 2000. 1. Literature search extended to August 1999. 2. Synopsis added. 3. One more excluded study. 4. Scores for individual items of the methodological quality assessment scheme changed from 3,2,1 to 2,1,0. |
Acknowledgements
We would like to express our thanks to Mr Amar Rangan for his early encouragement and Prof William Gillespie for his comments on an earlier draft. We thank Mr Agop der Tavitian for his contribution to the first version of the review. We would also like to thank the following for their useful comments at editorial review of one or more versions of this review: Prof William Gillespie, Assoc Prof Peter Herbison, Mr Geoffrey Hooper, Dr Vicki Livingstone, Prof Rajan Madhok, Prof Gordon Murray, Prof Marc Swiontkowski and Dr Janet Wale. We thank the following for their help during the editorial review of successive updates: Dr Catherine Deering, Dr Joanne Elliott, Mrs Lindsey Elstub, Mrs Lesley Gillespie, Prof William Gillespie, Ms Leeann Morton and Ms Kate Rowntree.
We thank Mrs Sonia Stewart for translating two articles.
We are grateful to Jo Kamen for providing separate data for isolated ulnar fractures for Leung 2003; and to Mr Tom Van Leemput for providing information on Van Leemput 2007.
Dr Helen Handoll's work on the first two versions of the review was supported by the Chief Scientist Office, Department of Health, The Scottish Office, UK.
Appendices
Appendix 1. Search strategies (April 2012)
MEDLINE (OVID WEB)
Database: Ovid MEDLINE(R) <1946 to April Week 1 2012>, Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations <April 13, 2012>, Ovid MEDLINE(R) Daily Update <April 13, 2012>
1. Ulna/ (5083) 2. (ulna or ulnar).tw. (16670) 3. 1 or 2 (18916) 4. Fractures, Compression/ or Fractures, Ununited/ or Fractures, Cartilage/ or Fractures, Malunited/ or Fractures, Spontaneous/ or Fractures, Bone/ or Fractures, Open/ or Fractures, Closed/ or Fractures, Stress/ or Fractures, Comminuted/ (63419) 5. fracture$.tw. (151560) 6. 4 or 5 (170179) 7. 3 and 6 (3854) 8. Ulna Fractures/ (2379) 9. 7 or 8 (5299) 10. (shaft or diaphys$ or nightstick).tw. (19159) 11. 9 and 10 (662) 12. randomized controlled trial.pt. (325110) 13. controlled clinical trial.pt. (83947) 14. randomized.ab. (240446) 15. placebo.ab. (135056) 16. drug therapy.fs. (1521978) 17. randomly.ab. (176791) 18. trial.ab. (249112) 19. groups.ab. (1156060) 20. or/12‐19 (2913061) 21. exp animals/ not humans.sh. (3700604) 22. 20 not 21 (2486651) 23. 11 and 22 (52) 24. limit 23 to ed=20081201‐20121231 (12)
EMBASE (OVID WEB)
Embase <1980 to 2012 Week 15>
1. ulna/ (5082) 2. (ulna or ulnar).tw. (18405) 3. 1 or 2 (20243) 4. fracture/ (51767) 5. fracture$.tw. (172500) 6. 4 or 5 (189127) 7. 3 and 6 (3862) 8. ulna fracture/ (2190) 9. 7 or 8 (5112) 10. (shaft or diaphys$ or nightstick).tw. (21624) 11. 9 and 10 (642) 12. Randomized controlled trial/ (319715) 13. Clinical trial/ (863983) 14. controlled clinical trial/ (387873) 15. Randomization/ (57791) 16. single blind procedure/ (15702) 17. double blind procedure/ (108172) 18. crossover procedure/ (33524) 19. placebo/ (196187) 20. prospective study/ (200629) 21. ((clinical or controlled or comparative or placebo or prospective$ or randomi#ed) adj3 (trial or study)).tw. (615786) 22. (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. (149723) 23. ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. (142000) 24. (cross?over$ or (cross adj1 over$)).tw. (60500) 25. ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. (186385) 26. RCT.tw. (8967) 27. or/12‐26 (1654663) 28. Case Study/ or Abstract Report/ or Letter/ (842421) 29. 27 not 28 (1619614) 30. 11 and 29 (57) 31. (2008$ or 2009$ or 2010$ or 2011$ or 2012$).em. (4695270) 32. 30 and 31 (16)
CINAHL EBSCO
CINAHL search update 16 April 2012
1. (MH "Ulna") (338) 2. TX ulna OR TX ulnar (2277) 3. S1 or S2 (2277) 4. (MH "Fractures") (9257) 5. Fracture* (34335) 6. S4 or S5 (34335) 7. S3 and S6 (748) 8. (MH "Ulna Fractures") (323) 9. S7 or S8 (748) 10. TX shaft OR TX diaphys* OR TX nightstick (1635) 11. S9 and S10 (79) 12. (MH "Clinical Trials+") (139513) 13. (MH "Evaluation Research+") (18165) 14. (MH "Comparative Studies") (66011) 15. (MH "Crossover Design") (9090) 16. PT Clinical Trial (71819) 17. (MH "Random Assignment") (32070) 18. S12 or S13 or S14 or S15 or S16 or S17 (226747) 19. TX ((clinical or controlled or comparative or placebo or prospective or randomi?ed) and (trial or study)) (389667) 20. TX (random* and (allocat* or allot* or assign* or basis* or divid* or order*)) (55845) 21. TX ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)) (608576) 22. TX ( crossover* or 'cross over' ) or TX cross n1 over (11455) 23. TX ((allocat* or allot* or assign* or divid*) and (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)) (69824) 24. S19 or S20 or S21 or S22 or S23 (925151) 25. S18 or S24 (981806) 26. S11 and S25 (29) 27. EM 2008 OR EM 2009 OR EM 2010 OR EM 2011 OR EM 2012 (1533737) 28. S26 and S27 (13)
CENTRAL (Wiley InterScience)
The Cochrane Library Issue 3, 2012
#1 MeSH descriptor Ulna, this term only (33) #2 (ulna or ulnar) (959) #3 (#1 OR #2) (959) #4 MeSH descriptor Fractures, Bone, this term only (985) #5 MeSH descriptor Fracture Fixation explode all trees (958) #6 MeSH descriptor Fracture Healing, this term only (311) #7 (fracture) (7936) #8 (#4 OR #5 OR #6 OR #7) (7940) #9 (#3 AND #8) (154) #10 MeSH descriptor Ulna Fractures explode all trees (33) #11 (#9 OR #10) (154) #12 (shaft or diaphys$ or nightstick) (540) #13 (#11 AND #12), from 2008 to 2012 (19)
Other searches
Current Controlled Trials (accessed April 2012) ‐ 1 entry
WHO International Clinical Trials Registry Platform (accessed April 2012) ‐ searched: ulna* and fracture* ‐ 8 entries
Journal of Bone and Joint Surgery ‐ British Volume and conference proceedings from 2006 onwards (26 April 2012). Searched using "randomised" and then checked through the 1782 citations using Find: "ulna" ‐ no results
Data and analyses
Comparison 1. Immediate mobilisation versus plaster cast immobilisation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Delayed union (at 12 weeks) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 2. Short arm plaster cast versus long arm plaster cast immobilisation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Delayed union (at 12 weeks) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3. Point contact fixator (PC‐Fix) versus the limited contact dynamic compression plate (LC‐DCP).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Anatomical outcomes | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Delayed union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Non‐anatomical reduction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Functional outcomes | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Pain | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Limitation in range of motion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Deep infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Superficial infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Compartment syndrome | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Nerve injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.5 Refracture on implant removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Atkin 1995.
| Methods | Randomisation by order of hospital admission Assessor blinding: not stated Intention‐to‐treat analysis: only for those followed up Loss to follow‐up: 29 (48%) | |
| Participants | Highland General Hospital, University of California, USA 60 participants. Of 31 analysed: 22 male (71%), mean age 35 years, range 19‐50 years. Transverse, oblique, comminuted, and displaced fractures included. Inclusion criteria: closed midshaft, or distal isolated ulnar fracture. Exclusion criteria: proximal ulnar fracture, distal radioulnar fracture. | |
| Interventions | No details of when treatment started. Infer that treatment ended when fracture union confirmed. 1. Ace Wrap ‐ elastic bandage 2. Short arm plaster cast 3. Long arm plaster cast Allocated: ?/?/? (numbers in each group not stated) Assessed: 8/14/9 (subjective results: 7/10/5) | |
| Outcomes | Length of follow‐up: until union (mean 20 weeks) Fracture union (radiographic and pain free) Treatment failure Patient evaluation: pain, cosmetic deformity, satisfaction. Range of motion (wrist, elbow, forearm) Anatomic: varus and volar/dorsal angulation Return to previous employment | |
| Notes | Large loss of follow‐up attributed to common violent origin of this fracture. Six participants did not tolerate Ace wrap due to pain: 3 were changed to short arm plaster casts and 3 to long arm plaster casts. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Based on order of hospital admission", thus quasi‐randomised. |
| Allocation concealment (selection bias) | High risk | Inadequate because "based on order of hospital admission". |
| Blinding (performance bias and detection bias) Patient‐rated outcomes | High risk | There was no report of blinding. |
| Blinding (performance bias and detection bias) Clinician‐rated outcomes | Unclear risk | There was no report of blinding. |
| Incomplete outcome data (attrition bias) Patient‐rated outcomes | High risk | Large loss to follow‐up: 29/60 (48%). Inadequate data available to examine effects. |
| Incomplete outcome data (attrition bias) Clinician‐rated outcomes | Unclear risk | Large loss to follow‐up: 29/60 (48%). Inadequate data available to examine effects. |
| Selective reporting (reporting bias) | Unclear risk | Reports on typical set of outcomes for these fractures. |
| Selection bias (baseline imbalances)? | High risk | Data not provided for whole study population. Some imbalances in patient characteristics of the 31 followed up (e.g. fracture type). |
| Performance bias (care programme discrepancies)? | Unclear risk | Insufficient information. |
Gebuhr 1992.
| Methods | Randomisation used random numbers generated from the 'Medstat' program Assessor blinding: not stated Intention‐to‐treat analysis: only for those followed up Loss to follow‐up: 7 (15%) | |
| Participants | University hospitals, Denmark 46 participants. Of 39 analysed: 19 male (49%), median age 44 years, range 12‐85 years. Transverse, oblique and comminuted fractures included. Inclusion criteria: closed midshaft or distal isolated ulnar fracture. Exclusion criteria: proximal ulnar fracture, Monteggia fracture dislocations | |
| Interventions | Interventions started after initial immobilisation in an above elbow cast aimed to relieve pain and allow swelling to subside. Interventions removed when healed. 1. Short arm pre‐fabricated functional brace 2. Long arm plaster cast Allocated: 23/23 Assessed: 20/19 | |
| Outcomes | Length of follow‐up: maximum 20 weeks Fracture union (radiographic and pain free) Patient evaluation: satisfaction, pain Range of motion (wrist, elbow, forearm: elbow extension/flexion, forearm pronation/supination and wrist extension/flexion) Anatomic: varus and volar/dorsal angulation Return to previous employment, use of device at work | |
| Notes | Letter from Gebuhr gave details of the method of randomisation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation "used random numbers generated from the 'Medstat' program". |
| Allocation concealment (selection bias) | Unclear risk | No confirmation of this: "allocated randomly". |
| Blinding (performance bias and detection bias) Patient‐rated outcomes | High risk | There was no report of blinding. |
| Blinding (performance bias and detection bias) Clinician‐rated outcomes | Unclear risk | There was no report of blinding. |
| Incomplete outcome data (attrition bias) Patient‐rated outcomes | Low risk | Moderate loss to follow‐up: 7/46 (15%). Six participants failed to attend follow‐up examinations but this is unlikely to affect results. |
| Incomplete outcome data (attrition bias) Clinician‐rated outcomes | Unclear risk | Moderate loss to follow‐up: 7/46 (15%). Treatment group of person with putative non‐union who had operation not known. |
| Selective reporting (reporting bias) | Unclear risk | Reports on typical set of outcomes for these fractures. |
| Selection bias (baseline imbalances)? | Unclear risk | Brace group were younger (mean age 42 versus 48 years) but otherwise characteristics of the participants included in the analyses of the two groups seemed comparable. However, data for 7 participants are missing. |
| Performance bias (care programme discrepancies)? | Unclear risk | Insufficient information ‐ initial treatment was the same and subsequent advice on activity seemed similar too. |
Leung 2003.
| Methods | Randomisation initially involved use of an open, predetermined randomisation chart and then was changed to "strict" alternation Assessor blinding: none; independent assessment of quality of reduction Intention‐to‐treat analysis: yes, though data from one participant who withdrew immediately post‐randomisation were excluded and the numbers of participants in each group at long‐term follow‐up were not reported Loss to follow‐up: 10 (11%) of 93 in trial. | |
| Participants | Queen Mary Hospital, University of Hong Kong, Hong Kong, China 29 participants (subgroup of 93 participants with forearm fractures): 26 male (90%), mean age 35 years, range 13‐79 years. Open (3) and closed fractures: (21); 72% from low energy trauma. Inclusion criteria: acute forearm shaft fracture in patients over 10 years old. Exclusion criteria: pathological fracture, rheumatoid arthritis, history of long‐term steroid therapy, judged unlikely to complete follow‐up, no consent. | |
| Interventions | No details of when surgery occurred except that it was performed after randomisation. All participants were admitted into hospital and received a single injection of antibiotic. Reduction mainly done via direct fracture manipulation ‐ a distraction device was used in some cases. Both implants were titanium. 1. Point contact fixator (PC‐Fix) ‐ screws lock into screw‐hole on plate and do not enter the cortical bone on the other side of the bone 2. Limited contact dynamic compression plate (LC‐DCP) ‐ screws cross through the bone to the other side from the plate and lock into bone rather than the plate Allocated: 17/12 Assessed: 17/12 (12 months) | |
| Outcomes | Length of follow‐up: (for whole trial population) mean 22 months (14‐40 months) but also 2, 4 and 12 months Fracture union (radiographic) Pain (with and without load bearing) Complications: infection, compartment syndrome, nerve injury (0), refracture on removal of implant (0), screw pull out (0) Range of motion (wrist and forearm) Anatomic reduction Length of operation Ease of fixation | |
| Notes | Separate data for participants with isolated ulnar fracture obtained from trial investigators. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "For the initial thirty‐two cases, an open, predetermined randomization chart was used. The chart was constructed of blocks containing four allocations. For the subsequent cases, the choice of fixation was determined in a strictly alternating fashion." Hence, quasi‐randomised. |
| Allocation concealment (selection bias) | High risk | As above: "open" list and then alternation. Hence no concealment of allocation. |
| Blinding (performance bias and detection bias) Patient‐rated outcomes | Unclear risk | No mention of blinding. |
| Blinding (performance bias and detection bias) Clinician‐rated outcomes | Unclear risk | No mention of blinding. Independent observer for judging anatomical reduction. |
| Incomplete outcome data (attrition bias) Patient‐rated outcomes | Unclear risk | Only pain assessed. Inadequate information but all participants appear to have been followed up. |
| Incomplete outcome data (attrition bias) Clinician‐rated outcomes | Unclear risk | Inadequate information but all participants appear to have been followed up |
| Selective reporting (reporting bias) | Unclear risk | Reports on typical set of outcomes for these fractures. |
| Selection bias (baseline imbalances)? | Unclear risk | Data provided for isolated ulnar fractures indicated a reasonable balance. |
| Performance bias (care programme discrepancies)? | Unclear risk | Incomplete information. Both surgeons were experienced with the devices. Slight difference in use of open reduction: 83% versus 93% for overall population. Similar follow‐up times. |
Van Leemput 2007.
| Methods | Randomisation by date of hospital presentation (group 1 = 1st, 4th, etc of each month; group 2 = 2nd, 5th, etc; group 3 = 3rd, 6th, etc). Assessor blinding: not stated Intention‐to‐treat analysis: probably yes, implied but no explicit statement on loss to follow‐up Loss to follow‐up: probably none but no confirmation received | |
| Participants | Frere Hospital, East London, South Africa 102 participants: 43 male (42%), mean age 42 years, range 18‐78 years with a minimally displaced ulnar shaft fracture. All fractures resulted from "focal low‐energy trauma due to a direct hit on the forearm". Inclusion criteria: isolated minimally displaced (< 50% displacement) of the distal two‐thirds of the ulnar shaft. Exclusion criteria: open or severely comminuted fracture, signs of infection, multiple trauma, age < 18 years. | |
| Interventions | No details of when treatment started, all treated on an outpatient basis. 1. Immediate mobilisation ‐ supplied with compression bandage 2. Short arm (below elbow) plaster cast for 6 weeks 3. Long arm (above elbow) plaster cast for 3 weeks, then 3 weeks in a below elbow cast Allocated: 34/36/32 (assuming no losses) Assessed: 34/36/32 | |
| Outcomes | Length of follow‐up: 12 weeks, also at 6 and 9 weeks Fracture union (delayed union assessed radiographically) Patient evaluation: pain (Visual Analogue Scale: 0 = worst to 10 = none) Range of motion (elbow extension/flexion, forearm rotation) Anatomic: time to bony union | |
| Notes | Details of method of randomisation, baseline characteristics and pain scale provided by Van Leemput. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Patient selection in three different groups was strictly randomised, purely based on date of first presentation at the hospital.". Thus, quasi‐randomised. |
| Allocation concealment (selection bias) | High risk | Not concealed ‐ quasi‐randomised trial. |
| Blinding (performance bias and detection bias) Patient‐rated outcomes | High risk | No mention of blinding. |
| Blinding (performance bias and detection bias) Clinician‐rated outcomes | Unclear risk | No mention of blinding. |
| Incomplete outcome data (attrition bias) Patient‐rated outcomes | Unclear risk | Follow‐up of all participants likely but not confirmed. |
| Incomplete outcome data (attrition bias) Clinician‐rated outcomes | Unclear risk | Follow‐up of all participants likely but not confirmed. Four participants in each group excluded from range of motion analyses because of prior fracture in the contralateral arm. |
| Selective reporting (reporting bias) | Unclear risk | Reports on typical set of outcomes for these fractures. |
| Selection bias (baseline imbalances)? | Low risk | Baseline characteristics provided by Van Leemput showed sufficient similarity in age, sex and dominant side injury. |
| Performance bias (care programme discrepancies)? | Unclear risk | Insufficient information. Similar follow‐up times and advice on pain. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Buch 1989 | Comparative study of functional treatments and immobilisation for 124 people with isolated ulnar shaft fracture. Translation from German showed it was not randomised. |
| Chirstos 2002 | Author confirmed that some of the 125 people with forearm bone compound fractures resulting from missile injuries had isolated ulnar shaft fractures. He also explained that the use of the term "at random" in the abstract of the report did not refer to a randomised trial but that there was a "lack of standard management and implements to dictate management protocol". |
| Collinge 2000 | Randomised trial comparing open reduction and plating with intramedullary nailing in 36 people with 37 diaphyseal forearm fractures, six of whom only had ulnar fractures. The sample size, which may have been further reduced through inadequate follow‐up, of people with isolated fractures of the ulnar shaft was considered too small to pursue separate data for these patients. |
| Coulibaly 2010 | Conference abstract reporting a retrospective series of 70 people with isolated ulnar shaft fractures and a comparison of the outcomes of operative versus conservative treatment. |
| Goel 1991 | Comparative prospective study of 89 people with 90 isolated ulna fractures who were treated with either plaster cast splintage (45 fractures) or elastic crepe bandage support and early mobilisation (45 fractures). It is not clear how the two groups were derived. Only 60 people were followed up. There was no response to a request for further information sent to the authors in March 1999. |
| Labbe 1998 | Abstract only. Authors confirmed (reply March 1998) that this was a retrospective study but also indicated that they were working on a randomised study of the same comparison. |
| Piatek 2000 | Randomised trial of nailing versus plate fixation for closed fractures in the middle third of both lower arm bones in 11 people. Not isolated ulnar shaft fractures. |
| Skinner 1989 | Abstract initially downloaded from web. However the full abstract in Orthopaedic Transactions confirmed this was not a randomised trial. |
Characteristics of ongoing studies [ordered by study ID]
NCT01123447.
| Trial name or title | A prospective randomized trial comparing open reduction and internal fixation with non‐operative treatment for ulnar shaft fractures |
| Methods | Multi‐centre randomised controlled trial |
| Participants | Skeletally mature patients (age 10 years of above) with isolated ulnar shaft fractures presenting within 14 days of their injury Estimated enrolment: 100 |
| Interventions | 1. Surgery: open reduction and internal fixation using a limited contact dynamic compression (LC‐DC) plate with screws 2. Non‐operative treatment with closed reduction and short‐arm (below‐elbow) cast for 6 weeks |
| Outcomes | Length of follow‐up: 1 year (also assessed: 2 weeks, 6 weeks, 12 weeks, 6 months) Primary outcome: Disabilities of the Arm, Shoulder and Hand (DASH) score Secondary outcomes: SF‐36, range of motion, pain, grip strength, return to work, and time to union |
| Starting date | May 2010 Estimated study completion date: December 2015 |
| Contact information | Contact: Kimberly D Carcary, kdcarcar@ucalgary.ca Chief Investigator: Dr. Paul Duffy, University of Calgary/Foothills Medical Centre |
| Notes |
Contributions of authors
Paddy Pearce initiated the review and, with Agop Der Tavitian, developed the protocol. Paddy Pearce and Helen Handoll undertook the literature search. All three reviewer authors assessed trial quality and extracted trial data. Paddy Pearce wrote the first draft of the review. Helen Handoll critically rewrote the review and subsequent revisions.
All updates, including updating the literature search, of the review were prepared by Helen Handoll and checked by Paddy Pearce. For the fifth and eight updates, Helen Handoll contacted the trialists of the newly identified/included trial. Both authors assessed trial quality and extracted trial data.
Helen Handoll and Paddy Pearce are the guarantors for the review.
Sources of support
Internal sources
University of Teesside, Middlesbrough, UK.
External sources
No sources of support supplied
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Atkin 1995 {published data only}
- Atkin DM, Bohay DR, Slabaugh P, Smith BW. Treatment of ulnar shaft fractures: A prospective, randomised study. Orthopedics 1995;18(6):543‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gebuhr 1992 {published and unpublished data}
- Gebuhr P, Holmich P, Orsnes T, Soelberg M, Krasheninnikoff M, Kjersgaard AG. Isolated ulnar shaft fractures: Comparison of treatment by a functional brace and long‐arm cast. Journal of Bone and Joint Surgery ‐ British Volume 1992;74(5):757‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Leung 2003 {published and unpublished data}
- Kamen J. personal communication January 13 2004.
- Leung F, Chow S‐P. A prospective, randomized trial comparing the limited contact dynamic compression plate with the point contact fixator for forearm fractures. Journal of Bone and Joint Surgery ‐ American Volume 2003;85(12):2343‐8. [DOI] [PubMed] [Google Scholar]
- Rajasekhar C, Goyal R, Leung F, Chow S‐P. Fixation of forearm fractures [letter and reply]. Journal of Bone and Joint Surgery ‐ American Volume 2004;86‐A(8):1830. [DOI] [PubMed] [Google Scholar]
Van Leemput 2007 {published data only}
- Leemput T. personal communication December 31 2008.
- Leemput T, Mahieu G. Conservative management of minimally displaced isolated fractures of the ulnar shaft. Acta Orthopaedica Belgica 2007;73(6):710‐3. [PubMed] [Google Scholar]
References to studies excluded from this review
Buch 1989 {published data only}
- Buch J, Hoffmann G. Functional treatment of ulnar shaft breakages [Funktionelle behandlung von ellenschaftbruchen]. Hefte zur Unfallheikunde 1989;201:149‐51. [Google Scholar]
Chirstos 2002 {published and unpublished data}
- Chirstos CG. personal communication October 31 2002.
- Chirstos CG. Forearm bone non‐union and its management. Ethiopian Medical Journal 2002;40(1):53‐8. [PubMed] [Google Scholar]
Collinge 2000 {published data only}
- Collinge CA, Herscovici D. Open reduction and plating vs. intramedullary nailing for diaphyseal forearm fractures: A prospective randomized study [abstract]. Journal of Orthopaedic Trauma 2000;14(2):121. [Google Scholar]
Coulibaly 2010 {unpublished data only}
Goel 1991 {published data only}
- Goel SC, Raj KB, Srivastava TP. Isolated fractures of the ulnar shaft. Injury 1991;22(3):212‐4. [DOI] [PubMed] [Google Scholar]
Labbe 1998 {published data only}
- Labbe JL, Leclair O, Goulon R. The treatment of fractures of the shaft of the ulna by closed percutaneous pinning [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1997;79 Suppl 1:62. [Google Scholar]
- Labbe JL, Peres O, Leclair O, Goulon R, Bertrou V. Isolated fractures of the adult ulnar shaft; treatment by percutaneous intramedullary nailing versus plate fixation (AO) [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1996;78 Suppl 2 & 3:108. [Google Scholar]
- Labbe JL, Peres O, Leclair O, Goulon R, Bertrou V, Saint‐Lanne S. Fixation of isolated ulnar shaft fracture by open reduction and internal fixation with plate or percutaneous intramedullary nailing [La fracture isolee de la diaphyse ulnaire, de l'osteosynthese par plaque a l'embrochage centro‐medullaire]. Revue de Chirurgie Orthopedique et Reparatrice de l'Appareil Moteur 1998;84(6):515‐22. [PubMed] [Google Scholar]
Piatek 2000 {published data only}
- Piatek S, Westphal T, Schubert S, Winckler S. Sealing nailing versus plate osteosynthesis in diaphysaric lower arm fractures [Verriegelungsnagelung versus plattenosteosynthese bei diaphysaren unterarmfrakturen]. Hefte zur der Unfallchirurg 2000;282:427‐8. [Google Scholar]
Skinner 1989 {published data only}
- Skinner M, Szabo RM. Isolated ulna shaft fractures [Abstract]. Orthopaedic Transactions 1989;13(3):530. [Google Scholar]
References to ongoing studies
NCT01123447 {unpublished data only}
- Duffy PJ, Carcary KD. Study comparing surgical treatment versus non‐surgical treatment of ulnar fractures. http://clinicaltrials.gov/show/NCT01123447 (accessed April 18 2012).
Additional references
Atkin 1995a
- Atkin DM, Bohay DR, Slabaugh P, Smith BW. Treatment of ulnar shaft fractures: A prospective, randomized study. Orthopedics 1995;18(6):543‐7. [DOI] [PubMed] [Google Scholar]
Beaton 2001
- Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. Journal of Hand Therapy 2001;14(2):128‐46. [PubMed] [Google Scholar]
Bhandari 2004
- Bhandari M, Schemitsch EH. Fractures of the shaft of the ulna. Journal of Orthopaedic Trauma 2004;18(7):473‐5. [DOI] [PubMed] [Google Scholar]
DARE 2006
- Centre for Reviews and Dissemination. The treatment of isolated ulnar fractures in adults: a systematic review (Structured abstract). Database of Abstracts of Reviews of Effects: DARE‐20001826. In The Cochrane Library 2006; Vol. 3.
De Jong 1989
- Jong T, Jong PCM. Ulnar‐shaft fracture needs no treatment. A pilot study of 10 cases. Acta Orthopaedica Scandinavica 1989;60(3):263‐4. [DOI] [PubMed] [Google Scholar]
Du Toit 1979
- Du Toit FP, Grabe RP. Isolated fractures of the shaft of the ulna. South African Medical Journal 1979;56(1):21‐5. [PubMed] [Google Scholar]
Grace 1980
- Grace TG, Witmer BJ. Isolated fractures of the ulnar shaft [abstract]. Orthopaedic Transactions 1980;4:299. [Google Scholar]
Hawe 2004
- Hawe P, Shiell A, Riley T, Gold L. Methods for exploring implementation variation and local context within a cluster randomised community intervention trial. Journal of Epidemiology and Community Health 2004;58(9):788‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2006
- Higgins JPT, Green S (editors). Highly sensitive search strategies for identifying reports of randomized controlled trials in MEDLINE. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6 [updated September 2006]; Appendix 5b. www.cochrane.org/resources/handbook/hbook.htm (accessed 14 Nov 2006).
Higgins 2008
- Higgins JPT, Altman DG (editors). Chapter 8: Assessing risk of bias in included studies Table 8.5a. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 (updated September 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Mackay 2000
- Mackay D, Wood L, Rangan A. The treatment of isolated ulnar fractures in adults: a systematic review. Injury 2000;31(8):565‐70. [DOI] [PubMed] [Google Scholar]
McQueen 2000
- McQueen MM. Epidemiology of fractures of the radius and ulna. In: McQueen MM, Jupiter JB editor(s). Radius and ulna. Oxford: Butterworth Heinemann, 2000:1‐11. [Google Scholar]
Perren 1995
- Perren SM, Buchanan JS. Basic concepts relevant to the design and development of the point contact fixator (PC‐Fix). Injury 1995;26(Suppl 2):SB1‐4. [Google Scholar]
Perren 2003
- Perren SM. Backgrounds of the technology of internal fixators. Injury 2003;34(Suppl 2):SB1‐3. [DOI] [PubMed] [Google Scholar]
Pollock 1983
- Pollock FH, Pankovich AM, Prieto JJ, Lorenz M. The isolated fracture of the ulnar shaft. Treatment without immobilization. Journal of Bone and Joint Surgery ‐ American Volume 1983;65(3):339‐42. [PubMed] [Google Scholar]
Rajasekhar 2004
- Rajasekhar C, Goyal R, Leung F, Chow S‐P. Fixation of forearm fractures [letter and reply]. Journal of Bone and Joint Surgery ‐ American Volume 2004;86‐A(8):1830. [DOI] [PubMed] [Google Scholar]
Smith 2004
Swiontkowski 1999
- Swiontkowski MF, Engelberg R, Martin DP, Agel J. Short Musculoskeletal Function Assessment Questionnaire: validity, reliability, and responsiveness. Journal of Bone and Joint Surgery ‐ American Volume 1999;81(9):1245‐60. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Handoll 2009
- Handoll HHG, Pearce P. Interventions for treating isolated diaphyseal fractures of the ulna in adults. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD000523.pub3] [DOI] [PubMed] [Google Scholar]


