Abstract
Background
Mental health problems are common in primary care and mental health workers (MHWs) are increasingly working in this setting delivering psychological therapy and psychosocial interventions to patients. In addition to treating patients directly, the introduction of on‐site MHWs represents an organisational change that may lead to changes in the clinical behaviour of primary care providers (PCPs).
Objectives
To assess the effects of on‐site MHWs delivering psychological therapy and psychosocial interventions in primary care on the clinical behaviour of primary care providers (PCPs).
Search methods
The following sources were searched in 1998: the Cochrane Effective Practice and Organisation of Care Group Specialised Register, the Cochrane Controlled Trials Register, MEDLINE, EMBASE, PsycINFO, CounselLit, NPCRDC skill‐mix in primary care bibliography, and reference lists of articles. Additional searches were conducted in February 2007 using the following sources: MEDLINE, EMBASE, PsycINFO, CINAHL, and Cochrane Central Register of Clinical Trials (CENTRAL) (The Cochrane Library).
Selection criteria
Randomised trials, controlled before and after studies, and interrupted time series analyses of MHWs working alongside PCPs in primary care settings. The outcomes included objective measures of PCP behaviours such as consultation rates, prescribing, and referral.
Data collection and analysis
Two review authors independently extracted data and assessed study quality.
Main results
Forty‐two studies were included in the review. There was evidence that MHWs caused significant reductions in PCP consultations (standardised mean difference ‐0.17, 95% CI ‐0.30 to ‐0.05), psychotropic prescribing (relative risk 0.67, 95% CI 0.56 to 0.79), prescribing costs (standardised mean difference ‐0.22, 95% CI ‐0.38 to ‐0.07), and rates of mental health referral (relative risk 0.13, 95% CI 0.09 to 0.20) for the patients they were seeing. In controlled before and after studies, the addition of MHWs to a practice did not affect prescribing behaviour towards the wider practice population and there was no consistent pattern to the impact on referrals in the wider patient population.
Authors' conclusions
This review provides some evidence that MHWs working in primary care to deliver psychological therapy and psychosocial interventions cause a significant reduction in PCP behaviours such as consultations, prescribing, and referrals to specialist care. However, the changes are modest in magnitude, inconsistent, do not generalise to the wider patient population, and their clinical or economic significance is unclear.
Plain language summary
On‐site mental health workers delivering psychological therapy and psychosocial interventions to patients in primary care: effects on the professional practice of primary care providers
Most people with mental health problems are treated by their family physician or general practitioner. Physicians will treat these problems, often without referral to mental health specialists, and at times the care is not consistent and could be improved. This review investigated whether having mental health workers on‐site to work with physicians at their offices would change the care that physicians provide. Forty‐two studies were reviewed in which on‐site mental health workers, such as counsellors or psychiatrists, worked alongside physicians to provide therapy to patients. The review found that when there were mental health workers on‐site, patients may reduce the number of visits to their doctors; doctors may reduce how often they refer patients to off‐site mental health specialists; doctors may reduce the number of drugs they prescribe to the patients who see the mental health workers; and the costs related to those drugs may be lower. However, these reductions were small and not found consistently in all the studies. The review also found that there may be little or no difference in how the doctors prescribe drugs or refer patients who have mental health problems but are not seeing the on‐site mental health workers. It is also not known what the effect of on‐site mental health workers had on how well physicians recognised and diagnosed mental health problems.
Background
In most healthcare systems primary care providers (PCPs) act as 'gatekeepers' to care in specialist settings (WHO 2001). Research indicates that the vast bulk of mental health problems in the community are dealt with by PCPs without referral to mental health specialists; and there is also evidence that the care provided by PCPs is variable, with significant room for improvement (Gilbody 2003; Goldberg 1992).
In response, mental health workers (MHWs) from a variety of disciplines are increasingly bringing their specialist skills into primary care to provide a range of interventions to patients, including psychological therapy and psychosocial interventions (Sibbald 1993). In addition to their role in treatment provision, the addition of an on‐site MHW represents an organisational change which may lead to changes in professional roles, the alteration of established clinical routines, and improvements in the clinical practice of PCPs.
There are a number of different models of the interface between MHWs and PCPs (Bower 2005; Gask 1997; Pincus 1987). The mechanisms of change by which MHWs may change PCP behaviour range from specific education and skill sharing between professionals to more diffuse processes, such as raising the profile of mental health in the primary care setting. Some models are organised such that the PCP refers the patient to the MHW, who assumes responsibility for the management of the patient's mental health problem by providing psychological therapy and psychosocial interventions. This way of working has been described as a 'replacement' model (Bower 2005). In this model, the main focus of interest concerns the effects of the direct provision of psychological therapy and psychosocial interventions on patient outcomes. Any changes in the behaviour of the PCP are viewed as a beneficial 'side effect' of the direct treatment function of the MHW. Nevertheless, these 'side effects' may have a beneficial impact on the overall costs of mental health care and the workload of PCPs. For example, referral of patients to on‐site MHWs operating in a replacement model may reduce both consultation rates with the PCP (thus freeing up clinical time for other duties) and prescribing of psychotropic medication (thus reducing the overall costs of care). The costs of employing on‐site MHWs in a replacement model is sometimes hypothesised to be recouped from the savings associated with these changes. Medical utilisation may decrease as a result of the MHW intervention if the psychological therapy or psychosocial intervention leads to changes in patients' mental health, social function, or need for care. This is referred to as a 'cost offset' (Fiedler 1989) and has been a significant feature of the literature on psychological therapies both generally and in primary care following the introduction of large numbers of MHWs in this setting (Martin 1985; Mumford 1984; Pharoah 1996). Cost offset reflects an economic perspective on service delivery since the focus is on reduction in health service utilisation, rather than quality of care or patient outcomes.
In other models, the PCP remains at the forefront of mental health care. In this case the main aim of the MHW is to support the PCP's management of the patient's mental health problem through education, advice, and support to the PCP (although the MHW may, in addition, provide some direct intervention to patients). These models have been described as 'consultation‐liasion' or 'collaborative care' (Bower 2005). Although MHWs and PCPs in a replacement model will interact and collaborate in informal ways (through common medical records, opportunities to discuss potential referrals, or informal discussions about patients), such interactions are explicit and standardised in consultation‐liaison and collaborative care. Because such models explicitly seek to change the clinical behaviour of PCPs, they are generally much more complex interventions involving behaviour change interventions with the PCP (Bower 2002). The effects of these models are the subject of separate future reviews (Fletcher 2007; Parker 2008).
This review sought to determine the effects of a replacement model by systematically reviewing evidence on the influence of MHWs on the clinical practice of PCPs. On‐site MHWs functioning in a replacement model potentially have two different effects on the behaviour of the PCP. Direct effects involve changes in PCP behaviour towards clients under the direct clinical care of the on‐site MHW. For example, does referring a patient to a clinical psychologist for psychological therapy change the likelihood that a PCP will prescribe antidepressant medication for that patient compared to patients who remain under the care of the PCP? Direct effects will largely reflect the impact on the PCP of referring their patient to an MHW.
Indirect effects are changes in PCP behaviour which occur in the wider primary care population, not just for those patients who were referred to MHWs. For example, does the addition of a clinical psychologist working on‐site in primary care change the overall prescribing of antidepressants by the PCPs within that organisation for their entire practice population? Indirect effects indicate whether the presence of a MHW has a more general effect on PCP behaviour.
Objectives
To determine the direct and indirect effects of on‐site mental health workers (MHWs) delivering psychological therapy and psychosocial interventions in primary care on the clinical behaviour of primary care providers (PCPs).
Investigation of direct effects involved comparison of PCP behaviour towards patients who were allocated to an on‐site MHW for psychological therapy and psychosocial interventions with those patients who remained under the care of the PCP.
Investigation of indirect effects involved comparison of PCP behaviour towards patient populations in practices, clinics, or other primary care organisations with or without access to on‐site MHWs.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), controlled before and after studies (CBAs), and interrupted time series (ITS).
Types of participants
Primary care providers. In order to ensure comparability of interventions, the review was restricted to PCPs who fulfilled the following definition:
'PCPs are medical health care professionals providing first contact and on‐going care to patients, regardless of the patient's age, gender or presenting problem'.
Types of interventions
For the purposes of the present review, the addition of the MHW on‐site in primary care was the intervention, rather than the particular therapeutic approach taken by that worker in his or her management of individual patients.
MHWs working on‐site in primary care settings differ in terms of experience, training, therapeutic approach, funding, and relationship with the PCP (Sibbald 1993). Mental health interventions may be conducted by a wide range of staff with an equally wide range of qualifications and experience: practice counsellors, social workers, psychiatric or non‐psychiatric nurses, psychiatrists, psychotherapists, psychologists, clergy, and lay volunteers. Equally, the interventions may vary from psychotherapy and counselling to broader psychosocial interventions such as occupational therapy and social casework. PCPs may take on a specialist MHW role and provide psychological therapy and psychosocial interventions with additional training and a change in clinical role. Furthermore, the patient groups served by these individuals may differ widely. For the purposes of the review, the main requirements for the interventions to be included were:
(1) psychological therapy and psychosocial interventions provided by an on‐site MHW as a separate and distinct activity and not solely part of normal primary care consultations;
(2) the MHW was employed by or attached to the PCP organisation and worked on‐site i.e. the PCP and MHW worked for at least part of the time in geographical proximity and as part of the same clinical team.
For the purposes of the review, psychological therapy and psychosocial interventions were defined broadly. Psychological therapy refers to formal treatments based on a theory of psychological functioning; whereas psychosocial interventions represent less specific interventions designed to improve mental health through general support, advice, and encouragement.
Interventions where the MHW additionally provided behaviour change interventions directly to the PCP (such as provision of guidelines or in‐practice training), or where the MHW provided psychological therapy and psychosocial interventions as part of a wider quality improvement intervention which included behaviour change interventions delivered directly to the PCP, were excluded from the review. These interventions will be the subject of future reviews (Fletcher 2007; Parker 2008).
Psychological therapy and psychosocial interventions in primary care based on the use of technology such as screening tools, computerised aids, or self‐help interventions, without the use of a specific MHW, were excluded from the present review.
Types of outcome measures
Outcome measures used in the review for the analysis of both direct and indirect effects included the following objective PCP clinical behaviours. Although some of these behaviours may reflect, in part, the behaviour of the patient (for example adherence to medication, primary care consultations), PCPs have an important role in determining such patient behaviours and thus the PCP clinical behaviours were considered relevant for the review.
(1) Diagnostic behaviour ‐ this included both the accuracy of specific psychiatric diagnoses or more general detection of disorder i.e. whether a patient was recognised as 'psychiatrically distressed' (Marks 1979). It was hypothesised that recognition and diagnosis would increase with the presence of a MHW.
(2) Prescribing behaviour ‐ this involved overall prescribing rates and costs, types of prescription, patient adherence to medication, and the overall adequacy of medication compared with clinical guidelines. It was hypothesised that prescribing would decrease with the presence of a MHW.
(3) Referral behaviour ‐ this involved off‐site referrals (both to psychiatric and non‐psychiatric agencies), laboratory tests and investigations, and overall referral costs. It was hypothesised that referrals would decrease with the presence of a MHW.
(4) Consultations ‐ in the review a consultation referred to visits by patients to the PCP or other primary care staff (such as primary care nurses) and the associated costs of these visits. All consultations (both mental health, non‐mental health, and mixed) were included, where reported. Visits to specialist staff (including other mental health providers) were labelled as referrals in the present review. It was hypothesised that consultations would decrease with the presence of a MHW.
Although outcomes involving changes in the knowledge, skills, and attitudes of PCPs were of potential relevance, the present review focussed on objective measures of PCPs' actual clinical behaviours rather than psychological characteristics which may potentially impact on those behaviours.
Patient mental health outcomes (for example scores on standardised depression questionnaires) are of obvious relevance to the evaluation of the cost‐effectiveness of MHWs delivering psychological therapy and psychosocial interventions in primary care. However, the present review was restricted to the impact of MHWs on the behaviour of the PCP, and studies examining patient mental health outcomes only were excluded.
Search methods for identification of studies
The search strategy used in 1998 is shown in Appendix 1. These searches were augmented in February 2007 through searches of MEDLINE, EMBASE, PsycINFO, CINAHL and the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library) to cover the period 1998 to 2007. An example of the search strategy is outlined below, and the full strategies are listed in Appendix 2.
CENTRAL
#1 MeSH descriptor Primary Health Care explode all trees #2 MeSH descriptor Physicians, Family explode all trees #3 MeSH descriptor Family Practice explode all trees #4 family near/2 pract* #5 general near/2 pract* #6 primary near/2 care #7 (#1 OR #2 OR #3 OR #4 OR #5 OR #6) #8 counsel* #9 psychotherap* #10 clin* near/2 psy* #11 beh* near/2 therap* #12 group near/2 therap* #13 psychoanal* #14 psychiat* #15 cog* near/2 therap* #16 psychodynam* #17 MeSH descriptor Counseling explode all trees #18 MeSH descriptor Psychotherapy explode all trees #19 MeSH descriptor Psychology, Clinical explode all trees #20 MeSH descriptor Mental Health explode all trees #21 MeSH descriptor Mental Disorders explode all trees #22 (#8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21) #23 (#7 AND #22) #24 (#23), from 1998 to 2007
Data collection and analysis
A single review author (PB) read all the abstracts or full articles of the citations retrieved from the searches to identify potentially relevant studies. These publications were then independently read by both review authors who included studies that met the relevant criteria. Disagreements were resolved by discussion.
Information concerning each study was extracted independently by both authors using a modified version of the Effective Practice and Organisation of Care Group (EPOC) checklist (http://www.epoc.cochrane.org/Files/Website%20files/Documents/Reviewer%20Resources/datacollectionchecklist.pdf). Disagreements were resolved by discussion.
EPOC quality criteria for RCTs involve consideration of unit of allocation and analysis, concealment of allocation, follow‐up rates, blinding, comparability of groups at baseline, reliability of outcome assessment, and protection against contamination. For inclusion in the review, CBAs must include contemporaneous data collection and the use of appropriate control groups. Quality criteria include baseline measurement in intervention and control groups, comparability of characteristics of intervention and controls, blinded assessment of primary outcome, protection against contamination, follow‐up rates, and reliability of outcome assessment. For inclusion in the review, ITSs must include an intervention delivered at a defined point in time, contemporaneous data collection, and the presence of more than three data points before and after the intervention. Quality criteria include protection against secular change, presence of sufficient data points before and after the intervention, formal test for trend, data collection uncontaminated by the intervention, data identical before and after the intervention, blinded assessment of outcome, reliable outcomes, and completeness of the data set (Bero 2000).
As noted earlier, the review included examination of both direct and indirect effects. The examination of direct effects is amenable to RCTs. However, a number of CBAs of direct effects were also reported. Given the weakness of the CBA design and the availability of a significant number of RCTs, CBA studies of direct effects have been identified and extracted into tables but the data have not been presented in the text and have not been used in the interpretation of the main findings. In the examination of indirect effects, the use of an RCT design is potentially problematic and the proportion of CBA studies is much higher. Therefore, CBA studies have been presented and analysed fully in the examination of indirect effects.
Meta‐analysis was conducted where multiple trials were reported examining the same outcome, and outcomes were reported in a standardised fashion suitable for pooling. The following data were used for the pooled analysis.
PCP consultations were pooled when the data were reported as mean number of consultations (with a standard deviation). Trials reporting consultation outcomes in alternative formats (for example medians, range of consultations, costs of consultations, or means without standard deviations) were excluded from the pooled analysis and reported narratively.
Psychotropic prescribing data were pooled when the data were reported as the percentage of patients in each group taking psychotropic medication. Where different types of psychotropic prescriptions were distinguished in the same paper (for example antidepressants, anxiolytics), a decision was made to include the most frequently reported psychotropic prescriptions in the pooled analysis.
Costs of prescribing were pooled when data were reported as mean cost of prescribing (with a standard deviation).
Mental health referrals were pooled when the data were reported as the percentage of patients in each group referred to a mental health professional other than the MHW involved in the intervention. Trials reporting mental health referral outcomes in alternative formats (for example mean number of referrals) were excluded from the pooled analysis and reported narratively.
Where two comparisons from the same trial were included in a meta‐analysis, the sample size in the control group was halved to avoid a unit of analysis error. The proportion, or mean outcome, in the control group was not changed.
For the pooled analyses, relative risks (RR) were calculated for dichotomous outcomes and standardised mean differences (SMD) for continuous outcomes. Although the same outcome (number of consultations) was used in the pooled analysis of consultation rates it should be noted that this outcome relates to a clinical behaviour which is a function of time. Since the included studies calculated outcomes over varying time periods, the SMD was reported for consultations. It should be noted that cost data are sometimes skewed and demonstrate much higher levels of variability than clinical outcomes, and caution must be exercised in the interpretation of statistical significance in single studies reporting cost data, and in the interpretation of SMD in meta‐analysis of cost data.
Heterogeneity among the study results was assessed using the Chi2 test for heterogeneity and the I2 statistic. Where heterogeneity was low to moderate (I2 < 50%), a fixed‐effect model was reported. Otherwise a random‐effects model was used.
In accordance with EPOC guidelines, all results (both those included in the meta‐analyses and those excluded) were also presented in the 'Comparisons and data' tables as 'Other data'. For all data, the following statistics were computed.
Absolute change (mean or proportion in experimental group minus control).
Relative percentage change (absolute change divided by post‐test score in the control group).
Absolute change from baseline (pre‐intervention to post‐intervention changes in both groups).
Difference in absolute change from baseline.
In studies without baseline data, only absolute change and relative percentage change were calculated.
Results
Description of studies
Forty‐two studies comparing MHW and usual PCP care were included in the review; four were included in the same two papers (Kendrick 2005a; Kendrick 2005b; King 2000a; King 2000b). Thirty‐three were studies of direct effects and nine examined indirect effects. One hundred and fifty‐four studies were excluded as they met several inclusion criteria but not all (for example, trials of MHWs in primary care that failed to report objective PCP behaviours). These trials are listed in the excluded studies section.
Study populations
Generally, as PCPs were not the main focus of the studies, only very basic information was available on the PCP characteristics. Thirty‐five studies involved PCPs from the UK, two from the United States, and one each from Australia, New Zealand, Sri Lanka, Netherlands, and West Germany. PCPs were general practitioners and family physicians in all the studies.
Information was only routinely provided on patients participating in the studies of direct effects. However, studies could be broadly categorised according to whether they involved professionals managing common mental health problems (for example anxiety and depression), which represented the bulk of the studies, and those involving professionals dealing with patients with more severe and enduring disorders (Bruce 1998; Hunter 1983; Wells 1992). Of the studies in common mental health problems, two dealt specifically with patients identified as high utilisers of medical care (Benson 1988; Sumathipala 2000) and two studies were conducted in patients with chronic illness (Basler 1990; Spurgeon 2007).
In most randomised studies of direct effects patients were recruited by the participating PCP, although some used alternatives such as patients recruited through screening in the primary care centre. The types of patients recruited to the trials varied. Some studies used specific patient groups identified through screening procedures. These included specific diagnostic groups (such as DSM‐IIIR major and minor depression), problem types related to the intervention provided by the MHW (for example neuroses amenable to behavioural treatment, marital problems), or other groups (such as high utilisers of services or frequent attenders). Other studies recruited patients identified by the PCP as requiring psychological therapy or psychosocial intervention and thus included a heterogeneous mixture of patients.
Interventions
The studies involved a variety of MHWs including: counsellors (16 studies); psychologists (11 studies); psychiatrists (five studies); community psychiatric nurses (seven studies), nurse therapists (one study), practice nurses (one study), and social workers (one study). In two studies, the MHW profession was not clear (Lambert 2007; Walker 1989). Some studies examined more than one type of therapist, or treatments provided by therapists working together. Psychological therapy and psychosocial interventions provided by these MHWs included non‐directive counselling, behaviour therapy, cognitive‐behaviour therapy, cognitive‐analytic therapy, brief dynamic psychotherapy, problem solving therapy, interpersonal therapy, facilitated self help, occupational therapy, practice‐based psychiatric clinics, and social casework.
Risk of bias in included studies
Studies of direct effects
Twenty‐five studies of direct effects were RCTs. Concealment of allocation was adequate in 10 studies (Brouwers 2006; Corney 1984; Corney 2003; Harvey 1984; Kendrick 2005a; Kendrick 2005b; King 2000a; King 2000b; Richards 2003; Sumathipala 2000), unclear from the information provided in 12 studies (Boot 1994; Brodaty 1983; Catalan 1991; Earll 1982; Ginsberg 1984; Gournay 1995; Lambert 2007; Lave 1998; Mynors‐Wallis 1997; Robson 1984; Stanton 1998; Teasdale 1984), and the allocation procedure was considered open to bias in three studies (Ashurst 1983; Benson 1988; Hemmings 1997). There were eight studies of direct effects using a CBA design (Ashworth 2000; Basler 1990; Blakey 1986; Brantley 1986; Bruce 1998; Lyon 1993; Martin 1985; Spurgeon 2007). As noted above, details have been provided in the tables but these studies were not considered further in the text.
Although PCP behaviours were assessed objectively through medical record searches and chart reviews, the reliability of data gained through medical record searches and chart reviews was not assessed. Because patients were the unit of allocation in these studies of direct effects, the possibility of indirect effects associated with the presence of a MHW in the practice meant that contamination was always possible (whether the study was an RCT or CBA). Although a number of studies did report power analyses these were always related to the clinical outcome data rather than the PCP behaviours analysed in the present review, so their utility is unclear.
Studies of indirect effects
One RCT of indirect effects was identified (Lester 2007) and allocation concealment was adequate. There were eight studies of indirect effects using a CBA design (Baker 1996; Coe 1996; Hunter 1983; Pharoah 1996; Simpson 2003; Tarrier 1983; Walker 1989; Wells 1992). In the CBA studies, extensive information concerning the comparability of the sites chosen as controls was provided in two studies (Baker 1996; Simpson 2003). One used random selection of controls from a sample but did not provide any descriptive statistics (Pharoah 1996). Other studies described qualitative similarities between practices (Hunter 1983; Tarrier 1983; Walker 1989) or used practices in the same geographical area (Coe 1996; Wells 1992). The comparability of control and intervention practices in terms of outcome variables at baseline was examined statistically in only three studies (Hunter 1983; Pharoah 1996; Simpson 2003) and confirmed in two (Pharoah 1996; Simpson 2003). Four studies provided data on baseline measures without statistical testing (Coe 1996; Baker 1996; Tarrier 1983; Walker 1989).
In the indirect studies, most of the PCP behaviours were assessed objectively and the reliability was enhanced through the use of automated recording systems. Practices were the unit of allocation and control practices were specifically chosen so as not to have access to the intervention under test.
Effects of interventions
Studies of direct effects
Consultations
Ten RCTs provided data for the pooled analysis of the effects of an on‐site MHW on consultation rates, involving 1061 patients (Benson 1988; Brouwers 2006; Gournay 1995; Kendrick 2005a; Kendrick 2005b; King 2000a, King 2000b, Lave 1998; Mynors‐Wallis 1997; Richards 2003). The test for heterogeneity was not significant (Chi2 = 14.76, df = 9, P = 0.10, I2 = 39.0%). Overall, consultation rates for patients under the care of a MHW were significantly lower than for patients under usual care (SMD ‐0.17, 95% confidence interval (CI) ‐0.30 to ‐0.05).
Of those studies excluded from the pooled analysis, consultation rates were significantly lower in the intervention group in three out of seven studies that reported the significance of post‐intervention differences (Robson 1984; Sumathipala 2000; Teasdale 1984). No significant difference was found in the remaining studies (Ashurst 1983; Boot 1994; Corney 1984; Earll 1982). Five studies did not report tests of statistical significance (Catalan 1991; Corney 2003; Ginsberg 1984; Harvey 1998; Stanton 1998); in four, consultation rates or consultation times were lower in the intervention group (Catalan 1991; Corney 2003; Ginsberg 1984; Harvey 1998) and in one the rate was higher in the intervention group (Stanton 1998).
Prescribing
Thirteen RCTs provided data for the pooled analysis of the effects of an on‐site MHW on psychotropic prescribing rates, involving 1299 patients (Ashurst 1983; Boot 1994; Brouwers 2006; Catalan 1991; Corney 1984; Corney 2003; Earll 1982; Gournay 1995; Hemmings 1997; King 2000a; King 2000b; Stanton 1998; Teasdale 1984). The test for heterogeneity was not significant (Chi2 = 9.94, df = 12, P = 0.62, I2 = 0%). The proportion of patients under the care of an on‐site MHW prescribed psychotropic medication was significantly lower than for those under usual care (RR 0.67, 95% CI 0.56 to 0.79).
One study excluded from the pooled analysis did not report tests of statistical significance but showed increases in the intervention group (Brodaty 1983).
Seven RCTs provided data for the pooled analysis of the costs of prescribing, involving 701 patients (Corney 2003; Kendrick 2005a; Kendrick 2005b; King 2000a; King 2000b; Mynors‐Wallis 1997; Richards 2003). The test for heterogeneity was not significant (Chi2 = 7.37, df = 6, P = 0.29, I2 =8.6%). Overall, prescribing costs for patients under the care of a MHW were significantly lower than for those under usual care (SMD ‐0.22, 95% CI ‐0.38 to ‐0.07).
One study excluded from the pooled analysis showed significant reductions in psychotropic prescribing costs in the intervention group (Robson 1984).
Ten studies reported data on the effects on non‐psychotropic or combined prescribing. Four studies reported no significant differences in prescribing (Earll 1982; Ginsberg 1984; Richards 2003; Robson 1984). Of the six studies not reporting statistical significance, three reported higher rates or costs in the MHW group (Brodaty 1983; Brouwers 2006; Corney 2003) and three reported lower rates or costs (Harvey 1998; Kendrick 2005a; Kendrick 2005b).
Referral
Seven RCTs provided data for the pooled analysis of mental health referrals, involving 793 patients (Boot 1994; Brouwers 2006; Catalan 1991; Corney 1984; Hemmings 1997; Lambert 2007; Teasdale 1984). The test for heterogeneity approached significance (Chi2 = 1.24, df = 6, P = 0.08, I2 = 46.6%). The proportion of patients under the care of a MHW referred for mental health care was significantly lower than for those under usual care (RR 0.13, 95% CI 0.09 to 0.20, fixed‐effect model). A post hoc sensitivity analysis excluding the study with inadequate concealment (Hemmings 1997) reported similar results (Chi2 = 10.10, df = 5, P = 0.07, I2 = 50.5%; RR 0.17, 95% CI 0.07 to 0.41, random‐effects model).
Of those studies excluded from the pooled analysis, one found no significant difference (Richards 2003); five studies did not report tests of statistical significance but found lower mean referrals and costs in the intervention group (Harvey 1998; Kendrick 2005a; Kendrick 2005b; King 2000a; King 2000b).
Four studies examined the effect on non‐mental health referral. Three reported very similar mean referrals in intervention and control groups (Brouwers 2006; King 2000a; King 2000b) while one reported slightly higher proportions of referrals in the control group (Lambert 2007).
Seven studies examined the effect on overall referral, including both mental health and non‐mental health patients. One found no significant differences between groups (Earll 1982). The other studies did not report tests of statistical significance. One reported a lower rate of referral in the intervention group (Harvey 1998), two reported lower costs in the intervention group (King 2000a; King 2000b), and three reported a higher rate of referral in the intervention group (Kendrick 2005a; Kendrick 2005b; Stanton 1998).
Studies of indirect effects
Consultations
One RCT found no significant difference in primary care consultation costs (Lester 2007).
Prescribing
One RCT found no significant difference in combined psychotropic and non‐psychotropic drug costs (Lester 2007).
Four CBA studies found no significant differences in rates of psychotropic prescribing (Baker 1996; Coe 1996; Pharoah 1996; Simpson 2003).
Referral
One RCT examined the effects on referrals (Lester 2007) and found largely similar rates of referrals but increases in referrals to psychiatrists and an overall increase in costs. The same study also reported effects on non‐mental health referrals and costs and found reduced rates and costs in the intervention group.
Six CBA studies examined the effects on mental health referrals (Baker 1996; Coe 1996; Hunter 1983; Tarrier 1983; Walker 1989; Wells 1992). In one study the intervention group had higher rates of referral to clinical psychology services, but that there were no significant differences in rates of referral to other services (Baker 1996). A second study found higher referral rates to psychiatry in the intervention group before the intervention and lower rates after the intervention (Coe 1996). Intervention practices also had lower referral rates to community mental health teams. A third study found an increased referral rate of chronic psychiatric cases to both outpatient and inpatient facilities in the intervention group (Walker 1989). In a fourth study, the intervention reduced overall referrals to psychiatry, first referrals, and emergency referrals, but had no effect on re‐referrals (Wells 1992). In a further two studies, there were conflicting results in the different intervention practices studied with some outcomes showing increases and others no change in mental health referrals (Hunter 1983; Tarrier 1983).
Discussion
Literature search
The literature search was restricted to English language publications. At present it is not known whether there is a significant foreign‐language literature relating to these issues. Future updates of the review may benefit from inclusion of studies without language restriction and searches of the NHS Economic Evaluation Database for further studies of cost effectiveness.
Analysis and outcomes
As noted in the introduction, the perspective taken in this review is related to issues of cost offset, which is concerned with the effects of mental health workers on service utilisation rather than issues of quality of care or patient outcomes. Service utilisation was reported as a secondary outcome in most of the studies included in the present review. It is likely that decisions concerning the provision of MHWs in primary care, in replacement models, will depend crucially on the clinical or cost effectiveness of the psychological therapy and psychosocial interventions that they provide in terms of patient outcomes (such as symptoms and perceived distress). Many of the direct studies included in the review reported data on patient outcomes; and reviews of the effects of MHWs in primary care on patient outcomes are available (Bower 2006; Brown 1995; Churchill 1999; Friedli 1996; Schulberg 2002). However, the present review was focussed on a second issue, the influence of MHWs on PCP behaviour and the consequent resource use and costs of mental health care in primary care.
Although patient outcomes are important, it should be noted that the effects examined in the present review are important determinants of the overall cost effectiveness of MHWs in primary care, and thus may inform decision making alongside studies of patient outcome. Adherents of the replacement model suggest that the costs of provision of on‐site MHWs will be recouped from savings in health service utilisation, although the cost offset may not always be sufficient to overcome the costs of the MHW (Bower 2003).
It should be noted that changes in PCP behaviour, such as reductions in antidepressant prescribing, are generally viewed as positive from the cost‐offset perspective as they reduce the costs of care, all other things being equal. This assumption was present explicitly or implicitly in the bulk of the papers in the review. However, other commentators have pointed out that this assumption can be challenged as reductions may alter the overall cost effectiveness of care if the new pattern of care (for example the treatment provided by the MHW) achieves inferior clinical or quality outcomes to the treatment that it is replacing (Wessely 1996). The net effect of this on cost effectiveness will depend upon the relative magnitude of changes in costs and effectiveness. Consultation‐liaison and collaborative care models often seek to increase certain aspects of utilisation (such as medication).
Quality of included studies
Overall, the quality of studies of direct effects was variable. In part this reflects the fact that issues of relevance to the present review were often secondary to the main aim of the primary studies. This meant that information was often not presented on quality issues, for example the proportion of patients for whom information was available from medical records about PCP behaviour.
The examination of direct effects is amenable to RCT designs and the utility of CBA designs must be questioned. However, because care over a significant time span is a key characteristic of primary care, RCTs would benefit from longer follow up in order to examine the degree to which direct effects endure past the initial response of the PCP to the MHW referral.
The use of RCTs in the examination of indirect effects was rare and only one study using a cluster randomised design was identified (Lester 2007). This may be the result of the fact that the introduction of MHWs in primary care may reflect service innovation in individual primary care practices (Sibbald 1993) and practices that have independently introduced a MHW are unlikely to allow removal of the service for the purposes of research. CBA designs may have an important role as methods of evaluation where random allocation is unacceptable to participants. As differences between control and intervention groups in the characteristics of both providers and practices introduces selection bias, more consistent and detailed reporting of such characteristics would undoubtedly aid interpretation of results from such studies. It is likely that the interpretative difficulties caused by lack of control over allocation can only be offset by a significant weight of evidence from a number of CBA studies demonstrating consistent results. Studies in the present review (for example Baker 1996) have demonstrated that service evaluations using automated databases can provide both large samples of participating practices and examination of the long‐term effects of interventions. However, it is important that studies using a unit of allocation other than the patient (for example practitioner or practice) use appropriate statistical techniques to take into account the clustering of patients within practices or organisations.
It should be noted that data were lacking on the degree to which the PCPs and organisations in the studies were representative. It is likely that volunteers to such research studies differed from non‐volunteers. It is not clear how such bias would impact on the results. Volunteers to such studies may have more positive attitudes to mental health issues, or may have less positive attitudes (and thus are more likely to take part in studies where access to MHWs is part of the protocol). The majority of the studies in the review were conducted in the UK, which might limit the applicability of the studies to other contexts with different systems of primary care and mental health service delivery.
Results of the included studies
There was evidence from the pooled analysis that referral to a MHW caused reduction in PCP consultations. The effect size was 'small' according to current convention (Cohen 1988; Lipsey 1990). To give an example of the size of such an effect, patients in the control group of a UK study included in the review reported a mean of 9.12 consultations over 12 months, with a standard deviation of 5.1 (King 2000a; King 2000b). If the effect on consultations estimated in the meta‐analysis was robust over 12 months, this would equate to a reduction of approximately one consultation over that period that was associated with referral to a MHW. The modest nature of the difference was consistent with the heterogenous results from studies excluded from the pooled analysis. It should be noted that two of the studies (Benson 1988; Sumathipala 2000) examined interventions specifically aimed at those who frequently consulted in primary care and both reported positive results.
The pooled analyses also suggested that referral to a MHW reduced the likelihood of the PCP prescribing psychotropic medication and the overall costs of psychotropic prescribing. The impact on costs was again 'small' according to current convention (Cohen 1988; Lipsey 1990).
Finally, the pooled analyses suggested that referral to a MHW reduced the likelihood of the PCP referring to another MHW off site. Although the effect was of significant magnitude, it should be noted that the effects included in this analysis were highly heterogenous; the largest effect was found in a study which failed to use adequate concealment of allocation (Hemmings 1997). However, most of the studies not included in the pooled analysis also showed reductions, and a post hoc sensitivity analysis excluding the inadequately concealed study made little difference to the results.
In terms of the indirect effects, four CBA studies were consistent in showing that there is no statistically significant reduction in psychotropic prescribing in the primary care population associated with an on‐site MHW, although the possibility of bias remains with this type of design. In terms of mental health referrals, the evidence is mixed, with some studies reporting decreases in referral rates and some studies finding that the intervention may actually increase certain types of mental health referrals.
These observed outcomes of the replacement model seem reasonable to the degree that an on‐site MHW provides an accessible alternative to off‐site referral and medication for an individual patient. Given the modest direct effects on PCP behaviour, it would be expected that indirect effects would be rare. Indeed, the presence of an on‐site MHW may sometimes increase referral rates, possibly through sensitising the PCP to psychological and psychiatric problem presentations which cannot be managed within the resources available to the on‐site MHWs.
Authors' conclusions
Implications for practice.
The evidence presented provides some support for the hypothesis that MHWs providing psychological therapy and psychosocial interventions on‐site in primary care cause reductions in consultation rates, psychotropic prescribing, and mental health referrals among patients treated by the MHW. However, the effects are modest. There is evidence that on‐site MHWs do not impact on prescribing behaviour towards the wider practice population. The impact on referral rates is very inconsistent and no firm conclusions can be stated.
Overall, the present evidence suggests that on‐site MHWs are associated with changes in PCP behaviour. The evidence does not support the addition of MHWs to primary care teams with the aim of reducing demand on PCPs or achieving enduring changes in their clinical behaviour which will generalise to the wider practice population.
Implications for research.
Evaluation of the effects of MHWs on PCP behaviour would generally benefit from longer‐term follow up in order to determine the stability of any effects that are demonstrated and their deterioration over time. This is especially true of the indirect effects of MHWs, which may only occur when the MHW is a permanent and integral member of the primary care team.
The use of quasi‐experimental designs (CBAs and ITSs) and routinely collected data may provide a model for the efficient evaluation of indirect effects where participants (for example PCPs and MHWs) object to random allocation (Baker 1996). Greater detail concerning the baseline characteristics of participating practices and PCPs would allow more accurate judgement concerning the magnitude of selection bias in those variables.
The addition of MHWs to primary care teams is a complex intervention in the sense that it operates by altering inter‐professional as well as inter‐personal working relationships in ways which are poorly understood. Pragmatic RCTs treat such interventions as a 'black box' and generally give little information on how or why a particular intervention has (or has not) caused change. Future RCTs of MHW in primary care would benefit from the addition of qualitative research to increase knowledge about the conditions (relating to person, profession, and practice) which facilitate or prevent behaviour change in PCPs by MHWs. This might be facilitated if the interventions were more specifically linked to a model of PCP clinical behaviour and decision making in mental health work.
What's new
| Date | Event | Description |
|---|---|---|
| 16 June 2010 | Amended | Typos corrected |
History
Protocol first published: Issue 4, 1997 Review first published: Issue 3, 2000
| Date | Event | Description |
|---|---|---|
| 12 November 2008 | New search has been performed | Review Updated Nov 2008 |
| 12 November 2008 | New citation required and conclusions have changed | Review has been divided into two reviews. The second will be published at a later date. |
| 10 October 2008 | Amended | Converted to new review format. |
| 1 February 2008 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
The review authors would like to thank Jeremy Grimshaw, Graham Mowatt, Alain Mayhew, and Emma Tavender of the Cochrane Effective Practice and Organisation of Care Group for advice and support throughout; Steve Rose (ex‐National Primary Care Research and Development Centre) and Doug Salzwedel for assistance with the literature searches; and Nick Kates, Marjukka Makela, Lisa Rubenstein, Luke Vale, Craig Ramsay, Sarah Hetrick, and Andy Oxman for their helpful comments on drafts of the review.
Appendices
Appendix 1. Original Search Strategy
| Given the broad range of study designs that are of relevance to Effective Practice and Organisation of Care Group (EPOC) reviews (i.e. RCTs, CBAs and ITSs) and the expectation that data of relevance to the present review might be included in studies with a different primary aim (e.g. those evaluating clinical outcome of management by MHWs), it was decided to use a broad strategy for the identification of studies based on the types of mental health professionals in the primary care setting rather than specific methodological keywords (except when searching specialist mental health databases). The searches described below were therefore of relatively low specificity. MEDLINE (1966 ‐ 1998), PsycInfo (1984 ‐ 1998) and EMBASE (1980 ‐ 1998) were searched using the following terms: (family pract* OR general pract* OR primary care OR primary health care) AND (counsel* OR psychotherap* OR clin* psy* or beh* therap* OR fam* therap* OR group therap* OR psychoanal* OR psychiat* OR cog* therap* OR psychodynam*) The Cochrane Controlled Trials Register was searched using the following terms: ((primary near care) OR (general near pract*) OR (fam* near pract*)) AND (counsel* OR psychotherap* OR (clin* near psy*) OR (beh* near therap*) OR (fam* near therap*) OR (group near therap*) OR psychoanal* OR psychiat* OR (cog* near therap*) OR psychodynam*) The EPOC register was searched using the following terms: primary (near) care (or) general (near) practitioner (or) general (near) practice (or) family (near) practice (or) family (near) practitioner (or) family (near) medicine and psychiat* (OR) psycho* (OR) mental* (OR) emot* The Counselling in Primary Care Trust CounselLit database was searched using the following search terms: random OR meta OR trial OR effectiveness OR efficacy OR outcome OR control OR evaluation OR review OR comparative 2. The references lists of all relevant studies were searched for further studies. Searches for the initial review were conducted between 18‐22 June 1998. Papers of potential relevance that were identified after this date through means other than electronic database searching were added to the list of studies 'awaiting assessment'. Given the broad range of study designs that are of relevance to Effective Practice and Organisation of Care Group (EPOC) reviews (i.e. RCTs, CBAs and ITSs) and the expectation that data of relevance to the present review might be included in studies with a different primary aim (e.g. those evaluating clinical outcome of management by MHWs), it was decided to use a broad strategy for the identification of studies based on the types of mental health professionals in the primary care setting rather than specific methodological keywords (except when searching specialist mental health databases). The searches described below were therefore of relatively low specificity. MEDLINE (1966 ‐ 1998), PsycInfo (1984 ‐ 1998) and EMBASE (1980 ‐ 1998) were searched using the following terms: (family pract* OR general pract* OR primary care OR primary health care) AND (counsel* OR psychotherap* OR clin* psy* or beh* therap* OR fam* therap* OR group therap* OR psychoanal* OR psychiat* OR cog* therap* OR psychodynam*) The Cochrane Controlled Trials Register was searched using the following terms: ((primary near care) OR (general near pract*) OR (fam* near pract*)) AND (counsel* OR psychotherap* OR (clin* near psy*) OR (beh* near therap*) OR (fam* near therap*) OR (group near therap*) OR psychoanal* OR psychiat* OR (cog* near therap*) OR psychodynam*) The EPOC register was searched using the following terms: primary (near) care (or) general (near) practitioner (or) general (near) practice (or) family (near) practice (or) family (near) practitioner (or) family (near) medicine and psychiat* (OR) psycho* (OR) mental* (OR) emot* The Counselling in Primary Care Trust CounselLit database was searched using the following search terms: random OR meta OR trial OR effectiveness OR efficacy OR outcome OR control OR evaluation OR review OR comparative 2. The references lists of all relevant studies were searched for further studies. Searches for the initial review were conducted between 18‐22 June 1998. Papers of potential relevance that were identified after this date through means other than electronic database searching were added to the list of studies 'awaiting assessment'. |
Appendix 2. Search strategies for the updated review
| CENTRAL #1MeSH descriptor Primary Health Care explode all trees #2MeSH descriptor Physicians, Family explode all trees #3MeSH descriptor Family Practice explode all trees #4family near/2 pract* #5general near/2 pract* #6primary near/2 care #7(#1 OR #2 OR #3 OR #4 OR #5 OR #6) #8counsel* #9psychotherap* #10clin* near/2 psy* #11beh* near/2 therap* #12group near/2 therap* #13psychoanal* #14psychiat* #15cog* near/2 therap* #16psychodynam* #17MeSH descriptor Counseling explode all trees #18MeSH descriptor Psychotherapy explode all trees #19MeSH descriptor Psychology, Clinical explode all trees #20MeSH descriptor Mental Health explode all trees #21MeSH descriptor Mental Disorders explode all trees #22(#8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21) #23(#7 AND #22) #24(#23), from 1998 to 2007 MEDLINE 1randomized controlled trial.pt. 2controlled clinical trial.pt. 3intervention studies/ 4experiment$.tw. 5(time adj series).tw. 6(pre test or pretest or (posttest or post test)).tw. 7random allocation/ 8impact.tw. 9intervention?.tw. 10chang$.tw. 11evaluation studies/ 12evaluat$.tw. 13effect?.tw. 14comparative studies/ 151 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 16Primary Health Care/ 17Family Practice/ 18(family adj2 pract$).mp. 19(general adj2 pract$).mp. 20(primary adj2 care).mp. 2116 or 17 or 18 or 19 or 20 22counsel$.mp. 23psychotherap$.mp. 24(clin$ adj2 psy$).mp. 25(beh$ adj2 therap$).mp. 26(group adj2 therap$).mp. 27psychoanal$.mp. 28psychiat$.mp. 29(cog$ adj2 therap$).mp. 30psychodynam$.mp. 31Counseling/ 32exp Psychotherapy/ 33Preventive Psychiatry/ or Community Psychiatry/ 34exp Psychology, Clinical/ 35exp Mental Health/ 36Mental Disorders/ 3722 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 3815 and 21 and 37 39limit 38 to yr="1998 ‐ 2007" EMBASE 1randomized controlled trial/ 2(randomised or randomized).tw. 3experiment$.tw. 4(time adj series).tw. 5(pre test or pretest or post test or posttest).tw. 6impact.tw. 7intervention?.tw. 8chang$.tw. 9evaluat$.tw. 10effect?.tw. 11compar$.tw. 121 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 13Primary Medical Care/ 14exp General Practice/ 15(family adj2 pract$).mp. 16(general adj2 pract$).mp. 17(primary adj2 care).mp. 1813 or 14 or 15 or 16 or 17 19counsel$.mp. 20psychotherap$.mp. 21(clin$ adj2 psy$).mp. 22(beh$ adj2 therap$).mp. 23(group adj2 therap$).mp. 24psychoanal$.mp. 25psychiat$.mp. 26(cog$ adj2 therap$).mp. 27psychodynam$.mp. 28exp Counseling/ 29exp PSYCHOTHERAPY/ 30exp PSYCHIATRY/ 31exp Mental Health/ 32exp Mental Disease/ 3319 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 3412 and 18 and 33 35limit 34 to yr="1998 ‐ 2007" CINHAL 1clinical trial/ 2(controlled adj (study or trial)).tw. 3(randomised or randomized).tw. 4(random$ adj1 (allocat$ or assign$)).tw. 5exp pretest‐posttest design/ 6exp quasi‐experimental studies/ 7comparative studies/ 8time series.tw. 9experiment$.tw. 10impact.tw. 11intervention?.tw. 12evaluat$.tw. 13effect?.tw. 1410 or 11 or 12 or 13 15exp Primary Health Care/ 16exp Family Practice/ 17(family adj2 pract$).mp. 18(general adj2 pract$).mp. 19(primary adj2 care).mp. 2015 or 16 or 17 or 18 or 19 21counsel$.mp. 22psychotherap$.mp. 23(clin$ adj2 psy$).mp. 24(beh$ adj2 therap$).mp. 25(group adj2 therap$).mp. 26psychoanal$.mp. 27psychiat$.mp. 28(cog$ adj2 therap$).mp. 29psychodynam$.mp. 30exp Counseling/ 31exp PSYCHOTHERAPY/ 32exp PSYCHIATRY/ 33exp Mental Health/ 34exp Mental Disorders/ 3521 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 3614 and 20 and 35 37limit 36 to yr="1998 ‐ 2007" PSYCINFO 1Clinical Trial/ 2exp Treatment Effectiveness Evaluation/ 3exp treatment outcomes/ 4experiment$.tw. 5(time adj series).tw. 6(pre test or pretest or (posttest or post test)).tw. 7intervention?.tw. 81 or 2 or 3 or 4 or 5 or 6 or 7 9exp Primary Health Care/ 10exp General Practitioners/ 11exp Family Medicine/ 12exp Family Physicians/ 13(family adj2 pract$).mp. 14(general adj2 pract$).mp. 15(primary adj2 care).mp. 169 or 10 or 11 or 12 or 13 or 14 or 15 17exp Counseling/ 18exp Psychotherapy/ 19exp Psychiatry/ 20exp Mental Health/ 21exp Mental Disorders/ 22counsel$.mp. 23psychotherap$.mp. 24(clin$ adj2 psy$).mp. 25(beh$ adj2 therap$).mp. 26(group adj2 therap$).mp. 27psychoanal$.mp. 28psychiat$.mp. 29(cog$ adj2 therap$).mp. 30psychodynam$.mp. 3117 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 328 and 16 and 31 33limit 32 to yr="1998 ‐ 2007" 34cost offset.mp. 35exp "Costs and Cost Analysis"/ or exp Health Care Costs/ or exp Health Care Utilization/ or exp "Cost Containment"/ 36 34 or 35 37 8 or 36 38 16 and 31 and 37 39 limit 38 to yr="1998 ‐ 2007" 40 39 not 33 |
Data and analyses
Comparison 1. Direct effects.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PCP consultations | 10 | 1061 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.30, ‐0.05] |
| 2 PCP psychotropic prescribing | 13 | 1299 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.56, 0.79] |
| 3 PCP prescribing costs | 7 | 701 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.22 [‐0.38, ‐0.07] |
| 4 PCP mental health referrals | 7 | 793 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.09, 0.20] |
| 5 PCP consultations | Other data | No numeric data | ||
| 6 PCP prescribing | Other data | No numeric data | ||
| 6.1 PCP prescribing ‐ psychotropics | Other data | No numeric data | ||
| 6.2 PCP prescribing ‐ non‐psychotropic or combined prescribing | Other data | No numeric data | ||
| 7 PCP referrals | Other data | No numeric data | ||
| 7.1 Mental health referrals | Other data | No numeric data | ||
| 7.2 Non‐mental health referrals | Other data | No numeric data | ||
| 7.3 All referrals | Other data | No numeric data | ||
| 8 Total costs | Other data | No numeric data | ||
| 9 PCP mental health referrals (sensitivity analysis on quality) | 6 | 639 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.07, 0.41] |
1.1. Analysis.
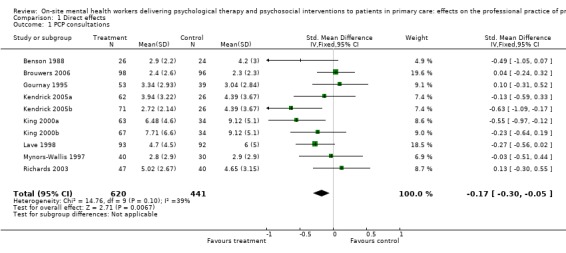
Comparison 1 Direct effects, Outcome 1 PCP consultations.
1.2. Analysis.
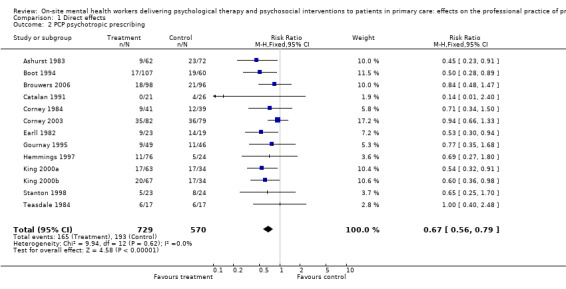
Comparison 1 Direct effects, Outcome 2 PCP psychotropic prescribing.
1.3. Analysis.
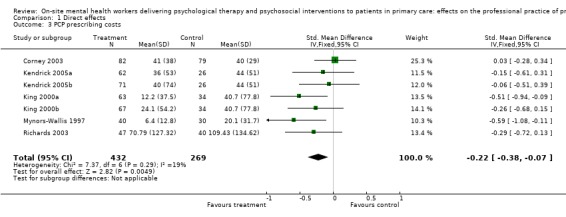
Comparison 1 Direct effects, Outcome 3 PCP prescribing costs.
1.4. Analysis.
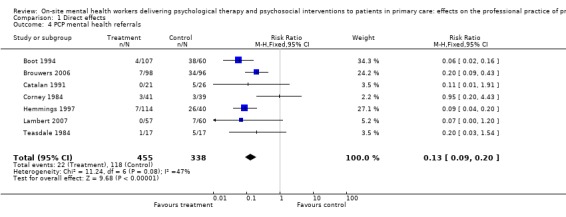
Comparison 1 Direct effects, Outcome 4 PCP mental health referrals.
1.5. Analysis.
Comparison 1 Direct effects, Outcome 5 PCP consultations.
| PCP consultations | |||
|---|---|---|---|
| Study | Study design | Outcomes | Results |
| Ashurst 1983 | Randomized controlled trial | GP consultations Average length of consultation | GP consultations 12 months post‐treatment Int 7 (n=112) Con 6.3 (n=121) Absolute change=0.7 Relative % change=11% Average length of consultation Int 10.4 (n=112) Con 10.1 (n=121) Absolute change=0.3 Relative % change=3% Total GP time Int 64 Con 59 Absolute change=5 Relative % change=9% Reported t=0.91, df=231, p=0.36 |
| Ashworth 2000 | Controlled before‐after study | GP consultations | GP consultations 1 year comparison 2 Pre treatment Int 6.33 (5.67) (n=75) Con 1.6 (1.59) (n=75) Post treatment Int 7.08 (6.33) (n=75) Con 1.41 (1.27) (n=75) Absolute change post 5.67 Relative % change 402.1 Absolute change from baseline Int 0.75, Con ‐0.19 Difference in absolute change from baseline 0.94 GP consultations 2 year comparison 2 Pre treatment Int 6.33 (5.67) (n=75) Con 1.6 (1.59) (n=75) Post treatment 3.93 (3.58) (n=71) Con 1.71 (2.15) (n=63) Absolute change post 2.22 Relative % change 129.8 Absolute change from baseline Int ‐2.4, Con 0.11 Difference in absolute change from baseline ‐2.51 GP consultations 1 year comparison 1 Pre treatment Int 7.23 (6.67) (n=30) Con 4 (3.98) (n=30) Post treatment Int 8.23 (7.54) (n=30) Con 5 (3.36) (n=30) Absolute change post 3.23 Relative % change 64.6 Absolute change from baseline Int 1, Con 1 Difference in absolute change from baseline 0 GP consultations 2 year comparison 1 Pre treatment Int 7.23 (6.67) (n=30) Con 4 (3.98) (n=30) Post treatment Int 4.74 (4.43) (n=27) Con 4.48 (3.88) (n=27) Absolute change post 0.26 Relative % change 5.8 Absolute change from baseline Int ‐2.49, Con 0.48 Difference in absolute change from baseline ‐2.97 |
| Basler 1990 | Controlled before‐after study | GP consultations | GP consultations 3 months pre‐treatment Int Pre 7.08 (3.43) (n=25?) Con Pre 6.15 (3.07) (n=20?) 3 months post‐treatment Int 3.90 (1.13) (n=25?) Con 7.8 (4.14) (n=20?) Absolute change=‐3.9 Relative % change=‐50% Absolute change from baseline Int ‐3.18 Con 1.65 Difference in absolute change from baseline=‐4.83 Reported chisq=22.43, df=1, p<0.01 |
| Benson 1988 | Randomized controlled trial | GP consultations | Consultations 12 months pre‐treatment Int 4.6 (2.8) (n=26) Con 5.8 (5.3) (n=24) 6 months pre‐treatment Int 5.5 (3.3) (n=26) Con 5.0 (3.4) (n=24) 1st 6 months during treatment Int 2.9 (2.2) (n=26) Con 4.2 (3.0) (n=24) Absolute change=‐1.3 Relative % change=‐31% Absolute change from baseline Int ‐1.7 Con ‐1.6 Difference in absolute change from baseline=‐0.1 2nd 6 months during treatment Int 2.5 (1.6) (n=26) Con 3.2 (2.8) (n=24) Absolute change=‐0.7 Relative % change=‐22% Absolute change from baseline Int ‐2.1 Con ‐2.6 Difference in absolute change from baseline=0.5 6 months post‐treatment Int 1.5 (1.5) (n=26) Con 3.1 (2.5) (n=24) Absolute change=‐1.6 Relative % change=‐52% Absolute change from baseline Int ‐3.1 Con ‐2.7 Difference in absolute change from baseline=‐0.4 Reported t=2.84, df=36, p<0.01 versus treatment group 12 months post‐treatment Int 1.6 (n=14) Con 3.0 (n=19) Absolute change=‐1.4 Relative % change=‐47% Absolute change from baseline Int ‐3.0 Con ‐2.8 Difference in absolute change from baseline=‐0.2 (s.d. not given) |
| Blakey 1986 | Controlled before‐after study | GP consultations | Note: Data presented in form of tables only |
| Boot 1994 | Randomized controlled trial | GP consultations | Consultations 6 weeks Int 54/107 (51%) Con 39/60 (65%) Absolute change=‐14% Relative % change=‐22% Reported p=0.1 (chisq) |
| Brantley 1986 | Controlled before‐after study | GP consultations | FP visits 12m pre treatment Int 9.14 (8.59) (n=21) Con 5.52 (4.25) (n=21) 12 months post‐treatment Int 5.95 (6.26) (n=21) Con 4.38 (3.35) (n=21) Absolute change=1.57 Relative % change=36% Absolute change from baseline Int ‐3.19 Con ‐1.14 Difference in absolute change=‐2.05 Int greater decrease than con (reported z=‐1.891, p<0.05) |
| Brouwers 2006 | Randomized controlled trial | GP consultations | GP consultations Post treatment Int 2.4 (2.6) (n=98) Con 2.3 (2.3) (n=96) Absolute change post 0.1 Relative % change 4.3 GP surgery contacts Post treatment Int 5 (5.1) (n=96) Con 5.7 (3.3) (n=96) Absolute change post ‐0.7 Relative % change ‐12.3 GP telephone contacts Post treatment Int 0.7 (1.1) (n=96) Con 0.6 (1.3) (n=96) Absolute change post 0.1 Relative % change 16.7 GP home contacts Post treatment 0 (0.2) (n=96) Con 0 (0.5) (n=96) Absolute change post 0 Relative % change NA GP minor surgery contacts Post treatment Int 0.5 (0.8) (n=96) Con 0.5 (1) (n=96) Absolute change post 0 Relative % change 0.0 GP prescription contacts Post treatment Int 2.6 (4.1) (n=96) Con 3.3 (4.6) (n=96) Absolute change post ‐0.7 Relative % change ‐21.2 |
| Bruce 1998 | Controlled before‐after study | GP consultations | GP mental health Pre treatment Int 1.6 (n=16) Con 3.3 (n=11) Post treatment Int 0.4 (n=16) Con 2.3 (n=11) Absolute change post ‐1.9 Relative % change ‐82.6 Absolute change from baseline Int ‐1.2, Con ‐1 Difference in absolute change from baseline ‐0.2 p<0.05 GP physical health Pre treatment Int 3 (n=16) Con 3.2 (n=11) Post treatment Int 3.8 (n=16) Con 3.6 (n=11) Absolute change post 0.2 Relative % change 5.6 Absolute change from baseline Int 0.8, Con 0.4 Difference in absolute change from baseline 0.4 GP other Pre treatment Int 3.6 (n=16) Con 1.8 (n=11) Post treatment Int 2.8 (n=16) Con 1.5 (n=11) Absolute change post 1.3 Relative % change 86.7 Absolute change from baseline Int ‐0.8, Con ‐0.3 Difference in absolute change from baseline ‐0.5 Practice nurse Pre treatment Int 14.8 (n=16) Con 8.1 (n=11) Post treatment Int 18.4 (n=16) Con 3.6 (n=11) Absolute change post 4.8 Relative % change 35.3 Absolute change from baseline Int 3.6 Con 5.5 Difference in absolute change from baseline‐1.9 Total GP Pre treatment Int 8.43 (n=16) Con 8.36 (n=11) Post treatment Int 6.93 (n=16) Con 7.73 (n=11) Absolute change post ‐0.8 Relative % change ‐10.3 Absolute change from baseline Int ‐1.5, Con ‐0.63 Difference in absolute change from baseline ‐0.87 |
| Catalan 1991 | Randomized controlled trial | GP consultations | Median consultations 4 weeks Int 3 (n=21) Con 2 (n=26) 5‐10 weeks Int 2 (n=21) Con 3 (n=26) 11‐28 weeks Int 1 (n=21) Con 3 (n=26) |
| Corney 1984 | Randomized controlled trial | GP consultations | Note: No data presented although stated that no significant differences were found 12 months post treatment |
| Corney 2003 | Randomized controlled trial | GP consultations | GP consultation 6 months Pre treatment Int 97.8% (n=91) Con 97.8% (n=89) Post treatment Int 92.7% (n=82) Con 98.7% (n=79) Absolute change Post treatment‐6 Relative % change ‐6.1 Absolute change from baseline Int ‐5.1, Con 0.9 Difference in absolute change from baseline ‐6 PN consultation 6 months Pre treatment Int 48.4% (n=91) Con 57.3 (n=89) Post treatment Int 42.7% (n=82) Con 39.2% (n=79) Absolute change Post treatment 3.5 Relative % change 8.9 Absolute change from baseline Int ‐5.7, Con ‐18.1 Difference in absolute change from baseline 12.4 GP consultation 12 months Pre treatment Int 97.8% (n=91) Con 97.8% (n=89) Post treatment Int 90.7% (n=75) Con 95.6% (n=68) Absolute change Post treatment ‐4.9 Relative % change ‐5.1 Absolute change from baseline Int ‐7.1, Con ‐2.2 Difference in absolute change from baseline ‐4.9 PN consultation 12 months Pre treatment Int 48.4% (n=91) Con 57.3% (n=89) Post treatment Int 34.7% (n=75) Con 35.3% (n=68) Absolute change Post treatment ‐0.6 Relative % change ‐1.7 Absolute change from baseline Int ‐13.7, Con ‐22 Difference in absolute change from baseline 8.3 |
| Earll 1982 | Randomized controlled trial | GP consultations | GP consultations Treatment Int 3.4 Con 2.8 Absolute change=0.6 Relative % change=21% Reported n.s. 7m follow up Int 5.6 Con 5.2 Absolute change=0.4 Relative % change=8% Reported n.s. |
| Ginsberg 1984 | Randomized controlled trial | GP consultations and costs of consultations | Consultations 12 months pre‐treatment Int 5.7 (n=19) Con 6.4 (n=23) 12 months post‐treatment Int 4.4 (n=19) Con 7.0 (n=23) Absolute change=‐2.6 Relative % change=‐37% Absolute change from baseline Int ‐1.3 Con 0.6 Difference in absolute change from baseline=‐1.9 (no sds or tests reported) Home visits 12 months pre‐treatment Int 0.14 (n=19) Con 0.18 (n=23) 12 months post‐treatment Int 0.0 (n=19) Con 0.04 (n=23) Absolute change=‐0.04 Relative % change=‐100% Absolute change from baseline Int ‐0.14 Con ‐0.14 Difference in absolute change from baseline=0 (no sds or tests reported) Costs of GP visits 12 months pre‐treatment Int £8.00 (n=22) Con £9.00 (n=26) 12 months post treatment Int £6.27 (n=22) Con £9.10 (n=26) Absolute change=‐2.83 Relative % change=‐‐31% Absolute change from baseline Int ‐1.73 Con 0.1 Difference in absolute change from baseline=‐1.83 |
| Gournay 1995 | Randomized controlled trial | GP consultations | Consultations 6 months pre‐treatment Int 4.37 (3.46) (n=53?) Con 5.30 (4.01) (n=39) 6 months post‐treatment Int 3.34 (2.93) (n=53?) Con 3.04 (2.84) (n=39) Absolute change=‐0.3 Relative % change=‐10% Absolute change from baseline Int‐1.03 Con ‐2.26 Difference in absolute change from baseline=1.23 Authors reported that reduction in control significant over time (p<0.05), n.s. between int and con |
| Harvey 1998 | Randomized controlled trial | GP consultations and costs of consultations | Mean GP time 4 months Int 0.63 hours Con 1.50 hours Absolute change=‐0.87 Relative % change=‐58% (no s.d. or tests reported) Costs of GP time Int £15.75 Con £28.75 Absolute change=‐£13 Relative % change=‐45% |
| Kendrick 2005a | Randomized controlled trial | GP consultations and costs of consultations | GP surgery consultations 26 weeks Post treatment Int 3.94 (3.22) (n=62) Con 4.39 (3.67) (n=51) Absolute change Post treatment ‐0.45 Relative % change ‐10.3 GP surgery consultations costs 26 weeks Post treatment Int 81 (67) (n=62) Con 91 (76) (n=51) Absolute change Post treatment ‐10 Relative % change ‐11.0 Home visits 26 weeks Post treatment Int 0.05 (0.28) (n=62) Con 0.04 (0.2) (n=51) Absolute change Post treatment 0.01 Relative % change 25.0 Home visits costs 26 weeks Post treatment Int 3 (18) (n=62) Con 3 (12) (n=51) Absolute change Post treatment 0 Relative % change 0.0 CMHN telephone consultations 26 weeks Post treatment Int 0.63(1.76) (n=62) Con 0.27 (0.69) (n=51) Absolute change Post treatment 0.36 Relative % change 133.3 Telephone consultations costs 26 weeks Post treatment Int 15 (42) (n=62) Con 7 (16) (n=51) Absolute change Post treatment 8 Relative % change 114.3 PN surgery consultations costs 26 weeks Post treatment Int 0.4 (0.73) (n=62) Con 0.48 (0.7) (n=51) Absolute change Post treatment ‐0.08 Relative % change ‐16.7 PN surgery consultations costs 26 weeks Post treatment Int 4 (8) (n=62) Con 5 (7) (n=51) Absolute change Post treatment ‐1 Relative % change ‐20.0 |
| Kendrick 2005b | Randomized controlled trial | GP consultations and costs of consultations | GP surgery consultations 26 weeks Post treatment Int 2.72(2.14) (n=71) Con 4.39 (3.67) (n=51) Absolute change Post treatment ‐1.67 Relative % change ‐38.0 GP surgery consultations costs 26 weeks Post treatment Int 56 (44) (n=71) Con 91(76) (n=51) Absolute change Post treatment ‐35 Relative % change ‐38.5 Home visits 26 weeks Post treatment Int 0.11(0.65) (n=71) Con 0.04 (0.2) (n=51) Absolute change Post treatment 0.07 Relative % change 175.0 Home visits costs 26 weeks Post treatment Int 7 (41) (n=71) Con 3 (12) (n=51) Absolute change Post treatment 4 Relative % change 133.3 Telephone consultations 26 weeks Post treatment Int 0.49(1.58) (n=71) Con 0.27 (0.69) (n=51) Absolute change Post treatment 0.22 Relative % change 81.5 Telephone consultations costs 26 weeks Post treatment Int 12 (38) (n=71) Con 7 (16) (n=51) Absolute change Post treatment 5 Relative % change 71.4 PN surgery consultations costs 26 weeks Post treatment Int 0.56(1.08) (n=71) Con 0.48 (0.7) (n=51) Absolute change Post treatment 0.08 Relative % change 16.7 PN surgery consultations costs 26 weeks Post treatment Int 6 (11) (n=71) Con 5 (7) (n=51) Absolute change Post treatment 1 Relative % change 20.0 |
| King 2000a | Randomized controlled trial | GP consultations and costs of consultations | GP surgery 12 months Post treatment Int 6.48 (4.6) (n=63) Con 9.12 (5.1) (n=67) Absolute change post ‐2.64 Relative % change ‐28.9 GP home visits 12 months Post treatment Int 0.03 (0.18) (n=63) Con 0.05 (0.27) (n=67) Absolute change post ‐0.02 Relative % change ‐40.0 PN 12 months Post treatment Int 0.69 (0.95) (n=63) Con 0.53 (1.1) (n=67) Absolute change post 0.16 Relative % change 30.2 |
| King 2000b | Randomized controlled trial | GP consultations and costs of consultations | GP surgery 12 months Post treatment Int 7.71 (6.6) (n=67) Con 9.12 (5.1) (n=67) Absolute change post ‐1.41 Relative % change ‐15.5 GP home visits 12 months Post treatment Int 0.04 (0.27) (n=67) Con 0.05 (0.27) (n=67) Absolute change post ‐0.01 Relative % change ‐20.0 PN 12 months Post treatment Int 0.41 (0.68) (n=67) Con 0.53 (1.1) (n=67) Absolute change post ‐0.12 Relative % change ‐22.6 |
| Lave 1998 | Randomized controlled trial | GP consultations and costs of consultations | Non protocol consultations 12 months Post treatment Int 4.7(4.5) (n=93) Con 6 (5) (n=92) Absolute change post ‐1.3 Relative % change ‐21.7 Non protocol consultations costs Post treatment Int 308.04 (353.2) (n=93) Con 553.2 (490.48) (n=92) Absolute change post ‐245.16 Relative % change ‐44.3 |
| Lyon 1993 | Controlled before‐after study | GP consultations | GP consultations 3 months pre‐treatment Int 8.6 (n=38) Con 9.1 (n=33) 3 months post‐treatment Int 4.6 (n=38) Con 7.8 (n=33) Absolute change=‐3.2 Relative % change=‐41% Absolute change from baseline Int ‐4.0 Con ‐1.3 Differences in pre‐post change=‐2.7 No tests reported |
| Martin 1985 | Controlled before‐after study | GP consultations | GP consultations 12 months pre‐treatment Int 7.8 (n=87) Con 3.4 (n=87) 12 months post‐treatment Int 7.4 (n=87) Con 2.6 (n=87) Absolute change=4.8 Relative % change=185% Absolute change from baseline Int ‐0.4 Con ‐0.8 Difference in pre‐post change=0.4 No tests reported |
| Mynors‐Wallis 1997 | Randomized controlled trial | GP consultations | GP consultations During treatment Int 2.2 (1.8) (n=40) Con 2.3 (1.5) (n=30) Absolute change=‐0.1 Relative % change=‐4% Reported p=0.844 4 months Int 2.8 (2.9) (n=40) Con 2.9 (2.9) (n=30) Absolute change=‐0.1 Relative % change=‐4% Reported p=0.975 Treatment plus follow up combined Int 5.0 (4.1) (n=40) Con 5.1 (3.7) (n=30) Absolute change=‐0.1 Relative % change=‐2% Reported p=0.914 Cost of consultations During treatment Int £28.1 (22.9) (n=40) Con £29.3 (19.2) (n=30) Absolute change=‐£1.2 Relative % change=‐4% p=0.844 Cost of consultations 4 months Int £36.2 (37.7) (n=40) Con £36.5 (37.5) (n=30) Absolute change=‐£0.3 Relative % change=‐1% p=0.975 Treatment and 4 months combined Int £63.9 (52.0) (n=40) Con £65.2 (46.9) (n=30) Absolute change=‐£1.3 Relative % change=‐2% p=0.914 |
| Richards 2003 | Randomized controlled trial | GP consultations and costs of consultations | GP consultations 12 months Post treatment Int 5.02 (2.67) (n=47) Con 4.65 (3.15) (n=40) Absolute change Post treatment 0.37 Relative % change 8.0 GP consultation costs 12 months Post treatment Int 57.45 (43.87) (n=47) Con 84.6 (55.92) (n=40) Absolute change Post treatment ‐27.15 Relative % change ‐32.1 Mean difference ‐27.15, 95% CI ‐48.44 to 5.87, p=0.013 |
| Robson 1984 | Randomized controlled trial | GP consultations | Consultations 10 weeks to 6 months Int (1‐2) 35 (3‐4) 20 (5+) 22 (n=77) Con (1‐2) 60 (3‐4) 40 (5+) 30 (n=130) Reported p=0.0008 by chisq test |
| Spurgeon 2007 | Controlled before‐after study | GP consultations | GP consultations 12 months Pre treatment Int 52.9 Con 42.18 Post treatment Int 42.5 Con 49.16 Absolute change post ‐6.66 Relative % change ‐13.5 Absolute change from baseline Int ‐10.4, Con 6.98 Difference in absolute change from baseline ‐17.38 Home visits 12 months Pre treatment Int 0.5 Con 1.9 Post treatment Int 0.48 Con 1.86 Absolute change post ‐1.38 Relative % change ‐74.2 Absolute change from baseline Int ‐0.02 Con ‐0.04 Difference in absolute change from baseline 0.02 |
| Stanton 1998 | Randomized controlled trial | GP consultations | Consultations 6 months Int 0‐2 (30%) 3‐4 (22%) 5+ (35%) Missing (13%) (n=23) Con 0‐2 (46%) 3‐4 (25%) 5+ (12%) Missing (17%) (n=24) No tests reported |
| Sumathipala 2000 | Randomized controlled trial | GP consultations | Visits (adjusted means) 6 months Pre treatment Int 6.3 (4) Con 7.7(6.3) Post treatment (adjusted) Int 3.1 (n=34) Con 7.9 (n=34) Absolute change post ‐4.8 Relative % change ‐60.8 Absolute change from baseline Int ‐3.2, Con 0.2 Difference in absolute change from baseline ‐3.4 Difference in means 6.3 (95% CI 1.8 to 11.0, p<0.001) |
| Teasdale 1984 | Randomized controlled trial | GP consultations | Consultations During treatment Int 0.51 (n=17) Con 1.07 (n=17) Absolute change=‐0.56 Relative % change=‐52% Reported t=2.11, p<0.05 3 months Int 0.41 (n=17) Con 0.41 (n=17) Absolute change=0 Relative % change=0% No s.d.s or tests reported |
1.6. Analysis.
Comparison 1 Direct effects, Outcome 6 PCP prescribing.
| PCP prescribing | |||
|---|---|---|---|
| Study | Study design | Outcomes | Results |
| PCP prescribing ‐ psychotropics | |||
| Ashurst 1983 | Randomized controlled trial | Psychotropic prescribing | % on tranquilisers 12 months post treatment Int 14.5% (n=62) Con 31.9% (n=72) Absolute change=‐17.4% Relative % change=‐55% Reported chisq=4.65, df=1, p=0.03 % on antidepressants 12 months post treatment Int 17.1% (n=41) Con 18.2% (n=55) Absolute change=‐1.1% Relative % change=‐6% Reported chisq=0, df=1, p=1.0 |
| Ashworth 2000 | Controlled before‐after study | Psychotropic prescribing | Change in medication 1 year Pre treatment Int 30 (n=30) Con 30 (n=30) Post treatment Int 14 (n=30) Con 29 (n=30) Absolute change post ‐15 Relative % change ‐51.7 Absolute change from baseline Int ‐16, Con ‐1 Difference in absolute change from baseline ‐15 Change in medication 2 years Pre Int 27 (n=27) Con 27 (n=27) Post treatment Int 16 (n=27) Con 23 (n=27) Absolute change post ‐7 Relative % change ‐30.4 Absolute change from baseline Int ‐11, Con ‐4 Difference in absolute change from baseline ‐7 Change in medication 1 year comparison 2 Pre treatment Int 30 (n=75) Con 0 (n=75) Post treatment Int 24 (n=75) Con 0 (n=75) Absolute change post 24 Relative % change 0 Absolute change from baseline Int ‐6, Con 0 Difference in absolute change from baseline ‐6 Change in medication 2 years comparison 2 Pre treatment Int 24 (n=75) Con 0 (n=75) Post treatment Int 27 (n=71) Con 4 (n=63) Absolute change post 23 Relative % change, 575.0 Absolute change from baseline Int 3, Con 4, Difference in absolute change from baseline ‐1 |
| Blakey 1986 | Controlled before‐after study | Psychotropic prescribing | Note: Data presented in form of tables only |
| Boot 1994 | Randomized controlled trial | Psychotropic prescribing | Overall psychotropic prescriptions 6 weeks Int: 17/107 (16%) Con: 19/60 (32%) Absolute change=‐16% Relative % change=‐50% Reported chisq=4.8, df=1, p=0.029 Antidepressants Int: 10/107 (9%) Con: 14/60 (23%) Absolute change=‐14% Relative % change=‐61% Reported chisq=5, df=1, p=0.02 Anxiolytic prescriptions Int: 6 (9%) Con: 3 (8%) Absolute change=1% Relative % change=13% Reported Fisher's exact p=0.28 |
| Brodaty 1983 | Randomized controlled trial | Psychotropic prescribing | Psychotropics Pre‐treatment Int 0.83 (0.71) (n=18) Con 0.50 (0.89) (n=20) No test reported Post‐treatment Int 0.94 (0.87) Con 0.50 (0.69) Absolute change=0.44 Relative % change=88% Absolute change from baseline Int 0.11 Con 0.0 Difference in absolute change in baseline=0.11 No test reported 12 month Int 0.75 (0.86) Con 0.40 (0.60) Absolute change=0.35 Relative % change=88% Absolute change from baseline Int ‐0.08 Con ‐0.10 Difference in absolute change in baseline=0.02 No test reported |
| Brouwers 2006 | Randomized controlled trial | Psychotropic prescribing | Prescribed psychotropic 18 months Post treatment Int 18.4% (n=98) Con 21.9% (n=96) Absolute change post ‐3.5 Relative % change ‐16.0 Psychotropic medication prescription Post treatment Int 1.1 (3.9) (n=96) Con 1.4 (4.3) (n=96) Absolute change post ‐0.3 Relative % change ‐21.4 |
| Catalan 1991 | Randomized controlled trial | Psychotropic prescribing | Prescriptions (absolute numbers) 5‐10 weeks Int 1 (n=21) (5%) Con 5 (n=26) (19%) Absolute change=‐14% Relative % change=‐74% 11‐28 weeks Int 0 (n=21) (0%) Con 4 (n=26) (15%) Absolute change=‐15% Relative % change=‐100% No significance tests reported |
| Corney 1984 | Randomized controlled trial | Psychotropic prescribing | Psychotropic prescribing Pre‐treatment Int 80.5% (n=41) Con 82.1% (n=39) 6 months Int 22% (9/41) Con 31% (12/39) Absolute change=‐9% Relative % change=‐29% Absolute change from baseline Int ‐58.5% Con ‐51.1% Difference in absolute change from baseline=‐7% Reported n.s. Time on psychotropic drugs Int None (19.5%) 1 month (39.0%) 2‐3 months (14.6%) 4‐6 months (26.8%) (n=41) Con None (17.9%), 1 month (38.5%), 2‐3 months (15.4%), 4‐6 months(28.2%) (n=39) |
| Corney 2003 | Randomized controlled trial | Psychotropic prescribing | Mental health medication 12 months (data from page 46, column 1) Pre treatment Int 50% (n=90) Con 33.7% (n=89) 6 months Int 42.7% (n=82) Con 45.6% (n=79) Absolute change post ‐2.9 Relative % change ‐6.4 Absolute change from baseline Int ‐7.3, Con 11.9 Difference in absolute change from baseline ‐19.2 12 months Int 40.0% (n=75) Con 38.2% (n=68) Absolute change post 1.8 Relative % change 4.7 Absolute change from baseline Int ‐10.0, Con 4.5 Difference in absolute change from baseline ‐14.5 Mental health medication costs 6 months Pre treatment Int 11 (24) Con 16 (32) Post treatment Int 41 (38) Con 40 (29) Absolute change post 1 Relative % change 2.5 Absolute change from baseline Int 30, Con 24 Difference in absolute change from baseline 6 Mental health medication costs 12 months Pre treatment Int 11 (24) Con 16 (32) Post treatment Int 50 (54) Con 66 (77) Absolute change post ‐16 Relative % change ‐24.2 Absolute change from baseline Int 39, Con 50 Difference in absolute change from baseline ‐11 |
| Earll 1982 | Randomized controlled trial | Psychotropic prescribing | Psychotropic prescriptions Post‐treatment Int 39% (n=23) Con 74% (n=19) Absolute change=‐35% Relative % change=‐47% Reported p<0.05 7 month follow up Int 65% (n=23) Con 74% (n=19) Absolute change=‐9% Relative % change=‐12% Reported n.s. |
| Gournay 1995 | Randomized controlled trial | Psychotropic prescribing | Drugs and dispensing Baseline Int 4/49 (8%) Con 3/46 (7%) 24 weeks Int 9/49 (18%) Con 11/46 (24%) Absolute change=‐6% Relative % difference=‐25% Absolute change from baseline Int 10% Con 17% Difference in absolute change from baseline=‐7% |
| Hemmings 1997 | Randomized controlled trial | Psychotropic prescribing | Psychotropics Baseline Int 34/136 (25%) Con 17/52 (33%) 4 months Int 23/114 (20%) Con 13/40 (33%) Absolute change=‐13% Relative % change=‐39% Absolute change from baseline Int ‐5% Con 0% Difference in absolute change in baseline =‐5% Reported chisq=2.9, df=1, p=0.09 8 months Int 11/76 (15%) Con 5/24 (21%) Absolute change=‐6% Relative % change=‐29% Absolute change from baseline Int ‐10% Con ‐12% Difference in absolute change in baseline =2% Reported chisq=0.07, df=1, p=0.8 |
| King 2000a | Randomized controlled trial | Psychotropic prescribing | Antidepressants 12 months Post treatment Int 27% (n=63) Con 49.3% (n=67) Absolute change post ‐22.3 Relative % change ‐45.2 Minor tranquilisers 12 months Post treatment Int 6.3% (n=63) Con 17.9% (n=67) Absolute change post ‐11.6 Relative % change ‐64.8 Beta blockers 12 months Post treatment Int 7.9% (n=63) Con 4.5% (n=67) Absolute change post 3.4 Relative % change 75.6 Major tranquilisers 12 months Post treatment Int 0% (n=63) Con 0% (n=67) Absolute change post 0 Relative % change NA Medication costs 12 months Post treatment Int 12.2 (37.5) (n=63) Con 40.7 (77.8) (n=67) Absolute change post ‐28.5 Relative % change ‐70.0 |
| King 2000b | Randomized controlled trial | Psychotropic prescribing | Antidepressants 12 months Post treatment Int 29.9% (n=67) Con 49.3% (n=67) Absolute change post ‐19.4 Relative % change ‐39.4 Minor tranquilisers 12 months Post treatment Int 14.9% (n=67) Con 17.9% (n=67) Absolute change post ‐3 Relative % change ‐16.8 Beta blockers 12 months Post treatment Int 3% (n=67) Con 4.5% (n=67) Absolute change post ‐1.5 Relative % change ‐33.3 Major tranquilisers 12 months Post treatment Int 1.5% (n=67) Con 0% (n=67) Absolute change post 1.5 Relative % change NA Medication costs 12 months Post treatment Int 24.1(54.2) (n=67) Con 40.7 (77.8) (n=67) Absolute change post ‐16.6 Relative % change ‐40.8 |
| Lyon 1993 | Controlled before‐after study | Psychotropic prescribing | Tranquilisers (numbers of patients) 3m pre‐treatment Int 6/38 (16%) Con 7/33 (21%) 3 months post treatment Int 3/38 (8%) Con 6/33 (18%) Absolute change=‐10% Relative % change=‐56% Absolute change from baseline Int ‐8% Con ‐3% Difference in absolute change from baseline=‐5% Antidepressants Pre‐treatment Int 3/38 (8%) Con 0/33 (0%) 3 months post‐treatment Int 4/38 (11%) Con 8/33 (24%) Absolute change=‐13% Relative % change=‐54% Absolute change from baseline Int 3% Con 24% Difference in absolute change from baseline=‐21% |
| Martin 1985 | Controlled before‐after study | Psychotropic prescribing | Psychotropic prescriptions 12 months pre‐treatment Int 1.86 Con 0.62 12 months post‐treatment Int 2.91 Con 0.64 Absolute change=2.27 Relative % change=355% Absolute change from baseline Int 1.05 Con 0.02 Difference in absolute change from baseline=1.03 |
| Mynors‐Wallis 1997 | Randomized controlled trial | Psychotropic prescribing | Cost of medications During treatment Int £3.8 (9.0) (n=40) Con £6.8 (11.9) (n=30) Absolute change=‐£3.0 Relative % change=‐44% Reported p=0.251 Cost of medications 4 months post‐treatment Int £2.5 (6.6) (n=40) Con £13.3 (23.3) (n=30) Absolute change=‐£10.8 Relative % change=‐81% Reported p=0.008 Cost of medications (from entry) Int £6.4 (12.8) (n=40) Con £20.1 (31.7) (n=30) Absolute change=‐13.7 Relative % change=‐68% Reported p=0.018 |
| Robson 1984 | Randomized controlled trial | Psychotropic prescribing | Prescribing (category A ‐ psychotropics) 3 months Int £2.00 Con £4.10 Absolute change=‐£2.1 Relative % change=‐51% Reported p=0.004 6 months Int £3.77 Con £6.34 Absolute change=‐£2.57 Relative % change=‐41% Reported p=0.02 12 months Int £5.63 Con £9.69 Absolute change=‐£4.06 Relative % change=‐42% Reported p=0.01 |
| Stanton 1998 | Randomized controlled trial | Psychotropic prescribing | Psychotropics prescribed 6 months Int 0 (65%) 1+ (22%) Missing (13%) (n=23) Con 0 (50%) 1+ (33%) Missing (17%) (n=24) Absolute change=‐11% Relative % change=‐33% No tests |
| Teasdale 1984 | Randomized controlled trial | Psychotropic prescribing | Antidepressant medication Baseline Int 11/17 (65%) Con 10/17 (59%) Post‐treatment Int (increase) 0 (same) 3 (decrease) 3 (none) 5 (% medication = 6/17=35%) Con (increase) 2 (same) 3 (decrease) 1 (none) 4 (% medication = 6/17=35%) Absolute change=0% Relative % change=0% Absolute change from baseline Int ‐30% Con ‐24% Difference in absolute change from baseline=‐6% 3 months Int (increase) 0 (same) 4 (decrease) 2 (none) 5 (% medication = 6/17=35%) Con (increase) 1 (same) 4 (decrease) 0 (none) 5 (% medication = 5/17=29%) Absolute change=6% Relative % change=9% Absolute change from baseline Int ‐30% Con ‐30% Difference in absolute change from baseline=0 No tests reported |
| PCP prescribing ‐ non‐psychotropic or combined prescribing | |||
| Brodaty 1983 | Randomized controlled trial | Combined prescribing | Total tablet types Pre‐treatment Int 3.06 (1.86) (n=18) Con 2.35 (1.76) (n=20) No test reported Post‐treatment Int 3.00 (2.03) Con 2.05 (1.57) Absolute change=0.95 Relative % change=46% Absolute change from baseline Int ‐0.06 Con ‐0.30 Difference in absolute change from baseline=0.24 No test reported 12 month Int 3.19 (1.91) Con 2.05 (1.99) Absolute change=1.14 Relative % change=56% Absolute change from baseline Int 0.13 Con ‐0.30 Difference in absolute change from baseline=0.43 No test reported |
| Brouwers 2006 | Randomized controlled trial | Non psychotropic prescribing | Prescribed non‐psychotropic 18 months Post treatment Int 60.2% (n=98) Con 50% (n=96) Absolute change post 10.2 Relative % change 20.4 Non‐psychotropic medication prescription Post treatment Int 4.4 (7.5) (n=96) Con 3.9 (7.1) (n=96) Absolute change post 0.5 Relative % change 12.8 |
| Corney 2003 | Randomized controlled trial | Combined prescribing | Medication 6 months Pre treatment Int 49.5% (n=91) Con 34.8% (n=89) Post treatment Int 42.7% (n=82) Con 45.6% (n=79) Absolute change Post treatment ‐2.9 Relative % change ‐6.4 Absolute change from baseline Int ‐6.8, Con 10.8 Difference in absolute change from baseline ‐17.6 Medication 12 months Pre treatment Int 49.5% (n=91) Con 34.8% (n=89) Post treatment Int 40% (n=75) Con 42.6% (n=68) Absolute change Post treatment‐2.6 Relative % change ‐6.1 Absolute change from baseline Int ‐9.5, Con 7.8 Difference in absolute change from baseline ‐17.3 |
| Earll 1982 | Randomized controlled trial | Non‐psychotropic prescribing | Other medication Post‐treatment Int 61% (n=23) Con 42% (n=19) Absolute change=19% Relative % change=45% Reported n.s. 7 months Int 87% (n=23) Con 63% (n=19) Absolute change=24% Relative % change=38% Reported n.s. |
| Ginsberg 1984 | Randomized controlled trial | Combined prescribing | Costs of drugs and dispensing 12 months pre‐treatment Int £12.45 (n=22) Con £6.27 (n=26) 12 months post‐treatment Int £9.75 (n=22) Con £6.33 (n=26) Absolute change=£3.42 Relative % change=54% Absolute change from baseline Int ‐£2.7 Con £0.06 Difference in absolute change from baseline=‐£2.76 Reported n.s. |
| Harvey 1998 | Randomized controlled trial | Combined prescribing | Mean costs of drugs prescribed Int £10.97 Con £25.38 Absolute change=‐£14.41 Relative % change=‐57% No s.d. or tests |
| Kendrick 2005a | Randomized controlled trial | Combined prescribing | Medication costs 26 weeks Post treatment Int 36 (53) (n=62) Con 44 (51) (n=51) Absolute change Post treatment ‐8 Relative % change ‐18.2 |
| Kendrick 2005b | Randomized controlled trial | Combined prescribing | Medication costs 26 weeks Post treatment Int 40 (74) (n=71) Con 44(51) (n=51) Absolute change Post treatment ‐4 Relative % change ‐9.1 |
| Richards 2003 | Randomized controlled trial | Combined prescribing | Medication costs 12 months Post treatment Int 70.79 (127.32) (n=47) Con 109.03 (134.62) (n=40) Absolute change Post treatment ‐38.24 Relative % change ‐35.1 Mean difference ‐38.24, 95% CI ‐94.15 to 17.68, p=0.178 |
| Robson 1984 | Randomized controlled trial | Non‐psychotropic prescribing | Prescribing (category B ‐ nutritional, blood and skin) 3 months Int £0.60 Con £0.60 Absolute change=£0 Relative % change=0 Reported p=0.9 6 months Int £1.13 Con £1.17 Absolute change=‐£0.04 Relative % change=‐3% Reported p=0.9 12 months Int £2.36 Con £2.03 Absolute change=£0.33 Relative % change=16% Reported p=0.7 Prescribing (category C ‐ all other drugs) 3 months Int £1.90 Con £2.20 Absolute change=‐£0.30 Relative % change=‐14% Reported p=0.5 6 months Int £4.23 Con £4.61 Absolute change=‐£0.38 Relative % change=‐8% Reported p=0.7 12 months Int £8.75 Con £9.69 Absolute change=£0.94 Relative % change=‐10% Reported p=0.7 |
1.7. Analysis.
Comparison 1 Direct effects, Outcome 7 PCP referrals.
| PCP referrals | |||
|---|---|---|---|
| Study | Study design | Outcomes | Results |
| Mental health referrals | |||
| Boot 1994 | Randomized controlled trial | Mental health referrals | Referrals 6 weeks Int 4/107 (4%) Con 38/60 (63%) Absolute change=‐59% Relative % change=‐94% Reported chisq=69.4, df=1, p=0.000 |
| Brouwers 2006 | Randomized controlled trial | Mental health referrals | Referred to specialised mental health care Post treatment Int 7% (n=98) Con 35% (n=96) Absolute change post ‐28 Relative % change ‐80.0 Social worker contacts Post treatment Int 4.7 (1.1) (n=96) Con 0.9 (2.4) (n=96) Absolute change post 3.8 Relative % change 422.2 Referrals to psychologist Post treatment Int 0.1 (0.3) (n=96) Con 0.1 (0.3) (n=96) Absolute change post 0 Relative % change 0.0 |
| Catalan 1991 | Randomized controlled trial | Mental health referrals | Psychiatric referrals Weeks 11‐28 Int 0 (n=21) (0%) Con 5 (n=26) (19%) Absolute change=‐19% Relative % change=‐100% Fisher's exact p=0.056 |
| Corney 1984 | Randomized controlled trial | Mental health referrals | Referrals to psychiatric/psychological services 12 months post‐treatment Int 3 (7%) (n=41) Con 3 (8%) (n=39) Absolute change=‐1% Relative % change=‐13% |
| Harvey 1998 | Randomized controlled trial | Mental health referrals costs | MH referral costs 4 months Int £1.06 to £7.34 Con £9.45 to £26.04 (Range depends on assumptions used to cost referrals) Absolute change=‐£8.39 to ‐£18.70 Relative % change=‐89% to ‐72% |
| Hemmings 1997 | Randomized controlled trial | Mental health referrals | External referral to MH professional 4 months Int 7/114 (6%) Con 26/40 (65%) Absolute change=‐59% Relative % change=91% Reported chisq=50.9, df=1, p=0.00 |
| Kendrick 2005a | Randomized controlled trial | Mental health referrals and costs | Practice counsellor referrals 26 weeks Post treatment Int 0.11(0.89) (n=62) Con 0.57 (1.8) (n=51) Absolute change Post treatment ‐0.46 Relative % change ‐80.7 Practice counsellor referrals costs 26 weeks Post treatment Int 4 (29) (n=62) Con 18 (57) (n=51) Absolute change Post treatment ‐14 Relative % change ‐77.8 Social worker referrals 26 weeks Post treatment Int 0.18(1.17) (n=62) Con 0.16 (0.99) (n=51) Absolute change Post treatment 0.02 Relative % change 12.5 Social worker referrals costs 26 weeks Post treatment Int 9 (58) (n=62) Con 8 (51) (n=51) Absolute change Post treatment 1 Relative % change 12.5 Psychiatric referrals 26 weeks Post treatment Int 0.1 (0.43) (n=62) Con 0.14 (0.4) (n=51) Absolute change Post treatment ‐0.04 Relative % change ‐28.6 Psychiatric referrals costs 26 weeks Post treatment Int 9 (39) (n=62) Con 12 (36) (n=51) Absolute change Post treatment ‐3 Relative % change ‐25.0 Psychologist referrals 26 weeks Post treatment Int 0 (0) (n=62) Con 0.69 (4.48) (n=51) Absolute change Post treatment ‐0.69 Relative % change ‐100.0 Psychologist referrals costs 26 weeks Post treatment Int 0 (0) (n=62) Con 20 (130) (n=51) Absolute change Post treatment ‐20 Relative % change ‐100.0 |
| Kendrick 2005b | Randomized controlled trial | Mental health referrals and costs | Practice counsellor referrals 26 weeks Post treatment Int 0.21(1.01) (n=71) Con 0.57 (1.8) (n=51) Absolute change Post treatment ‐0.36 Relative % change‐63.2 Practice counsellor referrals costs 26 weeks Post treatment Int 7 (31) (n=71) Con 18 (57) (n=51) Absolute change Post treatment ‐11 Relative % change ‐61.1 Social worker referrals 26 weeks Post treatment Int 0 (0) (n=71) Con 0.16 (0.99) (n=51) Absolute change Post treatment‐0.16 Relative % change ‐100.0 Social worker referrals costs 26 weeks Post treatment Int 0 (0) (n=71) Con 8 (51) (n=51) Absolute change Post treatment ‐8 Relative % change ‐100.0 Psychiatric referrals 26 weeks Post treatment Int 0.13 (0.51) (n=71) Con 0.14 (0.4) (n=51) Absolute change Post treatment ‐0.01 Relative % change ‐7.1 Psychiatric referrals costs 26 weeks Post treatment Int 11 (45) (n=71) Con 12 (36) (n=51) Absolute change Post treatment ‐1 Relative % change ‐8.3 Psychologist referrals 26 weeks Post treatment Int 0.1 (0.61) (n=71) Con 0.69 (4.48) (n=51) Absolute change Post treatment ‐0.59 Relative % change ‐85.5 Psychologist referrals costs 26 weeks Post treatment Int 3 (18) (n=71) Con 20 (130) (n=51) Absolute change Post treatment ‐17 Relative % change ‐85.0 |
| King 2000a | Randomized controlled trial | Mental health referrals | Mental health referrals 12 months Post treatment Int 0.22 (0.52) (n=63) Con 0.52 (0.88) (n=67) Absolute change post ‐0.3 Relative % change ‐57.7 |
| King 2000b | Randomized controlled trial | Mental health referrals | Mental health referrals 12 months Post treatment Int 0.25 (0.59) (n=67) Con 0.52 (0.88) (n=67) Absolute change post ‐0.27 Relative % change ‐51.9 |
| Lambert 2007 | Randomized controlled trial | Mental health referrals | Mental health referrals (3 months before 20 week FU) Pre Int 3.5% (n=57) Con 13.3% (n=60) Post treatment Int 3.5% (n=57) Con 5% (n=60) Absolute change post ‐1.5 Relative % change ‐30.0 Absolute change from baseline Int 0, Con ‐8.3 Difference in absolute change from baseline 8.3 Mental health referrals (3 months before 10 month FU) Pre Int 3.5% (n=57) Con 13.3% (n=60) Post treatment Int 0% (n=57) Con 11.7% (n=60) Absolute change post ‐11.7 Relative % change ‐100.0 Absolute change from baseline Int ‐3.5, Con ‐1.6 Difference in absolute change from baseline ‐1.9 |
| Richards 2003 | Randomized controlled trial | Mental health referral costs | Mental health worker costs Post treatment Int 1.27 (6.12) (n=47) Con 0 (0) (n=40) Absolute change Post treatment 1.27 Relative % change NA Mean difference 1.28, 95% CI ‐0.65 to 3.20, p=0.191 Outpatient mental health costs 12 months Post treatment Int 27.26 (132.67) (n=47) Con 14.55 (57.75) (n=40) Absolute change Post treatment 12.71 Relative % change 87.4 Mean difference 12.71, 95% CI ‐32.56 to 57.99, p=0.578 Counselling costs 12 months Post treatment Int 13.26 (64.91) (n=47) Con 23.25 (71.73) (n=40) Absolute change Post treatment ‐9.99 Relative % change ‐43.0 Mean difference ‐9.99, 95% CI ‐39.84 to 19.84, p=0.509 |
| Teasdale 1984 | Randomized controlled trial | Mental health referrals | Referrals to psychiatry Int 1/17 (6%) Con 5/17 (29%) Absolute change=‐23% Relative % change=‐79% No tests reported |
| Non‐mental health referrals | |||
| Brantley 1986 | Controlled before‐after study | Non‐mental health referrals | Speciality clinics 12 months pre‐treatment Int 1.33 (2.29) (n=21) Con 0.48 (0.87) (n=21) 12 months post‐treatment Int 0.57 (1.03) Con 0.48 (1.33) Absolute change=0.09 Relative % change=19% Absolute change from baseline Int ‐0.76 Con 0 Difference in absolute change from baseline=‐0.76 Emergency room visits 12 months pre‐treatment Int 0.43 (0.97) (n=21) Con 0.67 (1.10) (n=21) 12 months post‐treatment Int 0.33 (0.64) Con 0.28 (0.56) Absolute change=0.05 Relative % change=18% Absolute change from baseline Int ‐0.10 Con ‐0.39 Difference in absolute change from baseline=0.29 Hospitalisations 12 months pre‐treatment Int 0.48 (1.12) (n=21) Con 0.09 (0.30) (n=21) 12 months post‐treatment Int 0.09 (0.03) Con 0.00 (0.00) Absolute change=0.09 Relative % change=NA Absolute change from baseline Int ‐0.39 Con ‐0.09 Difference in absolute change from baseline=‐0.30 |
| Brouwers 2006 | Randomized controlled trial | Non mental health referrals | Referrals to medical outpatients Post treatment Int 0.4 (0.8) (n=96) Con 0.5 (0.8) (n=96) Absolute change post ‐0.1 Relative % change ‐20.0 Referrals to physical therapist Post treatment Int 0.3 (0.6) (n=96) Con 0.3 (0.6) (n=96) Absolute change post 0 Relative % change 0.0 Referrals to mensendieck physical therapist Post treatment Int 0 (0.1) (n=96) Con 0.1 (0.2) (n=96) Absolute change post ‐0.1 Relative % change ‐100.0 Referrals to nutritionist Post treatment Int 0 (0.1) (n=96) Con 0 (0.1) (n=96) Absolute change post 0 Relative % change NA Referrals to haptonomist Post treatment Int 0 (0.2) (n=96) Con 0 (0.2) (n=96) Absolute change post 0 Relative % change NA Referrals to lab research Post treatment Int 1.1 (1.8) (n=96) Con 1.3 (2.1) (n=96) Absolute change post ‐0.2 Relative % change ‐15.4 Referrals to X ray Post treatment Int 0.2 (0.6) (n=96) Con 0.2 (0.5) (n=96) Absolute change post 0 Relative % change 0.0 |
| King 2000a | Randomized controlled trial | Non‐mental health referrals | Non mental health referrals 12 months Post treatment Int 0.92 (1.26) (n=63) Con 0.93 (1.28) (n=67) Absolute change post ‐0.01 Relative % change ‐1.1 |
| King 2000b | Randomized controlled trial | Non‐mental health referrals | Non mental health referrals 12 months Post treatment Int 0.93 (1.13) (n=67) Con 0.93 (1.28) (n=67) Absolute change post 0 Relative % change 0.0 |
| Lambert 2007 | Randomized controlled trial | Non‐mental health referrals | Non‐mental health referrals (3 months before 20 week FU) Pre Int 12.3% (n=57) Con 6.7% (n=60) Post treatment Int 3.5% (n=57) Con 5% (n=60) Absolute change post ‐1.5 Relative % change ‐30.0 Absolute change from baseline Int ‐8.8, Con ‐1.7 Difference in absolute change from baseline ‐7.1 Non‐mental health referrals (3 months before 10 month FU) Pre Int 12.3% (n=57) Con 6.7% (n=60) Post treatment Int 10.5% (n=57) Con 16.7% (n=60) Absolute change post ‐6.2 Relative % change ‐37.1 Absolute change from baseline Int ‐1.8, Con 10 Difference in absolute change from baseline ‐11.8 |
| All referrals | |||
| Earll 1982 | Randomized controlled trial | All referrals | OP appointments Post treatment Int 0.52 Con 0.58 Absolute change=‐0.06 Relative % change=‐10% Reported n.s. 7 months Int 0.83 Con 1.32 Absolute change=‐0.49 Relative % change=‐37% Reported n.s. Hospital inpatient admissions Post treatment Int 0/23 (0%) Con 2/19 (11%) Absolute change=‐11% Relative % change=‐100% No test reported 7 months Int 1/23 (4%) Con 4/19 (21%) Absolute change=‐17% Relative % change=‐81% No test reported |
| Harvey 1998 | Randomized controlled trial | All referrals | Referrals 4 months Int 0.07 Con 0.22 Absolute change=‐0.15 Relative % change=‐68% |
| Kendrick 2005a | Randomized controlled trial | All referrals and costs | Outpatient referrals 26 weeks Post treatment Int 0.05 (0.22) (n=62) Con 0 (0) (n=51) Absolute change Post treatment 0.05 Relative % change 0 Outpatient referrals costs 26 weeks Post treatment Int 6 (26) (n=62) Con (0) (0) (n=51) Absolute change Post treatment 6 Relative % change NA |
| Kendrick 2005b | Randomized controlled trial | All referrals and costs | Outpatient referrals 26 weeks Post treatment Int 0.07 (0.49) (n=71) Con 0 (0) (n=51) Absolute change Post treatment 0.07 Relative % change NA Outpatient referrals costs 26 weeks Post treatment Int 8 (55) (n=71) Con 0 (0) (n=51) Absolute change Post treatment 8 Relative % change NA |
| King 2000a | Randomized controlled trial | All referrals | Outpatient costs 12 months Post treatment Int 105.9 (251.9) (n=63) Con 201.2 (344.9) (n=67) Absolute change post ‐95.3 Relative % change ‐47.4 |
| King 2000b | Randomized controlled trial | All referrals | Outpatient costs 12 months Post treatment Int 90.3 (175.8) (n=67) Con 201.2 (344.9) (n=67) Absolute change post ‐110.9 Relative % change ‐55.1 |
| Spurgeon 2007 | Controlled‐before after study | All referrals | Referrals 12 months Pre treatment Int 16.8 Con 14.92 Post treatment Int 16.29 Con 17.12 Absolute change post ‐0.83 Relative % change ‐4.8 Absolute change from baseline Int ‐0.51 Con 2.2 Difference in absolute change from baseline ‐2.71 Tests and investigations 12 months Pre treatment Int 11.35 Con 13.9 Post treatment Int 8.6 Con 16.62 Absolute change post ‐8.02 Relative % change ‐48.3 Absolute change from baseline Int ‐2.75 Con 2.72 Difference in absolute change from baseline ‐5.47 |
| Stanton 1998 | Randomized controlled trial | All referrals | Referrals 6 months Int 0 (61%) 1 (26%) Missing (13%) (n=23) Con 0 (71%) 1 (12%) Missing (17%) (n=24) Absolute change=14% Relative % change=116% No tests reported |
1.8. Analysis.
Comparison 1 Direct effects, Outcome 8 Total costs.
| Total costs | |||
|---|---|---|---|
| Study | Study design | Outcomes | Results |
| Corney 2003 | Randomized controlled trial | Primary care total costs | Primary care costs 6 months Pre treatment Int 101 (87) (n=90) Con 113 (104) (n=89) Post treatment Int 321 (191) (n=82) Con 149 (194) (n=79) Absolute change Post treatment 172 Relative % change 115.4 Absolute change from baseline Int 220, Con 36 Difference in absolute change from baseline 184 Primary care costs 12 months Pre treatment Int 101 (87) (n=90) Con 113 (104) (n=89) Post treatment Int 157 (186) (n=75) Con 174 (215) (n=68) Absolute change Post treatment ‐17 Relative % change ‐9.8 Absolute change from baseline Int 56, Con 61 Difference in absolute change from baseline ‐5 |
| King 2000a | Randomized controlled trial | Primary care total costs | Primary care costs 12 months Post treatment Int 86.6 (59.7) (n=63) Con 118.5 (93.7) (n=67) Absolute change post ‐31.9 Relative % change ‐26.9 |
| King 2000b | Randomized controlled trial | Primary care total costs | Primary care costs 12 months Post treatment Int 98.4 (84.5) (n=67) Con 118.5 (93.7) (n=67) Absolute change post ‐20.1 Relative % change ‐17.0 |
1.9. Analysis.
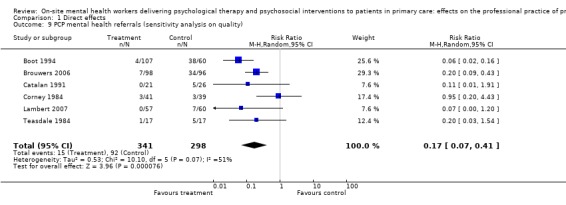
Comparison 1 Direct effects, Outcome 9 PCP mental health referrals (sensitivity analysis on quality).
Comparison 2. Indirect effects.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 PCP consultations | Other data | No numeric data | ||
| 2 Prescribing | Other data | No numeric data | ||
| 2.1 Psychotropic prescribing | Other data | No numeric data | ||
| 2.2 Psychotropic and non‐psychotropic prescribing | Other data | No numeric data | ||
| 3 Referrals | Other data | No numeric data | ||
| 3.1 Mental health referrals | Other data | No numeric data | ||
| 3.2 Non‐mental health referrals | Other data | No numeric data | ||
| 4 Total costs | Other data | No numeric data |
2.1. Analysis.
Comparison 2 Indirect effects, Outcome 1 PCP consultations.
| PCP consultations | |||
|---|---|---|---|
| Study | Study design | Outcomes | Results |
| Lester 2007 | Randomized controlled trial | GP consultations | GP consultations 12 months Post treatment Int 7.88 (6.46) (n=162) Con 7.69 (6.41) (n=165) Absolute change Post treatment 0.19 Relative % change 2.5 PN consultations 12 months Post treatment Int 1.7 (2.54) (n=162) Con 1.69 (2.66) (n=165) Absolute change Post treatment 0.01 Relative % change 0.6 Primary care consultation costs 12 months Post treatment Int 261.79 Con 232.21 Absolute change Post treatment 29.58 Relative % change 12.7 Mean difference 29.58, 95% CI ‐49.07 to 110.51 |
2.2. Analysis.
Comparison 2 Indirect effects, Outcome 2 Prescribing.
| Prescribing | |||
|---|---|---|---|
| Study | Study design | Outcomes | Results |
| Psychotropic prescribing | |||
| Baker 1996 | Controlled before‐after study | Psychotropic prescribing | Anxiolytic/hypnotic prescription
15 months pre and post
Reported Group by Time MANOVA
p=0.73 (group) p=0.00 (Time) p=0.56 (GroupxTime)
Antidepressant prescription
15 months pre and post
Reported Group by Time MANOVA
p=0.61 (group) p=0.00 (Time) p=0.89 (GroupxTime) Note: Absolute change cannot be calculated (F statistics and graphs only) |
| Coe 1996 | Controlled before‐after study | Psychotropic prescribing costs | Hypnotics and anxiolytic spend per patient 12 months pre‐treatment Int £0.66 (n=29) Con £0.71 (n=29) 12 months post‐treatment Int £0.55 Con £0.55 Absolute change=£0 Relative % change=0% Absolute change from baseline Int ‐£0.11 Con ‐£0.16 Difference in absolute change from baseline =£0.05 Reported difference post p=0.6 Antidepressant spend per patient 12 months pre‐treatment Int £1.64 (n=29) Con £2.09 (n=29) 12 months post‐treatment Int £2.73 Con £2.89 Absolute change=‐0.16 Relative % change=‐6% Absolute change from baseline Int £1.09 Con £0.80 Difference in absolute change from baseline = £0.29 Reported difference post p=0.07 |
| Pharoah 1996 | Controlled before‐after study | Psychotropic prescribing | Mean monthly prescription items per 1000 PU 6 months pre‐treatment Int 19.93 (n=16) Con 20.71 (n=16) Reported n.s. (Wilcoxon z=1.03, p=0.30) 6 months post‐treatment Int 18.97 (n=16) Con 19.32 (n=16) Absolute change=‐0.35 Relative % change=‐2% Absolute change from baseline Int ‐0.96 Con ‐1.39 Difference in absolute change from baseline=0.43 Reported change post not significant (Wilcoxon z=0.517, p=0.61) |
| Simpson 2003 | Controlled before‐after study | Psychotropic prescribing | Median percentage change in drug costs per 1000 PU Antidepressants Int 425 Con 486 Hypnotics Int ‐9 Con ‐6 CNS Int 157 Con 165 Median costs per 1000 PU Antidepressants Pre treatment Int 628 Con 647 Post treatment Int 3713 Con 3962 Hypnotics Pre treatment Int 227 Con 219 Post treatment Int 198 Con 188 CNS Pre treatment Int 3320 Con 3178 Post treatment Int 8830 Con 9279 All comparisons NS |
| Psychotropic and non‐psychotropic prescribing | |||
| Lester 2007 | Randomized controlled trial | Combined prescribing | Medication costs 12 months Post treatment Int 25.12 Con 40.43 Absolute change Post treatment ‐15.31 Relative % change ‐37.9 Mean difference ‐15.31, 95% CI ‐48.40 to 13.48 |
2.3. Analysis.
Comparison 2 Indirect effects, Outcome 3 Referrals.
| Referrals | |||
|---|---|---|---|
| Study | Study designs | Outcomes | Results |
| Mental health referrals | |||
| Baker 1996 | Controlled before‐after study | Short and long‐term mental health referrals | Psychiatric OP referrals
12 months pre and post
Reported Group by Time MANOVA
p=0.57 (group) p=0.00 (Time) p=0.10 (GroupxTime)
Psychiatric IP
12 months pre and post
Reported Group by Time MANOVA
p=0.07 (group) p=0.00 (Time) p=0.94 (GroupxTime)
Psychology
12 months pre and post
Reported Group by Time MANOVA
p=0.07 (group) p=0.00 (Time) p=0.05 (GroupxTime)
Greater increase in referrals in intervention practices
Group therapy
12 months pre and post
Reported Group by Time MANOVA
p=0.20 (group) p=0.00 (Time) p=0.69 (GroupxTime)
Community OT
12 months pre and post
Reported Group by Time MANOVA
p=0.78 (group) p=0.00 (Time) p=0.43 (GroupxTime)
CPN
12 months pre and post
Reported Group by Time MANOVA
p=0.60 (group) p=0.00 (Time) p=0.33 (GroupxTime) Note: Absolute change cannot be calculated (ANOVAs and graphs only) |
| Coe 1996 | Controlled before‐after study | Long‐term mental health referrals | Referral rates to Psychiatry per 1000 12 months pre‐treatment Int 6.18 (n=29) Con 4.62 (n=29) 12 months post‐treatment Int 5.84 Con 7.61 Absolute change=‐1.77 Relative % change=‐23% Absolute change from baseline Int ‐0.34 Con 2.99 Difference in absolute change from baseline= ‐3.33 Referral to CMHT per 1000 12 months post‐treatment Int 7.15 (n=29) Con Post 12.60 (n=29) Absolute change=‐5.45 Relative % change=43% |
| Hunter 1983 | Controlled before‐after study | Long term mental health referrals | Referrals (new and re‐referred) 12 months pre‐treatment Int1 6.4 Con1 3.9 12 months post‐treatment Int1 6.3 Con1 4.3 Absolute change=2 Relative % change=47% Absolute change from baseline Int ‐0.1 Con 0.4 Difference in absolute change from baseline=‐0.5 24 months post‐treatment Int1 5.3 Con1 5.4 Absolute change=‐0.1 Relative % change=‐2% Absolute change from baseline Int ‐1.1 Con 1.5 Difference in absolute change from baseline=‐2.6 Referrals (new and re‐referred) 12 months pre‐treatment Int2 7.5 Con2 7.5 12 months post‐treatment Int2 10.3 Con2 5.6 Absolute change=4.7 Relative % change=84% Absolute change from baseline Int 2.8 Con ‐1.9 Difference in absolute change from baseline=4.7 Reported p<0.05 difference between Int1 and Con1 pre‐test, n.s. at 1 year or two years Reported p<0.05 increase in Int2 from pre to post, P<0.05 decrease in Con2 pre to post. |
| Lester 2007 | Randomized controlled trial | Long term mental health referrals and costs | Counsellor consultations 12 months Post treatment Int 0.06 (0.23) (n=162) Con 0.05 (0.25) (n=165) Absolute change Post treatment 0.01 Relative % change 20.0 Psychiatrist referrals 12 months Post treatment Int 0.19 (0.58) (n=162) Con 0.11 (0.37) (n=165) Absolute change Post treatment 0.08 Relative % change 72.7 CPN referrals 12 months Intervention Post treatment Int 0.07 (0.26) (n=162) Con 0.05 (0.23) (n=165) Absolute change Post treatment 0.02 Relative % change 40.0 CMHT referrals 12 months Post treatment Int 0.06 (0.27) (n=162) Con 0.09 (0.45) (n=165) Absolute change Post treatment ‐0.03 Relative % change ‐33.3 Specialist mental health costs 12 months Post treatment Int 34.36 Con 24.2 Absolute change Post treatment 10.16 Relative % change 42.0 Mean difference 10.16, 95% CI ‐5.61 to 29.52 |
| Tarrier 1983 | Controlled before‐after study | Long‐term mental health referrals | Total referrals 2 years pre‐treatment Practice Int 56 Practice Con 159 2 years post‐treatment Practice Int 57 Practice Con 215 Absolute change=‐158 Relative % change=‐74% Absolute change from baseline Int 1 Con 56 Differences in absolute change from baseline=‐55 2 years pre‐treatment Health Centre Int 162 Health Centre Con 144 2 years post‐treatment Health Centre Int 203 Health Centre Con 142 Absolute change=61 Relative % change=43% Absolute change from baseline Int 41 Con ‐2 Differences in pre‐post change=43 |
| Walker 1989 | Controlled before‐after study | Long‐term mental health referrals | GP referral rates (calculated from base population) OP referrals Pre‐treatment Int 12/9231 (0.13%) Con 9/3125 (0.29%) Post‐treatment Int 16/8926 (0.18%) Con 5/2895 (0.17%) Absolute change=0.01 Relative % change=6% Absolute change from baseline Int 0.05% Con ‐0.12% Difference in absolute change from baseline=0.17% IP referrals Pre‐treatment Int 9/9318 (0.10%) Con 6/3117 (0.19%) Post‐treatment Int 29/9310 (0.31%) Con 5/3247 (0.15%) Absolute change=0.16% Relative % change=107% Absolute change from baseline Int 0.21% Con ‐0.04% Difference in absolute change from baseline=0.25% |
| Wells 1992 | Controlled before‐after study | Mental health referrals | 1982/83 versus 1984‐1986 All referrals All referrals chi square=6.79, p<0.01 First referrals chi square=7.65, p<0.01 Re‐referrals chi square=0.52, NS Emergency referrals chi square=6.11, p<0.02 |
| Non‐mental health referrals | |||
| Lester 2007 | Randomized controlled trial | Non mental health referrals | Non mental health referrals 12 months Post treatment Int 0.94 (1.35) (n=162) Con 1.16 (1.99) (n=165) Absolute change Post treatment ‐0.22 Relative % change ‐19.0 Non mental health costs 12 months Post treatment Int 118.69 Con 147.2 Absolute change Post treatment ‐28.51 Relative % change ‐19.4 Mean difference ‐28.51 95% CI ‐111.30 to 41.97 |
2.4. Analysis.
Comparison 2 Indirect effects, Outcome 4 Total costs.
| Total costs | |||
|---|---|---|---|
| Study | Study design | Outcomes | Results |
| Lester 2007 | Randomized controlled trial | Total costs | Total costs 12 months Post treatment Int 439.97 Con 444.05 Absolute change Post treatment ‐4.08 Relative % change ‐0.9 |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ashurst 1983.
| Methods | Design: RCT Allocation concealment: Not done Follow up: Professionals: Done Patients: Not done Blind assessment: Done Baseline: Not clear Reliable: Not done Contamination: Not done | |
| Participants | 248 patients Neurotic problems 12 PCPs One health centre and one practice UK | |
| Interventions | Practice counsellor Eclectic counselling | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Ashworth 2000.
| Methods | Design: CBA Base measurement: Not done Base control (patient): Done Blind assessment: Done Contamination protection (patient): Not done Reliable: Not clear Follow up: Professionals: Done Patients: NA | |
| Participants | 180 patients Patients receiving psychotherapy 6 PCPs 1 practice UK | |
| Interventions | Two counsellors, a clinical psychologist and a psychiatric nurse. Cognitive analytic therapy, cognitive and behavioural therapy and behavioural therapy. | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Baker 1996.
| Methods | Design: CBA Base measurement: Done Base control (2nd site): Done Blind assessment: Done Contamination protection (2nd site): Done Reliable: Done/Not clear Follow up: Professionals: Done Patients: NA | |
| Participants | 75 practices UK | |
| Interventions | Practice counsellors | |
| Outcomes | Indirect effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Basler 1990.
| Methods | Design: CBA Base measurement: Done Base control (patient): Done Blind assessment: Done Contamination protection: Not done Reliable: Not clear Follow up: Professionals: Not clear Patients: Not done | |
| Participants | 60 patients Pain problems 3 PCPs Germany | |
| Interventions | Psychologist Group cognitive‐behaviour therapy | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Benson 1988.
| Methods | Design: RCT Allocation concealment: Not done Follow up: Professionals: Done/Not done Patients: NA Blind assessment: Done Baseline: Done Reliable: Not clear Contamination: Not done | |
| Participants | 50 patients Frequent attenders 6 PCPs 1 practice UK | |
| Interventions | Psychologist and PCP Group therapy | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Blakey 1986.
| Methods | Design: CBA Base measurement: Not done Base control (patient): Done Blind assessment: Done Contamination: Not done Reliable: Not clear Follow up: Professionals: Done Patients: Not clear | |
| Participants | 178 patients Mixed psychological problems 7 PCPs 1 health centre UK | |
| Interventions | Psychologist Behavioural treatment | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Boot 1994.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Done Patients: Not done Blind assessment: Done Baseline: Done/Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 192 patients Mixed emotional problems 28 PCPs 7 practices UK | |
| Interventions | Practice counsellors Non‐directive counselling 2. Usual PCP care | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Brantley 1986.
| Methods | Design: CBA Base measurement: Not clear Base control (patient): Done Blind assessment: Done Contamination protection: Not done Reliable: Not clear Follow up: Professionals: Done Patients: Done | |
| Participants | 42 patients Mixed psychological problems 17 PCPs 1 family practice clinic USA | |
| Interventions | Psychologists Behavioural treatment | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Brodaty 1983.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Not clear Patients: Not done Blind assessment: Not clear Baseline: Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 56 patients Persistent psychological problems 10 practices Australia | |
| Interventions | Psychiatrist Brief dynamic psychotherapy | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Brouwers 2006.
| Methods | Design: RCT Allocation concealment: Done Follow up: Professionals: Done Patients: Done Blind assessment: Done Baseline: Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 194 patients Patients with emotional distress or minor mental disorders 70 PCPs Netherlands | |
| Interventions | Social workers Coping and problem solving | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Bruce 1998.
| Methods | Design: CBA Base measurement: Not clear Base control (2nd site): Done Base control (patient): Done Blind assessment: Done Contamination protection (2nd site): Done Reliable: Not done Follow up: Professionals: Not clear Patients: Not clear | |
| Participants | 27 patients Patients with a chronic mental illness discharged from long stay wards 12 PCPs 2 practices UK | |
| Interventions | G grade Community psychiatric nurse Community psychiatric nurse care | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Catalan 1991.
| Methods | Design: RCT Allocation concealment: Not clear Follow up Professionals: Not clear Patients: Not clear Blind assessment: Done Baseline: Done/Not done Reliable: Not clear Contamination: Not done | |
| Participants | 47 patients Mixed emotional problems 26 PCPs 16 practices UK | |
| Interventions | Psychiatrist Problem solving | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Coe 1996.
| Methods | Design: CBA Base measurement: Not clear Base control (2nd site): Not clear Blind assessment: Done Contamination protection (2nd site): Done Reliable: Done/Not clear Follow up: Professionals: Done Patients: Not done | |
| Participants | UK | |
| Interventions | Practice counsellors | |
| Outcomes | Indirect effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Corney 1984.
| Methods | Design: RCT Allocation concealment: Done Follow up: Professionals: Not clear Patients: Done Blind assessment: Done Baseline: Done/Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 80 patients Depression 6 PCPs 4 practices UK | |
| Interventions | Social worker Casework counselling | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Corney 2003.
| Methods | Design: RCT Allocation concealment: Done Follow up professionals: Done Patients: Done/not done Blinded assessment: Done Baseline: Not done Reliable: Not clear Contamination: Not done | |
| Participants | 181 patients Patients who had suffered depression or depression/anxiety as their main symptom for over 6 months 9 practices UK | |
| Interventions | Counsellors Counselling (psychodynamic or CBT) | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Earll 1982.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Done Patients: Not done Blind assessment: Done Baseline: Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 50 patients Mixed psychological problems 4 PCPs 1 practice UK | |
| Interventions | Psychologist Behavioral treatment | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Ginsberg 1984.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Not done Patients: Not done Blind assessment: Done/Not done Baseline: Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 92 patients Neurotic patients 20 PCPs 4 health centres UK | |
| Interventions | Nurse therapist Behavioural psychotherapy | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Gournay 1995.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Not done/Not clear Patients: Not done Blind assessment: Done Baseline: Done Reliable: Not clear Contamination: Not done | |
| Participants | 177 patients Non‐psychotic problems 36 PCPs 6 practices UK | |
| Interventions | Community psychiatric nurse Counselling | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Harvey 1998.
| Methods | Design: RCT Allocation concealment: Done Follow up: Professionals: Not clear Patients: Not done Blind assessment: Not clear Baseline: Done/Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 162 patients Mixed emotional problems 9 practices UK | |
| Interventions | Practice counsellors Person‐centred counselling | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Hemmings 1997.
| Methods | Design: RCT Allocation concealment: Not done Follow up: Professionals: Not clear Patients: Done/Not done Blind assessment: Done Baseline: Done/Not done Reliable: Not clear Contamination: Not done | |
| Participants | 188 patients Mixed emotional problems 15 PCPs 3 practices UK | |
| Interventions | Practice counsellor Eclectic counselling | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Hunter 1983.
| Methods | Design: CBA Base measurement: Done/Not done Base control (2nd site): Not clear Blind assessment: Done Contamination protection (2nd site): Not done Reliable: Not clear Follow up: Professionals: Not clear Patients: NA | |
| Participants | 6 practices UK | |
| Interventions | Psychiatrist Psychiatric clinics | |
| Outcomes | Indirect effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Kendrick 2005a.
| Methods | Design: RCT Allocation concealment: Done Follow up professionals: Done Patients: Done/Not done Blinded assessment: Done Baseline: Done Reliable: Not clear Contamination: Not done | |
| Participants | 168 patients Patients aged 18‐65 years with a new episode of anxiety, depression, or reaction to life difficulties. 243 PCPs 62 practices UK | |
| Interventions | Community mental health nurses (CMHN) Generic CMHN treatment | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Kendrick 2005b.
| Methods | Design: RCT Allocation concealment: Done Follow up professionals: Done Patients: Done/Not done Blinded assessment: Done Baseline: Done Reliable: Not clear Contamination: Not done | |
| Participants | 157 patients Patients aged 18‐65 years with a new episode of anxiety, depression or reaction to life difficulties 243 PCPs 62 practices UK | |
| Interventions | Community mental health nurses Problem‐solving treatment | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
King 2000a.
| Methods | Design: RCT Allocation concealment: Done Follow up professionals: Done Patients: Not done Blinded assessment: Done Baseline: Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 130 patients Patients diagnosed as suffering from depression, or mixed anxiety and depression 93 PCPs 24 practices UK | |
| Interventions | Psychologists CBT | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
King 2000b.
| Methods | Design: RCT Allocation concealment: Done Follow up professionals: Done Patients: Not done Blinded assessment: Done Baseline: Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 134 patients Patients diagnosed as suffering from depression, or mixed anxiety 93 PCPs 24 practices UK | |
| Interventions | Counsellors Non directive counselling | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Lambert 2007.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Not clear Patients: Not done Blind assessment: Done Baseline: Not done Reliable: Not clear Contamination: Not done | |
| Participants | 117 patients Panic disorder with or without agorophobia 15 practices UK | |
| Interventions | Occupational therapy led lifestyle intervention | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Lave 1998.
| Methods | Design: RCT Allocation concealment: Not clear Follow up professionals: Not clear Patients: Not clear Blinded assessment: Done Baseline: Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 185 patients Patients diagnosed with DSM IIIR current major depression 4 practices USA | |
| Interventions | Experienced and trained psychiatrists and psychologists Interpersonal therapy | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Lester 2007.
| Methods | Design: RCT Allocation concealment: Done Follow‐up professionals: Done Patients: Not done Blinded assessment: Done Baseline: Not clear Reliable: Not clear Contamination: Done | |
| Participants | 368 patients Patients identified by their GP as having an ongoing or newly diagnosed common mental health problem 19 practices UK | |
| Interventions | Primary care mental health workers | |
| Outcomes | Indirect effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Lyon 1993.
| Methods | Design: CBA Base measurement: Done Base control (patient): Done Blind assessment: Not clear Contamination protection: Not done Reliable: Not clear Follow up: Professionals: Done Patients: Done | |
| Participants | 87 patients Mental health problems 1 practice UK | |
| Interventions | Practice counsellor Counselling | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Martin 1985.
| Methods | Design: Controlled before and after (CBA) Base measurement: Not done Base control (patient): Done Blind assessment: Done Contamination protection: Not done Reliable: Not clear Follow up: Professionals: Done Patients: Done | |
| Participants | 174 patients Mixed emotional problems 6 PCPs 1 practice UK | |
| Interventions | Marriage guidance counselling Practice counsellors | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Mynors‐Wallis 1997.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Not clear Patients: Done Blind assessment: Done Baseline: Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 70 patients Mixed emotional problems 4 health centres UK | |
| Interventions | Community nurses Problem solving | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Pharoah 1996.
| Methods | Design: CBA Base measurement: Done Base control (2nd site): Not clear Blind assessment: Done Contamination protection (2nd site): Done Reliable: Done Follow up: Professionals: Done Patients: NA | |
| Participants | 32 practices UK | |
| Interventions | Practice counsellors | |
| Outcomes | Indirect effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Richards 2003.
| Methods | Design: RCT Allocation concealment: Done Follow up professionals: Not done Patients: Not done Blinded assessment: Done Baseline: Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 139 patients All patients aged 18+ consulting GPs with mild to moderate symptoms of anxiety and/or depression 17 practices UK | |
| Interventions | Practice nurses with 3 days training Facilitated self help | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Robson 1984.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Not clear Patients: Not clear Blind assessment: Done/Not clear Baseline: Done/Not clear Reliable: Done/Not clear Contamination: Not done | |
| Participants | 429 patients Mixed psychological problems 6 PCPs UK | |
| Interventions | Psychologists Behavioural treatment | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Simpson 2003.
| Methods | Design: CBA Base measurement: Done Base control (2nd site): Done Blind assessment: Done Contamination protection (2nd site): Done Reliable: Done Follow up: Professionals: Done Patients: NA | |
| Participants | 85 practices UK | |
| Interventions | Counsellors Counselling | |
| Outcomes | Indirect effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Spurgeon 2007.
| Methods | Design: CBA Base measurement: Not done Base control (patients): Not done Blind assessment: Done Contamination protection (patients): Not done Reliable: Not clear Follow up: Professionals: Not clear Patients: NA | |
| Participants | 271 patients All patients recorded on the chronic disease register for diabetes, asthma or hypertension, or 'frequent attenders' 4 PCPs 1 practice UK | |
| Interventions | Qualified and trained counsellors Group counselling sessions, counselling orientation primarily CBT | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Stanton 1998.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Done Patients: Done Blind assessment: Done Baseline: Done Reliable: Not clear Contamination: Not done | |
| Participants | 47 patients Relationship problems 6 practices UK | |
| Interventions | Marriage guidance counsellors Counselling | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Sumathipala 2000.
| Methods | Design: RCT Allocation concealment: Done Follow up professionals: Not clear Patients: Not done Blinded assessment: Done Baseline: Done Reliable: Done Contamination: Not done | |
| Participants | 68 patients Patients who had repeated consultations for medically unexplained symptoms 7 PCPs A general outpatient clinic providing primary care Sri Lanka | |
| Interventions | Research psychiatrist CBT | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Tarrier 1983.
| Methods | Design: CBA Base measurement: Not clear Base control (2nd site): Not clear Blind assessment: Done Contamination protection (2nd site): Done Reliable: Not clear Follow up: Professionals: Done Patients: NA | |
| Participants | 2 practice and 2 health centres UK | |
| Interventions | Clinical psychologist | |
| Outcomes | Indirect effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Teasdale 1984.
| Methods | Design: RCT Allocation concealment: Not clear Follow up: Professionals: Not clear Patients: Not done Blind assessment: Not clear Baseline: Done/Not clear Reliable: Not clear Contamination: Not done | |
| Participants | 44 patients Depression 13 practices UK | |
| Interventions | Psychologist Cognitive‐behaviour therapy | |
| Outcomes | Direct effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Walker 1989.
| Methods | Design: CBA Base measurement: Not done Base control (2nd site): Not clear Blind assessment: Done Contamination protection (2nd site): Done Reliable: Not clear Follow up: Professionals: Done Patients: NA | |
| Participants | 2 health centres New Zealand | |
| Interventions | Counselling service | |
| Outcomes | Indirect effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Wells 1992.
| Methods | Design: CBA Base measurement: Not clear Base control (2nd site): Not clear Blind assessment: Done Contamination protection (2nd site): Done Reliable: Not clear Follow up: Professionals: Done Patients: NA | |
| Participants | UK | |
| Interventions | CPN CPN attachment | |
| Outcomes | Indirect effects | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adler 2004 | Direct RCT Collaborative care |
| Akerblad 2003 | Direct RCT Collaborative care |
| Appleby 1997 | Direct RCT No objective PCP behaviours reported (patient outcome only). No PCP usual care group. |
| Araya 2003 | Direct RCT Collaborative care |
| Bannerjee 1996 | Direct RCT MHW in community setting rather than primary care. |
| Barksy 2004 | Direct RCT Consultation liaison |
| Barrowclough 2001 | Direct RCT No objective PCP behaviours reported (patient outcome only). No PCP usual care group. |
| Basler 1996 | Direct CBA Psychological treatment of physical disorder. |
| Bernal 1995 | Direct CBA No PCP usual care group. |
| Bindman 2001 | Indirect CBA No objective PCP behaviours reported (specialist only) |
| Blackburn 1981 | Direct RCT No objective PCP behaviours reported (patient outcome only). No PCP usual care group. |
| Blanchard 1995 | Direct RCT Collaborative care |
| Blay 2002 | Direct RCT No objective PCP behaviours reported (patient outcome only). No PCP usual care group. MHW not based in primary care. |
| Blomhoff 2001 | Direct RCT No PCP usual care group. |
| Blowers 1987 | Direct RCT No objective PCP behaviours reported (patient outcome only). MHW not based in primary care. |
| Brook 2003 | Direct RCT Collaborative care |
| Brooker 1994 | Direct CBA No objective PCP behaviours reported (patient outcome only). MHW in community setting rather than primary care. |
| Brown 1996 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Browne 2002 | Direct RCT No PCP usual care group. |
| Bruce 2004 | Direct RCT Collaborative care |
| Busch 1996 | Direct CBA Comparison group of non‐attenders for treatment rather than true control group. |
| Butler 1987 | Direct RCT No objective PCP behaviours reported (patient outcome only). Not clear if MHW based in primary care. |
| Butler 1991 | Direct RCT No objective PCP behaviours reported (patient outcome only). MHW not based in primary care. |
| Callahan 1994 | Direct RCT No MHW ‐ provision of treatment recommendations only. |
| Cappocia 2004 | Direct RCT Collaborative care |
| Carr 1997 | Direct and indirect CBA No objective PCP behaviours reported (patient outcome only, GP knowledge and attitudes only). Consultation liaison |
| Catalan 1984 | Direct RCT MHW was specially trained PCP, no PCP usual care group. |
| Ceroni 2002 | Direct RCT Consultation liaison |
| Chalder 1997 | Direct RCT No MHW ‐ self help intervention only. |
| Chilvers 2001 | Direct RCT No PCP usual care group |
| Clarke 2005 | Direct RCT Collaborative care |
| Coleman 1999 | Direct RCT Collaborative care |
| Cooper 1975 | Direct CBA Data collection periods for intervention and control groups not contemporaneous. |
| Cooper 1997 | Direct RCT No objective PCP behaviours reported (patient and infant outcome only). |
| Cooper 2003 | Direct RCT No objective PCP behaviours reported (patient and infant outcome only). |
| Coulehan 1997 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Cullen 1976 | Direct RCT No objective PCP behaviours reported (patient outcome only). MHW was trained PCP. |
| Dalgard 2006 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Datto 2003 | Direct RCT Collaborative care |
| Dey 2002 | Direct RCT Consultation liaison |
| Dietrich 2004 | Direct RCT Collaborative care |
| Donnan 1990 | Direct RCT No MHW ‐ self help intervention only. |
| Eayrs 1984 | Direct CBA No objective PCP behaviours reported (patient outcome only). Only a proportion of MHW interventions in primary care. |
| Emmanuel 2002 | Direct RCT Consultation liaison |
| Escobar 2007 | Direct RCT Consultation liaison |
| Espie 2001 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Espie 2007 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Finley 2000 | Direct RCT Collaborative care |
| Finney 1989 | Direct CBA Unclear whether MHW based in primary care. |
| Finney 1991 | Direct CBA Unclear whether MHW based in primary care. |
| Friedli 1999 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Gater 1997 | Indirect RCT Consultation liaison |
| Gilham 2006 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Goldberg 1996 | Direct CBA Consultation liaison |
| Grant 2000 | Direct RCT Unclear whether MHW based in primary care. |
| Graves 1981 | Direct CBA MHW in community setting rather than primary care. |
| Hebert 1994 | Direct RCT No objective PCP behaviours reported (patient outcome only). MHW in community setting rather than primary care. |
| Hedrick 2003 | Direct RCT Collaborative care |
| Hellman 1990 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Hemmings 1993 | Direct RCT MHW in teaching setting rather than primary care. |
| Hirsch 1997 | Direct CBA No objective PCP behaviours reported (patient outcome only). MHW in primary care setting in London dataset only. |
| Holden 1987 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Holdsworth 1996 | Direct RCT No MHW ‐ self help intervention only. |
| Honey 2002 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Horowitz 1996 | Indirect RCT No MHW ‐ pharmacists as intervention rather than MHW. |
| Hunkeler 2000 | Direct RCT Collaborative care |
| Hunter 1995 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Jackson 1993 | Indirect RCT Consultation liaison |
| Jenkins 1994 | Direct RCT No objective PCP behaviours reported (patient outcome only). MHW in community setting rather than primary care, interventions inititiated by community mental health team. |
| Judd 2001 | Direct RCT MHW was specially trained PCP, no PCP usual care group. No objective PCP behaviours reported (patient outcome only). |
| Karlberg 1998 | Direct RCT No objective PCP behaviours reported (patient outcome only). Unclear whether MHW based in primary care. |
| Kashner 1992 | Direct RCT No MHW ‐ provision of treatment recommendations only. |
| Katon 1992 | Direct RCT Consultation liaison |
| Katon 1995 | Direct RCT Consultation liaison |
| Katon 1996 | Direct RCT Consultation liaison |
| Katon 2001 | Direct RCT Collaborative care |
| Katon 2003 | Direct RCT Collaborative care |
| Katzelnick 2000 | Direct RCT Collaborative care |
| Kiely 1986 | Direct RCT No MHW ‐ self help intervention only. |
| King 1994 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Klerman 1996 | Direct CBA Data collection periods for intervention and control groups not contemporaneous. |
| Kolk 2004 | Direct RCT MHW not based in primary care. |
| Lang 2003 | Direct CBA No objective PCP behaviours reported (patient outcome only). |
| Lang 2006 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Lewis 1996 | Direct RCT No MHW ‐ computerised diagnosis only. |
| Lidbeck 1997 | Direct RCT No objective PCP behaviours reported (patient outcome only). MHW not based in primary care. |
| Lin 1997 | Indirect CBA Consultation liaison |
| Lindsay 1987 | Direct RCT No objective PCP behaviours reported (patient outcome only). Not clear if MHW based in primary care. |
| Lofvander 1997 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Lynch 1997 | Direct RCT No objective PCP behaviours reported (patient outcome only). MHW not based in primary care. |
| Malcolm 2002 | Direct RCT No objective PCP behaviours reported (patient outcome only). MHW was PCP |
| Mann 1998 | Direct RCT Consultation liaison |
| Marks 1985 | Direct RCT No objective PCP behaviours reported (patient outcome only) |
| McKechnie 1981 | Direct CBA No pre‐treatment measures of PCP behaviour. |
| McLeod 1997 | Direct RCT No objective PCP behaviours (patient outcome only). Unclear if MHW based in primary care. |
| Milgrom 2005 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Milne 1988 | Direct ITS Less than 2 data points either side of intervention. |
| Miranda 1994 | Direct RCT No objective PCP behaviours recorded (missed medical appointments only). Not clear if MHW based in primary care. |
| Miranda 2003 | Direct RCT Collaborative care |
| Munoz 1995 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Mynors‐Wallis 1995 | Direct RCT No objective PCP behaviours reported (patient outcome only). No PCP usual care group. |
| Mynors‐Wallis 2000 | Direct RCT No PCP usual care group. No objective PCP behaviours reported (patient outcome only). |
| Nazareth 1996 | Direct RCT No MHW ‐ management checklist only. |
| Onyett 1988 | Direct RCT Not clear if MHW based in primary care. PCP care group used appointment schedule as specified by protocol. |
| Oslin 2003 | Direct RCT Collaborative care |
| Paykel 1982 | Direct RCT MHW in community setting rather than primary care. |
| Petrou 2006 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Peveler 1999 | Direct RCT Collaborative care |
| Power 1989 | Direct RCT No objective PCP behaviours measured apart from prescribing which was part of study protocol. Not clear if MHW based in primary care. |
| Power 1990 | Direct RCT No objective PCP behaviours measured apart from prescribing which was part of study protocol. Not clear if MHW based in primary care. |
| Raphael 1977 | Direct RCT No objective PCP behaviours reported (patient outcome only). MHW in community setting rather than primary care. |
| Rickles 2004 | Direct RCT Collaborative care |
| Ridsdale 2001 | Direct RCT No PCP usual care group |
| Ridsdale 2004 | Direct RCT No PCP usual care group |
| Risdale 1999 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Roberts 2006 | Direct RCT Not clear if MHW based in primary care. No objective PCP behaviours reported (patient outcome only). |
| Ross 1985 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Rost 1994 | Direct RCT No MHW ‐ provision of treatment recommendations only. |
| Rost 2001 | Direct RCT Collaborative care |
| Roy‐Byrne 2001 | Direct RCT Collaborative care |
| Roy‐Byrne 2005 | Direct RCT Collaborative care |
| Saarijarvi 1991 | Direct RCT No objective PCP behaviours reported (patient outcome only). Not clear if MHW based in primary care. |
| Salminen 2005 | Direct RCT No objective PCP behaviours reported (patient outcome only). Not clear if MHW based in primary care. |
| Saxon 2006 | Direct RCT Patients randomised to primary care in different settings |
| Schreuders 2007 | Direct RCT No objective PCP behaviours reported (patient outcome only). . |
| Schulberg 1996 | Direct RCT Objective PCP behaviours reported for usual care group only. |
| Scott 1992 | Direct RCT PCP behaviours recorded in PCP group only. |
| Scott 1997 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Sharp 2000 | Direct RCT No PCP usual care group |
| Sharp 2004 | Direct RCT No objective PCP behaviours reported (patient outcome only). . |
| Simon 2000 | Direct RCT Collaborative care |
| Simon 2004 | Direct RCT Collaborative care |
| Simons 2001 | Direct RCT Not clear if MHW based in primary care. No objective PCP behaviours reported (patient outcome only). |
| Smit 2005 | Direct RCT Collaborative care |
| Smith 1986 | Direct RCT No MHW ‐ provision of treatment recommendations only. |
| Smith 1995 | Direct RCT No MHW ‐ provision of treatment recommendations only. |
| Sorby 1991 | Direct RCT No objective PCP behaviours reported (patient outcome only). No MHW ‐ self help only. |
| Stanley 2003 | Direct RCT No objective PCP behaviours reported (self report only). |
| Swindle 2003 | Direct RCT Collaborative care |
| Trepka 1986 | Direct RCT No PCP usual care group |
| Tudiver 1992 | Direct RCT MHW in community setting rather than primary care. |
| Turner 2006 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Unutzer 2002 | Direct RCT Collaborative care |
| van Boeijen 2005 | Direct RCT No PCP usual care group. No objective PCP behaviours reported (patient outcome only). |
| van Schaik 2006 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
| Vines 2004 | Direct CBA No objective PCP behaviours reported (patient outcome only). |
| Warner 1993 | Indirect RCT Consultation liaison |
| Wells 2000 | Direct RCT Collaborative care |
| Whooley 2000 | Direct RCT Collaborative care |
| Wickberg 1996 | Direct RCT No objective PCP behaviours measured (patient outcome only). |
| Wilkinson 1993 | Direct RCT Consultation liaison |
| Willemse 2006 | Direct RCT No objective PCP behaviours reported. |
| Williams 1989 | Indirect ITS No objective PCP behaviours measured (psychiatric admissions only). |
| Wood 1994 | Direct CBA No objective PCP behaviours reported (psychiatric admissions only). |
| Zayas 2004 | Direct RCT No objective PCP behaviours reported (patient outcome only). |
Contributions of authors
Peter Bower was responsible for the planning of the review and writing the original protocol.
Peter Bower and Elaine Harkness conducted the searches, extracted and recorded trial data.
Bonnie Sibbald extracted data and assisted in the writing of the first version of the review.
Sources of support
Internal sources
National Primary Care Research and Development Centre, UK.
External sources
No sources of support supplied
Declarations of interest
PB works as a paid consultant to the British Association of Counselling and Psychotherapy.
Edited (no change to conclusions)
References
References to studies included in this review
Ashurst 1983 {published data only}
- Ashurst P, Ward D. An evaluation of counselling in general practice: final report of the Leverhulme Counselling Project. Mental Health Foundation report 1983.
Ashworth 2000 {published data only}
- Ashworth M, Wastie J, Reid F, Clement S. The effects of psychotherapeutic interventions upon psychotropic prescribing and consultation rates in one general practice. Journal of Mental Health 2000;9:625‐35. [Google Scholar]
Baker 1996 {published data only}
- Baker R, Allen H, Gibson S, Newth J, Baker E. Evaluation of a primary care counselling service in Dorset. British Journal of General Practice 1998;48:1049‐53. [PMC free article] [PubMed] [Google Scholar]
- Baker R, Allen H, Gibson S, Newth J, Baker E. The Dorset Primary Care Counselling Service research evaluation report. Institute of Health & Community Studies, Bournemouth University, 1996.
Basler 1990 {published data only}
- Basler H, Rehfisch H. Follow up results of a cognitive‐behavioural treatment for chronic pain in a primary care setting. Psychology and Health 1990;4:293‐304. [Google Scholar]
Benson 1988 {published data only}
- Benson P, Turk T. Group therapy in a general practice setting for frequent attenders: a controlled study of mothers with pre‐school children. Journal of the Royal College of General Practitioners 1988;38(317):539‐41. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Blakey 1986 {published data only}
- Blakey R. Psychological treatment in general practice: its effect on patients and their families. Journal of the Royal College of General Practitioners 1986;36(286):209‐11. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Boot 1994 {published data only}
- Boot D, Gillies P, Fenelon J, Reubin R, Wilkins M, Gray P. Evaluation of the short‐term impact of counseling in general practice. Patient Education and Counseling 1994;24(1):79‐89. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Brantley 1986 {published data only}
- Brantley PJ, Veitia MC, Callon EB, Buss RR, Sias CR. Assessing the impact of psychological intervention on family practice clinic visits. Family Medicine 1986;18(6):351‐4. [MEDLINE: ] [PubMed] [Google Scholar]
Brodaty 1983 {published data only}
- Brodaty H, Andrews G. Brief psychotherapy in family practice. A controlled prospective intervention trial. British Journal of Psychiatry 1983;143:11‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Brouwers 2006 {published data only}
- Brouwers E, Tiemens B, Terluin B, Verhaak P. Effectiveness of an intervention to reduce sickness absence in patients with emotional distress or minor mental disorders: a randomized controlled effectiveness trial. General Hospital Psychiatry 2006;38:223‐9. [DOI] [PubMed] [Google Scholar]
- Brouwers E, dr Bruijne M, Terluin B, Tiemens B, Verhaak P. Cost effectiveness of an activating intervention by social workers for patients with minor mental disorders on sick leave: a randomized controlled trial. European Journal of Public Health 17;2:214‐20. [DOI] [PubMed] [Google Scholar]
Bruce 1998 {published data only}
- Bruce J, Watson D, Teijlingen E, Lawton K, Watson M, Palin A. Dedicated psychiatric care within general practice: health outcome and service providers' views. Journal of Advanced Nursing 1999;25:1060‐7. [DOI] [PubMed] [Google Scholar]
- Bruce J, Watson MS, Watson D, Palin AN, Lawton K. Workload implications of community psychiatric nurse employment by a general practice: a pilot study. British Journal of General Practice 1998;48(432):1419‐20. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Catalan 1991 {published data only}
- Catalan J, Gath DH, Anastasiades P, Bond SA, Day A, Hall L. Evaluation of a brief psychological treatment for emotional disorders in primary care. Psychological Medicine 1991;21(4):1013‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Coe 1996 {published data only}
- Coe N, Ibbs A, O'Brien J. The cost effectiveness of introducing counselling into the primary care setting in Somerset. Somerset Health Authority report 1996.
Corney 1984 {published data only}
- Corney R. Social work effectiveness in the management of depressed women: a clinical trial. Psychological Medicine 1981;11:417‐23. [DOI] [PubMed] [Google Scholar]
- Corney R. The effectiveness of attached social workers in the management of depressed female patients in general practice. Psychological Medicine 1984;Monograph Suppl 6:1‐47. [DOI] [PubMed] [Google Scholar]
- Corney R, Clare A. The effectiveness of attached social workers in the management of depressed women in general practice. British Journal of Social Work 1983;13:57‐74. [Google Scholar]
Corney 2003 {published data only}
- Corney R, Simpson S. Thirty‐six month outcome data from a trial of counselling with chronically depressed patients in a general practice setting. Psychology and Psychotherapy: Therapy, Research and Practice 2005;78:127‐38. [DOI] [PubMed] [Google Scholar]
- Simpson S, Corney R, Fitzgerald P, Beecham J. A randomised controlled trial to evaluate the effectiveness and cost‐effectiveness of counselling patients with chronic depression. Health Technology Assessment 2000;4(36):1‐83. [PubMed] [Google Scholar]
- Simpson S, Corney R, Fitzgerald P, Beecham J. A randomised controlled trial to evaluate the effectiveness and cost‐effectiveness of psychodynamic counselling with GP patients with chronic depression. Psychological Medicine 2003;33:229‐39. [DOI] [PubMed] [Google Scholar]
Earll 1982 {published data only}
- Earll L, Kincey J. Clinical psychology in general practice: a controlled trial evaluation. Journal of the Royal College of General Practitioners 1982;32(234):32‐7. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Ginsberg 1984 {published data only}
- Ginsberg G, Marks I, Waters H. Cost‐benefit analysis of a controlled trial of nurse therapy for neuroses in primary care. Psychological Medicine 1984;14(3):683‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gournay 1995 {published data only}
- Gournay K, Brooking J. An evaluation of the effectiveness of community psychiatric nurses in treating patients with minor mental disorders in primary care. London: Department of Health, 1992. [Google Scholar]
- Gournay K, Brooking J. Community psychiatric nurses in primary health care. British Journal of Psychiatry 1994;165(2):231‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Gournay K, Brooking J. The community psychiatric nurse in primary care: an economic analysis. Journal of Advanced Nursing 1995;22(4):769‐78. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Harvey 1998 {published data only}
- Harvey I. Counselling in general practice: the results of a randomised controlled trial. South Glamorgan FHSA report 1994.
- Harvey I, Nelson SJ, Lyons RA, Unwin C, Monaghan S, Peters TJ. A randomized controlled trial and economic evaluation of counselling in primary care. British Journal of General Practice 1998;48(428):1043‐8. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Hemmings 1997 {published data only}
- Hemmings A. Counselling in primary care: a randomised controlled trial. Patient Education and Counselling 1997;32(3):219‐30. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hunter 1983 {published data only}
- Hunter D, McCance C. Referrals to the psychiatric services by general practitioners in relation to the introduction of sessions by psychiatrists in health centres. Health Bulletin 1983;41(2):78‐83. [PubMed] [Google Scholar]
Kendrick 2005a {published data only}
- Kendrick T, Simons L, Mynors WL, Gray A, Lathlean J, Pickering R. A trial of problem‐solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN‐GP study. Health Technology Assessment 2005;9(37):1‐104, iii. [DOI] [PubMed] [Google Scholar]
- Kendrick T, Simons L. Mynors‐Wallis L, Gray A, Lathlean J, Pickering R, et al. Cost‐effectiveness of referral for generic care or problem‐solving treatment from community mental health nurses, compared with usual general practitioner care for common mental disorders: Randomised controlled trial. British Journal of Psychiatry 2006;189:50‐9. [DOI] [PubMed] [Google Scholar]
Kendrick 2005b {published data only}
- Kendrick T, Simons L, Mynors WL, Gray A, Lathlean J, Pickering R. A trial of problem‐solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN‐GP study. Health Technology Assessment 2005;9(37):1‐104, iii. [DOI] [PubMed] [Google Scholar]
- Kendrick T, Simons L. Mynors‐Wallis L, Gray A, Lathlean J, Pickering R, et al. Cost‐effectiveness of referral for generic care or problem‐solving treatment from community mental health nurses, compared with usual general practitioner care for common mental disorders: Randomised controlled trial. British Journal of Psychiatry 2006;189:50‐9. [DOI] [PubMed] [Google Scholar]
King 2000a {published data only}
- Bower P, Byford S, Sibbald B, Ward E, King M, Lloyd M, Gabbay M. Randomised controlled trial of non‐directive counselling, cognitive‐behaviour therapy and usual GP care for patients with depression. II: Cost effectiveness. BMJ 2000;321:1389‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, Byford S. Randomised controlled trial of non‐directive counselling, cognitive‐behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care. Health Technology Assessment 2000;4(19):1‐83. [PubMed] [Google Scholar]
- Ward E, King M, Lloyd M, Bower P, Sibbald B, Farrelly S, et al. Randomised controlled trial of non‐directive counselling, cognitive‐behaviour therapy and usual GP care for patients with depression. I: Clinical effectiveness. BMJ 2000;321:1383‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
King 2000b {published data only}
- Bower P, Byford S, Sibbald B, Ward E, King M, Lloyd M, Gabbay M. Randomised controlled trial of non‐directive counselling, cognitive‐behaviour therapy and usual GP care for patients with depression. II: Cost effectiveness. BMJ 2000;321:1389‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, Byford S. Randomised controlled trial of non‐directive counselling, cognitive‐behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care. Health Technology Assessment 2000;4(19):1‐83. [PubMed] [Google Scholar]
- Ward E, King M, Lloyd M, Bower P, Sibbald B, Farrelly S, et al. Randomised controlled trial of non‐directive counselling, cognitive‐behaviour therapy and usual GP care for patients with depression. I: Clinical effectiveness. BMJ 2000;321:1383‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lambert 2007 {published data only}
- Lambert R, Harvey I, Poland F. A pragmatic, unblinded randomised controlled trial comparing an occupational therapy‐led lifestyle approach. Journal of Affective Disorders 2007;99:63‐71. [DOI] [PubMed] [Google Scholar]
Lave 1998 {published data only}
- Lave J, Frank R, Schulberg H, Kamlet M. Cost‐effectiveness of treatments for major depression in primary care practice. Archives of General Psychiatry 1998;55:645‐51. [DOI] [PubMed] [Google Scholar]
Lester 2007 {published data only}
- Lester H, Freemantle N, Wilson S, Sorohan H, England E, Griffin C, Shankar A. Cluster randomised controlled trial of the effectiveness of primary care mental health workers. British Journal of General Practice 2007;57:196‐203. [PMC free article] [PubMed] [Google Scholar]
Lyon 1993 {published data only}
- Anon. Can counselling bring benefits for all?. Fundholding 1995;4(4):23‐4. [Google Scholar]
- Lyon D. The evaluation of counselling in primary care. Health Direct 1993;30:11. [Google Scholar]
Martin 1985 {published data only}
- Martin E, Martin PM. Changes in psychological diagnosis and prescription in a practice employing a counsellor. Family Practice 1985;2(4):241‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mynors‐Wallis 1997 {published data only}
- Mynors‐Wallis L, Davies I, Gray A, Barbour F, Gath D. A randomised controlled trial and cost analysis of problem‐solving treatment for emotional disorders given by community nurses in primary care. British Journal of Psychiatry 1997;170:113‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Pharoah 1996 {published data only}
- Pharoah P. Do counsellors in general practice change the prescribing of hypnotics and anxiolytics?. Primary Care Psychiatry 1996;1:263‐4. [Google Scholar]
Richards 2003 {published data only}
- Richards A, Barkham M, Cahill J, Richards D, Williams C, Heywood P. PHASE: a randomised, controlled trial of supervised self‐help cognitive behavioural therapy in primary care. British Journal of General Practice 2003;53:764‐70. [PMC free article] [PubMed] [Google Scholar]
Robson 1984 {published data only}
- Robson MH, France R, Bland M. Clinical psychologist in primary care: controlled clinical and economic evaluation. British Medical Journal (Clinical Research Ed) 1984;288(6433):1805‐8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Simpson 2003 {published data only}
- Simpson S, Corney R, Fitzgerald P. Counselling provision, prescribing and referral rates in a general practice setting. Primary Care Psychiatry 2003;8(4):115‐9. [Google Scholar]
Spurgeon 2007 {published data only}
- Spurgeon P, Hicks C, Barwell F, Walton I, Spurgeon T. Counselling in primary care: a study of the psychological impact and cost benefits of four chronic conditions. Journal of Psychotherapy and Counselling 2005;7(4):269‐90. [Google Scholar]
Stanton 1998 {published data only}
- Stanton R, Corney R. The effectiveness of counselling for general practice patients with marital problems. University of Greenwich report 1998.
Sumathipala 2000 {published data only}
- Sumathipala A, Hewege S, Hanwella R, Mann A. Randomized controlled trial of cognitive behaviour therapy for repeated consultations for medically unexplained complaints. Psychological Medicine 2000;30:747‐57. [DOI] [PubMed] [Google Scholar]
Tarrier 1983 {published data only}
- Tarrier N, Woof K. Psychologists in primary care and their effects on GP referrals to psychiatry. British Journal of Clinical and Social Psychiatry 1998;2:85‐7. [Google Scholar]
Teasdale 1984 {published data only}
- Teasdale JD, Fennell MJ, Hibbert GA, Amies PL. Cognitive therapy for major depressive disorder in primary care. British Journal of Psychiatry 1984;144:400‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Walker 1989 {published data only}
- Walker F, McKerracher D, Johnson G. Taking mental health services to the people: the effects of referral to traditional psychiatric facilities. New Zealand Medical Journal 1989;102(876):504‐6. [MEDLINE: ] [PubMed] [Google Scholar]
Wells 1992 {published data only}
- Wells A, Eagles J, Hunter D, Fowlie D. Changes in referral rates following community psychiatric nurse attachment to a primary care team. Psychiatric Bulletin 1992;16:264‐5. [Google Scholar]
References to studies excluded from this review
Adler 2004 {published data only}
- Adler D, Bungay K, Wilson I, Pei Y, Supran S, Peckham E, et al. The impact of a pharmacist intervention on 6 month outcomes in depressed primary care patients. General Hospital Psychiatry 2004;26:199‐209. [DOI] [PubMed] [Google Scholar]
Akerblad 2003 {published data only}
- Akerblad A, Bengtsson F, Ekselius L, Knorring L. Effects of an educational compliance enhancement programme and therapeutic drug monitoring on treatment adherence in depressed patients managed by general practitioners. International Clinical Psychopharmacology 2003;18:347‐54. [DOI] [PubMed] [Google Scholar]
Appleby 1997 {published data only}
- Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive‐behavioural counselling in the treatment of postnatal depression. BMJ 1997;314(7085):932‐6. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Araya 2003 {published data only}
- Araya R, Rojas G, Fritsch R, Gaete J, Rojas M, Simon G, Peters T. Treating depression in primary care in low income women in Santiago, Chile: a randomised controlled trial. Lancet 2003;361:995‐1000. [DOI] [PubMed] [Google Scholar]
Bannerjee 1996 {published data only}
- Bannerjee S, Shamash K, Macdonald AJ, Mann AH. Randomised controlled trial of effect of intervention by psychogeriatric team on depression in frail elderly people at home. BMJ 1996;313(7064):1058‐61. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barksy 2004 {published data only}
- Barsky A, Ahern D. Cognitive behavior therapy for hypochondriasis: a randomized controlled trial. JAMA 2004;291:1464‐70. [DOI] [PubMed] [Google Scholar]
Barrowclough 2001 {published data only}
- Barrowclough C, King P, Colville J, Russell E, Burns A, Tarrier N. A randomized trial of the effectiveness of cognitive‐behavioural therapy and supportive counselling for anxiety symptoms in older adults. Journal of Consulting and Clinical Psychology 2001;69:756‐62. [DOI] [PubMed] [Google Scholar]
Basler 1996 {published data only}
- Basler H, Brinkmeier U, Buser K, Haehn K, Molders‐Kober R. Psychological group treatment of obese essential hypertensives by lay therapists in rural general practice settings. Journal of Psychosomatic Research 1996;29:383‐91. [DOI] [PubMed] [Google Scholar]
Bernal 1995 {published data only}
- Bernal A, Fuste R, Urbieta R, Montesinos I. Relaxation therapy in primary care for patients with anxiety and somatoform disorders [Tratamentio de relajacion en pacientes con trastornos de ansiedad y somatoformes en atencion primaria]. Atencion Primaria 1995;15(8):39‐48. [PubMed] [Google Scholar]
Bindman 2001 {published data only}
- Bindman A, Goldberg D, Chisholm D, Amponsah S, Shetty G, Brown J. Primary and secondary care for mental illness: impact of a link worker service on admission rates and costs. Journal of Mental Health 2001;10:637‐44. [Google Scholar]
Blackburn 1981 {published data only}
- Blackburn I, Moore R. Controlled acute and follow up trial of cognitive therapy and pharmacotherapy in out‐patients with recurrent depression. British Journal of Psychiatry 1981;171:328‐34. [DOI] [PubMed] [Google Scholar]
- Blackburn IM, Eunson KM, Bishop S. A two‐year naturalistic follow‐up of depressed patients treated with cognitive therapy, pharmacotherapy and a combination of both. Journal of Affective Disorders 1986;10(1):67‐75. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Blanchard 1995 {published data only}
- Blanchard M, Waterreus A, Mann A. Can a brief intervention have a longer term benefit? The case of the research nurse and depressed older people in the community. International Journal of Geriatric Psychiatry 1999;14:733‐8. [PubMed] [Google Scholar]
- Blanchard M, Waterreus A, Mann A. The effect of primary care nurse intervention upon older people screened as depressed. International Journal of Geriatric Psychiatry 1995;10:289‐98. [Google Scholar]
Blay 2002 {published data only}
- Blay S, Vel Fucks J, Barruzi M, Pietro M, Gastal F, Neto A, et al. Effectiveness of time‐limited psychotherapy for minor psychiatric disorders: Randomised controlled trial evaluating immediate v. long‐term effects. British Journal of Psychiatry 2002;180:416‐22. [DOI] [PubMed] [Google Scholar]
Blomhoff 2001 {published data only}
- Blomhoff S, Tangen Haug T, Hellstrom K, Holme I, Humble M, Madsbu H, Wold J. Randomised controlled general practice trial of sertraline, exposure therapy and combined treatment in generalised social phobia. British Journal of Psychiatry 2001;179:23‐30. [DOI] [PubMed] [Google Scholar]
Blowers 1987 {published data only}
- Blowers C, Cobb J, Mathews A. Generalised anxiety: a controlled treatment study. Behaviour Research and Therapy 1987;25(6):493‐502. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Brook 2003 {published data only}
- Brook O, Hout B, Nieuwenhuyse H, Haan M. Effects of coaching by community pharmacists on psychological symptoms of antidepressant users: a randomised controlled trial. European Neuropsychopharmacology 2003;13:347‐54. [DOI] [PubMed] [Google Scholar]
- Brook O, Hout H, Nieuwenhuyse H, Heerdink E. Impact of coaching by community pharmacists on drug attitude of depressive primary care patients and acceptability to patients: a randomized controlled trial. European Neuropsychopharmacology 2003;13:1‐9. [DOI] [PubMed] [Google Scholar]
Brooker 1994 {published data only}
- Brooker C, Falloon I, Butterworth A, Goldberg D, Graham‐Hole V, Hillier V. The outcome of training community psychiatric nurses to deliver psychosocial intervention. British Journal of Psychiatry 1994;165(2):222‐30. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Brown 1996 {published data only}
- Brown C, Schulberg HC, Madonia MJ, Shear MK, Houck PR. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. American Journal of Psychiatry 1996;153(10):1293‐300. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Browne 2002 {published data only}
- Browne G, Steiner M, Roberts J, Gafni A, Byrne C, Dunn E, et al. Sertaline and/or interpersonal psychotherapy for patients with dysthymic disorder in primary care: 6 month comparison with longitudinal 2 year follow up of effectiveness and costs. Journal of Affective Disorders 2002;68:317‐30. [DOI] [PubMed] [Google Scholar]
Bruce 2004 {published data only}
- Bruce M, Have T, Reynolds C, Katz I, Schulberg H, Mulsant B, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients. JAMA 2004;291(9):1081‐91. [DOI] [PubMed] [Google Scholar]
Busch 1996 {published data only}
- Busch C, Bartholomew J, Sharp D. Group treatment of anxiety and stress in a general practice setting. Primary Care Psychiatry 1996;2:59‐67. [Google Scholar]
Butler 1987 {published data only}
- Butler G, Cullington A, Hibbert G, Klimes I, Gelder M. Anxiety management for persistent generalised anxiety. British Journal of Psychiatry 1987;151:535‐42. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Butler 1991 {published data only}
- Butler G, Fennell M, Robson P, Gelder M. Comparison of behavior therapy and cognitive behavior therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology 1991;59(1):167‐75. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Callahan 1994 {published data only}
- Callahan CM, Hendrie HC, Dittus RS, Brater DC, Hui SL, Tierney WM. Improving treatment of late life depression in primary care: a randomized clinical trial. Journal of the American Geriatrics Society 1994;42(8):839‐46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cappocia 2004 {published data only}
- Boudreau D, Capoccia K, Sullivan S, Blough D, Ellsworth A, Clark D, et al. Collaborative care to improve outcomes in major depression. Annals of Pharmacotherapy 2002;36:585‐91. [DOI] [PubMed] [Google Scholar]
- Capoccia K, Boudreau D, Blough D, Ellsworth A, Clark D, Stevens N, et al. Randomized trial of pharmacist interventions to improve depression care and outcomes in primary care. American Journal of Health System Pharmacy 2004;61:364‐72. [DOI] [PubMed] [Google Scholar]
Carr 1997 {published data only}
- Carr VJ, Lewin TJ, Walton JM, Faehrmann C, Reid AL. Consultation‐liaison psychiatry in general practice. Australian and New Zealand Journal of Psychiatry 1997;31(1):85‐94. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Catalan 1984 {published data only}
- Catalan J, Gath D, Bond A, Martin P. The effects of non‐prescribing anxiolytics in general practice. II. Factors associated with outcome. British Journal of Psychiatry 1984;144:603‐10. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Catalan J, Gath D, Edmonds G, Ennis J. The effects of non‐prescribing of anxiolytics in general practice. I. Controlled evaluation of psychiatric and social outcome. British Journal of Psychiatry 1984;144:593‐602. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ceroni 2002 {published data only}
- Ceroni G, Rucci P, Beradi D, Ceroni F, Katon W. Case review vs. usual care in primary care patients with depression: a pilot study. General Hospital Psychiatry 2002;24:71‐80. [DOI] [PubMed] [Google Scholar]
Chalder 1997 {published data only}
- Chalder T, Wallace P, Wessely S. Self help treatment of chronic fatigue in the community: a randomised controlled trial. British Journal of Health Psychology 1997;2:189‐97. [Google Scholar]
Chilvers 2001 {published data only}
- Bedi N, Chilvers C, Churchill R, Dewey M, Duggan C, Fielding K, et al. Assessing effectiveness of treatment of depression in primary care: partially randomised preference trial. British Journal of Psychiatry 2000;177:312‐8. [DOI] [PubMed] [Google Scholar]
- Chilvers C, Dewey M, Fielding K, Gretton V, Miller P, Palmer B, et al. Counselling versus Antidepressant in Primary Care Study group. Antidepressant drugs and generic counselling for treatment of major depression in primary care: randomised trial with patient preference arms. BMJ 2001;322:772‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller P, Chilvers C, Dewey M, Fielding K, Gretton V, Palmer B, et al. Counseling versus antidepressant therapy for the treatment of mild to moderate depression in primary care: economic analysis. International Journal of Technology Assessment in Health Care 2003;19:80‐90. [DOI] [PubMed] [Google Scholar]
Clarke 2005 {published data only}
- Clarke G, Debar L, Lynch F, Powell J, Gale J, O'Connor E, et al. A randomized effectiveness trial of brief cognitive‐behavioral therapy for depressed adolescents receiving antidepressant medication. Journal of the American Academy of Child and Adolescent Psychiatry 2005;44:888‐98. [PubMed] [Google Scholar]
Coleman 1999 {published data only}
- Coleman E, Grothaus L, Sandhu N, Wagner E. Chronic care clinics: a randomized controlled trial of a new model of primary care for frail older adults. Journal of the American Geriartrics Society 1999;47:775‐83. [DOI] [PubMed] [Google Scholar]
Cooper 1975 {published data only}
- Cooper B, Harwin BG, Depla C, Shepherd M. Mental health care in the community: an evaluative study. Psychological Medicine 1975;5(4):372‐80. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cooper 1997 {published data only}
- Cooper P, Murray L. The impact of psychological treatments of postpartum depression on maternal mood and infant development. In: Murray L, Cooper P editor(s). Postpartum Depression and Child Development. New York: The Guildford Press, 1997:201‐20. [Google Scholar]
Cooper 2003 {published data only}
- Cooper P, Murray L, Wilson A, Romaniuk H. Controlled trial of the short‐ and long‐term effect of psychological treatment of post‐partum depression 1. Impact on maternal mood. British Journal of Psychiatry 2003;182:412‐9. [PubMed] [Google Scholar]
- Murrray L, Cooper P, Wilson A, Romaniuk H. Controlled trial of the short‐ and long‐term effect of psychological treatment of post‐partum depression 2. Impact on the mother‐child relationship and child outcome. British Journal of Psychiatry 2003;182:420‐7. [PubMed] [Google Scholar]
Coulehan 1997 {published data only}
- Coulehan JL, Schulberg HC, Block MR, Madonia MJ, Rodriguez E. Treating depressed primary care patients improves their physical, mental, and social functioning. Archives of Internal Medicine 1997;157(10):1113‐20. [MEDLINE: ] [PubMed] [Google Scholar]
Cullen 1976 {published data only}
- Cullen KJ. A six‐year controlled trial of prevention of children's behavior disorders. Journal of Pediatrics 1976;88(4 Pt. 1):662‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Dalgard 2006 {published data only}
- Dalgard O. A randomized controlled trial of a psychoeducational group program for unipolar depression in adults in Norway. Clinical Practice and Epidemiology in Mental Health 2006;2:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Datto 2003 {published data only}
- Datto C, Thompson R, Horowitz D, Disbot M, Oslin D. The pilot study of a telephone disease management program for depression. General Hospital Psychiatry 2003;25:169‐77. [DOI] [PubMed] [Google Scholar]
Dey 2002 {published data only}
- Dey P, Roaf E, Collins S, Shaw H, Steele R, Donmall M. Randomized controlled trial to assess the effectiveness of a primary health care liaison worker in promoting shared care for opiate users. Journal of Public Health Medicine 2002;24:38‐42. [DOI] [PubMed] [Google Scholar]
Dietrich 2004 {published data only}
- Dietrich A, Oxman T, Williams J, Schulberg H, Bruce M, Lee P, et al. Re‐engineering systems for the treatment of depression in primary care: cluster randomised controlled trial. BMJ 2004;327(7466):602. [DOI] [PMC free article] [PubMed] [Google Scholar]
Donnan 1990 {published data only}
- Donnan P, Hutchinson A, Paxton R, Grant B, Firth M. Self‐help materials for anxiety: a randomized controlled trial in general practice. British Journal of General Practice 1990;40(341):498‐501. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Eayrs 1984 {published data only}
- Eayrs C, Rowan D, Harvey P. Behavioural group training for anxiety management. Behavioural Psychotherapy 1984;12:117‐29. [Google Scholar]
Emmanuel 2002 {published data only}
- Emmanuel JS, McGee A, Ukoumunne OC, Tyrer P. A randomised controlled trial of enhanced key‐worker liaison psychiatry in general practice. Social Psychiatry and Psychiatric Epidemiology 2002;37:261‐6. [DOI] [PubMed] [Google Scholar]
Escobar 2007 {published data only}
- Escobar J, Gara M, Martinez A, Interian A, Warman M, Allen L, et al. Effectiveness of a time‐limited cognitive behavior therapy type intervention among primary care patients with medically unexplained symptoms. Annals of Family Medicine 2007;5:328‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Espie 2001 {unpublished data only}
- Espie C, Inglis S, Tessier S, Harvey L. The clinical effectiveness of cognitive behaviour therapy for chronic insomnia: implementation and evaluation of a sleep clinic in general medical practice. Behaviour Research and Therapy 2001;39:45‐60. [DOI] [PubMed] [Google Scholar]
Espie 2007 {published data only}
- Espie C, MacMahon K, Kelly H, Broomfield N, Douglas N, Engleman H, et al. Randomized clinical effectiveness trial of nurse‐administered small‐group cognitive behavior therapy for persistent insomnia in general practice. Sleep 2007;30:574‐84. [DOI] [PubMed] [Google Scholar]
Finley 2000 {published data only}
- Finley P, Rens H, Gess S, Loiue C. Case management of depression by clinical pharmacists in a primary care setting. Formulary 1999;34:864‐70. [Google Scholar]
- Finley P, Rens H, Pont J, Gess S, Louie C, Bull S, et al. Impact of a collaborative care model on depression in a primary care setting: a randomized controlled trial. Pharmacotherapy 2003;23(9):1175‐85. [DOI] [PubMed] [Google Scholar]
Finney 1989 {published data only}
- Finney J, Lemanek K, Cataldo M, Katz H, Fuqua R. Pediatric psychology in primary health care: brief targeted therapy for recurrent abdominal pain. Behaviour Therapy 198;20:283‐91. [Google Scholar]
Finney 1991 {published data only}
- Finney J, Riley A, Cataldo M. Psychology in primary health care: effects of brief targeted therapy on children's medical care utilisation. Journal of Pediatric Psychology 1991;16(4):447‐61. [DOI] [PubMed] [Google Scholar]
Friedli 1999 {unpublished data only}
- Friedli K, King M, Lloyd M. Randomised controlled assessment of counselling versus routine general practitioner care: cost minimisation analysis. British Journal of General Practice 2000;50:276‐83. [Google Scholar]
- Friedli K, King M, Lloyd M, Horder J. Randomised controlled assessment of non‐directive psychotherapy versus routine general‐practitioner care. Lancet 1997;350:1662‐5. [DOI] [PubMed] [Google Scholar]
Gater 1997 {published data only}
- Gater R, Goldberg D, Jackson G, Jennett N, Lowson K, Ratcliffe J, et al. The care of patients with chronic schizophrenia: a comparison between two services. Psychological Medicine 1997;27(6):1325‐36. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gilham 2006 {published data only}
- Gilham J, Hamilton J, Freres D, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn resiliency program. Journal of Abnormal Child Psychology 2006;34:203‐19. [DOI] [PubMed] [Google Scholar]
Goldberg 1996 {published data only}
- Goldberg D, Jackson G, Gater R, Campbell M, Jennett N. The treatment of common mental disorders by a community team based in primary care: a cost‐effectiveness study. Psychological Medicine 1996;26(3):487‐92. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Grant 2000 {published data only}
- Grant C, Goodenough T, Harvey I, Hine C. A randomised controlled trial and economic evaluation of a referrals facilitator between primary care and the voluntary sector. BMJ 2000;320:419‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Graves 1981 {published data only}
- Graves R, Hastrup J. Psychological intervention and medical utilisation in children and adolescents of low‐income families. Professional Psychology 1981;12:426‐33. [Google Scholar]
Hebert 1994 {published data only}
- Hebert R, Leclerc G, Bravo G, Girouard D, LeFrancois R. Efficacy of a support group programme for caregivers of demented patients in the community: a randomized controlled trial. Archives of Gerontology and Geriatrics 1994;18:1‐14. [DOI] [PubMed] [Google Scholar]
Hedrick 2003 {published data only}
- Hedrick S, Chaney E, Felker B, Liu C, Hasenberg N, Heagerty P, et al. Effectiveness of collaborative care depression treatment in Veterans' Affairs Primary Care. Journal of General Internal Medicine 2003;18:9‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hellman 1990 {published data only}
- Hellman CJ, Budd M, Borysenko J, McClelland DC, Benson H. A study of the effectiveness of two group behavioral medicine interventions for patients with psychosomatic complaints. Behavioral Medicine 1990;16(4):165‐73. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hemmings 1993 {published data only}
- Hemmings A, Cogan M. The non‐pharmacological management of anxiety. University of Sussex report 1993.
Hirsch 1997 {published data only}
- Hirsch T, Perry P, Hirsch S, Bagadia V, Pradhan P, Kumar R, et al. Effects of benzodiazepenes and counselling on minor psychiatric morbidity: report from a WHO collaborative study. WHO report 1997.
Holden 1987 {published data only}
- Holden JM, Sagovsky R, Cox JL. Counselling in a general practice setting: controlled study of health visitor intervention in treatment of postnatal depression. BMJ 1989;298(6668):223‐6. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Holdsworth 1996 {published data only}
- Holdsworth N, Paxton R, Seidel S, Thomson D, Shrubb S. Parallel evaluations of new guidance materials for anxiety and depression in primary care. Journal of Mental Health 1996;5:195‐207. [Google Scholar]
Honey 2002 {published data only}
- Honey K, Bennett P, Morgan M. A brief psycho‐educational group intervention for postnatal depression. British Journal of Clinical Psychology 2002;41:405‐9. [DOI] [PubMed] [Google Scholar]
Horowitz 1996 {published data only}
- Horowitz CR, Goldberg HI, Martin DP, Wagner EH, Fihn SD, Christensen DB, et al. Conducting a randomized controlled trial of CQI and academic detailing to implement clinical guidelines. Joint Commission Journal on Quality Improvement 1996;22(11):734‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hunkeler 2000 {published data only}
- Hunkeler E, Meresman J, Hargreaves W, Fireman B, Berman W, Kirsch A, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Archives of Family Medicine 2000;9(8):700‐8. [DOI] [PubMed] [Google Scholar]
Hunter 1995 {published data only}
- Hunter M, Liao K. Problem solving groups for mid‐aged women in general practice: a pilot study. Journal of Reproductive and Infant Psychology 1995;13:147‐51. [Google Scholar]
Jackson 1993 {published data only}
- Jackson G, Gater R, Goldberg D, Tantam D, Loftus L, Taylor H. A new community mental health team based in primary care: a description of the service and its effect on service use in the first year. British Journal of Psychiatry 1993;162:375‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Jenkins 1994 {published data only}
- Jenkins D, MacDonald A. Should general practitioners refer more of their elderly patients to psychiatric services?. International Journal of Geriatric Medicine 1994;9:461‐5. [Google Scholar]
Judd 2001 {published data only}
- Judd F, Piterman L, Cockram A, McCall L, Weissman M. A comparative study of venlafaxine with a focused education and psychotherapy program versus venlafaxine alone in the treatment of depression in general practice. Human Psychopharmacology 2001;16:423‐8. [DOI] [PubMed] [Google Scholar]
Karlberg 1998 {published data only}
- Karlberg L, Krakau I, Unden AL. Type A behavior intervention in primary health care reduces hostility and time pressure: a study in Sweden. Social Science and Medicine 1998;46(3):397‐402. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kashner 1992 {published data only}
- Kashner M, Rost K, Cohen B, Anderson M, Smith G. Enhancing the health of somatization disorder patients. Psychosomatics 1995;36:462‐70. [DOI] [PubMed] [Google Scholar]
- Kashner M, Rost K, Smith R, Lewis S. An analysis of panel data: the impact of a psychiatric consultation letter on the expenditures and outcomes of care for patients with somatisation disorder. Medical Care 1992;30:811‐21. [PubMed] [Google Scholar]
- Rost K, Kashner M, Smith R. Effectiveness of psychiatric intervention with somatization disorder patients: improved outcomes at reduced costs. General Hospital Psychiatry 1994;16:381‐7. [DOI] [PubMed] [Google Scholar]
Katon 1992 {published data only}
- Katon W, Korff M, Lin E, Bush T, Russo J, Lipscomb P, et al. A randomized trial of psychiatric consultation with distressed high utilizers. General Hospital Psychiatry 1992;14(2):86‐98. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Katon 1995 {published data only}
- Katon W, Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA 1995;273(13):1026‐31. [MEDLINE: ] [PubMed] [Google Scholar]
Katon 1996 {published data only}
- Katon W, Robinson P, Korff M, Lin E, Bush T, Ludman E, et al. A multifaceted intervention to improve treatment of depression in primary care. Archives of General Psychiatry 1996;53(10):924‐32. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Katon 2001 {published data only}
- Katon W, Rutter C, Ludman E, Korff M, Lin E, Simon G, et al. A randomized trial of relapse prevention of depression in primary care. Archives of General Psychiatry 2001;58:241‐7. [DOI] [PubMed] [Google Scholar]
Katon 2003 {published data only}
- Katon W, Korff M, Lin E, Simon G, Ludman E, Bush T, et al. Improving primary care treatment of depression among patients with diabetes mellitus: the design of the Pathways study. General Hospital Psychiatry 2003;25:158‐68. [DOI] [PubMed] [Google Scholar]
- Katon W, Korff M, Lin E, Simon G, Ludman E, Russo J, et al. The Pathways study: a randomized trial of collaborative care in patients with diabetes and depression. Archives of General Psychiatry 2004;61:1042‐9. [DOI] [PubMed] [Google Scholar]
Katzelnick 2000 {published data only}
- Katzelnick D, Simon G, Pearson S, Manning W, Helstad C, Henk H, et al. Randomized trial of a depression management program in high utilizers of medical care. Archives of Family Medicine 2000;9(4):345‐51. [DOI] [PubMed] [Google Scholar]
- Simon G, Manning W, Katzelnick D, Pearson S, Henk H, Helstad C. Cost‐effectiveness of systematic depression treatment for high utilisers of general medical care. Archives of General Psychiatry 2001;58:181‐7. [DOI] [PubMed] [Google Scholar]
Kiely 1986 {published data only}
- Kiely BG, McPherson IG. Stress self‐help packages in primary care: a controlled trial evaluation. Journal of the Royal College of General Practitioners 1986;36:307‐9. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
King 1994 {published data only}
- King M, Broster G, Lloyd M, Horder J. Controlled trials in the evaluation of counselling in general practice. British Journal of General Practice 1994;44(382):229‐32. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Klerman 1996 {published data only}
- Klerman G, Budman S, Berwick S, Weissman M, Damico‐White J, Demby A, et al. Efficacy of a brief psychosocial intervention for symptoms of stress and distress among patients in primary care. Medical Care 1996;25(11):1078‐88. [DOI] [PubMed] [Google Scholar]
Kolk 2004 {published data only}
- Kolk A, Schagen S, Hanewald G. Multiple medically unexplained physical symptoms and health care utilization: outcome of psychological intervention and patient‐related predictors of change. Journal of Psychosomatic Research 2004;57:379‐89. [DOI] [PubMed] [Google Scholar]
Lang 2003 {published data only}
- Lang A. Brief intervention for co‐occurring anxiety and depression in primary care: a pilot study. International Journal of Psychiatry in Medicine 2004;33(2):141‐54. [DOI] [PubMed] [Google Scholar]
Lang 2006 {published data only}
- Lang A, Norman G, Pollyanna C. A randomized trial of a brief mental health intervention for primary care patients. Journal of Consulting and Clinical Psychology 2006;74:1173‐9. [DOI] [PubMed] [Google Scholar]
Lewis 1996 {published data only}
- Lewis G, Sharp D, Bartholomew J, Pelosi AJ. Computerized assessment of common mental disorders in primary care: effect on clinical outcome. Family Practice 1996;13(2):120‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lidbeck 1997 {published data only}
- Lidbeck J. Group therapy for somatization disorders in general practice: effectiveness of a short cognitive‐behavioural treatment model. Acta Psychiatrica Scandinavica 1997;96(1):14‐24. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lin 1997 {published data only}
- Lin EH, Katon WJ, Simon GE, Korff M, Bush TM, Rutter CM, et al. Achieving guidelines for the treatment of depression in primary care: is physician education enough?. Medical Care 1997;35(8):831‐42. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lindsay 1987 {published data only}
- Lindsay W, Gamsu C, McLaughlin E, Hood E, Espie C. A controlled trial of treatments for generalised anxiety. British Journal of Clinical Psychology 1987;26:3‐15. [DOI] [PubMed] [Google Scholar]
Lofvander 1997 {published data only}
- Lofvander M. Cognitive‐behavioural treatment of chronic pain in primary care: a three year follow up. European Journal of General Practice 2002;8:151‐8. [Google Scholar]
- Lofvander M, Engstrom A, Theander H, Furhoff AK. Rehabilitation of young immigrants in primary care. A comparison between two treatment models. Scandinavian Journal of Primary Health Care 1997;15(3):123‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lynch 1997 {published data only}
- Lynch DJ, Tamburrino MB, Nagel R. Telephone counseling for patients with minor depression: preliminary findings in a family practice setting. The Journal of Family Practice 1997;44(3):293‐8. [MEDLINE: ] [PubMed] [Google Scholar]
Malcolm 2002 {published data only}
- Malcolm H. Stress management groups in general practice. Australian Family Physician 2007;36(4):276‐78. [PubMed] [Google Scholar]
Mann 1998 {published data only}
- Mann AH, Blizard R, Murray J, Smith JA, Botega N, MacDonald E, et al. An evaluation of practice nurses working with general practitioners to treat people with depression. British Journal of General Practice 1998;48(426):875‐9. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Marks 1985 {published data only}
- Marks I. Controlled trial of psychiatric nurse therapists in primary care. British Medical Journal 1985;290:1181‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKechnie 1981 {published data only}
- McKechnie AA, Philip AE, Ramage JG. Psychiatric services in primary care: specialized or not?. Journal of the Royal College of General Practitioners 1981;31(231):611‐4. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
McLeod 1997 {published data only}
- McLeod CC, Budd MA, McClelland DC. Treatment of somatization in primary care. General Hospital Psychiatry 1997;19(4):251‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Milgrom 2005 {published data only}
- Milgrom J, Negri L, Gemmill A, McNeil M, Martin P. A randomized controlled trial of psychological intervention for postnatal depression. British Journal of Clinical Psychology 2005;44:529‐42. [DOI] [PubMed] [Google Scholar]
Milne 1988 {published data only}
- Milne D, Souter K. A re‐evaluation of the clinical psychologist in general practice. Journal of the Royal College of General Practitioners 1988;38(315):457‐60. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Miranda 1994 {published data only}
- Miranda J, Munoz R. Intervention for minor depression in primary care patients. Psychosomatic Medicine 1994;56(2):136‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Miranda 2003 {published data only}
- Miranda J, Azocar F, Organista K, Dwyer E, Areane P. Treatment of depression among improverished primary care patients from ethnic minority groups. Psychiatric Services 2003;54:219‐25. [DOI] [PubMed] [Google Scholar]
Munoz 1995 {published data only}
- Munoz RF, Ying YW, Bernal G, Perez‐Stable EJ, Sorensen JL, Hargreaves WA, et al. Prevention of depression with primary care patients: a randomized controlled trial. American Journal of Community Psychology 1995;23(2):199‐222. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mynors‐Wallis 1995 {published data only}
- Mynors‐Wallis LM, Gath DH, Lloyd‐Thomas AR, Tomlinson D. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. British Medical Journal 1995;310(6977):441‐5. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mynors‐Wallis 2000 {published data only}
- Mynors‐Wallis LM, Gath DH, Day A, Baker F. Randomised controlled trial of problem solving treatment, antidepressant medication, and combined treatment for major depression in primary care. BMJ 2000;320(7226):26‐30. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nazareth 1996 {published data only}
- Nazareth I, King M, Tai SS. Monitoring psychosis in general practice: a controlled trial. British Journal of Psychiatry 1996;169(4):475‐82. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Onyett 1988 {published data only}
- Onyett S, Turpin G. Benzodiazepene withdrawal in primary care: a comparison of behavioural group training and individual sessions. Behavioral Psychotherapy 1988;16:297‐312. [Google Scholar]
Oslin 2003 {published data only}
- Oslin D, Sayers S, Ross J, Kane V, Have T, Conigliaro J, Cornelius J. Disease management for depression and at risk drinking via telephone in an older population of veterans. Psychosomatic Medicine 2003;65:931‐7. [DOI] [PubMed] [Google Scholar]
Paykel 1982 {published data only}
- Paykel ES, Mangen SP, Griffith JH, Burns TP. Community psychiatric nursing for neurotic patients: a controlled trial. British Journal of Psychiatry 1982;140:573‐81. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Petrou 2006 {published data only}
- Petrou S, Cooper P, Murray L, Davidson L. Cost‐effectiveness of a preventive counseling and support package for postnatal depression. International Journal of Technology Assessment in Health Care 2006;22(4):443‐53. [DOI] [PubMed] [Google Scholar]
Peveler 1999 {published data only}
- Peveler R, George C, Kinmonth A, Campbell M, Thompson C. Effect of antidepressant drug counselling and information leaflets on adherence to drug treatment in primary care: randomised controlled trial. BMJ 1999;319:612‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Power 1989 {published data only}
- Power K, Jerrom W, Simpson R, Mitchell M, Swanson V. A controlled comparison of cognitive‐behaviour therapy, diazepam and placebo in the management of generalised anxiety. Behavioural Psychotherapy 1989;17:1‐14. [Google Scholar]
Power 1990 {published data only}
- Power K, Simpson R, Swanson V, Wallace L, Feistner A, Sharp D. A controlled comparison of cognitive‐behaviour therapy, diazepam, and placebo, alone and in combination, for the treatment of generalised anxiety disorder. Journal of Anxiety Disorders 1990;4:267‐92. [Google Scholar]
- Power KG, Simpson RJ, Swanson V, Wallace LA. Controlled comparison of pharmacological and psychological treatment of generalized anxiety disorder in primary care. British Journal of General Practice 1990;40(336):289‐94. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Raphael 1977 {published data only}
- Raphael B. Preventive intervention with the recently bereaved. Archives of General Psychiatry 1977;34:1450‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rickles 2004 {published data only}
- Rickles, N. A randomized controlled study evaluating the impact of an antidepressant monitoring program on consumer outcomes. University of Wisconsin‐Madison, 2003. [Google Scholar]
Ridsdale 2001 {published data only}
- Ridsdale L, Godfrey E, Chalder T, Seed P, King M, Wallace P, Wessely S, Fatigue Trialists Group. Chronic fatigue in general practice: is counselling as good as cognitive behaviour therapy? A UK randomised trial. British Journal of General Practice 2001;51:19‐24. [PMC free article] [PubMed] [Google Scholar]
Ridsdale 2004 {published data only}
- McCrone P, Ridsdale L, Darbishire L, Seed P. Cost‐effectiveness of cognitive‐behavioural therapy, graded exercise and usual care for patients with chronic fatigue in primary care. Psychological Medicine 2004;34:991‐9. [DOI] [PubMed] [Google Scholar]
- Ridsdale L, Darbishire L, Seed P. Is graded exercise better than cognitive behaviour therapy for fatigue? A UK randomized trial in primary care. Psychological Medicine 2004;34:37‐49. [DOI] [PubMed] [Google Scholar]
Risdale 1999 {published data only}
- Risdale L, Kwan I, Cryer C. The effect of a special nurse on patients' knowledge of epilepsy and their emotional state. British Journal of General Practice 1999;49:285‐9. [PMC free article] [PubMed] [Google Scholar]
Roberts 2006 {published data only}
- Roberts L, Wilson S, Singh S, Roalfe A, Greenfield S. Gut directed hypnotherapy for irritable bowel syndrome: piloting a primary care‐based randomised controlled trial. British Journal of General Practice 2006;56:115‐21. [PMC free article] [PubMed] [Google Scholar]
Ross 1985 {published data only}
- Ross M, Scott M. An evaluation of the effectiveness of individual and group cognitive therapy in the treatment of depressed patients in an inner city health centre. Journal of the Royal College of General Practitioners 1985;35(274):239‐42. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Rost 1994 {published data only}
- Rost K, Kashner TM, Smith RG Jr. Effectiveness of psychiatric intervention with somatization disorder patients: improved outcomes at reduced costs. General Hospital Psychiatry 1994;16(6):381‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rost 2001 {published data only}
- Pyne J, Smith J, Fortney J, Zhang M, Williams D, Rost K. Cost‐effectiveness of a primary care intervention for depressed females. Journal of Affective Disorders 2003;74:23‐32. [DOI] [PubMed] [Google Scholar]
- Rost K, Nutting P. Managing depression as a chronic disease: a randomised trial of ongoing treatment in primary care. BMJ 2002;325:934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rost K, Nutting P, Smith J, Werner J, Duan N. Improving depression outcomes in community primary care practice: a randomized trial of the QuEST intervention. Journal of General Internal Medicine 2001;16:143‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rost K, Smith J, Dickinson M. The effect of improving primary care depression management on employee absenteeism and productivity: a randomized trial. Medical Care 2004;42(12):1202‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roy‐Byrne 2001 {published data only}
- Roy‐Byrne P, Katon W, Cowley D, Russo J. A randomized effectiveness trial of collaborative care for patients with panic disorder in primary care. Archives of General Psychiatry 2001;59:869‐76. [DOI] [PubMed] [Google Scholar]
Roy‐Byrne 2005 {published data only}
- Roy‐Byrne P, Craske M, Stein M, Sullivan G, Bystrisky A, Katon W, et al. A randomized effectiveness trial of cognitive‐behavioral therapy and medication for primary care panic disorder. Archives of General Psychiatry 2005;62:290‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saarijarvi 1991 {published data only}
- Saarijarvi S. A controlled study of couple therapy in chronic low back pain patients. Effects on marital satisfaction, psychological distress and health attitudes. Journal of Psychosomatic Research 1991;35(2‐3):265‐72. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Saarijarvi S, Rytokoski U, Alanen E. A controlled study of couple therapy in chronic low back pain patients. No improvement of disability. Journal of Psychosomatic Research 1991;35(6):671‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Salminen 2005 {published data only}
- Salminen M, Isoaho R, Vahlberg T, Ojanlatva A, Kivela S. Effects of a health advocacy, counselling, and activation programme on depressive symptoms in older coronary heart disease patients. International Journal of Geriatric Psychiatry 2005;20:552‐8. [DOI] [PubMed] [Google Scholar]
Saxon 2006 {published data only}
- Saxon A, Malte C, Sloan K, Baer, J, Calsyn D, Nichol P, et al. Randomized trial of onsite versus referral primary medical care for veterans in addictions treatment. Medical Care 2006;44:334‐42. [DOI] [PubMed] [Google Scholar]
Schreuders 2007 {published data only}
- Schreuders B, Marwijk H, Smit J, Rijmen F, Stalman W, Oppen P. Primary care patients with mental health problems: Outcome of a randomised clinical trial. British Journal of General Practice 2007;57(544):886‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schulberg 1996 {published data only}
- Lave J, Frank R, Schulberg H, Kamlet M. Cost‐effectiveness of treatments for major depression in primary care practice. Archives of General Psychiatry 1998;55:645‐51. [DOI] [PubMed] [Google Scholar]
- Schulberg H, Pilkonis P, Houck P. The severity of major depression and choice of treatment in primary care practice. Journal of Consulting and Clinical Psychology 1998;66(6):932‐8. [DOI] [PubMed] [Google Scholar]
- Schulberg HC, Block MR, Madonia MJ, Scott CP, Rodriguez E, Imber SD, et al. Treating major depression in primary care practice. Eight‐month clinical outcomes. Archives of General Psychiatry 1996;53(10):913‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Scott 1992 {published data only}
- Scott AI, Freeman CP. Edinburgh primary care depression study: treatment outcome, patient satisfaction, and cost after 16 weeks. BMJ 1992;304(6831):883‐7. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Scott 1997 {published data only}
- Scott C, Tacchi MJ, Jones R, Scott J. Acute and one‐year outcome of a randomised controlled trial of brief cognitive therapy for major depressive disorder in primary care. British Journal of Psychiatry 1997;171:131‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sharp 2000 {published data only}
- Sharp DM, Power KG, Swanson V. Reducing therapist contact in cognitive behaviour therapy for panic disorder and agoraphobia in primary care: global measures of outcome in a randomised controlled trial. The British Journal of General Practice 2000;50:963‐8. [PMC free article] [PubMed] [Google Scholar]
Sharp 2004 {published data only}
- Sharp D, Power K, Swanson V. A comparison of the efficacy and acceptability of group versus individual cognitive behaviour therapy in the treatment of panic disorder and agoraphobia in primary care. Clinical Psychology and Psychotherapy 2004;11:73‐82. [Google Scholar]
Simon 2000 {published data only}
- Simon G, Korff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback and management of care by telephone to improve treatment of depression in primary care. BMJ 2000;320:550‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simon 2004 {published data only}
- Simon G, Ludman E, Tutty S, Operskalski B, Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA 2004;292(8):935‐42. [DOI] [PubMed] [Google Scholar]
Simons 2001 {published data only}
- Simons J, Reynolds J, Morison L. Randomised controlled trial of training health visitors to identify and help couples with relationship problems following a birth. British Journal of General Practice 2001;51:793‐9. [PMC free article] [PubMed] [Google Scholar]
Smit 2005 {published data only}
- Smit A, Tiemens B, Ormel J, Kluiter H, Jenner J, Meer K, et al. Enhanced treatment for depression in primary care: first year results on compliance, self‐efficacy, the use of antidepressants and contacts with the primary care physician. Primary Care and Community Psychiatry 2005;10:39‐49. [Google Scholar]
Smith 1986 {published data only}
- Smith GR Jr, Monson RA, Ray DC. Psychiatric consultation in somatization disorder. A randomized controlled study. New England Journal of Medicine 1986;314(22):1407‐13. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Smith 1995 {published data only}
- Smith GR Jr, Rost K, Kashner TM. A trial of the effect of a standardized psychiatric consultation on health outcomes and costs in somatizing patients. Archives of General Psychiatry 1995;52(3):238‐43. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sorby 1991 {published data only}
- Sorby NG, Reavley W, Huber JW. Self help programme for anxiety in general practice: controlled trial of an anxiety management booklet. British Journal of General Practice 1991;41(351):417‐20. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Stanley 2003 {published data only}
- Stanley M, Hopko D, Diefenbach G, Bourland S, Rodriguez H, Wagener P. Cognitive‐behaviour therapy for late life generalized anxiety disorder in primary care. American Journal of Geriatric Psychiatry 2003;11(1):92‐6. [PubMed] [Google Scholar]
Swindle 2003 {published data only}
- Swindle R, Rao J, Helmy A, Plue L, Zhou X, Eckert G, Weinberger M. Integrating clinical nurse specialists into the treatment of primary care patients with depression. International Journal of Psychiatry in Medicine 2003;33:17‐37. [DOI] [PubMed] [Google Scholar]
Trepka 1986 {published data only}
- Trepka C, Laing I, Smith S. Group treatment of general practice anxiety problems. Journal of the Royal College of General Practitioners 1986;36(284):114‐7. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Tudiver 1992 {published data only}
- Tudiver F, Hilditch J, Permaul J, McKendree D. Does mutual help facilitate newly bereaved widowers?. Evaluation and the Health Professions 1992;15:147‐62. [Google Scholar]
- Tudiver F, Permaul‐Woods J, Hildritch J, Harmina J, Saini S. Do widowers use the health care system differently? Does intervention make a difference?. Canadian Family Physician 1995;41:392‐9. [PMC free article] [PubMed] [Google Scholar]
Turner 2006 {published data only}
- Turner K, Sanders M. Help when It’s needed first: a controlled evaluation of brief, preventive behavioral family intervention in a primary care setting. Behavior Therapy 2006;37:131–42. [DOI] [PubMed] [Google Scholar]
Unutzer 2002 {published data only}
- Unutzer J, Katon W, Callahan C, Williams J, Hunkeler E, Harpole L, et al. for the IMPACT investigators. Collaborative care management of late‐life depression in the primary care setting: a randomized controlled trial. JAMA 2003;288(22):2836‐45. [DOI] [PubMed] [Google Scholar]
- Unutzer J, Katon W, Williams J, Callahan C, Harpole L, Hunkeler E, et al. Improving primary care for depression in late life: the design of a multicenter randomized trial. Medical Care 2001;39(8):785‐99. [DOI] [PubMed] [Google Scholar]
van Boeijen 2005 {published data only}
- Boeijen C, Oppen P, Balkom A, Visser S, Kempe P, Blankenstein N, Dyck R. Treatment of anxiety disorders in primary care practice: a randomised controlled trial. British Journal of General Practice 2005;55:763‐9. [PMC free article] [PubMed] [Google Scholar]
van Schaik 2006 {published data only}
- Schaik A, Marwijk H, Ader H, Dyck R, Haan M, Penninx B, et al. Interpersonal therapy for elderly patients in primary care. American Journal of Geriatric Psychiatry 2006;14(9):777‐86. [DOI] [PubMed] [Google Scholar]
Vines 2004 {published data only}
- Vines R, Richards J, Thomson D, Brechman‐Toussaint M, Kluin M, Vesely L. Clinical Psychology in general practice: a cohort study. Medical Journal of Australia 2004;181(2):74. [DOI] [PubMed] [Google Scholar]
Warner 1993 {published data only}
- Warner RW, Gater R, Jackson MG, Goldberg DP. Effects of a community mental health service on the practice and attitudes of general practitioners. British Journal of General Practice 1993;43(377):507‐11. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Wells 2000 {published data only}
- Schoenbaum M, Unutzer J, Sherbourne C, Duan N, Rubenstein L, Miranda J, et al. Cost‐effectiveness of practice‐initiated quality improvement for depression: results of a randomized controlled trial. JAMA 2001;286:1325‐30. [DOI] [PubMed] [Google Scholar]
- Sherbourne C, Wells K, Duan N, Miranda J, Unutzer J, Jaycox L, Schoenbaum M, Meredith L, Rubenstein L. Long‐term Effectiveness of Disseminating Quality Improvement for Depression in Primary Care. Archives of General Psychiatry 2001;58(7):696‐703. [DOI] [PubMed] [Google Scholar]
- Wells K. The design of Partners in Care: evaluating the cost‐effectiveness of improving care for depression in primary care. Social Psychiatry and Psychiatric Epidemiology 1999;34:20‐9. [DOI] [PubMed] [Google Scholar]
- Wells K, Sherbourne C, Schoenbaum M, Duan N, Meredith L, Unutzer J, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA 2000;283(2):212‐20. [DOI] [PubMed] [Google Scholar]
- Wells K, Sherbourne C, Schoenbaum M, Ettner S, Duan N, Miranda J, et al. Five year impact of quality improvement for depression: results of a group‐level randomized controlled trial. Archives of General Psychiatry 2004;61:378‐86. [DOI] [PubMed] [Google Scholar]
Whooley 2000 {published data only}
- Whooley M, Stone B, Soghikian K. Randomized trial of case‐finding for depression in elderly primary care patients. J Gen Intern Med 2000;15:293‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wickberg 1996 {published data only}
- Wickberg B, Hwang CP. Counselling of postnatal depression: a controlled study on a population based Swedish sample. Journal of Affective Disorders 1996;39(3):209‐16. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wilkinson 1993 {published data only}
- Wilkinson G. The role of the practice nurses in the management of depression. International Review of Psychiatry 1992;4:311‐5. [Google Scholar]
- Wilkinson G, Allen P, Marshall E, Walker J, Browne W, Mann AH. The role of the practice nurse in the management of depression in general practice: treatment adherence to antidepressant medication. Psychological Medicine 1993;23(1):229‐37. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Willemse 2006 {published data only}
- Smit F, Willemse G, Koopmanschap M, Onrust S, Cuijpers P, Beekman A. Cost effectiveness of preventing depression in primary care patients: a randomised trial. British Journal of Psychiatry 2006;188:330‐336. [DOI] [PubMed] [Google Scholar]
- Willemse G, Smit F, Cuijpers P, Tiemens B. Minimal contact psychotherapy for sub‐threshold depression in primary care: randomised trial. British Journal of Psychiatry 2004;185:416‐421. [DOI] [PubMed] [Google Scholar]
Williams 1989 {published data only}
- Williams P, Balestrieri M. Psychiatric clinics in general practice. Do they reduce admissions?. British Journal of Psychiatry 1989;154:67‐71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wood 1994 {published data only}
- Wood K, Anderson J. The effect on hospital admissions of psychiatric case management involving general practitioners: preliminary results. Australian and New Zealand Journal of Psychiatry 1994;29(2):223‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zayas 2004 {published data only}
- Zayas L, McKee M, Jankowski K. Adapting psychosocial intervention research to urban primary care environments: a case example. Annals of Family Medicine 2004;2:504‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Bero 2000
- Bero L, Grilli R, Grimshaw J, Mowatt G, Oxman AD, Zwarenstein M. The Cochrane Effective Practice and Organisation of Care Group (EPOC) Module. Cochrane Database of Systematic Reviews 2000, Issue 2. [DOI: ] [Google Scholar]
Bower 2002
- Bower P, Gask L. The changing nature of consultation‐liaison in primary care: bridging the gap between research and practice. General Hospital Psychiatry 2002;24:63‐70. [DOI] [PubMed] [Google Scholar]
Bower 2003
- Bower P, Byford S, Barber J, Beecham J, Simpson S, Friedli K, et al. Meta‐analysis of data on costs from trials of counselling in primary care: using individual patient data to overcome sample size limitations in economic analyses. BMJ 2003;326(7401):1247‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bower 2005
- Bower P, Gilbody S. Managing common mental health disorders in primary care: conceptual models and evidence base. British Medical Journal 2005;330:839‐842. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bower 2006
- Bower P, Rowland N. Effectiveness and cost effectiveness of counselling in primary care. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD001025.pub2] [DOI] [PubMed] [Google Scholar]
Brown 1995
- Brown C, Schulberg H. The efficacy of psychosocial treatments in primary care: a review of randomised clinical trials. General Hospital Psychiatry 1995;17:414‐24. [DOI] [PubMed] [Google Scholar]
Churchill 1999
- Churchill R, Dewey M, Gretton V, Duggan C, Chilvers C, Lee A. Should general practitioners refer patients with major depression to counsellors? A review of current published evidence. British Journal of General Practice 1999;49:737‐43. [PMC free article] [PubMed] [Google Scholar]
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. 2nd Edition. New Jersey: Lawrence Erlbaum, 1988. [Google Scholar]
Fiedler 1989
- Fiedler J, Wight J. The medical offset effect and public health policy: Mental health industry in transition. New York: Praeger, 1989. [Google Scholar]
Fletcher 2007
- Fletcher J, Bower P, Gilbody S, Lovell K, Richards D, Gask L. Collaborative care for depression and anxiety problems in primary care. (Protocol). Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD006525] [DOI] [PubMed] [Google Scholar]
Friedli 1996
- Friedli K, King M. Counselling in primary care: a review. Primary Care Psychiatry 1996;2:205‐16. [Google Scholar]
Gask 1997
- Gask L, Sibbald B, Creed F. The changing nature of consultation‐liaison in primary care: bridging the gap between research and practice. British Journal of Psychiatry 1997;170:6‐11. [Google Scholar]
Gilbody 2003
- Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organisational interventions to improve the management of depression in primary care: a systematic review. JAMA 2003;289:3145‐51. [DOI] [PubMed] [Google Scholar]
Goldberg 1992
- Goldberg D, Huxley P. Common mental disorders: A biosocial model. London: Routledge, 1992. [Google Scholar]
Lipsey 1990
- Lipsey M. Design Sensitivity: Statistical Power for Experimental Research. Newbury Park: Sage, 1990. [Google Scholar]
Marks 1979
- Marks JN, Goldberg DP, Hillier VF. Determinants of the ability of general practitioners to detect psychiatric illness. Psychological Medicine 1979;9:337‐53. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mumford 1984
- Mumford E, Schlesinger H, Glass G. A new look at evidence about reduced cost of medical utilization following mental health treatment. American Journal of Psychiatry 1984;141:1145–58. [DOI] [PubMed] [Google Scholar]
Parker 2008
- Parker AG, Hetrick SE, Purcell R, Gillies D. Consultation liaison in primary practice for mental health problems. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD007193] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pincus 1987
- Pincus HA. Patient‐oriented models for linking primary care and mental health care. General Hospital Psychiatry 1987;9(2):95‐101. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schulberg 2002
- Schulberg H, Raue P, Rollman B. The effectiveness of psychotherapy in treating depressive disorders in primary care practice: clinical and cost perspectives. General Hospital Psychiatry 2002;24:203‐12. [DOI] [PubMed] [Google Scholar]
Sibbald 1993
- Sibbald B, Addington‐Hall J, Brenneman D, Freeling P. Counsellors in English and Welsh general practices: their nature and distribution. BMJ 1993;306(6869):29‐33. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wessely 1996
- Wessely S. The rise of counselling and the return of alienism. BMJ 1996;313(7050):158‐60. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2001
- WHO. The World Health Report 2001 Mental Health: New understanding, new hope. World Health Organisation, 2001. [Google Scholar]
References to other published versions of this review
Bower 2000
- Bower P, Sibbald B. Systematic review of the effect of on‐site mental health professionals on the clinical behaviour of general practitioners. BMJ 2000;320:614‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]


