Abstract
Cavernous hemangioma is an encapsulated nodular mass composed of dilated, cavernous vascular space separated by connective tissue stroma. Flattened endothelial cells line the vascular spaces, which were filled with blood. Though hemangiomas are the mast common benign neoplasms seen in children, they rarely occur in adults. In the head and neck region, the masseter and trapezius muscles are most commonly involved. Herein, the case is a 64 years old male who presented with a round, painless mass in the right temporal fossa with extension to infratemporal fossa. The lesion was surgically excised and histopathology confirmed the diagnosis of cavernous hemangioma.
Key Words: Cavernous hemangioma, Temporalis muscle, Iran
INTRODUCTION
Hemangiomas are benign tumors with vascular origin and three types of hemangioma have been described according to the vessel type involved: cavernous, capillary and mixed.1,2 Intramuscular hemangiomas make up less than 1% of all hemangiomas and are mostly located in the extremities and the trunk.3,4 Hemangiomas of the head and neck make up less than 15% of intramuscular hemangiomas.3,5 We present a patient with cavernous hemangioma located in the temporalis muscle with extension to infratemporal fossa.
CASE REPORT
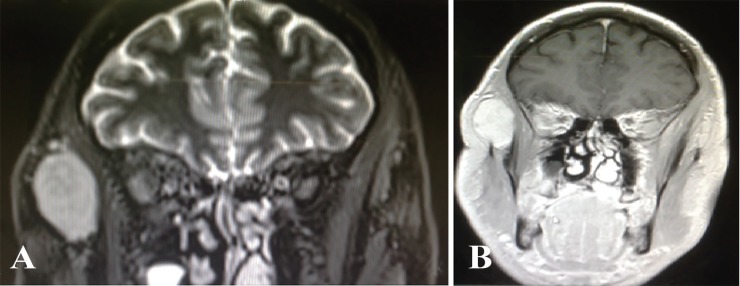
A 64-year old man with painless, soft right temporal swelling and right infraorbital edema that had been noticed by himself several months ago has been presented. Physical examination showed 4×5 cm round and painless mass situated lateral to orbital wall. His problem was associated with right infraorbital edema. Fine needle aspiration was not diagnostic (Figure 1). MRI showed a large soft tissue mass within the right temporalis muscle with extension to right infratemporal fossa. The tumor had isointense signal on T1 weighted sequences and a high signal on T2 weighted sequences (Figure 2).
Fig. 1.

Initial photography of the patient showed swelling of right temporal area and infraorbital region
Fig. 2.
MRI shows a large soft tissue mass within the right temporalis muscle with extension to right infratemporal fossa. (A): The tumor has isointense signal on T1 weighted sequences. (B): The tumor has a high signal on T2 weighted sequences
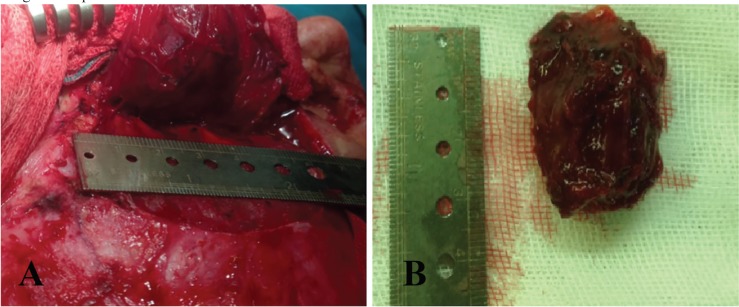
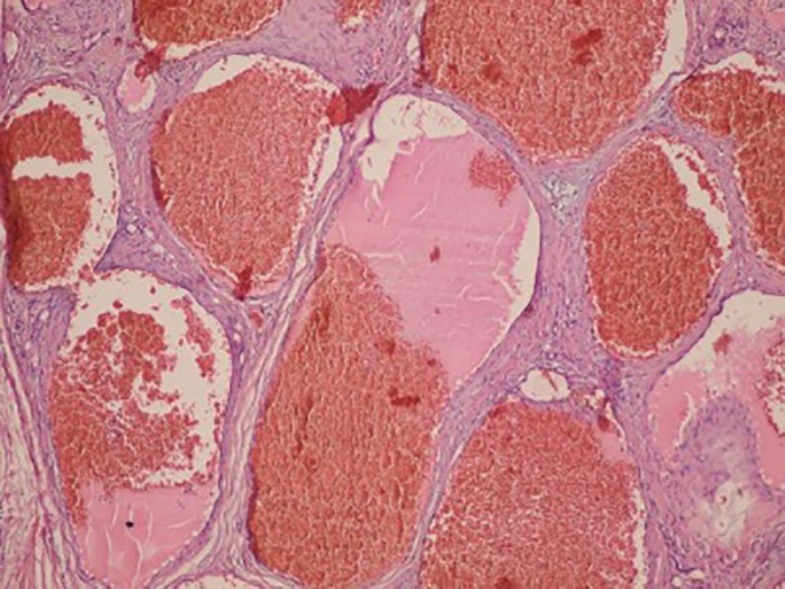
Surgical excision was performed through coronal incision. The mass was found within the temporal muscle and was excised with loupe magnification to protect right frontal branch of facial nerve. Blood loss during operation was trace. Postoperative recovery was uneventful and functional and cosmetic results were excellent (Figure 3). Gross examination of mass showed a rubbery round tissue with measurement of 3.5×2.8×2 cm, and cut sections showed dark red brown surface with microcytic appearance. Histological study showed an ill-defined mass consisted of dilated channel-like blood vessels, containing lymph and blood, which were entrapped between muscles. There was no evidence of atypia, necrosis and mitosis. The diagnosis of intramuscular cavernous hemangioma was signed out for him. Postoperative follow up during 1-year period showed no recurrence (Figure 4).
Fig. 3.
(A): Intra-operative view of the hemangioma approached through coronal incision. (B): Surgical specimen. Mass was well circumscribed and excised with a margin of normal mu
Fig. 4.
Section shows dilated blood vessels arranged back to back and containing blood and lymph (Hematoxylin and Eosin, ×100).
DISCUSSION
Hemangiomas are benign vascular proliferations and one of the commonest benign soft tissue tumors consisting 7% of all soft tissue tumors. They are usually present in infants and children, while females are more affected than males. The etiology is unclear. Intramuscular hemangiomas are rare tumors accounting for 0.8% of all hemangiomas and approximately 14% of cases are localized in the musculature of the head and neck.6 The masseter (36%), followed by the trapezious (24%) are the muscles most frequently affected, whereas temporalis muscle hemangioma are extremely rare.7
In 1972, Allen and Enzinger classified intramuscular hemangioma according to the vessel size as (i) capillary type (small vessel), (ii) large vessel or cavernous type, and (iii) mixed type (consisting of both).1 The most common presentation is a smooth, non-tender and mobile mass. The lesion usually does not show any of the vascular signs such as thrill or skin discoloration like superficial hemangioma.8 Plain x-ray films, CT scan, angiography may not be specific for this tumor. CT scan is helpful for evaluation of bone involvement. MRI is the method of choice. On MRI, the tumor is isointense on T1 and hyperintense on T2 weighted sequences.9
Treatment options are variable depending on the size, vascularization and location.10 Preoperative embolization can help to reduce intra-operative bleeding.11 Sclerosing agents, corticosteroids and radiotherapy are another modalities for treatment.12 But, in this case; embolization was not performed due to relatively slow and small amount of blood pooling. Surgical excision is the treatment of choice. Coronal incision is the best way to approach this tumor and the tumor should be excised with loupe magnification to protect frontal branch of facial nerve and securely ligate feeding vessels. Long term clinical and radiological follow up are necessary to detect any relapse.13
Hemangiomas are benign vascular tumors and are rarely seen in the temporalis muscle. This case showed a cavernous intramuscular hemangioma involving temporalis muscle in old adult. Surgery is the treatment of choice to exclude malignancy and for adequate treatment of these lesions. Coronal incision is the best way to approach this tumor and the tumor should be excised with loupe magnification to protect frontal branch of facial nerve and securely ligate feeding vessels. Long term clinical and radiological follow up are necessary to detect any relapse.
ACKNOWLEDGEMENT
The authors wish to thank Mr. H. Argasi at the Research Consultation Center (RCC) of Shiraz University of Medical Sciences for his invaluable assistance in editing this manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
References
- 1.Allen PW, Enzinger FM. Hemangioma of skeletal muscle An analysis of 89 cases. Cancer. 1972;29:8–22. doi: 10.1002/1097-0142(197201)29:1<8::aid-cncr2820290103>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 2.Mehrabani D, Tabei S, Heydari S, Shamsina S, Shokrpour N, Amini M, Masoumi S, Julaee H, Farahmand M, Manafi A. Cancer occurrence in Fars province, southern Iran. Iran Red Crescent Med J. 2008;10:314–22. [Google Scholar]
- 3.Batsakis JG. Vasoformative tumors. In: Batsakis JG, editor. Tumors of the head and neck: clinical and pathological considerations. 2nd ed. Baltimore: Williams & Wilkins; 1979. pp. 294–6. [Google Scholar]
- 4.Beecham JE, Behrens HW. Intramuscular hemangioma of the head and neck: report of a case involving the prevertebral muscles. Head Neck Surg. 1988;10:402–5. doi: 10.1002/hed.2890100607. [DOI] [PubMed] [Google Scholar]
- 5.Clemis JD, Briggs DR, Changus GW. Intramuscular hemangioma in the head and neck. Can J Otolaryngol. 1975;4:339–46. [PubMed] [Google Scholar]
- 6.Lopez-Cedrun JL, Urtasun Fernandez J, Melendez Baltanas J, Lopez Garcia JA. Hemangioma of the temporalis muscle: a case report and review of the literature. J Oral Maxillofac Surg. 1996;54:1130–2. doi: 10.1016/s0278-2391(96)90177-9. [DOI] [PubMed] [Google Scholar]
- 7.Odabasi AO, Metin KK, Mutlu C, Basak S, Erpek G. Intramuscular hemangioma of the masseter muscle. Eur Arch Otorhinolaryngol. 1999;256:366–9. doi: 10.1007/s004050050165. [DOI] [PubMed] [Google Scholar]
- 8.Sharma BS, Chari PS, Joshi K, Rajvanshi A. Hemangioma of the temporalis muscle. Ann Otol Rhinol Laryngol. 1991;100:76–8. doi: 10.1177/000348949110000113. [DOI] [PubMed] [Google Scholar]
- 9.Uraloglu M, Uysal AC, Sensoz O, Ortak T, Unlu RE. Intramuscular hemangioma of the temporalis muscle. J Craniofac Surg. 2006;17:745–7. doi: 10.1097/00001665-200607000-00027. [DOI] [PubMed] [Google Scholar]
- 10.Heckl S, Aschoff A, Kunze S. Cavernous hemangioma of the temporal muscle. Neurosurg Rev. 2002;25:63–5; discussion 6-7. doi: 10.1007/s101430100181. [DOI] [PubMed] [Google Scholar]
- 11.Bennett JE, Zook EG. Treatment of arteriovenous fistulas in cavernous hemangiomas of face by muscle embolization. Case report. Plast Reconstr Surg. 1972;50:84–7. doi: 10.1097/00006534-197207000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Giudice M, Piazza C, Bolzoni A, Peretti G. Head and neck intramuscular haemangioma: report of two cases with unusual localization. Eur Arch Otorhinolaryngol. 2003;260:498–501. doi: 10.1007/s00405-003-0626-7. [DOI] [PubMed] [Google Scholar]
- 13.Sherman JA, Davies HT. Intramuscular hemangioma of the temporalis muscle. J Oral Maxillofac Surg. 2001;59:207–9. doi: 10.1053/joms.2001.20496. [DOI] [PubMed] [Google Scholar]