Abstract
BACKGROUND
Immediate Breast Reconstruction (IBR) is an additional surgical procedure that may increase postoperative complications (such as flap necrosis, infection, and hematoma) and delay the initial time for adjuvant chemotherapy in some patients. In this systematic and meta-analysis, we provide overall survival rates of patients who underwent mastectomy with and without IBR.
METHODS
The following databases were systematically searched between 2015 to 2019 without language restrictions in PUBMED, EMBASE, Web of Science, and Cochrane Library. In addition, the relevant references in the list of all included articles were also checked. The search term included “breast cancer” and “breast reconstruction” “mastectomy”.
RESULTS
The sample size was a range from 339 to 5644 patients. The median age was 46.3 years. The results showed no significant differences in terms of overall survival between two groups.
CONCLUSION
The results showed that IBR after mastectomy did not affect the overall survival.
Key Words: Breast, Reconstruction, Mastectomy, Cancer
INTRODUCTION
Breast cancer is the leading cause of cancer and death in women worldwide.1 Its surgical approach has become less and less mutilating in the last decades. However, the overall number of breast reconstructions has significantly increased lately.2 Nowadays, breast reconstruction should be individualized at its best, first of all taking into consideration not only the oncological aspects of the tumor, neo-/adjuvant treatment, and genetic predisposition, but also its timing (immediate versus delayed breast reconstruction), as well as the patient’s condition and wish.3 Breast cancer is the leading cause of cancer death among women worldwide with ~1.7 million new diagnoses and 521.900 deaths in 2012.4,5
One important modality of breast cancer therapy is surgical treatment, which has become increasingly less mutilating over the last century.6,7 Mastectomy aims at resecting as much breast tissue as possible, knowing that glandular tissue will almost always remain in the region of the inframammary fold.8 Breast reconstruction after mastectomy is oncologic ally safe and is associated with high satisfaction and improved psychosocial outcomes.9 Although the rates of major complications after immediate reconstruction are greater than after mastectomy alone, clinically significant delays in the receipt of adjuvant therapy after immediate reconstruction have not been found.10
Breast reconstruction (BR) is an option for women who are treated with mastectomy; however, there has been concern regarding the oncologic safety of BR.11 Breast reconstruction is dependent primarily on the type of mastectomy and may be classified in various ways, such as reconstruction type and reconstruction time point. Breast reconstruction is a surgical procedure that restores shape to breast after mastectomy surgery that removes breast to treat or prevent breast cancer.12
Breast reconstruction surgery aims to restore the appearance of a natural breast after a mastectomy and can help a woman look and feel better. Many women find that breast reconstruction significantly improves their self-image, self-confidence and quality of life. On the practical side, breast reconstruction eliminates the need for external artificial prostheses, which can sometimes be uncomfortable to wear.13 The latter includes delayed breast reconstruction (DBR; secondary breast reconstruction) and immediate breast reconstruction during the same surgery (IBR; primary breast reconstruction).2
IBR is advantageous over DBR, because it decreased the total number of surgical procedures and the risks therein. Breast reconstruction surgery is the creation of a new breast shape, or mound, using surgery. IBR is an additional surgical procedure, it may increase postoperative complications (such as flap necrosis, infection, and hematoma) and delay the initial time to adjuvant chemotherapy in some patients.14 It may be done after removal of a whole breast (mastectomy) or part of the breast (breast-conserving surgery).15 Nonetheless, IBR is advantageously associated with a reduced recovery time, a better esthetic outcome, an improved quality of life, lower surgery, and recovery related costs.12,16,17 In this systematic and meta-analysis, we provided overall survival between patients who underwent IBR after mastectomy.
MATERIALS AND METHODS
Search Strategy
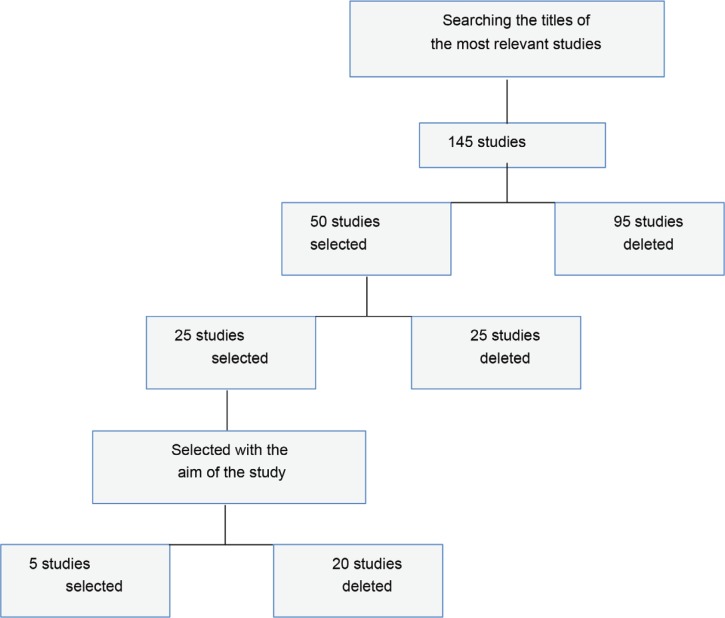
The following databases were systematically searched between years 2015 to 2019 without any language restrictions in PUBMED, EMBASE, Web of Science, and Cochrane Library. In addition, the relevant references in the list of all included articles were also checked. The search term included “breast cancer”, “breast reconstruction” and “mastectomy”. In the preliminary study, 145 studies were selected which were selected by studying the titles of the most relevant studies (n=50). Fifty studies were conducted, and studies were conducted with the aim of the study (n=25). Then, the full text of 25 studies was studied. Finally, five studies that were included in the study were selected and evaluated (Figure 1).
Fig. 1.
Flow chart of study selection process
Study Inclusion and Exclusion Criteria
Inclusion criteria were involving retrospective or prospective studies, patients with a diagnosis of breast cancer, and breast reconstruction after mastectomy. Exclusion criteria were involving reviews without original data, meta-analysis, case reports, and studies lacking control group.
Data Extraction
We recorded the following information for each study according to a prespecified protocol: author, year, study demographics, number and characteristics of participants, duration of follow-up, end-point data.
Statistical Analysis
We analyzed the data by the stata 14 software that was expressed risk ratio (RR) with 95% confidence interval (CI).
Results
The sample size was a range from 339 to 5644 patients. The median age was 46.3 years. Table 1 shows the data recorded and documented. A total of five studies reported data on the overall survival of advanced breast cancer patients and two studies reported data on the disease-free survival. There was no statistically significant heterogeneity between studies (Tables 2 and 3). The comprehensive therapy for breast cancer significantly changed over the last decade, and would clearly have an impact on survival and disease recurrence. The increased screening and means for detection of early disease and identification of patients with BRCA genes and genetic predispositions have also changed which would also impact survival and recurrence. Therefore, studies published after 2015 were assessed, and the results did not show any significant differences in terms of overall survival between two groups. Figure 2 showed Forest plot of overall survival.
Table 1.
The findings and results of the studies that entered the study
| Result of study | Apparent survival benefit | Irrespective of the adjuvant treatment | Complication risks after immediate BR | Mastectomy and BR for cancer | Implant-based reconstruction compared to mastectomy | |
|---|---|---|---|---|---|---|
| Outcomes | Overall survival | Overall survival | Overall survival | Overall survival | Disease-free survival, overall survival | |
| Follow up median | Mastectomy alone | 23.4 | 8.6 | Not available | Not available | Not available |
| IBR | 23.4 | 8.6 | Not available | Not available | Not available | |
| Lymph-node | Mastectomy alone | 324/267/167 | 41/16/48 | Not available | Not available | 11, 5, 27 |
| IBR | 384/236/138 | 137/102/100 | Not available | 21/37/22 | 5, 10,4 | |
| stage (I/II/III/I V) | Mastectomy alone | Not available | Not available | Not available | Not available | 38, 19,28 |
| IBR | Not available | Not available | Not available | Not available | 41,31,15 | |
| Age median | Mastectomy alone | 45 | Not available | Not available | Not available | 58 |
| IBR | 45 | Not available | Not available | 46 | 48 | |
| Patients (n) | Mastectomy alone | 758 | 105 | 9250 | 210 | |
| IBR | 758 | 339 | 5644 | 400 | 681 | |
| Study design | RCS | CC | RCS | CC | PCR | |
| Author | Platt et al., 2015 | Aurilio et al., 2015 | Jagsi et al., 2016 | Howes et al., 2019 | Miller et al., 2016 | |
Table 2.
Overall survival in to groups (without reconstruction and breast reconstruction)
| Author | Overall survival (without reconstruction) |
Overall survival
(breast reconstruction) |
|---|---|---|
| Platt et al., 2015 | 57.5 | 47.5 |
| Aurilio et al., 2015 | 69.5 | 79.5 |
| Jagsi et al., 2016 | 52.3 | 74.6 |
| Howes et al., 2019 | 42 | 57.9 |
| Miller et al., 2016 | 24 | 76 |
Table 3.
Heterogeneity Chi-Square
| Author | ES | 95% Confidence Interval | Weight (%) | |
|---|---|---|---|---|
| Upper | Lower | |||
| Platt et al., 2015 | 57.5 | -35.59 | 150.59 | 35.38 |
| Aurilio et al., 2015 | 69.5 | -86.31 | 225.31 | 12.63 |
| Jagsi et al., 2016 | 52.3 | -93.91 | 198.51 | 14.35 |
| Howes et al., 2019 | 42.0 | 071.48 | 155.48 | 23.81 |
| Miller et al., 2016 | 24 | -124.95 | 172.95 | 13.83 |
I-squared (variation in ES attributable to heterogeneity)=0.0% Test of ES=0, z=1.77, P=0.077
Fig. 2.
Forest plot of overall survival
DISCUSSION
The present meta-analysis indicated that patients treated with breast reconstruction after mastectomy in women with breast cancer were comparable in terms of overall survival. Breast reconstruction is an option for women who are treated with mastectomy; however, there has been concern regarding the oncologic safety of BR. Two studies design were retrospective cohort study.12,10 Two studies design were case control study,13,14 and one study was prospective cohort study.15
Patients who received immediate breast reconstruction or mastectomy alone followed by PMRT, except in patients who were younger than 50 years of age. These younger patients appeared to have a survival advantage after immediate breast reconstruction. The survival outcomes are in relation to immediate breast reconstruction followed by PMRT for both the physicians and the patients.18 There are comparable survival outcomes compared to mastectomy alone, immediate post mastectomy reconstruction had limited advantage in survival after adjusting for confounding factor of family income. LABC patients who received immediate breast reconstruction or mastectomy alone followed by PMRT, except in patients who were younger than 50 years of age. These younger patients appeared to have a survival advantage after immediate breast reconstruction.19,20
Compared to mastectomy alone, immediate post mastectomy reconstruction had limited advantage in survival after adjusting for confounding factor of family income, if validated in other large databases, may help to illustrate the actual effect of immediate post mastectomy reconstruction on patient survival,21,22 It was shown that patients for whom implant-based reconstruction is available, immediate implant reconstruction does not increase the risk of lymphedema compared to mastectomy alone.15 It was demonstrated that women who undergo total mastectomy and breast reconstruction for cancer achieve a quality-of-life outcome that is at least as good as that following breast-conserving surgery.14
Furthermore, breast conservation has been found to be associated with lower physical well-being (i.e., more pain and discomfort) in the chest area and poorer sexual well-being outcomes.23,24 Overall survival, disease- free survival, and surgical site infection in patients who underwent IBR after mastectomy versus mastectomy alone, and the results demonstrated that there were no significant differences between IBR after mastectomy and mastectomy alone in overall survival, disease-free survival and local recurrence.25
The results revealed that patients who underwent IBR after mastectomy were associated with a significantly higher risk of surgical site infection. IBR patients exhibited a better survival trend that was maintained along a prolonged follow-up time, as exemplified by the survival curves.26 Also, no IBR group was characterized by unfavorable prognostic factors, including a higher number of metastatic lymph nodes. Taken together, the clinical data in the neoadjuvant and adjuvant setting favor the attitude to perform an IBR intervention, and not confirm preclinical evidence that points toward an augmented risk of relapse linked to breast reconstruction. IBR after mastectomy does not affect the overall survival and disease-free survival of breast cancer, which is in line with our findings.13
In either meta-analysis demonstrated no evidence for increased frequency of local breast cancer recurrence with IBR compared with mastectomy.27 At other systematic review study, rates of breast reconstruction were highly variable. Reconstruction appeared to be offered to a minority of women; around half took up the offer. The main reasons reported for no reconstruction included patient-related and adjuvant therapy-related factors. Clinicians’ beliefs about reconstruction may be an important factor. Rates of reconstruction could be increased with early discussion of the options when mastectomy is chosen or required.28-30
At a systematic review study of the literature, it was shown that IBR did not necessarily delay the start of adjuvant chemotherapy to a clinically relevant extent, suggesting that in general IBR was a valid option for non- metastatic breast cancer patients.25 We can conclude that IBR after mastectomy does not affect the overall survival and the incidence of surgical site infection in the IBR after mastectomy is higher than that in the mastectomy alone. The limitations of this study were failure to check disease-free survival, and incidence of local recurrence. It is recommended that these cases to be considered in future studies.
ACKNOWLEDGEMENT
Study Sponsors were none.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
References
- 1.Mehrabani D, Tabei S, Heydari S, Shamsina S, Shokrpour N, Amini M, Masoumi S, Julaee H, Farahmand M, Manafi A. Cancer occurrence in Fars province, southern Iran. Iran Red Crescent Med J. 2008;10:314–22. [Google Scholar]
- 2.Shaterian A, Gandy J, Lalezari S, Smith S, Paydar K. Patient Race and Provider Predict Patient Satisfaction Following Post-Mastectomy Breast Reconstruction. World J Plast Surg. 2016;5:114–23. [PMC free article] [PubMed] [Google Scholar]
- 3.Parra L. Stacked PAP Flaps for Two-Stage Immediate Bilateral Breast Reconstruction: A Case Report. World J Plast Surg. 2017;6:243–5. [PMC free article] [PubMed] [Google Scholar]
- 4.Ilonzo N, Tsang A, Tsantes S, Estabrook A, Thu Ma AM. Breast reconstruction after mastectomy: A ten-year analysis of trends and immediate postoperative outcomes. Breast. 2017;32:7–12. doi: 10.1016/j.breast.2016.11.023. [DOI] [PubMed] [Google Scholar]
- 5.Mehrabani D, Almasi A, Farahmand M, Ahrari Z, Rezaianzadeh A, Mehrabani G, Talei AR. Incidence of breast cancer in fars province, southern iran: a hospital-based study. World J Plast Surg. 2012;1:16–21. [PMC free article] [PubMed] [Google Scholar]
- 6.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 7.Mehrabani D, Manafi A. Breast implants and breast cancer. World J Plast Surg. 2012;1:62–3. [PMC free article] [PubMed] [Google Scholar]
- 8.Mukherji A. Basics of Planning and Management of Patients during Radiation Therapy. Springer. 2018 oi: 10.1007/978-981-10-6659-7. [Google Scholar]
- 9.Barton FE Jr, English JM, Kingsley WB, Fietz M. Glandular excision in total glandular mastectomy and modified radical mastectomy: a comparison. Plast Reconstr Surg. 1991;88:389–92; discussion 93-4. doi: 10.1097/00006534-199109000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Yang X, Zhu C, Gu Y. The prognosis of breast cancer patients after mastectomy and immediate breast reconstruction: a meta-analysis. PLoS One. 2015;10:e0125655. doi: 10.1371/journal.pone.0125655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cordeiro PG. Breast reconstruction after surgery for breast cancer. N Engl J Med. 2008;359:1590–601. doi: 10.1056/NEJMct0802899. [DOI] [PubMed] [Google Scholar]
- 12.Platt J, Baxter NN, McLaughlin J, Semple JL. Does breast reconstruction after mastectomy for breast cancer affect overall survival? Long-term follow-up of a retrospective population-based cohort. Plast Reconstr Surg. 2015;135:468e–76e. doi: 10.1097/PRS.0000000000001054. [DOI] [PubMed] [Google Scholar]
- 13.Aurilio G, Bagnardi V, Nole F, Pruneri G, Graffeo R, Petit JY, Cullura D, Martella S, Locatelli M, Iera M, Rey P, Curigliano G, Rotmensz N, Munzone E, Goldhirsch A. Outcome of Immediate Breast Reconstruction in Patients With Nonendocrine-Responsive Breast Cancer: A Monoinstitutional Case-Control Study. Clin Breast Cancer. 2015;15:e237–41. doi: 10.1016/j.clbc.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Jagsi R, Jiang J, Momoh AO, Alderman A, Giordano SH, Buchholz TA, Pierce LJ, Kronowitz SJ, Smith BD. Complications After Mastectomy and Immediate Breast Reconstruction for Breast Cancer: A Claims-Based Analysis. Ann Surg. 2016;263:219–27. doi: 10.1097/SLA.0000000000001177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howes BH, Watson DI, Xu C, Fosh B, Canepa M, Dean NR. Quality of life following total mastectomy with and without reconstruction versus breast-conserving surgery for breast cancer: A case-controlled cohort study. J Plast Reconstr Aesthet Surg. 2016;69:1184–91. doi: 10.1016/j.bjps.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Miller CL, Colwell AS, Horick N, Skolny MN, Jammallo LS, O’Toole JA, Shenouda MN, Sadek BT, Swaroop MN, Ferguson CM, Smith BL, Specht MC, Taghian AG. Immediate Implant Reconstruction Is Associated With a Reduced Risk of Lymphedema Compared to Mastectomy Alone: A Prospective Cohort Study. Ann Surg. 2016;263:399–405. doi: 10.1097/SLA.0000000000001128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu SG, Zhang WW, Sun JY, Lin Q, He ZY. Comparison of survival outcomes of locally advanced breast cancer patients receiving post-mastectomy radiotherapy with and without immediate breast reconstruction: a population-based analysis. Cancer Manag Res. 2018;10:1993–2002. doi: 10.2147/CMAR.S162430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang YZ, Liu YR, Yu KD, Zuo WJ, Shao ZM. Immediate postmastectomy breast reconstruction showed limited advantage in patient survival after stratifying by family income. PLoS One. 2013;8:e82807. doi: 10.1371/journal.pone.0082807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu SG, Zhang WW, Sun JY, Lin Q, He ZY. Comparison of survival outcomes of locally advanced breast cancer patients receiving post-mastectomy radiotherapy with and without immediate breast reconstruction: a population-based analysis. Cancer Manag Res. 2018;10:1993–2002. doi: 10.2147/CMAR.S162430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Howard-McNatt MM. Patients opting for breast reconstruction following mastectomy: an analysis of uptake rates and benefit. Breast Cancer (Dove Med Press) 2013;5:9–15. doi: 10.2147/BCTT.S29142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O’Halloran N, Lowery A, Kalinina O, Sweeney K, Malone C, McLoughlin R, Kelly J, Hussey A, Kerin M. Trends in breast reconstruction practices in a specialized breast tertiary referral centre. BJS Open. 2017;1:148–57. doi: 10.1002/bjs5.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bezuhly M, Wang Y, Williams JG, Sigurdson LJ. Timing of Postmastectomy Reconstruction Does Not Impair Breast Cancer-Specific Survival: A Population-Based Study. Clin Breast Cancer. 2015;15:519–26. doi: 10.1016/j.clbc.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 23.J LS, Metcalfe K, Shoukat F, Sun P, Narod S. Survival Differences in Women with and without Autologous Breast Reconstruction after Mastectomy for Breast Cancer. Plast Reconstr Surg Glob Open. 2017;5:e1281. doi: 10.1097/GOX.0000000000001281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mundy LR, Homa K, Klassen AF, Pusic AL, Kerrigan CL. Breast Cancer and Reconstruction: Normative Data for Interpreting the BREAST-Q. Plast Reconstr Surg. 2017;139:1046e–55e. doi: 10.1097/PRS.0000000000003241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Howes BH, Watson DI, Xu C, Fosh B, Canepa M, Dean NR. Quality of life following total mastectomy with and without reconstruction versus breast-conserving surgery for breast cancer: A case-controlled cohort study. J Plast Reconstr Aesthet Surg. 2016;69:1184–91. doi: 10.1016/j.bjps.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Xavier Harmeling J, Kouwenberg CA, Bijlard E, Burger KN, Jager A, Mureau MA. The effect of immediate breast reconstruction on the timing of adjuvant chemotherapy: a systematic review. Breast Cancer Res Treat. 2015;153:241–51. doi: 10.1007/s10549-015-3539-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van der Geest LGM, van Eijck CHJ, Groot Koerkamp B, Lemmens V, Busch OR, Vissers PAJ, Wilmink JW, Besselink MG, Dutch Pancreatic Cancer G. Trends in treatment and survival of patients with nonresected, nonmetastatic pancreatic cancer: A population-based study. Cancer Med. 2018;7:4943–51. doi: 10.1002/cam4.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McManus MT, Sharp PA. Gene silencing in mammals by small interfering RNAs. Nat Rev Genet. 2002;3:737–47. doi: 10.1038/nrg908. [DOI] [PubMed] [Google Scholar]
- 29.Wilkins EG, Hamill JB, Kim HM, Kim JY, Greco RJ, Qi J, Pusic AL. Complications in Postmastectomy Breast Reconstruction: One-year Outcomes of the Mastectomy Reconstruction Outcomes Consortium (MROC) Study. Ann Surg. 2018;267:164–70. doi: 10.1097/SLA.0000000000002033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Somogyi RB, Ziolkowski N, Osman F, Ginty A, Brown M. Breast reconstruction: Updated overview for primary care physicians. Can Fam Physician. 2018;64:424–32. [PMC free article] [PubMed] [Google Scholar]