Abstract
This pilot study investigated factors influencing the application of connected health (CH) in Taiwanese remote areas. These factors cover issues of cost, infrastructure, technology, business sustainability, business model, collaboration, and communication. It aimed to explore the significance and to assess the feasibility of researching CH in Taiwan. A qualitative exploratory study was conducted by interviewing relevant stakeholders (n = 18). The majority were healthcare providers as most of them are the CH end users. Their feedback was essential in reflecting the effectiveness of CH products and services. Therefore, understanding their views is significant in the design of a successful and user-friendly interactive system. A theoretical framework on the introduction of innovations in healthcare was employed to guide data collection and thematic analysis. Additionally, stakeholders proposed strategies for enhancing the implementation of CH in remote areas. This pilot study also contributed to identifying future directions and information for conducting the multi-stage interviews for collecting the data more effectively. Although the results reveal that the study of CH is meaningful, there is an issue of business sustainability which is obscured by some barriers that need to be addressed. These barriers will be further investigated in the first-stage interview and second-stage interview in future research. The research findings also suggest that strategies and sustainability for CH implementation should be included from the planning phase to benefit all the stakeholders in the CH ecosystem.
Keywords: connected healthcare, remote areas, business sustainability, population ageing
1. Introduction
1.1. The Needs of an Ageing Society and Remote Residents
There is a controversy over the concern of rural health disparities in the practice of a democratic society. Some believe that health disparities should not exist in a democratic society due to equality consideration, while others think the power of influence will determine the focus of health facilities dispense. Undoubtedly, more rural areas do present adverse health conditions than suburban areas [1]. To tackle rural health disparities and ageing society challenges, connected health (CH) is proposed as a promising solution worldwide. Where CH is practiced, it usually fulfills the pre-conditions of advanced information technology (IT), integrated healthcare, significant geographic isolation and population of ageing or with chronic conditions.
Taiwanese CH, as a case study, is significant and valuable as it demonstrates typical features which may impact and interest the whole of society. Taiwan has become one of the fastest ageing populations in the world due to advancements in medical technology, changes in family structure, and the low birth rate [2]. Over the past century, there has been a dramatic increase in life expectancy accompanied by a growth in chronic conditions (such as hypertension, diabetes, coronary diseases, and obesity) [3]. Geographically, Taiwan’s remote areas cover mountain areas, isolated islands, and remote townships [4]. In these areas, medical and care services are allowed to be practiced remotely according to the law and regulation of the state. There are 48 remote townships that account for 44% of the area in Taiwan, while their residents are only 0.36 million people which accounts for 1.6% of the total population [5,6,7]. These features make Taiwan a typical case to study CH’s challenges and strategies in remote areas accompanied by ageing populations.
Much health-related research is conducted through quantitative method due to its evidence-based nature. Quantitative research is designed for the natural sciences and covers surveys, laboratory experiments, econometrics, statistical analysis and others. On the other hand, qualitative research methods are developed in social sciences for the study of social and cultural phenomena [8]. It features on seeing the world from the participants’ lenses to discover insights that will contribute to the development of empirical knowledge. Although this study was conducted in a qualitative manner, which differs from a qualitative research that can offer a statistics variation, it may contribute knowledge by offering insights and implications that may inspire areas that encounter similar challenges [8,9]. Based on findings of this study, a further discovery of the root causes of the issues in CH can be identified. Their connection with business model innovation can be developed as an innovation driver to sustain CH’s practice.
Studies of Taiwanese universal health insurance (UHI) are of interest for researchers due to the comprehensive coverage of care for residents and the reduction of health disparity in the society [10]. Particularly, the Taiwanese society has distinct universal health insurance that covers all citizens both in remote and urban areas. However, significant benefits for the insured elderly among remote residents need to be explored and addressed. In the past, challenges in accessing health care associated with transportation, social isolation, poverty, and a lack of health care providers, especially medical specialists confronted the rural residents to facilitate the benefits of UHI, CH is expecting to make contributions to equitable right to access healthcare. What is disputed in the democratic society is the right of equality and the contributions of its participants [11,12]. It is seen that citizens pay for the same insurance fees, while not everyone enjoys the same health benefits. Although the implementation of health facilities in remote areas may be costly, it is relevant to concern oneself with the needs of remote residents in a democratic society [13]. Therefore, the authors aimed to identify key challenges and possible strategies in CH to ensure the quality of care and equality. It is expected that the finding of this research can benefit an ageing society and remote residents. The objective of this study was to discover CH’s influencing factors so as to develop strategies of removing barriers and improving access to health services for remote residents.
1.2. The Selection of Research Target
Several essential features are identified to conduct a meaningful connected health study based on literature review [14,15,16]. These are demographics of population ageing; comprehensive CH ecosystem, Information Communication Technology (ICT) infrastructure; and the region or area with significant geographic features. Taiwan has been selected as a critical case study as it meets the preconditions and essential requirements for the successfully implementation of CH. Taiwan has its importance uniqueness, and revelatory in researching CH due to the following characteristics: Taiwan has become one of the fastest ageing population areas in the world due to the advancement of medical technology, changing family concepts, and a low birth rate as well as its significant geographic features [17,18,19,20,21].
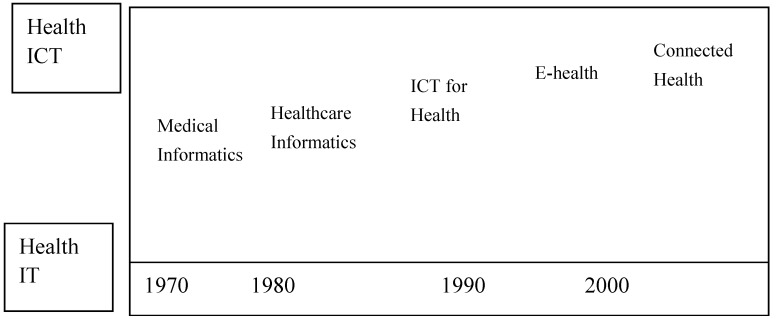
Although in Taiwan, different terms, such as remote health, Telecare or Telehealth, in general, are more frequently used rather than the term “connected health” (CH) for describing similar models by healthcare professionals, it is still in the same domain for discussion and comparison (Figure 1) [22,23,24,25,26,27]. Currently, researchers tend to use Connected Health as a term that applies to the linked systems and people in the application of ICT in healthcare in general [14,28,29].
Figure 1.
The evolution of names from ‘medical informatics’ to ‘connected health’ (Rossi Mori et al., 2007).
The literature indicates that CH includes the whole Telemedicine (TM) family: Telemedicine (TM), Telehealth (TH), and Telecare (TC) [14,28,29]. Although Taiwanese Telecare pilot schemes have proven the feasibility of TC, there were not many remarkable results of cost-saving from TH and TM. Moreover, the cases of successful business models (BMs) still remain open issues. The results of Taiwanese pilot schemes were varied. Among these issues of CH, payment models are one of the most important issues as they play an important role in keeping CH businesses sustainable. The CH in Taiwan, like many other areas, have an issue of being sustainable after government funding has finished. Designing comprehensive BMs becomes the key to success.
According to Pare et al. [30,31], the results of a systematic review of home telemonitoring, after surveying 65 programs across North America, Europe, and Asia, show the feasibility of telemonitoring healthcare [32]. However, the results for Taiwanese telemonitoring programs from 2007–2009 have shown that Taiwanese programs are competitive in terms of patient acceptance and satisfaction; a decrease in hospital admissions and a decrease in emergency room visits (shown in Table 1 and Table 2).
Table 1.
Comparison of telecare results in Taiwan with the combined results of North America and Europe.
| Characteristics | Taiwan n = 8 | North America and Europe n = 65 |
|---|---|---|
| Study period | 2007–2009 | 1990–2006 |
| Duration of each single study | 6–18 months | 5–12 months |
| Patient symptom detection | Good | Good |
| Improved physiological values | Yes | Yes |
| Patient acceptance and satisfaction | High * | High |
| Decrease in hospital admissions | Yes | Yes ** |
| Decrease in emergency room visits | Yes | Yes ** |
| Improved medicine consumption | Yes | Unknown |
| Reduction in medical costs | Yes | Not clear |
Source: Lin, 2010. * = in the case of free services, ** = except for patients with diabetes.
Table 2.
Comparison of connected health (CH) in the US and EU.
| CH | US | EU |
|---|---|---|
| Stage | Developed, mature. | Initial, pilot. |
| Service | Remote monitoring, such as remote consultation, video conferencing, and self-management via vital signs parameter measurement, helping patients adhere to medication regimens, and reducing referral wait times. | Self-management, such as with the aim of preventing fall injuries among the elderly. Remote monitoring, such as via alarms, general nursing tasks, physical therapy, social work, nutrition and health consultation, meal delivery, patient transportation, and emergency help provision. |
| Samples | Up to 18,000. | Up to 6000. |
| Main segment | Chronic conditions, such as depression, diabetes, heart failure, and Intensive Care Units (ICU). | Diabetes, heart failure. |
| Public or private | Mainly private. | Mainly public. |
| Leader | Mainly hospital-led, some are government-led. | Government-led. |
| Coverage | Nationwide for veterans only, others are regionwide. | Regionwide. |
| Care model | Institution, home. | Institution, home. |
| Outcomes | Significant outcomes in quality improvement and cost savings. | Outcomes are varied and limited to small populations. |
| Business model | Mainly privatized. | Mainly government sponsored. |
Source: Summary of literature review by the author.
The reasons, such as “preventing ill health”, “maximizing the potential of technology”, and “supporting workforce” were those which drove the Telehealth (TH) pilot project in Taiwan [33]. It was initially executed in 2008 and within one year, three different models had a noticeable performance:
In the home care model: the hospital readmission rate had a reduction of around 61%; the hospital visit rate had a decrease of over 1%;
In community care models, the medication non-adherence rate had a decline of over 76%;
In the residential-care model, the readmission rate to the hospital was reduced by over 25%, nosocomial infection decreased by over 38%, and the drug duplication rate declined to 53% [34].
The concept of this TC monitoring is to allow the long-term management of chronic illnesses as well as providing immediate information, to give an early warning of possible diseases—both of which meet the goal of preventive healthcare.
People in Taiwan tend to share the same feeling of being “Aging-in-Place”, which offers remote health a strong reason to develop [35,36,37,38]. Pressure on financially constrained healthcare systems is exacerbated by the stress of heavy workloads among healthcare staff. Irrespective of the national effort involved, the wish of the Taiwanese democracy is to maintain and improve its universal healthcare system, but hard work alone cannot maintain it anymore. Therefore, what are the options when putting in more human effort is no longer an option?
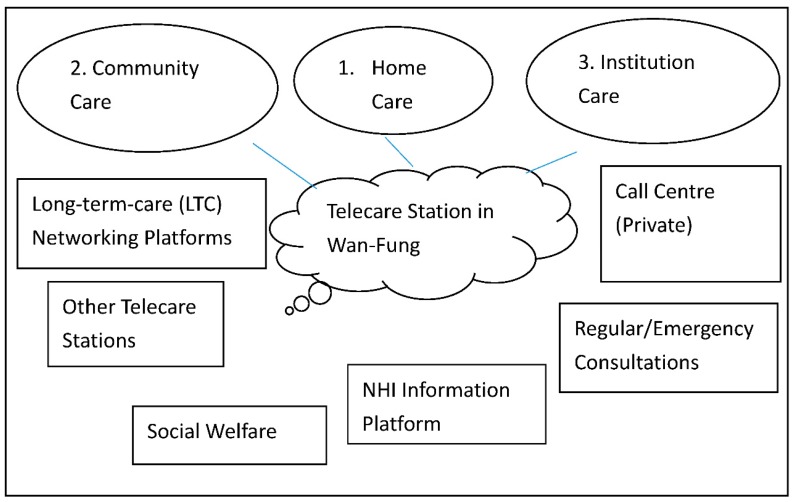
In the TC pilot project, an electronic care records exchange system and an authorized environment were constructed under three service models (home care, community care, and institutional care) in order to offer more integrated care services (shown in Figure 2). These three models are classified and featured according to where the care is facilitated. The home care is mainly supported full time by the family members of the care receivers while the community model is supported by community facilitators in the daytime and family members after their working hours. As for the institutional model, it is commonly for those who cannot be supported by their family and community members. They will be cared by the institution required in a fulltime base, such as a care home. In general, these three models work independently. However, they will seek help from each other once they are in need. The community care service model aims to establish a community model by connecting various community medical care service resources. The home service model seeks to introduce more than 150 home subjects and connect more than five home care service resources. The institutional care service model cooperates with hospitals and nursing homes to construct two nursing home models. In order to support and monitor quality customer service, 24-hour call centers are established. Long-term care (LTC) networking platforms are built to offer integrated, seamless care by connecting subjects’ information from different care service providers with a referral system to increase resource connecting efficiency. Many educational and promotional events are held to spread the word about these three care service models in order to encourage their potential duplication and expansion.
Figure 2.
Telecare (TC) in Taiwan (source: Department of Health, Taiwan, 2009).
While some researchers argue that the incorporation of new technologies may not contribute to patient satisfaction, a successful Taiwanese pilot project has proven that this application is beneficial for building up trust and mutual understanding between patients and hospitals and also for reducing criticisms of hospitals [39,40]. This project has also proven that TC is effective in maximizing the potential of technology in addition to showing several other immeasurable benefits, such as allocated medical resources and preventive health [14].
Although this government-sponsored platform can enable tele-monitoring and patients’ self-management to allow remote residents living independently, some issues remained to be addressed. Compared to the institution care model, community care and home care models are more culturally accepted among these three models. As the concept of living with parents and taking care of parents at home are the mainstream in Taiwanese society. To promote the facilities and benefits of institutional care may be an opportunity of action. With the shift of family concept, institutional care may become more and more population in the future. For the other two models, the cost issue may be the most relevant factor influencing people using CH facilities. Most of the users are happy about the services, but only a few people are willing to pay for them. It is suggested that developing a comprehensive business model will be critical for sustaining the CH system of home and community model. What they have in common is that concerns of system integration, information security, and multidisciplinary collaboration need to be resolved among these three models. These challenges will be further communicated in the Result and Discussion Section. The findings of Taiwanese experience imply that users, especially older adults are seeking the care environment that can allow them to live with dignity and comfort. Therefore, it is relevant to understand the key factors of CH’s service models for the benefits of promoting and developing the CH industry.
1.3. Conceptual Framework
A conceptual framework was developed according to the literature review and will be further developed accordingly after the data analysis, as shown in Figure 3. The initial issues of CH have been identified in the literature review and further CH challenges have been assessed through data collection and analysis.
Figure 3.
A conceptual framework of this study.
According to the three care models mentioned above, they reveal that the institutional care model has potential to be expanded; a sustainable BM needs to be developed to resolve issues of system integration, information security, and multidisciplinary collaboration. Specifically, these issues can be concluded as costs, infrastructure, technology, business model, communication and collaboration, and business sustainability. A further study can be designed based on the characteristics of the factors related to CH in the results section, so that effective investigations of next stage can be developed and followed up.
In the discussion, the disruptive innovation theory and relevant literature are employed to communicate with the findings. Key factors were identified and classified into two groups: generic to health systems and specific to CH inclusion. Generally, it seeks to discover how current health infrastructure can support the implementation of CH. Specifically, it aims to investigate how technology can mediate between geographic isolation and accessibility and how a business model can interact with cost and purchase capability/affordability. Business model and business sustainability are also crucial factors to be discussed, as both direct cost and indirect cost are relevant factors influencing remote residents’ affordability. Therefore, it is relevant to understand the key factors influencing the application of Connected Health in remote areas in Taiwan with a qualitative pilot study for the benefits of promoting and developing the CH industry.
This pilot study aimed to identify future directions and information for conducting the multi-stage interviews for collecting the data more effectively. According to the finding of this study, a comprehensive research for investigating CH’s sustainability and potential strategies that may contribute to academia, industry and government can be designed in the next stage.
Research questions:
-
(1)
What are the factors influencing the implementation of connected health in Taiwanese remote areas as perceived by stakeholders?
-
(2)
Which factors are perceived by stakeholders as specifically important to the adoption, implementation, and continuation of connected health in remote areas?
-
(3)
What are the perceived facilitators and barriers for users in remote areas to access healthcare service through technology?
This research topic is valuable and valid as it influences a human being’s life to such a significant degree. It is particularly important when we are facing global economic and social challenges. It could possibly transfer threats into opportunities. It potentially can generate knowledge that will make contributions to improving efficiency and effectiveness in the healthcare sector.
2. Methods
2.1. Participant Selection
Stakeholders and experts were selected for the interviews according to the literature review and snowball sampling [41]. These participants were interviewed on a voluntary basis and gave verbal consent according to ethical guidelines. This study was approved by Ulster University’s institutional review board. The reference no. is RG3 RMcAdam2. The study’s participants included healthcare professionals, industry players, academic researchers, and government agents. The researchers identify participants’ backgrounds, competencies, gender, their geographic locations, etc., as they may relate to the outcomes of this research. Our semi-structured interview guide comprised the following:
Working sectors;
Background information;
Gender;
Levels of competency.
2.2. Justification of Method Used
The reason why the qualitative method was employed in this study is justified here through the comparison of quantitative and qualitative research, as shown in Table 3. According to Bryman, contrasting aspects of quantitative and qualitative research is presented to demonstrate the main features of these methods [41]. The former focuses on numbers and a statistics variation to test theory from the point of researcher while the latter emphasizes the meaning of words or phrases to emerge theory from the point of view of participants. This study aimed to discover and explore factors influencing the application of CH in remote areas, it closes to the nature of obtaining contextual understanding of qualitative research from rich and deep data. The most important one is the feature of seeing the world from the participants’ lenses to discover insights that will contribute to the development of empirical knowledge. As this study seeks to obtain the inner experience of participants, to determine how meanings are formed through and in culture rather than test variables, which meet the features of the qualitative approach. Qualitative research is fluid, evolving and dynamic in nature; on the contrary, a quantitative approach is more rigid and structured in format. Statistics might be interesting; however, exploring the infinite possibilities of targeted participants may be more attractive to qualitative researchers [42]. Therefore, qualitative research is more suitable to this study.
Table 3.
Contrasting quantitative and qualitative research.
| Quantitative Research | Qualitative Research |
|---|---|
| Numbers | Words |
| Point of view of researcher | Point of view of participants |
| Researcher is distant | Researcher is close |
| Theory testing | Theory emergent |
| Static | Process |
| Structured | Unstructured |
| Generalisation | Contextual understanding |
| Hard, reliable data | Rich, deep data |
| Macro | Micro |
| Behaviour | Meaning |
| Artificial setting | Natural setting |
Source: Bryman, 2008, p. 393 [41].
2.3. Data Collection
In this pilot study, an exploratory approach was conducted involving semi-structured in-depth interviews with 18 participants from remote allied case studies and their stakeholders. “Four administrative areas of applied CH based on geographic and rural location” was the main criteria for selecting participants. “Those who have experiences in CH” was the second selection criteria. These sampling criteria were chosen in order to include the inputs of major and significant participants with various levels of rural experience and management that can be covered. Consequently, health institutions covering from northern, central, southern, and eastern Taiwan were covered in this study.
Following the informed consent, researchers conducted face-to-face interviews with seventeen participants from 30 min to 2 h. Being aware of the significance of validity and rigor of qualitative research, several research strategies were conducted to ensure the quality of data collection. These protocols cover the use of the Agile method to allow interviewees’ opinions to be validated and exchanged through a semi-structured interview manner. Any differences between the interviews were discussed until a consensus was reached. Audio-taping interviews and transcribed verbatim by an independent typist were subsequently validated by the researcher. Meaningful quotations were adapted to represent important themes. To address participants’ confidentiality, data were processed through de-identified considerations.
2.3.1. Pilot Interviews
There were 18 interviewees to be chosen in the pilot interviews (as shown in Table 4). They were chosen according to CH literature and snowball sampling, which were classified based on working sectors, background information, gender, and levels of competency. The age indicator is not included as this study considered that competency is more relevant than age and can be covered by competency. Apart from that, most of participants were between the ages of 40 and 50; therefore, it does not show significant difference in this study. Although the sample size is small, it covered representative participants in the microenvironment. In the pilot study, the variety of participants are more important than the numbers. A bigger population size and a more uniform distribution will be made in the next stage of research. The majority were healthcare facilitators as they were inevitable in the CH ecosystem. Their feedback was significant in reflecting the effectiveness of CH products and services. Therefore, understanding their views was significant in the successful and user-friendly interactive system design. This pilot interview focused on health professionals rather than patients and their families due to ethical concerns.
Table 4.
Pilot interviewees’ profile.
| Organization | Gender (M: 56%/F: 46%) | Title/Level of Competency | |
|---|---|---|---|
| Industry (4) (22%) | June Sun Digicom | M | 1. General Manager |
| DigiO2 | M | 2. Tech Advisor | |
| Netown Corporation | M | 3. Manager | |
| Far EasTone Telecommunications | M | 4. Manager | |
| Government/Semi-government (2) (11%) | Taiwan forces for Medical Travel | M | 5. CEO |
| F | 6. Vice Project Manager | ||
| Academia (1) (6%) | Taipei Medical University School of Gerontology Health Management College of Nursing | F | 7. Assistant Professor/Attending Physician |
| Healthcare providers (11) (61%) | Chang Gung Memorial health Village | F | 8. Staff |
| Antai Medical Care Hospital | M | 9. Director/G.P. | |
| F | 10. General Physician (G.P.) | ||
| San-Chung Health Center | F | 11. Head Nurse. | |
| Y.R. Chinese Medicine Clinic | M | 12. Doctor | |
| F | 13. Manager | ||
| Tri-service General Hospital | M | 14. Medical doctor | |
| Taiwan University Hospital | M | 15. Medical doctor | |
| Kaohsiung Municipal Hsiaokang Hospital | F | 16. Pharmacist | |
| Zhang Bi Zheng Family Physicians Clinic | M | 17. Director/G.P. | |
| Home Physics | M | 18. Therapist |
2.3.2. Data Analysis Methods
Data are concurrently collected and analyzed until theoretical saturation is reached as suggested by Yin [41]. In this research, a thematic and a systematic approach to qualitative analysis was performed collaboratively. The thematic analysis was organized via deep familiarization with the data collected leading to the development of major themes. The systematic analysis was employed as quasi-statistical (content) analysis to ensure the validity of the analysis. These themes were further analyzed to identify sub-themes and were structured to provide a comprehensive account.
The author adopted a data triangulation testing method to ensure that the analysis of the results was valid. Data triangulation examined the consistency of different data sources with the same method. They can be at different points in time and space; allowing for the comparison of people with different viewpoints. This included interviews taking place at different points in time and with four different entities (such as government, academia, industry, and healthcare providers). The theory triangulation included a content analysis, a template analysis, and an editing analysis (thematic analysis), which led to the use of multiple theoretical perspectives to analyze and interpret the same phenomenon in this research.
In this study, data were categorized using a thematic analysis. Codes were derived from the data through several steps, including data cleaning, data summarizing, data analysis, and data mining. The categorization of data consisted of continually revisiting and reviewing until the themes and categories used to summarize and describe the findings were verified and accurately reflected the data. A qualitative data management system, the Nvivo 12 software (produced by QSR International, Melbourne, Australia), was employed to manage the data throughout the process. Firstly, data were cleaned through the integration process to merge different terms which have the same meaning. For example, connected health could be called remote health, telehealth, and telecare in the interviews. Terms were merged according to the actual meaning of interviewees. Secondly, data were summarized, clustered, and categorized based on the meaning of interviewees. Thirdly, data were analyzed and extracted according to the insightful meaning from interviewees as it is the stage of the data mining process. For example, some issues were raised by interviewees but the meaning behind the issues and the root cause of the issues need to be analyzed.
3. Results
3.1. Pilot Interview Results
A sample of 18 respondents was interviewed. These covered key influencers, including government, academics, health professionals, and relevant business professionals. They were selected through voluntary participation and a significant sampling method across various health system levels. The purpose of the pilot interviews was to identify factors influencing application of CH in remote areas. This pilot study also has the advantages of identifying potential directions and information for conducting the multi-stage interviews for collecting the data more effectively. Although the results reveal that the study of CH is meaningful, there is an issue of business sustainability, which is obscured by some barriers that need to be addressed. These barriers will be further investigated in the first-stage interview.
Figure 4 and Table 5 illustrate the relationships and collaboration between CH players and stakeholders in its business ecosystem [43]. Interviewees are selected and grouped into eight categories based on this business ecosystem. What Figure 4 presents is the relationship diagram among CH players and its stakeholders. It is seen that a CH ecosystem should cover Government sectors (No. 7), Industry players (No. 1–6) and Academic and consultant institutes (No. 8). What is noticeable is that Connected Health service provider (No 4) is in the central position that interacts with government and industry. It also communicates with data centre for data storage and retrieval. There is a variety of End users (No. 6), they can be patients and their family, health professionals and others according to the circumstance that occurred. As for the Academia and consultant institutes (No. 8), they play a role of providing fundamental knowledge for CH players to act upon. Although it seems to be relatively passive and invisible, it is evitable in the system. Due to the limitation of the current regulation, CH can only be practiced in hospitals or care institutions in Taiwan. Although they are difficult to define as academia or industry, they are important roles in this field. By collecting different perspectives in this research, it aims to inspire more creative approaches to exploit the innovative advantages accruing from healthcare innovations.
Figure 4.
CH players and stakeholders’ relationship diagram [43].
Table 5.
Interviewees’ categories.
| Categories | No. | Name | |
|---|---|---|---|
| 1 | Software developers | 101 | June Sun Digicom |
| 102 | DigiO2 | ||
| 2 | Hardware manufacturers | 201 | Netown Corporation |
| 3 | Total solution providers | 301 | Not Applicable |
| 4 | CH care service providers | 401 | Chang Gung Memorial health Village |
| 402 | Antai Medical Care Hospital | ||
| 403 | San-Chung Health Center | ||
| 404 | Y.R. Chinese Medicine Clinic | ||
| 405 | Tri-service General Hospital | ||
| 406 | National Taiwan University Hospital | ||
| 407 | Kaohsiung Municipal Hsiaokang Hospital | ||
| 408 | Zhang Bi Zheng Family Physicians Clinic | ||
| 409 | Home Physics | ||
| 5 | Network providers | 501 | Far EasTone Telecommunications |
| 6 | End users | 601 | Not Applicable |
| 7 | Government sectors | 701 | Taiwan forces for Medical Travel |
| 8 | Academia | 801 | Taipei Medical University School of Gerontology Health Management College of Nursing |
Source: Summarized by the authors.
Table 6 presents the results of the CH issues that are scored by the interviewees. Interviewees were numbered (101, 201, …) based on the eight categories from Table 5. If the issue is considered “important”, it gets one point. If the interviewees think the issue “may be important”, it gets 1 point, if they are “not sure” about it, it gets 0 points. If the issue is considered as “not important,” it gets −1 point. The table sums up the results to see the importance of CH issues identified in the stage one data collection (shown in Table 6). This table measures the importance of each category according to participants’ perspective. The description of each category is presented in Section 3.2.1, Section 3.2.2, Section 3.2.3, Section 3.2.4, Section 3.2.5 and Section 3.2.6.
Table 6.
Interviewees’ perspectives score in terms of CH issues.
| Cost | Infrastructure | Technology | Business Sustainability | Collaboration and Communication Related | Business Model | Others | |
|---|---|---|---|---|---|---|---|
| 101 | −1 | 1 | 1 | 1 | 0 | 1 | Trend of ageing and low birth rate |
| 102 | 0 | 1 | 1 | 0 | 0 | 0 | Technology is there to use |
| 201 | 1 | 0 | 1 | 1 | 1 | 1 | Mobility and integration of devices |
| 301 | 0 | 0 | 0 | 0 | 0 | 0 | It is replaced by 101 and 201 in this study. |
| 401 | 1 | 0 | 1 | 1 | 1 | 1 | Human care |
| 402 | 1 | 0 | 1 | 0 | 1 | 1 | Government’s incentive matters |
| 403 | 1 | 0 | 0 | 0 | 1 | 1 | Government’s policy matters |
| 404 | 1 | 0 | 1 | 1 | 1 | 1 | Willing to collaborate once the solution is ready |
| 405 | 1 | 1 | 1 | 1 | 1 | 1 | Fellow Government’s policy and projects |
| 406 | 1 | 1 | 1 | 1 | 1 | 1 | Holistic health matters |
| 407 | 1 | 1 | 1 | 1 | 1 | 1 | CH is essential but an economic scale is requested to sustain this business |
| 408 | 1 | 0 | 1 | 0 | 1 | 1 | Happy to accept all the solutions for the benefits of patients and businesses |
| 409 | 1 | 0 | 1 | 1 | 1 | 1 | Holistic health matters |
| 501 | 1 | 0 | 1 | 0 | 1 | 1 | CH has great potential |
| 601 | 0 | 0 | 0 | 0 | 0 | 0 | Their opinions are reflected by health professional. |
| 701 | 1 | 1 | 1 | 1 | 0 | 1 | Expand Taiwanese models worldwide |
| 801 | 0 | 1 | 1 | 0 | 1 | 1 | Universal design application matters |
| Total | 11 | 7 | 14 | 9 | 12 | 14 |
Important: 1, maybe or not sure: 0, not important: −1.
3.2. Characteristics of the Factors Related to CH
What influences the implementation of connected health in Taiwanese remote areas varies in regard to the nature of stakeholders based on Table 6. Factors are explored with interviewees from government, industry, academia, and health institutions. They identified factors relating to CH in Taiwanese remote areas as determinants of successful adoption, implementation, and continuation. Factors are scored by importance in Table 6 according to respondents’ viewpoint. They reported that the engagement of remote residents, reachable health service infrastructure, accessible methods of communication, and the availability of human resources and equipment were all important characteristics of CH projects in remote areas. According to Table 6, the factor of technology and business model obtain the highest score, while the factor of collaboration and communication comes next. The factor of infrastructure seems to be less important for participants. Health facilitators of remote residents highlighted factors relating to inclusive costs, infrastructure, technology, business model, communication and collaboration, and business sustainability. Their characteristics are described below.
3.2.1. Cost
Initially, the Taiwanese government sponsored several pilot schemes to assess the feasibility of CH in remote areas. It can be seen that the efficiency of care can be delivered through these services. However, after the sponsorship ceased, residents had little interest in using CH services as they have a limited purchase capability. Alternative solutions should be provided to sustain the business.
“Remote residents are usually voluntary groups; they have low purchase capability … They often rely on physicians to visit or public resources to manage their health.”
(General physician, male)
As far as cost is concerned, some health institutions request that their suppliers offer a free trial for a period of time to initiate these businesses. The industrial players need to take the risk first before getting the payment from customers.
“Hospitals request a free trial from us to motivate their end users, … once they are not happy about the products, we cannot make any money.”
(Business manager, male)
In the CH industry, health professionals have authority over customers. If the products are recommended by them, customers are more likely to adapt them. Therefore, companies prefer to partner with hospitals. However, hospitals usually do not want to take the business risk for them, so they will ask for a free trial prior to payment to reduce the cost burden for consumers.
“Health professionals have a strong authority over end users, so we need to work with them, even though we might need to sacrifice some benefits.”
(CH tech adviser, male)
3.2.2. Infrastructure
Infrastructure refers to the essential requirements for constructing CH platforms. As the literature suggests, CH requires collaboration from the government, academia, and industry to build a comprehensive ecosystem. Although cost issues are important, without essential infrastructure, CH services cannot be provided, especially as they are closely related to national infrastructure. Reducing the cost of traveling to remote areas is one of the most proposed features of CH but many remote areas currently lack the ICT infrastructure necessary to implement CH services. Low population density makes it less cost-effective to build up infrastructure, such that profit-oriented companies are likely not to be eager to adopt it. In this case, government intervention is necessary.
“Network companies think building up infrastructure in remote areas is not cost-effective, as the scale of economy is too small, they are not willing to make efforts on it … Without the government’s intervention, CH infrastructure is difficult to be accomplished.”
(General Physician, male)
“Although infrastructure is essential, there is nothing we can do about it… maybe the government has the power and authority to do it,… what we can do is to design a product that relies on current resources as much as possible.”
(Manager, male)
3.2.3. Technology
Technology issues refer to the technical challenges based on the current infrastructure. It not only enables CH in practice but also ensures accurate and reliable data that can be converted into useful information. The focus has been on vital sign parameter measurement management and audio/video consultations technology. In remote areas, internet infrastructure is very expensive. According to research, it usually requires 5 to 10 years to earn back initial expenditure, such that it is often not considered cost-effective for ICT companies to establish infrastructure. In addition, many people still have fear and uncertainty in relation to new technological interventions. Therefore, the concern needs to be with user-friendly customer-focused infrastructure.
“Building infrastructure is very expensive. We aim to offer an all-inclusive service through our connected device, in this case, users do not need to rely on the government’s infrastructure but current resources …”
(Manager, male)
“We use the technology of smart house to monitor residents’ health and connect to health institutions.”
(Social worker, female)
Apart from this, associated standards such as data exchange security, safety, and privacy, are essential to take into account. Controversy has continued over the feasibility and customer satisfaction within CH practices as it has been argued that there is both a lack of evidence and a lack of confidence in the successful implementation of CH. The issues of resistance to change and a slow clinical acceptance of CH remain.
“I have been a general physician for over a decade, and I only believe personal contract, any what is called technology in health, is only a buzz word for me!”
(General physician, male)
What matters to health professionals is whether technology can achieve their mission to improve the care experience, enhance outcomes, and reduce costs rather than the means that technology is addressed. Health professionals want technologies that can be deeply embedded into their workflow and be situated in one location rather than increase their workload. This implies that technology not only plays the role of solution provider or enabler but, most important, that it should also integrate all players in pursuit of customer value and a user-friendly interface and design.
“Our clinic is open to all the solutions that are beneficial to our patients. We are happy to accept all the new technology as long as it works.”
(Director/General physician, male)
3.2.4. Collaboration and Communication
As CH involves roles in many different sectors and departments, the versions of CH and the interests of stakeholders may be diverse. Therefore, the authority and the executor may have different opinions on the same project. Support from the top is important; however, how to integrate resources and to build up cross-department collaboration remains a challenge to be overcome.
“I only know our part of the business and take orders from my supervisor. I have no clue about the business from other sectors …”
(Tech advisor, male)
“CH can do more things than we have known today, especially the holistic healthcare management … that is why our government wants to integrate the department of health with social welfare to enable more integration and cooperation.”
(General physician, male)
Quality problems are caused by poor integration. It is essential, therefore, to carefully consider issues of integration when planning or implementing a healthcare service that seeks improvements both to quality and cost-effectiveness. The importance of communication-related challenges by pointing out that participants in CH have different interests and concerns makes it more difficult to speak in a common language or to share common ground.
“Our institution aims to offer a more integrated service to help people to find suitable facilitators to solve their problems as we understand many health provisions are isolated from departments …”
(CEO, male)
“… an ideal project-based management that can integrate resources is essential to deliver comprehensive services to the public.”
(Vice-project manager, female)
3.2.5. Business Sustainability
CH businesses encounter challenges related to their sustainability after government funding ceases. Many government-led pilot schemes have pointed to the feasibility of CH and the satisfaction of its clients, but some schemes have proved unsustainable after governmental funding has ceased. Although people have high expectations of CH, sustainability issues remain a major challenge—in the pilot scheme period, the government-sponsored CH expenditure. However, after sponsorship ceases, CH businesses encounter sustainability issues. Some businesses close down while others only barely survive. This may be because of the homogeneity of CH’s business models; although every company has its unique business model, BMs tend to be a similar “pay for service” structure in the case of CH.
“We have contacted as many CH users as possible, but they are only willing to use our products in the condition of government’s sponsor … They stop using our products once the funding from the government ceases.”
(Manager, male)
“This business is not as promising as people seen in the public media, as many of us encounter the issue of business sustainability.”
(Manager, male)
3.2.6. Business Model
A comprehensive business model not only seeks to solve business sustainability issues but also the other issues mentioned above. Crucial principles and themes of successful implementation of technology-driven healthcare innovation remain to be investigated; agreement needs to be reached and knowledge disseminated. Solutions that promise cost-effectiveness and efficiency may meet the needs of the market. Business modeling of CH care and a social care model may be able to meet these goals.
“A comprehensive business model under the current health infrastructure may be helpful to keep the connected health business sustained.”
(Manager, male)
“I think to make connected health successful is not only about health facilitators but also how to design a comprehensive business model to couple with current stakeholders.”
(Pharmacist, female)
4. Discussions
This study addresses what factors influence the application of connected health in Taiwanese remote areas. The influence of the adoption, implementation, and continuation of connected health in remote areas is informed. As there was a significant overlap in the factors identified based on the responses from these groups, we combined responses of both types of respondents when reporting results. Technology and business models (BM) are perceived by stakeholders as specifically important to the adoption of CH in remote areas.
Key factors were identified for the introduction of CH at two groups: (1) generic to health systems: infrastructure and collaboration and communication; (2) specific to CH inclusion: costs, technology, business model, business sustainability. These factors highlight the fact that CH in remote areas is achievable with the help of leadership, management, and strategic planning.
The findings suggest that geographic isolation and purchase capability were key restraints for participants. Therefore, how technology and business model mediated between purchase capability and geographic isolation should be highlighted. Health facilitators also indicate that those who seek or accept CH services due to not being able to afford the direct costs and indirect costs (e.g., transport and any accompanying person) may benefit from disruptive technology and business model innovation. These findings are similar to Hwang and Christensen’s perspectives on how disruptive technology can leverage challenges to opportunities for remote residents and why strategies for remote area should be included from the planning phase of a connected health program. [42,43,44]. CH reduce the inability to access healthcare due to poverty increases the risk of poor health. In remote areas, chronic conditions further exacerbate this interaction between poverty and health [45,46]. People with chronic conditions are at greater risk of poverty due to lower employment rates and lower educational attainment [45,46,47,48]. Furthermore, this risk leads to greater inequities in accessing healthcare and having their healthcare needs met, including those relating to chronic conditions, compared to the broader population. Thus, CH is critically needed in remote areas.
The findings of this study indicate that CH can reduce the indirect costs in remote settings. As at a higher risk of poverty, people with chronic conditions may also incur higher indirect healthcare costs [48]. The need for an accompanying person to enable an ageing population to attend health services was underlined [49,50]. In addition to the transport and other costs for the accompanying person, their opportunity cost of income-earning activities creates a greater risk of household poverty, perpetuating the interaction between poor health and low purchase capability for the person with chronic conditions and their household [51,52,53].
Although those who are close to communities, with the availability of national insurance or a poor certificate, may get reduction of healthcare cost, it is relevant to have an alternative provision of healthcare that can reduce the geographic barriers. These discoveries confirm the needs of a CH study in remote areas. Addressing the factors such as cost, transport, and health workers’ availability through CH are therefore important for providing healthcare to remote residents. Moreover, CH platform can also be used and transferrable for mental health or various age groups [54,55,56]. This study confirms the feasibility of CH in remote areas and seeks to explore deeper its scalability and sustainability in the next stage investigation.
5. Conclusions
This pilot study in Taiwan provided the opportunity to learn what is feasible for CH in remote areas. This study found that factors influencing the adoption, implementation, and continuation of the CH in Taiwanese remote areas were costs, infrastructure, technology, business model, business sustainability, collaboration, and communication. The factors of technology and business model are considered more important than others. These findings echo the theory of disruptive innovation that disruptive technology may leverage healthcare into a more affordable and accessible service. The findings also confirm the needs for a CH study in Taiwanese remote areas and they highlight that strategies development for the remote area should be included from the planning phase of a connected health program. Knowledge of the CH platform can also be used and transferred for mental health or various age groups. This study confirms the feasibility of CH in remote areas and seeks to explore deeper into its scalability and sustainability in the next stage investigation. Information from this research can be used to develop a larger-scale investigation to obtain business vision in future work.
6. Limitations
This study is limited by the sample of participants and ethical concerns; patients were therefore excluded from this study; however, their opinions are reflected by their health facilitators. Some relevant people in CH such as IT security were not included as their influence on the CH system and service is low. Other people such as total solution providers are missed due to the time limitation and the nature of a pilot study and may be covered in the next stage of the interview. After having explored the factors and feasibility of CH in remote areas, another stage of interview is required to get the management’s insights and depth of the research.
Acknowledgments
The author would like to thank Rodney McAdam, Michael Brennan, and Shirley Davey from Ulster University for sharing their pearls of wisdom during this research.
Author Contributions
Conceptualization, S.C.-I.C.; Data curation, S.C.-I.C.; Formal analysis, S.C.-I.C.; Funding acquisition, S.C.-I.C.; Investigation, S.C.-I.C.; Methodology, S.C.-I.C.; Software, C.L.; Supervision, C.L.; Validation, C.L.; Visualization, C.L.; Writing—original draft, S.C.-I.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by Huaqiao University High-level Talent Research Startup Project and The Straits Postdoctoral Fellowship Funding Program in 2018, Fujian Financial office no. [2017]60532/50X18137.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Weeks W.B., Kazis L.E., Shen Y., Cong Z., Ren X.S., Miller D., Lee A., Perlin J.B. Differences in Health-Related Quality of Life in Rural and Urban Veterans. Am. J. Public Health. 2004;94:1762–1767. doi: 10.2105/AJPH.94.10.1762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Su Y.-Y., Wang S.-H., Chou H.-C., Chen C.-Y., Hsieh W.-S., Tsao P.-N., Tsou K.-I., Network T.P.I.F.-U., Hsu C.-H., Mu S.-C., et al. Morbidity and mortality of very low birth weight infants in Taiwan-Changes in 15 years: A population based study. J. Formos. Med. Assoc. 2016;115:1039–1045. doi: 10.1016/j.jfma.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 3.Lo W.-C., Shie R.-H., Chan C.-C., Lin H.-H. Burden of disease attributable to ambient fine particulate matter exposure in Taiwan. J. Formos. Med. Assoc. 2017;116:32–40. doi: 10.1016/j.jfma.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Du P.-L., Huang I.-C., Huang Y.-H., Chang C.-S. Dual normative commitments mediating the relationship between perceived investment in employees’ development and intention to leave among the healthcare workforce in underserviced areas of Taiwan. Rural Remote Health. 2019;19:1–8. doi: 10.22605/RRH4837. [DOI] [PubMed] [Google Scholar]
- 5.Chiu W.-T., Hsu M.-H., Teng S.-W. Using health information technology to reduce regional health inequality in Taiwan. J. Formos. Med. Assoc. 2015;114:1–2. doi: 10.1016/j.jfma.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Hsu C.-H., Tsao T.-C., Huang C.-M., Lee C.-F., Lee Y.-T. Using Remote Sensing Techniques to Identify the Landslide Hazard Prone Sections along the South Link Railway in Taiwan. Procedia Eng. 2016;143:708–716. doi: 10.1016/j.proeng.2016.06.107. [DOI] [Google Scholar]
- 7.Wu P.C., Lay J.G., Guo H.R., Lin C.Y., Lung S.C., Su H.J. Higher temperature and urbanization affect the spatial patterns of dengue fever transmission in subtropical Taiwan. Sci. Total Environ. 2009;407:2224–2233. doi: 10.1016/j.scitotenv.2008.11.034. [DOI] [PubMed] [Google Scholar]
- 8.Creswell J.W., Creswell J.D. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Sage Publications; Southend Oaks, CA, USA: 2017. [Google Scholar]
- 9.Angeli F., Jaiswal A.K. Business Model Innovation for Inclusive Health Care Delivery at the Bottom of the Pyramid. Organ. Environ. 2016;29:486–507. doi: 10.1177/1086026616647174. [DOI] [Google Scholar]
- 10.Liao P.-A., Chang H., Yang F.-A. Does the Universal Health Insurance Program Affect Urban-Rural Differences in Health Service Utilization Among the Elderly? Evidence from a Longitudinal Study in Taiwan. J. Rural Health. 2011;28:84–91. doi: 10.1111/j.1748-0361.2011.00363.x. [DOI] [PubMed] [Google Scholar]
- 11.Culyer T. Efficiency, Equity and Equality in Health and Health Care. Centre for Health Economics, University of York; York, UK: 2015. [Google Scholar]
- 12.Roberts D. Debating the cause of health disparities: Implications for bioethics and racial equality. Camb. Q. Healthc. Ethics. 2012;21:332–341. doi: 10.1017/S0963180112000059. [DOI] [PubMed] [Google Scholar]
- 13.Yamin A.E., Norheim O.F. Taking Equality Seriously: Applying Human Rights Frameworks to Priority Setting in Health. Hum. Rights Q. 2014;36:296. doi: 10.1353/hrq.2014.0027. [DOI] [Google Scholar]
- 14.Caulfield B.M., Donnelly S. What is Connected Health and why will it change your practice? QJM Int. J. Med. 2013;106:703–707. doi: 10.1093/qjmed/hct114. [DOI] [PubMed] [Google Scholar]
- 15.Carroll N., Travers M., Richardson I. Evaluating multiple perspectives of a connected health ecosystem; Proceedings of the 9th International Conference on Health Informatics (HEALTHINF); Rome, Italy. 21–23 February 2016. [Google Scholar]
- 16.Harte R., Quinlan L.R., Glynn L., Rodriguez-Molinero A., Scharf T., Carenas C., Reixach E., García J., Carrabina J., Laighin G.Ó.A. Multi-Stage Human Factors and Comfort Assessment of Instrumented Insoles Designed for Use in a Connected Health Infrastructure. J. Pers. Med. 2015;5:487–508. doi: 10.3390/jpm5040487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker A. In: Active Ageing in Asia. Aspalter C., editor. Routledge; Abingdon, UK: 2014. [Google Scholar]
- 18.Hui L., Wang K.M. Frontier Computing. Springer; Singapore: 2016. Decision Analyses of Medical Resources for Disabled Elderly Home Care: The Hyper Aged District in Taiwan; pp. 85–95. [Google Scholar]
- 19.Yonezawa A., Hou A.Y. How World-Class Universities Affect Global Higher Education. Brill Sense; Leiden, The Netherland: 2014. Continuity and Transformation: Continuous Challenges for World-Class Status among Universities in Taiwan and Japan as Ageing Societies; pp. 85–101. [Google Scholar]
- 20.Glaser K. Global Ageing in the Twentieth-First Century: Challenges, Opportunities and Implications. Taylor & Francis; Abingdon, UK: 2013. [Google Scholar]
- 21.Li S.-C. Explore the relationships among service quality, customer loyalty and word-of mouth for private higher education in Taiwan. Asia Pac. Manag. Rev. 2013;18:375–389. [Google Scholar]
- 22.Brummer C. Disruptive technology and securities regulation. Fordham Law Rev. 2015;84:977. doi: 10.2139/ssrn.2546930. [DOI] [Google Scholar]
- 23.Lin T.C., Chang H.J., Huang C.C. An analysis of telemedicine in Taiwan: A business model perspective. Int. J. Gerontol. 2011;5:189–192. doi: 10.1016/j.ijge.2011.09.039. [DOI] [Google Scholar]
- 24.Kuo K.M., Talley P.C., Lee C.M., Yen Y.C. The influence of telemedicine experience on physicians’ perceptions regarding adoption. Telemed. E-Health. 2015;21:388–394. doi: 10.1089/tmj.2014.0091. [DOI] [PubMed] [Google Scholar]
- 25.Wu Z.Y., Lee Y.C., Lai F., Lee H.C., Chung Y. A secure authentication scheme for telecare medicine information systems. J. Med. Syst. 2012;36:1529–1535. doi: 10.1007/s10916-010-9614-9. [DOI] [PubMed] [Google Scholar]
- 26.Chiang K.F., Wang H.H., Chien I.K., Liou J.K., Hung C.L., Huang C.M., Yang F.Y. Healthcare providers’ perceptions of barriers in implementing of home telecare in Taiwan: A qualitative study. Int. J. Med. Inform. 2015;84:277–287. doi: 10.1016/j.ijmedinf.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 27.Ho Y.L., Yu J.Y., Lin Y.H., Chen Y.H., Huang C.C., Hsu T.P., Chuang P.Y., Hung C.S., Chen M.F. Assessment of the cost-effectiveness and clinical outcomes of a fourth-generation synchronous telehealth program for the management of chronic cardiovascular disease. J. Med. Internet Res. 2014;16:e145. doi: 10.2196/jmir.3346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mori A.R., Mercurio G., Verbicaro R. Enhanced policies on Connected Health are essential to achieving accountable social and health systems. Eur. J. ePract. 2012;15:4–25. [Google Scholar]
- 29.Kvedar J., Coye M.J., Everett W. Connected health: A review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff. 2014;33:194–199. doi: 10.1377/hlthaff.2013.0992. [DOI] [PubMed] [Google Scholar]
- 30.Merriel S.W., Andrews V., Salisbury C. Telehealth interventions for primary prevention of cardiovascular disease: A systematic review and meta-analysis. Prev. Med. 2014;64:88–95. doi: 10.1016/j.ypmed.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 31.Paré G., Jaana M., Sicotte C. Systematic review of home telemonitoring for chronic diseases: The evidence base. J. Am. Med. Inform. Assoc. 2007;14:269–277. doi: 10.1197/jamia.M2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin C. Telecare projects in Taiwan. Gerontechnology. 2010;9:400–407. doi: 10.4017/gt.2010.09.03.003.00. [DOI] [Google Scholar]
- 33.Ackerman M.J., Filart R., Burgess L.P., Lee I., Poropatich R.K. Developing next-generation telehealth tools and technologies: Patients, systems, and data perspectives. Telemed. E-Health. 2010;16:93–95. doi: 10.1089/tmj.2009.0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chiu K.H., Yang Y.Y.H. A case study of remote monitoring of health status of the elderly at home in Taiwan; Proceedings of the Ninth International Conference on Electronic Business; San Sebastián, Spain. 24–26 June 2009. [Google Scholar]
- 35.Procter R., Wherton J., Greenhalgh T., Sugarhood P., Rouncefield M., Hinder S. Telecare call centre work and ageing in place. Comput. Support. Coop. Work (CSCW) 2016;25:79–105. doi: 10.1007/s10606-015-9242-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Golant S.M. Geographical Gerontology. Routledge; Abingdon, UK: 2017. Explaining the ageing in place realities of older adults; pp. 189–202. [Google Scholar]
- 37.Sixsmith J., Fang M.L., Woolrych R., Canham S.L., Battersby L., Sixsmith A. Ageing well in the right place: Partnership working with older people. Work. Older People. 2017;21:40–48. doi: 10.1108/WWOP-01-2017-0001. [DOI] [Google Scholar]
- 38.Stones D., Gullifer J. ‘At home it’s just so much easier to be yourself’: Older adults’ perceptions of ageing in place. Ageing Soc. 2016;36:449–481. doi: 10.1017/S0144686X14001214. [DOI] [Google Scholar]
- 39.Stowe S., Harding S. Telecare, telehealth, and telemedicine. Eur. Geriatr. Med. 2010;1:193–197. doi: 10.1016/j.eurger.2010.04.002. [DOI] [Google Scholar]
- 40.Kao H.Y., Wei C.W., Yu M.C., Liang T.Y., Wu W.H., Wu Y.J. Integrating a mobile health applications for self-management to enhance Telecare system. Telemat. Inform. 2018;35:815–825. doi: 10.1016/j.tele.2017.12.011. [DOI] [Google Scholar]
- 41.Yin R.K. Case Study Research and Applications: Design and Methods. Sage publications; London, UK: Sep 27, 2017. [Google Scholar]
- 42.Marcus B., Weigelt O., Hergert J., Gurt J., Gelléri P. The use of snowball sampling for multisource organizational research: Some cause for concern. Pers. Psychol. 2017;70:635–673. doi: 10.1111/peps.12169. [DOI] [Google Scholar]
- 43.Chen S.C. Technological health intervention in population aging to assist people to work smarter not harder: Qualitative study. J. Med. Internet Res. 2018;20:e3. doi: 10.2196/jmir.8977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hwang J., Christensen C.M. Disruptive innovation in health care delivery: A framework for business-model innovation. Health Aff. 2008;27:1329–1335. doi: 10.1377/hlthaff.27.5.1329. [DOI] [PubMed] [Google Scholar]
- 45.Kao Y.S., Nawata K., Huang C.Y. An exploration and confirmation of the factors influencing adoption of IoT-based wearable Fitness trackers. Int. J. Environ. Res. Public Health. 2019;16:3227. doi: 10.3390/ijerph16183227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gulliford M., Figueroa-Munoz J., Morgan M., Hughes D., Gibson B., Beech R., Hudson M. What does’ access to health care’mean? J. Health Serv. Res. Policy. 2002;7:186–188. doi: 10.1258/135581902760082517. [DOI] [PubMed] [Google Scholar]
- 47.Mikati I., Benson A.F., Luben T.J., Sacks J.D., Richmond-Bryant J. Disparities in distribution of particulate matter emission sources by race and poverty status. Am. J. Public Health. 2018;108:480–485. doi: 10.2105/AJPH.2017.304297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Braveman P., Gruskin S. Poverty, equity, human rights and health. Bull. World Health Organ. 2003;81:539–545. [PMC free article] [PubMed] [Google Scholar]
- 49.Levesque J.F., Harris M.F., Russell G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thornton R.L., Glover C.M., Cené C.W., Glik D.C., Henderson J.A., Williams D.R. Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Aff. 2016;35:1416–1423. doi: 10.1377/hlthaff.2015.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Haluza D., Naszay M., Stockinger A., Jungwirth D. Prevailing opinions on connected health in Austria: Results from an online survey. Int. J. Environ. Res. Public Health. 2016;13:813. doi: 10.3390/ijerph13080813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gupta N. Population Ageing: Health and Social Care of Elderly Persons. Artha Vijnana. 2016;58:397–406. doi: 10.21648/arthavij/2016/v58/i4/153078. [DOI] [Google Scholar]
- 53.Adorno G., Fields N., Cronley C., Parekh R., Magruder K. Ageing in a low-density urban city: Transportation mobility as a social equity issue. Ageing Soc. 2018;38:296–320. doi: 10.1017/S0144686X16000994. [DOI] [Google Scholar]
- 54.Chomik R., Piggott J. Population Ageing and Social Security in Asia. Asian Econ. Policy Rev. 2015;10:199–222. doi: 10.1111/aepr.12098. [DOI] [Google Scholar]
- 55.Christensen H., Batterham P.J., O’Dea B. E-health interventions for suicide prevention. Int. J. Environ. Res. Public Health. 2014;11:8193–8212. doi: 10.3390/ijerph110808193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wood A., MacKay D., Fitzsimmons D., Derkenne R., Kirkham R., Boyle J.A., Connors C., Whitbread C., Welsh A., Brown A., et al. Primary Health Care for Aboriginal Australian Women in Remote Communities after a Pregnancy with Hyperglycaemia. Int. J. Environ. Res. Public Health. 2020;17:720. doi: 10.3390/ijerph17030720. [DOI] [PMC free article] [PubMed] [Google Scholar]