Abstract
Background
Calcium sodium phosphor-silicate material, a type of bio-glass was originally developed as an implant material to regenerate bone and recently adapted for use in oral care products (NovaMin Technology Inc.). Novamin is used for many dental problems like hypersensitivity, gingivitis, bleeding, non-carious lesions, carious lesions, whitening and is currently emerging as one of the treatment modality for the remineralization of the tooth. Since the prescription of these novel materials to the patients are based on cost effectiveness, efficacy and effectiveness, a clinician should make decision based on best available evidence. Hence, the objective of this review is to find out the current evidence available on the use of Novamin as an agent for remineralization.
Materials and methods
Relevant articles were searched and screened from several databases including PubMed, Cochrane review, Science Direct and trip which were published till 1988 to July 2017; The articles relevant to the objective of this review were included (RCT's) and articles out of interest of this review were excluded. The primary outcome for the chosen studies is the remineralization capacity of Novamin. Data extraction is done independently and jointly by 3 authors using data collection forms. Studies obtained were evaluated using the Cochrane Collaboration tools for accessing risk bias. The assessment of the quality of the evidence and the bias risk was obtained using the Grading of Recommendations Assessment Development and evaluation System.
Results
The articles from the database obtained for further review was N = 1. According to the study reviewed, the baseline comparisons using decalcification index obtained between Novamin study group (ReNew) and the control group (Crest) yield a P-value of 0.97 whereas after a 3 months interval follow up the value is 0.0403 suggesting there was a trend towards improvement in white spot lesions in the control group and at 6 months’ time point the p-value is 0.81 concluding that there are no significant difference of remineralization process obtained by using traditional toothpaste and Novamin.
Conclusion
Review shows that Novamin has significantly less clinical evidence to prove its effectiveness as a remineralization agent in treating both carious and non-carious lesion. Hence, better designed clinical trials should be carried out in the future before definitive recommendations can be made.
Keywords: Novamin, Calcium sodium phosphosilicate, Caries, Non-caries lesions, White spot lesions remineralization, Dentine remineralization, Tooth remineralization
1. Introduction
White Spot Lesions (WSLS) is defined as the early demineralization of the enamel at surface and subsurface, they are reversible and present on the smooth surfaces of teeth as a milky white opacity.1, 2, 3 Carious process involves a cycle of both reversible and irreversible stages.4Demineralization at subsurface level increases porosity that eventually changes the optical properties of the teeth further leading to cavitation if no treatment is undertaken.5
Enamel is crystalline in structure and the hardest known tissue in the body of human beings, composed of 96% hydroxyapatite, 3% water, minute amounts of proteins and lipids.6,7
Enamel must withstand a wide range of physical and chemical processes including compressive forces (up to about 700N), physiologic and pathologic wearing a way of tooth structure and importantly acidic environment due to the presence of bacterial plaque and diet. Surface of the HAP crystals at surface of enamel are ever dynamic due to their closeness to saliva and salivary plaque.8,9
Hence, the process of demineralization occurs at pH < 5.5 where dissolution of HAP as a result of acid secreted via the product of bacterial metabolism or by consumption of acidic food.10 If left for a prolonged period of time, excessive mineral loss leads to loss of enamel and further cavitation. The demineralization process continues till the pH rises causing remineralization to occur with deposition of calcium, phosphate, and fluoride ions (fluoroapatite), which are more resistant to crystals’ dissolution by organic acids as fluoroapatite crystals have advancing growth pattern resulting in a formation of large crystals with hexagonal outlines. Therefore, the best method for caries control is to focus on the ways to improve the remineralizing process with the help of remineralization products10
Dentistry in 21st century is rapidly changing with new innovations in technology and developing newer dental materials.11 These recent developments have changed the approach towards the management of dental problems. The evidence based dentistry is considered as best practice and the management of dental problems should be based on best available evidence. This approach will help to make informed decision in managing dental diseases.12
New improved materials capable of enamel remineralization even in low salivary calcium and phosphate ion concentrations is the need.13 Some of them are bio active glass (BAG), casein phosphpeptide-amorphous calcium phosphate (CPP-ACP). Several paste formulas are available, such as tooth mousse, topacal C-5 and MI paste plus.14
One such material recently developed is Novamin.15 It was developed and patented by NovaMin Technology, Inc., which was acquired by GlaxoSmithKline in May 2010.NovaMin is a bio active glass that is used in dental care products for remineralization of teeth, hypersensitivity, gingivitis, bleeding, non-carious lesions, carious lesions, whitening of the teeth. The effectiveness, efficacy and cost-effectiveness compared to other products are a need for its use and prescription by dentists to their patients for better outcome.16
NovaMin consists of calcium sodium phosphosilicate which is the active ingredient that enables it to bind to the surface of the tooth to initiate the process of remineralization on the enamel. This occurs instantly on contact with saliva or any aqueous media.17, 18, 19, 20
The objective of this study is to analyze the previous published RCT's articlesto find out an evidence of Novamin's use in remineralization of the tooth.
2. Materials and Methods
The guidelines followed in the publication of this study are the Preferred Items for Systematic reviews and Metas-Analyses (PRISMA) statement guidelines (www.prisma-statement.org).
2.1. Search strategy
For the preparation of this review, articles in English publication were searched, obtained and screened from several databases including PubMed, Cochrane review, Science Direct & Trip which were published till 1988 to July 2017 using the keywords “Novamin” or “calcium sodium phosphosilicate”, "caries", "non-caries lesions", "white spot lesions" "remineralization", "enamel remineralization", "dentine remineralization", "tooth remineralization", and "remineralization dental". The RCT articles relevant to the objective of this review were included and articles out of interest of this review were excluded. The primary outcome for the chosen studies was the remineralization capacity of Novamin. Additional automated searches were done to review some of the reference lists of the related papers and review articles associated with the need of this topic also searched for relevant information.
2.2. Study selection
Screening of the core databases were done by two reviewers separately after going through titles, their abstracts and keywords to omit out of interest records. Potentially relevant papers were then obtained. According to the predetermined inclusion criteria for the review, the reviewers examined every text report without any selection bias. Lack of supporting data to include a study or any other disagreement encountered during this stage was solved with opinion from a third reviewer. Studies excluded were then put into an excluded studies table with reasons for the same. The inclusion criteria were as followings:
Participants (P): Live human with evidence of demineralization (white spot lesions and/ or cavitation on teeth).
Intervention (I): Various types of Novamin containing vehicles such as toothpaste, mouth rinses or any prophylactic pastes without any limitation in their formulations, concentration, vehicles, method, duration and frequency of application.
Comparison (C): Negative control.
Outcomes (O): Remineralization of teeth is the primary outcome.
Studies (S): Prospective RCTs (randomised controlled trials).
2.3. Data extraction
The review authors manually extracted data independently from each included study and any disagreements in data extraction were resolved via discussion. For each selected RCTs the following data were check-listed based on guidelines used in the official statement from Consort 2010 for Group Randomised Trials. The datas extracted were:
2.4. Data synthesis and grading
The Cochrane Collaboration's tool to assess risk of bias, from the Cochrane Handbook for Systematic Reviews of Interventions 5th version (Higgins 2011) was used for assessing the risk of bias separately by 2 reviewers under 7 key domains namely:
-
•
Sequence generation and allocation concealment-Selection Bias
-
•
Blinding of participants and personnel comes under Performance bias
-
•
Bias due to blinding of outcome assessment that comes under Detection bias
-
•
Bias due to incomplete outcome data, called Attrition bias
-
•
Bias from selective outcome reporting which comes under Reporting bias
-
•
Bias that myoccur from source of funding, exposure to co intervention etc.
A table comprising the risk of bias will be used to record the scoring for risk of bias in each domain of the selected study with explanation for the decision. Scoring/Judgments assigned will be categorized as ‘Low risk of bias', ‘High risk of bias' or ‘Unclear risk of bias'. Results will then plotted in graphs. As differences in opinion will be resolved with review from third author until consensus reached (Table 2).
Table 2.
Risk of bias.
| Bias | Risk |
|---|---|
| Selection bias | |
| λ sequence generation | Unclear |
| λ allocation concealment | Unclear |
| Performance bias (blinding of participants and personnel) | Unclear |
| Detection bias (blinding of outcome assessment) | Low |
| Attrition bias (incomplete outcome data) | Unclear |
| Reporting bias (selective outcome reporting) | Low |
| Additional bias (e.g. source of funding, exposure to co interventions). | High - use of fluoridated toothpaste |
3. Results
3.1. Study selection
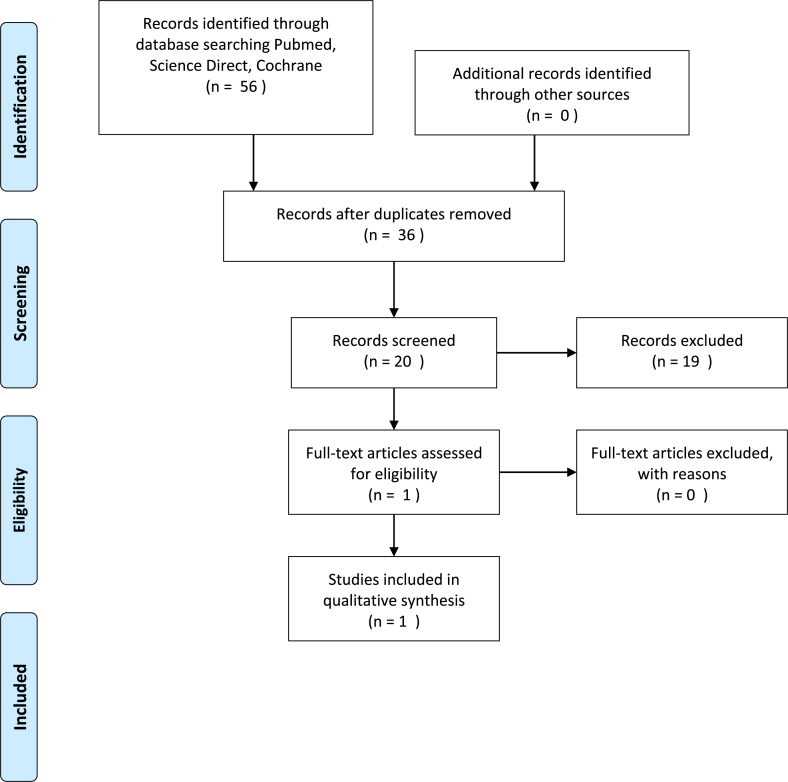
Initial records were identified and obtained from various databases like PubMed, Science Direct, Trips and Cochrane Review. Following the initial search, N = 56 records were obtained. For the construction of this systematic review, N = 36 records were removed after the screening the titles, keywords and abstracts for duplication or irrelevancy. The remaining N = 20 articles underwent full text assessment and as a result, according the predetermined eligibility criteria, N = 19 were excluded. To show the process of study selection, a flowchart is shown in Fig. 1. Finally, only one randomised trial was included in this qualitative analysis.19
Fig. 1.
PRISMA Flow Chart for the inclusion and exclusion of the articles that aims to select the RCT's related to Novamin and Remineralization.
3.2. Description of the included study
Table 1 shows detailed data extracted from the included study. The study selected is a RCT comparing Novamin in the form of Renew with a control group. Novamin was prescribed by researchers to be self-administered in the concentration of 5% to a total of N = 48 patients initially. The patients were followed up twice at the third and sixth month after the baseline appointment. During the follow up process, pictures were taken and several clinical procedures were carried out such as measurement of decalcification index, modified gingival and plaque index and plaque bacterial counts19(see Table 1).
Table 1.
Characteristics of the included study.
| Authors | Hoffman et al. |
|---|---|
| Test/Control Participants | 24/24 |
| Follow up | Third and sixth month |
| Test vs control | ReNew & Crest |
| Assessment method | Decalcification index |
| Start test/control (SD) | 0.34/0.4 |
| End test/control (SD) | 0.37/0.47 |
| Start test/control(p value) | 0.97 |
| End test/control(p value) | 0.81 |
3.3. Summary of included study
3.4. Primary study outcome
According to the study reviewed, the baseline comparisons using decalcification index obtained between Novamin study group (ReNew) and the control group (Crest) yield a p-value of 0.97 whereas after a 3 months interval follow up the value is 0.0403 suggesting there was a trend towards improvement in white spot lesions in the control group and at 6 months’ time point the p- value is 0.81 concluding that there are no significant difference of remineralization process obtained by using traditional toothpaste and Novamin.The study selected also shows that there is no favourable difference in the plaque and gingival health after 6 months.
3.5. Secondary study outcome
The only reported secondary outcome in this RCT is the possibility of allergy development in one of the patient.19
3.6. Risk of bias
As a result of the risk of bias assessment, it can be concluded that this study has an unclear risk of bias (Table 2).
3.7. Level of Evidence
Although the included study is a randomised controlled clinical trial, which is a high level of evidence on the herarchy table but to give concrete recommendations to policy makes and healthcare workers need further minimal bias studies. Therefore, the level of evidenceavailable to frame a recommendation is low.
4. Discussion
4.1. Enamel structure
Enamel is known to be the most mineralized and the hardest tissue component in the human body forming a delicate and thin but tough calcified translucent layer encasing the entire coronal structure. Characteristics vary between every tooth and every person, in terms of thickness and strength. Thickness determines the mineral content and quality of tooth and variation in color ranging from yellow to grayish white may seen as well.21, 22, 23, 24
Enamel does not receive any blood nor nerve supply. Hardness of enamel is attributed to the primary inorganic ions of phosphate and calcium and phosphate which form strong hydroxyapatite crystals and make up 95–98% volume. Enamel is an organized structure formed of inorganic, organic and water components. While the organic content of enamel makes up 1-2%, majority of which is made of enamel-specific proteins also called ‘Enamelins’. They are proteins with affinity for hydroxyapatite and end up binding with them.
Enamel is formed from ameloblasts which are primarily epithelial cells, they develop just before tooth eruption when ameloblasts are broken down losing its ability to regenerate. It loses its ability to self-heal by remineralization during injury or trauma. Complete tooth mineralization is incomplete at time of eruption, salivary calcium, phosphorus and fluoride help achieve complete mineralization by forming a 10–100 μm layer of enamel.
Enamel substructure has several carbonated hydroxyapatite crystals as long, thin structures called rods, they are 4 μm–8 μm in diameter. Arranged at right angles from DEJ towards surface of tooth. The number of rods may be vary in number from 5 to 12 million in a lower lateral incisor and upper first molar. Every rod is covered by protein matrix of enamelin which constitutes a rod sheath. Some minute voids remain which do not contain any crystals between rods called as pores, giving enamel its permeability. This favors the fluid movement and diffusion but causes variations in density and hardness of tooth, creating spots that are more likely to be demineralized.41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51
4.2. Concept of remineralization
In the oral cavity there is a constant cycle of remineralization followed by demineralization. If the balance is altered, advance in demineralization will lead to degradation of tooth structure. The ratio of demineralization and remineralization must be balanced as it determines the hardness and strength of the tooth structure.24 Demineralization happens when the oral environment is under saturated with mineral ions, at a low pH relative to the mineral content of a tooth.25 The carbonated apatite of enamel crystals is dissolved by organic acids such as lactic and acetic acids produced from dietary carbohydrates by plaque bacteria. Remineralization on the other hand is a natural process to restore minerals by addition of mineral ions to the lattice work structure of hydroxyapatite.25
White spot lesions on an intact surface zone while subsurface is affected are a classic clinical sign of demineralization. White spot development helps easy identification of demineralized areas, whereas remineralized areas are not as easily observed on clinical examination.
Remineralization replaces fluoroapatite crystals in areas which have lost calcium, phosphate and fluoride ions. The new replaced crystals are larger in size and much more resistant to acid dissolution than their predecessors, thereby portray higher resistance to breakdown when faced with organic acids from diet.26
Two key players in remineralization are saliva and fluoride. Using remineralization agents to attain a higher plaque pH than the critical pH is the best approach for caries management. Commercially a variety of remineralization agents like Bio active glass (BAG), casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) fluorides, ozone, xylitol, etc are available.26
The following conditions occur simultaneously for enamel remineralization:
-
-
The saliva must be saturated with minerals.
-
-
A carbonic acid molecule reaction is mandatory.
-
-
Close proximity of the carbonic acid molecule to a mineral molecule.
All of the above must occur close to a demineralized spot in the latticework of hydroxyapatite (HA). A clean tooth surface is required to access the mineral-deficient spot.27 Conversion of carbonic acid into water and carbon dioxide should occur before any of these circumstances undergoes alterations.28, 29, 30
4.3. Novamin effects on enamel
NovaMin is composed primarily of calcium, sodium, phosphorus and silica. The byproduct released is hydroxyl-carbonate apatite (HCA) which is crystalline in nature, has a structural resemblance similar to the mineral in teeth. Nanohydroxyapatite (NHA) has proven to be highly biocompatible due to affinity for tooth enamel. They also have a resemblance to apatite crystals in tooth enamel. As a compounding factor in remineralizing agents like NovaMin it helps to achieve the objective to preserve tooth in a conservative manner.31
4.3.1. Mechanism of action
Novamin is capable of sodium ion diffusion rapidly on contact with any aqueous media. It causes a calcium and phosphate release along with rise in pH.32 They act as reservoirs for calcium and phosphate ions which may be released over several days. Finally, the calcium-phosphate complexes are capable of crystallizing into hydroxycarbonate apatite.33
4.3.2. Enamel remineralization
NovaMin on contact with an aqueous medium like saliva shows that its most active component calcium sodium phosphor silicate has a tendency to bind to the tooth surface therefore initiating remineralization process on the tooth enamel.34
This is done by providing the tooth structure with silica, calcium, phosphorous and sodium ions. Sodium ions present in the formulation of calcium sodium phosphosilicate bioactive glass are replaced with hydrogen ions and, thus, the pH increases.35,36 Subsequently, calcium and phosphate ions deposit and form a superficial layer saturated with calcium phosphate on the tooth surface. This ionic reservoir can inhibit the process of demineralization and enhance remineralization by protecting the enamel against cariogenic conditions. Following the immersion of calcium sodium phosphosilicate in the saliva or body fluid analogs, Hydrogen cations (H+ or H3O+) are interchanged with seconds to Na + ions are exchanged with hydrogen cations within a minute, also termed as a rapid ion exchange leading to release of calcium(Ca2+) and phosphate (PO4 3-) from the particles.37,38 Subsequently, a local transient rise in the pH results in the release of phosphate ions along with Ca ions present in saliva and within particles, and the formation of an amorphous layer of calcium phosphate (CaO–P2O5) on the tooth surfaces as well as within the demineralized dentin.39 Simultaneously, with the continuation of these reactions and the deposition of Ca–P compounds, this layer crystallizes inside the HA, forming a structure that chemically and structurally resembles biological apatite. The interaction between the HA layer and calcium sodium phosphosilicate causes physical occlusion of dentinal tubules due to formation of reminerization deposits.55,56 Calcium sodium phosphosilicate also induces chemical reactions to enhance the formation of HA. This may prevent demineralization of tooth structure and enhance remineralization.40
4.3.3. Sensitivity
The most notable effect of Novamin is on dentinal sensitivity. Several studies 21, 22, 23, 24 have explained the before and after effects of treatment by showing open dentinal tubules before and closed occluded tubules after sensitivity treatment. There is a lack of scientific evidence to prove the long term effects of sensitivity treatments and their added benefits like tooth whitening and remineralizing.52,53,54
4.3.4. Erosion
As the acidic conditions of the oral cavity increases it is subjected to erosion, these effects can be subdued by precipitation.57 A large number of consumables used on a day to day basis with a low Ph cause damage to the tooth surface. These include aerated beverages and acidic drinks which overcome the natural buffering capacity of saliva causing loss of tooth minerals increasing the vulnerability of tooth to caries.58
An efficient remineralization agent like NovaMin should enable to fill up minute irregularities on enamel surface and thereby preventing erosion from acidic foods and beverages.59 By doing so the overall appearance and esthetics of the tooth like luster and gloss may enhance. Eroded surface defects can be remineralized by providing calcium and phosphate and thereby reduce the mineral loss.60
According to this systematic review there is no statistically significant different results obtained between the Novamin and the control group even though initially a P = 0.0403 suggesting of statistically significant value were recorded at three-month point. However, this result is based on only one clinical trial. In addition, the RCT selected also presented with some drawbacks such as inaccuracy in assessment of WSL due to the presence of gingival hyperplasia and plaque in some patient, dependence on patients’ compliance and finally the subjectivity of decalcification index on measuring WSL.
To conclude, this systematic review has its own sets of limitation. Firstly, the articles were searched in English which might have predisposed to selection bias. Second, there was only one available RCT contributing to low value power for this review due to the limitation of an extremely low amount of extracted data. Third the number of study was relatively low. Finally, within the selected article presence of a few unclear biases that have further reduced the eligibility of this review.
4.4. Quality of evidence
Although the study included is a randomised controlled clinical trial, the evidence is regarded as high-quality evidence but the factors like selection bias, performance bias and attrition bias the level of evidence of the study included is graded as low. Therefore, further more clinical studies with minimal bias are required to propose recommendation to interested parties.
5. Conclusion
According to this review, the evidence states that there is no significant scientific data to support the remineralizing capacity of Novamin when compared to traditional toothpaste.
Hence, before any definitive recommendation can be made in the future more number of studies with scientific evidence should be carried out provided it is done by concealing the allocation, avoid bias by following a blind study design for participants and the personnel assessing the outcome. Most appropriate analysis and strict criteria for eligibility should be determined. All compounding factors which cause a qualitative analysis with less value such as poor methodology selection, disparate measurements and different materials should be avoided.
Declaration of competing interest
There are no funding support for this systematic review and we declare there are no conflict of interest for this systematic review.
Acknowledgement
We would like to thank Miss KIRTHANA Muthu, an undergraduate student for initial input.
Contributor Information
Shahnawaz Khijmatgar, Email: khijmatgar@gmail.com.
Upasana Reddy, Email: upasana.reddy.88@gmail.com.
References
- 1.López López E.A., Dominguez J.A., Gomes G.M. Effect of conditioning protocols and ultrasonic application of an infiltrant resin in white spot lesions. Braz Dent J. 2019 Feb;30(1):58–65. doi: 10.1590/0103-6440201902329. [DOI] [PubMed] [Google Scholar]
- 2.Bishara S.E., Ostby A.W. White spot lesions: formation, prevention, and treatment. InSeminars Orthod. 2008 Sep 1;14(3):174–182. WB Saunders. [Google Scholar]
- 3.Abdullah Z., John J. Minimally invasive treatment of white spot lesions--A systematic review. Oral Health Prev Dent. 2016 May 1;14(3) doi: 10.3290/j.ohpd.a35745. [DOI] [PubMed] [Google Scholar]
- 4.Nuca C., Amariei C., Ungureanu L., Barascu L. The remineralization of the artificial “white spot” lesions–experimental research. OHDMBSC. 2002;(2):48. [Google Scholar]
- 5.Neel E.A., Aljabo A., Strange A. Demineralization–remineralization dynamics in teeth and bone. Int J Nanomed. 2016;11:4743. doi: 10.2147/IJN.S107624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGuire J.D., Walker M.P., Dusevich V., Wang Y., Gorski J.P. Enamel organic matrix: potential structural role in enamel and relationship to residual basement membrane constituents at the dentin enamel junction. Connect Tissue Res. 2014 Aug 1;55(sup1):33–37. doi: 10.3109/03008207.2014.923883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lacruz R.S., Habelitz S., Wright J.T., Paine M.L. Dental enamel formation and implications for oral health and disease. Physiol Rev. 2017 May 3;97(3):939–993. doi: 10.1152/physrev.00030.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith C.E. Cellular and chemical events during enamel maturation. Crit Rev Oral Biol Med. 1998 Apr;9(2):128–161. doi: 10.1177/10454411980090020101. [DOI] [PubMed] [Google Scholar]
- 9.Alkattan R., Lippert F., Tang Q., Eckert G.J., Ando M. The influence of hardness and chemical composition on enamel demineralization and subsequent remineralization. J Dent. 2018 Aug 1;75:34–40. doi: 10.1016/j.jdent.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Kidd E.A., Fejerskov O. Oxford University Press; 2016 Jun 16. Essentials of Dental Caries. [Google Scholar]
- 11.Rekow E.D. High-technology innovations--and limitations--for restorative dentistry. Dent Clin. 1993 Jul;37(3):513–524. [PubMed] [Google Scholar]
- 12.Toledano M., Osorio R. InBiomaterials for Oral and Craniomaxillofacial Applications. Vol. 17. Karger Publishers; 2015. New advanced materials for high performance at the resin-dentine interface; pp. 39–48. [DOI] [PubMed] [Google Scholar]
- 13.Philip N. State of the art enamel remineralization systems: the next frontier in caries management. Caries Res. 2019;53(3):284–295. doi: 10.1159/000493031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang G.J., Roloff-Chiang B., Mills B.E. Effectiveness of MI Paste Plus and PreviDent fluoride varnish for treatment of white spot lesions: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2013 Jan 1;143(1):31–41. doi: 10.1016/j.ajodo.2012.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alexandrino L.D., Alencar C.D., Silveira A.D., Alves E.B., Silva C.M. Randomized clinical trial of the effect of NovaMin and CPP-ACPF in combination with dental bleaching. J Appl Oral Sci. 2017 Jun;25(3):335–340. doi: 10.1590/1678-7757-2016-0408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baino F., Hamzehlou S., Kargozar S. Bioactive glasses: where are we and where are we going? J Funct Biomater. 2018 Mar;9(1):25. doi: 10.3390/jfb9010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Golpayegani M.V., Sohrabi A., Biria M., Ansari G. Remineralization effect of topical NovaMin versus sodium fluoride (1.1%) on caries-like lesions in permanent teeth. J Dent. 2012;9(1):68. [PMC free article] [PubMed] [Google Scholar]
- 18.Mason S, Hughes N, Sufi F. RESEARCH UPDATE SENSODYNE® RAPID RELIEF.
- 19.Hoffman D.A., Clark A.E., Rody W.J., McGorray S.P., Wheeler T.T. A prospective randomized clinical trial into the capacity of a toothpaste containing NovaMin to prevent white spot lesions and gingivitis during orthodontic treatment. Prog Orthod. 2015 Dec;16(1):25. doi: 10.1186/s40510-015-0095-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Acharya A.B., Surve S.M., Thakur S.L. A clinical study of the effect of calcium sodium phosphosilicate on dentin hypersensitivity. J. Clin. Exp. Dent. 2013 Feb;5(1):e18. doi: 10.4317/jced.50955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al‐Bakri I.A., Harty D., Al‐Omari W.M., Swain M.V., Chrzanowski W., Ellakwa A. Surface characteristics and microbial adherence ability of modified polymethylmethacrylate by fluoridated glass fillers. Aust Dent J. 2014 Dec;59(4):482–489. doi: 10.1111/adj.12218. [DOI] [PubMed] [Google Scholar]
- 22.Aladağ A., Elter B., Çömlekoğlu E. Effect of different cleaning regimens on the adhesion of resin to saliva‐contaminated ceramics. J Prosthodont. 2015 Feb;24(2):136–145. doi: 10.1111/jopr.12170. [DOI] [PubMed] [Google Scholar]
- 23.Amaechi B.T., Mathews S.M., Mensinkai P.K. Effect of theobromine-containing toothpaste on dentin tubule occlusion in situ. Clin Oral Invest. 2015 Jan 1;19(1):109–116. doi: 10.1007/s00784-014-1226-1. [DOI] [PubMed] [Google Scholar]
- 24.Bajwa N.K., Pathak A. Change in surface roughness of esthetic restorative materials after exposure to different immersion regimes in a cola drink. ISRN Dent. 2014 Mar 23:2014. doi: 10.1155/2014/353926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bakry A.S., Tamura Y., Otsuki M., Kasugai S., Ohya K., Tagami J. Cytotoxicity of 45S5 bioglass paste used for dentine hypersensitivity treatment. J Dent. 2011 Sep 1;39(9):599–603. doi: 10.1016/j.jdent.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 26.Balakrishnan A., Jonathan R., Benin P., Kuumar A. Evaluation to determine the caries remineralization potential of three dentifrices: an in vitro study. J Conserv Dent: J Comput Dynam. 2013 Jul;16(4):375. doi: 10.4103/0972-0707.114347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ballard R.W., Hagan J.L., Phaup A.N., Sarkar N., Townsend J.A., Armbruster P.C. Evaluation of 3 commercially available materials for resolution of white spot lesions. Am J Orthod Dentofacial Orthop. 2013 Apr 1;143(4):S78–S84. doi: 10.1016/j.ajodo.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 28.Bhatia S., Krishnaswamy M.M. Effect of two different dentin desensitizers on shear bond strength of two different bonding agents to dentin: an in vitro study. Indian J Dent Res. 2012 Nov 1;23(6):703. doi: 10.4103/0970-9290.111242. [DOI] [PubMed] [Google Scholar]
- 29.Bichu Y.M., Kamat N., Chandra P.K., Kapoor A., Aravind N.K. Prevention of enamel demineralization during orthodontic treatment: an in vitro comparative study. Orthod - Art Pract Dentofac Enhanc. 2013 Mar 1;14(1) doi: 10.11607/ortho.870. [DOI] [PubMed] [Google Scholar]
- 30.Burwell A.K., Litkowski L.J., Greenspan D.C. Calcium sodium phosphosilicate (NovaMin®): remineralization potential. Adv Dent Res. 2009 Aug;21(1):35–39. doi: 10.1177/0895937409335621. [DOI] [PubMed] [Google Scholar]
- 31.Burwell A., Jennings D., Greenspan D.C. NovaMin and dentin hypersensitivity--in vitro evidence of efficacy. J Clin Dent. 2010;21(3):66–71. [PubMed] [Google Scholar]
- 32.Cajazeira M.R., De T.S., Maia L.C. Influence of the operatory field isolation technique on tooth-colored direct dental restorations. Am J Dent. 2014 Jun;27(3):155–159. [PubMed] [Google Scholar]
- 33.Christie J.K., Pedone A., Menziani M.C., Tilocca A. Fluorine environment in bioactive glasses: ab initio molecular dynamics simulations. J Phys Chem B. 2011 Mar 10;115(9):2038–2045. doi: 10.1021/jp110788h. [DOI] [PubMed] [Google Scholar]
- 34.Mahesh D.R., Komali G., Jayanthi K., Dinesh D., Saikavitha T.V. Evaluation of salivary flow rate, pH and buffer in pre, post & post-menopausal women on HRT. J Clin Diagn Res: J Clin Diagn Res. 2014 Feb;8(2):233. doi: 10.7860/JCDR/2014/8158.4067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Araújo D.F., Chaves L.P., Júnior O.B. Influence of 2% chlorhexidine digluconate on bond strength of a glass-fibre post luted with resin or glass-ionomer based cement. J Dent. 2014 Jun 1;42(6):735–741. doi: 10.1016/j.jdent.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 36.Diamanti I., Koletsi-Kounari H., Mamai-Homata E., Vougiouklakis G. Effect of fluoride and of calcium sodium phosphosilicate toothpastes on pre-softened dentin demineralization and remineralization in vitro. J Dent. 2010 Aug 1;38(8):671–677. doi: 10.1016/j.jdent.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 37.Diamanti I., Koletsi-Kounari H., Mamai-Homata E., Vougiouklakis G. In vitro evaluation of fluoride and calcium sodium phosphosilicate toothpastes, on root dentine caries lesions. J Dent. 2011 Sep 1;39(9):619–628. doi: 10.1016/j.jdent.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 38.Du Q.M., Bian Z., Jiang H. Clinical evaluation of a dentifrice containing calcium sodium phosphosilicate (novamin) for the treatment of dentin hypersensitivity. Am J Dent. 2008 Aug;21(4):210–214. [PubMed] [Google Scholar]
- 39.Earl J.S., Leary R.K., Muller K.H., Langford R.M., Greenspan D.C. Physical and chemical characterization of dentin surface following treatment with NovaMin technology. J Clin Dent. 2011;22(3):62–67. [PubMed] [Google Scholar]
- 40.Earl J.S., Topping N., Elle J., Langford R.M., Greenspan D.C. Physical and chemical characterization of the surface layers formed on dentin following treatment with a fluoridated toothpaste containing NovaMin. J Clin Dent. 2011;22(3):68–73. [PubMed] [Google Scholar]
- 41.Fan Y., Townsend J., Wang Y. Formulation and characterization of antibacterial fluoride-releasing sealants. Pediatr Dent. 2013 Jan 15;35(1) 13E-8E. [PMC free article] [PubMed] [Google Scholar]
- 42.Farmakis E.T., Beer F., Kozyrakis K., Pantazis N., Moritz A. The influence of different power settings of Nd: YAG laser irradiation, bioglass and combination to the occlusion of dentinal tubules. Photomed Laser Surg. 2013 Feb 1;31(2):54–58. doi: 10.1089/pho.2012.3333. [DOI] [PubMed] [Google Scholar]
- 43.Farmakis E.T., Kozyrakis K., Khabbaz M.G., Schoop U., Beer F., Moritz A. In vitro evaluation of dentin tubule occlusion by Denshield and Neodymium-doped yttrium-aluminum-garnet laser irradiation. J Endod. 2012 May 1;38(5):662–666. doi: 10.1016/j.joen.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 44.Farmer S.N., Ludlow S.W., Donaldson M.E., Tantbirojn D., Versluis A. Microleakage of composite and two types of glass ionomer restorations with saliva contamination at different steps. Pediatr Dent. 2014 Jan 15;36(1):14–17. [PubMed] [Google Scholar]
- 45.Galo R., Contente M.M., Borsatto M.C. Wear of two pit and fissure sealants in contact with primary teeth. Eur J Dermatol. 2014 Apr;8:241–248. doi: 10.4103/1305-7456.130619. 02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gendreau L., Barlow A.P., Mason S.C. Overview of the clinical evidence for the use of NovaMin in providing relief from the pain of dentin hypersensitivity. J Clin Dent. 2011;22(3):90–95. [PubMed] [Google Scholar]
- 47.Gjorgievska E.S., Nicholson J.W. A preliminary study of enamel remineralization by dentifrices based on RECALDENTTM (CPP-ACP) and Novamin®(calcium-sodium-phosphosilicate) Acta Odontol Latinoam. 2010 Dec;23(3):234–239. [PubMed] [Google Scholar]
- 48.Gjorgievska E., Nicholson J.W. Prevention of enamel demineralization after tooth bleaching by bioactive glass incorporated into toothpaste. Aust Dent J. 2011 Jun;56(2):193–200. doi: 10.1111/j.1834-7819.2011.01323.x. [DOI] [PubMed] [Google Scholar]
- 49.Goldstep F. Proactive intervention dentistry: a model for oral care through life. Comp Cont Educ Dent. 2012 Jun;33(6):394–396. [PubMed] [Google Scholar]
- 50.Goswami M., Saha S., Chaitra T.R. Latest developments in non-fluoridated remineralizing technologies. J Indian Soc Pedod Prev Dent. 2012 Jan 1;30(1):2. doi: 10.4103/0970-4388.95561. [DOI] [PubMed] [Google Scholar]
- 51.Graumann S.J., Sensat M.L., Stoltenberg J.L. Air polishing: a review of current literature. Am Dent Hygienists' Assoc. 2013 Aug 1;87(4):173–180. [PubMed] [Google Scholar]
- 52.Greenspan D.C. NovaMin® and tooth sensitivity—an overview. J Clin Dent. 2010;21(3):61. [PubMed] [Google Scholar]
- 53.Han L., Okiji T. Effects of a novel fluoride-containing aluminocalciumsilicate-based tooth coating material (Nanoseal) on enamel and dentin. Am J Dent. 2013 Aug;26(4):191–195. [PubMed] [Google Scholar]
- 54.Joshi S., Gowda A.S., Joshi C. Comparative evaluation of NovaMin desensitizer and Gluma desensitizer on dentinal tubule occlusion: a scanning electron microscopic study. J periodont Implant Sci. 2013 Dec 1;43(6):269–275. doi: 10.5051/jpis.2013.43.6.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kakodkar G., Lavania A., De Ataide I.D. An in vitro SEM study on the effect of bleaching gel enriched with NovaMin on whitening of teeth and dentinal tubule occlusion. J Clin Diagn Res: J Clin Diagn Res. 2013 Dec;7(12):3032. doi: 10.7860/JCDR/2013/5831.3841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.LaTorre G., Greenspan D.C. The role of ionic release from NovaMin®(calcium sodium phosphosilicate) in tubule occlusion: an exploratory in vitro study using radio-labeled isotopes. J Clin Dent. 2010;21(3):72. [PubMed] [Google Scholar]
- 57.Layer T.M. Development of a fluoridated, daily-use toothpaste containing NovaMin technology for the treatment of dentin hypersensitivity. J Clin Dent. 2011;22(3):59–61. [PubMed] [Google Scholar]
- 58.Litkowski L., Greenspan D.C. A clinical study of the effect of calcium sodium phosphosilicate on dentin hypersensitivity—proof of principle. J Clin Dent. 2010;21(3):77. [PubMed] [Google Scholar]
- 59.Ludlow S.W., Farmer S.N., Donaldson M.E., Tantbirojn D., Versluis A. Microleakage of resin-modified glass ionomer restorations with selective enamel etching. Operat Dent. 2014 Jul;39(4):E154–E159. doi: 10.2341/13-290-L. [DOI] [PubMed] [Google Scholar]
- 60.Manton D.J. Dental caries: where to from here? Ann Roy Australas Coll Dent Surg. 2008 Jun;19:73. [PubMed] [Google Scholar]