Around 25% of thoracic aortic aneurysms and dissections (TAAD) result from single gene mutations1, including PRKG12, 3. Current AHA/ACC guidelines provide recommendations for other mutations, such as FBN1, TGFßR1, and MYH114, 5, but not specifically PRKG1. We present a patient with a known PRKG1 mutation and a story about her family (Video).
CLINICAL SUMMARY
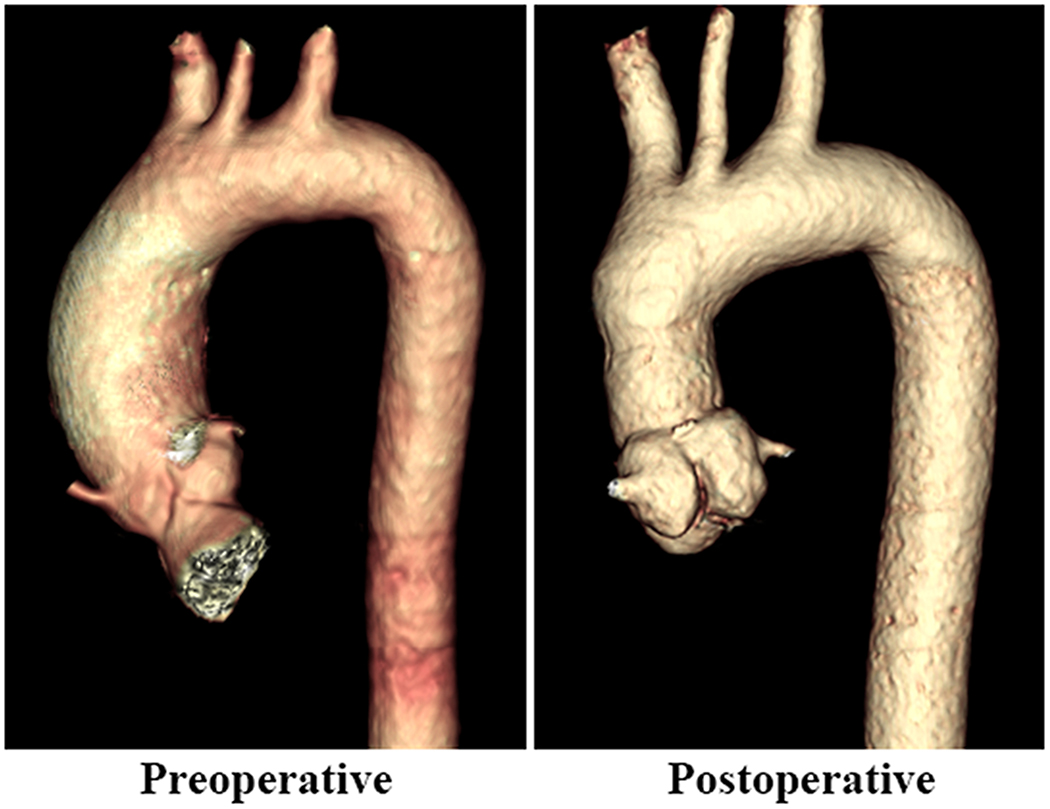
A 47-year-old female with a strong family history of TAAD was found to have a PRKG1 mutation (p.R192Q). Her PRKG1 positive brother suffered an aortic dissection at the age of 35, her niece died at 16-years-old from an aortic dissection, one brother died at 16-days-old from a congenital heart defect (3-chambered heart), another brother was stillborn at seven months, her four daughters: two are negative carriers and two have the PRKG1 mutation, and one granddaughter has the PRGK1 mutation. Both affected daughters (diagnosed at 24- and 22-years-old) were found to have tricuspid aortic valves, normal ejection fractions, and the oldest had a 29mm aortic root and other had a 23-25mm aortic root and 29mm ascending aorta. The patient had had an echocardiogram in her thirties, when her brother suffered an aortic dissection, and all measurements were within normal range. Following positive genetic testing, an echocardiogram demonstrated a trileaflet aortic valve with trace aortic insufficiency and a left ventricular ejection fraction of 62% and a CT angiogram revealed a 37mm aortic root and 38mm ascending aorta (Figure 1).
Figure 1:
Preoperative and 3-month post valve-sparing aortic root and ascending aorta replacement computed tomography angiography in a patient with a PRKG1 mutation.
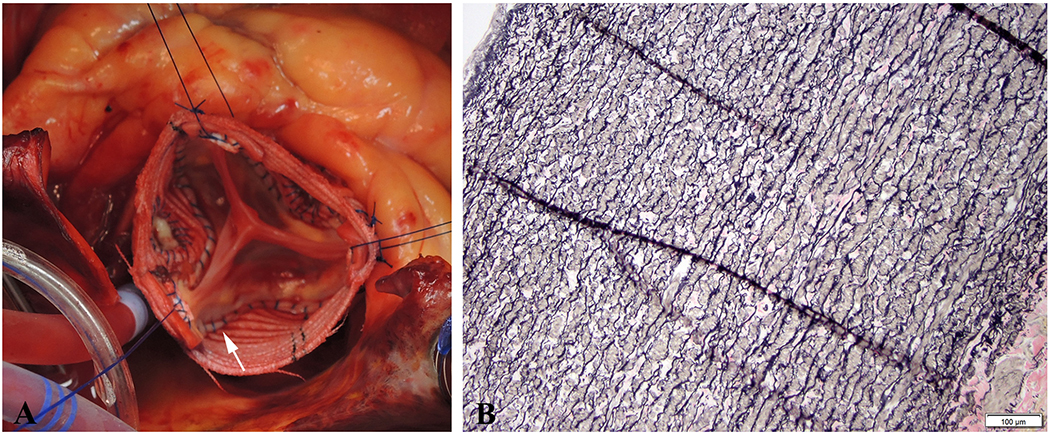
The patient suffered significant anxiety regarding possible aortic dissection and eventually underwent a valve-sparing aortic root replacement (VSARR, David V procedure–Stanford modification, 32 and 24mm Dacron grafts) and ascending aorta replacement-as much as possible without circulatory arrest. The distal anastomosis was completed without surgical adjuncts (Figure 2B). Most notably, the wall of the proximal ascending aorta and aortic root was exceptionally thin (1mm, Figure 2A), almost as thin as the outer layer of a dissected aorta. The right ventricular outflow tract could be visualized through the right coronary sinus. The distal ascending aortic wall was about 2mm. The aorta was very fragile, and noted to be easy to tear during cannulation of the aortic arch. We used a single 3-0 ethibond purse-string without pledgets for aortic cannulation at the mid arch and the cannulation site was re-enforced with 5-0 prolene in a figure-eight fashion after decannulation. Histology showed thin aortic media without typical changes as seen in patients with Marfan or Loeys-Dietz syndrome (Figure 2C, 2D). She has been doing well for >1 year with a competent aortic valve since her operation (Figure 1). Interestingly but sadly, on her post-operative day 4, her other 30-year-old cousin with the same PRKG1 mutation suffered an acute type A aortic dissection with mesenteric malperfusion and necrotic bowel.
Figure 2:
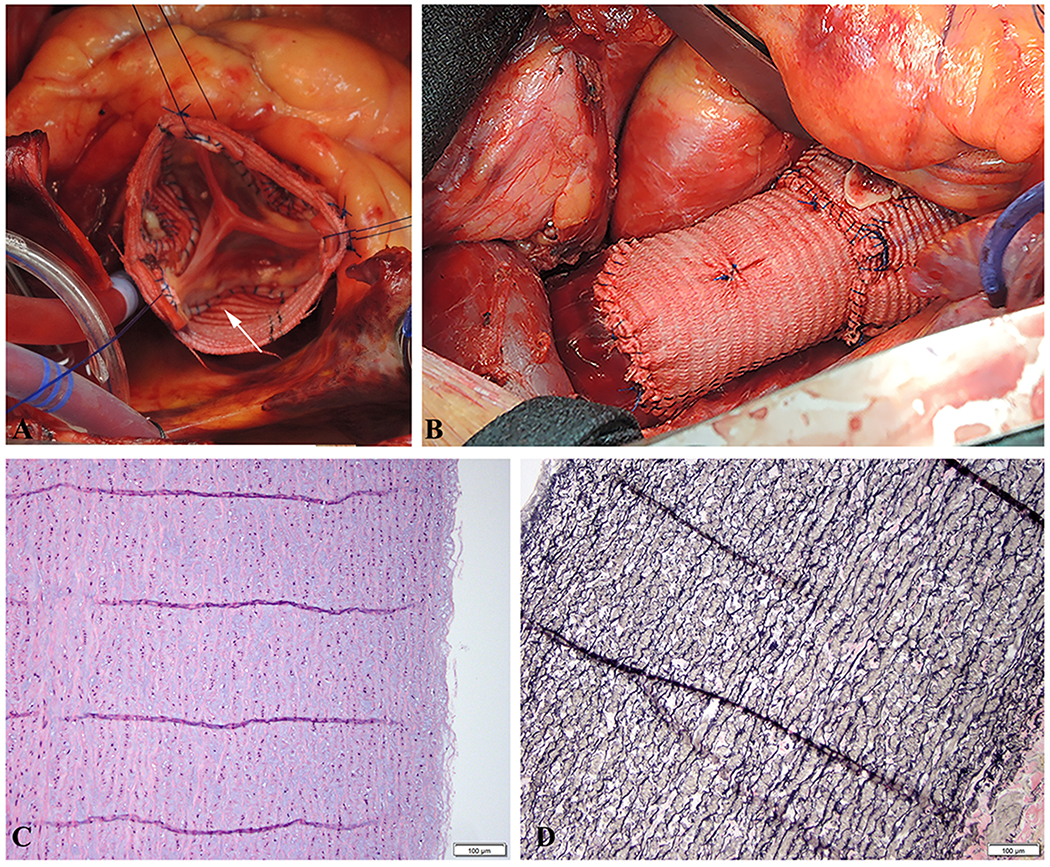
A. Valve-sparing root replacement (David procedure) in a PRKG1 affected patient with a thin and fragile aortic wall. Suture for aortic valve implantation was meticulously placed through the aortic annulus, which was strong enough to hold the suture. The arrow indicates the extremely thin remnant of the aortic sinus wall. B. Completion of the repair showing the distal anastomosis of the Dacron graft to the ascending aorta. C. Moderate, multifocal intralamellar mucoid extracellular matrix accumulation (MEMA-I) without altering the arrangement of the lamellar units. Medial fibrosis and inflammation were also absent. Thus, overall the media displayed mild-to-moderate medial degeneration. Additionally, there was no evidence of aortitis or dissection. (H&E stain). D. The aortic media also displayed moderate, multifocal elastica fragmentation, plus multifocal mild-to-moderate elastic fiber thinning. However, there was no elastic fiber disorganization, no smooth muscle loss or disorganization, and no laminar medial collapse. (EVG stain).
DISCUSSION
Although mutation in the PRKG1 gene has been linked to familial thoracic aortic aneurysms and dissection2, 3, there is no evidence to guide the clinical management of affected patients, yielding clinical decision making difficult. PRKG1 encodes a type 1 cGMP-dependent kinase involved in smooth muscle relaxation and contraction2, 3 crucial in maintaining the integrity of the thoracic aortic wall throughout life2. Patients with a PRKG1 mutation present with aortic dissection relatively early in life, around 31 years (range 17-51 years; n=31)2. In the study by Guo et al.2, an acute type A aortic dissection occurred at an aortic root diameter of 37mm and ascending aorta diameter of 43mm in a 27-year-old affected female patient. Gago-Diaz et al.3 reported an affected female patient who suffered a type B dissection at the age of 41 and a type A dissection at the age of 43, prior to dissection the aortic root measured 44mm and the ascending aorta measured 37mm. Patients with the PRKG1 mutation are predisposed to an aggressive form of thoracic aortic disease; suffering aortic events at relatively young ages and small aortic diameters2, 3. Therefore, prophylactic aortic repair should be considered at smaller aortic diameters in affected patients, but specific indications for prophylactic repair remain undecided. Although mutations in PRKG1 is not the most common cause of genetic TAAD, guidelines regarding this specific presentation are warranted.
In the case presented, the intraoperative finding of an extremely thin aortic wall and strong family history of aortic dissections and death support early aggressive management of the aorta in patients with pathogenic PRKG1 variants, and if possible, a VSARR should be performed. The patient’s affected daughters (now 26- and 24-years-old), with normal aortic root and ascending aorta dimensions continue to be monitored with annual echocardiogram, but the question of when to consider prophylactic aortic repair remains.
Supplementary Material
Discussion of prophylactic management of the aortic root and ascending aorta in patients with a known PRKG1 mutation.
CENTRAL PICTURE.
Extremely thin remnant of the aortic sinus wall and mild diffuse elastica fragmentation.
CENTRAL MESSAGE.
Aggressive prophylactic replacement of the proximal aorta should be considered for patients with a pathogenic PRKG1 mutation and family history of thoracic aortic dissection.
Footnotes
Conflict of Interest: No conflicts of interest to disclose.
REFERENCES
- 1.Milewicz D, Hostetler E, Wallace S, Mellor-Crummey L, Gong L, Pannu H, et al. Precision medical and surgical management for thoracic aortic aneurysms and acute aortic dissections based on the causative mutant gene. J Cardiovasc Surg (Torino). 2016;57:172–177. [PubMed] [Google Scholar]
- 2.Guo DC, Regalado E, Casteel DE, Santos-Cortez RL, Gong L, Kim JJ, et al. Recurrent gain-of-function mutation in PRKG1 causes thoracic aortic aneurysms and acute aortic dissections. Am J Hum Genet. 2013;93:398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gago-Diaz M, Blanco-Verea A, Teixido G, Huguet F, Gut M, Laurie S, et al. PRKG1 and genetic diagnosis of early-onset thoracic aortic disease. Eur J Clin Invest. 2016;46:787–794. [DOI] [PubMed] [Google Scholar]
- 4.Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr., et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. Circulation. 2010;121:e266–369. [DOI] [PubMed] [Google Scholar]
- 5.Mokashi SA, Svensson LG. Guidelines for the management of thoracic aortic disease in 2017. Gen Thorac Cardiovasc Surg. 2017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Discussion of prophylactic management of the aortic root and ascending aorta in patients with a known PRKG1 mutation.