Abstract
Background
The location of death is an important component of end-of-life care. However, contemporary trends in the location of death for cardiovascular (CV) deaths related to heart failure (HF) and comparison to cancer deaths has not been fully examined.
Methods
We analyzed data from the Center for Disease Control Wide-Ranging Online Data for Epidemiologic Research database between 2003 and 2017 to identify location of death for CV-HF and cancer deaths. The proportions of deaths that occurred in a hospice facility, home, and medical facility were tested for trends using linear regression. Odds ratios were calculated to determine the odds of death occurring in a hospice facility or home (versus a medical facility) stratified by sex and race.
Results
We identified 2,940,920 CV-HF and 8,852,066 cancer deaths. Increases were noted in the proportion of CV-HF deaths in hospice facilities (0.2% to 8.2%; Ptrend < 0.001) and at home (20.6% to 30.7%; Ptrend < 0.001), while decreases were noted in the proportion of deaths in medical facilities (44.5% to 31.0%; Ptrend < 0.001) and nursing homes (30.8% to 25.7%; Ptrend < 0.001). The odds of dying in a hospice facility (OR 1.79 [1.75, 1.82]) or at home (OR 1.55 [1.53, 1.56]). versus a medical facility was higher for whites versus blacks. The rate of increase in proportion of deaths in hospice facilities was higher for cancer deaths (β= 1.05, 95% CI 0.97–1.12) than for CV-HF deaths (β= 0.61, 95% CI 0.58, 0.64).
Conclusions
The proportion of CV-HF deaths occurring in hospice facilities is increasing but remains low. Disparities are noted whereby whites are more likely to die in hospice facilities or at home vs. medical facilities compared to blacks. More research is needed to determine end-of-life preferences for patients with HF and identify the basis for these differences in location of death.
Keywords: Heart Failure, CVD Mortality
INTRODUCTION
Despite advances in treatments, advanced heart failure (HF) is associated with high mortality.1 Unfortunately, patients with HF often experience high symptom burden2 and poor health-related quality of life at the end of life.3
Dying in the patient’s preferred location is considered an important aspect of end-of-life care and most patients prefer to die at home irrespective of their underlying condition.4 However, patients with cardiovascular disease (CVD), and HF in particular, may be more likely than patients with other disorders, such as cancer, to die in a medical facility and less likely to die in a hospice facility or at home.5
Understanding where patients with HF die may inform provision of more patient-centered end-of-life care. Therefore, we sought to (1) examine the distribution of and trends in place of death for cardiovascular deaths related to HF (CV-HF deaths), and (2) compare these trends to deaths due to cancer, which is the most common diagnosis of hospice enrollees.
METHODS
The authors declare that all supporting data are available within the article [and its online supplementary files].
We analyzed the publicly available multiple cause of death files from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER),6 which captures death certificates of all in- and out-of-hospital US resident deaths, for deaths from 2003 to 2017. Studying HF deaths is difficult given that HF is not considered an underlying cause of death by nosologists, but rather a mediator between death and disease.7 As a result, coding rules for mortality statistics discourage the recording of HF as the underlying cause of death when other diseases are present and are considered to have more directly contributed to death.7 CV causes of death represent the predominant mode of death for patients with HF.8 Therefore, we identified CVD deaths related to HF (CV-HF deaths) using the International Classification of Disease, Tenth Revision (ICD-10), whereby CVD (codes I00-I78) was listed as the underlying cause of death and HF (codes I50) was listed as a contributing cause of death. Because HF is listed as the underlying cause of death on approximately 3% of death certificates, deaths were also included if HF was listed as the underlying cause of death. Deaths due to cancer were identified whereby malignant neoplasms (codes C00-C97) were listed as the underlying cause of death. We began our study period in 2003 as this was the year that deaths in hospice facilities started being coded in a standardized manner in death certificate data. The institutional review board of Northwestern University deemed this study to be exempt since it utilizes deidentified data.
Statistical Analysis
Proportionate mortality due to CV-HF and due to cancer was calculated for each year of the study period, using annual US Census Data as the reference. Univariate logistic regression was used to test for trends in proportion of CV-HF deaths that occurred in each location for each year, and in proportions of CV-HF deaths that occurred in a hospice facility and at home stratified by sex (male, female), race (white, black) and age (≥ 65 years, < 65 years) for each year. Odds ratios were calculated to determine the odds of death occurring in a hospice facility or home (versus a medical facility) stratified by sex and race for each year of the study period. Finally, the proportions of CV-HF deaths and cancer-deaths that occurred in the locations of hospice facility, home, and medical facility were tested for trends using linear regression. The rate of increase in proportion of deaths in each location for CV-HF deaths and cancer-deaths was compared.
RESULTS
We identified 2,940,920 CV-HF deaths from 2003 to 2017, with 45% occurring in men, 9% in blacks, and 92% among individuals over age 65. Proportionate mortality due to CV-HF deaths was 8.2% in 2003 and 8.0% in 2017.
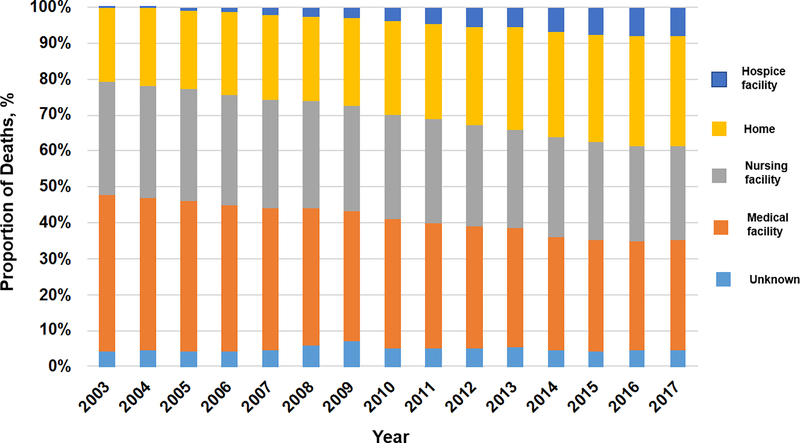
From 2003 to 2017, the proportion of CV-HF deaths in hospice facilities increased from 0.2% to 8.2% (Ptrend < 0.001) and the proportion of deaths at home increased from 20.6% to 30.7% (Ptrend < 0.001) (Figure 1). Modest decreases were noted in the proportion of deaths occurring in medical facilities (44.5% to 31.0%; Ptrend < 0.001) and nursing homes (30.8 to 25.7%; Ptrend < 0.001).
Figure 1.
Trends in location of death for heart failure-related cardiovascular mortality during 2003 to 2017 in the United States.
From 2003 to 2017, the proportion of deaths in hospice facilities increased among both sexes (0.2% to 7.9% in women, Ptrend < 0.001; 0.1% to 8.1% in men, Ptrend < 0.001), races (0.1% to 7.0% in blacks, Ptrend < 0.001; 0.2% to 8.2% in whites, Ptrend < 0.001), and age groups examined (0.1% to 4.9% in < age 65, Ptrend < 0.001; 0.2% to 8.3% in age ≥ 65, Ptrend < 0.001). The proportion of deaths at home also increased among both sexes (18.5% to 28.9% in women, Ptrend < 0.001; 23.3% to 32.7% in men, Ptrend < 0.001), races (19.1% to 29.7% in blacks, Ptrend < 0.001; 20.6% to 30.4% in whites, Ptrend < 0.001), and age groups examined (26.6% to 30.5% in < age 65, Ptrend < 0.001; 20.0% to 30.8% in age ≥ 65, Ptrend < 0.001).
The odds of dying in a hospice facility versus a medical facility remained lower for males versus females across all years of the study period and overall (OR 0.90 [0.89, 0.91]), but higher for whites compared with blacks across all years of the study period and overall (OR 1.79 [1.75, 1.82]). Additionally, the odds of dying at home versus a medical facility were lower for males compared with females across all years of the study period and overall (OR 0.99 [0.98, 0.99]), but higher for whites compared with blacks across all years of the study period and overall (OR 1.55 [1.53, 1.56]).
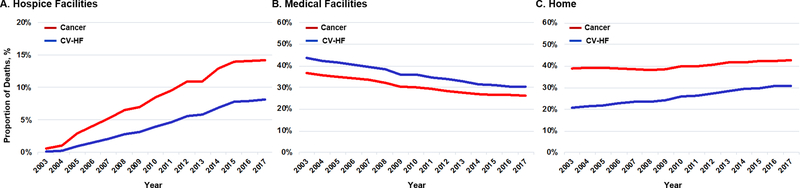
CV-HF deaths were compared to 8,852,066 deaths due to cancer over the study period. Proportionate mortality due to cancer was 23.3% in 2003 and 21.8% in 2017. From 2003 to 2017, the proportion of cancer deaths that occurred in hospice facilities and at home increased from 0.6% to 14.2% (Ptrend < 0.001) and from 38.9% to 42.7% (Ptrend < 0.001), respectively, while the proportion of deaths in medical facilities decreased from 36.7% to 26.4% (Ptrend < 0.001). (Figure 2)
Figure 2.
Proportion of cardiovascular disease deaths related to HF and cancer deaths in (A) hospice facilities, (B) medical facilities, and (C) at home during 2003 to 2017 in the United States.
The rate of increase in the proportion of deaths in hospice facilities was higher for cancer deaths (β= 1.05%, 95% CI 0.97–1.12) than for CV-HF deaths (β= 0.61%, 95% CI 0.58–0.64), reflecting a 1.05% and 0.61% increase in the proportion of deaths in hospice facilities per year from 2003 to 2017. However, the rate of increase in proportion of deaths at home was higher for CV-HF deaths (β= 0.78%, 95% CI 0.73–0.83) than for cancer deaths (β= 0.32%, 95% CI 0.22–0.41). The rate of decrease in the proportion of deaths in medical facilities was higher for CV-HF deaths (β= 1.02%, 95% CI 0.95–1.09) than for cancer deaths (β= 0.80%, 95% CI 0.71 to 0.88).
DISCUSSION
Our analysis demonstrates that an increasing number of CV-HF deaths are occurring in hospice facilities and at home, with fewer CV-HF deaths occurring in medical facilities. Notable differences by sex, race, and age exist in location of death.
These data build upon prior work9 wherein the authors found that those with HF died at home or in hospice more frequently during later years than earlier, however the definition of “HF deaths” was not clearly described. In contrast, we were deliberate in our case definition, intentionally examining only patients who died of cardiovascular causes related to HF, for notable reasons. First, as described above, HF is not considered an underlying cause of death by nosologists, and thus describing death due to HF requires the provision of a clear description of the underlying cause of death. Second, as described in our paper, individuals who die of cancer are more likely to die in hospice facilities and at home than patients who die of cardiovascular causes related to HF. Patients with HF who are primarily dying of cardiovascular causes therefore represent a different phenotype in terms of end-of-life care than patients who die of other causes (e.g. cancer) and carry HF as a comorbidity. The reason for these differences may be related to provider (oncologist versus cardiologist) comfort and familiarity with hospice referral and the challenges in prognosticating time of death for patients who are dying primarily of HF versus malignancy.
In contrast to other studies which have shown that the majority of patients with CVD5 and HF9 are still dying in medical facilities, our study showed that more patients dying of CV-HF are dying at home than in medical facilities. The increase in CV-HF deaths in a hospice facility or at home may reflect an increased emphasis on patient-centered care at the end of life. However, many questions remain. First, our analyses are limited by the available data collected on death certificates, and therefore do not include ejection fraction, etiology, and/or duration of HF. The inclusion of these variables would be informative, highlighting the need for a national surveillance program for non-fatal HF events in the US. Second, we do not know the preferred place of death for patients with HF. Anecdotally patients who are suffering from HF at the end-of-life may find more symptom relief at the hospital where intravenous diuretics are more readily available and where staff may be more adept at addressing patient needs. Further, recent data demonstrated that almost a quarter of Medicare HF patients who are discharged to hospice die within 3 days of discharge.10 For many of these patients, the transition to hospice may represent a burdensome one that has come too late in the disease course rather than the result of a timely, personalized end-of-life decision. Third, while we examined trends in hospice facility deaths over time, hospice services are most commonly provided outside of inpatient facilities- either at home or in nursing facilities. The inability to determine trends in total hospice usage is an important limitation of this paper, and highlights the need for prospectively designed studies. Finally, the significance of home deaths for this patient population is unclear. We do not know what proportion of deaths at home truly represent a patient-centered experience versus whether a proportion of these deaths may represent death due to sudden cardiac death.
We identified important racial disparities in location of death. While the proportion of deaths occurring at home and in hospice increased to almost equivalent levels in blacks and whites in 2017, the odds of dying in a hospice facility or at home versus a medical facility were significantly higher for whites compared with blacks across all years of the study period. The discrepancy between these two findings is likely related to nursing home deaths. Nonetheless, the greater odds of dying at home or in a hospice facility versus a medical facility among whites is troubling given the greater risk of development of HF as well as dying from CV-HF that has been described among blacks.11 Racial disparities in utilization of hospice services have been well described,12 and a recent analysis of patients in the Palliative Care in Heart Failure (PAL-HF) trial also demonstrated that African Americans with advanced HF are more likely to die in a health care facility than at home or in hospice.13 To our knowledge, this finding has not been reported for patients dying of cardiovascular causes related to HF. Whether these disparities are primarily due to differences in access to palliative care services or to variations in care preferences, whereby African Americans display a greater preference for death in the hospital14 and for life-prolonging treatments than whites15 is unknown.
Overall, our study reveals an important shift that has occurred in place of death for patients with HF: patients dying of CV-HF are now dying more commonly at home than in medical facilities, and deaths in hospice facilities are increasing. Importantly, however, patients dying of CV-HF mortality are still less likely to die in hospice facilities or at home than patients dying of cancer, and blacks are less likely to die in hospice facilities or at home vs. medical facilities compared to whites. Integration of palliative care in a multi-disciplinary personalized approach to the HF patient, improved tools to assess prognosis, and education for both patients and cardiologists about the benefits of palliative care and hospice may lead to a narrowing of these gaps.
Acknowledgments
Sources of Funding
Supported by grants from the National Institutes of Health/National Heart, Lung, and Blood Institute (KL2TR001424) and the American Heart Association (AHA#19TPA34890060) to Dr. Khan. Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number KL2TR001424 (SSK). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosure Statement: None.
REFERENCES
- 1.Curtis LH, Greiner MA, Hammill BG, Kramer DM, Whellan DJ, Schulman KA, Hernandez AF. Early and long-term outcomes of heart failure in elderly persons, 2001–2005. Arch Int Med. 2008; 168:2481–2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levenson JW, McCarthy EP, Lynn J, Davis RB, Phillips RS. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc. 2000; 48:S101–109. [DOI] [PubMed] [Google Scholar]
- 3.Bekelman DB, Rumsfeld JD, Havranek EP, Yamashita TA, Hutt E, Gottlieb SH, Dy SM, Kutner JS. Symptom burden, depression, and spiritual well-being: a comparison of heart failure and advanced cancer patients. J Gen Intern Med. 2009; 24:592–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Earle CC, Park ER, Lai B, Weeks JC, Ayanian JZ, Block S. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol. 2003; 21:1133–1138. [DOI] [PubMed] [Google Scholar]
- 5.Warraich HJ, Hernandez AF, Allen LA. How medicine has changed the end of life for patients with cardiovascular disease. J Am Coll Cardiol. 2017; 70:1276–1289. [DOI] [PubMed] [Google Scholar]
- 6.Hamideh D, Alvarez O. Sickle cell disease related mortality in the United States (1999–2009). Pediatr Blood Cancer. 2013; 60:1482–1486. [DOI] [PubMed] [Google Scholar]
- 7.Foreman KJ, Naghavi M, Ezzati M. Improving the usefulness of US mortality data: new methods for reclassification of underlying cause of death. Popul Health Metr. 2016;14:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaduganath M, Patel RB, Michel A, Shah SJ, Senni M, Gheorghiade M, Butler J. Mode of death in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2017; 69:556–569. [DOI] [PubMed] [Google Scholar]
- 9.Al-kindi SG, Koniaris C, Oliveira GH, Robinson MR. Where patients with heart failure die: trends in location of death of patients with heart failure in the United States. J Card Fail. 2017; 23: 713–714. [DOI] [PubMed] [Google Scholar]
- 10.Warraich JH, Xu H, Devore AD, Matsouaka R, Heidenerich PA, Bhatt DL, Hernandez AF, Yancy CW, Fonarow GC, Allen LA. Trends in hospice discharge and relative outcomes among Medicare patients in the Get With The Guidelines–Heart Failure registry. JAMA Cardiol. 2018; 3:917–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glynn P, Lloyd-Jones DM, Feinstein MJ, Carnethon M, Khan SS. Disparities in cardiovascular mortality related to heart failure in the United States. J Am Coll Cardiol. 2019; 73:2354–2355. [DOI] [PubMed] [Google Scholar]
- 12.Cohen LL. Racial/ethnic disparities in hospice care: a systematic review. J Palliat Med. 2008; 11:763–768. [DOI] [PubMed] [Google Scholar]
- 13.Warraich HJ, O’Connor CM, Yang H, Granger BB, Johnson KS, Mark DB, Anstrom KJ, Patel CB, Steinhauser KE, Tulsky JA, Taylor DJ Jr, Rogers JG, Mentz RJ. African americans with advanced heart failure are more likely to die in a health care facility than at home or in hospice: an analysis from the PAL-HF trial. J Card Fail. 2019; 25:693–694. [DOI] [PubMed] [Google Scholar]
- 14.Barnato AE, Anthony DL, Skinner J, Gallagher PM, Fisher ES. Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med. 2009; 24:695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hopp FP, Duffy SA. Racial variations in end-of-life care. J Am Geriatr Soc. 2008; 48:658–663. [DOI] [PubMed] [Google Scholar]