Abstract
Catamenial pneumothorax (CP) is considered to be the most common form of thoracic endometriosis syndrome, which also includes catamenial hemothorax, catamenial hemopneumothorax, catamenial hemoptysis, and endometriosis lung nodules. Diagnosis can be hinted by high recurrence rates of lung collapse in a woman of reproductive age with endometriosis. In our case we present a 41 year old woman at the time of the second incidence with a left pneumothorax and holes in the pericardium in the diaphragm location. Laparoscopic evaluation was performed along with video-assisted thoracoscopy and treatment was performed with both techniques.
Keywords: Catamenial pneumothorax (CP), Chest tube, Endometriosis
1. Introduction
Catamenial pneumothorax (CP) is defined as spontaneous recurrent pneumothorax, occurring in women of reproductive age, in temporal relationship with menses [1]. Usually it occurs in less than 72 hours after menstruation. It usually occurs in women from 30 to 40 years, it has been also diagnosed in young girls as early as 10 years of age and post-menopausal women (exclusively in women of menstrual age) mostly with a history of pelvic endometriosis [2]. Until now the relationship of catamenial pneumothorax with significant lung disease including chronic obstructive pulmonary disease (COPD), acute asthma, and bullous disease has not been investigated, however; in these cases pneumothoraces considered secondary to a known underlying lung disease have not been classified as catamenial [3]. Nevertheless, co-existence of catamenial pneumothorax and a known underlying lung disease cannot be excluded. Co-existence of cystic fibrosis and endometriosis-related catamenial pneumothorax and haemoptysis has only been reported in a patient [4]. At least two episodes of pneumothorax in total have to be observed in order to fulfill the definition criteria. Nevertheless, the mean number of recurrences of surgically treated patients is usually higher [3].
Catamenial pneumothorax is a syndrome generally considered to occur in ovulating women, while women during pregnancy, menarche and on ovulatory suppressants are generally not considered subject to it [5]. However; there are rare case reports of catamenial pneumothorax in women on ovulatory suppression [5] and during pregnancy [6].
2. Case presentation
In September 2018 a 41 year old patient was admitted with pneumothorax in the left hemithorax and was taken to surgery. The patient reported having known endometriosis in the abdomen. In specific, she had difficulty in childbirth. Ten years ago, she had undergone a mass removal from the umbilical cord area, which proved to be endometriosis.
The VATS method examined her left hemithorax but did not recognize a pathological condition in the pulmonary parenchyma, instead small confined holes in the tendon of the left hemidiaphragm, were observed which are indicative of endometriosis. Fig. 1, Fig. 2.
Fig. 1.
Conflicting holes in the left semicircle during thoracoscopy.
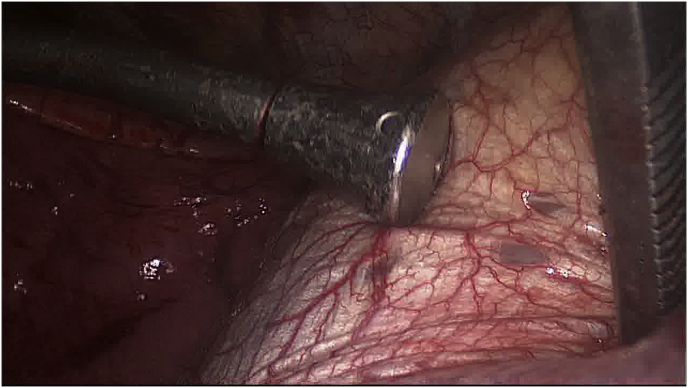
Fig. 2.
Suture of the diaphragm by thoracoscopic method (VATS).
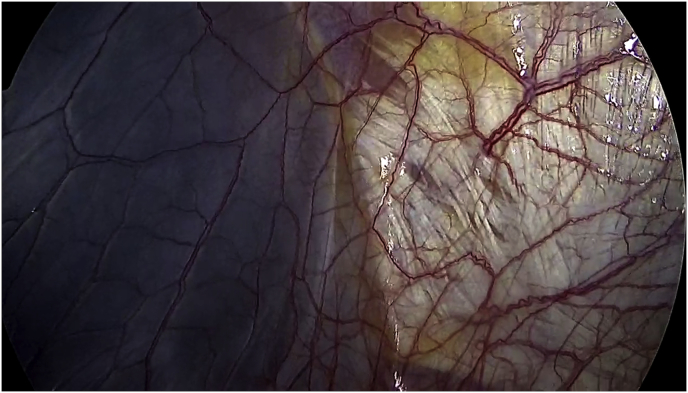
At the same time and by the same method, the diaphragm holes were stitched with a non-absorbable suture. Immediately thereafter, the pleural effusion was rubbed off with a 35% Detrox hypertensive solution followed by Talc's use. Careful haemostasis was performed and Buelau-type drainage tubes were inserted. Fig. 3, Fig. 4, Fig. 5, Fig. 6 The postoperative course of the patient was smooth and after two (2) days she left the clinic. The patient was advised to discontinue her menstrual cycle for six (6) months. Her subsequent course was checked by a CT scan every six (6) months and one (1) year after surgery and was unremarkable. One (1) month after the last re-examination, the patient was admitted with left pneumothorax on the left base and re-admitted to the clinic. A Buelau-type thoracic drain was immediately inserted and talc was laterally inserted through the tube. The patient remained in the clinic and was subsequently discharged. The patient was advised to discontinue her menstrual cycle for six (6) months. One (1) month later (November 2019), the patient has no pneumothorax and undergoes a laparoscopy during which the diaphragm is sprayed with a biological glue from the abdominal area. The Percuvance Percutaneous Surgical System from Teleflex was used. The operation was performed with the use of a single 10 mm Hassan Trocar port and a 30° degree camera. The patients' condition six (6) months afterwards is irreversible.
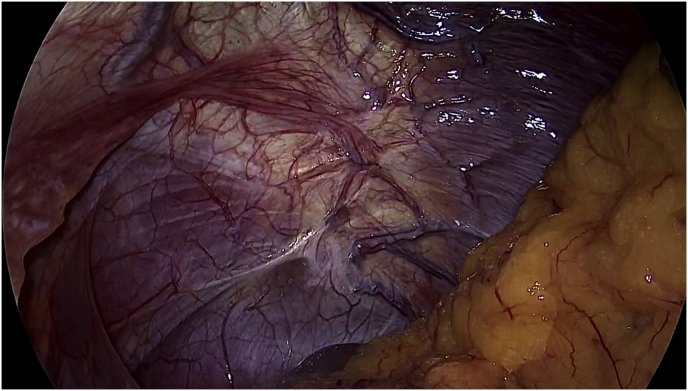
Fig. 3.
During the laparoscopy, the seams in the left semicircle placed in the thoracic surgery are distinguished.
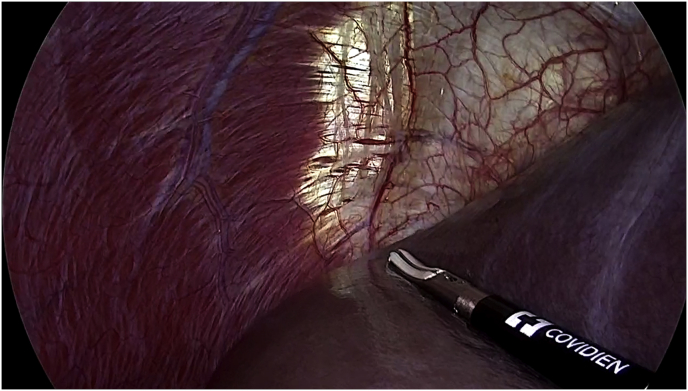
Fig. 4.
Confluent holes in the right semicircle are distinguished.
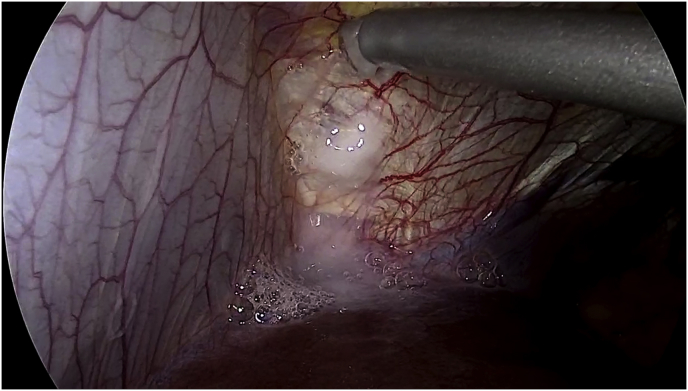
Fig. 5.
There are confluent holes in the left hemithorax just below the pericardium.
Fig. 6.
Spreading the left hemithorax with biological glue.
3. Discussion
Thus, the CP can be thoracic endometriosis-related or non-endometriosis-related [6]. Endometriosis-related pneumothoraces can be catamenial or non-catamenial [6]. Pneumothoraces with catamenial character (with or without evidence of thoracic endometriosis) as well as pneumothoracies with evidence of thoracic endometriosis (with or without catamenial character) can be classified under the term catamenial and/or endometriosis related pneumothorax. In the everyday clinical practice it seems that in the literature pneumothoracies are diagnosed as “catamenial” without strict relationship with menses, even in the case when occurring during pregnancy (24). There is the case of “endometriosis-related” without histologic evidence of endometrial glands or even stroma, based on clinical and macroscopic surgical findings [2,7]. It is known that hormonal treatment as an adjunct to surgery prevents recurrences of catamenial and/or endometriosis-related pneumothorax. In any case multidisciplinary management and administration of gonadotrophin-releasing hormone (GnRH) analogue, in the immediate postoperative period, for 6–12 months is essential for all patients with proven catamenial and/or endometriosis-related pneumothorax. Hormonal treatment may be beneficial even for patients without documented catamenial character and/or histologically proven thoracic endometriosis in the presence of characteristic lesions. It has been observed that incomplete surgical management of the lesions and/or no adjunctive hormonal treatment in the immediate postoperative period might increase the risk of recurrences. Early investigation and treatment of pelvic endometriosis is essential for the prevention of thoracic spread. In our case the incident was peculiar because; firstly this is an older woman (41 years old) compared to the usual present in the 3rd decade, secondly; it is a left-sided pneumothorax that is usually right and thirdly; pneumothorax recurred at year 1 (relatively soon) and as evidenced by laparoscopy the patient had holes in the diaphragmatic surface of the pericardium, which could not be identified by thoracoscopy.
Declaration of competing interest
None to declare.
References
- 1.Fonseca P. Catamenial pneumothorax: a multifactorial etiology. J. Thorac. Cardiovasc. Surg. 1998;116(5):872–873. doi: 10.1016/S0022-5223(98)00434-6. [DOI] [PubMed] [Google Scholar]
- 2.Kramer A.W., Bautista M. Catamenial pneumothorax in a 14-year-old female: a case report and literature review. Respir. Med. Case Rep. 2019;28:100951. doi: 10.1016/j.rmcr.2019.100951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alifano M., Roth T., Broet S.C., Schussler O., Magdeleinat P., Regnard J.F. Catamenial pneumothorax: a prospective study. Chest. 2003;124(3):1004–1008. doi: 10.1378/chest.124.3.1004. [DOI] [PubMed] [Google Scholar]
- 4.Triponez F., Alifano M., Bobbio A., Regnard J.F. Endometriosis-related spontaneous diaphragmatic rupture. Interact. Cardiovasc. Thorac. Surg. 2010;11(4):485–487. doi: 10.1510/icvts.2010.243543. [DOI] [PubMed] [Google Scholar]
- 5.Schoenfeld A., Ziv E., Zeelel Y., Ovadia J. Catamenial pneumothorax--a literature review and report of an unusual case. Obstet. Gynecol. Surv. 1986;41(1):20–24. doi: 10.1097/00006254-198601000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Yoshioka H., Fukui T., Mori S., Usami N., Nagasaka T., Yokoi K. Catamenial pneumothorax in a pregnant patient, the Japanese journal of thoracic and cardiovascular surgery: official publication of the Japanese Association for Thoracic Surgery = Nihon. Kyobu Geka Gakkai zasshi. 2005;53(5):280–282. doi: 10.1007/s11748-005-0042-6. [DOI] [PubMed] [Google Scholar]
- 7.Visouli A.N., Darwiche K., Mpakas A., Zarogoulidis P., Papagiannis A., Tsakiridis K., Machairiotis N., Stylianaki A., Katsikogiannis N., Courcoutsakis N., Zarogoulidis K. Catamenial pneumothorax: a rare entity? Report of 5 cases and review of the literature. J. Thorac. Dis. 2012;4(Suppl 1):17–31. doi: 10.3978/j.issn.2072-1439.2012.s006. [DOI] [PMC free article] [PubMed] [Google Scholar]