Abstract
Rationale: Obesity is the primary risk factor for obstructive sleep apnea (OSA). Tongue fat is increased in obese persons with OSA, and may explain the relationship between obesity and OSA. Weight loss improves OSA, but the mechanism is unknown.
Objectives: To determine the effect of weight loss on upper airway anatomy in subjects with obesity and OSA. We hypothesized that weight loss would decrease soft tissue volumes and tongue fat, and that these changes would correlate with reductions in apnea–hypopnea index (AHI).
Methods: A total of 67 individuals with obesity and OSA (AHI ≥ 10 events/h) underwent a sleep study and upper airway and abdominal magnetic resonance imaging before and after a weight loss intervention (intensive lifestyle modification or bariatric surgery). Airway sizes and soft tissue, tongue fat, and abdominal fat volumes were quantified. Associations between weight loss and changes in these structures, and relationships to AHI changes, were examined.
Measurements and Main Results: Weight loss was significantly associated with reductions in tongue fat and pterygoid and total lateral wall volumes. Reductions in tongue fat were strongly correlated with reductions in AHI (Pearson’s rho = 0.62, P < 0.0001); results remained after controlling for weight loss (Pearson’s rho = 0.36, P = 0.014). Reduction in tongue fat volume was the primary upper airway mediator of the relationship between weight loss and AHI improvement.
Conclusions: Weight loss reduced volumes of several upper airway soft tissues in subjects with obesity and OSA. Improved AHI with weight loss was mediated by reductions in tongue fat. New treatments that reduce tongue fat should be considered for patients with OSA.
Keywords: obstructive sleep apnea, upper airway, weight loss, apnea–hypopnea index
At a Glance Commentary
Scientific Knowledge on the Subject
This study examines the effect of weight loss on changes in tongue fat and other upper airway structures in individuals with obesity and sleep apnea assessed with Dixon magnetic resonance imaging. We also examined the influence of changes in upper airway structures with weight loss on improvements in apnea severity. Results indicate that tongue fat decreases with weight loss and is strongly associated with reductions in the apnea–hypopnea index.
What This Study Adds to the Field
This is the first study to show that weight loss decreases tongue fat in patients with sleep apnea, which explains one mechanism for the improvements in sleep apnea with reductions in weight. These findings suggest a potential unique therapeutic target for patients with obesity and sleep apnea, namely, reductions in tongue fat.
Over 70% of adults in the United States are overweight (body mass index [BMI] > 25 kg/m2) or obese (BMI > 30 kg/m2) (1). Excess body weight is the primary risk factor for obstructive sleep apnea (OSA) (2–6), and studies support a relationship between weight change and OSA risk or severity (6–8). Weight loss is recommended for the treatment of OSA (9). Across multiple studies, weight losses secondary to a range of dietary and lifestyle modifications are associated with significant reductions in the apnea–hypopnea index (AHI) (3, 6–8, 10–15). For example, in the Wisconsin Sleep Cohort, a 1% increase/decrease in body weight was associated with a corresponding 3% increase/decrease in AHI, and a 10% weight gain was associated with sixfold-increased risk of developing an AHI greater than 15 events/h (6). Systematic reviews and meta-analyses of surgical (14) and nonsurgical (15) weight loss support this relationship. However, although OSA severity is generally improved, OSA may not be eliminated after weight loss. Why obesity is associated with OSA, why weight loss improves OSA, and why weight gain exacerbates OSA remain unanswered, fundamental questions. Addressing these questions is important for optimizing clinical management and personalized OSA treatments.
The mechanisms for improved AHI with weight loss are not well understood. Evidence suggests that weight loss may differentially affect AHI in the supine versus nonsupine position (16). Decreased size of the upper airway and larger upper airway soft tissue volumes increase risk for OSA (17). Changes in these anatomical factors with weight loss may explain the improvements in AHI. Our group has shown that tongue fat is increased in obese patients with OSA compared with obese patients without OSA (18). Thus, reduced tongue fat with weight loss may reduce OSA severity. Similar relationships may exist for other upper airway anatomy implicated in OSA risk (17).
The primary goal of this study was to evaluate changes in upper airway anatomy with weight loss in patients with OSA, and to understand how these changes relate to improvements in AHI. We hypothesized that weight loss would result in corresponding changes in upper airway anatomy (e.g., increased airway size and decreased soft tissue volumes), and these changes, particularly decreased tongue fat, would associate with decreased OSA severity.
Methods
See detailed methods in the online supplement.
Subjects
This study included subjects with obesity and OSA presenting for bariatric surgery or lifestyle modification intervention for weight loss, recruited from the Penn Center for Sleep Disorders, the University of Pennsylvania’s Bariatric Surgery Program, or the Center for Weight and Eating Disorders. The study was approved by the University of Pennsylvania Institutional Review Board. Written informed consent was obtained from all participants. Participants were over 18 years of age with an AHI of 10 events/h or greater on polysomnography (18). Exclusion criteria included inability to undergo magnetic resonance imaging (MRI) or pregnancy. MRI and polysomnography were performed before weight loss treatment and repeated after 6 months.
Weight Loss Protocols
Participants underwent lifestyle modification for weight loss (n = 49) or bariatric surgery (n = 18; gastric sleeve [n = 8], bypass [Roux-en-Y; n = 9], or banding [n = 1]). The lifestyle modification was based upon the Diabetes Prevention Program and designed to promote weight loss of 5–10% through caloric restriction, increased physical activity, and behavioral modifications (19).
Polysomnography
Standard polysomnography was conducted as previously described (17, 18).
MRI
MRI studies were acquired using a 1.5-Tesla MAGNETOM Espree scanner (Siemens Medical Systems) as previously described (17, 18, 20, 21). Amira 4.1.2 analysis software (Visage Imaging) was used to quantify MRI measures in three domains: airway sizes (10 measures)—airway volume, average cross-sectional area, minimum airway area, minimum anterior–posterior distance, and minimum lateral distance in the retropalatal (RP) and retroglossal (RG) regions; soft tissue volumes (12 measures)—tongue, tongue fat, soft palate, parapharyngeal fat pads, lateral walls, pterygoids, epiglottis, and combined soft tissue volume (the sum of these structures); and abdominal fat volumes (3 measures)—total, subcutaneous, and visceral fat volumes.
Reproducibility Assessment
Reproducibility of measurements was assessed by calculating intraclass correlation coefficients (ICCs) from data quantified on separate MRIs performed 6 months apart in a sample of 17 weight-stable individuals (defined as follow-up weight within 2.5% of baseline weight). This sample was chosen to represent individuals that did not undergo weight loss intervention. ICCs quantify reproducibility as poor (<0.00), slight (0.00–0.20), fair (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80), and almost perfect (0.81–1.00) (22).
Statistical Analysis
Analyses were performed using Stata, Version 14 (StataCorp LP), SAS Version 9.4 (SAS Institute Inc.), and SPSS 24 (IBM Corp.). Changes scores were calculated as follow-up minus baseline. Relationships between weight loss and anatomic changes were assessed using unadjusted Pearson’s linear correlations and partial Pearson’s correlations adjusted for baseline age, sex, race, height, and AHI. Associations between anatomy changes and AHI change were performed similarly. Complementary analyses comparing patients that lost 2.5% weight or greater and those with stable/increased weight were conducted using t tests and linear regression adjusted for age, sex, race, height, AHI, and baseline MRI measure (absolute changes only). Within-group changes were assessed with paired t tests. A domain-specific Hochberg step-up correction (23–25) was used to control for multiple comparisons (see online supplement); a P value less than 0.05 was considered nominally significant. Mediators between percent changes in weight and AHI were evaluated using conditional process analysis (26, 27) (see Figure E1 in the online supplement). Bias-corrected 95% confidence intervals (CIs) were estimated via bootstrapping to verify indirect (mediating) effects; mediation was shown if the CI excluded zero (26, 28).
Results
Measurement Reproducibility
To assess measurement reproducibility, we calculated ICCs using data from MRIs taken 6 months apart in a sample of weight-stable patients with apnea and those without apnea (Table E1). Nearly all measurements demonstrated substantial (ICC between 0.61 and 0.80) or almost perfect (ICC between 0.81 and 1.00) reproducibility. Fat pad volume (ICC = 0.353) and both total (ICC = 0.489) and subcutaneous (ICC = 0.536) abdominal fat volumes showed fair to moderately reproducible.
Participants Characteristics
A total of 67 patients with OSA were included (Table 1). Participants were middle aged (49.4 ± 11.9 yr) and obese (BMI of 42.6 ± 8.5 kg/m2), 40.3% were male, and 47.0% were white. Overall, participants lost 9.5 (±10.8)% of their body weight (P < 0.0001) and AHI improved by 30.7 (±66.7)% (P = 0.0004). Patients with apnea who lost 2.5% weight or more had a significant AHI reduction (−23.3 ± 21.9; P < 0.0001) compared with no change in those that did not (P = 0.856) (see online supplement).
Table 1.
Demographics of the Study Sample, Overall and by Weight-Loss Group
| Variable | All Participants | Weight Stable/Gain* | Weight Loss* | P Value† |
|---|---|---|---|---|
| n | 67 | 20 | 47 | — |
| Age, yr | 49.4 ± 11.9 | 51.1 ± 11.8 | 48.7 ± 12.0 | 0.472 |
| Male, % | 40.3 | 35.0 | 42.6 | 0.564 |
| White, % | 47.0 | 40.0 | 50.0 | 0.454 |
| Height, cm | 170.3 ± 10.8 | 169.8 ± 11.6 | 170.5 ± 10.6 | 0.814 |
| Weight, kg | ||||
| Baseline | 123.4 ± 25.3 | 130.3 ± 28.0 | 120.4 ± 23.7 | 0.143 |
| Follow-up | 111.1 ± 24.6 | 132.9 ± 26.5 | 101.8 ± 16.9 | 0.0001 |
| Change | −12.3 ± 15.0‡ | 2.5 ± 5.3‡ | −18.6 ± 13.2‡ | <0.0001 |
| % Change | −9.5 ± 10.8‡ | 2.3 ± 4.5‡ | −14.5 ± 8.5‡ | <0.0001 |
| BMI, kg/m2 | ||||
| Baseline | 42.6 ± 8.5 | 45.3 ± 8.8 | 41.5 ± 8.2 | 0.099 |
| Follow-up | 38.4 ± 8.5 | 46.2 ± 8.7 | 35.1 ± 5.8 | <0.0001 |
| Change | −4.2 ± 5.2‡ | 0.9 ± 2.0‡ | −6.4 ± 4.5‡ | <0.0001 |
| % Change | −9.5 ± 10.8‡ | 2.3 ± 4.5‡ | −14.5 ± 8.5‡ | <0.0001 |
| AHI, events/h | ||||
| Baseline | 40.8 ± 28.6 | 39.2 ± 31.5 | 41.4 ± 27.6 | 0.776 |
| Follow-up | 25.1 ± 23.6 | 40.1 ± 24.7 | 18.6 ± 20.0 | 0.0004 |
| Change | −16.0 ± 24.5‡ | 0.9 ± 21.9 | −23.3 ± 21.9‡ | 0.0001 |
Definition of abbreviations: AHI = apnea–hypopnea index; BMI = body mass index.
Weight loss was defined as ≥2.5% decrease in weight from baseline, and stable/gain was defined as <2.5% decrease in weight.
P value from t test or chi-square test comparing values between weight loss and stable/gain groups.
Within-group change significantly different from zero (P < 0.05) in paired t test.
Changes in Anatomy with Weight Loss
To understand how weight loss affected the upper airway and abdominal fat, we assessed Pearson’s correlations between percent changes in weight and anatomical structures (Table 2). Analyses of absolute changes are presented in Tables E2A–E2C. Comparisons of patients that lost 2.5% weight or more and those that were weight stable or gained weight are detailed in the online supplement (see Tables E3 and E4A–E4C).
Table 2.
Pearson’s Correlations between Percent Change in Weight and Percent Change in Airway Dimensions, Soft Tissue Volumes, and Abdominal Fat Measures among Patients with Obstructive Sleep Apnea
| Unadjusted |
Adjusted |
|||||
|---|---|---|---|---|---|---|
| n | Rho* | P Value | n | Rho† | P Value | |
| Airway sizes | ||||||
| RP airway volume | 64 | −0.05 | 0.668 | 63 | −0.09 | 0.502 |
| RP cross-sectional area | 64 | −0.14 | 0.285 | 63 | −0.18 | 0.179 |
| RP minimum area | 64 | 0.01 | 0.942 | 63 | 0.01 | 0.936 |
| RP minimum AP distance | 64 | 0.30 | 0.017 | 63 | 0.36 | 0.006 |
| RP minimum lateral distance | 64 | −0.26 | 0.035 | 63 | −0.34 | 0.009 |
| RG airway volume | 62 | 0.08 | 0.523 | 61 | 0.10 | 0.443 |
| RG cross-sectional area | 60 | 0.16 | 0.224 | 59 | 0.14 | 0.321 |
| RG minimum area | 61 | −0.33 | 0.008 | 60 | −0.43 | 0.001 |
| RG minimum AP distance | 60 | 0.15 | 0.253 | 59 | 0.12 | 0.385 |
| RG minimum lateral distance | 60 | −0.02 | 0.875 | 59 | −0.05 | 0.701 |
| Soft tissue volumes | ||||||
| Combined soft tissue | 63 | 0.14 | 0.268 | 62 | 0.18 | 0.187 |
| Soft palate | 64 | −0.15 | 0.234 | 63 | −0.14 | 0.303 |
| Genioglossus | 64 | −0.02 | 0.866 | 63 | −0.01 | 0.937 |
| Other tongue | 64 | 0.01 | 0.962 | 63 | 0.04 | 0.788 |
| Tongue fat | 52 | 0.62 | <0.0001 | 51 | 0.62 | <0.0001 |
| Total tongue | 64 | −0.03 | 0.833 | 63 | 0.00 | 0.993 |
| Epiglottis | 63 | 0.07 | 0.591 | 62 | 0.09 | 0.486 |
| Fat pads | 63 | 0.08 | 0.529 | 62 | 0.08 | 0.536 |
| Pterygoid | 64 | 0.42 | 0.001 | 63 | 0.40 | 0.002 |
| RP lateral walls | 64 | 0.25 | 0.044 | 63 | 0.31 | 0.017 |
| RG lateral walls | 64 | 0.19 | 0.137 | 63 | 0.23 | 0.088 |
| Total lateral walls | 64 | 0.32 | 0.011 | 63 | 0.40 | 0.002 |
| Abdominal fat volume | ||||||
| Abdominal total fat | 51 | 0.52 | 0.0001 | 50 | 0.54 | 0.0001 |
| Abdominal subcutaneous fat | 51 | 0.50 | 0.0002 | 50 | 0.52 | 0.0003 |
| Abdominal visceral fat | 51 | 0.46 | 0.001 | 50 | 0.49 | 0.001 |
Definition of abbreviations: AP = anterior–posterior; RG = retroglossal; RP = retropalatal.
Significant values after Hochberg correction are shown in bold.
Unadjusted Pearson’s linear correlation.
Partial Pearson’s correlation adjusted for age, sex, race, apnea–hypopnea index, and height.
Airway sizes
Table 2 shows associations between changes in weight and airway sizes. Larger percent decreases in weight were significantly associated with greater percent increases in RG minimum area (Pearson’s partial rho = −0.43, P = 0.001), controlling for covariates. Significant or nominal correlations were also observed with changes in the shape of the RP airway (Table 2). Weight loss was associated with decreased anterior–posterior distance (partial rho = 0.36, P = 0.006) and increased lateral distance (partial rho = −0.34, P = 0.009) in the RP region. Similar effects on RP airway shape, but not RG minimum area, were observed for absolute changes (Table E2A). Comparisons between weight loss groups are shown in Tables E3A and E4A (detailed in the online supplement). RP airway sizes and RG minimum area increased in patients that lost weight; changes in RP minimum lateral distance and RG minimum area were different between those that lost weight and those that did not.
Soft tissue volumes
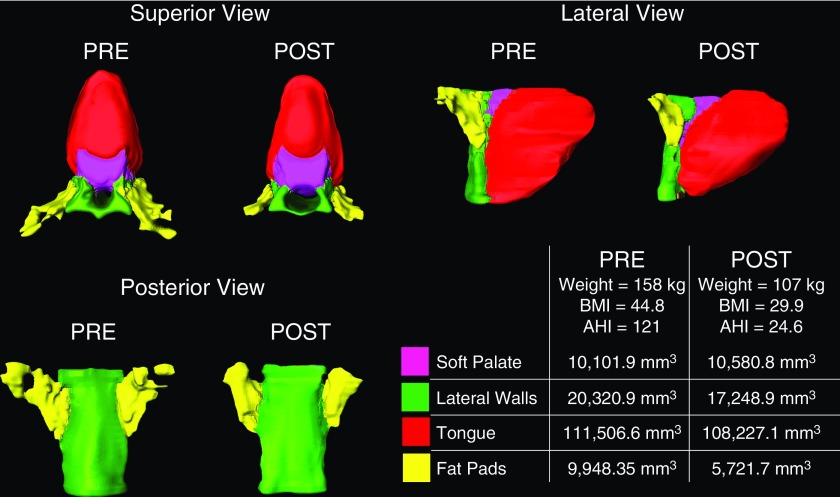
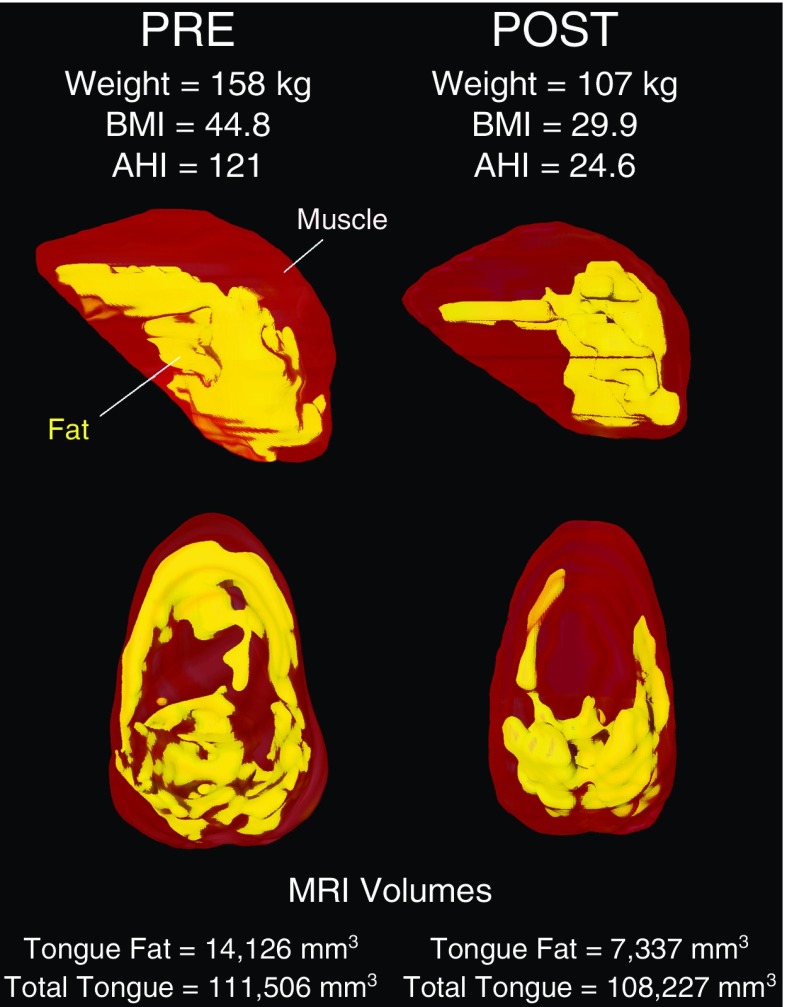
Table 2 details correlations between percent changes in weight and soft tissue volumes. In adjusted analyses, larger percent reductions in weight were significantly correlated with greater percent reductions in tongue fat (partial rho = 0.62, P < 0.0001), pterygoid (partial rho = 0.40, P = 0.002), and total lateral wall (partial rho = 0.40, P = 0.002) volumes, and nominally correlated with greater percent reductions in RP lateral wall volume (partial rho = 0.31, P = 0.017). The relationship between reduction in tongue fat volume and percentage change in weight is illustrated in Figure 1. Similar results were observed for absolute changes (Table E2B), with correlations between absolute weight change and change in tongue fat (partial rho = 0.48, P = 0.001), pterygoid (partial rho = 0.37, P = 0.005), and total lateral wall (partial rho = 0.28, P = 0.035) volumes. Most soft tissue measures showed significant decreases among patients with OSA who lost weight (Tables E3B and E4B), and there were significant differences in tongue fat volume, pterygoid volume, and total lateral wall volume changes between weight loss groups. Changes in soft tissue volumes and tongue fat are illustrated in Figures 2 and 3.
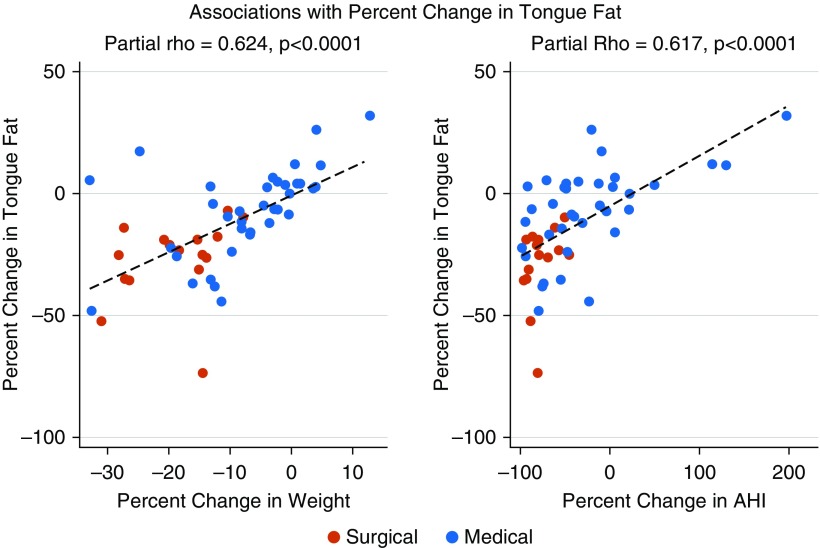
Figure 1.
The relationship of percentage change in tongue fat volume with percentage change in weight and apnea–hypopnea index (AHI). The associations between the percentage change in tongue fat and weight loss (left panel) and AHI change (right panel) are illustrated among obese subjects with apnea undergoing surgical or medical weight loss. Strong positive correlations were observed between tongue fat change and both measures (Pearson’s partial rho = 0.62, P < 0.0001) in covariate adjusted analyses. Mediation analyses suggest that percentage change in tongue fat was the primary upper airway mediator between percentage weight loss and percentage reductions in AHI.
Figure 2.
Changes in upper airway soft tissue structures with weight loss. Three-dimensional reconstructions derived from axial magnetic resonance imaging (T1-weighted, spin echo, 3-mm slice thickness), demonstrating changes in selected upper airway soft tissue structures between baseline and 6-month follow-up in a male patient with sleep apnea. Structures include: tongue, defined as the genioglossus muscle (red); soft palate (magenta); parapharyngeal fat pads (yellow); and lateral pharyngeal walls (green). The region of interest extends from the superior appearance of the tongue to the appearance of the hyoid bone. AHI = apnea–hypopnea index; BMI = body mass index.
Figure 3.
Change in tongue fat volume with weight loss. Three-dimensional reconstruction of tongue (red) and tongue fat (yellow) derived from axial magnetic resonance imaging (MRI; T1-weighted, spin echo, 3-mm slice thickness) and Dixon fat-only MRI (3-mm slice thickness), demonstrating loss of tongue fat between baseline and a 6-month follow-up visit in the same male subject with apnea as shown in Figure 2. The tongue is defined as the genioglossus muscle, and tongue fat is defined as all fat within the genioglossus. AHI = apnea–hypopnea index; BMI = body mass index.
Abdominal fat volumes
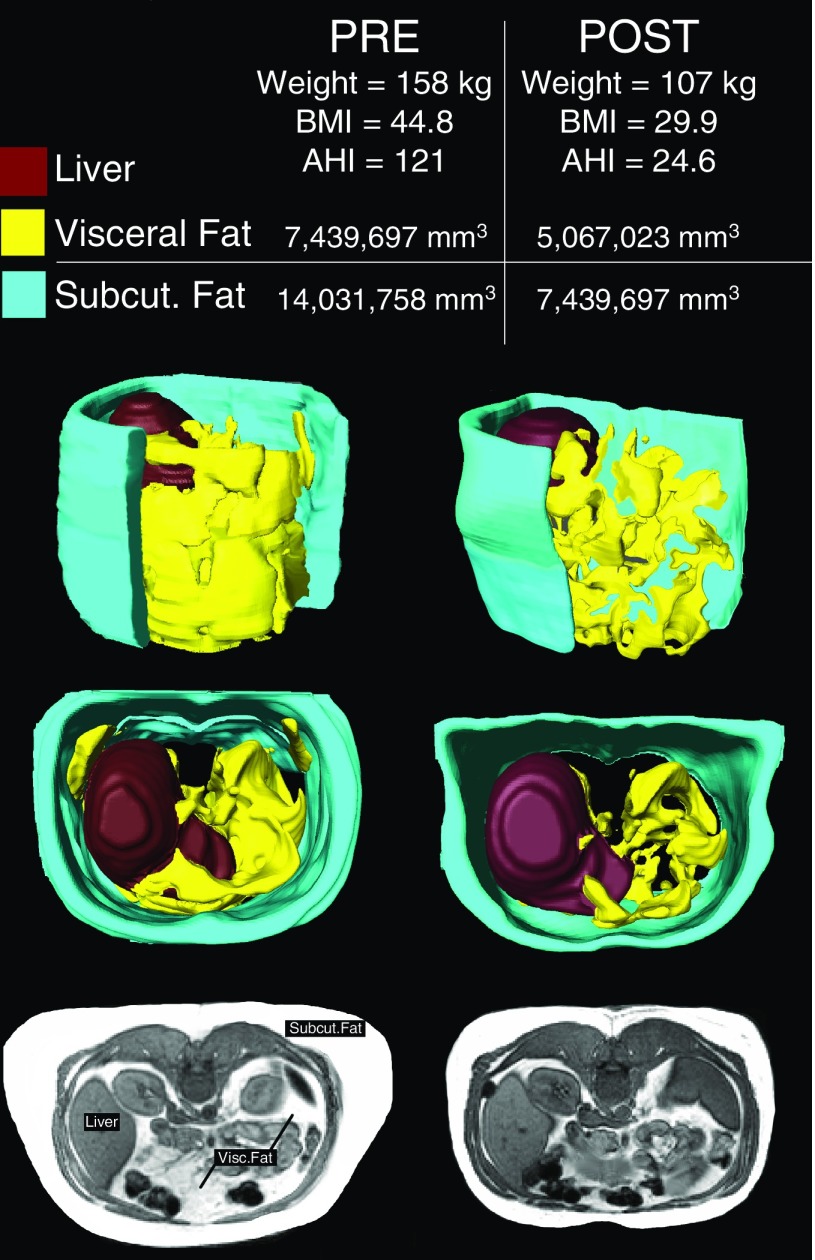
Table 2 shows relationships between changes in weight and abdominal fat. Strong positive correlations were observed between percent change in weight and percent changes in total (partial rho = 0.54, P = 0.0001), subcutaneous (partial rho = 0.52, P = 0.0003), and visceral (partial rho = 0.49, P = 0.001) abdominal fat in adjusted analyses. Similar associations were seen for absolute changes (Table E2C). There were larger reductions in each measurement among those who lost weight compared with no change in those who did not (Tables E3C and E4C). The percentage change in visceral fat was greater than the percentage change in subcutaneous fat among participants who lost weight (P = 0.002). Changes in abdominal fat are illustrated in Figure 4.
Figure 4.
Change in abdominal fat volumes with weight loss. Three-dimensional reconstructions of abdomen derived from axial magnetic resonance imaging (T1-weighted, spin echo, 10-mm slice thickness) showing fat loss between baseline and a 6-month follow-up visit in the same male subject with apnea as shown in Figures 2 and 3. Subcutaneous fat (cyan), visceral fat (yellow), and the liver (brown) have been highlighted. Subcutaneous fat is defined as all fat superficial to the abdominal fascia. Visceral fat is defined as all fat within the abdominal fascia that is not part of the spinal column. The region of interest extends from the superior appearance of the liver to the L5–S1 intervertebral disc. AHI = apnea–hypopnea index; BMI = body mass index; Subcut. = subcutaneous; Visc. = visceral.
Associations between Changes in Tongue Fat and Abdominal Fat
We assessed correlations between tongue fat and abdominal fat changes, given that both were associated with percent changes in weight. Results are detailed in the online supplement.
Associations between Changes in Anatomy and Changes in AHI
To understand the relationship between changes in upper airway anatomy and OSA severity, we evaluated correlations with percentage changes in AHI (Table 3). Larger percentage reductions in weight were strongly correlated with greater reductions in AHI (partial rho = 0.68, P < 0.0001). Complementary analyses with absolute changes are presented in Tables E5A–E5C. Given evidence of positional differences in the AHI response to weight loss (16), analyses examining correlations with changes in supine and nonsupine AHI are presented in Tables E6A–E6C among patients with positional AHI of 5 events/h or greater at baseline. Percentage reductions in weight were strongly correlated with nonsupine AHI (partial rho = 0.63, P < 0.0001), but not supine AHI (partial rho = −0.06, P = 0.753).
Table 3.
Pearson’s Correlations between Percent Change in Apnea–Hypopnea Index and Percent Change in Airway Size, Percent Change in Soft Tissues, and Percent Change in Abdominal Fat Measures among Patients with Obstructive Sleep Apnea
| Unadjusted |
Adjusted Results |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Covariates Only |
Covariates and Weight Change |
||||||||
| n | Rho* | P Value | n | Rho† | P Value | n | Rho‡ | P Value | |
| Airway sizes | |||||||||
| RP airway volume | 63 | 0.13 | 0.318 | 62 | 0.10 | 0.453 | 62 | 0.21 | 0.124 |
| RP cross-sectional area | 63 | 0.07 | 0.562 | 62 | 0.03 | 0.817 | 62 | 0.19 | 0.155 |
| RP minimum area | 63 | 0.02 | 0.904 | 62 | −0.01 | 0.946 | 62 | −0.02 | 0.862 |
| RP minimum AP distance | 63 | 0.25 | 0.045 | 62 | 0.30 | 0.022 | 62 | 0.09 | 0.494 |
| RP minimum lateral distance | 63 | −0.23 | 0.076 | 62 | −0.32 | 0.015 | 62 | −0.14 | 0.304 |
| RG airway volume | 61 | 0.11 | 0.396 | 60 | 0.08 | 0.558 | 60 | 0.03 | 0.804 |
| RG cross-sectional area | 59 | 0.34 | 0.009 | 58 | 0.30 | 0.025 | 58 | 0.28 | 0.039 |
| RG minimum area | 60 | −0.28 | 0.033 | 59 | −0.35 | 0.008 | 59 | −0.11 | 0.428 |
| RG minimum AP distance | 59 | 0.18 | 0.175 | 58 | 0.16 | 0.233 | 58 | 0.09 | 0.512 |
| RG minimum lateral distance | 59 | 0.10 | 0.470 | 58 | 0.04 | 0.753 | 58 | 0.11 | 0.428 |
| Soft tissue volumes | |||||||||
| Combined soft tissue | 62 | 0.19 | 0.139 | 61 | 0.23 | 0.090 | 61 | 0.17 | 0.204 |
| Soft palate | 63 | −0.16 | 0.202 | 62 | −0.14 | 0.305 | 62 | −0.06 | 0.664 |
| Genioglossus | 63 | 0.13 | 0.324 | 62 | 0.16 | 0.228 | 62 | 0.23 | 0.082 |
| Other tongue | 63 | 0.07 | 0.577 | 62 | 0.11 | 0.401 | 62 | 0.13 | 0.343 |
| Tongue fat | 51 | 0.61 | <0.0001 | 50 | 0.62 | <0.0001 | 50 | 0.36 | 0.014 |
| Total tongue | 63 | 0.12 | 0.340 | 62 | 0.18 | 0.185 | 62 | 0.25 | 0.063 |
| Epiglottis | 62 | 0.05 | 0.687 | 61 | 0.10 | 0.459 | 61 | 0.05 | 0.712 |
| Fat pads | 62 | 0.14 | 0.278 | 61 | 0.15 | 0.281 | 61 | 0.12 | 0.364 |
| Pterygoid | 63 | 0.24 | 0.055 | 62 | 0.19 | 0.145 | 62 | −0.09 | 0.488 |
| RP lateral walls | 63 | 0.26 | 0.037 | 62 | 0.32 | 0.014 | 62 | 0.18 | 0.189 |
| RG lateral walls | 63 | 0.07 | 0.600 | 62 | 0.04 | 0.791 | 62 | −0.12 | 0.357 |
| Total lateral walls | 63 | 0.24 | 0.055 | 62 | 0.26 | 0.051 | 62 | 0.03 | 0.813 |
| Abdominal fat volume | |||||||||
| Abdominal total fat | 50 | 0.37 | 0.008 | 49 | 0.38 | 0.009 | 49 | −0.04 | 0.790 |
| Abdominal subcutaneous fat | 50 | 0.38 | 0.006 | 49 | 0.39 | 0.008 | 49 | 0.00 | 0.993 |
| Abdominal visceral fat | 50 | 0.29 | 0.041 | 49 | 0.31 | 0.040 | 49 | −0.11 | 0.466 |
For definition of abbreviations, see Table 2.
Significant values after Hochberg correction are shown in bold.
Unadjusted Pearson’s linear correlation.
Partial Pearson’s correlation adjusted for age, sex, race, and height.
Partial Pearson’s correlation adjusted for age, sex, race, height, and percent change in weight.
Airway sizes
When evaluating the effect of changes in airway size on the AHI (Table 3), controlling for covariates, greater reductions in RP minimum anterior–posterior distance (partial rho = 0.30, P = 0.022) and increases in RP minimum lateral distance (partial rho = −0.32, P = 0.015) were nominally associated with greater decreases in AHI. Thus, changes in the shape of the RP airway affect OSA severity. In the RG region, larger increases in the minimum area were associated with greater AHI reductions (partial rho = −0.35, P = 0.008). These correlations became nonsignificant after correction for multiple comparisons. There were no significant correlations with absolute changes (Table E5A) or positional AHI (Table E6A).
Soft tissue volumes
Among soft tissue measures (Table 3), greater percentage decreases in tongue fat were associated with larger reductions in AHI (partial rho = 0.62, P < 0.0001), controlling for clinical covariates. This result remained nominally significant also controlling for weight change (partial rho = 0.36, P = 0.014), suggesting that reduced tongue fat is independently associated with reduced AHI (Figure 1). Reductions in RP lateral wall volume were nominally correlated with reductions in AHI (partial rho = 0.32, P = 0.014); results were not significant controlling for change in weight. Associations between absolute changes in tongue fat and AHI were also observed (Table E5B). Percentage reduction in tongue fat was more strongly correlated with reductions in nonsupine AHI (partial rho = 0.59, P = 0.0004) than supine AHI (partial rho = 0.22, P = 0.260) (Table E6B).
Abdominal fat volumes
In adjusted analyses, we observed significant correlations between reductions in AHI and reductions in total (partial rho = 0.38, P = 0.009), subcutaneous (partial rho = 0.39, P = 0.008), and visceral (partial rho = 0.31, P = 0.039) abdominal fat (Table 3). Unlike tongue fat, correlations were nonsignificant controlling for change in weight. Similar results were found for absolute changes (Table E5C). Correlations were similar for supine and nonsupine AHI, but were not significant in the smaller sample (Table E6C).
Mediation Analyses
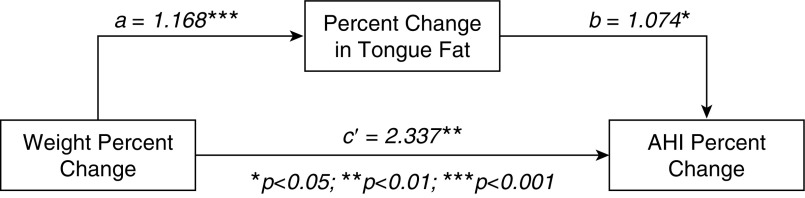
We next evaluated whether changes in specific anatomical structures mediate the relationship between percentage change in weight and percentage change in AHI. In our patients, each 1% change in weight was associated with a corresponding 4% change in AHI (unstandardized total effect [95% CI] = 3.98 [2.74–5.22]; standardized total effect = 0.648). Percent change in airway size or abdominal fat volumes did not significantly mediate this relationship (Table 4). On the other hand, analyses of soft tissue volumes indicated that percent reduction in tongue fat volume was a significant individual mediator between percent change in weight and AHI (unstandardized indirect effect [95% CI] = 1.255 [0.238–2.572]; standardized indirect effect = 0.225; Table 4). Changes in tongue fat accounted for approximately 30% of the total effect of weight loss on AHI improvement (Figure 5). No other soft tissues were significant individual mediators. Thus, these results indicate that change in tongue fat volume is the primary upper airway mediator of the relationship between weight change and change in AHI.
Table 4.
Single Mediator Modeling Results Evaluating Percent Changes in Airway, Soft Tissue, and Abdominal Fat as Mediators of the Relationship between Percent Change in Weight and Apnea–Hypopnea Index
| Domain/Measure | Indirect Effect (Bias-corrected 95% CI)*† |
|
|---|---|---|
| Standardized | Unstandardized | |
| Airway sizes | ||
| RP airway volume | −0.013 (−0.101 to 0.025) | −0.082 (−0.559 to 0.157) |
| RP average airway area per slice | −0.025 (−0.116 to 0.019) | −0.154 (−0.656 to 0.117) |
| RP minimum area | −0.0002 (−0.025 to 0.018) | −0.002 (−0.156 to 0.107) |
| RP minimum AP distance | 0.027 (−0.052 to 0.189) | 0.166 (−0.311 to 1.270) |
| RP minimum lateral distance | 0.037 (−0.033 to 0.146) | 0.229 (−0.194 to 0.913) |
| RG airway volume | 0.002 (−0.034 to 0.032) | 0.013 (−0.205 to 0.188) |
| RG average airway area per slice | 0.030 (−0.040 to 0.120) | 0.184 (−0.230 to 0.814) |
| RG minimum area | 0.040 (−0.060 to 0.133) | 0.246 (−0.405 to 0.667) |
| RG minimum AP distance | 0.011 (−0.030 to 0.048) | 0.065 (−0.180 to 0.285) |
| RG minimum lateral distance | −0.006 (−0.048 to 0.023) | −0.034 (−0.296 to 0.137) |
| Soft tissue volumes | ||
| Combined soft tissues | 0.020 (−0.041 to 0.057) | 0.122 (−0.249 to 0.330) |
| Soft palate | 0.006 (−0.036 to 0.039) | 0.039 (−0.209 to 0.247) |
| Genioglossus | −0.004 (−0.072 to 0.036) | −0.026 (−0.426 to 0.235) |
| Other tongue | 0.002 (−0.053 to 0.030) | 0.014 (−0.333 to 0.170) |
| Tongue fat | 0.225 (0.049 to 0.413) | 1.255 (0.238 to 2.572) |
| Total tongue | −0.003 (−0.077 to 0.036) | −0.021 (−0.443 to 0.223) |
| Epiglottis | 0.004 (−0.043 to 0.053) | 0.023 (−0.281 to 0.307) |
| Fat pads | 0.007 (−0.058 to 0.052) | 0.046 (−0.355 to 0.318) |
| Pterygoid | −0.031 (−0.123 to 0.068) | −0.189 (−0.759 to 0.393) |
| RP lateral walls | 0.042 (−0.011 to 0.121) | 0.255 (−0.064 to 0.705) |
| RG lateral walls | −0.019 (−0.082 to 0.034) | −0.116 (−0.539 to 0.190) |
| Total lateral walls | 0.009 (−0.061 to 0.123) | 0.058 (−0.400 to 0.649) |
| Abdominal fat volumes | ||
| Abdominal visceral fat | −0.043 (−0.183 to 0.090) | −0.289 (−1.303 to 0.583) |
| Abdominal subcutaneous fat | 0.001 (−0.121 to 0.119) | 0.004 (−0.792 to 0.841) |
| Abdominal total fat | −0.018 (−0.153 to 0.103) | −0.120 (−1.029 to 0.742) |
Definition of abbreviations: AP = anterior–posterior; CI = confidence interval; RG = retroglossal; RP = retropalatal.
Significant values are shown in bold.
Estimate of indirect (mediating) effect and bootstrapped 95% CI.
All models corrected for age, sex, race, and height.
Figure 5.
Mediation of percentage change in weight and apnea–hypopnea index (AHI) by percentage change in tongue fat. Results of the single mediator model of percent change in tongue fat volume mediating the relationship between percent change in weight and in AHI are shown. Unstandardized path coefficients, interpreted as the expected percentage change in outcome for a 1% change in predictor, of the relationships between percent weight change and percent change in tongue fat (path a = 1.168), between percent change in tongue fat and percent change in AHI (path b = 1.074), and the remaining direct effect between percent change in weight and percent change in AHI (path c′ = 2.337) are also shown. Significance of path coefficients is denoted as: *P < 0.05, **P < 0.01, and ***P < 0.001.
Discussion
This study of patients with obesity and OSA undergoing lifestyle modification or bariatric surgery is the first to show that weight loss decreases tongue fat, and that the reduction in tongue fat is a mediator of the improvement in AHI. Primary findings include: 1) weight loss was significantly associated with reduced tongue fat volume, pterygoid volume, and total lateral wall volume; 2) strong correlations were observed between reductions in tongue fat volume and reductions in AHI; and 3) reduction in tongue fat volume was the primary upper airway mediator of the relationship between reductions in weight and AHI. Beyond providing important mechanistic insights, these results suggest that tongue fat could be a potential new target for OSA therapy.
Effect of Weight Loss on Upper Airway Caliber and Surrounding Soft Tissues
Several upper airway measurements changed with weight loss, including RP airway shape and volumes of tongue fat, pterygoid, and the lateral walls. However, other upper airway measurements showed no changes. Thus, weight loss may differentially affect upper airway anatomy; the pathogenesis of this is unclear, but could be genetically determined.
Weight loss reduces adipose tissue volume. Thus, the reduction in tongue fat was expected. However, reductions were also observed for the lateral walls and pterygoid, both of which do not contain fat deposits observable with MRI (although intramyocellular lipid droplets have been observed using electron microscopy in the pharyngeal constrictors that make up the lateral walls) (29). The mechanisms by which weight loss affects soft tissues likely differ for tissues that are primarily fat versus relatively fat free (30–32). Analyses have shown reduced muscle mass and volume with weight loss (32–36), which could account for reductions in pterygoid and lateral wall volumes. The change in lateral wall volume may be due to other mechanisms, including reduced size of the parapharyngeal fat pads (providing space for the lateral walls) and/or tracheal tug (putting tension and thereby narrowing the lateral walls) secondary to improved lung volume with weight loss.
The repeated trauma of obstruction with OSA may also trigger an edematous response (37). As OSA improves with weight loss, the trauma becomes less severe, reducing the inflammation of pharyngeal tissues. Although this would explain the reduction in lateral wall and pterygoid volumes, it does not account for the lack of change in soft palate volume. Because the soft palate contains fat (38), high-resolution Dixon imaging (18) may be required to detect fat-specific effects, as seen in the tongue. Alternatively, the soft palate has been shown to be inflamed and fibrosed in subjects with apnea (39), and weight loss should not reverse fibrosis. Ultimately, differences in the changes of distinct upper airway soft tissues with weight loss underscore the complexity of these relationships. Understanding the reasons for these differences may provide insight into OSA heterogeneity, and inform personalized treatments.
Tongue Fat as a Potential Therapeutic Target
This study observed strong correlations between tongue fat reduction and improvement in AHI, and mediation analyses supported changes in tongue fat as the primary upper airway mediator between weight loss and AHI reduction. Although the mechanism for this relationship is unknown, reduction in tongue fat affects tongue size, and may increase upper airway caliber or improve tongue function. In particular, fat can infiltrate the muscle bundles and affect muscle strength, and obesity adversely affects muscle function, with inverse relationships between muscle lipid content and muscle force, velocity, and power (29, 32, 40, 41). Thus, reduced tongue fat should improve muscle function and could prevent collapsibility during sleep. Regardless of mechanism, our results underscore the potential efficacy of OSA therapies that reduce tongue fat.
Although not directly studied, several potential therapies exist. Dixon MRI before and after these interventions is a logical step to determine feasibility and efficacy. Upper airway exercises improve OSA and reduce AHI (42–44); reduced tongue fat is one potential mechanism. Tongue fat may differentially respond to weight loss approaches that vary in dietary composition, although this remains to be investigated. Cold therapies could also potentially remove tongue fat. For example, cryolipolysis is a noninvasive cooling technique that lyses adipocytes and is effective and safe for reducing abdominal and submental fat (45, 46); a similar technique may reduce tongue fat. Although experimental, our data provide the foundation for investigation of these therapies through animal or human studies.
Our study may also explain why upper airway surgery is not more effective in treating OSA. Coblation has been used to treat patients with OSA by reducing tongue size, but has limited efficacy (47, 48). Coblation does not discriminate between muscle and fat, but instead uses radiofrequency and water to generate a plasma that vaporizes all soft tissue types. Thus, our results demonstrating a specific role for tongue fat volume could explain the observed lack of efficacy. If only fat tissue was removed, coblation could be more effective. Future studies are warranted to study this.
Measurement Reproducibility
Our results confirm reproducibility of MRI measurements at two time points. Nearly all measures showed substantial or almost perfect reproducibility within weight-stable individuals. Moderate-to-fair reproducibility was observed for fat pad volume, as well as total and subcutaneous abdominal fat. The likely explanation for this comparatively lower reproducibility is related to lumbar flexion/extension (which is difficult to control) and its effect on the L4–L5 junction, which is the inferior boundary for the abdominal fat measurements. Depending on the amount of lumbar flexion/extension, the region of interest analyzed may be different by one MRI slice, which can alter the quantitative abdominal fat measures. Nonetheless, our results are consistent with our prior studies demonstrating the validity and reproducibility of volumetric measurements quantified by MRI. Previously (20), we demonstrated the accuracy of volumetric measures against a phantom of known volume, the reliability of analyses on the same images, and high reproducibility on repeated MRI taken approximately 1 month apart. Similarly, our study on tongue fat demonstrated high reproducibility of the measurement technique (18). Moreover, our previous study on abdominal fat measurements demonstrated high reproducibility across multiple raters on repeated images (21). Thus, results from the present study extend evidence of reproducibility to a 6-month follow-up period in a weight-stable population.
Limitations
One limitation of using MRI at multiple time points is that anatomic changes may reflect MRI variability (e.g., differences in head and/or neck position), rather than solely the effect of weight loss. The use of standardized protocols and observation that nearly all upper airway measurements showed substantial or almost perfect reproducibility in weight-stable patients mitigates this concern. Including medical and surgical weight loss could be viewed as a limitation. However, using multiple types of weight loss interventions increased variability in weight changes (augmenting statistical power) and improves generalizability. Ultimately, we were able to show changes to the upper airway soft tissues and abdominal fat across different treatments and weight loss amounts. However, 6 months may not be enough time for all structures to show meaningful changes; longer studies should be conducted.
The lack of significant mediation of airway size on the relationship between weight change and AHI may reflect difficulties in measuring airway caliber with MRI during wakefulness. Airway caliber changes during inspiration and expiration (49, 50), but our imaging sequences were performed over several minutes, resulting in average measurements of airway size. Averages may not be sensitive enough to detect mediating effects. In future studies, dynamic MRI should be performed to better capture the effect of awake airway dimensional changes with weight loss.
Conclusions
This study is the first to use volumetric MRI to examine changes in airway sizes, pharyngeal soft tissues, and abdominal fat with weight loss in persons with obesity and OSA. We confirmed that our analysis techniques are a reliable means of quantifying the size of upper airway structures over a 6-month period. Weight loss reduced adipose tissue volumes in the abdomen and upper airway (in particular tongue fat), as well as volumes of soft tissues consisting primarily of fat-free mass (lateral walls and pterygoid). Analyses indicated that reduction in tongue fat was the primary upper airway mediator of the relationship between reductions in weight and AHI. These results elucidate, in part, the mechanism by which weight loss improves OSA, and provide targets for potential new therapies in lieu of weight loss.
Supplementary Material
Footnotes
Supported by NIH grants R01HL089447 and P01HL094307.
Author Contributions: Conception and design—D.B.S., N.W., A.I.P., and R.J.S.; analysis and interpretation—S.H.W., B.T.K., Y.Z., B.S., D.A.T., and R.J.S.; drafting of the manuscript—S.H.W., B.T.K., and R.J.S.; critical revision—S.H.W., B.T.K., A.W., Y.Z., B.S., D.B.S., D.A.T., N.W., A.I.P., and R.J.S.; final approval of the version to be published—S.H.W., B.T.K., A.W., B.S., D.B.S., D.A.T., N.W., A.I.P., and R.J.S.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.201903-0692OC on January 10, 2020
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319:1723–1725. doi: 10.1001/jama.2018.3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, et al. Sleep AHEAD Research Group. Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care. 2009;32:1017–1019. doi: 10.2337/dc08-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foster GD, Borradaile KE, Sanders MH, Millman R, Zammit G, Newman AB, et al. Sleep AHEAD Research Group of Look AHEAD Research Group. A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the Sleep AHEAD study. Arch Intern Med. 2009;169:1619–1626. doi: 10.1001/archinternmed.2009.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berger G, Berger R, Oksenberg A. Progression of snoring and obstructive sleep apnoea: the role of increasing weight and time. Eur Respir J. 2009;33:338–345. doi: 10.1183/09031936.00075408. [DOI] [PubMed] [Google Scholar]
- 5.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 6.Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284:3015–3021. doi: 10.1001/jama.284.23.3015. [DOI] [PubMed] [Google Scholar]
- 7.Tuomilehto H, Seppä J, Uusitupa M, Tuomilehto J, Gylling H Kuopio Sleep Apnea Group. Weight reduction and increased physical activity to prevent the progression of obstructive sleep apnea: a 4-year observational postintervention follow-up of a randomized clinical trial. [corrected] JAMA Intern Med. 2013;173:929–930. doi: 10.1001/jamainternmed.2013.389. [Published erratum appears in JAMA Intern Med 173:996.] [DOI] [PubMed] [Google Scholar]
- 8.Kuna ST, Reboussin DM, Borradaile KE, Sanders MH, Millman RP, Zammit G, et al. Sleep AHEAD Research Group of the Look AHEAD Research Group. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep (Basel) 2013;36:641–649A. doi: 10.5665/sleep.2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hudgel DW, Patel SR, Ahasic AM, Bartlett SJ, Bessesen DH, Coaker MA, et al. American Thoracic Society Assembly on Sleep and Respiratory Neurobiology. The role of weight management in the treatment of adult obstructive sleep apnea: an official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e70–e87. doi: 10.1164/rccm.201807-1326ST. [DOI] [PubMed] [Google Scholar]
- 10.Johansson K, Neovius M, Lagerros YT, Harlid R, Rössner S, Granath F, et al. Effect of a very low energy diet on moderate and severe obstructive sleep apnoea in obese men: a randomised controlled trial. BMJ. 2009;339:b4609. doi: 10.1136/bmj.b4609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tuomilehto HP, Seppä JM, Partinen MM, Peltonen M, Gylling H, Tuomilehto JO, et al. Kuopio Sleep Apnea Group. Lifestyle intervention with weight reduction: first-line treatment in mild obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179:320–327. doi: 10.1164/rccm.200805-669OC. [DOI] [PubMed] [Google Scholar]
- 12.Tuomilehto H, Gylling H, Peltonen M, Martikainen T, Sahlman J, Kokkarinen J, et al. Kuopio Sleep Apnea Group. Sustained improvement in mild obstructive sleep apnea after a diet- and physical activity–based lifestyle intervention: postinterventional follow-up. Am J Clin Nutr. 2010;92:688–696. doi: 10.3945/ajcn.2010.29485. [DOI] [PubMed] [Google Scholar]
- 13.Newman AB, Foster G, Givelber R, Nieto FJ, Redline S, Young T. Progression and regression of sleep-disordered breathing with changes in weight: the Sleep Heart Health Study. Arch Intern Med. 2005;165:2408–2413. doi: 10.1001/archinte.165.20.2408. [DOI] [PubMed] [Google Scholar]
- 14.Feigel-Guiller B, Drui D, Dimet J, Zair Y, Le Bras M, Fuertes-Zamorano N, et al. Laparoscopic gastric banding in obese patients with sleep apnea: a 3-year controlled study and follow-up after 10 years. Obes Surg. 2015;25:1886–1892. doi: 10.1007/s11695-015-1627-5. [DOI] [PubMed] [Google Scholar]
- 15.Joosten SA, Hamilton GS, Naughton MT. Impact of weight loss management in OSA. Chest. 2017;152:194–203. doi: 10.1016/j.chest.2017.01.027. [DOI] [PubMed] [Google Scholar]
- 16.Joosten SA, Khoo JK, Edwards BA, Landry SA, Naughton MT, Dixon JB, et al. Improvement in obstructive sleep apnea with weight loss is dependent on body position during sleep. Sleep. 2017;40:zsx047. doi: 10.1093/sleep/zsx047. [DOI] [PubMed] [Google Scholar]
- 17.Schwab RJ, Pasirstein M, Pierson R, Mackley A, Hachadoorian R, Arens R, et al. Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med. 2003;168:522–530. doi: 10.1164/rccm.200208-866OC. [DOI] [PubMed] [Google Scholar]
- 18.Kim AM, Keenan BT, Jackson N, Chan EL, Staley B, Poptani H, et al. Tongue fat and its relationship to obstructive sleep apnea. Sleep (Basel) 2014;37:1639–1648. doi: 10.5665/sleep.4072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25:2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Welch KC, Foster GD, Ritter CT, Wadden TA, Arens R, Maislin G, et al. A novel volumetric magnetic resonance imaging paradigm to study upper airway anatomy. Sleep. 2002;25:532–542. [PubMed] [Google Scholar]
- 21.Maislin G, Ahmed MM, Gooneratne N, Thorne-Fitzgerald M, Kim C, Teff K, et al. Single slice vs. volumetric MR assessment of visceral adipose tissue: reliability and validity among the overweight and obese. Obesity (Silver Spring) 2012;20:2124–2132. doi: 10.1038/oby.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 23.Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75:800–802. [Google Scholar]
- 24.Hochberg Y, Benjamini Y. More powerful procedures for multiple significance testing. Stat Med. 1990;9:811–818. doi: 10.1002/sim.4780090710. [DOI] [PubMed] [Google Scholar]
- 25.Huang Y, Hsu JC. Hochberg’s step-up method: cutting corners off Holm’s step-down method. Biometrika. 2007;94:965–975. [Google Scholar]
- 26.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 27.Hayes AF. Introduction to mediation, moderation and conditional process analysis: a regression-based approach, 2nd ed. New York: Guilford Press; 2018.
- 28.Mallinckrodt B, Abraham WT, Wei M, Russell DW. Advances in testing the statistical significance of mediation effects. J Couns Psychol. 2006;53:372–378. [Google Scholar]
- 29.Choi SJ, Files DC, Zhang T, Wang ZM, Messi ML, Gregory H, et al. Intramyocellular lipid and impaired myofiber contraction in normal weight and obese older adults. J Gerontol A Biol Sci Med Sci. 2016;71:557–564. doi: 10.1093/gerona/glv169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dulloo AG, Jacquet J, Girardier L. Autoregulation of body composition during weight recovery in human: the Minnesota Experiment revisited. Int J Obes Relat Metab Disord. 1996;20:393–405. [PubMed] [Google Scholar]
- 31.Elia M, Stubbs RJ, Henry CJ. Differences in fat, carbohydrate, and protein metabolism between lean and obese subjects undergoing total starvation. Obes Res. 1999;7:597–604. doi: 10.1002/j.1550-8528.1999.tb00720.x. [DOI] [PubMed] [Google Scholar]
- 32.Cava E, Yeat NC, Mittendorfer B. Preserving healthy muscle during weight loss. Adv Nutr. 2017;8:511–519. doi: 10.3945/an.116.014506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–1229. doi: 10.1056/NEJMoa1008234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ryan AS, Harduarsingh-Permaul AS. Effects of weight loss and exercise on trunk muscle composition in older women. Clin Interv Aging. 2014;9:395–402. doi: 10.2147/CIA.S56662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yoshimura E, Kumahara H, Tobina T, Matsuda T, Watabe K, Matono S, et al. Aerobic exercise attenuates the loss of skeletal muscle during energy restriction in adults with visceral adiposity. Obes Facts. 2014;7:26–35. doi: 10.1159/000358576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chomentowski P, Dubé JJ, Amati F, Stefanovic-Racic M, Zhu S, Toledo FG, et al. Moderate exercise attenuates the loss of skeletal muscle mass that occurs with intentional caloric restriction–induced weight loss in older, overweight to obese adults. J Gerontol A Biol Sci Med Sci. 2009;64:575–580. doi: 10.1093/gerona/glp007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barbarroja-Escudero J, Asunsolo-Del-Barco A, Sanchez-Gonzalez MJ, Rodriguez-Rodriguez M, Alvarez-Mon M. Heterogeneous predisposing factors and etiology of edema of the uvula in a Spanish population. J Investig Allergol Clin Immunol. 2019;29:280–286. doi: 10.18176/jiaci.0324. [DOI] [PubMed] [Google Scholar]
- 38.Berger G, Gilbey P, Hammel I, Ophir D. Histopathology of the uvula and the soft palate in patients with mild, moderate, and severe obstructive sleep apnea. Laryngoscope. 2002;112:357–363. doi: 10.1097/00005537-200202000-00028. [DOI] [PubMed] [Google Scholar]
- 39.Boyd JH, Petrof BJ, Hamid Q, Fraser R, Kimoff RJ. Upper airway muscle inflammation and denervation changes in obstructive sleep apnea. Am J Respir Crit Care Med. 2004;170:541–546. doi: 10.1164/rccm.200308-1100OC. [DOI] [PubMed] [Google Scholar]
- 40.Lafortuna CL, Tresoldi D, Rizzo G. Influence of body adiposity on structural characteristics of skeletal muscle in men and women. Clin Physiol Funct Imaging. 2014;34:47–55. doi: 10.1111/cpf.12062. [DOI] [PubMed] [Google Scholar]
- 41.Therkelsen KE, Pedley A, Hoffmann U, Fox CS, Murabito JM. Intramuscular fat and physical performance at the Framingham Heart Study. Age (Dordr) 2016;38:31. doi: 10.1007/s11357-016-9893-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Puhan MA, Suarez A, Lo Cascio C, Zahn A, Heitz M, Braendli O. Didgeridoo playing as alternative treatment for obstructive sleep apnoea syndrome: randomised controlled trial. BMJ. 2006;332:266–270. doi: 10.1136/bmj.38705.470590.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guimarães KC, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filho G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2009;179:962–966. doi: 10.1164/rccm.200806-981OC. [DOI] [PubMed] [Google Scholar]
- 44.Verma RK, Johnson J JR, Goyal M, Banumathy N, Goswami U, Panda NK. Oropharyngeal exercises in the treatment of obstructive sleep apnoea: our experience. Sleep Breath. 2016;20:1193–1201. doi: 10.1007/s11325-016-1332-1. [DOI] [PubMed] [Google Scholar]
- 45.Ingargiola MJ, Motakef S, Chung MT, Vasconez HC, Sasaki GH. Cryolipolysis for fat reduction and body contouring: safety and efficacy of current treatment paradigms. Plast Reconstr Surg. 2015;135:1581–1590. doi: 10.1097/PRS.0000000000001236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lipner SR. Cryolipolysis for the treatment of submental fat: review of the literature. J Cosmet Dermatol. 2018;17:145–151. doi: 10.1111/jocd.12495. [DOI] [PubMed] [Google Scholar]
- 47.Hwang CS, Kim JW, Kim JW, Lee EJ, Kim CH, Yoon JH, et al. Comparison of robotic and coblation tongue base resection for obstructive sleep apnoea. Clin Otolaryngol. 2018;43:249–255. doi: 10.1111/coa.12951. [DOI] [PubMed] [Google Scholar]
- 48.Cammaroto G, Montevecchi F, D’Agostino G, Zeccardo E, Bellini C, Galletti B, et al. Tongue reduction for OSAHS: TORSs vs coblations, technologies vs techniques, apples vs oranges. Eur Arch Otorhinolaryngol. 2017;274:637–645. doi: 10.1007/s00405-016-4112-4. [DOI] [PubMed] [Google Scholar]
- 49.Schwab RJ, Gefter WB, Hoffman EA, Gupta KB, Pack AI. Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am Rev Respir Dis. 1993;148:1385–1400. doi: 10.1164/ajrccm/148.5.1385. [DOI] [PubMed] [Google Scholar]
- 50.Feng Y, Keenan BT, Wang S, Leinwand S, Wiemken A, Pack AI, et al. Dynamic upper airway imaging during wakefulness in obese subjects with and without sleep apnea. Am J Respir Crit Care Med. 2018;198:1435–1443. doi: 10.1164/rccm.201711-2171OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.