Abstract
Rhinoentomophthoromycosis due to Conidiobolus coronatus is a rare, chronic, granulomatous disease, occurring mainly in tropical countries including India. We report two cases of rhinoentomophthoromycosis in an 18-year-old female and a farmer of 35 years residents of Chhattisgarh shifted from Madhya Pradesh and Orrisa. It was diagnosed by microscopy and isolation C. coronatus in culture. The patient presented with a swollen nose with obstruction that had progressed slowly over 1 year. His nasal swelling was bilateral, diffuse, mildly tender, erythematous, nonpitting, with mucosal crusting and hypertrophy of inferior turbinates but no regional lymphadenopathy. Culture of tissue from the nasal biopsy on sabouraud dextrose agar yielded multiple colonies of a mold with satellite smaller colonies at periphery. The isolate demonstrated the macroscopic and microscopic morphologic characteristics of C. coronatus. The patients were earlier treated with itraconazole or its combination with potassium iodide and the patients were treated successfully with amphotericin B.
Keywords: Antifungal, conidiobolomycosis, Conidiobolus coronatus, mucorales, rhinoentomophthoromycosis
INTRODUCTION
Entomophthoramycosisisis caused by Basidiobolus ranarum and nasofacial or rhinoentomophthoramycosisis caused primarily by Conidiobolus coronatus. Entomophthoramycosis is used to distinguish this disease from clinical forms that is caused by Mucorales which is clinically known as rhino-orbital mucormycosis.[1]
The cases of Conidiobolus has been reported from Central America, equatorial Africa, India.[2] It is reported from Tamil Nadu, Madras, Ludhiana, Delhi, Mangalore, India.[3,4,5,6] No case of rhinoentomophthoramycosis from Chhattisgarh was reported. Recently, single clinical case of basidiobolomycosis has been reported from Chhattisgarh.[7]
Herewith, a series of two cases diagnosed of nasofacial rhinoentomopthoromycosis has been discussed for the first time from the state of Chhattisgarh.
CASE REPORTS
Case 1
A 18-year-old girl presented to the ear, nose, throat, (ENT) Head-and-neck surgery outpatient department (OPD) of our institute with complaints of bleeding from the right nostril, on and off along with swelling of the upper lip for the past 6 months. Her disease started with lateral nasal swelling which was gradual in onset for that she was treated with right lateral rhinotomy with excision of the nasal mass. On histopathology, her lesions showed chronic granulomatous pattern with the possibility of sarcoidosis. The lesion recurred again with similar complaints and provisional diagnosis of infective subcutaneous granulomatous lesion/tuberculosis/sarcoidosis/leprosy/rhinoscleroma was made. After a review of the same histopathology of slides, the impression of nonnecrotizing granulomatous inflammation with possible tuberculous etiology was made. She was put on antitubercular therapy but within 2 months, she developed adverse drug reactions. A second-time biopsy was performed from the right ala of the nose and from right middle meatus, and the histopathology findings were the same as the previous. As there was a significant regression of the lesion, the histopathology slides of the second biopsy were again reviewed and revealed the presence of eosinophil, rich mycotic granulomatous inflammation. Fungal stain revealed thick, nonseptate branching hyphal forms of zygomycosis species. She was advised intravenous amphotericin B and posaconazole which was not taken by her due to financial constraints.
After 4 months she visited the ENT, Head-and-Neck Surgery OPD of our institute. On local examination, swelling over the upper lip and bleeding from the nasal floor was observed. No abnormality detected on examination of the neck. Nasal endoscopy was done which showed septal deviation with synechiae present between the septum and left side of the nose. On the right-side crusts were present in the nasal cavity with mucoid discharge. Mass or polyp was absent. Swelling was also present on both anterior and posterior aspect extending up to the ventricular border crossing the midline. It was firm, nontender and nonfluctuant [Figure 1] with the congested posterior pharyngeal wall. The mucosal biopsy was taken from the upper lip with all aseptic precautions and sent for KOH mount, fungal culture.
Figure 1.

Presentation of patient with swelling on upper lip
KOH showed ribbon-like broad hyaline sparsely septate hyphae [Figure 2]. Growth on sabouraud dextrose agar at 27°C: starts appearing after 48 h and after 3 days of incubation white colored, waxy to powdery with reverse was pale with satellite colonies at periphery seen [Figure 3]. Lacto phenol cotton blue stain of colonies revealed broad sparsely sepatate hyphae, indistinguishable sporangiophore and hyphae, sporangioles surface was smooth, covered with papilla [Figure 4]. It is identified as C. coronatus.[8]
Figure 2.
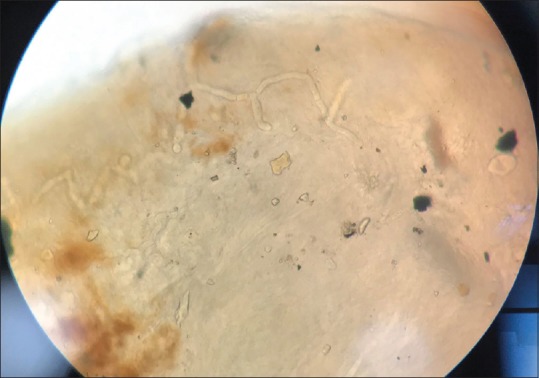
KOH ribbon like hyaline sparsely septate hyphae
Figure 3.
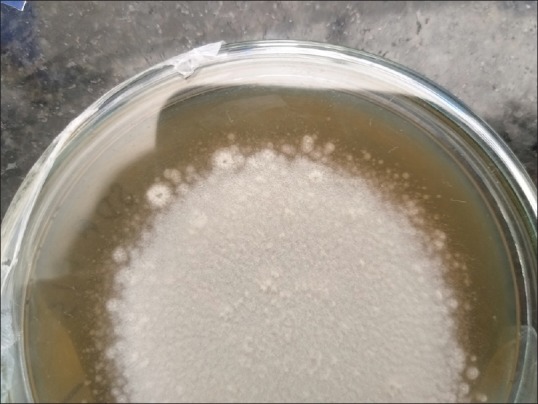
Colony morphology on sabouraud dextrose agar after 3 days of incubation white satellite colonies waxy to powdery
Figure 4.
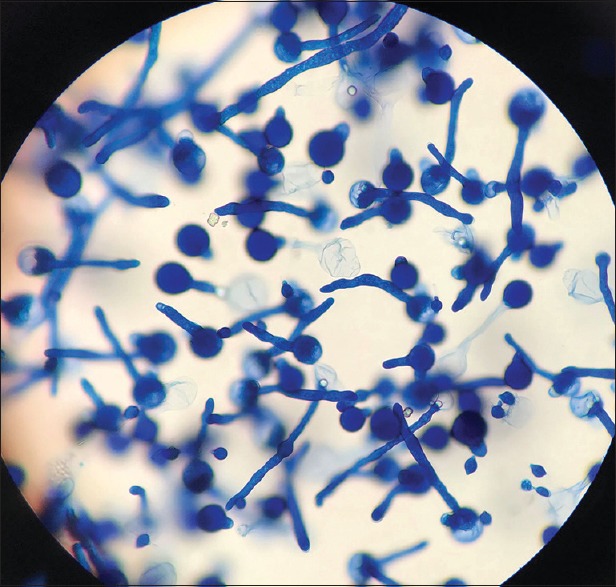
Lactophenol cotton blue mount of colonies showing unbranched sporophore bears single celled round spores
After culture confirmation patient was treated with itraconazole and saturated solution of potassium iodide (KI) after doing the hormonal level. As her hormonal levels disturbed, she was shifted to amphotericin B. The patient responded well to the treatment [Figure 5].
Figure 5.

Presentation of patient after recovery
Just after the interval of 2 weeks, the second case which is discussed below came across.
Case 2
A 37-year-old, diabetic farmer had noticed protruding mass and swelling on the right side of the nose, which was painless, gradually increased in size which leads to nasal obstruction after 4 months. Contrast-enhanced computed tomography of paranasal sinuses (PNS), fine-needle aspiration cytology (FNAC) was suggestive of papilloma and fibrohistiocytic lesion, respectively. Histopathology report was suggestive of rhinoentomophthoromycosis and itraconazole was given. However, the swelling reappeared during antifungal therapy and involved the left side of the nose. Repeat FNAC showed granulomatous lesion possibly of fungal etiology.
When she had visited our institute, on examination, swelling was seen on both sides of the nose, right > left side and extending inferiorly over dorsum, had indistinct margins and stony hard consistency, nontender and immobile on palpation. Diagnostic nasal endoscopy was done in which fleshy reddish mass occupying the right nasal cavity reaching up to floor and bleeding on touch was identified. Mild deviated nasal septum to left was noted in the left nasal cavity and nasopharynx was clear. His provisional diagnosis was rhinoentomophthoromycosis. His serological investigations for HIV, HbsAg and hepatitis C virus for patients were negative.
Biopsied tissue was sent for KOH and fungal culture. Similar observations were found mentioned in case one. C. coronatus was isolated and reported. The patient was started on amphotericin B. Planned radical maxillectomy with skin lesion debridement was done after 3 weeks. Tissues removed and sent for fungal KOH and culture. It was negative for fungus. Total amphotericin B administered for 27 days, following which the patient developed and switched to oral ketoconazole. No residual fungal evidence was found on multiple clinical examinations.
DISCUSSION
Entomophthoramycosisis subcutaneous mycosis localized to the nasofacial region caused by C. coronatus or Conidiobolus incongruus or Conidiobolus lamprauges.[3] This fungus is normally found in soil and rotten plant material.
It is an uncommon disease reported from the tropical and subtropical zones. It is disease of immunocompetent individuals while Mucorales infect immunocompromised individuals. The disorder is found particularly in healthy outdoor workers of tropical rainforests of West Africa. It is also reported from Burkitt's lymphoma.[2]
Both the cases were visited the institute with the gap of 15 days, and it states us to be vigilant regarding these rare cases where may found more cases.
The age variability was observed in the cases reported from India and reviewed by Chowdhary et al.[9] Nose was commonly affected site followed by cheek and upper lips with PNS. Subramanian and Sobel described the involvement of the vagina for this infection.[10] Pulmonary and cardiac involvement with angioinvasion in a patient with lymphoma had been reported by Walsh et al.[11] A nasal lesion in horse and dog was reported by Zamos et al.[12] and Lemairé et al.,[13] respectively. The most common species isolated was C. coronatus was concordant with other reports.[9]
Chowdhary et al. mentioned the case confirmation by histopathological evidence, in the first case repeated examination of histopathology, could not make confirmed diagnosis or differentiate from mucormycosis.[9,14] One of the differential diagnoses was tuberculosis and she was treated for that.
No defined antifungal therapy of rhinoentomo phthoramycosis is recommended, as it is not frequently reported.KI, miconazole, cotrimoxazole, ketoconazole, itraconazole, amphotericin B, terbinafine, hyperbaric oxygen and surgical debridement have been used in various combinations with variable success.[9] Although it is mentioned that saturated KI is the treatment of choice due to its ease of administration and low cost, in our first case, saturated KI disturbed the hormonal levels and also itraconazole had not responded. She was successfully treated with Amphotericin B while in second case itraconazole had not responded and had to shift on amohotericin B.
Among people who may have limited access to appropriate medical care has hidden the epidemiology of this geographical area. Hence, reporting cases most often will help in the diagnosis and management of the disease.
CONCLUSION
It is concluded that clinical suspicious and appropriate investigations are needed to reach the confirmatory diagnosis of infrequently encountered infections like nasofacial rhinoentomophthoramycosis. All the suspicious cases should be investigated and reported to know the prevalence. It will be also helpful to standardize and implement the appropriate surgical management along with effective antifungal treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Errol Reiss H, JeanShadomy G, Lyon M. Fundamental Medical Mycology. 1st ed. New Jersey: John Wiley & Sons; 2011. [Google Scholar]
- 2.de Hoog GS, Guarro J, Gene J, Figueras MJ. Online Atlas of Clinical Fungi (beta version) The Netherlands: Westerdlink fungal Biodiversity, Centraalbureau voor Schimmelcultures; 2019. [Google Scholar]
- 3.Grüber HL. Subcutaneous phycomycosis in India. J Christ Med Assoc India. 1966;41:284–90. [PubMed] [Google Scholar]
- 4.Gruber HL. Rhino-entomophthoromycosis. J Christ Med Assoc India. 1969;44:20–4. [Google Scholar]
- 5.Klokke AH, Job CK, Warlow PF. Subcutaneous phycomycosis in India. Report of four patients with a review of the disease. Trop Geogr Med. 1966;18:20–5. [PubMed] [Google Scholar]
- 6.Ramalingam KK, Kamalam A, Venkateswaran V, Rajan NJ, Selvaraju SM, Thulasi Dhas P. Rhinoentomophthoromycosis. Indian J Otolaryngol. 1983;35:95–6. [Google Scholar]
- 7.Patro P, Das P, Sachdev D, Borkar N, Ganguly S, Hussain N. An instance of excellent response of subcutaneous zygomycosis to itraconazole monotherapy. Med Mycol Case Rep. 2019;24:13–7. doi: 10.1016/j.mmcr.2019.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Larone DH. Medically Important Fungi: A Guide to Identification. 5th ed. Washington, DC: ASM Press; 2011. [Google Scholar]
- 9.Chowdhary A, Randhawa HS, Khan ZU, Ahmad S, Khanna G, Gupta R, et al. Rhinoentomophthoromycosis due to Conidiobolus coronatus. A case report and an overview of the disease in India. Med Mycol. 2010;48:870–9. doi: 10.3109/13693786.2010.486010. [DOI] [PubMed] [Google Scholar]
- 10.Subramanian C, Sobel JD. A case of Conidiobolus coronatus in the vagina. Med Mycol. 2011;49:427–9. doi: 10.3109/13693786.2010.537700. [DOI] [PubMed] [Google Scholar]
- 11.Walsh TJ, Renshaw G, Andrews J, Kwon-Chung J, Cunnion RC, Pass HI, et al. Invasive zygomycosis due to Conidiobolus incongruus. Clin Infect Dis. 1994;19:423–30. doi: 10.1093/clinids/19.3.423. [DOI] [PubMed] [Google Scholar]
- 12.Zamos DT, Schumacher J, Loy JK. Nasopharyngeal conidiobolomycosis in a horse. J Am Vet Med Assoc. 1996;208:100–1. [PubMed] [Google Scholar]
- 13.Lemairé SL, Bauer RW, Foil CS, Roy AF. Conidiobolomycosis in a dog. Vet Derm. 1994;5:144. [Google Scholar]
- 14.Shaikh N, Hussain KA, Petraitiene R, Schuetz AN, Walsh TJ. Entomophthoramycosis: A neglected tropical mycosis. Clin Microbiol Infect. 2016;22:688–94. doi: 10.1016/j.cmi.2016.04.005. [DOI] [PubMed] [Google Scholar]


