Abstract
Patient: Male, 30-year-old
Final Diagnosis: Acute myeloid leukemia
Symptoms: Jaw numbness and pain
Medication:—
Clinical Procedure: None
Specialty: Hematology
Objective:
Rare co-existance of disease or pathology
Background:
Numb chin syndrome is a rare and under diagnosed neuropathy of the inferior alveolar branch of the trigeminal nerve usually causing a lower lip and chin anesthesia or paresthesia. The syndrome is commonly associated with broad-spectrum malignant and non-malignant conditions.
Case Report:
Here we report a case of a 30-year-old male who presented with numb chin syndrome in the form of jaw pain, paresthesia, and hypoesthesia of the mental area as the presenting symptoms of acute of myeloid leukemia with t(8;21) treated with (3+7) protocol (3 days anthracycline+7 days cytarabine). The pain and paresthesia improved but hypothesia persisted.
Conclusions:
Acute myeloid leukemia is one of the most serious causes of numb chin syndrome which should not be overlooked.
MeSH Keywords: Chin; Leukemia, Myeloid, Acute; Paresthesia
Units: Hemoglobin gm/dL (normal range: 13.0–17.0 mg/dL), platelet 103 μL (normal range: 150–400×103/μL), WBC 103/μL (normal range: 4.0–10×103/μL)
Background
Numb chin syndrome (NCS), also known as mental nerve neuropathy and earlier named hypoesthesia of the chin, is a rare and under diagnosed neuropathy of the inferior alveolar branch of the trigeminal nerve usually causing a lower lip and chin anesthesia or paresthesia [1,2]. The syndrome is commonly associated with broad-spectrum malignant and non-malignant conditions such as trauma, infection, neurologic, or odontogenic cause [3–5]. This syndrome is most often a sign of malignancy presentation, progression, or relapse [6–8].
The association of NCS with both solid tumors and hemato-logic malignancies has been estimated to be up to 30% to 50% of patients at presentation [1,4,9]. However, no extensive prospective studies were done to confirm these percentages.
The association between acute of myeloid leukemia and NCS has been described, but only a few cases have been reported in the literature (see discussion). In this case, we highlight this association to draw the attention to acute myeloid leukemia as an important differential to look for in patients with such presentation and to invite further researches in describing cytogenetic abnormalities linked to NCS.
Case Report
We report a case of 30-year-old Indian male with no significant past medical history. The patient presented initially to a health center with severe jaw pain which was present for 4 days along with decreased sensation over the entire lower jaw. He also had an on-and-off fever, malaise, and 4 kg unintentional weight loss during the preceding 1 month. There was no preceding trauma, recent skin or mucosal eruptions, or hepatitis vaccination. At the time of assessment, he looked pale and there was obvious swelling over the submandibular area bilaterally and he had restricted opening of the mouth due to pain. Neurologically, pain; touch, and temperature sensations were reduced over the mental area; however, vibration sensation and motor function were spared. Other parts of the nervous system were intact as well as the rest of other systems.
Laboratory results revealed hemoglobin of 3.6 mg/dL (normal range: 13.0–17.0 mg/dL), platelet of 12×103 μL (normal range: 150–400×103/μL), WBC of 6.3×103/μL (normal range: 4.0–10×103/μL). Based on the picture of bicytopenia, peripheral smear was sent and it showed marked neutropenia with left shift, dysplastic features, and 47% circulating blasts with some Auer rods, a picture highly suggestive of acute myeloid leukemia, and that was confirmed by flow cytometry of bone marrow aspirate with the presence of 52% abnormal precursors. Chromosome analysis revealed 45, X,-Y with t(8;21) (q22;q22); RUNX1-RUNX1T1. Infectious causes like Epstein Barr virus and human immune virus (HIV) were ruled out; of note, herpes serology was not done. Antinuclear antibodies, anti-neutrophil cytoplasmic antibodies, and rheumatoid factor were all negative.
A magnetic resonance imaging (MRI) of the head was performed, to further explore the reason of his neurological deficit, and showed subtle heterogeneous marrow signal of the bone marrow with no focal destructive bony lesions or soft tissue masses, with a possibility of underlying infiltrative process. There was also near total opacification of the left mastoid air cells suggestive of left mastoiditis, otherwise no definite focal brain parenchymal abnormality seen; all ventricles looked normal with no midline shift or deformity. The submandibular glands were normal as well. No destructive bony lesion was seen (Figures 1, 2).
Figure 1.

X-ray of skull anteroposterior view shows subtle heterogeneity of bone marrow of both mandibles with no definite focal osseous lesions.
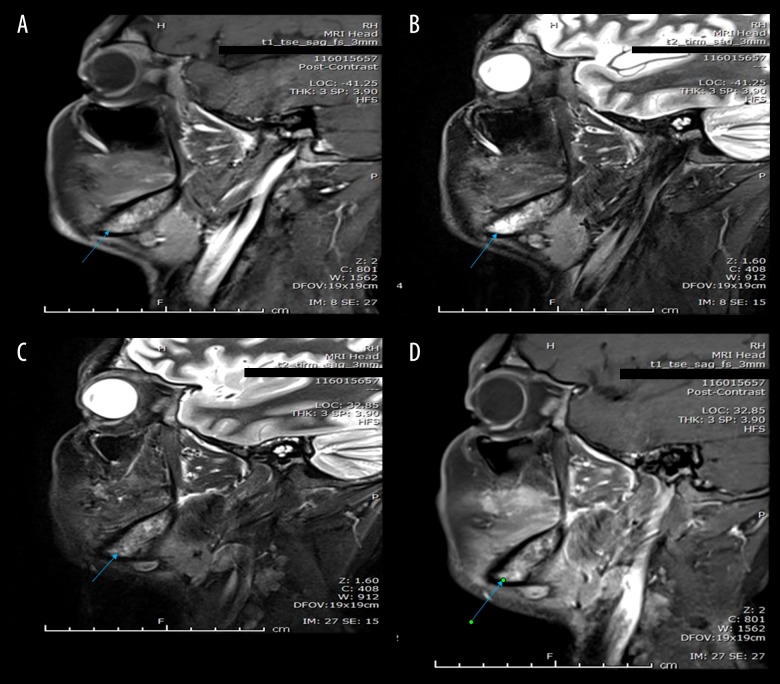
Figure 2.
(A, B) Sagittal STIR and post contrast fat saturated images of right mandible. (C, D) Sagittal STIR and post contrast fat saturated images of left mandible show heterogeneous appearance of bone marrow of mandible with high signal intensity in STIR images and heterogeneous enhancement after intravenous contrast administration (blue arrows) suggesting underlying infiltration.
After the first induction cycle with (3+7) protocol (3 days anthracycline + 7 days cytarabine), the patient had a resolution of jaw pain and swelling. Paresthesia over the left half of the mental area resolved, however, decreased sensation and pares-thesia persist over the right half of the mental area even after the second induction cycle. X-ray of the skull done 7 weeks after diagnosis showed the heterogeneous texture of the mandible.
He received a total of 2 cycles of induction and 3 cycles of consolidation, as per hospital protocol, and the end of therapy bone marrow examination revealed 4% blasts. He traveled back to his home country.
Discussion
Numb chin syndrome is a sensory neuropathy of the mental branch of the inferior alveolar nerve that presents by hypoesthesia, paresthesia, and rarely pain [1].
The non-malignant cause include: trauma, infection (bacterial, viral, Lyme disease, syphilis, HIV, and osteomyelitis), multiple sclerosis, benign sensory trigeminal neuropathy, radiotherapy, chemical exposure, vasculitis, systemic amyloidosis, sickle cell disease, sarcoidosis, diabetes mellitus, and vertebro-basilar insufficiency [23].
Any lesion along the course of the trigeminal nerve from its nucleolus in the Pons down to the mandibular endings can result in numb chin syndrome. The proposed mechanisms for malignancy-associated NCS are: direct infiltration of the bone or nerve, leptomeningeal seeding, or inflammation or compression of the nerve [23].
The malignant causes are very important to know and to be noticed by physicians, as NCS can be the first sign of both solid and hematological malignancies, and it can be the sign of recurrence as well. It is reported with metastatic malignancies of the liver, lung, kidney, breast, and prostate, among others. We suggest as an approach the taking detailed history including previous history of malignancies and risk factors, physical examination of the aforementioned solid organs followed by appropriate imaging.
For hematological malignancies, in particular, there are very few cases reported in the literature of this sign to be the presenting sign. It has been reported mostly with non-Hodgkin lymphoma and acute lymphoblastic leukemia. For acute myeloid leukemia, 5 cases were reported to our knowledge and literature review. Our case is the sixth case. One of the most interesting findings in our case, the chromosomal abnormalities, which were t(8,21), which carries favorable prognosis, same like Jenkins et al. reported case who is a 33-year-old female presented with chills, malaise, nausea and vomiting, and numbness of the lower lip and chin. Her computed tomography scan of the brain was normal and she had leukocytosis with circulating blast forms, morphologically it was consistent with FAB M2 subtype, numbness improved completely on day 12 of induction chemotherapy with cytarabine and daunorubicin (7+3) in contrast to our case in which pain resolved but paresthesia persisted [1].
Another observation that all the cases reported were de novo acute myeloid leukemia. See Table 1 for a summary of the cases.
Table 1.
Summary of acute myeloid leukemia (AML) with numb chin syndrome case reports and some of the acute lymphocytic leukemia (ALL) with numb chin syndrome cases.
| Author | Year | Age | Gender | Primary diagnosis | Chromosome analysis | NCS timing |
|---|---|---|---|---|---|---|
| Barrett [17] | 1985 | 28 | M | ALL | NA | Progression |
| Nagano [15] | 1991 | 21 | F | AML | NA | Presentation |
| Ohno [16] | 1994 | 32 | F | AML-M5 | NA | Presentation |
| Kuklok [18] | 1997 | 35 | M | ALL | NA | Presentation |
| Kraigher-Krainer [2] | 2008 | 11 | M | ALL (B-cell) | NA | Presentation |
| Mantadakis [19] | 2008 | 17 | M | ALL (B-cell) | 46,XY,del(9)(p22.1),add(16)(q22) and 46,XY,add(9) (p22.1),del(9) (p11.2)add(16)(q22)] | Presentation |
| Liapis [20] | 2010 | 52 | M | AMKL | (+Y, +1, +3q, −3p, −4, −5q, +6, −7q, +8, −9q, −15) | Presentation |
| Lata [13] | 2010 | 45 | M | NHL | NA | Presentation |
| Sasaki [11] | 2011 | 48 | F | Burkitt’s cell acute lymphocytic leukemia | NA | Presentation |
| Fan [12] | 2011 | 51 | F | NHL | NA | Presentation |
| Jenkins [1] | 2012 | 33 | F | AML | t(8;21) translocation | Presentation |
| Romo [21] | 2014 | 22 | M | ALL | NA | Relapse |
| Algahtani [10] | 2016 | 57 | M | Burkitt’s lymphoma/leukemia | Translocation (8;14) | Presentation |
| Algahtani [10] | 2016 | 39 | M | Burkitt’s lymphoma/leukemia | t(8;14)(q24;q32) | Presentation |
| Quintela [22] | 2017 | 27 | M | AML | 47, XX, ?8[4]/46, XY[16] | Presentation |
| Present case | 2017 | 30 | M | AML | 45, X,-Y with t(8;21) (q22;q22);RUNX1-RUNX1T1 | Presentation |
AML – acute myeloid leukemia; AML-M5 – acute monoblastic leukemia; ALL – acute lymphoblastic leukemia; AMKL – acute megakaryoblastic leukemia; NA – not available; NHL – Non-Hodgkin’s lymphoma.
It is difficult to tell whether the presentation was due to infiltration of the mental nerve itself by leukemic cells or due to entrapment caused by marrow infiltration at the mandible area. Biopsy of the mandible was not obtained as the risk of bleeding (given the severe thrombocytopenia at presentation) and further damage to the nerve outweigh the small benefit of identifying the exact pathophysiology of numb chin in this patient.
Conclusions
Acute myeloid leukemia is one of the most sinister diagnoses which should not be missed in a patient presenting with numb chin syndrome. Our case report highlights this association to encourage physicians to look deliberately for a malignant cause in patients who present with such sign without preceding trauma or infection. Further research is needed to study the link between NCS and specific cytogenetic abnormalities and its prognostic value.
Acknowledgments
Internal Medicine Residency Program, Department of Medical Education, Hamad Medical Corporation.
Abbreviations
- AML
acute myeloid leukemia;
- MNN
mental nerve neuropathy;
- NCS
numb chin syndrome
Footnotes
Department and Institution where work was done
National Center of Cancer Care and Research (NCCCR), Hamad Medical Corporation.
Conflict of interest
None.
References:
- 1.Jenkins RW, McDonald K, Greenberg CS. Numb chin syndrome in acute myeloid leukemia. Am j Med Sci. 2012;344(3):237–40. doi: 10.1097/MAJ.0b013e318256041f. [DOI] [PubMed] [Google Scholar]
- 2.Kraigher-Krainer E, Lackner H, Sovinz P, et al. Numb chin syndrome as initial manifestation in a child with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2008;51(3):426–28. doi: 10.1002/pbc.21627. [DOI] [PubMed] [Google Scholar]
- 3.Marinella M. Metastatic large cell lung cancer presenting with numb chin syndrome. Respir Med. 1997;91(4):235–36. doi: 10.1016/s0954-6111(97)90044-5. [DOI] [PubMed] [Google Scholar]
- 4.Massey EW, Moore J, Schold SC. Mental neuropathy from systemic cancer. Neurology. 1981;31(10):1277–77. doi: 10.1212/wnl.31.10.1277. [DOI] [PubMed] [Google Scholar]
- 5.Ryba F, Rice S, Hutchison I. Numb chin syndrome: An ominous clinical sign. Br Dent J. 2010;208(7):283–85. doi: 10.1038/sj.bdj.2010.292. [DOI] [PubMed] [Google Scholar]
- 6.Baskaran RK, Smith M. Numb chin syndrome – a reflection of systemic malignancy. World J Surg Oncol. 2006;4:52. doi: 10.1186/1477-7819-4-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burt RK, Sharfman WH, Karp BI, Wilson WH. Mental neuropathy (numb chin syndrome). A harbinger of tumor progression or relapse. Cancer. 1992;70(4):877–81. doi: 10.1002/1097-0142(19920815)70:4<877::aid-cncr2820700425>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 8.Seymour JF, Rodriguez MA. Mental neuropathy (Numb chin syndrome): A harbinger of tumor progression or relapse case reports. Cancer. 1993;71(3):874–75. doi: 10.1002/1097-0142(19930201)71:3<874::aid-cncr2820710336>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 9.Maillefert JF, Gazet-Maillefert MP, Tavernier C, Farge P. Numb chin syndrome. Joint Bone Spine. 1999;67(2):86–93. [PubMed] [Google Scholar]
- 10.Algahtani H, Shirah B, Bassuni W, Adas R. Bilateral numb chin syndrome as the initial presentation of Burkitt’s lymphoma/leukemia: A report of two cases and review of the literature. Case Rep Hematol. 2016;2016:3791045. doi: 10.1155/2016/3791045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sasaki M, Yamazaki H, Aoki T, et al. Bilateral numb chin syndrome leading to a diagnosis of Burkitt’s cell acute lymphocytic leukemia: A case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(3):e11–16. doi: 10.1016/j.tripleo.2010.09.066. [DOI] [PubMed] [Google Scholar]
- 12.Fan Y, Luka R, Noronha A. Non-Hodgkin lymphoma presenting with numb chin syndrome. BMJ Case Rep. 2011;2011:bcr0120113712. doi: 10.1136/bcr.01.2011.3712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lata J, Kumar P. Numb chin syndrome: A case report and review of the literature. Indian J Dent Res. 2010;21(1):135–37. doi: 10.4103/0970-9290.62795. [DOI] [PubMed] [Google Scholar]
- 14.Carbone M, Ferrera FD, Carbone L, et al. Numb chin syndrome as first symptom of diffuse large B-cell lymphoma. Case Rep Dent. 2014;2014:413162. doi: 10.1155/2014/413162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagano N, Adachi N, Ohnishi M. [Acute myelogenous leukemia with numb chin syndrome as the first symptom] Japanese Oral Society Journal. 1993;42(4):791–94. [in Japanese] [Google Scholar]
- 16.Ohno T, Yasuda Y, Furukawa H. Acute monobiastic leukemia (M5a) presenting numb chin syndrome. Am J Hematol. 1994;45(4):352. doi: 10.1002/ajh.2830450422. [DOI] [PubMed] [Google Scholar]
- 17.Barrett AP. Selective anesthesias of the inferior alveolar nerve in leukemia and lymphoma. J Oral Maxillofac Surg. 1985;43(12):992–94. doi: 10.1016/0278-2391(85)90020-5. [DOI] [PubMed] [Google Scholar]
- 18.Kuklok KB, Burton RG, Wilhelm ML. Numb chin syndrome leading to a diagnosis of acute lymphoblastic leukemia: report of a case. J Oral Maxillofac Surg. 1997;55(12):1483–85. doi: 10.1016/s0278-2391(97)90656-x. [DOI] [PubMed] [Google Scholar]
- 19.Mantadakis E, Katragkou A, Papadaki E, et al. Spinal cord compression in an adolescent with relapsed B-precursor acute lymphoblastic leukemia and mental neuropathy. Int J Hematol. 2008;88(3):294–98. doi: 10.1007/s12185-008-0159-3. [DOI] [PubMed] [Google Scholar]
- 20.Liapis K, Apostolidis I, Karmiris T, Harhalakis N. Numb chin syndrome as the initial manifestation of acute megakaryoblastic leukemia. Leuk Lymphoma. 2010;51(12):2310–11. doi: 10.3109/10428194.2010.520776. [DOI] [PubMed] [Google Scholar]
- 21.Romo CG, Jain P, Cortes JE. Numb chin syndrome by precursor B acute lymphoblastic leukemia. Am J Hematol. 2014;89(8):860–61. doi: 10.1002/ajh.23766. [DOI] [PubMed] [Google Scholar]
- 22.Quintela A, Sujobert P, Tigaud I, et al. Bone marrow necrosis in newly diagnosed acute leukemia: two case reports and review of the literature. Oncol Ther. 2017;5(1):111–18. doi: 10.1007/s40487-017-0041-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robertson CE. Numb chin syndrome. UpToDate [serial online] 2018 Sep [Cited 2019 Aug 15]: https://www.uptodate.com/contents/numb-chin-syndrome?search=numb%20chin%20syndrome&source=search_result&selectedTitle=1~2&usage_type=default&display_rank=1#H3922042884.