Abstract
Background
The prevalence of obesity has shown a dramatic increase over recent decades. Obesity is associated with underdosing of antimicrobial drugs for prophylaxis and treatment. Posaconazole is a broad-spectrum triazole antifungal drug licensed for prophylaxis and treatment of invasive fungal infections. It is unclear how posaconazole should be dosed in obese patients.
Methods
We performed a prospective study investigating the pharmacokinetics of posaconazole in morbidly obese (n = 16) and normal-weight (n = 8) subjects, with a weight ranging between 61.4 and 190 kg, after a 300 or 400 mg IV dose. Population pharmacokinetic modelling was used to assess the effect of body size on posaconazole pharmacokinetics. ClinicalTrials.gov Identifier: NCT03246386.
Results
Total body weight best predicted changes in CL and V. Model-based simulations demonstrated that, for treatment of fungal infections, a daily IV dose of 300 mg will result in a PTA of ≥90% in individuals up to 140 kg, after which both twice daily loading and the daily maintenance dose should be increased to 400 mg. For prophylaxis, a 300 mg IV dose is adequate in patients up to 190 kg.
Conclusions
Body size has a significant impact on posaconazole CL and V, resulting in a lower exposure in obese subjects compared with normal-weight subjects. For therapeutic use of posaconazole, a dose increase is required in patients above 140 kg. For prophylaxis, a 300 mg IV dose is adequate. For oral treatment, these recommendations can act as a starting point followed by therapeutic drug monitoring.
Introduction
The global prevalence of obesity (BMI >30 kg/m2) reached 11.6% in 2016 compared with only 3.0% in 1975. This trend seems likely to continue, and if it does one in five individuals will be obese in 2025. Large regional differences in obesity prevalence are reported, with a prevalence in high-income Western countries that had already reached 30% in 2016.1 Obesity is associated with many comorbidities, including an increased risk of (nosocomial) infections.2 Additionally, obesity is associated with pharmacokinetic changes, which increases the probability of suboptimal exposure of antimicrobial drugs for prophylaxis and treatment of (life-threatening) infections.3,4
Posaconazole is a broad-spectrum triazole antifungal drug mostly used for prophylaxis as well as treatment of invasive mould infections. It is highly protein bound (>98%), predominantly to serum albumin. Posaconazole is partly (20%–30%) metabolized through glucuronidation by uridine diphosphate glucuronosyltransferase (UGT) followed by excretion in faeces and urine with a terminal half-life of ∼35 h.5 Several pharmacodynamic targets are reported. First, the summary of product characteristics reports a correlation between AUC/MIC and clinical outcome, with a critical ratio of 200 for Aspergillus spp. infections.6 Second, the European Public Assessment Report mentions dose selection for prophylaxis based on a steady-state average concentration (Cavg) >0.5 mg/L in at least 90% of subjects, a mean Cavg <2.5 mg/L and no subjects with Cavg >3.75 mg/L.7 This upper toxicity threshold is based on data from trials with the posaconazole suspension, where a 3.75 mg/L Cavg was considered safe.7 Finally, the 2017 ESCMID-ECMM-ERS guideline for management of Aspergillus disease as well as the FDA recommend target Ctrough values of 0.7 and 1.0 mg/L for prophylaxis and treatment, respectively.8–10 In practice, the trough targets are used as susceptibility information is lacking in the vast majority of patients. Furthermore, quantifying AUC typically requires several plasma samples unless model-informed algorithms are used. Furthermore, an AUC-driven approach is less feasible in practice due to increased patient burden and costs.
Posaconazole is available as an oral suspension, a solid oral tablet and an IV formulation. The oral suspension demonstrated very poor bioavailability, which made therapeutic drug monitoring (TDM) a necessity. Bioavailability of posaconazole was improved with the development of an extended-release tablet and recently the IV solution. Despite this advancement in pharmaceutical formulations, the product label warns of breakthrough infections due to a decreased exposure in patients >120 kg receiving the oral tablet formulation.6 In addition, it was shown that patients weighing >90 kg had significantly lower Ctrough values compared with patients with a weight <90 kg (0.74 and 1.3 mg/L, respectively), which is considered clinically relevant.11 The study by Miceli et al.11 included only a small number of patients above 90 kg with a maximum weight of 122 kg, and no dose recommendations were provided.
With a growing population of obese patients in need of therapy for fungal infections there is a need for dosing guidelines for prophylaxis and therapy with posaconazole. In order to study the effect of (morbidly) increased body weight on posaconazole pharmacokinetics, we performed a prospective clinical trial in normal-weight and (morbidly) obese subjects. On the basis of the study results, we aim to calculate the probability of reaching the target concentration for prophylaxis and therapy and propose a weight-based dosing strategy.
Methods
Study design
This open-label, single-dose, multicentre pharmacokinetic study in obese but otherwise healthy volunteers and non-obese healthy volunteers was conducted in accordance with the Declaration of Helsinki and good clinical practice regulations (ClinicalTrials.gov Identifier: NCT03246386). This study was approved by the local Ethics Committee (NL59354.100.17). All subjects gave written informed consent before inclusion.
Study population
Obese subjects (BMI >35 kg/m2) undergoing laparoscopic gastric bypass or sleeve gastrectomy surgery and normal-weight subjects (BMI 18.5–25 kg/m2) were included from St Antonius Hospital (Utrecht, The Netherlands) and Radboud University Medical Center (Nijmegen, The Netherlands), respectively. Subjects between 18 and 65 years of age and within the specified BMI range on the day of screening were included. Subjects were excluded if they were pregnant or nursing an infant, had a documented history of posaconazole sensitivity, were using medication with a known interaction with posaconazole, were unable to understand trial procedures or had a history of drug, alcohol or solvent abuse.
Study procedures
Obese subjects were randomized to receive either 300 or 400 mg of posaconazole by peripheral venous catheter in 30 min prior to bariatric surgery, while normal-weight subjects all received 300 mg of posaconazole. Blood samples were collected from a venous catheter in the other arm in lithium–heparin tubes at 0.75, 1, 1.25, 1.5, 2, 4, 8, 12 and 24 h after start of infusion. An additional sample was drawn at 48 h after infusion in all normal-weight subjects and the obese subjects that were still admitted at that time. Samples were centrifuged at 1900 g for 5 min and immediately stored at −40°C.
Analytical assay
Posaconazole was separated from plasma components by liquid–liquid extraction with n-hexane/dichloromethane (70:30). After extraction, samples were dissolved in methanol/phosphate buffer 0.01 M, pH 2.5 (60:40), and posaconazole concentrations were quantified by validated UPLC with UV detection. A phosphate buffer of 0.01 M, pH 2.5, and an acetonitrile/phosphate buffer (70:30) were used as the mobile phase. The lower and higher limits of quantification were 0.053 and 10.55 mg/L, respectively, and accuracy ranged from 101% to 102% (n = 15). The intra-day and inter-day precision ranged from 3.8% to 5.1% (n = 5) and from 2.0% to 4.2% (n = 15), respectively. The stability of posaconazole in plasma was 7 days at room temperature and 28 months at −40°C.
Pharmacokinetic analysis
For direct comparison between groups, the observed AUC0–24 was calculated using the linear-up log-down trapezoidal rule in R (version 3.4.3) with R Studio interface (version 1.1.456). Geometric means were compared between the normal-weight group and the two obese groups using an unpaired t-test with a significance level of P = 0.05.
Then, concentration–time data were analysed by non-linear mixed effects modelling using NONMEM (version 7.3.0; Icon Development Solutions, Ellicott City, MD, USA) and Perl-Speaks-NONMEM (PsN; version 4.7.0) with the Pirana (version 2.9.7) interface.12 Graphical processing of the data and NONMEM output was done in R. We explored one-, two- and three-compartment models and used the first-order conditional estimation method with interaction for all model runs. Inter-individual variability and residual variability were assumed to be log-normally distributed. Additive, proportional and combined (additive and proportional) residual error models were evaluated.
Structural model selection was based on a decrease in objective function value (OFV) by 3.84, corresponding to −2 log-likelihood with a significance level of P = 0.05 for one degree of freedom from the χ2 distribution. Throughout model development we assessed shrinkage, root squared error (based on the covariance step in NONMEM), parameter correlation and goodness-of-fit scatter plots.
For the covariate analysis the relationships between empirical Bayes estimates and covariates were investigated in scatter plots. We explored the following covariates: total body weight (TBW), lean body weight (LBW),13 BMI, body surface area, ideal body weight (IBW), age and sex. Linear and power functions were investigated and standardized for a typical 70 kg male with a height of 1.8 m. Covariates were included one at a time if they resulted in an OFV decrease of at least 3.84 points (χ2 distribution, P = 0.05) followed by backward deletion with an OFV increase of at least 6.64 (χ2 distribution, P = 0.01).
The performance of the final model was assessed by prediction-corrected visual predictive check (pcVPC) based on 1000 Monte Carlo simulations. Parameter precision and model robustness of the structural and the covariate model was done by the sampling importance resampling (SIR) procedure.14
Simulations
The final model was used for simulation of five typical individuals with empirical chosen weights of 60, 90, 120, 150 and 180 kg with a standard loading dose of 300 mg IV twice daily followed by a 300 mg once-daily maintenance dose for 6 days of treatment. An augmented dose of 400 mg was simulated from day 7 onwards to visualize the effect on exposure to posaconazole. Additional Monte Carlo simulations were performed to calculate the PTA in a population of 9450 virtual subjects with a uniform weight distribution between 60 and 190 kg (in 5 kg increments, resulting in 27 weight groups, each consisting of 350 subjects). Daily dosing regimens of 300, 400 and 500 mg were investigated. The frequently used TDM Ctrough on day 7 of 0.7 mg/L for prophylaxis and 1.0 mg/L for treatment were used as the primary targets for the PTA.8–10 In addition, we investigated the Cavg target of 0.5 mg/L for prophylaxis and the maximum Cavg of 3.75 mg/L for toxicity as secondary targets. The simulations for the PTAs were performed with parameter uncertainty through the stochastic simulation and estimation functionality in PsN using the SIR results as model input (n = 500 models). As a cut-off for dose adjustments we aimed for a PTA >90% for efficacy and 0% for the 3.75 mg/L toxicity target.
Results
Data for analysis
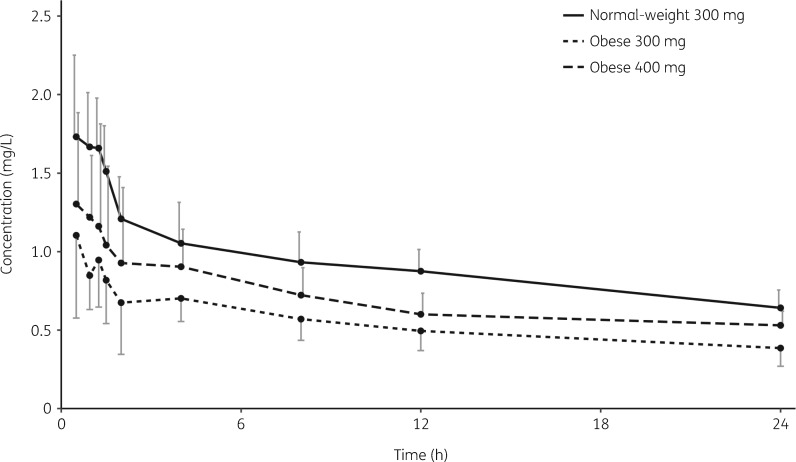
Twenty-four subjects with a TBW ranging from 61.4 to 190 kg were included. Liver function, kidney function and haematological parameters were all within the normal range. Subject characteristics are summarized in Table 1. A total of 226 plasma samples were available for analysis. Figure 1 shows the observed mean plasma concentration–time profiles in the different groups.
Table 1.
Summary of subject characteristics
| 300 mg IV |
400 mg IV obese | ||
|---|---|---|---|
| normal weight | obese | ||
| Gender, n (%) | |||
| male | 4 (50) | 4 (50) | 4 (50) |
| female | 4 (50) | 4 (50) | 4 (50) |
| Age (years), median (range) | 22 (20–37) | 51 (31–63) | 37.5 (25–50) |
| Weight (kg), median (range) | 72.3 (61.4–85.4) | 129 (109–190) | 144 (107–175) |
| BMI (kg/m2), median (range) | 22.5 (20.2–25.4) | 42.1 (38.3–51.5) | 43.6 (34.9–46.0) |
| LBWa (kg), median (range) | 52.3 (41.3–65.1) | 69.6 (54.2–98.9) | 69.3 (61.5–98.9) |
According to Janmahasatian et al.13
Figure 1.
Observed mean (SD) posaconazole plasma concentrations.
Pharmacokinetic analysis
The observed geometric mean (range) AUC0–24 in normal-weight (n = 8) versus obese (n = 8) subjects receiving 300 mg of posaconazole IV was 21.4 (15.6–29.1) versus 13.1 (9.1–18.5) mg·h/L (P < 0.05). Obese subjects receiving 400 mg of posaconazole IV (n = 8) had an AUC0–24 of 16.8 mg·h/L (12.2–25.6). Despite the higher dose of 400 mg in the obese group, their exposure was lower than that in normal-weight subjects receiving 300 mg (P < 0.05).
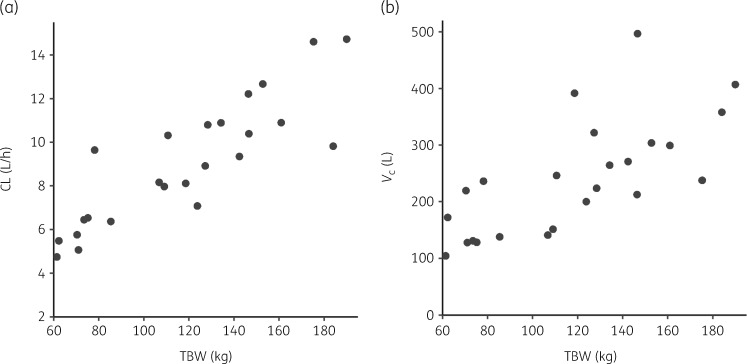
The plasma concentration–time data were best described using a two-compartment structural model with first-order elimination, a proportional residual error model and inter-individual variability on CL and the central compartment (Vc). TBW outperformed LBW, body surface area and IBW in describing pharmacokinetic variability (P < 0.05). Figure 2 shows the relationship between TBW and the individual empirical Bayes estimates for CL and Vc from the structural model without covariates.
Figure 2.
Empirical Bayes estimates for CL (a) and Vc (b) versus TBW from the structural model.
The addition of TBW to the model with a power function on the peripheral compartment (Vp) resulted in the largest reduction in OFV, of 62.6 points (P < 0.05). This was followed by addition of TBW to Vc and CL, with an OFV drop of 14.3 (P < 0.05) and 6.7 (P < 0.05), respectively. As the addition of TBW to CL resulted in a decrease in the inter-individual variability of CL to almost zero, we removed the inter-individual variability on CL, resulting in an OFV increase of <1 (P > 0.05). In the final model, CL, Vc and Vp of the ith individual were best described using the equations:
Backward elimination did not result in removal of any covariates (P > 0.01). Addition of age or sex did not improve the model. Parameter estimates of the structural and final models are presented in Table 2.
Table 2.
Pharmacokinetic parameter estimates for the structural and final models
| Parameter | Structural model (RSE %) [95% CI] | Final model (RSE %) [95% CI] |
|---|---|---|
| CL (L/h) | 8.42 (9.3) [7.0–10.0] | – |
| CL70kg | ||
| CL70kg (L/h) | – | 5.83 (4.4) [5.33–6.27] |
| θ1 | – | 0.54 (26) [0.26–0.78] |
| Q (L/h) | 51.9 (27) [30.0–83.0] | 60.3 (19) [41.2–85.8] |
| V c (L) | 222 (11) [182–267] | – |
| V c; 70kg | ||
| Vc; 70kg (L) | – | 150 (12) [119–187] |
| θ2 | – | 0.77 (24) [0.40–1.12] |
| V p (L) | 132 (9.3) [109–153] | – |
| V p; 70kg | ||
| Vp; 70kg (L) | – | 96.2 (12) [73.7–118] |
| θ3 | – | 1.16 (18) [0.779–1.56] |
| Inter-individual variability (%)a | ||
| CLb | 37.1 (19) [25.0–55.2] | – |
| Vcb | 44.4 (17) [33.0–66.2] | 29.5 (16) [22.2–42.6] |
| Residual error (%) | ||
| σpropb | 17.6 (5.4) [16.0–19.6] | 16.4 (5.1) [15.1–18.2] |
| OFV | −506.2 | −589.8 |
Q, inter-compartmental CL between Vc and Vp; σprop, proportional residual error; RSE, relative standard error based on covariance step in NONMEM; 95% CI, 95% CI obtained from the SIR procedure.
Calculated as .
η and ε shrinkage of inter-individual variability and residual error are <10%.
Goodness-of-fit scatter plots indicate that the structural and final models are appropriate for the data, as shown in Figure S1 (available as Supplementary data at JAC Online). Population and individual predicted concentrations are in concordance with the observed concentrations. The conditional weighted residuals indicate no model misspecification, the distribution is homogeneous and the majority of the data lies within the [−2, 2] interval. The pcVPC of the final model shows that predictions are consistent with observations indicating a good internal validity of the model with respect to the data (Figure S2).
Simulations
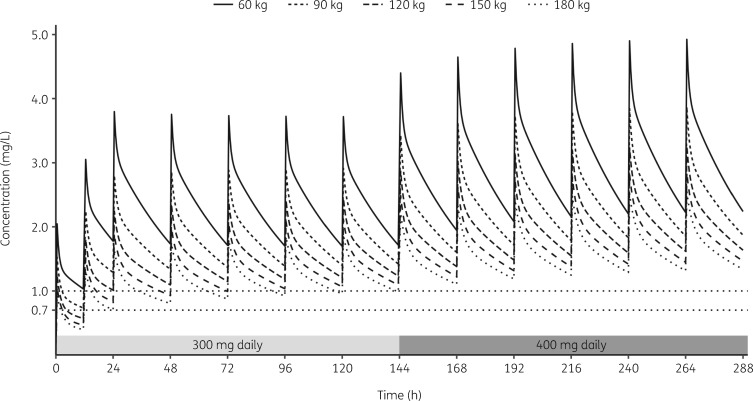
Model-based simulations of pharmacokinetic curves in five typical subjects with weights of 60, 90, 120, 150 and 180 kg receiving 300 mg of IV posaconazole up to steady-state on day 7 followed by 400 mg of posaconazole are shown in Figure 3. This figure illustrates the significantly lower exposure and peak and trough plasma concentrations with increasing weight.
Figure 3.
Simulated posaconazole plasma concentrations in five typical patients after a twice-daily 300 mg IV loading dose over the first 24 h followed by a daily 300 mg IV dose. From day 7 (144 h) a daily 400 mg dose is simulated. The horizontal dotted lines indicate the target Ctrough values for prophylaxis (0.7 mg/L) and treatment (1.0 mg/L).
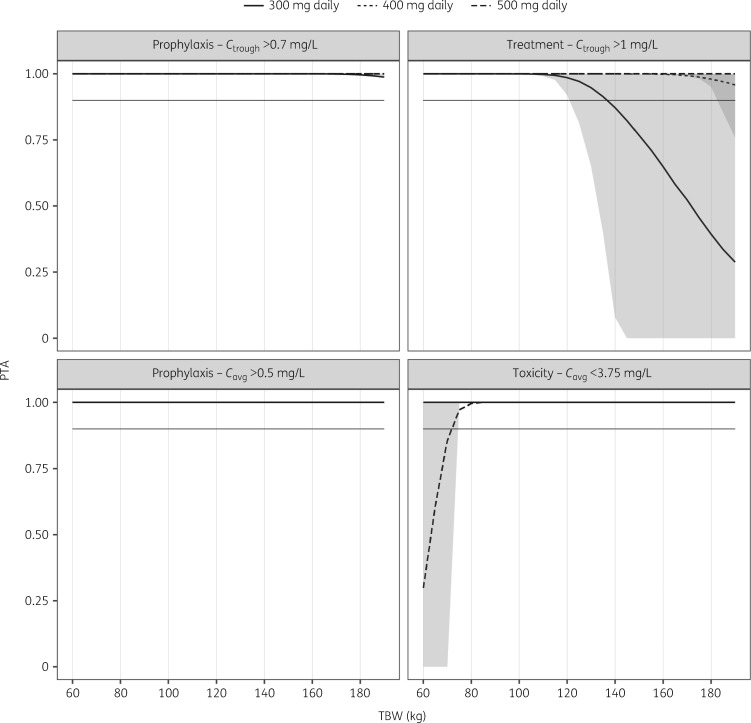
Figure 4 shows the model-based PTA plots, confirming that, in a treatment setting, the 300 mg dose administered as an IV formulation is sufficient up to 140 kg, after which a dose increase to 400 mg daily will result in >90% PTA. A further augmented dose of 500 mg should be considered in patients >190 kg in the treatment setting. In a prophylactic setting, the standard 300 mg IV dose results in >90% PTA in patients up to 190 kg for both the 0.7 mg/L trough target and the Cavg target of 0.5 mg/L. Finally, we show that the above recommendations result in a Cavg below the 3.75 mg/L toxicity threshold.
Figure 4.
PTA versus TBW in steady-state for targets for prophylaxis, treatment and toxicity for three dosage regimens. The grey horizontal line represents a target attainment of 90%. The light grey shading around the lines represents the 95% CI of the prediction. The dark grey shading represents the overlap between the CIs of the 300 and 400 mg daily doses. For the toxicity PTA the value 1 represents the probability of staying below the 3.75 mg/L Cavg.
Discussion
In this study we investigated the pharmacokinetics of posaconazole in morbidly obese and normal-weight individuals with a wide body weight range of 61.4–190 kg. In a direct comparison we found that obese individuals had a 39% lower exposure (AUC0–24) to posaconazole after receiving a single IV dose of 300 mg compared with normal-weight individuals, i.e. 13.1 mg·h/L in obese versus 21.4 mg·h/L in normal-weight subjects. A 33% dose increase to 400 mg in obese subjects resulted in an exposure of 16.8 mg·h/L, which is still significantly lower than the exposure found in normal-weight subjects receiving 300 mg.
A two-compartment model with first-order elimination best described the observed posaconazole plasma concentration–time profiles in the normal-weight and obese populations. Previous population pharmacokinetic studies investigated the pharmacokinetics of posaconazole upon administration as an oral suspension or the tablet formulation and reported one-compartment models to describe their data.15–20 The prolonged absorption phase after an oral posaconazole dose might have obscured the initial distribution phase, resulting in a one-compartment model.
TBW was the body size descriptor best predicting pharmacokinetic differences between subjects. The effect of weight was most significant on the Vp, but the Vc also increased with weight, although to a lesser extent. The increase in V means that, given the same dose as normal-weight patients, obese patients will have a lower maximum plasma concentration. We found a limited but still clinically relevant effect of weight on CL. Possible explanations provided by the literature are an increase in liver size and blood flow and/or an increased UGT metabolism that is associated with obesity.5,21,22 Our study provides an explanation of the previously reported lower Ctrough values in patients above 90 kg.11 Recently, van Iersel et al.20 reported that weight was a predictor of decreasing bioavailability (F) in a large population of patients and healthy subjects receiving the solid tablet formulation of posaconazole. In retrospect, this finding might also have been the result of weight on apparent CL (CL/F) and/or apparent V (V/F).
Our simulations showed that the PTA with a 300 mg IV posaconazole dose is significantly affected by weight, and dose adjustments are required. By means of simulations using the defined target concentrations, a change in dose is not required for patients up to 190 kg in the prophylactic setting as the vast majority achieved the needed concentrations while on an IV 300 mg dose. In the setting of treatment of invasive mould disease, patients above 140 kg would benefit from a 400 mg daily IV dose. Simultaneously, a higher loading dose of posaconazole in obese patients is needed to achieve early steady-state conditions that are equivalent to those of their normal-weight counterparts. The loading dose should be increased following the maintenance dose recommendations. Our results are in line with the statement in the product label warning of a low exposure in obese patients.6 Although a PTA >90% is reached, the dose escalations we recommend to reach the prophylactic and treatment targets will still result in a lower exposure (Cmax, Ctrough and AUC) compared with normal-weight patients receiving 300 mg and are therefore expected to have a similar safety profile. We emphasize that our recommendations are focused on achieving optimal PTA and not bioequivalence. To achieve a bioequivalent exposure a higher posaconazole IV dose is required than the dose we recommend, as we have shown in a direct comparison of the exposure after a 300 and 400 mg dose. As the exposure is lower, the Cavg in steady-state will remain below the EMA-recommended upper concentration of 3.75 mg/L (Figure 4).7 The threshold associated with efficacy is subject to debate. Both 1.0 and 1.25 mg/L can be used and brought forward for discussion. We have chosen 1.0 mg/L as this is most widely reported for primary therapy of aspergillosis. Obviously these recommendations do not take into account the setting of treatment of less susceptible species with attenuated MICs (i.e. 0.25 or 0.5 mg/L) or the use of posaconazole as salvage therapy. Here higher dosages are a must to achieve desired targets.
Our study has some limitations that should be considered. First, the pharmacokinetics in the obese subjects were investigated during their stay in hospital for bariatric surgery. Because this is a short (<1 h) laparoscopic procedure with minor blood loss and little administration of IV fluids, we expect this additional variability to have a minimal impact. Second, in the normal-weight group we were able to obtain a sample at 48 h after dose, while for the majority of the obese subjects only samples up to 24 h could be obtained. Although we were able to accurately estimate CL (indicated by a narrow CI) we were not able to include inter-individual variability of CL in our model after inclusion of weight as covariate. This resulted in an under-prediction of the variability. Third, the obese subjects were older than the normal-weight subjects. Studies with the posaconazole suspension observed that Cmax and AUC are almost 30% higher in subjects >65 years of age compared with subjects between 18 and 45 years.6 These results could not be reproduced using the tablet and IV formulations and are most likely due to differences in bioavailability of the suspension between these groups.6 Therefore, we expect age to have no effect on our analysis. Finally, we studied the effect of weight in obese but otherwise healthy volunteers; this enabled a good estimation of the effect of weight without the effect of illness on the pharmacokinetics. Of course, other clinical factors may influence drug exposure, which holds true for any dosing recommendation. For instance, Sime et al.23 recently reported higher posaconazole CL in critically ill patients.
Our dosing recommendations hold for treatment of patients with the IV formulation. When using a posaconazole extended-release tablet formulation, bioavailability will play an important role and the exposure will be lower compared with IV drug administration. To our knowledge, the bioavailability of the tablets has not been reported. We emphasize that further studies are needed to characterize oral dosing of posaconazole in obese patients but speculate that here at least the same dose augmentation is needed. Therefore, our dosing recommendations should be considered a starting point supported by TDM to confirm an adequate exposure in this special population.
In conclusion, we show that a 300 mg daily IV posaconazole dose results in >90% PTA for prophylaxis in patients up to 190 kg. For treatment of fungal diseases, a dose increase to 400 mg should be used in patients with a weight >140 kg. For patients using posaconazole tablets these recommendations can act as a starting point followed by TDM.
Supplementary Material
Acknowledgements
We thank Sylvia Samson, Brigitte Bliemer, Sanne Houba and Veroniek Harbers for their assistance with patient inclusion and sample collection. Technical assistance was kindly provided by Arthur Pistorius. Finally, we thank Merck Sharp & Dohme Corp. for sponsoring this work with an unrestricted grant.
Funding
R.J.M.B. received an unrestricted educational grant from Merck Sharp & Dohme Corp. for this trial.
Transparency declarations
P.E.V. and R.J.M.B. have served as consultants to Astellas Pharma, Inc., F2G, Gilead Sciences, Merck Sharp & Dohme Corp. and Pfizer, Inc., and have received unrestricted and research grants from Astellas Pharma, Inc., Gilead Sciences, Merck Sharp & Dohme Corp. and Pfizer, Inc. All contracts were through Radboudumc and all payments were invoiced by Radboudumc. All other authors: none to declare.
Author contributions
R.E.W. participated in study design, data collection, analysis of the data and writing of the article. C.S. and M.H.v.D. participated in data collection, analysis of the data and writing of the article. C.A.J.K. and R.J.M.B. participated in study design, analysis of the data and writing of the article. E.P.A.v.D. and R.M.J.W. participated in data collection and writing of the article. D.M.B. and P.E.V. participated in writing of the article.
References
- 1.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017; 390: 2627–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Falagas ME, Kompoti M.. Obesity and infection. Lancet Infect Dis 2006; 6: 438–46. [DOI] [PubMed] [Google Scholar]
- 3. Huttunen R, Karppelin M, Syrjanen J.. Obesity and nosocomial infections. J Hosp Infect 2013; 85: 8–16. [DOI] [PubMed] [Google Scholar]
- 4. Knibbe CA, Brill MJ, van Rongen A. et al. Drug disposition in obesity: toward evidence-based dosing. Annu Rev Pharmacol Toxicol 2015; 55: 149–67. [DOI] [PubMed] [Google Scholar]
- 5. Krieter P, Flannery B, Musick T. et al. Disposition of posaconazole following single-dose oral administration in healthy subjects. Antimicrob Agents Chemother 2004; 48: 3543–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.EMA. Summary of Product Characteristics: Noxafil. 7 December 2018. https://www.ema.europa.eu/documents/product-information/noxafil-epar-product-information_en.pdf.
- 7.EMA. European Public Assessment Report: Scientific Discussion - Extension. 10 June 2014. https://www.ema.europa.eu/documents/variation-report/noxafil-h-c-610-x-0028-epar-scientific-discussion-extension_en.pdf.
- 8. Walsh TJ, Raad I, Patterson TF. et al. Treatment of invasive aspergillosis with posaconazole in patients who are refractory to or intolerant of conventional therapy: an externally controlled trial. Clin Infect Dis 2007; 44: 2–12. [DOI] [PubMed] [Google Scholar]
- 9. Ullmann AJ, Aguado JM, Arikan-Akdagli S. et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect 2018; 24 Suppl 1: e1–38. [DOI] [PubMed] [Google Scholar]
- 10. Jang SH, Colangelo PM, Gobburu JV.. Exposure-response of posaconazole used for prophylaxis against invasive fungal infections: evaluating the need to adjust doses based on drug concentrations in plasma. Clin Pharmacol Ther 2010; 88: 115–9. [DOI] [PubMed] [Google Scholar]
- 11. Miceli MH, Perissinotti AJ, Kauffman CA. et al. Serum posaconazole levels among haematological cancer patients taking extended release tablets is affected by body weight and diarrhoea: single centre retrospective analysis. Mycoses 2015; 58: 432–6. [DOI] [PubMed] [Google Scholar]
- 12. Keizer RJ, Karlsson MO, Hooker A.. Modeling and simulation workbench for NONMEM: tutorial on Pirana, PsN, and Xpose. CPT: Pharmacomet Syst Pharmacol 2013; 2: e50.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Janmahasatian S, Duffull SB, Ash S. et al. Quantification of lean bodyweight. Clin Pharmacokinet 2005; 44: 1051–65. [DOI] [PubMed] [Google Scholar]
- 14. Dosne AG, Bergstrand M, Harling K. et al. Improving the estimation of parameter uncertainty distributions in nonlinear mixed effects models using sampling importance resampling. J Pharmacokinet Pharmacodyn 2016; 43: 583–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Boonsathorn S, Cheng I, Kloprogge F. et al. Clinical pharmacokinetics and dose recommendations for posaconazole in infants and children. Clin Pharmacokinet 2019; 58: 53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Petitcollin A, Boglione-Kerrien C, Tron C. et al. Population pharmacokinetics of posaconazole tablets and Monte Carlo simulations to determine whether all patients should receive the same dose. Antimicrob Agents Chemother 2017; 61: e01166-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vehreschild JJ, Muller C, Farowski F. et al. Factors influencing the pharmacokinetics of prophylactic posaconazole oral suspension in patients with acute myeloid leukemia or myelodysplastic syndrome. Eur J Clin Pharmacol 2012; 68: 987–95. [DOI] [PubMed] [Google Scholar]
- 18. AbuTarif MA, Krishna G, Statkevich P.. Population pharmacokinetics of posaconazole in neutropenic patients receiving chemotherapy for acute myelogenous leukemia or myelodysplastic syndrome. Curr Med Res Opin 2010; 26: 397–405. [DOI] [PubMed] [Google Scholar]
- 19. Kohl V, Muller C, Cornely OA. et al. Factors influencing pharmacokinetics of prophylactic posaconazole in patients undergoing allogeneic stem cell transplantation. Antimicrob Agents Chemother 2010; 54: 207–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van Iersel M, Rossenu S, de Greef R. et al. A population pharmacokinetic model for a solid oral tablet formulation of posaconazole. Antimicrob Agents Chemother 2018; 62: e02465-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Smit C, De Hoogd S, Bruggemann RJM. et al. Obesity and drug pharmacology: a review of the influence of obesity on pharmacokinetic and pharmacodynamic parameters. Expert Opin Drug Metab Toxicol 2018; 14: 275–85. [DOI] [PubMed] [Google Scholar]
- 22. Brill MJ, Diepstraten J, van Rongen A. et al. Impact of obesity on drug metabolism and elimination in adults and children. Clin Pharmacokinet 2012; 51: 277–304. [DOI] [PubMed] [Google Scholar]
- 23. Sime FB, Stuart J, Butler J. et al. Pharmacokinetics of intravenous posaconazole in critically ill patients. Antimicrob Agents Chemother 2018; 62: e00242-18.. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.