Abstract
Background:
Construction is among the most dangerous industries. In addition to traditional hazards for workplace injury and illness, other threats to health and well-being may occur from work organization and work environment factors, including irregular employment, long commutes, long work hours, and employer policies regarding health and safety. These non-traditional hazards may affect work and health outcomes directly, or through effects on health behaviors. The cumulative impacts of both traditional and non-traditional hazards on health-related outcomes among construction workers are largely unknown.
Methods:
We conducted a survey among apprentice construction workers to identify relationships between work organization and environmental factors with five outcomes of economic relevance to employers: missed work due to work-related injury, missed work due to any pain or injury, self-reported work ability, health-related productivity, and use of prescription medications for pain.
Results:
963 surveys were completed (response rate 90%) in this young (mean age 28) working cohort. Multivariate Poisson regression models found associations between the outcomes of interest and multiple work factors, including job strain, safety behaviors of co-workers, and mandatory overtime. Univariate analysis showed additional associations, including precarious work and supervisor support for safety.
Conclusions:
Findings from this cross-sectional study suggest that work organization and environment factors influence health and work outcomes among young construction trade workers. Future work with longitudinal data will examine the hypothesized paths between work factors, health behaviors, health outcomes, and work outcomes.
Keywords: Total Worker Health, construction workers, work organization, health related productivity, workplace safety, safety climate, work environment
INTRODUCTION
Construction is among the most hazardous industries in the US, with high rates of fatal and non-fatal injuries.1 Safety in construction is complicated due to rapidly changing work environments, unique hazards of the industry, and the organizational issues of coordinating interactions between multiple contractors.2,3 Further complicating work organization is the large number of small construction contractors, whose owners often lack sufficient safety resources, and whose workers represent a disproportionate number of fatalities compared to the overall sector.4
The work organization and work environment of construction is complex: work is often short-term and episodic,5 workers from multiple employers frequently share a job site, and the physical work environment changes daily with weather and different stages of a build. All of these factors contribute to both the high risks of injury and illness seen in construction, and to the difficulty of implementing effective health and safety interventions.
In addition to high rates of work injury, construction workers have higher rates of mortality and morbidity from chronic diseases than workers from other occupations,3 and the prevalence of functional health problems that limit work is 36% in construction workers, versus 23% in white-collar occupations.6 Construction workers also have higher rates of alcohol use, smoking, and other unhealthy behaviors.7–9 These disparities in health-related behaviors contribute to the higher rates of mortality and morbidity seen among construction and other blue-collar workers; these health behaviors are driven in part by work organization and work environment factors. Numerous studies have shown the negative health consequences of workplace organizational and environmental factors such as physical and mental stress, low autonomy over work tasks and schedule, poor coworker and managerial support, and unhealthy physical work environments.10 These workplace risk factors are more common in low-wage jobs, and contribute to disparities in the prevalence of chronic health conditions seen between different working populations.11,12
While past studies have attempted to change diet and smoking among construction workers with interventions directed at individual workers,13–18 few studies have addressed the work organization and work environment factors that influence these and other health behaviors among construction workers. We used a Total Worker Health® approach that considered multiple work organization and environment factors that may influence health and wellbeing of construction workers.19–22 Our initial analyses were focused on worker health outcomes of direct relevance to employers, including measures of both “absenteeism” (missed work days due to pain or injury) and measures of “presenteeism” (workplace productivity losses related to health status).23
In addition to missed work and workplace productivity losses due to health, we also analyzed use of medications prescribed for pain as an additional outcome. Use of pain medication is relevant to employers due to increasing evidence that construction workers are at uniquely high risk of opioid use and overdose, and to increasing recognition by the construction industry of the need for improved prevention of opioid use disorder. Recent studies have shown that construction workers and miners are more likely than workers in other industries to be prescribed opioids and to receive prescriptions for longer periods of time,24 and that construction workers and miners are at markedly high risk of opioid overdose fatalities (up to six times the rate of overdose fatalities compared to the general workforce in Massachusetts).25,26 There is growing awareness and calls for action among construction employers and safety professionals for action to reduce the high personal and economic costs of opioid use in this industry.27,28
The goal of this exploratory study was to describe the associations of work organization and work environment factors on five outcomes relevant to employers among construction apprentices: missed work due to work-related injury, missed work due to any pain or injury, work ability, health-related productivity, and use of prescription medications for pain.
MATERIALS & METHODS
Participants:
Apprentices attending training classes offered by two union apprenticeship programs in Missouri (Carpentry and Floor Laying) at any time between February 15 and June 14, 2017 were invited to complete a survey on health and work. These trades were chosen because of their willingness to participate, and their large size. Participants provided informed consent and were compensated $15 for survey completion; each individual apprentice could complete the survey only once. Institutional review and ethics approval was obtained from the Human Subjects Office at University of Iowa, Iowa City, USA.
Survey:
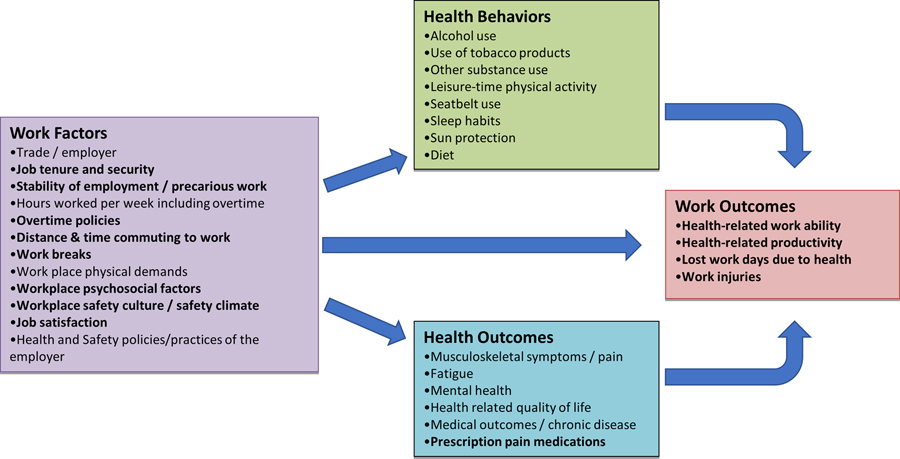
The survey contained 78 items addressing four major domains: work organization and environment, health behaviors, health outcomes, and work outcomes. Data collection was guided by a conceptual model that hypothesized both direct and mediated effects of work organization and environment on the other three domains (Figure 1). Work organization and environment factors included apprenticeship stage, reported job security and steadiness of work, mandatory overtime, formal work breaks, and primary construction sector of employment (residential vs. commercial construction). We assessed job satisfaction, decision latitude, and skill discretion using the Job Content Questionnaire (JCQ),29 and computed the JCQ strain ratio from these variables (strain = JCQ job demand*2/JCQ decision latitude).29 Work organizational factors also assessed workplace safety climate including the supervisor’s support for safety assessed using the Zohar scale,30 and coworkers’ support for safety using the scale of Neil and Griffin.30,31 Health outcomes included the use of prescription drugs for pain. Work outcomes included self-reported work-related injuries and missed work due to pain or injury. As measures of “presenteeism” we assessed health-related work ability via the Work Ability Index,32 and work productivity via the Work Productivity and Activity Impairment Questionnaire.33
Figure 1:
Conceptual Model Linking Work Factors, Health Behaviors, Health Outcomes and Work Outcomes (Bolded items indicate measures used in the current analysis).
Analysis:
This initial cross-sectional analysis focused on five outcomes of economic relevance to employers: missed work due to work-related injury, missed work due to any pain or injury, self-reported work ability, health-related productivity, and use of prescription medications for pain. Potential risk factors for these outcomes included apprentice term (stage of training), formal workplace breaks, supervisor and co-worker support for work safety practices, precarious employment (defined as poor job security or work that was not regular and steady), mandatory overtime, job satisfaction, and the JCQ strain ratio. Multivariate analyses also controlled for type of construction (residential vs. commercial), as work organization and injury rates differ between these two sectors.4 Analyzed outcomes and risk factors are shown in Table 1.
Table I:
Variables and proportion of workers with outcomes and exposures to work factors. (total n=929)
| Variables | Definition/Source | n | % |
|---|---|---|---|
| Outcomes | |||
| Prescribed medication for pain | Any, past 12 months | 112 | 12.12 |
| Missed days due to work-related injury | Any, past 12 months | 85 | 9.49 |
| Missed days due to any injury or pain | Any, past 12 months | 183 | 20.47 |
| Work ability | Work Ability Index31 | 78 | 8.72 |
| Health related productivity | Work Productivity and Activity Impairment Questionnaire32 | 133 | 14.84 |
| Work factors | |||
| Senior apprentice | Third term or higher (generally > 1 year as an apprentice) | 551 | 59.31 |
| Formal work breaks | Y/N | 743 | 84.72 |
| Low supervisor support for safety | Foreman / supervisor safety scale below median29 | 182 | 19.8 |
| Low co-worker support for safety | Coworker safety scale below median30 | 427 | 46.06 |
| Precarious work | Disagree with “my job security is good” OR report work not “regular and steady”28 | 209 | 22.72 |
| Mandatory overtime | Y/N | 73 | 7.9 |
| High job strain | Strain ratio >1 (JCQ demand*2/JCQ decision latitude)28 | 563 | 65.24 |
| Low job satisfaction | Satisfaction response other than “very satisfied” on 4 point scale28 | 373 | 40.15 |
In order to test our overall hypothesis that work organization and environment factors common in the construction sector would be associated with adverse health and work outcomes, we used Poisson regression models with robust sandwich estimators to examine univariate and multivariate associations between work organizational and environmental factors with health and work outcomes. We used multiple imputation with predictive mean matching to impute missing predictor variables. All analyses were performed using R.34
RESULTS
1070 surveys were distributed to apprentice workers; 963 surveys were completed and returned (response rate = 90%). Respondents were predominantly male, with a mean age of 28 years and average time in the construction trade of 2.6 years. Analyses were limited to male workers (n=929). No single variable was missing in more than 8% of respondents; approximately 20% of participants were missing at least one variable. There were no significant differences between missingness of predictor variables based on outcomes; compared to use of imputed data, limiting analyses to only those participants with full data showed very similar associations. Data shown in Tables 2 and 3 use imputed data.
Table II:
Univariate associations between work outcomes and exposure to work factors (n=929, Prevalence Ratio (PR) calculated using Poisson regression).
| Prescribed medication for pain | Missed days due to work-related injury | Missed days due to any injury or pain | Low work ability | Low health related productivity | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | PR | CI | PR | CI | PR | CI | PR | CI | PR | CI |
| Late term (senior) apprentice | 1.33 | (0.92 – 1.92) | 1.55 | (1.00 – 2.41) | 1.44 | (1.09 – 1.90) | 0.50 | (0.32 – 0.77) | 0.69 | (0.51 – 0.95) |
| Formal work breaks | 0.86 | (0.54 – 1.36) | 1.11 | (0.60 – 2.03) | 1.02 | (0.70 – 1.48) | 0.60 | (0.36 – 1.00) | 0.74 | (0.49 – 1.11) |
| Low supervisor support | 1.50 | (1.02 – 2.21) | 1.57 | (1.00 – 2.46) | 1.27 | (0.94 – 1.72) | 1.61 | (1.01 – 2.55) | 1.85 | (1.34 – 2.57) |
| Low coworker support | 1.50 | (1.06 – 2.13) | 1.39 | (0.93 – 2.09) | 1.61 | (1.24 – 2.09) | 1.77 | (1.15 – 2.73) | 1.62 | (1.17 – 2.23) |
| Precarious work | 1.53 | (1.05 – 2.22) | 1.75 | (1.14 – 2.68) | 1.35 | (1.02 – 1.80) | 1.13 | (0.69 – 1.85) | 1.40 | (0.99 – 1.97) |
| Mandatory overtime | 0.44 | (0.17 – 1.15) | 0.61 | (0.23 – 1.60) | 0.94 | (0.57 – 1.57) | 0.67 | (0.25 – 1.78) | 1.86 | (1.20 – 2.91) |
| High job strain | 1.93 | (1.24 – 2.99) | 2.26 | (1.31 – 3.89) | 1.86 | (1.34 – 2.59) | 1.86 | (1.08 – 3.18) | 1.81 | (1.21 – 2.71) |
| Low job satisfaction | 1.35 | (0.95 – 1.90) | 1.45 | (0.97 – 2.18) | 1.42 | (1.10 – 1.83) | 1.87 | (1.22 – 2.86) | 2.23 | (1.62 – 3.09) |
Table III.
Multivariable associations between work outcomes and exposure to work factors (n=929, Prevalence Ratio (PR) calculated using Poisson multiple regression. All variables entered into model; model also includes residential vs. commercial construction as primary work over past year.
| Prescribed medication for pain | Missed days due to work-related injury | Missed days due to any injury or pain | Low work ability | Low health related productivity | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | PR | CI | PR | CI | PR | CI | PR | CI | PR | CI |
| Late term (senior) apprentice | 1.32 | (0.89 – 1.96) | 1.53 | (0.96 – 2.43) | 1.39 | (1.04 – 1.87) | 0.50 | (0.32 – 0.76) | 1.21 | (0.95 – 1.54) |
| Formal work breaks | 0.91 | (0.58 – 1.42) | 1.15 | (0.64 – 2.05) | 1.05 | (0.74 – 1.49) | 0.70 | (0.42 – 1.15) | 0.90 | (0.68 – 1.17) |
| Low supervisor support | 1.19 | (0.78 – 1.81) | 1.21 | (0.76 – 1.91) | 0.97 | (0.71 – 1.31) | 1.14 | (0.70 – 1.87) | 1.11 | (0.86 – 1.43) |
| Low coworker support | 1.26 | (0.86 – 1.84) | 1.10 | (0.74 – 1.64) | 1.39 | (1.06 – 1.82) | 1.46 | (0.93 – 2.29) | 1.37 | (1.08 – 1.75) |
| Precarious work | 1.37 | (0.93 – 2.02) | 1.54 | (0.99 – 2.40) | 1.20 | (0.90 – 1.60) | 0.88 | (0.53 – 1.45) | 0.98 | (0.76 – 1.25) |
| Mandatory overtime | 0.42 | (0.19 – 1.10) | 0.62 | (0.24 – 1.60) | 0.93 | (0.57 – 1.53) | 0.66 | (0.25 – 1.76) | 1.39 | (1.00 – 1.94) |
| High job strain | 1.68 | (1.06 – 2.66) | 1.75 | (1.01 – 3.02) | 1.52 | (1.09 – 2.12) | 1.46 | (0.85 – 2.50) | 1.35 | (0.99 – 1.82) |
| Low job satisfaction | 0.96 | (0.64 – 1.43) | 1.01 | (0.66 – 1.56) | 1.11 | (0.84 – 1.46) | 1.53 | (0.95 – 2.46) | 1.68 | (1.32 – 2.15) |
Univariate Poisson regression analyses (Table 2) showed that all five outcomes were associated with high job strain, and four were associated with low supervisor and coworker support for safety. Precarious work was associated with greater use of pain medication, missed days due to work injury, and missed days from all injury or pain. Formal work breaks were associated with a decreased risk of low work ability, while mandatory overtime was associated with lower health related productivity.
Multivariate Poisson regression (Table 3) showed that the JCQ strain ratio was associated with higher prescription pain medication use, missed work due to work injury, and missed work due to injury or pain when controlled for all other variables. High job strain approached a statistically significant association with low health-related productivity, with lower 95% confidence intervals that were slightly below 1.0. Senior apprentices (those who had completed 3 or more of 8 instructional terms) reported higher rates of missed days due to injury or pain, but were less likely to report low work ability due to health. Lower reported coworker safety behaviors was associated with missed days due to any injury or pain, and to low health related productivity. Mandatory overtime and low job satisfaction were associated with low health related productivity.
DISCUSSION
While work organization and environment have been studied as determinants of workplace safety in construction,35 there is less work examining their influence on worker health and well-being. Much research on changing health behaviors among construction workers has focused only on changing individual health behaviors as opposed to changing the workplace factors or policies influencing these behaviors.36,37 This study found that work organization and environmental factors such as supervisor support, safety behaviors by co-workers, the balance between psychological job demands and work autonomy (job strain), mandatory overtime, and the type of construction work were associated with important outcomes of missed work days, health-related productivity, and use of prescription medications for pain.
In addition to traditional workplace hazards in the construction industry, there are other threats to worker health and well-being that arise from work organization and work environment factors. Previous research has indicated that workplace safety climate38 and psychosocial stress39 can influence safety behaviors, injuries, and health outcomes in the construction industry,40–44 but less is known about their impact on other outcomes, such as absenteeism and presenteeism, that have direct economic relevance to employers.22
Qualitative data have described negative effects from overtime work in construction including higher injury rates, lower productivity, and fatigue,45 and fatigue has been shown to influence construction workers’ physical and cognitive function.46 Our study found an association between mandatory overtime and lower health related productivity. Workplace psychosocial factors have been associated with absence from work in several studies. In particular, increased job strain has been associated with work-related injury absence47 and overall absence from work48 among construction workers, and lack of job control (a component of job strain) was linked to higher sick leave.49 The JCQ strain ratio was associated with both measures of work absence controlling for all other variables in our study. Reports of coworkers’ commitment to safety and safety practice have been linked to safety behaviors on the job and to injury outcome among construction workers.50,51 Our study also found that co-workers’ safety behaviors were associated with lost days due to injury or illness; we also found an association with lower health related productivity. This latter finding is consistent with a study showing that lack of support at work was a strong predictor of work ability among construction workers.52
A major new finding from our study are the observed associations between work factors and use of prescription pain medications. Univariate analyses found that use of prescribed medication for pain was associated with lower co-worker support for safety, precarious work, and high job strain. High job strain remained significantly associated with pain medication use in the multivariable models. While we cannot be certain what medications were prescribed for pain, it is highly likely that most of these prescriptions were for opioids. The disproportionately high rates of use and overdose of opioids seen in the construction industry24–26 likely rises from several causes, including high rates of injury and subsequent medical care among construction workers,53 the intermittent nature of construction work, and the lack of paid sick leave: the need to return to work soon after an injury or to work while in pain may contribute to high rates of opioid use among construction workers and workers in other occupations with lower availability of paid sick leave and lower job security.26
Though the personal and social costs of the opioid crisis resulting from mortality and morbidity are well known, employment costs are less appreciated. It is estimated that 46% of the total societal costs of prescription opioid misuse in the U.S. are workplace costs, driven by lost earnings from reduced compensation, lost employment, and premature death.54 Costs to employers include lowered productivity from absenteeism, higher healthcare costs, and higher hiring and training costs resulting from turnover of skilled workers.55 Manufacturing and construction firms in hard-hit states report shortages in the blue-collar labor market because workers are unable to pass mandatory drug testing.56 These economic costs related to opioid use may motivate employers to modify the work environment to reduce opioid use among their workers; it is likely that reducing rates of work-related injuries and chronic musculoskeletal disorders would reduce opioid use among construction workers.57
The major limitation of our study is the use of a cross-sectional survey design, which does not allow us to determine the direction of the observed associations. Longitudinal follow-up of this cohort is ongoing; future analyses will clarify the natural history of health and disability outcomes, and the temporal sequence of putative risk factors for these outcomes. It is likely that some effects of work environment on work and health outcomes are mediated through changes in health behaviors; this question and others will be addressed with longitudinal follow-up. For example, while a few studies in other industries have examined the additive effects of multiple workplace factors on worker health and well-being,46,58 none have examined these relationships in construction, a workplace characterized by highly variable and changing work environments, nor have they examined the impact of these factors over time. Our study was conducted among unionized carpenter and floor layer apprentices, who may not be representative of older workers, other construction trades, or non-unionized workers. Our study population of apprentices were relatively young (mean age 28, average of <3 years in the construction trade). They differ from older workers in having less autonomy and job security, and also by having fewer years of cumulative exposure to heavy physical work and to workplace psychosocial stressors. While younger construction workers have markedly higher rates of chronic musculoskeletal disorders than a general working population,59 older construction workers have even higher rates of chronic musculoskeletal disorders, which are associated with work limitation, missed work, and reduced physical functioning.60 We studied carpenters and floorlayers, though other literature suggests that the work environment, work exposures, and outcomes we assessed are common across other construction trades. Compared to union trade workers, existing literature on non-union workers suggests that they are likely to have higher exposures to work stressors such as precarious work, injury hazards, and lack of management support.61
Findings from our study suggest that work organization and environment factors influence health and work outcomes among young construction trade workers. Future work with longitudinal data will examine the hypothesized paths between work factors, health behaviors, health outcomes, and work outcomes. This work further suggests that construction employer and union programs, policies, and practices should be examined for potential changes that would promote health and well-being among this large and growing population of workers. One approach to improving the safety and health of workers is through Total Worker Health® (TWH) programs, policies, and practices that address the protection of workers and promote workers’ health and well-being.20,62 Implementing such changes will be challenging, as most construction contractors are small businesses with limited financial resources and rudimentary occupational safety and health programs.62 The construction industry is also a complex system, where multiple parties including owners, insurers, general contractors, subcontractors, unions, and regulators influence work organization and environment. The use of intermediary organizations that interact closely with employers, such as labor unions and trade organizations, is one way to reach employers and to increase adoption of TWH interventions, particularly among small contractors.63
Engaging employers in efforts to change health habits is challenging, as these factors are seen as individual behaviors not under the employers’ control. The current paper adds to the literature demonstrating that employer policies and procedures are linked to workers’ health and health-based work abilities. We deliberately focused this paper on outcomes of prescription pain medication use, lost work days, work ability, and health-related productivity in order to help make a case for change in workplace policies and practices related to work organization and environmental factors.
Acknowledgements:
The Authors wish to thank the instructors and leaders of the Carpenters Joint Apprenticeship Program of St. Louis and Vicinity, Ms. Anna Kinghorn, and Mr. Skye Buckner-Petty.
Funding: Grant sponsor: National Institute for Occupational Safety and Health (NIOSH); Grant number: U19 OH008868.
Footnotes
Institution and Ethics approval and informed consent: Institutional review and ethics approval was obtained from the Human Subjects Office at University of Iowa, Iowa City, USA. Participants provided informed consent.
Disclosure (Authors): The authors declare no conflicts of interest.
Disclaimer: None
REFERENCES
- 1.Bureau of Labor Statistics. Occupational outlook handbook: Carpenters. 2012; 2012–2013 Edition Available at: http://www.bls.gov/ooh/Construction-and-Extraction/Carpenters.htm Accessed April 23, 2019.
- 2.National Institute for Occupational Safety and Health (NIOSH). National academies niosh program review: Construction. 2013; Available at: https://www.cdc.gov/niosh/nas/default.html Accessed April 23, 2019.
- 3.Ringen K, Englund A, Welch L, Weeks JL, Seegal JL. Why construction is different. Occup Med. 1995;10(2):255–259. [PubMed] [Google Scholar]
- 4.CPWR - The Center for Construction Research and Training. The construction chart book: The united states construction industry and its workers. 5th ed. Silver Spring, MD: CPWR - The Center for Construction Research and Training; 2013. [Google Scholar]
- 5.Sparer EH, Okechukwu CA, Manjourides J, Herrick RF, Katz JN, Dennerlein JT. Length of time spent working on a commercial construction site and the associations with worker characteristics. Am J Ind Med. 2015;58(9):964–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong XWS, Wang XW, Daw C, Ringen K. Chronic diseases and functional limitations among older construction workers in the united states: A 10-year follow-up study. J Occup Environ Med. 2011;53(4):372–380. [DOI] [PubMed] [Google Scholar]
- 7.Strickland JR, Eyer AA, Purnell JQ, Kinghorn AM, Herrick C, Evanoff BA. Enhancing workplace wellness efforts to reduce obesity: A qualitative study of low-wage workers in st louis, missouri, 2013–2014. Prev Chronic Dis. 2015;12(E67) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnes AJ, Brown ER. Occupation as an independent risk factor for binge drinking. Am J Drug Alcohol Abuse. 2013;39(2):108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee D, Fleming L, Arheart K, et al. Smoking rate trends in u.S. Occupational groups: The 1987 to 2004 national health interview survey. J Occup Environ Med. 2007;49(1):75–81. [DOI] [PubMed] [Google Scholar]
- 10.Solovieva S, Lallukka T, Virtanen M, Viikari-Juntura E. Psychosocial factors at work, long work hours, and obesity: A systematic review. Scand J Work Environ Health. 2013;39(3):241–258. [DOI] [PubMed] [Google Scholar]
- 11.Champagne N, Abreu M, Nobrega S, et al. Study report: Obesity/overweight and the role of working conditions: A qualitative, participatory investigation. In: UMass Lowell, MassCosh, Boston Worker’s Alliance; 2012:25. [Google Scholar]
- 12.Luckhaupt SE, Cohen MA, Li J, Calvert GM. Prevalence of obesity among u.S. Workers and associations with occupational factors. Am J Prev Med. 2014;46(3):237–248. [DOI] [PubMed] [Google Scholar]
- 13.Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W. Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease – a systematic review. Scand J Work Environ Health. 2010;36(3):202–215. [DOI] [PubMed] [Google Scholar]
- 14.Harley AE, Devine CM, Beard B, Stoddard AM, Hunt MK, Sorensen G. Multiple health behavior changes in a cancer prevention intervention for construction workers, 2001–2003. Prev Chronic Dis. 2010;7(3):A55. [PMC free article] [PubMed] [Google Scholar]
- 15.Okechukwu CA, Krieger N, Sorensen G, Li Y, Barbeau EM. Massbuilt: Effectiveness of an apprenticeship site-based smoking cessation intervention for unionized building trades workers. Cancer Causes Control. 2009;20(6):887–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ringen K, Anderson N, McAfee T, Zbikowski SM, Fales D. Smoking cessation in a blue-collar population: Results from an evidence-based pilot program. Am J Ind Med. 2002;42(5):367–377. [DOI] [PubMed] [Google Scholar]
- 17.Sorensen G, Barbeau E, Stoddard A, et al. Tools for health: The efficacy of a tailored intervention targeted for construction laborers. Cancer Causes Control. 2007;18(1):51–59. [DOI] [PubMed] [Google Scholar]
- 18.Strickland JR, Smock N, Casey C, Poor T, Kreuter W, Evanoff BA. Development of targeted messages to promote smoking cessation among construction trade workers. Health Educ Res. 2015;30(1):107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schill AL. Advancing well-being through total worker health(r). Workplace Health Saf. 2017;65(4):158–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schill AL, Chosewood LC. The niosh total worker health program: An overview. J Occup Environ Med. 2013;55(12 Suppl):S8–11. [DOI] [PubMed] [Google Scholar]
- 21.Tamers SL, Chosewood LC, Childress A, Hudson H, Nigam J, Chang C-C. Total worker health® 2014–2018: The novel approach to worker safety, health, and well-being evolves. 2019;16(3):321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schulte PA, Pana-Cryan R, Schnorr T, et al. An approach to assess the burden of work-related injury, disease, and distress. Am J Public Health. 2017;107(7):1051–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting u.S. Employers. J Occup Environ Med. 2004;46(4):398–412. [DOI] [PubMed] [Google Scholar]
- 24.Bush DM, Lipari RN. Substance use and substance use disorder by industry: Short report. Rockville, MD: April 16, 2015 2015. [PubMed] [Google Scholar]
- 25.Harduar Morano L, Steege AL, Luckhaupt SE. Occupational patterns in unintentional and undetermined drug-involved and opioid-involved overdose deaths - united states, 2007–2012. MMWR Morb Mortal Wkly Rep. 2018;67(33):925–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Massachusetts Department of Public Health, Bureau of Substance Addiction Services, Injury Surveillance Program, Office of Special Analytic Projects. Opioid-related overdose deaths in massachusetts by industry and occupation, 2011–2015. 2018.
- 27.CNA. 2015 risk outlook: Construction. Prescription opioid abuse: Risk factors and solutions. Chicago, IL: June 29, 2015 2015. [Google Scholar]
- 28.American Society of Safety Professionals. National crisis: Opioid abuse in the construction industry. 2018. https://www.assp.org/news-and-articles/2018/08/28/national-crisis-opioid-abuse-in-the-construction-industry Accessed August 22, 2019.
- 29.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The job content questionnaire (jcq): An instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. [DOI] [PubMed] [Google Scholar]
- 30.Zohar D, Luria G. A multilevel model of safety climate: Cross-level relationships between organization and group-level climates. J Appl Psychol. 2005;90(4):616–628. [DOI] [PubMed] [Google Scholar]
- 31.Neal A, Griffin MA. A study of the lagged relationships among safety climate, safety motivation, safety behavior, and accidents at the individual and group levels. J Appl Psychol. 2006;91(4):946–953. [DOI] [PubMed] [Google Scholar]
- 32.Ilmarinen J. The work ability index (wai). Occupational Medicine-Oxford. 2007;57(2):160–160. [Google Scholar]
- 33.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–365. [DOI] [PubMed] [Google Scholar]
- 34.R: A language and environment for statistical computing [computer program]. Version 3.5.0. Vienna, Austria: R Foundation for Statistical Computing; 2018. [Google Scholar]
- 35.CPWR - The Center for Construction Research and Training. Safety culture and climate in construction: Bridging the gap between research and practice. 2014; Available at: http://www.cpwr.com/sites/default/files/publications/CPWR_Safety_Culture_Final_Report_0.pdf Accessed April 23, 2019.
- 36.Chin DL, Hong O, Gillen M, Bates MN, Okechukwu CA. Occupational factors and smoking cessation among unionized building trades workers. Workplace Health Saf. 2012;60(10):445–452. [DOI] [PubMed] [Google Scholar]
- 37.Ham DC, Przybeck T, Strickland JR, Luke DA, Bierut LJ, Evanoff BA. Occupation and workplace policies predict smoking behaviors: Analysis of national data from the current population survey. J Occup Environ Med. 2011;53(11):1337–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zohar D. Safety climate in industrial organizations: Theoretical and applied implications. J Appl Psychol. 1980;65(1):96–102. [PubMed] [Google Scholar]
- 39.Karasek R, Theorell T. Health work, stress, productivity, and the reconstruction of working life Basic book. Inc, New York: 1990 [Google Scholar]
- 40.Dedobbeleer N, Beland F. A safety climate measure for construction sites. Journal of Safety Research. 1991;22(2):97–103. [Google Scholar]
- 41.Gillen M, Faucett JA, Beaumont JJ, McLoughlin E. Injury severity associated with nonfatal construction falls. Am J Ind Med. 1997;32(6):647–655. [DOI] [PubMed] [Google Scholar]
- 42.Mattila M, Rantanen E, Hyttinen M. The quality of work environment, supervision and safety in building construction. Safety Science. 1994;17(4):257–268. [Google Scholar]
- 43.Holmström EB, Lindell J, Moritz U. Healthy lower backs in the construction industry in sweden. Work Stress. 1993;7(3):259–271. [Google Scholar]
- 44.Dutra LM, Kim SS, Williams DR, Kawachi I, Okechukwu CA. Worksite safety climate, smoking, and the use of protective equipment by blue-collar building workers enrolled in the massbuilt smoking cessation trial. J Occup Environ Med. 2014;56(10):1082–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goldenhar LM, Hecker S, Moir S, Rosecrance J. The “goldilocks model” of overtime in construction: Not too much, not too little, but just right. J Safety Res. 2003;34(2):215–226. [DOI] [PubMed] [Google Scholar]
- 46.Zhang M, Murphy LA, Fang D, Caban-Martinez AJ. Influence of fatigue on construction workers’ physical and cognitive function. Occup Med (Lond). 2015;65(3):245–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lu ML, Nakata A, Park JB, Swanson NG. Workplace psychosocial factors associated with work-related injury absence: A study from a nationally representative sample of korean workers. Int J Behav Med. 2014;21(1):42–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kristensen TS. Sickness absence and work strain among danish slaughterhouse workers: An analysis of absence from work regarded as coping behaviour. Soc Sci Med. 1991;32(1):15–27. [DOI] [PubMed] [Google Scholar]
- 49.Alavinia SM, van den Berg TI, van Duivenbooden C, Elders LA, Burdorf A. Impact of work-related factors, lifestyle, and work ability on sickness absence among dutch construction workers. Scand J Work Environ Health. 2009;35(5):325–333. [DOI] [PubMed] [Google Scholar]
- 50.Kim SS, Dutra LM, Okechukwu CA. Contractor-, steward-, and coworker-safety practice: Associations with musculoskeletal pain and injury-related absence among construction apprentices. Int Arch Occup Environ Health. 2014;87(5):493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schwatka NV, Rosecrance JC. Safety climate and safety behaviors in the construction industry: The importance of co-workers commitment to safety. Work (Reading, Mass). 2016;54(2):401–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alavinia SM, van Duivenbooden C, Burdorf A. Influence of work-related factors and individual characteristics on work ability among dutch construction workers. Scand J Work Environ Health. 2007;33(5):351–357. [DOI] [PubMed] [Google Scholar]
- 53.Dale AM, Gardner BT, Zeringue A, et al. Self-reported physical work exposures and incident carpal tunnel syndrome. Am J Ind Med. 2014;57(11):1246–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the united states. Pain Med. 2011;12(4):657–667. [DOI] [PubMed] [Google Scholar]
- 55.Reinhart M, Scarpati LM, Kirson NY, Patton C, Shak N, Erensen JG. The economic burden of abuse of prescription opioids: A systematic literature review from 2012 to 2017. Appl Health Econ Health Policy. 2018;16(5):609–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Reidhead M, Porth L, Braman K. Overdose deaths, hospital visits and unfilled jobs: The opioid crisis in missouri and kansas. Missouri Hospital Association & Kansas Hospital Association; September 2017 2017. [Google Scholar]
- 57.Dale AM, Evanoff B, Macomber M, O’Reilly M, Rosen R, Schneider S. Can ergonomics programs help solve the opioid crisis? In. the Synergist: the Synergist; 2019. [Google Scholar]
- 58.Miranda H, Gore RJ, Boyer J, Nobrega S, Punnett L. Health behaviors and overweight in nursing home employees: Contribution of workplace stressors and implications for worksite health promotion. The Scientific World Journal. 2015;2015:915359–915369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dale AM, Ryan D, Welch L, Olsen MA, Buchholz B, Evanoff B. Comparison of musculoskeletal disorder health claims between construction floor layers and a general working population. Occup Environ Med. 2015;72(1):15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Welch L, Haile E, Boden LI, Hunting KL. Musculoskeletal disorders among construction roofers—physical function and disability. Scand J Work Environ Health. 2009;35(1):56–63. [DOI] [PubMed] [Google Scholar]
- 61.Ringen K, Dong XS, Goldenhar LM, Cain CT. Construction safety and health in the USA: Lessons from a decade of turmoil. Ann Work Expo Health. 2018;62(suppl_1):S25–S33. [DOI] [PubMed] [Google Scholar]
- 62.Rohlman DS, Campo S, Hall J, Robinson EL, Kelly KM. What could total worker health(r) look like in small enterprises? Ann Work Expo Health. 2018;62(suppl_1):S34–s41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sinclair R, Cunningham T, Schulte P. A model for occupational safety and health intervention diffusion to small businesses. Am J Ind Med. 2013;56(12):1442–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]