Supplemental Digital Content is available in the text.
Keywords: catecholamine, critical care, intensive care unit–acquired delirium, interaction effect, norepinephrine, secondary analysis
Objectives:
Abnormal secretion of catecholamines is well known to cause delirium. In particular, disturbances of catecholamine balance can cause ICU-acquired delirium. The aim of this study was to evaluate the association between the serum levels of catecholamines and the risk of occurrence of ICU-acquired delirium separately in patients who had/had not received exogenous catecholamines before ICU admission.
Design:
A secondary analysis of the data of 81 patients enrolled in our previous randomized clinical trial.
Setting:
ICU of an academic hospital.
Patients:
ICU patients in whom the serum levels of catecholamines were measured at ICU admission.
Interventions:
None.
Measurements and Main Results:
We evaluated the association between the serum levels of catecholamines measured at ICU admission and the risk of ICU-acquired delirium separately in patients who had received exogenous catecholamines at ICU admission (Ex[+] group) and those who had not received exogenous catecholamines (Ex[–] group). The serum levels of norepinephrine measured at ICU admission were significantly associated with the risk of ICU-acquired delirium in the Ex(–) group (odds ratio, 2.58; 95% CI, 1.02–6.52; p = 0.046), but not in the Ex(+) group (odds ratio, 1.02; 95% CI, 0.88–1.18; p = 0.823). Furthermore, there was a statistically significant interaction effect between the serum levels of norepinephrine and the use/nonuse of exogenous catecholamines at ICU admission in relation to the risk of occurrence of ICU-acquired delirium (pinteraction = 0.017).
Conclusions:
The serum levels of norepinephrine measured at admission were associated with the risk of occurrence of ICU-acquired delirium in patients who had not received exogenous catecholamines at ICU admission, whereas no such association was observed in those who had received exogenous catecholamines previously. Thus, the association between the serum levels of catecholamines measured at admission and the risk of ICU-acquired delirium differed between patients who had/had not received exogenous catecholamines at ICU admission.
Delirium, a neurobehavioral syndrome caused by dysregulation of the baseline neuronal activity secondary to systemic disturbances (1), is seen at a higher frequency in patients admitted to the ICU than in those hospitalized in general wards and is associated with a higher mortality, prolonged length of ICU stay, and higher treatment costs of ICU patients (2–6).
It has been suggested that the elevation of the serum levels of catecholamines may be one of the mechanisms underlying the development of delirium in patients admitted to the ICU. In the review article by Maldonado (7) on the subject, disturbances of catecholamine balance (neurotransmitter hypothesis) have been hypothesized as one of the seven hypotheses proposed to explain the pathophysiology of delirium. Elevated dopamine levels may lead, directly or indirectly, to neurobehavioral alterations via the excitotoxic effects of glutamine, and acute norepinephrine release may lead to further neuronal injury and delirium.
Although a few small studies have shown that the serum levels of stress markers, including norepinephrine, are significantly elevated in patients with delirium (8–10), these studies included only postoperative patients, and there are no reported studies that have investigated the association between the serum levels of catecholamines and the risk of ICU-acquired delirium. Considering the fact that the secretion of catecholamines is more severely disturbed in ICU patients than in patients admitted to general wards, the association with catecholamines may differ between ICU-acquired delirium and postoperative delirium.
Although investigation of the association between the serum levels of catecholamines and the risk of ICU-acquired delirium would be of great interest, an important problem in relation to analysis of the data is that both exogenous and endogenous catecholamines contribute to increased serum levels of catecholamines in ICU patients; therefore, even if an association was identified between the serum levels of catecholamines and the risk of ICU-acquired delirium, it would be difficult to judge whether it is exogenous or endogenous catecholamines that contribute more to the risk of development of ICU-acquired delirium. Therefore, for more precise evaluation of the association, we conducted the analysis separately in ICU patients who had received exogenous catecholamines and those who had not received exogenous catecholamines.
From this standpoint, the aim of this study was to evaluate the association between the serum catecholamine levels measured at ICU admission and the risk of occurrence of ICU-acquired delirium using data from the randomized controlled clinical trial conducted by us previously in non–postoperative ICU patients (11). We divided the patients into two groups, the Ex(–) group, consisting of patients who had not received exogenous catecholamines, and the Ex(+) group, consisting of patients who had received exogenous catecholamines, and evaluated the association between the serum catecholamine levels and the risk of occurrence of ICU-acquired delirium separately in the two groups, to determine if the association is modified by exogenous catecholamines administered before ICU admission.
MATERIALS AND METHODS
Study Design
This study was a secondary analysis, conducted with the approval of the Research Ethics Board of Nagoya University Hospital (2015-0005), of data obtained from the Melatonin Evaluation of Lowered Inflammation of ICU trial (MELIt) (11), which was a single-center, triple-blinded, randomized, placebo-controlled trial conducted previously by us to evaluate the prophylactic effect of ramelteon against the development of ICU-acquired delirium. The MELIt trial was conducted in 92 adult patients (≥ 20 yr old) admitted to our ICU between May 2015 and April 2017, who could receive their medications orally or through a nasogastric tube during the first 48 hours after their admission to the ICU. Patients who were already receiving ramelteon or fluvoxamine maleate prior to admission to the ICU, who had known allergy to ramelteon, or who refused to participate were excluded from the trial.
In the MELIt trial (11), we measured the serum levels of catecholamines (norepinephrine, epinephrine, and dopamine) at the time of admission to the ICU in the eligible patients, all of whom were included in the analysis in this study. For the analysis in this study, we classified the patients into two groups according to whether they had or had not received exogenous catecholamines (norepinephrine, epinephrine, and dopamine) at the time of their admission to the ICU.
Outcome
The primary endpoint of this study was the occurrence of delirium during the patients’ stay in the ICU. Delirium was assessed every 4 hours using the Confusion Assessment Method for the ICU (12) by trained ICU nurses (the assessment was skipped if the patients were sleeping), and also by ICU doctors, as needed.
Use of Catecholamines in our ICU
We use norepinephrine as a first-line treatment for all types of shock. Epinephrine or dopamine may be added to norepinephrine in patients with decreased cardiac contractility.
Statistical Analysis
For comparison of the patients’ baseline characteristics, we performed Fisher exact test for categorical variables and Mann-Whitney U test for continuous variables. To evaluate the association between the serum levels of catecholamines and the risk of occurrence of delirium, univariate and multivariable logistic regression analysis were performed. The multivariable logistic regression analysis was adjusted for three covariates (age, < 60 yr/≥ 60 yr; Acute Physiology and Chronic Health Evaluation [APACHE] II score, < 30/≥ 30; and the use/nonuse of mechanical ventilation), which were considered as clinical factors that could potentially exert a significant influence on the risk of occurrence of delirium. These were the same covariates that we used for adjustment in our primary analysis in the MELIt trial (11).
Multivariable logistic regression analysis was also conducted to evaluate the interaction effect between the serum levels of norepinephrine and the use/nonuse of exogenous catecholamines in relation to the risk of occurrence of delirium. All reported p values are two-sided, and p values of less than 0.05 were regarded as indicative of statistical significance. All the statistical analyses were conducted using the R software, version 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria; http://www.r-project.org).
RESULTS
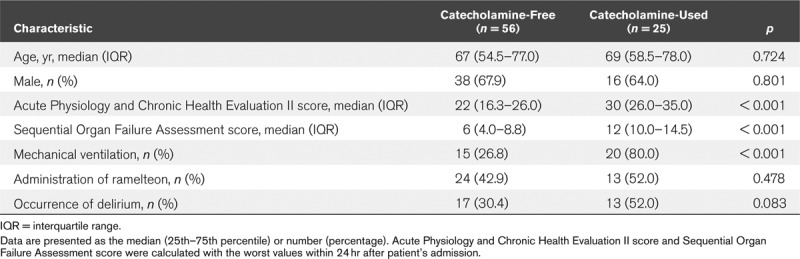
Of the 92 patients enrolled in our previous trial, the serum levels of catecholamines were measured at the time of admission to the ICU in 81 patients. Of these 81 patients, 25 had received exogenous catecholamines at the time of their ICU admission (Ex[+] group), whereas the remaining 56 subjects had not received exogenous catecholamines (Ex[–] group). The baseline characteristics of the 81 patients in the Ex(+) and Ex(–) groups are summarized in Table 1, and the plots of the serum levels of catecholamines in the Ex(+) and Ex(–) groups are shown in Supplemental Figure 1 (Supplemental Digital Content 1, http://links.lww.com/CCX/A134; and legend, Supplemental Digital Content 7, http://links.lww.com/CCX/A140) and Supplemental Figure 2 (Supplemental Digital Content 2, http://links.lww.com/CCX/A135; and legend, Supplemental Digital Content 7, http://links.lww.com/CCX/A140). We analyzed the data of the two groups separately.
TABLE 1.
Baseline Characteristics of the Analyzed Patients in This Study
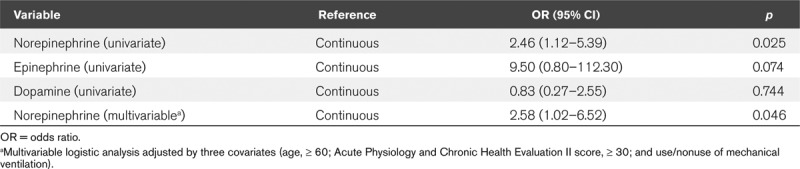
The characteristics of the patients in the Ex(–) group are summarized in Supplemental Table 1 (Supplemental Digital Content 3, http://links.lww.com/CCX/A136). ICU-acquired delirium occurred in 30.4% of the patients (17/56) in this group. Patients with delirium had significantly higher serum levels of catecholamines, as well as higher APACHE II scores (p = 0.047). The results of the univariate and multivariable regression analyses conducted to evaluate the association between the serum levels of catecholamines and the risk of occurrence of delirium in the Ex(–) group are summarized in Table 2. The multivariable logistic regression analysis identified serum level of norepinephrine as an independent risk factor for the occurrence of delirium (odds ratios [OR], 2.58; 95% CI, 1.02–6.52; p = 0.046). For detecting the optimal cutoff value of the serum norepinephrine level as a predictor of the risk of delirium, a receiver operating characteristic curve was constructed plotted (Supplemental Fig. 3, Supplemental Digital Content 4, http://links.lww.com/CCX/A137; and legend, Supplemental Digital Content 7, http://links.lww.com/CCX/A140). The most optimal cutoff value was determined to be 0.844 ng/mL, with a sensitivity of 0.65 and a specificity of 0.72 (area under the curve, 0.686) for predicting the risk of delirium. The sensitivity and specificity were 0.94 and 0.23, respectively, for the cutoff value of 0.388 ng/mL, and 0.29 and 0.95, respectively, for the cutoff value of 2.005 ng/mL.
TABLE 2.
Univariate and Multivariable Analyses Conducted to Evaluate the Association Between the Serum Levels of Catecholamines and the Risk of Occurrence of Delirium in Patients Who Had Not Received Exogenous Catecholamine Administration
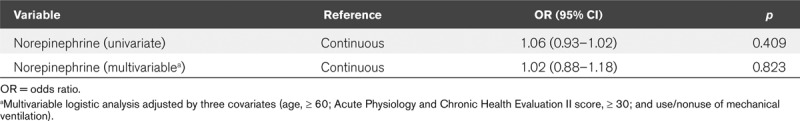
Next, the data of the patients in the Ex(+) group were analyzed. The characteristics of the patients in the Ex(+) group are summarized in Supplemental Table 2 (Supplemental Digital Content 5, http://links.lww.com/CCX/A138). Delirium occurred in 52.0% (13/25) of the patients in this group during their ICU stay. Although there was a statistically significant difference in age between the patients with and without delirium (p = 0.017), there was no significant difference in the serum levels of catecholamines between the patients with and without delirium. The results of the univariate and multivariable regression analyses conducted to evaluate the association between the serum levels of norepinephrine and the risk of occurrence of delirium in the Ex(+) group are summarized in Table 3. There was no statistically significant association between the serum levels of norepinephrine and the risk of occurrence of delirium (OR, 1.02; 95% CI, 0.88–1.18; p = 0.823).
TABLE 3.
Univariate and Multivariable Analyses Conducted to Evaluate the Association Between the Serum Levels of Norepinephrine and the Risk of Occurrence of Delirium in Patients Who Had Received Exogenous Catecholamine Administration
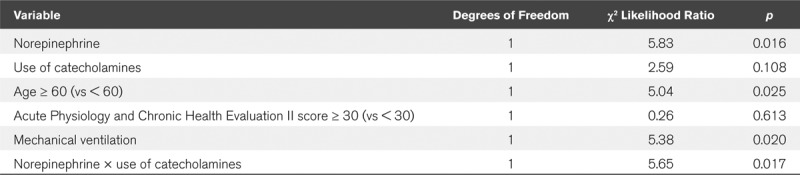
Using the data of all the 81 patients in whom the serum levels of catecholamines were measured, regardless of whether they had received exogenous catecholamines or not, we performed multivariable logistic regression analysis to determine the interaction effect between the serum levels of norepinephrine and the use/nonuse of exogenous catecholamines in relation to the risk of occurrence of delirium, with adjustments for three covariates (age, < 60 yr/≥ 60 yr; APACHE II score, < 30/≥ 30; and the use/nonuse of mechanical ventilation); the results revealed a statistically significant interaction effect (pinteraction = 0.017) (Table 4). In addition, we performed sensitivity analysis using three other variables for adjustment (male/female, Sequential Organ Failure Assessment score, and presence/absence of dementia before admission), which also revealed a statistically significant interaction effect between the serum levels of norepinephrine and the use/nonuse of exogenous catecholamines in relation to the risk of occurrence of delirium (Supplemental Table 3, Supplemental Digital Content 6, http://links.lww.com/CCX/A139).
TABLE 4.
Interaction Analysis Between the Serum Levels of Norepinephrine and the Use/Nonuse of Exogenous Catecholamines in Relation to the Risk of Occurrence of Delirium
DISCUSSION
Several basic studies have indicated the influence of the serum levels of catecholamines on the risk of occurrence of delirium (13). However, the actual association between the serum levels of catecholamines and the risk of ICU-acquired delirium in actual clinical practice still remains unclear. In the present study, although the serum levels of norepinephrine measured at the time of admission to the ICU were not associated with the risk of occurrence of ICU-acquired delirium in the Ex(+) group, a significant association between the two parameters was observed in the Ex(–) group. Our interaction analysis showed that this association was statistically significantly modified by the use/nonuse of exogenous catecholamines. To the best of our knowledge, our study is the first to suggest the possibility that the association between ICU-acquired delirium and the serum levels of catecholamines may differ between patients administered and not administered exogenous catecholamines.
Norepinephrine has been shown to have a negative effect on the CNS in animal models, leading to the occurrence of delirium. A previous published animal study showed that acute norepinephrine release could lead to neuronal injury and the development of delirium (13). However, in actual clinical practice, the administration of norepinephrine is often needed for hemodynamic stabilization. It may be easy to conceive this as being beneficial for preventing the development of delirium in patients admitted to the ICU because hemodynamic instability itself is one of the strong risk factors for the occurrence of delirium (14). Considering the results of our interaction analysis and analysis of data from the Ex(+) group, our study results suggest that exogenously administered norepinephrine may not contribute to the increased risk of ICU-acquired delirium in patients with elevated catecholamine levels, which would validate the use of norepinephrine for patients who need it for hemodynamic stabilization, even if the patients are at an elevated risk for delirium, in actual clinical practice.
On the other hand, the results of our analysis of data from the Ex(–) group showed that the serum levels of norepinephrine measured at the time of admission to ICU were an independent risk factor for the occurrence of ICU-acquired delirium. Because the area under the curve (AUC) was nearly 0.70 (an AUC of 0.70 is regarded as reflecting a moderate discriminative ability according to a previous study [15]), we considered it important to evaluate the risk of development of ICU-acquired delirium associated with the serum levels of norepinephrine in combination with other factors. Nevertheless, it appears that critical care patients with increased serum levels of norepinephrine at the time of ICU admission, in the absence of exogenous catecholamine administration, are likely to develop ICU-acquired delirium during their ICU stay and may be candidates for intensive prophylactic treatment against the development of delirium.
Why were serum levels of catecholamines associated with the risk of occurrence of delirium in ICU patients who did not receive exogenous catecholamines, while they were not in those who received exogenous catecholamines? This discrepancy could be explained by the differential association of endogenous and exogenous catecholamines on the activity of the sympathetic nervous system in patients. Delirium has been reported to be associated with excessive activity of the sympathetic nervous system (16), and the serum levels of endogenous norepinephrine may directly reflect the activity of the sympathetic nervous system, in the absence of exogenous catecholamine administration. This could be a possible reason why the serum levels of norepinephrine were associated with the risk of occurrence of delirium in patients who had not received exogenous catecholamines in the present study. On the other hand, the serum levels of norepinephrine in patients receiving exogenous catecholamines may not reliably reflect the activity of the sympathetic nervous system because in actual clinical practice, exogenous catecholamines are administered for improving the hemodynamic stability in critically ill patients, and possibly serve to reduce the excessive activity of the sympathetic nervous system. Therefore, the serum levels of norepinephrine may be no longer associated with the risk of occurrence of delirium in the presence of both endogenous catecholamines (which reflect the activity of the sympathetic nervous system) and exogenous catecholamines (which serve to reduce excessive sympathetic nervous activity). It would be great interest to collect data on the serum levels of catecholamines before and after administration of exogenous catecholamines in the same patient, to evaluate the differential association of the parameter under the two different conditions with the risk of occurrence of delirium.
Because this study was a secondary analysis of the MELIt trial, the interaction between the serum levels of norepinephrine and the use/nonuse of exogenous catecholamines could have been potentially affected by ramelteon. Given that melatonin can influence the production of catecholamines biologically (17), it is possible that exogenous ramelteon can also modify the association between the serum levels of catecholamines and the risk of occurrence of delirium in patients not receiving exogenous catecholamines. Our data showed no statistically significant interaction effect between the serum levels of norepinephrine and the use/nonuse of ramelteon in relation to the risk of occurrence of delirium (pinteraction = 0.264), but this could also possibly be because of the small sample size. Thus, it will be a great interest to examine the relationship among the serum levels of catecholamines, delirium, and melatonin administration in the future.
There were several limitations to this study. First, this study was a small-sized single-center study, which could make generalization of the results difficult. Second, the influence of treatment after ICU admission on the risk of occurrence of delirium was not analyzed in this study, although we assumed that the treatment was not different between the two groups, because we used the data of our previous randomized controlled clinical trial for this study. Third, we did not consider the influence of exogenous catecholamine administration on the serum levels of catecholamines in the analysis of the Ex(+) group because there was no method of converting the concentration of exogenous catecholamines administered to the serum levels. Finally, in this study, we evaluated the relationships of the serum concentrations of the three components of catecholamines measured at ICU admission. On the other hand, as in the evaluation of catecholamine exposure as management of pheochromocytoma, new findings may be obtained if the levels of urinary metabolites, including metanephrine, normetanephrine, vanillylmandelic acid, and homovanillic acid, were evaluated. We did not determine the relationship between the urinary catecholamine metabolite levels measured at ICU admission and the risk of development of delirium. A large prospective study to determine the association between the serum levels of catecholamines and the risk of occurrence of ICU-acquired delirium is warranted.
CONCLUSIONS
The serum levels of norepinephrine measured at admission were associated with the risk of occurrence of ICU-acquired delirium in patients who had not received exogenous catecholamines at ICU admission, whereas no such association was observed in those who had received exogenous catecholamines previously. Thus, the association between the serum levels of catecholamines measured at admission and the risk of ICU-acquired delirium differed between patients who had/had not received exogenous catecholamines at ICU admission.
ACKNOWLEDGMENTS
We thank the residents, fellows, paramedical staff, and the secretary Teruko Mizutani of our ICU and also Nagoya University Hospital and the Department of Emergency and Critical Care Medicine for the data collection and treatment support.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Supported, in part, by grant from funding agencies in the public, commercial, or not-for-profit sectors. Supported by the Clinical Research Program at Nagoya University.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Maldonado JR. Pathoetiological model of delirium: A comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin. 2008; 24:789–856, ix [DOI] [PubMed] [Google Scholar]
- 2.Inouye SK. Delirium in older persons. N Engl J Med. 2006; 354:1157–1165 [DOI] [PubMed] [Google Scholar]
- 3.Ely EW, Gautam S, Margolin R, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001; 27:1892–1900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shehabi Y, Riker RR, Bokesch PM, et al. ; SEDCOM (Safety and Efficacy of Dexmedetomidine Compared With Midazolam) Study Group. Delirium duration and mortality in lightly sedated, mechanically ventilated intensive care patients. Crit Care Med. 2010; 38:2311–2318 [DOI] [PubMed] [Google Scholar]
- 5.Barr J, Fraser GL, Puntillo K, et al. ; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013; 41:263–306 [DOI] [PubMed] [Google Scholar]
- 6.Milbrandt EB, Deppen S, Harrison PL, et al. Costs associated with delirium in mechanically ventilated patients. Crit Care Med. 2004; 32:955–962 [DOI] [PubMed] [Google Scholar]
- 7.Maldonado JR. Neuropathogenesis of delirium: Review of current etiologic theories and common pathways. Am J Geriatr Psychiatry. 2013; 21:1190–1222 [DOI] [PubMed] [Google Scholar]
- 8.Kazmierski J, Banys A, Latek J, et al. Cortisol levels and neuropsychiatric diagnosis as markers of postoperative delirium: A prospective cohort study. Crit Care. 2013; 17:R38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mu DL, Wang DX, Li LH, et al. High serum cortisol level is associated with increased risk of delirium after coronary artery bypass graft surgery: A prospective cohort study. Crit Care. 2010; 14:R238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deiner S, Lin HM, Bodansky D, et al. Do stress markers and anesthetic technique predict delirium in the elderly? Dement Geriatr Cogn Disord. 2014; 38:366–374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishikimi M, Numaguchi A, Takahashi K, et al. Effect of administration of ramelteon, a melatonin receptor agonist, on the duration of stay in the ICU: A single-center randomized placebo-controlled trial. Crit Care Med. 2018; 46:1099–1105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: Validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001; 286:2703–2710 [DOI] [PubMed] [Google Scholar]
- 13.Bhardwaj A, Brannan T, Martinez-Tica J, et al. Ischemia in the dorsal hippocampus is associated with acute extracellular release of dopamine and norepinephrine. Neural Transm Gen Sect. 1990; 80:195–201 [DOI] [PubMed] [Google Scholar]
- 14.Zaal IJ, Devlin JW, Peelen LM, et al. A systematic review of risk factors for delirium in the ICU. rit Care Med. 2015; 43:40–47 [DOI] [PubMed] [Google Scholar]
- 15.Akobeng AK. Understanding diagnostic tests 3: Receiver operating characteristic curves. Acta Paediatr. 2007; 96:644–647 [DOI] [PubMed] [Google Scholar]
- 16.Maldonado JR. Delirium pathophysiology: An updated hypothesis of the etiology of acute brain failure. Int J Geriatr Psychiatry. 2018; 33:1428–1457 [DOI] [PubMed] [Google Scholar]
- 17.Komatsubara M, Hara T, Hosoya T, et al. Melatonin regulates catecholamine biosynthesis by modulating bone morphogenetic protein and glucocorticoid actions. J Steroid Biochem Mol Biol. 2017; 165:182–189 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


