Abstract
Objective The objective of this study was to evaluate the effect of nano-SiO 2 addition on the flexural strength (FS) of repaired acrylic denture base.
Materials and Methods Heat-polymerized acrylic resin specimens were fabricated in dimensions of (65 × 10 × 2.5 ± 0.1 mm 3 ) and then sectioned and prepared, creating repair gap with butt (90 degrees) and bevel (45 degrees) repair surface designs forming two main groups according to joint design. Further subdivision was done into four groups ( n = 10) according to nano-SiO 2 concentration: one unmodified group and three modified groups (0.25, 0.5, and 0.75 wt %) in the autopolymerized repair resin. Each pair of a specimen was assembled in a mold and repaired according to manufacturer’s recommendations.
Statistical Analysis Three-point bending test was done to measure FS, followed by scanning electron microscope (SEM) examination for fracture surface analysis. Data were analyzed using ANOVA and Tukey’s post hoc test (α = 0.05).
Results The addition of nano-SiO 2 significantly improved FS of repaired acrylic resin in comparison to the unmodified group ( p ˂ 0.05). For butt joint, significant differences between nano-SiO 2 reinforced groups were noticed ( p ˂ 0.05), while reinforced beveled groups did not differ significantly ( p ˃ 0.05). Bevel design remarkably increased FS compared with butt design per respective filler concentration. From the SEM images, improved FS was presented with a homogeneous distribution of nano-SiO 2 within polymethyl methacrylate.
Conclusion Nano-SiO 2 addition to repair resin and 45 degree-beveled repair surface increased FS of repaired acrylic resin.
Keywords: denture repair, flexural strength, reinforcement, SiO 2 nanoparticles
Introduction
Polymethyl methacrylate (PMMA) denture base material has low impact and flexural strength (FS); therefore, denture fracture is very common. 1 2 Repair of fractured denture is recommended to reduce the cost or the time needed for new denture fabrication. 3 4 A satisfactory denture repair material has to be of the same color of the original denture base and restores its original strength. Autopolymerized acrylic resin was found to meet the first aforementioned requirement; however, due to its poor mechanical properties, repeated denture fracture may occur. 5 6 Such situations act as major annoyance to clinicians and consume their time. Numerous researches investigated different repair materials, reinforcements, surface treatments, and repair surface designs to improve the repair strength and avoid recurrent fracture of the denture base. 3 7
Repair surface design modifications were proposed as an attempt to improve repair strength. 8 9 Butt joint is commonly used due to its ease of preparation and clinical application. On the other hand, bevel joint demonstrated high mechanical properties. 10 Moreover, the damaging tensile stress can be shifted to shear stress by having larger bonding area and creating 45 degrees bevel at the interface. 3 9 Although surface design modifications improved the repair strength, the poor strength of repair material was reported based on the increased cohesive fractures within repair materials. 11 Therefore, reinforcement of the repair resin is considered an appropriate solution for denture repair. These reinforcements included metal wires, fibers, 11 12 or nanoparticles. 3 12
Nanoparticles gained their importance due to their size, large specific surface area, and good interfacial interaction with organic polymers. 13 14 Among these nanoparticles, silicon dioxide (nano-SiO 2 ) was reported by previous studies 1 15 16 to produce high mechanical and thermal properties when incorporated with PMMA. Pervious study found that low concentrations of nano-SiO 2 addition into PMMA denture base materials allowed uniform dispersion, prevented agglomeration, and finally enhanced the mechanical properties of the nanocomposite. 17 In 2014, Balos et al reported that adding low amount of nano-SiO 2 to conventional PMMA dentures could strengthen them, improve their resistance to cracking, and make them more durable. 18 In addition to the mentioned advantages, the properties of PMMA nanocomposite depend on the type, shape, concentration, and size of the nanofillers as well as their interaction with the PMMA matrix. 1 19 Moreover, the treatment of reinforcement material with silane coupling agent improved the bond strength between the filler and the resin, subsequently enhancing repair strength. 18
Up to now, the effect of nano-SiO 2 on repair strength of acrylic resin has not been well evaluated. Therefore, this study was performed to assess and compare the effects of nano-SiO 2 addition with different repair surface design on the FS of repaired PMMA denture base. The null hypothesis was that the addition of various concentrations of nano-SiO 2 and repair surface designs will not improve FS of repaired PMMA denture base.
Materials and Methods
A pilot study done with nano-SiO 2 concentrations of 0.25 to 5% revealed that lower than 1% nano-SiO 2 improved the FS of the resin base. The World Health Organization sample size calculation equation with 80% power and 0.05 significance value was used. Based on previous studies, 3 16 the power analysis revealed that 80 specimens (total of eight groups, four groups per surface design, n = 10) were required to detect differences among different reinforcement groups and their effects on FS of repaired acrylic resin.
Specimens Preparation
Heat-polymerized (Major Base 20; Major Prodotti Dentari SPA, Moncalieri, Italy) acrylic resin specimens were prepared in dimensions of 65 × 10 × 2.5 ± 0.1 mm according to ADA specifications no. 12 for denture base polymer. 20 The specimens were fabricated according to the methodology described in previous studies. 3 12 Once polymerized, finished, and polished, they were stored in distilled water at 37°C for 1 week. Following that, specimens were prepared and standardized for repair as stated by Gad et al 3 and illustrated in Fig. 1 , where specimens were sectioned and prepared with two surface designs; butt (90 degrees) and bevel (45 degrees) repair surfaces with 2.5 mm repair-gap measured at the intaglio side. Specimens per surface design were randomly categorized into four groups according to nano-SiO 2 concentration in the repair resin ( Table 1 ).
Fig. 1.
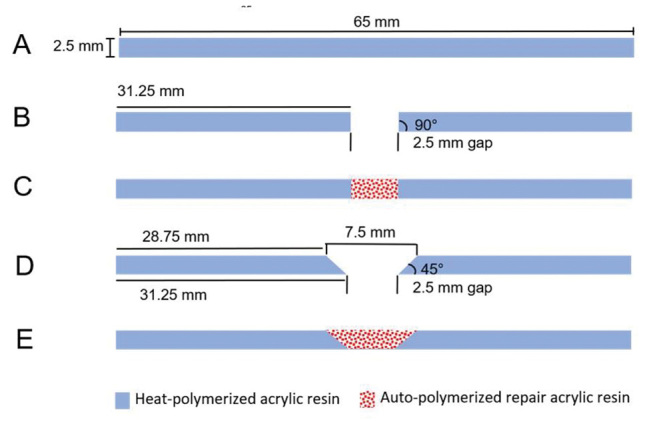
Illustrated diagram for acrylic resin specimen dimensions, preparation, and repair. ( A ) Intact specimen; ( B ) butt joint preparation; ( C ) repaired butt joint specimen; ( D ) bevel joint preparation; and ( E ) repaired bevel joint specimen.
Table 1. Specimens grouping and coding according to surface design and nano-SiO 2 concentration .
| Nano-SiO 2 concentration | Surface design | |
|---|---|---|
| Butt joint (90 degrees) | Bevel joint (45 degrees) | |
| 0% | BT0 | BV0 |
| 0.25% | BT25 | BV25 |
| 0.5% | BTS | BV5 |
| 0.75% | BT75 | BV75 |
Nano-SiO 2 (AEROSIL R812; Evonik-Degussa white color, 99.5% purity, size 12 nm, specific surface area 150 to 550 m 2 /g, and intensity 2.2 g/cm 3 ) was silanized using 97% (γ-MPS), (Shanghai Richem International Co., Ltd.) following the steps described by Karci et al, 16 and da Silva et al. 21 Salinized nano-SiO 2 was weighted using digital balance (WENSAR Mab Dab Series Analytical Balance, DAB 220) in concentrations of 0.25, 0.5, and 0.75 wt% of repair acrylic powder 16 21 (Major Repair; Major Prodotti Dentari SPA, Moncalieri, Italy). To assure equal filler distribution within PMMA powder, the nano-SiO 2 concentrations were independently blended with the PMMA powder at 400 rpm for 30 minutes. 3 16 21
A metal mold with internal dimensions of 65 × 10 × 2.5 mm was used for repair procedure standardization. To repair the sectioned specimens, repair surfaces were treated with monomer for 120 seconds 22 and then each pair of a specimen was assembled in the mold insuring a repair gap of 2.5 mm at the intaglio side. Prepared repair resin with the different nano-SiO 2 concentrations was mixed independently according to manufacturer instructions and packed into the repair gap. The polymerization was done in a pressure vessel for 15 minutes at two bars and 55°C. After polymerization, the specimens were retrieved and tungsten carbide bur (HM 79GX-040 HP; Meisinger, Centennial, CO, United States) was used to remove excess resins, followed by polishing using progressively finer grits of silicon carbide papers (320, 400, and 600). Pumice (Steribim Super; Bego, Wilhelm-Herbst-Strabe, Germany) was mixed with water and used for final polish with soft bristle brush. A digital caliper was utilized to evaluate repaired specimens’ dimensions. After that, the specimens were stored in distilled water for 48 hours at 37°C prior to testing.
To measure the FS of repaired specimens, three-point bending test was performed using universal testing machine (Instron 8871; Instron Co., Norwood, MA, United States) where specimens were positioned horizontally on two vertical supports 50 mm apart. The load was applied centrally at the repaired area at intaglio surface of the specimens using a round-ended tip (2.5 mm diameter hardened steel rod) attached to a 5KN load cell. The load was applied at a crosshead speed of 5 mm/min until fracture. The predetermined variables of distance between the supports (L), the width (b), and thickness (d) of the specimen; all in (mm); in addition to the load at fracture (W) recorded in newton (N) were used to calculate the FS in (MPa) using the following formula:
 .
7
22
.
7
22
Scanning Electron Microscopy
The nature of failure was examined by bare eye and SEM as described by Gad et al 22 and Qaw et al. 23 The morphology of the fractured surfaces of specimens was further examined using SEM (FEI; INSPECT S50, Czech Republic), where various magnifications were used to classify the nature of failure. Compact and smooth surface represents brittle fracture, while rough and jagged appearance represents ductile fracture mode. 23
Statistical Analysis
Data analysis was performed using SPSS-20.0 (IBM software; Chicago, IL, United States). Kolmogorov–Smirnov test assured that results were well distributed. The results were presented as means and standard deviations. Groups were compared by means of one-way ANOVA to study the effects of different nano-SiO 2 concentrations on FS (between and within groups), followed by Tukey’s post hoc test for pairwise comparisons within groups at α = 0.05.
Results
The mean values, standard deviations, statistical significances of FS between and within groups are summarized in Table 2 . The results showed that the mean values varied widely between unmodified and nano-SiO 2 modified repaired groups. Regarding butt joint groups (BT), and in comparison to the control group, the FS was significantly increased with nano-SiO 2 addition for all groups ( p < 0.05). Among reinforced butt joint groups, there was no significant difference between BT25/BT5 ( p = 0.310) and BT5/BT75 ( p = 0.230) while a significant difference in FS was found between BT25/BT75 ( p < 0.05) with the latter showing lower value.
Table 2. Mean (± standard deviation) and statistical significance of flexural strength (MPa) for all tested groups.
| Surface design | Flexural strength-MPa (±SD) | |||
|---|---|---|---|---|
|
Abbreviations: BT, butt joint; BV, bevel joint; SD, standard deviation. Note: Identical lowercase letters denote no significant differences within respective raw regarding nano-SiO 2 concentration ( p > 0.05), while per surface design, all groups are showing significant differences per column ( p ˂ 0. 001). | ||||
| Butt (90 degrees) | BT0 | BT25 | BT5 | BT75 |
| 54.23 (±5.21) | 75.43 (±4.84) a | 73.06 (±3.91) a,b | 71.79 (±6.32) b | |
| Bevel (45 degrees) | BV0 | BV25 | BV5 | BV75 |
| 61.34 (±5.09) | 81.54 (±6.93) a | 80.42 (±4.05) a | 79.82 (±6.11) a | |
For bevel groups (BV), and in comparison to control group, FS was significantly increased with nano-SiO 2 addition for all groups ( p < 0.05). Among bevel joint reinforced groups, there was no significant difference between any of the groups ( p > 0.05).
Comparing BT and BV groups, results showed a significant increase in FS for bevel groups per respective nano-SiO 2 concentration ( p < 0.05), and the highest FS value of any modified group reported in this study was with BV25 (81.54 ± 6.93 MPa) and the lowest was with BT75 (71.79 ± 6.32 MPa).
As shown in Fig. 2 , for butt joint (BT0) and bevel joint (BV0), cohesive failure was more dominant. While for all modified groups (BT25, BT5, and BT75) and (BV25, BV5, and BV75), adhesive failure was more prevalent.
Fig. 2.
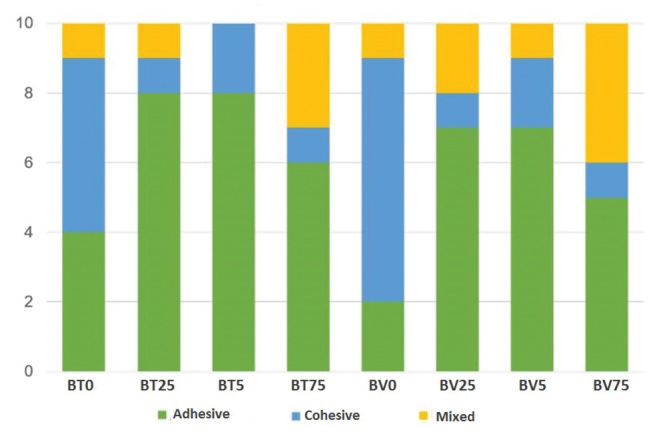
Nature of failure of fractured specimens.
SEM analysis for the different types of fracture modes revealed that adhesive fracture was present at the edge profile of repaired surface, while cohesive fracture happened within repair material. A mixed type of fracture was clearly present as the fractured surface displayed two types of materials, denture base resin and repair resin with different percentages. SEM examinations for fractured surfaces revealed that the control group specimens exhibited rough surfaces with few lamellae like structures as well as smooth background. According to the topography of fractured-surfaces of nano-SiO 2 containing specimens, more lamellae and deep pits were noticed suggesting ductile mode of fracture. Images also showed homogeneous distribution of nano-SiO 2 within the resin matrix at low concentrations. The amount of particle aggregation increased as the percentage of nano-SiO 2 increased in the polymer matrix with signs of particle agglomeration resulting in cluster formation.
Discussion
Some important factors dictate which repair material is to be used including the material strength, repair surface design, and the use of repair reinforcements. 11 Although previous studies investigated PMMA/SiO 2 nanocomposite denture base properties and recommended using nano-SiO 2 in low concentrations, its effect on repair strength has not been evaluated. Therefore, this study was conducted to evaluate the effect of nano-SiO 2 addition and surface design on the repair strength of PMMA acrylic resin. According to the results, the null hypothesis was rejected because the addition of different concentrations of nano-SiO 2 and the modification of repair surface design affected the FS of repaired PMMA acrylic resin bases.
Repair surface design is considered one of the most important factors that affect repair strength. 3 11 Beveling significantly increased FS in comparison to butt joint and this was noticed even with nano-SiO 2 addition. This might be due to the increase in the surface area available for bonding between denture base and repair material. 4 Furthermore, having a 45 degrees bevel at the interface could change the tensile stress into less damaging shear stress. 9 This finding is in agreement with previous studies, 8 9 where it was found that beveled surfaces improved the mechanical properties of repaired resin bases over butt surface design. The analysis of the nature of failure supported these suggestions, where BT groups failed mainly adhesively. This could be linked to the small surface area that butt joint offers for bonding. 24 The BV had an overall more cohesive and mixed failures compared with the BT groups, confirming that repair surface beveling increases FS by increasing the interface and having larger bonding area.
With both surface designs, nano-SiO 2 addition increased the FS in comparison to unmodified groups. The increase in low nano-SiO 2 concentration may be attributed to the homogeneous distribution of nanoparticles and their ability to fill interpolymeric chain spaces and restrict their movement. 16 25 26 Additionally, the silane treatment enabled nano-SiO 2 to form strong bonds with the polymer matrix. 27 To add to that, interfacial shear strength between nanoparticles and resin matrix owing to crosslinking or supramolecular bonding could prevent crack propagation and increase FS. 28 The results of this study agree with Balos et al, 18 who concluded that low nano-SiO 2 content provides better mechanical properties compared with high content.
The nanocomposites mechanical properties can be enhanced using different techniques, fillers with different shapes, sizes, concentrations, distribution, and connection to the polymer matrix. 1 As nano-SiO 2 concentrations increased from 0.25 to 0.75%, the FS gradually but significantly decreased with butt joint while the reduction was insignificant with bevel joint. The 0.75% nano-SiO 2 reinforced groups for both joint designs presented the lowest FS values for reinforced groups. This can be explained by silica nanoparticle aggregation and cluster formation responsible for weak bonding and stress concentration. 16 Previous studies by da Silva et al, 21 Zuccari et al, 29 Mc Nally et al, 30 Sodogar et al, 31 and Mansour et al 32 found similar results to those of the current study.
Generally, and as reported in the literature, SEM images of ductile type of fractures are characterized by rough fracture surfaces, microcracks, crack deflection or restriction, and particle yielding, 16 while brittle type of fracture is usually represented by mirror like appearance of fracture surface with no cracking. 23 Based on the SEM findings of this study, the nano-SiO 2 addition in low concentrations resulted in features of ductile nature which proves the positive effect of nano-SiO 2 on FS of repaired resin. While in high concentrations, loosely attached clusters were formed and may have acted as stress concentration areas leading to a decrease in FS.
Other confirming finding of the effect of reinforcement on the repair material is that the unreinforced groups failed mainly with cohesive type of fracture. While for reinforced groups, the most common failure type was adhesive, indicating that the incorporation of nano-SiO 2 into repair resin increased the strength of rapier material itself making the denture base/repair resin junction the weakest point, necessitating more focus on the interface. The attention could be directed toward chemical, mechanical, or combination technique of modification with intermediate coupling agents in addition to repair material reinforcement. 23
Clinically, low concentrations of nano-SiO 2 addition to repair resin material could be a promising method for improving denture longevity and repair strength. Finally, the results of this study should be interpreted with caution due to its limitations, such as conducting this study in a laboratory setting, which lacks the conditions seen in oral environment, one brand of acrylic resin was used, specimens configuration was standardized and did not reflect the actual geometry of a denture, and lack of chewing forces. Therefore, further investigations with different concentrations of nano-SiO 2 , different brands of acrylic resins and testing under conditions mimicking the oral environment with aging procedures are recommended.
Conclusion
Within the limitations of the current study, it could be concluded that:
The addition of low concentration of nano-SiO 2 to repair material increased the FS.
Beveled repair surface design increased the FS of repaired denture base.
Funding Statement
Funding None.
Footnotes
Conflict of Interest None declared.
References
- 1.Gad M M, Fouda S M, Al-Harbi F A, Näpänkangas R, Raustia A. PMMA denture base material enhancement: a review of fiber, filler, and nanofiller addition. Int J Nanomedicine. 2017;12:3801–3812. doi: 10.2147/IJN.S130722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ozkir S E, Yilmaz B, Unal S M, Culhaoglu A, Kurkcuoglu I. Effect of heat polymerization conditions and microwave on the flexural strength of polymethyl methacrylate. Eur J Dent. 2018;12(01):116–119. doi: 10.4103/ejd.ejd_199_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gad M M, Rahoma A, Al-Thobity A M, ArRejaie A S. Influence of incorporation of ZrO2nanoparticles on the repair strength of polymethyl methacrylate denture bases. Int J Nanomedicine. 2016;11:5633–5643. doi: 10.2147/IJN.S120054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faot F, da Silva W J, da Rosa R S, Del Bel Cury A A, Garcia R C. Strength of denture base resins repaired with auto- and visible light-polymerized materials. J Prosthodont. 2009;18(06):496–502. doi: 10.1111/j.1532-849X.2009.00470.x. [DOI] [PubMed] [Google Scholar]
- 5.Rashid H, Sheikh Z, Vohra F. Allergic effects of the residual monomer used in denture base acrylic resins. Eur J Dent. 2015;9(04):614–619. doi: 10.4103/1305-7456.172621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agarwal M, Nayak A, Hallikerimath R B. A study to evaluate the transverse strength of repaired acrylic denture resins with conventional heat-cured, auto-polymerizing and microwave-cured resins: an in vitro study. J Indian Prosthodont Soc. 2008;8:36–41. [Google Scholar]
- 7.Alkurt M, Yeşil Duymuş Z, Gundogdu M. Effect of repair resin type and surface treatment on the repair strength of heat-polymerized denture base resin. J Prosthet Dent. 2014;111(01):71–78. doi: 10.1016/j.prosdent.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Ward J E, Moon P C, Levine R A, Behrendt C L. Effect of repair surface design, repair material, and processing method on the transverse strength of repaired acrylic denture resin. J Prosthet Dent. 1992;67(06):815–820. doi: 10.1016/0022-3913(92)90591-w. [DOI] [PubMed] [Google Scholar]
- 9.Hanna E A, Shah F K, Gebreel A A. Effect of joint surface contours on the transverse and impact strength of denture base resin repaired by various methods: an in vitro study. J Am Sci. 2010;6:115–125. [Google Scholar]
- 10.Beyli M S, von Fraunhofer J A. Repair of fractured acrylic resin. J Prosthet Dent. 1980;44(05):497–503. doi: 10.1016/0022-3913(80)90067-0. [DOI] [PubMed] [Google Scholar]
- 11.Seó R S, Neppelenbroek K H, Filho J N. Factors affecting the strength of denture repairs. J Prosthodont. 2007;16(04):302–310. doi: 10.1111/j.1532-849X.2007.00191.x. [DOI] [PubMed] [Google Scholar]
- 12.Gad M, ArRejaie A S, Abdel-Halim M S, Rahoma A. The reinforcement effect of nano-zirconia on the transverse strength of repaired acrylic denture base. Int J Dent. 2016;2016:7.094056E6. doi: 10.1155/2016/7094056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu Y H, Chen C Y, Wang C C. Viscoelastic properties and thermal degradation kinetics of silica/PMMA nanocomposites. Polym Degrad Stabil. 2004;84:545–553. [Google Scholar]
- 14.Mahross H Z, Baroudi K. Effect of silver nanoparticles incorporation on viscoelastic properties of acrylic resin denture base material. Eur J Dent. 2015;9(02):207–212. doi: 10.4103/1305-7456.156821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lazzara G, Milioto S. Dispersions of nanosilica in biocompatible copolymers. Polym Degrad Stabil. 2010;95:610–617. [Google Scholar]
- 16.Karci M, Demir N, Yazman S. Evaluation of flexural strength of different denture base materials reinforced with different nanoparticles. J Prosthodont. 2019;28(05):572–579. doi: 10.1111/jopr.12974. [DOI] [PubMed] [Google Scholar]
- 17.Zhu A, Cai A, Zhou W, Shi Z. Effect of flexibility of grafted polymer on the morphology and property of nanosilica/PVC composites. Appl Surf Sci. 2008;254:3745–3752. [Google Scholar]
- 18.Balos S, Pilic B, Markovic D, Pavlicevic J, Luzanin O. Poly(methyl-methacrylate) nanocomposites with low silica addition. J Prosthet Dent. 2014;111(04):327–334. doi: 10.1016/j.prosdent.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 19.Jordan J, Jacop K L, Tannenbaum R, Ashraf M A, Jasiuk I. Experimental trends in polymer nanocomposites- a review. Mater Sci Eng. 2005;393:1–11. [Google Scholar]
- 20.Revised American Dental Association Specification No . Revised American Dental Association specification no. 12 for denture base polymers. J Am Dent Assoc. 1975;90(02):451–458. doi: 10.14219/jada.archive.1975.0069. [DOI] [PubMed] [Google Scholar]
- 21.da Silva L H, Feitosa S A, Valera M C, de Araujo M A, Tango R N. Effect of the addition of silanated silica on the mechanical properties of microwave heat-cured acrylic resin. Gerodontology. 2012;29(02):e1019–e1023. doi: 10.1111/j.1741-2358.2011.00604.x. [DOI] [PubMed] [Google Scholar]
- 22.Gad M M, Rahoma A, Abualsaud R, Al-Thobity A M, Fouda S M. Effect of repair gap width on the strength of denture repair: an in vitro comparative study. J Prosthodont. 2019;28(06):684–691. doi: 10.1111/jopr.13091. [DOI] [PubMed] [Google Scholar]
- 23.Qaw M S, Abushowmi T H, Almaskin D F et al. A novel approach to improve repair bond strength of repaired acrylic resin: an in vitro study on the shear bond strength. J Prosthodont. 2018 doi: 10.1111/jopr.12970. [DOI] [PubMed] [Google Scholar]
- 24.Sarac Y S, Sarac D, Kulunk T, Kulunk S. The effect of chemical surface treatments of different denture base resins on the shear bond strength of denture repair. J Prosthet Dent. 2005;94(03):259–266. doi: 10.1016/j.prosdent.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 25.Cevik P, Yildirim-Bicer A Z. The effect of silica and prepolymer nanoparticles on the mechanical properties of denture base acrylic resin. J Prosthodont. 2018;27(08):763–770. doi: 10.1111/jopr.12573. [DOI] [PubMed] [Google Scholar]
- 26.Vasthare A, Shetty S, Kamalakanth Shenoy K K, Shetty M S, Parveen K A, Shetty R. Effect of different edge profile, surface treatment, and glass fiber reinforcement on the transverse strength of denture base resin repaired with autopolymerizing acrylic resin: an in vitro study . J Interdiscip Dent. 2017;7(01):31–37. [Google Scholar]
- 27.Tukmachi M S, Azeez Z A, Mohammed D H. Evaluation of bond strength of acrylic artificial teeth with unreinforced and nano silica reinforced denture base material after chemical disinfection. J Res Med Dent Sci. 2018;6:76–82. [Google Scholar]
- 28.Katsikis N, Franz Z, Anne H, Munstedt H, Vital A. Thermal stability of poly(methyl methacrylate)/silica nano- and microcomposite as investigated by dynamic-mechanical experiment. Polym Degrad Stabil. 2007;22:1966–1976. [Google Scholar]
- 29.Zuccari A G, Oshida Y, Moore B K. Reinforcement of acrylic resins for provisional fixed restorations. Part I: Mechanical properties. Biomed Mater Eng. 1997;7(05):327–343. [PubMed] [Google Scholar]
- 30.Mc Nally L, O’Sullivan D J, Jagger D C. An in vitro investigation of the effect of the addition of untreated and surface treated silica on the transverse and impact strength of poly(methyl methacrylate) acrylic resin. Biomed Mater Eng. 2006;16(02):93–100. [PubMed] [Google Scholar]
- 31.Sodagar A, Bahador A, Khalil S, Shahroudi A S, Kassaee M Z. The effect of TiO2 and SiO2 nanoparticles on flexural strength of poly (methyl methacrylate) acrylic resins. J Prosthodont Res. 2013;57(01):15–19. doi: 10.1016/j.jpor.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Mansour M M, Wagner W C, Chu T M. Effect of mica reinforcement on the flexural strength and microhardness of polymethyl methacrylate denture resin. J Prosthodont. 2013;22(03):179–183. doi: 10.1111/j.1532-849X.2012.00923.x. [DOI] [PubMed] [Google Scholar]


