Abstract
Background:
The Addictions Neuroclinical Assessment (ANA), a framework for measuring heterogeneity in alcohol use disorder (AUD), focuses on three domains that reflect neurobiological dysfunction in addiction and correspond to the cycles of addiction: executive function, incentive salience, and negative emotionality. Kwako and colleagues (2019) validated a 3-factor model of the ANA with neuropsychological and self-report indicators among treatment-seekers and non-treatment-seekers with and without AUD. The present analysis replicated and extended these findings in a treatment-seeking sample, focusing on the negative emotionality domain.
Methods:
Participants (n=563; 58.8% male; mean age=34.3) were part of a multisite prospective study of individuals entering AUD treatment. We examined the factor structure of the negative emotionality domain at the baseline, 6-month, and 12-month follow-up assessments. The Beck Depression Inventory, Beck Anxiety Inventory, State-Trait Anger Expression Inventory-Trait Anger Subscale, and three Drinker Inventory of Consequences items assessing negative affective consequences were indicators in the model.
Results:
Results indicated that a 1-factor model was an excellent fit at all assessments, and that the domain was time and gender invariant. Furthermore, negative emotionality was associated with drinking patterns and reasons for alcohol use (i.e., drinking because of negative emotions and urges/withdrawal) at all assessments.
Conclusions:
This analysis provides evidence for the construct validity and measurement invariance of the ANA negative emotionality domain among AUD treatment-seekers. Future studies are needed to evaluate prospective associations between negative emotionality and specific treatment modalities, and whether individuals with greater negative emotionality are more likely to respond to treatment that targets drinking to relieve negative affective states.
Keywords: alcohol use disorder treatment, negative emotions, alcohol relapse, addiction cycle, addictions neuroclinical assessment
Introduction
Approximately 14.5 million United States (U.S.) citizens ages 12 and older meet criteria for a current alcohol use disorder (AUD) (Center for Behavioral Health Statistics and Quality, 2018). There are several effective interventions for AUD, including both behavioral and pharmacological treatments (Witkiewitz et al., 2019a). However, attrition and relapse are common in AUD treatment, with 10 to 35% of participants dropping out of AUD clinical trials (Hallgren and Witkiewitz, 2013) and over 60% experiencing a drinking lapse in the first year following treatment (Maisto and Connors, 2006; Witkiewitz and Masyn, 2008). These findings underscore the need to improve outcomes in AUD treatment.
Precision medicine—identifying treatment approaches that will be most effective based on patient characteristics—represents a method for improving outcomes in currently established, empirically-supported treatments (Kranzler and McKay, 2012). Indeed, previous studies have found evidence that patient characteristics moderate AUD treatment efficacy. Those with greater substance use and negative affect severity are more likely to benefit from mindfulness-based relapse prevention (Roos et al., 2017a). Furthermore, reasons for alcohol use (e.g., reward vs. relief motives, drinking to cope) differentially predict response to naltrexone and acamprosate (Mann et al., 2018; Roos et al., 2017b; Witkiewitz et al., 2019b) and cognitive-behavioral therapy (Anker et al., 2016).
Addictions Neuroclinical Assessment
To more thoroughly capture the heterogeneity within AUD, the Alcohol Addiction Research Domain Criteria (AARDoC) has been proposed by Litten and colleagues (2015) as an organizing framework for research on the behavioral, neurobiological, and genetic features of AUD. One of the ultimate goals of AARDoC is to more effectively advance precision medicine for AUD. However, further research on patient characteristics that moderate treatment outcome and implementation of findings from such studies requires a common battery of measures that capture the heterogeneity of AUD and is accessible for both researchers and clinicians.
Building from AARDoC, Kwako and colleagues (2016) recently proposed a framework for measuring heterogeneity in AUD patients, called the Addictions Neuroclinical Assessment (ANA). The ANA focuses on three functional domains that reflect neurobiological dysfunction common in addiction and correspond to the Koob and Volkow (2010) addiction cycle: executive function, incentive salience, and negative emotionality (Kwako et al., 2016). Establishing a common battery to measure these domains can help to understand mechanisms underlying AUD development and maintenance, and how different patient profiles predict response to treatment (Kwako et al., 2016). A recent study validated this model using factor analytic techniques. Specifically, a three-factor model, representing executive function, incentive salience, and negative emotionality, with neuropsychological and self-report indicators provided a good fit to the observed data among a treatment-seeking and non-treatment-seeking sample with and without AUD (Kwako et al., 2019).
Project Aims and Hypotheses
The purpose of the present study was to replicate and extend Kwako and colleagues’ findings (2019), with a specific focus on the latent construct of negative emotionality. This previous study found that negative emotionality (as well as executive function and incentive salient) is a unidimensional construct measured by self-report assessments, including measures of trait anxiety, aggression, and neuroticism. Negative emotionality has been shown to be particularly important in predicting alcohol treatment outcomes. Individuals with comorbid diagnoses of depression or anxiety tend to have higher AUD severity entering treatment and greater drinking and functional impairment following treatment (Burns et al., 2005). Furthermore, changes in negative affect have been shown to play a mediating role in alcohol treatment outcomes (Wilcox and Tonigan, 2018).
The negative emotionality construct of the ANA has only been evaluated in one sample that includes individuals seeking treatment for AUD. Compared to non-treatment-seekers, individuals who are treatment-seeking have greater AUD symptom severity, longer AUD duration, and greater alcohol consumption, all of which are variables that have been shown to impact treatment outcomes (Ray et al., 2017). Given that negative affect and drinking to regulate negative affect are important factors influencing treatment outcome, it is necessary to validate the ANA construct of negative emotionality among additional samples of individuals seeking treatment for AUD. Furthermore, one limitation of the ANA assessment battery proposed by Kwako and colleagues (2016) is the substantial time burden on participants, with the battery requiring an estimated 10 hours to complete (Ghitza, 2017). Accordingly, the aim of the present analysis was to utilize confirmatory factor analysis to further examine the dimensionality using fewer indicators of a negative emotionality latent construct that could be measured in less time. We utilized a set of indicators that corresponds to the negative emotionality construct proposed and tested by Kwako and colleagues (2016, 2019), but is less burdensome to clinicians and participants and is routinely administered in clinical practice (e.g., negative affective consequences of drinking, depression and anxiety symptoms). We also determined the construct validity of the negative emotionality construct in this sample by examining concurrent associations between negative emotionality and drinking patterns and patient reported reasons for drinking.
The second aim of the present study was to examine longitudinal and gender invariance of the negative emotionality construct. Establishing longitudinal invariance is necessary to determine mean changes in a construct over time. Regulating negative affect is a target of numerous behavioral treatments for AUD, such as cognitive-behavioral therapy (Carroll and Kiluk, 2017) and mindfulness-based relapse prevention (Witkiewitz et al., 2014), necessitating the ability to examine changes in negative emotionality during treatment. Likewise, gender invariance is needed to examine gender differences in a construct. As compared to men with substance use disorders, women tend to have more co-morbid psychiatric disorders, endorse more coping motives for drinking, and demonstrate stronger relationships between negative affect and substance use (Conway et al., 2006; McHugh et al., 2018, 2017). Establishing gender invariance of the negative emotionality domain is critical, given that women might demonstrate greater negative emotionality and stronger associations between negative emotionality and the development and maintenance of AUD.
Method
Data Source and Participants
The present study was a secondary analysis of data from a multisite naturalistic prospective observational study, the Relapse Replication and Extension Project (RREP) (Lowman et al., 1996), which aimed to replicate and extend a taxonomy of relapse developed by G. Alan Marlatt (Marlatt, 1996). Participants were recruited at the time of admission from 15 community AUD treatment programs, both inpatient and outpatient, in Albuquerque, NM (1 site), Providence, RI (6 sites), and Buffalo, NY (8 sites). Treatment was not randomly assigned and individuals were in a variety of treatments for an unspecified amount of time. Treatment received and amount of time in treatment were not recorded in the dataset.
A common battery of measures was administered at each site, but each site also had unique study aims and measures. Inclusion criteria were: aged 18 or older; met criteria for alcohol abuse or dependence according to the Diagnostic Interview Schedule for DSM III-R (DIS-R; Robins, Cottler, & Keating, 1989); could read at an 8th grade level; had completed alcohol detoxification; and were willing to complete study procedures. Exclusion criteria were: severe drug use disorders; intravenous drug use in the previous six months; and major psychiatric disorders or cognitive impairment. A baseline assessment was conducted at treatment admission and participants completed six follow-up assessments at bi-monthly intervals; the present analysis utilized data from the baseline, 6-month, and 12-month assessments. Detailed study methodology has been previously reported (Lowman et al., 1996).
Overall, 563 participants completed the baseline assessment. The majority of participants were male (58.8%) and Non-Hispanic White (67.3%), and had an average age of 34.3 (SD=8.7) years. A majority (80.6%) of participants were not married or cohabitating. Participants completed an average of 12.0 (SD=2.4) years of education and a majority of participants were currently “homemakers” (40.0%), unemployed (28.1%), or employed part-time (25.2%).
Measures
All measures were administered at baseline, 6-month, and 12-month follow-up assessments, with the exception of the Comprehensive Drinker Profile, which assessed demographics and was assessed only at baseline. All measures in the present analysis were administered at each study site, with the exception of the Drinker Inventory of Consequences, which was only completed at the Albuquerque site, and the Reasons for Drinking Questionnaire, which was completed at the Albuquerque and Buffalo sites.
Comprehensive Drinker Profile.
The Comprehensive Drinker Profile was utilized to assess demographics, including participants’ self-reported gender, age, racial/ethnic identity, education, and marital and employment status.
Beck Depression Inventory.
The Beck Depression Inventory (BDI) is a 21-item measure (rated from 0–3) of the current severity of depression symptoms. Items are summed to compute the total score, with a range of 0–63. The BDI has displayed internal consistency reliability, concurrent validity, and discriminant validity (Beck et al., 1988b). In the present study, the BDI demonstrated good to excellent internal consistency reliability at all assessments (Cronbach’s αs≥0.89).
Beck Anxiety Inventory.
The Beck Anxiety Inventory (BAI) is a 21-item measure (rated from 0–3) assessing severity of anxiety symptoms in the past week (total scores range from 0–63). The BAI has demonstrated internal consistency reliability, test-retest reliability, concurrent validity, and discriminant validity (Beck et al., 1988a). The BAI demonstrated excellent internal consistency reliability at all assessments (Cronbach’s αs≥0.93).
Spielberger State-Trait Anger Expression Inventory.
The State-Trait Anger Expression Inventory (STAXI) is a 44-item questionnaire designed to measure the expression of emotion in a situational context (state) and a predisposition toward anger (trait) (Spielberger and Sydeman, 1994). The trait anger subscale was utilized in the present analysis. This 10-item subscale includes questions such as “I am a hot headed person” with response options ranging from never (rated as a 1) to always (rated as a 4), with a potential range of scores from 10 to 40. In the present study, the trait anger subscale demonstrated good internal consistency reliability at all assessments (Cronbach’s αs=0.87–0.88).
Drinker Inventory of Consequences.
The Drinker Inventory of Consequences (DrInC) is a 50-item questionnaire of consequences in five domains: physical, intrapersonal, interpersonal, social responsibility, and impulse control. At the baseline assessment, the DrInC assessed consequences over the previous three months and at the follow-up assessments, consequences were assessed over the previous six months. We utilized three items from the intrapersonal subscale assessing negative affective consequences: “I have been unhappy because of my drinking” (DrInC Item 12), “I have felt guilty or ashamed because of my drinking” (DrInC Item 16) and “I have lost interest in activities or hobbies because of my drinking” (DrInC Item 34). The baseline and follow-up DrInC questionnaires had slightly different response options. At the baseline assessments, all response options ranged from never (rated as a 1) to daily or almost daily (rated as a 4). At the follow-up assessments, response options for items 12 and 16 ranged from never (rated a 1) to almost every day (rated a 6), and response options for item 34 ranged from not at all (rated a 1) to very much (rated a 4).
Reasons for Drinking Questionnaire.
The Reasons for Drinking Questionnaire (RFDQ) is a 16-item measure that was developed to meet the aims of the RREP study (Zywiak et al., 1996). The RFDQ asks participants to rate the reasons why they started drinking again at their most recent relapse. Accordingly, participants only completed this questionnaire if they drank since the prior assessment. The measure includes items such as “I felt sad” and “I saw others drinking,” which were rated on a Likert-type scale (0=not at all important, 10=very important). This questionnaire includes three subscales, including the following: a 7-item negative emotions subscale (subscale scores range from 0–70; Cronbach’s αs=0.84–0.90), a 3-item social pressure subscale (scores range from 0–30; Cronbach’s αs=0.84–0.85), and a 5-item urges/withdrawal subscale (scores range from 0–50; Cronbach’s αs=0.53–0.68).
Form 90 Timeline Followback.
The Form 90 (Sobell and Sobell, 1992) utilizes the Timeline Followback (TLFB) method (i.e., calendar and event-based cues) to retrospectively recall daily drinking patterns. At baseline, the TLFB captured daily drinking in the 90 days prior to the assessment. The TLFB was then administered in bimonthly intervals, thus assessing daily drinking over approximately 60 prior days at each assessment. The Form 90 TLFB was utilized to calculate several drinking indicators: percent days abstinent, percent heavy drinking days (defined as 4/5+ drinks for women/men; National Institute on Alcohol Abuse and Alcoholism (NIAAA), n.d.), average drinks per day, and average drinks per drinking day. Previous studies of the TLFB have reported good reliability and validity (Maisto et al., 2008).
Statistical Analyses
Confirmatory Factor Analyses.
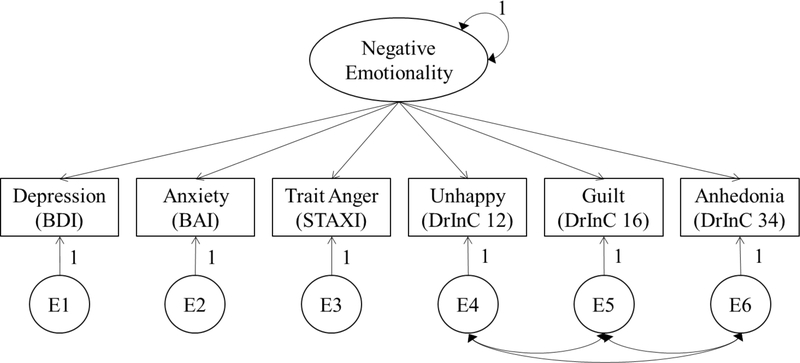
To examine the factor structure of negative emotionality indicators, we conducted confirmatory factor analyses (CFA) at each timepoint using a diagonally weighted least squares (WLSMV) estimator in Mplus 8.2 (Muthén and Muthén, 2017). We utilized WLSMV estimation, given that three of our indicators (DrInC Items 12, 16, and 34) were categorical. Although other indicators included in the present analysis were continuous, simulation studies indicate that the WLSMV estimator produces less biased results than maximum likelihood estimation when using ordinal indicators (Li, 2016). WLSMV estimation utilizes pairwise deletion of missing data, which allows participants to contribute information to the models if they had data on at least one indicator variable. Indicators included the following variables: BDI total score, BAI total score, STAXI trait anger subscale, DrInC Item 12, DrInC Item 16, and DrInC Item 34. A single latent factor, shown in Figure 1, with these 6 indicators was tested with the variance set to 1 for model identification and correlated residuals for the three DrInC items given conceptual and methodological overlap. To evaluate model fit, we used model fit criteria suggested by Hu and Bentler (1999) including a non-significant χ2 test, the Comparative Fit Index (CFI) >.90 (acceptable) > .95 (optimal), Tucker-Lewis Index (TLI) >.90 (acceptable) > .95 (optimal), Root Mean Square Error of Approximation (RMSEA) < .06 and Standardized Root Mean Square Residual (SRMR) < .08.
Figure 1.
Confirmatory Factor Analysis Model of Negative Emotionality Domain. BDI = Beck Depression Inventory, BAI = Beck Anxiety Inventory, STAXI = State‐Trait Anger Expression Inventory, DrInC = Drinker Inventory of Consequences.
Measurement Invariance.
To examine invariance over time, we conducted confirmatory factor analyses with parameter constraints using the WLSMV estimator to examine configural, metric, scalar, and strict invariance. At baseline, three of our negative emotionality indicators were assessed on a different response scale (4-point vs. 6-point response scale) and for a different time window (past 3-months vs. past 6-months) compared to the follow-up assessments. Thus, we examined time invariance across the 6-month and 12-month follow-ups only. To examine configural invariance, the negative emotionality indicators were allowed to load on a single-factor at each time point with all parameters estimated freely over time. To examine metric invariance, we constrained the factor loadings to equality over time. To examine scalar invariance, we constrained the factor loadings and indicator thresholds to equality over time. To examine strict invariance, we constrained the factor loadings, indicator thresholds, and residuals for continuous indicators to equality over time. With strict invariance, we can interpret changes in the negative emotionality factor over time and changes in the observed indicators over time as reflective of true change, and not a byproduct of measurement error. To examine gender invariance (men vs. women), we conducted multi-group confirmatory factor analyses at each timepoint using the WLSMV estimator to examine configural, metric, and scalar, and strict invariance using the same parameter constraint procedure as described above. Residuals for categorical items were constrained to 1 for identification across all models (Widaman et al., 2010). For all invariance testing, given that the model χ2 test statistic is sensitive to sample size (Brown, 2015), we used model comparison criteria of a negative change in CFI ≥.01 (Cheung and Rensvold, 2002) and a positive change in RMSEA ≥.015 (Chen, 2007) to indicate significant decrement in fit when testing for measurement invariance.
Construct Validity.
To examine the construct validity of the negative emotionality factor, we examined how this factor was related to concurrent drinking patterns (i.e., percent days abstinent, drinks per drinking days, drinks per day, and percent heavy drinking days) and reasons for drinking following a period of abstinence (negative emotions, pressure from others, urges/withdrawal). Drinking patterns were measured over the previous 90 days at the baseline assessment, while drinking patterns represent 60 days prior to the assessment at follow-up assessments. Confidence intervals for the correlations between negative emotionality and drinking patterns and reasons for drinking were obtained using bootstrapped resampling (nboot=500).
Multiple Imputation Analyses.
We had substantial amounts of missing data for some measures (see Table 1) due to aspects of the study methods (e.g., some measures only presented in the case of a relapse, not all measures assessed at all sites). We conducted sensitivity analyses to assess the impact of missing data by re-estimating the models using multiple imputation procedures to account for missing data. Parameter estimates were pooled across 50 imputed data sets. Imputation models comprised all indicators included in CFAs and variables included in construct validity analyses. We then re-estimated all CFAs and assessed gender invariance at baseline, longitudinal invariance across the 6- to 12-month assessment, and construct validity.
Table 1.
Descriptive Statistics of All Measures Included in the Analysis at Baseline, 6-, and 12-Month Follow-Ups
| Baseline | 6-Month Follow-up | 12-Month Follow-Up | ||||
|---|---|---|---|---|---|---|
| Measure | n | M (SD) or % | n | M (SD) or % | n | M (SD) or % |
| Depression (BDI) | 551 | 14.8 (9.9) | 455 | 11.1 (10.0) | 477 | 11.3 (10.9) |
| Anxiety (BAI) | 554 | 14. 9 (11.5) | 454 | 11.3 (11.6) | 487 | 11.2 (11.5) |
| Trait Anger (STAXI) | 538 | 22.3 (6.3) | 458 | 20.1 (6.2) | 487 | 19.7 (6.1) |
| DrInC Item 12: “I have been unhappy because of my drinking.” | 236 | Never=5.5% Once to twice a month=30.5% Twice a week=21.6% Daily/almost daily=42.4% |
169 | Never=26.0% Once or twice=26.0% Once or twice a month=10.1% Once a week=7.1% Twice a week=8.9% Almost everyday=21.9% |
160 | Never=23.8% Once or twice=27.5% Once or twice a month=10.0% Once a week=5.0% Twice a week=11.3% Almost everyday=22.5% |
| DrInC Item 16: “I have felt guilty or ashamed because of my drinking.” | 230 | Never=6.0% Once to twice a month=29.5% Twice a week=21.4% Daily/almost daily=43.2% |
169 | Never=25.4% Once or twice=22.5% Once or twice a month=14.2% Once a week=8.3% Twice a week=9.5% Almost everyday=20.1% |
160 | Never=24.4% Once or twice=24.4% Once or twice a month=11.3% Once a week=5.0% Twice a week=11.3% Almost everyday=23.8% |
| DrInC Item 34: “I have lost interest in activities or hobbies because of my drinking.” | 216 | Never=12.0% Once to twice a month=26.9% Twice a week=28.7% Daily/almost daily=32.4% |
167 | Not at all=40.1% A little=25.1% Somewhat=15.6% Very much=19.2% |
163 | Not at all=36.8% A little=27.6% Somewhat=13.5% Very much=22.1% |
| Percent Days Abstinent | 562 | 47.0 (30.0) | 526 | 82.8 (27.6) | 494 | 82.9 (29.1) |
| Drinks per Drinking Day | 562 | 20.2 (13.0) | 526 | 7.2 (10.0) | 494 | 6.2 (9.5) |
| Drinks per Day | 562 | 11.4 (10.9) | 526 | 2.6 (6.1) | 494 | 2.3 (5.2) |
| Percent Heavy Drinking Days | 562 | 48.5 (30.0) | 526 | 14.0 (25.2) | 494 | 13.8 (26.0) |
| RFD Negative Emotions | 247 | 30.1 (19.3) | 110 | 22.8 (19.3) | 105 | 23.6 (20.4) |
| RFD Social Pressure | 245 | 9.8 (10.3) | 110 | 8.8 (10.1) | 105 | 10.6 (9.8) |
| RFD Urges/Withdrawal | 246 | 17.7 (10.7) | 110 | 15.9 (11.4) | 105 | 16.1 (10.1) |
Note. n=number of participants with complete data on each measure. BDI = Beck Depression Inventory, BAI = Beck Anxiety Inventory, STAXI = State-Trait Anger Expression Inventory, DrInC = Drinker Inventory of Consequences, RFD = Reasons for Drinking.
Results
Descriptive Statistics
Descriptive statistics for the measures utilized in the present analysis are presented in Table 1. On average, participants reported a minimal level of depression (Beck et al., 1988b) and anxiety (Julian, 2011) across assessments. Specifically, at baseline, 34% of participants reported BDI scores that were in the range of “no to minimal depression,” 32% reported scores in the range of “mild to moderate” depression, 24% reported scores in the range of “moderate to severe” depression, and 9% had scores in the range of “severe” depression (not reported in Table 1; Beck et al., 1988b). Similarly, 40% of participants’ BAI scores were in the range of “no to minimal” anxiety, with 30% reporting “mild to moderate” anxiety, 18% reporting “moderate to severe” anxiety, and 13% reporting “severe” anxiety (not reported in Table 1; Julian, 2011). Across assessments, average trait anger scores ranged from 19.7 to 22.3 out of 40 total points. Participants’ negative affective consequences decreased during and after treatment. Specifically, one third to one-half of participants endorsed the highest response option ( “daily or almost daily”) for each negative affective consequences of drinking at the baseline appointment. At the 6- and 12-month follow-up assessments, less than a quarter of participants endorsed the highest response option for each negative affective consequence. Expectedly, participants reported more frequent and heavier drinking at the baseline assessment, as compared to the 6- and 12-month follow-up assessments. At baseline, participants reported 47.0 (SD=30.0) percent days abstinent, 48.5 (SD=30.0) percent heavy drinking days, and they drank an average of 11.4 (SD=10.9) drinks per day and 20.2 (SD=13.0) drinks per drinking day. Percent days abstinent increased across the follow-up period and percent heavy drinking days, drinks per day, and drinks per drinking day decreased.
Confirmatory Factor Analyses (CFA)
A single-factor CFA model (Figure 1) of our six negative emotionality indicators demonstrated excellent fit at baseline, 6-month follow-up, and 12-month follow-up (see Table 2). The BDI and BAI indicators had the highest factor loadings at all time points.
Table 2.
Summary of Confirmatory Factor Analyses of the Negative Emotionality Construct at Baseline, 6-month, and 12-month Follow-Ups
| Baseline (n=562) | 6-month (n=484) | 12-month (n=494) | |
|---|---|---|---|
| Negative Emotionality Indicators | Factor Loadings | ||
| Depression (BDI) | .801 | .797 | .781 |
| Anxiety (BAI) | .669 | .765 | .780 |
| Trait Anger (STAXI) | .418 | .426 | .370 |
| Negative Affective Consequence (DrInC item 12) | .545 | .373 | .488 |
| Negative Affective Consequence (DrInC item 16) | .367 | .439 | .450 |
| Negative Affective Consequence (DrInC item 34) | .374 | .354 | .472 |
| Residual Correlations | |||
| DrInC item 12 with DrInC item 16 | .888 | .859 | .877 |
| DrInC item 12 with DrInC item 34 | .514 | .523 | .668 |
| DrInC item 16 with DrInC item 34 | .436 | .537 | .662 |
| Model Fit Statistics | |||
| Model χ2 (df) | 2.525 (6) | 9.765 (6) | 6.393 (6) |
| p-value | .8657 | .1349 | .3807 |
| Confirmatory Fit Index (CFI) | 1.000 | .988 | 1.000 |
| Tucker-Lewis Index (TLI) | 1.005 | .995 | 1.000 |
| Root Mean Squared Error of Approximation (RMSEA) | .000 | .036 | .012 |
| Standardized Root Mean Square Residual (SRMR) | .012 | .026 | .021 |
Note. All factor loadings and residual correlations were statistically significant (p < .05).
Measurement Invariance Over Time
Results from the invariance testing over time from the 6- to the 12-month follow-up and across gender are shown in Table 3. Strict invariance was demonstrated for the negative emotionality factor from the 6- to 12-month follow-ups as indicated by improvements in CFI and RMSEA (rather than decrements). We found that the negative emotionality construct at 6-months was strongly correlated with the negative emotionality construct at 12-months, r = .738, and we did not observe a significant change in the negative emotionality construct over time (Δ in latent mean = .043, p = .681)
Table 3.
Invariance Testing of the Negative Emotionality Construct over Time and Across Gender at Each Time Point (Men vs. Women)
| Measurement Invariance Over Time (from 6-month to 12-month Follow-Up; n=523) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall Fit Indices | Comparative Fit Indices | |||||||||
| χ2 | df | p | CFI | RMSEA | Model Comparison | Δχ2 | Δdf | ΔCFI | ΔRMSEA | |
| 1. Configural | 89.86 | 41 | <.001 | .986 | 0.048 [0.034, 0.061] | |||||
| 2. Metric | 87.85 | 46 | <.001 | .988 | 0.042 [0.028, 0.055] | 1 vs. 2 | 2.01 | 5 | +.002 | −.006 |
| 3. Scalar | 99.22 | 61 | <.001 | .989 | 0.035 [0.022, 0.047] | 2 vs. 3 | 11.37 | 15 | +.001 | −.007 |
| 4. Strict | 102.37 | 64 | .002 | .989 | 0.034 [0.021, 0.046] | 3 vs. 4 | 3.15 | 3 | .000 | −.001 |
| Measurement Invariance Across Gender (Baseline; n=562) | ||||||||||
| Overall Fit Indices | Comparative Fit Indices | |||||||||
| χ2 | df | p | CFI | RMSEA | Model Comparison | Δχ2 | Δdf | ΔCFI | ΔRMSEA | |
| 1. Configural | 29.85 | 18 | .039 | .993 | 0.048 [0.011, 0.078] | |||||
| 2. Metric | 49.66 | 24 | .002 | .984 | 0.062 [0.037, 0.086] | 1 vs. 2 | 19.81 | 6 | −.009 | +.014 |
| 3. Scalar | 64.20 | 30 | <.001 | .979 | 0.064 [0.042, 0.085] | 2 vs. 3 | 14.54 | 6 | −.005 | +.002 |
| 4. Strict | 66.12 | 33 | <0.01 | .980 | 0.060 [0.038, 0.081] | 3 vs. 4 | 1.92 | 3 | +.001 | −0.004 |
| Measurement Invariance Across Gender (6-month; n=484) | ||||||||||
| Overall Fit Indices | Comparative Fit Indices | |||||||||
| χ2 | df | p | CFI | RMSEA | Model Comparison | Δχ2 | Δdf | ΔCFI | ΔRMSEA | |
| 1. Configural | 30.36 | 22 | .109 | .997 | 0.040 [0.000, 0.071] | |||||
| 2. Metric | 36.41 | 28 | .133 | .997 | 0.035 [0.000, 0.064] | 1 vs. 2 | 6.05 | 6 | .000 | −.005 |
| 3. Scalar | 43.97 | 34 | .118 | .996 | 0.035 [0.000, 0.062] | 2 vs. 3 | 7.56 | 6 | −.001 | .000 |
| 4. Strict | 45.98 | 37 | .148 | .997 | 0.032 [0.000, 0.058] | 3 vs. 4 | 2.01 | 3 | +.001 | −.003 |
| Measurement Invariance Across Gender (12-month; n=494) | ||||||||||
| Overall Fit Indices | Comparative Fit Indices | |||||||||
| χ2 | df | p | CFI | RMSEA | Model Comparison | Δχ2 | Δdf | ΔCFI | ΔRMSEA | |
| 1. Configural | 17.02 | 22 | .762 | 1.00 | 0.000 [0.000, 0.038] | |||||
| 2. Metric | 25.29 | 28 | .612 | 1.00 | 0.000 [0.000, 0.043] | 1 vs. 2 | 8.27 | 6 | .000 | .000 |
| 3. Scalar | 32.06 | 34 | .563 | 1.00 | 0.000 [0.000, 0.043] | 2 vs. 3 | 6.77 | 6 | .000 | .000 |
| 4. Strict | 33.47 | 37 | .403 | .999 | 0.013 [0.000, 0.047] | 3 vs. 4 | 1.41 | 3 | −.001 | +.013 |
Measurement Invariance Across Gender
Strict invariance across gender was demonstrated for the negative emotionality construct at baseline, 6-month, and 12-month follow-up. At baseline, there was a slight decrement in fit from the configural to metric invariance model based on the CFI (−.009) and RMSEA (+.014), but the change in CFI and RMSEA did not exceed the a priori thresholds. At 6-month follow-up, there was an improvement in fit from the configural to metric invariance model based on the RMSEA (−.005), and no decrements in fit exceeding the a priori thresholds across models. At 12-month follow-up, there was a slight decrement in fit from the scalar to strict invariance model based on RMSEA (+.013) but this did not exceed the a priori threshold.
As demonstrated by the correlations between gender (0 = women, 1 = men) and the negative emotionality construct at each time point, men reported lower scores on the negative emotionality domain, which was statistically significant at baseline (r = −.244, p < .001) and 6-months (r = −.199, p = .005), but not at 12-months (r = −.127, p = .079). See Table 4.
Table 4.
Concurrent Associations between the Negative Emotionality Construct and Alcohol Use, Reasons for Drinking, and Gender
| Baseline r (95% CI) | 6-month r (95% CI) | 12-month r (95% CI) | |
|---|---|---|---|
| Percent Days Abstinent | −.066 (−.192, .091) | −.321 (−.446, −.178) | −.331 (−.456, −.223) |
| Drinks per Drinking Day | .297 (.176, .410) | .367 (.211, .489) | .393 (.263, .513) |
| Drinks per Day | .239 (.100, .394) | .466 (.255, .617) | .329 (.234, .452) |
| Percent Heavy Drinking Days | .133 (−.029, .262) | .349 (.195, .474) | .364 (.261, .487) |
| RFD Drinking due to Negative Emotions | .482 (.384, .605) | .538 (.311, .708) | .635 (.425, .825) |
| RFD Drinking due to Social Pressure | −.188 (−.327, −.036) | −.074 (−.289, .161) | −.129 (−.342, .080) |
| RFD Drinking due to Urges/Withdrawal | .336 (.193, .466) | .378 (.169, .546) | .346 (.140, .524) |
| Gender (0 = women, 1 = men) | −.244 (−.381, −.114) | −.199 (−.344, −.048) | −.127 (−.273, .006) |
Note. RFD = Reasons for Drinking scale; 95% CI = bootstrapped 95% confidence interval; confidence intervals that do not include zero represent statistically significant associations between the negative emotionality construct and alcohol use, reasons for drinking, and gender.
Construct Validity
Correlations between negative emotionality and drinking patters and reasons for drinking (with bootstrapped confidence intervals) are shown in Table 4. The negative emotionality construct was moderately related to drinking outcomes at 6-month and 12-month follow-ups, and non-significantly or weakly associated with drinking outcomes at baseline. The negative emotionality domain was strongly positively related to drinking due to negative emotions at each time point (.48 < r < .64), moderately positively relatedly to drinking due to urges/withdrawal at each time point (.34 < r < .38), and weakly (or non-significantly) negatively related to drinking due to social pressure at each time point (−.07 < r < −.19).
Multiple Imputation Analyses
In the primary analyses, described above, we utilized pairwise deletion to account for missing data and at least 484 participants contributed information to all analyses. Attrition analyses indicated that missing data on any indicator variable at baseline was associated with greater drinks per drinking day and drinks per day at baseline, poorer outcomes on all drinking measures at the 6-month follow-up, and lower scores on the RFD Negative Emotions scale at baseline (ps<0.05). Similarly, missing data on any indicator variable at the 6-month follow-up was significantly associated with several variables included in analyses (i.e., greater baseline drinks per drinking day and drinks per day, lower 6-month BDI scores, lower 12-month percent heavy drinking days), as was missing data on any indicator variable at the 12-month follow-up (i.e., greater baseline drinks per drinking day and drinks per day; greater percent days abstinent, lower percent heavy drinking days, and lower RFD social pressure scores at 12-months). Therefore, data were assumed to be missing at random, given that they were associated with other measured variables included in the models. Given the degree of missing data we re-estimated all models using multiple imputation, which is a more robust method for handling missing data under the assumption that data were missing at random. The multiple imputation models did not yield substantive differences with the original analyses using pairwise deletion for missing data. A summary of confirmatory factor analyses of the negative emotionality construct using multiple imputation for missing data is presented in Supplementary Table 1, while a summary of construct validity analyses using multiple imputation is presented in Supplementary Table 2.
Discussion
The present analysis examined the factor structure, construct validity, and measurement invariance of the negative emotionality domain, as proposed by the ANA, among individuals seeking treatment for AUD. A single-factor CFA model provided an excellent fit to the observed data before (at baseline) and during/following treatment (at 6- and 12-month follow-ups). This construct was invariant across time (from 6- to 12-month follow-up assessments) and gender. Furthermore, the negative emotionality domain demonstrated concurrent associations with more frequent and heavier drinking and drinking to regulate negative affect.
Our findings are largely consistent with a previous analysis among individuals with and without AUD (including treatment-seekers and non-treatment-seekers), which found that negative emotionality is a unidimensional domain indicated by self-report measures of trait anxiety, aggression, neuroticism, positive urgency, agreeableness, and extraversion (Kwako et al., 2019). Based on our analysis, current measures of depression and anxiety symptoms, affective consequences of alcohol use, and trait anger might also be useful and practical indicators of the negative emotionality domain. Indeed, both the BDI and BAI were part of the originally proposed battery of ANA measures (Kwako et al., 2016). It is important to note that our indicators were both state (e.g., BDI, BAI) and trait (e.g., STAXI trait anxiety scale) measures, while Kwako and colleagues (2019) primarily utilized trait indicators. This difference in study methods might have contributed to discrepancies between our study and the previous analysis investigating the factor structure and indicators of the negative emotionality domain. Specifically, Kwako and colleagues (2019) found that trait aggression had the highest factor loading, while trait anxiety and neuroticism demonstrated comparatively lower factor loadings. Conversely, anxiety and depression symptoms had the highest factor loadings in the present analysis, while trait anger and negative affective consequences of drinking had relatively lower factor loadings. Future research is needed to determine if trait vs. state measures (or a combination of both) are more useful indicators of the negative emotionality domain.
Beyond replicating the factor structure of the negative emotionality domain, we also found that this construct was invariant over the 6- to 12-month follow-up assessments. Demonstrating longitudinal invariance is necessary to examine mean changes in a construct over time. This finding has important implications for clinical research and practice, given that decreases in negative emotionality over time might signify better quality of life (Kirouac et al., 2017) and lower risk of relapse (Witkiewitz and Villarroel, 2009). Indeed, regulating negative affect is a target of numerous behavioral treatments for AUD, such as cognitive-behavioral therapy (Carroll and Kiluk, 2017) and affect regulation training (Stasiewicz et al., 2013). Future research should assess if certain treatments are better suited to decrease negative emotionality, and if individuals with AUD and high negative emotionality benefit more from particular treatment modalities.
We did not identify a decrease (or increase) in mean levels of negative emotionality from the 6- to 12-month assessment. Participants in the present study were receiving both inpatient and outpatient treatment across 15 community programs (Lowman et al., 1996), and it is therefore possible that not all participants were receiving treatment that targeted negative affect. We were also unable to examine measurement invariance and changes in negative emotionality from the baseline to follow-up assessments due to methodological differences between those time points. It will be important for future studies to determine if the negative emotionality domain is invariant across baseline to follow-up assessments among individuals seeking treatment for AUD.
We also found that the negative emotionality construct was invariant across gender at all assessments, thus allowing future research on gender differences in negative emotionality among those with AUD. Females had higher mean scores on the negative emotionality construct than men. This is consistent with previous findings that women with substance use disorders report greater negative affect than men, and that negative affect might have a larger contribution to women’s drinking than to men’s drinking (Conway et al., 2006; McHugh et al., 2018, 2017). Future efforts should examine multiple group measurement invariance of the negative emotionality domain across those with and without AUD and those with AUD who are treatment-seeking and non-treatment seeking. This will be an important area of research, given that the ANA constructs are theorized to contribute to both the development and maintenance of alcohol use and AUD (Kwako et al., 2016).
Negative emotionality was associated with heavier drinking at baseline and more frequent and heavier drinking at the 6- and 12-month assessments. These findings extend previous work by Kwako and colleagues (2019) by showing that greater negative emotionality was also strongly associated with relapse to regulate negative affect, moderately associated with relapse in response to urges and withdrawal, and was not associated with relapse due to social pressure. Taken together, these findings provide support for the construct validity of the negative emotionality domain among individuals seeking treatment for AUD. Future studies are needed to determine the predictive validity of the negative emotionality domain, including prospective associations between negative emotionality and AUD relapse. In addition, we found that negative emotionality was strongly related to drinking to regulate negative affect and a large body of literature has demonstrated that coping motives are associated with more drinking-related problems (Cooper et al., 2015). In future analyses, it will be important to determine if negative emotionality incrementally predicts drinking outcomes after controlling for coping motives.
Several methodological features of the present analysis limit our findings. First, the present study comprised secondary data analysis of a larger study which was conducted in the mid-1990s (Lowman et al., 1996). Replication of these results among a contemporary sample is needed to ensure generalizability of study findings. In addition, all indicators included in the present analysis were retrospective, self-report measures, which might be affected by recall bias. Furthermore, negative affective consequence items were assessed differently at baseline as compared to the follow-up assessments (e.g., different measurement windows and response options). We were therefore unable to assess invariance from baseline to follow-up assessments given that noninvariance could be due to differences in scaling and/or time window. It is possible that measurement invariance demonstrated in the present analysis, across both time and gender, is attributable to factors beyond equality in construct measurement. For example, the exclusion of major psychiatric disorders might have contributed to less variability and greater stability in item indicators that resulted in measurement equivalence in negative emotionality across gender and time. In addition, the indicators included in the present analysis might not be adequately sensitive to the construct of negative emotionality. Indicators included in the present analysis were limited to the measures assessed in the larger study. Therefore, we were not able to evaluate other potential indicators of the negative emotionality latent construct that might increase measurement sensitivity, including self-report measures (e.g., personality traits, measures of alexithymia; Kwako et al., 2016, 2019), behavioral measures (e.g., behavioral distress intolerance, Trier social stress task; Kwako et al., 2016; Lejuez et al., 2003), and biomarkers (e.g., heart rate variability, neuroimaging). Future studies should also replicate findings in samples with substance use and co-occurring psychiatric disorders.
In conclusion, we provided support for the unidimensional factor structure, construct validity, and measurement invariance of the ANA negative emotionality domain among individuals seeking treatment for AUD. These findings can inform future research on the ANA negative emotionality domain, as well as clinical applications of this domain. We also demonstrated the ability to examine changes in negative emotionality across time and gender, which will be useful in both research and clinical practice. Future studies are needed to solidify the utility of the negative emotionality domain in precision medicine efforts. In addition, continued evaluation of the negative emotionality domain using a range of indicators (e.g., self-report, behavioral, biomarkers) is needed to ultimately develop a common battery of measures with optimal validity.
Supplementary Material
Acknowledgments
This work was supported by the National Institute of Alcoholism and Alcohol Abuse of the National Institutes of Health, award numbers R01AA022328, T32AA018108, and K01AA023233. The content is the sole responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors have no conflicts of interest.
Contributor Information
Victoria R. Votaw, Department of Psychology, Center on Alcoholism, Substance Abuse, & Addictions, University of New Mexico.
Matthew R. Pearson, Center on Alcoholism, Substance Abuse, & Addictions, University of New Mexico
Elena Stein, Department of Psychology, Center on Alcoholism, Substance Abuse, & Addictions, University of New Mexico
Katie Witkiewitz, Department of Psychology, Center on Alcoholism, Substance Abuse, & Addictions, University of New Mexico.
References
- Anker JJ, Kushner MG, Thuras P, Menk J, Unruh AS (2016) Drinking to cope with negative emotions moderates alcohol use disorder treatment response in patients with co-occurring anxiety disorder. Drug Alcohol Depend 159:93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA (1988a) An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol 56:893–897. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Carbin MG (1988b) Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev 8:77–100. [Google Scholar]
- Brown T (2015) Confirmatory Factor Analysis for Applied Research, Second Edition, Guilford Publications, 2015. [Google Scholar]
- Burns L, Teesson M, O’Neill K (2005) The impact of comorbid anxiety and depression on alcohol treatment outcomes. Addiction 100:787–796. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Kiluk BD (2017) Cognitive behavioral interventions for alcohol and drug use disorders: Through the stage model and back again. Psychol Addict Behav 31:847–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality (2018) Results from the 2017 National Survey on Drug Use and Health: Detailed Tables. Rockville, Maryland. [Google Scholar]
- Chen FF (2007) Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Model 14:464–504. [Google Scholar]
- Cheung GW, Rensvold RB (2002) Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model 9:233–255. [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF (2006) Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 67:247–57. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Kuntsche E, Levitt A, Barber LL, Wolf S (2015) Motivational Models of Substance Use. [Google Scholar]
- Ghitza UE (2017) Commentary: Addictions Neuroclinical Assessment: A Neuroscience-Based Framework for Addictive Disorders. Front Psychiatry 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren KA, Witkiewitz K (2013) Missing data in alcohol clinical trials: a comparison of methods. Alcohol Clin Exp Res 37:2152–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model. [Google Scholar]
- Julian LJ (2011) Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirouac M, Stein ER, Pearson MR, Witkiewitz K (2017) Viability of the World Health Organization quality of life measure to assess changes in quality of life following treatment for alcohol use disorder. Qual Life Res 26:2987–2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, Volkow ND (2010) Neurocircuitry of addiction. Neuropsychopharmacology 35:217–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kranzler HR, McKay JR (2012) Personalized treatment of alcohol dependence. Curr Psychiatry Rep 14:486–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D (2016) Addictions Neuroclinical Assessment: A Neuroscience-Based Framework for Addictive Disorders. Biol Psychiatry 80:179–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwako LE, Schwandt ML, Ramchandani VA, Diazgranados N, Koob GF, Volkow ND, Blanco C, Goldman D (2019) Neurofunctional Domains Derived From Deep Behavioral Phenotyping in Alcohol Use Disorder. Am J Psychiatry appiajp201818030357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Kahler CW, Brown RA (2003) A modified computer version of the Paced Auditory Serial Addition Task (PASAT) as a laboratory-based stressor. Behav Ther. [Google Scholar]
- Li C-H (2016) Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behav Res Methods 48:936–49. [DOI] [PubMed] [Google Scholar]
- Litten RZ, Ryan ML, Falk DE, Reilly M, Fertig JB, Koob GF (2015) Heterogeneity of Alcohol Use Disorder: Understanding Mechanisms to Advance Personalized Treatment. Alcohol Clin Exp Res 39:579–584. [DOI] [PubMed] [Google Scholar]
- Lowman C, Allen J, Stout RL (1996) Replication and extension of Marlatt’s taxonomy of relapse precipitants: overview of procedures and results. The Relapse Research Group. Addiction 91 Suppl:S51–71. [PubMed] [Google Scholar]
- Maisto SA, Conigliaro JC, Gordon AJ, McGinnis KA, Justice AC (2008) An experimental study of the agreement of self-administration and telephone administration of the Timeline Followback interview. J Stud Alcohol Drugs 69:468–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Connors GJ (2006) Relapse in the addictive behaviors: integration and future directions. Clin Psychol Rev 26:229–31. [DOI] [PubMed] [Google Scholar]
- Mann K, Roos CR, Hoffmann S, Nakovics H, Leménager T, Heinz A, Witkiewitz K (2018) Precision Medicine in Alcohol Dependence: A Controlled Trial Testing Pharmacotherapy Response Among Reward and Relief Drinking Phenotypes. Neuropsychopharmacology 43:891–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt AG (1996) Taxonomy of high-risk situations for alcohol relapse: evolution and development of a cognitive-behavioral model. Addiction 91. [PubMed] [Google Scholar]
- McHugh RK, Geyer R, Karakula S, Griffin ML, Weiss RD (2018) Nonmedical benzodiazepine use in adults with alcohol use disorder: The role of anxiety sensitivity and polysubstance use. Am J Addict 27:485–490. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Votaw VR, Sugarman DE, Greenfield SF (2017) Sex and gender differences in substance use disorders. Clin Psychol Rev. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO (2017) Mplus users guide (Version 8). [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (n.d.) Drinking Levels Defined. Available at: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking Accessed October 10, 2019.
- Ray LA, Bujarski S, Yardley MM, Roche DJO, Hartwell EE (2017) Differences between treatment-seeking and non-treatment-seeking participants in medication studies for alcoholism: do they matter? Am J Drug Alcohol Abuse 43:703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins L, Cottler L, Keating S (1989) The NIMH Diagnostic Interview Schedule, Version III, revised (DIS-III-R). Rockville, Maryland, National Institute on Mental Health. [Google Scholar]
- Roos CR, Bowen S, Witkiewitz K (2017a) Baseline patterns of substance use disorder severity and depression and anxiety symptoms moderate the efficacy of mindfulness-based relapse prevention. J Consult Clin Psychol 85:1041–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos CR, Mann K, Witkiewitz K (2017b) Reward and relief dimensions of temptation to drink: construct validity and role in predicting differential benefit from acamprosate and naltrexone. Addict Biol 22:1528–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB (1992) Timeline Follow-Back In: Measuring Alcohol Consumption , pp 41–72. Humana Press. [Google Scholar]
- Spielberger CD, Sydeman SJ (1994) State-trait anxiety inventory and state-trait anger expression inventory In: The Use of Psychological Testing for Treatment Planning and Outcome Assessment . [Google Scholar]
- Stasiewicz PR, Bradizza CM, Schlauch RC, Coffey SF, Gulliver SB, Gudleski GD, Bole CW (2013) Affect regulation training (ART) for alcohol use disorders: Development of a novel intervention for negative affect drinkers. J Subst Abuse Treat 45:433–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widaman KF, Ferrer E, Conger RD (2010) Factorial invariance within longitudinal structural equation models: Measuring the same construct across time. Child Dev Perspect 4:10–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox CE, Tonigan JS (2018) Changes in depression mediate the effects of AA attendance on alcohol use outcomes. Am J Drug Alcohol Abus 44:193–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Harrop EN, Douglas H, Enkema M, Sedgwick C (2014) Mindfulness-based treatment to prevent addictive behavior relapse: Theoretical models and hypothesized mechanisms of change. Subst Use Misuse. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Litten RZ, Leggio L (2019a) Advances in the science and treatment of alcohol use disorder. Sci Adv 5:eaax4043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Masyn KE (2008) Drinking trajectories following an initial lapse. Psychol Addict Behav 22:157–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Roos CR, Mann K, Kranzler HR (2019b) Advancing Precision Medicine for Alcohol Use Disorder: Replication and Extension of Reward Drinking as a Predictor of Naltrexone Response. Alcohol Clin Exp Res acer.14183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Villarroel NA (2009) Dynamic Association Between Negative Affect and Alcohol Lapses Following Alcohol Treatment. J Consult Clin Psychol 77:633–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zywiak WH, Connors GJ, Maisto SA, Westerberg VS (1996) Relapse research and the Reasons for Drinking Questionnaire: a factor analysis of Marlatt’s relapse taxonomy. Addiction 91 Suppl:S121–30. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.