Abstract
Background
Lifestyle modification is a key component of cardiovascular disease prevention before and concurrently with pharmacologic interventions. We evaluated whether lifestyle factors change in relation to the initiation of antihypertensive or lipid‐lowering medication (statins).
Methods and Results
The study population comprised 41 225 participants of the FPS (Finnish Public Sector) study aged ≥40 years who were free of cardiovascular disease at baseline and responded to ≥2 consecutive surveys administered in 4‐year intervals in 2000–2013. Medication use was ascertained through pharmacy‐claims data. Using a series of pre–post data sets, we compared changes in body mass index, physical activity, alcohol consumption, and smoking between 8837 initiators and 46 021 noninitiators of antihypertensive medications or statins. In participants who initiated medication use, body mass index increased more (difference in change 0.19; 95% CI, 0.16–0.22) and physical activity declined (−0.09 metabolic equivalent of task hour/day; 95% CI, −0.16 to −0.02) compared with noninitiators. The likelihood of becoming obese (odds ratio: 1.82; 95% CI, 1.63–2.03) and physically inactive (odds ratio: 1.08; 95% CI, 1.01–1.17) was higher in initiators. However, medication initiation was associated with greater decline in average alcohol consumption (−1.85 g/week; 95% CI, −3.67 to −0.14) and higher odds of quitting smoking (odds ratio for current smoking in the second survey: 0.74; 95% CI, 0.64–0.85).
Conclusions
These findings suggest that initiation of antihypertensive and statin medication is associated with lifestyle changes, some favorable and others unfavorable. Weight management and physical activity should be encouraged in individuals prescribed these medications.
Keywords: antihypertensive agents, lifestyle, longitudinal, primary prevention, statins
Subject Categories: Cardiovascular Disease, Lifestyle, Primary Prevention, Lipids and Cholesterol, High Blood Pressure
Clinical Perspective
What Is New?
Few longitudinal studies have examined whether initiation of preventive medication affects lifestyle, either increasing or decreasing the likelihood of unhealthy behaviors.
What Are the Clinical Implications?
Because initiation of antihypertensive or statin therapy appears to be associated with some negative lifestyle changes, expansion of pharmacologic interventions toward populations at low cardiovascular disease risk may not necessarily lead to expected benefits at the population level.
Effective measures are needed to support the recommended lifestyle change in relation to the initiation of pharmacologic interventions for primary prevention.
Introduction
Use of antihypertensive medications and statins for the primary prevention of cardiovascular disease (CVD) has expanded over the past few decades1, 2, 3 and may increase further in response to recent guideline changes.4, 5, 6 However, lifestyle modification remains a key component of CVD prevention before and concurrently with pharmacologic interventions.4, 5, 7, 8
Whether and how initiation of preventive medication affects lifestyle remains unclear. Because lifestyle counseling should precede prescription of preventive medication,8 medication users may have better perception of their CVD risk9, 10 and a healthier lifestyle compared with nonusers.11, 12 The perceived effectiveness of pharmacotherapy may provide an incentive to adhere to a lifestyle that also prevents other diseases.13, 14 The counterargument is that individuals may substitute medication for a healthy lifestyle and continue an unhealthy lifestyle or even engage in it,14 which may reduce the effectiveness of pharmacotherapy.15, 16
The diagnosis of CVD or diabetes mellitus has been found to trigger lifestyle changes, including weight loss,17 increase in physical activity,18 decrease in alcohol consumption,18 and smoking cessation.17, 19 Participants of the Danish Inter99 trial with hypertension or hyperlipidemia who initiated medication for these conditions were more likely to engage in favorable dietary changes compared with noninitiators during 5‐year follow‐up.20 Statin initiators also increased their physical activity. Recently, however, studies have reported lower physical activity among people who initiate21 or use statins14, 22 or antihypertensive medications10 compared with nonusers. According to the US NHANES (National Health and Nutrition Examination Survey) data,23 in the early 2000s statin users had lower caloric and fat intake compared with nonusers. The difference disappeared by the mid‐2000s and was reversed by 2010. Most recent findings suggested statin users consumed more calories and fat than nonusers. Simultaneously, the prevalence of obesity increased faster among users.22, 23
We used repeat observational data to assess the extent to which initiation of antihypertensive or lipid‐lowering (statin) therapy predicts changes in lifestyle factors, such as body mass index (BMI), leisure‐time physical activity, alcohol consumption, and smoking, in a large cohort of Finnish adults. We sought to determine whether initiation of preventive medication is more likely to complement a healthy lifestyle change or substitute for it. To obtain robust estimates, we analyzed data as a series of pre–post studies.24, 25
Methods
Study Population and Design
Participants were drawn from the FPS (Finnish Public Sector) study cohort of employees of 10 towns and 6 hospital districts.25, 26 Data were sourced from questionnaire surveys administered to FPS subcohorts in 4‐year intervals from 2000 to 2013 (average response rate 70%),25 employer records, and national health registers. We included participants who responded to ≥2 consecutive surveys (waves 1 and 2) and were aged ≥40 years and free of CVD at wave 1. Individual‐level survey data could not be made publicly available, but information on the data and analyses are available upon request to the corresponding author.
We constructed a long‐form data set using subsets of the original data and organized them into 3 pre–post sets with separate baselines (2000–2002, 2004–2005, or 2008–2009) and corresponding follow‐ups (2004–2005, 2008–2009, or 2012–2013, respectively). In all, 41 225 participants belonged to these data sets: 15 880 to 1 data set, 10 143 to 2 data sets, and 15 202 to 3 data sets.
According to Finnish law, written consent is not required for register‐based and survey research as long as the participation is voluntary. The FPS study participants were informed about the aims of the study and the record linkage. The ethics committees of Helsinki University Hospital and the Finnish Institute of Occupational Health approved the FPS study protocol.
Initiator, Prevalent User, and Nonuser Cohorts of Preventive Medication
We used the participants’ personal identification numbers (a unique number assigned to each Finnish citizen) to link participants to the electronic records of the Social Insurance Institution (SII) of Finland covering the years 1994–2011. Records of pharmacy claims were used to ascertain medication use. We identified antihypertensive medications with Anatomical Therapeutic Chemical (ATC) codes C02 (antihypertensives), C03 (diuretics), C07 (β‐blockers), C08 (calcium channel blockers), C09 (renin–angiotensin system blockers), and C10AA and C10BA02 (both for statins).
We defined initiators as those who filled ≥1 prescription for any preventive medication for the first time after their baseline response date but before their wave 2 response date. Participant observations with no prescription fills by wave 2 were defined as noninitiators. We focused on comparing initiators of either antihypertensive medications or statins with those who remained noninitiators of both. For secondary comparisons, we included prevalent users, defined as those participant observations for which ≥1 prescription for any preventive medication was filled before or on the baseline response date.
Lifestyle Factors
Height, weight, physical activity, average weekly alcohol consumption, and smoking status were assessed using standard questionnaires. Based on self‐reported height and weight, we calculated BMI (kg/m2) and defined BMI 25 to <30 as overweight and BMI ≥30 as obesity. Physical activity was assessed using the following questions26: “How much did you exercise per week on average during the past year?” and “Estimate whether the level of intensity of the exercise corresponded to walking, vigorous walking, jogging, or running.” The number of hours per week spent on activity at each intensity level was multiplied by the average energy expenditure of each activity, expressed in metabolic equivalent of task (MET) hours. We used the sum of MET hours to identify active (>4 h/day), moderately active (2–4 h/day), and inactive participants (<2 h/day).27 Drinking habits were requested as follows28: “Have you ever consumed at least one glass of some alcoholic drink?” and “How much do you consume of the following alcoholic drinks on average (beer per week; wine or other mild drinks per week; spirits per month)?” We combined alcohol consumption into 1 measure of average weekly consumption (grams of pure alcohol). High alcohol consumption equated to consuming >240 g/week in men and >160 g/week in women.29 In addition, we considered answering “yes” to the following question as an indicator of high consumption: “Have you ‘passed out’ due to drinking during the past year?” Any other consumption was considered moderate. Smoking status was assessed with the following questions30: “Do you smoke or have you previously smoked regularly, that is daily or nearly daily?” and “Do you still smoke regularly?” Those responding “yes” to the second question were categorized as current smokers at each survey wave. Those who responded “yes” to the first and “no” to the second questions were categorized as former smokers, and those who responded “no” to both of the questions were categorized as never smokers. To depict clustering of lifestyle‐related risks, we calculated the number of lifestyles at the unhealthiest level (obesity, physical inactivity, high alcohol consumption, current smoking).31
The outcome measures included changes in continuous BMI, physical activity, alcohol consumption, and number of cigarettes smoked per day between the waves and the presence of obesity, physical inactivity, high alcohol consumption, current smoking, or their clustering (3 or 4 unhealthy lifestyles) at wave 2.
Covariates
Covariates were assessed at baseline. Information on sex, age, employment, and occupational status (upper grade nonmanual workers, lower grade nonmanual workers, clerks, or manual workers) came from employer records. Information on marital status and, for those who had left the FPS organizations, employment status came from survey responses. Nationwide hospital discharge and SII special reimbursement registers were used to ascertain history of CVD (acute myocardial infarction, chronic coronary heart disease, chronic heart failure, and stroke) at baseline and between the waves. Information on special reimbursements and prescription fills (A10) were used to ascertain history of diabetes mellitus.
Statistical Analyses
The results from the data sets were pooled. We modeled each lifestyle factor as a separate outcome with a generalized estimating equation approach accounting for within‐person correlation across data sets and applied bootstrapping to obtain stable 95% CIs.
We estimated the associations between medication initiation and continuous outcomes using linear regression. Associations with unhealthy lifestyles at wave 2 were estimated with logistic regression, stratifying by presence of the respective unhealthy lifestyle at baseline. To account for the changes in clinical guidelines and prescribing and the general lifestyle trends, all models included baseline period and time interval between the survey waves, as this interval influences the potential for change in lifestyles. Fully adjusted models included age; sex; marital, occupational, and employment status; diabetes mellitus; and other lifestyle factors measured at baseline. Participant observations that were missing data on any covariate were excluded from the multivariable models.
Sensitivity and Subgroup Analyses
First, we excluded participant observations with diabetes mellitus at baseline and those diagnosed with diabetes mellitus or CVD between waves 1 and 2 because our focus was on primary prevention. Second, to identify true medication initiators, we redefined initiation as refilling a prescription for preventive medication at least once within a year since initiation. Third, to confirm the temporal order between medication initiation and lifestyle change, we restricted our cohort to respondents of 3 consecutive surveys and compared the presence of unhealthy lifestyles at wave 3 between initiators and noninitiators who maintained the same lifestyle at waves 1 and 2.25 Fourth, we repeated the main analyses separately for antihypertensive medications and statins to see whether the results were specific to a therapeutic class. Last, we stratified the analyses by baseline period and sex. We tested statistical significance of the interactions by including user‐group‐by‐period or user‐group‐by‐sex interaction terms in the outcome models, respectively. Analyses were performed using SAS v9.4 (SAS Institute).
Results
Of a total of 81 772 participant observations based on the 41 225 FPS participants, 84% were female, with mean age of 52±7.2 years (Table 1); and 8837 (10.8%) presented as initiators of preventive medication, 26 914 (32.9%) as prevalent users, and 46 021 (56.3%) as noninitiators between waves 1 and 2 (mean interval: 4.0 years; range: 2.0–5.4 years). Medication initiation took place a median of 1.7 years (interquartile range: 0.9–2.7 years) after baseline and a median of 2.4 years (interquartile range: 1.3–3.3 years) before the second survey wave. Between waves, 318 (3.6%) initiators, 477 (1.8%) prevalent users, and 48 (0.1%) noninitiators were newly diagnosed with CVD.
Table 1.
Baseline Characteristics of the 81 772 Participant Observations
| Characteristic | All Observations (n=81 772) | Initiators (n=8837) | Prevalent Users (n=26 914) | Noninitiators (n=46 021) |
|---|---|---|---|---|
| Baseline year, % | ||||
| 2000–2002 | 25.8 | 27.2 | 18.3 | 29.9 |
| 2004–2005 | 33.4 | 42.0 | 31.5 | 32.8 |
| 2008–2009 | 40.8 | 30.8 | 50.2 | 37.4 |
| Age, y, mean (SD) | 52.2 (7.24) | 52.4 (6.61) | 55.1 (7.24) | 50.4 (6.78) |
| 40–49 | 41.7 | 38.0 | 25.7 | 51.7 |
| 50–59 | 43.1 | 49.0 | 48.4 | 38.8 |
| 60–78 | 15.3 | 13.0 | 25.9 | 9.5 |
| Women, % | 83.9 | 83.8 | 82.6 | 84.3 |
| Married/cohabiting, % | 76.3 | 76.5 | 75.6 | 76.6 |
| Occupational status, % | ||||
| Upper grade nonmanual workers | 32.1 | 29.8 | 30.6 | 33.3 |
| Lower grade nonmanual workers | 26.5 | 26.1 | 25.4 | 27.2 |
| Clerks | 7.4 | 7.2 | 8.3 | 6.9 |
| Manual workers | 34.1 | 36.9 | 35.7 | 32.6 |
| Employed, % | 89.4 | 92.3 | 81.0 | 93.7 |
| Body weight, % | ||||
| Normal | 49.8 | 43.0 | 37.2 | 58.3 |
| Overweight | 35.5 | 39.4 | 39.8 | 32.3 |
| Obese | 14.7 | 17.6 | 23.0 | 9.4 |
| Physical activity, % | ||||
| Active | 40.8 | 38.1 | 34.5 | 45.0 |
| Moderate | 33.6 | 33.5 | 34.7 | 33.0 |
| Inactive | 25.6 | 28.4 | 30.9 | 22.0 |
| Alcohol consumption, % | ||||
| Moderate | 71.7 | 70.9 | 69.5 | 73.2 |
| None | 14.9 | 14.3 | 16.5 | 14.1 |
| High | 13.4 | 14.8 | 14.1 | 12.7 |
| Smoking, % | ||||
| Never | 68.2 | 65.1 | 68.5 | 68.6 |
| Former | 18.3 | 19.7 | 19.5 | 17.4 |
| Current | 13.4 | 15.1 | 12.0 | 14.0 |
| No. of unhealthy lifestyles,a % | ||||
| 0 | 52.0 | 47.0 | 45.4 | 56.8 |
| 1–2 | 45.2 | 49.3 | 50.7 | 41.3 |
| 3–4 | 2.8 | 3.6 | 3.9 | 2.0 |
| History of antihypertensive medication use, % | 29.3 | NA | 89.1 | NA |
| History of statin use, % | 9.6 | NA | 29.1 | NA |
| Diabetes mellitus, % | 2.7 | 2.0 | 6.7 | 0.6 |
The observations are based on the 41 225 participants of the FPS (Finnish Public Sector) study. Numbers are percentages unless otherwise specified. Of all participant observations included, 79 889 (97.7%) had data available on body mass index, 80 988 (99.0%) on physical activity, 81 337 (99.5%) on alcohol consumption, and 79 675 (97.4%) on smoking at baseline. NA indicates not applicable.
Obesity, physical inactivity, high alcohol consumption, and current smoking.
Change in Lifestyle
Average BMI increased among both initiators and noninitiators (Table 2), but in the fully adjusted model, the mean increase in BMI was larger (difference in change: 0.19; 95% CI, 0.16–0.22) among initiators. Among wave 1 obese participants, the odds of obesity at wave 2 were 1.37 times greater (95% CI, 1.15–1.65) for initiators compared with noninitiators (Figure). Among wave 1 nonobese participants, the odds of obesity at wave 2 were 1.82 times greater (95% CI, 1.63–2.03) for initiators versus noninitiators. Furthermore, average MET h/day declined among initiators versus noninitiators (−0.09; 95% CI, −0.16 to −0.02; Table 2). Initiators had greater odds of physical inactivity at wave 2 regardless of baseline activity (Figure). Table S1 shows the shifts of participant observations between levels of lifestyle factors within user groups.
Table 2.
Changes in BMI, Physical Activity, and Alcohol Consumption Between the Survey Waves in Initiators and Prevalent Users of Preventive Medication Versus Noninitiators
| Lifestyle Factor/User Group | Outcome | ||||
|---|---|---|---|---|---|
| Mean (SDa) | Mean Change (P Valuea) | β Value (95% CI)b | |||
| Baseline | Second Survey | Unadjusted Differencec | Adjusted Differenced | ||
| BMI, kg/m2 | |||||
| Initiators (n=8425) | 26.3 (4.2) | 26.8 (4.5) | 0.51 (<0.001) | 0.13 (0.08–0.17) | 0.19 (0.16–0.22) |
| Prevalent users (n=25 348) | 27.0 (4.6) | 27.3 (4.7) | 0.31 (<0.001) | −0.04 (−0.07 to 0.01) | 0.08 (0.06–0.10) |
| Noninitiators (n=44 091) | 24.9 (3.7) | 25.2 (3.9) | 0.37 (<0.001) | Reference | Reference |
| Physical activity (MET h/d) | |||||
| Initiators (n=8658) | 4.15 (3.77) | 3.97 (3.60) | −0.18 (<0.001) | −0.13 (−0.22 to −0.04) | −0.09 (−0.16 to −0.02) |
| Prevalent users (n=26 368) | 3.78 (3.44) | 3.69 (3.38) | −0.09 (<0.001) | −0.12 (−0.17 to −0.06) | −0.08 (−0.13 to −0.04) |
| Noninitiators (n=45 312) | 4.71 (4.00) | 4.70 (4.03) | −0.01 (0.47) | Reference | Reference |
| Alcohol consumption, g/wk | |||||
| Initiators (n=8721) | 69.0 (108) | 66.4 (110) | −2.64 (0.011) | −2.57 (−4.75 to −0.38) | −1.85 (−3.67 to −0.14) |
| Prevalent users (n=26 546) | 66.7 (109) | 63.9 (111) | −2.38 (<0.001) | −1.73 (−3.13 to 0.34) | −0.72 (−1.92 to 0.49) |
| Noninitiators (n=45 488) | 61.1 (93.2) | 60.6 (95.6) | −0.44 (0.26) | Reference | Reference |
| No. of cigarettes/daye | |||||
| Initiators (n=876) | 13.1 (7.05) | 12.5 (6.83) | −0.60 (<0.001) | −0.37 (−0.63 to −0.11) | −0.34 (−0.60 to −0.08) |
| Prevalent users (n=2251) | 12.3 (6.65) | 12.1 (6.71) | −0.23 (0.016) | −0.02 (−0.20 to 0.16) | 0.05 (−0.13 to 0.24) |
| Noninitiators (n=4532) | 11.9 (6.60) | 11.7 (6.45) | −0.19 (0.002) | Reference | Reference |
Only participant‐observations who had data available on all baseline covariates were included in adjusted models (n=74 291 or 95.4% of those with data on body mass index at both surveys, n=75 613 or 94.1% of those with data on physical activity at both surveys, n=75 781 or 93.8% of those with data on alcohol consumption at both surveys, n=7339 or 95.8% of those reporting number of cigarettes smoked at both surveys). BMI indicates body mass index; MET, metabolic equivalent of task.
SDs and P values reported here do not take into account that each individual may have contributed to >1 data set.
Derived from generalized estimating equations.
Adjusted for baseline year and time interval between the survey waves.
Adjusted for baseline year; time interval; age; sex; marital, occupational, and employment status; diabetes mellitus; smoking status; and other lifestyle factors.
Among those who were current smokers at both waves.
Figure 1.
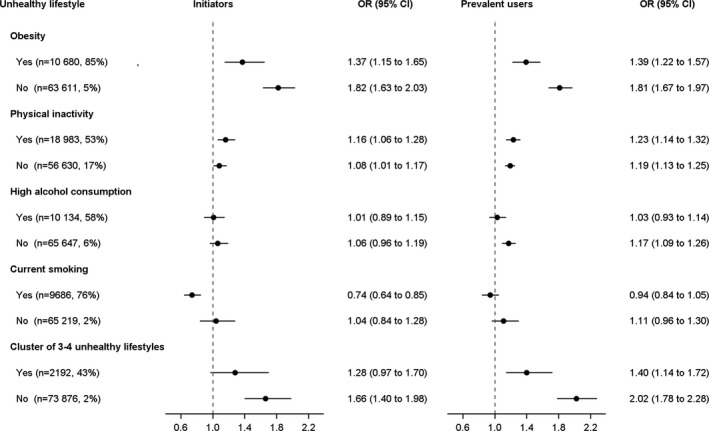
Adjusted odds ratios (ORs) for unhealthy lifestyles at the second survey for users of preventive medication (vs noninitiators) by presence of the respective unhealthy lifestyle at baseline. Number of participant observations and prevalence of unhealthy lifestyle at the second survey in parentheses.
Average weekly alcohol consumption declined more among initiators compared with noninitiators (−1.85 g/week; 95% CI, −3.67 to −0.14; Table 2). When the comparison was restricted to those initiators (n=7014) and noninitiators (n=37 297) who reported any alcohol consumption at both waves, the adjusted difference in change in weekly consumption was −1.67 g (95% CI, −3.72 to 0.39). No difference in the odds of high alcohol consumption at wave 2 was observed between user groups regardless of baseline drinking (Figure).
The prevalence of current smoking tended to decrease in all subgroups (Table 1, Table S1). However, baseline smokers who initiated medication use were more likely to quit smoking compared with smokers who remained untreated (adjusted odds ratio [OR] for current smoking among initiators versus noninitiators: 0.74; 95% CI, 0.64–0.85; Figure). Furthermore, initiators who were current smokers at both waves decreased smoking more than their noninitiator counterparts (adjusted difference in change in the number of cigarettes per day: −0.34; 95% CI: −0.60 to −0.08; Table 2).
Among those with 0–2 unhealthy lifestyles at baseline, the adjusted OR of a cluster of 3 to 4 unhealthy lifestyles at wave 2 was 1.66 (95% CI, 1.40–1.98) for initiators compared with noninitiators (Figure). The relative difference between user groups was smaller in the subgroup that already had 3 to 4 unhealthy lifestyles at baseline. In this subgroup (n=1231), BMI increased (adjusted difference: 0.32; 95% CI, 0.06–0.59) and MET h/day declined (−0.33; 95% CI, −0.57 to −0.09) more among initiators compared with noninitiators, whereas there was no significant difference in change in average alcohol consumption (0.09 g/week; 95% CI, −17.6 to 17.8) or in the odds of current smoking at wave 2 (adjusted OR: 0.92; 95% CI, 0.69–1.24).
Prevalent users’ lifestyle changed in the same direction as initiators’ lifestyle, although the average changes in BMI and weekly alcohol consumption were smaller in comparison with noninitiators (Table 2). Prevalent users were more likely to develop obesity, physical inactivity, and high alcohol consumption than were noninitiators (Figure). Within the subgroup with 0 to 2 unhealthy lifestyles at baseline, in particular, prevalent users had twice the odds of having 3 to 4 unhealthy lifestyles at wave 2 compared with noninitiators (adjusted OR: 2.02; 95% CI, 1.78–2.28).
Sensitivity and Subgroup Analyses
Exclusion of participants with diabetes mellitus or new CVD (Tables S2 and S3) or initiators with no refills within the first year since initiation (Tables S4 and S5) did not materially change the main results. The analyses including initiators and noninitiators who maintained the same lifestyle at waves 1 and 2 showed that initiators were more likely to develop obesity and a cluster of unhealthy lifestyles by wave 3 (Table S6). These analyses support the temporal order between medication initiation and unhealthy lifestyle change.
The associations between antihypertensive medication use and lifestyle changes resembled those in the main analyses (Tables S7 and S8). Conversely, the associations for statin initiation were generally weaker. However, statin initiation appeared to be more strongly associated with decline in average weekly alcohol consumption (−2.38 g; 95% CI, −4.33 to −0.43) and quitting smoking (OR for current smoking: 0.63; 95% CI, 0.53–0.75). Almost half (43.9%) of initiators and 24.3% of noninitiators of statins were users of antihypertensive medication at wave 1 (Table S9). In addition, 7.6% of initiators of antihypertensive medication and 4.7% of noninitiators had used statins.
The baseline period did not appear to modify the associations between user group and changes in BMI, alcohol consumption, or physical activity or between user group and odds of any of unhealthy behaviors at wave 2 (Tables S10 and S11; P>0.05 for user group‐by‐period interactions). Sex did not modify the associations between user group and change in BMI or weekly alcohol consumption or between user group and odds of any of unhealthy behaviors at wave 2 (Tables S12 and S13; P>0.05 for user‐group‐by‐sex interactions). The average decline in physical activity was of the same magnitude in both sexes (Table S12). Among women, however, physical activity declined more among initiators than noninitiators (adjusted difference in change: −0.11 MET h/day; 95% CI, −0.19 to −0.04). Among men, no difference was found (adjusted difference in change: 0.01 MET h/day; 95% CI, −0.19 to 0.20; P=0.20 for user group‐by‐sex interaction). In the subgroup of physically inactive participants at baseline, the odds of physical inactivity associated with medication initiation were increased among women (OR: 1.20; 95% CI, 1.08–1.32) but not in men (OR: 1.01; 95% CI, 0.81–1.26; P=0.21 for user‐group‐by‐sex interaction). Among those at least moderately active at baseline, no such sex difference was observed (OR, women: 1.10 [95% CI, 1.00–1.22]; men: 1.09 [95% CI, 0.91–1.30]).
Discussion
In this large cohort study of Finnish adults free of CVD, there are 4 key findings. First, initiators experienced greater increases in BMI and were more likely to become obese than did noninitiators. This attenuates positive treatment effects and supports the substitution hypothesis. Second, the likelihood of becoming physically inactive was higher among initiators, a finding supporting the substitution hypothesis. Third, in support of the complementation hypothesis, smokers who initiated preventive medication were more likely to either quit or decrease smoking compared with untreated smokers. This is likely to amplify the effectiveness of pharmacotherapy. Fourth, although average alcohol consumption decreased more among initiators than noninitiators, there was no difference in the odds of heavy drinking.
This was the first large‐scale, prospective, cohort study on the associations between use of preventive medications and lifestyle change. Prior research on the relationships between preventive medication use and lifestyle has typically considered either use of antihypertensive medications10, 32 or statins9, 11, 14, 21, 22, 23, 33 but rarely both.12, 20 Most previous studies have been cross‐sectional9, 11, 14, 22, 23, 33 and provide no information on potential lifestyle changes during the time window around the initiation of medication use. We included both antihypertensive and statin medications and also studied them separately. Using individual‐level data with repeated measurements, we were able to determine each individual's lifestyle before and after medication initiation.
Our results on greater declines in smoking and increases in obesity among initiators of preventive medication agree with those from a small Canadian cohort study involving 769 new hypertensive participants of the National Population Survey (1994–2002) who also reported use of antihypertensive medication.32 Another longitudinal study based on the Framingham Heart Study Offspring Cohort (1983–2001) showed an increase in obesity among statin users but no clear decrease in smoking.14 Furthermore, statin use was associated with an increase in moderate alcohol consumption and physical activity in men but not in women. In addition, a study including 871 participants of the Inter99 health behavior intervention trial reported an association between increased physical activity and likelihood of initiating statin use over a 5‐year period (up to 2006),20 but no association was observed with initiation of antihypertensive medication. These results are consistent with the observations in our study population, the majority of whom started preventive therapy with antihypertensive medications. Together with the preceding observations and data from repeated cross‐sectional surveys from the United States23 and Korea22 showing faster increases in fat and caloric intake, obesity, and physical inactivity among statin users versus nonusers, our study provides more support for the substitution hypothesis (unfavorable or no lifestyle change) than for the complementation hypothesis (positive lifestyle change).
Statin initiation is associated with increase in muscle complaints,34 potentially interfering with physical activity. A US study among older men reported that prevalent statin use was associated with modestly lower physical activity.21 However, a longitudinal analysis showed that physical activity declined faster among initiators than among prevalent users or noninitiators. We observed virtually no differences in change in physical activity between initiators, prevalent users, and nonusers of statins in our cohort, which was younger, predominantly female, and free of CVD.
It is well documented that smoking cessation often results in weight gain, particularly in women, that cannot be prevented by increasing physical activity.35 In our data, the average increase in BMI among quitters was 1.20 (SD: 2.05) for initiators and 1.09 (SD: 2.07) for noninitiators (data not shown). Although initiation of preventive medication was associated with quitting smoking, the difference in the increase of BMI remained approximately the same for initiators and noninitiators after excluding the quitters (adjusted difference: 0.18; 95% CI, 0.15–0.22).
Limitations
A key limitation of our study is the generalizability of the results. Our study population consisted of a relatively homogenous sample of white public sector workers, with only 16% of the participant observations related to men and the mean age being slightly >50 years. Furthermore, during the study period, intensive public health action took place in Finland36 and may have affected the lifestyles of both medication users and nonusers. For example, smoking in public indoor places and workplaces was prohibited already in the 1990s and in restaurants in 2006. The national development program for the prevention and care of diabetes mellitus was implemented in 2000–2010.37 This program aimed to increase awareness of diabetes mellitus and its risk factors (including the same lifestyle factors considered in this study) in the whole population through various activities, such as media campaigns and health fairs. Consequently, our results may not be generalizable to countries or settings with different preventive policies.
Furthermore, initiators of preventive medication have presumably received counseling from health professionals before initiation, as the clinical guidelines have recommended lifestyle change lasting for weeks or months as the sole intervention among individuals in primary prevention.29, 38 Unfortunately, we have no information on the contents and timing of this counseling or other forms of health promotion to which the medication users in this study were exposed. Because some participants may have initiated lifestyle change before baseline, we may have underestimated the change related to medication initiation. However, high‐risk behaviors were more common among initiators than noninitiators at baseline; therefore, there was more room for improvement.
We did not have information on each participant's diet (eg, fat or fruit and vegetable intake), blood pressure, or cholesterol levels. Our noninitiator population is likely to be a mixture of patients free of hypertension or dyslipidemia and those who may have been diagnosed with these conditions but did not use medications; that is, a small proportion of noninitiators may be individuals among whom lifestyle modification alone was effective. Our definition of medication use was based on dispensation data, and we could not verify whether and how the dispensed medications were consumed. Self‐reporting has been found to underestimate obesity,39 smoking,40 and alcohol consumption.41 However, this is unlikely to have changed between waves, and each lifestyle factor has been shown to be associated with increased all‐cause mortality and CVD event risk in these data, except for high alcohol consumption.26
In sensitivity analyses, we excluded participant observations linked to records indicating myocardial infarction, chronic coronary heart disease, chronic heart failure, or stroke between the survey waves and those indicating diabetes mellitus at any time before the second wave. This did not alter observed associations. However, other conditions such as respiratory events, cancers, or chronic gastrointestinal disease could also affect lifestyle factors and, if distributed unevenly between initiators and noninitiators of preventive medication, may have confounded the associations between medication initiation and lifestyle change. Furthermore, it is possible that the associations between medication initiation and increases in BMI were confounded by menopausal status (among women) or age‐related weight gain. When we analyzed these associations within 10‐year age groups, BMI seemed to increase more among initiators than noninitiators in each age group, but the association between medication initiation and change in BMI was stronger among those aged 40 to 49 years (adjusted difference in change in BMI: 0.30; 95% CI, 0.22–0.37) than among the older age groups in the whole study population (adjusted difference in change in BMI, 50–59 years: 0.11 [95% CI, 0.05–0.17]; ≥60 years: 0.13 [95% CI, 0.02–0.24). This was true for women and men (data not shown); therefore, our conclusions did not change.
Our findings support the notion that there is scope to improve management of lifestyle‐related risk factors among individuals who have initiated preventive medication. Patients’ awareness of their risk factors alone seems not to be effective in improving health behaviors.42 The most recent primary prevention guidelines in Europe8 and the United States43 emphasize cognitive‐behavioral strategies (eg, motivational interviewing, shared decision‐making), multidisciplinary and team‐based approaches, and evaluation of social and other individual‐level determinants of health when choosing the optimal strategy for each patient.
Perspectives
Initiation of antihypertensive or statin therapy appears to be associated with lifestyle changes, some positive and others negative. This means that expansion of pharmacologic interventions toward populations at low CVD risk may not necessarily lead to expected benefits at the population level. More effective measures are needed to support the recommended lifestyle change in relation to the initiation of pharmacologic interventions for primary prevention.
Sources of Funding
This work was funded by the Academy of Finland (grant no. 138255), NordForsk (the Nordic Research Program on Health and Welfare to Kivimäki), the Academy of Finland (grant no. 311492 to Kivimäki) and Helsinki Institute of Life Science (to Kivimäki), and Hospital District of Southwest Finland (to Korhonen).
Disclosures
Setoguchi received research funding from and was a consultant for Pfizer Inc. and Janssen Research & Development, LLC. The remaining authors have no disclosures to report.
Supporting information
Table S1. Cross‐Tabulation of Unhealthy Lifestyle Factors at Baseline and During the Second Survey Wave by Use of Preventive Medication
Table S2. Changes in Body Mass Index, Physical Activity, and Alcohol Consumption From the Baseline Survey to the Second Survey Wave Among Users of Preventive Medication Versus Noninitiators
Table S3. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Users of Preventive Medication (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline
Table S4. Changes in Body Mass Index, Physical Activity, and Alcohol Consumption From the Baseline Survey to the Second Survey Wave Among Initiators With at Least 1 Refill of Preventive Medication Versus Noninitiators
Table S5. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Initiators of Preventive Medication With at Least 1 Refill (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline
Table S6. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Third Survey Wave for Initiators of Preventive Medication (Versus Noninitiators) Stratified by Presence/Absence of the Respective Unhealthy Lifestyle at Baseline and Wave 2
Table S7. Changes in Body Mass Index, Physical Activity, and Alcohol Consumption From the Baseline Survey to the Second Survey Wave Among Users of Antihypertensive Medications and Statins Versus Noninitiators
Table S8. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Users of Antihypertensive Medications and Statins (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline
Table S9. Baseline Characteristics of the 81 772 Participant Observations Stratified by Use of Antihypertensive Medications and Statins
Table S10. Changes in Body Mass Index, Alcohol Consumption, and Physical Activity From Baseline Survey to the Second Survey Wave Among Users of Preventive Medication Versus Noninitiators, by Baseline Year
Table S11. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Users of Preventive Medication (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline, by Baseline Year
Table S12. Changes in Body Mass Index, Physical Activity, and Alcohol Consumption From the Baseline Survey to the Second Survey Wave Among Users of Preventive Medication (Versus Noninitiators), by Sex
Table S13. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Users of Preventive Medication (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline, by Sex
(J Am Heart Assoc. 2020;9:e014168 DOI: 10.1161/JAHA.119.014168.)
References
- 1. Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health and Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126:2105–2114. [DOI] [PubMed] [Google Scholar]
- 2. Rikala M, Huupponen R, Helin‐Salmivaara A, Korhonen MJ. Channelling of statin use towards low‐risk population and patients with diabetes. Basic Clin Pharmacol Toxicol. 2013;113:173–178. [DOI] [PubMed] [Google Scholar]
- 3. Gu QP‐RR, Burt VL, Kit BK. Prescription cholesterol‐lowering medication use in adults aged 40 and over: United States, 2003–2012. NCHS data brief, no 177. Hyattsville, MD: National Center for Health Statistics. 2014. [PubMed] [Google Scholar]
- 4. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd‐Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–S45. [DOI] [PubMed] [Google Scholar]
- 5. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e426–e483. [DOI] [PubMed] [Google Scholar]
- 6. Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr, Whelton PK. Potential U.S. population impact of the 2017 ACC/AHA high blood pressure guideline. J Am Coll Cardiol. 2018;71:109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, Lee IM, Lichtenstein AH, Loria CM, Millen BE, Nonas CA, Sacks FM, Smith SC Jr, Svetkey LP, Wadden TA, Yanovski SZ, Kendall KA, Morgan LC, Trisolini MG, Velasco G, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S76–S99. [DOI] [PubMed] [Google Scholar]
- 8. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FD, Lochen ML, Lollgen H, Marques‐Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WM; Authors/Task Force M . 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lytsy P, Burell G, Westerling R. Cardiovascular risk factor assessments and health behaviours in patients using statins compared to a non‐treated population. Int J Behav Med. 2012;19:134–142. [DOI] [PubMed] [Google Scholar]
- 10. Siven SS, Niiranen TJ, Aromaa A, Koskinen S, Jula AM. Social, lifestyle and demographic inequalities in hypertension care. Scand J Public Health. 2015;43:246–253. [DOI] [PubMed] [Google Scholar]
- 11. Johal S, Jamsen KM, Bell JS, Mc Namara KP, Magliano DJ, Liew D, Ryan‐Atwood TE, Anderson C, Ilomaki J. Do statin users adhere to a healthy diet and lifestyle? The Australian Diabetes, Obesity and Lifestyle Study. Eur J Prev Cardiol. 2017;24:621–627. [DOI] [PubMed] [Google Scholar]
- 12. Kinjo MC‐CLE, Korhonen MJ, McGill RL, Setoguchi S. Potential contribution of lifestyle and socioeconomic factors to healthy user bias in antihypertensives and lipid lowering drugs. Open Heart. 2017;4:e000417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Becker GS. Health as human capital: synthesis and extensions. Oxf Econ Pap. 2007;59:379–410. [Google Scholar]
- 14. Kaestner R, Darden M, Lakdawalla D. Are investments in disease prevention complements? The case of statins and health behaviors. J Health Econ. 2014;36:151–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhang Y, Tuomilehto J, Jousilahti P, Wang Y, Antikainen R, Hu G. Lifestyle factors and antihypertensive treatment on the risks of ischemic and hemorrhagic stroke. Hypertension. 2012;60:906–912. [DOI] [PubMed] [Google Scholar]
- 16. Milionis HJ, Rizos E, Mikhailidis DP. Smoking diminishes the beneficial effect of statins: observations from the landmark trials. Angiology. 2001;52:575–587. [DOI] [PubMed] [Google Scholar]
- 17. Keenan PS. Smoking and weight change after new health diagnoses in older adults. Arch Intern Med. 2009;169:237–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schneider KL, Andrews C, Hovey KM, Seguin RA, Manini T, Lamonte MJ, Margolis KL, Waring ME, Ning Y, Sims S, Ma Y, Ockene J, Stefanick ML, Pagoto SL. Change in physical activity after a diabetes diagnosis: opportunity for intervention. Med Sci Sports Exerc. 2014;46:84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gorin AA, Phelan S, Hill JO, Wing RR. Medical triggers are associated with better short‐ and long‐term weight loss outcomes. Prev Med. 2004;39:612–616. [DOI] [PubMed] [Google Scholar]
- 20. Hempler NF, Krasnik A, Pisinger C, Jorgensen T. The relationship between changes in health behaviour and initiation of lipid‐lowering and antihypertensive medications in individuals at high risk of ischaemic heart disease. BMC Public Health. 2012;12:626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lee DS, Markwardt S, Goeres L, Lee CG, Eckstrom E, Williams C, Fu R, Orwoll E, Cawthon PM, Stefanick ML, Mackey D, Bauer DC, Nielson CM. Statins and physical activity in older men: the osteoporotic fractures in men study. JAMA Intern Med. 2014;174:1263–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Oh JY, Chekal L, Kim SW, Lee JY, Lee DC. Comparing the trend of physical activity and caloric intake between lipid‐lowering drug users and nonusers among adults with dyslipidemia: Korean National Health and Nutrition Examination Surveys (2010–2013). Korean J Fam Med. 2016;37:105–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sugiyama T, Tsugawa Y, Tseng CH, Kobayashi Y, Shapiro MF. Different time trends of caloric and fat intake between statin users and nonusers among US adults: gluttony in the time of statins? JAMA Intern Med. 2014;174:1038–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Danaei G, Rodriguez LA, Cantero OF, Logan R, Hernan MA. Observational data for comparative effectiveness research: an emulation of randomised trials of statins and primary prevention of coronary heart disease. Stat Methods Med Res. 2013;22:70–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lallukka T, Halonen JI, Sivertsen B, Pentti J, Stenholm S, Virtanen M, Salo P, Oksanen T, Elovainio M, Vahtera J, Kivimaki M. Change in organizational justice as a predictor of insomnia symptoms: longitudinal study analysing observational data as a non‐randomized pseudo‐trial. Int J Epidemiol. 2017;46:1277–1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Halonen JI, Stenholm S, Pentti J, Kawachi I, Subramanian SV, Kivimaki M, Vahtera J. Childhood psychosocial adversity and adult neighborhood disadvantage as predictors of cardiovascular disease: a cohort study. Circulation. 2015;132:371–379. [DOI] [PubMed] [Google Scholar]
- 27. Kujala UM, Kaprio J, Koskenvuo M. Modifiable risk factors as predictors of all‐cause mortality: the roles of genetics and childhood environment. Am J Epidemiol. 2002;156:985–993. [DOI] [PubMed] [Google Scholar]
- 28. Kouvonen A, Kivimaki M, Elovainio M, Vaananen A, De Vogli R, Heponiemi T, Linna A, Pentti J, Vahtera J. Low organisational justice and heavy drinking: a prospective cohort study. Occup Environ Med. 2008;65:44–50. [DOI] [PubMed] [Google Scholar]
- 29.[Update on current care guidelines. Treatment of hypertension]. Duodecim. 2004;120:2473–2474. [PubMed] [Google Scholar]
- 30. Pulakka A, Halonen JI, Kawachi I, Pentti J, Stenholm S, Jokela M, Kaate I, Koskenvuo M, Vahtera J, Kivimaki M. Association between distance from home to tobacco outlet and smoking cessation and relapse. JAMA Intern Med. 2016;176:1512–1519. [DOI] [PubMed] [Google Scholar]
- 31. Kivimaki M, Lawlor DA, Davey Smith G, Kouvonen A, Virtanen M, Elovainio M, Vahtera J. Socioeconomic position, co‐occurrence of behavior‐related risk factors, and coronary heart disease: the Finnish Public Sector study. Am J Public Health. 2007;97:874–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Neutel CI, Campbell N; Canadian Hypertension Society . Changes in lifestyle after hypertension diagnosis in Canada. Can J Cardiol. 2008;24:199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Thomsen RW, Nielsen RB, Norgaard M, Horsdal HT, Sturmer T, Larsen FB, Sorensen HT. Lifestyle profile among statin users. Epidemiology. 2013;24:619–620. [DOI] [PubMed] [Google Scholar]
- 34. Parker BA, Capizzi JA, Grimaldi AS, Clarkson PM, Cole SM, Keadle J, Chipkin S, Pescatello LS, Simpson K, White CM, Thompson PD. Effect of statins on skeletal muscle function. Circulation. 2013;127:96–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Parsons AC, Shraim M, Inglis J, Aveyard P, Hajek P. Interventions for preventing weight gain after smoking cessation. Cochrane Database Syst Rev. 2009;1:CD006219. [DOI] [PubMed] [Google Scholar]
- 36. Borodulin K, Vartiainen E, Peltonen M, Jousilahti P, Juolevi A, Laatikainen T, Mannisto S, Salomaa V, Sundvall J, Puska P. Forty‐year trends in cardiovascular risk factors in Finland. Eur J Public Health. 2015;25:539–546. [DOI] [PubMed] [Google Scholar]
- 37. Wikstrom K, Lindstrom J, Tuomilehto J, Saaristo TE, Helakorpi S, Korpi‐Hyovalti E, Oksa H, Vanhala M, Keinanen‐Kiukaanniemi S, Uusitupa M, Peltonen M. National diabetes prevention program (DEHKO): awareness and self‐reported lifestyle changes in Finnish middle‐aged population. Public Health. 2015;129:210–217. [DOI] [PubMed] [Google Scholar]
- 38. Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvanne M, Scholte op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F; European Association for Cardiovascular Prevention, Rehabilitation and Guidelines, ESC Committee for Practice Guidelines . European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012;33:1635–1701. [DOI] [PubMed] [Google Scholar]
- 39. Taylor AW, Dal Grande E, Gill TK, Chittleborough CR, Wilson DH, Adams RJ, Grant JF, Phillips P, Appleton S, Ruffin RE. How valid are self‐reported height and weight? A comparison between CATI self‐report and clinic measurements using a large cohort study. Aust N Z J Public Health. 2006;30:238–246. [DOI] [PubMed] [Google Scholar]
- 40. Fendrich M, Mackesy‐Amiti ME, Johnson TP, Hubbell A, Wislar JS. Tobacco‐reporting validity in an epidemiological drug‐use survey. Addict Behav. 2005;30:175–181. [DOI] [PubMed] [Google Scholar]
- 41. Ekholm O, Strandberg‐Larsen K, Gronbaek M. Influence of the recall period on a beverage‐specific weekly drinking measure for alcohol intake. Eur J Clin Nutr. 2011;65:520–525. [DOI] [PubMed] [Google Scholar]
- 42. Scheltens T, Beulens JW, Verschuren WM, Boer JM, Hoes AW, Grobbee DE, Bots ML. Awareness of hypertension: will it bring about a healthy lifestyle? J Hum Hypertens. 2010;24:561–567. [DOI] [PubMed] [Google Scholar]
- 43. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd‐Jones D, McEvoy JW, Michos ED, Miedema MD, Munoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary. Circulation. 2019;140:e563–e595. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Cross‐Tabulation of Unhealthy Lifestyle Factors at Baseline and During the Second Survey Wave by Use of Preventive Medication
Table S2. Changes in Body Mass Index, Physical Activity, and Alcohol Consumption From the Baseline Survey to the Second Survey Wave Among Users of Preventive Medication Versus Noninitiators
Table S3. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Users of Preventive Medication (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline
Table S4. Changes in Body Mass Index, Physical Activity, and Alcohol Consumption From the Baseline Survey to the Second Survey Wave Among Initiators With at Least 1 Refill of Preventive Medication Versus Noninitiators
Table S5. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Initiators of Preventive Medication With at Least 1 Refill (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline
Table S6. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Third Survey Wave for Initiators of Preventive Medication (Versus Noninitiators) Stratified by Presence/Absence of the Respective Unhealthy Lifestyle at Baseline and Wave 2
Table S7. Changes in Body Mass Index, Physical Activity, and Alcohol Consumption From the Baseline Survey to the Second Survey Wave Among Users of Antihypertensive Medications and Statins Versus Noninitiators
Table S8. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Users of Antihypertensive Medications and Statins (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline
Table S9. Baseline Characteristics of the 81 772 Participant Observations Stratified by Use of Antihypertensive Medications and Statins
Table S10. Changes in Body Mass Index, Alcohol Consumption, and Physical Activity From Baseline Survey to the Second Survey Wave Among Users of Preventive Medication Versus Noninitiators, by Baseline Year
Table S11. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Users of Preventive Medication (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline, by Baseline Year
Table S12. Changes in Body Mass Index, Physical Activity, and Alcohol Consumption From the Baseline Survey to the Second Survey Wave Among Users of Preventive Medication (Versus Noninitiators), by Sex
Table S13. Odds Ratios for Obesity, Physical Inactivity, High Alcohol Consumption, and Current Smoking at the Second Survey Wave for Users of Preventive Medication (Versus Noninitiators) Stratified by Presence of the Respective Unhealthy Lifestyle at Baseline, by Sex


