Abstract
Background
Troponin levels are frequently obtained in pediatric patients, but the benefit remains unclear.
Methods and Results
This retrospective study included 1993 patients aged 0 to 21 years without history of cardiac disease in whom troponin levels were obtained during clinical evaluation of cardiac and noncardiac presentations. Troponin was elevated (≥0.1 ng/mL) in 182 patients (9%). A cardiac diagnosis was made in 109 (60%) of those with elevated troponin and in 208 (12%) of those without (P<0.001). The positive predictive value of elevated troponin for a cardiac diagnosis was 60% for the entire cohort and 85% for patients with a cardiac presentation. The negative predictive value of nonelevated troponin was 89% for the entire cohort and 96% in patients without a cardiac presentation. Serial testing did not improve these predictive values. However, among 404 patients with initially nonelevated levels who had serial measurements, subsequent elevation was found in 80 (20%), of whom 15 (19%) had a cardiac diagnosis. The optimal troponin cutoff value to differentiate cardiac from noncardiac diagnosis was higher in children aged <3 months (0.045 ng/mL) compared with those aged ≥3 months (0.005 ng/mL).
Conclusions
Troponin can be a useful adjunctive test in the evaluation of children when the differential diagnosis includes cardiac etiologies. Serial measurement was not helpful when troponin was elevated at presentation but may merit consideration when the initial level is not elevated and there is ongoing concern about cardiac involvement. Lower reference values may be appropriate when evaluating children in contrast to adults.
Keywords: chest pain, children, reference value, troponin
Subject Categories: Congenital Heart Disease, Inflammatory Heart Disease, Cardiomyopathy
Chest symptoms occur frequently in previously healthy children, in whom the incidence of underlying cardiac pathology is exceedingly low.1, 2 In these patients, serum troponin levels are often obtained, but the merits of troponin testing in children are debated. Among published studies, some authors have concluded that troponin testing can be useful in this population,3, 4, 5 but others have reported that it leads to increased resource utilization with minimal incremental benefit.6 A potential limitation has been the lack of age‐specific troponin reference values for children and adolescents. Age‐related variation in troponin levels has been well studied in adults7, 8 and in a pediatric analysis that showed higher troponin I levels in younger children.9 Accordingly, the purpose of this work was to analyze the contribution of troponin testing in detection of heart disease in a large cohort of previously healthy children and adolescents and to explore age‐related differences in troponin levels that may be relevant to the utility of this testing.
Methods
This retrospective study included children and young adults aged <21 years in whom at least 1 troponin level was obtained at Boston Children's Hospital during outpatient or inpatient evaluation between January 01, 2005, and December 30, 2018. Patients with prior cardiac diagnoses were excluded. The study was approved by the Boston Children's Hospital institutional review board; no informed consent was required. The data that support the findings of this study are available from the corresponding author on reasonable request.
Elevated troponin was defined as an initial troponin T level ≥0.1 ng/mL—the established clinical laboratory reference value at this institution, defined as consistent with significant myocardial injury. The same troponin assay was used throughout the duration of the study period. Presenting complaints and discharge diagnoses were obtained from review of the International Classification of Diseases codes in the medical record, either Ninth Revision or Tenth Revision (ICD‐9 or ICD‐10), depending on the date of the encounter. The chief complaint at presentation was classified as one of the following: cardiac, respiratory, gastrointestinal, febrile, or other. Cardiac presentations, as defined, included chest pain, tachycardia or other arrhythmia, syncope, cardiomegaly, or ventricular dysfunction. Abnormal ECG was defined as the presence of ST‐segment changes, ventricular hypertrophy, atrioventricular block (second‐degree Mobitz II or third degree), supraventricular tachycardia, or ventricular tachycardia. Myocarditis was defined as possible if based solely on the clinical discharge diagnosis or as probable if there was also ≥1 of the following findings: ventricular dysfunction (left ventricular ejection fraction <50%) on echocardiogram and/or cardiac magnetic resonance, myocardial late gadolinium enhancement on magnetic resonance, and/or endomyocardial biopsy indicative of myocarditis. Discharge diagnoses were classified as either cardiac or noncardiac.
Categorical variables were summarized as frequencies and percentages, and continuous variables as mean±SD. A Fisher exact test was used for comparison of categorical variables. The positive predictive value (PPV) and negative predictive value of troponin testing was calculated in the entire cohort and in patients with and without cardiac signs or symptoms at time of presentation. Receiver operating characteristic curve analyses were used to evaluate the diagnostic accuracy of troponin testing to differentiate cardiac from noncardiac diagnosis and to determinate cutoff values (overall and within age groups) and to calculate their sensitivity and specificity. Youden's J statistic test was used to define the optimal cutoff value. Univariate and multivariable logistic regression was performed to evaluate the predictors of cardiac diagnosis at time of discharge. Only variables with P<0.20 on univariate analysis were included in the multivariable model. All analyses were performed with SPSS Statistics v23 (IBM Corp). A 2‐tailed P value of <0.05 was deemed statistically significant.
Results
During the study period, 1993 patients met the study criteria, with mean age of 8.4±5.8 years. Among these, the presenting signs or symptoms were classified as respiratory in 611 (31%), cardiac in 561 (28%), febrile in 273 (14%), gastrointestinal in 109 (6%), and other in 439 (22%). Troponin level was first measured at the time of initial evaluation in 1693 (85%) patients and during hospital stay (>24 hours after admission) in 300 (15%).
Troponin was elevated (≥0.1 ng/mL) at presentation in 182 patients and not elevated in 1811. Cardiac testing performed in patients with and without elevated troponin level is described in Table 1. A cardiac diagnosis was made in 109 (60%) of those with elevated troponin and in 208 (12%) of those without (P<0.001; Figure). Elevated troponin was the strongest predictor of a cardiac diagnosis at discharge both on univariate and multivariable analyses (Table 2). Cardiac presentation and abnormal ECG were also independently associated with an increased risk of cardiac diagnosis at discharge, whereas respiratory and febrile presentations were associated with a lower risk of cardiac diagnosis. Although age was a significant predictor of cardiac diagnosis on univariate analysis, it did not remain significant after accounting for potential confounding variables. The PPV of initial elevated troponin for cardiac diagnosis was 60% for the entire cohort and 85% in patients with a cardiac presentation (PPV of a cardiac presentation independent of troponin level was 41%). The negative predictive value of nonelevated troponin was 89% for the entire cohort and 96% in patients without a cardiac presentation.
Table 1.
Cardiac Testing Performed in Patients With and Without Elevated Troponin Level
| Patients With Elevated Troponin Level (n=182) | Patients Without Elevated Troponin Level (n=1811) | |
|---|---|---|
| ECG, n (%) | 156 (86) | 1268 (70) |
| Echocardiogram, n (%) | 166 (91) | 554 (31) |
| Cardiac magnetic resonance, n (%) | 41 (23) | 31 (2) |
| Cardiac catheterization, n (%) | 41 (23) | 29 (2) |
Figure A.
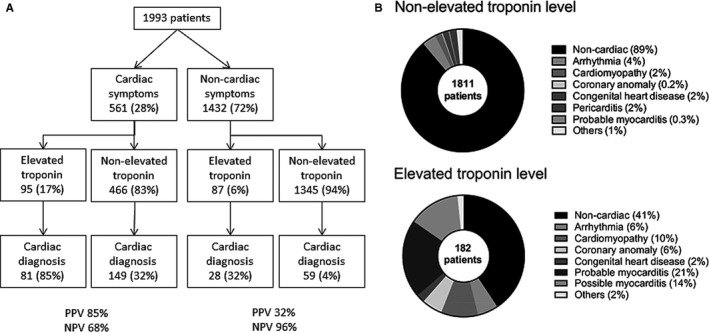
Flowchart of cardiac diagnosis based on cardiac vs noncardiac presentation and troponin level. The positive predictive value (PPV) and negative predictive value (NPV) are listed for patients with cardiac symptoms and for patients with noncardiac symptoms. B, Diagnosis at discharge in patients with and without elevated troponin.
Table 2.
Univariate and Multivariable Predictors of Cardiac Diagnosis at Discharge (n=1993; 317 Cardiac Diagnoses)
| Univariate | Multivariable | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P Value | OR | 95% CI | P Value | |
| Age (per 1‐y increase) | 1.05 | 1.03–1.07 | <0.001 | 1.01 | 0.99–1.04 | 0.30 |
| Chief complaint at presentation | ||||||
| Other | 1 | 1 | ||||
| Cardiac symptoms | 5.29 | 3.80–7.47 | <0.001 | 4.77 | 3.26–7.10 | <0.001 |
| Respiratory symptoms | 0.15 | 0.08–0.28 | <0.001 | 0.14 | 0.07–0.26 | <0.001 |
| Gastrointestinal symptoms | 0.85 | 0.41–1.64 | 0.65 | 0.85 | 0.39–1.74 | 0.67 |
| Febrile illness | 0.38 | 0.19–0.69 | 0.003 | 0.39 | 0.19–0.74 | 0.006 |
| ECG | ||||||
| Normal | 1 | 1 | ||||
| Abnormal | 3.68 | 2.82–4.83 | <0.001 | 3.79 | 2.71–5.34 | <0.001 |
| Not performed | 0.36 | 0.23–0.55 | <0.001 | 0.49 | 0.30–0.76 | 0.002 |
| Elevated troponin | 11.51 | 8.30–16.05 | <0.001 | 6.46 | 4.21–9.98 | <0.001 |
C statistic associated with the multivariable model was 0.88. OR indicates odds ratio.
Among the 561 patients with a cardiac presentation, 244 (43%) had a chief complaint of chest pain, 138 (25%) had tachycardia or other arrhythmia, 42 (7%) had syncope, 28 (5%) had cardiomegaly on chest x‐ray, 28 (5%) had ventricular dysfunction, and 81 (14%) had other presentations. Of the 244 patients with chest pain, 28 (12%) had elevated troponin, of which 27 (96%) had a cardiac diagnosis at discharge, compared with 33 (15%) of the 216 patients without elevated troponin levels (P<0.001). Cardiac diagnoses in patients with chest pain and elevated troponin included myocarditis in 25 (93%) and cardiomyopathy in 2 (7%), whereas cardiac diagnoses in patients with nonelevated troponin included pericarditis in 20 (61%), newly identified congenital heart disease in 8 (24%), arrhythmia in 3 (9%), myocarditis in 1 (3%), and cardiomyopathy in 1 (3%).
Serial troponin levels were not obtained systematically. However, among 404 patients with initially nonelevated levels who had serial measurements, subsequent elevation was found in 80 (20%). Of these, 15 (19%) had a cardiac diagnosis at discharge, including cardiomyopathy in 4, probable myocarditis in 4, arrhythmia in 3, coronary anomaly in 2, other congenital heart disease in 1, and Kawasaki disease without coronary aneurysm in 1. For the entire cohort, the predictive value of elevated troponin level at any time during hospital stay (PPV, 56%; negative predictive value, 89%) was not superior to that of the level at initial presentation (PPV, 60%; negative predictive value, 89%).
Receiver operating characteristic curve analysis identified an optimal cutoff of 0.005 ng/mL with an area under the curve of 0.71 (95% CI, 0.67–0.75) to differentiate cardiac from noncardiac disease in this pediatric cohort. With subgroup analysis by age, the optimal troponin cutoff value to differentiate cardiac from noncardiac diagnosis was higher in children aged <3 months (0.045 ng/mL) compared with children aged ≥3 months (0.005 ng/mL). Using this new age‐based cutoff value for troponin level, the C statistic of the model to differentiate cardiac from noncardiac diagnosis was 0.87 (95% CI, 0.84–0.90).
Discussion
In this retrospective study, we found that children and young adults with cardiac presentations and elevated troponin levels had high likelihood of cardiac disease, with diagnoses similar to those reported in other pediatric studies.3, 4, 5, 6 Conversely, those with a nonelevated troponin level were highly unlikely to have cardiac disease regardless of presenting signs and symptoms. Consequently, troponin can be a useful adjunctive test in pediatrics, helping to distinguish patients with and without heart disease among those presenting with chest symptoms or cardiac signs and to exclude heart disease in patients without such presentations. Moreover, troponin level remained an independent predictor of cardiac diagnosis at discharge after accounting for clinical presentation and ECG findings. This finding contrasts with the report of Liesemer et al,6 who found that troponin did not add significant diagnostic value in the absence of an abnormal ECG in children with chest pain, albeit with a different troponin assay and study cohort.6
Serial troponin measurement in pediatric patients with elevated troponin at presentation did not improve the predictive value of troponin testing. This finding contrasts with the established utility of serial troponin measurement in adult patients in whom the predominant diagnosis is coronary ischemia with evolving myocardial injury. Serial measurement in children without elevated troponin levels at presentation did appear to identify additional cases of heart disease, albeit at a lower rate, likely because of a relative selection bias against heart disease in the group with delayed but not initial elevation. It is likely that repeat testing was done because of ongoing clinical concern for cardiac involvement.
Currently, the clinical laboratory reference values for troponin assay in children are those based on the adult literature. However, reference standards validated in adult patients may not be suitable for children, in whom age‐specific thresholds may exist. Indeed, our data suggest that lower threshold values for troponin T elevation may be appropriate when evaluating children.
This study should be interpreted in light of its limitations, including those inherent in a retrospective analysis. The indications for initial and serial troponin testing and for other cardiac diagnostic testing were clinically determined, not prespecified, and probably not uniformly applied. The reason for troponin testing in patients without reported cardiac signs or symptoms was not documented. It may be assumed that features not captured in the medical record raised concern about cardiac involvement. Administrative diagnostic coding is subject to error. To minimize this, the medical record was reviewed for all patients with cardiac discharge diagnoses. Although the diagnostic performance of troponin may vary according to cardiac diagnosis, power was insufficient for such subanalysis. It was also not possible, in this retrospective study, to determine the incremental diagnostic value of troponin level over history, physical examination, and other testing.
In summary, troponin can be a useful adjunctive test in the evaluation of children when the differential diagnosis includes cardiac etiologies. Serial measurement was not helpful when the troponin was elevated at presentation but may merit consideration when the initial level is not elevated and there is ongoing concern about cardiac involvement. Lower reference values may be appropriate when evaluating children in contrast to adults.
Sources of Funding
This study was supported by the Greer Family Cardiology Research Fund and by the Boston Children's Heart Foundation.
Disclosures
None.
(J Am Heart Assoc. 2020;9:e012897 DOI: 10.1161/JAHA.119.012897.)
References
- 1. Friedman KG, Kane DA, Rathod RH, Renaud A, Farias M, Geggel R, Fulton DR, Lock JE, Saleeb SF. Management of pediatric chest pain using a standardized assessment and management plan. Pediatrics. 2011;128:239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kane DA, Friedman KG, Fulton DR, Geggel RL, Saleeb SF. Needles in Hay II: detecting cardiac pathology by pediatric chest pain standardized clinical assessment and management plan. Congenit Heart Dis. 2016;11:396–402. [DOI] [PubMed] [Google Scholar]
- 3. Brown JL, Hirsh DA, Mahle WT. Use of troponin as a screen for chest pain in the pediatric emergency department. Pediatr Cardiol. 2012;33:337–342. [DOI] [PubMed] [Google Scholar]
- 4. Thankavel PP, Mir A, Ramaciotti C. Elevated troponin levels in previously healthy children: value of diagnostic modalities and the importance of a drug screen. Cardiol Young. 2014;24:283–289. [DOI] [PubMed] [Google Scholar]
- 5. Harris TH, Gossett JG. Diagnosis and diagnostic modalities in pediatric patients with elevated troponin. Pediatr Cardiol. 2016;37:1469–1474. [DOI] [PubMed] [Google Scholar]
- 6. Liesemer K, Casper TC, Korgenski K, Menon SC. Use and misuse of serum troponin assays in pediatric practice. Am J Cardiol. 2012;110:284–289. [DOI] [PubMed] [Google Scholar]
- 7. Gore MO, Seliger SL, Defilippi CR, Nambi V, Christenson RH, Hashim IA, Hoogeveen RC, Ayers CR, Sun W, McGuire DK, Ballantyne CM, de Lemos JA. Age‐ and sex‐dependent upper reference limits for the high‐sensitivity cardiac troponin T assay. J Am Coll Cardiol. 2014;63:1441–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Monneret D, Gellerstedt M, Bonnefont‐Rousselot D. Determination of age‐ and sex‐specific 99th percentiles for high‐sensitive troponin T from patients: an analytical imprecision‐ and portioning‐based approach. Clin Chem Lab Med. 2018;56:685–696. [DOI] [PubMed] [Google Scholar]
- 9. Caseli C, Changemi G, Masotti S, Ragusa R, Gennai I, Del Ry S, Prontera C, Clerico A. Plasma cardiac troponin I concentrations in healthy neonates, children and adolescents measured with a high sensitive immunoassay method: high sensitive troponin I in pediatric age. Clin Chim Acta. 2016;458:68. [DOI] [PubMed] [Google Scholar]


