Abstract
Doxorubicin (DOX) is a cytotoxic anthracycline antibiotic and one of the important chemotherapeutic agents for different types of cancers. DOX treatment is associated with adverse effects, particularly cardiac dysfunction. This study examined the cardioprotective effects of carvedilol (CAR) and/or resveratrol (RES) and liposomal RES (LIPO-RES) against DOX-induced cardiomyopathy, pointing to their modulatory effect on oxidative stress, inflammation, S100A1 and sarco/endoplasmic reticulum calcium ATPase2a (SERCA2a). Rats received CAR (30 mg/kg) and/or RES (20 mg/kg) or LIPO-RES (20 mg/kg) for 6 weeks and were challenged with DOX (2 mg/kg) twice per week from week 2 to week 6. DOX-administered rats exhibited a significant increase in serum creatine kinase-MB (CK-MB), troponin-I and lactate dehydrogenase (LDH) along with histological alterations, reflecting cardiac cell injury. Cardiac toll-like receptor 4 (TLR-4), inducible nitric oxide synthase (iNOS), tumor necrosis factor (TNF)-α and interleukin (IL)-6 protein expression were up-regulated, and lipid peroxidation was increased in DOX-administered rats. Treatment with CAR, RES or LIPO-RES as well as their alternative combinations ameliorated all observed biochemical and histological alterations with the most potent effect exerted by CAR/LIPO-RES. All treatments increased cardiac antioxidants, and the expression of S100A1 and SERCA2a. In conclusion, the present study conferred new evidence on the protective effects of CAR and its combination with either RES or LIPO-RES on DOX-induced inflammation, oxidative stress and calcium dysregulation.
Keywords: doxorubicin, S100A1, carvedilol, phenols, oxidative stress, cardiomyopathy
1. Introduction
Doxorubicin (DOX) is a member of the anthracyclines and one of the most effective anti-cancer agents for solid tumors and leukemia [1]. The main antitumor effects of DOX are attributed to inhibition of topoisomerase II that leads to DNA damage and suppression of protein synthesis [2]. However, its use is restricted by its cardiotoxic adverse effects, including arrhythmia and cardiomyopathy which may consequently lead to congestive heart failure (CHF) [3]. Different mechanisms appear to be responsible for DOX cardiotoxicity. One of these mechanisms is the increased production of free radicals that lead to oxidative stress and lipid peroxidation [1]. Other mechanisms include the increase in intracellular iron and suppression of natural antioxidants, such as reduced glutathione (GSH). Furthermore, DOX can activate inducible nitric oxide synthase (iNOS) and NO production that can provoke cardiomyocyte apoptosis [4]. Moreover, DOX provokes apoptosis either by up-regulating the expression of p53 and caspase-3 [5] or by increasing intracellular calcium level [6]. DOX also stimulates the inflammatory process and increases the levels of tumor necrosis factor-alpha (TNF-α) [7].
Toll-like receptors (TLRs) are important for initiating the innate immune responses [8]. TLRs in the heart are expressed mainly in cardiac myocytes, smooth muscle cells and endothelial cells [9]. TLR-4 is considered to be the main member of the TLRs implicated in DOX-induced cardiomyopathy that initiates left ventricles (LV) damage [7]. Besides TLR-4, TLR-2 has been reported to play a role in regulating inflammation and apoptosis in the heart after DOX administration [10]. Activation of TLR-4 by a ligand stimulates nuclear factor-kappa B (NF-κB) transcriptional activity and the liberation of NF-κB from its inhibitor IkBα and translocation into the nucleus. Activated NF-κB promotes the production of pro-inflammatory cytokines, such as, TNF-α and interleukin (IL)-6 [11,12]. Riad et al have reported that DOX causes oxidative stress that stimulates NF-ĸB, which enhances the inflammatory pathway, and demonstrated the crucial role of the TLR-4/NF-ĸB pathway in LV dysfunction in DOX-induced cardiomyopathy [7].
S100 proteins are Ca2+ binding proteins of the EF-hand type that can be expressed in many tissues and play important functions. Various heart diseases are related to S100 proteins which are considered as new markers for cardiac toxicity [13]. S100A1 protein improves cardiac contractility and its expression is reduced following cardiac damage [14]. Human cardiomyopathy exhibited down-regulation of S100A1 expression that decreased the performance of myocardial contraction as documented by Remppis et al [15]. Additionally, Ritterhoff’s group revealed that the mRNA of S100A1 was decreased following dilated and ischemic human cardiomyopathy [16]. Reduced mRNA expression of sarcoplasmic/endoplasmic reticulum calcium ATPase2a (SERCA2a) is a characteristic feature of heart failure (HF). SERCA2a is the main protein involved in calcium reabsorption during relaxation and its low level causes a rise in diastolic calcium [17]. Brinks et al reported that gene therapy with S100A1 in cardiac cell dysfunction enhanced SERCA2a activity 2-fold [18]. During diastole, S100A1 augments SERCA2a function that reduces sarcoplasmic reticulum (SR) Ca2+ sparks and raises SR Ca2+ load leading to cardiac relaxation; while in systole, S100A1 elevates both SR Ca2+ load and ryanodine receptor 2 (RyR2) opening that mediates a high level of intracellular Ca2+ transients and supports heart contractile function [16].
Several treatments are used as cardioprotective agents against DOX-induced cardiomyopathy. β-blockers such as carvedilol (CAR) are examples of these drugs [19]. CAR possesses an antioxidant effect and inhibits oxygen radical generation, which is related to its carbazole moiety [20]. Furthermore, CAR restores calcium dysregulation by the enhancement of SERCA2a activity in myocytes [21]. The anti-inflammatory action of CAR was documented in adriamycin-induced cardiotoxicity where CAR significantly attenuated the TNF-α/NF-κB pathway and consequently cyclooxygenase 2 (COX2) and IL-6 expression [22]. However, CAR enhanced hepatic dysfunction and protected against cardiotoxicity induced by DOX as confirmed by the biochemical and histopathological examinations of the hepatic and cardiac tissues [23]. The protective effect of CAR against DOX cardiomyopathies has been reported in rodent models as well as in humans [24,25,26,27]. Given its ability to selectively block β1-adrenoceptor (AR), CAR improves heart function and is effective in the treatment of HF [28]. In contrast, the beneficial role of β2-AR blockade in patients with HF is debated [28]. Previous reports have demonstrated a moderate β1-AR selectivity and a slight β2-selectivity of CAR [29]. However, CAR can block β2-AR more selectively than β1 and accumulate in the cardiac tissue [30]. The higher selectivity towards β2-AR resulted in persistent blockade of these receptors and contributed to the beneficial effects of CAR in HF [30]. Therefore, CAR may preferentially inhibit arrhythmias and other harmful effects of adrenaline [30]. Additionally, CAR prevented tissue injury and decreased β3-AR expression in the ventricle of diabetic rats subjected to myocardial infarction [31].
Resveratrol (RES) is a small natural polyphenol product with the chemical structure 3,5,4ʹ-trihydroxystilbene [32]. RES plays a protective role against cardiovascular disease (CVD) that is documented by its action against oxidation, inflammation and thrombus aggregation [33]. Vella et al reported that RES has multiple pharmacological actions, including anti-inflammatory and antioxidant activities. Furthermore, it reduces the left ventricular remodeling and dysfunction [34]. The anti-inflammatory action of RES is mediated via inhibition of lipopolysaccharide (LPS)-TLR-4/NF-κB pathway [35,36]. RES affects many calcium signaling pathways in the cardiac cells. These pathways mediate different mechanisms that control calcium influx, release and other calcium sensitive molecules. Previous studies have reported that RES improved heart function and reduced cardiac hypertrophy, which was attributed to silent information regulator 1 (SIRT1) protein that enhanced SERCA2a expression [32,37]. Additionally, RES inhibited l-type Ca2+ channels which are the main plasma membrane targets of RES mediating low extracellular Ca2+ influx. In normal conditions, Ca2+ enters the cell by l-type Ca2+ channels which facilitates potassium ion efflux. RES indirectly causes a reduction of potassium efflux and relaxation in the endothelium. The effect of RES on potassium efflux is responsible for its effects on hypertension and arteriosclerosis reduction [37]. Although RES can prevent oxidative stress and inflammation, there is a disagreement regarding its beneficial effects on cardiovascular markers and endothelial dysfunction and in type 2 diabetes patients. The contrasting effects of RES reported in different studies could be explained in terms of different factors, including doses, administration medium and form, age, gender, health status of the intestinal microbiota and its pharmacokinetics [38]. The pharmacokinetic properties of RES are less acceptable and limit its success. RES has poor bioavailability, inadequate water solubility, is chemically unstable and rapidly metabolized in the body with a very short half-life [39]. In order to overcome these pharmacokinetic limitations, a drug delivery system using liposomes becomes an excellent option in order to provide many advantages for the enhancement of RES bioavailability. In this study, we investigated the cardioprotective effect of CAR and/or RES or liposomal (LIPO)-RES against DOX-induced cardiotoxicity with emphasis on inflammation, oxidative stress and calcium dysregulation.
2. Materials and Methods
2.1. Chemicals
RES and CAR raw powders were purchased from Sigma (St. Louis, MO, USA). DOX (Ebewe Pharma Co, Unterach Am Attersee, Austria) was obtained from a local pharmacy in Riyadh (Saudi Arabia) and marketed liposomal Trans RES® (particle size = 200 nm) was purchased from Lipolife® (Drakes Lane, Chelmsford, UK). Primary antibodies for S100A1 (ab4066), iNOS (ab15323) and GAPDH (ab9483) were purchased from Abcam® (Cambridge, MA, USA). The primary antibody for TLR-4 (NB100-56580) was obtained from Novus Biologicals® (Centennial, CO, USA). The primary antibody for horseradish peroxidase (HRP) conjugated secondary antibody (sc-516102) was obtained from Santa Cruz Biotechnology (Dallas, TX, USA). All other chemicals were of analytical grade and obtained from standard commercial sources.
2.2. Animal and Experimental Design
Adult male 8-week old albino Wistar rats weighing 150–180 g were supplied by the Animals Care Centre at the College of Pharmacy, King Saud University (Riyadh, Saudi Arabia). The rats were housed in standard cages and adapted to laboratory conditions (temperature 23 ± 2 °C with 12 h light/dark cycle) for one week prior to the experiment. They were provided food and water ad libitum. The experimental protocol was conducted according to the Research Ethics Committee at King Saud University (Ref. No: KSU-SE-18-31).
Forty-two rats were randomly allocated into seven groups (n = 6) as following:
Group I (Control): received 1% carboxy methylcellulose (CMC) as the vehicle of the drugs orally for 6 weeks and intraperitoneal (i.p.) injection of physiological saline twice/week from week 2 to week 6.
Group II (DOX): received 1% CMC orally for 6 weeks and DOX (2 mg/kg i.p.) twice/week for 5 weeks (from week 2 to 6) to produce a total cumulative dose of 20 mg/kg [40].
Group III (CAR): received CAR (30 mg/kg) orally for 6 weeks [41] and DOX as per group II.
Group IV (RES): received RES (20 mg/kg) orally for 6 weeks [42,43] and DOX as per group II.
Group V (CAR/RES): received CAR (30 mg/kg) and RES (20 mg/kg) orally for 6 weeks and DOX as per group II.
Group VI (LIPO-RES): received LIPO-RES (20 mg/kg) orally for 6 weeks and DOX as per group II.
Group VII (CAR/LIPO-RES): received CAR (30 mg/kg) and LIPO-RES (20 mg/kg) orally for 6 weeks and DOX as per group II.
CAR, RES and LIPO-RES were dissolved in 1% CMC. At the end of week 6, all rats were anesthetized, and blood was collected and centrifuged at 3000 rpm for 20 min at 4 °C to separate serum. The rats were dissected, and hearts were removed, washed and parts of the LV were fixed in 10% neutral buffered formalin whereas other parts were frozen in liquid nitrogen and stored at −80 °C.
2.3. Assay of Markers of Cardiac Injury, SERCA2a and Cytokines
Serum CK-MB and troponin-I were assayed using ELISA kits (MyBioSource, San Diego, CA, USA) and LDH was determined using a kit supplied by Randox (Crumlin, UK). To assay cardiac SERCA2a, TNF-α and IL-6, samples from the LV were homogenized (10% w/v) in cold phosphate buffered saline (PBS) with proteinase inhibitors, centrifuged and the supernatant was separated. Protein content in the supernatant was assayed using Bradford reagent [44] and SERCA2a, TNF-α and IL-6 were determined using ELISA kits (MyBioSource, San Diego, CA, USA), following the provided instructions.
2.4. Assay of Lipid Peroxidation, GSH and Superoxide Dismutase (SOD)
The levels of malondialdehyde (MDA), a marker of lipid peroxidation, and GSH were measured according to the methods of Ohkawa et al [45] and Beutler et al [46], respectively. SOD activity was assayed following the method of Marklund and Marklund [47].
2.5. Histology and Immunohistochemistry
Samples of the LV fixed in 10% neutral buffered formalin were dehydrated and embedded in paraffin wax. The blocks were cut into 5-μm sections which were subjected to deparaffinization, rehydration and staining with hematoxylin and eosin (H&E) for examination using a light microscope. To determine the expression levels of TLR-4 and iNOS, the ABC technique was used as previously described [48]. Briefly, the sections were deparaffinized, rehydrated and washed under tap water and incubated in 3% hydrogen peroxide (H2O2) for 10 min. The sections were blocked with 5% bovine serum albumin in Tris-buffered saline (TBS) and incubated with anti-TLR-4 or anti-iNOS (1:100 dilution). The sections were washed 3 times in TBS and incubated with secondary antibodies. After washing in TBS, the peroxidase activity was developed using diaminobenzidine followed by hematoxylin counter-staining. The sections were washed in water, dehydrated, cleared, mounted and examined. Quantitative analysis of TLR-4 and iNOS immunostaining was performed using ImageJ (version 1.32j, NIH, USA) and the results are expressed as percent of control.
2.6. Western Blotting
To determine the effect of DOX and CAR and/or RES and LIPO-RES on cardiac S100A1 expression, samples from the LV were homogenized in RIPA buffer with proteinase inhibitors, centrifuged and the supernatant was separated. Forty µg total protein was subjected to 12% SDS/PAGE and the separated bands were transferred to a nitrocellulose membrane. After blocking in 5% skimmed milk in TBST, the membranes were probed with anti-S100A1 overnight at 4 °C or anti-GAPDH for 1 h at room temperature. The membranes were washed with TBST and incubated with secondary antibodies and then washed. Thereafter, the membranes were developed using a Bio-Rad ECL kit, scanned, and the band intensity was determined using ImageJ (version 1.32j, NIH, USA).
2.7. Statistical Analysis
The data were expressed as mean ± standard error of the mean (SEM). The results were analyzed using one-way ANOVA followed by Tukey’s test on GraphPad 7 (GraphPad Software Inc., La Jolla, CA, USA). A p value ≤ 0.05 was considered significant.
3. Results
3.1. CAR, RES and LIPO-RES Prevent DOX-Induced Cardiac Injury
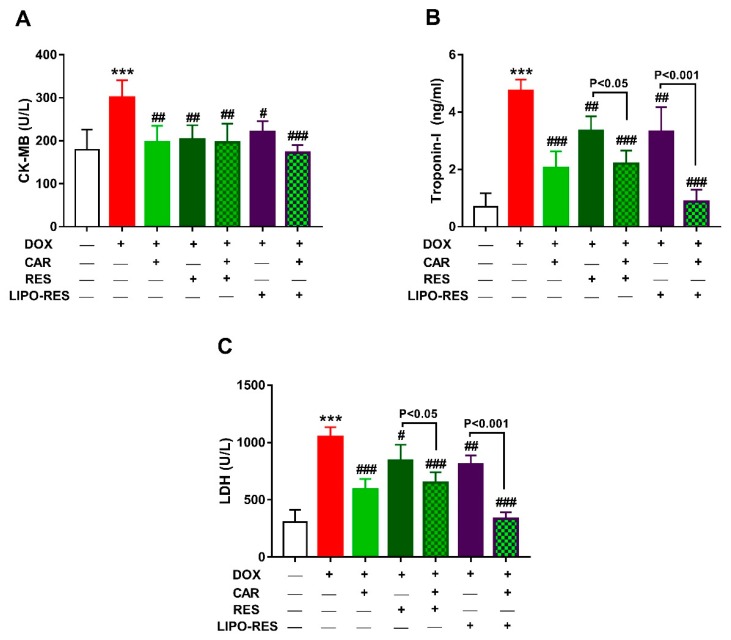
To evaluate the protective effects of CAR and/or RES and LIPO-RES on DOX cardiotoxicity, we determined serum CK-MB, troponin-I and LDH and conducted a histopathological investigation. DOX caused significant elevation of serum CK-MB (Figure 1A), troponin-I (Figure 1B) and LDH (Figure 1C). Treatment of the DOX-intoxicated rats with CAR, RES or LIPO-RES ameliorated serum troponin-I levels and CK-MB and LDH activities. Treatment with CAR/RES and CAR/LIPO-RES significantly ameliorated troponin-I and LDH when compared with RES and LIPO-RES, respectively.
Figure 1.
Carvedilol (CAR) and/or resveratrol (RES) and LIPO-RES ameliorate serum CK-MB (A), troponin-I (B) and LDH (C) in DOX-intoxicated rats. Data are expressed as mean ± SEM, (n = 6). *** p < 0.001 versus Control. # p < 0.05, ## p < 0.01 and ### p < 0.001 versus DOX.
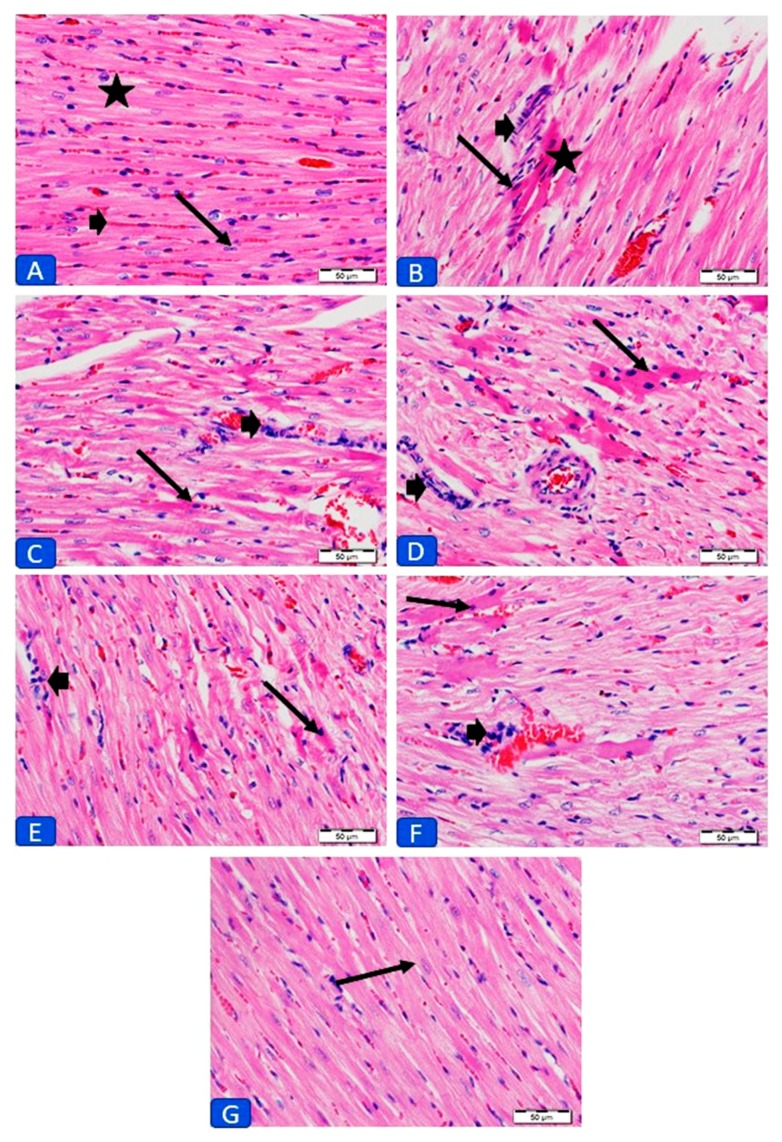
The cardiotoxic effect of DOX was further confirmed by the histopathological examination. While the control rats (Figure 2A) showed normal structure, examination of sections in the heart of DOX-intoxicated rats revealed foci of degenerated myocardium, infiltration of inflammatory cells in the endomysium, along with other manifestations (Figure 2B). Heart sections from DOX-intoxicated rats treated with CAR showed mild cell degeneration (Figure 2C), whereas foci of degenerated myocardium were seen in rats received RES (Figure 2D). Treatment with CAR/RES resulted in moderate improvement with few inflammatory cells (Figure 2E). LIPO-RES supplementation resulted in moderate decrease in degenerated myocardium cells with inflammatory cellular infiltration (Figure 2F), whereas its combination with CAR resulted in the absence of cellular degeneration and inflammatory cells, and the cardiomyocytes appear normal (Figure 2G).
Figure 2.
Photomicrographs of sections in the left ventricles (LV) of (A) control rats showing normal histology of cardiomyocyte cytoplasm (star) and nuclei (arrows) and normal distribution of endomysium (bold arrow). (B) DOX-intoxicated rats showing foci of degenerated cardiomyocytes and collection of inflammatory cells in the endomysium (bold arrow). (C) CAR-treated rats showing mild improvement of myocardium with less degeneration (arrow) and inflammatory cells (bold arrow). (D) RES-treated rats showing foci of degenerated cardiomyocytes (arrow) and few inflammatory cells (bold arrow). (E) CAR/RES- and (F) LIPO-RES-treated rats showing moderate decrease in degeneration (arrow) and inflammatory cells (bold arrow); and (G) CAR/LIPO-RES-treated rats with no degeneration or inflammatory cells and the cardiomyocytes appear normal. (× 400; H&E; scale bar: 50 µm).
3.2. CAR, RES and LIPO-RES Attenuate Cardiac Inflammation in DOX-Intoxicated Rats
Stimulation of TLR-4 has been reported to decrease cardiomyocyte contractility and provoke the activation of NF-κB-dependent inflammatory response, resulting in increased expression of TNF-α, IL-6, iNOS and other inflammatory mediators [11]. Therefore, we determined the effect of CAR and/or RES and LIPO-RES on the expression of TLR-4, TNF-α, IL-6 and iNOS in the heart of DOX-intoxicated rats.
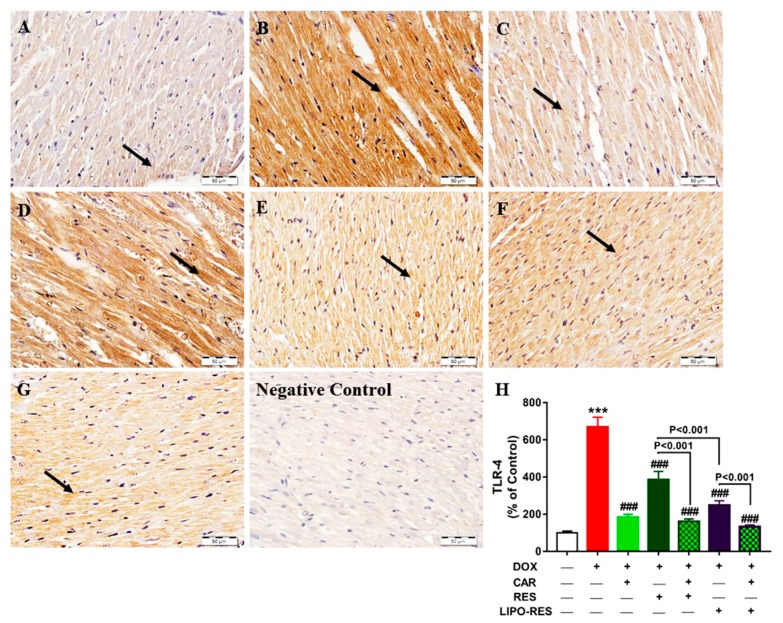
Control rats exhibited normal immune staining of TLR-4 in the myocardium as represented in Figure 3A. In contrast, the heart of DOX-intoxicated rats showed very strong immune positivity of TLR-4 in the cardiomyocytes (Figure 3B). Sections in the heart of DOX-intoxicated rats treated with CAR (Figure 3C), RES (Figure 3D) and their combination (Figure 3E) showed mild, strong positive and very mild TLR-4 expression, respectively. Oral supplementation of LIPO-RES (Figure 3F) and its combination with CAR (Figure 3G) resulted in moderate and marked decrease in TLR-4 expression, respectively.
Figure 3.
Photomicrographs of anti-TLR-4-stained LV sections in: (A) Control rats showing the absence of immune reaction in cardiomyocytes cytoplasm and nuclei (arrow); (B) DOX-intoxicated rats showing very strong immune positivity; (C) CAR-treated rats showing mild immune positive reaction; (D) RES-treated rats showing strong positive immune reaction; (E) CAR/RES-treated rats showing very mild immunostaining; (F) LIPO-RES-treated rats showing moderate immune reaction and (G) CAR/LIPO-RES-treated rats showing marked decrease in TLR-4 immune reactivity. (H) Mean ± SEM of TLR-4 immunostaining in LV sections of different groups, (n = 6). *** p < 0.001 versus Control and ### p < 0.001 versus DOX.
Quantitative analysis of TLR-4 expression revealed a significant up-regulation in DOX-intoxicated rats (p < 0.001) when compared with the control group (Figure 3H). CAR, RES and LIPO-RES decreased TLR-4 expression significantly in DOX-intoxicated rats (p < 0.001). CAR/RES and CAR-LIPO-RES reduced TLR-4 expression significantly when compared with RES and LIPO-RES, respectively. Additionally, LIPO-RES decreased TLR-4 significantly when compared with RES (Figure 3H).
Control rats exhibited normal expression of iNOS (Figure 4A) whereas DOX increased its expression markedly (Figure 4B). Sections in the heart of rats received CAR (Figure 4C), RES (Figure 4D), CAR/RES (E), LIPO-RES (Figure 4F) and CAR/LIPO-RES (Figure 4G) showed significant decrease in iNOS expression (Figure 4H). The statistical analysis showed non-significant differences between the different treatments on iNOS expression in the heart of DOX-intoxicated rats (Figure 4H).
Figure 4.
Photomicrographs of anti-iNOS-stained LV sections in: (A) Control rats showing the absence of immune reaction in cardiomyocytes cytoplasm and nuclei (arrow); (B) DOX-intoxicated rats showing multiple scattered foci of strong immune positivity; (C) CAR- (D) RES- (E) CAR/RES- and (F) LIPO-RES-treated rats showing moderate decrease in iNOS expression, and; (G) CAR/LIPO-RES-treated rats showing marked decrease in iNOS immune reactivity. (H) Mean ± SEM of iNOS immunostaining in LV sections of different groups, (n = 6). *** p < 0.001 versus Control and ### p < 0.001 versus DOX.
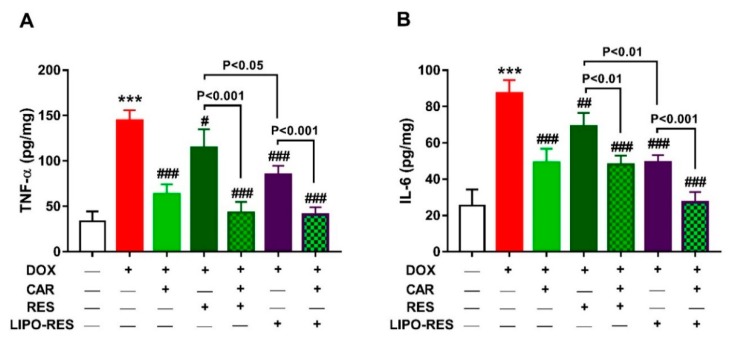
The pro-inflammatory cytokines TNF-α (Figure 5A) and IL-6 (Figure 5B) were significantly increased in the heart of rats that received DOX. CAR, RES and LIPO-RES decreased TNF-α and IL-6 significantly in DOX-intoxicated rats. LIPO-RES was more effective in reducing TNF-α (p < 0.05) and IL-6 (p < 0.01) when compared with RES. The combination of CAR with RES or LIPO-RES reduced TNF-α and IL-6 significantly when compared with the individual drugs.
Figure 5.
CAR and/or RES and LIPO-RES decrease cardiac TNF-α (A) and IL-6 (B) in DOX-intoxicated rats. Data are expressed as mean ± SEM, (n = 6). *** p < 0.001 versus Control. # p < 0.05, ## p < 0.01 and ### p < 0.001 versus DOX.
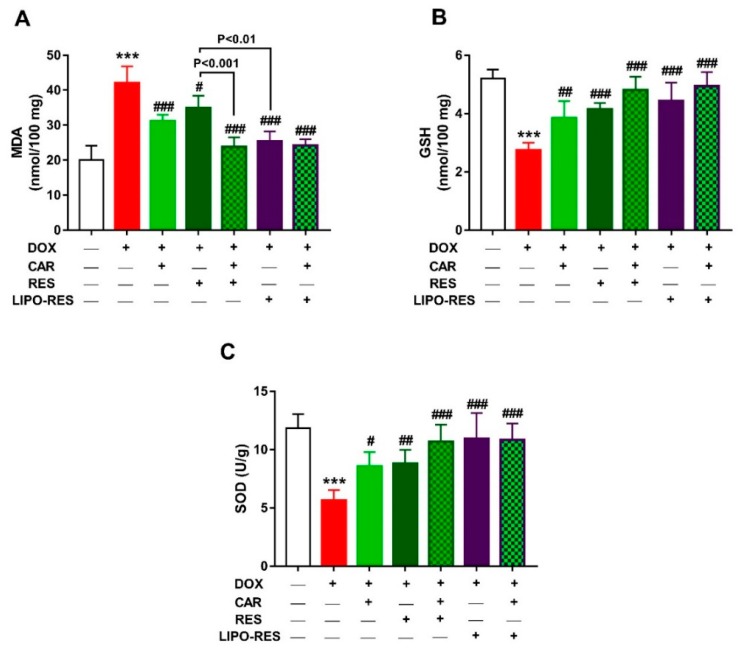
3.3. CAR, RES and LIPO-RES Prevent Oxidative Stress in the Heart of DOX-Intoxicated Rats
MDA, GSH and SOD were measured to assess the protective effect of CAR, RES and LIPO-RES on DOX-induced oxidative stress. DOX-intoxicated rats exhibited a significant increase in cardiac MDA (Figure 6A) and decreased GSH (Figure 6B) and SOD (Figure 6C). Treatment with CAR, RES and LIPO-RES markedly decreased MDA and increased antioxidants. When compared with RES, LIPO-RES and CAR/RES decreased cardiac MDA levels significantly.
Figure 6.
CAR and/or RES and LIPO-RES decrease cardiac MDA (A) and increase GSH (B) and SOD (C) in DOX-intoxicated rats. Data are expressed as mean ± SEM, (n = 6). *** p < 0.001 versus Control. # p < 0.05, ## p < 0.01 and ### p < 0.001 versus DOX.
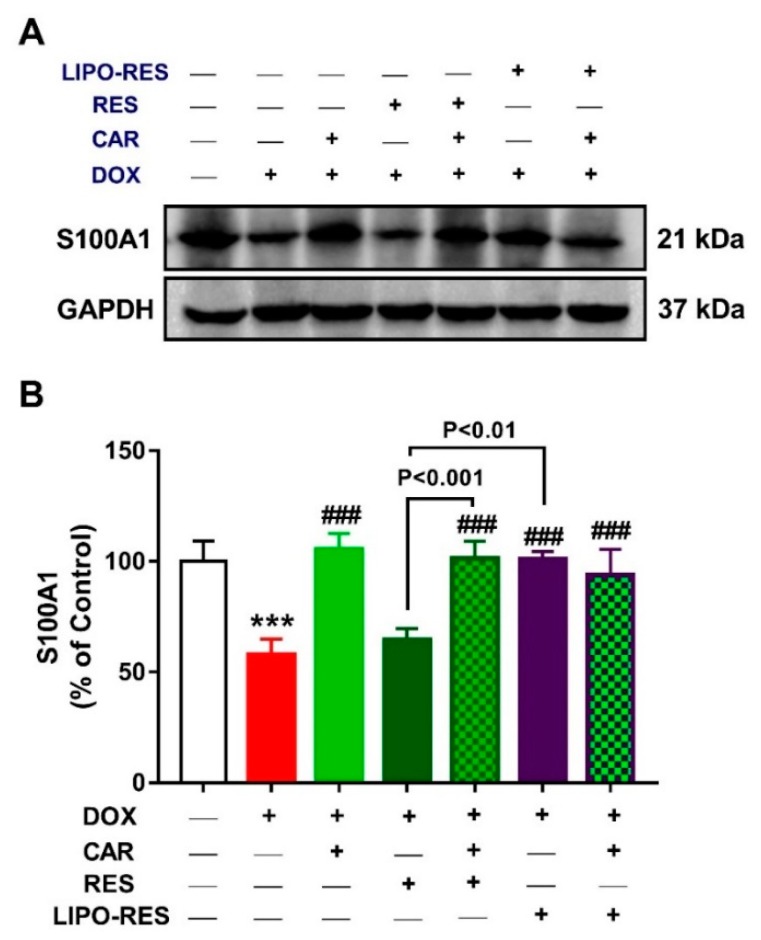
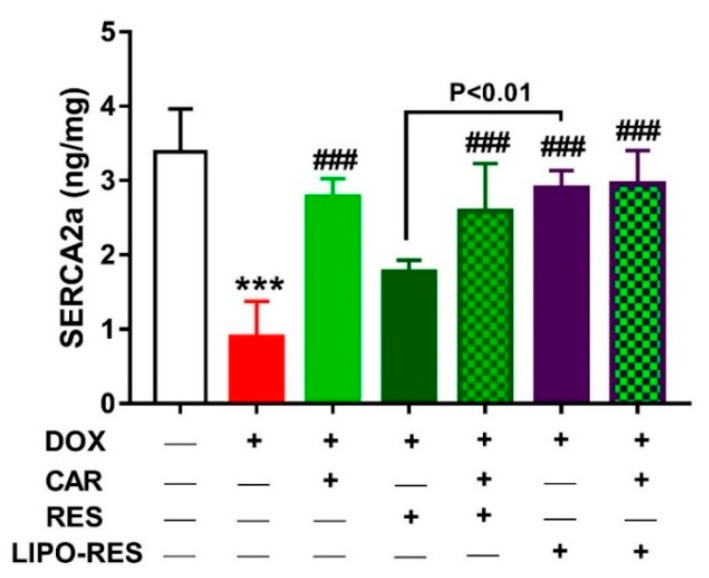
3.4. CAR, RES and LIPO-RES Upregulate Cardiac S100A1 and SERCA2a in DOX-Intoxicated Rats
Given the role of the Ca2+ binding protein S100A1 in improving Ca2+ handling and contractile performance of the cardiomyocytes via its interaction with SERCA2a RyR2 [49], we investigated the impact of DOX and the effects of CAR and/or RES and LIPO-RES on the expression levels of S100A1 (Figure 7) and SERCA2a (Figure 8). DOX suppressed S100A and SERCA2a in the heart of rats when compared with the control group (p < 0.001). Treatment with RES didn’t improve the expression of both S100A1 and SERCA2a, whereas CAR and LIPO-RES exerted a significant ameliorative effect. In addition, the combination of CAR with RES and LIPO-RES significantly improved the expression of S100A1 and SERCA2a.
Figure 7.
Effect of CAR and/or RES and LIPO-RES on cardiac S100A1. (A) Representative Western blotting of S100A1 and GAPDH. (B) CAR and/or RES and LIPO-RES up-regulated cardiac S100A1 in DOX-intoxicated rats. Data are expressed as mean ± SEM, (n = 6). *** p < 0.001 versus Control. ### p < 0.001 versus DOX.
Figure 8.
CAR and/or RES and LIPO-RES increase cardiac SERCA2a in DOX-intoxicated rats. Data are expressed as mean ± SEM, (n = 6). *** p < 0.001 versus Control. ### p < 0.001 versus DOX.
4. Discussion
DOX is a broad-spectrum antibiotic and antineoplastic agent for hematological and solid tumors. The use of DOX has been limited by the occurrence of dose-dependent toxicity to vital organs, particularly the heart [3]. Although the mechanisms of DOX-induced cardiotoxicity are not fully understood, oxidative stress, intracellular calcium dysregulation, inflammation and apoptosis of cardiomyocytes are the most proposed mechanisms [1]. The challenge for the management of its cardiotoxicity is selecting an agent that has cardioprotective effects and at the same time does not affect its antitumor activity. In this context, CAR showed some promising effects against DOX-induced cardiotoxicity [22]. RES is a polyphenol product possessing important pharmacological effects such as antioxidant- and anti-inflammatory activities [43,50]. It produced cardio-protective effects in different cardiac disorders including DOX-induced cardiomyopathy [19]. However, these treatments do not produce sufficient therapeutic effects. Therefore, there is an urgent need for novel strategies for the control DOX’s cardiac side effects. LIPO-RES is considered as one of these promising cardioprotective approaches [51]. Therefore, we aimed to explore the cardioprotective effects of RES and LIPO-RES alone and in combination with CAR in DOX-intoxicated rats, pointing to their ability to modulate oxidative stress, inflammatory response, S100A1 and SERCA2a.
Herein, the cardiotoxicity of DOX in rats was manifested by elevated serum levels of troponin-I, LDH and CK-MB, and was also confirmed by the histopathological examination, which revealed massive changes in the cardiac tissue, fragmentation and degeneration of cytoplasm and nuclei. These data were supported by previous studies where similar findings have been reported [40,52]. CAR, RES and LIPO-RES reduced the cardiotoxicity induced by DOX administration as evidenced by significant reduction of CK-MB, LDH and troponin-I levels and decreased myocardium degeneration in the histopathological findings that were in line with previous studies [40,53,54]. The combination of CAR and LIPO-RES showed significant reduction in serum LDH and troponin-I and the better enhancement in cardiac architecture that indicated improvement of cardiac injury following DOX administration versus other treated groups. However, RES treatment showed weak ameliorative effects on CK-MB, LDH and troponin-I in the DOX-administered group and this was also confirmed by the histopathological examination which indicated more degeneration of cardiac muscle versus the other treated groups.
Inflammation is one of the critical characteristics of DOX cardiotoxicity. DOX stimulates TLR-4 that consequently activates NF-κB which is necessary for cardiac apoptosis [55,56]. NF-κB is a sensitive transcription factor that controls inflammatory signaling cascades that mediate transcription of important inflammatory mediators, such as COX-2, IL6, iNOS and TNF-α [57,58]. There is a growing evidence revealing that cardiac NO level is raised in cardiotoxicity induced by DOX treatment [59]. The increase in cardiac NO level by DOX is attributed to the overexpression of iNOS that is generated through inflammation. The high levels of NO produce peroxynitrite by reacting with the free radical superoxide anion, then peroxynitrite induces cardiac oxidative damage, apoptosis and lipid peroxidation [4]. In accordance to the previously mentioned data, the present study revealed significant elevation of cardiac TNF-α, IL6 levels, TLR-4 and iNOS protein expression in the DOX-administered group. CAR, RES and LIPO-RES significantly attenuated the myocardial TNF-α level and decreased TLR-4 and iNOS protein expression. These results were in parallel with the findings of previous studies that proved the anti-inflammatory effect of CAR and RES [22,60,61]. Clearly, the combination of CAR and LIPO-RES exerted a more potent anti-inflammatory effect than each individual agent, and the combination CAR/RES showed a better effect than either drug alone on TNF-α levels and TLR-4 protein expression. Therefore, it is noteworthy assuming that CAR has synergistic effects with RES as well as LIPO-RES on TNF-α and TLR-4. Interestingly, concurrent administration of CAR and LIPO-RES exerted a superior effect matched with the other treated groups regarding to TLR-4 pathway that consequently produced low levels of the main cytokines IL-6 and TNF-α which reflect the additive anti-inflammatory effect of this combination. The present results were in line with Mahmoud et al who found that CAR administration significantly decreased iNOS that is mediated via its inhibitory effect on NF-κB expression [62]. One of the possible mechanisms of the cardioprotective effects of RES is the anti-inflammatory action that mediated by its ability to increase the expression of SIRT1 and AMPK proteins [61]. RES inhibits NF-κB inflammatory pathway through stimulating the AMPKa/SIRT1 pathway, thereby alleviating the inflammatory process [63]. SIRT1 controls the transcription of NF-κB and p53. SIRT1 inactivates NF-κB p65 subunit and causes deacetylation of NF-κB that consequently inhibits the transcription of inflammatory cytokines, including IL-6, iNOS and TNF-α [64,65]. Csiszar et al reported that TNF-α induces NF-κB activation, and RES directly attenuates the expression of TNF-α in human coronary arterial cells [66]. The current study showed that the liposomal product enhanced the anti-inflammatory action of native RES as evidenced by the significantly decreased TNF-α and IL-6 in rats received LIPO-RES.
Besides inflammation, oxidative stress has been implicated in cardiotoxicity induced by DOX [40,41]. Here, DOX administration induced oxidative stress evidenced by the significant increase in cardiac MDA levels along with abolished GSH and SOD. Accordingly, previous studies have demonstrated that DOX increases ROS generation mediated via NADPH oxidase and MDA and decreases SOD and catalase activities in the heart of rodents [40]. Excess ROS are well-acknowledged to damage cellular macromolecules, such as proteins, lipids and DNA. In this context, Tatlidede et al have shown increased DNA damage in DOX-intoxicated rats [40]. Therefore, attenuation of oxidative stress plays a role, at least in part, in the protective effects of CAR and/or RES and LIPO-RES. This notion is supported by previous studies showing the ability of CAR and RES to suppress ROS and MDA, and boost antioxidant enzymes in DOX-intoxicated rats [40,41]. Interestingly, LIPO-RES reduced MDA significantly in the heart of DOX-intoxicated rats when compared with RES. These findings support the superior cardioprotective effect of LIPO-RES.
Disturbance of calcium homeostasis is another mechanism involved in DOX-induced cardiac toxicity. Doxorubicinol, a major metabolite of DOX, alters the ability of SR to sequester calcium by interfering with SERCA2 function and stimulates the release of calcium from SR [19]. In the present work, DOX exhibited a significant reduction of SERCA2a that is similar to the results of Zhang et al, who reported that DOX decreased SERCA2a expression in rats [67]. In contrast, concomitant administration of CAR, RES and LIPO-RES significantly restored SERCA2a activity. Of note, LIPO-RES significantly restored SERCA2a when compared with RES. The present results were supported by the finding of Kalay et al, who documented that CAR enhanced SERCA2a activity and increased its gene expression [21]. The effect of CAR on SERCA2a gene transcription is mediated mainly by its effect on specificity protein 1 (Sp1) sites in the SERCA2a gene promoter region [68]. Moreover, the present study is in agreement with previous studies proving the beneficial effect of RES on SERCA2a [69,70]. RES affects SERCA2a gene expression mostly through the SIRT1 transcriptional pathway. SIRT1 function is involved in cardiac contractility via regulating SERCA2a promoter activity [71]. To further explore the ameliorative mechanism of CAR and/or RES and LIPO-RES on DOX cardiotoxicity, the expression of S100A1 was determined. This study is considered the first one that discussed the effect of DOX, CAR, RES and LIPO-RES individually as well as the alternative combinations on S100A1 protein expression. S100A1 exhibits its actions mainly in the heart but is also expressed in skeletal muscle, brain and kidneys [72]. It interacts with both SERCA2a and RyR2, which are important for Ca2+ handling and cardiac contraction. S100A1 enhances Ca2+ transient and reduces diastolic Ca2+ overload by decreasing SR Ca2+ leakage to modulate cardiac function [49]. The data of this study revealed that DOX caused down-regulation of S100A1 and that may be considered as one of the causes for the reduction of SERCA2a. Up till now, there has not been enough data to demonstrate the regulation of S100A1 protein expression. Kiewitz et al reported that SP1 elements are involved in the S100A1 promoter region [73]. Additionally, cyclic adenosine monophosphate (cAMP) responsive elements were also detected in the S100A1 gene [73,74]. Previous data showed that Sp1 was down-regulated after DOX administration, and Fatemi et al found that cAMP-stimulating agents ameliorated DOX-induced apoptosis [75]. As a result, DOX may affect S100A1 via decreasing SP1 protein level. In the present work, CAR and LIPO-RES increased S100A1 protein expression while RES showed non-significant increase versus the DOX-administered group. It was expected that CAR may affect S100A1 protein expression as mentioned previously by its effects on SP1 similar pathway to SERCA2 protein. Whereas the beneficial effect of LIPO-RES on S100A1 is suggested to be attributed to its effect on cAMP activation [76]. The beneficial effect of CAR or LIPO-RES on S100A1 may be the reason for the improvement of cardiac contractility and enhancement of the SERCA2 level.
5. Conclusions
This study is the first one that evaluated the protective effect of the combination of CAR with either RES or LIPO-RES against inflammation, oxidative stress and calcium dysregulation induced by DOX administration, as well as their effect on S100A1 protein. The present results proved that treatment of DOX-administered rats with either CAR or LIPO-RES alone or together alleviated inflammation, oxidative stress and tissue injury evidenced by biochemical and molecular as well as histopathological studies. The combination of CAR and LIPO-RES clearly exerted the best beneficial effects according to most of the previous aforementioned measured parameters. Concomitant administration of CAR in combination with LIPO-RES could be considered as a promising candidate for protection against DOX cardiotoxicity.
Acknowledgments
The authors would like to thank the Deanship of the Scientific Research at King Saud University for funding and supporting this research through the initiative of DSR Graduate Students Research Support (GSR).
Author Contributions
Conceptualization, A.A. and A.M.M.; methodology, A.M.A.; L.F.; A.A.; R.A.; I.H.H. and A.M.M.; validation, A.M.M.; I.H.H. and A.A.; formal analysis, A.M.M.; A.M.A. and I.H.H.; investigation, A.M.A.; L.F.; A.A.; R.A.; I.H. and A.M.M.; resources, A.A. and L.F.; data curation, A.M.A. and A.M.M.; writing—original draft preparation, A.M.A.; A.A.; I.H.H. and A.M.M.; writing—review and editing, A.M.M.; visualization, A.A. and A.M.M.; supervision, I.H.H. and A.A.; project administration, I.H.H. and A.A.; funding acquisition, A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Deanship of the Scientific Research at King Saud University through the initiative of DSR Graduate Students Research Support (GSR).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Octavia Y., Tocchetti C.G., Gabrielson K.L., Janssens S., Crijns H.J., Moens A.L. Doxorubicin-Induced Cardiomyopathy: From Molecular Mechanisms to Therapeutic Strategies. J. Mol. Cell. Cardiol. 2012;52:1213–1225. doi: 10.1016/j.yjmcc.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Carvalho F.S., Burgeiro A., Garcia R., Moreno A.J., Carvalho R.A., Oliveira P.J. Doxorubicin-Induced Cardiotoxicity: From Bioenergetic Failure and Cell Death to Cardiomyopathy. Med. Res. Rev. 2014;34:106–135. doi: 10.1002/med.21280. [DOI] [PubMed] [Google Scholar]
- 3.Jungsuwadee P. Doxorubicin-Induced Cardiomyopathy: An Update Beyond Oxidative Stress and Myocardial Cell Death. Cardiovasc. Regen. Med. 2016;3:1–8. [Google Scholar]
- 4.Bahadır A., Kurucu N., Kadıoğlu M., Yenilme E. The Role of Nitric Oxide in Doxorubicin-Induced Cardiotoxicity: Experimental Study. Turk. J. Hematol. 2014;31:68. doi: 10.4274/Tjh.2012.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun Y., Xia P., Zhang H., Liu B., Shi Y. P53 Is Required for Doxorubicin-Induced Apoptosis via the TGF-Beta Signaling Pathway in Osteosarcoma-Derived Cells. Am. J. Cancer Res. 2015;6:114–125. [PMC free article] [PubMed] [Google Scholar]
- 6.Tombal B., Denmeade S.R., Gillis J.M., Isaacs J.T. A Supramicromolar Elevation of Intracellular Free Calcium ([Ca (2+)] (i)) Is Consistently Required to Induce the Execution Phase of Apoptosis. Cell Death Differ. 2002;9:561–573. doi: 10.1038/sj.cdd.4400999. [DOI] [PubMed] [Google Scholar]
- 7.Riad A., Bien S., Gratz M., Escher F., Heimesaat M.M., Bereswill S., Krieg T., Felix S.B., Schultheiss H.-P., Kroemer H.K., et al. Toll-Like Receptor-4 Deficiency Attenuates Doxorubicin-Induced Cardiomyopathy in Mice. Eur. J. Hear. Fail. 2008;10:233–243. doi: 10.1016/j.ejheart.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Hasan U., Chaffois C., Gaillard C., Saulnier V., Merck E., Tancredi S., Guiet C., Brière F., Vlach J., Lebecque S., et al. Human TLR10 Is a Functional Receptor, expressed by B Cells and Plasmacytoid Dendritic Cells, which Activates Gene Transcription through MyD88. J. Immunol. 2005;174:2942–2950. doi: 10.4049/jimmunol.174.5.2942. [DOI] [PubMed] [Google Scholar]
- 9.Yang Y., Lv J., Jiang S., Ma Z., Wang D., Hu W., Deng C., Fan C., Di S., Sun Y. The Emerging Role of Toll-Like Receptor 4 in Myocardial Inflammation. Cell death Dis. 2017;7:2234–2245. doi: 10.1038/cddis.2016.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nozaki N. Modulation of Doxorubicin-Induced Cardiac Dysfunction in Toll-Like Receptor-2-Knockout Mice. Circulation. 2004;110:2869–2874. doi: 10.1161/01.CIR.0000146889.46519.27. [DOI] [PubMed] [Google Scholar]
- 11.Boyd J.H., Mathur S., Wang Y., Bateman R.M., Walley K.R. Toll-Like Receptor Stimulation in Cardiomyoctes Decreases Contractility and Initiates an NF-κB Dependent Inflammatory Response. Cardiovasc. Res. 2006;72:384–393. doi: 10.1016/j.cardiores.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 12.Takeuchi O., Akira S. Pattern Recognition Receptors and Inflammation. Cell. 2010;140:805–820. doi: 10.1016/j.cell.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 13.Wang X.-J., Wang M. The S100 Protein Family and Its Application in Cardiac Diseases. World J. Emerg. Med. 2010;1:165–168. [PMC free article] [PubMed] [Google Scholar]
- 14.Eryilmaz U., Demirci B., Aksun S., Boyacioglu M., Akgullu C., Ilgenli T.F., Yalinkilinc H.S., Bilgen M. S100a1 as a Potential Diagnostic Biomarker for Assessing Cardiotoxicity and Implications for the Chemotherapy of Certain Cancers. PLoS ONE. 2015;10:418–445. doi: 10.1371/journal.pone.0145418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Remppis A., Greten T., Schäfer B.W., Hunziker P., Erne P., Katus H.A., Heizmann C.W. Altered Expression of the Ca2+-Binding Protein s100a1 in Human Cardiomyopathy. Biochim. Biophys. Acta. 1996;1313:253–257. doi: 10.1016/0167-4889(96)00097-3. [DOI] [PubMed] [Google Scholar]
- 16.Ritterhoff J., Most P. Targeting S100A1 in Heart Failure. Gene Ther. 2012;19:613–621. doi: 10.1038/gt.2012.8. [DOI] [PubMed] [Google Scholar]
- 17.Duarte-Costa S., Castro-Ferreira R., Neves J.S., Leite-Moreira A.F. S100A1: A Major Player in Cardiovascular Performance. Physiol. Res. 2014;63:669–681. doi: 10.33549/physiolres.932712. [DOI] [PubMed] [Google Scholar]
- 18.Brinks H., Rohde D., Voelkers M., Qiu G., Pleger S.T., Herzog N., Rabinowitz J., Ruhparwar A., Silvestry S., Lerchenmüller C., et al. S100A1 Genetically Targeted Therapy Reverses Dysfunction of Human Failing Cardiomyocytes. J. Am. Coll. Cardiol. 2011;58:966–973. doi: 10.1016/j.jacc.2011.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mitry M.A., Edwards J. Doxorubicin Induced Heart Failure: Phenotype and Molecular Mechanisms. IJC Hear. Vasc. 2016;10:17–24. doi: 10.1016/j.ijcha.2015.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jhorawat R., Kumari S., Varma S.C., Rohit M.K., Narula N., Suri V., Malhotra P., Jain S. Preventive Role of Carvedilol in Adriamycin-Induced Cardiomyopathy. Indian J. Med. Res. 2016;144:725–729. doi: 10.4103/ijmr.IJMR_1323_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalay N., Başar E., Ozdogru I., Er O., Cetinkaya Y., Dogan A., Oguzhan A., Eryol N.K., Topsakal R., Ergin A., et al. Protective Effects of Carvedilol Against Anthracycline-Induced Cardiomyopathy. J. Am. Coll. Cardiol. 2006;48:2258–2262. doi: 10.1016/j.jacc.2006.07.052. [DOI] [PubMed] [Google Scholar]
- 22.Sari F.R., Arozal W., Watanabe K., Harima M., Veeravedu P.T., Thandavarayan R.A., Suzuki K., Arumugam S., Soetikno V., Kodama M. Carvedilol Attenuates Inflammatory-Mediated Cardiotoxicity in Daunorubicin-Induced Rats. Pharmaceuticals. 2011;4:551–566. doi: 10.3390/ph4030551. [DOI] [Google Scholar]
- 23.Ibrahim S.S., Barakat M.A., Helmy H.S. Modulating Effect of Carvedilol on Doxorubicininduced Cardiomyopathy and Hepatic Damage. J. Am. Sci. 2010;6:20–32. [Google Scholar]
- 24.Fazio S., A Palmieri E., Ferravante B., Bonè F., Biondi B., Saccà L. Doxorubicin-Induced Cardiomyopathy Treated with Carvedilol. Clin. Cardiol. 1998;21:777–779. doi: 10.1002/clc.4960211017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matsui H., Morishima I., Numaguchi Y., Toki Y., Okumura K., Hayakawa T. Protective Effects of Carvedilol against Doxorubicin-Induced Cardiomyopathy in Rats. Life Sci. 1999;65:1265–1274. doi: 10.1016/S0024-3205(99)00362-8. [DOI] [PubMed] [Google Scholar]
- 26.Chen Y.-L., Chung S.-Y., Chai H.-T., Chen C.-H., Liu C.-F., Chen Y.-L., Huang T.-H., Zhen Y.-Y., Sung P.-H., Sun C.-K., et al. Early Administration of Carvedilol Protected against Doxorubicin-Induced Cardiomyopathy. J. Pharmacol. Exp. Ther. 2015;355:516–527. doi: 10.1124/jpet.115.225375. [DOI] [PubMed] [Google Scholar]
- 27.Beheshti A.T., Toroghi H.M., Hosseini G., Zarifian A., Fazlinezhad A., Shandiz F.H. Carvedilol Administration Can Prevent Doxorubicin-Induced Cardiotoxicity: A Double-Blind Randomized Trial. Cardiology. 2016;134:47–53. doi: 10.1159/000442722. [DOI] [PubMed] [Google Scholar]
- 28.A Poole-Wilson P., Swedberg K., Cleland J.G.F., Di Lenarda A., Hanrath P., Komajda M., Lubsen J., Lutiger B., Metra M., Remme W.J., et al. Comparison of Carvedilol and Metoprolol on Clinical Outcomes in Patients with Chronic Heart Failure in the Carvedilol or Metoprolol European Trial (COMET): Randomised Controlled Trial. Lancet. 2003;362:7–13. doi: 10.1016/S0140-6736(03)13800-7. [DOI] [PubMed] [Google Scholar]
- 29.Baker J.G. The Selectivity of Beta-Adrenoceptor Antagonists at the Human Beta1, Beta2 and Beta3 Adrenoceptors. Br. J. Pharmacol. 2005;144:317–322. doi: 10.1038/sj.bjp.0706048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molenaar P., Christ T., Ravens U., Kaumann A. Carvedilol Blocks β2- more than β1-Adrenoceptors in Human Heart. Cardiovasc. Res. 2006;69:128–139. doi: 10.1016/j.cardiores.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 31.Zhang R., Kang X., Wang Y., Wang F., Yu P., Shen J., Fu L. Effects of Carvedilol on Ventricular Remodeling and the Expression of Beta3-Adrenergic Receptor in a Diabetic Rat Model Subjected Myocardial Infarction. Int. J. Cardiol. 2016;222:178–184. doi: 10.1016/j.ijcard.2016.07.188. [DOI] [PubMed] [Google Scholar]
- 32.Raj P., Louis X.L., Thandapilly S.J., Movahed A., Zieroth S., Netticadan T. Potential of Resveratrol in the Treatment of Heart Failure. Life Sci. 2014;95:63–71. doi: 10.1016/j.lfs.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 33.Bonnefont-Rousselot D. Resveratrol and Cardiovascular Diseases. Nutrients. 2016;8:250. doi: 10.3390/nu8050250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vella R.K., Pullen C., Coulson F.R., Fenning A.S. Resveratrol Prevents Cardiovascular Complications in the SHR/STZ Rat by Reductions in Oxidative Stress and Inflammation. BioMed Res. Int. 2015;2015:1–8. doi: 10.1155/2015/918123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li J., Xie C., Zhuang J., Li H., Yao Y., Shao C., Wang H. Resveratrol Attenuates Inflammation in the Rat Heart Subjected to Ischemia-Reperfusion: Role of the TLR4/NF-κB Signaling Pathway. Mol. Med. Rep. 2015;11:1120–1126. doi: 10.3892/mmr.2014.2955. [DOI] [PubMed] [Google Scholar]
- 36.Wang G., Hu Z., Fu Q., Song X., Cui Q., Jia R., Zou Y., He C., Li L., Yin Z. Resveratrol Mitigates Lipopolysaccharide-Mediated Acute Inflammation in Rats by Inhibiting the TLR4/NF-κBp65/MAPKs Signaling Cascade. Sci. Rep. 2017;7:45006–45019. doi: 10.1038/srep45006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang H., Yang Y.J., Qian H.Y., Zhang Q., Xu H., Li J.J. Resveratrol in Cardiovascular Disease: What Is Known from Current Research? Heart Fail. Rev. 2012;17:437–448. doi: 10.1007/s10741-011-9260-4. [DOI] [PubMed] [Google Scholar]
- 38.Ramírez-Garza S.L., Laveriano-Santos E.P., Marhuenda-Muñoz M., Storniolo C.E., Tresserra-Rimbau A., Vallverdú-Queralt A., Lamuela-Raventós R.M. Health Effects of Resveratrol: Results from Human Intervention Trials. Nutrients. 2018;10:1892. doi: 10.3390/nu10121892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reis S., Neves A.R., Lúcio M., Martins S., Lima J. Novel Resveratrol Nanodelivery Systems Based on Lipid Nanoparticles to Enhance Its Oral Bioavailability. Int. J. Nanomed. 2013;8:177–187. doi: 10.2147/IJN.S37840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tatlidede E., Şehirli Ö., Velioğlu-Öğünç A., Çetinel Ş., Yeğen B.Ç., Yarat A., Suleymanoglu S., Şener G., Yeǧ B.Ç. Resveratrol Treatment Protects against Doxorubicin-Induced Cardiotoxicity by Alleviating Oxidative Damage. Free. Radic. Res. 2009;43:195–205. doi: 10.1080/10715760802673008. [DOI] [PubMed] [Google Scholar]
- 41.Arozal W., Watanabe K., Veeraveedu P.T., Vijayakumar S., Thandavarayan R.A., Sukumaran V., Suzuki K., Kodama M., Aizawa Y. Protective Effect of Carvedilol on Daunorubicin-Induced Cardiotoxicity and Nephrotoxicity in Rats. Toxicology. 2010;274:18–26. doi: 10.1016/j.tox.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 42.Arafa M.H., Mohammad N.S., Atteia H.H., Abd-Elaziz H.R. Protective Effect of Resveratrol against Doxorubicin-Induced Cardiac Toxicity and Fibrosis in Male Experimental Rats. J. Physiol. Biochem. 2014;70:701–711. doi: 10.1007/s13105-014-0339-y. [DOI] [PubMed] [Google Scholar]
- 43.Shoukry H.S., Ammar H.I., Rashed L.A., Zikri M.B., Shamaa A.A., Elfadl S.G.A., Rub E.A.-A., Saravanan S., Dhingra S. Prophylactic Supplementation of Resveratrol is more Effective than Its Therapeutic Use against Doxorubicin Induced Cardiotoxicity. PLOS ONE. 2017;12:e0181535. doi: 10.1371/journal.pone.0181535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bradford M.M. A Rapid and Sensitive Method for the Quantitation of Microgram Quantities of Protein Utilizing the Principle of Protein-Dye Binding. Anal. Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 45.Ohkawa H., Ohishi N., Yagi K. Assay for Lipid Peroxides in Animal Tissues by Thiobarbituric Acid Reaction. Anal. Biochem. 1979;95:351–358. doi: 10.1016/0003-2697(79)90738-3. [DOI] [PubMed] [Google Scholar]
- 46.Beutler E., Duron O., Kelly B.M. Improved Method for the Determination of Blood Glutathione. J. Lab. Clin. Med. 1963;61:882–888. [PubMed] [Google Scholar]
- 47.Marklund S., Marklund G. Involvement of the Superoxide Anion Radical in the Autoxidation of Pyrogallol and a Convenient Assay for Superoxide Dismutase. JBIC J. Boil. Inorg. Chem. 1974;47:469–474. doi: 10.1111/j.1432-1033.1974.tb03714.x. [DOI] [PubMed] [Google Scholar]
- 48.Hsu S., Raine L., Fanger H. Use of Biotin-Avidin-Peroxidase Conplex (abc) in Immunoperoxidase Techniques: A Comparison between abc and Unlabeled Antibody Techniques. Am. J. Clin. Pathol. 1981;75:816–821. doi: 10.1093/ajcp/75.6.816. [DOI] [PubMed] [Google Scholar]
- 49.Völkers M., Rohde D., Goodman C., Most P. S100a1: A Regulator of Striated Muscle Sarcoplasmic Reticulum Ca2+ Handling, Sarcomeric, and Mitochondrial Function. J. Biomed. Biotechnol. 2010;2010:1–10. doi: 10.1155/2010/178614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hua M., Shan J., Li J., Zhang Y., Lin X.L. Resveratrol Inhibits Doxorubicin-Induced Cardiotoxicity via Sirtuin 1 Activation in h9c2 Cardiomyocytes. Exp. Ther. Med. 2016;12:1113–1118. doi: 10.3892/etm.2016.3437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Franco Y.L., Vaidya T.R., Ait-Oudhia S. Anticancer and Cardio-Protective Effects of Liposomal Doxorubicin in the Treatment of Breast Cancer. Breast Cancer: Targets Ther. 2018;10:131–141. doi: 10.2147/BCTT.S170239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shaker R.A., Abboud S.H., Assad H.C., Hadi N. Enoxaparin Attenuates Doxorubicin Induced Cardiotoxicity in Rats via Interfering with Oxidative Stress, Inflammation and Apoptosis. BMC Pharmacol. Toxicol. 2018;19:3. doi: 10.1186/s40360-017-0184-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Qarakhanlou B., Ebrahimi Kalan A., Tofighi A. Effect of Resveratrol and Aerobic Exercise on Some Cardiovascular Risk Factors in Rats with Acute Myocardial Infarction. Surgut State Univ. J. 2017;25:501–511. [Google Scholar]
- 54.Moloudi A., Sabzi F., Rashidi S. Suppression of Myocardial Injury Markers following Percutaneous Coronary Interventions by Pre-Treatment with Carvedilol. Int. Cardivascular Res. J. 2012;6:88–91. [PMC free article] [PubMed] [Google Scholar]
- 55.Shi Y., Moon M., Dawood S., McManus B., Liu P. Mechanisms and Management of Doxorubicin Cardiotoxicity. Herz. 2011;36:296–305. doi: 10.1007/s00059-011-3470-3. [DOI] [PubMed] [Google Scholar]
- 56.Valen G., Yan Z.-Q., Hansson G.K. Nuclear Factor Kappa-B and the Heart. J. Am. Coll. Cardiol. 2001;38:307–314. doi: 10.1016/S0735-1097(01)01377-8. [DOI] [PubMed] [Google Scholar]
- 57.Vyas D., Laput G., Vyas A.K. Chemotherapy-Enhanced Inflammation May Lead to the Failure of Therapy and Metastasis. OncoTargets Ther. 2014;7:1015–1023. doi: 10.2147/OTT.S60114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bartekova M., Radosinska J., Jelemensky M., Dhalla N.S. Role of Cytokines and Inflammation in Heart Function during Health and Disease. Hear. Fail. Rev. 2018;23:733–758. doi: 10.1007/s10741-018-9716-x. [DOI] [PubMed] [Google Scholar]
- 59.Sayed-Ahmed M.M., Khattab M.M., Gad M., Osman A.-M.M. Increased Plasma Endothelin-1 and Cardiac Nitric Oxide during Doxorubicin-Induced Cardiomyopathy. Pharmacol. Toxicol. 2001;89:140–144. doi: 10.1034/j.1600-0773.2001.d01-148.x. [DOI] [PubMed] [Google Scholar]
- 60.Wong V.Y., Laping N.J., Nelson A.H., Contino L.C., A Olson B., Gygielko E., Campbell W.G., Barone F., Brooks D.P. Renoprotective Effects of Carvedilol in Hypertensive-Stroke Prone Rats May Involve Inhibition of TGFβ Expression. Br. J. Pharmacol. 2001;134:977–984. doi: 10.1038/sj.bjp.0704329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Coutinho D.D.S., Pacheco M.T., Frozza R.L., Bernardi A. Anti-Inflammatory Effects of Resveratrol: Mechanistic Insights. Int. J. Mol. Sci. 2018;19:1812. doi: 10.3390/ijms19061812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mahmoud H.M., Abo-Youssef A.M., Abo-Saif A.A. Protective Effect of Carvedilol on Paracetamol-induced Hepatotoxicity; Role of Modulation Inflammation and Lipid Peroxidation. Int. J. Pharmacol. 2017;13:33–43. doi: 10.3923/ijp.2017.33.43. [DOI] [Google Scholar]
- 63.Tian Y., Ma J., Wang W., Zhang L., Xu J., Wang K., Li D. Resveratrol Supplement Inhibited the NF-κB Inflammation Pathway through Activating Ampkα-sirt1 Pathway in Mice with Fatty Liver. Mol. Cell. Biochem. 2016;422:75–84. doi: 10.1007/s11010-016-2807-x. [DOI] [PubMed] [Google Scholar]
- 64.Quivy V., Van Lint C. Regulation at Multiple Levels of NF-κB-Mediated Transactivation by protein acetylation. Biochem. Pharmacol. 2004;68:1221–1229. doi: 10.1016/j.bcp.2004.05.039. [DOI] [PubMed] [Google Scholar]
- 65.Zhu X., Liu Q., Wang M., Liang M., Yang X., Xu X., Zou H., Qiu J. Activation of Sirt1 by Resveratrol Inhibits TNF-α Induced Inflammation in Fibroblasts. PLoS ONE. 2011;6:e27081. doi: 10.1371/journal.pone.0027081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Csiszar A., Smith K., Labinskyy N., Orosz Z., Rivera A., Ungvari Z. Resveratrol Attenuates TNF-α-Induced Activation of Coronary Arterial Endothelial Cells: Role of NF-κB inhibition. Am. J. Physiol. Heart Circ. Physiol. 2006;291:1694–1699. doi: 10.1152/ajpheart.00340.2006. [DOI] [PubMed] [Google Scholar]
- 67.Zhang Y., Chen Y., Zhang M., Tang Y., Xie Y., Huang X., Li Y. Doxorubicin Induces Sarcoplasmic Reticulum Calcium Regulation Dysfunction via the Decrease of SERCA2 and Phospholamban Expressions in Rats. Cell Biochem. Biophys. 2014;70:1791–1798. doi: 10.1007/s12013-014-0130-2. [DOI] [PubMed] [Google Scholar]
- 68.Koitabashi N., Arai M., Tomaru K., Takizawa T., Watanabe A., Niwano K., Yokoyama T., Wuytack F., Periasamy M., Nagai R. Carvedilol Effectively Blocks Oxidative Stress-Mediated Downregulation of Sarcoplasmic Reticulum Ca2+-Atpase 2 Gene Transcription through Modification of sp1 Binding. Biochem. Biophys. Res. Commun. 2005;328:116–124. doi: 10.1016/j.bbrc.2004.12.139. [DOI] [PubMed] [Google Scholar]
- 69.Dong Q., Wu Z., Li X., Yan J., Zhao L., Yang C., Lu J., Deng J., Chen M. Resveratrol Ameliorates Cardiac Dysfunction Induced by Pressure Overload in Rats via Structural Protection and Modulation of Ca2+ Cycling Proteins. J. Transl. Med. 2014;12:323–334. doi: 10.1186/s12967-014-0323-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sung M.M., Dyck J.R. Therapeutic Potential of Resveratrol in Heart Failure. Ann. New York Acad. Sci. 2015;1348:32–45. doi: 10.1111/nyas.12839. [DOI] [PubMed] [Google Scholar]
- 71.Sulaiman M., Matta M.J., Sunderesan N.R., Gupta M.P., Periasamy M. Resveratrol, an Activator of SIRT1, Upregulates Sarcoplasmic Calcium ATPase and Improves Cardiac Function in Diabetic Cardiomyopathy. Am. J. Physiol. Circ. Physiol. 2009;298:H833–H843. doi: 10.1152/ajpheart.00418.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kraus C., Rohde D., Weidenhammer C., Qiu G., Pleger S.T., Voelkers M., Boerries M., Remppis A., Katus H.A., Most P. S100A1 in Cardiovascular Health and Disease: Closing the Gap between Basic Science and Clinical Therapy. J. Mol. Cell. Cardiol. 2009;47:445–455. doi: 10.1016/j.yjmcc.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kiewitz R., Lyons G.E., Schäfer B.W., Heizmann C.W. Transcriptional Regulation of S100A1 and Expression during Mouse Heart Development. Biochim. Biophys. Acta. 2000;1498:207–219. doi: 10.1016/S0167-4889(00)00097-5. [DOI] [PubMed] [Google Scholar]
- 74.Song W., Zimmer D.B. Expression of the Rat S100A1 Gene in Neurons, Glia, and Skeletal Muscle. Brain Res. 1996;721:204–216. doi: 10.1016/0006-8993(96)00172-2. [DOI] [PubMed] [Google Scholar]
- 75.Fatemi A., Kazemi A., Kashiri M., Safa M. Elevation of cAMP Levels Inhibits Doxorubicin-Induced Apoptosis in Pre-B ALL NALM- 6 Cells Through Induction of BAD Phosphorylation and Inhibition of P53 Accumulation. Int. J. Mol. Cell. Med. 2015;4:94–102. [PMC free article] [PubMed] [Google Scholar]
- 76.El-Mowafy A., Alkhalaf M. Resveratrol Activates Adenylyl-Cyclase in Human Breast Cancer Cells: A Novel, Estrogen Receptor-Independent Cytostatic Mechanism. Carcinogenesis. 2003;24:869–873. doi: 10.1093/carcin/bgg015. [DOI] [PubMed] [Google Scholar]