Abstract
Aims
We examined the extent to which associations between education and cardiovascular disease (CVD) morbidity and mortality are attributable to income and work stress.
Methods and results
We included all employed Danish residents aged 30–59 years in 2000. Cardiovascular disease morbidity analyses included 1 638 270 individuals, free of cardiometabolic disease (CVD or diabetes). Mortality analyses included 41 944 individuals with cardiometabolic disease. We assessed education and income annually from population registers and work stress, defined as job strain, with a job-exposure matrix. Outcomes were ascertained until 2014 from health registers and risk was estimated using Cox regression. During 10 957 399 (men) and 10 776 516 person-years (women), we identified 51 585 and 24 075 incident CVD cases, respectively. For men with low education, risk of CVD was 1.62 [95% confidence interval (CI) 1.58–1.66] before and 1.46 (95% CI 1.42–1.50) after adjustment for income and job strain (25% reduction). In women, estimates were 1.66 (95% CI 1.61–1.72) and 1.53 (95% CI 1.47–1.58) (21% reduction). Of individuals with cardiometabolic disease, 1736 men (362 234 person-years) and 341 women (179 402 person-years) died from CVD. Education predicted CVD mortality in both sexes. Estimates were reduced with 54% (men) and 33% (women) after adjustment for income and job strain.
Conclusion
Low education predicted incident CVD in initially healthy individuals and CVD mortality in individuals with prevalent cardiometabolic disease. In men with cardiometabolic disease, income and job strain explained half of the higher CVD mortality in the low education group. In healthy men and in women regardless of cardiometabolic disease, these factors explained 21–33% of the higher CVD morbidity and mortality.
Keywords: Nationwide study, Universal coverage, Social determinants, Mechanisms, Cardiovascular disease, Cardiovascular mortality
See page 1179 for the editorial comment on this article (doi: 10.1093/eurheartj/ehaa134)
Introduction
Despite declines in age-adjusted mortality rates, cardiovascular disease (CVD) remains the leading cause of death worldwide. For the year 2016, the Global Burden of Disease Collaborators estimated that 17.6 million deaths were due to CVD, including 9.5 million due to coronary heart disease (CHD) and 5.5 million due to cerebrovascular disease (CBD).1
The major modifiable risk factors for CVD are hypertension, dyslipidaemia, diabetes mellitus, obesity, and smoking.2 Low socioeconomic position and, particularly low educational attainment is a further important risk factor for CVD.3–6 A recent meta-analysis of 72 cohort studies from the USA, Europe, and Asia reported a pooled relative risk of 1.50 [95% confidence interval (CI) 1.17–1.92] for incident CVD events in individuals with low compared to high education.3 Further, studies have shown that low education is associated with a poorer prognosis of CVD.4,5 While more CVD hazardous health-related behaviours in individuals with low education may explain part of this higher risk,6 material and psychosocial pathways have also been suggested as mechanisms. One hypothesis is that individuals with low education are more often selected into jobs of low income and a high level of work stress. These two factors, according to meta-analyses of cohort studies, are associated with higher risk of CVD.3,7,8
However, to our knowledge, no large-scale studies have examined the extent to which the association between low education and risk of CVD morbidity and mortality is attributable to low income, work stress, or the combination of low income and work stress. If it could be demonstrated that low income and work stress explain a substantial part of the low education CVD association, then interventions on low income and work stress may be considered as public health strategies for reducing the social inequality in CVD. Therefore, we quantified the extent to which the association between low education and CVD morbidity and mortality is attributable to low income and work stress in all employed individuals, aged 30–59 years, residing in Denmark in the year 2000. Using information from the comprehensive nationwide Danish registers, we ascertained education and income with individual-level data from registers and measured job strain, the most widely tested conceptualization of a work-related stressor,9 with a job-exposure matrix. To account for changes in exposure, we updated information on exposure annually from 2000 to 2009.
We hypothesized that low education predicts incident CVD among initially healthy individuals and CVD mortality among individuals with prevalent cardiometabolic disease, defined as prevalence of CHD, CBD, or diabetes at baseline.7 We further hypothesized that income and job strain partly explain the associations. We had no a priori assumption to what extent income and job strain would explain the associations and also no assumption whether income or job strain would explain a larger proportion of the associations.
Methods
Study design and population
We used data from the JEMPAD (Job Exposure Matrix Analyses of Psychosocial Factors and Healthy Ageing in Denmark) cohort, a nationwide cohort with information on employment, psychosocial factors at work, health, and socio-demographics. The study population was drawn from the ‘Integrated Database for Labour Market Research’ by Statistics Denmark.10 We included all employed individuals residing in Denmark in the year 2000, 30–59 years old with complete data on age, sex, and migration background, a total of 1 680 214 individuals. Using the unique Danish civil registration number, we linked these individuals and their information from the Integrated Database for Labour Market Research to other population-based registers providing information on socio-demographics, health services use, diagnoses for in- and out-patient hospital treatment, and causes of death. All data linkages and analyses were performed at a protected research server environment hosted by Statistics Denmark, conducted by researchers approved by Statistics Denmark. At baseline, we identified 1 638 270 individuals free of diagnosed cardiometabolic disease and 41 944 individuals with a diagnosed cardiometabolic disease.
We ascertained education, income, and covariates with individual-level data and job strain with a job-exposure matrix. All variables were assessed at baseline (year 2000) and annually updated until the end of 2009, when the job-exposure matrix for job strain could no longer be applied due to changes in the Danish job title registration system. After 2009, all variables were kept as time-invariant with their 2009 values. Outcomes were ascertained in nationwide registers from 1 January 2001 to 31 December 2014.
Education
We retrieved information on the highest completed education from the Danish education register.11 Using the International Standard Classification of Education (ISCED),12 we categorized participants in groups of (i) low (primary and lower secondary, ISCED level 0-2), (ii) medium (upper secondary and post-secondary, ISCED level 3-4), and (iii) high education (first and second stage tertiary, ISCED level 5 or higher).
Income
We ascertained annual disposable household income (after tax) by information from registers on personal income and transfer payments.13 We categorized income into low, medium, and high based on tertiles of the distribution within each year.
Job strain
We ascertained job strain with a job-exposure matrix based on information from the Danish Work Environment Cohort Study (DWECS).14,15 We measured psychological demands at work and job control and defined job strain as scoring above the median for demands and below the median for job control in DWECS. Using multilevel modelling, we constructed job exposure matrices from DWECS data as the predicted probability of job strain given job group [coded according to DISCO-88, the Danish version of the International Standard Classification of Occupations (ISCO)-88 system], sex, age, and year of data collection (2000, 2005) and assigned these predicted probabilities to the individuals of the JEMPAD cohort. We categorized individuals into groups with low, medium, and high job strain risk based on tertile split of the distribution within each year. Individuals not employed, for example due to unemployment or retirement, were assigned to a separate category of ‘Not applicable (NA) job strain’ during years outside employment. See Supplementary material online, e-Appendix 1, for a more detailed description of DWECS and the construction of the job-exposure matrix, including the wording of the psychological demands and job control items (Supplementary material online, Table S1).
Prevalent cardiometabolic disease
Prevalent cardiometabolic disease was defined as diagnoses of either CHD, CBD, or diabetes from 1977 (when information first became available in Danish registers)16 until 31 December 2000. Eligible codes were ICD-8 codes 410-414 (CHD), 430-438 (CBD), and 249-250 (diabetes) and ICD-10 codes I20-I25 (CHD), I60-I69 (CBD), and E10-E11 (diabetes). ICD-9 was never used in Denmark.
Incident cardiovascular disease
We ascertained incident CVD, CHD, and CBD by diagnoses from the Danish National Patient Register16 and the Danish Register of Causes of Death17 from 1 January 2001 to 31 December 2014. Incident CVD was defined as either incident CHD, including fatal CHD (ICD-10 codes I20-I25) or non-fatal myocardial infarction (I21, I22) or incident CBD, including fatal CBD (I60-I69) or non-fatal stroke (I60, I61, I63, I64).
Mortality
Using the Danish Register of Causes of Death,17 we identified all-cause mortality, CVD mortality (ICD-10 codes I20-I25 and I60-I69), and non-CVD mortality, defined as mortality due to all other causes than CVD.
Covariates
As covariates, we included age, migration background, and family type, because they might be associated with both educational attainment and risk of CVD. We further included health services use as an indicator for health status, including undiagnosed prevalent CVD. All covariates were updated annually from 2000 to 2009, with the exception of migration background that was kept time-invariant based on the measure in 2000.
For migration background, we used the classification of Statistics Denmark’s population register, distinguishing between (i) individuals without migration background, (ii) immigrants, and (iii) descendants of immigrants. Information on family type was retrieved by combining information from the Population Register and the Family Relation Register at Statistics Denmark and categorized into six groups combining marital/cohabitation status and living with or without children at home (see Table 1 for details). We obtained information on use of health services, provided by primary health care professionals, such as general practitioners, from the Danish National Health Service Register18 and categorized the number of health services used into deciles based on the distribution within each year.
Table 1.
Characteristics of the study population at baseline in 2000, stratified by cardiometabolic disease status and sex
| Participants without prevalent cardiometabolic disease |
Participants with prevalent cardiometabolic disease |
|||
|---|---|---|---|---|
| Men, n (%) | Women, n (%) | Men, n (%) | Women, n (%) | |
| Sex | ||||
| Men | 837 488 (51.1) | 28 430 (67.8) | ||
| Women | 800 782 (48.9) | 13 514 (32.2) | ||
| Education | ||||
| Low education | 186 957 (22.3) | 192 645 (24.1) | 7967 (28.0) | 4242 (31.4) |
| Medium education | 411 815 (49.2) | 339 339 (42.4) | 14 153 (49.8) | 5689 (42.1) |
| High education | 226 070 (27.0) | 260 606 (32.5) | 5799 (20.4) | 3408 (25.2) |
| Missing education | 12 646 (1.5) | 8192 (1.0) | 511 (1.8) | 175 (1.3) |
| Income | ||||
| Low income | 268 269 (32.0) | 244 623 (30.6) | 8785 (30.9) | 4501 (33.3) |
| Medium income | 264 180 (31.5) | 248 712 (31.1) | 9159 (32.2) | 4126 (30.5) |
| High income | 249 492 (29.8) | 263 404 (32.9) | 9045 (31.8) | 4240 (31.4) |
| Missing income | 55 547 (6.6) | 44 043 (5.5) | 1441 (5.1) | 647 (4.8) |
| Job strain | ||||
| Low job strain | 299 356 (35.7) | 246 738 (30.8) | 10 076 (35.4) | 3903 (28.9) |
| Medium job strain | 254 844 (30.4) | 291 108 (36.4) | 8983 (31.6) | 5003 (37.0) |
| High job strain | 283 288 (33.8) | 262 936 (32.8) | 9371 (33.0) | 4608 (34.1) |
| NA job strain | ||||
| Family type | ||||
| Single without children | 189 917 (22.7) | 125 907 (15.7) | 6721 (23.6) | 2900 (21.5) |
| Single with children (age 0–7) | 9021 (1.1) | 18 410 (2.3) | 117 (0.4) | 167 (1.2) |
| Single with children (age 8–17) | 15 207 (1.8) | 41 452 (5.2) | 542 (1.9) | 620 (4.6) |
| Married/cohabitant without children | 246 759 (29.5) | 255 742 (31.9) | 12 828 (45.1) | 6103 (45.2) |
| Married/cohabitant with children (age 0–7) | 134 009 (16.0) | 108 315 (13.5) | 1793 (6.3) | 805 (6.0) |
| Married/cohabitant with children (age 8–17) | 149 255 (17.8) | 153 974 (19.2) | 4797 (16.9) | 2106 (15.6) |
| Missing family type | 93 320 (11.4) | 96 982 (12.1) | 1632 (5.7) | 813 (6.0) |
| Migration background | ||||
| No migration background | 796 480 (95.1) | 767 729 (95.9) | 27 130 (95.4) | 12 941 (95.8) |
| Immigrant | 39 729 (4.7) | 31 904 (4.0) | 1268 (4.5) | 559 (4.1) |
| Descendant of immigrants | 1279 (0.2) | 1149 (0.1) | 32 (0.1) | 14 (0.1) |
| Age, mean (SD) | 43.6 (8.5) | 43.7 (8.3) | 49.4 (7.5) | 48.0 (7.9) |
| Number of health services used, mean (SD) | 11.8 (16.4) | 19.7 (23.0) | 24.9 (29.3) | 34.6 (37.2) |
| Job strain, mean (SD) | 0.14 (0.08) | 0.14 (0.08) | 0.14 (0.08) | 0.14 (0.08) |
| Disposable household income (€), mean | 42 440 | 43 721 | 41 348 | 40 899 |
| Years from first diagnosis of prevalent cardiometabolic until baseline, mean (SD) | — | — | 3.8 (2.8) | 3.9 (3.1) |
NA, not applicable; SD, standard deviation.
Statistical analysis
All analyses were conducted using SAS 9.4 using proc phreg applying robust sandwich variance estimates to account for clustering by the repeated measures at the individual level, and stratified by sex. We fitted four models. In Model 1, estimates were adjusted for age, migration background, family type, and health services use. In subsequent models, the estimates were further adjusted for income (Model 2), job strain (Model 3), and income and job strain (Model 4). We calculated the percentage of excess risk (hazard) explained by income and job strain using the formula (HR1−HR2)/(HR1−1)*100,19,20 where HR1 is the hazard ratio (HR) of Model 1 and HR2 is the HR of either Model 2, Model 3, or Model 4, depending on which model was compared to Model 1.
To indicate missing values, we added a category ‘missing value’ to the variables education, income, and family type. All other variables were complete. Percentage of missing values was low at baseline, ranging from 1.0% (for education among women without prevalent cardiometabolic disease) to 12.1% (for family type among women without prevalent cardiometabolic disease). See Table 1 for details.
Incident cardiovascular disease among individuals without prevalent cardiometabolic disease
Participants were followed from 1 January 2001 to the first CVD event or censoring due to emigration from Denmark, non-CVD death, or end of follow-up (31 December 2014), whichever came first. Using Cox proportional hazards models with calendar time as the underlying time axis, we calculated HRs and 95% CIs for the association between education and incident CVD. Education, income, and job strain were treated as time-varying variables using a 1-year time lag between their ascertainment and the ascertainment of the outcome. For example, education ascertained in the year 2000 (year t) was used to predict CVD in the year 2001 (year t + 1). After 2009, all time-varying variables were kept time-invariant, based on their 2009 values. We repeated all analyses with CHD and CBD as separate events. To avoid censoring on a competing risks outcome, we did not censor for CBD in the CHD analyses and vice versa, thus the same individuals could become cases both in the CHD and CBD analyses.
Of the covariates, age and family type were treated as time-varying variables including measurements from the same year as education. Health services use was treated as time-varying measured the year before education, to account for pre-existing ill-health. Migration background was used as time-invariant based on the year 2000 data.
Mortality among individuals with prevalent cardiometabolic disease
Participants were followed from 1 January 2001 until all-cause mortality, CVD mortality, or non-CVD mortality. We censored due to emigration from Denmark, non-CVD mortality (in analyses on CVD mortality), CVD mortality (in analyses on non-CVD mortality), or end of follow-up (31 December 2014), whichever came first. Using Cox proportional hazards regression models with calendar time as the underlying time axis we calculated HRs and 95% CI for the association of education with all-cause mortality, CVD mortality, and non-CVD mortality.
Similar to the analyses on incident CVD, education was treated as a time-varying variable, using a 1-year time lag between ascertainment of education and outcome. Covariates were also treated similarly as in the analyses on incident CVD.
Supplementary analyses
We conducted three supplementary analyses. First, we repeated Model 4 on incident CVD while censoring cases during the first year of follow-up, to examine whether results might have been biased by undetected prevalent CVD at baseline. Second, we repeated Model 4 on incident CVD and CVD mortality separately for women aged ≤50 and >50 years to examine if associations were affected by menopausal status. Third, we repeated the analyses while excluding participants with missing values on education, income, or family type to examine if the missing variable indicator approach may have biased the results.
Results
Characteristics of the study population at baseline
Table 1 shows the baseline characteristics of the study population in the year 2000, separately for 1 638 270 participants without prevalent cardiometabolic disease and 41 944 participants with prevalent cardiometabolic disease. Among participants without prevalent cardiometabolic disease, the proportions of men (51.1%) and women (48.9%) were similar. The mean age was about 44 years, most had a medium-level education and were married or cohabiting without children at home. The mean yearly number of health services used was 11.8 and 19.7 for men and women, respectively. Participants with prevalent cardiometabolic disease were, as expected, more likely to be men and of older age and used more health services compared to participants without prevalent cardiometabolic disease.
Education and incident cardiovascular disease among individuals without prevalent cardiometabolic disease
Among men, during 10 957 399 person-years, we identified 51 585 cases of incident CVD (47 per 10 000 person-years), including 27 624 CHD cases (25 per 10 000 person-years) and 25 858 CBD cases (23 per 10 000 person-years). Among women, during 10 776 516 person-years, we identified 24 075 cases of incident CVD (22 per 10 000 person-years), including 8300 CHD cases (8 per 10 000 person-years) and 16 326 CBD cases (15 per 10 000 person-years).
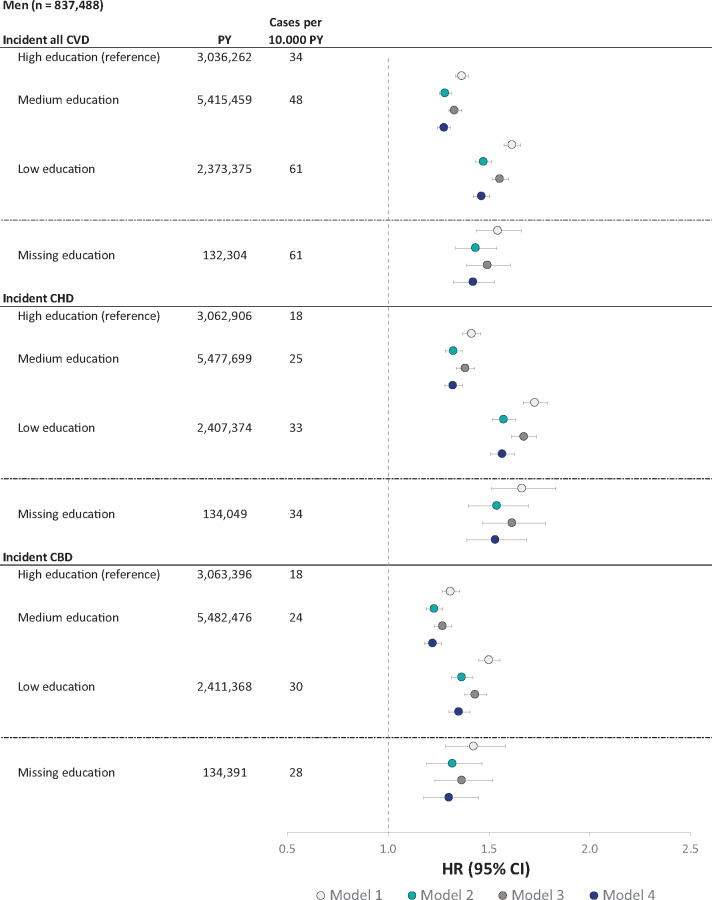
Figure 1 and Table 2 show the estimates for the association between education and incident CVD, CHD, and CBD in men. Compared to high education, medium, and low education was associated with a higher risk of incident CVD in a dose–response fashion in all models. The HR for CVD associated with low education was 1.62 (95% CI 1.58–1.66, Model 1) before and 1.46 (95% CI 1.42–1.50, Model 4) after adjustment for income and job strain, a 25% reduction. The reduction was larger after adjustment for income (23%) than after the adjustment for job strain (10%). Results were similar for CHD and CBD.
Figure 1.
Association between education and incident cardiovascular disease in men after 14-year follow-up. See Table 2 for an explanation of the models. CBD, cerebrovascular disease; CHD, coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; PY, person-years.
Table 2.
Association between education and incident cardiovascular disease in men after 14-year follow-up
| Men (n = 837 488) | PY | Cases per 10 000 PY | Model 1 | Model 2 | % excess risk explained | Model 3 | % excess risk explained | Model 4 | % excess risk explained |
|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | ||||||
| Incident all CVD | |||||||||
| High education (reference) | 3 036 262 | 34 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 5 415 459 | 48 | 1.37 (1.34–1.40) | 1.28 (1.25–1.31) | 22% | 1.33 (1.30–1.36) | 10% | 1.28 (1.25–1.31) | 24% |
| Low education | 2 373 375 | 61 | 1.62 (1.58–1.66) | 1.48 (1.44–1.51) | 23% | 1.56 (1.52–1.60) | 10% | 1.46 (1.42–1.50) | 25% |
| Missing education | 132 304 | 61 | 1.55 (1.44–1.66) | 1.43 (1.33–1.54) | 21% | 1.49 (1.39–1.61) | 10% | 1.42 (1.32–1.53) | 23% |
| Incident CHD | |||||||||
| High education (reference) | 3 062 906 | 18 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 5 477 699 | 25 | 1.42 (1.37–1.46) | 1.33 (1.28–1.37) | 21% | 1.38 (1.34–1.43) | 7% | 1.32 (1.28–1.37) | 22% |
| Low education | 2 407 374 | 33 | 1.73 (1.67–1.79) | 1.57 (1.52–1.63) | 21% | 1.67 (1.61–1.74) | 7% | 1.57 (1.51–1.63) | 22% |
| Missing education | 134 049 | 34 | 1.67 (1.51–1.83) | 1.54 (1.40–1.70) | 19% | 1.62 (1.47–1.78) | 7% | 1.53 (1.39–1.69) | 20% |
| Incident CBD | |||||||||
| High education (reference) | 3 063 396 | 18 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 5 482 476 | 24 | 1.31 (1.27–1.35) | 1.23 (1.19–1.27) | 26% | 1.27 (1.23–1.31) | 13% | 1.22 (1.18–1.27) | 28% |
| Low education | 2 411 368 | 30 | 1.50 (1.45–1.56) | 1.37 (1.32–1.42) | 27% | 1.43 (1.38–1.49) | 14% | 1.35 (1.30–1.41) | 30% |
| Missing education | 134 391 | 28 | 1.43 (1.29–1.58) | 1.32 (1.19–1.47) | 25% | 1.37 (1.23–1.52) | 14% | 1.30 (1.18–1.45) | 29% |
Model 1: Adjusted for age, migration background, family type, and health services use. Model 2: Adjusted for covariates in Model 1 plus income. Model 3: Adjusted for covariates in Model 1 plus job strain. Model 4: Adjusted for covariates in Model 1 plus income and job strain.
CBD, cerebrovascular disease; CHD, coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; PY, person-years.
The HR of incident CVD for low vs. high income and high vs. low job strain were 1.33 (95% CI 1.29–1.37) and 1.01 (95% CI 0.98–1.03), respectively (Model 4, not shown in Table 2).
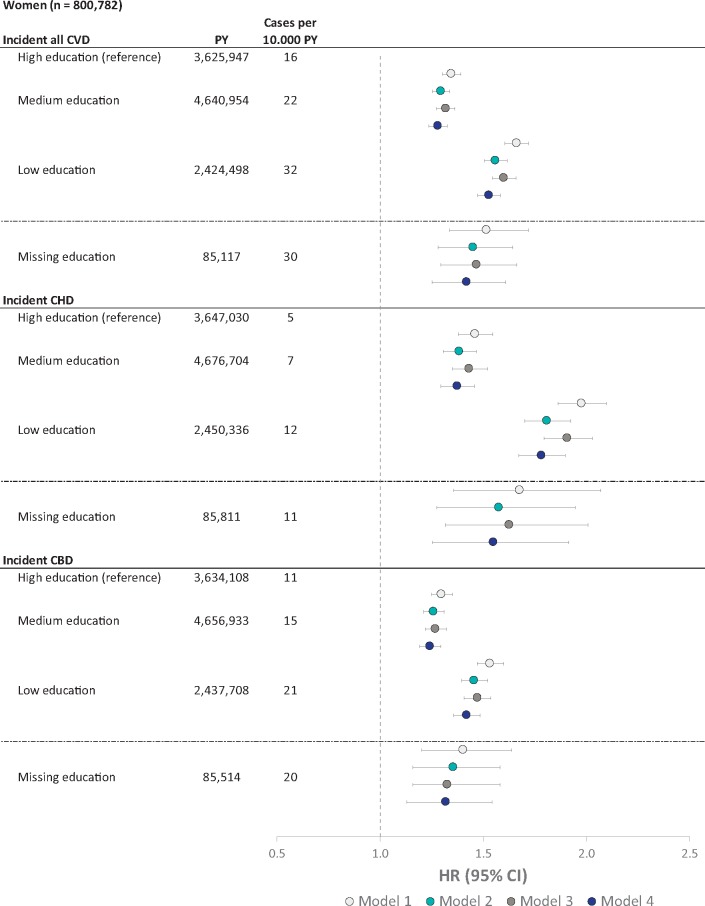
Figure 2 and Table 3 show the corresponding estimates for women. As in men, medium, and low education was associated with a higher risk of incident CVD in a dose–response fashion in all models. The HR for CVD associated with low education was 1.66 (95% CI 1.61–1.72, Model 1) before and 1.53 (95% CI 1.47–1.58, Model 4) after adjustment for income and job strain, a 21% reduction. The reduction was larger after the adjustment for income (16%) than after the adjustment for job strain (10%). Results were similar for CHD and CBD.
Figure 2.
Association between education and incident cardiovascular disease in women after 14-year follow-up. See Table 3 for an explanation of the models. CBD, cerebrovascular disease; CHD, coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; PY, person-years.
Table 3.
Association between education and incident cardiovascular disease in women after 14-year follow-up
| Women (n = 800 782) | PY | Cases per 10 000 PY | Model 1 | Model 2 | % excess risk explained | Model 3 | % excess risk explained | Model 4 | % excess risk explained |
|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | ||||||
| Incident all CVD | |||||||||
| High education (reference) | 3 625 947 | 16 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 4 640 954 | 22 | 1.35 (1.30–1.39) | 1.30 (1.25–1.34) | 14% | 1.32 (1.27–1.36) | 8% | 1.28 (1.24–1.33) | 19% |
| Low education | 2 424 498 | 32 | 1.66 (1.61–1.72) | 1.56 (1.51–1.62) | 16% | 1.60 (1.54–1.66) | 10% | 1.53 (1.47–1.58) | 21% |
| Missing education | 85 117 | 30 | 1.52 (1.34–1.72) | 1.45 (1.28–1.64) | 13% | 1.47 (1.29–1.66) | 10% | 1.42 (1.25–1.61) | 19% |
| Incident CHD | |||||||||
| High education (reference) | 3 647 030 | 5 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 4 676 704 | 7 | 1.46 (1.38–1.55) | 1.38 (1.31–1.47) | 17% | 1.43 (1.35–1.52) | 6% | 1.37 (1.29–1.46) | 19% |
| Low education | 2 450 336 | 12 | 1.98 (1.86–2.10) | 1.81 (1.70–1.92) | 17% | 1.91 (1.79–2.03) | 7% | 1.78 (1.67–1.90) | 20% |
| Missing education | 85 811 | 11 | 1.68 (1.36–2.07) | 1.57 (1.27–1.95) | 15% | 1.63 (1.32–2.01) | 8% | 1.55 (1.25–1.91) | 19% |
| Incident CBD | |||||||||
| High education (reference) | 3 634 108 | 11 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 4 656 933 | 15 | 1.30 (1.25–1.35) | 1.26 (1.21–1.31) | 13% | 1.27 (1.22–1.32) | 10% | 1.24 (1.19–1.29) | 19% |
| Low education | 2 437 708 | 21 | 1.53 (1.47–1.60) | 1.46 (1.40–1.52) | 14% | 1.47 (1.41–1.54) | 12% | 1.42 (1.36–1.48) | 21% |
| Missing education | 85 514 | 20 | 1.40 (1.20–1.64) | 1.35 (1.16–1.58) | 12% | 1.33 (1.16–1.58) | 19% | 1.32 (1.13–1.54) | 21% |
Model 1: Adjusted for age, migration background, family type, and health services use. Model 2: Adjusted for covariates in Model 1 plus income. Model 3: Adjusted for covariates in Model 1 plus job strain. Model 4: Adjusted for covariates in Model 1 plus income and job strain.
CBD, cerebrovascular disease; CHD, coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; PY, person-years.
The HR of incident CVD for low vs. high income and high vs. low job strain were 1.29 (95% CI 1.24–1.34) and 1.01 (95% CI 0.97–1.06), respectively (Model 4, not shown in Table 3).
Education and mortality among individuals with prevalent cardiometabolic disease
Among men with prevalent CVD, during 362 234 person-years, 5022 deaths occurred (139 per 10 000 person-years), 1736 due to CVD (48 per 10 000 person-years), and 3286 due to non-CVD (91 per 10 000 person-years). Among women with prevalent CVD, during 179 402 person-years, 1346 deaths occurred (75 per 10 000 person-years), 341 due to CVD (19 per 10 000 person-years), and 1005 due to non-CVD (56 per 10 000 person-years).
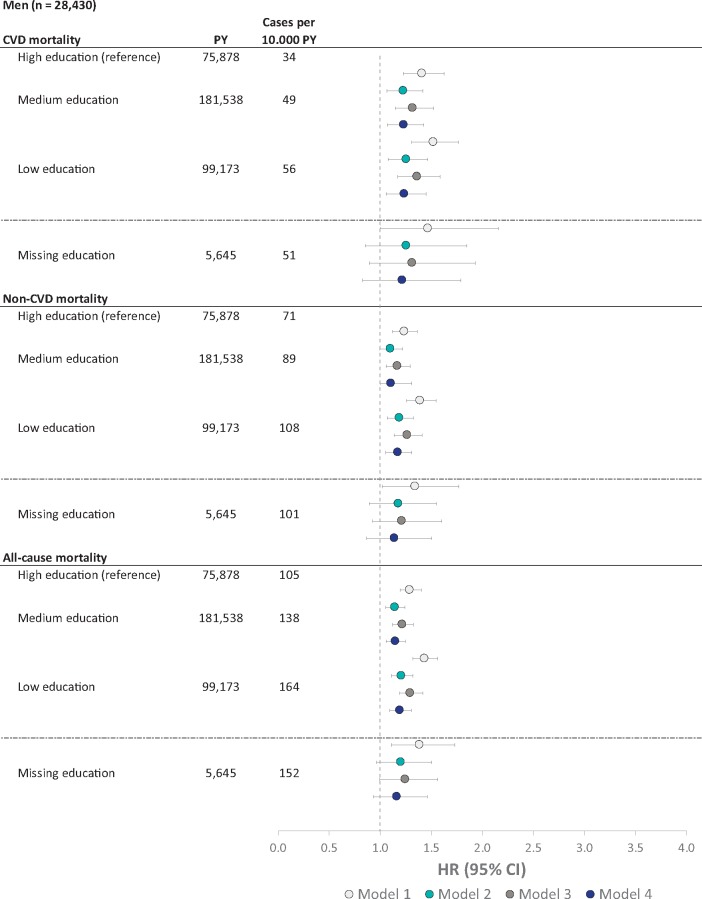
Figure 3 and Table 4 show the estimates for the association between education and mortality in men. Low and medium education was associated with a higher risk of CVD, non-CVD, and all-cause mortality in all models. The HR for CVD mortality in men with low education was 1.52 (95% CI 1.31–1.77, Model 1) before and 1.24 (95% CI 1.06–1.45, Model 4) after adjustment for income and job strain, a 54% reduction. The reduction was larger after adjustment for income (51%) than after adjustment for job strain (31%).
Figure 3.
Association between education and mortality in men after 14-year follow-up. See Table 4 for an explanation of the models. CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; PY, person-years.
Table 4.
Association between education and mortality in men after 14-year follow-up
| Men (n = 28 430) | PY | Cases per 10 000 PY | Model 1 | Model 2 | % excess risk explained | Model 3 | % excess risk explained | Model 4 | % excess risk explained |
|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | ||||||
| CVD mortality | |||||||||
| High education (reference) | 75 878 | 34 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 181 538 | 49 | 1.41 (1.23–1.62) | 1.23 (1.07–1.42) | 45% | 1.32 (1.15–1.53) | 22% | 1.24 (1.07–1.43) | 43% |
| Low education | 99 173 | 56 | 1.52 (1.31–1.77) | 1.26 (1.08–1.46) | 51% | 1.36 (1.17–1.59) | 31% | 1.24 (1.06–1.45) | 54% |
| Missing education | 5645 | 51 | 1.47 (1.00–2.16) | 1.26 (0.86–1.85) | 45% | 1.31 (0.90–1.93) | 33% | 1.22 (0.83–1.79) | 54% |
| Non-CVD mortality | |||||||||
| High education (reference) | 75 878 | 71 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 181 538 | 89 | 1.24 (1.12–1.36) | 1.10 (1.00–1.22) | 57% | 1.17 (1.06–1.29) | 28% | 1.11 (1.00–1.31) | 54% |
| Low education | 99 173 | 108 | 1.40 (1.26–1.55) | 1.19 (1.07–1.32) | 52% | 1.27 (1.14–1.41) | 33% | 1.18 (1.05–1.31) | 56% |
| Missing education | 5645 | 101 | 1.35 (1.02–1.77) | 1.18 (0.90–1.55) | 48% | 1.22 (0.92–1.60) | 38% | 1.14 (0.87–1.51) | 59% |
| All-cause mortality | |||||||||
| High education (reference) | 75 878 | 105 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 181 538 | 138 | 1.29 (1.19–1.40) | 1.14 (1.05–1.24) | 51% | 1.22 (1.12–1.32) | 25% | 1.15 (1.06–1.25) | 49% |
| Low education | 99 173 | 164 | 1.44 (1.32–1.56) | 1.21 (1.11–1.32) | 52% | 1.30 (1.19–1.42) | 32% | 1.20 (1.09–1.31) | 55% |
| Missing education | 5645 | 152 | 1.39 (1.11–1.73) | 1.21 (0.97–1.51) | 47% | 1.25 (1.00–1.56) | 36% | 1.17 (0.93–1.46) | 57% |
Model 1: Adjusted for age, migration background, family type, and health services use. Model 2: Adjusted for covariates in Model 1 plus income. Model 3: Adjusted for covariates in Model 1 plus job strain. Model 4: Adjusted for covariates in Model 1 plus income and job strain.
CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; PY, person-years.
The HR of CVD mortality for low vs. high income and high vs. low job strain were 1.57 (95% CI 1.33–1.85) and 0.90 (95% CI 0.74–1.09), respectively (Model 4, not shown in Table 4).
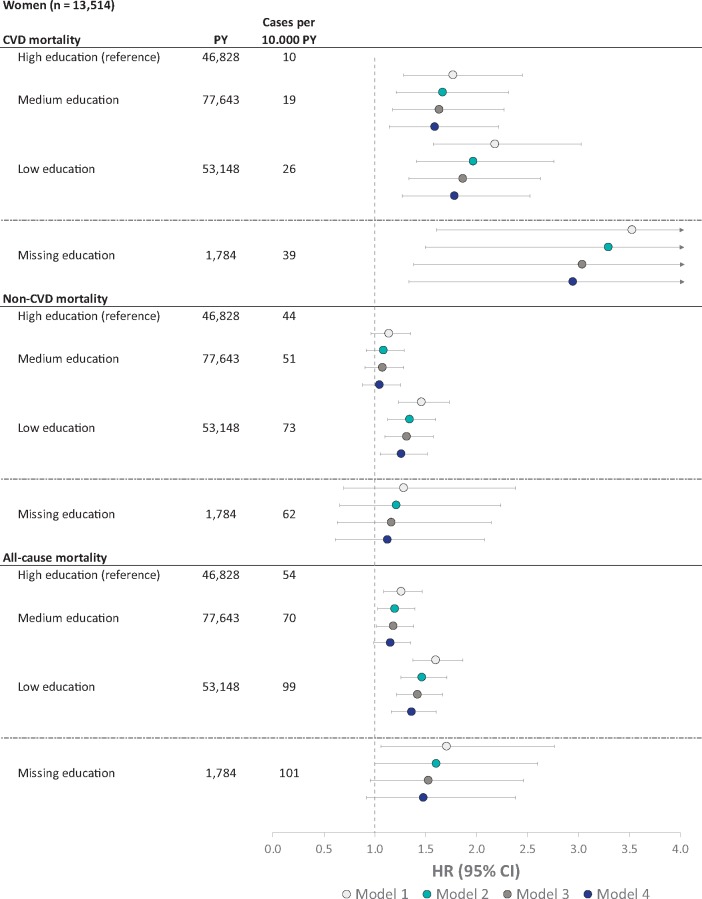
Figure 4 and Table 5 show the corresponding estimates for women. Low education was associated with a higher risk of CVD, non-CVD, and all-cause mortality in all models. Medium education was associated with a higher risk of CVD and all-cause mortality but not with risk of non-CVD mortality. The HR for CVD mortality in women with low education was 2.18 (95% CI 1.57–3.03, Model 1) before and 1.79 (95% CI 1.27–2.52, Model 4) after adjustment for income and job strain, a 33% reduction. The reduction was larger after adjustment for job strain (26%) than after adjustment for income (18%).
Figure 4.
Association between education and mortality in women after 14-year follow-up. See Table 5 for an explanation of the models. CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; PY, person-years.
Table 5.
Association between education and mortality in women after 14-year follow-up
| Women (n = 13 514) | PY | Cases per 10 000 PY | Model 1 | Model 2 | % excess risk explained | Model 3 | % excess risk explained | Model 4 | % excess risk explained |
|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | ||||||
| CVD mortality | |||||||||
| High education (reference) | 46 828 | 10 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 77 643 | 19 | 1.77 (1.28–2.45) | 1.67 (1.21–2.31) | 13% | 1.63 (1.18–2.27) | 18% | 1.59 (1.14–2.21) | 24% |
| Low education | 53 148 | 26 | 2.18 (1.57–3.03) | 1.97 (1.41–2.76) | 18% | 1.87 (1.33–2.62) | 26% | 1.79 (1.27–2.52) | 33% |
| Missing education | 1784 | 39 | 3.53 (1.60–7.76) | 3.30 (1.50–7.28) | 9% | 3.04 (1.38–6.68) | 19% | 2.95 (1.34–6.49) | 23% |
| Non-CVD mortality | |||||||||
| High education (reference) | 46 828 | 44 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 77 643 | 51 | 1.14 (0.96–1.35) | 1.09 (0.92–1.29) | 39% | 1.08 (0.90–1.28) | 46% | 1.05 (0.88–1.25) | 64% |
| Low education | 53 148 | 73 | 1.46 (1.23–1.73) | 1.34 (1.13–1.60) | 25% | 1.32 (1.10–1.57) | 32% | 1.26 (1.05–1.51) | 43% |
| Missing education | 1784 | 62 | 1.29 (0.70–2.38) | 1.21 (0.66–2.24) | 26% | 1.16 (0.63–2.15) | 43% | 1.13 (0.61–2.07) | 56% |
| All-cause mortality | |||||||||
| High education (reference) | 46 828 | 54 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Medium education | 77 643 | 70 | 1.26 (1.09–1.46) | 1.20 (1.03–1.39) | 24% | 1.18 (1.02–1.38) | 30% | 1.16 (0.99–1.35) | 40% |
| Low education | 53 148 | 99 | 1.60 (1.38–1.86) | 1.47 (1.26–1.71) | 23% | 1.42 (1.22–1.67) | 30% | 1.37 (1.16–1.60) | 39% |
| Missing education | 1784 | 101 | 1.71 (1.06–2.77) | 1.61 (1.00–2.60) | 14% | 1.53 (0.95–2.46) | 25% | 1.48 (0.92–2.38) | 32% |
Model 1: Adjusted for age, migration background, family type, and health services use. Model 2: Adjusted for covariates in Model 1 plus income. Model 3: Adjusted for covariates in Model 1 plus job strain. Model 4: Adjusted for covariates in Model 1 plus income and job strain.
CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; PY, person-years.
Take home figure.
Association between low compared to high education and cardiovascular disease and cardiovascular death after 14-year follow-up. Association between educational attainment and cardiovascular disease and cardiovascular death after 14-year follow-up in men and women without and with cardiometabolic disease with % excess risk explained by income and job strain. HR (95% CI) for low compared to high educational attainment adjusted for age, migration background, family type, and health services use in Step 1 and further adjusted for income and job strain in Step 2. CI, confidence interval; HR, hazard ratio.
The HR of CVD mortality for low vs. high income and high vs. low job strain were 1.28 (95% CI 0.87–1.88) and 1.34 (95% CI 0.83–2.15), respectively (Model 4, not shown in Table 5).
Supplementary analyses
When repeating Model 4 while censoring incident CVD cases during the first year of follow-up, results were similar to the results in the main analyses (Supplementary material online, e-Appendix 2, Table S2).
When repeating Model 4 separately for women aged ≤50 and >50 years, results of the two groups were similar (Supplementary material online, e-Appendix 2, Table S3).
When excluding participants with missing values on education, income, or family type instead of using a missing value indicator, results were similar to the main analyses (data available upon request).
Discussion
In the Danish workforce, low education was associated with higher risk of incident CVD and, among those already diagnosed with cardiometabolic disease, higher risk of mortality due to CVD. In men with cardiometabolic disease, material and psychosocial factors, such as income and job strain, explained half of the higher CVD mortality among individuals with low educational attainment. In men without cardiometabolic disease and in women with and without cardiometabolic disease, these factors explained between 21% and 33% of the higher CVD morbidity and mortality risk among those with low educational attainment.
Comparison with previous research studies
To our knowledge, this register-based study is the first one that examined the association between education and both CVD incidence and mortality in a cohort that included all employees, aged 30–59 years, of a national workforce. Mackenbach et al.21 previously reported associations between low education and CVD mortality in 22 European countries, based on national registers but did not examine morbidity and did not account for changes in exposures and covariates over time.
The present study is, to our knowledge, also the first nationwide study to examine the extent to which the association between low education and CVD morbidity and mortality is reduced by accounting for low income and work stress. Huisman et al.22 previously reported in a study of 5775 employees from the southern parts of the Netherlands that the association between low education and risk of myocardial infarction was slightly reduced after adjustment for work stress. Measures of income were not available in that study.
Our study confirms that low education is an important predictor of CVD3,6 and adds new knowledge that this contribution is partly explained by income and job strain. Our study is the largest study to date on the contribution of low education to the prognosis of individuals with a cardiometabolic disease. That education is a stronger predictor of CVD mortality in women than in men with cardiometabolic disease is, to our knowledge, a novel finding.
Strengths and limitations
Strengths of the study are the large cohort, including all employees in Denmark in the age group 30–59, the use of annually updated exposure and covariate measurements from population registers and the follow-up in nationwide health registers leading to minimal attrition and avoidance of reporting bias. We accounted for changes over time regarding CVD prevalence and treatment by using calendar time as the time axis.
We used the percentage of excess risk explained measure to estimate to what extent the association between education and the outcome was explained by income and job strain.19,20 This is an estimation of the mediated proportion based on comparing the total effect and the controlled direct effect, a method assuming no interaction between exposure and mediator on the outcome.23 As methods for mediation analyses are rapidly developing,24 alternative approaches may have yielded different results. However, as no common best practice for these alternative approaches have been established yet,24 we adhered to the percentage of excess risk explained measure as this approach is common practice25 and has frequently been used in analyses on social inequalities in health.26,27
The generalization of the study results is limited to the examined age groups (30–59 years at baseline, 44–73 years at end of follow-up) and to the Danish context and we cannot rule out that associations might have been different in different age groups or countries. Further, reverse causation is in principal possible, if undetected prevalent CVD had impacted educational attainment. However, since level of educational attainment is usually determined in adolescence and young adulthood, i.e. at an age when prevalent CVD is very rare, we regard reverse causation as unlikely.
Our data lacked information about biological (e.g., blood pressure, blood lipid profile) and behavioural (e.g., smoking, diet) CVD risk factors. As it is unlikely that these risk factors had impacted educational attainment, it appears improbable that these risk factors could have confounded the association between education and CVD. However, data on these risk factors may have provided us with greater insight into the mechanisms and pathways linking education, income, and job strain with CVD. Results from a recent Mendelian randomization study suggest that smoking, body mass index, and blood lipid profile are important pathways linking educational level with risk of CVD.6 Information on biological and behavioural risk factors would have allowed us to examine what extent of the remaining association between education and CVD in our study, which was not explained by income and job strain, was explained by these risk factors and what extent remained unexplained. Information on these risk factors would have also allowed us to analyse their role in the pathways linking income and job strain with CVD.
Although job strain is the most commonly used measure of a work-related stressor in epidemiological studies, our study would have benefited from a more comprehensive assessment, as other work-related stressors may also contribute to risk of CVD.8
Public health implications
The results of this study support the statement in the ‘2016 European Guidelines on CVD prevention in clinical practice’ by the European Society of Cardiology (ESC) that ‘low socio-economic status […] contribute to the risk of developing CVD and a worse prognosis of CVD’.28 We demonstrated that the association between low education and CVD was attenuated after adjustment for income and job strain. This attenuation was particularly pronounced for CVD mortality in men with prevalent cardiometabolic disease, as low income and job strain together explained 54% of the association between education and CVD mortality. From a tertiary prevention perspective, this is an encouraging result. Educational attainment is usually determined relatively early in the life, and it seems difficult to improve the level of education in middle-aged adults with cardiometabolic disease. In this population, improvement of disposable income, e.g., through taxation or social transfer payments, and reduction of job strain, e.g., through changes in work organization, are likely more amenable to change than educational level.
Conclusion
Low education predicted risk of incident CVD in initially healthy men and women and risk of CVD mortality in men and women with prevalent cardiometabolic disease in this nationwide cohort study of the Danish workforce. These associations were partly explained by income and job strain. In men with cardiometabolic disease, income and job strain explained half of the higher CVD mortality risk among individuals with low educational attainment.
Supplementary Material
Acknowledgements
The authors are grateful to Trine Larsen for creating the Take home figure for this article.
Funding
This study was supported by the NordForsk Nordic Program on Health and Welfare (#75021), the Danish Working Environment Research Fund (#17-2014-03 and #27-2017-03), and the Swedish Research Council of Health, Working Life and Welfare (#2017-01943).
Declaration of Helsinki
This study complies with the Declaration of Helsinki. No patients were involved. In Denmark, studies that are based on questionnaire and register-data only do not require approval from the National Committee on Health Research Ethics. The study was approved by the Danish Data Protection Agency through the joint notification of the National Research Centre for the Working Environment (no. 2015-57-0074). All data are stored in a protected server environment hosted by Statistics Denmark.
Conflict of interest: none declared.
References
- 1.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1151–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cheng S, Claggett B, Correia AW, Shah AM, Gupta DK, Skali H, Ni H, Rosamond WD, Heiss G, Folsom AR, Coresh J, Solomon SD.. Temporal trends in the population attributable risk for cardiovascular disease: the Atherosclerosis Risk in Communities Study. Circulation 2014;130:820–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khaing W, Vallibhakara SA, Attia J, McEvoy M, Thakkinstian A.. Effects of education and income on cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol 2017;24:1032–1042. [DOI] [PubMed] [Google Scholar]
- 4. Rashid S, Simms A, Batin P, Kurian J, Gale CP.. Inequalities in care in patients with acute myocardial infarction. World J Cardiol 2015;7:895–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mehta RH, O'Shea JC, Stebbins AL, Granger CB, Armstrong PW, White HD, Topol EJ, Califf RM, Ohman EM.. Association of mortality with years of education in patients with ST-segment elevation myocardial infarction treated with fibrinolysis. J Am Coll Cardiol 2011;57:138–146. [DOI] [PubMed] [Google Scholar]
- 6. Tillmann T, Vaucher J, Okbay A, Pikhart H, Peasey A, Kubinova R, Pajak A, Tamosiunas A, Malyutina S, Hartwig FP, Fischer K, Veronesi G, Palmer T, Bowden J, Smith GD, Bobak M, Holmes MV. Education and coronary heart disease: mendelian randomisation study. BMJ 2017;358:j3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kivimäki M, Pentti J, Ferrie JE, Batty GD, Nyberg ST, Jokela M, Virtanen M, Alfredsson L, Dragano N, Fransson EI, Goldberg M, Knutsson A, Koskenvuo M, Koskinen A, Kouvonen A, Luukkonen R, Oksanen T, Rugulies R, Siegrist J, Singh-Manoux A, Suominen S, Theorell T, Väänänen A, Vahtera J, Westerholm PJM, Westerlund H, Zins M, Strandberg T, Steptoe A, Deanfield J; for the IPD-Work consortium. Work stress and risk of death in men and women with and without cardiometabolic disease: a multicohort study. Lancet Diabetes Endocrinol 2018;6:705–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kivimäki M, Steptoe A.. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol 2018;15:215–229. [DOI] [PubMed] [Google Scholar]
- 9. Karasek R. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q 1979;24:285–307. [Google Scholar]
- 10. Petersson F, Baadsgaard M, Thygesen LC.. Danish registers on personal labour market affiliation. Scand J Public Health 2011;39:95–98. [DOI] [PubMed] [Google Scholar]
- 11. Jensen VM, Rasmussen AW.. Danish education registers. Scand J Public Health 2011;39:91–94. [DOI] [PubMed] [Google Scholar]
- 12.The United Nations Educational Scientific and Cultural Organization (UNESCO). International Standard Classification of Education (ISCED). http://uis.unesco.org/en/topic/international-standard-classification-education-isced (15 December 2018).
- 13. Baadsgaard M, Quitzau J.. Danish registers on personal income and transfer payments. Scand J Public Health 2011;39:103–105. [DOI] [PubMed] [Google Scholar]
- 14. Burr H, Bjorner JB, Kristensen TS, Tüchsen F, Bach E.. Trends in the Danish work environment in 1990-2000 and their associations with labor-force changes. Scand J Work Environ Health 2003;29:270–279. [DOI] [PubMed] [Google Scholar]
- 15. Feveile H, Olsen O, Burr H, Bach E.. Danish Work Environment Cohort Study 2005: from idea to sampling design. Stat Transit 2007;8:441–458. [Google Scholar]
- 16. Lynge E, Sandegaard JL, Rebolj M.. The Danish National Patient Register. Scand J Public Health 2011;39:30–33. [DOI] [PubMed] [Google Scholar]
- 17. Helweg-Larsen K. The Danish register of causes of death. Scand J Public Health 2011;39:26–29. [DOI] [PubMed] [Google Scholar]
- 18. Andersen JS, Olivarius Nde F, Krasnik A.. The Danish National Health Service Register. Scand J Public Health 2011;39:34–37. [DOI] [PubMed] [Google Scholar]
- 19. Szklo M, Nieto F.. Epidemiology: Beyond the Basics. Gaithersburg, MD: Aspen Publishers; 2000. [Google Scholar]
- 20. Schempf AH, Kaufman JS.. On the percent of excess risk explained. J Epidemiol Community Health 2011;65:190.. [DOI] [PubMed] [Google Scholar]
- 21. Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, Kunst AE; European Union Working Group on Socioeconomic Inequalities in Health. Socioeconomic inequalities in health in 22 European countries. N Engl J Med 2008;358:2468–2481. [DOI] [PubMed] [Google Scholar]
- 22. Huisman M, Van Lenthe F, Avendano M, Mackenbach J.. The contribution of job characteristics to socioeconomic inequalities in incidence of myocardial infarction. Soc Sci Med 2008;66:2240–2252. [DOI] [PubMed] [Google Scholar]
- 23. VanderWeele TJ. Controlled direct and mediated effects: definition, identification and bounds. Scand Stat Theory Appl 2011;38:551–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lange T, Hansen KW, Sorensen R, Galatius S.. Applied mediation analyses: a review and tutorial. Epidemiol Health 2017;39:e2017035.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ditlevsen S, Christensen U, Lynch J, Damsgaard MT, Keiding N.. The mediation proportion: a structural equation approach for estimating the proportion of exposure effect on outcome explained by an intermediate variable. Epidemiology 2005;16:114–120. [DOI] [PubMed] [Google Scholar]
- 26. van Oort FV, van Lenthe FJ, Mackenbach JP.. Material, psychosocial, and behavioural factors in the explanation of educational inequalities in mortality in The Netherlands. J Epidemiol Community Health 2005;59:214–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Laaksonen M, Talala K, Martelin T, Rahkonen O, Roos E, Helakorpi S, Laatikainen T, Prattala R.. Health behaviours as explanations for educational level differences in cardiovascular and all-cause mortality: a follow-up of 60 000 men and women over 23 years. Eur J Public Health 2008;18:38–43. [DOI] [PubMed] [Google Scholar]
- 28. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Lochen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Binno S; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by Representatives of 10 Societies and by Invited experts) Developed With the Special Contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.