Abstract
Objective
Laryngeal cancer is an important oncologic entity, whose prognosis depends on establishing appropriate preventive and diagnostic measures, especially in populations at higher risk.
Methods
Epidemiologic information including worldwide incidence, prevalence, burden of health loss (disability-adjusted life year; DALYs) and mortality of larynx cancer was obtained from the Global Health Data Exchange (GHDx) database.
Results
The current incidence, prevalence and mortality of laryngeal cancer are estimated at 2.76 cases/year per 100,000 inhabitants, 14.33 cases/year per 100,000 inhabitants and 1.66 deaths/year per 100,000 inhabitants, respectively, averaging 3.28 million DALYs each year. Incidence and prevalence have increased by 12% and 24%, respectively during the past 3 decades, whilst mortality has declined by around 5%. The epidemiologic burden of this malignancy is approximately 5-fold higher in males and increases in parallel with ageing, peaking after 65 years of age. Both incidence and mortality rates are higher in Europe and lower in Africa, but the ratio between deaths and incidence is the highest in Africa. Incidence has gradually declined in Europe during the past 3 decades, whilst it has increased in South-East Asia and Western Pacific. Cigarette smoking and alcohol abuse contribute for about 90% of overall worldwide mortality for laryngeal cancer.
Conclusions
Laryngeal cancer still poses a high clinical and societal burden, with an escalating temporal trend not expected to reverse soon.
Keywords: Larynx, laryngeal cancer, larynx cancer, epidemiology, mortality
Introduction
Laryngeal cancer is a form of malignancy originating from the anatomic site called larynx (also commonly known as “voice box”), which is anatomically divided in three regions including the supraglottic larynx (encompassing the epiglottis, false vocal cords, ventricles, aryepiglottic folds and arytenoids), the glottis (encompassing the true vocal cords and the anterior and posterior commissures) and the subglottic region (1,2). According to a large cases series recently published by Ciolofan et al, the majority of larynx malignancies (i.e., over 98%) are well-differentiated squamous cell carcinomas, whilst chondrosarcomas, leiomyosarcomas and melanomas only account for 2%−5% of all laryngeal cancers (3). Among squamous cell carcinomas, the well and moderately differentiated forms slightly prevail over poorly differentiated tumors, accounting for 43.5% and 41.5% of all cases, respectively. The larger number of laryngeal cancer cases originate from the glottic region (i.e., approximately two-third), followed by the supraglottic area (about 30%), whilst transglottic and purely subglottic tumors are generally less frequent (4,5).
The more important risk factors for laryngeal cancer include tobacco use, excessive alcohol ingestion, gastro-esophageal reflex, Plummer-Vinson syndrome, anatomical malformations, exposure to heat, chemicals, asbestos, nickel or ionizing radiations, along with some viral infections [e.g., human papilloma virus (HPV)] (2). The most frequent symptoms of laryngeal malignancies include hoarseness, sore throat, dysphagia and/or painful swallowing, impairment in voice quality, otalgia, cough and hemoptysis. Despite hoarseness can develop early in patients with laryngeal malignancies, in many cases the cancer has already deeply involved the vocal cords and spreads to regional lymphatics at diagnosis (1,2). Primary tumor volume, composite nodal volumes, composite primary tumor and nodal volumes are significant predictors of unfavorable prognosis, along with advanced age, performance status, grade and depth of invasion (2,6). Most patients are unfortunately diagnosed at advanced stages (i.e., over 75% at stage III or stage IV), especially those with supraglottic tumors (3,7), when the therapeutic options have a remarkably lower favorable impact on prognosis. The 5-year survival in treatable patients approximates 80% and 50% for glottic and supraglottic cancers, respectively (1,2).
Although some reports have described the local epidemiology of laryngeal cancer (4,5,7-9), a recent worldwide perspective is lacking to the best of our knowledge. This is especially important if one considers that a recent retrospective analysis of hospital data has revealed that the cumulative healthcare cost for laryngeal cancer management is as high as 92.4 million £ in the UK, with about 95% of these expenditures being attributable to inpatient care (i.e., bundled costs) (10). Since the implementation of effective strategies for prevention and early diagnosis of larynx cancer needs to be based on accurate and reliable epidemiologic information, renewed epidemiological data on the worldwide clinical burden of laryngeal cancer are necessary and will be provided in this article.
Materials and methods
Electronic searches
Epidemiologic information on larynx cancer was obtained with electronic searches in the Global Health Data Exchange (GHDx) database, which is a large worldwide repository of health-related information provided by the Institute for Health Metrics and Evaluation (11). The Global Burden of Diseases, Injuries, and Risk Factors Study 2017 (GBD 2017) database now includes comprehensive data on as many as 354 human diseases from 195 countries and territories, in the period between 1990−2017 (12).
Some specific electronic searches were hence carried out in the GHDx database for “larynx cancer” [International Classification of Diseases (ICD) codes C32−C32.9, Z85.21, which include malignant neoplasm of intrinsic larynx, laryngeal commissure and vocal cords, encompassing squamous cell, all primary malignant neoplasms of larynx, the most frequent of which is indeed squamous cell carcinoma]. In the GHDx database, disability for this cancer for all locations, by age, year, and sex was defined with DisMod-MR 2.1, by using a fixed effect logistic regression model to estimate with covariates for sex, categorical age, and the Healthcare Access and Quality index (HAQ index). After transforming the final GBD cancer mortality to incidence estimates, incidence was then combined with the relative yearly survival estimates up to 10 years. Further information is available in the GBD 2017 publication (12).
The electronic searches were complemented with additional epidemiologic measures such as “metric” (i.e., “number”), “measure” (i.e., “incidence”, “prevalence”, “DALYs” and “deaths”), “year” (i.e., from “1992” to “2017”), “sex” (i.e., “male” and “female”), “age” (i.e., from “<1 year” to “95 plus”) and “location” (i.e., “World Health Organization Regions”). Mortality projections were obtained from the health statistics and information systems maintained by the World Health Organization (WHO) (13).
The study was performed in accordance with the Declaration of Helsinki and under the terms of relevant local legislation. Ethics board approval is unnecessary at the local institution (University of Verona) for articles based on free scientific databases searches.
Statistical analysis
Information obtained from these our electronic searches was imported into Microsoft Excel (Microsoft, Redmond, WA, USA) and then analyzed with Analyse-it (Vertion 2.30, Analyse-it Software Ltd, Leeds, UK) and MedCalc statistical software (MedCalc Software, Ostend, Belgium). Simple (Pearson’s correlation) regression analyses were used for assessing potential associations among different epidemiologic measures, whilst the risk was expressed as odds ratio (OR) and its relative 95% confidence interval (95% CI).
Results
Global epidemiology
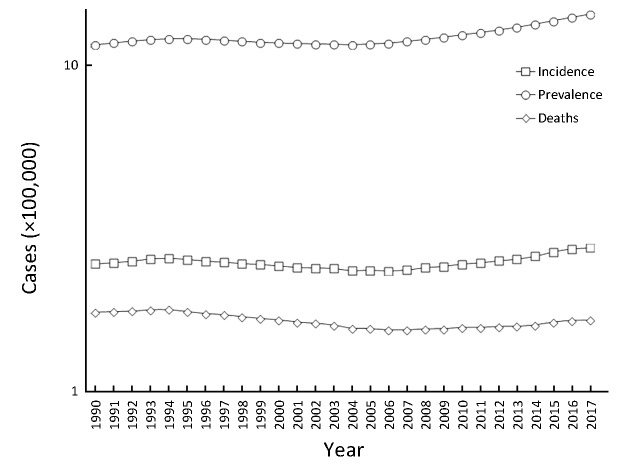
The global burden of larynx cancer during the past 3 decades is shown in Figure 1. A total number of 210,606 new cases of larynx cancer have been diagnosed in 2017 (2.76 new cases per 100,000 inhabitants) worldwide, with a prevalence in that same year of 1.09 million cases (14.33 cases per 100,000 inhabitants), accounting for as many as 126,471 deaths (1.66 per 100,000 inhabitants) and 3.28 million DALYs (0.13% of all DALYs). The incidence and prevalence have both increased by 12.0% and 23.8%, respectively during the past 3 decades, whilst mortality has declined by approximately 5%. Among all types of cancer, larynx malignancies are listed as the 22nd in terms of incidence (0.89% of all cancers), the 18th in terms of prevalence (1.44% of all cancers), the 18th in terms of DALYs (1.50% of all cancers) and mortality (1.39% of all cancer deaths). According to the GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 86.5% of larynx cancer patients are in primary therapy or controlled phase, 7.3% are in metastatic stage, 1.0% are in terminal stage, whist 5.1% are surviving with laryngectomy (12).
1. Worldwide incidence, prevalence, cause-specific disability-adjusted life years (DALYs) and mortality of laryngeal cancer recorded during the last 3 decades.
Gender and age epidemiology
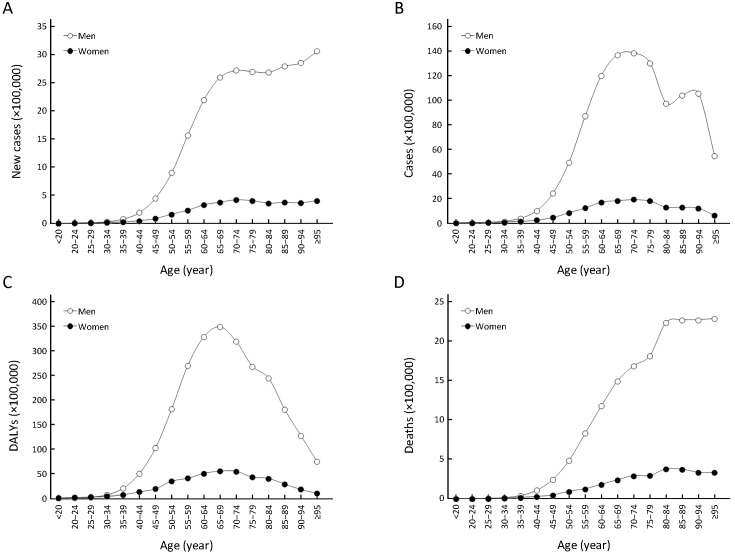
The worldwide age and sex distribution of larynx cancer is shown in Figure 2. All the epidemiologic measures of this malignancy are substantially higher in men. More specifically, men have an over 5-fold higher incidence (4.64 vs. 0.86 per 100,000; OR, 5.4; 95% CI, 4.3−6.8; P<0.001), prevalence (24.40vs. 4.18 per 100,000; OR, 5.8; 95% CI, 5.3−6.5; P<0.001) and mortality (2.75vs. 0.55 per 100,000; OR, 5.0; 95% CI, 3.7−6.7; P<0.001), and are also 5-fold more likely to have severe disability for larynx cancer (DALYs, 71.27vs. 14.36 per 100,000; OR, 5.0; 95% CI, 4.7−5.3; P<0.001). Interestingly, the gap of incidence and death between men and women has been narrowing during the past 3 decades (i.e., OR from 5.8 to 5.4 for incidence and from 5.3 to 5.0 for mortality, respectively). Concerning the age distribution, a constant increase of all the epidemiologic measures can be seen after the age of 35 years in both sexes. The incidence of larynx malignancies peaks after the age of 65 years in both sexes and then remains stable at around 25−30 new cases per 100,000 in men and around 4 cases per 100,000 in women. The prevalence follows a similar trend, reaching the peak at around 60−80 years of age in both sexes (i.e., 120−140 cases per 100,000 in men and 17−20 cases per 100,000 in women, respectively), but then gradually declining afterwards. The trend of deaths mirrors exactly that of incidence, but reaches the peak at the age of 80 years in both sexes and then remains fairly stable afterwards (i.e., about 23 per 100,000 in men and about 3 per 100,000 in women). The larynx cancer-related disability (i.e., DALYs) peaks in the age of 60−75 years old in both sexes (approximately 350 per 100000 in men and approximately 56 per 100,000 in women), but then sharply declines afterwards.
2. Worldwide age and sex distribution of larynx cancer. Worldwide incidence (A), prevalence (B), cause-specific disability-adjusted life years (DALYs) (C) and mortality (D) of laryngeal cancer between sexes and across ages.
Geographic epidemiology
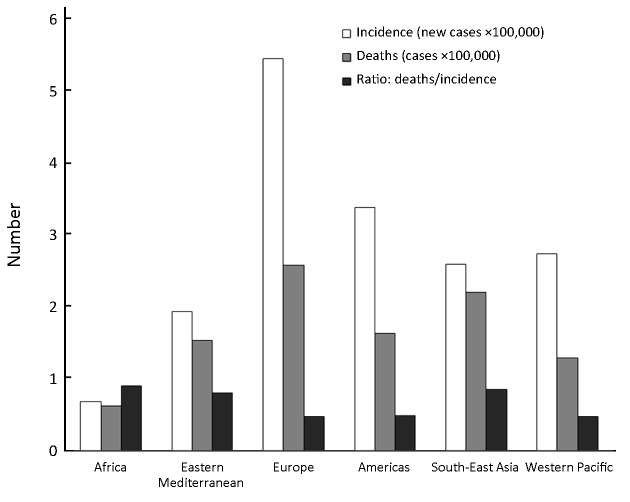
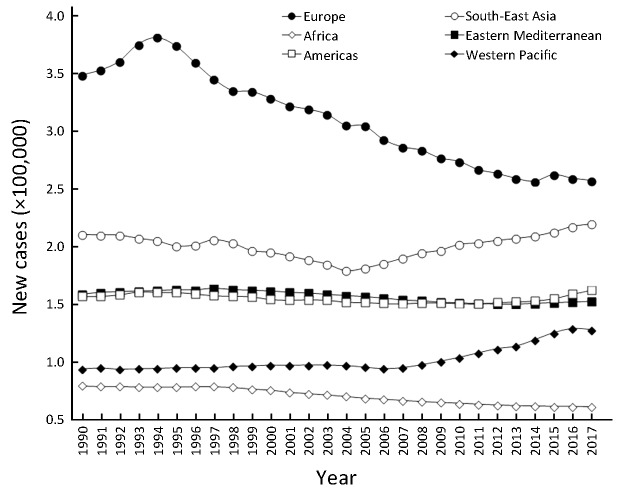
The geographic distribution of larynx cancer burden is shown in Figure 3. The current incidence appears the highest in Europe (5.45 new cases per 100,000), followed by Americas (3.37 new cases per 100,000), Western Pacific (2.73 new cases per 100,000), South-East Asia (2.59 new cases per 100,000) and Eastern Mediterranean (1.93 new cases per 100,000), whilst the lowest is in Africa (0.68 new cases per 100,000). The mortality follows a similar pattern, with the highest number of deaths for larynx cancer recorded in Europe (2.57 per 100,000), then followed by South-East Asia (2.20 per 100,000), Americas (1.62 per 100,000), Eastern Mediterranean (1.53 per 100,000), Western Pacific (1.28 per 100,000) and Africa (0.61 per 100,000). Notably, the ratio between death and incidence of larynx cancer is considerably higher in Africa (0.90) and South-East Asia (0.85), intermediate in Eastern Mediterranean (0.79), whilst is nearly 50% lower in Americas (0.48), Western Pacific and Europe (0.47). Interestingly, although the incidence of laryngeal cancer in Europe and Africa has declined by approximately 25%, in all the other WHO regions the incidence has remained virtually stable, except in Western Pacific (+36% increase) (Figure 4).
3. Incidence and mortality of laryngeal cancer across different geographic areas.
4. Incidence of laryngeal cancer across different geographic areas recorded during the last 3 decades.
Risk factors
According to GHDx data, cigarette smoking and alcohol abuse contribute for about 60% and 30% of the overall mortality for laryngeal cancers, respectively, whilst the contribution of occupational exposure (i.e., asbestos or sulfuric acid) is estimated at around 6%.
Future projections
The projection of global mortality between the year 2016 and 2060 according to WHO data (13), reported globally for mouth and oropharynx cancers, is predicted to escalate from 332,561 deaths in 2016 (4.46 per 100,000) to 439,212 in 2030 (5.14 per 100,000), 563,115 in 2045 (5.93 per 100,000), up to approximately 680,000 in 2060 (6.66 per 100,000), thus exhibiting an approximately 50% relative increase and displaying a virtually perfect linear progression (r=1.000; 95% CI, 0.993−1.000; P<0.001).
Discussion
Laryngeal cancer is an important oncologic entity, whose prognosis strictly depends on accurate and especially timely diagnosis. Regarding the risk factors, a recent case series published by Menach et al. revealed that as many as 66% of laryngeal squamous cell carcinoma patients were current cigarette smokers, but nearly 75% had smoked for over 30 years before the diagnosis (7). Alcohol consumption was also found to be commonplace (i.e., >75% of all cases), whilst heavy alcohol intake was found to be associated with a 6-fold higher risk for this type of cancer. Similar figures have recently been published by Markou et al, who reviewed the clinical history of 1,104 patients with malignant laryngeal tumors (98.4% of which are squamous cell carcinomas) (5), and reported that 87% were current cigarette smokers, 43% were consuming alcohol on daily basis and nearly 36% had positive family history for malignancy. Another recent study based on 106 consecutive patients with laryngeal squamous cell carcinoma revealed that the prevalence of HPV infection was 13.2%, the vast majority of which attributable to HPV-16 (14).
The survival of patients with very advanced stage of larynx cancer is still dramatically poor, in part attributable to delayed diagnosis (15). Beside change or hoarseness of voice in patients with cancers involving the vocal cords, other symptoms are mostly vague and poorly specific and may be often underestimated, thus favoring local tumor growth and distance spread before a final diagnosis can be made. This would inevitably reduce efficacy of treatment and lead to a more unfavorable outcome (16). Continuous epidemiologic monitoring, based on data obtained from accurate and reliable sources, shall hence be seen as a mainstay for addressing reinforced preventive and early diagnostic interventions in categories of patients at higher risk for this type of malignancy.
The results of our updated analysis on the GHDx repository, which is now universally recognized as one of the most comprehensive and reliable healthcare database (17), attest that larynx cancer still poses a considerable clinical, societal and economic burden worldwide, and that its biology appears to be associated with some epidemiologic variables. Although both incidence and prevalence of laryngeal cancer have considerably increased during the past decades, this escalating epidemiologic trend has not been reflected by a similar increase of mortality (Figure 1). This evidence, which confirms earlier figures published by Chatenoud et al. in some European countries (8), may be explained by some recent improvements in curative management of this malignancy, especially those based on transoral robotic surgery (TORS), transoral videolaryngoscopic surgery (TOVS), along with improved radiotherapic treatments and targeted chemotherapy by means of epithelial growth factor receptor (EGFR) inhibitors (1,18). Notably, although the epidemiologic trend recorded over the past 3 decades shows laryngeal cancer mortality has marginally declined during the years 2004−2009, a constant (virtually linear: r=0.96; 95% CI, 0.81−0.99; P<0.001) progression could be observed during the past 10 years. This recent escalation is especially alarming and is in keeping with WHO data, estimating that deaths for mouth and oropharynx cancers will further increase by 50% in the year 2060. Although a definitive explanation cannot be easily found, it is conceivable that the growing incidence of this cancer in Western Pacific and South-East Asia will have a strong impact on the worldwide burden, since exposure to the two major risk factors for larynx cancer (i.e., cigarette smoking and alcohol) is exponentially increasing in these regions (19,20), where care access and efficiency are also lower than in other worldwide regions. In agreement with previous data, the epidemiologic burden of laryngeal cancer remains approximately 5-fold higher in men, although the gap between sexes has recently narrowed, and this is probably due to a recent lifestyle change in women, whereby the worldwide prevalence of cigarette smoking and (heavy) alcohol drinking is considerably growing in females (3). As concerns the age-related distribution, larynx cancer shall be considered a malignancy whose incidence, prevalence and mortality increase in parallel with ageing, reaching a peak and then an ensuing plateau after the age of 60 years.
The geographical distribution of laryngeal cancer also reveals some important aspects. Europe remains the most prevalent continent for this type of malignancy, whilst the epidemiologic burden in Africa remains low. This is not really unexpected, since a recent analysis of the scientific literature revealed that the majority of patients with head and neck squamous cell carcinoma were not exposed to cigarette smoking and alcohol (8). Nevertheless, our data shows that the mortality (i.e., the ratio between incidence and deaths) in Africa is the highest among the six WHO regions (Figure 3), thus confirming that the therapeutic options for this and other types of cancers remain limited in this continent (8). As concerns the risk factors, the GDB 2017 Collaborators have acknowledged tobacco, alcohol and exposure to asbestos or sulfuric acid as major predisposing conditions (12). Among these, cigarette smoking and daily alcohol consumption would contribute to about 90% of the overall worldwide mortality for larynx cancer, which calls for urgent healthcare interventions aimed at limiting population exposure to these important carcinogens.
Conclusions
Our data shows that laryngeal cancer still poses a high clinical and societal burden, following a temporal trend that is not expected to reverse soon.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Steuer CE, El-Deiry M, Parks JR, et al An update on larynx cancer. CA Cancer J Clin. 2017;67:31–50. doi: 10.3322/caac.21386. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer Facts and Figures 2019. Atlanta: American Cancer Society, 2019. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf
- 3.Ciolofan MS, Vlăescu AN, Mogoantă CA, et al Clinical, histological and immunohistochemical evaluation of larynx cancer. Curr Health Sci J. 2017;43:367–75. doi: 10.12865/CHSJ.43.04.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoffman HT, Porter K, Karnell LH, et al Laryngeal cancer in the United States: changes in demographics, patterns of care, and survival. Laryngoscope. 2006;116:1–13. doi: 10.1097/01.mlg.0000236095.97947.26. [DOI] [PubMed] [Google Scholar]
- 5.Markou K, Christoforidou A, Karasmanis I, et al Laryngeal cancer: epidemiological data from Northern Greece and review of the literature. Hippokratia. 2013;17:313–8. [PMC free article] [PubMed] [Google Scholar]
- 6.Issa MR, Samuels SE, Bellile E, et al Tumor volumes and prognosis in laryngeal cancer. Cancers (Basel) 2015;7:2236–61. doi: 10.3390/cancers7040888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menach OP, Patel A, Oburra HO Demography and histologic pattern of laryngeal squamous cell carcinoma in Kenya. Int J Otolaryngol. 2014;2014:507189. doi: 10.1155/2014/507189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chatenoud L, Garavello W, Pagan E, et al Laryngeal cancer mortality trends in European countries. Int J Cancer. 2016;138:833–42. doi: 10.1002/ijc.29833. [DOI] [PubMed] [Google Scholar]
- 9.Jones TM, De M, Foran B, et al Laryngeal cancer: United Kingdom National Multidisciplinary guidelines. J Laryngol Otol. 2016;130:S75–S82. doi: 10.1017/S0022215116000487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Keeping ST, Tempest MJ, Stephens SJ, et al The cost of oropharyngeal cancer in England: A retrospective hospital data analysis. Clin Otolaryngol. 2018;43:223–9. doi: 10.1111/coa.12944. [DOI] [PubMed] [Google Scholar]
- 11.Institute for Health Metrics and Evaluation. Global Health Data Exchange. Available online: http://ghdx.healthdata.org/gbd-results-tool
- 12.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Projections of mortality and causes of death, 2016 to 2060. Available online: https://www.who.int/healthinfo/global_burden_disease/projections/en/
- 14.Chen WC, Chuang HC, Lin YT, et al Clinical impact of human papillomavirus in laryngeal squamous cell carcinoma: a retrospective study. PeerJ. 2017;5:e3395. doi: 10.7717/peerj.3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Britt CJ, Gourin CG Contemporary management of advanced laryngeal cancer. Laryngoscope Investig Otolaryngol. 2017;2:307–9. doi: 10.1002/lio2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gourin CG, Conger BT, Sheils WC, et al The effect of treatment on survival in patients with advanced laryngeal carcinoma. Laryngoscope. 2009;119:1312–7. doi: 10.1002/lary.20477. [DOI] [PubMed] [Google Scholar]
- 17.Das A Cancer registry databases: an overview of techniques of statistical analysis and impact on cancer epidemiology. Methods Mol Biol. 2009;471:31–49. doi: 10.1007/978-1-59745-416-2_2. [DOI] [PubMed] [Google Scholar]
- 18.Hay A, Nixon IJ. Recent advances in the understanding and management of oropharyngeal cancer. F1000Res. 2018;7.pii: F1000 Faculty Rev-1362.
- 19.West R Tobacco smoking: Health impact, prevalence, correlates and interventions. Psychol Health. 2017;32:1018–36. doi: 10.1080/08870446.2017.1325890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Global status report on alcohol and health 2018. Geneva: World Health Organization, 2018.