Abstract
Background
Vaginismus is an involuntary contraction of the vaginal muscles which makes sexual intercourse difficult or impossible. It is one of the more common female psychosexual problems. Various therapeutic strategies for vaginismus, such as sex therapy and desensitisation, have been proposed, and uncontrolled case series appear promising.
Objectives
To assess the effects of different interventions for vaginismus.
Search methods
We searched the Cochrane Depression, Anxiety and Neurosis Group's Specialised Register (CCDANCTR‐Studies and CCDANCTR‐References) to August 2012. This register contains relevant randomised controlled trials from: The Cochrane Library (all years), EMBASE (1974 to date), MEDLINE (1950 to date) and PsycINFO (1967 to date). We searched reference lists and conference abstracts. We contacted experts in the field regarding unpublished material.
Selection criteria
Controlled trials comparing treatments for vaginismus with another treatment, a placebo treatment, treatment as usual or waiting list control.
Data collection and analysis
The review authors extracted data which we verified with the trial investigator where possible.
Main results
Five studies were included, of which four with a total of 282 participants provided data. No meta‐analysis was possible due to heterogeneity of comparisons within included studies as well as inadequate reporting of data. All studies were considered to be at either moderate or high risk of bias. The results of this systematic review indicate that there is no clinical or statistical difference between systematic desensitisation and any of the control interventions (either waiting list control, systematic desensitisation combined with group therapy or in vitro (with women under instruction by the therapist) desensitisation) for the treatment of vaginismus. The drop‐out rates were higher in the waiting list groups.
Authors' conclusions
A clinically relevant effect of systematic desensitisation when compared with any of the control interventions cannot be ruled out. None of the included trials compared other behaviour therapies (e.g. cognitive behaviour therapy, sex therapy) to pharmacological interventions. The findings are limited by the evidence available and as such conclusions about the efficacy of interventions for the treatment of vaginismus should be drawn cautiously.
Keywords: Female; Humans; Bibliotherapy; Bibliotherapy/methods; Desensitization, Psychologic; Desensitization, Psychologic/methods; Exercise Therapy; Exercise Therapy/methods; Hypnosis; Pelvic Floor; Randomized Controlled Trials as Topic; Vaginismus; Vaginismus/therapy; Waiting Lists; Watchful Waiting
Plain language summary
Interventions for vaginismus
Vaginismus is when the muscles in the vagina tighten and prevent a woman having (vaginal) intercourse. It can cause distress, relationship problems and also infertility. Many treatments have been tried including sex therapy, education, hypnosis and drug treatments. Sex therapy may involve relaxation techniques and gradually inserting a dilator or finger into the vagina (this may be called systematic desensitisation).
This review found five poor to moderate quality studies, of which four with a total of 282 women provided data. There was not enough evidence to say if systematic desensitisation worked better than another treatment. Further studies including larger numbers of women are needed to show if systematic desensitisation if effective for the treatment of women with vaginismus.
Background
Description of the condition
Vaginismus is the recurrent or persistent involuntary contraction of the musculature of the vagina, which interferes with sexual intercourse. It causes marked distress or interpersonal difficulty amongst affected women (APA 1994) and is moderately correlated with stress levels (r2 = 0.47, P = 0.009, Bodenmann 2006). As with other sexual dysfunctions it can lead to marital and interpersonal problems (Catalan 1981; Frank 1976), and it is likely to result in infertility. Vaginismus has been associated with a high risk of disruption of marital relationships, anxiety, depression and low self esteem.
Vaginismus can be classified as either primary or secondary. Primary vaginismus occurs when the woman has never been able to have penetrative intercourse because of the involuntary contraction of her vaginal muscles. It is sometimes referred to as 'unconsummated marriage'. Secondary vaginismus occurs when a woman has previously been able to have intercourse but is no longer able to be penetrated, because of the involuntary muscle spasms. Secondary vaginismus may be situational and is often associated with dyspareunia (i.e. pain during sex), indicating a need for a specific pain management strategy in its treatment. The recent proposal for the 5th Diagnostic and Statistical Manual of Mental Disorders (DSM‐5) is to scrap the traditional differentiation between vaginismus and dyspareunia and to collapse these two categories into one. This has not yet been adopted and if it is it would have significant implications for evaluating outcome (Binik 2010).
Vaginismus is thought to be one of the most common female psychosexual dysfunctions. A study of 301 randomly selected women in Ghana found that 205 (68.1%) reported symptoms of vaginismus (Amidu 2010). Among Italian women phoning a helpline for sexual concerns 9% were enquiring about vaginismus (Simonelli 2010). A study of women attending a family planning clinic in Iran found that 12% of women suffered vaginismus at least 50% of the time with 4% always suffering vaginismus (Shokrollahi 1999). A study of 54 women attending a psychiatric outpatient department in Turkey found that 41 (75.9%) reported vaginismus, of which 36 reported a lifelong problem (Dogan 2009). A case‐control study in Mexico found that 35 women (9.1%) had vaginismus which met the DSM‐IV‐TR criteria (Bravo 2005). A survey of 49 gynaecologists in Holland found that vaginismus accounted for 4.2% of all sexual problems or concerns seen over a one‐week period (Frenken 1987). Studies of referrals to sexual dysfunction clinics in the UK and the USA indicate a prevalence rate of between 5% and 17% of female patients (Bancroft 1976; Catalan 1990; Hawton 1985; Hirst 1996; Masters 1970; Renshaw 1988). The lowest estimate (5%) comes from Renshaw who used the most stringent criteria and excluded patients who had vaginismus together with another sexual dysfunction (Renshaw 1988). Is important to mention that the variety in the figures for the prevalence of vaginismus is possibly due to the unclear and differing definitions used in the studies.
Description of the intervention
The ideal treatment for vaginismus must access the complex interplay between the biological, emotional, psychological and relational components of women's and couples' lives (Basson 2003). Considerations in forming and maintaining an effective psychotherapeutic treatment relationship should include an investigation of: a) variations in presenting sexual disorders, aetiologies, concurrent symptoms and behaviour; b) chronological age, sexual developmental history, risk factors and life stage; c) socio cultural and familiar factors (e.g. gender identity, ethnicity, race, social class, religion, disability status, family structure and sexual orientation); d) environmental context (e.g. health care disparities) and stressors (e.g. unemployment, major life events); and e) personal sexual preferences, values and preferences related to treatment (e.g. goals, beliefs, world views and treatment expectations).
Psychological therapies
Psychological therapies have to be conducted face to face and a minimum number of sessions is required. For vaginismus, these include combinations of systematic desensitisation including the Masters and Johnson method (in vivo, imaginal or both) together with the use of graded dilators; sex therapy including sex education (individual, conjoint or with a surrogate partner), in which a gradual approach is taken to overcoming the disorder, including education, homework assignments and cognitive therapy (Crowley 2009; Hawton 1985; Ng 1993; O'Donohue 1997; Rosen 1995); relaxation therapy; hypnotherapy (Al‐Sughayir 2005; Lew Starowicz 1982) or pelvic‐perineal re‐education combined within cognitive behaviour therapy (Bergeron 2003),
The Masters and Johnson method is the basis for most forms of psychological therapy for vaginismus. It is relatively brief, problem‐focused and directive. Detailed information about relevant human anatomy (structure) and physiology (functioning) is provided to the woman and partner. In the original form Masters and Johnson conducted their work as a male‐female pair of co‐therapists; hence, traditional sex therapy involved four individuals (the co‐therapists and the client couple). Additionally, the intervention consisted of direct behavioural exercises, including prescription of non‐demand pleasuring, or 'sensate focus', wherein the objective was to (re)experience sexual pleasure in the absence of anxiety from perceptions of performance demand or excessive self monitoring of sexual performance.
Over the past decade or so, the types of cases commonly seen in sex therapy clinics have changed dramatically from the earliest days of contemporary sex therapy. Recently this programme was modified by some sexologists and includes the systematic desensitisation technique (LoPiccolo 1994). Flooding, as used in Jarrousse 1986, is a more focused version of desensitisation. Flooding is also a method used to overcome phobias and uses a technique based on Pavlov's classical conditioning that uses exposure. There are different forms of exposure, such as imaginal exposure, virtual reality exposure and in vivo exposure. A patient is confronted with a situation in which the stimulus that provoked the original trauma is present. It involves total immersion in the therapy and women and partners are not allowed to progress until they have completed the exercises satisfactorily.
Pharmacological treatments
Other approaches may include pharmacotherapy, including benzodiazepines or antidepressants in combination with either relaxation therapy, interviews, or both (Mikhail 1976) and botulinum toxin injections (Brin 1997; Pacik 2009; Shafik 2000).
The use of antidepressants (tricyclics or venlafaxine) or anticonvulsants (usually carbamazepine or gabapentin) has been tried, however resolution with these drugs appears infrequent. The starting dose of amitriptyline and other tricyclic antidepressants is low (10 mg) but can be gradually increased to 40 to 60 mg daily, as tolerated (Crowley 2006)
Anxiolytic medication, such as diazepam, in combination with psychological therapy has been the most commonly used pharmacological intervention. Medication is most often used in the case of patients who do not respond adequately to psychological therapies alone and have high anxiety levels.
Local anaesthetics, such as lidocaine gel, have been proposed as a form of treatment. Muscle spasms may be due to the repeated pain experienced with vaginal penetration and, hence, the use of a topical anaesthetic aimed at reducing the pain is hypothesised to resolve the spasm. This causal relationship was disputed by a recent study that showed that the spasm‐based definition of vaginismus is not adequate as a diagnostic marker for the condition. Pain and fear of pain, pelvic floor dysfunction and behavioural avoidance need to be included in a multidimensional reconceptualisation of vaginismus (Reissing 2004).
Botulinum toxin, a temporary muscle paralytic, has been recommended in the treatment of vaginismus with the aim of decreasing the hypertonicity of the pelvic floor muscles. The use of botulism toxin (150 to 400 units of botulism toxin type A injected in the levator ani at three points) is an experimental intervention and no randomised controlled trials (RCTs) exist.
How the intervention might work
After complete psychosexual assessments considering all the aetiological and predisposing factors that could be involved in the case (sexual complaint, the sexual experience and significant events in the sexual education of participants and partners), the most appropriate intervention is then chosen. The assumption behind psychological therapy is that when women learn about vaginismus they begin to develop new sexual management strategies to deal with fear of sexual penetration, avoidance of sexual activity and unwillingness to discuss sex with a partner. Psychological therapy can be conducted in an individual or couple format. Psychological interventions are often based on the notion that vaginismus results from marital problems, negative sexual experiences in childhood or a lack of sexual education. Generally, in individual therapy, the treatment is to identify and resolve underlying psychological problems that could be causing the disorder. In couples therapy, vaginismus is conceptualised as a problem for the couple and the treatment tends to focus on the couple's sexual history and any other problems that may be occurring in the relationship. Pelvic floor muscle dysfunction has been suggested as a predisposing factor in the development of vaginismus, and strategies to reduce the hypertonicity and muscle control (Jacobson 1938) may be undertaken in combination with psychological therapy.
Cognitive therapy alone or in combination with pelvic perineal re‐education is intended to modify maladaptive sexual 'scripts' (some forms of cognitive distortions, e.g. 'my vagina is too tight', 'I'm afraid to experience pain and bleeding') that may interfere with sexual function. From a cognitive perspective, fear of penetration in women with vaginismus is maintained through the effect of avoidance behaviour on erroneous cognitions (Hawton 1986). The aim of the therapy is to provide an empathetic, supportive clinician‐patient relationship, reduce or eliminate performance anxiety and fear of penetration, and help gain sexual confidence (Kabakci 2003).
Behaviour therapy in combination with the Masters and Johnson technique (Masters 1970) aims to change dysfunctional feelings and attitudes and to help women to develop healthier and more effective patterns of sexual behaviour (Hawton 1990). Behavioural approaches vary, however; they focus mostly on how some behaviours may accidentally get 'rewarded' within one's environment, contributing to an increase in the frequency of these thoughts and behaviours
Systematic desensitisation (in vivo, imaginal or both), together with the use of graded dilators, is a behaviour therapy technique often used for the treatment of vaginismus in which deep muscle relaxation and gradually inserting a dilator or finger into the vagina is used to reduce the anxiety and fear associated with penetration (Rosen 2000). In the behavioural model of vaginismus, the vaginal reaction represents a conditioned fear response to certain (sexual) stimuli that can be overcome by exposure therapy. Women with vaginismus should thus be able to achieve intercourse after fear reduction. This might be accomplished by reducing avoidance behaviour and by establishing prolonged exposure to the feared stimuli (van de Wiel 1990).
Relaxation therapy uses graduated vaginal dilators to help gain control over and relax muscles and stretch the vagina (Basson 2003).
Bibliotherapy is an additional alternative that may be use during the psychological treatment and incorporates appropriate books or other written materials. The goal of bibliotherapy is to broaden and deepen the patient's understanding of the disorder that requires treatment. The written materials may educate the client about the disorder itself or be used to increase the patient's adherence to the treatment (Basson 2003).
Sexual therapy and education provides information about human sexual anatomy and functional aspects, sexual reproduction and sexual intercourse. In vaginismus therapy the goal of sexual education is to describe biological and psychological mechanisms held responsible for the origin and maintenance of the condition (Hawton 1986a).
Hypnotherapy is a therapeutic intervention usually conducted once a week for approximately 60 minutes. It aims to encourage thoughts (pleasurable sexual mental images) of more favourable outcomes and experiences during intercourse. Verbal interaction is facilitated in order to understand whether the positive suggestions could be implemented in a woman's sexual life. During hypnosis, the problems causing vaginismus may be explored, or an attempt may even be made to reverse feelings or fears that could be causing the disorder. Exploring causal relationships, as well as suggesting to the woman she can overcome her vaginal muscle spasms, can be very effective for certain patients (Fuchs 1980).
Why it is important to do this review
As vaginismus is a relatively common dysfunction, a significant cause of personal distress and difficulty in sustaining intimate relationships, and a cause of infertility, it is important to examine the efficacy of therapies for this condition. Indeed there are many reasons for the relevance of this review: women with vaginismus report decreased self esteem, difficulty in establishing relationships and a negative impact on their quality of life (Basson 2003). The effect of vaginismus on the individual and their sexual relationships is usually highly significant. Vaginismus is also associated with high rates of unconsummated marriage and divorce.
A literature review concluded that sex therapy was more effective than psychological therapy for most female sexual dysfunctions but concluded that most of the studies had some methodological shortcomings (O'Donohue 1997). That review did not identify any controlled trials specifically for the treatment of vaginismus. An overview of vaginismus (Crowley 2006) and a later review (Crowley 2009) found that systematic desensitisation involving insertion training appears to be effective in uncontrolled studies.
This is an update of a Cochrane review first published in 2001 and previously updated in 2005 (McGuire 2001). The findings in 2005 were that systematic desensitisation appears to be more effective than waiting list or control treatment conditions, but may also result in more participants dropping out of treatment. Since the 2005 update no additional studies have been identified but new methodologies including 'Risk of bias' assessment have been incorporated into this update.
Objectives
To assess the effects of different interventions for vaginismus.
Methods
Criteria for considering studies for this review
Types of studies
Studies eligible for inclusion were:
randomised (parallel, cluster‐randomised and cross‐over trials); or
quasi‐randomised controlled trials (where allocation is by alternation or by some other non‐random method of selection, e.g. date of birth).
Studies could be either published or unpublished.
Types of participants
Trial participants were women aged over 16 years, in any setting, with a primary diagnosis of vaginismus according to the International Classification of Diseases 10th edition (ICD‐10) (WHO 1992) or the Diagnostic and Statistical Manual (DSM‐IV) (APA 1994; APA 2000), of any ethnic group and nationality, regardless of co‐morbidities or use of concomitant medications for other diseases.
Exclusion criteria
Studies including women with a prior diagnosis of either dyspareunia, pelvic floor muscle dysfunction, vaginal lesions and tumours, major depressive disorder, psychotic disorder, substance‐related disorder or post‐traumatic‐stress disorder related to the genitals (e.g. as a sequel to sexual abuse). Studies that include populations with different sexual dysfunctions will be excluded unless participants were stratified according to diagnosis and data is available of those women with vaginismus.
We have excluded secondary vaginismus as this is often a sequelae to other pelvic pain disorders which have since been resolved.
Types of interventions
Experimental interventions
Face to face psychological therapies of any duration (including systematic desensitization, sex therapy, sex education, behavior therapy, cognitive therapy. relaxation therapy; hypnotherapy or pelvic‐perineal re‐education combined within cognitive behaviour therapy)
Pharmacological treatment (including anti‐depressants, anxiolytics, local anaesthetics or botulinum toxin A)
Combinations of pharmacological treatments and psychological therapies
Control Interventions
Bibliotherapy
Placebo
Non‐intervention/waiting list control/treatment as usual
Types of outcome measures
Primary outcomes
Effectiveness
Successful outcome was defined as the ability to complete sexual intercourse or (where measured) the successful completion of a gynaecological examination including a cervical smear test
Acceptability
Drop‐out
Secondary outcomes
Changes in the status of vaginismus, measured by validated questionnaires (e.g. behavioural functioning (Penetration Behavior Questionnaire, PBQ), Fear of Sexuality Questionnaire (FSQ), Golombok Rust Inventory of Sexual Satisfaction GRISS)
Patient (or partner, or both) reports of improvement in satisfaction with sexual intercourse
Change in GRIMS Inventory (Golombok Rust Inventory of Marital State), Maudsley Marital Questionnaire (MMQ)
Satisfaction with the treatment
Sexual Interaction Inventory (SII), Female Sexual Function Index (FSFI)
Self rating Anxiety Scale (SAS)
Generic quality of life
Relapse rates
Search methods for identification of studies
Electronic searches
Cochrane Depression, Anxiety and Neurosis Group (CCDAN) Specialised Register (CCDANCTR)
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintain two clinical trials registers at their editorial base in Bristol, UK, a references register and a studies‐based register. The CCDANCTR‐References Register contains over 30,000 reports of randomised controlled trials in depression, anxiety and neurosis. Approximately 65% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual. Please contact the CCDAN Trials Search Co‐ordinator for further details. Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950 ‐), EMBASE (1974 ‐) and PsycINFO (1967 ‐); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and review‐specific searches of additional databases. Reports of trials are also sourced from international trials registers c/o the World Health Organization’s trials portal (ICTRP), drug companies, the handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCDAN's generic search strategies can be found on the Group's website.
We searched the CCDANCTR‐Studies Register (to 30 August 2012) using the following search terms: Diagnosis = Vaginismus
We searched the CCDANCTR‐References Register (to 30 August 2012) using the following free‐text term: Vaginism*
Search strategies for MEDLINE, PsycINFO, EMBASE and CINAHL appear in Appendix 1. We conducted these additional searches in September 2009 when the CCDANCTR was out of date due to a changeover of staff at the editorial base.
International trial registries
We also searched the WHO Trials portal (ICTRP) and ClinicalTrials.gov (to 30 August 2012) to identify any additional unpublished or ongoing studies.
Searching other resources
Handsearching
We handsearched the following journals.
Journal of Sex and Marital Therapy (1974 to September 2009)
Archives of Sexual Behavior (1990 to September 2006)
Journal of Sex Research (1978 to 1996)
Sexual and Relationship Therapy (previously 'Sexual and Marital Therapy') (1986 to 2009)
Sexual Dysfunction (1998 to 1999)
Reference lists
We searched the reference lists of relevant articles. We searched the Social Sciences and Science Citation Index for all included studies.
Personal contacts
We contacted the first author on all included studies and experts in the field for information regarding published and unpublished trials.
Data collection and analysis
We used the Review Manager 5.0 software developed by the Cochrane Collaboration (RevMan 5.0) to organise and analyse the results.
Selection of studies
Authors HM and TM independently inspected citations identified from the search. We ordered all potentially relevant reports this identified for reassessment. Where difficulties or disputes arose we asked KH for assistance/adjudication and if it was impossible to decide, we ordered full texts for assessment. This process was repeated for the assessment of the full texts. If it was impossible to resolve disagreements, we contacted the authors of the papers for clarification.
Data extraction and management
HM and TM used a standardised data extraction sheet (see Appendix 3) to collect data on methods, participants, intervention, adherence to treatment, outcome measurements and other relevant results of the studies, to provide a detailed descriptive analysis. In cases of disagreement TM adjudicated. The review authors independently extracted the data and entered data using RevMan 5. In cases where inadequate information was available within the papers, we contacted the investigators and asked them to supply additional information. Where no further usable data were provided, studies did not contribute to meta‐analyses.
Main comparisons
We planned the following treatment comparisons.
Psychological therapies versus treatment as usual, waiting list or no treatment
Pharmacological treatment in association with psychological therapies versus either alone
Pharmacological treatment in association with psychosocial treatment versus treatment as usual, waiting list or no treatment
Assessment of risk of bias in included studies
HM and TM independently assessed risk of bias using the tool described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). This tool encourages consideration of:
how the sequence was generated;
how allocation was concealed;
the integrity of blinding of outcome assessors;
the completeness of outcome data;
selective reporting; and
other potential sources of bias.
We provided a description of what was reported to have happened in each study and made a judgement on the risk of bias for each domain within and across studies, based on the following three categories: low risk of bias, unclear risk of bias and high risk of bias.
Two review authors (TM and HM) independently assessed the risk of bias in the selected studies. Any disagreement was discussed with a third review author (KH). Where necessary, we contacted the authors of the studies for further information. All 'Risk of bias' data are presented graphically and described in the text. We used allocation concealment as a marker of trial quality for the purposes of undertaking sensitivity analyses.
Measures of treatment effect
Dichotomous outcomes
We analysed these outcomes by calculating risk ratios (RR) with 95% confidence intervals (CI) and presented them in this form for ease of interpretation.
Continuous outcomes
Where studies used the same outcome measure for comparison, we pooled data by calculating the mean difference (MD). Where different measures were used to assess the same outcome, we pooled data using the standardised mean difference (SMD) with 95% confidence intervals.
Change versus endpoint data
We used change data only when endpoint data were not available.
Unit of analysis issues
Studies with more than two intervention arms can pose analytical problems in pair‐wise meta‐analysis. Where studies had two or more active treatment arms to be compared against treatment as usual, we managed data as follows.
Continuous data
We pooled means, standard deviations (SDs) and number of participants for each active treatment group across treatment arms as a function of the number of participants in each arm to be compared against the control group (Higgins 2008; Higgins 2008a; Law 2003).
Dichotomous data
We collapsed active treatment groups into a single arm for comparison against the control group, or split the control group equally between the treatment groups.
Dealing with missing data
Missing participants
Dichotomous data
We analysed all data on the basis of the intention‐to‐treat (ITT) principle: drop‐outs were included in this analysis. Where participants withdrew from the trial before the endpoint, it was assumed that their condition would have remained unchanged if they had stayed in the trial. This is conservative for outcomes related to response to treatment (because these participants will be considered to have not responded to treatment). It is not conservative for adverse events, but we think that for the adverse events of interest in our review (see outcomes) a worst‐case scenario is clinically unlikely. When there were missing data and the method of 'last observation carried forward' (LOCF) had been used to do an ITT analysis, then we used the LOCF data, with due consideration of the potential bias and uncertainty introduced. We did not perform a 'worst‐case' and 'best‐case' ITT analysis.
Continuous data
Concerning continuous data, the Cochrane Handbook recommends avoiding imputations of continuous data and suggests rather that the data must be used in the form in which they have been presented by the original authors. Whenever ITT data had been presented by the authors they were preferred to 'per protocol/completer' data sets. Furthermore, we acknowledge that all methods of imputation to deal with missing data introduce uncertainty about the reliability of the results. This depended on the degree of 'missingness', the pooled estimate of the treatment effect and the variability of the outcomes. We considered variation in the degree of missing data as a potential source of heterogeneity.
Missing statistics
When only the standard error (SE) or P values were reported, we calculated SDs according to Altman (Altman 1996). In the absence of supplemental data after requests to the authors, we calculated the SDs according to a validated imputation method (Furukawa 2006). We examined the validity of these imputations in the sensitivity analyses.
Assessment of heterogeneity
We quantified heterogeneity using the I2 statistic, which calculates the percentage of variability due to heterogeneity rather than chance. We expected, a priori, that there would be considerable clinical heterogeneity between studies and so I2 values in the range of 50% to 90% were considered to represent substantial statistical heterogeneity and we explored this further. However, the importance of the observed I2 will depend on the magnitude and direction of treatment effects and the strength of evidence for heterogeneity (Deeks 2008; Higgins 2003). Forest plots generated in RevMan 5 now also provide an estimate of tau2, the between‐study variance in a random‐effects meta‐analysis. To give an indication of the spread of true intervention effects we used the tau2 estimate to form an approximate range of intervention effects using the method outlined in section 9.5.4 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2008). This was undertaken for the primary outcomes only.
Assessment of reporting biases
As far as possible, we minimised the impact of reporting biases by undertaking comprehensive searches of multiple sources (including trial registries), increasing efforts to identify unpublished material, and including non‐English language publications.
We also assessed and identified outcome reporting bias in trials by recording all trial outcomes, planned and reported, and noting where there were missing outcomes. Where we found evidence of missing outcomes, we attempted to obtain any available data direct from the authors.
In addition, if a minimum of 10 studies were included, we planned to examine small study effects and potential publication bias using funnel plots.
Data synthesis
We employed the random‐effects model for analysis (DerSimonian 1986) which incorporates an assumption that the different studies are estimating different, yet related, intervention effects.
Subgroup analysis and investigation of heterogeneity
We planned to carry out subgroup analyses as follows.
Age of onset (women ≤ 40 years old versus ≥ 41 years old)
Diagnosis ‐ primary versus secondary vaginismus
Whether the partner took an active part in the therapy or not
Sensitivity analysis
We had planned to conduct the following sensitivity analyses.
Fidelity to treatment: studies that have not assessed fidelity to the psychological therapy model(s) under evaluation through assessment of audio or videotapes of therapy sessions were to be excluded.
Study quality: allocation concealment was to be used as a marker of trial quality. Studies that had not used allocation concealment were to be excluded.
Trials where missing data had been imputed were to be excluded.
Results
Description of studies
Results of the search
The electronic and manual searches identified 186 references, of which 164 were clearly not relevant to this review. Of the remaining 24 papers, 19 were excluded after reading the full papers and the other five references were included.
Included studies
Five studies met the criteria for inclusion in the current version of this review. One study (Jarrousse 1986) did not provide any outcome data and another was split into two studies for the purposes of the review (Van Lankveld 2006a/Van Lankveld 2006b). Summary information is provided below (please see the Characteristics of included studies for more details on these studies). We sought and obtained additional information from the authors.
In Jarrousse 1986, participants were alternately allocated to waiting list control, 'flooding' or systematic desensitisation for a period of no more than 20 weeks. No data were supplied in the publication. We made unsuccessful attempts to contact the authors.
In Schnyder 1998, out of 51 outpatients who gave informed consent to take part in the study, seven were lost before randomisation, leaving 44 patients who were randomly allocated to two forms of systematic desensitisation. Both groups received information and relaxation exercises. In the first group, the physician introduced an appropriately sized dilator. In the second group, the physician provided verbal instruction for introducing the dilator. We sought and obtained additional information from the author.
In Al‐Sughayir 2005 participants were alternately allocated to either systematic desensitisation or hypnotherapy. Interventions were maintained until successful intercourse was achieved. Thus efficacy data from this study could not be included in the meta‐analysis.
In Van Lankveld 2006a and Van Lankveld 2006b participants were randomised to either waiting list, bibliotherapy (systematic desensitisation) combined with minimal contact or bibliotherapy combined with group therapy. On completion of the study, those in the waiting list group were re‐randomised to either bibliotherapy combined with minimal contact or bibliotherapy combined with group therapy.
In Zukerman 2005 participants were alternately allocated to either systematic desensitisation or systematic desensitisation combined with pelvic floor exercises. Interventions were maintained until successful intercourse was achieved. Thus efficacy data from this study could not be included in the meta‐analysis.
We contacted trialists for either missing data or clarification of reported data and two authors responded to our requests for more information.
Design
Only one study (Van Lankveld 2006a/Van Lankveld 2006b) was randomised; the remaining four (Al‐Sughayir 2005; Jarrousse 1986; Schnyder 1998; Zukerman 2005) were quasi‐randomised, and in all these cases alternate allocation was used. Most studies involved two comparisons only, but two (Jarrousse 1986; Van Lankveld 2006a/Van Lankveld 2006b) included three comparisons.
Sample sizes
Studies included within this review were relatively small, varying from 36 to 117 participants (no information on numbers of participants was provided in one study (Jarrousse 1986)).
Setting
One study was carried out in the Netherlands (Van Lankveld 2006a/Van Lankveld 2006b) and one each in France (Jarrousse 1986), Israel (Zukerman 2005), Saudi Arabia (Al‐Sughayir 2005) and Switzerland (Schnyder 1998).
Participants
The mean age of the women included in these studies ranged from 23 ± 6.78 years to 30.6 ± 7.5 years and was not reported in one study (Jarrousse 1986). The mean duration of symptoms ranged from 9.52 ± 10.32 months to 132 ± 84 months but was not reported in two studies (Jarrousse 1986; Schnyder 1998).
Women were included in one study (Schnyder 1998) if they met DSM‐III‐R criteria for primary or secondary vaginismus and in another study (Al‐Sughayir 2005) if they met DSM‐IV criteria for vaginismus (primary or secondary vaginismus was not reported). Van Lankveld 2006a/Van Lankveld 2006b) included women with primary vaginismus according to DSM‐IV‐TR and the diagnostic criteria used were not reported in the final two studies (Jarrousse 1986; Zukerman 2005).
Interventions
Psychological therapies
All studies which met inclusion criteria for this review used broadly the same intervention (systematic desensitisation) but comparators differed:
In Jarrousse 1986 (a trial with three arms) participants were allocated to waiting list control, 'flooding' or systematic desensitisation for a period of no more than 20 weeks. No information on treatment fidelity was provided.
In Schnyder 1998 participants were allocated to one of two forms of systematic desensitisation (involving information and relaxation exercises). Groups differed in that an appropriately sized dilator was either introduced by the physician or by the participant following verbal instruction by the physician. Treatment was continued until symptoms abated (i.e. duration was not for a set period). No information on treatment fidelity was provided. While the two interventions are very similar, it was felt that a study examining whether dilators introduced by the woman or by the clinician would be an important source of information not least by potentially giving a steer for further research into systematic desensitization.
In Al‐Sughayir 2005 interventions consisted of systematic desensitisation compared with hypnotherapy. Again, treatment was intended to continue until successful intercourse was achieved (thus efficacy data from this study could not be included in the meta‐analysis). No information on treatment fidelity was provided.
In Van Lankveld 2006a/Van Lankveld 2006b interventions consisted of systematic desensitisation delivered by bibliotherapy (manual and CD) combined with minimal contact, compared with bibliotherapy combined with group therapy, and with a third group (waiting list control). Group therapy included sexual education, relaxation exercises, gradual exposure and sensate focus exercises. No information on treatment fidelity was provided.
In Zukerman 2005 interventions were systematic desensitisation or systematic desensitisation combined with pelvic floor exercises. Interventions were maintained until successful intercourse was achieved. Thus efficacy data from this study could not be included in the meta‐analysis. Ten therapists (nine female and one male) were involved in treatment delivery. Seven were senior therapists, including the male therapist, with a minimum of seven years of experience in the treatment of sexual dysfunction. The senior therapists supervised the junior therapists and had primary responsibility for guidance in group therapy, whereas junior therapists were co‐therapists.
Pharmacological interventions
No studies involving pharmacological treatments were identified in this version of the review.
Outcomes
The primary outcome in most studies was successful sexual intercourse.
Excluded studies
Seventeen studies are excluded from this review. Reasons are given in the Characteristics of excluded studies. The main reasons for exclusion were that studies included mixed samples (women with any sexual dysfunction not just vaginismus) or that the studies were not controlled in any way.
Risk of bias in included studies
Overall the risk of bias was high with five of the items (adequate sequence generation, allocation concealment, blinding, incomplete outcome data addressed, other bias) judged to have a high risk of some bias (50% or more). (Please see Figure 1 and the 'Risk of bias' tables).
1.
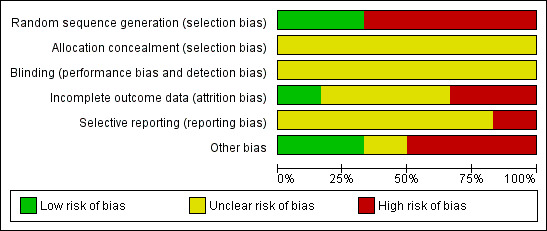
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Only one item (selective reporting) had a low risk of bias.
Allocation
We considered all studies apart from Van Lankveld 2006a/Van Lankveld 2006b to be at high risk of bias for this domain. Although this study was randomised we rated it as 'unclear' for allocation concealment as this was not reported on.
Blinding
Blinding of participants and therapists is not possible for psychological therapies. An acceptable alternative for studies of psychological therapy is to blind the evaluators.
Only Van Lankveld 2006a/Van Lankveld 2006b reported attempts to blind outcome assessors, and even these were not entirely successful. No other study reported on whether or not outcome assessors were blinded to treatment status.
Incomplete outcome data
Information on numbers/reasons for withdrawal was given in four of the five included studies (Al‐Sughayir 2005; Van Lankveld 2006a; Van Lankveld 2006b; Zukerman 2005). Drop‐outs in these three studies ranged from 7.9% to 30.3%. Investigators in one study (Van Lankveld 2006a/Van Lankveld 2006b) attempted intention‐to‐treat analysis using the last observation carried forward method.
Selective reporting
There was no evidence that any study included in this review reported fewer outcome data than were collected, with the exception of Jarrousse 1986, for which no data are available.
Other potential sources of bias
In one study (Schnyder 1998) participants were at liberty to change treatment groups. There is a matter of contention concerning studies which a priori limited length of treatment and those whose protocols dictate that treatment should persist until 'symptoms abate'. In practice, however, this performance bias had no effect on results but would conceivably have an impact on how these interventions would work in the 'real world'.
Effects of interventions
Comparison one: Systematic desensitisation versus waiting list
Primary outcomes
Successful intercourse
The risk ratio (RR) of successful intercourse was 14.23 (95% confidence interval (CI) 0.84 to 240.46) for women in the systematic desensitisation group in a single study of 74 women (Analysis 1.1).
1.1. Analysis.
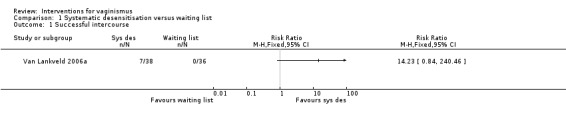
Comparison 1 Systematic desensitisation versus waiting list, Outcome 1 Successful intercourse.
Drop‐outs
The RR of drop‐out was 3.47 (95% CI 1.05 to 11.45) for women in the waiting list group in a single study of 74 women (Analysis 1.2).
1.2. Analysis.
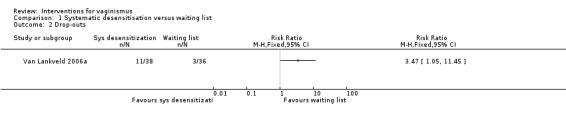
Comparison 1 Systematic desensitisation versus waiting list, Outcome 2 Drop‐outs.
Comparison two: Systematic desensitisation versus systematic desensitisation + group therapy
Primary outcomes
Successful intercourse
The RR of successful intercourse was 1.98 (95% CI 0.63 to 6.24) for women in the systematic desensitisation and group therapy group in a single study of 74 women (Analysis 2.1).
2.1. Analysis.
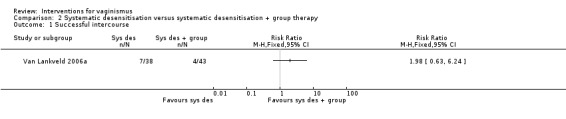
Comparison 2 Systematic desensitisation versus systematic desensitisation + group therapy, Outcome 1 Successful intercourse.
Drop‐outs
The RR of drop‐out was 1.32 (95% CI 0.71 to 2.46) for women in the systematic desensitisation and group therapy group in two studies including 114 women. The I2 value was 0% (Analysis 2.2).
2.2. Analysis.
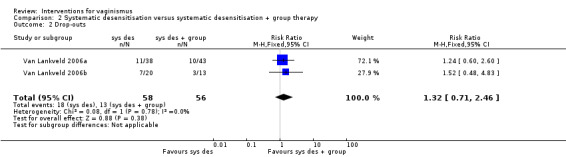
Comparison 2 Systematic desensitisation versus systematic desensitisation + group therapy, Outcome 2 Drop‐outs.
Comparison three: Systematic desensitisation versus in vitro desensitisation
Primary outcomes
Successful intercourse
The RR of successful intercourse was 1.37 (95% CI 0.42 to 4.43) for women in the in vitro desensitisation group in a single study of 44 women (Analysis 3.1).
3.1. Analysis.
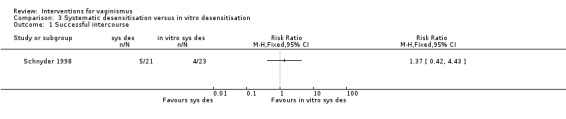
Comparison 3 Systematic desensitisation versus in vitro desensitisation, Outcome 1 Successful intercourse.
Drop‐outs
Drop‐outs were not reported for this study.
Comparison four: Systematic desensitisation versus pelvic floor exercises
Primary outcomes
Successful intercourse
Successful intercourse was not an outcome in the study.
Drop‐outs
The RR of drop‐out was 1.45 (95% CI 0.26 to 8.14) for women in the pelvic floor exercises group in a single study of 65 women (Analysis 4.1).
4.1. Analysis.
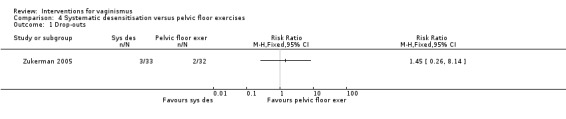
Comparison 4 Systematic desensitisation versus pelvic floor exercises, Outcome 1 Drop‐outs.
Comparison five: Systematic desensitisation versus hypnotherapy
Primary outcomes
Successful intercourse
Successful intercourse was not an outcome in the study.
Drop‐outs
The RR of drop‐out was 1.43 (95% CI 0.27 to 7.67) for women in the hypnotherapy group in a single study of 41 women (Analysis 5.1).
5.1. Analysis.
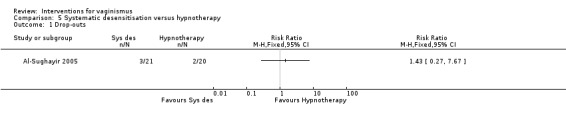
Comparison 5 Systematic desensitisation versus hypnotherapy, Outcome 1 Drop‐outs.
Secondary outcomes
No studies reported on the following secondary outcomes.
Changes in the status of vaginismus, measured by validated questionnaires (e.g. behavioural functioning (Penetration Behavior Questionnaire, PBQ), Fear of Sexuality Questionnaire (FSQ), Golombok Rust Inventory of Sexual Satisfaction GRISS)
Patient (or partner, or both) reports of improvement in satisfaction with sexual intercourse
Change in GRIMS Inventory (Golombok Rust Inventory of Marital State), Maudsley Marital Questionnaire (MMQ)
Satisfaction with the treatment
Sexual Interaction Inventory (SII), Female Sexual Function Index (FSFI)
Self rating Anxiety Scale (SAS)
Generic quality of life
Relapse rates
Subgroup analyses
There were insufficient studies included to undertake these analyses.
Sensitivity analyses
There were insufficient studies included to undertake these analyses.
Discussion
Summary of main results
We performed no meaningful meta‐analyses, since all five studies eligible for inclusion used a different control intervention.
The results of this systematic review indicate that there is no statistically significant difference between systematic desensitisation and any of the control interventions (either waiting list control, systematic desensitisation combined with group therapy or in vitro desensitisation) for the treatment of vaginismus when successful intercourse is the outcome. One study showed a statistically significant finding in favour of the waiting list group in terms of fewer drop‐outs.
Overall completeness and applicability of evidence
The review question was supported by clear inclusion and exclusion criteria in terms of the participants, interventions, outcomes and study designs. No studies involving pharmacological treatments were identified by the search strategy.
Since the 1970s, vaginismus has traditionally been considered as an easily treatable female sexual dysfunction. The high success rates, reported by Masters and Johnson (Masters 1970) and others authors (72% to 100%), however, have not been replicated and should be considered in the light of methodological considerations such as uncontrolled design, small sample sizes, elevated or unreported drop‐out rates, lack of intention‐to‐treat analysis, as well as a lack of long‐term follow‐up data.
The current review is the most comprehensive assessment of all the treatments for vaginismus to date. Strong conclusions are limited by the small number of studies included (five studies), lack of evidence for important psychological or pharmacological interventions and the heterogeneity in the treatment protocols. The issue is further complicated by that fact that a number of studies were excluded on the basis that the population included women with various sexual dysfunctions which meant that these studies could not provide data to this review. It is expected that botulinum toxin A will be investigated as a possible treatment option for vaginismus in the future but no studies have yet been identified.
None of the included trials compared other psychological therapies to pharmacological interventions. Comparison with pharmacological interventions or other types of control conditions (e.g. waiting list) would provide evidence for statistically and clinically significant differences in treatment outcomes with psychological therapies, if they exist.
One of the included studies (Jarrousse 1986) did not provide any outcome data and only one of the five included studies performed intention‐to‐treat analyses (Van Lankveld 2006a/Van Lankveld 2006b). Most trials had a short duration (up to 10 x 120‐minute sessions or until symptoms abated) and none had any long‐term follow‐up, further restricting the conclusions that can be reached.
Quality of the evidence
Despite the results of this systematic review which indicate that there is no statistically significant difference between systematic desensitisation and any of the controls, the current review is limited by the evidence available and hence conclusions about the efficacy of interventions for the treatment of vaginismus should be drawn cautiously. Four of the included studies were quasi‐randomised and this had an impact on the overall quality of the evidence.
The most important limitation regarding this review is the small number of trials. In addition, most of the studies were underpowered, which can hide clinically important differences due to small sample sizes. Therefore, the generalisation of results is uncertain.
Fifty per cent or more of the studies had a high risk of bias for all items, with the exception of selective reporting bias.
Potential biases in the review process
Previous versions of this review used different criteria for assessing methodological quality of the included studies. In this version, we reassessed all of the included studies for bias using the Cochrane 'Risk of bias' tool.
We made stringent attempts to limit bias in the review process by ensuring a comprehensive search for potentially eligible studies. Our independent assessments of eligibility of studies for inclusion in this review and extraction of data minimised the potential for additional bias beyond that detailed in the 'Risk of bias' tables.
The discussion of the results and the conclusions of the review were written by a third author who was not involved in the previous versions of this review.
Agreements and disagreements with other studies or reviews
The conclusions of the first comparison (systematic desensitisation versus waiting list), which showed an increased likelihood of successful intercourse teamed with a higher risk of drop‐out with systematic desensitisation, are in line with the overview of vaginismus by the British Association for Sexual Health and HIV (BASHH) Special Interest Group for Sexual Dysfunction (Crowley 2006) and a later review (Crowley 2009), which found that there is low‐quality evidence (uncontrolled trials) that systematic desensitisation involving insertion training appears to be effective, where the outcome measure is the ability to have penetrative vaginal intercourse.
Due to our use of intention to treat (ITT) analysis we have in one case reported an effect size lower than that reported by the trial authors (Schnyder 1998). ITT takes into account all dropouts and is therefore a more robust methodological approach.
Authors' conclusions
Implications for practice.
Since the diagnosis of vaginismus is complex and, according to the literature, vaginismus, vestibulodynia and dyspareunia can overlap in clinical practice, a multidisciplinary team, including a gynaecologist, physical therapist and psychologist/sex therapist, should be involved in the assessment and treatment of vaginismus to address its different dimensions.
The findings of this review have limited clinical implications because of the small number of trials, and the heterogeneity of protocols and patients included in the analysis. Our main finding indicates that there is no statistically significant difference between systematic desensitisation and any of the control interventions, with the exception of drop‐outs, in the systematic desensitisation versus waiting list comparison. It Is important to mention that the current review is limited by the evidence available and, as such, conclusions about the efficacy of interventions in the treatment of vaginismus should be drawn cautiously.
Implications for research.
A relevant issue in treatment evaluation is how a successful treatment outcome is defined. The great majority of trials have defined the main outcome as the ability to achieve vaginal penetration through sexual intercourse. While successful penetration is clearly a crucial first step, if it is not accompanied by the couple's satisfaction and pleasurable feelings, then treatment effectiveness is questionable.
Further well‐designed trials of psychological therapies and pharmacological intervention trials are required. These trials should include larger numbers of participants, longer follow‐up times and adequate control groups. Further trials of psychological therapies should be designed to assess not only whether psychological therapy is effective, but also which elements are active, how long psychological therapy should continue and whether partner participation is crucial.
Finally, to assist future comparisons between randomised controlled trials, trials should use outcome measures which consider the different relevant dimensions and address the complexity of vaginismus (e.g. sexual satisfaction), and should use a validated assessment scale for vaginismus. Recommendations include (i) revising the definitions of vaginismus and dyspareunia; (ii) integration of treatment approaches (especially psychological therapy with pharmacological therapy); (iii) validation of non‐specific treatment effects; (iv) controlled studies to test interventions; and (v) sexuality education to help prevent sexual pain.
What's new
| Date | Event | Description |
|---|---|---|
| 24 October 2012 | New search has been performed | Searches updated |
| 24 October 2012 | New citation required but conclusions have not changed | Methods updated and new studies included |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 2, 2001
| Date | Event | Description |
|---|---|---|
| 18 September 2009 | New citation required and conclusions have changed | Three new studies have been added to this update of the review. |
| 12 August 2009 | Amended | Converted to new review format. |
| 9 July 2007 | New search has been performed | Substantive amendment. |
| 23 May 2005 | New search has been performed | Minor update. The search strategy for this review was run on 23 May 2005 and no new studies were identified. Only the search strategy sections (in Abstract and main text) have been amended. |
| 21 November 2002 | New search has been performed | One new study added to review. |
Acknowledgements
This review was carried out as an orphan review under the auspices of the Cochrane Collaboration Depression, Anxiety & Neurosis (CCDAN) review group. We would like to thank the CCDAN editorial staff.
We would also like to thank the Cochrane Menstrual Disorders group for co‐refereeing previous versions of this review and the authors (Dr.Schnyder, Dr van Lankveld and Professor Ng) for providing information on their studies.
Appendices
Appendix 1. Search strategies (MEDLINE, EMBASE, PsycINFO, CINAHL)
OVID MEDLINE
1. Vaginism/ 2. vaginism$.ti,ab. 3. or/1‐2 4. randomized controlled trial.pt. 5. controlled clinical trial.pt. 6. randomi#ed.ti,ab. 7. placebo$.tw. 8. trial$.ti,ab. 9. randomly.ab. 10. (clinic$ adj3 (trial$ or study or studies$)).ti,ab. 11. ((singl$ or doubl$ or tripl$) adj (blind$ or mask$ or dummy)).ti,ab. 12. (control$ or prospectiv$ or volunteer$).ti,ab. 13. or/4‐12 14. (animals not (humans and animals)).sh. 15. 13 not 14 16. 3 and 15
OVID EMBASE
1. Vaginism/ 2. vaginism$.ti,ab. 3. or/1‐2 4. clinical trial.de. 5. controlled clinical trial.de. 6. randomized controlled trial.de. 7. major clinical study.de. 8. double blind procedure.de. 9. single blind procedure.de. 10. randomization.de. 11. placebo.de. 12. prospective study.de. 13. comparative study.de. 14. follow up.de. 15. randomi#ed or randomly.ti,ab. 16. ((singl$ or doubl$ or tripl$ or trebl$) adj (blind$ or mask$ or dummy)).ti,ab. 17. placebo$.tw. 18. (clinic$ adj (trial$ or study or studies$)).ti,ab. 19. comparative stud$.ti,ab. 20. (control$ or prospectiv$ or volunteer$).ti,ab. 21. or/4‐20 22. ((animal or nonhuman) not (human and (animal or nonhuman))).de. 23. 21 not 22 24. 23 and 3
OVID PsycINFO
1. Vaginismus/ 2. vaginism$.ti,ab. 3. or/1‐2 4. treatment effectiveness evaluation.de. 5. clinical trials.de. 6. placebo.de. 7. treatment outcomes.de. 8. mental health program evaluation.de. 9. evaluation.de. 10. followup studies.de. 11. random$.ti,ab. 12. placebo$.tw. 13. comparative stud$.ti,ab. 14. (clinical adj3 trial$).ti,ab. 15. (research adj3 design).ti,ab. 16. (evaluat$ adj3 stud$).ti,ab. 17. (prospectiv$ adj3 stud$).ti,ab. 18. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).ti,ab. 19. or/4‐18 21. animal.po. 22. (human or inpatient or outpatient).po. 23. 21 and 22 24. 21 not 23 25. 20 not 24 26. 25 and 3
EBSCOhost CINAHL
1. TX vaginism* 2. PT clinical trial 3. (MH "Clinical Trials+") 4. (MH "Placebos") 5. (MH "Prospective Studies") 6. (MH "Evaluation Research+") 7. TX (clin* N25 trial*) 8. TX singl* N5 blind* 9. TX singl* N5 mask* 10.TX singl* N5 dummy* 11. TX doubl* N5 blind* 12. TX doubl* N5 mask* 13.TX doubl* N5 dummy 14. TX tripl* N5 blind* 15. TX tripl* N5 mask* 16.TX tripl* N5 dummy 17. control* or prospectiv* or volunteer* 18. S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S12 or S13 or S14 or S15 or S16 or S17 or S18 19. S18 and S1
Appendix 2. Methods to be used in future updates of the review
We will use the methods stated in this version of the review unless there are changes in either methodology or diagnosis.
Appendix 3. Data extraction sheet
| Study ID |
Initials of person extracting data |
|
Type of report (e.g. peer‐reviewed journal article, full report, brief report, letter, unpublished data) | |
| Language of report | |
|
Full citation | |
|
Design of study (e.g. controlled trial, cross‐over trial) | |
|
Site of intervention (e.g. single site, multiple sites, country) | |
|
Setting of intervention (e.g. urban, rural, mixed) | |
|
Ethics committee approval | |
|
Age of participants (e.g. mean, SD, range) | |
|
Ethnicity and other demographics of participants | |
|
Baseline characteristics | |
|
Inclusion criteria | |
|
Exclusion criteria | |
|
Description of intervention(s) (including control condition, placebo, treatment as usual etc.) | |
|
Duration of intervention(s) | |
|
Total number of participants randomised | |
|
Unit of allocation | |
|
Power calculation or sample size estimate | |
|
Prospectively stated outcome(s) | |
Data and analyses
Comparison 1. Systematic desensitisation versus waiting list.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Successful intercourse | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Drop‐outs | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 2. Systematic desensitisation versus systematic desensitisation + group therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Successful intercourse | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Drop‐outs | 2 | 114 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.71, 2.46] |
Comparison 3. Systematic desensitisation versus in vitro desensitisation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Successful intercourse | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 4. Systematic desensitisation versus pelvic floor exercises.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Drop‐outs | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 5. Systematic desensitisation versus hypnotherapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Drop‐outs | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Al‐Sughayir 2005.
| Methods | Design: quasi‐randomised controlled trial Allocation method: alternation Blinding: not stated | |
| Participants | Diagnosis: vaginismus (primary or secondary not reported) Criteria: DSM‐IV Setting: outpatient clinic Number: 36 Age: 23 years, SD = 6.78 (range 17 to 40) Duration of vaginismus: 9.52 months, SD = 10.32 (range 4 to 47) | |
| Interventions | Intervention 1: hypnotherapy
Number of sessions: until symptoms abated
Duration of sessions: 45 to 60 minutes
Therapist level: not stated
Adjunctive interventions: not stated Intervention 2: systematic desensitisation Number of sessions: until symptoms abated Duration of sessions: 45 to 50 minutes Therapist level: not stated Adjunctive interventions: not stated |
|
| Outcomes | Sex‐related anxiety ‐ wife Sexual satisfaction ‐ wife ‐ Brief Index of Sexual Functioning for Women (BISF‐W) scale Sexual Satisfaction ‐ husband Drop‐outs | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No outcome data for 5 of 36 women could be reported. "During the study period, three women in the behavior group [SD] were excluded; two were divorced and one travelled outside Riyadh City. Two patients in the hypnotherapy group dropped out after the second session; both expressed ambivalent emotions toward their husbands." No ITT analysis attempted |
| Selective reporting (reporting bias) | Unclear risk | Outcome data provided for all stated outcomes but we have no access to study protocols so cannot be certain other outcomes were not assessed |
| Other bias | High risk | Participants kept in treatment until symptoms abated |
Jarrousse 1986.
| Methods | Design: quasi‐randomised controlled trial Allocation method: alternation Blinding: not stated | |
| Participants | Diagnosis: vaginismus (primary or secondary not reported) Criteria: not stated Setting: outpatient clinic Number: not stated Age: not stated Duration of vaginismus: not stated | |
| Interventions | Intervention 1: systematic desensitisation
Number of sessions: up to 20 sessions
Duration of sessions: 45 minutes
Therapist level: not stated
Adjunctive interventions: not stated Intervention 2: flooding Number of sessions: not stated Duration of sessions: 30 to 120 minutes Therapist level: not stated Adjunctive interventions: not stated Intervention 3: waiting list Number of sessions: NA Duration of sessions: NA Therapist level: NA Adjunctive interventions: not stated |
|
| Outcomes | Not stated | |
| Notes | No data available Each flooding session would be finished when anxiety was resolved | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | High risk | No outcome data reported |
| Other bias | Unclear risk | Not reported |
Schnyder 1998.
| Methods | Design: quasi‐randomised controlled trial Allocation method: alternation Blinding: not stated | |
| Participants | Diagnosis: primary or secondary vaginismus Criteria: DSM‐III‐R Setting: outpatient clinic Number: 51 but data only on 44 available Age: 28 years, SD = 7.72 (range 19 to 55) Duration of vaginismus: not stated for all participants | |
| Interventions | Intervention 1: systematic desensitisation (in vitro)
Number of sessions: until symptoms abated
Duration of sessions: not stated
Therapist level: not stated
Adjunctive interventions: not stated Intervention 2: systematic desensitisation (in vivo) Number of sessions: until symptoms abated Duration of sessions: not stated Therapist level: not stated Adjunctive interventions: not stated |
|
| Outcomes | Successful sexual intercourse Drop‐outs | |
| Notes | Data on 44 patients from contact with author 7 patients excluded due to insufficient data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Because of insufficient data, particularly subsequent to therapy, 7 women had to be eliminated from the evaluation..." No attempt at ITT analysis reported |
| Selective reporting (reporting bias) | Unclear risk | Outcome data provided for all stated outcomes but we have no access to study protocols so cannot be certain other outcomes were not assessed |
| Other bias | High risk | Participants were free to change treatments after the initial allocation procedure (2 migrated from the in vivo to the in vitro arm of the trial). This equates with a high risk of selection bias which seriously weakens confidence in the results. Participants kept in treatment until symptoms abated. |
Van Lankveld 2006a.
| Methods | Design: randomised controlled trial Allocation method: urn randomisation (stratified design) Blinding: assessor blind | |
| Participants | Diagnosis: primary vaginismus Criteria: DSM‐IV‐TR Setting: outpatient clinic Number: 117 Age: 28.6 years, SD = 6.9 Duration of vaginismus: 132 months, SD = 84 | |
| Interventions | Intervention 1: bibliotherapy + minimal contact (n = 43)
Number of sessions: 6
Duration of sessions: 15
Therapist level: NA
Adjunctive interventions: NA Intervention 2: bibliotherapy + group therapy (n = 38) Number of sessions: 10 Duration of sessions: 120 minutes Therapist level: senior therapist Adjunctive interventions: not stated Intervention 3: waiting list (n = 36) Number of sessions: NA Duration of sessions: NA Therapist level: NA Adjunctive interventions: not stated |
|
| Outcomes | Successful intercourse Drop‐outs Primary endpoint questionnaire Female Sexual Function Index Maudsley Marital Questionnaire Golombok Rust Inventory of Sexual Satisfaction | |
| Notes | Bibliotherapy (manual and CD) comprised sexual education, relaxation exercises, systematic desensitisation, cognitive therapy and sensate focus therapy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A person not involved in assessment or treatment delivery performed urn randomization." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding is not possible for participants or therapists. However, most assessors were blinded to treatment status ‐ "assessment was performed at each research center by two research assistants who were not involved in treatment delivery and who were blinded to the treatment condition of participants, with the exception of one of two assessors in one research center, who was also involved in treatment delivery." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 24 of 117 participants dropped out of treatment. Drop‐outs were roughly equivalent across the 2 active treatment arms of the study (10 and 11 respectively) whilst 3 drop‐outs came from the waiting list control arm. Investigators used LOCF (last observation carried forward) to impute missing data for drop‐outs. |
| Selective reporting (reporting bias) | Unclear risk | Outcome data provided for all stated outcomes but we have no access to study protocols so cannot be certain other outcomes were not assessed |
| Other bias | Low risk | None suspected |
Van Lankveld 2006b.
| Methods | Design: randomised controlled trial Allocation method: urn randomisation (stratified design) Blinding: assessor blind | |
| Participants | Diagnosis: primary vaginismus Criteria: DSM‐IV‐TR Setting: outpatient clinic Number: 33 Age: 30.6 years, SD = 7.5 Duration of vaginismus: 127 months, SD = 65 | |
| Interventions | Intervention 1: bibliotherapy + minimal contact
Number of sessions: 6
Duration of sessions: 15
Therapist level: NA
Adjunctive interventions: NA Intervention 2: bibliotherapy + group therapy Number of sessions: 10 Duration of sessions: 120 minutes Therapist level: senior therapist Adjunctive interventions: not stated |
|
| Outcomes | Successful intercourse Drop‐outs Primary endpoint questionnaire Female Sexual Function Index Maudsley Marital Questionnaire Golombok Rust Inventory of Sexual Satisfaction | |
| Notes | Subjects were re‐randomised waiting list from Van Lankveld 2006a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A person not involved in assessment or treatment delivery performed urn randomisation." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding was not possible for participants or therapists. However, most assessors were blinded to treatment status ‐ "assessment was performed at each research center by two research assistants who were not involved in treatment delivery and who were blinded to the treatment condition of participants, with the exception of one of two assessors in one research center, who was also involved in treatment delivery." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 10 of 33 participants dropped out of treatment. Drop‐outs were not equivalent across the different treatment arms of the study (3 out of 13 left the group treatment (23%) compared to 7 out of 20 (35%) in the minimal contact group). Investigators used LOCF (last observation carried forward) to impute missing data for drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | Outcome data provided for all stated outcomes but we have no access to study protocols so cannot be certain other outcomes were not assessed |
| Other bias | Low risk | None suspected |
Zukerman 2005.
| Methods | Design: randomised controlled trial Allocation method: not stated Blinding: not stated | |
| Participants | Diagnosis: vaginismus (primary or secondary not reported) Criteria: not stated Setting: outpatient Number: 65 Age: control group 25.3 years, SD = 3.8, experimental group 25.2 years, SD = 3.5 Duration of vaginismus: control group range 6 to 144 months, experimental group range 6 to 108 months | |
| Interventions | Intervention 1: systematic desensitisation
Number of sessions: until symptoms abated
Duration of sessions: not stated
Therapist level: not stated
Adjunctive interventions: not stated Intervention 2: systematic desensitisation + pelvic floor exercises + relaxation Number of sessions: until symptoms abated Duration of sessions: not stated Therapist level: not stated Adjunctive interventions: not stated |
|
| Outcomes | Drop‐outs | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 5 women dropped out of the study after the first or second meeting, 2 from the intervention arm and 3 from the control. Analysis was per protocol (no ITT analysis undertaken). |
| Selective reporting (reporting bias) | Unclear risk | Outcome data provided for all stated outcomes but we have no access to study protocols so cannot be certain other outcomes were not assessed |
| Other bias | High risk | Participants kept in treatment until symptoms abated |
DSM‐III‐R: Diagnostic and Statistical Manual of Mental Disorders III ‐ revision DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders IV ITT: intention‐to‐treat LOCF: last observation carried forward NA: not applicable SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Crowe 1981 | Randomised controlled trial Patients with mixed sexual dysfunctions which do not allow for separate analysis of women with vaginismus |
| Duddle 1977 | Controlled study Comparison of patients with vaginismus and healthy controls |
| Fuchs 1973 | Comparison study of 2 case series |
| Hartman 1980 | Controlled clinical trial Patients with mixed sexual dysfunctions which do not allow for separate analysis of women with vaginismus |
| Hartman 1983 | Randomised controlled trial Patients with mixed sexual dysfunctions which do not allow for separate analysis of women with vaginismus |
| Huws 1992 | Randomised controlled trial Marital and sex therapy clinic Patients with mixed dysfunctions |
| Jeng 2006 | Uncontrolled study |
| Kennedy 1995 | Uncontrolled study |
| Lew Starowicz 1982 | Controlled trial Participants allocated on basis of scores on neurosis scale |
| LoPiccolo 1985 | Randomised controlled trial
Patients attending a sex therapy clinic Patients with mixed sexual dysfunctions which do not allow for separate analysis of women with vaginismus |
| Mathews 1976 | Randomised controlled trial
Patients presenting for treatment of a sexual dysfunction Patients with mixed sexual dysfunctions which do not allow for separate analysis of women with vaginismus |
| Mathews 1983 | Randomised controlled trial Sex therapy clinic Patients with female sexual unresponsiveness not vaginismus |
| O'Gorman 1978 | Randomised controlled trial No clinical diagnosis of vaginismus |
| Obler 1973 | Controlled clinical trial Patients with mixed sexual dysfunctions which do not allow for separate analysis of women with vaginismus |
| Seo 2005 | Uncontrolled study |
| Shafik 2000 | Comparative study Control group were a convenience sample |
| van der Velde 1999 | Comparative study Patients with vaginismus and healthy controls No treatment |
| Van Lankveld 2001 | Randomised controlled trial Patients with any sexual dysfunction but not stratified by diagnosis so not possible to do a separate analysis of women with vaginismus |
| Wincze 1976 | Randomised controlled trial No clinical diagnosis of vaginismus |
Differences between protocol and review
Methods decisions have been revised in accordance with the recommendations of the current Cochrane Handbook (Higgins 2008). Retrospective 'Risk of bias' tables have been created for studies included in previous versions of this review as well as for new studies.
Contributions of authors
HM and KH developed the protocol. HM read all abstracts and selected articles for inclusion. KH double‐checked a random sample of the studies identified by the search strategy. HM, KH and TM extracted the data. HM, TM and KH wrote the review. TM re‐wrote the discussion,conclusions and implications for practice and research for the 2011 update.
Sources of support
Internal sources
Health Services Research, King's College Institute of Psychiatry, UK.
National Collaborating Centre for Women's and Children's Health, UK.
External sources
No sources of support supplied
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Al‐Sughayir 2005 {published data only}
- Al‐Sughayir MA. Vaginismus treatment: hypnotherapy versus behavior therapy. Neurosciences 2005;10(2):163‐7. [PubMed] [Google Scholar]
Jarrousse 1986 {published data only}
- Jarrousse N, Poudat F‐X. Vaginismus: therapeutic management: implosive therapy or systematic desensitization? [Prise en charge therapeutique: flooding ou desensibilisation systematique?]. Psychologie Medicale 1986;18:771‐2. [Google Scholar]
Schnyder 1998 {published and unpublished data}
- Schnyder U, Schnyder‐Luthi C, Ballinari P, Blaser A. Therapy for vaginismus: in vivo versus in vitro desensitization. Canadian Journal of Psychiatry ‐ Revue Canadienne De Psychiatrie 1998;43:941‐4. [DOI] [PubMed] [Google Scholar]
Van Lankveld 2006a {published data only}
- Lankveld JJ, ter Kuile MM, Groot HE, Melles R, Nefs J, Zandbergen M. Cognitive‐behavioral therapy for women with lifelong vaginismus: a randomized waiting‐list controlled trial of efficacy. Journal of Consulting and Clinical Psychology 2006;74(1):168‐78. [DOI] [PubMed] [Google Scholar]
- ter Kuile MM, Lankveld JJ, Groot E, Melles R, Neffs J, Zandbergen M. Cognitive‐behavioral therapy for women with lifelong vaginismus: process and prognostic factors. Behavior Research Therapy 2007;45(2):359‐73. [DOI] [PubMed] [Google Scholar]
Van Lankveld 2006b {published data only}
- Lankveld JJ, ter Kuile MM, Groot HE, Melles R, Nefs J, Zandbergen M. Cognitive‐behavioral therapy for women with lifelong vaginismus: a randomized waiting‐list controlled trial of efficacy. Journal of Consulting and Clinical Psychology 2006;74(1):168‐78. [DOI] [PubMed] [Google Scholar]
- ter Kuile MM, Lankveld JJ, Groot E, Melles R, Neffs J, Zandbergen M. Cognitive‐behavioral therapy for women with lifelong vaginismus: process and prognostic factors. Behavior Research Therapy 2007;45(2):359‐73. [DOI] [PubMed] [Google Scholar]
Zukerman 2005 {published data only}
- Zukerman Z, Roslik Y, Orvieto R. Treatment of vaginismus with the Paula Garburg sphincter muscle exercises. Harefuah 2005;144(4):246‐8. [PubMed] [Google Scholar]
References to studies excluded from this review
Crowe 1981 {published data only}
- Crowe MJ, Gillan P, Golombok S. Form and content in the conjoint treatment of sexual dysfunction: a controlled study. Behavior Research & Therapy 1981;19:47‐54. [DOI] [PubMed] [Google Scholar]
Duddle 1977 {published data only}
- Duddle M. Etiological factors in the unconsummated marriage. Journal of Psychosomatic Research 1977;21:157‐60. [DOI] [PubMed] [Google Scholar]
Fuchs 1973 {published data only}
- Fuchs K, Hoch Z, Paldi E, Abramovici H, Brandes JM, Timor‐Tritsch I, et al. Hypno‐desensitization therapy of vaginismus: Part 1. "In vitro" method. Part 2. "In vivo" method. International Journal of Clinical and Experimental Hypnosis. 1973;21:144‐56. [DOI] [PubMed] [Google Scholar]
Hartman 1980 {published data only}
- Hartman LM. Relationship factors and sexual dysfunction: implications for assessment and treatment. Canadian Journal of Psychiatry 1980;25:560‐3. [DOI] [PubMed] [Google Scholar]
Hartman 1983 {published data only}
- Hartman LM, Daly EM. Relationship factors in the treatment of sexual dysfunction. Behavior Research & Therapy 1983;21:153‐60. [DOI] [PubMed] [Google Scholar]
Huws 1992 {published data only}
- Huws R. Non‐attendance at a marital and sexual difficulties clinic: a controlled intervention study. International Journal of Social Psychiatry 1992;38:304‐8. [DOI] [PubMed] [Google Scholar]
Jeng 2006 {published data only}
- Jeng CJ, Wang LR, Chou CS, Shen J, Tzeng CR. Management and outcome of primary vaginismus. Journal of Sex and Marital Therapy 2006;32:379‐87. [DOI] [PubMed] [Google Scholar]
Kennedy 1995 {published data only}
- Kennedy P, Doherty N, Barnes J. Primary vaginismus: a psychometric study of both partners. Sexual & Marital Therapy 1995;10:9‐22. [Google Scholar]
Lew Starowicz 1982 {published data only}
- Lew‐Starowicz Z. Results of treatment of women with diagnosed vaginismus [Wyniki leczenia kobiet z rozpoznaniem pochwicy]. Ginekologia Polska 1982;33:691‐4. [PubMed] [Google Scholar]
LoPiccolo 1985 {published data only}
- LoPiccolo J, Heiman JR, Hogan DR, Roberts CW. Effectiveness of single therapists versus cotherapy teams in sex therapy. Journal of Consulting & Clinical Psychology 1985;53:287‐94. [DOI] [PubMed] [Google Scholar]
Mathews 1976 {published data only}
- Mathews A, Bancroft J, Whitehead A, Hackmann A, Julier D, Bancroft J, et al. The behavioural treatment of sexual inadequacy: a comparative study. Behavior Research & Therapy 1976;14:427‐36. [DOI] [PubMed] [Google Scholar]
Mathews 1983 {published data only}
- Mathews A, Whitehead A, Kellett J. Psychological and hormonal factors in the treatment of female sexual dysfunction. Psychological Medicine 1983;13:83‐92. [DOI] [PubMed] [Google Scholar]
O'Gorman 1978 {published data only}
- O'Gorman E. The treatment of frigidity: a comparative study of group and individual desensitization. British Journal of Psychiatry 1978;132:580‐4. [DOI] [PubMed] [Google Scholar]
Obler 1973 {published data only}
- Obler M. Systematic desensitization in sexual disorders. Journal of Behavior Therapy & Experimental Psychiatry 1973;4:93‐101. [Google Scholar]
Seo 2005 {published data only}
- Seo JT, Choe JH, Lee WS, Kim KH. Efficacy of functional electrical stimulation‐biofeedback with sexual cognitive behavioural therapy as treatment of vaginismus. Urology 2005;66:77‐81. [DOI] [PubMed] [Google Scholar]
Shafik 2000 {published data only}
- Shafik A, El‐Sibai O. Vaginismus: results of treatment with botulin toxin. Journal of Obstetrics and Gynaecology 2000;20(3):300‐2. [DOI] [PubMed] [Google Scholar]
van der Velde 1999 {published data only}
- Velde J, Everaerd W. Voluntary control over pelvic floor muscles in women with and without vaginistic reactions. International Urogynecology Journal 1999;10:230‐6. [DOI] [PubMed] [Google Scholar]
Van Lankveld 2001 {published and unpublished data}
- Lankveld JJ, Everaerd W, Grotjohann Y. Cognitive‐behavioral bibliotherapy for sexual dysfunctions in heterosexual couples: a randomized waiting‐list controlled clinical trial in the Netherlands. Journal of Sex Research 2001;38:51‐67. [Google Scholar]
Wincze 1976 {published data only}
- Wincze JP, Caird WK. The effects of systematic desensitization and video desensitization in the treatment of essential sexual dysfunction in women. Behavior Therapy 1976;7:335‐42. [Google Scholar]
References to ongoing studies
Ghazizadeh 2008 {unpublished data only}
- Ghazizadeh S. Comparison of efficacy of 250 units versus 500 units of botulinum toxin in the treatment of refractory vaginismus. ClinicalTrials.gov (www.clinicaltrials.gov/ct2/show/NCT00638066) 2008.
- Ghazizadeh S. Comparison of two different doses of botulinum toxin a in the treatment of severe vaginismus (500 vs. 250U Dysport) [conference abstract]. Abstracts of the 20th World Congress of Sexual Health; 2011 Jun 12‐16, Glasgow United Kingdom. Journal of Sexual Medicine 2011;8(s3):164. [Google Scholar]
Additional references
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313(7066):1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Amidu 2010
- Amidu N, Owiredu W, Woo E, Addai‐Mensah O, Quaye L, Alhassan A, et al. Incidence of sexual dysfunction: a prospective survey in Ghanaian females. Reproductive Biology and Endocrinology 2010;8:106‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington DC: American Psychiatric Association, 2000. [Google Scholar]
Bancroft 1976
- Bancroft J, Coles L. Three years' experience in a sexual problems clinic. British Medical Journal 1976;1:1575‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Basson 2003
- Basson R, Leiblum S, Brotto L, Derogatis L, Fourcroy J, Fugl‐Meyer K, et al. Definitions of women's sexual dysfunction reconsidered: advocating expansion and revision. Journal of Psychosomatic Obstetrics and Gynaecology 2003;24:221‐9. [DOI] [PubMed] [Google Scholar]
Bergeron 2003
- Bergeron S, Lord MJ. The integration of pelvi‐perineal re‐education and cognitive‐behavioural therapy in the multidisciplinary treatment of the sexual pain disorders. Sexual and Relationship Disorders 2003;18(2):135‐41. [Google Scholar]
Binik 2010
- Binik YM. The DSM diagnostic criteria for vaginismus. Archives of Sexual Behavior 2010;39(2):292‐303. [DOI] [PubMed] [Google Scholar]
Bodenmann 2006
- Bodenmann G, Ledermann T, Blattner D, Galluzzo C. Associations among everyday stress, critical life events, and sexual problems. Journal of Nervous and Mental Disease 2006;194(2):494‐501. [DOI] [PubMed] [Google Scholar]
Bravo 2005
- Bravo CS, Melendez JC, Ramirez SM, Lopez ME. Feminine and masculine sexual dysfunctions: gender comparison in a Mexico City sample [Disfunciones sexuales femininas y masculinas: Comparacion de genero en una muestra de la Ciudad de Mexico]. Salud Mental 2005;28(4):74‐80. [Google Scholar]
Brin 1997
- Brin MF, Vapnek JM. Treatment of vaginismus with botulinum toxin injections. Lancet 1997;349:252‐3. [DOI] [PubMed] [Google Scholar]
Catalan 1981
- Catalan J, Bradley M, Gallwey J, Hawton K. Sexual dysfunction and psychiatric morbidity in patients attending a clinic for sexually transmitted diseases. British Journal of Psychiatry 1981;138:292‐6. [DOI] [PubMed] [Google Scholar]
Catalan 1990
- Catalan J, Hawton K, Day A. Couples referred to a sexual dysfunction clinic. British Journal of Psychiatry 1990;156:61‐7. [DOI] [PubMed] [Google Scholar]
Crowley 2006
- Crowley T, Richardson D, Goldmeier D. Recommendations for the management of vaginismus. International Journal of STD and AIDS 2006;17(1):14‐8. [DOI] [PubMed] [Google Scholar]
Crowley 2009
- Crowley T, Goldmeier D, Hiller J. Diagnosing and managing vaginismus. BMJ 2009;339:225‐9. [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7:177‐88. [DOI] [PubMed] [Google Scholar]
Dogan 2009
- Dogan S. Vaginismus and accompanying sexual dysfunctions in a Turkish clinical sample. Journal of Sexual Medicine 2009;6:184‐92. [DOI] [PubMed] [Google Scholar]
Frank 1976
- Frank E, Anderson C, Kupfer DJ. Profiles of couples seeking sex therapy and marital therapy. American Journal of Psychiatry 1976;133:559‐62. [DOI] [PubMed] [Google Scholar]
Frenken 1987
- Frenken J, Tol P. Sexual problems in gynaecological practice. Journal of Psychosomatics Obstetrics & Gynecology 1987;6:143‐55. [Google Scholar]
Fuchs 1980
- Fuchs K. Therapy of vaginismus by hypnotic desensitization. American Journal of Obstetrics and Gynecology 1980;137:177. [DOI] [PubMed] [Google Scholar]
Furukawa 2006
- Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta‐analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59:7‐10. [DOI] [PubMed] [Google Scholar]
Hawton 1985
- Hawton K. Sex Therapy: A Practical Guide. Oxford: Oxford University Press, 1985. [Google Scholar]
Hawton 1986
- Hawton K, Catalan J, Martin P, Fagg J. Long‐term outcome of sex therapy. Behaviour Research and Therapy 1986;24:665‐75. [DOI] [PubMed] [Google Scholar]
Hawton 1986a
- Hawton K, Catalan J. Prognostic factors in sex therapy. Behaviour Research and Therapy 1986;14:377‐85. [DOI] [PubMed] [Google Scholar]
Hawton 1990
- Hawton K, Catalan J. Sex therapy for vaginismus: characteristics of couples and treatment outcome. Sexual and Marital Therapy 1990;5:39‐48. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Altman DG, editors. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Hirst 1996
- Hirst JF, Baggaley MR, Watson JP. A four year survey of an inner city psychosexual problems clinic. Sexual & Marital Therapy 1996;11:19‐36. [Google Scholar]
Jacobson 1938
- Jacobson E. Progressive Relaxation. Chicago, IL: University of Chicago Press, 1938. [Google Scholar]
Kabakci 2003
- Kabakci E, Batur S. Who benefits from cognitive behavioral therapy for vaginismus?. Journal of Sex and Marital Therapy 2003;20:277‐88. [DOI] [PubMed] [Google Scholar]
LoPiccolo 1994
- LoPiccolo J. The evolution of sex therapy. Sexual and Marital Therapy 1994;9:5‐7. [Google Scholar]
Masters 1970
- Masters W, Johnson V. Human Sexual Inadequacy. Boston: Little & Brown, 1970. [Google Scholar]
Mikhail 1976
- Mikhail AR. Treatment of vaginismus by i.v. diazepam (Valium(R)) abreaction interviews. Acta Psychiatrica Scandinavica 1976;53:328‐32. [DOI] [PubMed] [Google Scholar]
Ng 1993
- Ng ML. Treatment of a case of resistant vaginismus using modified Mien‐Ling. Sexual and Marital Therapy 1993;7:295‐9. [Google Scholar]
O'Donohue 1997
- O'Donohue W, Dopke CA, Swingen DN. Psychotherapy for female sexual dysfunction: a review. Clinical Psychology Review 1997;17:537‐66. [DOI] [PubMed] [Google Scholar]
Pacik 2009
- Pacik PT. Botox treatment for vaginismus. Plastic and Reconstructive Surgery 2009;124:455e‐6e. [DOI] [PubMed] [Google Scholar]
Reissing 2004
- Reissing ED, Binik YM, Khalife S, Cohen D, Amsel R. Vaginal spasm, pain, and behavior: an empirical investigation of the diagnosis of vaginismus. Archives of Sexual Behavior 2004;33:5‐17. [DOI] [PubMed] [Google Scholar]
Renshaw 1988
- Renshaw DC. Profile of 2376 patients treated at Loyola Sex Clinic between 1972 and 1987. Sexual and Marital Therapy 1988;3:111‐7. [Google Scholar]
RevMan 5.0 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008.
Rosen 1995
- Rosen RC, Leiblum SR. Treatment of sexual disorders in the 1990s: an integrated approach. Journal of Consulting and Clinical Psychology 1995;63:877‐90. [DOI] [PubMed] [Google Scholar]
Rosen 2000
- Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self‐report instrument for the assessment of female sexual function. Journal of Sex and Marital Therapy 2000;26:191‐208. [DOI] [PubMed] [Google Scholar]
Shokrollahi 1999
- Shokrollahi P, Mirmohamadi M, Mehrabi F, Babaei GH. Prevalence of sexual dysfunction in women seeking services at a family planning centers in Tehran. Journal of Sex & Marital Therapy 1999;25:211‐5. [DOI] [PubMed] [Google Scholar]
Simonelli 2010
- Simonelli C, Tripodi F, Cosmi V, Rossi R, Fabrizi A, Silvaggi C, et al. What do men and women ask a helpline on sexual concerns? Results of an Italian telephone counselling service. International Journal of Clinical Practice 2010;64:360‐70. [DOI] [PubMed] [Google Scholar]
van de Wiel 1990
- Wiel HB, Jaspers JP, Weijmar Schultz WC, Gal J. Treatment of vaginismus: a review of concepts and treatment modalities. Journal of Psychosomatic Obstetrics and Gynaecology 1990;11:1‐18. [Google Scholar]
WHO 1992
- World Health Organization. The ICD‐10 Classification of Mental and Behavioural Disorders. 10th Edition. Geneva: World Health Organization, 1992. [Google Scholar]
References to other published versions of this review
McGuire 2001
- McGuire H, Hawton KKE. Interventions for vaginismus. Cochrane Database of Systematic Reviews 2001, Issue 2. [DOI: 10.1002/14651858.CD001760] [DOI] [PubMed] [Google Scholar]


