Abstract
PURPOSE:
To determine the frequency of strabismus among children initially diagnosed with pseudostrabismus using big data.
DESIGN:
Population-based retrospective cohort study.
METHODS:
Setting: Population-based retrospective cohort study using claims data. Study Population: 17,885 children diagnosed with pseudostrabismus at age ≤3 years who were later diagnosed with strabismus using the Optum© de-identified Clinformatics® Data Mart Database (2003–2016). We excluded patients diagnosed with strabismus before the diagnosis of pseudostrabismus or diagnosed simultaneously with strabismus and pseudostabismus.
Observations:
We assessed age, refractive error, and presence of amblyopia. Patients with pseudostrabismus were compared to a group of patients from the Optum dataset diagnosed with esotropia, exotropia, and unspecified heterotropia who had not been previously diagnosed with pseudostrabismus.
Main Outcome Measures:
Incidence of strabismus, among patients initially diagnosed with pseudostrabismus versus those without an initial diagnosis of pseudostrabismus.
RESULTS:
Strabismus was diagnosed in 9.6% (n=1,725) of children initially diagnosed with pseudostrabismus at a median age of 1.65 years (IQR; 1.19 – 2.46) compared to 1.7% (136,047 of 7,787,743) of children in the control group (P<.001). Strabismus was diagnosed more than a year later in the pseudostrabismus group (3.32 years; IQR, 2.28 – 4.74) compared to the control group (2.28 years; IQR, 1.43 – 3.16) (P<0.001). Esotropia was the most common type of strabismus in both groups (pseudostrabismus, 69.7%; control, 62.1%). 377 children (21.9%) in the pseudostrabismus group underwent strabismus surgery compared to 12.1% of children in the control group (P<.001).
CONCLUSIONS:
Young children diagnosed with pseudostrabismus are at increased risk of developing strabismus and undergoing strabismus surgery.
Table of Contents Statement
The Optum© de-identified Clinformatics® Database (2003–2016) was used to compare the incidence of strabismus among children age ≤3 years initially diagnosed with pseudostrabismus versus a control group. Strabismus was diagnosed in 9.6% of children in the pseudostrabismus group versus 1.7% in the control group. Strabismus was diagnosed more than a year later in the pseudostrabismus group. Strabismus surgery was performed on 21.9% of children in the pseudostrabismus group versus 12.1% in the control group.
Diagnosing strabismus can be challenging in young children due to poor cooperation, unreliable fixation, and stranger anxiety. Consequently, young children with intermittent or small angle strabismus may be mistakenly diagnosed as having pseudostrabismus.1 Later, because the angle of the deviation becomes larger, the deviation becomes constant or a more thorough examination is performed, these children may be diagnosed with strabismus. The most common types of strabismus that are misdiagnosed as pseudostrabismus in early childhood are accommodative esotropia and intermittent exotropia.1–4 The incidence of strabismus among normal children in population based studies has been reported to be between 2.1% and 3.6%.5–8 In contrast, the incidence of strabismus has been reported to be high as 20% among young children initially diagnosed with pseudostrabismus.9 However, most of these studies are small and from single clinical centers.1–4,9,10
In the present study, we used the Optum SES Medical Claims dataset from The Optum©’s Clinformatics® Data Mart (CDM) to determine the frequency with which children in the United States who were initially diagnosed with pseudostrabismus were later found to have strabismus.
Methods
Study design and data source
This study was a population-based retrospective cohort study using claims data from the CDM database (2003–2016). The CDM is a de-identified database of administrative health claims for members of a large national managed care company affiliated with Optum. The database contains de-identified patients’ claims information from approximately 15 to 18 million annual covered lives for a total of around 63 million lives from a geographically diverse population spanning all 50 states. The Optum database from the CDM provides demographic and medical claims data for inpatient and outpatient services including surgery. Data access for this project was provided by the Stanford Center for Population Health Sciences (PHS) Data Core. The PHS Data Core is supported by a National Institutes of Health National Center for Advancing Translational Science Clinical and Translational Science Award (UL1 TR001085) and internal Stanford funding. The content of the article is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The Stanford University School of Medicine Institutional Review Board determined that this study did not require IRB approval since it only used de-identified data.
Study Population
Children were included if they were diagnosed with pseudostrabismus as defined by the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) (743.63) and International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) (Q10.3) and they were ≤3 years of age between 2003 and 2013 and born after 1998. Patients were classified as having strabismus if they were coded with any one of the diagnostic codes in Table 1 during an encounter. Patients were then divided into three groups: esotropia, exotropia, and unspecified heterotropia, based on the ICD-9-CM or ICD-10-CM codes used. The presence of amblyopia and hypermetropia, myopia and astigmatism were also identified based on the ICD-9-CM or ICD-10-CM codes used (Table 1). Current Procedure Terminology (CPT) codes (CPT 67311, 67312) were used to identify patients who underwent strabismus surgery. Patients diagnosed with strabismus before the diagnosis of pseudostrabismus or diagnosed simultaneously with strabismus and pseudostrabismus were excluded. We also assessed age when pseudostrabismus and strabismus were first diagnosed, gender, race, type of refractive error, presence of amblyopia, and surgical rate from Optum claims data. We compared this dataset to a control group of covered children diagnosed with esotropia, exotropia, and unspecified heterotropia who were born after 1998 and were 3 years of age or younger at any time point between 2003–2016. We also excluded children who were diagnosed with pseudostrabismus prior to being diagnosed with strabismus. We calculated the rates of amblyopia and strabismus surgery among patients initially diagnosed with pseudostrabismus who later developed strabismus and among patients in the control group who developed strabismus.
Table 1.
International Classification of Disease (ICD) codes used to identify the type of strabismus, refractive error, and amblyopia
| ICD-9 Codes | ICD-10 Codes | Brief Descriptor |
|---|---|---|
| Esotropia | ||
| 378.00 | H50.00 | Unspecified esotropia |
| 378.01, 378.02, 378.03, 378.04 | H50.01x, H50.02x, H50.03x, H50.04x | Monocular esotropia |
| 378.05, 378.06, 378.07, 378.08 | H50.05, H50.06, H50.07, H50.08 | Alternating esotropia |
| 378.21 | H50.31x | Intermittent monocular esotropia |
| 378.22 | H50.32 | Intermittent alternating esotropia |
| 378.35 | H50.43 | Accommodative component esotropia |
| Exotropia | ||
| 378.10 | H50.10 | Unspecified exotropia |
| 378.11, 378.12, 378.13, 378.14 | H50.11x, H50.12x, H50.13x, H50.14x | Monocular exotropia |
| 378.15, 378.16, 378.17, 378.18 | H50.15, H50.16, H50.17, H50.18 | Alternating exotropia |
| 378.23 | H50.33x | Intermittent monocular exotropia |
| 378.24 | H50.34 | Intermittent alternating exotropia |
| Unspecified heterotropia | ||
| 378.30 | H50.40 | Unspecified heterotropia |
| 378.20 | H50.30 | Unspecified intermittent heterotropia |
| Refractive error | ||
| 367.0 | H52.0x | Hypermetropia |
| 367.1 | H52.1x | Myopia |
| 367.20, 367.21, 367.22 | H52.20x, H52.21x, H52.22x | Astigmatism |
| 367.31 | H52.31 | Anisometropia |
| Amblyopia | ||
| 368.00 | H53.00x | Unspecified amblyopia |
| 368.01 | H53.03x | Strabismic amblyopia |
| 368.02 | H53.01x | Deprivation amblyopia |
| 368.03 | H53.02x | Refractive amblyopia |
Statistical Analysis
We used a chi-square test to compare each type of strabismus (i.e., gender, race, presence of amblyopia, strabismus surgery, and type of refractive error) and the development of strabismus among children initially diagnosed as having pseudostrabismus and the control group. The time interval between the diagnosis of pseudostrabismus and different types of strabismus was compared using a Mann-Whitney test. The relationship between the time of diagnosis of pseudostrabismus and the time interval until a diagnosis of strabismus was analyzed using the Spearman correlation coefficient (rho). The statistical analyses were performed using SPSS software, version 25.0 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Armonk, NY).
Results
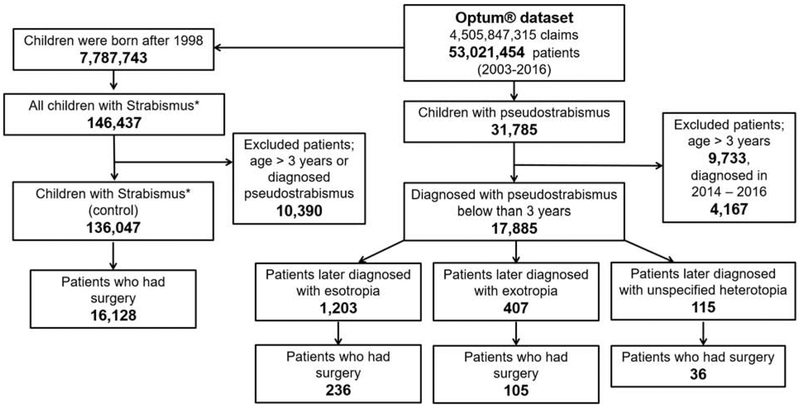
A total of 4,505,847,315 claims for 53,021,454 patients were analyzed in the Optum® SES Medical Claims between 2003 and 2016. Pseudostrabismus was diagnosed in 31,785 of these patients. An analysis was then performed on a subset of 17,885 of these patients who were diagnosed with pseudostrabismus when 3 years of age or younger (Figure 1). Their median age at the time pseudostrabismus was diagnosed was 1.65 years (interquartile range [IQR]; 1.17 – 2.46) and their ethnicities were: Caucasian – 12,278 (68.6%), Hispanic-2,014 (11.3%), Asian-1,562 (8.7%), African American-934 (5.2%), and unknown-1,097 (6.1%). A total of 8,934 (50.0%) were male. Strabismus was subsequently diagnosed in 9.6% (n=1,725) of these children at a median age of 3.32 years (IQR; 2.28 – 4.74). The most common types of strabismus diagnosed were esotropia (69.7%), exotropia (23.6%) and unspecified heterotropia (6.7%) (Table 2). Gender and race were not statistically different for these different types of strabismus. Among patients diagnosed as having strabismus (n=1,725), 834 (48.3%) also had an ICD code for a refractive error. The most common refractive error was hypermetropia (n=605, (72.5%)) including hypermetropia and astigmatism. Other refractive errors included astigmatism (n=317, (38.0%)) and myopia (n=112, (12.2%)). The types of strabismus differed for hypermetropia and myopia (P<0.001). Hypermetropia was more common in patients diagnosed with esotropia (76.4%, 453 of 593 patients) and myopia in patients diagnosed with exotropia (26.3%, 50 of 190 patients). A total of 134 patients (16.1%) had anisometropia. Amblyopia was present in 32.4% (n=498) of these patients (Table 3). The incidence of amblyopia was similar for all types of strabismus (P=0.123). Strabismus surgery was subsequently performed on 21.9% (n=377) of these patients. Two or more strabismus surgeries was performed on 63 (16.7%) of these patients (Table 4). The median time interval between the diagnosis of pseudostrabismus and strabismus was 1.21 (IQR; 0.50 – 2.80) years (Table 5). Esotropia (3.14 years) was diagnosed at a younger median age than exotropia (3.83 years) (P<0.001). No correlation was found (rho = 0.007, P=0.782) between the age pseudostrabismus was diagnosed and the time interval until strabismus was diagnosed.
Figure 1.
Flow diagram illustrating the path taken to identify children with strabismus from the general population in the left column (control group) and children who were initially diagnosed with pseudostrabismus in the center column. The only types of strabismus* evaluated were esotropia, exotropia, and unspecified heterotropia.
Table 2.
Number and Proportion of Patients with Esotropia, Exotropia, and Unspecified heterotropia in the pseudostrabismus group
| Esotropia | Exotropia | Unspecified heterotropia | Total | P value | |
|---|---|---|---|---|---|
| No. | 1,203 | 407 | 115 | 1,725 | |
| Proportion (%) | 69.7 | 23.6 | 6.7 | N/A | |
| Incidence (%) | 6.7 | 2.3 | 0.6 | 9.6 | |
| Gender | 0.844* | ||||
| Male (%) | 583 (48.5) | 191 (46.9) | 54 (47.0) | 828 (48.0) | |
| Female (%) | 620 (51.5) | 216 (53.1) | 61 (53.0) | 897 (52.0) | |
| Race | 0.755* | ||||
| White (%) | 873 (72.6) | 280 (68.8) | 82 (71.3) | 1,235 (71.6) | |
| Black (%) | 72 (6.0) | 26 (6.4) | 5 (4.3) | 103 (6.0) | |
| Hispanic (%) | 112 (9.3) | 45 (11.1) | 9 (7.8) | 166 (9.6) | |
| Asian (%) | 85 (7.1) | 34 (8.4) | 10 (8.7) | 129 (7.5) | |
| Unknown (%) | 61 (5.1) | 22 (5.4) | 9 (7.8) | 92 (5.3) |
P values were obtained using chi-square test.
Table 3.
The number and type of amblyopia for each type of strabismus in the pseudostrabismus group
| Esotropia (N=1,203) |
Exotropia (N=407) |
Unspecified
heterotropia (N=115) |
Total (N=1,725) |
|
|---|---|---|---|---|
| Unspecified | 172 (38.0%) | 40 (32.5%) | 15 (35.7%) | 194 (39.0%) |
| Strabismic | 160 (35.3%) | 52 (42.3%) | 21 (50.0%) | 190 (38.2%) |
| Strabismic + Refractive | 41 (9.1%) | 6 (4.9%) | 1 (2.4%) | 34 (6.8%) |
| Strabismic + Deprivation | 10 (2.2%) | 2 (1.5%) | 1 (2.4%) | 10 (2.0%) |
| Deprivation | 14 (3.1%) | 6 (4.4%) | 1 (2.4%) | 18 (3.6%) |
| Refractive | 56 (12.4%) | 17 (13.8%) | 3 (7.1%) | 54 (10.8%) |
| Refractive + Deprivation | 1 (0.2%) | 0 (0%) | 0 (0%) | 1 (0.2%) |
| Total Amblyopia* | 453 (37.7%) | 123 (30.2%) | 42 (36.5%) | 498 (32.4%) |
P=0.123, Chi-square test.
Table 4.
Number of surgical procedures for each type of strabismus in the pseudostrabismus group
| Esotropia (N=1,203) |
Exotropia (N=407) |
Unspecified
heterotropia (N=115) |
Total (N=1,725) |
|
|---|---|---|---|---|
| Patients who had strabismus surgery* | 236 (18.6%) | 105 (25.8%) | 36 (31.3%) | 377 (21.9%) |
| No. of surgeries (%) | ||||
| 1 | 201 (85.5%) | 84 (80.0%) | 29 (80.6%) | 314 (83.3%) |
| 2 | 32 (13.3%) | 18 (17.1%) | 6 (16.7%) | 56 (14.9%) |
| 3 | 2 (0.8%) | 2 (1.9%) | 1 (2.8%) | 5 (1.3%) |
| 4 | 1 (0.4%) | 1 (1.0%) | 0 (0.0%) | 2 (0.5%) |
P<0.001, Chi-square test.
Table 5.
The median age pseudostrabismus and each type of strabismus was diagnosed (years).
| Esotropia | Exotropia | Unspecified heterotropia | Total | |
|---|---|---|---|---|
| Age pseudostrabismus* diagnosed | 1.67a (IQR; 1.16 – 2.37) |
1.87ab (IQR; 1.32 – 2.51) |
1.72b (IQR; 1.16 – 2.34) |
1.72 (IQR; 1.19 – 2.42) |
| Age strabismus* diagnosed | 3.14cd (IQR; 2.11 – 4.62) |
3.83c (IQR; 2.76 – 5.58) |
3.45d (IQR; 2.55 – 4.79) |
3.32 (IQR; 2.28 – 4.74) |
| Time interval between diagnosis of pseudostrabismus and strabismus* | 1.04de (IQR; 0.42 – 2.61) |
1.71d (IQR; 0.68 – 3.38) |
1.74e (IQR; 0.68 – 2.93) |
1.21 (IQR; 0.50 – 2.80) |
Mann-Whitney test for each pair. The times as marked same alphabets (a-a, b-b, c-c, d-d, e-e, f-f) were significant differences with Mann-Whitney test. IQR; interquartile range.
Strabismus was diagnosed in 136,047 (1.7%) children in the control group at a median age of 2.28 (IQR; 1.43 – 3.16) years. The incidence of strabismus was more than 5 times higher among children initially diagnosed with pseudostrabismus compared to the control group (P<0.001). The incidence of esotropia (62.4%) was lower and the incidence of exotropia (32.1%) higher in the control group compared to the pseudostrabismus group (P<0.001). The incidence of unspecified hetereotropia was similar in the control (5.4%) and pseudostrabismus groups. Amblyopia was diagnosed more frequently in the pseudostrabismus group (32.4%) than the control group (31.6% (42,977 of 136,047) (P<0.001). Lastly, strabismus surgery was performed less frequently on patients in the control group (12.1%; 16,406 of 136,047) compared to the pseudostrabismus group (P<0.001).
Discussion
In this population-based retrospective cohort study, the incidence of manifest strabismus among 17,885 children initially diagnosed as having pseudostrabismus when 3 years of age or younger was 9.6%. Among patients later diagnosed with strabismus, about two-thirds of them had esotropia and one-third had exotropia. Furthermore, about one-third of them developed amblyopia and almost one-quarter of them underwent strabismus surgery. Compared with a control group from the same Optum dataset, the incidence of strabismus was 5 times higher and the rate of strabismus surgery was nearly two times higher in the pseudostrabismus group. Many previous studies have reported a higher incidence of strabismus among children previously diagnosed with pseudostrabismus presumably because many of these children had intermittent strabismus during the initial examination that was not recognized.1–3,9,10 The incidence of strabismus among children initially diagnosed with pseudostrabismus was lower in our series (9.6%) compared to other studies (10.0% to 19.4%)The higher incidence of strabismus in other studies may have occurred because they used different methodologies to identify children with pseudostrabismus or they may have used alternative techniques to perform clinical examinations. Silbert and coworkers11 reported they identified patients with pseudostrabismus by reviewing medical records using ICD codes for esotropia. Other studies state that the records of patients diagnosed with pseudostrabismus were reviewed without stating the specific methods used. We identified children with pseudostrabismus by searching a large dataset for the ICD codes 743.63 (ICD-9-CM) (other specified congenital anomalies of eyelid) or Q10.3 (ICD-10-CM) (other congenital malformations of eyelid). Children who were diagnosed with pseudostrabismus who did not have prominent epicanthal folds or a flat nasal bridge may have been coded with an ICD code other than 743.63 or Q10.3 and therefore would not have been included in our analysis. Nevertheless, the 9.6% incidence of strabismus among children diagnosed with pseudostrabismus in our study is more than three times greater than the 2.75% prevalence of strabismus reported in a recent IRIS Registry study.7 The lower incidence of patients with strabismus among our control population (1.7%) compared to other population based studies such as the Multi-Ethnic Pediatric Eye Disease Study (MEPEDS) and Baltimore Pediatric eye Disease Study (BPEDS), suggests that many children in our control population had undiagnosed strabismus.5,6,8
Several risk factors likely contributed to the development of manifest strabismus in children initially diagnosed with pseudostrabismus. Perhaps the most important was moderate or high hypermetropia.3,4,12 For this reason, it is imperative that children with suspected pseudostrabismus undergo a cycloplegic refraction. Hypermetropia was diagnosed in 72.5% of the patients in our series who were initially diagnosed with pseudostrabismus who later were diagnosed as having strabismus. Using our dataset, it was not possible to ascertain how many patients in our series underwent a cycloplegic refraction during their initial ocular examination. It is also possible that some had a cycloplegic refraction but were incompletely cyclopleged. Anisometropia is also a risk factor for accommodative esotropia.1,13 In our series, 16.1% of the children who were initially diagnosed with pseudostrabismus and who were later diagnosed with strabismus had anisometropia. Birch et al.13 has reported that hypermetropic anisometropia is a risk factors for developing accommodative esotropia. Pritchard and Ellis1 reported that 10% of patients who were initially diagnosed with pseudostrabismus and later were diagnosed with strabismus had anisometropia. In addition to being a risk factor for developing accommodative esotropia, untreated anisometropia also increases the risk of amblyopia. The higher incidence of amblyopia among patients in our series who later developed esotropia may have been partially due to anisometropic amblyopia.1,9,10
Other series have also reported a higher incidence of intermittent exotropia among children initially diagnosed with pseudostrabismus.1,2,4 Silbert and coworkers2 reported 20 of 201 (10.0%) children initially diagnosed with pseudostrabismus later developed strabismus and 3 of these 20 (15%) patients had intermittent exotropia. Among all patients who were initially diagnosed with pseudostrabismus in our series who were later diagnosed with strabismus, 23.6% of them had exotropia. Exotropia in young children is usually intermittent. We recommend that all children with presumed pseudostrabismus undergo cover-uncover testing to facilitate the diagnosis of intermittent exotropia.
Amblyopia was present in 37.7% of the children initially diagnosed with pseudostrabismus who were later diagnosed with esotropia. The prevalence of amblyopia in esotropic patients in our series was similar to other studies (21.6%,14 27.3%,15 30.7%,16 and 32.7%,17). Reddy and coworkers18 reported that the absence of amblyopia on the initial examination helped to predict whether children would be able to achieve alignment with single-vision glasses. In addition, children with accommodative esotropia and amblyopia were more than twice as likely to require strabismus surgery compared to non-amblyopic children. Amblyopia was present in 30.2% of the children in our series initially diagnosed with pseudostrabismus who were later diagnosed with exotropia. In our series the prevalence of amblyopia in exotropic patients was higher than other population-based studies (8.7%19, 15.6%20, and 25.9%21). The prevalence of amblyopia might have been higher in our series than other studies because patients were identified as having amblyopia if an ICD code for amblyopia was only used once.
In our study, esotropia was diagnosed at a younger age than exotropia. Other studies have also reported esotropia being diagnosed at a younger age than exotropia although this varies among different ethnicities.5,6 In our study, the incidence of esotropia was highest among white children. Strabismus was diagnosed more than a year later in the pseudostrabismus group (median; 3.21 years, IQR; 2.13 – 4.63) compared to the control group (median; 2.28 years (IQR; 1.43 – 3.16)). There are several possible explanations for the difference. First, the parents of children initially diagnosed with pseudostrabismus may have been reluctant to seek medical attention again since they had already been told by a medical professional that their child did not have strabismus. Second, when the parent of a child who had been previously diagnosed with pseudostrabismus called to schedule an appointment, it may have been scheduled as a routine rather than an urgent appointment.
In our series, 21.9% of the children diagnosed with pseudostrabismus underwent at least one strabismus surgery and 3.7% (63 of 1,725 patients) underwent two or more strabismus surgeries. In contrast, only 12.1% of the children in our control group who were diagnosed with strabismus underwent strabismus surgery. It is generally accepted that a delay in diagnosing accommodative esotropia increases the risk of a child needing strabismus surgery to achieve ocular alignment. Park and Oh22 have also reported that delaying the treatment of children with esotropia is associated with worse stereopsis outcomes. We hypothesize that many of the children in our pseudostrabismus group who underwent strabismus surgery would not have required surgery if they would have been correctly diagnosed with accommodative esotropia at an earlier age and prescribed the appropriate spectacle correction.
Study Limitations
This study should be interpreted in the context of several limitations. First, our study used claims data and ICD codes. Claims data has intrinsic limitations arising from miscoding and changing insurance companies. We do not know what definitions were used for diagnosing amblyopia and refractive errors. We also do not know if the claims were submitted by pediatric or general ophthalmologists. Second, the dataset we used may not be representative of the entire United States population because it is based on private health insurance claims. For this reason, certain ethnicities may be over or underrepresented in this dataset. However, race/ethnicity data from our dataset is similar to the 2010 Census in the United States.23 Third, we limited our analysis of manifest strabismus to ICD codes for esotropia, exotropia, and unspecified heterotropia. We did not evaluate whether patients had other types of strabismus because our study was focused on the misdiagnosis of pseudoesotropia or pseudoexotropia. Finally, there may have been a selection bias among children diagnosed with pseudostrabismus. Perhaps they had a higher risk of developing strabismus because they were more likely to have a family history of strabismus that motivated their parents to bring them in for an ocular examination even before they had true strabismus.
Young children diagnosed with pseudostrabismus are at an increased risk of developing strabismus. We recommend that children only be diagnosed with pseudostrabismus after they have undergone a cycloplegic refraction to exclude moderate or high hypermetropia and after performing an alternate prism cover test.
Supplementary Material
ACKNOWLEDGMENT/DISCLOSURE
Finding/Support: This work was supported in part by the Dong-A University Research Fund, NIH UL1 TR001085, P30 EY026877 and Research to Prevent Blindness, Inc
Financial Disclosures: The following authors have no financial disclosures: Won Yeol Ryu, and Scott R. Lambert.
Other Acknowledgments: The authors thank Laurel Stell, Ph.D, from the Department of Biomedical Data Science, Stanford University and Carrie Marino for biostatistical assistance.
Biographies
Biosketch
Dr. Ryu is an Associate Professor at Dong-A University College of Medicine, Busan, South Korea. He did his ophthalmology residency at Dong-A University followed by a fellowship in strabismus and pediatric ophthalmology at Anam Hospital of Korea University Medical Center in Seoul, South Korea. His areas of interest include strabismus and neuro-ophthalmology.

Lambert Biosketch
Scott R. Lambert, MD, is a professor of ophthalmology at Stanford University School of Medicine. He is the chair of the Infant Aphakia Treatment Study and the Pediatric Ophthalmic Technology Assessment Committee for the American Academy of Ophthalmology. He is co-editor of the fifth edition of the Taylor & Hoyt’s Pediatric Ophthalmology and Strabismus and the author or coauthor of over 200 peer reviewed articles. His clinical interests include pediatric cataract and strabismus surgery.

References
- 1.Pritchard C, Ellis GS Jr. Manifest strabismus following pseudostrabismus diagnosis. American Orthoptic Journal. 2007;57(1):111–117. [DOI] [PubMed] [Google Scholar]
- 2.Silbert AL, Matta NS, Silbert DI. Incidence of strabismus and amblyopia in preverbal children previously diagnosed with pseudoesotropia. J AAPOS. 2012;16(2):118–119. [DOI] [PubMed] [Google Scholar]
- 3.Mohan K, Sharma A. Development of refractive accommodative esotropia in children initially diagnosed with pseudoesotropia. J AAPOS. 2012;16(3):266–268. [DOI] [PubMed] [Google Scholar]
- 4.Roh IH, Choi MY. Clinical characteristics of strabismic children with a history of pseudoesotropia. Journal of the Korean Ophthalmological Society. 2006;47(9):1449–1453. [Google Scholar]
- 5.Friedman DS, Repka MX, Katz J, et al. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116(11):2128–2134 e2121–2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McKean-Cowdin R, Cotter SA, Tarczy-Hornoch K, et al. Prevalence of amblyopia or strabismus in asian and non-Hispanic white preschool children: multi-ethnic pediatric eye disease study. Ophthalmology. 2013;120(10):2117–2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Repka MX, Lum F, Burugapalli B. Strabismus, Strabismus Surgery, and Reoperation Rate in the United States: Analysis from the IRIS Registry. Ophthalmology. 2018;125(10):1646–1653. [DOI] [PubMed] [Google Scholar]
- 8.Multi-ethnic Pediatric Eye Disease Study G. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months the multi-ethnic pediatric eye disease study. Ophthalmology. 2008;115(7):1229–1236 e1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anwar DS, Woreta FA, Weng CY, Repka MX. Incidence of esotropia developing in subjects previously diagnosed with pseudoesotropia: a pilot study. Strabismus. 2012;20(3):124–126. [DOI] [PubMed] [Google Scholar]
- 10.Sefi-Yurdakul N, Tugcu B. Development of Strabismus in Children Initially Diagnosed with Pseudostrabismus. Strabismus. 2016;24(2):70–73. [DOI] [PubMed] [Google Scholar]
- 11.Silbert AL, Matta NS, Silbert DI. Incidence of strabismus and amblyopia in preverbal children previously diagnosed with pseudoesotropia. Am Orthopt J. 2013;63:103–106. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs HB. Pseudostrabismus: an audit. Br J Ophthalmol. 1978;62(11):763–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Birch EE, Fawcett SL, Morale SE, Weakley DR Jr., Wheaton DH. Risk factors for accommodative esotropia among hypermetropic children. Invest Ophthalmol Vis Sci. 2005;46(2):526–529. [DOI] [PubMed] [Google Scholar]
- 14.Wan MJ, Chiu H, Shah AS, Hunter DG. Long-term Surgical Outcomes for Large-angle Infantile Esotropia. Am J Ophthalmol. 2018;189:155–159. [DOI] [PubMed] [Google Scholar]
- 15.Esposito Veneruso P, Bruzzese D, Magli A. Long-term development of refractive error in refractive, nonrefractive and partially accommodative esotropia. PLoS One. 2018;13(9):e0204396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohney BG, Lilley CC, Green-Simms AE, Diehl NN. The long-term follow-up of accommodative esotropia in a population-based cohort of children. Ophthalmology. 2011;118(3):581–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mohan K, Sharma A. Long-term treatment results of accommodative esotropia. J AAPOS. 2014;18(3):261–265. [DOI] [PubMed] [Google Scholar]
- 18.Reddy AK, Freeman CH, Paysse EA, Coats DK. A data-driven approach to the management of accommodative esotropia. Am J Ophthalmol. 2009;148(3):466–470. [DOI] [PubMed] [Google Scholar]
- 19.Fu J, Li SM, Liu LR, et al. Prevalence of amblyopia and strabismus in a population of 7th-grade junior high school students in Central China: the Anyang Childhood Eye Study (ACES). Ophthalmic Epidemiol. 2014;21(3):197–203. [DOI] [PubMed] [Google Scholar]
- 20.Romanchuk KG, Dotchin SA, Zurevinsky J. The natural history of surgically untreated intermittent exotropia - Looking into the distant future. Journal of Aapos. 2006;10(3):225–231. [DOI] [PubMed] [Google Scholar]
- 21.Robaei D, Kifley A, Mitchell P. Factors associated with a previous diagnosis of strabismus in a population-based sample of 12-year-old Australian children. Am J Ophthalmol. 2006;142(6):1085–1088. [DOI] [PubMed] [Google Scholar]
- 22.Park KA, Oh SY. Early alignment versus delayed alignment in patients with hyperopia and esotropia. J AAPOS. 2016;20(1):3–6. [DOI] [PubMed] [Google Scholar]
- 23.Humes KR, Jones NA, Ramirez RR. Overview of race and Hispanic origin: 2010. US Census Bureau; In: March; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.