Abstract
In the United States, sexual minority (SM) status is associated with a number of health disparities. Based on mounting evidence, stigma and discrimination have been cited as key barriers to health equity for this population. We estimated the prevalence of three types of discrimination as a function of age among SM adults from the National Epidemiological Study of Alcohol Use and Related Conditions III (NESARC-III) (2012-2013). Among SM adults, reports of past-year general discrimination, victimization, and healthcare discrimination varied by age, with peaks in early adulthood and again in midlife. Age trends varied by biological sex, with males experiencing significantly more general discrimination, victimization, and healthcare discrimination at specific ages. Age trends also varied by sexual identity, as LGB-identifying SMs were significantly more likely to experience all forms of discrimination across all ages. Policies preventing homophobic discrimination and victimization are necessary given the pervasiveness of these experiences across adulthood.
Keywords: sexual minority, LGB, discrimination, minority stress
Introduction
Compared to heterosexuals, sexual minorities (SMs) (i.e., those who identify as lesbian, gay, and bisexual [LGB], have same-sex attractions, or have same-sex partners) demonstrate persistent and vexing health disparities in health (IOM, 2011), including higher rates of depression (Hatzenbuehler, 2009), anxiety (Bostwick, Boyd, Hughes, & McCabe, 2008), suicidality (King et al., 2008), substance use and abuse (McCabe, Hughes, Bostwick, West, & Boyd, 2009), cardiovascular disease (Lick, Durso, & Johnson, 2013), preventable morbidity (Hatzenbuehler, Keyes, & McLaughlin, 2011; Branstrom, Hatzenbuehler, Pachankis, & Link, 2016), and all-cause mortality (Cochran, Bjorkenstam, & Mays, 2016; Hatzenbuehler, Bellatorre, Lee, Finch, Muennig, & Fiscella, 2014). Based on mounting evidence detailing SM-related health disparities, the National Institute on Minority Health and Health Disparities formally recognized SMs as a health disparity population in 2016, citing stigma and discrimination as key barriers to health equity for this population (NIMHD, 2016).
Stigma is a fundamental cause of population health inequalities (Hatzenbuehler, 2014). That is, stigma (1) has been linked to mental, behavioral, and physical health outcomes; (2) prevents access to resources that buffer or correct poor health; and (3) persists across time and place through ever-evolving mechanisms that maintain health inequities for marginalized populations (Hatzenbuehler, Phelan, & Link, 2013). Discrimination represents aparticularly well-studied form of stigma. In their meta-analysis on discrimination and health, Pascoe and Richman (2009) noted three primary pathways through which discrimination impacts health: 1) a direct relationship—discrimination results in poorer mental and physical health, even after controlling for confounders; 2) a relationship via heightened stress response—discrimination results in increased stress, which then leads to poorer mental and physical health; and 3) a relationship via health behaviors—discrimination results in poor health behavior choices, subsequently resulting in negative mental and physical health outcomes (Pascoe & Richman, 2009).
The ways in which stigma contributes to poor health among SMs has largely been captured by the minority stress model (Hatzenbuehler, 2009; Meyer, 2003), which posits that proximal and distal stressors, such as internalized (e.g., internalized homophobia, expectations of rejection) and enacted stigma (e.g., discrimination, victimization) are mechanisms through which health disparities manifest. Indeed, research has linked these unique, chronic, and socially-based minority-specific stressors to sexual orientation-related disparities in mental (Mustanski, Andrews, & Puckett, 2016), behavioral (McCabe, Bostwick, Hughes, West, & Boyd, 2010), and physical health (Lick et al., 2013; Evans-Polce et al., 2019). For example, sexual minorities who experienced anti-LGB discrimination were more likely to report recent suicidal behavior (Fish, Rice, Lanza, and Russell; 2018).Odds of past year substance use disorders are nearly four times greater among LGB adults who reported recent discrimination (McCabe, Bostwick, Hughes, West, & Boyd, 2010). Further, SMs living in communities with high levels of anti-gay prejudice how shorter life-expectancies than SMs living in communities characterized by low levels of prejudice (Hatzenbuehler, Slopen, & McLaughlin, 2014). Importantly, these premature deaths were largely attributed to stress-related illness (e.g., suicide, cardiovascular disease).
Researchers consistently find that SMs report more victimization and discrimination than heterosexuals(Mays & Cochran, 2001; Toomey, Russell, & Denny, 2016). Studies that document experiences of SM-based discrimination and victimization among youth have outnumbered those of adults, and few examine SM-based discrimination during middle or late adulthood (ages 50+) (IOM, 2011; Fredriksen-Goldsen & Muraco, 2010). Yet, the limited research using adult samples demonstrates that experiences with anti-gay prejudice, discrimination, and victimization are prevalent in adulthood (McCabe et al., 2010) and impact health and well-being (Lick, Durso, & Johnson, 2013; Hatzenbuehler & McLaughlin, 2014).
Theoretically-grounded mechanisms of health disparities are necessary to develop empirically informed interventions for at-risk populations (Stall et al., 2016). Stigma-related experiences are key drivers of sexual orientation-related population health disparities, morbidity, and mortality (IOM, 2011; Hatzenbuehler et al., 2013); it is therefore important to understand and contextualize these experiences across the lifespan to address the health inequities that result from them (NIMHD, 2016; Gee, Walsemann, & Brondolo, 2012). A simple but important strategy for understanding the link between discrimination and health among SMs, and the policies and interventions to address it, is to identify the prevalence of the experience across the life course. That is, at what age(s) are discriminatory experiences most likely to occur? Understanding when discrimination occurs improves the sensitivity and efficacy of discrimination measures, thus improving research and prevention strategies (Gee et al., 2012). Conversely, disregarding age-related differences in discrimination may oversimplify our view of discrimination and its relationship with health. This could result in misreporting these experiences during critical developmental periods of highest exposure and missing opportunities for relevant policies and health promotion strategies.
Given that adjacent literature suggests that different forms of discrimination (i.e., racial discrimination) vary in nature and intensity across the life course (Gee, Walsemann, Brandolo, 2012), we hypothesized that discrimination would not be a static experience across the life course, and that different types of discrimination would be more prevalent at different points of adulthood. To examine this hypothesis, we used weighted time-varying effect models (Lanza, Vasilenko, & Russell, 2016; Dziak, Li, & Wagner, 2017) to estimate the age-varying prevalence of past-year SM-based (1) general discrimination, (2) verbal and physical victimization, and (3) healthcare discrimination using a large, nationally-representative sample of SM adults from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) III. The application of TVEM offers an novel perspective on developmentally-situated experiences of SM-based discrimination and victimization and how these experiences may vary as a function of sex and sexual identity.
Methods
Sample
Data are from NESARC-III, a nationally representative study noninstitutionalized civilian adults. Using a stratified probability-sampling method (described in detail elsewhere)(Grant, et al., 2015), interviewers collected data via face-to-face interviews in 2012-2013. We restricted these analyses to SMs, aged 18-65, who provided a response to at least one of the discrimination assessment items.
Sexual minority health scholars argue that measures of sexual minority status should reflect your research question of interest (IOM, 2011; The Williams Institute, 2009). Minority stress theory explains how experiences of stigma influence the health of sexual minorities, regardless of identification. Indeed, research indicates that sexual minorities who do not identify as LGB (e.g., MSM, questioning youth) are still likely to report stigma on the basis of their sexuality. We defined SM status using an inclusive classification strategy and included participants who endorsed one or more of the following: same-sex attraction, same-sex sexual partners, or a lesbian, gay, or bisexual identity. Specifically, participants were asked to describe their sexual attraction as: “only attracted to females”, “mostly attracted to females”, “equally attracted to females and males”, “mostly attracted to males”, “only attracted to males”, and “unknown”). If a participant endorsed any same-sex attraction, they were included in our sample. Finally, participants were also asked to report the sex of their sexual partners throughout lifetime. Response options included “only males”, “only females”, “both males and females”, “never had sex”, and “unknown”. Participants who endorsed any same-sex sexual partners were coded as SM sample. Finally, participants were asked to state which of the following best described them, with response options of “heterosexual (straight)”, “gay or lesbian”, “bisexual”, “not sure”, and “unknown”. Participants who endorsed gay/lesbian or bisexual were included in our sample. These criteria resulted in a final sample of 2,993 sexual minorities. This approach allowed for an inclusive analytic sample of sexual minorities while offering the ability to compare sexual minorities who identified as LGB to those who did not.
Study Measures
NESARC-III asks a series of six questions derived from the Experiences of Discrimination Scale (Krieger, Smith, Naishadam, Hartman, & Barbeau, 2005) to assess how often participants experienced discrimination in the last 12 months because they were “assumed to be gay, lesbian or bisexual” with response options ranging from 0 = never to 5 = very often. The six questions included “About how often did you experience discrimination in”: (1) “your ability to obtain health care or health insurance coverage,” (2) “how you were treated when you got care,” (3) “public, like on the street, in stores or in restaurants,” (4) “any other situation ” as well as how often they were (5) “called names ”, and (6) “made fun of, picked on, pushed, shoved, hit, or threatened with harm”. These six items were collapsed into three types of discrimination: general discrimination (i.e, in public, on the street, in stores and restaurants, and other situations), victimization (i.e. called names, picked on, pushed, hit, or threatened), and healthcare discrimination (i.e., obtaining health care or health insurance coverage, discrimination in treatment). Each category of discrimination was recoded to reflect respondents who did and did not experience each for discrimination or victimization in the past year (yes = 1, no = 0).
Analyses
First, we calculated weighted frequencies of all variables to describe the study sample. We used weighted time-varying effect models (The Methodology Center, n.d.; Lanza et al., 2016; Dziak, et al., 2017) to estimate the weighted prevalence of each type of anti-LGB discrimination by age. TVEM is a flexible, semi-parametric model that estimates rates and associations as a flexible function of age (Lanza et al., 2016). The main advantage of this approach is that it provides specific age ranges of risk, as well as age ranges during which covariates are significantly associated with an outcome. For all analyses, we graphically displayed age trends for the estimated prevalence of each type of discrimination, along with the corresponding 95% confidence intervals. All analyses were conducted in SAS 9.4 using the %TVEM macro (The Methodology Center, n.d; Dziak, et al., 2017). We first specified an intercept-only logistic TVEM for each outcome (general discrimination, victimization, and healthcare discrimination) to estimate age trends in rates of exposure. Second, we included sex and sexual identity as predictors in each model to identify differences in age-varying rates of discrimination and victimization by sex (male versus female) and sexual identity (to compare SMs who identify as LGB to SMs with same-sex attractions and/or behaviors but do not identify as LGB). Finally, we used weighted logistic TVEM to statistically test the age-specific differences in discrimination and victimization by sex and sexual identity.
Results
Weighted Demographic Characteristics and Sexual Minority Indicators
Consistent with previous research (IOM, 2011; McCabe et al., 2009), attraction to both men and women was the most commonly reported indicator of SM status (64%) followed by exclusive same-sex attraction (19%). Nearly half (45%) of the sample reported sexual behavior with both male and female sexual partners over their lifetime, with 14% reporting exclusively same-sex partners, and 37% reporting exclusively other-sex partners. Fifty-nine percent of the sample identified as heterosexual, 18% as bisexual, 17% as gay or lesbian, and 5% as unsure of their sexual identity.
The median age of participants was 37 (IQR: 26,51). The sample was racially and ethnically diverse; 64% were White, 13% Black, and 15% Hispanic, which reflects similar diversity as documented in the overall NESARC-III sample (Grant et al., 2015).
Among the full sample of sexual minorities (N=2993), 37% identified as lesbian, gay, or bisexual. Among those who identified as LGB, 43% were male, while 36% of those who didn’t identify as LGB were male. Race/ethnicities were similar among those who identified as LGB and those who didn’t. 65% of those who identified as LGB were White, 15% were Black. Among those who didn’t identify as LGB, 63% were White and 13% were Black. Those who identified as LGB had a mean age of 36 which was slightly lower than the mean age (mean = 40) of those who didn’t identify.
Among the full sample, 61% identified as female and 39% male. Males were 65% White and 12% Black. Females were 63% White and 14% Black. Males were slightly older on average, with a mean age of 41 compared to the female mean age of 37.
Weighted Age-Varying Rates of Discrimination Attributed to SM Status
In total, 17% of SMs, aged 18-65, reported experiencing at least one form of discrimination in the past year that was attributed to their SM status: Thirteen percent of the sample reported general discrimination, 12% reported victimization, and 7% reported healthcare discrimination. Four percent of the sample reported all three types of discrimination in the past year.
Figure 1 illustrates weighted past-year prevalence for each type of discrimination by age. General discrimination was significantly more common than healthcare discrimination until age 33; victimization was significantly more common than healthcare discrimination until 29. Specifically, among SM adults age 18, approximately 21% reported victimization and 18% reported general discrimination in the last year, compared to 6% who reported healthcare discrimination. The prevalence of general discrimination and victimization decreases across ages 18 to 34, when they plateau at about 10% and 7%, respectively, until the early 40s. Rates of discrimination and victimization showed a second peak in the mid-50s before decreasing again, with fewer than 10% reporting general discrimination or victimization at age 65. Healthcare discrimination was lowest among those in early adulthood (~8%) and highest reports (11% prevalence) among people in their early fifties.
Figure 1.
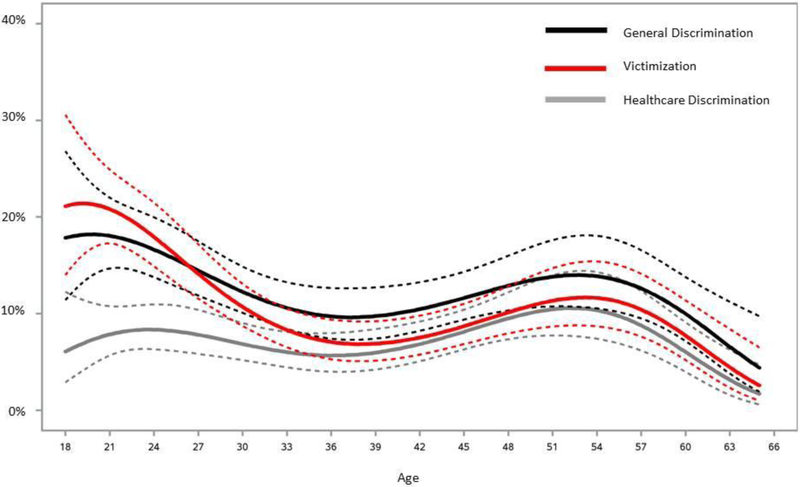
Age-varying effects estimating the prevalence of past-year general discrimination, victimization, and healthcare discrimination attributed to sexual minority status among sexual minorities, ages 18-65, in the United States using NESARC-III (2012-2013) data. 95% confidence intervals (CIs) shown with dashed lines.
General Discrimination
Experiences with general discrimination varied by both sex and sexual identity (Figure 2) across age, although the shape of these age trends followed a pattern similar to the overall sample with general discrimination most commonly reported among those in their late teens and middle age. Reports of general discrimination in the past year peaked for males around age 24 (22% prevalence) and for females around age 18 (20%). The prevalence dropped to 3% and 5%, respectively, by age 65 (Figure 2). Odds of experiencing general discrimination were significantly higher among SM males, compared to SM females, between the ages of 23-30 and again between the ages of 49-56.
Figure 2.
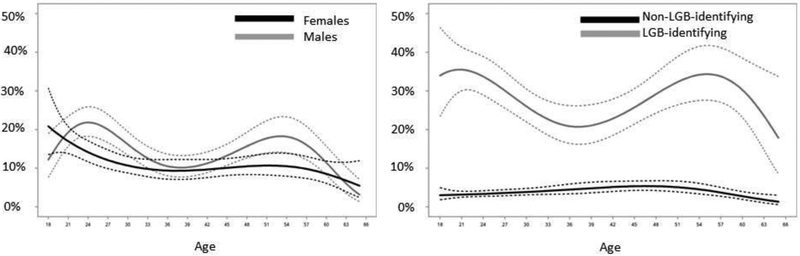
Age-varying effects estimating the prevalence of past-year general discrimination attributed to sexual minority status among sexual minority females and males (Panel 1) and non-LGB-identified and LGB-identified (Panel 2), ages 18-65, in the United States using NESARC-III (2012-2013) data. 95% confidence intervals (CIs) shown with dashed lines.
For those who identify as LGB, the prevalence of general discrimination in the past year was approximately 35% at age 18, and was equally high among those in their mid-fifties. In sharp contrast, less than 6% of non-LGB-identified participants, regardless of age, reported general discrimination in the previous year. LGB-identified individuals had significantly higher odds of reporting general discrimination across all ages compared to non-LGB-identified participants. For example, among 30-year-old SMs, LGB-identified adults were 9 times more likely than non-LGB-identified adults to report general discrimination in the past year (OR = 8.5, 95% CI: 5.0, 14.5).
Victimization
Experiences with victimization also varied considerably by sex, sexual identity, and age (Figure 3). Past year victimization among SM females was most common at age 18 (21% prevalence) and plateaued to approximately 7% by age 30. Rates of victimization among SM males were highest around age 21 (28%) declined to around 10% in the thirties, and then rose again to approximately 16% by age 55. The odds of past-year victimization were significantly higher for SM males compared to SM females between the ages of 20-33 and again between 44-57. The disparity between SM males and SM females with respect to victimization was greatest at age 25 (OR: 2.47, 95% CI: 1.53, 3.97) and again at age 53 (OR: 2.32, 95% CI: 1.23, 4.38).
Figure 3.
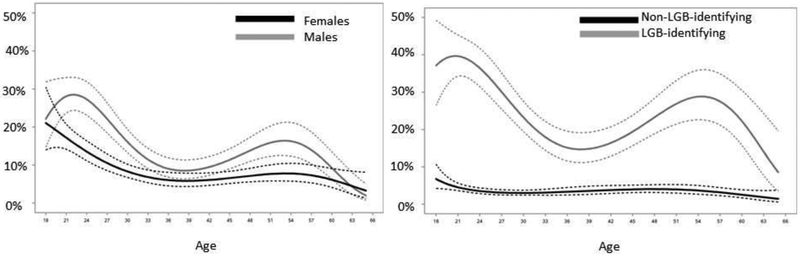
Age-varying effects estimating the prevalence of past-year victimization attributed to sexual minority status among sexual minority females and males (Panel 1) and non-LGB-identified and LGB-identified (Panel 2), ages 18-65, in the United States using NESARC-III (2012-2013) data. 95% confidence intervals (CIs) shown with dashed lines.
Age-specific experiences of victimization also varied by sexual identity. Among LGB-identified individuals, the prevalence of past-year victimization was highest among 21 year olds (40%). Rates were lower for those in their late twenties, thirties, and early forties, but rates peaked again for those in their late forties and fifties (~28%). Notably, the prevalence of past-year victimization among SMs who identify as LGB only fell below 10% for 65-year-olds. Across all ages, less than 7% of non-LGB-identifying participants reported experiencing victimization in the previous year. Statistical tests revealed that the association between sexual identity and victimization was strongest for those in their early twenties, where LGB-identified adults were approximately 16 times (OR:15.7, 95% CI:8.8,28.1 at age 24) more likely to have experienced victimization in the last year compared to non-LGB-identified SM adults. Differences in LGB-identified and non-LGB-identified reports of past year victimization were smallest, but still significant, at age 39 (OR:4.7; 95% CI:2.4,9.4).
Healthcare Discrimination
Healthcare-related discrimination experiences (Figure 3) followed a distinct age trend compared to general discrimination and victimization: regardless of subpopulation, healthcare discrimination peaked in middle age, during the early fifties. Males reported the highest prevalence of past-year healthcare discrimination at age 54 (14% prevalence) and females at age 50 (8%). Males had significantly higher odds of reporting past-year healthcare discrimination between the ages of 52 and 59. The odds ratio comparing healthcare discrimination among SM males to SM females was greatest at age 57 (OR: 2.39, 95% CI: 1.13, 5.05).
Adults who identified as LGB had the highest prevalence of healthcare discrimination in their mid-fifties (23% at age 55). Non-LGB-identified adults were most likely to experience healthcare discrimination in their late forties (5% at age 49). The odds of experiencing healthcare discrimination were significantly higher for LGB-identified individuals across ages 18-65. Sexual identity differences in healthcare discrimination were largest in the late teens and early 20s and again in the late fifties and early sixties.
Discussion
Among a national sample of SM adults, we found that reports of past-year discrimination and victimization significantly varied by age, and that experiences with discrimination and victimization differed on the basis of sex (i.e., male vs. female) and sexual identity (i.e., LGB- vs. non-LGB identified). General discrimination and victimization were statistically more common than healthcare discrimination until the age of 30, but prevalence rates of the three types of discrimination did not significantly differ between the ages of 30 and 65 among the full SM sample. Young adult and midlife males (compared to females) were more likely to experience general discrimination and victimization; males in midlife were also more likely to report past-year healthcare discrimination. Those who identified as LGB (compared to those who reported same-sex attractions and/or partners but did not identify as LGB) were more likely to experience all types of discrimination across ages. Minority stress theory posits that SMs suffer compromised health because of stigma-related stressors such as discrimination and victimization (Meyer, 2009). Our study documents changing rates of discrimination across the lifespan and that age-graded experiences differ for specific SM subpopulations. Results offer important information regarding the developmental differences in experiences of enacted anti-LGB stigma and potential critical periods for focused policy and prevention.
Although we report nuanced findings by age and type of discrimination, in general, results suggest that that experiences of discrimination peak in early adulthood, decline, and then increase again in middle adulthood. Given that a dearth of literature has evaluated how discrimination experiences vary by adult age among sexual minorities (c.f., Evans-Polce et al., 2019, although with the same data), we compare these findings to the literature on racial discrimination. A systematic review (Paradies, 2006) of empirical research on racism reveals that self-reported racism varies inconsistently across age, with some studies finding higher prevalence of reports of experiencing racism among older individuals and others finding higher prevalence among younger adults. Our bi-modal trajectory of sexual minority discrimination suggests that both older and younger adults might be most vulnerable to experiencing discrimination, thus reflecting the findings related to race-based discrimination. Of course, LGB people espouse unique cohort and generational differences in the experience of anti-LGB sentiment (see Hammack, Frost, Meyer, & Pletta, 2018), and the sociopolitical forces that confer anti-LGB sentiment have vastly different historical and contemporary contexts than other forms of prejudice and stimga (e.g., racism, xenophobia, etc.). Thus, more work is needed to better understand how experiences of discrimination and victimization may vary for different cohorts of LGB people, as well as its impact on health.
Our results extend the current literature in a number of important ways. First, our analyses provide the first report of how three stigma-related experiences vary by age across the life course (ages 18-65). Consistent with previous studies (Toomey, et al., 2016; Katz-Wise & Hyde, 2012), our results suggest high levels of anti-LGB stigma among SM young people; nearly one in four 18-year-olds reported victimization based on their actual or perceived sexual identity, nearly one in five indicated experiencing general discrimination, and approximately 7% reported discrimination in health care settings in the past year. In tracking these reports across ages, we note a steeper decline in victimization relative to general discrimination from age 18 to the mid-thirties, but an appreciable rise in the experience of healthcare discrimination. Given that discrimination in healthcare settings peaked during the late-forties and early-fifties, midlife may be an important developmental period to examine the experience of healthcare discrimination and its impact on health and health-seeking behavior among SMs.
Second, consistent with previous research (Herek, 2009; Toomey, et al., 2016; Katz-Wise & Hyde, 2012), we note a considerable sex disparity in the experience of anti-LGB discrimination and victimization among SM adults. Compared to SM females, SM males were more likely to experience general discrimination and victimization, both in early adulthood and again in midlife. Additional findings reveal that SM males may be more vulnerable to discrimination in healthcare settings in the fifties relative to SM females. These findings reflect sex-differences in homophobic attitudes. For example, a study by Herek (2002) found that heterosexual people were more likely to regard gay men as mentally ill, were less supportive of gay men’s adoption rights, and had more negative reactions to gay men, relative to lesbians (Herek, 2002).
Finally, we tested whether experiences of discrimination and victimization varied between those who self-identified as LGB compared to those who reported same-sex attraction and/or behavior but did not identify as LGB. In doing so, we note stark differences in the prevalence of discrimination and victimization by sexual identity, and substantial variability among LGB-identified participants by age. For example, compared to SMs who did not identify as LGB, LGB-identified SMs were more likely to experience all three types of discrimination across all ages. These relationships reflect a jarring disparity, whereby LGB individuals have consistently greater exposure to recent discrimination, up to nearly 40% for certain ages, while less than 10% of non-LGB-identifying participants reported experiencing any form of discrimination in the past year, regardless of age. These findings suggest that adopting a stigmatized social identity may confer greater risk for enacted stigma such as discrimination and victimization.
Notably, patterns of discrimination by age were similar across males, females, and LGB-identifying SMs with the exception of non-LGB SMs, although the magnitude of the effects varied by type of stigma. That is, general discrimination and victimization were most prevalent in early adulthood followed by a second peak in middle age (i.e., during the fifties). Explanations for the elevated prevalence during midlife cannot be ascertained with these data. It is possible that the patterns we see are cohort- rather than age-related (Hammack et al., 2018). Coming of age during eras defined by distinct LGB-relevant events and issues (i.e., AIDs epidemic, fight for marriage equality) could predispose some cohorts to be hypervigilant, or espouse expectations of rejection. Those in the middle-aged cohort may therefore be more attuned to experiences of anti-LGB prejudice given that they would have been young adults during the AIDs epidemic.(Hammack et al., 2018).
Healthcare discrimination also peaked in middle age (late forties and early fifties).We hypothesize that this trend is likely related to greater healthcare usage, as per-person health care spending increases with age (CME, 2019). Future research should evaluate whether experiences of discrimination in healthcare settings vary by age even after adjustment for healthcare usage and how older LGB people’s interaction with healthcare providers may impede or inhibit their healthcare-seeking behavior.
This research is strengthened by its use of a large and diverse nationally-representative dataset. Historically, research documenting discrimination among SMs has been limited by small non-probability samples (IOM, 2011). The scope of the NESARC-III data also allowed us to examine weighted estimates of anti-LGB stigma-related experiences across a wide variety of ages and life stages among different subsamples of SM adults, enabling us to elucidate unique patterns of minority stress that were age-, sex-, and sexual identity-specific. The inclusion of multiple sexual-orientation-specific discrimination measures strengthened our analysis, and our results highlight the importance of incorporating such measures in nationally-representative data (Sell, 2017).
Despite these strengths, we note several limitations. First, measures of discrimination relied on self-reports, though recall bias (Coughlin, 1990) was likely minimized by limiting analysis to reports of discrimination in the past year. Our measure of anti-LGB discrimination also explictily prompted participants to report discrimination and victimization because they were “assumed to be gay, lesbian or bisexual”. These items may therefore have different meaning for those who do and do not identify as LGB. Second, because the sample size was too small to allow for intersectional analyses, we were unable to investigate differences in the experience of interlocking stigmas on the basis of sexual identity and sex or sexual identity and race. For this same reason we were unable to assess whether lesbian- and gay-identified participants reported differences in discrimination compared to bisexual-identified individuals. Further attention to heterogeneity among those who identify as LGB is important given documentation of biphobia (Israel & Mohr, 2004) and elevated health risk among bisexuals (Fredriksen-Goldsen & Muraco, 2010; Plöderl & Tremblay, 2016). Additionally, we used a definition of SM status that included those who report any same-sex attraction, behavior, or SM identity (Lindley, Walsemann, Carter, 2012). Given that some sexual minorities are more likely than others to experience or report discrimination (i.e., people with LGB identities), this is a conservative approach for estimating the total prevalence of discrimination for sexual minorities. At the same time, this inclusive measure of sexual minority status affords comparisons among sexual minorities, as we have done here. Finally, we were unable to contextualize these experiences of discrimination and victimization. For example, we could not ascertain whether the rise in reported anti-LGB stigma during midlife is the result of cohort or developmental effects. Additional work is needed to tease apart these potential subgroup differences in identity, sex, cohort, and development. An examination of discrimination across the life course may also contribute to our understanding of the minority stress theory, as discrimination may have differential effects by age. Given that stress reactivity literature finds that older people have better coping strategies and are less reactive to stressful experiences (Almeida & Horn, 2004), similar patterns may exist for discrimination. This is an important area for future research.
Our results illustrate age-varying rates of three types of anti-SM stigma. SMs in early (before age 30) and middle adulthood (the fifties) are most likely to report general discrimination, victimization, and healthcare discrimination particularly among male and LGB-identified participants. Importantly, reports of healthcare discrimination peaked in midlife, around age 55. Understanding how experiences of discrimination change across the lifespan is an important step in explicating its role in health among SMs and policies and practices needed to address it. Future studies should continue to explore subgroup differences in the experience of stigma as well as how intersecting identities inform experiences of discrimination, their contexts, and the degree to which they occur across the life course. Future research should consider age-related effects when examining the link between discrimination and health to better understand associations between SM-related discrimination on health across life course, as well as the factors that contribute to resilience in the face of such discrimination.
Public Health Implications
Reducing discrimination will likely require broad cultural and societal approaches, and efforts within a multitude of systems that shape the health and wellbeing of SMs across the life course. These include families, communities, schools, workplaces, and healthcare, which are often informed by city, state, and national policy (Russell & Fish, 2016). For example, SMs living in states with enumerated protections report lower levels of internalized homophobia (Riggle, Rostosky, & Horne, 2010), substance abuse (Hatzenbuehler, 2009), mood disorders, and psychiatric comorbidity. Youth in LGB-supportive climates are also less likely to engage in suicidal behavior (Hatzenbuehler, et al., 2011). LGB-affirming policies and programs at work and school are associated with less discrimination, and subsequently better health (Lick et al., 2013; Badgett, Durso, Kastanis, & Mallory, 2013). Given the documented health effects of stigma and discrimination (Lick, et al., 2013; Branstrom, et al., 2016; Cochran, et al., 2016; Hatzenbuehler et al., 2014; Meyer, 2003), these analyses highlight a critical need for investigations and intervention across the life course.
Figure 4.
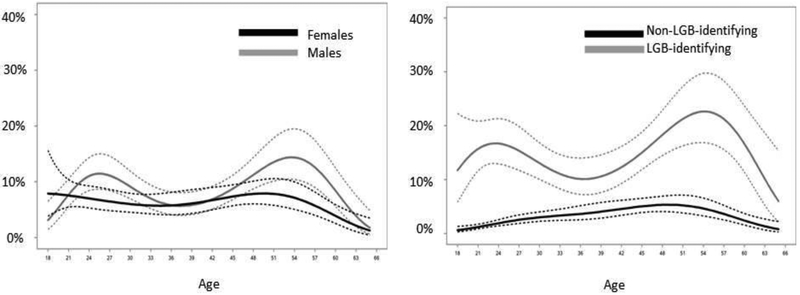
Age-varying effects estimating the prevalence of past-year healthcare discrimination attributed to sexual minority status among sexual minority females and males (Panel 1) and non-LGB-identified and LGB-identified (Panel 2), ages 18-65, in the United States using NESARC-III (2012-2013) data. 95% confidence intervals (CIs) shown with dashed lines.
ACKNOWLEDGEMENTS:
The project described was partially supported by the National Center for Advancing Translational Sciences, Grant KL2 TR002015 and Grant UL1 TR002014.This study was further supported in part by award P50DA039838 and award DA039854 from the National Institute on Drug Abuse and by the National Institute on Alcohol Abuse and Alcoholism grant number F32AA023138. We gratefully acknowledge support from Eunice Kennedy Shriver National Institute of Child Health and Human Development viaP2CHD042849, awarded to the Population Research Center at The University of Texas at Austin and P2CHD041041 awarded to the Maryland Population Research Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This manuscript was prepared using a limited access dataset obtained from the National Institute on Alcohol Abuse and Alcoholism and does not reflect the opinions or views of NIAAA or the U.S. Government.
Footnotes
The authors have no conflicts of interest to report.
Contributor Information
Cara Exten Rice, The Methodology Center, Pennsylvania State University, 426 HHD, University Park, PA, 16802, USA; School of Health Sciences, College of Health Sciences, Walden University, Minneapolis, MN, USA.
Jessica N. Fish, Department of Family Science, School of Public Health, University of Maryland, College Park, MD, 20742, USA.
Stephen T. Russell, Population Research Center, Human Development & Family Sciences, University of Texas at Austin, Austin, TX, 78712, USA.
Stephanie T. Lanza, Department of Biobehavioral Health, Pennsylvania State University, University Park, PA, 16802, USA.
References
- Almeida DM, Horn MC. Is daily life more stressful during middle adulthood? In: Brim OG, Ryff CD, Kessler RC, editors. How healthy are we?: A national study of well-being at midlife. The University of Chicago Press; Chicago: 2004. pp. 425–450. [Google Scholar]
- Badgett MVL, Durso LE, Mallory C, & Kastanis A (2013). The Business Impact of LGBT-Supportive Workplace Policies. Retrieved from https://escholarship.org/uc/item/3vt6t9zx
- Bostwick WB, Boyd CJ, Hughes TL, & McCabe SE (2010). Dimensions of sexual orientation and the prevalence of mood and anxiety disorders in the United States. American Journal of Public Health, 100(3), 468–475. 10.2105/AJPH.2008.152942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bränström R, Hatzenbuehler ML, Pachankis JE, & Link BG (2016). Sexual Orientation Disparities in Preventable Disease: A Fundamental Cause Perspective. American Journal of Public Health, 106(6), 1109–15. 10.2105/AJPH.2016.303051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services (CME). NHE-Fact-Sheet. (2019, February 20).Retrieved April 3, 2019, from https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet.html [PubMed]
- Cochran SD, Björkenstam C, & Mays VM (2016). Sexual Orientation and All-Cause Mortality Among US Adults Aged 18 to 59 Years, 2001–2011. American Journal of Public Health, 106(5), 918–20. 10.2105/AJPH.2016.303052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin SS (1990). Recall bias in epidemiologic studies. Journal of Clinical Epidemiology, 43(1), 87–91. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2319285 [DOI] [PubMed] [Google Scholar]
- Dziak JJ, Li R, Wagner AT. (2017). WeightedTVEM SAS Macro for Accommodating Survey Weights and Clusters. University Park: The Methodology Center, Penn State; 2017. Retrieved from http://methodology.psu.edu [Google Scholar]
- Evans-Polce RJ, Veliz PT, Boyd CJ, Hughes TL, & McCabe SE (2019). Associations between sexual orientation discrimination and substance use disorders: differences by age in US adults. Social Psychiatry and Psychiatric Epidemiology. 10.1007/s00127-019-01694-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, & Muraco A (2010). Aging and Sexual Orientation: A 25-Year Review of the Literature. Research on Aging, 32(3), 372–413. 10.1177/0164027509360355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Walsemann KM, & Brondolo E (2012). A life course perspective on how racism may be related to health inequities. American Journal of Public Health. 10.2105/AJPH.2012.300666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Smith SM, Jung J, Zhang H, Chou SP, … Hasin DS (2015). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): reliability of substance use and psychiatric disorder modules in a general population sample. Drug and Alcohol Dependence, 148, 27–33. 10.1016/j.drugalcdep.2014.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammack PL, Frost DM, Meyer IH, Pletta D. (2018). Gay men’s health and identity: Social change and the life course. Archives of Sexual Behavior 47(1), 59–74.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135(5), 707–30. 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, & McLaughlin KA (2011). The protective effects of social/contextual factors on psychiatric morbidity in LGB populations. International Journal of Epidemiology, 40(4), 1071–80. 10.1093/ije/dyr019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, & Link BG (2013). Stigma as a fundamental cause of population health inequalities. American Journal of Public Health, 103(5), 813–21. 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, & Fiscella K (2014). Structural stigma and all-cause mortality in sexual minority populations. Social Science & Medicine (1982), 103, 33–41. 10.1016/j.socscimed.2013.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Slopen N, McLaughlin KA, & McLaughlin KA (2014). Stressful life events, sexual orientation, and cardiometabolic risk among young adults in the United States. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association, 33(10), 1185–94. 10.1037/hea0000126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, & McLaughlin KA (2014). Structural stigma and hypothalamic-pituitary-adrenocortical axis reactivity in lesbian, gay, and bisexual young adults. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine, 47(1), 39–47. 10.1007/s12160-013-9556-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM (2002). Gender gaps in public opinion about lesbians and gay men. Public Opinion Quarterly 66 (1), 40–66. [Google Scholar]
- Herek GM (2009). Hate Crimes and Stigma-Related Experiences Among Sexual Minority Adults in the United States. Journal of Interpersonal Violence, 24(1), 54–74. 10.1177/0886260508316477 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Lesbian, G. B. and T. H. I. and R. G. and O. (2011). The Health of Lesbian, Gay, Bisexual, and Transgender People. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. National Academies Press; (US: ). Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22013611 [PubMed] [Google Scholar]
- Israel T & Mohr JJ. (2004). Attitudes toward bisexual men and women. Journal of Bisexuality, 4(1–2): 117–134. [Google Scholar]
- Katz-Wise SL, & Hyde JS (2012). Victimization Experiences of Lesbian, Gay, and Bisexual Individuals: A Meta-Analysis. Journal of Sex Research, 49(2–3), 142–167. 10.1080/00224499.2011.637247 [DOI] [PubMed] [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, & Nazareth I (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 8, 70 10.1186/1471-244X-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Smith K, Naishadham D, Hartman C, & Barbeau EM (2005). Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Social Science & Medicine, 61(7), 1576–1596. 10.1016/j.socscimed.2005.03.006 [DOI] [PubMed] [Google Scholar]
- Lanza ST, Vasilenko SA, & Russell MA (2016). Time-varying effect modeling to address new questions in behavioral research: Examples in marijuana use. Psychology of Addictive Behaviors, 30(8), 939–954. 10.1037/adb0000208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lick DJ, Durso LE, & Johnson KL (2013). Minority Stress and Physical Health Among Sexual Minorities. Perspectives on Psychological Science, 8(5), 521–548. 10.1177/1745691613497965 [DOI] [PubMed] [Google Scholar]
- Lindley LL, Walsemann KM, & Carter JW (2012). The Association of Sexual Orientation Measures With Young Adults’ Health-Related Outcomes. American Journal of Public Health, 102(6), 1177–1185. 10.2105/AJPH.2011.300262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays VM, & Cochran SD (2001). Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health, 91(11), 1869–76. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11684618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, & Boyd CJ (2009). Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction (Abingdon, England), 104(8), 1333–45. 10.1111/j.1360-0443.2009.02596.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Bostwick WB, Hughes TL, West BT, & Boyd CJ (2010). The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health, 100(10), 1946–52. 10.2105/AJPH.2009.163147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Methodology Center, Penn State: WeightedTVEM SAS Macro (Version 2.6.0) [Software]. http://methodology.psu.edu. Accessed June 28, 2017. [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–97. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Andrews R, & Puckett JA (2016). The Effects of Cumulative Victimization on Mental Health Among Lesbian, Gay, Bisexual, and Transgender Adolescents and Young Adults. American Journal of Public Health, 106(3), 527–33. 10.2105/AJPH.2015.302976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Minority Health and Health Disparities (NIMHD). (2016). Sexual and gender minorities formally designated as a health disparity population for research purposes. 2016; Retrieved February 28, 2017, from https://www.nimhd.nih.gov/about/directors-corner/message.html
- Paradies Y (2006). A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology, 35(4), 888–901. 10.1093/ije/dyl056 [DOI] [PubMed] [Google Scholar]
- Pascoe EA, & Smart Richman L (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531–554. 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggle EDB, Rostosky SS, & Horne SG (2010). Psychological distress, well-being, and legal recognition in same-sex couple relationships. Journal of Family Psychology, 24(1), 82–86. 10.1037/a0017942 [DOI] [PubMed] [Google Scholar]
- Russell ST, & Fish JN (2016). Mental Health in Lesbian, Gay, Bisexual, and Transgender (LGBT) Youth. Annual Review of Clinical Psychology, 12(1), 465–487. 10.1146/annurev-clinpsy-021815-093153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sell RL (2017). LGBTQ Health Surveillance: Data = Power. American Journal of Public Health, 107(6), 843–844. 10.2105/AJPH.2017.303798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Matthews DD, Friedman MR, Kinsky S, Egan JE, Coulter RWS, … Markovic N (2016). The Continuing Development of Health Disparities Research on Lesbian, Gay, Bisexual, and Transgender Individuals. American Journal of Public Health, 106(5), 787–9. 10.2105/AJPH.2016.303183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toomey RB, Russell ST, & Denny T (2016). The Role of Sexual Orientation in School-Based Victimization: A Meta-Analysis. Youth & Society, 48(2), 176–201. 10.1177/0044118X13483778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Williams Institute. (2009). Best Practices for Asking Questions about Sexual Orientation on Surveys. Retrieved from https://williamsinstitute.law.ucla.edu/wp-content/uploads/SMART-FINAL-Nov-2009.pdf


