Abstract
Purpose:
The success of checkpoint blockade against glioblastoma (GBM) has been disappointing. Anti-PD-1 strategies may be hampered by severe T-cell exhaustion. We sought to develop a strategy that might license new efficacy for checkpoint blockade in GBM.
Experimental Design:
We characterized 4-1BB expression in tumor infiltrating lymphocytes (TIL) from human GBM. We implanted murine tumor models including glioma (CT2A), melanoma (B16), breast (E0771), and lung carcinomas (LLC) intracranially (IC) and subcutaneously (SC), characterized 4-1BB expression, and tested checkpoint blockade strategies in vivo.
Results:
Our data reveal that 4-1BB is frequently present on non-exhausted CD8+ tumor-infiltrating lymphocytes (TIL) in human and murine GBM. In murine gliomas, 4-1BB agonism and PD-1 blockade demonstrate a synergistic survival benefit in a CD8+ T-cell dependent manner. The combination decreases TIL exhaustion and improves TIL functionality. This strategy proves most successful against intracranial (IC) CT2A gliomas. Efficacy in all instances correlates with the levels of 4-1BB expression on CD8+ TIL, rather than with histology or with IC versus SC tumor location. Proffering 4-1BB expression to T-cells licenses combination 4-1BB agonism and PD-1 blockade in models where TIL 4-1BB levels had previously been low and the treatment ineffective.
Conclusion:
While poor T-cell activation and severe T-cell exhaustion appear to be limiting factors for checkpoint blockade in GBM, 4-1BB agonism obviates these limitations and produces long-term survival when combined with anti-PD-1 therapy. Furthermore, this combination therapy is limited by TIL 4-1BB expression, but not by the intracranial compartment, and therefore may be particularly well-suited to GBM
Keywords: Glioblastoma, Immunotherapy, Immune Checkpoint Blockade, 4-1BB agonism
Introduction
Immune checkpoint blockade targeting PD-1 +/− CTLA-4 is now an FDA-approved strategy for a number of solid tumors. Despite its promise, checkpoint blockade has demonstrated limited success as a monotherapy in glioblastoma (GBM) (1). Efficacy against other intracranially situated tumors, such as melanoma brain metastases, has been modest, but responses remain limited to a minority of patients (2). GBM in particular may hinder checkpoint blockade strategies by proffering a low mutational burden (3); broad tumor heterogeneity (4); restricted CNS drug / immune access (5); and perhaps most saliently, rampant T cell dysfunction with little baseline effective T cell activation to perpetuate with therapy (6-12). Resistance to immune checkpoint blockade at the T cell level is marked by the upregulation of multiple alternative immune checkpoints (13), a state that frequently signals T cell exhaustion. Our group recently demonstrated severe T cell exhaustion amongst tumor-infiltrating lymphocytes (TIL) isolated from patients and mice with GBM and the corresponding inability to respond to PD-1 blockade (10). Improving and sustaining T cell activation within the CNS thus remains an important goal for licensing checkpoint blockade strategies against cancers harbored within the intracranial (IC) compartment.
Costimulatory receptors of the tumor necrosis factor receptor superfamily (TNFRSF) such as 4-1BB (CD137, TNFRSF9) accumulate on T cells upon activation. Co-stimulation through 4-1BB powerfully augments T cell activation via several downstream signaling pathways, including c-Jun N-terminal kinase (JNK) (14), extracellular signal-regulated kinase (ERK) (15), and phosphatidylinositol 3-kinase (PI3K) and Akt (Protein Kinase B) (16). Stimulation-induced signaling ultimately converges on the master transcription factor NF-κB (17), profoundly augmenting T cell proliferation, cytokine production, and cytolytic effector function. Additionally, 4-1BB signaling inhibits activation-induced cell death (AICD) in T cells (18) and promotes long-term survival and immunologic memory (19). These features make 4-1BB a potentially attractive target for cancer immunotherapies. Targeting 4-1BB with agonist antibodies in clinical trials, however, has yielded only modest benefit in patients with solid tumors, while also conferring risks for hepatotoxicity (20). Newer therapeutic tactics, such as with 4-1BB-stimulating aptamers, offer the ability to limit off-target toxicity and have renewed interest in this approach (21-23). Furthermore, combining 4-1BB agonism with immune checkpoint blockade has demonstrated substantial synergy, and may diminish the toxicities associated with either treatment alone (24). 4-1BB agonism, however, remains an unexplored approach within the IC compartment, where checkpoint blockade failures have been notable to date.
We investigated 4-1BB agonism as both a monotherapeutic and a checkpoint blockade adjuvant in GBM and other IC tumors. We characterized 4-1BB expression on TIL isolated from human and murine GBM, finding that 4-1BB is expressed disproportionately and at high levels on non-exhausted, activated GBM TIL. 4-1BB agonism on 4-1BB expressing GBM TIL improves their function and averts their exhaustion. In murine models of both IC and subcutaneous (SC) glioma (CT2A), melanoma (B16), breast (E0771), and lung carcinomas (LLC), IC CT2A glioma TIL demonstrated the highest levels of 4-1BB expression. Likewise, we found that 4-1BB agonism substantially licensed PD-1 blockade in IC CT2A, producing 50% long-term survivors. Success for this combination strategy was dependent on CD8+ T cells and directly correlated with TIL 4-1BB expression across tumor histologies and location, with efficacy being most pronounced for IC GBM, even compared to its SC counterpart. Furthermore, in models where TIL 4-1BB levels had previously been low and treatment ineffective, proffering 4-1BB expression to T-cells was sufficient to newly license the combination of 4-1BB agonism and PD-1 blockade.
Materials and Methods
Patient samples
According to protocols approved by the Duke Cancer Center Institutional Review Board, tumor samples were obtained from newly diagnosed GBM patients at the time of resection. All studies were conducted in accordance with recognized ethical guidelines (U.S. Common Rule, 45 CFR 46, 21 CFR 50, 21 CFR 56, 21 CFR 312, 21 CFR 812, and 45 CFR 164.508–514). Written consent was obtained from all subjects when necessary. All blood and tumor specimens were stored at room temperature and processed within 12 hours. Samples were digested and processed as described previously (25). Tumor digests were frozen in 90% FBS/10% DMSO and stored at −80C. Blood was obtained healthy individuals or from patients at time of surgery, PBMC were isolated, and samples were frozen and stored in the same conditions. All TILs and PBMC were thawed and analyzed simultaneously.
Mice
The Institutional Animal Care and Use Committee (IACUC) approved all experimental procedures. Animal experiments involved the use of female C57BL/6 mice at 6–12 weeks of age. C57BL/6 mice were purchased from Charles River Laboratories. Mice were housed at the Duke University Medical Center Cancer Center Isolation Facility (CCIF) under pathogen-free conditions.
Cell lines
Cell lines examined in this study included CT2A malignant glioma, B16F10 melanoma, Lewis Lung Carcinoma (LLC), and E0771 breast medullary adenocarcinoma. All four cell lines are syngeneic on the C57BL/6 background in which they were studied. In preparation for implantation, CT2A, B16F10, and LLC cells were grown in vitro in Dulbecco’s Modified Eagle Medium (DMEM) with 2mM 1-glutamine and 4.5 mg/mL glucose (Gibco, Gaithersburg, MD) containing 10% FBS. E0771 cells were grown in vitro in RPMI 1640 (Gibco) containing 10% FBS plus 1% HEPES (Gibco). Cells were split and harvested in the logarithmic growth phase. For intracranial (i.c.) implantation, tumor cells in PBS were then mixed 1:1 with 3% methylcellulose and loaded into a 250 μL syringe (Hamilton). The needle was positioned 2 mm to the right of the bregma and 4 mm below the surface of the skull at the coronal suture using a stereotactic frame. Note that 1 × 104 SMA-560, CT2A, E0771, and LLC cells or 500 B16F10 cells were delivered in a total volume of 5 μL per mouse. For subcutaneous (s.c.) implantation, 5 × 105 SMA-560, CT2A, E0771, and LLC cells or 2.5 × 105 B16F10 cells were delivered in a total volume of 200 μL per mouse into the s.c. tissues of the left flank.
Tissue processing and flow cytometry
Mouse-specific antibodies were purchased from BD Biosciences, eBioscience, or Biolegend (see supplementary Table 1). Human-specific antibodies were purchased from BD Biosciences, eBioscience, or Biolegend (see supplementary Table 2). Tissue processing, T cell stimulation, flow cytometry and cytokine detection was performed as described previously (25).
Antibody injections
Mouse-specific antibodies were obtained from Bio X Cell including anti-mouse PD-1 (RMP1–14, Catalog #BE0146) and anti-mouse 4-1BB (LOB12.3, Catalog # BE0169). For PD-1 and 4-1BB antibody treatments, 200 μg of each antibody was diluted with PBS for a total injection volume of 200 μL. Mice received intraperitoneal (IP) injections of antibody every 3 days, starting on day 9 after tumor implantation, for a total of 3–4 treatments. Control treatments consisted of 200 μL PBS. CD8 and CD4 depletion was performed as described previously (26). In brief, CD8 or CD4 T cells were depleted via IP injection of 200ug anti-CD8 (53–6.7, BioXCell Catalog #BE0004) or 200ug anti-CD4 (GK1.5, BioXCell Catalog #BE0003–1) at day 5, 6, 7, and 14 following tumor implantation for early CD8 depletion or at day 12, 13, and 14 for late-start CD8 depletion.
In vitro stimulation with 4-1BB agonist antibody
Stimulation of human TIL was performed as described previously (18). In brief, GBM tumor digests with previously determined 4-1BB expression patterns were thawed, rested overnight in T cell media (RPMI supplemented with 10% FBS and 1x Non-Essential Amino Acids (NEAA), Sodium Pyruvate, β-mercaptoethanol, and Penicillin/Streptomycin), and added into stimulation plates (approximately 200,000 lymphocytes per well in a 96-well plate). Plates were prepared via overnight coating at 4C with 10ng/mL OKT3 (Abbott) and 1000ng/mL 4-1BB (AF838, R&D Systems) and subsequent blocking with 2% BSA for 30 min at room temperature. Cells were cultured for 72h at 37C, then split into fresh uncoated plates and cultured in the presence of IL-2 (200IU/mL) for 48 more hours. Following the 5-day period of stimulation, cells were harvested, stimulated with PMA/Ionomycin in the presence of Golgiplug for 6 hours, and intracellular staining was performed via flow cytometry.
4-1BB T cell transduction
To overexpress 4-1BB on T cells, we cloned 4-1BB cDNA (Dharmacon, Cat # MMM1013-202799845) into the MSGV backbone as described previously (27). The following primers were used to amplify the 4-1BB fragment: Forward 5’ TTTTGGATCCCATGGGAAACAACTGTTAC, Reverse 5’ TTTTGCGGCCGCTCACAGCTCATAGCCTCCT. A restriction digest using Nco1 and Not1 (NEB) was performed on both the 4-1BB fragment and the MSGV backbone. Following a gel extraction of both the 4-1BB fragment and the MSGV backbone, the rapid DNA dephosphorylation and ligation kit (Sigma) was used to anneal the fragment into the backbone. The ligation reaction was transformed into One Shot Top10 E. coli (Thermo Fischer) according to manufacturer’s directions, cells were plated on LB-ampicillin plates, and positive colonies were sent for sequencing to confirm correct insertion. In order to transduce naïve splenocytes with 4-1BB, we transfected 4-1BB into HEK 293 T cells with Lipofectamine Transfection Reagent (Invitrogen). We used 14.1ug of vector plasmid and 9.9ug pCL-Eco helper plasmid (Imgenex). On the same day, splenocytes were freshly harvested from OT-1 mice and cultured in T cell media supplemented with 50IU/mL IL-2 and 2.5μg/mL Concanavalin A. After 48 hours, splenic T cells were transduced with retroviral supernatant. Transduction was performed on non-tissue culture 24-well plates previously coated with 0.5mL of RetroNectin (Clontech) at a concentration of 25 μg/mL in PBS. Cells were plated at a density of 1×106/mL in viral supernatant supplemented with 50IU/mL IL-2. Cells were split every 48h for 5 days.
Statistical analysis
Statistical analysis was conducted in GraphPad Prism version 5.0 (GraphPad Software, La Jolla, CA), primarily using two-tailed, unpaired t-tests or one-way ANOVAs to compare means across groups with a designated significance level of 0.05. Analyses were adjusted for multiple comparisons using the Bonferoni adjustment as indicated. Bar graphs and dot plots display the mean +/− the standard error of the mean. Kaplan-Meier curves were generated for survival analyses and the Gehan-Breslow-Wilcoxon test was used to compare curves. The statistical tests employed for each data presentation are designated in respective figure legends.
Results
Activated, non-exhausted TIL express high levels of 4-1BB in GBM and are subject to improved function by 4-1BB agonism
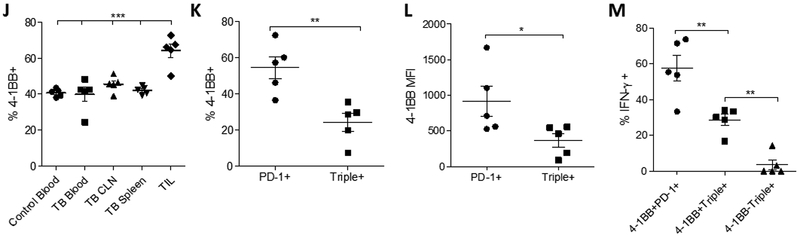
We initially examined 4-1BB expression on TIL and peripheral blood mononuclear cells (PBMC) isolated from patients with GBM. 4-1BB levels were found to be highest amidst GBM CD8+ TIL when compared to PBMC from either GBM patients or healthy donors (Fig 1A, representative histogram depicted in Fig 1B). 4-1BB+ TIL were also more likely to exhibit an activated, PD-1+ phenotype, rather than to express multiple immune checkpoints (PD-1+TIM-3+LAG-3+) (“triple positive”) (Fig 1C). Likewise, 4-1BB surface levels on PD-1+ TIL were higher than levels on PD-1+TIM-3+LAG-3+ triple positive TIL, as determined by median fluorescent intensity (MFI) (Fig 1D). We have recently shown that the “triple positive” phenotype typifies severe exhaustion among TIL in GBM, while PD-1 “single positive” TIL maintain function (10). Accordingly, among our patient samples here, 4-1BB+ TIL expressing PD-1 alone trended toward more IFN-γ production than PD-1- TIL and were significantly more likely to produce IFN-γ than CD8+ T cells co-expressing PD-1, TIM-3, and LAG-3 upon stimulation with PMA and ionomycin (Fig 1E).
Figure 1:
Activated, non-exhausted TIL express high levels of 4-1BB in GBM and are subject to improved function by 4-1BB agonism. A. Frequency of 4-1BB expression on CD8+ T cells, p values as calculated by unpaired t-test. B. Representative histogram of 4-1BB expression on control PBMC, GBM PBMC and GBM TIL. Plots are gated on singlets, live cells, and CD3+CD8+. C. Frequency of CD8+ 4-1BB+ TIL expressing PD-1 alone or PD-1, TIM-3, and LAG-3 (Triple+). ***p<0.001 by paired t-test. D. Median fluorescent intensity (MFI) of 4-1BB levels on PD-1+ or PD-1+TIM-3+LAG-3+ (Triple+) TIL isolated from human GBM. E. Frequency of IFN-γ+ TIL among PD-1 negative, PD-1 single positive, or PD-1/TIM-3/LAG-3 triple-positive CD8 TIL. **p<0.01 by paired t-test. F. Representative histogram showing TIL samples expressing either low (black) or high (red) levels of 4-1BB. Gated on singlets, live cells, lymphocytes, CD3+CD8+. G. Representative contour plot of IFN-γ following in vitro stimulation with a 4-1BB agonist antibody in patients’ CD8 TILs expressing either high or low levels of 4-1BB. H. IFN-γ production among CD8+ TIL from patients with either high or low levels of 4-1BB. Median Fluorescent Intensity (MFI) is depicted. *p<0.05 by unpaired t-test. I. Linear regression of IFN-γ production and expression of 4-1BB. p<0.0702. J. Frequency of 4-1BB expression on CD8 T cells in the blood of control mice vs. various compartments in tumor-bearing (TB) mice. CLN = ipsilateral tumor-draining cervical lymph nodes. ***p<0.001 by One-way ANOVA followed by Bonferroni’s Multiple Comparison Test. K. Frequency of CD8+ 4-1BB+ TIL expressing PD-1 alone or PD-1, TIM-3, and LAG-3. **p<0.01 by paired t-test. L. MFI of 4-1BB on PD-1+ or PD-1+TIM-3+LAG-3+ (Triple+) T cells isolated from CT2A TIL. M. Frequency of IFN-γ on cells expressing PD-1 and 4-1BB; 4-1BB, PD-1, TIM-3, and LAG-3; and PD-1, TIM-3, and LAG-3 but not 4-1BB as determined by Boolean gating of CT2A TIL re-stimulated in vitro with PMA/Ionomycin.
To determine whether 4-1BB expression on CD8+ TIL might permit a functional response to 4-1BB agonism, we performed an in vitro stimulation assay with a 4-1BB agonist antibody. To begin, TIL were isolated from patient GBM samples and separated into those expressing high or low levels of 4-1BB (Fig 1F). We then stimulated these cells in vitro with a 4-1BB agonist antibody (AF838, R&D systems) as described previously (18), and performed intracellular staining for the production of IFN-γ. CD8+ TIL with high levels of 4-1BB expression proved uniquely those able to produce IFN- γ when stimulated via 4-1BB agonism (Fig 1G, 1H) in a manner that appeared to correlate with levels of 4-1BB expression (p-value <0.07) (Fig 1I).
We next examined whether TIL 4-1BB expression might be recapitulated in murine GBM models, permitting further study in vivo. For these purposes, the CT2A murine glioma model was employed. Mice were implanted intracranially (IC) with CT2A glioma cells and blood, tumor, and lymphoid organs subsequently harvested. Levels of 4-1BB were compared on T cells from these tissues in tumor-bearing (TB) and control mice. CD8+ TIL isolated from CT2A glioma tumors consistently expressed higher levels of 4-1BB than T cells isolated from blood and lymphoid organs (Fig 1J). As with patient GBM TIL, 4-1BB-expressing murine CD8+ TIL were more likely to express PD-1 alone than to co-express the immune checkpoints PD-1, TIM-3, and LAG-3 (Fig 1K). Surface levels of 4-1BB were also lower in TIL co-expressing PD-1, TIM-3, and LAG-3 than TIL expressing PD-1 alone (Fig 1L). When TIL function was assessed by IFN-γ production, PD-1+ TIL expressing 4-1BB proved the most functional, while PD-1+TIM-3+LAG-3+ TIL not expressing 4-1BB were least capable of producing IFN-γ. The small numbers of PD-1+TIM-3+LAG-3+ TIL that co-expressed 4-1BB demonstrated intermediate functionality (Fig 1M).
4-1BB agonism improves GBM TIL function in vivo and synergizes with PD-1 blockade to avert T cell exhaustion
In order to ascertain whether 4-1BB agonism can restore TIL function in vivo in GBM, we employed an anti-4-1BB agonist antibody in CT2A-bearing mice and assayed TIL surface markers and cytokine producing ability by flow cytometry. Likewise, we assessed the capacity of PD-1 blockade to synergize with or perpetuate the effects of 4-1BB agonism on GBM TIL activation and function. Mice were implanted IC with CT2A and treated with control, PD-1 antibody alone, 4-1BB antibody alone, or PD-1 and 4-1BB antibodies together. Mice were sacrificed at day 17–20 following tumor implantation (when control animals were moribund). TIL were isolated, stained for classical and alternative immune checkpoints, and stimulated with PMA and ionomycin to assay for function. Among analyzed CD8+ PD-1+ TIL, co-expression of the immune checkpoints TIM-3 and LAG-3 decreased dramatically, but exclusively in the group receiving the combination treatment (Fig 2A). The proportions of severely exhausted CD8+ TIL co-expressing PD-1, TIM-3, and LAG-3 were also lower in animals treated with combined 4-1BB agonism and PD-1 blockade compared to untreated animals or to animals treated with either antibody alone (Fig 2B). Likewise, we observed trends toward increased numbers of CD8+ TIL (Fig 2C) and greater IFN-γ production by TIL (Fig 2D) in animals treated with both anti-4-1BB and anti-PD-1.
Figure 2:
4-1BB agonism improves TIL function in vivo and synergizes with PD-1 blockade to avert TIL exhaustion. A. Representative pseudocolor dot plots of TIM-3 and LAG-3 co-expression in mice bearing intracranial CT2A and treated with either vehicle (control), anti-PD-1 alone, anti-4-1BB alone, or anti-PD-1 and anti-4-1BB, as previously described. Tumors were harvested at day 17 following tumor implantation and TIL were isolated and stained. Plots are gated on singlets, live cells, CD3+, CD8+, PD-1+. B. Frequency of CD8+ TIL co-expressing PD-1, TIM-3, and LAG-3 in mice treated as indicated. *p<0.05, **p<0.01, ***p<0.001 by 1 way ANOVA followed by Bonferroni’s Multiple Comparison Test. C. Counts of CD8+ TIL per gram of tumor across treatment groups. D. Frequency of CD8+ TIL producing IFN-γ across treatment groups.
4-1BB agonism licenses previously ineffective PD-1 blockade in GBM in CD8+ T cell-dependent fashion
Given the observed impact on TIL function, we sought to determine whether 4-1BB agonism might license efficacy for anti-PD-1 in the CT2A model. Much as in human GBM, PD-1 blockade has been ineffective in this model (1). Once again, mice were implanted with CT2A and randomized to the following treatment groups: 1) control (isotype); 2) PD-1 blockade alone; 3) 4-1BB agonist alone; or 4) combination anti-PD-1 and anti-4-1BB. All mice received intraperitoneal (IP) injections of the respective treatment beginning at day 9 and every 3 days thereafter until day 18. Consistent with prior experience, mice treated with anti-PD-1 alone did not demonstrate a survival benefit (Fig. 3A). While 4-1BB agonism did prolong median survival from 28 to 35 days, no long-term survivors were seen (Fig. 3A). In contrast, mice treated with the combination of anti-PD-1 and anti-4-1BB achieved 50% long-term survival, observed even at day 80 after tumor implantation (Fig. 3A).
Figure 3:
4-1BB agonism licenses PD-1 blockade in IC glioma in a CD8+ T cell-dependent manner. A. Survival curve of mice bearing IC CT2A and treated with isotype (control), anti-PD-1, anti-4-1BB, or the combination (n=8 per group). Mice were treated at day 9, 12, 15, and 18 with 200μg of each antibody via IP injection. *p<0.05, **p<0.01, ***p<0.001 by Log-rank (Mantel-Cox) Test. B. Survival curve of mice bearing IC CT2A and treated with vehicle (control), anti-CD8, anti-PD-1 and anti-4-1BB, or anti-CD8 and anti-PD-1/anti-4-1BB (n=8 per group). Mice were depleted of CD8+ T cells at day 5, 6, 7, and 14 with 200μg anti-CD8. Anti-PD-1 and anti-4-1BB were administered as above. ***p<0.001 by log-rank (Mantel-Cox) Test. C. Survival curve of mice bearing IC CT2A and treated with vehicle (control), anti-PD-1 and anti-4-1BB, anti-PD-1 and anti-4-1BB and early start CD8 depletion (starting at day 5), and anti-PD-1 and anti-4-1BB and late start CD8 depletion (starting at day 12) (n=8 per group). ***p<0.001 by log-rank (Mantel-Cox) Test. (n=8 per group). D. Survival curve of mice bearing IC CT2A and treated with vehicle (control), anti-CD4, anti-PD-1 and anti-4-1BB, or anti-CD4 and anti-PD-1/anti-4-1BB (n=8 per group). Mice were depleted of CD4+ T cells at day 5, 6, 7, and 14 with 200μg anti-CD4. Anti-PD-1 and anti-4-1BB were administered as above. ***p<0.001 by log-rank (Mantel-Cox) Test.
Given our earlier finding of high 4-1BB expression amongst CD8+ TIL, we investigated whether the observed efficacy for the combination therapy was dependent on CD8+ T cells. Mice were implanted with CT2A and randomized to the following treatment groups: 1) control; 2) CD8+ T cell depletion alone; 3) combination anti-PD-1 and anti-4-1BB; or 4) CD8+ T cell depletion in conjunction with combination anti-PD-1 and anti-4-1BB treatment. For groups undergoing CD8+ T cell depletion, respective mice received anti-CD8 antibody at days 5, 6, 7, and 14 following tumor implantation, as described previously (26). CD8+ T cell depletion regimen alone did not impact survival in GBM-bearing mice, but it completely abrogated the long-term survival that was again observed with combination anti-4-1BB and anti-PD-1 treatment (Fig 3B). When the time course of CD8 depletion was varied, CD8+ T cells maintained their importance for efficacy even when depleted later at days 12, 13, 14 following tumor implantation (Fig 3C).
As CD8+ T cells do not act in isolation, we additionally assessed the role of CD4+ T cell help in mediating anti-4-1BB and anti-PD-1 treatment efficacy. Mice were implanted with CT2A and randomized to the following treatment groups: 1) control; 2) CD4+ T cell depletion alone; 3) combination anti-PD-1 and ant-4-1BB; or 4) CD4+ T cell depletion in conjunction with combination anti-PD-1 and anti-4-1BB treatment. As above, groups undergoing CD4+ T cell depletion received anti-CD4 antibody at days 5, 6, 7, and 14 following tumor implantation. CD4+ T cell depletion did not abrogate the survival benefit obtained with combined antibody treatment, and even trended towards enhancing efficacy (perhaps due to depletion of regulatory T cells) (Fig 3D).
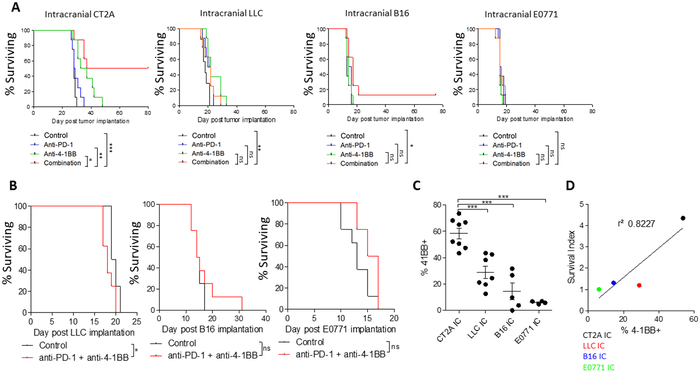
Anti-4-1BB + Anti PD-1 treatment efficacy correlates with 4-1BB expression on CD8+ TIL and not tumor histology or location
The efficacy observed against GBM led us to question whether the combination strategy of 4-1BB agonism and PD-1 blockade might likewise be effective against other difficult-to-treat brain-situated tumors, particularly those commonly metastatic to the brain. To this end, we employed murine IC models of lung cancer (Lewis Lung Carcinoma - LLC), melanoma (B16), and breast cancer (E0771). The respective mice were treated with either control, anti-PD-1 alone, anti-4-1BB alone, or the combination. While a mild prolongation of median survival was observed in the IC LLC model, and modest long-term survival was observed in the IC B16 model, the combination treatment was most effective in IC CT2A (Fig 4A). As the non-glioma models each exhibit shorter median survival than CT2A, even when untreated, the possibility existed that the differences in observed efficacy might be attributable instead to variations in the degree of tumor burden present at treatment outset. To control for this, experiments were repeated with treatment initiated at an earlier time point (Day 3 rather than 9) in the IC lung, melanoma, and breast cancer models. Despite the earlier treatment, efficacy of the combined antibody treatment remained poor in each model (Fig 4B).
Figure 4:
Anti-4-1BB + Anti PD-1 treatment efficacy correlates with 4-1BB expression on CD8+ TIL and not tumor histology or location. A. Survival curve of mice bearing IC CT2A, LLC, B16, or E0771 and treated with vehicle (control), anti-PD-1, anti-4-1BB, or the combination (n=8 per group). Mice were treated at day 9, 12, 15, and 18 with 200μg of each antibody via IP injection. *p<0.05, **p<0.01, ***p<0.001 by Log-rank (Mantel-Cox) Test. B. Survival curve of mice bearing IC LLC, B16, or E0771 and treated with vehicle (control) or anti-PD-1 and anti-4-1BB (n=8 per group). Mice were treated at day 3, 6, 9, 12, 15, and 18 with 200μg of each antibody via IP injection. *p<0.05, **p<0.01, ***p<0.001 by Log-rank (Mantel-Cox) Test. C. Frequency of CD8+ TIL expressing 4-1BB across different tumor types in untreated mice. Tumors were harvested when mice were moribund (day 15-20 after tumor implantation). ***p<0.001 by 1 way ANOVA followed by Bonferroni Multiple Comparison Test. D. Linear regression of 4-1BB levels on CD8+ TIL by the survival index, as measured by the ratio of median survival in mice treated with PD-1 and 4-1BB antibody to median survival in mice with tumor alone. p<0.09. E. Tumor growth curves of CT2A, LLC, B16, and E0771 implanted SC and subjected to the indicated treatments. Mice were sacrificed when tumors reached >2000mm3. 2-way ANOVA demonstrated significant effect of treatment in CT2A, B16, and E0771. *p<0.05, **p<0.01, ***p<0.001 by subsequent Bonferroni posttests. F. Frequency of CD8+ TIL expressing 4-1BB across IC and SC tumors. *p<0.05 by unpaired t-test.
Given this varying efficacy seen across models, we examined whether levels of 4-1BB expression on CD8+ TIL might likewise vary across tumors. We found that CD8+ lymphocytes infiltrating CT2A were significantly more likely to express 4-1BB than CD8+ lymphocytes infiltrating LLC, B16, or E0771 (Fig 4C). Furthermore, the percentages of CD8+ TIL expressing 4-1BB in a given IC tumor appeared to correlate somewhat with the efficacy of combination treatment against that tumor (p value <0.09) (Fig 4D).
Not finding universal efficacy against IC tumors, we investigated whether similar variability in both efficacy and TIL 4-1BB expression might be seen in tumors in the periphery. We implanted CT2A, LLC, B16, and E0771 subcutaneously (SC), and treated mice with either control, anti-PD-1 alone, anti-4-1BB alone, or anti-PD-1 and anti-4-1BB. Efficacy was assessed as a function of tumor volume. We found that the combination treatment was no longer more effective than PD-1 treatment alone in either SC CT2A or LLC, but it did confer additive efficacy against SC B16 and E0771 (Fig 4E). These differences in treatment effect across the IC and SC compartments prompted us to compare TIL 4-1BB expression across locations for a given histology. In so doing, we found that differences in the expression of 4-1BB on CD8+ TIL again corresponded to efficacy: for instance, 4-1BB expression was higher in CD8+ TIL isolated from IC CT2A than in SC CT2A, but instead was higher in SC B16 than in IC B16 (Fig 4F), matching the differential efficacy seen for each tumor in each location. For each tumor type then, CD8+ TIL 4-1BB expression was the better indicator of treatment efficacy than was tumor location, with IC CT2A demonstrating the both the highest TIL 4-1BB levels and the most impressive efficacy across all tumors and locations.
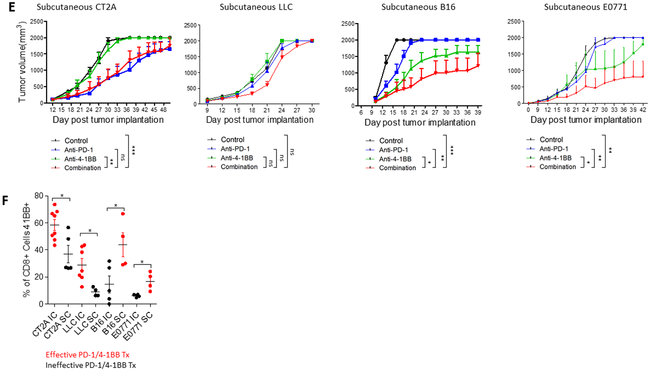
Enhancing 4-1BB levels on CD8+ T cells is sufficient to proffer an effective response to 4-1BB agonism and PD-1 blockade
Given the correlation observed between TIL 4-1BB expression and treatment efficacy, we sought to determine whether “providing” 4-1BB to T-cells would be sufficient to proffer efficacy in an IC tumor model where none had been observed before. We employed the IC B16 melanoma model, as these tumors had poorly responded to anti-PD-1 and anti-4-1BB treatment in prior experiments (Fig 4A) and had shown correspondingly low levels of 4-1BB on CD8+ TIL (Fig 4B). To provide a model antigen for targeting and for determining treatment impact on antigen-specific T cell responses, B16 cells were transfected with chicken ovalbumin (OVA). Accordingly, antigen-specific responses were enhanced in relevant host mice by adoptively transferring in OT-1 (OVA-specific CD8) T cells, which could also be engineered to over-express 4-1BB.
4-1BB was overexpressed on OT-1 T cells by retrovirally transducing OT-1 naïve splenocytes with a 4-1BB construct cloned into the MSGV backbone. 46.4% of OVA-tetramer+ CD8+ T cells expressed 4-1BB after transduction and 5-day expansion (Fig. 5A). We then implanted B16-OVA IC and randomized mice into the following groups (n=8 per group): 1) Control (untreated); 2) anti-PD-1 and anti-4-1BB combination treatment; 3) adoptive transfer of OT-1 cells only; 4) adoptive transfer of OT-1 cells overexpressing 4-1BB; 5) adoptive transfer of OT-1 cells followed by anti-PD-1 and anti-4-1BB combination treatment; or 6) adoptive transfer of OT-1 cells overexpressing 4-1BB followed by combination PD-1/4-1BB antibody treatment. Mice receiving adoptive transfers (ALT) received 107 either OT-1 T cells or OT-1 T cells overexpressing 4-1BB on day 7 following tumor implantation. Relevant antibody treatments were administered at days 9, 12, and 15. In the B16-OVA model, PD-1 and 4-1BB antibody treatment prolonged median survival slightly from 18 to 21 days. Neither the OT-1 ALT nor the OT-1 / 4-1BB ALT alone prolonged median survival. However, the OT-1 ALT followed by combinatorial anti-PD-1 and anti-4-1BB prolonged median survival from 18 to 30 days, while the OT-1 / 4-1BB ALT followed by combinatorial anti-PD-1 and anti-4-1BB prolonged median survival from 18 to 38 days and resulted in 40% long term survival (Fig 5B). We further assessed the impact of the anti-PD-1 and anti-4-1BB antibodies individually when given with the OT-1 / 4-1BB ALT. Neither anti-PD-1 nor anti-4-1BB individually enhanced survival when combined with OT-1 / 4-1BB ALT, where the combination of anti-PD-1 and anti-4-1BB with OT-1 / 4-1BB ALT significantly prolonged median survival and resulted in long-term survivors (Fig 5C).
Figure 5:
Enhancing 4-1BB levels on CD8+ T cells is sufficient to proffer an effective response to 4-1BB agonism and PD-1 blockade. A. representative dot plot of 4-1BB expression on OVA-tetramer+ CD8+ T cells isolated from OT-1 splenocytes (gray) and transduced with 4-1BB (black). B. Survival curve of mice bearing IC B16-OVA and treated with vehicle (control), anti-PD-1 and anti-4-1BB, OT-1 ALT, OT-1 ALT transduced with 4-1BB, OT-1 ALT in combination with anti-PD-1 and anti-4-1BB, or OT-1 ALT transduced with 4-1BB and treated with anti-PD-1 and anti-4-1BB (n=8 per group). Mice receiving ALT were given 107 cells intravenously at day 7. Mice receiving antibody treatments were treated at day 9, 12, and 15 with 200μg of anti-PD-1 and anti-4-1BB via IP injection. C. Survival curve of mice bearing IC B16-OVA and treated with OT-1 ALT transduced with 4-1BB. Mice were either treated with ALT alone, ALT and anti-PD-1, ALT and anti-4-1BB, or ALT and anti-PD-1 and anti-4-1BB. ALT and antibody treatments were given as described above. *p<0.05, **p<0.01, ***p<0.001 by Log-rank (Mantel-Cox) Test.
Discussion
Immune checkpoint blockade has rapidly emerged as a promising therapeutic strategy against a variety of solid tumors, yet has shown limited success in GBM and the intracranial compartment (1,2,28). While checkpoint blockade may be limited in the intracranial setting by several factors (3-5), severe T cell exhaustion is a prominent saboteur amidst GBM (10,11). Checkpoint blockade is dependent upon the availability of functional, activated T cells for its effectiveness, an amenity not afforded amongst dysfunctional, exhausted GBM TIL with poor tumor infiltration. We hypothesized that a strategy that could improve TIL numbers and activation while averting T cell exhaustion might proffer newly licensed efficacy to checkpoint blockade in GBM.
As 4-1BB signaling in T cells can improve T cell effector functions (16), inhibit activation-induced cell death (AICD) (18), and promote long-term T cell survival and immunologic memory (19), we set out to investigate the effects of 4-1BB agonism on GBM TIL. We examined TIL 4-1BB levels, ultimately finding it present at particularly high levels on activated, non-exhausted TIL within GBM. Although the higher levels of 4-1BB observed on GBM patient TIL did not quite reach significance, certain patients clearly demonstrated high levels of 4-1BB on their tumor-infiltrating T cells. Likewise, we found that 4-1BB agonism is indeed a viable strategy for improving TIL function in both human and murine GBM, when 4-1BB is present. Amongst the patient GBM TIL we examined, 57% expressed high levels of 4-1BB, suggesting that 4-1BB agonism may be a viable therapeutic outlet in a significant proportion of GBM patients.
Given its capacity to improve TIL function, we investigated 4-1BB agonism as both a monotherapeutic and as an adjuvant to checkpoint blockade in GBM and other IC tumors. Our study is the first to demonstrate that 4-1BB agonism can license PD-1 blockade in glioma. Previous preclinical studies show that PD-1 blockade can be efficacious in murine glioma (29,30), yet these studies have not translated to clinical efficacy. We utilized an immunologically stringent model of murine glioma that is resistant to PD-1 blockade to better mimic human GBM, and showed that 4-1BB agonism licensed responses to PD-1 blockade in this model. Traditionally, PD-1 blockade is thought to rescue the function of exhausted T cells that have sustained a progressive, hierarchical, yet sometimes reversible loss of function. A pair of recent studies, however, has demonstrated that PD-1 blockade may instead act on the activation and effector phases of T cell responses (31,32). The implication is that PD-1 blockade may require T cells that are not yet exhausted (33). In light of these findings, the failure of PD-1 blockade in GBM is altogether unsurprising, and may reflect the severe T cell exhaustion we have previously shown (10,11).
We demonstrate here that 4-1BB is expressed on activated, non-exhausted TIL, and that agonizing the 4-1BB on these TIL appears to improve their function while simultaneously avoiding their exhaustion. While further studies are needed to provide definitive evidence that 4-1BB agonism when combined with PD-1 blockade is capable of reversing T cell exhaustion, we do see some evidence that “triple positive” T cells may retain some functional activity (IFN-γ production) when 4-1BB is present. These findings suggest that 4-1BB agonism may play a tailored, complementary role improving baseline T cell activation and averting exhaustion, thereby overcoming resistance to immune checkpoint blockade.
Surprisingly, the efficacy of combined 4-1BB agonism and checkpoint blockade was independent of (and unfazed by) tumor type or location (brain vs. flank), but instead dependent simply on levels of TIL 4-1BB expression. This finding has multiple implications. First, this strategy is not seemingly subject to the typical limitations conferred by intracranial tumor locale. An exceedingly unusual finding, for instance, was the greater efficacy we observed with the combination treatment when used against IC gliomas compared to the SC gliomas implanted within the flank. This may make strategies combining 4-1BB agonism and checkpoint blockade especially well suited to the intracranial compartment (and perhaps GBM), where few systemically delivered treatment options are effective.
A second implication of therapeutic dependence on TIL 4-1BB levels (rather than tumor type or location) is that if TIL can be either provided with or coaxed into 4-1BB expression, then 4-1BB agonism may be utilized somewhat broadly in tumors, even in those whose TIL otherwise express low levels of 4-1BB. This was indeed our finding, as providing 4-1BB-expressing T cells to mice with IC melanoma proffered new efficacy to the combination of 4-1BB agonism and PD-1 blockade. While adoptive transfer of T cells overexpressing 4-1BB may improve responses, however, such strategies are expensive and subject to significant clinical variability. Further studies then to assess mechanistic determinants of TIL 4-1BB expression are needed. Such investigations may yield needed approaches to increase TIL 4-1BB expression and advance them as viable strategies for reducing resistance to PD-1 blockade in a variety of tumors.
Supplementary Material
Statement of Translational Relevance: Immune checkpoint blockade has shown limited success in glioblastoma and the intracranial compartment. Our study demonstrates that while poor T-cell activation and severe T-cell exhaustion appear to be limiting factors for checkpoint blockade in GBM, 4-1BB agonism obviates these limitations and produces long-term survival when combined with anti-PD-1 therapy. Furthermore, this combination therapy is limited by TIL 4-1BB expression, but not by the intracranial compartment, and therefore may be particularly well-suited to GBM. Our findings suggest that 4-1BB agonism may play a tailored, complementary role in overcoming resistance to immune checkpoint blockade by improving baseline T cell activation and averting exhaustion.
Acknowledgments
Funding: The work was supported in part by the National Institutes of Health Duke Brain SPORE Developmental Research Program (P.E. Fecci) and the Medical Scientist Training Program at Duke University School of Medicine (K. Woroniecka).
Abbreviations:
- GBM
(glioblastoma)
- TIL
(tumor-infiltrating lymphocytes)
Footnotes
Competing interests: none to disclose.
References
- 1.Filley AC, Henriquez M, Dey M. Recurrent glioma clinical trial, CheckMate-143: the game is not over yet. Oncotarget 2017;8(53):91779–94 doi 10.18632/oncotarget.21586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tawbi HA, Forsyth PA, Algazi A, Hamid O, Hodi FS, Moschos SJ, et al. Combined Nivolumab and Ipilimumab in Melanoma Metastatic to the Brain. The New England journal of medicine 2018;379(8):722–30 doi 10.1056/NEJMoa1805453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hodges TR, Ott M, Xiu J, Gatalica Z, Swensen J, Zhou S, et al. Mutational burden, immune checkpoint expression, and mismatch repair in glioma: implications for immune checkpoint immunotherapy. Neuro-oncology 2017;19(8):1047–57 doi 10.1093/neuonc/nox026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel AP, Tirosh I, Trombetta JJ, Shalek AK, Gillespie SM, Wakimoto H, et al. Single-cell RNA-seq highlights intratumoral heterogeneity in primary glioblastoma. Science 2014;344(6190):1396–401 doi 10.1126/science.1254257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kmiecik J, Poli A, Brons NH, Waha A, Eide GE, Enger PO, et al. Elevated CD3+ and CD8+ tumor-infiltrating immune cells correlate with prolonged survival in glioblastoma patients despite integrated immunosuppressive mechanisms in the tumor microenvironment and at the systemic level. Journal of neuroimmunology 2013;264(1–2):71–83 doi 10.1016/j.jneuroim.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 6.Brooks WH, Caldwell HD, Mortara RH. Immune responses in patients with gliomas. Surgical neurology 1974;2(6):419–23. [PubMed] [Google Scholar]
- 7.Brooks WH, Roszman TL, Rogers AS. Impairment of rosette-forming T lymphocytes in patients with primary intracranial tumors. Cancer 1976;37(4):1869–73. [DOI] [PubMed] [Google Scholar]
- 8.Fecci PE, Mitchell DA, Whitesides JF, Xie W, Friedman AH, Archer GE, et al. Increased regulatory T-cell fraction amidst a diminished CD4 compartment explains cellular immune defects in patients with malignant glioma. Cancer research 2006;66(6):3294–302 doi 10.1158/0008-5472.CAN-05-3773. [DOI] [PubMed] [Google Scholar]
- 9.Dunn GP, Fecci PE, Curry WT. Cancer immunoediting in malignant glioma. Neurosurgery 2012;71(2):201–22; discussion 22–3 doi 10.1227/NEU.0b013e31824f840d. [DOI] [PubMed] [Google Scholar]
- 10.Woroniecka K, Chongsathidkiet P, Rhodin K, Kemeny H, Dechant C, Farber SH, et al. T-Cell Exhaustion Signatures Vary with Tumor Type and Are Severe in Glioblastoma. Clinical cancer research : an official journal of the American Association for Cancer Research 2018;24(17):4175–86 doi 10.1158/1078-0432.CCR-17-1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Woroniecka KI, Rhodin KE, Chongsathidkiet P, Keith KA, Fecci PE. T-cell Dysfunction in Glioblastoma: Applying a New Framework. Clinical cancer research : an official journal of the American Association for Cancer Research 2018;24(16):3792–802 doi 10.1158/1078-0432.CCR-18-0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chongsathidkiet P, Jackson C, Koyama S, Loebel F, Cui X, Farber SH, et al. Sequestration of T cells in bone marrow in the setting of glioblastoma and other intracranial tumors. Nature medicine 2018;24(9):1459–68 doi 10.1038/s41591-018-0135-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koyama S, Akbay EA, Li YY, Herter-Sprie GS, Buczkowski KA, Richards WG, et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nature communications 2016;7:10501 doi 10.1038/ncomms10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HH, Kwack K, Lee ZH. Activation of c-jun N-terminal kinase by 4-1BB (CD137), a T cell co-stimulatory molecule. Mol Cells 2000;10(3):247–52. [PubMed] [Google Scholar]
- 15.Lee DY, Choi BK, Lee DG, Kim YH, Kim CH, Lee SJ, et al. 4-1BB signaling activates the t cell factor 1 effector/beta-catenin pathway with delayed kinetics via ERK signaling and delayed PI3K/AKT activation to promote the proliferation of CD8+ T Cells. PloS one 2013;8(7):e69677 doi 10.1371/journal.pone.0069677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.So T, Croft M. Regulation of PI-3-Kinase and Akt Signaling in T Lymphocytes and Other Cells by TNFR Family Molecules. Frontiers in immunology 2013;4:139 doi 10.3389/fimmu.2013.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim JO, Kim HW, Baek KM, Kang CY. NF-kappaB and AP-1 regulate activation-dependent CD137 (4-1BB) expression in T cells. FEBS letters 2003;541(1–3):163–70. [DOI] [PubMed] [Google Scholar]
- 18.Hernandez-Chacon JA, Li Y, Wu RC, Bernatchez C, Wang Y, Weber JS, et al. Costimulation through the CD137/4-1BB pathway protects human melanoma tumor-infiltrating lymphocytes from activation-induced cell death and enhances antitumor effector function. J Immunother 2011;34(3):236–50 doi 10.1097/CJI.0b013e318209e7ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wiethe C, Dittmar K, Doan T, Lindenmaier W, Tindle R. Provision of 4-1BB ligand enhances effector and memory CTL responses generated by immunization with dendritic cells expressing a human tumor-associated antigen. Journal of immunology 2003;170(6):2912–22. [DOI] [PubMed] [Google Scholar]
- 20.Chester C, Sanmamed MF, Wang J, Melero I. Immunotherapy targeting 4-1BB: mechanistic rationale, clinical results, and future strategies. Blood 2018;131(1):49–57 doi 10.1182/blood-2017-06-741041. [DOI] [PubMed] [Google Scholar]
- 21.Schrand B, Berezhnoy A, Brenneman R, Williams A, Levay A, Kong LY, et al. Targeting 4-1BB costimulation to the tumor stroma with bispecific aptamer conjugates enhances the therapeutic index of tumor immunotherapy. Cancer immunology research 2014;2(9):867–77 doi 10.1158/2326-6066.CIR-14-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schrand B, Berezhnoy A, Brenneman R, Williams A, Levay A, Gilboa E. Reducing toxicity of 4-1BB costimulation: targeting 4-1BB ligands to the tumor stroma with bi-specific aptamer conjugates. Oncoimmunology 2015;4(3):e970918 doi 10.4161/21624011.2014.970918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Compte M, Harwood SL, Munoz IG, Navarro R, Zonca M, Perez-Chacon G, et al. A tumor-targeted trimeric 4-1BB-agonistic antibody induces potent anti-tumor immunity without systemic toxicity. Nature communications 2018;9(1):4809 doi 10.1038/s41467-018-07195-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bartkowiak T, Jaiswal AR, Ager CR, Chin R, Chen CH, Budhani P, et al. Activation of 4-1BB on Liver Myeloid Cells Triggers Hepatitis via an Interleukin-27-Dependent Pathway. Clinical cancer research : an official journal of the American Association for Cancer Research 2018;24(5):1138–51 doi 10.1158/1078-0432.CCR-17-1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woroniecka K, Chongsathidkiet P, Elsamadicy A, Farber H, Cui X, Fecci PE. Flow Cytometric Identification of Tumor-Infiltrating Lymphocytes from Glioblastoma. Methods Mol Biol 2018;1741:221–6 doi 10.1007/978-1-4939-7659-1_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Belcaid Z, Phallen JA, Zeng J, See AP, Mathios D, Gottschalk C, et al. Focal radiation therapy combined with 4-1BB activation and CTLA-4 blockade yields long-term survival and a protective antigen-specific memory response in a murine glioma model. PloS one 2014;9(7):e101764 doi 10.1371/journal.pone.0101764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kerkar SP, Sanchez-Perez L, Yang S, Borman ZA, Muranski P, Ji Y, et al. Genetic engineering of murine CD8+ and CD4+ T cells for preclinical adoptive immunotherapy studies. J Immunother 2011;34(4):343–52 doi 10.1097/CJI.0b013e3182187600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fukunaga A, Yamasaki T, Okuno T, Imai K, Ikeuchi R, Hishiki K, et al. [Initial Clinical Experience of Nivolumab for Metastatic Renal Cell Carcinoma]. Hinyokika Kiyo 2018;64(10):383–9 doi 10.14989/ActaUrolJap_64_10_383. [DOI] [PubMed] [Google Scholar]
- 29.Kim JE, Patel MA, Mangraviti A, Kim ES, Theodros D, Velarde E, et al. Combination therapy with anti-PD-1, anti-TIM-3, and focal radiation results in regression of murine gliomas. Clinical cancer research : an official journal of the American Association for Cancer Research 2016. doi 10.1158/1078-0432.CCR-15-1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zeng J, See AP, Phallen J, Jackson CM, Belcaid Z, Ruzevick J, et al. Anti-PD-1 blockade and stereotactic radiation produce long-term survival in mice with intracranial gliomas. Int J Radiat Oncol Biol Phys 2013;86(2):343–9 doi 10.1016/j.ijrobp.2012.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kamphorst AO, Wieland A, Nasti T, Yang S, Zhang R, Barber DL, et al. Rescue of exhausted CD8 T cells by PD-1-targeted therapies is CD28-dependent. Science 2017;355(6332):1423–7 doi 10.1126/science.aaf0683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hui E, Cheung J, Zhu J, Su X, Taylor MJ, Wallweber HA, et al. T cell costimulatory receptor CD28 is a primary target for PD-1-mediated inhibition. Science 2017;355(6332):1428–33 doi 10.1126/science.aaf1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clouthier DL, Ohashi PS. Costimulation, a surprising connection for immunotherapy. Science 2017;355(6332):1373–4 doi 10.1126/science.aan1467. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.