Abstract
Objective:
Ischemia and reperfusion injury (IRI) in cardiac arrest patients after return to spontaneous circulation causes dysfunctions in multiple organs. Kidney injury is generally transient but in some patients persists and contributes both to mortality and increased resource utilisation. Ongoing shock may compound renal injury from IRI, resulting in persistent dysfunction. We tested whether cardiac dysfunction was associated with the development of persistent acute kidney injury (PAKI) in the first 72 hours after cardiac arrest.
Methods:
We performed an observational retrospective study from January 2013 to April 2017. We included consecutive patients treated after out-of-hospital cardiac arrest at a single academic medical center with renal function measured and immediately and for 48 hours post arrest. We also recorded each patient’s pre arrest baseline creatinine, demographic and clinical characteristics. Our primary outcome of interest was PAKI, defined as acute kidney injury (AKI) on at least 2 measurements 24 hours apart. We compared demographics and outcomes between patients with PAKI and those without, and used logistic regression to identify independent predictors of PAKI.
Results:
Of 98 consecutive patients, we excluded 24 for missing data. AKI was present in 75% of subjects on arrival. PAKI developed in 35% of patients. PAKI patients had a longer hospital length of stay (median 21 vs 11 days) and lower hospital survival (47% vs 71%). Serum lactate levels, dosage of adrenaline during resuscitation and days of dobutamine infusion strongly predicted PAKI.
Conclusions:
Among patient who survive cardiac arrest, acute AKI is common and PAKI occurs in more than one third. PAKI is associated both with survival and with length of stay at the hospital. High doses of adrenaline, high serial serum lactate levels, and dose of dobutamine predict PAKI. Evaluation of the trajectory of renal function over the first few days after resuscitation can provide prognostic information about patient recovery.
Keywords: cardiac arrest, acute kidney injury, cardiogenic shock, ischemia and reperfusion injury, post resuscitation disease, outcomes
Introduction
Whole body ischemia and reperfusion injury causes high mortality and morbidity in survivors of cardiac arrest. In particular, brain injury represents the major cause of death and disability.[6] However, cardiac arrest also causes acute kidney injury (AKI), which can contribute to both mortality and increased resource utilization. [7][8, 9] In a recent meta analysis more than 50% of patients developed AKI stage-1 within 2 days after cardiac arrest.[5, 10]Similar to animal models, AKI in post cardiac arrest patients is mediated by inflammation and T cell-mediated injury.[11] Although AKI is transient in most patients, some develop persistent AKI.
The development of AKI is influenced both by preexisting renal disease and post- resuscitation hypoperfusion.[12][8] Renal dysfunction is associated with outcome after resuscitation. However, prior studies have not clearly defined the role of AKI after cardiac arrest, because of lack of baseline measures or renal function and clear definitions for AKI.
In order to understand the relative contributions of these factors to post-cardiac arrest AKI, we sought to evaluate the predictors of persistent AKI in resuscitated cardiac arrest patients treated with therapeutic normothermia for 24 hours after return to spontaneous circulation. In this cohort, we prospectively collected echocardiographic data on heart function, along with serial measurements of renal function and acidosis. We tested the specific hypothesis that cardiac dysfunction after cardiac arrest was associated with development of persistent AKI (PAKI) in the first 72 hours after cardiac arrest.
Methods
Study design and population
We studied consecutive unconscious (GCS<9) adult patients resuscitated after out of hospital cardiac arrest and admitted to the intensive care unit (ICU) of a single center from January 2013 to April 2017. Our university institutional review board approved this study and waived the need for informed consent because the study was minimal risk. We excluded patients for age less than 18 years, pregnancy, or pre-existing end-stage renal disease according to KDOQI guidelines.[1] In order to determine AKI, we also excluded patients with death within 72 hours (could not measure PAKI) or uncertain baseline of serum creatinine (SCr) data within 120 days of cardiac arrest (could not quantify AKI).
2.2. Study definitions and data collection
We defined cardiac arrest as the abrupt loss heart function with no pulse. We categorized initial EKG rhythm as ventricular fibrillation (VF), ventricular tachycardia pulseless (VT), pulseless electrical activity (PEA) or asystole. Time to achieve return to spontaneous circulation was defined as the total time from witnessed collapse until return of pulses. We determined the baseline serum creatinine from pre-arrest medical records, and used the most recent measures within 120 days before CA. We collected SCr values, lactate levels and serum bicarbonate (HCO3-) at the admission to the emergency department and at 6, 12, 24, 48 and 72 hours after admission. We calculated glomerular filtration rate using the modification of diet in renal disease (MDRD) study equation.
To estimate ventricular dysfunction, we recorded the total duration of utilization of vasoactive drugs during the ICU stay, and we performed a transthoracic echocardiogram 3 to 6 hours after CA. The wall motion score index (WMSI) is a semi-quantitative analysis of regional cardiac systolic function. Raters assign a score (1–5) for systolic wall cardiac motion to each single segment of the ventricle. Global WMSI is defined as the sum of all segmental scores divided by the number of segments rated (simple mean).
WMSI score:
score 1= normo-kinetic or hyperkinetic
score 2= hypo-kinetic
score 3= akinetic
score 4= dyskinetic
score 5= aneurysm
We defined AKI according to the Kidney Disease Improving Global Outcomes (KDIGO) guidelines as the increase in SCr by ≥0.3 mg/dl (26.5 μmol/l) from baseline within 48 hours or the increase in SCr to ≥1.5 times baseline, or urine output less than 0.5 ml/kg/h for 6 h. Staging of AKI is in table A. [13]
Table A.
Staging of AKI, KDIGO guidelines.
| Stage | SCr | Urine output |
|---|---|---|
| 1 | ≥ 0.3 mg/dl (26.5 μmol/l) or 1.5–1.9 times baseline | < 0.5 ml/kg/h for 6–12 hours |
| 2 | 2–2.9 times baseline | < 0.5 ml/kg/h 6–12 for ≥ 12hours |
| 3 | 3 times baseline or increase SCr ≥ 4 mg/dl (≥353.6 μmol/l) or initial RRT or in patients < 18 years, duress of GFR < 35 ml/min per 1.73 m2 | 1.03–1.06 |
We determined the presence of AKI at each measurement time relative to the SCr baseline value: ED arrival, 6, 12, 24, 48 and 72 hours after ROSC. Persistent AKI is characterized by renal dysfunction without recovery within 3 days. We considered as PAKI the presence of at least 2 sCr values that satisfy the KDIGO guidelines for AKI during the observation period.[2][3] Peak creatinine value was identified as the highest value during the observation period. Baseline chronic renal dysfunction was defined as baseline SCr>1.1 mg/dl.
Study data analysis
We compared patients with the presence of persistent AKI (PAKI) or not (NPAKI) during the first 72 hours after return to spontaneous circulation using descriptive statistics. We made univariate comparisons between PAKI and NPAKI groups using Chi-square test or Fisher exact test for categorical variables and Wilcoxon rank-sum test for continuous variables. We used a Generalised Linear Model for the binary family with a logit linkage to test the independent association of WMSI, duration of vasoactive support, and repeatedly measured lactate levels with PAKI, when adjusted for other variables. We censored repeated measures data occuring after development of PAKI so it was not included in our models. We tested for collinearity between variables before modelling, and did not include strongly collinear variables in the same model. We only included variables in our adjusted model if they had a strong univariate association with PAKI (p<0.05 on univariable tests). (Table 3) We performed all statistical analysis using STATA version 15 (StataCorp, 4905 Lakeway Drive College Station, Texas 77845 USA).
Tab 3.
Multivariate analysis on risk factors to development of persistent AKI
| Multivariate linear regression model | Odds | Conf. interval | p- Value |
|---|---|---|---|
| Adrenaline | 7.19 | 4.00–13 | <0.001 |
| Dobutamine | 1.04 | 1.03–1.06 | <0.001 |
| Serum lactate | 1.06 | 1.03–1.08 | <0.001 |
Results
Patient profile
We studied 98 consecutive comatose patients (GCS<9) patients successfully resuscitated after out of hospital cardiac arrest and threatened with therapeutic normothermia (TN) from January 2013 to April 2017. Only 74 patients were included in the analysis, because 24 had no SCr in their records within 120 days of arrest or did not survive for 72 hours. (Fig. 1)
Fig 1.
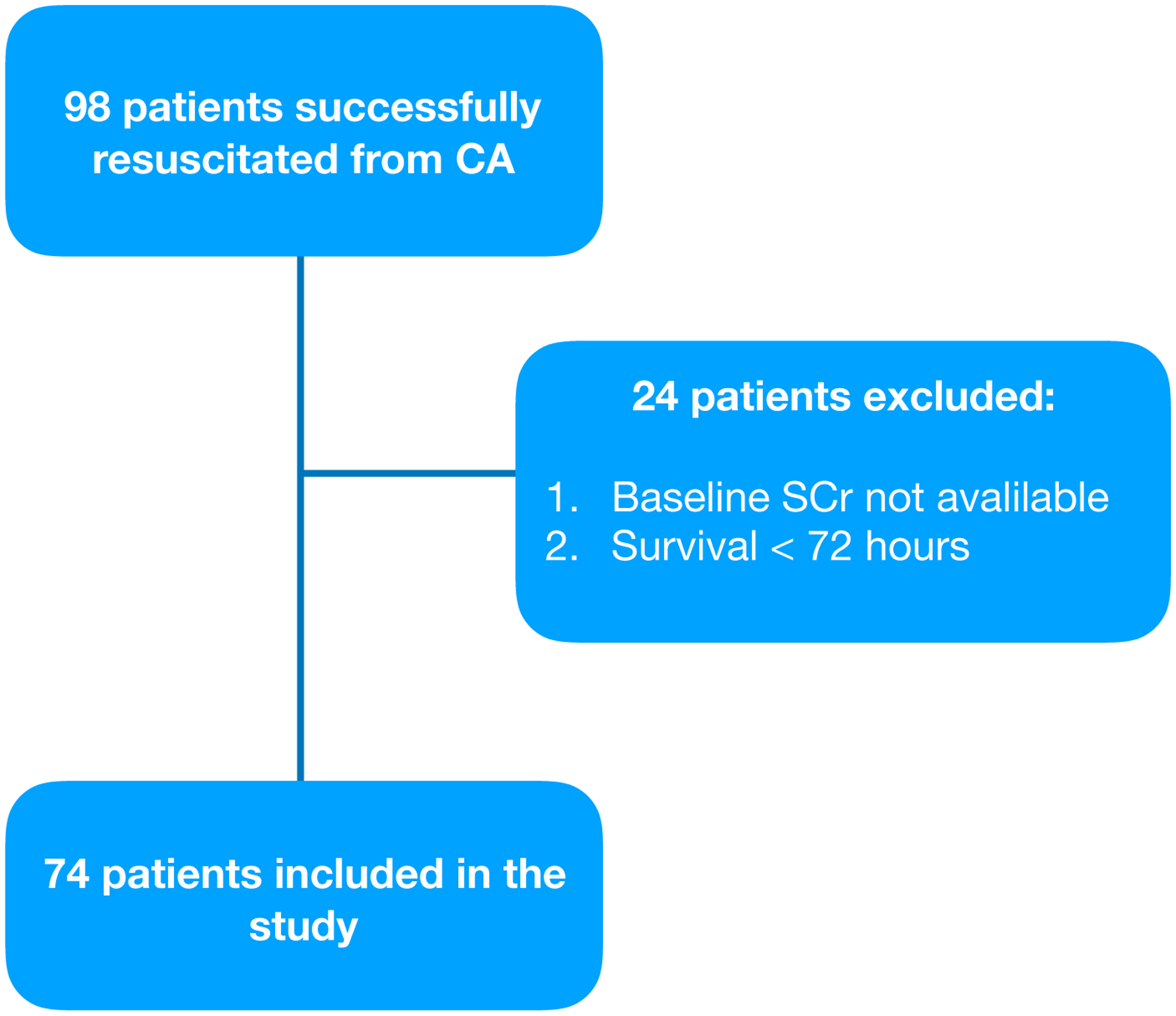
Flowchart of the study. CA, cardiac arrest, SCr serum creatinine.
Baseline demographic data are summarized in Table 1. Most subjects were male, median age was greater than 63 years old, and the most frequent cause of cardiac arrest was ventricular fibrillation (VF) (72%) due to a myocardial infarction (MI) (69%). PAKI developed in 26 (35%) subjects during the observation period. No subjects required RRT by 72 hours after cardiac arrest. None of the patients excluded for death prior to 72 hours required RRT. Subjects with PAKI compared to subjects without PAKI had a longer hospital length of stay (median 21 days vs 11; p<0.05) and lower hospital survival (47% vs 71%; p<0.05).
Tab 1.
Descriptive statistics, demographic and co-morbidities
| Tot | PAKI | NPAKI | p-Value | |
|---|---|---|---|---|
| number (%) | 74 (100) | 26 (35.1) | 48 (64.9) | |
| age median (IQR), y | 63.5 (54–71) | 65 (59–72) | 61 (50–70) | 0.09 |
| male gender, n (%) | 56 (77) | 19 (73) | 37 (77) | 0.71 |
| Presenting cardiac rhythms, n (%) | ||||
| FV/TV | 53 (71.6) | 17 (65.4) | 36 (75) | 0.38 |
| Pea/Asystole | 21 (28.4) | 9 (34.6) | 12 (25) | 0.38 |
| Resuscitation details | ||||
| median (IQR) | ||||
| Adrenaline (mg) | 0 (0–1) | 1 (0–2) | 0 (0–1) | 0.001 |
| Time to ROSC (mins) | 18 (13–24) | 21.5 (16–29) | 15.5 (11–20.5) | 0.004 |
| Baseline co-morbidities, n (%) | ||||
| Chronic renal failure | 2 (2.7) | 2 (7.2) | 0 (0) | 0.05 |
| Hypertension | 40 (54) | 17 (65) | 23 (48) | 0.15 |
| Coronary disease | 17 (23) | 8 (31) | 9 (19) | 0.24 |
| Liver disease | 5 (7) | 3 (11) | 2 (4) | 0.22 |
| Chronic hearth failure | 7 (9) | 4 (15) | 3 (6) | 0.2 |
| Diabetes | 6 (8) | 2 (8) | 4 (8) | 0.9 |
Subjects with PAKI received more adrenaline (p<0.001) and had longer duration of arrest prior to return of pulses (p<0.004) compared to those without PAKI.
Serum bicarbonate (p=0.028) and base excess (p=0.022) measured in the ED were lower in the PAKI group. Among the subjects with PAKI, only two (7%) suffered chronic renal dysfunction prior to arrest.
We calculated the illness severity indices with APACHE II score at the beginning of ICU admission. PAKI group had higher values than NPAKI (median 22 vs 29). Illness severity indices, renal function, acid base balance and hemodynamics are shown in Table 2. Value of SCr measured over time after ROSC was significantly greater in the PAKI group (p=0.0001). Serum lactate levels were strongly associated with PAKI, with significant differences between PAKI and NPAKI subjects at earlier time points and declining over time. Subjects with PAKI had longer durations of treatment with dobutamine for post arrest myocardial dysfunction (PAMD).[14] Total WMSI did not differ between groups.
Tab 2.
Illness severity indices and renal function
| Tot | PAKI | NPAKI | p-Value | |
|---|---|---|---|---|
| number (%) | 74 (100) | 26 (35.1) | 48 (64.9) | |
| Apache II, median (IQR) | 25 (22–27) | 28 (25–31) | 22 (19–23) | |
| Acid base balance | ||||
| HCO3- | 20.8 (18.8–22) | 19 (18–20.8) | 19.5 (21.2–22) | 0.028 |
| BE | −5.2 (−8– −3) | −7.9 (−10.4 – −4.3) | −4.4 (−7– −3) | 0.022 |
| Hemodinamic h, mean | ||||
| Noradrenaline | 18.8 | 24.9 | 15.5 | 0.08 |
| Dobutamine | 9.4 | 20.4 | 3.5 | 0.003 |
| WMSI median (IQR) | 1.3(1.13–1.57) | 1.2 (1.13–1.52) | 1.4 (1.19–1.97) | 0.46 |
| Renal function | ||||
| Delta sCr, median (IQR) | ||||
| Delta sCr 6 | 0.18 (0.05–0.3 | 0.43 (0.26–0.51) | 0.95 (−0.005– −0.2) | <0.0001 |
| Delta sCr 12 | 0.9 (−0.05–0.23) | 0.31 (0.14–0.51) | 0.005 (−0.75– 0.16) | <0.0001 |
| Delta sCr 24 | 0 (−13–0.18) | 0.2 (0.05–0.44) | −0.8 (−0.17– 0.01) | <0.0001 |
| Delta sCr 48 | 0.02 (−0.08–0.18) | 0.24 (0.05–0.43) | 0 (−0.16–0.04) | <0.0001 |
| Delta sCr 72 | 0.02 (−0.06–0.16) | 0.14 (0.02–0.45) | 0 (−0.08–0.07) | <0.001 |
| peak sCr, d (%) | 1 (75) | 5–6 (67) | 1 (75) | 0.01 |
| Survival, n (%) | 46 (62) | 12 (46) | 34 (71) | 0.037 |
| Day of stay, median (IQR) | 12.5 (7–21) | 20.5 (6–67) | 11 (8–17) | <0.05 |
Predictors of Persistent AKI
In multivariate analysis high serum lactate, days of usage of dobutamine, cumulative dosage of adrenaline during CPR, days of stay in hospital and survival were independently associated with persistent AKI. (Table 3).
Discussion
Impairment of renal function is reversible after cardiac arrest in most patients, but persisting AKI is associated with a poor outcome.[15] In this study, we confirmed that the incidence of AKI is variable and often resolves within two days after admission [5], and that persistent AKI was related to survival and days of stay in the hospital. None of our patients received renal replacement therapy during the first 72 hours, because they did not reach the life threatening KDIGO criteria for dialysis during this time. We determined that clinicians can recognize patients at risk for persistent AKI by higher early serum lactate values, the cumulative dose of adrenaline used during resuscitation, and the dosage of dobutamine required to maintain cardiac contractility.
Presence of AKI can be divided into two distinct time periods: an initial increase of sCr at admission, and a later rise over 24–48 hours in the subset of patients with PAKI. As reported in other studies before, the time to achieve Return to spontaneous circulation is greater in PAKI group and and the persistence AKI might be the reflection of prolonged cardiac arrest. [16] In our study, AKI at admission to the ED is present in 75% of patients. Other studies reported the immediate rise of serum creatinine after cardiac arrest, but the mechanism is unknown.[17] The muscular creatinine release during CPR and the lack of creatinine clearance during the no- flow and low-flow period are potential mechanisms.[18]
The peak of SCr level in PAKI group was 48 to 72 h after cardiac arrest. Direct ischemic damage to the kidney during cardiac arrest could result in impaired filtration and accumulation of creatinine over this time period. In our study we found that patients who developed PAKI received greater cumulative epinephrine doses. Even though not much is known about the effects of epinephrine on regional renal blood flow [19] vasoconstriction could lead to intrarenal haemodynamic changes.[20] Neumayr et al. recently considered in a large study how cumulative dose of epinephrine exposure lead to develop an acute kidney injury in children after cardiac arrest. [21]
We did not find a direct relationship between cardiac impairment, which can be rapidly estimated with WMSI [22] [23]and PAKI. We confirmed previous studies reporting that haemodynamic instability is frequent after cardiac arrest.[24][25] However, the WMSI data did not confirm that the presence of cardiogenic shock is independently associated with increase of serum creatinine after cardiac arrest [12]. We measured WMSI only in the initial 6 hours from return to spontaneous circulation, and it is possible that later decreases in cardiac contractility contributed to PAKI.
Indirect indices of cardiac output include early lactate clearance and lower requirements for dobutamine. These measures of tissue perfusion are related to better survival [26] and functional recovery. [27] Thus, our finding that lactate and dobutamine dose are related to PAKI indirectly suggest that adequacy of tissue perfusion is a factor in renal injury.[28]
We acknowledge several limitation of the study. This is a single center retrospective observational study in a tertiary care center, which may limit generalizability. Data about the cardiac arrest and acute kidney injury were collected from clinical and electronic laboratory findings which have variable reliability.
Some patients in this series had diagnostic coronary angiography. Kidney function may have been influenced by the infusion of contrast material. However, a recent meta analysis suggests that contrast induced AKI is a related to severity of illness and hemodynamic instability rather than to the contrast itself.[4]
WMSI is a valid tool for evaluation of early cardiac dysfunction in patients post MI [29] but may not be valid in cardiac arrest patients. Serial echocardiograms and WMSI scores beyond the first 6 hours after cardiac arrest also might reveal relationships with outcomes.
Our patients were all treated with therapeutic normothermia at 36 °C for 24 hours and then gradually re-warmed until reaching 37 °C for 48 h more. Other temperature management strategies might produce different results. However, in a recent meta analysis, target cooling temperature was not associated with the odds of AKI. [30]
Conclusions
Among patient who survive cardiac arrest, acute AKI is common (>75%) and persistent AKI occurs in more than one third of patients. Persistent AKI is associated both with survival and with length of stay at the hospital. High doses of adrenaline, high serial serum lactate levels, and dose of dobutamine predict persistent AKI. Evaluation of the trajectory of renal function over the first few days after resuscitation can provide prognostic information about patient recovery.
Figure 2.


Trends of median serum Creatinine and Serum Lactates in PAKI and nPAKI group during the first 72 h after ROSC.
Table 5.
Legend in the order of their appearance.
| CA | Cardiac Arrest |
| ROSC | Return to Spontaneous Circulation |
| AKI | Acute Kidney Injury |
| PAKI | Persistent Acute Kidney Injury |
| OHCA | Out of Hospital Cardiac Arrest |
| GCS | Pittsburgh-Glasgow Coma Scale |
| EKG | Cardiogram |
| VF | Ventricular Fibrillation |
| MI | Myocardial infarction |
| VT | Ventricular Tachicardia |
| PEA | Pulsless Electrical Activity |
| RRT | Renal Replacement Therapy |
| MDRD | Modification of Diet in Renal Disease |
| WMSI | Wall Motion Score Index |
| PAMD | Post arrest Myocardial Disfunction |
| CPR | Cardiopulmonary Resuscitation |
| KDIGO | Kidney Disease Improving Global Outcomes |
| APACHE | Acute Physiology And Chronic Health Evaluation |
| ED | Emergency Department |
| SCr | Serum Creatinine |
| TN | Normothermia treatment |
| ICU | Intensive Care Unit |
Footnotes
No conflict of interest declared by authors
Bibliography
- [1].Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Perinel S, Vincent F, Lautrette A, Dellamonica J, Mariat C, Zeni F, et al. Transient and Persistent Acute Kidney Injury and the Risk of Hospital Mortality in Critically Ill Patients: Results of a Multicenter Cohort Study. Crit Care Med 2015;43:e269–75. [DOI] [PubMed] [Google Scholar]
- [3].Kellum JA. Persistent Acute Kidney Injury. Crit Care Med 2015;43:1785–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].James MT, Samuel SM, Manning MA, Tonelli M, Ghali WA, Faris P, et al. Contrast- induced acute kidney injury and risk of adverse clinical outcomes after coronary angiography: a systematic review and meta-analysis. Circ Cardiovasc Interv 2013;6:37–43. [DOI] [PubMed] [Google Scholar]
- [5].Sandroni C, Dell’anna AM, Tujjar O, Geri G, Cariou A, Taccone FS. Acute kidney injury after cardiac arrest: a systematic review and meta-analysis of clinical studies. Minerva Anestesiol 2016;82:989–99. [PubMed] [Google Scholar]
- [6].Sandroni C, Cariou A, Cavallaro F, Cronberg T, Friberg H, Hoedemaekers C, et al. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Resuscitation 2014;85:1779–89. [DOI] [PubMed] [Google Scholar]
- [7].Yanta J, Guyette FX, Doshi AA, Callaway CW, Rittenberger JC. Renal dysfunction is common following resuscitation from out-of-hospital cardiac arrest. Resuscitation 2013;84:1371–4. [DOI] [PubMed] [Google Scholar]
- [8].Domanovits H, Schillinger M, Müllner M, Thoennissen J, Sterz F, Zeiner A, et al. Acute renal failure after successful cardiopulmonary resuscitation. Intensive Care Med 2001;27:1194–9. [DOI] [PubMed] [Google Scholar]
- [9].Mattana J, Singhal PC. Prevalence and determinants of acute renal failure following cardiopulmonary resuscitation. Arch Intern Med 1993;153:235–9. [PubMed] [Google Scholar]
- [10].Tujjar O, Mineo G, Dell’Anna A, Poyatos-Robles B, Donadello K, Scolletta S, et al. Acute kidney injury after cardiac arrest. Crit Care 2015;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Burne-Taney MJ, Kofler J, Yokota N, Weisfeldt M, Traystman RJ, Rabb H. Acute renal failure after whole body ischemia is characterized by inflammation and T cell-mediated injury. American Journal of Physiology-Renal Physiology 2003;285:F87–94. [DOI] [PubMed] [Google Scholar]
- [12].Chua H-R, Glassford N, Bellomo R. Acute kidney injury after cardiac arrest. Resuscitation 2012;83:721–7. [DOI] [PubMed] [Google Scholar]
- [13].Khwaja A KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron 2012;120:c179–84. [DOI] [PubMed] [Google Scholar]
- [14].Jentzer JC, Chonde MD, Dezfulian C. Myocardial Dysfunction and Shock after Cardiac Arrest. Biomed Res Int 2015;2015:314796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Geri G, Guillemet L, Dumas F, Charpentier J, Antona M, Lemiale V, et al. Acute kidney injury after out-of-hospital cardiac arrest: risk factors and prognosis in a large cohort. Intensive Care Med 2015;41:1273–80. [DOI] [PubMed] [Google Scholar]
- [16].De Rosa S, Antonelli M, Ronco C. Hypothermia and kidney: a focus on ischaemia- reperfusion injury. Nephrol Dial Transplant 2017;32:241–7. [DOI] [PubMed] [Google Scholar]
- [17].Domanovits H, Müllner M, Sterz F, Schillinger M, Klösch C, Paulis M, et al. Impairment of renal function in patients resuscitated from cardiac arrest: frequency, determinants and impact on outcome. Wien Klin Wochenschr 2000;112:157–61. [PubMed] [Google Scholar]
- [18].Hasper D, Haehling S von, Storm C, Jörres A, Schefold JC. Changes in serum creatinine in the first 24 hours after cardiac arrest indicate prognosis: an observational cohort study. Crit Care 2009;13:R168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Bersten AD, Rutten AJ, Summersides G, Ilsley AH. Epinephrine infusion in sheep: systemic and renal hemodynamic effects. Crit Care Med 1994;22:994–1001. [DOI] [PubMed] [Google Scholar]
- [20].Mauk RH, Patak RV, Fadem SZ, Lifscitz MD, Stein JH. Effect of prostaglandin E administration in a nephrotoxic and a vasoconstrictor model of acute renal failure. Kidney Int 1977;12:122–30. [DOI] [PubMed] [Google Scholar]
- [21].Neumayr TM, Gill J, Fitzgerald JC, Gazit AZ, Pineda JA, Berg RA, et al. Identifying Risk for Acute Kidney Injury in Infants and Children Following Cardiac Arrest. Pediatr Crit Care Med 2017;18:e446–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Palmieri V, Russo C, Buonomo A, Palmieri EA, Celentano A. Novel wall motion score- based method for estimating global left ventricular ejection fraction: validation by real-time 3D echocardiography and global longitudinal strain. Eur J Echocardiogr 2010;11:125–30. [DOI] [PubMed] [Google Scholar]
- [23].Eek C, Grenne B, Brunvand H, Aakhus S, Endresen K, Hol PK, et al. Strain echocardiography and wall motion score index predicts final infarct size in patients with non-ST-segment-elevation myocardial infarction. Circ Cardiovasc Imaging 2010;3:187–94. [DOI] [PubMed] [Google Scholar]
- [24].Kilgannon JH, Roberts BW, Reihl LR, Chansky ME, Jones AE, Dellinger RP, et al. Early arterial hypotension is common in the post-cardiac arrest syndrome and associated with increased in-hospital mortality. Resuscitation 2008;79:410–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Trzeciak S, Jones AE, Kilgannon JH, Milcarek B, Hunter K, Shapiro NI, et al. Significance of arterial hypotension after resuscitation from cardiac arrest. Crit Care Med 2009;37:2895–903; quiz 2904. [DOI] [PubMed] [Google Scholar]
- [26].Donnino MW, Miller J, Goyal N, Loomba M, Sankey SS, Dolcourt B, et al. Effective lactate clearance is associated with improved outcome in post-cardiac arrest patients. Resuscitation 2007;75:229–34. [DOI] [PubMed] [Google Scholar]
- [27].Lee DH, Cho IS, Lee SH, Min YI, Min JH, Kim SH, et al. Correlation between initial serum levels of lactate after return of spontaneous circulation and survival and neurological outcomes in patients who undergo therapeutic hypothermia after cardiac arrest. Resuscitation 2015;88:143–9. [DOI] [PubMed] [Google Scholar]
- [28].Kim YW, Cha KC, Cha YS, Kim OH, Jung WJ, Kim TH, et al. Shock duration after resuscitation is associated with occurrence of post-cardiac arrest acute kidney injury. J Korean Med Sci 2015;30:802–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Møller JE, Hillis GS, Oh JK, Reeder GS, Gersh BJ, Pellikka PA. Wall motion score index and ejection fraction for risk stratification after acute myocardial infarction. Am Heart J 2006;151:419–25. [DOI] [PubMed] [Google Scholar]
- [30].Susantitaphong P, Alfayez M, Cohen-Bucay A, Balk EM, Jaber BL. Therapeutic hypothermia and prevention of acute kidney injury: a meta-analysis of randomized controlled trials. Resuscitation 2012;83:159–67. [DOI] [PMC free article] [PubMed] [Google Scholar]


