Abstract
Objective:
To evaluate if completion of vital signs assessments in pediatric transports by emergency medical services (EMS) differs by age.
Methods:
We reviewed records by 20 agencies in a regional EMS system in Southwestern Pennsylvania between April 1, 2013 and December 31, 2016. We abstracted demographics, vital signs (systolic blood pressure, heart rate, respiratory rate), clinical and transport characteristics. We categorized age as neonates (≤30 days), infants (1 month to <1 year), toddler (1 to <2 years), early childhood (2 to <6 years), middle childhood (6 to <12 years), adolescent (12 to <18 years), and adult (≥18 years). We used unadjusted and adjusted logistic regression to test if age group was associated with vital signs documentation, reporting of Glasgow Coma Scale and pain scale after trauma, and recording of oxygen saturation and breath sounds in respiratory complaints, using adults as the reference group.
Results:
371,746 cases (21,883 pediatric, 5.9%) were included. In adjusted analysis, most pediatric categories had reduced odds of complete vitals documentation (percent, OR, 95%CI): neonates (49.6%, 0.02, 0.02–0.03), infants (68.2%, 0.04, 0.03–0.04), toddlers (78.1%, 0.07, 0.06–0.07), early childhood (87.4%, 0.13, 0.12–0.15), and middle childhood (95.3%, 0.54, 0.46–0.63). Pain score documentation was lower in children after trauma (OR 0.80, 95%CI 0.76–0.85) and oxygen saturation documentation was lower in children with respiratory complaints (OR 0.20, 95%CI 0.18–0.25).
Conclusion:
Pediatric patients were at increased risk of lacking vital signs documentation during prehospital care. This represents a critical area for education and quality improvement.
Introduction
Background.
Emergency Medical Services (EMS) systems are an integral component of medical care for acutely ill and injured patients. Children comprise up to 10% of all patients transported by EMS,1, 2 representing a small but substantial proportion of patients cared for by EMS personnel compared to adults. Pediatric patients that reach the emergency department by EMS are an at-risk population who are more likely to have higher acuity illness than other pediatric patients.3
Importance.
Prehospital care of children requires specific knowledge, equipment and interpersonal skills that are distinct from those used to manage adults. Primary and continuing education related to children is commonly less than that required for adult patients, potentially leading to a lack of comfort in patient assessment and management of children. In a study by Fleischman et al., a majority of EMS personnel identified themselves as less than “comfortable” in providing pediatric care.4 Brown et al. similarly identified suboptimal pediatric education and gaps in training of EMS personnel in pediatric care.5 Without the right knowledge, EMS personnel may have difficulty in effectively triaging and treating children. In a sample of children with traumatic brain injury, Zebrack et al. identified 31% did not have blood pressure recorded in the prehospital or emergency department setting, while children with untreated hypotension had a three-fold increased incidence of disability compared to treated hypotensive children.6
The effectiveness of efforts in education, clinical patient care, and future research begins with a robust understanding of patient assessments currently being completed. Previous investigators have noted discrepancies in rates of vital sign assessments in children as compared to adults.7, 8 Better identification of these assessments by age groups and after controlling for potential confounders can further inform aspects of education and practice guidelines that are needed for the management of pediatric patients.
Goals of this Investigation.
We aimed to evaluate the level of assessment currently being performed by EMS personnel for pediatric patients. We further aimed to compare patient assessments by age groups with those performed on adult patients in the out-of-hospital setting. We hypothesized that rates of prehospital vital signs and complaint-specific assessments differed in pediatric patients versus adults.
Methods
Study design and setting.
We performed a retrospective review of ground EMS transports from a scene to a hospital by 20 urban, suburban, and rural EMS agencies in Southwestern Pennsylvania between April 1, 2013 and December 31, 2016. These EMS agencies receive centralized medical oversight and have research data use agreements with the University of Pittsburgh Medical Center. This study was approved by the University of Pittsburgh Institutional Review Board with a waiver of informed consent.
Selection of participants.
Data were collected from a common electronic patient care record (emsCharts, Warrendale, PA), which has custom reporting software allowing the extraction of robust clinical patient data. We initially screened all patient reports from the participating EMS agencies over the study period. We excluded cases if there was documentation of cardiac arrest, no documentation of age, if the transport was between medical facilities, if the transport was a scene assist (an additional EMS crew called to the scene to provide additional assistance, but identified as not providing primary care of the patient), or if the patient was ultimately not transported. Cardiac arrest was defined as any of the following: 1) documented provider impression of cardiac arrest, death, traumatic arrest, or dead on arrival; 2) documented outcome listed as funeral home, pronounced, dead, or coroner transport; 3) documented rhythm of asystole, PEA, pulseless, agonal, or ventricular fibrillation; 4) documented procedure of defibrillation or CPR; or 5) documented use of epinephrine as dosed for cardiac arrest. Patients that were not transported from the scene were excluded, as patient assessments may differ substantially between patients that are or are not transported to the hospital, and patients or parents declining transport to the hospital after calling 911 may also decline complete assessments by EMS personnel.
Measurements.
From the study cohort, we abstracted patient demographics, transport characteristics, vital signs (systolic blood pressure, heart rate, and respiratory rate), Glasgow Coma Scale (GCS) score, pain scales, and lung sound assessment. Patient demographics included age, gender, race, ethnicity, weight, height, and medical complaint. Race was divided into categories of white, black, and other/unknown. Ethnicity was categorized as Hispanic, not Hispanic, or unknown. We considered patients to be pediatric if they were <18 years of age. Pediatric patients were further categorized as: neonates (≤30 days), infants (1 month to <1 year), toddlers (1 to <2 years), early childhood (2 to <6 years), middle childhood (6 to <12 years), and adolescent (12 to <18 years). Documented medical categories based on chief complaints were re-classified into 12 categories: general medical, trauma, respiratory, allergic, gastrointestinal, cardiovascular, neurologic, psychiatric, toxicological, dizziness/syncope, other, and unknown.
Transport characteristics included year and time of day of transport, response time (between dispatch and arrival to scene), time at scene (between arrival to scene and departure to hospital), transport time (between departure from scene to arrival at hospital), provider certification (basic versus advanced life support), and use of cardiac monitor.
We defined complete vital signs assessment as documentation of patient heart rate, respiratory rate, and systolic blood pressure at least once. Because pulse oximetry and temperature are not routinely collected in prehospital patients for all medical categories, these were not included as components of complete vital signs. For secondary assessment of patients with medical category of respiratory and traumatic complaints, we collected data regarding pulse oximetry, assessment of lung sounds, pain scores and Glasgow coma scale.
Analysis.
We used descriptive statistics to summarize data, and presented mean with standard deviation for continuous variables and raw number with corresponding percentages for categorical data. Percentages were also obtained for the rates of collection of individual and complete vital signs in each age group. We performed unadjusted analysis using univariate regression, followed by adjusted analysis using multivariate logistic regression to test associations of clinical predictors with outcomes, while adjusting for potential confounders. Our primary predictor of interest was age category. Our primary outcome of interest was documentation of complete vital signs. Secondary outcomes included documentation of pain scores and GCS in trauma patients and documentation of lung sounds and oxygen saturation in patients with a respiratory complaint. We included variables in adjusted models if they had an unadjusted association with outcome significant at a threshold of P <0.10. In adjusted models, we excluded height and weight as they were collinear with age. Because patients may cluster within primary EMS provider or ambulance service, it was our a priori analysis plan to perform hierarchical models using random effects for provider and service. However, even 2-level intercept-only models failed to converge. Instead, we repeated all analyses post hoc using robust Huber/White/sandwich estimators adjusting for clustering within these groups and noted no change in the results.
Results
Characteristics of study subjects.
We identified 661,800 EMS cases during the study period, of which 371,746 met study criteria and comprised the final cohort (Figure 1). The study cohort included 349,863 (94.1%) adult and 21,883 (5.9%) pediatric patients (Table 1).
Figure 1.
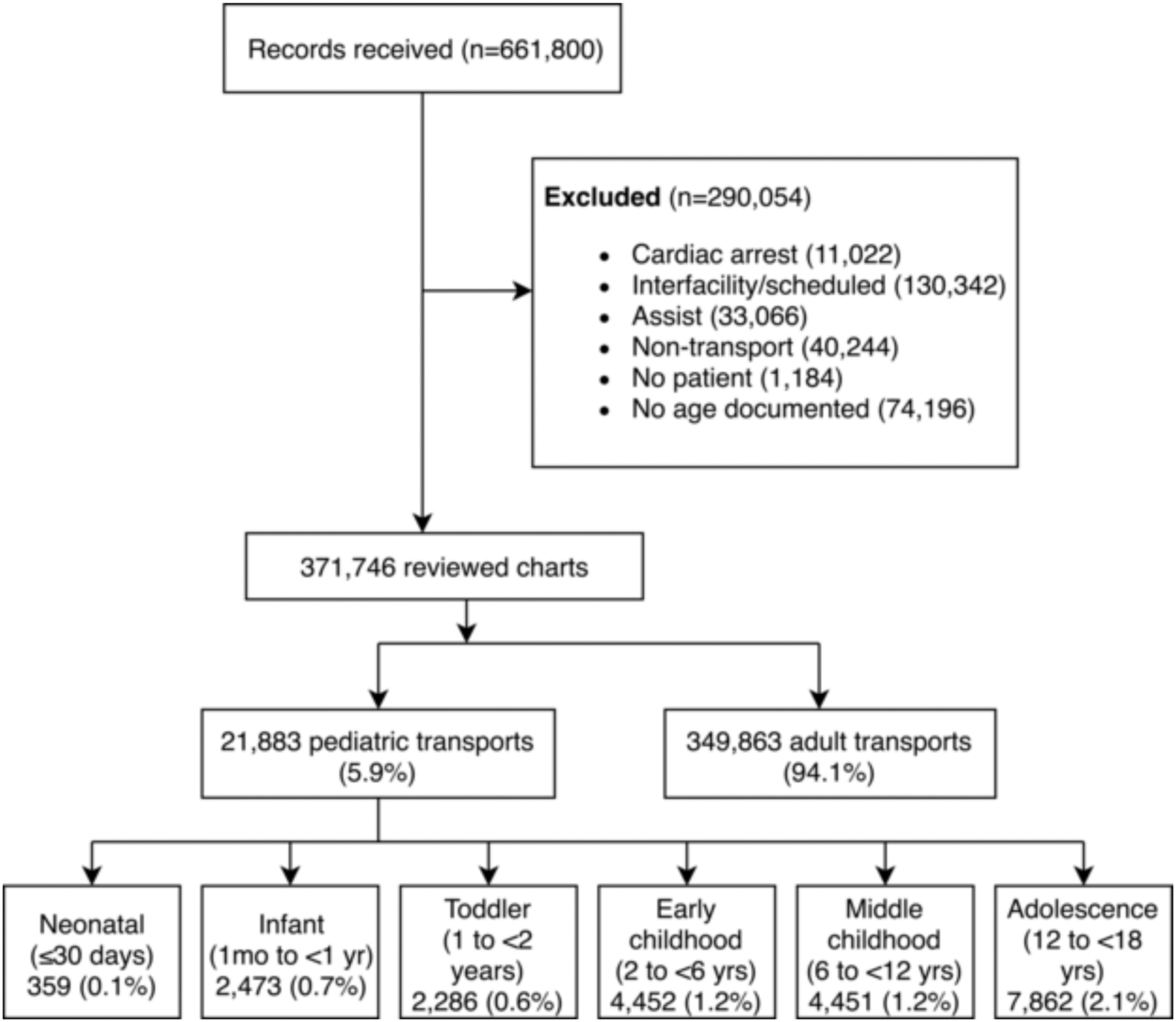
STROBE diagram illustrating patient inclusion.
Table 1.
Case characteristics, rates of vital signs and subgroup assessments by age group.
| Pediatric | Adult | ||||||
|---|---|---|---|---|---|---|---|
| Neonate | Infant | Toddler | Early childhood | Middle childhood | Adolescent | ||
| Demographics | |||||||
| Number | 359 (0.1%) | 2,473 (0.7%) | 2,286 (0.6%) | 4,452 (1.2%) | 4,451 (1.2%) | 7,862 (2.1%) | 349,863 (94.1%) |
| No. male/total (%) | 167/338 (49.4%) | 1,386/2,457 (56.4%) | 1,332/2,272 (58.6%) | 2,529/4,435 (57.0%) | 2,494/4,430 (56.3%) | 3,631/7,814 (46.5%) | 152,375/348,417 (43.7%) |
| EMS characteristics | |||||||
| Mean response time (min) [mean (SD)] |
8.8 (6.0) | 9.2 (5.1) | 9.2 (5.0) | 9.2 (5.3) | 9.0 (5.3) | 8.8 (5.3) | 9.2 (5.8) |
| Time at scene (min) [mean (SD)] |
13.5 (10.1) | 11.3 (7.0) | 10.9 (6.5) | 10.9 (6.8) | 12.4 (7.9) | 12.8 (8.1) | 15.5 (9.0) |
| Transport time (min) [mean (SD)] |
17.6 (10.3) | 18.6 (11.3) | 18.5 (11.2) | 18.0 (11.2) | 18.4 (12.1) | 16.6 (11.0) | 13.9 (9.1) |
| Lights and siren use [number/total (%)] |
117/358 (32.7%) | 547/2,468 (22.2%) | 529/2,282 (23.2%) | 1,033/4,446 (23.2%) | 902/4,437 (20.3%) | 1,537/7,846 (19.6%) | 69,578/349,077 (19.9%) |
| ALS Transport [number/total (%)] |
354/358 (98.9%) | 2,438/2,471 (98.7%) | 2,242/2,284 (98.2%) | 4,349/4,446 (98.3%) | 4,344/4,447 (97.4%) | 337,469/349,12 2 (96.7%) |
358,860/370,973 (96.7%) |
| Medical category | |||||||
| General medical | 123 (34.4%) | 1,279 (51.7%) | 884 (38.7%) | 1,524 (34.3%) | 1,034 (23.3%) | 1,542 (19.6%) | 108,796 (31.3%) |
| Trauma | 23 (6.2%) | 282 (11.4%) | 373 (16.3%) | 1,143 (25.7%) | 1,499 (33.8%) | 2,390 (30.4%) | 58,759 (16.9%) |
| Respiratory/airway | 104 (29.1%) | 524 (21.2%) | 354 (15.5%) | 655 (14.7%) | 492 (11.1%) | 530 (6.8%) | 34,472 (9.9%) |
| Allergic | 0 (0.0%) | 42 (1.7%) | 56 (2.5%) | 108 (2.4%) | 111 (2.5%) | 142 (1.8%) | 1,855 (0.5%) |
| Gastrointestinal | 13 (3.6%) | 63 (2.6%) | 50 (2.2%) | 193 (4.3%) | 232 (5.2%) | 515 (6.6%) | 29,599 (8.5%) |
| Cardiovascular | 1 (0.3%) | 5 (0.2%) | 5 (0.2%) | 12 (0.3%) | 60 (1.4%) | 164 (2.1%) | 24,387 (7.0%) |
| Neurological | 7 (2.0%) | 106 (4.3%) | 343 (15.0%) | 461 (10.4%) | 492 (11.1%) | 595 (7.6%) | 26,587 (7.6%) |
| Psychiatric/behavioral | 0 (0.0%) | 0 (0.0%) | 1 (0.0%) | 5 (0.1%) | 240 (5.4%) | 717 (9.1%) | 9,465 (2.7%) |
| Toxicological | 1 (0.3%) | 15 (0.6%) | 58 (2.6%) | 86 (1.9%) | 28 (0.6%) | 406 (5.2%) | 15,564 (4.5%) |
| Dizziness/syncope | 3 (0.8%) | 26 (1.1%) | 30 (1.3%) | 44 (1.0%) | 112 (2.5%) | 427 (5.4%) | 17,537 (5.0%) |
| Other | 78 (21.8%) | 115 (4.7%) | 121 (5.3%) | 188 (4.2%) | 122 (2.8%) | 397 (5.1%) | 18,403 (5.3%) |
| Unknown | 5 (1.4%) | 15 (0.6%) | 11 (0.5%) | 31 (0.7%) | 19 (0.4%) | 26 (0.3%) | 2,347 (0.7%) |
| Vital sign assessments | |||||||
| Heart rate | 310 (86.4%) | 2,368 (95.8%) | 2,198 (96.2%) | 4,331 (97.3%) | 4,364 (98.1%) | 7,802 (99.2%) | 347,042 (99.1%) |
| Systolic blood pressure | 181 (50.4%) | 1,705 (68.9%) | 1,805 (79.0%) | 3,949 (88.7%) | 4,299 (96.6%) | 7,782 (99.0%) | 345,996 (98.9%) |
| Respiratory rate | 302 (84.1%) | 2,324 (94.0%) | 2,167 (94.8%) | 4,269 (95.9%) | 4,313 (96.9%) | 7,734 (98.4%) | 343,485 (98.2%) |
| All three vital signs | 178 (49.6%) | 1,687 (68.2%) | 1,786 (78.1%) | 3,892 (87.4%) | 4,241 (95.3%) | 7,701 (98.0%) | 341,893 (97.7%) |
| Respiratory patients | |||||||
| Pulse oximetry | 65 (62.5%) | 413 (78.8%) | 321 (90.7%) | 631 (96.3%) | 489 (99.4%) | 525 (99.1%) | 33,833 (98.2%) |
| Lung sound assessment | 95 (91.4%) | 494 (94.3%) | 326 (92.1%) | 620 (94.7%) | 471 (95.7%) | 504 (95.1%) | 33,176 (96.2%) |
| Trauma patients | |||||||
| Pain score | 1 (4.4%) | 44 (15.6%) | 48 (12.9%) | 281 (24.6%) | 555 (37.0%) | 1,070 (44.8%) | 23,628 (40.2%) |
| GCS assessment | 20 (87.0%) | 281 (99.7%) | 368 (98.7%) | 1,131 (99.0%) | 1,487 (99.2%) | 2,378 (99.5%) | 58,293 (99.2%) |
| Cardiac | |||||||
| Monitor placement | 0 (0.0%) | 5 (100.0%) | 4 (80.0%) | 10 (83.3%) | 36 (60.0%) | 139 (84.8%) | 23,002 (94.3%) |
SD, standard deviation; ALS, Advanced life support; min, minutes; GCS, Glasgow coma scale
Main results.
Rates of vital signs documentation increased with age, with measurements of blood pressure constituting the primary driver of incomplete vital signs documentation. Blood pressure was measured in 50.4% of neonates versus 98.9% of adults. Documentation of complete vital signs (pulse, blood pressure, and respiratory rate) was lowest at 49.6% in neonates and increased in older age groups. Adolescents had similar rates of vital signs documentation compared to adults (98.0% versus 97.7%) (Table 1).
Odds of complete vital signs assessment were decreased in most pediatric age groups as compared to adults, a finding that was confirmed in the adjusted analysis. The adjusted odds ratio of complete vital signs assessment was 0.02 in neonates (95% CI 0.02 – 0.03), 0.04 in infants (95% CI 0.03 – 0.04), 0.07 in toddlers (95% CI 0.06 – 0.07), 0.13 in early childhood (95% CI 0.12 – 0.15), and 0.54 in middle childhood (95% CI 0.46 – 0.63). The only exception was in adolescents, who had slightly higher odds of vital signs assessment in the adjusted model (OR 1.40, 95% CI 1.18 – 1.66) (Tables 2, Figure 2).
Table 2.
Unadjusted and adjusted logistic regression of complete vital signs assessments.
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Age Group | ||||
| Adult | Ref | -- | Ref | -- |
| Neonate | 0.02 (0.02 – 0.03) | <0.001 | 0.02 (0.02 – 0.03) | <0.001 |
| Infant | 0.05 (0.05 – 0.05) | <0.001 | 0.04 (0.03 – 0.04) | <0.001 |
| Toddler | 0.08 (0.08 – 0.09) | <0.001 | 0.07 (0.06 – 0.07) | <0.001 |
| Early childhood | 0.16 (0.15 – 0.18) | <0.001 | 0.13 (0.12 – 0.15) | <0.001 |
| Middle childhood | 0.47 (0.41 – 0.54) | <0.001 | 0.54 (0.46 – 0.63) | <0.001 |
| Adolescent | 1.11 (0.95 – 1.31) | <0.176 | 1.40 (1.18 – 1.66) | <0.001 |
| Demographics | ||||
| Male sex | 0.87 (0.84 – 0.91) | <0.001 | 0.93 (0.89 – 0.97) | 0.001 |
| Height (inches) | 1.08 (1.07 – 1.08) | <0.001 | ||
| Weight (kg) | 1.01 (1.01 – 1.01) | <0.001 | ||
| Race/ethnicity | ||||
| White/Non-Hispanic | Ref | -- | Ref | -- |
| White/Hispanic | 1.00 (0.76 – 1.33) | 0.984 | 1.12 (0.81 – 1.54) | 0.488 |
| Black/Non-Hispanic | 1.16 (1.10 – 1.23) | <0.001 | 1.45 (1.37 – 1.55) | <0.001 |
| Black/Hispanic | 1.16 (0.73 – 1.86) | 0.526 | 1.46 (0.86 – 2.46) | 0.160 |
| Other/Unknown | 1.45 (1.39 – 1.52) | <0.001 | 1.71 (1.61 – 1.80) | <0.001 |
| Medical category | ||||
| Medical | Ref | -- | Ref | -- |
| Trauma | 0.79 (0.75 – 0.84) | <0.001 | 0.75 (0.70 – 0.80) | <0.001 |
| Respiratory | 1.04 (0.96 – 1.13) | 0.301 | 0.78 (0.71 – 0.85) | <0.001 |
| Allergy | 1.13 (0.85 – 1.51) | 0.409 | 1.26 (0.92 – 1.73) | 0.156 |
| GI/Abdominal | 1.27 (1.16 – 1.39) | <0.001 | 0.88 (0.80 – 0.97) | 0.010 |
| Cardiac | 2.45 (2.15 – 2.80) | <0.001 | 0.72 (0.62 – 0.83) | <0.001 |
| Neurology | 1.23 (1.12 – 1.35) | <0.001 | 0.86 (0.78 – 0.96) | 0.004 |
| Psychiatry | 0.19 (0.18 – 0.20) | <0.001 | 0.18 (0.17 – 0.20) | <0.001 |
| Toxicology | 2.97 (2.49 – 3.55) | <0.001 | 2.14 (1.77 – 2.59) | <0.001 |
| Dizziness/Syncope | 1.98 (1.72 – 2.28) | <0.001 | 0.87 (0.75 – 1.01) | 0.071 |
| Other | 0.23 (0.21 – 0.24) | <0.001 | 0.31 (0.29 – 0.33) | <0.001 |
| Unknown | 0.26 (0.22 – 0.30) | <0.001 | 0.43 (0.34 – 0.53) | <0.001 |
| Day period | ||||
| 00:00–05:59 | Ref | -- | Ref | -- |
| 06:00–11:59 | 1.03 (0.97 – 1.10) | 0.323 | 1.07 (1.00 – 1.16) | 0.057 |
| 12:00–17:59 | 0.93 (0.88 – 1.00) | 0.035 | 1.01 (0.94 – 1.08) | 0.789 |
| 18:00–23:59 | 0.99 (0.92 – 1.06) | 0.713 | 1.08 (1.00 – 1.16) | 0.037 |
| Year | ||||
| 2013 | Ref | -- | Ref | -- |
| 2014 | 0.84 (0.79 – 0.90) | <0.001 | 0.77 (0.72 – 0.83) | <0.001 |
| 2015 | 0.78 (0.73 – 0.84) | <0.001 | 0.70 (0.65 – 0.75) | <0.001 |
| 2016 | 0.81 (0.76 – 0.87) | <0.001 | 0.71 (0.66 – 0.76) | <0.001 |
| Response characteristics | ||||
| Advanced Life Support | 5.74 (5.42 – 6.08) | <0.001 | 3.12 (2.91 – 3.35) | <0.001 |
| Lights and siren use | 1.59 (1.50 – 1.68) | <0.001 | 1.19 (1.11 – 1.27) | <0.001 |
| Mileage | 1.00 (1.00 – 1.00) | 0.910 | ||
| Response time | 0.98 (0.98 – 0.98) | <0.001 | 1.00 (0.99 – 1.00) | 0.034 |
| Scene time | 1.01 (1.01 – 1.01) | <0.001 | 0.99 (0.99 – 0.99) | <0.001 |
| Transport time | 0.99 (0.99–0.99) | <0.001 | 1.00 (1.00 – 1.01) | <0.001 |
| Intravenous access | 6.02 (5.65 – 6.42) | <0.001 | 2.83 (2.60 – 3.08) | <0.001 |
| Monitor used | 4.04 (3.83 – 4.26) | <0.001 | 1.82 (1.69 – 1.95) | <0.001 |
| Glasgow Coma Score obtained | 1.08 (1.07 – 1.09) | <0.001 | 1.14 (1.12 – 1.15) | <0.001 |
OR, odds ratio; CI, confidence interval
Figure 2.
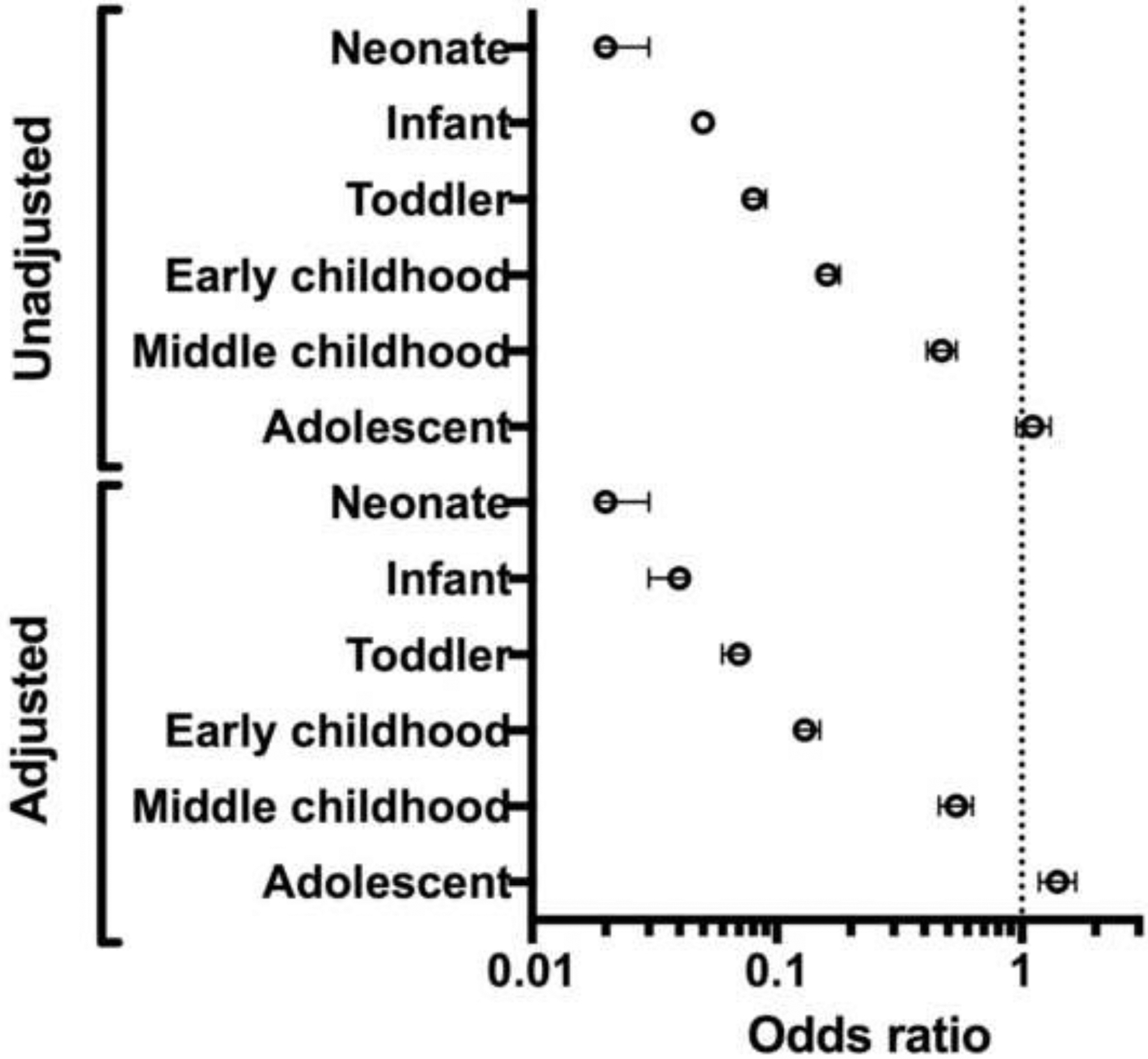
Odds ratios with 95% confidence intervals of complete vital signs assessments by age group in unadjusted and adjusted models.
In patients with a medical category of trauma, there were no significant age-related factors accounting for differences in GCS ascertainment after adjusted analysis (Tables 3–4; online). Pediatric pain scores were assessed less frequently in pediatric traumas compared to adult traumas in adjusted analysis (OR 0.80, 95% CI 0.76 – 0.85). This was noted specifically in neonates (OR 0.11, 95% CI 0.01 – 0.80), infants (OR 0.33, 95% CI 0.24 – 0.46), toddlers (OR 0.26, 95% CI 0.19 – 0.35), and in early childhood (OR 0.57, 95% CI 0.49 – 0.65) (Tables 5–6; online). In patients with a respiratory complaint, pulse oximetry was less frequently checked in pediatric patients following adjusted analysis (OR 0.20, 95% CI 0.18–0.25). This was noted in neonates (0.03, 95% CI 0.02 – 0.05), infants (OR 0.06, 95% CI 0.05 – 0.08), toddlers (OR 0.16, 95% CI 0.11 – 0.23), and in early childhood (OR 0.45, 95% CI 0.29 – 0.69) when compared to adults (Tables 7–8; online). No significant differences were noted in rates of lung sound assessments between pediatric and adult patients following adjusted analysis (Tables 9–10; online).
Table 3.
Trauma patients: assessment of GCS, unadjusted (univariate) analysis.
| Variable | OR (95% CI) | p |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.05 (0.02 – 0.18) | <0.001 |
| Infant | 2.25 (0.31 – 16.04) | 0.420 |
| Toddler | 0.59 (0.24 – 1.43) | 0.241 |
| Early childhood | 0.75 (0.42 – 1.34) | 0.335 |
| Middle childhood | 0.99 (0.56 – 1.76) | 0.974 |
| Adolescent | 1.58 (0.89 – 2.81) | 0.117 |
| Demographics | ||
| Male sex | 0.98 (0.82 – 1.17) | 0.856 |
| Height (inches) | 1.02 (0.96 – 1.09) | 0.547 |
| Weight (kg) | 1.00 (1.00 – 1.01) | 0.208 |
| Race/Ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 0.43 (0.18 – 1.06) | 0.066 |
| Black/Non-Hispanic | 1.19 (0.88 – 1.60) | 0.261 |
| Black/Hispanic | 1* | -- |
| Other/Unknown | 0.76 (0.63 – 0.92) | <0.001 |
| Day period | ||
| 00:00–05:59 | Ref | |
| 00:00–05:59 | 0.62 (0.45 – 0.87) | <0.01 |
| 06:00–11:59 | 0.63 (0.46 – 0.86) | <0.01 |
| 12:00–17:59 | 0.76 (0.55 – 1.06) | 0.10 |
| Year | ||
| 2013 | Ref | |
| 2014 | 1.03 (0.78 – 1.36) | 0.834 |
| 2015 | 0.99 (0.75 – 1.31) | 0.954 |
| 2016 | 1.10 (0.83 – 1.46) | 0.489 |
| Response Characteristics | ||
| Advanced Life support | 2.82 (2.07 – 3.84) | <0.001 |
| Lights and siren use | 1.24 (0.97 – 1.58) | 0.088 |
| Mileage | 1.00 (0.99 – 1.01) | 0.624 |
| Response time | 0.99 (0.97 – 1.00) | 0.058 |
| Scene time | 1.02 (1.00 – 1.03) | 0.005 |
| Transport time | 1.00 (0.99 – 1.01) | 0.762 |
| Intravenous Access | 3.16 (2.41 – 4.13) | <0.001 |
| Monitor placed | 4.19 (3.05 – 5.75) | <0.001 |
OR, odds ratio; CI, confidence interval.
Outcome in Black/Hispanic patients was collinear with outcome in this subanalysis.
Table 4.
Trauma patients: assessment of GCS, adjusted (multivariate) analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.21 (0.03 – 1.64) | 0.137 |
| Infant | 2.77 (0.39 – 19.80) | 0.311 |
| Toddler | 0.75 (0.31 – 1.84) | 0.528 |
| Early childhood | 1.02 (0.56 – 1.88) | 0.938 |
| Middle childhood | 1.16 (0.65 – 2.07) | 0.622 |
| Adolescent | 1.72 (0.95 – 3.16) | 0.075 |
| Demographics | ||
| Male sex | 0.90 (0.75 – 1.08) | 0.245 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 0.39 (0.16 – 0.95) | 0.038 |
| Black/Non-Hispanic | 1.17 (0.86 – 1.60) | 0.313 |
| Black/Hispanic | 1* | -- |
| Other/Unknown | 0.78 (0.64 – 0.95) | 0.012 |
| Day period | ||
| 00:00–05:59 | Ref | |
| 00:00–05:59 | 0.62 (0.45 – 0.87) | 0.006 |
| 06:00–11:59 | 0.62 (0.45 – 0.86) | 0.004 |
| 12:00–17:59 | 0.74 (0.53 – 1.04) | 0.079 |
| Year | ||
| 2013 | Ref | |
| 2014 | 1.016 (0.767 – 1.346) | 0.911 |
| 2015 | 1.065 (0.804 – 1.411) | 0.659 |
| 2016 | 1.215 (0.915 – 1.615) | 0.178 |
| Response Characteristics | ||
| Advanced Life Support | 2.30 (1.67 – 3.17) | <0.001 |
| Lights and siren use | 0.98 (0.76 – 1.26) | 0.879 |
| Response time | 0.99 (0.98 – 1.00) | 0.277 |
| Scene time | 1.00 (0.99 – 1.01) | 0.211 |
| Transport time | 0.99 (0.98 – 1.00) | <0.001 |
| Intravenous Access | 1.76 (1.27 – 2.45) | 0.001 |
| Monitor placed | 2.83 (1.95 – 4.11) | <0.001 |
OR, odds ratio; CI, confidence interval.
Outcome in Black/Hispanic patients was collinear with outcome in this subanalysis.
Table 5.
Trauma patients: assessment of pain scores; unadjusted (univariate) analysis.
| OR (95% CI) | p | |
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.07 (0.01 – 0.50) | 0.008 |
| Infant | 0.25 (0.20 – 0.38) | <0.001 |
| Toddler | 0.22 (0.16 – 0.30) | <0.001 |
| Early childhood | 0.49 (0.42 – 0.56) | <0.001 |
| Middle childhood | 0.87 (0.79 – 0.97) | 0.013 |
| Adolescent | 1.21 (1.11 – 1.31) | <0.001 |
| Demographics | ||
| Male sex | 0.99 (0.96 – 1.03) | 0.738 |
| Height (inches) | 1.01 (1.00 – 1.03) | 0.023 |
| Weight (kg) | 1.00 (1.00 – 1.00) | <0.001 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 1.11 (0.88 – 1.38) | 0.388 |
| Black/Non-Hispanic | 0.83 (0.79 – 0.87) | <0.001 |
| Black/Hispanic | 0.97 (0.66 – 1.44) | 0.896 |
| Other/Unknown | 0.60 (0.58 – 0.62) | <0.001 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 1.20 (1.14 – 1.26) | <0.001 |
| 12:00–17:59 | 1.19 (1.13 – 1.26) | <0.001 |
| 18:00–23:59 | 1.10 (1.05 – 1.16) | <0.001 |
| Year | ||
| 2013 | Ref | |
| 2014 | 1.03 (0.98 – 1.09) | 0.193 |
| 2015 | 0.97 (0.92 – 1.02) | 0.237 |
| 2016 | 0.93 (0.88 – 0.99) | 0.005 |
| Response Characteristics | ||
| Advanced Life Support | 1.42 (1.30 – 1.56) | <0.001 |
| Lights and sirens | 0.96 (0.92 – 1.00) | 0.060 |
| Mileage | 1.00 (1.00 – 1.000) | 0.444 |
| Response time | 1.01 (1.01 – 1.01) | <0.001 |
| Scene time | 1.02 (1.01 – 1.02) | <0.001 |
| Transport time | 1.01 (1.01 – 1.01) | <0.001 |
| Intravenous Access | 1.63 (1.57 – 1.69) | <0.001 |
| Monitor placed | 1.74 (1.68 – 1.80) | <0.001 |
| Glasgow Coma Score assessment | 1.23 (1.20 – 1.26) | <0.001 |
OR, odds ratio; CI, confidence interval
Table 6.
Trauma patients: assessment of pain scores; adjusted (multivariate) analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.11 (0.01 – 0.80) | 0.030 |
| Infant | 0.33 (0.24 – 0.46) | <0.001 |
| Toddler | 0.26 (0.19 – 0.35) | <0.001 |
| Early childhood | 0.57 (0.49 – 0.65) | <0.001 |
| Middle childhood | 0.99 (0.88 – 1.10) | 0.823 |
| Adolescent | 1.23 (1.17 – 1.39) | <0.001 |
| Demographics | ||
| Male sex | 1.01 (0.98 – 1.05) | 0.485 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 1.09 (0.86 – 1.38) | 0.465 |
| Black/Non-Hispanic | 0.89 (0.84 – 0.93) | <0.001 |
| Black/Hispanic | 1.10 (0.74 – 1.64) | 0.639 |
| Other/Unknown | 0.64 (0.61 – 0.66) | <0.001 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 1.15 (1.09 – 1.22) | <0.001 |
| 12:00–17:59 | 1.16 (1.10 – 1.22) | <0.001 |
| 18:00–23:59 | 1.09 (1.03 – 1.15) | 0.002 |
| Year | ||
| 2013 | Ref | |
| 2014 | 1.01 (0.96 – 1.07) | 0.707 |
| 2015 | 0.97 (0.92 – 1.02) | 0.203 |
| 2016 | 0.95 (0.90 – 1.00) | 0.050 |
| Response Characteristics | ||
| Advanced Life Support | 1.33 (1.21 – 1.47) | <0.001 |
| Lights and sirens | 1.01 (0.97 – 1.06) | 0.653 |
| Response time | 1.01 (1.01 – 1.01) | <0.001 |
| Scene time | 1.01 (1.01 – 1.01) | <0.001 |
| Transport time | 1.00 (1.00 – 1.01) | 0.001 |
| Intravenous Access | 1.27 (1.21 – 1.33) | <0.001 |
| Monitor placed | 1.39 (1.33 – 1.46) | <0.001 |
| Glasgow Coma Score assessment | 1.30 (1.27 – 1.33) | <0.001 |
OR, odds ratio; CI, confidence interval
Table 7.
Respiratory patients: assessment of pulse oximetry; unadjusted (univariate) analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.03 (0.21 – 0.05) | <0.001 |
| Infant | 0.07 (0.06 – 0.09) | <0.001 |
| Toddler | 0.18 (0.13 – 0.27) | <0.001 |
| Early childhood | 0.50 (0.33 – 0.75) | 0.001 |
| Middle childhood | 3.08 (0.99 – 9.60) | 0.053 |
| Adolescent | 1.98 (0.82 – 4.80) | 0.129 |
| Demographics | ||
| Male sex | 0.96 (0.83 – 1.10) | 0.529 |
| Height (inches) | 1.06 (1.04 – 1.08) | <0.001 |
| Weight (kg) | 1.00 (1.00 – 1.01) | <0.001 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 0.71 (0.29 – 1.73) | 0.453 |
| Black/Non-Hispanic | 1.54 (1.26 – 1.88) | <0.001 |
| Black/Hispanic | 0.79 (0.19 – 3.23) | 0.741 |
| Other/Unknown | 1.17 (1.00 – 1.37) | 0.055 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 1.03 (0.83 – 1.23) | 0.795 |
| 12:00–17:59 | 0.84 (0.68 – 1.04) | 0.109 |
| 18:00–23:59 | 0.92 (0.74 – 1.15) | 0.467 |
| Year | ||
| 2013 | Ref | |
| 2014 | 1.10 (0.90 – 1.35) | 0.361 |
| 2015 | 1.39 (1.13 – 1.72) | 0.002 |
| 2016 | 1.53 (1.23 – 1.89) | <0.001 |
| Response Characteristics | ||
| Advanced Life Support | 6.80 (5.04 – 9.18) | <0.001 |
| Lights and sirens use | 1.16 (1.00 – 1.35) | 0.057 |
| Mileage | 1.00 (1.00 – 1.00) | 0.403 |
| Response time | 1.01 (1.01 – 1.01) | <0.001 |
| Scene time | 1.02 (1.01 – 1.02) | <0.001 |
| Transport time | 1.02 (1.00 – 1.03) | 0.048 |
| Intravenous Access | 1.02 (1.01 – 1.03) | <0.001 |
| Monitor placed | 1.00 (1.00 – 1.01) | 0.290 |
| Glasgow Coma Score assessment | 1.08 (1.04 – 1.11) | <0.001 |
OR, odds ratio; CI, confidence interval
Table 8.
Respiratory patients: assessment of pulse oximetry; adjusted (multivariate) analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.03 (0.02 – 0.05) | <0.001 |
| Infant | 0.06 (0.05 – 0.08) | <0.001 |
| Toddler | 0.16 (0.11 – 0.23) | <0.001 |
| Early childhood | 0.45 (0.29 – 0.69) | <0.001 |
| Middle childhood | 2.56 (0.81 – 8.04) | 0.108 |
| Adolescent | 1.78 (0.73 – 4.32) | 0.207 |
| Demographics | ||
| Male sex | 1.08 (0.93 – 1.25) | 0.291 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 0.88 (0.34 – 2.27) | 0.799 |
| Black/Non-Hispanic | 2.25 (1.80 – 2.81) | <0.001 |
| Black/Hispanic | 2.39 (0.31 – 18.56) | 0.404 |
| Other/Unknown | 1.71 (1.42 – 2.07) | <0.001 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 0.94 (0.74 – 1.18) | 0.569 |
| 12:00–17:59 | 0.81 (0.65 – 1.01) | 0.066 |
| 18:00–23:59 | 0.97 (0.77 – 1.22) | 0.810 |
| Year | ||
| 2013 | Ref | |
| 2014 | 1.038 (0.84 – 1.29) | 0.737 |
| 2015 | 1.379 (1.11 – 1.73) | 0.004 |
| 2016 | 1.430 (1.14 – 1.80) | 0.002 |
| Response Characteristics | ||
| Advanced Life Support | 5.22 (3.74 – 7.27) | <0.001 |
| Lights and sirens use | 1.18 (1.00 – 1.40) | 0.048 |
| Response time | 1.01 (0.99 – 1.02) | 0.420 |
| Scene time | 1.00 (0.99 – 1.01) | 0.901 |
| Transport time | 1.02 (1.01 – 1.03) | <0.001 |
| Intravenous Access | 1.20 (0.99 – 1.45) | 0.066 |
| Monitor placed | 1.84 (1.53 – 2.20) | <0.001 |
| Glasgow Coma Score assessment | 1.09 (1.05 – 1.13) | <0.001 |
OR, odds ratio; CI, confidence interval
Table 9.
Respiratory patients: assessment of lung sounds; unadjusted (univariate) analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.41 (0.21 – 0.82) | 0.011 |
| Infant | 0.64 (0.44 – 0.93) | 0.020 |
| Toddler | 0.45 (0.31 – 0.67) | <0.001 |
| Early childhood | 0.69 (0.49 – 0.98) | 0.036 |
| Middle childhood | 0.88 (0.56 – 1.36) | 0.556 |
| Adolescent | 0.76 (0.50 – 1.13) | 0.171 |
| Demographics | ||
| Male sex | 0.96 (0.83 – 1.10) | 0.529 |
| Height (inches) | 1.06 (1.04 – 1.08) | <0.001 |
| Weight (kg) | 1.00 (1.00 – 1.01) | <0.001 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 0.71 (0.29 – 1.73) | 0.453 |
| Black/Non-Hispanic | 1.54 (1.26 – 1.88) | <0.001 |
| Black/Hispanic | 0.79 (0.19 – 3.23) | 0.741 |
| Other/Unknown | 1.17 (1.00 – 1.37) | 0.055 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 1.07 (0.91 – 1.25) | 0.414 |
| 12:00–17:59 | 1.24 (1.06 – 1.45) | 0.008 |
| 18:00–23:59 | 1.10 (0.94 – 1.30) | 0.249 |
| Year | ||
| 2013 | Ref | |
| 2014 | 1.24 (1.06 – 1.46) | 0.008 |
| 2015 | 1.45 (1.23 – 1.71) | <0.001 |
| 2016 | 1.25 (1.06 – 1.47) | 0.007 |
| Response Characteristics | ||
| Advanced Life Support | 1.39 (0.89 – 2.17) | 0.142 |
| Lights and sirens use | 0.44 (0.39 – 0.48) | <0.001 |
| Mileage | 1.08 (1.06 – 1.09) | <0.001 |
| Response time | 0.98 (0.97 – 0.99) | <0.001 |
| Scene time | 1.02 (1.01 – 1.02) | <0.001 |
| Transport time | 1.00 (0.99 – 1.00) | 0.161 |
| Intravenous Access | 2.53 (2.27 – 2.82) | <0.001 |
| Monitor placed | 3.82 (3.43 – 4.25) | <0.001 |
| Glasgow Coma Score assessment | 1.04 (1.01 – 1.07) | 0.005 |
OR, odds ratio; CI, confidence interval
Table 10.
Respiratory patients: assessment of lung sounds; adjusted (multivariate) analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 1.09 (0.47 – 2.53) | 0.837 |
| Infant | 1.31 (0.86 – 1.99) | 0.203 |
| Toddler | 0.85 (0.56 – 1.29) | 0.434 |
| Early childhood | 1.37 (0.95 – 1.99) | 0.096 |
| Middle childhood | 1.43 (0.90 – 2.28) | 0.126 |
| Adolescent | 1.15 (0.76 – 1.76) | 0.508 |
| Demographics | ||
| Male sex | 0.87 (0.78 – 0.98) | 0.017 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 0.60 (0.24 – 1.48) | 0.265 |
| Black/Non-Hispanic | 0.67 (0.38 – 0.50) | <0.001 |
| Black/Hispanic | 0.80 (0.19 – 3.31) | 0.754 |
| Other/Unknown | 0.43 (0.38 – 0.50) | <0.001 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 0.93 (0.79 – 1.10) | 0.424 |
| 12:00–17:59 | 1.11 (0.94 – 1.32) | 0.220 |
| 18:00–23:59 | 1.08 (0.90 – 1.29) | 0.395 |
| Year | ||
| 2013 | Ref | |
| 2014 | 1.27 (1.07 – 1.51) | 0.007 |
| 2015 | 1.54 (1.29 – 1.84) | <0.001 |
| 2016 | 1.29 (1.09 – 1.53) | 0.004 |
| Response Characteristics | ||
| Advanced Life Support | 0.88 (0.54 – 1.44) | 0.610 |
| Lights and sirens use | 0.57 (0.51 – 0.64) | <0.001 |
| Response time | 0.98 (0.97 – 1.00) | 0.005 |
| Scene time | 0.99 (0.98 – 1.00) | 0.005 |
| Transport time | 0.99 (0.99 – 1.00) | 0.048 |
| Intravenous Access | 1.40 (1.22 – 1.61) | <0.001 |
| Monitor placed | 2.86 (2.49 – 3.28) | <0.001 |
| Glasgow Coma Score assessment | 1.05 (1.02 – 1.09) | 0.002 |
OR, odds ratio; CI, confidence interval
We performed a sensitivity analysis for our primary outcome (vital signs assessment) adjusting for standard errors for clustering within service or providers. Overall results were similar in respect to age to those presented in the primary analysis (Tables 11–14; online).
Table 11.
Odds ratios of complete vital sign assessment following adjustment of standard error for clusters in primary caregiver (n=1,444); unadjusted (univariate) analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.02 (0.02 – 0.32) | <0.001 |
| Infant | 0.05 (0.04 – 0.06) | <0.001 |
| Toddler | 0.08 (0.06 – 0.11) | <0.001 |
| Early childhood | 0.16 (0.13 – 0.20) | <0.001 |
| Middle childhood | 0.47 (0.38 – 0.57) | <0.001 |
| Adolescent | 1.13 (0.94 – 1.37) | 0.185 |
| Demographics | ||
| Male sex | 0.87 (0.82 – 0.93) | <0.001 |
| Height (inches) | 1.08 (1.06 – 1.10) | <0.001 |
| Weight (kg) | 1.01 (1.01 – 1.02) | <0.001 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 0.99 (0.72 – 1.36) | 0.937 |
| Black/Non-Hispanic | 1.16 (0.97 – 1.38) | 0.094 |
| Black/Hispanic | 1.15 (0.62 – 2.11) | 0.660 |
| Other/Unknown | 1.46 (1.12 – 1.90) | 0.005 |
| Medical category | ||
| Medical | Ref | |
| Trauma | 0.80 (0.69 – 0.92) | 0.002 |
| Respiratory | 1.06 (0.84 – 1.33) | 0.641 |
| Allergy | 1.14 (0.81 – 1.62) | 0.458 |
| GI/Abdominal | 1.27 (1.07 – 1.50) | 0.005 |
| Cardiac | 2.50 (1.68 – 3.72) | <0.001 |
| Neurology | 1.23 (1.01 – 1.51) | 0.041 |
| Psychiatry | 0.19 (0.16 – 0.23) | <0.001 |
| Toxicology | 3.04 (2.26 – 4.07) | <0.001 |
| Dizziness/Syncope | 2.05 (1.49 – 2.82) | <0.001 |
| Other | 0.23 (0.17 – 0.31) | <0.001 |
| Unknown | 0.26 (0.20 – 0.36) | <0.001 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 1.03 (0.89 – 1.19) | 0.706 |
| 12:00–17:59 | 0.94 (0.81 – 1.09) | 0.420 |
| 18:00–23:59 | 0.99 (0.89 – 1.10) | 0.842 |
| Year | ||
| 2013 | Ref | |
| 2014 | 0.84 (0.70 – 1.00) | 0.056 |
| 2015 | 0.78 (0.61 – 1.00) | 0.048 |
| 2016 | 0.83 (0.64 – 1.08) | 0.173 |
| Response Characteristics | ||
| Advanced Life Support | 5.71 (4.02 – 8.12) | <0.001 |
| Lights and sirens use | 1.60 (1.26 – 2.03) | <0.001 |
| Mileage | 1.00 (1.00 – 1.00) | 0.506 |
| Response time | 0.98 (0.96 – 1.00) | 0.038 |
| Scene time | 1.01 (1.00 – 1.03) | 0.040 |
| Transport time | 0.99 (0.98 – 1.00) | 0.009 |
| Intravenous Access | 5.95 (3.98 – 9.10) | <0.001 |
| Monitor placed | 3.99 (2.79 – 5.70) | <0.001 |
| Glasgow Coma Score assessment | 1.08 (1.05 – 1.10) | <0.001 |
OR, odds ratio; CI, confidence interval
Table 14:
Odds ratios of complete vital sign assessment following adjustment of standard error for clusters in 20 EMS agencies evaluated in this study; adjusted (multivariate) analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.02 (0.01 – 0.06) | <0.001 |
| Infant | 0.04 (0.02 – 0.08) | <0.001 |
| Toddler | 0.07 (0.03 – 0.13) | <0.001 |
| Early childhood | 0.13 (0.08 – 0.23) | <0.001 |
| Middle childhood | 0.54 (0.40 – 0.73) | <0.001 |
| Adolescent | 1.40 (1.12 – 1.74) | 0.003 |
| Demographics | ||
| Male sex | 0.93 (0.88 – 0.98) | 0.010 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 1.12 (0.70 – 1.78) | 0.636 |
| Black/Non-Hispanic | 1.45 (0.88 – 2.41) | 0.147 |
| Black/Hispanic | 1.46 (0.49 – 4.34) | 0.500 |
| Other/Unknown | 1.71 (0.71 – 4.09) | 0.230 |
| Medical category | ||
| Medical | Ref | |
| Trauma | 0.75 (0.51 – 1.11) | 0.150 |
| Respiratory | 0.78 (0.56 – 1.07) | 0.123 |
| Allergy | 1.26 (0.89 – 1.78) | 0.197 |
| GI/Abdominal | 0.88 (0.60 – 1.30) | 0.518 |
| Cardiac | 0.72 (0.53 – 0.97) | 0.031 |
| Neurology | 0.86 (0.60 – 1.25) | 0.434 |
| Psychiatry | 0.18 (0.10 – 0.34) | <0.001 |
| Toxicology | 2.14 (1.07 – 4.28) | 0.031 |
| Dizziness/Syncope | 0.87 (0.60 – 1.25) | 0.449 |
| Other | 0.31 (0.16 – 0.60) | 0.001 |
| Unknown | 0.43 (0.24 – 0.77) | 0.004 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 1.07 (0.94 – 1.225) | 0.290 |
| 12:00–17:59 | 1.01 (0.86 – 1.188) | 0.909 |
| 18:00–23:59 | 1.08 (0.98 – 1.197) | 0.135 |
| Year | ||
| 2013 | Ref | |
| 2014 | 0.77 (0.65 – 0.93) | 0.005 |
| 2015 | 0.70 (0.46 – 1.06) | 0.089 |
| 2016 | 0.70 (0.47 – 1.07) | 0.100 |
| Response Characteristics | ||
| Advanced Life Support | 3.12 (1.54 – 6.31) | 0.002 |
| Lights and sirens use | 1.19 (0.66 – 2.15) | 0.566 |
| Response time | 1.00 (0.97 – 1.02) | 0.808 |
| Scene time | 0.99 (0.99 – 1.00) | 0.081 |
| Transport time | 1.00 (0.99 – 1.02) | 0.628 |
| Intravenous Access | 2.83 (2.18 – 3.67) | <0.001 |
| Monitor placed | 1.82 (1.00 – 3.29) | 0.048 |
| Glasgow Coma Score assessment | 1.14 (1.10 – 1.17) | <0.001 |
OR, odds ratio; CI, confidence interval
Discussion
The purpose of this study was to compare the quality of prehospital assessments in pediatric versus adult patients. Using multivariate logistic regression evaluating a regional EMS database, we found that rates of vital signs assessments in most pediatric age groups were significantly lower compared to adult patients. This study emphasizes the need to improve pediatric assessments in the prehospital setting and can inform future education and research efforts aimed to improve the assessment and management of pediatric patients in the out-of-hospital setting.
Our findings confirm and further characterize the results of other studies that have shown a comparatively low rate of pediatric prehospital vital signs acquisition. A lack of vital signs documentation has been reported in regional studies7, 8 and in specific evaluations of trauma patients.6, 9 A study evaluating records from the National EMS Information System (NEMSIS) found that though 61.5% of pediatric EMS transports had at least one abnormal vital sign, complete documentation of vitals was highly variable.10 Our data add to prior literature by providing a level of granularity not available in similarly large administrative datasets. Additionally, this study was able to provide rates of assessments by age group and to control for potential confounders.
Subgroup analyses provided additional insight into prehospital pediatric assessments. We found lower rates of pain score assessments in pediatric patients with traumatic complaints. Pain is the most common complaint requiring pediatric EMS transport,11 and guidelines have been established for prehospital analgesia in trauma requiring the use of age-appropriate pain scales.12 Our finding of lower rates of pulse oximetry measurements in pediatric patients with respiratory complaints is consistent with findings from children included in the NEMSIS dataset11 In the present study, we were able to segregate our analysis to only those patients with a respiratory complaint, where all should ideally have pulse oximetry documented.
Other study findings also correlate with findings from national datasets, further supporting their generalizability. Our finding that pediatric cases constituted 6% of EMS transports is generally consistent with the reported EMS literature,2, 4, 7, 10, 13, 14 including an analysis from the 2013 NEMSIS Public Release Research Data Set.11 The most common reasons for pediatric transports included traumatic and respiratory conditions, a finding that correlates well with other pediatric prehospital studies1, 11, 13 and further emphasizes the importance of obtaining a thorough assessment for these common pediatric complaints.
A variety of factors may underlie the discrepancies in assessment of pediatric vital signs. Normal values for vital signs are age-dependent and more difficult to interpret for children. Though mandates require EMS providers to carry dedicated pediatric equipment, providers may be unfamiliar with their use. A large proportion of prehospital personnel see three or fewer pediatric patients in a given month.15 A survey of EMS personnel noted that only 19% had conducted pediatric simulation training using a highly realistic simulator in the two years preceding the study.4
Educational initiatives are likely required to improve pediatric prehospital assessments as providers will be unable to obtain sufficient training by experience alone. Suggestions to improve pediatric prehospital care have included increasing the frequency of pediatric training, increasing hands-on and shadowing time with pediatric patients, adding mixed methods of instruction, and providing specific teaching on pediatric dosing and procedures.5 A retrospective statewide study from Utah found that educational initiatives consisting of a short lecture series and a hands-on session targeted toward vital signs improved the rates of assessments by EMS providers over time.8
This was a retrospective study that relied on previously collected data. Additionally, data were collected in a single region from Western Pennsylvania. This study was unable to associate the vital signs assessments to outcomes of patients on arrival to the Emergency Department or to identify which system factors may have impacted pediatric vital signs assessments. Despite this, we suspect that age-related differences in assessments likely occur across urban, suburban, and rural regions nationally.
Conclusion
Care of pediatric patients relies on accurate and timely assessments in the prehospital setting. Rates of thorough vital signs assessment in many of these groups are significantly less than those of adults, a finding which persists after controlling for a variety of other factors and within important subgroups. Educational initiatives, including increasing hands-on time with pediatric patients and simulation sessions, may serve a role in improving comfort and familiarity of pediatric assessments.
Table 12:
Odds ratios of complete vital sign assessment following adjustment of standard error for clusters in primary caregiver (n=1,444); adjusted analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.02 (0.01 – 0.03) | <0.001 |
| Infant | 0.04 (0.03 – 0.05) | <0.001 |
| Toddler | 0.07 (0.05 – 0.09) | <0.001 |
| Early childhood | 0.13 (0.09 – 0.19) | <0.001 |
| Middle childhood | 0.54 (0.42 – 0.68) | <0.001 |
| Adolescent | 1.42 (1.15 – 1.75) | 0.001 |
| Demographics | ||
| Male sex | 0.93 (0.89 – 0.98) | 0.006 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 1.11 (0.78 – 1.57) | 0.578 |
| Black/Non-Hispanic | 1.45 (1.24 – 1.70) | <0.001 |
| Black/Hispanic | 1.44 (0.71 – 2.92) | 0.315 |
| Other/Unknown | 1.72 (1.31 – 2.26) | <0.001 |
| Medical category | ||
| Medical | Ref | |
| Trauma | 0.75 (0.65 – 0.87) | <0.001 |
| Respiratory | 0.79 (0.66 – 0.95) | 0.013 |
| Allergy | 1.25 (0.88 – 1.78) | 0.204 |
| GI/Abdominal | 0.88 (0.74 – 1.04) | 0.128 |
| Cardiac | 0.74 (0.57 – 0.96) | 0.023 |
| Neurology | 0.87 (0.73 – 1.03) | 0.099 |
| Psychiatry | 0.18 (0.14 – 0.23) | <0.001 |
| Toxicology | 2.17 (1.54 – 3.05) | <0.001 |
| Dizziness/Syncope | 0.90 (0.72 – 1.13) | 0.363 |
| Other | 0.31 (0.22 – 0.42) | <0.001 |
| Unknown | 0.42 (0.29 – 0.63) | <0.001 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 1.06 (0.94 – 1.21) | 0.308 |
| 12:00–17:59 | 1.01 (0.89 – 1.16) | 0.795 |
| 18:00–23:59 | 1.09 (0.98 – 1.21) | 0.132 |
| Year | ||
| 2013 | Ref | |
| 2014 | 0.77 (0.64 – 0.94) | 0.009 |
| 2015 | 0.70 (0.53 – 0.92) | 0.009 |
| 2016 | 0.72 (0.54 – 0.96) | 0.027 |
| Response Characteristics | ||
| Advanced Life Support | 3.09 (2.23 – 4.28) | <0.001 |
| Lights and sirens use | 1.20 (0.95 – 1.52) | 0.129 |
| Response time | 1.00 (0.98 – 1.01) | 0.652 |
| Scene time | 0.99 (0.99 – 1.00) | 0.034 |
| Transport time | 1.00 (0.99 – 1.01) | 0.408 |
| Intravenous Access | 2.80 (1.95 – 4.03) | <0.001 |
| Monitor placed | 1.79 (1.31 – 2.44) | <0.001 |
| Glasgow Coma Score assessment | 1.13 (1.11 – 1.16) | <0.001 |
OR, odds ratio; CI, confidence interval
Table 13:
Odds ratios of complete vital sign assessment following adjustment of standard error for clusters in 20 EMS agencies evaluated in this study; unadjusted (univariate) analysis.
| OR (95% CI) | p | |
|---|---|---|
| Age Group | ||
| Adult | Ref | |
| Neonate | 0.02 (0.01 – 0.06) | <0.001 |
| Infant | 0.05 (0.02 – 0.11) | <0.001 |
| Toddler | 0.08 (0.04 – 0.16) | <0.001 |
| Early childhood | 0.16 (0.09 – 0.28) | <0.001 |
| Middle childhood | 0.47 (0.34 – 0.64) | <0.001 |
| Adolescent | 1.11 (0.92 – 1.36) | 0.276 |
| Demographics | ||
| Male sex | 0.87 (0.80 – 0.95) | 0.002 |
| Height (inches) | 1.08 (1.05 – 1.11) | <0.001 |
| Weight (kg) | 1.01 (1.00 – 1.02) | 0.032 |
| Race/ethnicity | ||
| White/Non-Hispanic | Ref | |
| White/Hispanic | 1.00 (0.66 – 1.52) | 0.989 |
| Black/Non-Hispanic | 1.16 (0.57 – 2.38) | 0.680 |
| Black/Hispanic | 1.16 (0.44 – 3.09) | 0.760 |
| Other/Unknown | 1.45 (0.50 – 4.26) | 0.497 |
| Medical category | ||
| Medical | Ref | |
| Trauma | 0.79 (0.48 – 1.31) | 0.368 |
| Respiratory | 1.04 (0.61 – 1.78) | 0.880 |
| Allergy | 1.13 (0.76 – 1.68) | 0.547 |
| GI/Abdominal | 1.27 (0.79 – 2.06) | 0.325 |
| Cardiac | 2.45 (1.27 – 4.75) | 0.008 |
| Neurology | 1.23 (0.64 – 2.34) | 0.532 |
| Psychiatry | 0.19 (0.09 – 0.40) | <0.001 |
| Toxicology | 2.97 (1.58 – 5.61) | 0.001 |
| Dizziness/Syncope | 1.98 (0.98 – 3.96) | 0.054 |
| Other | 0.23 (0.09 – 0.58) | 0.002 |
| Unknown | 0.26 (0.09 – 0.77) | 0.015 |
| Day Period | ||
| 00:00–05:59 | Ref | |
| 06:00–11:59 | 1.03 (0.76 – 1.41) | 0.832 |
| 12:00–17:59 | 0.93 (0.70 – 1.251 | 0.650 |
| 18:00–23:59 | 0.99 (0.87 – 1.12) | 0.852 |
| Year | ||
| 2013 | Ref | |
| 2014 | 0.84 (0.71 – 1.00) | 0.048 |
| 2015 | 0.78 (0.54 – 1.12) | 0.184 |
| 2016 | 0.81 (0.57 – 1.16) | 0.257 |
| Response Characteristics | ||
| Advanced Life Support | 5.74 (2.02 – 16.3) | 0.001 |
| Lights and sirens use | 1.60 (0.83 – 3.07) | 0.166 |
| Mileage | 1.00 (1.00 – 1.00) | 0.234 |
| Response time | 0.98 (0.94 – 1.02) | 0.346 |
| Scene time | 1.01 (0.99 – 1.04) | 0.358 |
| Transport time | 0.99 (0.97 – 1.01) | 0.273 |
| Intravenous Access | 6.02 (3.87 – 9.38) | <0.001 |
| Monitor placed | 3.99 (2.79 – 5.70) | <0.001 |
| Glasgow Coma Score assessment | 4.04 (2.00 – 8.14) | <0.001 |
OR, odds ratio; CI, confidence interval
Funding Source:
Dr. Elmer’s research time is supported by the NIH through grant 1K23NS097629.
Footnotes
Publisher's Disclaimer: This PDF receipt will be used only as the basis for generating PubMed Central (PMC) documents and will not appear on PMC. The PMC-ready documents will be made available for review after conversion. Any necessary corrections can be made at that time. No materials will be released to PMC without the Reviewer’s approval.
Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
References:
- [1].Tsai A, Kallsen G. Epidemiology of pediatric prehospital care. Ann Emerg Med. 1987;16:284–92. [DOI] [PubMed] [Google Scholar]
- [2].Seidel JS, Hornbein M, Yoshiyama K, Kuznets D, Finklestein JZ, St Geme JW Jr.. Emergency medical services and the pediatric patient: are the needs being met? Pediatrics. 1984;73:769–72. [PubMed] [Google Scholar]
- [3].Shah MN, Cushman JT, Davis CO, Bazarian JJ, Auinger P, Friedman B. The epidemiology of emergency medical services use by children: an analysis of the National Hospital Ambulatory Medical Care Survey. Prehosp Emerg Care. 2008;12:269–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Fleischman RJ, Yarris LM, Curry MT, Yuen SC, Breon AR, Meckler GD. Pediatric educational needs assessment for urban and rural emergency medical technicians. Pediatr Emerg Care. 2011;27:1130–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Brown SA, Hayden TC, Randell KA, Rappaport L, Stevenson MD, Kim IK. Improving Pediatric Education for Emergency Medical Services Providers: A Qualitative Study. Prehosp Disaster Med. 2017;32:20–6. [DOI] [PubMed] [Google Scholar]
- [6].Zebrack M, Dandoy C, Hansen K, Scaife E, Mann NC, Bratton SL. Early resuscitation of children with moderate-to-severe traumatic brain injury. Pediatrics. 2009;124:56–64. [DOI] [PubMed] [Google Scholar]
- [7].Joyce SM, Brown DE, Nelson EA. Epidemiology of pediatric EMS practice: a multistate analysis. Prehosp Disaster Med. 1996;11:180–7. [DOI] [PubMed] [Google Scholar]
- [8].Hewes H, Hunsaker S, Christensen M, Whitney J, Dalrymple T, Taillac P. Documentation of pediatric vital signs by EMS providers over time. J Pediatr Surg. 2016;51:329–32. [DOI] [PubMed] [Google Scholar]
- [9].Lerner EB, Drendel AL, Cushman JT, Badawy M, Shah MN, Guse CE, et al. Ability of the Physiologic Criteria of the Field Triage Guidelines to Identify Children Who Need the Resources of a Trauma Center. Prehosp Emerg Care. 2017;21:180–4. [DOI] [PubMed] [Google Scholar]
- [10].Drayna PC, Browne LR, Guse CE, Brousseau DC, Lerner EB. Prehospital Pediatric Care: 2015;19:441–7. [DOI] [PubMed] [Google Scholar]
- [11].Diggs LA, Sheth-Chandra M, De Leo G. Epidemiology of Pediatric Prehospital Basic Life Support Care in the United States. Prehosp Emerg Care. 2016;20:230–8. [DOI] [PubMed] [Google Scholar]
- [12].Gausche-Hill M, Brown KM, Oliver ZJ, Sasson C, Dayan PS, Eschmann NM, et al. An Evidencebased Guideline for prehospital analgesia in trauma. Prehosp Emerg Care. 2014;18 Suppl 1:25–34. [DOI] [PubMed] [Google Scholar]
- [13].Murdock TC, Knapp JF, Dowd MD, Campbell JP. Bridging the emergency medical services for children information gap. Arch Pediatr Adolesc Med. 1999;153:281–5. [DOI] [PubMed] [Google Scholar]
- [14].Foltin GL, Pon S, Tunik M, Fierman A, Dreyer B, Cooper A, et al. Pediatric ambulance utilization in a large American city: a systems analysis approach. Pediatr Emerg Care. 1998;14:254–8. [DOI] [PubMed] [Google Scholar]
- [15].Glaeser PW, Linzer J, Tunik MG, Henderson DP, Ball J. Survey of nationally registered emergency medical services providers: pediatric education. Ann Emerg Med. 2000;36:33–8. [DOI] [PubMed] [Google Scholar]


