Abstract
Background
Compared with similarly injured patients of a younger age, elderly patients have worse outcomes from acute injury. One factor adversely affecting outcomes is sarcopenia, which has been assessed in healthy elderly populations through established clinical and radiological criteria. However, in the acute care setting, no such criteria have been established. Sarcopenia has been opportunistically assessed via radiographic means but there is as of yet no gold standard. The purpose of this review is to summarize the radiological methods used to diagnose sarcopenia in the acute care setting, and suggest ways in which these methods may lead to a consensus definition of sarcopenia and its relationship to patient outcomes.
Methods
A systematic survey of medical databases was conducted, with 902 unique publications identified. After screening and application of inclusion and exclusion criteria, data regarding study population, outcome, imaging modality, and criteria for assessment of sarcopenia were extracted from 20 studies. Quality was assessed with the Newcastle-Ottawa Scale.
Results
CT was the imaging modality for 18 of the studies, with total psoas muscle cross-sectional area at the level of L3 and L4 being the dominant method for assessing sarcopenia. Adjustment for body morphology most commonly used patient height or L4 vertebral body area. The majority of articles found radiographically assessed sarcopenia to be significantly correlated to outcomes such as mortality, length of hospital stay, morbidity, and in-hospital complications
Conclusions
Establishing a consistent definition would strengthen its applicability and generalizability to admission and discharge planning.
Level of evidence
Systematic review, level III.
Background
Elderly patients suffering from a broad range of traumatic injuries have worse outcomes than younger patients with similar injury.1 2 One factor adversely affecting outcomes in ageing populations is sarcopenia.3 Sarcopenia is characterized by loss of skeletal muscle, decreased muscle strength and low physical performance.4 It has been demonstrated that the presence of sarcopenia is a marker for poor outcome in the elderly with a critical illness5 or traumatic injury.6 7 These patients therefore may require modification and personalization of care and interventions to counteract the increased likelihood of adverse health events.8 Consequently, identification, measurement, and stratification of sarcopenia in this population early in the course of clinical care can be beneficial in guiding clinical decision-making.8 Although it is acknowledged that sarcopenia plays a role in patient outcomes in the setting of trauma, there is no uniform, established method of measuring it, nor any consensus on practical application.
There are a number of existing sarcopenia assessment tools in the healthy elderly population. The European Working Group on Sarcopenia in Older People (EWGSOP) recently published a framework for diagnosing the elderly with sarcopenia.8 Their diagnostic algorithm in stepwise order includes a clinical questionnaire, muscle strength test, muscle quantity or quality test, and a physical performance test. The ESPEN Special Interest Group uses muscle mass and walking speed as the main criteria for a diagnosis of sarcopenia.9 Although such methods are available when assessing healthy elderly patients, many cannot be readily applied at the time of presentation in those with traumatic injury. This leaves muscle quantity or quality measurement through radiological imaging the only reliable assessment available in the acute setting.
Currently, there are several modalities to measure muscle quantity and quality. Appendicular skeletal muscle mass (ASMM) may be measured through dual-energy X-ray absorptiometry (DXA),10 whole-body skeletal muscle mass may be predicted by bioelectrical impedance analysis (BIA),11 12 and specific muscle cross-sectional area (CSA) or volume can be measured through CT or MRI.10 13 Of these assessments, only ASMM measured through DXA or BIA has established cut-off points for diagnosis of sarcopenia in the EWGSOP’s diagnostic algorithm.14 15 However, BIA is particularly sensitive to hydration status16 so will be potentially confounded when this is changing secondary to hemorrhage, resuscitation and fluid shifts between compartments. MRI and CT are considered to be the gold standard for non-invasive assessment of muscle quantity and mass,11 but there are a variety of stratification points, measurement locations, and methods employed to diagnose sarcopenia. In addition, the impact of demographic factors such as age, sex, body mass index, and ethnicity on specific muscle measurements has not been well explored. Given the wide use and availability of radiological measurement devices, establishment of a single criterion for measurement of sarcopenia in the acute setting could be greatly beneficial in bringing this information to bear on the clinical care of elderly patients. This review will therefore summarize the radiological methods that have been used to diagnose sarcopenia in the setting of trauma, and suggest ways in which these methods may lead to a consensus definition of sarcopenia and its role in patient outcomes.
Objectives
The objectives of this systematic review are: to summarize the current methods and outcomes associated with radiographically assessed sarcopenia in the setting of traumatic injury, to highlight areas of consensus and disagreement among researchers, and to propose directions for future research.
Methods
Research questions
This systematic review focuses on the radiographic evaluation of muscle mass as an indicator of potential pre-existing sarcopenia, in the setting of trauma, guided by the following research questions. First, what population are study subjects drawn from, with particular focus on inclusion criteria used. Second, what imaging modalities were used in the assessment of sarcopenia. Third, what were the criteria on which an assessment of sarcopenia was made and, finally, what was the reported relationship between sarcopenia and the outcomes of interest to investigators, specifically mortality, length of hospital stay, morbidity, in-hospital complications, and independence after discharge.
Search strategy
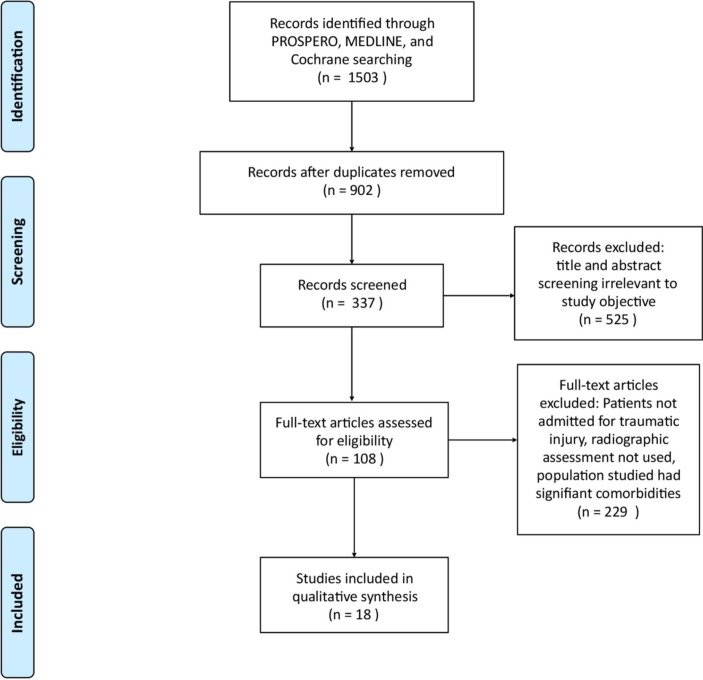
The following databases were searched for relevant studies: PROSPERO, MEDLINE, and Cochrane Central Register of Controlled Trials. Searches were conducted between January 17 and 30, 2019. The search strategy used keywords identified by the authors, informed by the results of a preliminary probing search, to capture published articles which addressed the concept of radiographically defined sarcopenia in the acute care setting. Search queries included combinations of the following sets of terms: ‘sarcopenia’, ‘iliopsoas’, ‘psoas’, ‘psoas major’, ‘trauma’, ‘acute care’, ‘imaging’, ‘measure’, and ‘radiographic’. Search results were limited to studies published in or translated to English on or after January 1, 1999. A total of 902 unique records were collected, after removal of duplicate articles. The flowchart of the article selection pathway is shown in figure 1.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram illustrating article selection. Source: Moher et al31
Inclusion criteria
Inclusion criteria were established prior to the literature search. Studies reporting the prevalence of radiographically defined sarcopenia and its association with outcomes in adult patients (>18 years of age) admitted after traumatic injury were sought. Studies were included if the radiographic studies used to assess sarcopenia were performed at admission or within the 72 hours after admission.
Exclusion criteria
Studies which did not specify the timing of the imaging studies relative to admission, or studies in which the patient population was not assessed in the acute care setting, were excluded. Studies published in languages other than English were also excluded, as were studies published prior to January 1, 1999.
Study selection
Duplicates were removed from the initial collection of records, after which investigators independently screened articles. The full texts of articles meeting inclusion criteria were independently reviewed for relevance to the research questions.
Data extraction
Data extraction was performed independently by two investigators (CEC, DMZ). Extracted data included study type, publication year, sample size, sex (%male), age, population, criteria for inclusion, timing of imaging, imaging modality, blinding of image assessor, muscles assessed, anatomic references used to assess muscles, muscle characteristics assessed, any adjustment for body morphology, criteria for sarcopenia, and relation of sarcopenia to outcome.
Quality assessment
The Newcastle-Ottawa Scale (NOS) is a tool for assessing the quality of non-randomized studies. For this review, the NOS permitted a consistent evaluation of each included study based on study group selection, comparability, and outcome.
Results
Measurement of the total CSA of the psoas via CT was the imaging modality of choice for the majority of the studies included in analysis. The L3 vertebral body was the most common anatomic landmark identified as a reference point, with patient height most commonly used for normalization of psoas CSA. With two exceptions, definitions of sarcopenia were made relative to the distribution of adjusted psoas CSA in the population studied, and the outcome most frequently explored by researchers was mortality.
Study quality
Each source included for analysis was evaluated for the selection of study groups, comparability of the groups, and assessment of outcome using the NOS. None of the studies specified whether patients in their study population had a history of sarcopenia, and there was variable comparability across studies regarding comparability of cohorts, but otherwise each study rated highly on the NOS (see online supplementary digital content 1).
tsaco-2019-000414supp001.pdf (673.4KB, pdf)
Study population characteristics
A total of 18 studies were included in the analysis, of which 17 were retrospective and the remaining study was prospective. Sample size varied widely, with the greatest sample size having 23 622 patients and the smallest having 16. Average age, gender ratio, and country of origin are shown in table 1. Populations included in studies were, on average, 55% male, with a mean age of 69 years. The average minimum age for inclusion across all studies was 54 years. The majority of studies included for review drew from North American cohorts, with a handful of other nationalities represented, including Italian, Australian, and Japanese.
Table 1.
Study population characteristics
| First author | Year | Study design | Sample size | Gender (%male) | Age (mean) | Population | Criteria for inclusion |
| Akahoshi22 | 2016 | Retrospective | 84 | 56 | 47.2 | Japanese | Age >20; not DOA; blunt force trauma |
| Chang21 | 2018 | Retrospective | 91 | 26 | 81.1 | American | Age >50; proximal femur fracture undergoing surgical repair |
| Couch32 | 2018 | Retrospective | 225 | 55 | 76.9 | Australian | Age >65; Injury Severity Score (ISS) >12 |
| DeAndrade33 | 2018 | Retrospective | 778 | 71 | 63 and 42 | American | Presented as a trauma alert at a single institution from 2012 to 2014 |
| Deren25 | 2017 | Retrospective | 99 | 62 | 74.3 | American | Age ≥60; Rhode Island Hospital Trauma Database; closed acetabular fracture |
| Ebbeling23 | 2014 | Retrospective | 180 | 57 | 74 | American | Age >55 years; ISS>15; and ICU LOS>48 hours; captured in Pennsylvania Trauma Outcomes Study (PTOS) |
| Fairchild19 | 2015 | Retrospective | 252 | 49 | 76 | American | Age >65; no TBI/SCI; admitted to level 1 trauma center in Milwaukee, WI, between January 2008 and April 2011 |
| Hida17 | 2016 | Retrospective; cross-sectional | 216 (OVF); 1608 (NF) | 0 | 79.9 (OVF); 69.1 (NF) | Japanese | Women ≥55 admitted to single hospital with osteoporotic vertebral fracture (OVF); (NF) consecutive female outpatients who underwent DXA during study period (June 2002 to January 2009) |
| Hu34 | 2018 | Retrospective | 108 | 73 | 67.4 | American | Age ≥55; all patients admitted to the trauma service of a single university hospital (level 1 trauma center); TBI |
| Kaplan18 | 2017 | Retrospective Cohort | 450 | 60 | Stratified by age, not specified | American | Age ≥65 years; admitted to the ICU of a single institution from January 2011 to May 2014 after traumatic injury |
| Leeper6 | 2016 | Retrospective | 23 622 | 61.70 | Stratified by age, not specified | American | Age ≥18 or older; level 1 or level 2 trauma alert; availability of at least 6 months of follow-up data |
| Lisiecki35 | 2013 | Retrospective | 16 | 75 | 47.1 | American | Age between 18 and 99 years old; mandible fracture; treated in initial hospital stay; GCS score of 14–15 |
| Malekpour26 | 2017 | Retrospective | 1175 | 51 | 78.17 | American | Age >65; blunt trauma; abdominal CT |
| Mccusker36 | 2018 | Retrospective | 325 | 64 | 76 | American | Age ≥65 years; trauma patients admitted to level 1 trauma center |
| Mitchell37 | 2018 | Retrospective | 146 | 73 | 70.1 | American | Age >60 with acetabular fractures treated at institution during a 12-year period |
| Oskutis38 | 2016 | Retrospective | 202 | 41 | 58.5 | American | Age >40; postcrash admission to a trauma center; single injury or Maximum Abbreviated Injury Scale (MAIS) score ≥3 |
| Shibahashi24 | 2017 | Retrospective | 74 | 72 | 74 | Japanese | Age ≥60 years; TBI; admitted to the intensive care unit between September 2013 and September 2015 |
| Touban20 | 2019 | Retrospective | 558 | 46 | 76.65 | American | Age >65 years; evaluation with abdominal and/or pelvic CT; orthopedic injury |
DOA, Dead On Arrival; DXA, dual-energy X-ray absorptiometry; GCS, Glasgow Coma Scale; ICU, intensive care unit; LOS, length of stay; NF, Non-fracture; SCI, Spinal Cord Injury; TBI, traumatic brain injury.
Imaging modalities
Imaging was undertaken in all studies at the time of admission, with a minority of studies specifying the window of time (eg, <1 hour after arrival). CT was the imaging modality for 17 of the studies included, with DXA used in one study. The blinding of the image assessors was specified in only five studies, of which blinding was present in three.
Of the 17 studies which used CT imaging modalities, the psoas was the dominant muscle group, assessed in 11 studies. Of those, two studies assessed additional muscles, such as paraspinal muscles (quadratus lumborum, erector spinae). Total skeletal muscle CSA at the level of the anatomic reference was used in four studies, and muscles of mastication (masseter, temporalis) in two studies. Finally, DXA imaging modalities assessed upper and lower extremity muscle mass.
Anatomic reference points
Anatomic reference points used for CT imaging modalities focused on the L3 and L4 vertebral level, as described in table 2. Nine studies assessed muscles via axial slices determined by the features of the L3 vertebrae, with three studies explicitly specifying the level (eg, caudal end), and four studies following similar methodology at the L4 vertebrae. Two studies assessed muscles at the level of an intervertebral disc; one at L3-L4 and one at L4-L5. Due to the nature of the DXA scan, no anatomic reference points were used for muscle assessment.
Table 2.
Anatomic reference points for CT imaging modalities
| Vertebral level | Further specification | Studies, n |
| L3 axial slice | 9 | |
| Not specified | 6 | |
| Superior aspect | 2 | |
| Inferior aspect | 1 | |
| L3-L4 disc | 1 | |
| Superior aspect | 1 | |
| L4 | 4 | |
| Not specified | 1 | |
| Inferior aspect | 3 | |
| L4-L5 disc | 1 | |
| Not specified | 1 | |
| Other | 2 | |
| Superior orbital rim, external meatus, mandibular coronoid process | 1 | |
| 2 cm below zygomatic arch | 1 | |
Assessment of sarcopenia
The assessment of sarcopenia in each study was predicated on characteristics of the muscles assessed, with or without adjustment for body morphology, as described in table 3. The majority of studies used skeletal muscle index (SMI) of the psoas, which normalizes the CSA of the muscles of interest against the height of the patient. Four studies assessed the CSA of the psoas without adjustment for body morphology, with one study assessing the CSA of the masseter. Other metrics included the psoas:lumbar vertebral index (computed as the ratio between the mean CSAs of the psoas muscles and the L4 vertebral body at the level of the L4 pedicles17 and muscle volume of the temporalis), used in one study each. ASMM-to-height ratio was used with DXA analysis.
Table 3.
Assessment of sarcopenia
| Muscle characteristics assessed | Morphology adjustment | Studies, n |
| Skeletal muscle index (SMI; cm2/m2) |
Height | 8 |
| Cross-sectional area (CSA; cm2) |
None | 7 |
| Appendicular skeletal muscle mass (ASMM)-to-height ratio (kg/m2) | Height | 1 |
| Psoas:lumbar vertebral index | L4 vertebral body area | 1 |
| Thickness, area, volume | None | 1 |
ASMM, appendicular skeletal muscle mass; CSA, cross-sectional area; SMI, skeletal muscle index.
Definition of sarcopenia
The most common method of defining sarcopenia was to establish a threshold intrinsic to the study cohort, as shown in table 4. For example, patients with sarcopenia were those with a CSA below the study population median, or 1 SD from the sex-based mean. Four studies defined sarcopenia as the lowest quartile of the CSA or SMI of the study population. Six studies used a threshold extrinsic to the cohort by using gender-specific reference values for sarcopenia taken from other publications. One study compared measured to estimated CSA to define sarcopenia. Four studies did not explicitly state their cut-off points. Detailed descriptions of the specific cut-off values in the diagnosis of sarcopenia can be found in table 4.
Table 4.
Sarcopenia definition
| Sarcopenia threshold | Relation | Studies, n |
| Intrinsic to cohort | 10 | |
| Lowest quartile for gender | 4 | |
| Below median | 2 | |
| Below sex-based mean | 1 | |
| 5th percentile for gender | 1 | |
| <80% of estimated CSA | 1 | |
| Below optimal sex-specific cut-off point established by analysis | 1 | |
| Extrinsic to cohort | 4 | |
| SMI<38.5 cm2/m2 in women (<52.4 cm2/m2 in men) 39 | 2 | |
| ASMM:height ratio <5.46 kg/m220 | 1 | |
| SMI<4 cm2/m2 | 1 | |
| Not specified | 4 |
ASMM, appendicular skeletal muscle mass; CSA, cross-sectional area; SMI, skeletal muscle index.
Sarcopenia and outcomes
Within the 18 studies, there were five outcomes of interest described: mortality, length of stay, morbidity, in-hospital complications, and independence after discharge (online supplementary digital content 2). Mortality was the most common outcome measured, with 11 studies investigating the association between mortality and sarcopenia. Nine of those studies found that sarcopenia status was correlated to increased patient mortality. There was a wide range of timeframes for mortality measured, with 30-day, 90-day, 6-month, and 1-year mortality all being assessed.
There were six articles that examined the association between length of stay in hospital and sarcopenia, five of which reported a significant correlation between sarcopenia and increased length of stay, and one study which reported no association.
Four articles studied the relationship between morbidity and sarcopenia, all of which suggested a correlation between the sarcopenia status and increased likelihood of various morbidities. Patients with sarcopenia had a higher rate of osteoporotic vertebral fractures,18 low-energy acetabular fractures,19 sustaining a severe thoracic injury from a motor vehicle collision,20 and medical complications such as pneumonia, liver failure, renal failure, and sepsis.17
Two of the four studies which analyzed the relationship between sarcopenia and in-hospital complications found that sarcopenia status was predictive of increased complication rates, whereas the other two studies did not find any relationship. In-hospital complications included adverse events related to respiratory, cardiovascular, infectious, hematological, or renal function.
One study analyzed elderly patient independent living post-traumatic injury and found that sarcopenia status prior to hospital admission was correlated with reduced independence.
As some studies reported multiple outcomes, there were a total of 26 sarcopenia/outcome relationships described within the 18 articles. In total, there were 19 instances of sarcopenia being related to outcome reported with five reporting no correlation. These five reports of no correlation came from three articles, with one article having both correlation and no correlation to outcome reported. For more details, see online supplementary digital content 2.
Discussion
With the exception of two studies which examined muscles of mastication and the study which used DXA imaging modality, there was a majority across studies to define sarcopenia in the acute setting by measuring muscle mass with an axial section of CT imaging at the level of the lumbar spine, with the psoas measured either in isolation or in conjunction with other muscle groups. The anatomic level of the imaging analysis centered around the L3-L4 vertebrae, but there was no clear preference for the exact level. Establishment of a standard anatomic reference site for evaluation of patients for sarcopenia would facilitate future research by removing variation in measurement technique, thereby permitting direct comparison of findings between studies. Based on our findings, we recommend that further investigation into radiographically assessed sarcopenia measure uses CT modalities with caudal end of the L3 vertebrae serving as the anatomic reference point.
SMI was the predominant mode of assessing sarcopenia among the reviewed studies, but there were several variations on this theme to account for morphological features of the patient. Studies like Chang et al21 calculated SMI using lean muscle mass, obtained by setting density thresholds to exclude fatty infiltrate in the imaging software used to calculate CSA. A more holistic approach was taken by Leeper et al, normalizing psoas CSA using a calculated value for body surface area (BSA).6 Akahoshi et al similarly used calculated BSA to generate an estimate for psoas CSA, and defined sarcopenia as a difference between estimate and actual psoas CSA.22
It is clear that muscle CSA alone is not sufficient to define sarcopenia, but exactly how to account for body morphology remains an area for future research. However this is done should be practical for the patient who is acutely ill. The majority of the studies reviewed in this article used height, and as such we recommend that future studies account for patient morphology using patient height. However, Ebbeling et al23 normalized psoas CSA against the CSA of the vertebral body, which has the benefit of being measured accurately and contemporaneously to psoas CSA, rather than a previously recorded height.
The definition of a sarcopenia threshold for nine of the studies was made in relation to the cohort studied, whereas five studies set the sarcopenic threshold using values obtained from other publications. Both intrinsically and extrinsically defined sarcopenic thresholds deserve close scrutiny, while acknowledging that a true reference standard is not possible until normative population data are available.
An intrinsically defined sarcopenia threshold suffers from a reduced ability to generalize findings, as the portion of the study population arbitrarily defined as sarcopenic may not be representative of the wider sarcopenic population. The best example of this is Shibahashi et al,24 where the sarcopenia cut-off value was established using a best fit analysis in which sarcopenic status reflected worse patient outcomes.
By contrast, an extrinsically defined sarcopenia threshold faces scrutiny as to the similarity between the study population and the populations for which those thresholds have been established. Both Deren et al25 and Kaplan et al18 used sarcopenia cut-off values from a 2008 study by Prado et al, which examined sarcopenic obesity in patients with solid tumors of the respiratory and gastrointestinal tract.8 26 27
The majority of the studies reviewed found a correlation between sarcopenia and outcome, despite a wide variability in methods used to measure sarcopenia as well as populations sampled. In total, 16 articles reported the presence of correlation with three reporting no correlation, lending credence to the usefulness of radiographic assessment in predicting the stratification of patient healthcare outcomes. However, clinical adoption of radiographically assessed sarcopenia is predicated on comparison between the patient’s psoas CSA and a normal distribution of psoas CSA which is representative of the population served. Therefore, we recommend further retrospective study using large pools of CT imaging to develop population-specific values for the mean and normal distribution of psoas CSA based on patient demographic factors such as age and sex.
The three studies, by Couch, Ebbeling, and Mccusker, that found no correlation between sarcopenia and measured outcomes had a few shared characteristics. All three studies were retrospective in nature and were performed in Western countries. All three had reasonable sample sizes with 225, 180, and 325, respectively. All three also had a very similar mean age and percentage of male participants, with the mean age of the studies being 76.9, 74 and 76 and the male percentage being 55%, 57%, and 64%. They each used abdominal CT scans to measure the psoas in assessing sarcopenia, although they differed in anatomic references used and muscle characteristics measured.
Couch and Ebbeling both measured the psoas using an axial slice at the L4 inferior aspect of the vertebral body whereas Mccusker measured at the most superior aspect of L3. Couch assessed lean psoas muscle area, Ebbeling measured psoas:lumbar vertebral index, and Mccusker measured total psoas area. In terms of adjustment for body morphology, Couch had none, Ebbeling used L4 vertebral body area and Mccusker used height. Cut-offs for sarcopenia diagnosis varied, with Couch not specifying their criteria, Ebbeling using patients with lower index values compared with cohort median, and Mccusker using the lowest quartile of total psoas CSA. It is not clear if these differences in methodology could account for the shared findings of no correlation between sarcopenia and outcome in these three studies.
There were some limitations to this review. First, most of the studies were performed in Western and English-speaking countries and examined trauma populations, all factors which limit the generalizability of conclusions drawn from such a narrow population. As the purpose of this review was to critically assess radiological measurement of muscle mass as an indicator sarcopenia in the setting of traumatic injury, other methods for diagnosing sarcopenia and non-acute settings were excluded. Furthermore, the results presented would carry more weight were this study conducted as a meta-analysis. However, a meta-analysis was not considered appropriate at this time due to the heterogeneity of method, classifications, and outcomes measured in the published literature.
We also must consider that sarcopenia largely affects the elderly, a population with more comorbidities and, given the opportunistic nature of data collection in the acute care setting, it is not possible to determine if patients included in each study were otherwise healthy prior to the event which resulted in their presentation for medical care. Any unknown or unlisted comorbidities at the time of patient presentation would confound assessment of sarcopenia status as well as outcome, increasing the apparent incidence of sarcopenia in the population studied, while also potentially artificially inflating any relationship between sarcopenia and morbidity or mortality. Finally, there is a bias against publication of research which does not demonstrate a significant relationship between an exposure and an outcome of interest, thus the association between sarcopenia and clinical outcomes may be weaker than the current literature suggests.
As previously noted, radiographic assessment of features like psoas CSA is a surrogate for total muscle mass, which is only one of several elements used in current clinical definitions of sarcopenia, such as the EWGSOP.28 The degree to which radiographic assessments of sarcopenia alone align with clinical definitions has not been clearly established. This is also a direction which we recommend future research focuses on, to clarify the association between clinical and radiographic assessments of sarcopenia.
Of note, the demographic characteristics and outcomes of patients with sarcopenia broadly parallel outcomes seen with the syndrome of frailty, with most frail patients exhibiting some evidence of sarcopenia.29 Although a uniform definition of frailty has yet to emerge, it has come to be recognized as a syndrome broadly characterized by diminished strength, endurance, and reduced physiologic function that thereby increases a person’s vulnerability for developing increased dependency and/or death.30 Although the Trauma-Specific Frailty Index has been used to predict discharge disposition in geriatric patients, it is limited by the requirement of a reliable historian who is able to answer lifestyle questions.30 Thus, in both frailty and sarcopenia, there remains a need for an assessment method for elderly patients who are acutely ill, whose condition may prevent full and accurate assessment using many of the current assessment tools. Radiographic measurements, despite their limitations, offer a first approximation of sarcopenia and the associated syndrome of frailty, and have demonstrated potential to inform admissions and care planning.
Establishing a standardized process for the radiographic assessment of sarcopenia is crucial to any deeper understanding of sarcopenia and its utility as a predictive marker in the clinical space. Further studies to elucidate the ideal measurement process are therefore needed, as it is still unclear which anatomic reference points, muscle characteristics, and body morphology adjustments are most salient. Additionally, there is still a wide variance in the criteria for the acute diagnosis of sarcopenia. Therefore, it would be useful to obtain a normative age and sex-adjusted data curve from a healthy adult population to establish both a uniform diagnostic threshold and methodology for the assessment of sarcopenia.
The majority of the articles analyzed in this review suggested a correlation between sarcopenia and outcomes such as morbidity, mortality, and complications. Taking this relationship into account, assessment of the effects of incorporating radiographic assessment of sarcopenia into patient management plan is needed. Furthermore, a consistent definition of sarcopenia strengthens its applicability to clinical care and ideally contributes to the optimization of hospital resource allocation. Establishing a consistent definition of radiographic sarcopenia also paves the way for future clinical trials to stratify acutely ill populations by degree of sarcopenia, which could increase the predictive capability of this measure, and by extension the strength of recommendations for therapy for these patients.
Footnotes
Contributors: All authors developed the protocol from the original idea from MJM. DMZ and CEC extracted the relevant literature from the search and all authors analyzed the data and wrote the article draft.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kuhne CA, Ruchholtz S, Kaiser GM, Nast-Kolb D. Mortality in severely injured elderly trauma Patients—When does age become a risk factor? World J Surg 2005;29:1476–82. 10.1007/s00268-005-7796-y [DOI] [PubMed] [Google Scholar]
- 2.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013;381:752–62. 10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Du Y, Karvellas CJ, Baracos V, Williams DC, Khadaroo RG. Sarcopenia is a predictor of outcomes in very elderly patients undergoing emergency surgery. Surgery 2014;156:521–7. 10.1016/j.surg.2014.04.027 [DOI] [PubMed] [Google Scholar]
- 4.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel J-P, Rolland Y, Schneider SM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working group on sarcopenia in older people. Age Ageing 2010;39:412–23. 10.1093/ageing/afq034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanna JS. Sarcopenia and critical illness. Journal of Parenteral and Enteral Nutrition 2015;39:273–81. 10.1177/0148607114567710 [DOI] [PubMed] [Google Scholar]
- 6.Leeper CM, Lin E, Hoffman M, Fombona A, Zhou T, Kutcher M, Rosengart M, Watson G, Billiar T, Peitzman A, et al. Computed tomography abbreviated assessment of sarcopenia following trauma. J Trauma Acute Care Surg 2016;80:805–11. 10.1097/TA.0000000000000989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Welch C, K. Hassan-Smith Z, A. Greig C, M. Lord J, A. Jackson T. Acute Sarcopenia Secondary to Hospitalisation - An Emerging Condition Affecting Older Adults. Aging Dis 2018;9:151–64. 10.14336/AD.2017.0315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16–31. 10.1093/ageing/afy169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schweitzer L, Geisler C, Pourhassan M, Braun W, Glüer C-C, Bosy-Westphal A, Müller MJ. What is the best reference site for a single MRI slice to assess whole-body skeletal muscle and adipose tissue volumes in healthy adults? Am J Clin Nutr 2015;102:58–65. 10.3945/ajcn.115.111203 [DOI] [PubMed] [Google Scholar]
- 10.Derstine BA, Holcombe SA, Goulson RL, Ross BE, Wang NC, Sullivan JA, Su GL, Wang SC. Quantifying sarcopenia reference values using lumbar and thoracic muscle areas in a healthy population. J Nutr Health Aging 2017;21:180–5. 10.1007/s12603-017-0983-3 [DOI] [PubMed] [Google Scholar]
- 11.Sergi G, De Rui M, Stubbs B, Veronese N, Manzato E. Measurement of lean body mass using bioelectrical impedance analysis: a consideration of the pros and cons. Aging Clin Exp Res 2017;29:591–7. 10.1007/s40520-016-0622-6 [DOI] [PubMed] [Google Scholar]
- 12.Maden-Wilkinson TM, Degens H, Jones DA, McPhee JS. Comparison of MRI and DXA to measure muscle size and age-related atrophy in thigh muscles. J Musculoskelet Neuronal Interact 2013;13:320–8. [PubMed] [Google Scholar]
- 13.van der Werf A, Langius JAE, de van der Schueren MAE, Nurmohamed SA, van der Pant KAMI, Blauwhoff-Buskermolen S, Wierdsma NJ. Percentiles for skeletal muscle index, area and radiation attenuation based on computed tomography imaging in a healthy Caucasian population. Eur J Clin Nutr 2018;72:288–96. 10.1038/s41430-017-0034-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, Ferrucci L, Guralnik JM, Fragala MS, Kenny AM, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 2014;69:547–58. 10.1093/gerona/glu010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gould H, Brennan SL, Kotowicz MA, Nicholson GC, Pasco JA. Total and appendicular lean mass reference ranges for Australian men and women: the Geelong osteoporosis study. Calcif Tissue Int 2014;94:363–72. 10.1007/s00223-013-9830-7 [DOI] [PubMed] [Google Scholar]
- 16.Beaudart C, McCloskey E, Bruyère O, Cesari M, Rolland Y, Rizzoli R, Araujo de Carvalho I, Amuthavalli Thiyagarajan J, Bautmans I, Bertière M-C, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr 2016;16:170 10.1186/s12877-016-0349-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hida T, Shimokata H, Sakai Y, Ito S, Matsui Y, Takemura M, Kasai T, Ishiguro N, Harada A. Sarcopenia and sarcopenic leg as potential risk factors for acute osteoporotic vertebral fracture among older women. Eur Spine J 2016;25:3424–31. 10.1007/s00586-015-3805-5 [DOI] [PubMed] [Google Scholar]
- 18.Kaplan SJ, Pham TN, Arbabi S, Gross JA, Damodarasamy M, Bentov I, Taitsman LA, Mitchell SH, Reed MJ. Association of radiologic indicators of frailty with 1-year mortality in older trauma patients: opportunistic screening for sarcopenia and osteopenia. JAMA Surg 2017;152:e164604 10.1001/jamasurg.2016.4604 [DOI] [PubMed] [Google Scholar]
- 19.Fairchild B, Webb TP, Xiang Q, Tarima S, Brasel KJ. Sarcopenia and frailty in elderly trauma patients. World J Surg 2015;39:373–9. 10.1007/s00268-014-2785-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Touban BM, Pavlesen S, Smoak JB, Sayegh MJ, Wang J, Zhao J, Anders MJ. Decreased lean psoas cross-sectional area is associated with increased 1-year all-cause mortality in male elderly orthopaedic trauma patients. J Orthop Trauma 2019;33:e1–7. 10.1097/BOT.0000000000001331 [DOI] [PubMed] [Google Scholar]
- 21.Chang C-D, Wu JS, Mhuircheartaigh JN, Hochman MG, Rodriguez EK, Appleton PT, Mcmahon CJ. Effect of sarcopenia on clinical and surgical outcome in elderly patients with proximal femur fractures. Skeletal Radiol 2018;47:771–7. 10.1007/s00256-017-2848-6 [DOI] [PubMed] [Google Scholar]
- 22.Akahoshi T, Yasuda M, Momii K, Kubota K, Shono Y, Kaku N, Tokuda K, Nagata T, Yoshizumi T, Shirabe K, et al. Sarcopenia is a predictive factor for prolonged intensive care unit stays in high-energy blunt trauma patients. Acute Med Surg 2016;3:326–31. 10.1002/ams2.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ebbeling L, Grabo DJ, Shashaty M, Dua R, Sonnad SS, Sims CA, Pascual JL, Schwab CW, Holena DN. Psoas:lumbar vertebra index: central sarcopenia independently predicts morbidity in elderly trauma patients. Eur J Trauma Emerg Surg 2014;40:57–65. 10.1007/s00068-013-0313-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shibahashi K, Sugiyama K, Hoda H, Hamabe Y. Skeletal muscle as a factor contributing to better stratification of older patients with traumatic brain injury: a retrospective cohort study. World Neurosurg 2017;106:589–94. 10.1016/j.wneu.2017.07.025 [DOI] [PubMed] [Google Scholar]
- 25.Deren ME, Babu J, Cohen EM, Machan J, Born CT, Hayda R. Increased mortality in elderly patients with sarcopenia and acetabular fractures. J Bone Joint Surg Am 2017;99:200–6. 10.2106/JBJS.16.00734 [DOI] [PubMed] [Google Scholar]
- 26.Malekpour M, Bridgham K, Jaap K, Erwin R, Widom K, Rapp M, Leonard D, Baro S, Dove J, Hunsinger M, et al. The effect of sarcopenia on outcomes in geriatric blunt trauma. Am Surg 2017;83:1203–8. [PubMed] [Google Scholar]
- 27.Cooper C, Dere W, Evans W, Kanis JA, Rizzoli R, Sayer AA, Sieber CC, Kaufman J-M, Abellan van Kan G, Boonen S, et al. Frailty and sarcopenia: definitions and outcome parameters. Osteoporosis International 2012;23:1839–48. 10.1007/s00198-012-1913-1 [DOI] [PubMed] [Google Scholar]
- 28.Keevil VL, Romero-Ortuno R. Ageing well: a review of sarcopenia and frailty. Proc Nutr Soc 2015;74:337–47. 10.1017/S0029665115002037 [DOI] [PubMed] [Google Scholar]
- 29.Cheung A, Haas B, Ringer TJ, McFarlan A, Wong CL. Canadian study of health and aging clinical frailty scale: does it predict adverse outcomes among geriatric trauma patients? J Am Coll Surg 2017;225:658–65. 10.1016/j.jamcollsurg.2017.08.008 [DOI] [PubMed] [Google Scholar]
- 30.Joseph B, Pandit V, Zangbar B, Kulvatunyou N, Tang A, O'Keeffe T, Green DJ, Vercruysse G, Fain MJ, Friese RS, et al. Validating trauma-specific frailty index for geriatric trauma patients: a prospective analysis. J Am Coll Surg 2014;219:10–17. 10.1016/j.jamcollsurg.2014.03.020 [DOI] [PubMed] [Google Scholar]
- 31.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Couch AP, Ho K, Darwood R, Hsu JM. Lean psoas area does not correlate with clinical outcomes in moderately to severely injured older people. Australas J Ageing 2018;37:E7–11. 10.1111/ajag.12482 [DOI] [PubMed] [Google Scholar]
- 33.DeAndrade J, Pedersen M, Garcia L, Nau P. Sarcopenia is a risk factor for complications and an independent predictor of hospital length of stay in trauma patients. Journal of Surgical Research 2018;221:161–6. 10.1016/j.jss.2017.08.018 [DOI] [PubMed] [Google Scholar]
- 34.Hu P, Uhlich R, White J, Kerby J, Bosarge P. Sarcopenia measured using masseter area predicts early mortality following severe traumatic brain injury. J Neurotrauma 2018;35:2400–6. 10.1089/neu.2017.5422 [DOI] [PubMed] [Google Scholar]
- 35.Lisiecki J, Zhang P, Wang L, Rinkinen J, De La Rosa S, Enchakalody B, Brownley RC, Wang SC, Buchman SR, Levi B, et al. Morphomic measurement of the temporalis muscle and zygomatic bone as novel predictors of hospital-based clinical outcomes in patients with mandible fracture. J Craniofac Surg 2013;24:1577–81. 10.1097/SCS.0b013e3182a12e02 [DOI] [PubMed] [Google Scholar]
- 36.Mccusker A, Khan M, Kulvatunyou N, Zeeshan M, Sakran JV, Hayek H, O'Keeffe T, Hamidi M, Tang A, Joseph B, et al. Sarcopenia defined by a computed tomography estimate of the psoas muscle area does not predict frailty in geriatric trauma patients. Am J Surg 2019;218:261–5. 10.1016/j.amjsurg.2018.07.024 [DOI] [PubMed] [Google Scholar]
- 37.Mitchell PM, Collinge CA, OʼNeill DE, Bible JE, Mir HR. Sarcopenia is predictive of 1-year mortality after acetabular fractures in elderly patients. J Orthop Trauma 2018;32:278–82. 10.1097/BOT.0000000000001159 [DOI] [PubMed] [Google Scholar]
- 38.Oskutis MQ, Lauerman MH, Kufera JA, Shanmuganathan K, Burch C, Kerns T, Ho S, Scalea TM, Stein DM. Are frailty markers associated with serious thoracic and spinal injuries among motor vehicle crash occupants? J Trauma Acute Care Surg 2016;81:156–61. 10.1097/TA.0000000000001065 [DOI] [PubMed] [Google Scholar]
- 39.Prado CMM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, Baracos VE. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 2008;9:629–35. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tsaco-2019-000414supp001.pdf (673.4KB, pdf)