Abstract
Background:
Preoperative computed tomography (CT)-guided coil localization can increase the technical success of video-assisted thoracoscopic surgery (VATS)-guided diagnostic wedge resection of lung nodules relative to cases treated without localization. When multiple lung nodules (MLNs) are to be resected, preoperative localization for each lung nodule is required. The aim of this study was to explore the feasibility, safety, and clinical efficacy of preoperative CT-guided coil localization of MLNs.
Methods:
Between November 2015 and July 2019, 31 patients with MLNs were assessed via CT-guided coil localization followed by VATS-guided wedge resection. Rates of technical success for both the localization and wedge resection procedures, as well as data pertaining to patient complication rates and long-term outcomes were recorded and assessed.
Results:
In total, 68 nodules (average of 2.2 nodules/patient) were localized and resected using this approach. Nodules were unilateral and bilateral in 23 and 8 patients, respectively. The rate of CT-guided coil localization technical success for these nodules was 98.5% (67/68), with a technical success rate of single-stage coil localization on a per-patient basis of 96.8% (30/31). Following localization, asymptomatic pneumothorax occurred in four patients (12.9%). The wedge resection technical success rate was 100%. Mean VATS operative time was 167.3 ± 75.2 min, with a mean blood loss of 92.6 ± 61.5 ml. Patients were followed between 3 and 46 months (median: 24 months), with no evidence of new nodules, distant metastases, or postoperative complications in any patients.
Conclusion:
Preoperative CT-guided multiple coil localization can be easily and safely used to guide single-stage VATS diagnostic wedge resection in patients with MLNs.
The reviews of this paper are available via the supplemental material section.
Keywords: computed tomography, coil localization, lung nodule, multiple
Introduction
Thoracic computed tomography (CT) is commonly used to detect lung nodules,1–6 with some patients presenting with multiple lung nodules (MLNs) that can correspond to metastatic lesions or to multiple primary lung cancers.7–9 When possible, a video-assisted thoracoscopic surgery (VATS)-guided diagnostic wedge resection approach has been employed to remove these MLNs from patients, as this procedure is less invasive and removes less healthy tissue than do other lobectomy-based resection strategies.7–9
To ensure that technical success rates for multiple wedge resections remain high, it is essential that all target nodules be preoperatively localized through a CT-based technique.7,8,10 Although some peripheral small solid nodules could be palpated,4 detection of these small nodules was time-consuming. When the preoperative localization was performed, the visualization of the localized marking could directly guide us to find the nodules. In previous studies, researchers have conducted preoperative MLNs localization using a hook-wire approach prior to VATS, with technical success rates from 83.5–96.7%.8,10 This approach, however, has been reported to be associated with complication rates as high as 89.5%.8
CT-guided coil localization has been widely used for preoperative localization of lung nodules.1,2,4,11,12 In contrast to hook-wire localization, coil localization of lung nodules has been found to exhibit a significant reduction in complication rates.12 A previous study regarding the comparison of coil and hook-wire localization for lung nodules indicated that a lower displacement rate (5% versus 46%, p < 0.01) and overall complication rate (25% versus 54%, p = 0.04) were found in the coil group.11 Although some previous coil localization studies included some patients with MLNs,1,2,4 there is still a lack of studies focusing on CT-guided coil localization for MLNs.
Herein, we sought to explore the feasibility, safety, and clinical efficacy of using a preoperative CT-guided coil-based approach to the localization of MLNs.
Patients and methods
This was a retrospective single-center analysis that received approval from our Institutional Review Board. As this study was retrospective in nature, the need for written informed consent for participants in this study was waived. The written informed consent for coil localization procedure was obtained from all patients.
Patients
A total of 31 patients presenting with MLNs were treated via CT-guided coil localization followed by VATS-guided wedge resection between November 2015 and July 2019. Patient inclusion criteria were: (a) a confirmed MLNs diagnosis based upon CT imaging; (b) all target lesions were less than 3 mm in diameter; (c) all target lesions had no definite pathologic diagnosis; and (d) all target lesions had a ⩽3 cm lesion-pleura distance. Patients were excluded from this study if they met the following criteria: (a) lesions were less than 3 mm in diameter; (b) lesions were benign, including calcifications or lesions that decreased in size when reexamined; (c) patients exhibited diffuse MLNs that could not be resected; and (d) extrapulmonary metastases were observed.
Of the 31 enrolled patients, three had previously undergone surgical tumor resections to treat lung cancer (n = 1), liver cancer (n = 1), or colon cancer (n = 1). The wedge resection-based treatment of these patients was scheduled following discussions with oncologists, radiologists, and surgeons.
CT-guided coil localization
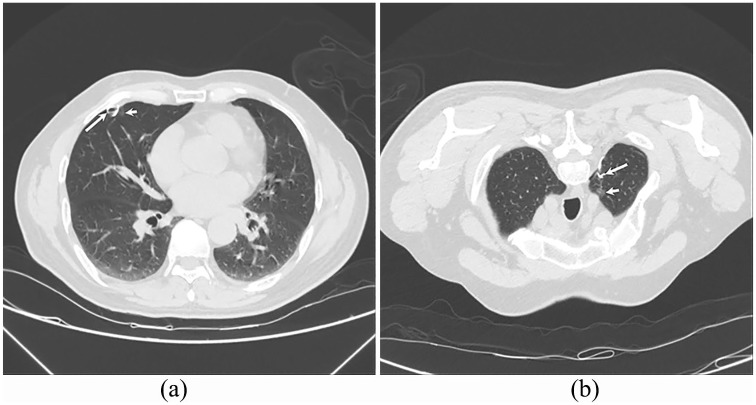
CT guidance was used for coil localization procedures. Local anesthesia was applied, after which a puncture was made in the lung using an 18 G coaxial needle (Precisa, Roma, Italy), with the tip of the needle maintained within 1 cm of the nodule of interest. Next, a 50 mm long, 0.038 diameter coil (Cook, Bjaeverskov, Denmark) was inserted through the needle into the parenchyma of the lung, after which the needle was carefully removed such that the coil tail remained visible over the visceral pleura. A subsequent CT scan was then conducted to assess rates of procedure-related complications in these patients. All nodules were localized synchronously in a single-stage procedure (Figure 1a and b).
Figure 1.
CT-guided coil localization for bilateral MLNs. CT demonstrates two lung nodules (short arrows) in the right middle (a) and left upper (b) lobes. These two nodules were simultaneously localized by coils (long arrows).
VATS procedure
Within 24 h of localization, VATS was performed in all patients, with the visible coil tail being used to guide the wedge resection procedure. All nodules in a given patient were resected during a single-stage VATS procedure, with the edge of the resection being at least 2 cm from the coil. The depth of the wedge resection was evaluated by the preoperative CT imaging. If the patient had unilateral MLNs, the second wedge resection was performed immediately after the first wedge resection. If the patient had bilateral MLNs, we first confirmed that there was no air leak after the first wedge resection, and then the contralateral wedge resection was performed. Following resection, nodules were immediately subjected to pathological analysis. When nodules were found to be benign, precancerous, adenocarcinomas in situ, minimally invasive adenocarcinomas (MIS), or metastatic lesions, then lobectomy was not performed, whereas it was performed in patients with multiple invasive carcinomas, with the lobe containing the highest stage lesion being removed.
Assessment
CT-guided coil localization technical success was determined based upon the successful thoracoscopy-based visualization of the coil tail. The technical success of wedge resection was defined based upon the successful identification of the target nodule within the resected tissue.
Statistical analysis
SPSS v16.0 (SPSS Inc., IL, USA) was used for all statistical testing. Fisher’s exact test or chi-squared tests were used for comparing categorical variables, whereas Student’s t tests or Mann–Whitney’s U tests were used to compare continuous variables, which are given as means ± SD. p < 0.05 was the significance threshold.
Results
Baseline data
Patient baseline characteristics are compiled in Table 1. In these 31 patients, 68 total nodules (2.2 nodules/patient) underwent localization and wedge resection. These nodules were unilateral and bilateral in 23 and 8 patients, respectively. At baseline, no significant differences between these two patient groups were detected (Tables 1 and 2).
Table 1.
Patients’ baseline data.
| Patients with unilateral nodules | Patients with bilateral nodules | p value | |
|---|---|---|---|
| Patients number | 23 | 8 | - |
| Age (y) | 56.8 ± 10.8 | 52.8 ± 5.2 | 0.172 |
| Gender (male/female) | 10/13 | 5/3 | 0.605 |
| Smoking history | 5 | 1 | 1.000 |
| Malignant history | 3 | 0 | 0.550 |
| Number of nodules | 1.000 | ||
| Patients with 2 lung nodules | 19 | 7 | |
| Patients with ⩾3 lung nodules | 4 | 1 |
Table 2.
Nodules’ baseline data.
| Patients with unilateral nodules | Patients with bilateral nodules | p value | |
|---|---|---|---|
| Nodules number | 51 | 17 | - |
| Diameter (mm) | 7.0 ± 4.1 | 6.6 ± 3.7 | 0.676 |
| Lesion-pleura distance (mm) | 5.8 ± 6.0 | 5.8 ± 4.3 | 0.990 |
| Nature of nodules (solid/GGN) | 13/38 | 4/13 | 1.000 |
| Lung sides (left/right) | 18/33 | 8/9 | 0.387 |
| Lobes (upper/non-upper) | 25/26 | 9/8 | 0.779 |
| Pathological diagnoses | 0.459 | ||
| Lung cancer | 28 | 7 | |
| Precancerosis | 10 | 3 | |
| Benign | 13 | 7 |
GGN: ground-glass nodule.
Localization procedure
The technical success rate of CT-guided coil localization was 98.5% (67/68) in a lesion-based analysis, while the technical success rate of single-stage coil localization in a patient-based analysis was 96.8% (30/31). Localization technical successful rates did not differ significantly between patients presenting with unilateral and bilateral MLNs (Table 3).
Table 3.
Details of coil localization.
| Patients with unilateral nodules | Patients with bilateral nodules | p value | |
|---|---|---|---|
| Patients number | 23 | 8 | - |
| Nodules number | 51 | 17 | - |
| Technical success of each nodule | 98.0% (50/51) | 100% (17/17) | 1.000 |
| Technical success of one-stage localization | 95.7% (22/23) | 100% (8/8) | 1.000 |
| Duration of one-stage localization (min) | 29.9 ± 9.0 | 30.5 ± 10.4 | 0.871 |
| Pneumothorax | 2 | 2* | 0.268 |
The pneumothorax was unilateral pneumothorax in both of the two patients.
Following localization, asymptomatic pneumothorax occurred in four patients (12.9%) but did not interfere with subsequent VATS-based wedge resection.
Wedge resection
The median interval between coil localization and VATS was 14 h. The technical success rate of the wedge resection was 100% in both lesion-based and patient-based analyses (Table 4). While one nodule was not successfully localized through the coil-based localization procedure, palpation of this nodule allowed for the successful localization and resection thereof. For all resected tissue sections, the presence of negative surgical margins was confirmed, and no patients underwent thoracotomy. A total of five nodules in five separate patients were diagnosed as invasive adenocarcinoma, with four patients undergoing additional lobectomy and one declining to undergo this procedure due to advanced age.
Table 4.
Details of VATS.
| Patients with unilateral nodules | Patients with bilateral nodules | p value | |
|---|---|---|---|
| Patients number | 23 | 8 | - |
| Technical success of one-stage wedge resection | 100% (23/23) | 100% (8/8) | - |
| Additional lobectomy | 2 | 2 | 0.268 |
| Duration of VATS (min) | 170.7 ± 82.6 | 157.5 ± 51.0 | 0.677 |
| Blood loss (ml) | 93.9 ± 64.6 | 88.8 ± 55.4 | 0.842 |
VATS: video-assisted thoracoscopic surgery.
The mean VATS procedure operative time was 167.3 ± 75.2 min, with a mean blood loss of 92.6 ± 61.5 ml. VATS procedure duration and blood loss did not differ significantly between patients presenting with unilateral and bilateral MLNs (Table 4).
Follow up
Patients were followed from 3 to 46 months (median: 24 months), with no evidence of new nodule development, postoperative complications, or distant metastasis in these patients during this time.
Discussion
The results of this study highlight the potential feasibility, safety, and clinical efficacy of using a CT-guided coil localization approach in patients with MLNs prior to wedge resection, with respective 98.5% and 96.8% localization technical success rates in lesion- and patient-based analyses. The technical success of this strategy did not differ based upon whether patients exhibited unilateral or bilateral MLNs. Together these findings suggest that the implantation of multiple coils in a single-stage procedure can effectively localize MLNs, and that nodule distribution does not have a significant impact on the success of this localization strategy.
In this study, the mean diameter of the target nodules was less than 10 mm and most nodules were ground-glass nodules (GGNs). It seems that coil localization mainly lies in the ability to identify small nodules or GGNs. For the larger solid nodules, CT-guided lung biopsy can be initially performed to make a pathologic diagnosis.13 If a malignant lesion is confirmed, VATS-guided lobectomy can be directly performed. In addition, larger solid nodules can likely be palpated. Therefore, coil localization for larger solid nodules is usually limited used.
In this study, we observed a 12.9% rate of pneumothorax in patients following coil-based nodule localization, which is substantially lower than in previous studies wherein MLNs were localized via a hook-wire-based approach.8,10 Although Kadeer and colleagues10 described a modified hook-wire localization strategy with lower rates of adverse events, in this previous report pneumothorax still occurred in 22% of treated patients. The structural property of the coil, which is composed of platinum and thrombogenic fiber coating, might reduce the risk of procedure-related pneumothorax.12 Given these high pneumothorax rates, hook-wire localization is not recommended for use when simultaneously localizing bilateral MLNs.10 In contrast, all eight patients with bilateral MLNs in this study underwent successful coil localization.
We were able to successfully conduct a single-stage VATS wedge resection procedure in all patients in the present study, despite the technical failure of coil localization for one nodule. For this nodule, palpation of the coil during the VATS procedure allowed for successful wedge resection of the affected nodule, as in previous reports.1 Diagnostic wedge resection has also been shown to be an effective curative strategy for managing lesions of an at most MIS stage.1 When invasive adenocarcinoma is identified following MLNs resection, a lobectomy of the lobe containing the highest stage tumor is typically sufficient to prevent tumor progression. As such, this coil localization strategy can help minimize the amount of tissue resection required in patients presenting with MLNs.
We were able to successfully conduct coil localization and VATS wedge resection in eight patients with bilateral MLNs in the present report, with comparable rates of technical success for both of these procedures when comparing unilateral and bilateral MLN patients. Procedure durations, blood loss, and procedure-related complication rates also did not differ between these two groups of patients. In a previous study, Yao and colleagues14 conducted a single-stage VATS resection of 29 patients with bilateral MLNs, determining that this approach was associated with a significantly reduced average hospital stay relative to that required for patients treated using a two-stage VATS resection strategy. This, coupled with our results, suggests that single-stage coil localization and VATS resection can be safely and effectively used to treat bilateral MLNs.
During follow up, no patients in this study developed additional lung nodules or distant metastases, consistent with a past study of the single-stage VATS-based bilateral resection of multiple small nodules.14 One patient in this study declined to undergo additional lobectomy to treat invasive lung cancer, and further observation is thus needed.
There are multiple limitations to this study. For one, this was a retrospective analysis. In addition, this study had a small sample size and lacked a control group or any other localization strategies for comparison. In addition, this was a single-center study. Third, deeply located lesions were excluded from this analysis and it may therefore underestimate the pneumothorax complication rate.
In summary, while further trials are needed to confirm these results, our data suggest that preoperative CT-guided multiple coil localization can be safely and effectively used to guide single-stage VATS diagnostic wedge resection in patients with MLNs.
Supplemental Material
Supplemental material, Author_response_1 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Author_Response_2 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Author_Response_3 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Reviewer_1_v.1 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Reviewer_2_v.1 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Reviewer_2_v.2 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Reviewer_2_v.3 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Footnotes
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The authors declare that there is no conflict of interest.
ORCID iD: Yu-Fei Fu  https://orcid.org/0000-0002-6772-6557
https://orcid.org/0000-0002-6772-6557
Supplemental material: The reviews of this paper are available via the supplemental material section.
Contributor Information
Fei Teng, Department of Radiology, Ningbo first hospital, Ningbo, Zhejiang, China.
An-Le Wu, Department of Radiology, Ningbo first hospital, Ningbo, Zhejiang, China.
Shan Yang, Department of Radiology, Ningbo first hospital, Ningbo, Zhejiang, China.
Jia Lin, Department of Radiology, Ningbo first hospital, Ningbo, Zhejiang, China.
Yu-Tao Xian, Department of Radiology, Ningbo first hospital, Ningbo, Zhejiang, China.
Yu-Fei Fu, Department of Radiology, Xuzhou central hospital, 199 South Jiefang Road, Xuzhou, Jiangsu, China.
Reference
- 1. Fu YF, Zhang M, Wu WB, et al. Coil localization-guided video-assisted thoracoscopic surgery for lung nodules. J Laparoendosc Adv Surg Tech A 2018; 28: 292–297. [DOI] [PubMed] [Google Scholar]
- 2. Su TH, Fan YF, Jin L, et al. CT-guided localization of small pulmonary nodules using adjacent microcoil implantation prior to video-assisted thoracoscopic surgical resection. Eur Radiol 2015; 25: 2627–2633. [DOI] [PubMed] [Google Scholar]
- 3. Zhang M, Wang T, Wang H. A segmental labeling technique for non-intubated thoracoscopic anatomical segmentectomy. J Thorac Dis 2017; 9: 1648–1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Finley RJ, Mayo JR, Grant K, et al. Preoperative computed tomography-guided microcoil localization of small peripheral pulmonary nodules: a prospective randomized controlled trial. J Thorac Cardiovasc Surg 2015; 149: 26–31. [DOI] [PubMed] [Google Scholar]
- 5. Iguchi T, Hiraki T, Gobara H, et al. Transfissural route used for preoperative localization of small pulmonary lesions with a short hook wire and suture system. Cardiovasc Intervent Radiol 2015; 38: 222–226. [DOI] [PubMed] [Google Scholar]
- 6. Iguchi T, Hiraki T, Matsui Y, et al. Preoperative short hookwire placement for small pulmonary lesions: evaluation of technical success and risk factors for initial placement failure. Eur Radiol 2018; 28: 2194–2202. [DOI] [PubMed] [Google Scholar]
- 7. Tseng YH, Lee YF, Hsieh MS, et al. Preoperative computed tomography-guided dye injection to localize multiple lung nodules for video-assisted thoracoscopic surgery. J Thorac Dis 2016; 8: S666–S671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Iguchi T, Hiraki T, Gobara H, et al. Simultaneous multiple preoperative localizations of small pulmonary lesions using a short hook wire and suture system. Cardiovasc Intervent Radiol 2015; 38: 971–976. [DOI] [PubMed] [Google Scholar]
- 9. Hattori A, Matsunaga T, Takamochi K, et al. Surgical management of multifocal ground-glass opacities of the lung: correlation of clinicopathologic and radiologic findings. Thorac Cardiovasc Surg 2017; 65: 142–149. [DOI] [PubMed] [Google Scholar]
- 10. Kadeer X, Wang L, Zhang L, et al. Modified hook-wire placement technique for localizing multiple pulmonary nodules. J Surg Oncol 2018; 118: 1188–1193. [DOI] [PubMed] [Google Scholar]
- 11. Rostambeigi N, Scanlon P, Flanagan S, et al. CT fluoroscopic-guided coil localization of lung nodules prior to video-assisted thoracoscopic surgical resection reduces complications compared to hook wire localization. J Vasc Interv Radiol 2019; 30: 453–459. [DOI] [PubMed] [Google Scholar]
- 12. Park CH, Han K, Hur J, et al. Comparative effectiveness and safety of preoperative lung localization for pulmonary nodules: a systematic review and meta-analysis. Chest 2017; 151: 316–328. [DOI] [PubMed] [Google Scholar]
- 13. Meng XX, Kuai XP, Dong WH, et al. Comparison of lung lesion biopsies between low-dose CT-guided and conventional CT-guided techniques. Acta Radiol 2013; 54: 909–915. [DOI] [PubMed] [Google Scholar]
- 14. Yao F, Yang H, Zhao H. Single-stage bilateral pulmonary resections by video-assisted thoracic surgery for multiple small nodules. J Thorac Dis 2016; 8: 469–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Author_response_1 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Author_Response_2 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Author_Response_3 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Reviewer_1_v.1 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Reviewer_2_v.1 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Reviewer_2_v.2 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease
Supplemental material, Reviewer_2_v.3 for Preoperative computed tomography-guided coil localization for multiple lung nodules by Fei Teng, An-Le Wu, Shan Yang, Jia Lin, Yu-Tao Xian and Yu-Fei Fu in Therapeutic Advances in Respiratory Disease