Abstract
Background
Physical conditioning as part of a return to work strategy aims to improve work status for workers on sick leave due to back pain. This is the second update of a Cochrane Review (originally titled 'Work conditioning, work hardening and functional restoration for workers with back and neck pain') first published in 2003, updated in 2010, and updated again in 2013.
Objectives
To assess the effectiveness of physical conditioning as part of a return to work strategy in reducing time lost from work and improving work status for workers with back pain. Further, to assess which aspects of physical conditioning are related to a faster return to work for workers with back pain.
Search methods
We searched the following databases to March 2012: CENTRAL, MEDLINE (from 1966), EMBASE (from 1980), CINAHL (from 1982), PsycINFO (from 1967), and PEDro.
Selection criteria
Randomized controlled trials (RCTs) and cluster RCTs that studied workers with work disability related to back pain and who were included in physical conditioning programmes.
Data collection and analysis
Two review authors independently extracted data and assessed risk of bias. We used standard methodological procedures expected by The Cochrane Collaboration.
Main results
We included 41 articles reporting on 25 RCTs with 4404 participants. Risk of bias was low in 16 studies.
Three studies involved workers with acute back pain, eight studies workers with subacute back pain, and 14 studies workers with chronic back pain.
In 14 studies, physical conditioning as part of a return to work strategy was compared to usual care. The physical conditioning mostly consisted of graded activity with work‐related exercises aimed at increasing back strength and flexibility, together with a set date for return to work. The programmes were divided into a light version with a maximum of five sessions, or an intense version with more than five sessions up to full time or as inpatient treatment.
For acute back pain, there was low quality evidence that both light and intense physical conditioning programmes made little or no difference in sickness absence duration compared with care as usual at three to 12 months follow‐up (3 studies with 340 workers).
For subacute back pain, the evidence on the effectiveness of intense physical conditioning combined with care as usual compared to usual care alone was conflicting (four studies with 395 workers). However, subgroup analysis showed low quality evidence that if the intervention was executed at the workplace, or included a workplace visit, it may have reduced sickness absence duration at 12 months follow‐up (3 studies with 283 workers; SMD ‐0.42, 95% CI ‐0.65 to ‐0.18).
For chronic back pain, there was low quality evidence that physical conditioning as part of integrated care management in addition to usual care may have reduced sickness absence days compared to usual care at 12 months follow‐up (1 study, 134 workers; SMD ‐4.42, 95% CI ‐5.06 to ‐3.79). What part of the integrated care management was most effective remained unclear. There was moderate quality evidence that intense physical conditioning probably reduced sickness absence duration only slightly compared with usual care at 12 months follow‐up (5 studies, 1093 workers; SMD ‐0.23, 95% CI ‐0.42 to ‐0.03).
Physical conditioning compared to exercise therapy showed conflicting results for workers with subacute and chronic back pain. Cognitive behavioural therapy was probably not superior to physical conditioning as an alternative or in addition to physical conditioning.
Authors' conclusions
The effectiveness of physical conditioning as part of a return to work strategy in reducing sick leave for workers with back pain, compared to usual care or exercise therapy, remains uncertain. For workers with acute back pain, physical conditioning may have no effect on sickness absence duration. There is conflicting evidence regarding the reduction of sickness absence duration with intense physical conditioning versus usual care for workers with subacute back pain. It may be that including workplace visits or execution of the intervention at the workplace is the component that renders a physical conditioning programme effective. For workers with chronic back pain physical conditioning has a small effect on reducing sick leave compared to care as usual after 12 months follow‐up. To what extent physical conditioning as part of integrated care management may alter the effect on sick leave for workers with chronic back pain needs further research.
Plain language summary
Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain
Review question
We reviewed the evidence about the effect of physical conditioning as part of a return to work strategy in people with low back pain. We found 25 studies.
Background
The main goal of physical conditioning as part of a return to work strategy, sometimes called work conditioning, work hardening or functional restoration and exercise programmes, is to return injured or disabled workers to work or improve the work status for workers performing modified duties. Such programmes may also simulate or duplicate work or functional tasks, or both, using exercises in a safe, supervised environment. These exercises or tasks are structured and progressively graded to increase psychological, physical and emotional tolerance and to improve endurance and work feasibility. In such environments, injured workers improve their general physical condition through an exercise programme aimed at increasing strength, endurance, flexibility and cardiovascular fitness. We wanted to discover whether physical conditioning was more or less effective than usual care and other types of interventions like exercise therapy.
Study characteristics
The evidence was current to March 2012. We analysed 17 comparisons of physical conditioning as part of a return to work strategy. Some trials examined physical conditioning in addition to care as usual versus care as usual only, and others compared physical conditioning to other types of interventions such as standard exercise therapy. Participants had either acute back pain (duration of symptoms less than six weeks), subacute back pain (duration of symptoms more than six but less than 12 weeks), or chronic back pain (duration of symptoms more than 12 weeks). Participants were followed for anywhere from three weeks to three years. We divided physical conditioning into light or intense, depending on its intensity and duration.
Key results
Results showed that light physical conditioning has no effect on sickness absence duration for workers with subacute or chronic back pain. We found conflicting results for intense physical conditioning for workers with subacute back pain. Intense physical conditioning probably had a small effect on reducing sick leave at 12 months follow‐up compared to usual care for workers with chronic back pain. Involving the workplace, or physical conditioning being part of integrated care management may have had a positive effect on reducing sick leave, but this needs further research.
Quality of the evidence
The quality of the evidence ranged from very low to moderate. Although 16 of the included studies were well designed and had no major flaws, some studies were poorly conducted and the small number of participants in most studies lowered the overall quality of the evidence.
Background
Description of the condition
Back pain is a major health and economic problem for society. In Western countries, the reported point prevalence varies from 12% to 30% (Anema 2009). Whether back symptoms are attributed to work, are reported to workers' compensation systems, lead to healthcare‐seeking behaviour, result in time off work, or any combination of these scenarios depend on complex individual psychosocial and work organizational and social security factors. People with physically or psychologically demanding jobs may have more difficulty working when they have back pain and so lose more time from work, but that can also be the effect rather than the cause of their pain (Waddell 1999). Nevertheless, most workers with back pain, their employers, and insurers agree that the goal of managing back pain is a timely return‐to‐work following back pain‐related work disability.
Description of the intervention
Physical conditioning as part of a return to work strategy, variously called work conditioning, work hardening or functional restoration and exercise programmes, aims for return‐to‐work or improvement in work status for workers performing modified duties. Such programmes either simulate or duplicate work or functional tasks, or both, in a safe, supervised environment. These tasks are structured and progressively graded to increase psychological, physical and emotional tolerance and improve endurance and work feasibility (Lechner 1994). In such environments, injured workers learn appropriate job performance skills in addition to improving their physical condition through an exercise programme aimed at increasing strength, endurance, flexibility and cardiovascular fitness. Work hardening programmes are individualized, work‐oriented activities that involve clients in simulated or actual work tasks. Work conditioning is a programme with an emphasis on physical conditioning, which addresses the issues of strength, endurance, flexibility, motor control and cardiopulmonary function (Lechner 1994). Functional restoration refers to any intervention aimed at restoring a reasonable functional level for activities of daily living, including work (Bendix 1996).
These programmes differ in their goals from other programmes, such as patient care management, multidisciplinary treatments, pain clinics, standard medical care or physiotherapy, which aim to reduce symptoms, pain intensity, use of medications and health services, and to increase global improvement and quality of life (Guzman 2001; Guzman 2002), physiological outcomes such as range of motion and spinal flexibility (Hayden 2005), or behavioural outcomes such as anxiety, depression and cognition (Ostelo 2000). Recent years have shown a development towards more involvement of the workplace in interventions aiming for return to work for various musculoskeletal disorders including back pain. A systematic review by Carroll 2010 reported that stakeholder participation and work modification are more effective and cost‐effective for returning adults with musculoskeletal conditions to work than other workplace‐linked interventions, including exercise.
How the intervention might work
Physical conditioning as part of a return to work strategy is characterized by some form of structured exercise or advice about exercise based on the idea that inactivity due to avoidance of painful activities can lead to so‐called ‘deconditioning syndrome’, which in turn can lead to more pain from attempts to move joints that are stiffened and muscles weakened by disuse. Central to these programmes is the notion that as physical and functional capacities improve, so will the person’s capability of returning to work. The programme may be comprised of actual or simulated work tasks, or interventions addressing individual and work‐related psychosocial factors that may play an important role in persisting symptoms and disability, or both (Waddell 1999). This intended work outcome or job‐attached status to the pre‐injury employer is important for a successful outcome with these physical conditioning programmes (Schonstein 1999).
Maintenance of a job‐attached status to the pre‐injury employer is often best accomplished by the provision of suitable modified duties (Voaklander 1995). The effectiveness of modified duties has been studied and comprehensively reviewed (Krause 1998; Loisel 2005) and results indicate that the provision of suitable duties facilitates return‐to‐work, reduces days lost due to injury, and is cost‐effective. Accordingly, this review documents work conditioning programmes that include the availability of modified duties in the back pain management plan.
Why it is important to do this review
This review focuses exclusively on workers with back pain who are either off work or are at risk of being off work due to reduced work capacity, and evaluates the effectiveness of work hardening and functional restoration in improving their work status. This review is the second update of a Cochrane review first published in 2003 that summarised the evidence on the effectiveness of physical conditioning programmes for workers with back and neck pain (Schonstein 2003; Schonstein 2003a). An update was performed in 2010 (Schaafsma 2010). Results of the in 2010 updated review indicated that the effectiveness of physical conditioning programmes in reducing sick leave, when compared to usual care or to other exercises, in workers with back pain remains uncertain. In workers with acute back pain, these programmes probably have no effect on sick leave, but there may be a positive effect on sick leave for workers with subacute and chronic back pain. Workplace involvement may improve the outcome. Better understanding of the mechanism behind physical conditioning programmes and return‐to‐work is needed to be able to develop more effective interventions.
Other reviews have evaluated the efficacy of multidisciplinary back pain management programmes (Guzman 2001; Heymans 2005; Karjalainen 2000; Teasell 1996) in reducing disability related to back pain. In a review of functional restoration programmes for chronic low‐back pain, Teasell 1996 concluded that evidence to support physical conditioning was lacking. In contrast, Karjalainen 2000 reported that multidisciplinary biopsychosocial rehabilitation reduces subacute low‐back pain among working age adults, and that a work site visit increases its effectiveness. While some of these reviews have incorporated return‐to‐work in their outcome measures, none have focused exclusively on work outcomes.
The review by Heymans 2005 on back schools for non‐specific low‐back pain stated that there is moderate evidence suggesting that back schools, in an occupational setting, reduce pain and improve function and return‐to‐work status, in the short‐ and intermediate‐term. This is compared with exercises, manipulation, myofascial therapy, advice, placebo or waiting list controls for workers with chronic and recurrent low‐back pain. Back schools are defined as programmes consisting of educational and skills acquisition components, including exercises, in which all sessions are given to groups of workers and supervised by allied health professionals or a medical specialist. Unlike the interventions of this review, the components of back schools are not generally tailored specifically to job demands.
Hayden 2005 questioned whether exercise is more effective than reference treatments for individuals with non‐specific low‐back pain. They concluded that specific exercises are as effective as either no treatment or other conservative treatments for acute low‐back pain. However, exercise therapy is slightly more effective than no treatment or other conservative treatments at decreasing pain and improving function in adults with chronic low‐back pain. For subacute low‐back pain, there is some evidence that a graded activity programme reduces absenteeism, though evidence for other types of exercise is unclear. Despite the fact that exercise is an integral component of physical conditioning programmes, in our review physical conditioning programmes also needed to have a stated focus on functional job demands.
This review is unique because it addresses the specific question of whether physical conditioning that has a stated focus on functional job demands is effective in reducing sick leave and improving work status for workers with work‐related low‐back pain. As a result, some of the studies are also included in other reviews that explore the effects of specific interventions on pain, function, general well‐being and disability (Guzman 2002; Hayden 2005; Heymans 2005; Karjalainen 2000; Ostelo 2000).
In this update, we changed the title from 'Physical conditioning programs for improving work outcomes in workers with back pain' to 'Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain;. This new title illustrates that over the years physical conditioning has become more and more part of an integrated care programme including various modules and more explicitly involving the workplace. We focused exclusively on workers with back pain and on work status outcomes and therefore excluded neck pain and secondary outcomes such as functional status and physiological outcomes, which were included in the original review. We only included interventions that have a stated relationship with the workplace, a focus on job demands, and measured work outcomes. We reviewed new evidence available since the previous search carried out in 2008. In the results section of this updated review, a distinction is again made between workers with acute (less than six weeks), subacute (between six and 12 weeks) and chronic (more than 12 weeks) back pain. Further, we made a distinction between comparisons of physical conditioning in addition to care as usual compared to care as usual only, or physical conditioning compared to care as usual.
Objectives
To assess the effectiveness of physical conditioning as part of a return to work strategy in reducing time lost from work and improving work status for workers with back pain. Further, to assess which aspects of physical conditioning are related to a faster return to work for workers with back pain.
Methods
Criteria for considering studies for this review
Types of studies
Only randomized controlled trials (RCTs) and cluster RCTs, regardless of the language in which they were published, were included in this review.
Types of participants
Male and female adults (> 16 years) with work disability related to back pain who took part in physical conditioning programmes were included in this review. Back pain was defined as pain in the thoracic, lumbar or gluteal region, or a combination, with or without radiation to the lower extremities. Studies with at least 50% of workers with back pain were included. Work disability was defined as being on full or partial sick leave, or not being able to perform adequately at work due to back pain.
All workers who were accepted into physical conditioning programmes, whether they had acute (duration of symptoms less than six weeks), subacute (duration of symptoms more than six but less than 12 weeks) or chronic back pain (duration of symptoms more than 12 weeks), met our inclusion criteria.
Studies with non‐workers, or workers with specific diagnoses such as infection, neoplasm, metastasis, osteoporosis, rheumatoid arthritis, fracture, inflammatory processes or other conditions for which valid diagnoses had been demonstrated were excluded.
Types of interventions
Physical conditioning programmes are also known as work conditioning or hardening, or functional restoration and exercise programmes. They include advice about exercise and may also simulate or duplicate work or functional tasks, or both, in a safe, supervised environment. These exercises or tasks are structured and progressively graded to increase psychological, physical and emotional tolerance and improve endurance and work feasibility. We included studies on physical conditioning programmes when they included the following three key elements:
(advice about ) exercises specifically designed to restore an individual's systemic, neurological, musculoskeletal (strength, endurance, movement, flexibility and motor control) or cardiopulmonary function, or a combination;
explicitly stated to have an intended improvement of work status;
a stated relationship between the intervention and functional job demands.
In addition to these three key elements, physical conditioning programmes could include components such as operant conditioning behavioural approach, pain management, back pain education, advice on return‐to‐work, workplace involvement and case‐management. The delivery of physical conditioning programmes could involve multidisciplinary teams or individual health professionals. In addition, they could be delivered in a one‐to‐one fashion or in a group situation.
Based on the intensity of the programme we differentiated between the following.
Light physical conditioning: these programmes included the three key elements and were delivered in fewer than five sessions (of one to two hours) or were described by the primary study author as a light intervention programme.
Intense physical conditioning: these programmes included the three key elements and were delivered in more than five sessions or were delivered on a full‐time basis for more than two weeks.
Types of outcome measures
Work status outcomes were:
1. time between intervention and return‐to‐work;
2. return‐to‐work status in terms of 'at work' or ‘off work';
3. time on light or modified duties.
Search methods for identification of studies
For this updated review, searches were conducted in the same databases as in the original review, for the period of June 2008 to March 2012. Searches were performed by the Trials Search Co‐ordinator of the Cochrane Back Review Group (CBRG). RCTs were identified by searching electronic databases, using the Ovid search strategy. Databases included were: CENTRAL, MEDLINE (from 1966), EMBASE (from 1980), CINAHL (from 1982), PsycINFO (from 1967), and PEDro. The CBRG Trials Register, ClinicalTrials.gov, and World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) were also searched until March 2012. In May 2013 we ran an additional search and all relevant trials were added to the 'Studies awaiting assessment' reference list.
All RCTs were included regardless of the language in which they were published. The highly sensitive search strategies of The Cochrane Collaboration were run in conjunction with a specific search for back pain and the interventions investigated (Furlan 2009). The MEDLINE search is based on the first two stages of the MEDLINE search strategy recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This search update added terms to the original search strategy, based on the results of testing terms synonymous with work. These were added with a combination of year limits and NOT. The logic here was to retroactively search for the new terms without retrieving all of the same results that were already retrieved in the previous searches up to 2008. See Appendix 1.
This strategy was modified for EMBASE, CINAHL, and PsycINFO. Search words used for the PEDro database were: low‐back pain, backache, lumbar, thoracic, work conditioning, work hardening, functional restoration, exercise, and gym.
Data collection and analysis
Selection of studies
Two review authors (FS, KW) independently examined search results and independently applied the selection criteria to the studies retrieved. A consensus method was used to resolve disagreements concerning inclusion of RCTs. A third review author (JV) was consulted if disagreements persisted.
Two review authors (FS, KW) read all papers independently and determined eligibility according to the inclusion and exclusion criteria listed above.
Data extraction and management
Data were independently extracted from the studies by two review authors (FS and LE) using an adapted version of the pre‐designed form from the CBRG for data extraction. Discrepancies were resolved by consensus or by consulting a third author (JV). The following criteria were used in our data extraction.
1. Characteristics of study population: number of workers, gender, age and setting, country and date of the study, duration of symptoms, work status.
2. Characteristics of interventions: the content, duration and frequency of the physical conditioning programmes and control interventions.
3. Results on outcomes of interest.
Assessment of risk of bias in included studies
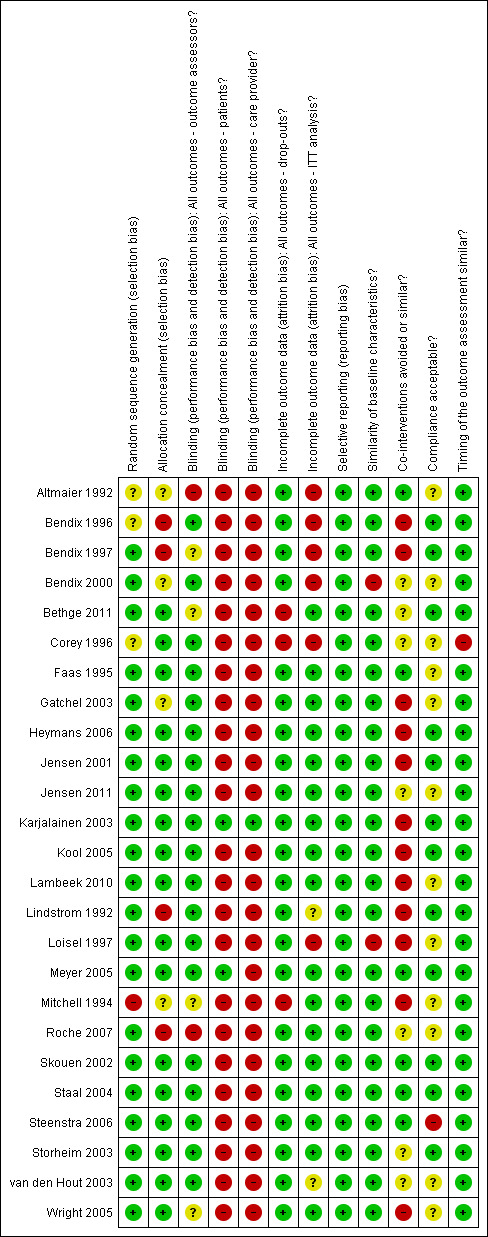
We used the criteria recommended by the CBRG (Furlan 2009) to assess the risk of bias of the selected RCTs. The criteria and their operational definitions are outlined in Appendix 2. Each of the criteria were scored 'high', 'low' or 'unclear' according to the operationalisation of the criteria. Following the recommendations of the CBRG (Furlan 2009), studies were rated as having a ‘low risk of bias’ when at least six of the 12 CBRG criteria were met and the study had no serious flaws. Serious flaws were inadequate concealment of treatment allocation, a large dropout rate, or statistically significant and clinically important baseline differences not accounted for in the analyses. Studies with serious flaws or those in which fewer than six of the criteria were met were rated as having a ‘high risk of bias’. The results of the assessment are presented in the 'Risk of bias' table and Figure 1.
1.
The risk of bias in the RCTs was independently assessed by two review authors (LE, AB). This process was not blinded with regard to the authors, institution or journal. A consensus method was used to resolve disagreements, and a third review author (JV) was consulted for persisting disagreements. If information was absent for evaluation of the methodological criteria, the authors of the study were contacted with a request to provide additional information.
Measures of treatment effect
Quantitative analysis
Studies expressed time to return‐to‐work as mean numbers of days off work. Rate of return‐to‐work was expressed as odds ratios (ORs). We regarded both time to return‐to‐work and the rate of return‐to‐work sufficiently alike, if they were measured at the same follow‐up time, to combine them as similar outcomes in the meta‐analysis. We converted the outcomes into standardized mean difference (SMD) because of the different scales used. We assumed that the continuous measurements in each intervention group followed a logistic distribution, and that the variability of the outcomes was the same in both the treated and control groups. Therefore, we were able to re‐express the calculated ORs as a standardized mean difference (SMD) according to the following simple formula (Chinn 2000; Chinn 2002) as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008): lnOR = π/√3 x SMD.
Pooling of studies was only considered when statistical heterogeneity was less than moderate (I² less than 60%).
Clinically worthwhile effect
Translating SMDs into daily practice and knowing what is a clinically worthwhile effect is difficult. Following the rules of thumb on SMDs from the Cochrane Handbook for Systematic Reviews of Interventions and the Cochrane Back Review Group (CBRG) guidelines (Furlan 2009; Higgins 2011), a SMD of more than 0.2 can be considered a small effect, more than 0.5 a moderate effect, and more than 0.8 a large effect.
However, in the original review it was stated that for continuous outcomes, a mean saving of 10 sick days per year was considered the smallest effect that would be clinically worthwhile, based on the assumption of the cost of providing physical conditioning programmes. For dichotomous outcomes, an OR of 0.65 was used as the smallest clinically worthwhile effect. This corresponded to a number needed to treat (NNT) of 10 when the baseline rate (prevalence of the event measured (on or off work)) was about 40%, based on the two comparisons from the original review (Schonstein 2003). An intervention that affected fewer than one in 10 people was considered not clinically worthwhile.
Following this original hypothesis, we decided that we would use an OR of 0.65 as the smallest clinically worthwhile effect. As we would recalculate all the continuous outcomes into SMDs, we also converted the OR of 0.65 back into a SMD. For this, we used the same formula: lnOR = π/ √3 x SMD. This led to a SMD of ‐0.24, which we considered the smallest clinically worthwhile effect.
Quality of the evidence
We assessed the overall quality of the evidence for each outcome using an adapted GRADE approach (Atkins 2004) as recommended by the CBRG (Furlan 2009). The quality of the evidence for a specific outcome was based on the study design, limitations of the study, consistency, directness, precision of results, and publication bias. For further details see Appendix 3.
The GRADE Working Group recommends four levels of evidence; the CBRG recommends the addition of a fifth.
High quality evidence: where there are consistent findings among 75% of RCTs with low risk of bias that are generalisable to the population in question; there are sufficient data, with narrow confidence intervals; there is no known or suspected publication bias; further research is unlikely to change either the estimate or our confidence in the results.
Moderate quality evidence: one of the domains is not met; further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality evidence: two of the domains are not met; further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality evidence: three of the domains are not met; we are very uncertain about the estimate.
No evidence: no RCTs are identified that address this outcome.
Assessment of clinical relevance
The clinical relevance of the studies was independently assessed by two review author (FS and AB). Clinical relevance tables were constructed using the five questions recommended by the CBRG (Furlan 2009).
1. Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice?
2. Are the interventions and treatment settings described well enough so that you can provide the same for your patients?
3. Were all clinically relevant outcomes measured and reported?
4. Is the size of the effect clinically important?
5. Are the likely treatment benefits worth the potential harms?
Regarding question 4. above, we converted the outcome data of studies into SMDs or ORs. We calculated cut‐off scores for these two effect sizes, as explained under 'Measures of treatment effect' below, to decide whether the size of the effect was considered clinically important and worthwhile. This conversion of study data and the use of cut‐off scores sometimes resulted in a conclusion that was different than the study authors' conclusions.
To clearly express the quality of the evidence and the magnitude of the effect on worker important outcomes we used the recommended statements by the GRADE Working Group in the results‐ and discussion sections.
Unit of analysis issues
For cluster designs we used the group estimates taking into account the cluster randomisation. For multiarm studies we used the data from both comparisons that included the physical conditioning programme.
Data synthesis
First, we assessed which studies were clinically homogeneous, with similar populations, interventions, comparisons and outcomes measured at the same follow‐up point. Populations were considered similar if their symptoms were of a similar duration (acute, subacute or chronic).
Interventions were considered homogeneous if they satisfied the inclusion criteria (that is exercises, improvement of work status, and explicit relation to job tasks), regardless of the inclusion of extra components or modes of delivery (that is group or individual, multi or monodisciplinary). Sensitivity analyses were performed to evaluate the effects of the variable components (see below).
We compared light or intense physical conditioning, with or without care as usual, to care as usual, exercise therapy, cognitive behavioural therapy (CBT), a cognitive intervention and to a brief clinical intervention. In addition, we compared intense physical conditioning to a combination of physical conditioning with a CBT component.
Outcomes were considered similar when they measured either the time to return‐to‐work or the proportion of workers that resumed work at specific times. These outcomes were similar because they both measured the time between injury and return‐to‐work, but were expressed in either days or percentages of workers returning to work. Follow‐up was classified into four categories: short‐term follow‐up refers to measures taken closest to three months, intermediate‐term follow‐up refers to measures taken closest to six months, long‐term follow‐up refers to outcomes closest to one year, very long‐term follow‐up refers to measures taken closest to two years. For an outcome measure of return‐to‐work, the return‐to‐work should be sustainable over a longer period of time, generally at least four weeks. For this reason, we did not consider a measurement of outcome at one month follow‐up as recommended by the CBRG method guidelines.
We tested for statistical heterogeneity by means of the I² in the meta‐analysis graphs. We used the criterion of 50%, mentioned in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008), to discern the presence or absence of heterogeneity between studies. When studies were statistically heterogeneous according to the I² statistic, a random‐effects model was used, otherwise a fixed‐effect model was used.
Subgroup analysis and investigation of heterogeneity
A subgroup analysis was performed for differences in components of physical conditioning programmes such as an operant conditioning behavioural approach, pain management, back pain education, advice on return‐to‐work and a workplace visit. A subgroup analysis was also performed on the mode of delivery of physical conditioning programmes, such as multidisciplinary or monodisciplinary and group or individual exercises.
Sensitivity analysis
A sensitivity analysis was performed to determine whether the overall results were the same when studies with different definitions of low or high risk of bias were analysed and when studies with different types of participants on full‐time or part‐time sick leave at baseline were analysed.
Results
Description of studies
Results of the search
Search results
The updated database search was run from 2008 up to March‐April 2012. This resulted in 358 references from CENTRAL, 544 references from MEDLINE, 725 references from CINAHL, 1114 references from EMBASE, and 22 references from PsycINFO. A separate search was conducted for the PEDro database until the end of March 2012, which yielded 13 references. Another separate search was conducted for the CBRG trial register, which resulted in 70 references. In April 2012 a search in ClinicalTrials.gov and WHO ICTRP resulted in another 46 registered trials. Duplicates of references and irrelevant articles were removed leaving 1761 references and 37 registered trials. Two review authors (FS and KW) independently assessed (by title or key words, or both) these references for appropriateness for inclusion.
Study selection results
After screening the abstracts of articles from the searches, seven papers were considered. An evaluation of the full text led to four new papers meeting our inclusion criteria. One paper reported a third set of follow‐up results from the same study (Roche 2007). Therefore, only the remaining three new studies were included in this updated version of the review. In the previous update we presented the data from Roche 2007 separately from the same study by Jousset 2004. In this update both articles will be referred to by only one reference: Roche 2007. The addition of three new studies (Bethge 2011; Jensen 2011; Lambeek 2010) resulted in a total of 25 studies published in 41 papers in this updated review. All data used in this review were obtained from these published studies.
Included studies
Participants
There were five small studies with fewer than 100 participants (Altmaier 1992; Bendix 1996; Meyer 2005; Storheim 2003; Wright 2005) and nine studies with more than 200 participants (Bethge 2011; Corey 1996; Faas 1995; Heymans 2006; Jensen 2001;Jensen 2011;Lambeek 2010; Mitchell 1994; Skouen 2002). The rest of the studies had between 100 and 200 participants (Bendix 1997; Bendix 2000; Gatchel 2003; Karjalainen 2003; Kool 2005; Lindstrom 1992; Loisel 1997; Roche 2007; Staal 2004; Steenstra 2006; van den Hout 2003).
We found four studies that did not specifically focus on back pain, but on workers with musculoskeletal pain (Bethge 2011; Corey 1996; Meyer 2005; Mitchell 1994). However, all three studies did have more than 50% of the workers with back pain and were therefore included in this updated review. All studies were RCTs, carried out between 1992 and 2012. Two studies had a cluster randomised design (Bethge 2011; Loisel 1997).
Fourteen studies focused on workers with chronic back pain (Altmaier 1992; Bendix 1996; Bendix 1997; Bendix 2000; Bethge 2011; Corey 1996; Jensen 2001; Jensen 2011; Lambeek 2010; Meyer 2005; Mitchell 1994; Roche 2007; Skouen 2002; van den Hout 2003), eight studies focused on workers with subacute back pain (Heymans 2006; Karjalainen 2003; Kool 2005; Lindstrom 1992; Loisel 1997; Staal 2004; Steenstra 2006; Storheim 2003), and three studies focused on workers with acute back pain (Faas 1995; Gatchel 2003; Wright 2005).
In 15 studies all workers were on sick leave, either part‐time or full‐time (Altmaier 1992; Corey 1996; Heymans 2006; Jensen 2001; Jensen 2011; Lambeek 2010; Lindstrom 1992; Loisel 1997; Meyer 2005; Mitchell 1994; Staal 2004; Steenstra 2006; Storheim 2003; van den Hout 2003; Wright 2005). In the other 10 studies not all workers were on sick leave, but all workers were described as having decreased ability to perform job requirements or may have had an episode of sick leave before randomisation (Bendix 1996; Bendix 1997; Bendix 2000; Bethge 2011; Faas 1995; Gatchel 2003; Karjalainen 2003; Kool 2005; Roche 2007; Skouen 2002). The average period of sick leave correlated with the duration of the back pain, between three weeks and six months.
Interventions
All interventions were related to work, contained physical exercises or advice about physical exercises, and had a focus on return‐to‐work. However, the number of sessions and their content varied greatly. For example, one intervention included one session only during which the worker was examined and engaged in a discussion about working conditions, trained to use five exercises and then referred back to the general practitioner (GP) with specific recommendations (Karjalainen 2003); another included a full‐time multidisciplinary treatment of eight weeks (Mitchell 1994). We labelled four interventions as light physical conditioning (Faas 1995; Heymans 2006; Jensen 2011; Karjalainen 2003; Skouen 2002; Wright 2005); the other 21 studies were labelled as intense physical conditioning. Seventeen interventions were delivered by a multidisciplinary group (for example physiotherapist, occupational therapist, ergonomist, social worker, case manager, rehabilitation physician, occupational health physician or nurse); five interventions were delivered by a physiotherapist (Faas 1995; Heymans 2006; Lindstrom 1992; Steenstra 2006; Storheim 2003). In Mitchell 1994, it was unclear who delivered the intervention.
Sixteen interventions included an operant conditioning behavioural approach (Altmaier 1992; Bendix 1996; Bendix 1997; Bendix 2000; Corey 1996; Heymans 2006; Jensen 2001; Lambeek 2010; Lindstrom 1992; Loisel 1997; Meyer 2005; Mitchell 1994; Skouen 2002; Staal 2004; Steenstra 2006; van den Hout 2003). Sixteen interventions included occupational training or ergonomic advice (Bendix 1996; Bendix 1997; Bendix 2000; Bethge 2011; Gatchel 2003; Heymans 2006; Jensen 2001; Jensen 2011; Kool 2005; Lambeek 2010; Meyer 2005; Roche 2007; Skouen 2002; Storheim 2003; van den Hout 2003; Wright 2005) and 12 mentioned explicitly that return‐to‐work advice was included in the intervention (Bethge 2011; Heymans 2006; Jensen 2001; Jensen 2011; Karjalainen 2003; Lambeek 2010; Lindstrom 1992; Loisel 1997; Meyer 2005; Staal 2004; Steenstra 2006; van den Hout 2003). Eight interventions also included a workplace visit in their intervention or explicitly involved the workplace in other ways (Jensen 2001; Jensen 2011; Karjalainen 2003; Lambeek 2010; Lindstrom 1992; Loisel 1997; Meyer 2005; van den Hout 2003) and one intervention was executed at the workplace (Staal 2004).
For more details about the content of the interventions, see Table 1; Table 2; Table 3; Table 4.
1. Contents of light physical conditioning programme (PCP).
| Faas 1995 | Heymans 2006 | Jensen 2011 | Karjalainen 2003 | Skouen 2002 | Wright 2005 | |
| Time span of training | 5 wks | 4 wks | 18 weeks median duration | na | na | 2 wks |
| Number of sessions | 2 per week | 1 per week | after the interview, the participant was seen at least once, and four times on average | 2 | approx. 4 hrs at the start + 6 follow up or individual sessions over a period of 1 year |
1 examination + treatment initially then 3 per week |
| Length of sessions | 20 min | 120 min | 1‐2 hrs | 1‐1,5 hr | unclear | 1 hr |
| Full time | no | no | no | no | no | no |
| group or individual | individual | group | individual | individual | both | both |
| exercises | yes | yes | yes in advice | yes | yes, advice and programme | yes |
| work related exercises | yes | yes | yes in advice | yes | yes in advice | yes |
| operant conditioning behavioural approach | no | no | no | no, although intervention was based on graded activity programme | no | no |
| pain coping/ management | no | no | yes | no | no | no |
| back pain education | no | yes | yes | no | no | no |
| ergonomic advice or occupational training | no | yes | no | no | no | advice on how to modify physical activities specific to the individual's work situation |
| return‐to‐work advice | no | yes | yes | no | no | no |
| workplace visit | no | no | yes | yes | no (not for all individuals) | no |
| therapists involved | physiotherapist | physiotherapist, occupational physician | rehabilitation physician, specialist in clinical social medicine, physiotherapist, social worker, occupational therapist, case manager | physiotherapist, physician | physio therapist, nurse, psychologist |
physiotherapist |
| other aspects | written compliance contract | CAU | brief clinical examination | CAU | no | CAU being a back book and advice on how to modify physical activities specific to the indivual's work situation |
| comparison | CAU | CAU/ intense PCP | brief clinical examination only | CAU | CAU / intense PCP | CAU being a back book and advice on how to modify physical activities specific to the individual's work situation ‐ only |
2. Contents of intense physical conditioning programme (PCP).
| Altmaier 1992 | Bendix 1996 | Bendix 1997 | Bendix 2000 | Bethge 2011 | Corey 1996 | Gatchel 2003 | Heymans 2006 | |
| Time span of training | 3 wks | 3 wks | 6 wks | 3 wks | 3 wks | 33 days | 3 wks | 8 wks |
| Number of sessions | 2 per day | 39 hrs per week + 3x6 hrs follow up | 135 hr in total | 39 hours per week + 3x6 hrs follow‐up | total of 82.2 hours of therapy | 6.5 hr per day | up to 41 | 2 per week |
| Length of sessions | ? | na | na | na | 1‐1.5 hrs | na | 15 min‐1hr | 1 hr |
| Full time | no | yes | yes | yes | yes | yes | no | no |
| group or individual | both | group | group | group | group | both | both | individual |
| exercises | yes | yes | yes | yes | yes | yes | yes | yes |
| work related exercises | yes | yes | yes | yes | yes | yes | yes | yes |
| operant conditioning behavioural approach | yes | yes | yes | yes | yes | yes | not clear | yes |
| pain coping/ management | yes | yes | yes | yes | unclear | yes | yes | no |
| back pain education | yes | yes | yes | yes | yes | yes | no | no |
| ergonomic advice or occupational training | no | occupational therapy and ergonomic training | occupational therapy and ergonomic training | occupational therapy and ergonomic training | no | no | occupational therapy | yes |
| return‐to‐work advice | no | no | no | no | yes | no | no | yes |
| workplace visit | no | no | no | no | no | no | no | no |
| therapists involved | multidisciplinary | multidisciplinary | multidisciplinary including physician, psychologist | occupational therapist, physician, psychologist,physical therapist, social worker | physician, social worker, psychologist, physical therapist | interdisciplinary programme | physiotherapist, occupational therapist, nurse, physician |
physiotherapist |
| other aspects | vocational rehabilitation | recreation activities | aerobics, recreational activities | recreation activities | no | no | no | CAU |
| comparison | PCP + CBT | CAU | exercise therapy / pain management | outpatient intensive physical training | inpatient conventional musculoskeletal rehabilitation | CAU | CAU | CAU‐only/ light PCP |
3. Contents of intense physical conditioning programme (PCP).
| Jensen 2001 | Kool 2005 | Lambeek 2010 | Lindstrom 1992 | Loisel 1997 | Meyer 2005 | Mitchell 1994 | Roche 2007 | |
| Time span of training | 4 wks | 3 wks | 12 wks | until RTW | 13 wks | 8 wks | 8 wks | 5 wks |
| Number of sessions | 6 sessions + 20 hrs exercise + 6 booster sessions |
4 hrs per day / 6 days a week | varying | approx. 11 with physical therapist, approx 10 self training sessions (3 per week) |
3,5 hr per day, 5 days a week | 6 hrs per day, 5 days a week | ||
| Lenght of sessions | ||||||||
| Full time | no | almost | no | no | unclear | almost | yes | yes |
| group or individual | both | group | individual | individual | unclear | both | group | group |
| exercises | yes | yes | yes | yes | yes | yes | yes | yes |
| work related exercises | yes | yes | yes | yes | yes | yes | yes | yes |
| operant conditioning behavioural approach | yes | no | yes | yes | yes | yes | yes | no |
| pain coping/ management | 2 didactic sessions on psychological aspects of pain + 2 sessions on medical aspects of pain |
no | no | no | no | yes | no | no |
| back pain education | yes | no | no | yes | yes | no | yes | no |
| ergonomic advice or occupational training | 2 sessions on ergonomics | work simulation | yes | no | yes, participatory ergonomics evaluation | education in ergonomics | no | occupational therapy |
| return‐to‐work advice | yes, workplace visit + rehabilitation plan | no | yes | yes | yes | yes | no | no |
| workplace visit | yes | no | yes | yes | yes | yes | no | no |
| therapists involved | physician, physical therapist, psychologist, | rheumatologist, physical and occupational therapist, sports therapist, social worker, nurse | clinical occupational physician, medical specialist, physiotherapist | physical therapist | back pain specialist; multidisciplinary medical, ergonomic and rehabilitation staff | interdisciplinary:rehabilitation physicians, psychologist, social worker, occupational therapist, physiotherapist | unclear | specialist in physical medicine, physiotherapist, psychologist |
| other aspects | no | no | CAU | CAU | CAU | case‐manager recreational activities |
no | no |
| comparison | CAU / CBT PCP + CBT |
pain centred treatment | CAU‐only | CAU‐only | CAU‐only | exercise therapy | CAU | active individual therapy |
4. Contents of intense physical conditioning programme (PCP).
| Skouen 2002 | Staal 2004 | Steenstra 2006 | Storheim 2003 | van den Hout 2003 | |
| Time span of training | 4 wks | max 3 months | 13 wks | 15 wks | 8 wks |
| Number of sessions | 5 per week for 4 weeks + follow‐up as in LMT | 2 per week until RTW | 2 per week 26 in total | 2‐3 per week | 28 |
| Lenght of sessions | 6 hr | 1 hr | 1 hr | 1 hr | 30‐90 min |
| Full time | almost | no | no | no | no |
| group or individual | both | individual | individual | group | both |
| exercises | yes | yes | yes | yes | yes |
| work related exercises | yes | yes | yes | not clear | yes |
| operant conditioning behavioural approach | yes | yes | yes | no | yes |
| pain/ coping management | no | no | no | no | no |
| back pain education | yes | no | no | no | yes |
| ergonomic advice or occupational training | yes | no | no | yes, training had a focus on ergonomic principles and functional tasks | yes, training by occupational therapist |
| return‐to‐work advice | no | yes | yes | no | yes |
| Workplace visit | no, occasional workplace intervention | no, but intervention was at workplace | no | no | yes, if necessary |
| therapists involved | physio therapist, nurse, psychologist | physiotherapist, occupational physician | physiotherapist, occupational physician | physical therapist | physiotherapist, occupational therapist, psychologist, occupational physician |
| other aspects | no | CAU/gradually increasing exercise, GP or occupational physician if workers wanted to | CAU/gradually increasing exercise | exercises accompanied by music | contact with patients' supervisor |
| comparison | CAU/ light PCP | CAU‐only | CAU‐only | CAU/ cognitive intervention | PCP + CBT |
Comparisons
There was a large variety of comparisons with physicial conditioning. The effectiveness of physical conditioning combined with usual care was compared to usual care in seven studies (Heymans 2006; Karjalainen 2003; Lambeek 2010; Lindstrom 1992; Loisel 1997; Staal 2004; Steenstra 2006). Usual care was mostly provided by a primary care physician without any restrictions on treatment such as referral or prescriptions. The studies by Heymans 2006; Staal 2004; Steenstra 2006 specifically mentioned the guidance of an occupational health physician in their usual care group. One study compared a multidisciplinary intervention involving a case manager who, together with the worker, constructed a tailored rehabilitation plan in addition to a brief clinical intervention (Jensen 2011). One study compared physical conditioning with a back book, workplace advice with a back book, and workplace advice only (Wright 2005). In nine studies physical conditioning was compared to care as usual (Bendix 1996; Bendix 1997; Bendix 2000; Corey 1996; Faas 1995; Gatchel 2003; Mitchell 1994; Skouen 2002; Storheim 2003). In six studies, exercise therapy was used as the comparison (Bendix 1997; Bendix 2000; Bethge 2011; Jensen 2001; Meyer 2005; Roche 2007). In two studies a comparison was made between light physical conditioning and intense physical conditioning (Heymans 2006; Skouen 2002); in two other studies a comparison was made between physical conditioning and physical conditioning with added CBT (delivered by psychologists) (Altmaier 1992; van den Hout 2003). Two studies compared physical conditioning with CBT (Bendix 1997; Jensen 2001). Two studies compared physical conditioning with multidisciplinary inpatient rehabilitation (Kool 2005; Bethge 2011). One study compared physical conditioning with a cognitive intervention that focused on explanation of pain mechanisms, staying active, and taking responsibility (Storheim 2003).
Follow‐up times varied from outcome data taken directly after a five‐week intervention up to three years. Five studies reported on short‐term follow‐up: three months (Bendix 1996; Kool 2005; Roche 2007; Storheim 2003; Wright 2005); eight studies reported on intermediate‐term follow‐up: six months (Altmaier 1992; Bethge 2011; Heymans 2006; Meyer 2005; Roche 2007; Staal 2004; Steenstra 2006; van den Hout 2003); 18 studies reported on long‐term follow‐up: one year (Bendix 1996; Bendix 1997; Bendix 2000; Bethge 2011; Corey 1996; Faas 1995; Gatchel 2003; Jensen 2001; Jensen 2011; Karjalainen 2003; Kool 2005; Lambeek 2010; Lindstrom 1992; Loisel 1997; Mitchell 1994; Staal 2004; Steenstra 2006; van den Hout 2003); and six studies reported on very long‐term follow‐up (Bendix 1996; Bendix 1997; Jensen 2001; Karjalainen 2003; Loisel 1997; Staal 2004), varying between two and three years.
Outcomes
All studies reported on work status, most often measured as mean days of sick leave until follow‐up or return‐to‐work rate at follow‐up. Several studies reported on 'work readiness' or work capability (Bendix 1996; Bendix 1997; Bendix 2000; Skouen 2002), and one study reported on percentages of full‐time workability (Meyer 2005). The data from these studies were recalculated in order to allow pooling of the data. For example, data on full work days of workers were extracted from the follow‐up days to calculate the sick leave days. For studies that measured mean days of sick leave, the results were shown using the SMD. Results from studies that reported on return‐to‐work rate were shown using odds ratios (OR). There were six studies that reported hazard ratios for return‐to‐work (Heymans 2006; Jensen 2001; Jensen 2011; Lambeek 2010; Staal 2004; Steenstra 2006). These data were recalculated or the authors were asked to provide mean days of sick leave to make it possible to pool the data with other study results.
We found four studies (Altmaier 1992; Loisel 1997; Roche 2007; Wright 2005) that reported on other work status outcomes, such as part‐time return‐to‐work, return to 'light' duties, or 'therapeutic' return‐to‐work. However, only the data from Altmaier 1992 and Roche 2007 could actually be used. Wright 2005 did not provide separate data on the change to or from 'light' duties, and Loisel 1997 only mentioned in the results section that analyses with return to any work as an outcome showed no significant benefit in any group or combination of groups.
Clinical relevance
Seven out of 25 studies scored positive on all the five questions regarding clinical relevancy (Bendix 1997; Karjalainen 2003; Kool 2005; Lambeek 2010; Lindstrom 1992; Loisel 1997; Staal 2004). All studies clearly explained the type of workers that participated in the intervention. Only one study (Altmaier 1992) scored a 'no' on the question about the clarity of the intervention. Two studies scored a 'no' on: 'were all clinically relevant outcomes measured and reported' (Corey 1996; Storheim 2003). With the recalculation of data into SMD or OR we found seven studies that scored positive on the fourth question: 'Is the size of the effect clinically important?' (Bendix 1997; Karjalainen 2003; Kool 2005; Lambeek 2010; Lindstrom 1992;Loisel 1997; Staal 2004). By consensus, we considered that the fifth question 'whether the likely treatment benefits would be worth the potential harms' would be scored positive for all studies as there was no apparent harm for the worker with these type of interventions. However, we realize that this is debatable and this topic therefore needs to be further explored (see Table 5).
5. Clinical relevance.
| Study ID | 1 | 2 | 3 | 4 | 5 |
| Altmaier 1992 | + | ‐ | + | ‐ | + |
| Bendix 1996 | + | + | + | ‐ | + |
| Bendix 1997 | + | + | + | + | + |
| Bendix 2000 | + | + | + | ‐ | + |
| Bethge 2011 | + | + | + | ‐ | + |
| Corey 1996 | + | + | ‐ | ‐ | + |
| Faas 1995 | + | + | + | ‐ | + |
| Gatchel 2003 | + | + | + | ‐ | + |
| Heymans 2006 | + | + | + | ‐ | + |
| Jensen 2001 | + | + | + | ‐ | + |
| Jensen 2011 | + | + | + | ‐ | + |
| Karjalainen 2003 | + | + | + | + | + |
| Kool 2005 | + | + | + | + | + |
| Lambeek 2010 | + | + | + | + | + |
| Lindstrom 1992 | + | + | + | + | + |
| Loisel 1997 | + | + | + | + | + |
| Meyer 2005 | + | + | + | ‐ | + |
| Mitchell 1994 | + | + | + | ‐ | + |
| Staal 2004 | + | + | + | + | + |
| Steenstra 2006 | + | + | + | ‐ | + |
| Storheim 2003 | + | + | ‐ | ‐ | + |
| Skouen 2002 | + | + | + | ‐ | + |
| Roche 2007 | + | + | + | ‐ | + |
| van den Hout 2003 | + | + | + | ‐ | + |
| Wright 2005 | + | + | + | ‐ | + |
Excluded studies
From the original and previously updated review, 13 studies were excluded because the interventions from those studies had no clear relationship with the work situation or functional job demands, the majority of workers were not on sick leave at baseline, or the outcome was not return‐to‐work (Alaranta 1994; Aure 2003; Bentsen 1997; Dahl 2001; Dettori 1995; Friedrich 1998; Hagen 2000; Hansen 1993; Kellett 1991; Linton 2005; Malmivaara 1995; Moffett 1999; Niemisto 2003; Schiltenwolf 2006; Seferlis 1998; Torstensen 1998). With the new search, another three studies were excluded because the majority of workers were not on sick leave at baseline due to low‐back pain (Rantonen 2012; Whitfill 2010), or physical conditioning was not considered a structural part of the intervention (Bültmann 2009).
Risk of bias in included studies
The risk of bias of the studies was independently assessed by two review authors (LE, AB), who used a consensus method if disagreements occurred. We used the 12 criteria recommended by the Back Review Group (Furlan 2009) to assess the risk of bias of the selected RCTs. The criteria are outlined in Appendix 2. Each of the criteria were scored 'high', 'low' or 'unclear'. Between the two risk of bias assessors, there were an average of one or two items of disagreement for every study. All disagreements were resolved after discussion. For the newly included studies, we sent the results of our risk of bias assessment to the (first) authors of the RCTs when there were answers with a 'high' or 'unclear' assessment asking them to comment on our scores, especially if the answers were 'unclear', and to provide us with additional information. We used the data on risk of bias of the originally included studies from the original review and did not ask those authors for comment.
Six authors responded to questions concerning the risk of bias tables and another four authors responded to questions concerning outcome data, leading to three changes in the risk of bias tables.
Following the advice of Furlan 2009, studies were rated as having a ‘high risk of bias’ if they had serious flaws (for example inadequate concealment of treatment allocation) or had met fewer than six of the risk of bias criteria. We found two studies (Corey 1996; Mitchell 1994 ) with a high risk of bias because they did not meet at least six of the risk of bias criteria. Another seven studies (Altmaier 1992; Bendix 1996; Bendix 1997; Gatchel 2003; Lindstrom 1992; Mitchell 1994; Roche 2007) were considered to have a high risk of bias because of unclear or no allocation concealment. The other 16 studies were considered to have a low risk of bias (Figure 1).
Effects of interventions
The included studies covered the following comparisons.
Acute back pain
1. Light physical conditioning and back book with advice versus back book with advice (N = 1) (Wright 2005)
2. Light physical conditioning versus care as usual (N = 1) (Faas 1995)
3. Intense physical conditioning versus care as usual (N = 1) (Gatchel 2003)
Subacute back pain
4. Light physical conditioning with care as usual versus care as usual (N = 2) (Heymans 2006; Karjalainen 2003)
5. Light physical conditioning and brief clinical intervention versus brief clinical intervention (N = 1) (Jensen 2011)
6. Intense physical conditioning with care as usual versus care as usual (N = 5) (Heymans 2006; Lindstrom 1992; Loisel 1997; Staal 2004; Steenstra 2006)
7. Intense physical conditioning versus light physical conditioning (N = 2) (Heymans 2006)
8. Intense physical conditioning versus cognitive intervention (N = 1) (Storheim 2003)
9. Intense physical conditioning versus care as usual (N = 1) (Storheim 2003)
10. Intense physical conditioning versus multidisciplinary exercise treatment (N = 2) (Bethge 2011; Kool 2005)
Chronic back pain
11. Light physical conditioning versus care as usual (N = 1) (Skouen 2002)
12. Intense physical conditioning with care as usual versus care as usual (N = 1) (Lambeek 2010)
13. Intense physical conditioning versus care as usual (N = 5) (Bendix 1996; Corey 1996; Jensen 2001; Mitchell 1994; Skouen 2002)
14. Intense physical conditioning versus an exercise programme (N = 5) (Bendix 1997; Bendix 2000; Meyer 2005; Roche 2007)
15. Intense physical conditioning versus intense physical conditioning with CBT (N = 3) (Altmaier 1992; Jensen 2001; van den Hout 2003)
16. Intense physical conditioning versus CBT (N = 2) (Bendix 1997; Jensen 2001)
17. Intense physical conditioning versus light physical conditioning (N = 1) (Skouen 2002)
Despite the heterogeneity of studies with respect to duration of back pain, comparison of treatment, follow‐up time and effect measure, we were able to pool some studies in specific subgroups and perform several meta‐analyses.
Acute back pain
Three studies reported on the effect of physical conditioning on work status for workers with acute back pain. Due to different type of comparisons none of the studies could be pooled.
1. Light physical conditioning and back book versus back book
One RCT with low risk of bias (Wright 2005) (80 workers) reported low quality evidence that there was no difference in the reduction of the proportion of workers off work at two‐month follow‐up between light physical conditioning and GP advice with a back book compared to GP advice with a back book only for workers with acute back pain, with an OR of 0.36 (95% CI 0.13 to 1.03).
2. Light physical conditioning versus care as usual
One RCT with low risk of bias (Faas 1995) (190 workers) reported low quality evidence that there was no difference in the reduction of mean days off work at one‐year follow‐up between light physical conditioning and care as usual for workers with acute back pain, with a SMD of ‐0.02 (95% CI ‐0.30 to 0.27).
3. Intense physical conditioning versus care as usual
One RCT with high risk of bias (Gatchel 2003) (70 workers) reported low quality evidence that there was no difference in the reduction of the proportion of workers off work at one‐year follow‐up between intense physical conditioning and care as usual for workers with acute back pain, with an OR of 0.22 (95% CI 0.05 to 1.06).
Subacute back pain
4. Light physical conditioning and care as usual versus care as usual
Intermediate follow‐up
One RCT with low risk of bias (Heymans 2006) (299 workers) reported low quality evidence that there was no difference in sickness absence duration at six‐month follow‐up when comparing light physical conditioning and care as usual to care as usual only for workers with subacute back pain, with a SMD of ‐0.18 (95% CI ‐0.45 to 0.10).
Long‐ and very long‐term follow‐up
Another RCT with low risk of bias (Karjalainen 2003) (112 workers) reported low quality evidence that there was no difference in sickness absence duration at one‐and two‐year follow‐up when comparing a light mobilization and graded activity programme to a workplace visit with care as usual and care as usual only for workers with subacute back pain, with a SMD of ‐0.35 (95% CI ‐0.74 to 0.03) and a SMD of ‐0.30 (95% CI ‐0.69 to 0.09), respectively.
5. Light physical conditioning with a brief clinical intervention versus a brief clinical intervention
One RCT with low risk of bias (Jensen 2011) (351 workers) reported low quality evidence that there was no difference in sickness absence duration at one‐year follow‐up when comparing a multidisciplinary intervention (that is case manager and worker constructed a tailored rehabilitation plan in addition to a brief clinical intervention) to a brief clinical intervention only for workers with subacute back pain at one‐year follow‐up, with a SMD of 0.21 (95% CI 0.00 to 0.42).
6. Intense physical conditioning with care as usual versus care as usual
Intermediate follow‐up
Three RCTs reported conflicting evidence on the effect of intense physical conditioning with care as usual versus care as usual for workers with subacute back pain at intermediate‐term follow‐up (Heymans 2006; Staal 2004; Steenstra 2006). We found high statistical heterogeneity when all three studies were pooled (I² = 75%). We compared the components of the three physical conditioning programmes and their style of delivery and found that Staal 2004 differed from the other two studies in that the intervention was conducted at the workplace. This RCT with low risk of bias (Staal 2004) (134 workers) reported that intense physical conditioning may be more effective than usual care at reducing the time to return‐to‐work, with a SMD of ‐ 0.42 (95% CI ‐0.76 to ‐0.08). In contrast, pooling the other two RCTs with low risk of bias (Heymans 2006; Steenstra 2006) (313 workers) resulted in low quality evidence that there was no difference in sickness absence duration between intense physical conditioning with care as usual versus care as usual for workers with subacute back pain at intermediate‐term follow‐up, with a pooled SMD of 0.13 (95% CI ‐0.09 to 0.35).
Long‐term follow‐up
Four RCTs reported conflicting evidence on the effect of intense physical conditioning with care as usual versus care as usual for workers with subacute back pain at long‐term follow‐up. Again, we found high statistical heterogeneity when all four studies were pooled (I² = 78%). We compared the components of the four physical conditioning programmes and their style of delivery and found that Steenstra 2006 differed from the other three studies in that no workplace visit was included in their physical conditioning. Lindstrom 1992 and Loisel 1997 had an explicit workplace visit included in their programme, and Staal 2004 executed the intervention at the workplace. This RCT with low risk of bias (Steenstra 2006) (112 workers) reported that care as usual alone was more effective in reducing sickness absence duration than physical conditioning plus care as usual, with a SMD of 0.39 (95% CI 0.02 to 0.77). In contrast, pooling the other three RCTs, one with high and two with low risk of bias (Lindstrom 1992; Loisel 1997; Staal 2004) (283 workers), showed that intense physical conditioning with explicit workplace involvement plus care as usual compared to care as usual only was more effective and clinically relevant in reducing the time to return‐to‐work, with a pooled SMD of ‐0.42 (95% CI ‐0.65 to ‐0.18) (Figure 2).
2.
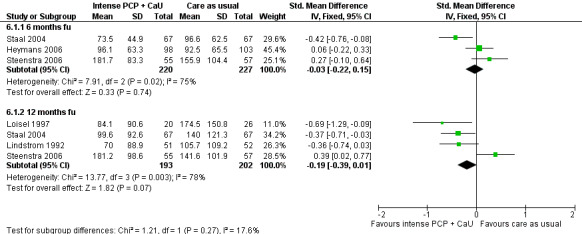
Forest plot of comparison: 7 Intense PC + CaU versus CaU only, subacute pain, outcome: 7.3 Time to return‐to‐work.
Very long‐term follow‐up
The pooled results of two RCTs, one with a high and one with a low risk of bias (Lindstrom 1992; Staal 2004) (257 workers), showed moderate quality evidence that intense physical conditioning with care as usual was more effective in reducing sickness absence duration compared to care as usual only for workers with subacute back pain at very long‐term follow‐up (two years), with a pooled SMD of ‐0.39 (95% CI ‐0.76 to ‐0.02) (Figure 3).
3.
Forest plot of comparison: 11 Intense PC versus multidisciplinary exercise treatment, subacute pain, outcome: 11.1 Proportion off work short‐term follow‐up.
7. Intense physical conditioning versus light physical conditioning
One RCT with low risk of bias (Heymans 2006) (196 workers) reported low quality evidence that there was no difference in sickness absence duration between light physical conditioning and intense physical conditioning for workers with subacute back pain at intermediate‐term follow‐up (six‐month), with a SMD of ‐0.24 (95% CI ‐0.52 to 0.04). Both interventions were combined with care as usual.
8. Intense physical conditioning versus a cognitive intervention
One RCT with low risk of bias (Storheim 2003) (64 workers) reported low quality evidence that physical conditioning consisting of intensive group training with a focus on ergonomic principles and functional tasks was no more effective in reducing time to return to work compared with a cognitive intervention for workers with subacute back pain at 18‐week follow‐up, with a SMD of ‐0.10 (95% CI ‐0.59 to 0.40). The cognitive intervention was provided by a specialist in physical medicine and a physical therapist, and consisted of two consultations in which pain mechanisms were explained, reassurance was given, and advice and instructions were given on how to stay active and use muscles for demanding tasks.
9. Intense physical conditioning versus care as usual
One RCT with low risk of bias (Storheim 2003) (59 workers) reported low quality evidence that there was no difference in sickness absence duration between an intense physical conditioning programme and care as usual for workers with subacute back pain at 18‐week follow‐up, with a SMD of ‐0.10 (95% CI ‐0.61 to 0.41).
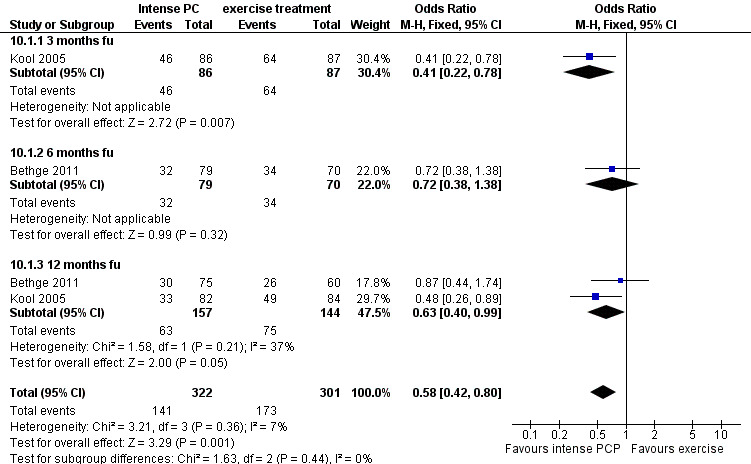
10. Intense physical conditioning versus multidisciplinary exercise treatment
Short‐term follow‐up
One RCT with low risk of bias (Kool 2005) (173 workers) reported low quality evidence that intense physical conditioning was more effective and clinically worthwhile than a multidisciplinary exercise treatment with a focus on pain reduction in reducing the proportion of workers off work, for workers with subacute back pain at short‐term (three months) follow‐up, with an OR of 0.41 (95% CI 0.22 to 0.78).
Intermediate‐term follow‐up
One RCT with low risk of bias (Bethge 2011) (149 workers) reported low quality evidence that intense physical conditioning was not more effective than a conventional musculoskeletal rehabilitation programme in reducing the proportion of workers off work, for workers with subacute back pain at intermediate‐term (six months) follow‐up, with an OR of 0.72 (95% CI 0.40 to 0.99).
Long‐term follow‐up
The pooled results of two RCTs with low risk of bias (Bethge 2011; Kool 2005) (301 workers) showed moderate quality evidence that intense physical conditioning was more effective and clinically worthwhile than a multidisciplinary exercise treatment in reducing the proportion of workers off work, for workers with subacute back pain at long‐term (12 months) follow‐up, with a pooled OR of 0.63 (95% CI 0.40 to 0.99) (Figure 3).
Chronic back pain
11. Light physical conditioning versus care as usual
One RCT with low risk of bias (Skouen 2002) (106 workers) reported low quality evidence that there was no difference in sickness absence duration between a light physical conditioning programme and usual care at one‐ and two‐year follow‐up, with a SMD of ‐0.33 (95% CI ‐0.67 to 0.02) and a SMD of ‐0.34 (95% CI ‐0.69 to 0.01) respectively, for workers with chronic back pain.
12. Intense physical conditioning with care as usual versus care as usual
One RCT with low risk of bias (Lambeek 2010) (134 workers) reported low quality evidence that intense physical conditioning with care as usual was more effective and clinically worthwhile than care as usual only for workers with chronic back pain in reducing duration of sickness absence, with a SMD of ‐4.42 (95% CI ‐5.06 to ‐3.79) at long‐term (12 months) follow‐up. The physical conditioning in this study was part of an integrated care protocol of three elements: integrated care management by a clinical occupational physician, workplace intervention and graded activity.
13. Intense physical conditioning versus care as usual
Short‐term follow‐up
One RCT with high risk of bias (Bendix 1996) (74 workers) reported very low quality evidence that intense physical conditioning was more effective and clinically worthwhile than care as usual for workers with chronic back pain in reducing the proportion of workers off work in the short‐term (four months), with an OR of 0.16 (95% CI 0.05 to 0.49).
Long‐term follow‐up
The pooled results of five RCTs (Bendix 1996; Corey 1996; Jensen 2001; Mitchell 1994; Skouen 2002) (1093 workers) showed moderate quality evidence that intense physical conditioning was more effective than care as usual for workers with chronic back pain in reducing the time to return‐to‐work at long‐term follow‐up. However, the size of the effect may not be clinically worthwhile with a SMD of ‐0.23 (95% CI ‐0.42 to ‐0.03). This comparison included workers who at baseline were on full or partial sick leave as well as workers who were at work but reported work disability (Figure 4).
4.
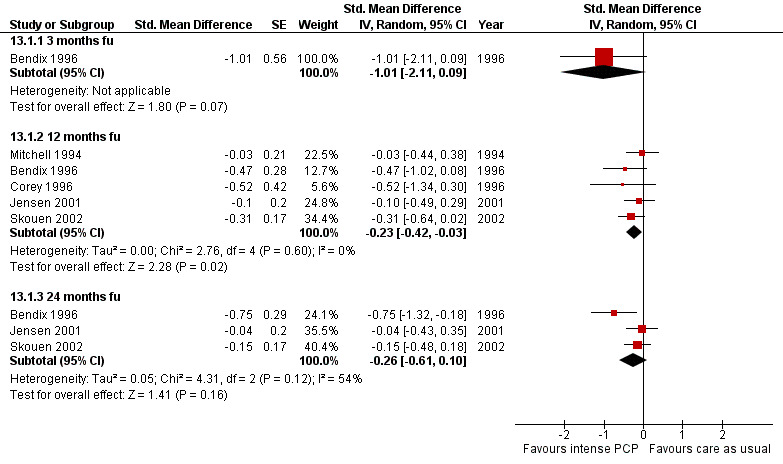
Forest plot of comparison: Intense PCP versus care as usual for workers with chronic back pain, outcome: Time to return‐to‐work at long‐term follow‐up
A sensitivity analysis of studies in which all workers were on full‐time sick leave due to chronic back pain at baseline (Corey 1996; Jensen 2001; Mitchell 1994) showed no difference in sickness absence duration between intense physical conditioning and exercise treatment at long‐term follow‐up (12 to 18 months), with a pooled SMD of ‐0.14 (95% CI ‐0.39 to 0.11).
The same effect was reported for another sensitivity analysis when only the two studies with low risk of bias (Jensen 2001; Skouen 2002) were included in this comparison, with a pooled SMD of ‐0.13 (95% CI ‐0.38 to 0.12).
Further subgroup analyses of differences in components of physical conditioning of these five studies did not change the results.
Very long‐term follow‐up
The pooled results of three RCTs (Bendix 1996; Jensen 2001; Skouen 2002) (297 workers) showed moderate quality evidence that intense physical conditioning was not more effective than care as usual for workers with chronic back pain in reducing sick leave time at two‐ to three‐year follow‐up, with a pooled SMD of ‐0.26 (95% CI ‐0.61 to 0.10) (Figure 4).
14. Intense physical conditioning versus exercise treatment
Four studies measured the effects of intense physical conditioning versus exercise treatment for workers with chronic back pain on the mean number of days off work or return‐to‐work rate at various follow‐up times.
Short‐term follow‐up
One RCT with high risk of bias (Roche 2007) (136 workers) reported very low quality evidence that intense physical conditioning was no more effective than active individual exercise therapy for workers with chronic back pain in reducing the proportion of workers off work, measured directly after the intervention programme of five weeks, with an OR of 1.00 (95% CI 0.37 to 2.70).
This study also reported on workers returning to any type of work (full time, partial or work adaptation) and again showed no difference in effect on return to any type of work.
Intermediate‐term follow‐up
The pooled results of two RCTs with a high risk of bias (Meyer 2005; Roche 2007) (114 workers) showed low quality evidence that there was no difference between intense physical conditioning and exercise treatment for workers with chronic back pain in the reduction of time to return‐to‐work at six‐month follow‐up, with a SMD of 0.19 (95 CI ‐0.63 to 0.24). The study by Meyer 2005 was actually a pilot study for a larger trial (Figure 5).
5.
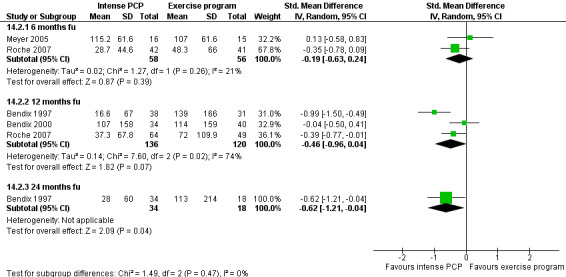
Forest plot of comparison: Intense PCP versus exercise programme for workers with chronic back pain, outcome: Time to return‐to‐work at intermediate‐term follow‐up.
Long‐term follow‐up
Three RCTs reported conflicting evidence on the effect of intense physical conditioning for workers with chronic back pain at long‐term follow‐up versus an exercise treatment. Due to high statistical heterogeneity, results could not be pooled (I² = 74%). Further analysis of components between the three physical conditioning programmes showed no differences. Two studies (Bendix 1997, high risk of bias; Roche 2007 low risk of bias) (182 workers) showed low quality evidence of a clinically worthwhile effect in favour of intense physical conditioning, with a SMD of ‐0.67 (95% CI ‐1.26 to ‐0.08). However, another RCT with high risk of bias from the same authors (Bendix 2000) (74 workers) showed very low quality evidence that there was no difference in effect, with a SMD of ‐0.04 (95% CI ‐0.50 to 0.41).
Very long‐term follow‐up
One RCT with high risk of bias (Bendix 1997) (52 workers) reported very low quality evidence that intense physical conditioning was more effective and clinically worthwhile than exercise therapy for workers with chronic back pain in reducing the time to return‐to‐work at very long‐term follow‐up (two years), with a SMD of ‐0.62 (95% CI ‐1.21 to ‐0.04).
15. Intense physical conditioning versus intense physical conditioning with CBT
Three studies reported on intense physical conditioning versus intense physical conditioning with CBT for workers with chronic back pain (Altmaier 1992; Jensen 2001; van den Hout 2003).
Intermediate‐term follow‐up
The pooled results of two RCTs with high and low risk of bias (Altmaier 1992; van den Hout 2003) (126 workers) showed low quality evidence that there was no difference in the reduction of the proportion of workers off work between intense physical conditioning and intense physical conditioning with CBT at the six‐month follow‐up, with a SMD of 0.26 (95% CI ‐0.50 to 1.03) (Figure 6).
6.
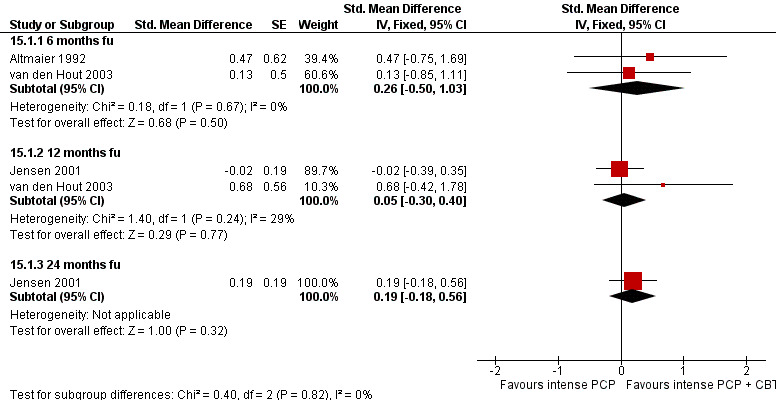
Forest plot of comparison: Intense PCP versus intense PCP with CBT for workers with chronic back pain, outcome: Time to return‐to‐work at long‐term follow‐up.
Altmaier 1992 also reported on the effectiveness of intense physical conditioning that included CBT for workers returning to full‐time work and for those who had made constructive efforts toward re‐employment. They concluded that this was not more effective in reducing the proportion of workers who were off work when compared with intense physical conditioning without CBT.
Long‐term follow‐up
The pooled results of two RCTs with low risk of bias (Jensen 2001; van den Hout 2003) (193 workers) showed moderate quality evidence that there was no difference in the reduction of sickness absence between intense physical conditioning without CBT and intense physical conditioning with CBT at one‐year follow‐up, with a pooled SMD of 0.05 (95% CI ‐0.30 to 0.40) (Figure 6).
Very long‐term follow‐up
One RCT with low risk of bias (Jensen 2001) (117 workers) reported low quality evidence that there was no difference in the reduction of time off work between intense physical conditioning without CBT and an intense physical conditioning programme with CBT at the 36‐month follow‐up, with a SMD of 0.19 (95% CI ‐0.18 to 0.56).
16. Intense physical conditioning versus CBT
Two studies measured the effect of intense physical conditioning versus CBT for workers with chronic back pain (Bendix 1997; Jensen 2001). CBT in these studies was delivered by psychologists. When studies were pooled, we found high statistical heterogeneity that may have been caused by differences in components of the physical conditioning. Further analysis showed that Jensen 2001 included a workplace visit and explicit return‐to‐work advice in their programme. However, these two components were also available for the control situation and therefore we have not been able to explain the high statistical heterogeneity.
Long‐ and very long‐term follow‐up
One RCT with high risk of bias (Bendix 1997) (57 workers) reported very low quality evidence of a clinically worthwhile effect in reducing the number of workers off work in favour of intense physical conditioning compared with CBT after one and two years follow‐up, with an OR of 0.04 (95% CI 0.01 to 0.17) and an OR of 0.14 (95% CI 0.05 to 0.43) respectively.
Another RCT with low risk of bias (Jensen 2001) (103 workers) reported low quality evidence of a clinically worthwhile effect in reducing time off work in favour of intense physical conditioning compared with CBT after one and a half years follow‐up, with a SMD of ‐0.46 (95% CI ‐0.85 to ‐0.07), but this effect was gone after three years with a SMD of ‐0.13 (95% CI ‐0.51 to 0.26).
17. Intense physical conditioning versus light physical conditioning
One RCT with low risk of bias (Skouen 2002) (109 workers) reported low quality evidence that there was no difference between intense physical conditioning and light physical conditioning in reducing the time to return‐to‐work for workers with chronic back pain at the one‐ and two‐year follow‐up, with a SMD of 0.10 (95% CI ‐0.28 to 0.48) and SMD of 0.20 (95% CI ‐0.18 to 0.58) respectively.
Discussion
Summary of main results
We included 25 studies in this updated review that evaluated the effectiveness of physical conditioning as part of a return to work strategy for workers with back pain. Based on these studies, we analysed 17 comparisons and were able to pool data in a few cases. There was high statistical heterogeneity and conflicting results about the effect of intense physical conditioning versus care as usual for workers with subacute back pain. Further exploration of the components of the physical conditioning programmes using subgroup analysis pointed towards a positive effect of a workplace visit included in the programme. However, these results were based on indirect evidence only and we should therefore be cautious to reach any conclusions. Moreover, high statistical heterogeneity and conflicting results were found for the effect of intense physical conditioning versus exercise treatment, which could not be explained by differences in components or style of delivery of the programmes. Our review showed the following results.
(1) There is low quality evidence that for workers with acute back pain both light and intense physical conditioning may have little or no impact on sickness absence duration compared with care as usual.
(2) There is low quality evidence that for workers with subacute back pain light physical conditioning may have little or no impact on sickness absence duration compared with care as usual. In addition, a multidisciplinary intervention supplementing a brief clinical intervention does not have added value in terms of return to work compared to a brief clinical intervention only.
(3) The evidence on the effectiveness of intense physical conditioning with care as usual versus care as usual only in workers with subacute back pain is conflicting. Further subgroup analysis shows that if the intervention is executed at the workplace, or includes a workplace visit, it may reduce sickness absence duration at intermediate and long‐term follow‐up based on low quality evidence.There is moderate quality evidence for this effect at the very long‐term follow‐up.
(4) Based on moderate quality evidence intense physical conditioning probably reduces sickness absence duration for workers with subacute back pain at long‐term follow‐up compared with a multidisciplinary exercise treatment. However, based on low quality evidence there may be no or little difference in effect at intermediate follow‐up, but physical conditioning may again reduce sickness absence duration at short‐term follow‐up.
(5) Based on low quality evidence, intense physical conditioning may have little or no effect in reducing sickness absence duration compared with a cognitive intervention for workers with subacute back pain at short‐term follow‐up.
(6) Based on moderate quality evidence, intense physical conditioning probably slightly reduces duration of sickness absence compared with care as usual for workers with chronic back pain, but only at long‐term follow‐up. Based on low quality evidence intense physical conditioning together with care as usual may reduce sickness absence duration compared with care as usual, but only at long‐term follow‐up.
(7) The evidence on the effectiveness of intense physical conditioning programmes versus exercise therapy for workers with chronic back pain at long‐term follow‐up is conflicting and missing at other follow‐up times.
(8) There is low quality evidence that intense physical conditioning without a workplace component may have little or no effect on sickness absence duration compared with light physical conditioning for workers with subacute and chronic back pain.
(9) There is very low to moderate quality evidence that CBT is probably not superior to physical conditioning as an alternative or in addition to physical conditioning.
Overall completeness and applicability of evidence
The objective of this updated review was to compare the effectiveness of work‐related physical conditioning in reducing time lost from work or improving work status for workers with back pain. Return to work and improving work status are the most important and relevant outcome measures in occupational health care. Other outcome measures such as functional status, psychological well‐being and satisfaction with the treatment are also important, however we chose to focus only on sickness absence and work status in an attempt to simplify this complex study topic.
Due to the variety of interventions, comparisons and follow‐up times, there were no studies available for some comparisons and only single studies for others. In this update we divided comparisons between physical conditioning in addition to care as usual and physical conditioning only. This resulted in 17 comparisons with physical conditioning. The comparisons with light physical conditioning programmes only included single studies. Because most included studies had small sample sizes, the results of the light physical conditioning programmes were not significantly effective, but had 95% confidence intervals that included the possibility of a clinically worthwhile effect. Therefore the effects of light physical conditioning programmes are still uncertain.
Another issue is the high statistical heterogeneity in the comparison of intense physical conditioning versus usual care. We ascribed this to differences in components of the physical conditioning programmes. We reported further subgroup analyses in an attempt to explain differences in the effect of physical conditioning programmes. Workplace involvement in the intervention may explain the positive results reported for intense physical conditioning versus usual care for workers with subacute back pain. However, no new studies were found to confirm added value for physical conditioning versus exercise therapy for chronic back pain. For these types of workers the evidence remains conflicting at long‐term follow‐up.
This updated review has good external validity because the participants in the trials resemble workers in occupational health practice and the interventions are considered feasible to carry out in daily medical practice. However, there may be differences in social benefit systems between the countries in which the studies were carried out, which may have an additional effect on the return‐to‐work outcome.
Quality of the evidence
Sixteen of the 25 studies that were included were assessed as having a low risk of bias. Eight studies had serious flaws due to unclear or no allocation concealment. Sparse data due to the small number of participants in most studies lowered the quality of the evidence further. The three newly included studies were all of high quality (Bethge 2011; Jensen 2011; Lambeek 2010). Due to the new division of comparisons in this updated version of the review there were 17 comparisons for the included studies. This complicated further pooling of studies and therefore the conclusion of the previous updated review (Schaafsma 2010) is still accurate.
The effectiveness of interventions with involvement of the workplace is supported by current literature (Anema 2007; van Oostrom 2009). It is argued that workplace‐based interventions can change both workers' and supervisors' perceptions about the workers' return‐to‐work capabilities and opportunities (Anema 2007). In our review, a subgroup analysis of interventions that were done at the workplace or included a workplace visit seems to point towards a positive effect when a workplace intervention is included in an intense physical conditioning programme. The positive effect of workplace involvement is also substantiated with the newly included high quality study of Lambeek 2010 for chronic back pain. In this study the physical conditioning was part of integrated care management with particular workplace involvement. What part of this integrated care management was actually (most) effective is unclear.
In the meta‐regression analysis based on the studies of the previous review (Schaafsma 2011), involvement of the workplace provided no explanation for any difference in effect of physical conditioning as part of a return to work strategy. This meta‐regression analysis will therefore need to be updated with these three new studies. In this updated review we found that for subacute back pain intense physical conditioning is more effective than exercise therapy at long‐term follow‐up. The difference between physical conditioning and exercise lies in the explicit objective of enabling the individual to return to work in the conditioning programmes (Schaafsma 2011). However, for workers with both subacute and chronic back pain the results of included studies did not clearly and consistently support physical conditioning over exercise therapy at different follow‐up times. The additional effect of the focus on return to work within physical conditioning compared to exercise therefore remains unclear. Furthermore, the study of Jensen 2011 also reported that no additional effect could be measured for a multidisciplinary intervention on top of a clinical intervention in terms of return to work. Therefore, also for subacute back pain the addtional effect of a return to work focus remains unclear.
For workers with chronic back pain, the combined results did show there is a small positive effect of intense physical conditioning in the long term compared with usual care. However, this combined result may not be clinically worthwhile according to our definition. The meta‐analysis consisted of five studies (Bendix 1996; Corey 1996; Mitchell 1994; Jensen 2001; Skouen 2002). The study by Lambeek 2010 differed from these five as they compared physical conditioning in addition to care as usual. However, it can be argued that the participants in this study did not receive any additional care as usual. Besides, it is not always clear what care as usual is. It might still be that alternative interventions use fewer resources and thus are less costly but equally effective. For example, there was one small study that showed no difference in return to work between physical conditioning programmes and a cognitive intervention that consisted of only two consultations. These consultations focused on explaining pain mechanisms, advice on how to stay active and take responsibility, and were delivered by a physical medicine specialist. More research is needed to clarify if such a 'light' intervention is actually enough to help workers with subacute back pain return to work.
The original review also highlighted the need for effective physical conditioning programmes to have a cognitive behavioural approach. In the previously updated review, we defined the cognitive behavioural approach (CBA) as an intervention component that encouraged workers with back pain to focus on functional gains rather than pain, as defined by Fordyce 1976. A CBA was included in 16 out of the 25 studies, mostly as a graded activity approach. A subgroup analysis of studies with a CBA included in their intervention could not be done because CBA was either included in all studies or in none of the meta‐analyses reported.
We found that the effectiveness of physical conditioning is not consistent at different times of follow‐up. Intuitively one would expect that the effect of physical conditioning is largest at the end of the intervention programme, with the effect then gradually wearing off. However, for intense physical conditioning with workplace intervention versus care as usual, there is a non‐significant outcome at short‐term follow‐up but significant outcomes at longer‐term follow‐up. This phenomenon, that the intervention is only effective at long‐term follow‐up, was also seen in some single studies. It might be that this is not due to the mechanism of the intervention but is the result of publication bias by which only positive long‐term results are published and not the negative ones.
We did not find that other aspects of the intervention. such as involvement of an occupational health physician, specific return‐to‐work advice, inclusion of ergonomic advice or specific occupational training, influenced time lost from work.
Other possible explanations for the high statistical heterogeneity of included studies may be the differences in healthcare or social security systems between countries. Also, different type of workers, for example blue collar versus white collar workers between studies or the type of industry branch, may have an impact on sickness absence. However, we did not have the opportunity to extensively study this.
Potential biases in the review process
In this updated review, we pooled data whenever possible. For this purpose we had to recalculate data from the original studies for example odds ratios and mean differences into standard mean differences (SMDs). These recalculations sometimes resulted in different conclusions than those reported by the authors. Differences could be attributed to recalculation of workability into sickness absence and recalculation to standard deviations from studies when only P values or 95% CIs were provided in the original literature. The advantage of using SMD was that it increased the number of possible meta‐analyses.
Further, in the original review it was stated that the minimal clinically worthwhile effect in reduction of sick leave was set at a number needed to treat (NNT) of 10 (odds ratio (OR) < 0.65) based on the consideration that an intervention that affected less than one in 10 people would not be clinically worthwhile. In this updated version we maintained this original size of minimal clinically worthwhile effect. Because of our use of SMDs for the meta‐analysis, the set OR of less than 0.65 as the minimal clinically worthwhile effect was also recalculated back to a SMD of less than ‐0.24.
Agreements and disagreements with other studies or reviews
Results of this updated Cochrane review are supported by previously published systematic reviews, even though their scope and methods are different. However, there are no existing reviews that focus solely on return to work with specific exercise interventions that have an explicit relation with work. In an older review by Ostelo 2000, it was found that CBT has no added value compared with waiting list controls on short‐term pain relief for chronic low‐back pain and no difference in effect was found between CBT and exercise. This finding supports the current review as the results of intense physical conditioning in terms of return to work are better than CBT in the long term but show no difference in effect in the very long term.
Our results are also in line with another more recent systematic review on specific functional restoration programmes that concluded that return‐to‐work improved when programmes incorporated the provision of suitable modified duties (Poiraudeau 2007). In this review, we found that physical conditioning programmes that particularly included workplace involvement reduced sickness absence for workers with subacute or chronic back pain compared to care as usual.
A Cochrane review on the effectiveness of back schools reported that there is moderate evidence suggesting that back schools for chronic low‐back pain in an occupational setting are more effective than other treatments, placebo, or waiting lists on pain, functional status and return to work during short‐ and intermediate‐term follow‐up (Heymans 2005). In the current updated review, back school interventions were only considered as physical conditioning programmes if there was a relationship with the work situation. We confirm that for workers with chronic back pain, intense physical conditioning in addition to care as usual is significantly more effective in reducing sick leave time compared with care as usual only. However, this result is based on one study only. In addition, physical conditioning only compared to care as usual may only have a small effect, which may not be clinically worthwhile in the long term, based on five studies.
A Cochrane review on the effectiveness of exercise therapy showed positive results for improving pain and function at short‐term follow‐up. Further, this review found evidence for effectiveness of graded activity exercise programmes in subacute low‐back pain in occupational settings, although the evidence for other types of exercise therapy in other populations is inconsistent (Hayden 2005). Since these conclusions are based on the same studies, these findings are not surprising.
Authors' conclusions
Implications for practice.
For workers with acute and subacute back pain, there was only low quality evidence regarding the effects of physical conditioning on sickness absence duration. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Implications for practice are therefore uncertain.
For workers with chronic back pain, there is moderate quality evidence that intense physical conditioning probably reduces sickness absence duration slightly compared to care as usual. The effect may not be clinically relevant, although further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Implications for practice are therefore uncertain.
Implications for research.
More than half of the included studies showed a low risk of bias, especially for the most recent studies, which implies that high quality studies are feasible in this area. More studies are needed that compare the effect of physical conditioning as part of coordinated and tailored work rehabilitation programmes in addition to usual care versus usual care only for workers with back pain. More research is also needed to understand the mechanism behind physical conditioning and return to work at different times of follow‐up and for various durations of back pain. Qualitative research would be an appropriate tool to reveal ideas and attitudes of workers that could be important factors in return to work. We recommend that work outcomes of new research are reported as the mean number of full‐time and part‐time sick days and analysed as censored events with survival analysis.
Feedback
Effect of CBT versus CBT + exercise
Summary
: Jan 5, 2005. Would be interesting to see the comparison between CBT and CBT‐exercise programme to see if there was additive benefit of exercise.
Reply
: Jan 5, 2005. A response was sent directly to Dr Hardy, in which he was referred to the updated review on 'Behavioural treatment for chronic low‐back pain', published in The Cochrane Library 2005 (1), for this comparison.
Contributors
: Vicki Pennick
What's new
| Date | Event | Description |
|---|---|---|
| 5 June 2013 | New citation required but conclusions have not changed | Conclusions have not changed. |
| 5 June 2013 | New search has been performed | 3 new trials were incorporated into this update. |
History
Protocol first published: Issue 4, 1999 Review first published: Issue 1, 2003
| Date | Event | Description |
|---|---|---|
| 19 January 2011 | Amended | Contact details updated. |
| 17 February 2010 | Amended | typos corrected in abstract and plain language summary |
| 9 June 2009 | New citation required and conclusions have changed | New GRADE approach to assessment of the quality of the evidence led to change in conclusions. |
| 30 June 2008 | New search has been performed | inclusion/exclusion criteria, methodology and outcome measures revised. Based on changes, literature search updated. New criteria led to exclusion of 12 studies from the previous review. Revised and updated search led to inclusion of 15 new studies. |
| 22 May 2008 | Amended | Converted to new review format. |
| 23 May 2003 | Amended | Issue 3, 2003 The authors of this review have made one modification since Issue 2, 2003. They removed the sensitivity analysis and subsequent tables (01/02) as they discovered an error with the data entered. Accordingly, they have also modified relevant text and removed one reference (Altman 2001). |
| 30 April 2003 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Rachel Couban from the Cochrane Back Review Group who updated and refined the literature searches.
Appendices
Appendix 1. MEDLINE search strategy
Search strategy for MEDLINE (Ovid):
1 randomized controlled trial.pt.
2 controlled clinical trial.pt.
3 randomized.ab.
4 placebo.ab,ti.
5 drug therapy.fs.
6 randomly.ab,ti.
7 trial.ab,ti.
8 groups.ab,ti.
9 or/1‐8
10 (animals not (humans and animals)).sh.
11 9 not 10
12 dorsalgia.ti,ab.
13 exp Back Pain/
14 backache.ti,ab.
15 exp Low Back Pain/
16 (lumbar adj pain).ti,ab.
17 coccyx.ti,ab.
18 coccydynia.ti,ab.
19 sciatica.ti,ab.
20 sciatic neuropathy/
21 spondylosis.ti,ab.
22 lumbago.ti,ab.
23 or/12‐22
24 work conditioning.mp.
25 work hardening.mp.
26 functional restoration.mp.
27 exercise$.mp. or exp Exercise/
28 gym$ prog$.mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
29 disability evaluation.mp. or exp Disability Evaluation/
30 exp Work/
31 exp Work Capacity Evaluation/
32 worker$.mp.
33 or/24‐32
34 11 and 23 and 33
35 limit 34 to yr="2008 ‐ 2012"
36 limit 34 to ed=20080601‐20120320
37 35 or 36
Appendix 2. Criteria for assessing risk of bias for internal validity
Random sequence generation (selection bias)
Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence
There is a low risk of selection bias if the investigators describe a random component in the sequence generation process such as: referring to a random number table, using a computer random number generator, coin tossing, shuffling cards or envelopes, throwing dice, drawing of lots, minimisation (minimisation may be implemented without a random element, and this is considered to be equivalent to being random).
There is a high risk of selection bias if the investigators describe a non‐random component in the sequence generation process, such as: sequence generated by odd or even date of birth, date (or day) of admission, hospital or clinic record number; or allocation by judgement of the clinician, preference of the participant, results of a laboratory test or a series of tests, or availability of the intervention.
Allocation concealment (selection bias)
Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment
There is a low risk of selection bias if the participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based and pharmacy‐controlled randomisation); sequentially numbered drug containers of identical appearance; or sequentially numbered, opaque, sealed envelopes.
There is a high risk of bias if participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on: using an open random allocation schedule (e.g. a list of random numbers); assignment envelopes were used without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; or other explicitly unconcealed procedures.
Blinding of participants
Performance bias due to knowledge of the allocated interventions by participants during the study
There is a low risk of performance bias if blinding of participants was ensured and it was unlikely that the blinding could have been broken; or if there was no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding.
Blinding of personnel and care providers (performance bias)
Performance bias due to knowledge of the allocated interventions by personnel and care providers during the study
There is a low risk of performance bias if blinding of personnel was ensured and it was unlikely that the blinding could have been broken; or if there was no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding.
Blinding of outcome assessor (detection bias)
Detection bias due to knowledge of the allocated interventions by outcome assessors
There is low risk of detection bias if the blinding of the outcome assessment was ensured and it was unlikely that the blinding could have been broken; or if there was no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding, or:
for patient‐reported outcomes in which the patient was the outcome assessor (e.g. pain, disability): there is a low risk of bias for outcome assessors if there is a low risk of bias for participant blinding (Boutron 2005);
for outcome criteria that are clinical or therapeutic events that will be determined by the interaction between patients and care providers (e.g. co‐interventions, length of hospitalisation, treatment failure), in which the care provider is the outcome assessor: there is a low risk of bias for outcome assessors if there is a low risk of bias for care providers (Boutron 2005);
for outcome criteria that are assessed from data from medical forms: there is a low risk of bias if the treatment or adverse effects of the treatment could not be noticed in the extracted data (Boutron 2005).
Incomplete outcome data (attrition bias)
Attrition bias due to amount, nature or handling of incomplete outcome data
There is a low risk of attrition bias if there were no missing outcome data; reasons for missing outcome data were unlikely to be related to the true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data were balanced in numbers, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with the observed event risk was not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, the plausible effect size (difference in means or standardised difference in means) among missing outcomes was not enough to have a clinically relevant impact on observed effect size, or missing data were imputed using appropriate methods (if drop‐outs are very large, imputation using even 'acceptable' methods may still suggest a high risk of bias) (van Tulder 2003). The percentage of withdrawals and dropouts should not exceed 20% for short‐term follow‐up and 30% for long‐term follow‐up and should not lead to substantial bias (these percentages are commonly used but arbitrary, not supported by literature) (van Tulder 2003).
Selective reporting (reporting bias)
Reporting bias due to selective outcome reporting
There is low risk of reporting bias if the study protocol is available and all of the study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way, or if the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon).
There is a high risk of reporting bias if not all of the study's pre‐specified primary outcomes have been reported; one or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis; the study report fails to include results for a key outcome that would be expected to have been reported for such a study.
Group similarity at baseline (selection bias)
Bias due to dissimilarity at baseline for the most important prognostic indicators.
There is low risk of bias if groups are similar at baseline for demographic factors, value of main outcome measure(s), and important prognostic factors (examples in the field of back and neck pain are duration and severity of complaints, vocational status, percentage of patients with neurological symptoms) (van Tulder 2003).
Co‐interventions (performance bias)
Bias because co‐interventions were different across groups
There is low risk of bias if there were no co‐interventions or they were similar between the index and control groups (van Tulder 2003).
Compliance (performance bias)
Bias due to inappropriate compliance with interventions across groups
There is low risk of bias if compliance with the interventions was acceptable, based on the reported intensity or dosage, duration, number and frequency for both the index and control intervention(s). For single‐session interventions (e.g. surgery), this item is irrelevant (van Tulder 2003).
Intention‐to‐treat‐analysis
There is low risk of bias if all randomised patients were reported and analysed in the group to which they were allocated by randomisation.
Timing of outcome assessments (detection bias)
Bias because important outcomes were not measured at the same time across groups
There is low risk of bias if all important outcome assessments for all intervention groups were measured at the same time (van Tulder 2003).
Other bias
Bias due to problems not covered elsewhere in the table
There is a low risk of bias if the study appears to be free of other sources of bias not addressed elsewhere (e.g. study funding).
Appendix 3. GRADE criteria
The GRADE criteria were operationalised in the following way.
Limitations of the study refers to the risk of bias assessment of studies. Studies with more than 5 points on the risk of bias assessment were regarded as studies with a low risk of bias. If 75% or more of the studies scored above 5, this item was scored as: no limitations. If between 50% and 75% of the studies scored above 5, this was scored as: serious limitations. If less that 50% of the studies scored above 5: very serious limitations.
Consistency refers to the similarity of estimates of treatment effects for the outcome across studies. Study results were considered consistent if direction, effect size and statistical significance were sufficiently similar to lead to the same conclusions. Consistency in direction was defined as 75% or more of the studies showing either benefit or no effect of the workplace intervention. In the case of a benefit, consistency in effect size was defined as 75% or more of the studies showing a clinically important or unimportant effect. Minimal clinically relevant differences were derived from the original review as mentioned above in the quantitative analysis. Consistency in statistical significance was defined by the Chi2 test for heterogeneity.
Directness (generalisability) refers to the extent to which the workers, interventions, and outcomes in the studies were comparable to those defined in the inclusion criteria of the review. If there was uncertainty about generalisablity of the results, or if the results were more applicable to a specific population than a general population on work disability, serious or very serious limitations were assigned.
Precision of the evidence refers to the confidence in the results. It takes into account the number of studies, patients, and events; and width of the CIs for each outcome. Data were interpreted to be imprecise as multiple studies were combined in a meta‐analysis but the CI (confidence interval) was sufficiently wide that the estimate could either support or refute the effectiveness of the workplace intervention. In the case of imprecise data serious limitations were assigned. Serious limitations could also be assigned if data were judged to be sparse, that is if only one study was available for an outcome, or fewer than 75% of the studies presented data that could be included in the meta‐analysis.
Publication bias refers to the probability of selective publication of studies and outcomes.
The overall quality of the evidence for each outcome was the result of the combination of the assessments in all domains.
Data and analyses
Comparison 1. Light physical conditioning programme (PCP) + backbook versus backbook intervention only, acute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion off work | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 3 months fu | 1 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
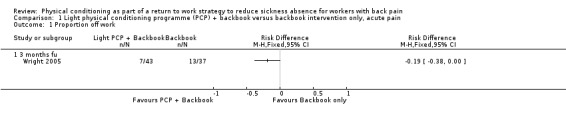
Comparison 1 Light physical conditioning programme (PCP) + backbook versus backbook intervention only, acute pain, Outcome 1 Proportion off work.
Comparison 2. Light physical conditioning programme (PCP) versus care as usual (CaU), acute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work long term follow up | 1 | 190 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.30, 0.27] |
| 1.1 12 months fu | 1 | 190 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.30, 0.27] |
2.1. Analysis.
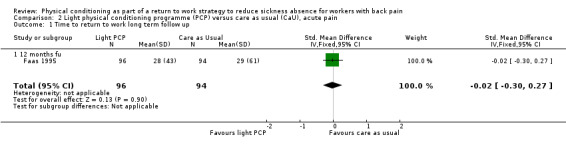
Comparison 2 Light physical conditioning programme (PCP) versus care as usual (CaU), acute pain, Outcome 1 Time to return to work long term follow up.
Comparison 3. Intense physical conditioning programme (PCP) versus care as usual (CaU), acute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion off work long term follow up | 1 | 70 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 1.06] |
3.1. Analysis.
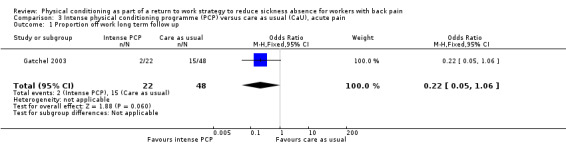
Comparison 3 Intense physical conditioning programme (PCP) versus care as usual (CaU), acute pain, Outcome 1 Proportion off work long term follow up.
Comparison 4. Light physical conditioning programme (PCP) + care as usual (CaU) versus CaU, subacute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 6 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 12 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 24 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
4.1. Analysis.
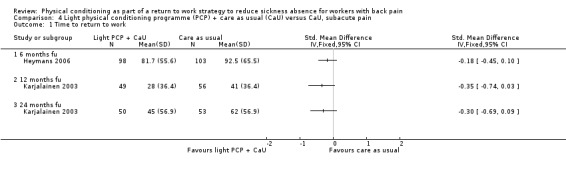
Comparison 4 Light physical conditioning programme (PCP) + care as usual (CaU) versus CaU, subacute pain, Outcome 1 Time to return to work.
Comparison 5. Light physical conditioning programme (PCP) + brief clinical intervention (CI) versus brief CI only, subacute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 1 | 351 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.21 [0.00, 0.42] |
| 1.1 12 months fu | 1 | 351 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.21 [0.00, 0.42] |
5.1. Analysis.
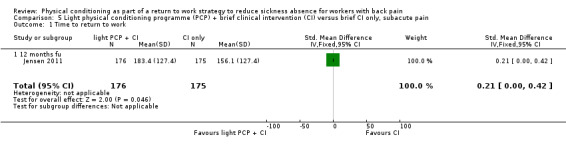
Comparison 5 Light physical conditioning programme (PCP) + brief clinical intervention (CI) versus brief CI only, subacute pain, Outcome 1 Time to return to work.
Comparison 6. Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, subacute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 5 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months fu | 3 | 447 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.22, 0.15] |
| 1.2 12 months fu | 4 | 395 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.39, 0.01] |
| 2 Time to return to work very long term follow up | 2 | Std. Mean Difference (Fixed, 95% CI) | ‐0.39 [‐0.76, ‐0.02] |
6.1. Analysis.
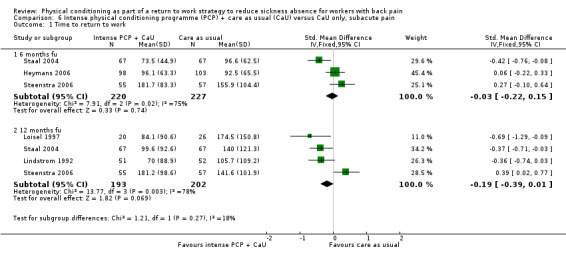
Comparison 6 Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, subacute pain, Outcome 1 Time to return to work.
6.2. Analysis.
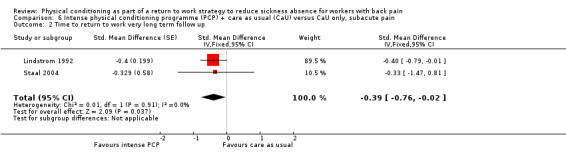
Comparison 6 Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, subacute pain, Outcome 2 Time to return to work very long term follow up.
Comparison 7. Intense physical conditioning programme (PCP) versus light PCP, subacute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 6 months fu | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
7.1. Analysis.
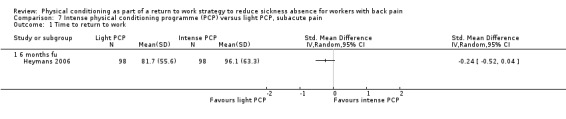
Comparison 7 Intense physical conditioning programme (PCP) versus light PCP, subacute pain, Outcome 1 Time to return to work.
Comparison 8. Intense physical conditioning programme (PCP) versus cognitive intervention, subacute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work short term follow up | 1 | 64 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.59, 0.40] |
8.1. Analysis.
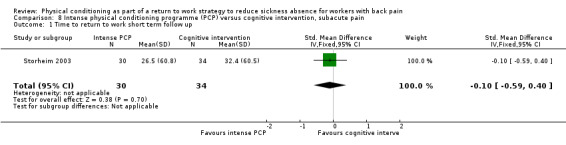
Comparison 8 Intense physical conditioning programme (PCP) versus cognitive intervention, subacute pain, Outcome 1 Time to return to work short term follow up.
Comparison 9. Intense physical conditioning programme (PCP) versus care as usual (CaU), subacute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐7.20 [‐43.64, 29.24] |
| 1.1 3 months fu | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐7.20 [‐43.64, 29.24] |
9.1. Analysis.
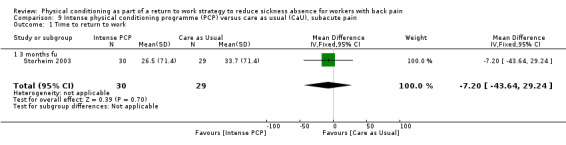
Comparison 9 Intense physical conditioning programme (PCP) versus care as usual (CaU), subacute pain, Outcome 1 Time to return to work.
Comparison 10. Intense physical conditioning programme (PCP) versus multidisciplinary exercise treatment, subacute pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion off work short term follow up | 2 | 623 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.42, 0.80] |
| 1.1 3 months fu | 1 | 173 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.22, 0.78] |
| 1.2 6 months fu | 1 | 149 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.38, 1.38] |
| 1.3 12 months fu | 2 | 301 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.40, 0.99] |
10.1. Analysis.
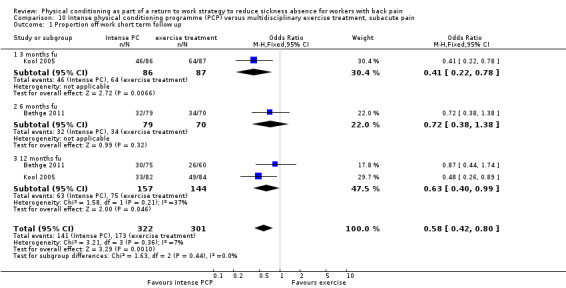
Comparison 10 Intense physical conditioning programme (PCP) versus multidisciplinary exercise treatment, subacute pain, Outcome 1 Proportion off work short term follow up.
Comparison 11. Light physical conditioning programme (PCP) versus care as usual (CaU), chronic pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 12 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 24 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
11.1. Analysis.
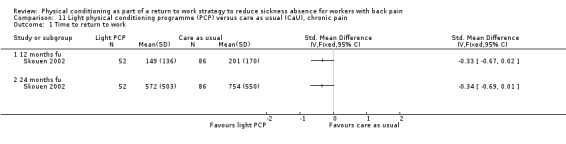
Comparison 11 Light physical conditioning programme (PCP) versus care as usual (CaU), chronic pain, Outcome 1 Time to return to work.
Comparison 12. Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, chronic pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to Return to Work | 1 | Std. Mean Difference (Fixed, 95% CI) | ‐4.42 [‐5.06, ‐3.79] | |
| 1.1 12 months fu | 1 | Std. Mean Difference (Fixed, 95% CI) | ‐4.42 [‐5.06, ‐3.79] |
12.1. Analysis.
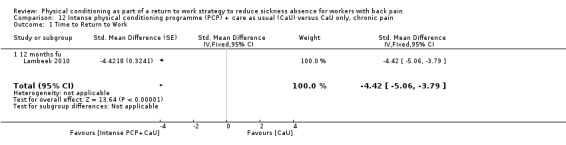
Comparison 12 Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, chronic pain, Outcome 1 Time to Return to Work.
Comparison 13. Intense physical conditioning programme (PCP) versus care as usual (CaU), chronic pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 5 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 3 months fu | 1 | Std. Mean Difference (Random, 95% CI) | ‐1.01 [‐2.11, 0.09] | |
| 1.2 12 months fu | 5 | Std. Mean Difference (Random, 95% CI) | ‐0.23 [‐0.42, ‐0.03] | |
| 1.3 24 months fu | 3 | Std. Mean Difference (Random, 95% CI) | ‐0.26 [‐0.61, 0.10] |
13.1. Analysis.
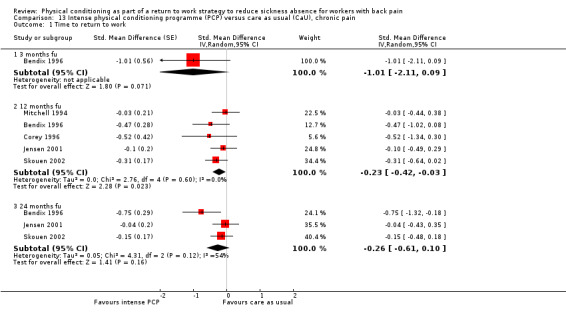
Comparison 13 Intense physical conditioning programme (PCP) versus care as usual (CaU), chronic pain, Outcome 1 Time to return to work.
Comparison 14. Intense physical conditioning programme (PCP) versus exercise program, chronic pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion off work short term follow up | 1 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.37, 2.70] |
| 2 Time to return to work | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 6 months fu | 2 | 114 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.63, 0.24] |
| 2.2 12 months fu | 3 | 256 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.96, 0.04] |
| 2.3 24 months fu | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.21, ‐0.04] |
14.1. Analysis.
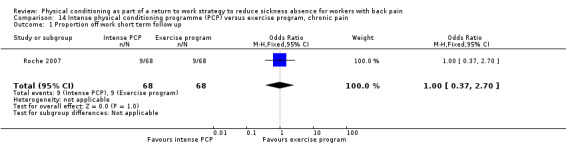
Comparison 14 Intense physical conditioning programme (PCP) versus exercise program, chronic pain, Outcome 1 Proportion off work short term follow up.
14.2. Analysis.
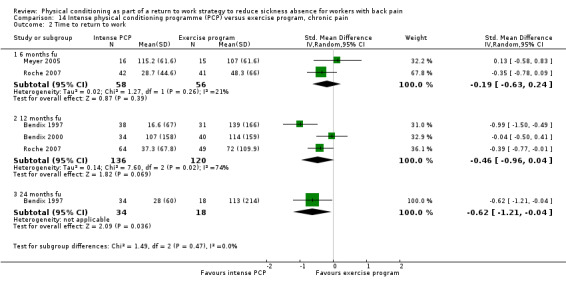
Comparison 14 Intense physical conditioning programme (PCP) versus exercise program, chronic pain, Outcome 2 Time to return to work.
Comparison 15. Intense physical conditioning programme (PCP) versus intense PCP + cognitive behavioural therapy (CBT), chronic pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 3 | Std. Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months fu | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.26 [‐0.50, 1.03] | |
| 1.2 12 months fu | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [‐0.30, 0.40] | |
| 1.3 24 months fu | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.19 [‐0.18, 0.56] |
15.1. Analysis.
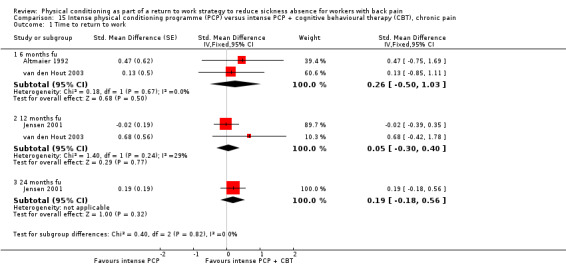
Comparison 15 Intense physical conditioning programme (PCP) versus intense PCP + cognitive behavioural therapy (CBT), chronic pain, Outcome 1 Time to return to work.
Comparison 16. Intense physical conditioning programme (PCP) versus cognitive behavioural therapy (CBT) for workers with chronic back pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 2 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 12 months fu | 2 | Std. Mean Difference (Random, 95% CI) | ‐1.75 [‐4.45, 0.95] | |
| 1.2 24 months fu | 2 | Std. Mean Difference (Random, 95% CI) | ‐0.47 [‐1.36, 0.42] |
16.1. Analysis.
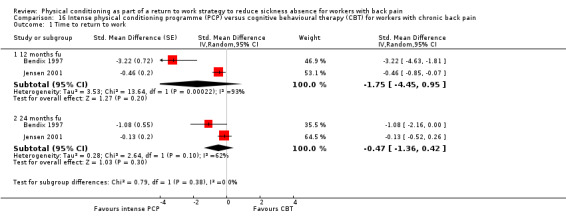
Comparison 16 Intense physical conditioning programme (PCP) versus cognitive behavioural therapy (CBT) for workers with chronic back pain, Outcome 1 Time to return to work.
Comparison 17. Intense physical conditioning programme (PCP) versus light PCP, chronic back pain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time to return to work | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 12 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 24 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
17.1. Analysis.
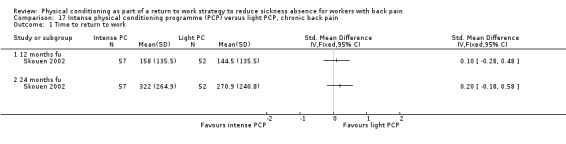
Comparison 17 Intense physical conditioning programme (PCP) versus light PCP, chronic back pain, Outcome 1 Time to return to work.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Altmaier 1992.
| Methods | RCT | |
| Participants | Workers (33 males and 12 females) disabled and not working due to low‐back pain for at least 3 month duration, with or without referred pain, mean age 39.91(8.91). | |
| Interventions | Intervention 1 : Standard treatment programme was a in‐patient, multidisciplinary approach to assisting workers in returning to function, that included twice daily sessions of physical therapy and daily aerobic fitness training to increase activity tolerance levels. Daily education classes on mechanisms of pain and group support were also added. Vocational rehabilitation was included through group and individual educational sessions. In addition, patients' medication intake was monitored (n =24). Intervention 2 : Psychological programme included in addition to the standard treatment programme an operant conditioning component involving daily charting of exercise behaviour, with contingent verbal praise, daily relaxation and biofeedback sessions. Group and individual training sessions to teach cognitive behavioural coping skills such as reconceptualisation of pain as an experience were also included. In addition, patients completed daily home work exercises that were reviewed with them on a daily basis (n = 21). Programme duration: three weeks. |
|
| Outcomes | Outcome assessed at 6 months after treatment. Return to employment (conservative ie full employment at same job; and liberal measures ie if full time on light duties or part‐time work or training) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Does not state |
| Allocation concealment (selection bias) | Unclear risk | Does not state |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Does not state |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care provider aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | All subjects recorded follow‐up data |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | 21 subjects in each group analysed (there was 2 workers in psychological group) |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | no statistical significant differences between groups in terms of demographic differences |
| Co‐interventions avoided or similar? | Low risk | no co‐interventions mentioned |
| Compliance acceptable? | Unclear risk | measured, but not reported what was considered non‐compliant |
| Timing of the outcome assessment similar? | Low risk | all measurements post‐treatment programme at 6 months |
Bendix 1996.
| Methods | RCT | |
| Participants | workers (28 males and 66 females) with low‐back pain with or without radiation for over 6 months. 78% not working or on suitable duties. | |
| Interventions | Intervention 1(A1) : A combination of 3 modalities was offered: 1. Intensive physical training including aerobic capacity, coordination, muscle strength, and endurance, flexibility, stretching exercises, work hardening, ergonomic training and recreation including ball games, swimming for 5 hrs/day. 2. Psychological pain management that included relaxation and biofeedback for 2 hours a day guided by the clinical psychologist. 3. Patient education of 1 hour/day on a variety of topics led by physicians, therapists, psychologists, social worker and nutritionist (n = 50). Programme duration: a full day (eight hour) programme every weekday for three consecutive weeks followed by a full day per week during the following three weeks (Total: 135 hours). Control: CAU: consisted of no treatment offered, but patients could receive treatment elsewhere. 80% reported seeking treatment elsewhere mostly traditional physical therapy with passive modalities (61%) and manipulation by chiropractor (35%). |
|
| Outcomes | Outcome assessed at 12 months. 1. Ability to work (5 categories); 2. contacts with healthcare system; 3. number of sick leave days; 4. back pain (scale of 0‐10); 5. leg pain (scale 0‐10); 6. activities of daily living (scale 0‐30) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Does not state |
| Allocation concealment (selection bias) | High risk | Does not state |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | The project was blinded in that the physician who saw the the patients for the initial examination and the 4‐month follow‐up did not know which group each patient was in. The same physician saw all the patients in both groups throughout the study. The blinding was broken in about 10% of the cases. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 2 before the treatment programme, 7 during the programme |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | dropouts not analysed at follow‐up |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | no significant differences |
| Co‐interventions avoided or similar? | High risk | intervention group had significantly less contacts with healthcare system than control group |
| Compliance acceptable? | Low risk | except for the dropouts. |
| Timing of the outcome assessment similar? | Low risk | all workers were analysed at baseline and after 4 months |
Bendix 1997.
| Methods | RCT | |
| Participants | Workers (28 males and 75 females) with chronic low‐back pain for over 6 months, and 73% not working or on suitable duties. | |
| Interventions | Intervention 1(B1): A combination of 3 modalities was offered: 1. Intensive physical training including aerobic capacity, coordination, muscle strength, and endurance, flexibility, stretching exercises, work hardening, ergonomic training and recreation including ball games, swimming for 5 hrs/day. 2. Psychological pain management that included relaxation and biofeedback for 2 hours a day guided by the clinical psychologist. 3. Patient education of 1 hour/day on a variety of topics led by physicians, therapists, psychologists, social worker and nutritionist (n = 50). Programme duration: a full day (eight hour) programme every week day for three consecutive weeks followed by a full day per week during the following three weeks (Total: 135 hours). Intervention 2 (B2): Outpatient programme for small group (7‐8) people receiving physical training: 45 min aerobics and 45 min progressive resistance training, twice a week for 6 weeks. One hour of theoretical back school lessons every second day. Intervention 3 (B3): Outpatient programme for small group (7‐8) people receiving 45 min physical training and 75 min psychological pain management. Twice a week for 6 weeks. |
|
| Outcomes | Measurement at 1 year after randomization. 1. Ability to work (5 categories); 2. Contacts with healthcare system; 3. Number of sick leave days; 4. Back pain (scale 0‐10); 5. Leg pain (scale 0‐10); 6. Activities of daily living (scale 0‐30); 7. Use of prescription medication (%); 8. Sports activity (%); 9. Overall assessment (scale 1‐5) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | randomization procedure followed minimization principle |
| Allocation concealment (selection bias) | High risk | Does not state |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Unclear risk | physician was blinded to treatment allocation, but the blinding was broken by patients in about 10% of cases. Unsure regarding RTW outcomes |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 14 out of 123 patients dropped out |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | dropouts not analysed at follow‐up |
| Selective reporting (reporting bias) | Low risk | No suggestion found |
| Similarity of baseline characteristics? | Low risk | No differences found |
| Co‐interventions avoided or similar? | High risk | All groups had contact with other health professionals before follow‐up |
| Compliance acceptable? | Low risk | 14 out of 123 did not complete programme |
| Timing of the outcome assessment similar? | Low risk | all subjects follow‐up at 1 year after completion of programme |
Bendix 2000.
| Methods | RCT | |
| Participants | 138 workers with chronic low‐back pain from Copenhagen Back Center of which 54% were sick listed; mean age 40, 32% men | |
| Interventions | Intervention: Function Restoration programme, including aerobics, strengthening excercises, occupational therapy, pain management/ group therapy or individual psychological sessions, stretching, theory/back school classes and recreational activities. 3 week schedule full time (8hrs per day) Control: Outpatient intensive physical training including aerobics and strenghtening exercises for 3x1, 5 hr for 8 weeks |
|
| Outcomes | Measurement at 1 year after treatment: work capability, number of sick leave days | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | stratification by minimization |
| Allocation concealment (selection bias) | Unclear risk | does not state |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | at 1 year follow‐up evaluation a few queries were discussed with the physician, who was blinded to treatment each specific patient had undergone. This blinding was successful for approx 80% of the patients, but relevant for less than half of the patients because most of them had filled out their quesitonnaire before their meeting with physician |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 21 out of 127 dropped out |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | intention‐to‐treat data were analysed but provided data were per protocol |
| Selective reporting (reporting bias) | Low risk | No suggestion found |
| Similarity of baseline characteristics? | High risk | not regarding sick leave; work capability better for FR group |
| Co‐interventions avoided or similar? | Unclear risk | no other interventions mentioned |
| Compliance acceptable? | Unclear risk | does not state |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 1 year |
Bethge 2011.
| Methods | cluster RCT | |
| Participants | 236 patients with MSDs resulting in severe restriction of work ability and who requested rehabilitation. Inclusion criteria were at least 12 weeks of sick leave in the year before rehabilitation OR subjective expectation of long‐term restrictions affecting occupational duties OR health‐related unemployment | |
| Interventions | Multimodal work hardening: a three week inpatient group programme for 6‐10 patients with 6 modules: work and health; occupational competence; exercise; aquatic exercise; functional capacity training; relaxation. Conventional musculoskeletal rehabilitation: 3 weeks inpatients therapy including exercises, patient education, and psychosocial interventions. |
|
| Outcomes | Work status at 6 and 12 months defined as positive if the patient was working and had <6 or <12 (after 12 months) weeks of sick leave. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated random numbers blocked to two sequences of 16 numbers |
| Allocation concealment (selection bias) | Low risk | Performed externally by the method centre of the Rehabilitation Research Association of Berlin‐Brandenburg‐Saxony |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Unclear risk | no report |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients were aware of their treatment |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers were not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | High risk | questionnaires after 6 and 12 months follow‐up were completed and returned by 169 (71.6%) and 146 (61.9%) patients, respectively |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | intention‐to‐treat analysis regardless of premature dropout |
| Selective reporting (reporting bias) | Low risk | No suggestion found |
| Similarity of baseline characteristics? | Low risk | two differences in parameters at baseline were considered as covariates in the analyses |
| Co‐interventions avoided or similar? | Unclear risk | no report |
| Compliance acceptable? | Low risk | treatment was completed according to protocol in 5 out of 6 modules for 91.5% of the MWH participants |
| Timing of the outcome assessment similar? | Low risk | at 6 and 12 months follow‐up |
Corey 1996.
| Methods | RCT | |
| Participants | 214 workers, with work related soft tissue injury and off work between 3 to 6 months. More than 50% had low‐back pain. | |
| Interventions | Intervention 1: Functional restoration approach: active physical therapy including stretching, strengthening and endurance building; work hardening; education and counselling to address pain related disability issues, attitudinal barriers to recovery, job satisfaction and entitlements, depression, anger and anxiety, medication reduction, sleep disruption, family problems and pain behaviours. Patients were also taught active pain management strategies, stress management and problem solving techniques, relaxation and guided imagery techniques as well as a multidimensional theory of pain. The emphasis was on acquisition of active strategies rather than reliance on passive methods to manage pain (n = 74). Programme duration: maximum of thirty five days at 6.5 hours per day. Intervention 2: Contol group: patients were discharged back to their treating physicians with a note re assessment findings, and recommendation for pro‐active management, including advice to limit narcotic medication and encourage activity despite pain (n = 64). |
|
| Outcomes | Outcome assessed at 18 months. 1. Self‐reported work status (dichotomous, 2 versions, %); 2. Pain rating (scale 0‐10); 3. Sleep rating (scale 1‐3); 4. Mean reported narcotic intake (pills/week). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "following intake, the claimant was randomly assigned to a treatment of usual care condition by an employee of the WCB, who was blind to the results of the intake assessment" |
| Allocation concealment (selection bias) | Low risk | Adequate |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | outcome assessor had no familiarity with the patients or the programme and was blind as to the patients group status |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | High risk | 26% for treatment and 36% for control dropped out, which could have led to substantial bias according to the authors |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | "only 74% and 64% in each group respectively were available for analysis" |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | subjects were screened in order to make sure all workers were similar in terms of prognostic indicators |
| Co‐interventions avoided or similar? | Unclear risk | does not state |
| Compliance acceptable? | Unclear risk | does not state |
| Timing of the outcome assessment similar? | High risk | 17 months ‐ 18.9 months |
Faas 1995.
| Methods | RCT | |
| Participants | 363 workers (240 males and 123 females) aged 16‐65 (mean age 36) with acute (< 3 weeks) pain radiating above knee who consulted their GP for back pain. 64% of workers had reported full sick leave at study entry. | |
| Interventions | Intervention 1: 20 minutes of individual instruction from a physiotherapist, consisting of 8 exercises and 7 pieces of advice applying to daily life, including work. Exercises (in supine) were: semi‐fowler resting position, knees on chest, limbering exercise, stretching of iliopsoas, pelvic flexion, isometric abdominal exercises. The patients were taught anatomy, and were given instructions on how to stand, bend, lift, and carry objects. Work Work difficulties and problems performing the exercises were discussed, and attempts were made, together with the patient, to find solutions in order to maximise compliance. Patients received an audiotape, as well as a book with complete instructions (n = 96). Programme duration: five weeks, twice weekly. Intervention 2: (usual care): information given by GP regarding cause and course of back pain. The role of GP was to exclude other specific causes of back pain, emphasise the importance of heat, movement and short‐lasting bed rest to deal with back pain, and the requirement of return visits by the patient to the GP for follow up (n = 94). |
|
| Outcomes | Measurement at 12 months after treatment. 1. Sickness absence during the follow‐up period (% of N; several levels); 2. Absence during back pain (% of N) 3. Relative duration of sickness absence (total sick days/total pain days); 4. Sickness absence during short, intermediate, and long episodes (several levels) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | block randomization ( blocks of 6) |
| Allocation concealment (selection bias) | Low risk | Adequate; patients were given sealed envelopes containing treatment group handled by nurse |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | blinded general practitioner |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | exercise group 30 out of 122 dropouts; placebo 11out of 119 dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis for all available data |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | Low risk | no other interventions noted |
| Compliance acceptable? | Unclear risk | exercise group; 92 out of 122 met criteria for 'on treatment', and 40 patients had a good compliance; placebo group108 out of 119 met criteria for 'on treatment' |
| Timing of the outcome assessment similar? | Low risk | all workers followed up after 2 and weeks and then every months until 12 months |
Gatchel 2003.
| Methods | RCT | |
| Participants | 124 workers from orthopaedic practices with acute low‐back pain and decreased ability to perform normal job requirements because of pain for about 3.8 weeks. Mean age was 38.2 and 65% was male. | |
| Interventions | Intervention: a functional restoration early intervention of 3 weeks which consisted of four major components‐pscyhology, physical therapy, occupational therapy and case‐management. Contents were 3 physical evaluations, 1 physician evaluation, 18 physical therapy sessions (individual and group) 9 biofeedback/pain management sessions, 9 group didactic sessions, 9 case manager/occupational therapy sessions and 3 interdisciplinary team conferences. The number of sessions administered to patients was tailored to their specific needs, with most patients not needing all of the aforementioned number of sessions. Control: non‐intervention, care as usual |
|
| Outcomes | measured at 1 year after first evaluation: % return‐to‐work | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | urn randomization procedure |
| Allocation concealment (selection bias) | Unclear risk | not stated |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | 'by raters blind to study hypotheses' |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | no dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | 'these three groups matched for age, gender, race, and time since original injury based upon and urn randomization procedure' |
| Co‐interventions avoided or similar? | High risk | control group received various types of treatment initiated by themselves |
| Compliance acceptable? | Unclear risk | not stated |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 3, 6, 9, 12 months |
Heymans 2006.
| Methods | RCT | |
| Participants | 299 workers with subacute LBP and sick leave between 3 and 6 weeks. Mean age 40.3, 79% male. 98 in high intensity back school, 98 in Low intensity back school, 103 in usual care group | |
| Interventions | Intervention 1: High‐Intensity Back School. This back school was conducted twice a week, for 8 weeks. It consisted of 16 sessions, each lasting 1 hour, supervised by a physiotherapist. Principles of cognitive‐behavioural therapy were applied throughout the back school programme. The physiotherapist promoted a timecontingent increase in the level of activity. The first two sessions consisted of individual exercises simulating the activities the worker experienced as the most problematic at the workplace. Work‐simulating and strength training exercises during subsequent sessions were performed with gradually increasing resistance. The workers were also given home exercises during the time they were participating in the back school programme. Intevention 2: Low‐Intensity Back School. This back school was based on the Swedish model and consisted of four group sessions once a week for 4 consecutive weeks. Each session was divided into an educational (30 minutes) and a practical part (90 minutes) and guided by written information and a standardized exercise programme. Workers were told that functional activities, like working, could be continued despite back pain. During the educational sessions, the physiotherapist discussed the workplace situation. Not only the most problematic activities experienced by the worker because of the low‐back pain will be discussed, workers also received information on how to cope with these activities. The practical part comprised of a standardized exercise programme consisting of strength training and home exercises. The strength training involved progressive resistance training as well as functional exercises. Workers were instructed to perform exercises at home twice a day, and again if they had any recurrences of back complaints. Control: usual cary by occupational physician according to Dutch guidelines for management of low‐back pain |
|
| Outcomes | number of sick leave days at 3 and 6 months follow‐up | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | sealed opaque envelopes, coded according to a computerized random number generator, workers were randomly allocated |
| Allocation concealment (selection bias) | Low risk | done by non‐involved researcher |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | comment by author: researcher was unaware of the randomization scheme |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 44 (15%) workers withdrew from the study |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis performed |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | no significant differences noted at baseline |
| Co‐interventions avoided or similar? | High risk | workers in the control group had free access and used other interventions |
| Compliance acceptable? | Low risk | of the 103 workers in the usual care group, 88 (85%) returned the diaries containing information about the content of their treatments. Of the 98 workers allocated to the low‐intensity back school, 75 (77%) completed all treatment sessions. In the high‐intensity back school group, 70 (71%) workers completed all treatments |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up 3 and 6 months |
Jensen 2001.
| Methods | RCT | |
| Participants | 208 workers with non‐specific spinal pain, sick listed for at least 1 month. Mean age 43.5, 45% male | |
| Interventions | Intervention: 4 weeks in groups of 4‐8 workers with 6 didactic sessions addressing psychological aspects of chronic pain, ergonomics and medical aspects of chronic pain, visits to the workplace; work managers and rehabilitation officials were invited to participate in the discharge session at which a rehabilitation plan was agreed upon. 6 booster sessions were held over a period of 1 year after the treatment. A combination of Behaviour‐oriented therapy (PT) for 20 hrs per week. Aimed at enhancing the physical functioning and facilitate a lasting behaviour change of the individual. And cognitive behaviour therapy (CBT) for 13‐14 hrs per week. Aimed at improving the subjects’ ability to manage their pain and resume a normal level of activity. Programme included activity planning, goal setting, problem solving, applied relaxation, cognitive coping techniques, activity pacing , the role of vicious circles and how to break them, the role of significant others and assertion training. Individually tailored homework assignments were given at the end of each session. Control 1: only behaviour oriented therapy (PT) Control 2: only cognitive behaviour therapy (CBT) Control 3: care as usual (usual routines in health care) |
|
| Outcomes | Measured at 18 and 36 months after rehabilitation: absence from work for more than 14 days | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | group randomization via blocks |
| Allocation concealment (selection bias) | Low risk | 'screening personnel were blinded to the results of the randomisation' |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | information from author |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 28 workers dropped out of treatment |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | both PP and ITT analysis |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | pg 66 (Jensen 2001) |
| Co‐interventions avoided or similar? | High risk | control group could seek other medical advice or therapy |
| Compliance acceptable? | Low risk | 56%‐70% adherence to treatment plan |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up post‐treatment at 6 and 12 months |
Jensen 2011.
| Methods | RCT | |
| Participants | 351 patients between 16 to 60 years, partly or fully sick‐listed from work for 4 to 12 weeks because of LBP | |
| Interventions | Intervention 1: brief clinical intervention: standard clinical LBP examination by a physician, relevant imaging and examinations were ordered and treatment options were discussed. Patients were informed about cause, prognosis and treatment options. Furthermore, they were informed about exercise being beneficial, medical pain management, and they were advised to resume work when possible. Physiotherapy examination, with advise about exercise, and general advise about increasing physical activity and exercise. Coordination between stakeholders was ensured. Follow‐up visit at physiotherapist after 2 weeks, and physician if necessary. Intervention 2: brief clinical intervention and case management. This included an interview with a case‐manager within 2‐3 days; with questions about work history, private life, pain and disability perception. The case manager and the participant made a tailored rehabilitaion plan aiming at full or partial RTW. Each case was discussed several times by the entire multidisciplinary team including the rehabilitation physician, a specialist in clinical social medicine, a physiotherapist, a social worker, and a occupational therapist. |
|
| Outcomes | return to work defined as the first 4 week period within the first year after inclusion, during which the participant received no social transfer payments. Follow‐up was 1 year. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated block randomization |
| Allocation concealment (selection bias) | Low risk | Performed by a secretary |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | data analyses were carried out by researchers outside the hospital |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients were aware of the result of the randomization |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | at the follow‐up consultation caregivers were aware of the result of the randomization |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | For primary outcome no dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | 100% follow‐up |
| Selective reporting (reporting bias) | Low risk | no suggestions found |
| Similarity of baseline characteristics? | Low risk | Adequate correction for any differences at baseline |
| Co‐interventions avoided or similar? | Unclear risk | not described |
| Compliance acceptable? | Unclear risk | no information |
| Timing of the outcome assessment similar? | Low risk | yes |
Karjalainen 2003.
| Methods | RCT | |
| Participants | 107 workers with subacute low‐back pain which made working difficult for > 4 weeks and < 3 months. Mean age 44, % female 58.7 | |
| Interventions | Intervention 1: Mini‐Intervention Group (A) (60 min). Interview and examination of patient, discussion of working conditions and result of clinical examination were explained. The main aim was to reduce the patients’ concerns about their back pain by providing accurate information and to encourage physical activity. Back straining activities were appraised and special movements required at the patient’s work were trained if necessary. No more than five exercises for improving the function of deep abdominal muscles and establishing symmetric use of the back. Other daily exercises were planned feasible enough for the patient to commit to and execute them. The aim was to increase body control and exercising in everyday life. Feedback to the patient’s GP included recommendations on further diagnostic tests, treatment, work, and sick leave. The GP at the patient’s local health care center subsequently coordinated the recommended treatment in his/her usual manner at the health care centre. Intervention 2: Work Site Visit Group (B). Identical to mini‐intervention plus a visit of the physiotherapist to the patient’s work site. The patient’s work supervisor and company nurse, physiotherapist, and physician were asked to join in the session to ensure that the patient had adapted to the information and practical instructions of appropriate ways of using the back at work and to encourage their cooperation. The company physician was advised to refer any patient who still had disabling low‐back pain or was on sick leave 3 months after randomization for inpatient rehabilitation. Control: usual care group received a leaflet on back pain and were treated by their GP in the usual manner |
|
| Outcomes | Measurement at 1 and 2 year after randomization: back pain related sick leave | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | research nurse randomized each patient into 1 out of 3 study groups using four piles of sealed envelopes. the randomization was done in blocks of 15. |
| Allocation concealment (selection bias) | Low risk | a biostatistician had prepared the order from a random number table. A secretary unconnected with the patients had numbered the envelopes sequentially to prevent their rearrangement. Research nurse and researchers were not aware of block size and therefore could not predict the group assignments |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | was not aware |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Low risk | until the end of intervention at the FIOH. The work site visit made the difference at the end |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | Low risk | until the end of intervention at the FIOH. The work site visit made the difference at the end |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 1 dropout |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | nu suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences at baseline |
| Co‐interventions avoided or similar? | High risk | control group were free to go seek help and went to more physiotherapists and spent more money on diagnostic tests |
| Compliance acceptable? | Low risk | high follow‐up percentages (94‐100%) in each group |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 3,6,12 months |
Kool 2005.
| Methods | RCT | |
| Participants | 174 workers with subacute LBP and sick leave of > 6 weeks in last half year. mean age 42, 79% male | |
| Interventions | Intervention: Function‐Centered Treatment for 6 days a week for 3 weeks. The FCT was based on work hardening and functional restoration programmes. Treatment activities were chosen based on a patient’s required capacities, as identified in the work‐related assessment. Treatment consisted of work simulation, strength and endurance training through isokinetic exercise, cardiovascular training performed by walking and aqua‐aerobics, sports therapy, and self‐exercise. Patients were told that increasing activity might cause more pain because the body had to adjust to the activity again. All team members emphasized that patients should continue therapeutic activities even if their pain increased. The treatment protocol did not contain massage, hot packs, and other passive treatments because we did not believe that they facilitate an increase in activity and self‐efficacy, nor has the research literature shown them to be effective. Control: Pain‐Centered Treatment. The primary goal in the PCT group was to reduce pain. The secondary goal was to increase strength and decrease disability. The physical therapist examined the patients to identify painful movements and limitations in mobility, strength, and muscle length in the lumbar region and lower extremities. Treatment was for 2.5 hours a day and consisted of individually selected passive and active mobilization, stretching, strength training, and a mini back school. Unlike with the FCT group, patients in the PCT group were told to stop activities when pain increased. Passive pain modulating treatments such as hot packs, electrotherapy, or massage were used daily. Low‐intensity movement therapy in the pool and progressive muscle relaxation further enhanced relaxation. Progressive muscle relaxation used systematic contraction and relaxation of specific muscle groups. Patients were encouraged to incorporate relaxation techniques into daily living as a coping skill to reduce stress, muscle tension, and pain. |
|
| Outcomes | Measured at 1 year after treatment: number of calender work days, the rate of patients receiving unemployment benefits or permanent benefits. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | an independent and blinded research assistant performed concealed randomisation within these 4 strata using a randomisation schedule with blocks of 2 generated on a computer by an independent researcher |
| Allocation concealment (selection bias) | Low risk | see above |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | days at work and other work‐related outcomes were assessed with a questionnaire sent to employers and the patients' primary physicians, who were blinded to the patients' group assignment |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware intervention content, but not of other treatment |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 1 dropout |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | High risk | subjects used other health care providers between 3 and 12 months |
| Compliance acceptable? | Low risk | all patients attended at least 90% of the scheduled treatments |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up post treatment and at 3 months |
Lambeek 2010.
| Methods | RCT | |
| Participants | 134 adults aged 18‐65 years sick listed for at least 12 weeks owing to low back pain | |
| Interventions | Integrated care: consisted of a workplace intervention based on participatory ergonomics, involving a supervisor, and a graded activity programme based on cognitive behavioural principles. Coordination was done by a clinical occupational physician. Usual care: Usual treatment by medical specialist, occupational physician, general practitioner and/or allied health professional |
|
| Outcomes | return‐to‐work defined as duration of sick leave due to low back pain in calendar days from the day of randomisation until full return‐to‐work in own or other work with equal earnings for at least four weeks without recurrence, partial or full. Measured at 3,6,9, and 12 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomization of four allocations, using a computer generated random sequence table |
| Allocation concealment (selection bias) | Low risk | For every stratum, an independent statistician carried out the block randomization. A research assistant prepared opaque, sequentially numbered and sealed coded envelopes for each stratum, containing a referral for either the integrated care group or the usual care group. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | All patients received a code according to which a research assistant entered all data in the computer. This ensured blinded analysis of the data by the researcher. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Patients were not blinded for treatment allocation |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | Care providers were also not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 7% loss to follow‐up |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | intention‐to‐treat (ITT) analysis |
| Selective reporting (reporting bias) | Low risk | No suggestion found |
| Similarity of baseline characteristics? | Low risk | No significant differences at baseline. |
| Co‐interventions avoided or similar? | High risk | More co‐interventions in the control group. |
| Compliance acceptable? | Unclear risk | 5 participants did not participate in the integrated care interention. 12 participants received only two elements of the integrated care. |
| Timing of the outcome assessment similar? | Low risk | Yes, at 3, 6, 9, and 12 months follow up |
Lindstrom 1992.
| Methods | RCT | |
| Participants | 103 patients (71 males and 32 females), aged between 19‐64 years, sick listed for at least 6 weeks because of any low‐back pain diagnosis. | |
| Interventions | Intervention 1 : the graded activity programme consisted of: 1. Measurement of functional capacity,including mobility strength and fitness. 2. A work place visit, 3. back school education 4. 5. Individual, submaximal, gradually increased, exercise programme, with an operant conditioning behavioural approach. The operant conditioning method was aimed to teach the patients that it was safe to move while regaining function (N = 51). Programme duration: three times per week until return‐to‐work was achieved. Intervention 2 = CAU: traditional care recommended by their physicians, general rest, analgesics and prescription of unspecific physical treatment modalities(n = 52). |
|
| Outcomes | Measurement at 1 and 2 years after randomisation. mean days of sick leave | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | block randomisation procedure |
| Allocation concealment (selection bias) | High risk | does not state |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | assessors blind to sick leave data until conclusion of study |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 2 out of 51 dropped out of activity group, 3 out of 52 dropped out of control group |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | does not state |
| Selective reporting (reporting bias) | Low risk | no suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | High risk | control group were not prevented from getting information from intervention programme, and traditional care was given to them which could include anything |
| Compliance acceptable? | Low risk | 96% of patients followed interventions |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 12 months |
Loisel 1997.
| Methods | RCT; cluster randomisation design was used by the generation of 50 random numbers by a computer, each number being placed in a sealed envelope | |
| Participants | 104 (62 males and 42 females), aged between 18‐65 years, with thoracic or lumbar pain incurred at work, not working or on suitable duties for more than 6 weeks | |
| Interventions |
Clinical intervention/full intervention Intervention 1 (CI): Clinical intervention: after 8 weeks of absence included a visit to a back pain specialist and a school for back care education and after 12 weeks absence a multidisciplinary work rehabilitation intervention (functional rehabilitation therapy) was proposed that included fitness development and work hardening with cognitive‐behavioural approach. The programme ended with a progressive return‐to‐work (therapeutic return‐to‐work), that consisted of alternating days at the original job and days receiving functional therapy (N = 31). Programme duration: twelve months from the initial absence from work. Intervention 2 (FI): Full intervention: Clinical and occupational intervention combined. Occupational intervention (OI): (after 6 weeks of absence from work) included visits to an occupational physician (who could recommend investigation or treatment or set up light duties to help patient RTW) and a participatory ergonomic evaluation conducted by an ergonomist (to determine the need for job modifications). After observation of the worker's tasks, a meeting between ergonomist, injured worker, supervisor, management and union representatives was organised to come up with a "specific" ergonomic diagnosis and precise solutions to improve the work site to be presented to management (n = 25).Programme duration: twelve months from the initial absence from work. Clinical intervention/unspecified intervention Intervention 1 (CI): Clinical intervention: after 8 weeks of absence included a visit to a back pain specialist and a school for back care education and after 12 weeks absence a multidisciplinary work rehabilitation intervention (functional rehabilitation therapy) was proposed that included fitness development and work hardening with cognitive‐behavioural approach. The programme ended with a progressive return‐to‐work (therapeutic return‐to‐work), that consisted of alternating days at the original job and days receiving functional therapy (n = 31). Programme duration: 12 months from the initial absence from work. Intervention 2 (UC): patients in this group received care from their attending physician who was free to prescribe any test, treatment or specialist referral (n = 26) |
|
| Outcomes | Measurement at 12 months after enrolment: Number days out of regular work; Number of days out of all work; Functional status (Oswestry questionnaire); Pain Level (McGill‐Melzack questionnaire) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | cluster randomisation on workplace; random number generated by computer |
| Allocation concealment (selection bias) | Low risk | random numbers generated by computer and sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | assessor blinded to subjects randomisation status |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 9% did not respond to follow‐up visit |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | those 9% were not included in analysis |
| Selective reporting (reporting bias) | Low risk | no suggestions found |
| Similarity of baseline characteristics? | High risk | not for age, comorbidity frequency, % women |
| Co‐interventions avoided or similar? | High risk | all groups were free to seek additional treatment in the community |
| Compliance acceptable? | Unclear risk | does not state adherence to protocol |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 4 weeks accumulated absence from work, and at 1 year after initial absence from work |
Meyer 2005.
| Methods | RCT | |
| Participants | 33 workers with chronic non‐specific musculoskeletal disorders with sick leave of at least 2 months or 50% work incapacity from a full‐time job over 3 months. mean age 43 years, 70% male | |
| Interventions | Intervention: called work rehabilitation programme, lasted 8 weeks, 3.5 hours per day, 5 days per week. The work rehabilitation programme aimed to increase functional capacity and improve the patient’s self‐efficacy using an operant behavioural therapy approach. The approach was interdisciplinary and involved rehabilitation physicians, a psychologist, a social worker, occupational and physiotherapists. Every patient had a therapist as a case manager to ensure that goals of the rehabilitation are adapted weekly and coordination between all members in the interdisciplinary team were guaranteed. The programme contained work‐specific exercises, progressive exercise therapy with training devices, education in ergonomics, learning strategies to cope with pain and to increase self‐efficacy, a group intervention with the psychologist, sports activities for recreation and a workplace visit to develop appropriate workload related exercises for the programme [24?26]. The uptake of work was designed to be gradual and started 4 weeks after the programme began. Control: The physician who referred the patient to the hospital administered the control treatment, called progressive exercise therapy. This physician had received specific recommendations concerning work reintegration, medication and training. 3 times a week for 8 weeks progressive exercises in a physiotherapy practice. |
|
| Outcomes | Measured at 8 weeks post‐rehabilitation: The ability to work in % of a full‐time job, and the actual performed work status in % of a full‐time job | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | an independent person conducted random allocation by using a minimization procedure and a random number table. After the patients inclusion, a concealed letter concerning the result of the randomisation was given to the therapist to allocated the patient to the respective group. |
| Allocation concealment (selection bias) | Low risk | see above |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | assessor was blinded regarding treatment allocation |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Low risk | patients knew about the common aim of the study and control treatment, namely the return‐to‐work, but were blinded concerning the two treatments. This meant they were told that they would undergo a fitness programme, but did not know what the exact content of the two treatments was until they started the treatment. |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | provider was aware of treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 2 dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | according to author |
| Selective reporting (reporting bias) | Low risk | no suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | Low risk | none of the intervention groups received co‐interventions |
| Compliance acceptable? | Low risk | page 70 |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 8 weeks post rehab assessment and at 32 weeks |
Mitchell 1994.
| Methods | RCT | |
| Participants | 542 patients (386 males and 156 females), age not stated, with chronic pain caused by low back injury for at least 90 days, with or without radiating pain and off work. | |
| Interventions | Intervention: functional restoration programme consisting of an active exercise programme (sports medicine approach). The programme had two parts, physical exercise and functional simulation programme developed in an occupational gymnasium. Circuit equipment used in this exercise component was designed to work specific muscle groups in sequence to diminish fatigue and to achieve mobility and strengthening of various muscle groups. Work related tasks included were: lifting station, working above head board, stair‐climbing, carrying weights and lifting while twisting. In addition, behavioural and cognitive therapy was included which consisted of education classes, relaxation therapy, biofeedback, individual and group counselling (n = 271). Programme duration: 8 to 12 weeks (40 treatment days ‐ seven hours per day, five days per week). Control: CAU: medical management left entirely in the hands of the GP and included a wide range of treatment methods such as physiotherapy, medication, manipulation, acupuncture, work hardening, back schools, and active exercise programmes using the sports medicine approach (n = 271). |
|
| Outcomes | Measurement at 12 months after the treatment. 1. Return to full time work; 2. Cost per workers' compensation claim; 3. Days lost from work | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | does not state |
| Allocation concealment (selection bias) | Unclear risk | does not state |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Unclear risk | does not state who was outcome assessor and he was blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | High risk | does not state dropout rate |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis reported |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | High risk | control group could use any consultant of facility that existed in the community |
| Compliance acceptable? | Unclear risk | does not state |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up monthly for 12 months in relation to RTW |
Roche 2007.
| Methods | RCT | |
| Participants | 132 workers with chronic low‐back pain and on sick leave or at risk of work disability for more than 3 months. Mean age 39.8, 65.1% men | |
| Interventions | Intervention: Functional restoration programme: 5 weeks, 6 hrs a day The group performed exercises supervised by a physiotherapist who adjusted the exercise intensity to each participant every week. Patients performed work simulations during occupational therapy sessions. They were referred to the psychologist at least once in the first week and for further treatment if requested. Dietary advice was given. The schedule of interventions was standardized for all patients. Control: Active individual therapy: 5 weeks 3x1 hr a week. only active exercises supervised directly by the physiotherapist. The last week focused on functional exercises and endurance training. The programme included 50 minutes of individual home exercises 2 days a week (these could include stretching, jogging, and swimming). In both groups, patients were off work during the 5 weeks of treatment. |
|
| Outcomes | Measurement directly after treatment: % self perceived ability to return to work, % return‐to‐work, % full‐time return‐to‐work | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | block randomisation using an 8 element permutation table |
| Allocation concealment (selection bias) | High risk | according to author |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | according to author |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | return‐to‐work data missing on 1 subject from each group |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | Unclear risk | according do author |
| Compliance acceptable? | Unclear risk | according to author |
| Timing of the outcome assessment similar? | Low risk | all subjects assessed at the end of treatment period of 5 weeks |
Skouen 2002.
| Methods | RCT | |
| Participants | 211 chronic low‐back pain patients of which 90% were on sick leave and 10% had been sick listed at least 2 months per year for last 2 years. Mean age 43.5, % male 35 | |
| Interventions | Intervention: light multidisciplinary treatment consisting of 3‐4 hours of evaluation, consultation and lecture at the start of intervention period with encouragement to gradually increase activity level. Topics were exercise, lifestyle, and fear avoidance. Intervention: extensive multidisciplinary treatment consisting of 4 wks of 6 hr per day group sessions with education, exercises, and occasional workplace interventions. |
|
| Outcomes | Measurement after 12, 18 and 24 months after treatment: information on sick leave status via National Health Insurance | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | random by means of a sequence of pre‐labelled cards contained in sealed envelopes; block randomisation |
| Allocation concealment (selection bias) | Low risk | prepared beforehand by physician outside clinic |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | data from national health insurance register |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 3 patients dropped out (out of 195) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | all subjects analysed (in terms of return‐to‐work) in the group to which they were allocated |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | only age and gender provided |
| Co‐interventions avoided or similar? | Low risk | control group could seek other medical advice via GP |
| Compliance acceptable? | Low risk | only 3 patients did not comply with treatment programme |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up once a month during the 26 follow‐up period |
Staal 2004.
| Methods | RCT | |
| Participants | 134 employees from Schiphol Airport in the Netherlands with low‐back pain of at least 4 weeks. mean age of 38 and 94% men: 67 in intervention group, 67 in control group; all workers were on full or partial sick leave between 6‐14 weeks. | |
| Interventions | Intervention: Graded activity intervention supervised by a physiotherapist along with usual guidance from the OP about work‐related problems and barriers to return to work. Including: physical examination, 1 hour exercise twice a week until complete RTW or 3 months, both generally and individually tailored exercises, proposal of a date for full return‐to‐work, modified hours and duties with a gradually increasing quota of exercises, time‐contingent management Control: care as usual being usual guidance and advice from occupational health physician |
|
| Outcomes | Measurement at 100 days and 1 year after randomisation: total number of days absent from work because of low‐back pain. Full return‐to‐work was defined as any full return to regular work with a minimum duration of 4 weeks. After 3 years numbers of workers that were still disabled for work. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | block randomisation after pre stratification for the organizational unit in the workplace from which they were recruited and for the severity of pain symptoms |
| Allocation concealment (selection bias) | Low risk | group allocation in sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | outcome assessor not aware |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 13 withdrawals of which 3 did not adhere to intervention protocol. 10% dropout |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences |
| Co‐interventions avoided or similar? | Low risk | no co‐interventions noted. In usual care subjects were allowed to seek any sort of intervention |
| Compliance acceptable? | Low risk | yes, only 3 did not adhere to protocol |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 3 and 6 months post‐randomisation and continuously (days away from work) |
Steenstra 2006.
| Methods | RCT | |
| Participants | 112 workers from the Netherlands with low‐back pain. mean age 42 years, 41% men. On sick leave for more than 8 weeks. 55 workers intervention group, 57 workers control group. | |
| Interventions | Intervention: Graded activity programme consisting of 26 one‐hour sessions maximally, with a frequency of two sessions a week. The first session took half an hour more since taking the patients history and a physical examination were part of this session. The programme ended as soon as a full RTW had been established, according to an earlier agreed upon individual schedule . During the programme the worker had an active role in RTW and the physiotherapist (PT) acted as a coach and supervisor, using a hands‐off approach. Control: care as usual including usual guidance by the occupational health physician |
|
| Outcomes | Measurement at 6 months and 1 year after first day of sick leave: lasting return to own or equal work, calculated as duration of work absenteeism in calender days from the first day of sick leave to full RTW | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | an independent researcher performed randomisation using a list of random numbers |
| Allocation concealment (selection bias) | Low risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | information from first author: data from automated databases, rest of data from questionnaires |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | all subjects included in follow‐up analysis |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis reported |
| Selective reporting (reporting bias) | Low risk | yes, no suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences |
| Co‐interventions avoided or similar? | Low risk | workers could seek other help e.g. physio, manual therapy, chiropractor, neurologist, orthopedic surgeon |
| Compliance acceptable? | High risk | 19 out of 55 = 35% from graded activity group did not comply |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up for primary outcome during first 12 months (continuously), secondary outcomes at 12, 26 and 52 weeks post‐treatment |
Storheim 2003.
| Methods | RCT | |
| Participants | 93 workers from Local Insurance Offices, and from 2 GPs with LBP and sick listed between 8‐12 weeks. Mean age 41, 48% male. 34 in Cognitive group, 30 in Exercise group, 29 in Control group | |
| Interventions | Both interventions: Routine back examination, X‐rays and CTscans and general encouragement to resume daily activities and work. Intervention 1: Intensive group training: 15 weeks of 2‐3 times a week1 hour exercise, following the Norwegian Aerobic Fitness Model, which is based on both exercise physiology and ergonomic principles, and designed to increase overall fitness and functional capacity. A physical therapist led the programme with focus on ergonomic principles and functional tasks, no pain focus, it is safe to move focus, the whole programme is accompanied by music. Intervention 2: cognitive intervention: 2 consultations between 30‐60 minutes. Including:explanation of pain mechanisms, questionnaire discussion, functional examination with individual feedback and advice, instruction in activation of deep stabilizing muscles and advice on how to use it actively in functional and demanding tasks of daily life, Instruction in the squat technique when lifting is required, How to cope with new attacks, Reassure and emphasize that it is safe to move, 2 consultations 30‐60 minutes. Control: Treated by their GP with to restrictions of treatments or referrals |
|
| Outcomes | Measurement at 18 weeks after inclusion: mean days of sick leave | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was conducted by an engineer working at the hospital who was not involved in the trial. Codes were kept locked in the engineers office. Sealed opaque envelope were handed to workers. |
| Allocation concealment (selection bias) | Low risk | subjects drew sealed envelopes with disclosure of randomisation |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | data collected from data registry and self reported questionnaires |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Described: 18% loss of patients to follow‐up. Dropout was higher in exercise group. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | No differences between groups, except a shorter mean time since first LBP episode for the control group |
| Co‐interventions avoided or similar? | Unclear risk | Not clear what control group used for co‐interventions |
| Compliance acceptable? | Low risk | 17 people dropped out (2 from cognitive, 9 from exercise and 6 from control group). Mean adherence to group training classes was 80.4% for people who didn't dropout. One fifth of people in cognitive group came back for more than the 2 recommended consultations. |
| Timing of the outcome assessment similar? | Low risk | yes, all subjects followed up 18 weeks after inclusion |
van den Hout 2003.
| Methods | RCT | |
| Participants | 138 workers with back pain. Selected from a rehabilitation centre from the Netherlands. 67% had chronic back pain, 28% subacute back pain. Sick leave between 7.4‐10 weeks. | |
| Interventions | GAPS: graded activity programme and group education with cognitive behavioural therapy focusing on problem solving. GAGE: graded activity programme and group education |
|
| Outcomes | Measurement at 6 months and 1 year after treatment: number of workers with 100% return‐to‐work; number of workers with part‐time return‐to‐work; number of workers with no return‐to‐work; mean days of sick leave first half year and mean days of sick leave second half year after treatment | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | randomisation scheme was computer generated, and only known by logistics planner of the rehabilitation centre |
| Allocation concealment (selection bias) | Low risk | see above |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | researchers obtaining data from data bases were blinded to group allocation |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 108 workers randomized; 84 followed up; 22% dropout |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | no clear information found, looks like PP analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestion found |
| Similarity of baseline characteristics? | Low risk | except for RDQ scores and treatment credibility |
| Co‐interventions avoided or similar? | Unclear risk | does not state whether subjects attended other care providers between end of treatment and follow‐up |
| Compliance acceptable? | Unclear risk | 31 of 108 dropped out before start of treatment, another 8 dropped out between treatment and follow up. It does not mention compliance (adherence) to treatment protocol for those that didn't dropout |
| Timing of the outcome assessment similar? | Low risk | both groups measured pre‐treatment and 6, 12 months after treatment stop |
Wright 2005.
| Methods | RCT | |
| Participants | 80 workers with acute or subacute back pain. Median time off work 20 days, mean age 41, 21% women. 43 workers in intervention and 37 in control group | |
| Interventions | Intervention: Back book + simple, practical advise on how to modify physical activities specific to the individual’s work situation + one treatment from senior physiotherapist depending on assessment findings + 3x1 hr group exercises for 2 weeks Control: back book + GP + additionally, simple, practical advise on how to modify physical activities specific to the individuals work situation was discussed |
|
| Outcomes | Measured at 2 months after study entry: rate of return‐to‐work, average number of days off work, light duties at study entry (were not included for analysis), percentage of patients changing from light duties to full duties | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | using a computer programme |
| Allocation concealment (selection bias) | Low risk | a sealed envelope containing the randomized group number was given to the patient to open |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Unclear risk | does not state who is assessor and if blinded |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) All outcomes ‐ care provider? | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 10 out of 56 dropped out in group 1 and 5 out of 50 in group 2 |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | High risk | control group could seek other interventions via GP |
| Compliance acceptable? | Unclear risk | does not state |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 1 and 2 months |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alaranta 1994 | no stated relationship between intervention and functional job demands |
| Aure 2003 | no stated relationship between intervention and functional job demands |
| Bentsen 1997 | no stated relationship between intervention and functional job demands |
| Bültmann 2009 | physical conditioning was not a structural part of the intervention |
| Dahl 2001 | outcome measure was not sickness absence |
| Dettori 1995 | no stated relationship between intervention and functional job demands |
| Friedrich 1998 | no stated relationship between intervention and functional job demands |
| Hagen 2000 | no stated relationship between intervention and functional job demands |
| Hansen 1993 | no stated relationship between intervention and functional job demands |
| Kellett 1991 | no stated relationship between intervention and functional job demands |
| Linton 2005 | No existing work disability or sickness absence at baseline |
| Malmivaara 1995 | no stated relationship between intervention and functional job demands |
| Moffett 1999 | no stated relationship between intervention and functional job demands |
| Niemisto 2003 | no stated relationship between intervention and functional job demands |
| Rantonen 2012 | at baseline majority of participants were not on sickleave |
| Schiltenwolf 2006 | outcome measure was not related to sickness absence or return‐to‐work |
| Seferlis 1998 | no stated relationship between intervention and functional job demands |
| Torstensen 1998 | no stated relationship between intervention and functional job demands |
| Whitfill 2010 | at baseline majority of participants were not on sickleave |
Characteristics of studies awaiting assessment [ordered by study ID]
Henchoz 2010.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Not yet assessed |
Jensen 2012.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Not yet assessed |
Vora 2012.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Not yet assessed |
Differences between protocol and review
This is a new update of the previously updated review published in 2010. For the previous update a new protocol was written. In that protocol, we stated that we would re‐calculate the SMDs into a mean difference in time to return‐to‐work. This would be done from the pooled effect size using the median standard deviation of the included studies in the formula: pooled mean difference = pooled effect size * median standard deviation.
However, we preferred not to re‐calculate the SMDs back and instead used the clinically worthwhile cut‐off points from the original review.
Another difference is the change of title in this updated version. The original title was: 'Work conditioning, work hardening and functional restoration for workers with back an neck pain'. In the previously updated version the title was: 'Physical conditioning programs for improving work outcomes in workers with back pain' (Schaafsma 2010).
In this second update we changed the comparisons of studies by making a clear distinction between those studies that compared the physical conditioning programme in addition to usual care with usual care, and the physical conditioning programme with usual care.
Contributions of authors
Frederieke Schaafsma updated the searches for new trials. Frederieke Schaafsma and Karyn Whelan conducted the study selection. Ludeke van Es and Allard van der Beek conducted the risk of bias assessment. Frederieke Schaafsma, Allard van der Beek and Ludeke van Es conducted the data extraction and analysis of all new studies. All review authors commented on the draft of the final manuscript.
Sources of support
Internal sources
The University of Sydney, Australia.
External sources
No sources of support supplied
Declarations of interest
None
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Altmaier 1992 {published data only}
- Altmaier EM, Lehmann TR, Russell DW, Weinstein JN, Kao CH. The effectiveness of psychological interventions for the rehabilitation of low back pain: a randomised controlled trial evaluation. Pain 1992;49:329‐35. [DOI] [PubMed] [Google Scholar]
Bendix 1996 {published data only}
- Bendix AF, Bendix T, Hæstrup C, Busch E. A prospective, randomized 5‐year follow‐up study of functional restoration in chronic low back pain patients. European Spine Journal 1998;7:111‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendix AF, Bendix T, Labriola M, Bœkgaard. Functional Restoration for Chronic Low Back Pain. Spine 1998;23(6):717‐25. [DOI] [PubMed] [Google Scholar]
- Bendix AF, Bendix T, Vaegter K, Busch E, Kirkbak S, Ostenfeld S. Intensive work rehabilitation [Intensiv tvaerfaglig rygbehandling]. Videnskab og Praksis 1994;156(16):2388‐95. [PubMed] [Google Scholar]
- Bendix AF, Bendix T, Vægter K, Lind C, Frølund L, Holm L. Multidisciplinary intensive treatment for chronic low back pain: a randomized, prospective study. Cleveland Clinic Journal of Medicine 1996;63(1):62‐9. [DOI] [PubMed] [Google Scholar]
Bendix 1997 {published data only}
- Bendix A, Bendix T, Labriola M, Bœkgaard P. Functional restoration for chronic low back pain/ two‐year follow‐up of two randomized clinical trials. Spine 1998;23(6):717‐25. [DOI] [PubMed] [Google Scholar]
- Bendix AE, Bendix T, Hæstrup C, Busch E. A prospective, randomized 5‐year follow‐up study of functional restoration in chronic low back pain patients. European Spine Journal 1998;7:111‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendix AF, Bendix T, Lund C, Kirkbak S, Ostenfeld S. Comparison of three intensive programs for chronic low back pain patients: a prospective, randomized, observer‐blinded study with one year follow‐up. Scandinavian Journal of Rehabilitation Medicine 1997;29:81‐9. [PubMed] [Google Scholar]
Bendix 2000 {published data only}
- Bendix T, Bendix A, Labriola M, Hæstrup C, Ebbehøj N. Functional restoration versus outpatient physical training in chronic low back pain. Spine 2000;25(19):2494‐500. [DOI] [PubMed] [Google Scholar]
Bethge 2011 {published data only}
- Bethge M, Herbold D, Jacobi C. Work status and health‐related quality of life following multimodal work hardening: a cluster randomised controlled trial. Journal of Back and Musculoskeletal Rehabilitation 2011;24:161‐72. [DOI] [PubMed] [Google Scholar]
Corey 1996 {published data only}
- Corey DT, Koepfler LE, Etlin D, Day HI. A limited functional restoration program for injured workers: A randomised trial. Journal of Ocupational Rehabilitation 1996;6(4):239‐49. [DOI] [PubMed] [Google Scholar]
Faas 1995 {published data only}
- Faas A, Eijk J Th M, Chavannes AW, Gubbels JW. A randomised trial of exercise therapy in patients with acute low back pain: Efficacy on sickness absence. Spine 1995;20(8):941‐7. [DOI] [PubMed] [Google Scholar]
Gatchel 2003 {published data only}
- Gatchel RJ, Polatin PB, Noe C, Gardea M, Pulliam C, Thompson J. Treatment‐ and cost‐effectiveness of early intervention for acute low‐back pain patients: A one‐year prospective study. Journal of Occupational Rehabilitation 2003;13(1):1‐9. [DOI] [PubMed] [Google Scholar]
Heymans 2006 {published data only}
- Heymans MW, Vet HCW, Bonger PM, Knol DL, Koes BW, Mechelen W. The effectiveness of high‐intensity versus low‐intensity back schools in an occupational setting. Spine 2006;31(10):1075‐82. [DOI] [PubMed] [Google Scholar]
Jensen 2001 {published data only}
- Jensen IB, Bergström G, Ljungquist T, Bodin L. A 3‐year follow‐up of a multidisciplinary rehabilitation programme for back and neck pain. Pain 2005;115:273‐83. [DOI] [PubMed] [Google Scholar]
- Jensen IB, Bergström G, Ljungquist T, Bodin L, Nygren ÅL. A randomized controlled component analysis of a behavioral medicine rehabilitation program for chronic spinal pain: are the effects dependent on gender. Pain 2001;91:65‐78. [DOI] [PubMed] [Google Scholar]
Jensen 2011 {published data only}
- Jensen C, Jensen OK, Christiansen DH, Nielsen CV. One‐year follow‐up in employees sick‐listed because of low back pain. Spine 2011;36(15):1180‐9. [DOI] [PubMed] [Google Scholar]
Karjalainen 2003 {published data only}
- Karjalainen K, Malmivaara A, Mutanen P, Roine R, Hurri H, Pohjolainen T. Mini‐intervention for subacute low back pain. Spine 2004;29(10):1069‐76. [DOI] [PubMed] [Google Scholar]
- Karjalainen K, Malmivaara A, Pohjolainen T, Hurri H, Mutanen P, Rissanen P, et al. Mini‐intervention for subacute low back pain. Spine 2003;28(6):533‐41. [DOI] [PubMed] [Google Scholar]
Kool 2005 {published data only}
- Kool J, Bachmann S, Oesch P, Knuesel O, Ambergen T, Bie R, Brandt P. Function‐centered rehabilitation increases work days in patients with nonacute nonspecific low back pain: 1‐Year results from a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2007;88(9):1089‐94. [DOI] [PubMed] [Google Scholar]
- Kool JP, Oesch PR, Backmann S, Knuesel O, Dierkes JG, Russo M, Bie RA, Brandt PA. Increasing days at work using function‐centered rehabilitation in nonacute nonspecific low back pain: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2005;86(5):857‐64. [DOI] [PubMed] [Google Scholar]
Lambeek 2010 {published data only}
- Lambeek LC, Mechelen W, Knol DL, Louisel P, Anema JR. Randomised controlled trial of integrated care to reduce disability from chronic low back pain in working and private life. BMJ 2010;340:c1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lindstrom 1992 {published data only}
- Lindstrom I, Ohlund C, Eek C, Wallin L, Peterson L‐E, Nachemson A. Mobility, strength, and fitness after a graded activity program for patients with subacute low back pain. A randomised prospective clinical study with a behavioural approach. Spine 1992;17(6):641‐52. [DOI] [PubMed] [Google Scholar]
- Lindstrom I, Ohlund C, Eek C, Wallin L, Peterson LE, Fordyce WE, Nachemson AL. The effect of graded activity on patients with subacute low back pain: a randomized prospective clinical study with an operant‐conditioning behavioral approach. Physical Therapy 1992;72(4):279‐90. [DOI] [PubMed] [Google Scholar]
- Lindstrom I, Ohlund C, Nachemson A. Physical performance, pain, pain behavior and subjective disability in patients with subacute low back pain. Scandinavian Journal of Rehabilitation Medicine 1995;27(3):153‐60. [PubMed] [Google Scholar]
Loisel 1997 {published data only}
- Loisel P, Abenhaim L, Durand P, Esdaile JM, Suissa S, Gosselin L, et al. A population based, randomised clinical trial on back pain management. Spine 1997;22(24):2911‐8. [DOI] [PubMed] [Google Scholar]
- Loisel P, Lemaire J, Poitras S, Durand M‐J, Champagne F, Stock S, et al. Cost‐benefit and cost‐effectiveness analysis of a disability prevention model for back pain management: a six year follow up study. Occupational and Environmental Medicine 2002;59(12):807‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Meyer 2005 {published data only}
- Meyer K, Fransen J, Huwiler H, Uebelhart D, Klipstein A. Feasibility and results of a randomised pilot‐study of a work rehabilitation programme. Journal of Back and Musculoskeletal Rehabilitation 2005;18:67‐78. [Google Scholar]
Mitchell 1994 {published data only}
- Mitchell RI, Carmen GM. The functional restoration approach to the treatment of chronic pain in patients with soft tissue and back injuries. Spine 1994;19(6):633‐42. [DOI] [PubMed] [Google Scholar]
Roche 2007 {published data only}
- Jousset N, Fanello S, Bontoux L, Dubus V, Billabert C, Vielle B, et al. Effects of functional restoration versus 3 hours per week physical therapy: a randomized controlled study. Spine 2004;29(5):487‐94. [DOI] [PubMed] [Google Scholar]
- Roche G, Ponthieux A, Parot‐Shinkel E, Jousset N, Bontoux L, Dubus V, et al. Comparison of a functional restoration program with active individual physical therapy for patients with chronic low back pain: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2007;88:1229‐35. [DOI] [PubMed] [Google Scholar]
- Roche‐Leboucher G, Petit‐Lemanac'h A, Bontoux L, Dubus‐Bausière V, Parot‐Shinkel E, Fanello S, et al. Multidisciplinary intensive functional restoration versus outpatient active physicotherapy in chronic low back pain. Spine 2011;36(26):2235‐42. [DOI] [PubMed] [Google Scholar]
Skouen 2002 {published data only}
- Skouen JS, Grasdal AL, Haldorsen EMH, Ursin H. Relative cost‐effectiveness of extensive and light multidisciplinary treatment programs versus treatment as usual for patients with chronic low back pain on long‐term sick leave. Spine 2002;27(9):901‐10. [DOI] [PubMed] [Google Scholar]
Staal 2004 {published data only}
- Hlobil H, Staal JB, Twisk J, Köke A, Ariëns G, Smid T, et al. The effects of a graded activity intervention for low back pain in occupational health on sick leave, functional status and pain: 12‐month results of a randomized controlled trial. Journal of Occupational Rehabilitation 2005;15(4):569‐80. [DOI] [PubMed] [Google Scholar]
- Hlobil H, Uegaki K, Staal JB, Bruyne MC, Smid T, Mechelen W. Substantial sick‐leave costs savings due to a graded activity intervention for workers with non‐specific sub‐acute low back pain. European Spine Journal 2007;16:919‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staal JB, Hlobil H, Twisk JWR, Smid T, Köke AJA, Mechelen W. Graded activity for low back pain in occupational health care. Annals of Internal Medicine 2004;140:142‐3. [DOI] [PubMed] [Google Scholar]
Steenstra 2006 {published data only}
- Anema JR, Steenstra IA, Bongers PM, Vet HCW, Knol DL, Loisel P, et al. Multidisciplinary rehabilitation for subacute low back pain: Graded activity or workplace intervention or both?. Spine 2007;32(3):291‐8. [DOI] [PubMed] [Google Scholar]
- Steenstra IA, Anema JR, Bongers PM, Vet HCW, Knol DL, Mechelen W. The effectiveness of graded activity for low back pain in occupational health care. Occupational and Environmental Medicine 2006;63:718‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Storheim 2003 {published data only}
- Storheim K, Brox JI, Holm I, Koller AK, Bø K. Intensive group training versus cognitive intervention in sub‐acute low back pain: short‐term results of a single‐blind randomized controlled trial. Journal of Rehabilitation Medicine 2003;35:132‐40. [DOI] [PubMed] [Google Scholar]
van den Hout 2003 {published data only}
- Hout JHC, Vlaeyen JWS, Heuts PHTG, Zijlema JHL, WIjnen JAG. Secondary prevention of work‐related disability in nonspecific low back pain: Does problem‐solving therapy help? A randomized clinical trial. The Clinical Journal of Pain 2003;19(2):87‐96. [DOI] [PubMed] [Google Scholar]
Wright 2005 {published data only}
- Wright A, Lloyd‐Davies A, Williams S, Ellis R, Strike P. Individual active treatment combined with group exercise for acute and subacute low back pain. Spine 2005;30(11):1235‐41. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Alaranta 1994 {published data only}
- Alaranta H, Rytokoski U, Rissanen A, Talo S, Ronnemaa T, Puukka P, et al. Intensive physical and psychosocial training program for patients with chronic low back pain. A controlled trial. Spine 1994;19(12):1339‐49. [DOI] [PubMed] [Google Scholar]
Aure 2003 {published data only}
- Aure OF, Hilsen JH, Vasseljen O. Manual therapy and exercise therapy in patients with chronic low back pain. Spine 2003;28(6):525‐32. [DOI] [PubMed] [Google Scholar]
Bentsen 1997 {published data only}
- Bentsen H, Lindgarde F, Manthorpe R. The effect of dynamic strength back exercise and/or a home training program in 57‐old women with chronic back pain. Results of a prospective randomized study with a 3 year follow‐up period. Spine 1997;22(13):1494‐500. [DOI] [PubMed] [Google Scholar]
Bültmann 2009 {published data only}
- Bültmann U, Sherson D, Olsen J, Hansen CL, Lund T, Kilsgaard J. Coordinated and tailored work rehabilitation: a randomized controlled trial with economic evaluation undertaken with workers on sick leave due to musculoskeletal disorders. Journal of Occupational Rehabilitation 2009;19:81‐93. [DOI] [PubMed] [Google Scholar]
Dahl 2001 {published data only}
- Dahl J, Nilsson A. Evaluation of a randomized preventive behavioural medicine work site intervention for public health workers at risk for developing chronic pain. European Journal of Pain 2001;5(4):421‐32. [DOI] [PubMed] [Google Scholar]
Dettori 1995 {published data only}
- Dettori JR, Bullock SH, Sutlive TG, Franklin RJ, Patience T. The effects of spinal flexion and extension exercises and their associated postures in patients with acute low back pain. Spine 1995;20(21):2303‐12. [DOI] [PubMed] [Google Scholar]
Friedrich 1998 {published data only}
- Friedrich M, Gittler G, Halberstadt Y, Cermak T, Heiller I. Combined exercise and motivation program: effect on the compliance and level of disablity of patients with chronic low back pain: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation 1998;79:475‐87. [DOI] [PubMed] [Google Scholar]
Hagen 2000 {published data only}
- Hagen EM, Eriksen HR, Ursin H. Does early intervention with a light mobilization program reduce long‐term sick leave for low back pain. Spine 2000;25(15):1973‐6. [DOI] [PubMed] [Google Scholar]
Hansen 1993 {published data only}
- Hansen FR, Bendix T, Skov P, Jensen CV, Kristensen JH, Krohn L, et al. Intensive, dynamic back muscle exercises, conventional physiotherapy, or placebo‐control treatment of low back pain. Spine 1993;18(1):98‐108. [DOI] [PubMed] [Google Scholar]
Kellett 1991 {published data only}
- Kellett KM, Kellett DA, Nordholm LA. Effects of an exercise program on sick leave due to back pain. Physical Therapy 1991;71(4):283‐93. [DOI] [PubMed] [Google Scholar]
Linton 2005 {published data only}
- Linton S, Boersma K, Jansson M, Svärd L, Botvalde M. The effects of cognitive‐behavioural and physical therapy preventive interventions on pain‐related sick leave: A randomized controlled trial. The Clinical Journal of Pain 2005;21(2):109‐19. [DOI] [PubMed] [Google Scholar]
Malmivaara 1995 {published data only}
- Malmivaraa A, Hakkinen UTA, Heinrichs M‐L, Koskenniemi L, Kuosma E, Lappi S, et al. The treatment of acute low back pain‐ bed rest, exercises or ordinary activity?. The New England Journal of Medicine 1995;332(6):351‐5. [DOI] [PubMed] [Google Scholar]
Moffett 1999 {published data only}
- Moffett JK, Torgerson D, Bell‐Syer S, Jackson D, Llewlyn‐Philips H, Farrin A, et al. Randomised controlled trial of exercise for low back pain: clinical outcomes, costs and preferences. BMJ 1999;319:279‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Niemisto 2003 {published data only}
- Niemistö L, Lahtinen‐Suopanki T, Rissanen P, Lindgren K, Sarna S, Hurri H. A randomized trial of combined manipulation, stabilizing exercises, and physician consultation compared to physician consultation alone for chronic low back pain. Spine 2003;28(19):2185‐91. [DOI] [PubMed] [Google Scholar]
Rantonen 2012 {published data only}
- Rantonen J, Luoto S, Vehtari A, Hupli M, Karppinen J, Malmivaara A, Taimela S. The effectiveness of two active interventions compared to self‐care advice in employees with non‐acute low back symptoms: a randomised controlled trial with a 4‐year follow‐up in the occupational health setting. Occupational and Environmental Medicine 2012;69:12‐20. [DOI] [PubMed] [Google Scholar]
Schiltenwolf 2006 {published data only}
- Schiltenwolf M, Buchner M. Comparison of a biopsychosocial therapy (BT) with a conventional biomedical therapy (MT) of subacute low back pain in the first episode of sick leave: a randomized controlled trial. European Spine Journal 2006;15(7):1083‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Seferlis 1998 {published data only}
- Seferlis T, Nemeth G, Carlsson AM, Girllstrom P. Conservative treatment in patients sick listed for acute low back pain: a prospective randomised study with 12 months' follow up. European Spine Journal 1998;7:461‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Torstensen 1998 {published data only}
- Torstensen TA, Ljunggren AE, Meen HD, Odland E, Mowinckel P, Geijerstam S. Efficiency and costs of medical exercise therapy, conventional physiotherapy, and self‐exercise in patients with chronic low back pain: A pragmatic, randomised, single‐blinded, controlled trial with 1 year follow‐up. Spine 1998;23(23):2616‐24. [DOI] [PubMed] [Google Scholar]
Whitfill 2010 {published data only}
- Whitfill T, Haggard R, Bierner SM, Pransky G, Hassett RG, Gatchel RJ. Early intervention options for acute low back pain patients: a randomized clinical trial with one‐year follow‐up outcomes. Journal of Occupational Rehabilitation 2010;20:256‐63. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Henchoz 2010 {published data only}
- Henchoz Y, Goumoënsa P, So AKL, Paillex R. Functional multidisciplinary rehabilitation versusoutpatient physiotherapy for non‐specific lowback pain: randomised controlled trial. Swiss Medical Weekly 2010;140:w13133. [DOI] [PubMed] [Google Scholar]
Jensen 2012 {published data only}
- Jensen C, Jensen OK, Nielsen CV. Sustainability of return to work in sick‐listed employees with low‐back pain. Two‐year follow‐up in a randomized clinical trial comparing multidisciplinary and brief intervention. BMC Musculoskeletal Disorders 2012;13:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vora 2012 {published data only}
- Vora RN, Barron BA, Almudevar A, Utell MJ. Work‐related chronic low back pain‐return‐to‐work outcomes after referral to interventional pain and spine clinics. Spine 2012;37(20):1282‐9. [DOI] [PubMed] [Google Scholar]
Additional references
Anema 2007
- Anema JR, Steenstra IA, Bongers PM, Vet HCW, Knol DL, Loisel P, et al. Multidisciplinary rehabilitation for subacute low back pain: Graded activity or workplace intervention or both?. Spine 2007;32(3):291‐8. [DOI] [PubMed] [Google Scholar]
Anema 2009
- Anema JR, Schellart AJ, Cassidy JD, Loisel P, Veerman TJ, Beek AJ. Can cross country differences in return‐to‐work after chronic occupational back pain be explained? An exploratory analysis on disability policies in a six country cohort study. Journal of Occupational Rehabilitation 2009;19:419‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Atkins 2004
- Atkins D, Best D, Briss PA, Eccles M, Falck‐Ytter Y, GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boutron 2005
- Boutron I, Moher D, Tugwell P, Giraudeau B, Poiraudeau S, Nizard R, et al. A checklist to evaluate a report of a non pharmacological trial (CLEAR NPT) was developed using consensus. Journal of Clinical Epidemiology 2005;58:1233‐40. [DOI] [PubMed] [Google Scholar]
Carroll 2010
- Carroll C, Rick J, Cameron J, Hillage J. Workplace involvement improves return to work rates among employees with back pain on long‐term sick leave: a systematic review of the effectiveness and cost‐effectiveness of interventions. Disability and Rehabilitation 2010;32(8):607‐21. [DOI] [PubMed] [Google Scholar]
Chinn 2000
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta‐analysis. Statistics in Medicine 2000;19(22):3127‐31. [DOI] [PubMed] [Google Scholar]
Chinn 2002
- Chinn S. Comparing and combining studies of bronchial responsiveness. Thorax 2002;57(5):393‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fordyce 1976
- Fordyce WE. Behavioral methods for chronic pain and illness. New York: Raven Press, 1976. [Google Scholar]
Furlan 2009
- Furlan AD, Pennick V, Bombardier C, Tulder M, Editorial Board, Cochrane Back Review Group. 2009 Updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009;34(18):1929‐41. [DOI] [PubMed] [Google Scholar]
Guzman 2001
- Guzman J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ 2001;322:1511‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guzman 2002
- Guzman J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary bio‐psycho‐social rehabilitation for chronic low back pain. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI: 10.1002/14651858.CD000963] [DOI] [PubMed] [Google Scholar]
Hayden 2005
- Hayden J, Tulder MW, Malmivaara A, Koes BW. Exercise treatment for treatment of non‐specific low back pain. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD000335.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heymans 2005
- Heymans M, Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non‐specific low‐back pain. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD000261] [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. Available from: www.cochrane‐handbook.org. The Cochrane Collaboration.
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Jousset 2004
- Jousset N, Fanello S, Bontoux L, Dubus V, Billabert C, Vielle B, et al. Effects of functional restoration versus 3 hours per week physical therapy: a randomized controlled study. Spine 2004;29(5):487‐94. [DOI] [PubMed] [Google Scholar]
Karjalainen 2000
- Karjalainen KA, Malmivaara A, Tulder MW, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low‐back pain among working age adults. Cochrane Database of Systematic Reviews 2000, Issue 3. [DOI: 10.1002/14651858.CD002193; Karjalainen K, Malmivaara A, Van Tulder M, Roine R, Juahiainen M, Koes B. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain in working‐age adults. Spine 2001;26(3):262‐9.] [DOI] [PubMed] [Google Scholar]
Krause 1998
- Krause N, Dasinger LK, Neuhauser F. Modified work and return to work: A review of the literature. Journal of Occupational Rehabilitation 1998;8(2):113‐39. [Google Scholar]
Lechner 1994
- Lechner DE. Work hardening and work conditioning interventions: Do they affect disability?. Physical Therapy 1994;74(4):471‐93. [DOI] [PubMed] [Google Scholar]
Loisel 2005
- Loisel P, Buchbinder R, Hazard R, Keller R, Scheel I, Tulder M, et al. Prevention of work disability due to musculoskeletal disorders: the challenge of implementing evidence. Journal of Occupational Rehabilitation 2005;15(4):507‐24. [DOI] [PubMed] [Google Scholar]
Ostelo 2000
- Ostelo RWJG, Tulder MW, Vlaeyen JWS, Linton SJ, Morley S, Assendelft WJJ. Behavioural treatment for chronic low‐back pain. Cochrane Database of Systematic Reviews 2000, Issue 2. [DOI: 10.1002/14651858.CD002014] [DOI] [PubMed] [Google Scholar]
Poiraudeau 2007
- Poiraudeau S, Rannou F, Revel M. Functional restoration programs for low back pain: a systematic review. Annales de Réadaptation et de Medicine Physique 2007;50:425‐9. [DOI] [PubMed] [Google Scholar]
Schonstein 1999
- Schonstein E, Kenny DT. Rethinking functional capacity evaluations. Proceedings of the Moving in on Occupational Injury; 1999 June 2‐5; Cairns, Australia. Oxford: Butterworth Heinemann, 1999.
Teasell 1996
- Teasell RW, Harth M. Functional restoration. Returning patients with chronic low back pain to work ‐ revolution or fad? [see comments]. Spine 1996;21(7):844‐7. [DOI] [PubMed] [Google Scholar]
van Oostrom 2009
- Oostrom SH, Driessen MT, Vet HCW, Franche RL, Schonstein E, Loisel P, et al. Workplace interventions for preventing work disability. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006955] [DOI] [PubMed] [Google Scholar]
van Tulder 2003
- Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 2003;28(12):1290‐9. [DOI] [PubMed] [Google Scholar]
Voaklander 1995
- Voaklander DC, Beaulne AP, Lessard RA. Factors related to outcome following a work hardening program. Journal of Occupational Rehabilitation 1995;5(2):71‐85. [DOI] [PubMed] [Google Scholar]
Waddell 1999
References to other published versions of this review
Schaafsma 2010
- Schaafsma FG, Schonstein E, Whelan KM, Ulvestad E, Kenny DT, Verbeek JH. Physical conditioning programs for improving work outcomes in workers with back pain. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD001822] [DOI] [PubMed] [Google Scholar]
Schaafsma 2011
- Schaafsma FG, Schonstein E, Ojajärvi A, Verbeek JH. Physical conditioning programs for improving work outcomes among workers with back pain. Scandinavian Journal of Work, Environment & Health 2011;37(1):1‐5. [DOI] [PubMed] [Google Scholar]
Schonstein 2003
- Schonstein E, Kenny DT, Keating JL, Koes BW. Work conditioning, work hardening and functional restoration for workers with back and neck pain. Cochrane Database of Systematic Reviews 2003, Issue 3. [DOI: 10.1002/14651858.CD001822] [DOI] [PubMed] [Google Scholar]
Schonstein 2003a
- Schonstein E, Kenny D, Keating J, Koes B, Herbert RD. Physical conditioning programs for workers with back and neck pain: a Cochrane systematic review. Spine 2003;28(19):E391‐5. [DOI] [PubMed] [Google Scholar]


