Abstract
Background
Coronavirus disease 2019 (COVID-19), formerly known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and 2019 novel coronavirus (2019-nCoV), was first identified in December 2019 in Wuhan City, China. Structural equation modeling (SEM) is a multivariate analysis method to determine the structural relationship between measured variables. This observational study aimed to use SEM to determine the effects of social support on sleep quality and function of medical staff who treated patients with COVID-19 in January and February 2020 in Wuhan, China.
Material/Methods
A one-month cross-sectional observational study included 180 medical staff who treated patients with COVID-19 infection. Levels of anxiety, self-efficacy, stress, sleep quality, and social support were measured using the and the Self-Rating Anxiety Scale (SAS), the General Self-Efficacy Scale (GSES), the Stanford Acute Stress Reaction (SASR) questionnaire, the Pittsburgh Sleep Quality Index (PSQI), and the Social Support Rate Scale (SSRS), respectively. Pearson’s correlation analysis and SEM identified the interactions between these factors.
Results
Levels of social support for medical staff were significantly associated with self-efficacy and sleep quality and negatively associated with the degree of anxiety and stress. Levels of anxiety were significantly associated with the levels of stress, which negatively impacted self-efficacy and sleep quality. Anxiety, stress, and self-efficacy were mediating variables associated with social support and sleep quality.
Conclusions
SEM showed that medical staff in China who were treating patients with COVID-19 infection during January and February 2020 had levels of anxiety, stress, and self-efficacy that were dependent on sleep quality and social support.
MeSH Keywords: Anxiety; SARS Virus; Social Support; Stress, Psychological
Background
Coronavirus disease 2019 (COVID-19), formerly known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and 2019 novel coronavirus (2019-nCoV), was first identified in December 2019 in Wuhan City in central China [1,2]. From the end of December 2019, COVID-19 began to spread rapidly throughout Hubei Province and other areas in China [2,3]. As of February 18th, 2020, more than 72,500 people had been diagnosed with COVID-19 in China, and more than 1,800 patients had died from this new viral infection, mainly from pneumonia and other respiratory complications [3].
From December 2019, medical staff in Wuhan, China, were working with an increased workload and at risk of infection to treat patients with COVID-19 infection. Up to February 18th, more than 30,000 doctors and nurses from other provinces in China arrived in Hubei Province to assist in the treatment of patients. Local and national medical staff worked in isolation wards, fever clinics, the Intensive Care Unit (ICU), and other related departments. Some medical staff became infected with COVID-19 when they were treating infected patients. Chinese medical staff have shown professionalism and care, but the physical and psychological health of medical staff is at risk when working under such conditions, and anxiety and stress can also adversely affect sleep.
Previous studies have shown that survivors of acute infectious diseases, such as SARS, can lead to anxiety, depression, stress, and posttraumatic stress disorder [4–6]. However, there have been few studies on the physical and psychological effects of outbreaks of serious infectious diseases on the medical staff, particularly when associated with increased workload and the stress associated with the risk of infection.
Sleep quality is a key indicator of health. For clinical staff, good sleep quality not only helps them to work better to treat patients but also maintains optimal immune function to prevent infection [7]. Therefore, sleep quality is an important indicator of health. Also, psychological wellbeing and sleep are affected by many socio-cultural factors [8]. Social support is a significant social factor. Social support refers to the care and support that people feel they get from other people [9]. Adequate social support has previously been reported to have a positive effect on psychological health and sleep function [10,11]. Also, anxiety is a common negative emotion experienced by medical staff during epidemics of infectious diseases [12]. The COVID-19 epidemic has become a stressor, particularly as this is a new viral infection does not have a vaccine and can only be treated symptomatically at present. Self-efficacy refers to individual judgment on the ability to complete a certain behavior or task [13]. Self-efficacy helps medical staff cope with high-risk and high-intensity work and help them maintain a stable mental state. The effect of emotion such as anxiety, stress, and self-efficacy on sleep quality has been shown by previous studies [14,15].
These variables of anxiety, self-efficacy, stress, sleep quality, and social support and their interactions can be analyzed by structural equation modeling (SEM), which is a multivariate analysis method to determine the structural relationship between measured variables. Therefore, this observational study, conducted at the Wuhan University School of Medicine, China, aimed to use SEM to determine the effects of social support on sleep quality and function of medical staff who treated patients with COVID-19 in January and February 2020. The two assumptions made in this observational study were that the social support given to the medical staff directly affected their sleep quality, and that social support affected sleep quality by reducing anxiety and stress and by increasing self-efficacy as intermediate variables.
Material and Methods
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki. All participants signed the consent form. The study was approved by the Wuhan University School of Medicine Ethics Committee (Approval number: 20180928).
Study participants
This study included 180 medical staff from several provinces who treated patients with COVID-19 infection in January and February 2020. All the study participants were either doctors or nurses who worked in departments of respiratory medicine, fever clinics, or the intensive care unit (ICU). All study participants volunteered to participate in the study.
Study design
An observational and cross-sectional clinical study was conducted that included the use of self-reported questionnaires. Demographic and social data from the medical staff were obtained. Levels of anxiety, self-efficacy, stress, sleep quality, and social support were measured using validated clinical questionnaires and scoring systems. All questionnaires were completed anonymously by the 180 participating medical staff.
Demographic and social data
Demographic and social data from the study participants included age, gender, education, and marital status. Professional and work information included their title, income, role, department, and work experience, or seniority.
The Social Support Rate Scale (SSRS) [16]
The SSRS was used to measure the type and levels of social support received by the medical staff [16]. The SSRS contained ten items consisting of three grades, with an aggregate score that ranged from 7–56. A higher score indicated higher levels of social support [16]. The Cronbach’s alpha for internal consistency for the use of the SSRS was 0.808.
The Self-Rating Anxiety Scale (SAS) [17]
The SAS was used to measure the levels of anxiety the mood of the medical staff [17]. The SAS questionnaire contained 20 items consisting of four grades, with questions based on feelings of anxiety and mood in the previous seven days. An aggregate score of 20 was then multiplied by 1.25, with higher scores indicating more severe levels of anxiety [17]. The Cronbach’s alpha for internal consistency for the use of the SAS was 0.821.
The General Self-Efficacy Scale (GSES) [18]
The Chinese version of the GSES was used to measure the feelings of self-efficacy by the medical staff [18]. The scale consisted of ten items, with a score for each item of between 1–4, and the total score of 10–40, with the final points were divided by 10. Higher scores indicated higher self-efficacy [18]. The Chinese version of the GSES has previously been shown to have high sensitivity and validity [18]. The Cronbach’s alpha for internal consistency for the use of the GSES was 0.805.
The Stanford Acute Stress Reaction (SASR) [19]
The SASR questionnaire was used to measure self-reported stress by the medical staff [19]. The SASR is a six-point Likert scale consisting of 30 items. Each item has a score of between 0–5, with a combined score ranging from 0–150, and a higher score indicating higher levels of self-reported stress [19]. The Cronbach’s alpha for internal consistency for the use of the SASR was 0.837.
The Pittsburgh Sleep Quality Index (PSQI) [20]
The PSQI questionnaire was used to measure sleep quality using an 18-item scale containing seven items that included sleep quality, sleep duration, sleep latency, habitual sleep efficiency, sleep disturbance, use of sleeping medications, and daytime dysfunction [20]. Each dimension scored between 0–3, with a total score ranging from 0–21, and a higher score indicating lower sleep quality [20]. The Cronbach’s alpha for internal consistency for the use of the PSQI was 0.811.
Statistical analysis
Data were presented as the mean ± standard deviation (SD). The chi-squared (χ2) test, Pearson’s correlation analysis, and multivariate analysis using the structural equation model (SEM) with path analysis were used to determine the structural relationship between the measured variables. Data were analyzed using EpiData version 3.1 software (EpiData, Buenos Aires, Argentina) and SAS version 9.4, software (SAS Institute, Cary, NC, USA), which were used for data entry and analysis. The intermediary effects of the variables were analyzed using IBM SPSS AMOS version 21.0 (IBM Corp., Armonk, NY, USA). The bootstrap number was set as 5,000. The significance of the specific intermediary was determined using the nonparametric percentile bootstrap method with deviation correction. Path analysis by the structural equation model (SEM) was performed to measure the associations and their importance. Path analysis included the use of the goodness-of-fit index (GFI), the adjusted goodness-of fit-index (AGFI) the incremental fit index (IFI), the comparative fit index (CFI), the Tucker-Lewis index (TLI), the normed fit index (NFI), and the root mean square error of approximation (RMSEA). The structural equation showed and ideal fit (GFI=0.995, CFI=0.995, TLI=0.953, IFI=0.996, NFI=0.991, AGFI=0.931, RMSEA=0.077, χ2/df=2.073). A P-value <0.05 was considered to be statistically significant.
Results
Demographic and working data of the medical staff who treated patients with COVID-19 in January and February 2020 in Wuhan, China
There were 220 medical staff who were initially asked to participate in the study, and 180 members of staff completed the study questionnaires, indicating a study participation rate of 81.82% at our medical center. The mean age of the medical staff was 32.31±4.88) years. The demographic and working data of the study participants are shown in Table 1.
Table 1.
Demographic and working data of the medical staff treating patients with COVID-19 in January and February 2020 in Wuhan, China.
| Variable | Number | % |
|---|---|---|
| Gender | ||
| Male | 51 | 28.3 |
| Female | 129 | 71.7 |
| Education | ||
| College degree or below | 34 | 18.9 |
| Bachelor’s degree | 82 | 45.6 |
| Master’s degree or above | 64 | 35.5 |
| Marital status | ||
| Unmarried | 41 | 22.8 |
| Married | 122 | 67.8 |
| Divorced or widowed | 17 | 9.4 |
| Seniority | ||
| Primary | 36 | 20.0 |
| Intermediate | 108 | 60.0 |
| Senior | 36 | 20.0 |
| Monthly income | ||
| <6000 yuan | 33 | 18.2 |
| 6000–10000 yuan | 110 | 70.6 |
| >10000 yuan | 37 | 11.2 |
| Profession | ||
| Doctor | 82 | 45.6 |
| Nurse | 98 | 54.4 |
| Department | ||
| Fever clinic or respiratory clinic | 86 | 47.8 |
| COVID-19 pneumonia isolation Hospital ward | 52 | 28.9 |
| Intensive Care Unit (ICU) | 42 | 23.3 |
| Working experience | ||
| <2 years | 26 | 14.4 |
| 2–5 years | 33 | 18.3 |
| >5 years | 121 | 67.2 |
Correlation between the findings from the self-reported questionnaires on anxiety, self-efficacy, stress, sleep quality, and social support
The levels of anxiety, self-efficacy, stress, sleep quality, and social support were measured using the Self-Rating Anxiety Scale (SAS), the General Self-Efficacy Scale (GSES), the Stanford Acute Stress Reaction (SASR) questionnaire, the Pittsburgh Sleep Quality Index (PSQI), and the Social Support Rate Scale (SSRS), respectively. Pearson’s correlation analysis was used to identify the correlations between the results from the responses of the medical staff.
There was a significant positive correlation between the SSRS scores and the GSES scores (r=0.405, P<0.01), and a negative correlation between the SSRS scores and the SAS scores (r=−0.565, P<0.01), the SASR scores (r=−0.391, P <0.01), and the PSQI scores (r=−0.413, P<0.01). There was a negative association between the GSES scores and the SAS scores (r=−0.351, P<0.01), and the SASR scores (r=−0.277, P<0.01), and the PSQI scores (r=−0.483, P <0.01). There was a significant positive correlation between the SAS scores and the SASR scores (r=0.397, P<0.01), and the PSQI scores (r=0.489, P<0.01). There was a significant positive association between the SASR scores and the PSQI scores (r=0.457, P<0.01). Table 2 summarizes these results.
Table 2.
The relationships between the Social Support Rate Scale (SSRS), the General Self-Efficacy Scale (GSES), the Stanford Acute Stress Reaction (SASR) questionnaire, the Self-Rating Anxiety Scale (SAS), and the Pittsburgh Sleep Quality Index (PSQI) of the medical staff treating patients with COVID-19.
| Mean | Standard deviation | SSRS | GSES | SAS | SASR | PSQI | |
|---|---|---|---|---|---|---|---|
| SSRS | 34.172 | 10.263 | 1 | ||||
| GSES | 2.267 | 0.767 | .405** | 1 | |||
| SAS | 55.256 | 14.183 | −.565** | −.351** | 1 | ||
| SASR | 77.589 | 29.525 | −.391** | −.277** | .397** | 1 | |
| PSQI | 8.583 | 4.567 | −.413** | −.483** | .489** | .457** | 1 |
P<0.01.
The data shown represent the scores of the questionnaires.
Path analysis of the effects of social support (from the SSRS) on sleep quality (from the PSQI)
Path analysis by the structural equation model (SEM) was performed to measure the associations and importance of social support on sleep quality in the medical staff. The structural equation showed and ideal fit (GFI=0.995, CFI=0.995, TLI=0.953, IFI=0.996, NFI=0.991, AGFI=0.931, RMSEA=0.077, χ2/df=2.073). The path analysis obtained from the SEM of the relationships from the results of the SSRS, the GSES, the SAS, the SASR, and the PSQI of medical staff (with standardized beta weighting) is shown in Figure 1.
Figure 1.
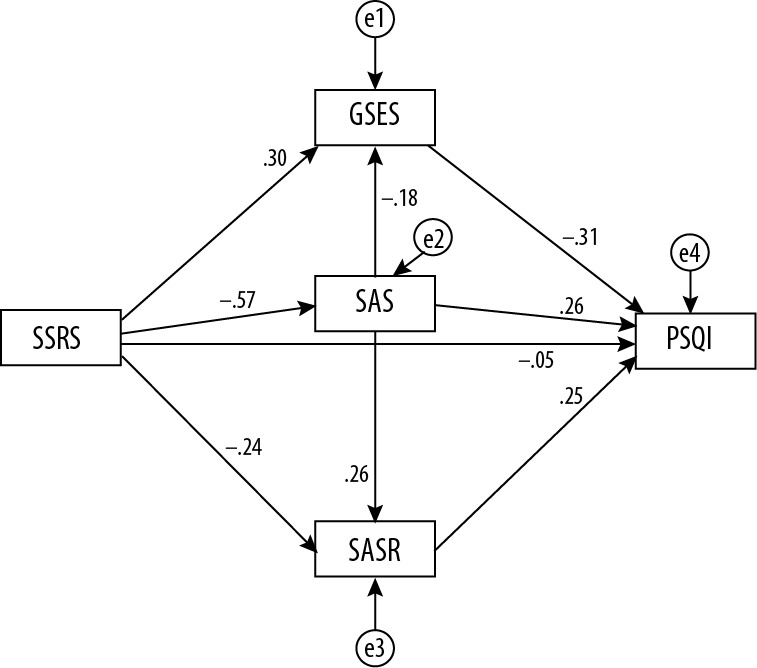
The path analysis obtained from the structural equation model (SEM) of the relationships from the results of the Social Support Rate Scale (SSRS), the General Self-Efficacy Scale (GSES), the Self-Rating Anxiety Scale (SAS), the Stanford Acute Stress Reaction (SASR), and the Pittsburgh Sleep Quality Index (PSQI) of medical staff (with standardized beta weighting).
Table 3 shows the normalized path coefficient. The SSRS scores of the medical staff negatively affected the SAS scores (β=−0.565, P<0.0001) and the SASR scores (β=−0.245, P=0.003) significantly and positively affected the GSES scores (β=0.304, P<0.001). The SAS scores positively affected the SASR scores (β=0.259, P=0.001) and the PSQI scores (β=0.257, P<0.001), and negatively affected the GSES scores (β=−0.179, P=0.029). The SASR scores significantly affected the PSQI scores (β=0.255, P<0.001). The GSES score negatively affected the PSQI scores (β=−0.308, P<0.001). However, the effect of the SSRS scores on the PSQI scores was not significant (β=−0.046, P=0.538).
Table 3.
The normalized path coefficients for the Social Support Rate Scale (SSRS), the General Self-Efficacy Scale (GSES), the Stanford Acute Stress Reaction (SASR) questionnaire, the Self-Rating Anxiety Scale (SAS), and the Pittsburgh Sleep Quality Index (PSQI) of the medical staff treating patients with COVID-19.
| Path | Standardization coefficient | Unstandardized coefficient | Standard error | Critical ratio | P-value | ||
|---|---|---|---|---|---|---|---|
| SAS | <--- | SSRS | −0.565 | −0.781 | 0.085 | −9.165 | *** |
| SASR | <--- | SSRS | −0.245 | −0.704 | 0.233 | −3.015 | 0.003 |
| GSES | <--- | SSRS | 0.304 | 0.023 | 0.006 | 3.723 | *** |
| SASR | <--- | SAS | 0.259 | 0.539 | 0.169 | 3.189 | 0.001 |
| GSES | <--- | SAS | −0.179 | −0.010 | 0.004 | −2.184 | 0.029 |
| PSQI | <--- | SAS | 0.257 | 0.082 | 0.023 | 3.514 | *** |
| PSQI | <--- | SASR | 0.255 | 0.039 | 0.010 | 3.937 | *** |
| PSQI | <--- | SSRS | −0.046 | −0.020 | 0.033 | −0.616 | 0.538 |
| PSQI | <--- | GSES | −0.308 | −1.820 | 0.380 | −4.788 | *** |
P<0.001 The data shown represent the scores of the questionnaires.
Hypothesis-testing using SEM
The two hypotheses tested in this study were hypothesis 1, that the social support given to the medical staff directly affected their sleep quality, and hypothesis 2, that social support affected sleep quality by reducing anxiety and stress and by increasing self-efficacy as intermediate variables. Based on the scores from the self-reported SSRS, SAS, GSES, SASR, and PSQI questionnaires, the results showed that the social support given to the medical staff negatively affected (reduced) their anxiety and stress levels, and positively affected their self-efficacy, but did not directly affect their sleep quality. The levels of staff anxiety significantly affected their levels of stress and significantly reduced their self-efficacy and sleep quality. Therefore, the hypothesis 1 was not supported and hypothesis 2 was confirmed.
Bootstrap indirect effects analysis of the intermediary effects of the variables
The intermediary effects of the variables were analyzed with the bootstrap number set as 5,000. The significance of the specific intermediary was determined using the nonparametric percentile bootstrap method with deviation correction. The path of SSRS→SAS→PSQI, when the confidence interval was not 0, showed that the SAS score had a significant effect between the SSRS score and the PSQI score (β=0.157, P=0.002). The path of SSRS→SASR→PSQI, when the confidence interval was not 0, showed that the SAS score had a significant effect between the SSRS score and the PSQI score (β=0.159, P<0.0001). Table 4 summarizes the findings of the bootstrap indirect effect analysis of the scores for the self-reporting questionnaires.
Table 4.
Result of the bootstrap indirect effects analysis of the Social Support Rate Scale (SSRS), the General Self-Efficacy Scale (GSES), the Stanford Acute Stress Reaction (SASR) questionnaire, the Self-Rating Anxiety Scale (SAS), and the Pittsburgh Sleep Quality Index (PSQI) of the medical staff treating patients with COVID-19.
| Mediation effect path | Standardization coefficient | Unstandardized coefficients | Standard error | 95% CI | P-value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| SSRS→SAS→PSQI | −0.145 | −0.064 | 0.019 | −0.107 | −0.031 | 0.000 |
| SSRS→GSES→PSQI | −0.094 | −0.041 | 0.014 | −0.075 | −0.018 | 0.000 |
| SSRS→SASR→PSQI | −0.062 | −0.028 | 0.012 | −0.056 | −0.009 | 0.002 |
| SSRS→SAS→GSES→PSQI | −0.031 | −0.014 | 0.007 | −0.030 | −0.002 | 0.025 |
| SSRS→SAS→SASR→PSQI | −0.037 | −0.016 | 0.008 | −0.037 | −0.005 | 0.002 |
Discussion
This study used the structural equation model (SEM) to determine the effects of social support on sleep quality and function of medical staff who treated patients with coronavirus disease 2019 (COVID-19) [1–3] in January and February 2020 in Wuhan, China. The levels of anxiety, self-efficacy, stress, sleep quality, and social support were measured using the Self-Rating Anxiety Scale (SAS), the General Self-Efficacy Scale (GSES), the Stanford Acute Stress Reaction (SASR) questionnaire, the Pittsburgh Sleep Quality Index (PSQI), and the Social Support Rate Scale (SSRS), respectively. The findings from this study showed that the sleep quality of the medical staff was low with a mean PSQI score of 8.583. Compared with the normal Chinese PSQI score of 7 points, the sleep quality of medical staff who treated COVID-19 was relatively low. There were several factors that may have resulted in reduced sleep quality in the medical staff. Doctors and nurses had to wear protective clothing every day, including hazardous materials (HazMat) suits. The staff worked continuously in the isolation wards with high work intensity and under pressure. Also, some of the patients could not be cured, and infection with COVID-19 is associated with patient mortality [1–3].
The findings from this study showed that social support of the medical staff did not directly affect their sleep quality, but had an indirect through several paths or steps. Firstly, social support reduces anxiety and stress, and improves self-efficacy. Social support can help medical staff reduce anxiety levels, as friends or family members provide social and emotional support and share empathy [21]. Social interactions reduce negative emotions such as anxiety and can improve mood [22]. Currently, with the increase in the number of cases of COVID-19 infection in China, front-line medical staff are required to wear protective masks and protective clothing, which may cause added stress. When medical staff have a wide social network, social support can help to reduce stress by reducing the perception of the threat of stressful events and the physiological response and inappropriate behavior that can result from stress [23]. Social support contributes to improving self-efficacy, leading to more understanding, respect, encouragement, courage, and a sense of professional achievement [24]. Self-efficacy results in increased confidence to do the job well, and when combined with social support, members of the medical profession suffer less from loneliness and might be more optimistic, which improves coping mechanisms when under stress [25,26].
Secondly, the combination of anxiety, stress, and self-efficacy of medical staff act on their sleep quality. Anxiety affects sleep quality because anxious people often find it difficult to fall asleep and may wake up frequently during sleep [27]. Also, the combination of anxiety with sleep disorders may make it difficult to fall asleep [28]. The fact that stress is closely related to sleep quality has been confirmed by a previous study [29]. Increased stress can increase the levels of vigilance regarding the environment, which will reduce sleep quality [30]. However, self-efficacy is a positive mental state that may enhance sleep quality [31]. People with high self-efficacy can maintain relatively stable emotions even under pressure, and they may experience fewer episodes of night waking, sleep anxiety, and sleep onset delay [32]. Self-efficacy also increases concentration and self-control [33]. Even though all medical staff experience pressure at work, people who have high self-efficacy are able to control their emotions and try to sleep regularly after work. Therefore, with high self-efficacy, medical staff may have good sleep quality. Anxiety has been shown to increase sensitivity to work pressure and the working environment and has a negative effect on self-efficacy because it reduces positive behaviors and initiative [34,35].
The findings from this study may provide support for the implementation of measures to improve the social support of medical staff during increased demands associated with COVID-19 infection at this time. For example, professional psychotherapy teams should take the initiative to support the mental health of medical staff and provide individually targeted interventions. Hospital managers should provide logistic support for medical staff, and support groups for medical staff should be established. However, this study had several limitations. Firstly, this was a cross-sectional study with a small sample size, and definitive causal relationships remain to be established. For example, anxiety may increase stress, and stress may increase anxiety [36]. However, anxiety has been shown to result in impaired sleep, and poor sleep quality increases anxiety [37]. Therefore, cohort studies with larger samples are needed to investigate the effects of social support on sleep quality and function of medical staff who are working with increased levels of stress and increased workloads, as with the COVID-19 infection epidemic in Wuhan, China. Also, this study used subjective self-reported questionnaires to obtain the data. Future studies should include objective indicators of stress, such as measurements of serum cortisol level with the questionnaire [38].
Conclusions
This observational cross-sectional clinical study aimed to use SEM to determine the effects of social support on sleep quality and function of medical staff who treated patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in Wuhan, China. Structural equation modeling (SEM) showed that medical staff had increased levels of anxiety, stress, and self-efficacy that were dependent on sleep quality and social support.
Acknowledgments
The authors thank the medical staff who participated in the study.
Footnotes
Source of support: This study was funded by the Basic Research Project of Coronavirus Disease 2019 Epidemic of Fundamental Research Funds for the Central Universities (Harbin Engineering University)
Conflict of interest
None.
References
- 1.World Health Organization. Novel Coronavirus (2019-nCoV) technical guidance. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance.
- 2.Centers for Disease Control and Prevention. 2019 Novel coronavirus. Wuhan China: Information for Healthcare Professionals; https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html. [Google Scholar]
- 3.World Health Organisation (WHO) Coronavirus disease 2019 (COVID-19) Situation Report-29. Feb 18, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200218-sitrep-29-covid-19.pdf.
- 4.Wu KK, Chan SK, Ma TM. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) J Trauma Stress. 2005;18:39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawryluck L, Gold WL, Robinson S, et al. SARS control and psychological effects of Quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10:1206–12. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu KK, Chan SK, Ma TM. Posttraumatic stress after SARS. Emerg Infect Dis. 2005;11:1297–300. doi: 10.3201/eid1108.041083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lange T, Dimitrov S, Born J. Effects of sleep and circadian rhythm on the human immune system. Ann NY Acad Sci. 2010;1193:48–59. doi: 10.1111/j.1749-6632.2009.05300.x. [DOI] [PubMed] [Google Scholar]
- 8.Yao KW, Yu S, Cheng SP, Chen IJ. Relationships between personal, depression and social network factors and sleep quality in community-dwelling older adults. J Nurs Res. 2008;16:131–39. doi: 10.1097/01.jnr.0000387298.37419.ff. [DOI] [PubMed] [Google Scholar]
- 9.Brugha TS. Social networks and social support. Curr Opin Psychiat. 1990;3:264–68. [Google Scholar]
- 10.Prati B, Pietrantoni L. The relation of perceived and received social support to mental health among first responders: A meta-analytic review. J Community Psychol. 2010;38:403–17. [Google Scholar]
- 11.Kent de Grey RG, Uchino BN, et al. Social support and sleep: A meta-analysis. Health Psychol. 2018;37:787–98. doi: 10.1037/hea0000628. [DOI] [PubMed] [Google Scholar]
- 12.Peng EY, Lee MB, Tsai ST, et al. Population-based post-crisis psychological distress: An example from the SARS outbreak in Taiwan. J Formos Med Assoc. 2010;109:524–32. doi: 10.1016/S0929-6646(10)60087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 14.Dahlgren A, Kecklund G, Akerstedt T. Different levels of work-related stress and the effects on sleep, fatigue and cortisol. Scand J Work Environ Health. 2005;31:277–85. doi: 10.5271/sjweh.883. [DOI] [PubMed] [Google Scholar]
- 15.Chen XF, Zhang Y, Xu XL, et al. The mediating effects of anxiety, self-efficacy and sleep quality on the relationship between doctor-patient’s empathy and inflammatory marker in patients with ulcerative colitis. Med Sci Monit. 2019;25:7889–97. doi: 10.12659/MSM.917552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang W, Xu H, Zhao S, et al. Prevalence and influencing factors of co-morbid depression in patients with type 2 diabetes mellitus: A general hospital based study. Diabetol Metab Syndr. 2015;7:60. doi: 10.1186/s13098-015-0053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olatunji BO, Deacon BJ, Abramowitz JS, Tolin DF. Dimensionality of somatic complaints: Factor structure and psychometric properties of the Self-Rating Anxiety Scale. J Anxiety Disord. 2006;20:543–61. doi: 10.1016/j.janxdis.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Zhang X, Zhan Y, Liu J, et al. Chinese translation and psychometric testing of the cardiac self-efficacy scale in patients with coronary heart disease in mainland China. Health Qual Life Outcomes. 2018;16:43. doi: 10.1186/s12955-018-0872-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cardeña E, Koopman C, Classen C, et al. Psychometric properties of the Stanford Acute Stress Reaction Questionnaire (SASRQ): A valid and reliable measure of acute stress. J Trauma Stress. 2000;13:719–34. doi: 10.1023/A:1007822603186. [DOI] [PubMed] [Google Scholar]
- 20.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 21.Yang NX, Xiao H, Wang W, et al. Effects of doctors’ empathy abilities on the cellular immunity of patients with advanced prostate cancer treated by orchiectomy: The mediating role of patients’ stigma and self-efficacy. Patient Prefer Adher. 2018;12:1305–14. doi: 10.2147/PPA.S166460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang NX, Xiao H, Cao YN, et al. Influence of oncology nurses’ empathy on lung cancer patients’ cellular immunity. Psychol Res Behav Manag. 2018;11:279–87. doi: 10.2147/PRBM.S168649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adamczyk K, Segrin C. Perceived social support and mental health among single vs. partnered polish young adults. Curr Psychol. 2015;34:82–96. doi: 10.1007/s12144-014-9242-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glozah FN. Exploring Ghanaian adolescents’ meaning of health and wellbeing: A psychosocial perspective. Int J Qual Stud Health Well-being. 2015;10:26370. doi: 10.3402/qhw.v10.26370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Segrin C, Passalacqua SA. Functions of loneliness, social support, health behaviors, and stress in association with poor health. Health Commun. 2010;25:312–22. doi: 10.1080/10410231003773334. [DOI] [PubMed] [Google Scholar]
- 26.Zhu MX, Sa D, Wu YL. The impact of social support on optimistic Tendency of college students: The mediating effects of sense of coherence and resilience. Psychol Sci. 2016;39:371–76. [Google Scholar]
- 27.Alvaro P, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36:1059–68. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. J Psych Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 29.Reeth OV, Weibel L, Spiegel K, et al. Interactions between stress and sleep: From basic research to clinical situations. Sleep Med Rev. 2000;4:201–19. [Google Scholar]
- 30.Jarrin DC, Chen IY, Ivers H, Morin CM. The role of vulnerability in stress-related insomnia, social support and coping styles on incidence and persistence of insomnia. J Sleep Res. 2014;23:681–88. doi: 10.1111/jsr.12172. [DOI] [PubMed] [Google Scholar]
- 31.Rutledge CM, La Guardia AC, Bluestein D. Predictors of self-efficacy for sleep in primary care. J Clin Nurs. 2013;22:1254–61. doi: 10.1111/jocn.12005. [DOI] [PubMed] [Google Scholar]
- 32.Bihlmaier I, Schlarb AA. Self-efficacy and sleep problems. Somnologie. 2016;20:275–80. [Google Scholar]
- 33.Przepiórka A, Błachnio A, Siu NY. The relationships between self-efficacy, self-control, chronotype, procrastination and sleep problems in young adults. Chronobiol Int. 2019;36:1–11. doi: 10.1080/07420528.2019.1607370. [DOI] [PubMed] [Google Scholar]
- 34.Miller RL, Pallant JF, Negri LM. Anxiety and stress in the postpartum: Is there more to postnatal distress than depression? BMC Psychiatry. 2006;6:12. doi: 10.1186/1471-244X-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bandura A, Adams NE. Analysis of self-efficacy theory of behavior change. Cognitive Ther Res. 1977;1:287–310. [Google Scholar]
- 36.Kolahkaj B, Zargar F. Effect of mindfulness-based stress reduction on anxiety, depression and stress in women with multiple sclerosis. Nurs Midwifery Stud. 2015;4:e29655. doi: 10.17795/nmsjournal29655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Poznanski B, Cornacchio D, Coxe S, et al. The link between anxiety severity and irritability among anxious youth: Evaluating the mediating role of sleep problems. Child Psychiatry Hum Dev. 2018;49:352–59. doi: 10.1007/s10578-017-0769-1. [DOI] [PubMed] [Google Scholar]
- 38.Luby JL, Heffelfinger A, Mrakotsky C, et al. Alterations in stress cortisol reactivity in depressed preschoolers relative to psychiatric and no-disorder comparison groups. Arch Gen Psychiatry. 2003;60:1248–55. doi: 10.1001/archpsyc.60.12.1248. [DOI] [PubMed] [Google Scholar]


