Abstract
Study Objectives:
Obstructive sleep apnea (OSA) is a sleep-related breathing disorder, commonly managed by either continuous positive airway pressure (CPAP) or a mandibular advancement device (MAD). Long-term follow-up and comparison regarding efficacy of these therapies is scarce. In this study the results of treatment, patient adherence, and satisfaction over a 10-year follow-up of these therapies are reported.
Methods:
This is a longitudinal follow-up study taken from a subset of patients initially enrolled in a randomized controlled clinical trial of 103 patients with OSA (51 and 52 patients randomized for MAD and CPAP, respectively). After a 10-year follow-up period, 14 patients using MAD and 17 patients using CPAP could be evaluated for this longitudinal follow-up study. Data were analyzed at baseline, after 3 months and at 1-, 2-, and 10-year follow-up. All 31 patients with OSA underwent polysomnography and self-reported measurements.
Results:
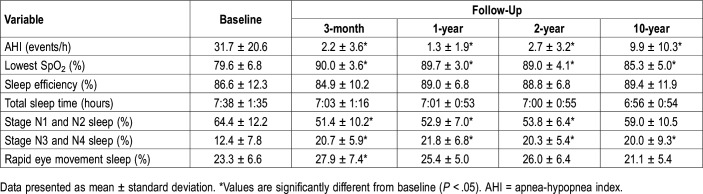
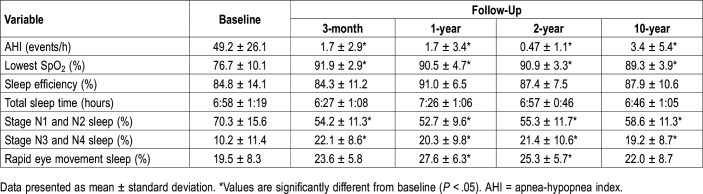
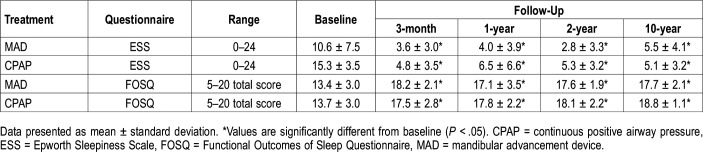
Polysomnography results showed a favorable outcome of both therapies at 10-year follow-up. At baseline, included patients in both groups did not significantly differ in apnea-hypopnea index (AHI) values. At 10-year follow-up, both the MAD and CPAP groups showed a significant reduction in AHI. At baseline the mean AHI in the MAD group was 31.7 ± 20.6 events/h whereas in the CPAP group it was 49.2 ± 26.1 events/h. At 10-year follow-up the mean AHI in the MAD group was 9.9 ± 10.3 events/h and in the CPAP group it was 3.4 ± 5.4 events/h. Both therapies resulted in a substantial improvement in self-reported neurobehavioral outcomes at 10-year follow-up.
Conclusions:
Both CPAP and MAD therapy demonstrate good and stable treatment effects after a 10-year follow-up period. Therefore, when indicated, both therapies are appropriate modalities for the long-term management of OSA.
Clinical Trial Registration:
Registry: Netherlands Trial Register; Name: Management of the Obstructive Sleep Apnea-Hypopnea Syndrome: Oral Appliance versus Continuous Positive Airway Pressure Therapy; Identifier: NL75; URL: https://www.trialregister.nl/trial/75
Citation:
Uniken Venema JAM, Doff MHJ, Joffe-Sokolova D, et al. Long-term obstructive sleep apnea therapy: a 10-year follow-up of mandibular advancement device and continuous positive airway pressure. J Clin Sleep Med. 2020;16(3):353–359.
Keywords: OSA-oral appliance therapy, OSA-PAP therapy, sleep disordered breathing, treatment outcome
BRIEF SUMMARY
Current Knowledge/Study Rationale: This study was performed to evaluate long-term efficacy of continuous positive airway pressure (CPAP) and mandibular advancement device (MAD) therapy in patients with obstructive sleep apnea. We evaluated the treatment effect of CPAP or MAD therapy over a 10-year treatment period in terms of changes in apnea-hypopnea index and quality of life, as well as patients’ adherence and treatment satisfaction.
Study Impact: In the current literature, no follow-up studies comparing CPAP or MAD therapy after a 10-year follow-up have been published. We found that both therapies show significant improvement in apnea-hypopnea index and saturation values, but also in self-reported sleepiness and quality of life. This study contributes to the knowledge of obstructive sleep apnea treatment and helps clinicians to inform patients on long-term effects of therapy.
INTRODUCTION
Selecting the appropriate treatment modality for obstructive sleep apnea (OSA) depends mainly on the severity of the disease and its symptoms.1 Anatomic characteristics and health status also are important. In mild to moderate OSA, mandibular advancement devices (MAD) are frequently used, whereas in moderate to severe OSA continuous positive airway pressure (CPAP) is usually applied.1–3
Short-term efficacy of MAD and CPAP therapy has been studied in many randomized controlled trials. CPAP is usually more effective in reducing the apnea-hypopnea index (AHI) in patients with moderate to severe OSA. However, CPAP can be complicated by suboptimal acceptance and adherence. In these cases an MAD is often a good and noninvasive alternative.3,4
Long-term studies of MAD and CPAP therapy generally show a more pronounced effect of CPAP in terms of AHI reductions and improvements in oxyhemoglobin saturation.1,5 Six studies have evaluated MAD treatment outcomes after a follow-up period exceeding 2 years.3,6–10 Of these six studies, only two studies compared the results of MAD with CPAP therapy.3,8 All patients experienced a reduction in AHI values at follow-up. In addition, no difference was observed between MAD and CPAP therapy in improvements of long-term daytime sleepiness. However, when evaluating the effects on daytime sleepiness only in patients with severe OSA, CPAP is more effective than MAD therapy.5 With long-term therapy aging and increases in weight may explain a relapse of treatment efficacy.11 However, with MAD therapy bite changes may also account for this phenomenon. This could reduce the advancement of the mandible, thereby reducing the efficacy of the MAD over the long term.12,13
Despite the numerous studies regarding treatment efficacy of MAD and CPAP therapy, long-term follow-up studies comparing both interventions are scarce. The aim of this longitudinal follow-up of a subset of individuals included in a randomized clinical trial is to evaluate the objective and self-reported outcomes of the both MAD and CPAP therapy in patients with OSA over the long term (10-year follow-up).13
METHODS
Patient selection
Participants were recruited for a randomized controlled trial, which was previously conducted and reported in two separate publications (ISRCTN18174167).3,13 Patients were recruited between September 2002 and August 2005 through the Department of Home Mechanical Ventilation of the University Medical Center Groningen, The Netherlands. This study was approved by the Groningen University Medical Center’s ethics committee (METc2002/032). A written informed consent was obtained from each patient before enrollment.
Study design
For this study initially 103 patients were selected. At baseline patients were randomly allocated to MAD or CPAP therapy (supplemental material). The current study is a longitudinal follow-up study taken from a subset of patients initially enrolled in this randomized controlled clinical trial. The focus of the current 10-year follow-up study was to evaluate only those patients still using their initially assigned treatment.
Interventions
At baseline all patients in the MAD group received the TAP appliance (Thornton Adjustable Positioner type-1, Airway Management Inc., Dallas, Texas). This duo-block MAD fixes the mandible in a forward position using a screw mechanism incorporated in the frontal area of the appliance. At baseline the appliance was set at approximately 50% of patients’ maximum protrusion. Patients were instructed to advance their appliance until symptoms abated or until further protrusion of the mandible resulted in discomfort. After an 8-week follow-up period a checkup was arranged to further adjust the appliance if necessary. When OSA symptomatology was improved or when further protrusion was not tolerated by the patient, a second evaluation was performed (a polysomnographic study, physical examination, or questionnaire evaluation).
The patients in the CPAP group received a nasal CPAP. After a 2-week adaptation period, patients returned for a follow-up visit to resolve any difficulties. After an 8-week follow-up period a checkup was arranged to further adjust the therapy if necessary. When OSA symptomatology was improved or when further pressure adjustments were not tolerated by the patient, a second evaluation was performed (a polysomnographic study, physical examination, or questionnaire evaluation). If polysomnography indicated an AHI ≥ 5 events/h, CPAP was adjusted if possible and a third polysomnography was performed.
Successful treatment was defined as an AHI < 5 events/h or reduction of AHI > 50% from the baseline value to a value < 20 events/h in a patient without symptoms while using the therapy. If treatment was not successful or if patients were nonadherent, the alternative (either MAD or CPAP therapy) was offered. Patients were excluded when they switched therapy or underwent upper airway surgery during follow-up. Furthermore, minimum therapeutic use for inclusion in this study was more than 5 nights/wk for more than 5 h/night.13 Patients were asked to fill out a questionnaire on how many h/night and how many nights/wk they used their therapy.
During follow-up, patients underwent a regular yearly checkup and were encouraged to contact the clinic when problems were faced concerning their OSA treatment.
Polysomnography
At baseline, 3-month follow-up, and at the 1, 2, and 10-year follow-up, a polysomnographic evaluation was performed (Embla A10 digital recorder, Medcare, Reykjavik, Iceland). Each polysomnographic recording started no later than 11:00 pm and ended no later than 9:00 am the next morning. Outcomes were limited to time in bed of the nocturnal part of the recording. All studies were conducted while patients slept at home and were analyzed by the same neurophysiologist, who was blinded for patients’ treatment (JHvdH).
Physical and neurobehavioral examinations
Physical and neurobehavioral examinations were also performed at baseline, 2 months, and at the 1, 2, and 10-year follow-up. This included registration of body mass index (BMI), neck circumference, alcohol consumption, tobacco use, and medications. The neurobehavioral examination was performed according to the following questionnaires: Epworth Sleepiness Scale (ESS), Functional Outcomes of Sleep Questionnaire (FOSQ), Short Form Health Survey, and a questionnaire evaluating adherence.14–16 Treatment satisfaction was evaluated by asking each patient to grade their treatment on a 10-point scale (with 1 indicating extreme dissatisfaction and 10 indicating extreme satisfaction).
Statistical analysis
Statistical analyses were performed with the Statistical Package for the Social Sciences (version 24, SPSS Inc., Chicago, Illinois). Means and standard deviations were reported. For comparing outcomes between continuous variables between baseline, 2 months, 1, 2 and 10-year follow-up, analysis of variance for repeated measurements analyses were performed. For comparing categorical variables, chi-square tests were performed. In all cases a significance level α of .05 was used.
RESULTS
Baseline characteristics
At baseline 103 patients were selected for this study, 51 were assigned to MAD and 52 were assigned to CPAP therapy (supplemental material). After 2 years of treatment 27 patients with a MAD (53%) and 37 using CPAP therapy (71%) completed the follow-up successfully while using their initial treatment modality.3 After 10 years of treatment, of the patients we were able to contact, we know that 18 patients with a MAD (35%) and 24 using CPAP therapy (46%) were still using their initial therapy. Of these patients, 4 in the MAD group and 7 in the CPAP group were not willing to undergo another polysomnographic evaluation at the 10-year follow-up. Consequently, 14 patients in the MAD group and 17 in the CPAP group could be included for this long-term follow-up study (supplemental material).
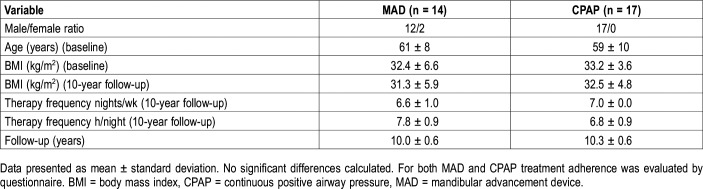
The mean follow-up in the MAD group was 10.0 ± 0.6 years, whereas the mean follow-up in the CPAP group was 10.3 ± 0.6 years (P > .05). None of the patients’ characteristics differed significantly at 10-year follow-up (Table 1). The mean therapeutic use in nights/wk at 10-year follow-up was 6.8 ± 0.5 and 6.8 ± 8.5 in the MAD and CPAP group, respectively. Furthermore, mean therapeutic use in h/night was 7.3 ± 1.2 and 7.1 ± 8.8 in the MAD and CPAP group, respectively. These data did not differ significantly (Table 1).
Table 1.
Patient characteristics.
Polysomnographic outcomes
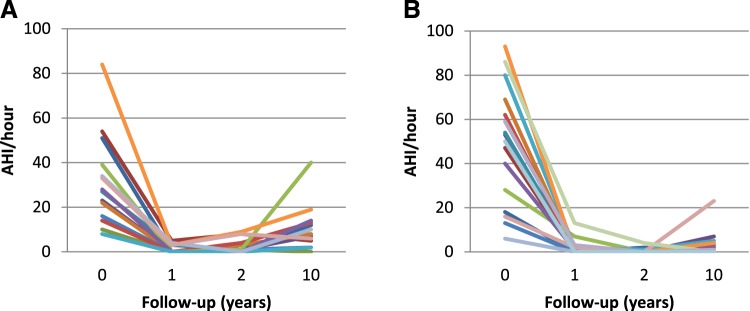
At baseline the mean AHI did not differ significantly between the groups. When evaluating the AHI after a 10-year treatment period, a slight increase in both groups was observed when compared with the 1- and 2-year follow-up (Figure 1, Table 2, and Table 3). At the 1-year follow-up the mean AHI in the MAD group was 1.3 ± 1.9 events/h and in the CPAP group 1.7 ± 3.4 events/h. At the 2-year follow-up the mean AHI in the MAD group was 2.7 ± 3.2 events/h and in the CPAP group 0.47 ± 1.1 events/h (P < .05). At the 10-year follow-up the mean AHI in the MAD group was 9.9 ± 10.3 events/h and in the CPAP group 3.4 ± 5.4 events/h (P < .05). Both therapies showed significant improvements (P < .05) from baseline to the 10-year follow-up (Figure 1, Table 2, and Table 3). When evaluating the patients in the MAD group individually, a wider statistical range in AHI results is seen at the 10-year follow-up compared with the CPAP group (Figure 2). When evaluating the lowest oxyhemoglobin saturation (SpO2) between baseline and 10-year follow-up a significant improvement is seen in both groups. Also, the percent of stage N3 and N4 sleep significantly increased between baseline and 10-year follow-up in both groups (Table 2 and Table 3).
Figure 1. Mean AHI values.
AHI = apnea-hypopnea index, CPAP = continuous positive airway pressure, MAD = mandibular advancement device.
Table 2.
Polysomnographic outcomes in the mandibular advancement device group (n = 14).
Table 3.
Polysomnographic outcomes in the continuous positive airway pressure group (n=17).
Figure 2. Individual AHI values of patients.
(A) Individual AHI values of patients who completed 10-year mandibular advancement device treatment follow-up. (B) Individual AHI values of patients who completed 10-year continuous positive airway pressure treatment follow-up. AHI = apnea-hypopnea index.
Treatment outcome
At the 2-month follow-up 80% of analyzed patients using a MAD and 86% of analyzed patients using CPAP therapy were treated successfully according to the predefined criteria. Unfortunately, the number of patients returning for treatment follow-up dropped over the years. At the 1-year follow-up 94% of analyzed patients using the MAD and 100% of analyzed patients using CPAP therapy were treated successfully. At 2-year follow-up this percentage was 93% and 95% for the MAD and CPAP group, respectively. Finally, at the 10-year follow-up, 86% of analyzed patients using a MAD and 94% of analyzed patients using a CPAP were treated successfully (Figure 3).
Figure 3. Treatment success.
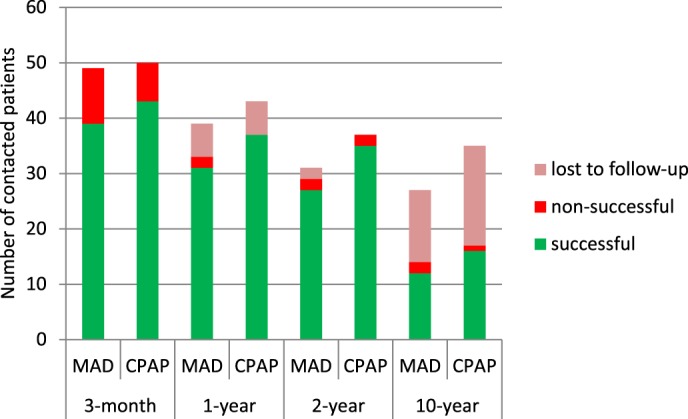
Successful treatment was defined by an AHI < 5 events/h or an AHI reduction of > 50% from the baseline value to a value < 20 events/h in a patient without symptoms while using the therapy (outcomes at the various time points were not statistically compared). AHI = apnea-hypopnea index, CPAP = continuous positive airway pressure, MAD = mandibular advancement device.
Of all patients initially treated with MAD therapy, 12 patients (24%) were treated successfully at 10-year follow-up. Of 51 patients, 22 patients (43%) were defined as unsuccessful, 3 (6%) were defined as nonadherent, and 14 (28%) were defined as lost to follow-up. In this 10-year period a total 12 patients (24%) switched from MAD to CPAP therapy (Figure S1 and Table S1 in the supplemental material).
At 10-year follow-up, 2 of 14 patients in the MAD group (14%) were defined as unsuccessful. One of these two patients switched to CPAP therapy, resulting in an AHI of 1.3 events/h. Another patient received a diagnosis of central sleep apnea. Another patient, who was already successfully treated at 10-year follow-up (AHI reduction from 28 to 14 events/h), received a new MAD that resulted in an AHI of 5.1 events/h. The first polysomnographic result of 10-year follow-up was used for the current analysis (Figure 2A).
Of all 52 patients initially treated with CPAP therapy, 16 (31%) were treated successfully at 10-year follow-up. Of the 52 patients, 6 (12%) were defined as unsuccessful, 8 (15%) were defined as nonadherent, and 22 (42%) were defined as lost to follow-up. In this 10-year period a total 4 patients (8%) switched from CPAP to MAD therapy (Figure S1 and Table S1).
At 10-year follow-up, therapy was defined as unsuccessful in 1 of 17 patients undergoing CPAP therapy (6%).
Patients using a MAD rated their therapy as 8.5 ± 1.3 points on a 10-point scale. Patients undergoing CPAP therapy rated it as 8.2 ± 0.9 points. These outcomes did not differ significantly.
Physical and neurobehavioral outcomes
Physical variables including BMI, neck circumference, alcohol consumption, tobacco use, and medication did not differ between both treatment groups at baseline. Also, no difference was observed between the baseline and 10-year follow-up data in both groups (Table S1). However, of the patients who were not successfully treated at 10-year follow-up, BMI was lowered in two patients (1 MAD and 1 CPAP group) and BMI increased in one (MAD group).
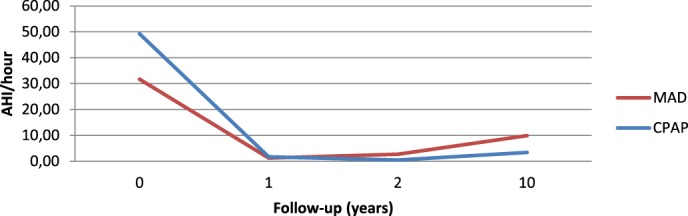
Outcomes with respect to the Epworth Sleepiness Scale (ESS) and Functional Outcomes of Sleep Questionnaire (FOSQ) showed improvement of neurobehavioral outcomes in both treatment groups. Most of the variables did not differ significantly between both therapies; only the baseline values of the ESS were significantly higher in the CPAP group. Significant improvements between baseline and the 10-year follow-up results in MAD and CPAP group were seen in all outcomes of the ESS and FOSQ questionnaires, except for the FOSQ-SE (intimate relationships and sexual activity) (Table 4 and Table S2 in the supplemental material).
Table 4.
Neurobehavioral outcomes in the MAD (n = 14) and CPAP (n=17) groups.
Outcomes on the Short Form Health Survey (RAND-36) did not differ significantly between the treatment groups. Significant improvement between baseline and 10-year follow-up were seen in the MAD group in Vitality, Social Functioning and Reported Change. Significant improvements between baseline and 10-year follow-up were seen in the CPAP group in Physical Health, Vitality, Social Functioning and Mental Health.
DISCUSSION
This study compared two major OSA therapies after a decade of treatment. To date it was largely unknown how treatment outcomes for patients with OSA develop over a 10-year treatment period. In this study we evaluated the basic characteristics, polysomnographic data, and self-reported data of patients treated with either CPAP or MAD therapy after a 3-month, 1-, 2-, and 10-year follow-up period. Many of the primarily included patients did not complete the 10-year treatment follow-up or did not respond to the invitation to participate in this long-term follow-up study. This is a longitudinal follow-up study taken from a subset of 31 patients initially enrolled in a randomized controlled clinical trial of 103 patients with OSA. However, of the patients who did still use their treatment most were still successfully treated in terms of AHI reduction and self-reported outcomes. It also appears that patients who maintain their therapy after a 10-year follow-up period are very content with their treatment. Striking, however, is that after 10 years most of the patients randomized to either MAD or CPAP therapy were either not using their device or we were not able to reach them.
When performing a 10-year follow-up study it is often challenging to perform the analysis with all patients included at baseline. At baseline, patients were randomly allocated to MAD or CPAP therapy. Consequently, the study started with two homogeneous groups. However, because of the high dropout and therapeutic failure rate in both groups, a reliable comparison between both groups at 10-year follow-up was not appropriate. This resulted in a longitudinal follow-up of a subset of patients included in a randomized clinical trial.
Although most of the patients were still effectively treated at 10-year follow-up, it was notable that the AHI in both the MAD and CPAP group increased compared with the previous follow-up periods. The relapse in AHI could possibly be explained by a change in lifestyle, health status, or aging. With aging, there is an increase in pharyngeal closing pressure and upper airway resistance, due to a decrease in upper airway dilatator muscle strength.17 Other possible reasons as to why AHI values increase with relative constant BMI values are not yet supported by scientific data. Relapse of MAD or CPAP therapy may result from an increase in upper airway laxity with time. In addition, BMI values reflect the body obesity that is not specific to the head and neck area. Fluid accumulation or shifts and local fat apposition in the head and neck area could also be factors attributing to changes in MAD and CPAP success on the very long-term. In addition, MAD therapy is known to result in changes in the dental occlusion and possibly maxillomandibular morphology. These aspects may also influence the amount of mandibular protrusion with the appliance, thereby affecting MAD outcome.18
Both therapies resulted in a successful treatment outcome at 10-year follow-up for most of the patients who completed the study. A confounding factor is that one of the inclusion criteria of the study was adherence of at least 5 h/night and 5 nights/wk. This results in a selected group of adherent patients evaluated for the current study. When both therapies are compared, CPAP is better in terms of lowering AHI values after a decade of treatment. However, MAD therapy tends to have a more positive result on improving the self-reported values such as sleepiness. Studies are performed on validity and reliability of the ESS and suggest that the score is useful for in-group comparison, however, not for individual-level comparison.19
Unfortunately, most of the initially included patients in this study did not complete the 10-year follow-up. Some of them were unsuccessful, whereas others were nonadherent, died, or were lost to follow-up. Eventually only 24% of patients in the MAD group and 31% of patients in the CPAP group completed the 10-year follow-up. Because we were not able to contact all patients, success rates are probably an underestimation of the true clinical effect of both therapies. Furthermore, patients in this study had the opportunity to switch therapy if they were considered nonadherent or unsuccessful. This might have biased our follow-up results.
Regarding success rates of the patients returning for follow-up polysomnography 76.5% of patients in the MAD group and 82.7% of patients in the CPAP group were treated successfully at 2-month follow-up.13 At 2-year follow-up success rates were 93.1% in the MAD group and 100% in the CPAP group.3 Regarding success rates of the patients who returned for 10-year follow-up, 86% of patients in the MAD group and 94% of patients in the CPAP group were treated successfully according to the success criterion used. Also, an improvement of SpO2, percent rapid eye movement sleep, and quality of life was observed. If we compare our data to success rates reported in other studies, similar outcomes are reported. A meta-analysis by Sharples et al concluded significant improvement of AHI in both MAD (−9.3 events/h, P < .01) and CPAP (−25.4 events/h, P < .01).5 In a meta-analysis, Li et al concluded improvement of AHI in both groups with a significant difference in favor of CPAP (P < .01), whereas quality of life improvements were scored similar in both groups.20 However, in both meta-analyses the mean follow-up of most analyzed studies was 12 weeks or less. Unfortunately, no studies have been done on the long-term outcomes of both interventions.
Some studies have reported on the success rates of long-term MAD therapy. In the 10-year follow-up study by Eriksson et al, 70% of patients in the MAD group were treated successful in terms of AHI reduction.8 However, the patients in the study overestimated treatment effect since 89% of MAD patients considered themselves cured. In the present study a similar phenomenon was observed. All patients rated their therapy positively at 10-year follow-up, despite the fact that 3 of 31 patients were not successfully treated. Consequently, a control polysomnographic study once every few years may be contemplated to check whether treatment is still effective. Wiman Eriksson et al analyzed 37 patients with OSA at 10-year follow-up. It was noted that weight and neck size remain stable in the group of positive responders.8 In the current study, BMI and neck circumference did not change significantly over time. Of the patients who were unsuccessfully treated at 10-year follow-up, BMI was lowered in 2 patients (1 in the MAD group and 1 in the CPAP group) and BMI increased in 1 patient (MAD group). Unfortunately we were not able to analyze the patients who dropped out of the study.
As mentioned previously, aging is one of the confounding factors for treatment success over the long term. Aging may result in anatomic changes in the upper airway that are associated with a decrease in upper airway dilator muscle activity and a decrease in the genioglossus negative pressure reflex.21 Consequently the AHI could increase as a result of an increased pharyngeal collapsibility and increased pharyngeal resistance.17 In addition, aging and other factors and systemic disorders, such as arthritis, cardiovascular disease, or stroke, may complicate OSA treatment.22,23 Finally, as a result of dental side effects and bite changes associated with long-term MAD therapy, a more protrusive position of the mandible may be necessary to maintain the same effect on the upper airway.12
When self-reported outcomes in this study are evaluated, an improvement is observed that is maintained at the 1-, 2-, and 10-year follow-up. In addition, patients were generally very satisfied with their treatment. Both therapies were graded higher than 8 on a scale of 1 to 10, slightly favoring the MAD group. However, similar to the objective outcomes we saw a slight deterioration in sleepiness between the 2- and 10-year follow-up, especially in the MAD group. However, self-reported outcomes are still significantly improved between baseline and the 10-year follow-up. If we compare the outcomes with normal values we can conclude that both therapies, if continued, have a favorable effect on long-term self-reported symptomatology.
It is concluded that MAD and CPAP therapy both result in a positive treatment outcome in terms of self-reported and objective improvements after 10-year follow-up. Both therapies significantly improve AHI, SpO2, percentage of rapid eye movement sleep, and have a positive effect on self-reported parameters. On average, patients who continued treatment remained stable in their favorable treatment outcome after a 3-month, 1-, 2-, and 10-year follow-up. Therefore, when indicated, both therapies are appropriate modalities for the long-term management of OSA.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- CPAP
continuous positive airway pressure
- ESS
Epworth Sleepiness Scale
- FOSQ
Functional Outcomes of Sleep Questionnaire
- MAD
mandibular advancement device
- OSA
obstructive sleep apnea
- SD
standard deviation
- SpO2
oxyhemoglobin saturation
DISCLOSURE STATEMENT
All authors, except for Dr. Stegenga, have seen and approved the manuscript. The deceased author qualifies as having made an authorship-worthy contribution to the paper. The deceased author knew the paper was being submitted and agreed to that prior to death. Work for this study was performed at the University Medical Center Groningen (UMCG), University of Groningen, Groningen, The Netherlands. This was not an industry-supported study. Dr. Hoekema is a medical advisor for Airway Management Inc, Somnomed and Zephyr Sleep Technologies. The other authors report no conflicts of interest.
REFERENCES
- 1.Ramar K, Dort LC, Katz SG, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015;11(7):773–827. doi: 10.5664/jcsm.4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383(9918):736–747. doi: 10.1016/S0140-6736(13)60734-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doff MH, Hoekema A, Wijkstra PJ, et al. Oral appliance versus continuous positive airway pressure in obstructive sleep apnea syndrome: a 2-year follow-up. Sleep. 2013;36(9):1289–1296. doi: 10.5665/sleep.2948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sawyer AM, Gooneratne NS, Marcus CL, et al. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343–356. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharples LD, Clutterbuck-James AL, Glover MJ, et al. Meta-analysis of randomised controlled trials of oral mandibular advancement devices and continuous positive airway pressure for obstructive sleep apnoea-hypopnoea. Sleep Med Rev. 2016;27:108–124. doi: 10.1016/j.smrv.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gauthier L, Laberge L, Beaudry M, et al. Mandibular advancement appliances remain effective in lowering respiratory disturbance index for 2.5-4.5 years. Sleep Med. 2011;12(9):844–849. doi: 10.1016/j.sleep.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Marklund M, Sahlin C, Stenlund H, et al. Mandibular advancement device in patients with obstructive sleep apnea: long-term effects on apnea and sleep. Chest. 2001;120(1):162–169. doi: 10.1378/chest.120.1.162. [DOI] [PubMed] [Google Scholar]
- 8.Wiman Eriksson E, Leissner L, Isacsson G, et al. A prospective 10-year follow-up polygraphic study of patients treated with a mandibular protruding device. Sleep Breath. 2015;19(1):393–401. doi: 10.1007/s11325-014-1034-5. [DOI] [PubMed] [Google Scholar]
- 9.Walker-Engström ML, Tegelberg A, Wilhelmsson B, et al. 4-year follow-up of treatment with dental appliance or uvulopalatopharyngoplasty in patients with obstructive sleep apnea: a randomized study. Chest. 2002;121(3):739–746. doi: 10.1378/chest.121.3.739. [DOI] [PubMed] [Google Scholar]
- 10.Marklund M. Long-term efficacy of an oral appliance in early treated patients with obstructive sleep apnea. Sleep Breath. 2016;20(2):689–694. doi: 10.1007/s11325-015-1280-1. [DOI] [PubMed] [Google Scholar]
- 11.Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. doi: 10.1016/j.smrv.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 12.Marklund M. Update on oral appliance therapy for OSA. Curr Sleep Med Rep. 2017;3(3):143–151. doi: 10.1007/s40675-017-0080-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoekema A, Stegenga B, Wijkstra PJ, et al. Obstructive sleep apnea therapy. J Dent Res. 2008;87(9):882–887. doi: 10.1177/154405910808700917. [DOI] [PubMed] [Google Scholar]
- 14.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 15.Weaver TE, Laizner AM, Evans LK. An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep. 1997;20:835–843. [PubMed] [Google Scholar]
- 16.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30((6):):473–483. [PubMed] [Google Scholar]
- 17.Eikermann M, Jordan AS, Chamberlin NL, et al. The influence of aging on pharyngeal collapsibility during sleep. Chest. 2007;131(6):1702–1709. doi: 10.1378/chest.06-2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doff MH, Finnema KJ, Hoekema A, et al. Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on dental side effects. Clin Oral Investig. 2013;17(2):475–482. doi: 10.1007/s00784-012-0737-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kendzerska TB, Smith PM, Brignardello-Petersen R, et al. Evaluation of the measurement properties of the Epworth sleepiness scale: a systematic review. Sleep Med Rev. 2014;18(4):321–331. doi: 10.1016/j.smrv.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Li W, Xiao L, Hu J. The comparison of CPAP and oral appliances in treatment of patients with OSA: a systematic review and meta-analysis. Respir Care. 2013;58(7):1184–1195. doi: 10.4187/respcare.02245. [DOI] [PubMed] [Google Scholar]
- 21.Pierce R, White D, Malhotra A, et al. Upper airway collapsibility, dilator muscle activation and resistance in sleep apnoea. Eur Respir J. 2007;30(2):345–353. doi: 10.1183/09031936.00063406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat 10. 2014;(260):1–161. [PubMed] [Google Scholar]
- 23.Kanasi E, Ayilavarapu S, Jones J. The aging population: demographics and the biology of aging. Periodontol 2000. 2016;72(1):13–18. doi: 10.1111/prd.12126. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.