Abstract
Background
Emotion dysregulation has emerged as a transdiagnostic factor that potentially exacerbates the risk of early-onset, maintenance, and relapse of psychosis. Mindfulness is described as the awareness that emerges from paying attention to the present moment without judgment. It gently pulls the mind out of the negative emotions induced by the disparity between expectation and reality by focusing on the present moment, instead of worrying about the future or regretting the past. However, only a few research has ever focused on the efficacy of using a mindfulness-based intervention to improve emotion regulation in schizophrenia spectrum disorders.
Purpose
The purpose of this study was to examine the effectiveness of a Mindfulness-Based Psychoeducation Programme (MBPP) on the emotion regulation of individuals with schizophrenia, in particular, to access emotion regulation strategies. The objective of this study was to find out whether MBPP is feasible for improving emotion regulation strategies, in terms of rumination, cognitive reappraisal, and expressive suppression, with a sustainable effect at a three-month follow-up.
Patients and Methods
A single-blinded pilot randomised controlled trial with repeated-measures designs was adopted. Forty-six participants diagnosed with schizophrenia and its subtypes were randomised in either the 8-week mindfulness-based psychoeducation programme or treatment-as-usual (control) group.
Results
The results of the Generalised Estimating Equations test indicated that the MBPP group showed a significant improvement in reappraisal at a three-month follow-up (β = −6.59, Wald’s χ2=4.55, p=0.033), and a significant reduction in rumination across time. However, the Generalised Estimating Equations indicated no significant difference in rumination and expressive suppression in the MBPP group. Two participants reported having unwanted experiences, including feelings of terror and distress during the mindfulness practice.
Conclusion
The MBPP appeared to be effective for improving emotion regulation, which will contribute to future large-scale RCT to confirm the treatment effects in more diverse groups of schizophrenic patients.
Keywords: schizophrenia, mindfulness, emotion regulation, reappraisal, suppression, rumination
Introduction
Schizophrenia is one of the top 25 leading causes of disability worldwide, it affects about 1.1% of the general population, i.e. more than 21 million people worldwide.1,2 It is highly associated with affective disturbance, psychiatric comorbidities, social dysfunction, illness relapse and suicide.3–5 Antipsychotics are effective in reducing the psychotic symptoms associated with schizophrenia but are considered ineffective for improving the functioning and residual symptoms.6,7 Recent practice guideline has informed the importance of using psychosocial intervention in conjunction with pharmacotherapy to improve the symptoms control, functioning, and relapse prevention.8–10 The guideline suggests that cognitive behavioural therapy (CBT), family intervention and social skills training have been confirmed to provide short-term benefits in mental status, symptom management, and enhance medication adherence.11 Unfortunately, these reports from CBT, social skills programme and family intervention are inconsistent with providing longer-term benefits, particularly in the mental status, functioning, and prevention of relapse.6,12–16 Besides, these interventions provide only limited empowerment of the patients’ illness management and fail to develop their acceptance attitude towards the illness and life difficulties, hence, resulting in a general pattern of unsuccessful long-term management and persistent unsatisfactory functioning in schizophrenia.7,17
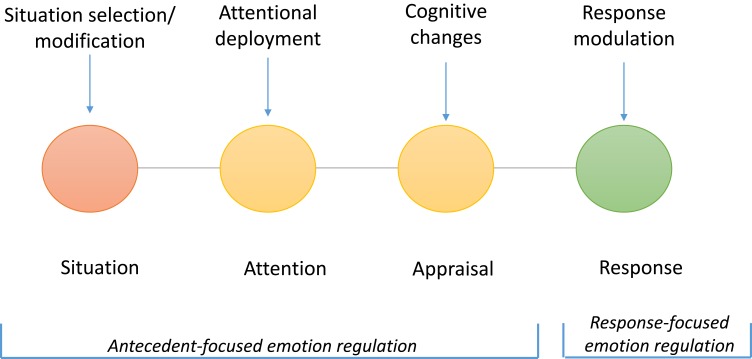
Emotion regulation difficulty refers to the difficulty of a person to modulate their emotions in response to emotion-elicited stimuli.18,19 The model for the process of emotion regulation by Gross (1998) explained that emotion regulation starts by selecting, or avoiding situation (situation selection/modification) that needs to be attended to (attentional deployment), giving rise to an appraisal of the situation’s valance and motivational relevance (cognitive appraisal), and expressing emotion in response to environmental demands (emotional modulation).20 (Figure 1). Attentional deployment refers to redirect one’s attention toward or away from an emotional situation; it may include rumination, which refers to a perseverative focus on thoughts and feelings associated with an emotion-eliciting event.21 Cognitive change involves one imbuing the emotional situation with meaning.22 Reappraisal is a form of cognitive change, involving a reinterpretation of the meaning of an emotional situation.21 Response modulation occurs when one attempts to directly influence the experiential, behavioural, and physiological response after the emotion is generated.22 Example includes expressive suppression in which people use expressive suppression to inhibit their emotional expression.21
Figure 1.
The process model of emotion regulation by Gross (1998).
Note: Gross JJ, The emerging field of emotion regulation: an integrative review, Rev Gen Psychol, 2(3), pp. 271-299, copyright © 1998 by SAGE Publications, Adapted with permission from SAGE Publications, Inc.22
It has been discovered that people with schizophrenia have difficulty with emotion regulation process. Findings exhibit that they have substantial emotion awareness deficits, and initiates more emotion regulation strategies at a lower threshold of negative emotional intensity.23,24 Studies also showed that schizophrenia patients select more emotion regulation strategies which include rumination, reappraisal, suppression, and situation modification, than healthy subjects.24 Besides, they become lost in the struggle of ruminations and attempts to confront negatively valenced experiences.24,25 Recent studies and meta-analysis suggested that compared to healthy controls, individuals with schizophrenia were associated with a greater use of rumination (g = −0.67, moderate to large effect size) and expressive suppression (g= −0.44), while an adaptive strategy, such as cognitive reappraisal (g = 0.49) was negatively associated with schizophrenia.24,26,27 Studies have discovered that the maladaptive use of rumination, reappraisal and suppression in schizophrenia is associated with negative emotion, affective blunting, exacerbation of symptoms, and relapse.28–32 The increased use of suppression is closely associated with reduced emotional expressivity or blunted affect, alongside the normal or even stronger emotional experience and intensity.33 Emotion regulation difficulties were also linked to the disruption of daily life and social function impairment.32,34–37
Better use of adaptive emotion regulation strategies may improve the emotion regulation process in schizophrenia, thus, informing a new therapeutic direction to help patients cope with emotional experiences.27 Studies have emerged to develop emotion regulation training in this population. There were a few pilot studies that investigated emotion regulation interventions involving third-wave CBT with integrated emotion regulation38 and Acceptance and Commitment Therapy (ACT).39,40 However, there is insufficient evidence to demonstrate its promising effects due to the limited sample sizes, lack of vigorous study designs and huge differences across the study protocols.
Mindfulness is described as an awareness that emerges from paying attention to the present moment without judgment. It gently pulls the mind away from the negative emotions induced by the disparity between expectation and reality by focusing on the present moment, instead of worrying about the future or regretting the past.25,41 Mindfulness-based interventions (MBI) have demonstrated good effects in reducing psychological outcomes in people with depression,42 anxiety disorders,43 substance use,44 bipolar affective disorder,45 and other chronic physical conditions.46,47 There is increasing evidence demonstrating the safety and effectiveness of MBI in schizophrenia. Our systematic review found that mindfulness-based intervention provides encouraging short-term benefits to people with schizophrenia; for instance improving depressive symptoms, functioning, and psychotic symptoms. Possible longer-term benefits include the improvement of psychotic symptoms and functioning from 6 months up to 2 years.48 Besides, mindfulness-based intervention integrated into psychoeducation has been confirmed to provide stronger and more desirable clinical outcomes in schizophrenia.48,49 Psychoeducation empowers patients with the knowledge, skills, strengths, and strategies, to overcome illness and its associated impairments.50 Mindfulness, on the other hand, engages the participants to accept the experience without explicitly reinforcing illness management and treatment compliance. Recent randomised controlled trials demonstrated that mindfulness psychoeducation provided significant improvements in cognitive insight, psychiatric symptoms, and functioning.41,51–53 A single-blind, multi-site, pragmatic randomised controlled trial conducted in Hong Kong, Mainland China, and Taiwan with 300 participants consistently demonstrated significant improvement with regard to insight into illness, functioning, mental state, and the length of rehospitalisations when compared with conventional psychoeducation and control groups.49 However, none of these studies identified mindfulness psychoeducation as a way to improve emotion regulation difficulty.
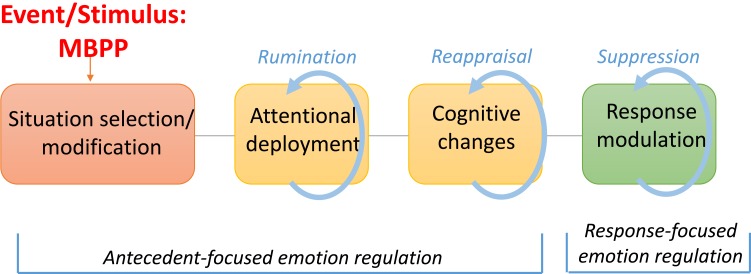
To the best of our knowledge, this is the first pilot randomised controlled trial (RCT) to explore the effectiveness of using MBPP as an emotion regulation skill training in schizophrenia. The objective of this study was to find out whether the MBPP would be feasible for improving the emotion regulation of these patients, in terms of rumination, cognitive appraisal, and suppression, and whether the positive effects could be sustainable up to a three-month follow-up period. The hypotheses encompassed the core emotion regulation process regarding attentional deployment, cognitive appraisal, and response modulation22 (Figure 2).
Figure 2.
A proposed conceptual framework.
Methods
Trial Registration
This trial was registered at ClinicalTrials.gov (ClinicalTrials.gov Identifier: NCT03632278).
Study Design
The study was a single-blind, multi-centre RCT, using a repeated-measures design to examine the treatment outcomes for people with schizophrenia spectrum disorders in the community. A parallel-group randomised closely at 1:1 was chosen. The study was approved by the Human Subjects Research Ethics Committee at the Institutional Review Boards of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW18-004) and The Hong Kong Polytechnic University (HSEARS2018531001). All research methods followed the Declaration of Helsinki, and conformed to the principles of medical ethics.
Participants
Samples were recruited from two Integrated Community Centres for Mental Wellness (ICCMWs), and two Long Stay Care Homes (LSCHs) covering a large geographical region (New Territories and Kowloon) of Hong Kong. ICCMW is a community mental health centre providing accessible community support and social rehabilitation services to patients with various mental health problems, ranging from suspected mental disturbance to ex-mentally ill persons in all age groups. LSCH provides long-term residential care for all kinds of chronic psychiatric patients who are in stable mental condition but require assistance and support with activities of daily living. The inclusion criteria for participants in this study includes: aged 18–65 years old; diagnosed with schizophrenia-spectrum disorders according to the criteria of the Diagnostic and Statistical Manual for Mental Disorders DSM-IV-TR (and the latest DSM-V) or International Classification of Diseases (ICD-10) – Classification of Mental Disorders; able to communicate in Chinese/Cantonese and give informed consent; and able to understand/follow the study and instructions for mindfulness training. Exclusion criteria include; individuals with comorbid organic brain disorders or substance abuse; recently participating in any forms of cognitive therapy, mind-body therapy, or mindfulness training (in forms of Tai Chi, Qi Gong or mind-body yoga) during the previous 3 months.
Whitehead et al (2016) determined that the optimal sample size of a pilot study was 20 per treatment arm for a small standardised effect size (0.2), and this rule of thumb was used to determine the sample size in the main trial designed with 80% power and two-sided 5% significance.54–56 The target number of recruitments in this study was therefore set at 50 with consideration of a 20% attrition rate.
Randomisation and Masking
The patients who applied to participate in the study were assessed by a trained research nurse in a face-to-face visit. The research nurse assessed these patients with the inclusion and exclusion criteria; explained to them the study’s aim, procedures, and the use of data. Participants then signed the full consent form if they agreed to participate. The trained research nurse administered the baseline measures after obtaining their informed written consent. This trained research nurse was blinded to treatment allocation.
The consenting participants were randomised into either the intervention or control group by an independent research assistant. This independent research assistant generated a randomised list, in which the eligible participants were assigned a unique number using a computer program for the randomisation.57 Block randomisation was adopted. Randomly mixed block sizes (from 2 to 10) were used to ensure the concealment of the allocation using a computer program.58 This sequence of randomisation was repeated until all patients were recruited. To minimise assessor bias, the outcome assessor was blinded to the treatment allocation. Participants were asked not to discuss their study participation with other patients throughout the study period to minimise potential contamination.
Intervention
The mindfulness-based psychoeducation programme (MBPP) was conducted for 90 mins in each session, once a week for 8 weeks, with 6–8 participants per group. The protocol was developed based on the model of mindfulness-based stress reduction proposed by Kabat-Zinn (1992)59 and Chien and Lee (2013).41 The treatment protocol and its main contents are shown in Table 1. There are four-key components in the programme:
Engagement and empowerment;
Mindfulness in daily living and problem solving;
Mindfulness in illness management; and
Equip and prepare for the future.
Table 1.
Treatment Protocol of Mindfulness-Based Psychoeducation Programme (MBPP)
| Session | Theme | Component and Goals of Each Session | Contents |
|---|---|---|---|
| 1 | Orientation & engagement |
|
|
| 2 | Awareness & Acceptance |
|
|
| 3 | Non-judgement |
|
|
| 4 | Stay present & Let go |
|
|
| 5 | Response without reacting |
|
|
| 6 | Our thoughts are not real |
|
|
| 7 | Empowerment of self-control |
|
|
| 8 | Relapse prevention and Care in community |
|
|
All sessions comprised the mindfulness practice (at least 20 mins) and group discussion. The programme is focused on cultivating in the participants an awareness of the present moment with an accepting, non-judgmental and letting go attitude. It also explored mindfulness approaches in illness management, problem-solving and daily living, and equipped the participants with future plans of relapse prevention and mindful living. There were two interventionists; one is a mindfulness instructor, an experienced mindfulness interventionist in psychosis. The other is a psychiatric nurse who has experience in psychoeducation group facilitation and assisting mindfulness-based interventions.
The participants were all encouraged to engage in a daily mindfulness practice guided by mindfulness audio-tracks on an MP3 player distributed to them. They were encouraged to practice mindfulness for at least 5 mins per day according to the practice manual, and submit their logbook records of daily self-practice each week to the researchers.
The treatment-as-usual group received routine psychiatric outpatient services. To minimise the inflated intervention effect due to awareness of no additional intervention received, the participants in the control group received a brief telephone contact once a week for 5 mins to discuss their illness condition and daily issues during the intervention period (i.e. weekly telephone contacts for 8 weeks).
Outcomes
Outcome assessments were conducted at recruitment, and immediately after and three-month post-intervention by the research nurse who was blind to the group/intervention assignment. The primary outcomes were reappraisal and suppression, which are measured by the Chinese version of the Emotion regulation questionnaire (ERQ),60,61 and rumination which was measured using the Short Ruminative Response Scale (SRRS).62,63 Secondary outcomes included affective symptoms, psychotic symptoms and ability of mindfulness, which were measured using the Chinese version of Depression Anxiety Stress Scale (DASS-21),64,65 Chinese version of Psychotic Symptom Rating Scale (C-PSYRATS),66,67 and the Five Facet Mindfulness Questionnaire – Short form (FFMQ-SF),68,69 respectively.
Patients’ demographic and clinical data were also collected at the baseline. The negative symptoms were measured by the Self-Assessment of Negative Symptoms (SANS)70 as a covariate in the outcome analysis. Dosages of antipsychotics were converted into chlorpromazine equivalents for comparison.71
Statistical Analyses
The quantitative data were analysed using IBM, SPSS for Windows version 19. The homogeneity of the demographic characteristics and baseline scores between the two study groups were examined using the independent sample t-test (two-tailed), or the Pearson Chi-square test, according to their level of measurement.
The statistical data analyses comparing the clinical outcomes between the MBPP and TAU were based on the intention-to-treat analysis (ITT), which included all randomised patients regardless of their adherence to the intervention.72 A generalised estimating equations (GEE) test was used to investigate the interactive (group × time) effect to compare the changes in all individual outcome variables between the two study groups across time (or measurements), and the effects of time on each of the outcome variables. AutoRegressive Order 1 (AR(1)) model was applied in the GEE model to consider the time dependence of outcome variables in the working correlation matrix.73 Pairwise comparison was used to examine the group differences on each of the outcome variables at each time of measurement. Potential covariates should be considered based on the anticipated prognostic variables rather than the significant baseline differences.56,73 Therefore, the results of this study presented the adjusted model of GEE to compare the difference after the adjustment of the covariant of emotion regulation, which includes age, gender, duration of illness, the dosage of antipsychotic medication, and negative symptoms. The statistical significance of all statistical tests was set at 0.05.
Results
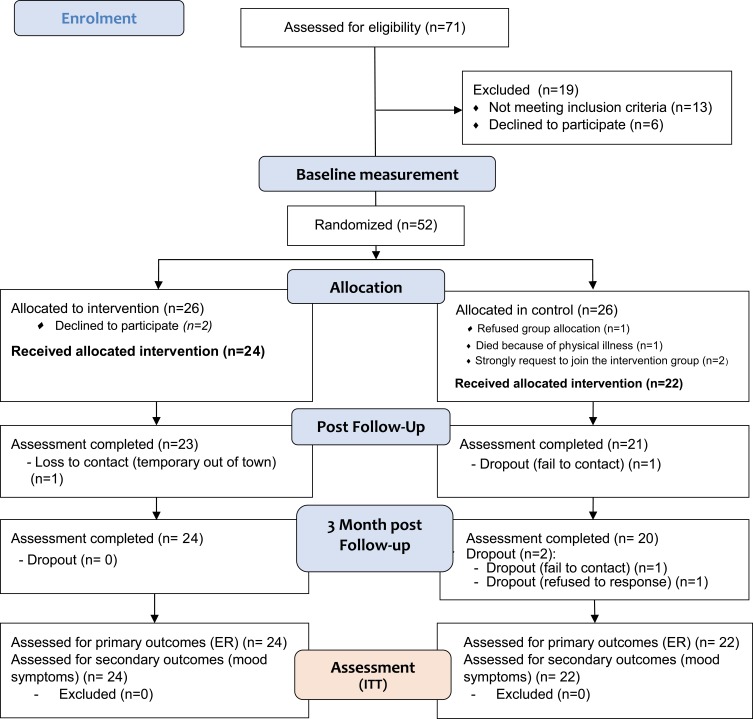
Seventy-one patients were referred to the MBPP during the subject recruitment period between April and October 2018. Nineteen of them were excluded, 13 of which did not meet the inclusion criteria and six refused to participate due to lack of interest or time (Figure 3).
Figure 3.
Flow through trial of MBPP (The CONSORT diagram).
Fifty-two participants were randomly assigned into either the intervention (n=26) or control (n=26) group. After the allocation, one of the participants died of an acute medical problem; and three participants disagreed to be in the intervention allocation group and withdrew from the study. Meanwhile, two participants from the control group repeatedly expressed a “strong preference” to the MBPP. They participated in the intervention group according to their preference but their results were omitted from the analysis. Finally, there were 46 participants used for the final data analysis. The majority of the participants were female (76.1%), aged over 45 years (80.4%), married (73.9%), and had a long duration of illness (ie, 93.5% had >10 years of illness. There were no statistically significant differences in all of these characteristics or in the mean scores of all outcome measures at the baseline (see Table 2).
Table 2.
Demographic and Clinical Characteristics of the Participants
| Total (n=46) | Intervention Group (n=24) | Control Group (n=22) | t-Test/ Chi-Square Test | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | Test Value | p-value | |||
| Gender | 0.330 | 0.857 | ||||||||
| Male | 11 | 23.9% | 6 | 25% | 5 | 23% | ||||
| Female | 35 | 76.1% | 18 | 75% | 17 | 77% | ||||
| Age | 2.589 | 0.460 | ||||||||
| 25–34 | 4 | 8.7% | 1 | 4.2% | 3 | 14% | ||||
| 35–44 | 5 | 10.9% | 2 | 8.3% | 3 | 14% | ||||
| 45–54 | 20 | 43.5% | 10 | 41.7% | 10 | 45% | ||||
| 55+ | 17 | 36.9% | 11 | 45.8% | 6 | 27% | ||||
| Education | 7.840 | 0.098 | ||||||||
| University/ College | 7 | 15.2% | 2 | 8.3% | 5 | 13% | ||||
| Secondary | 25 | 54.4% | 16 | 66.7% | 9 | 41% | ||||
| Primary | 6 | 13% | 3 | 12.5% | 3 | 23% | ||||
| No qualifications | 2 | 4.4% | 2 | 8.3% | 0 | - | ||||
| Others | 6 | 13% | 1 | 4.2% | 5 | 23% | ||||
| Marital status | 1.534 | 0.464 | ||||||||
| Single | 4 | 8.7% | 1 | 4.2% | 3 | 14% | ||||
| Married | 34 | 73.9% | 18 | 75% | 16 | 73% | ||||
| Divorced/ widowed | 8 | 17.4% | 5 | 20.8% | 3 | 13% | ||||
| Working status | 4.280 | 0.233 | ||||||||
| Employed FT | 6 | 13% | 2 | 8.3% | 4 | 18% | ||||
| Employed PT | 2 | 4.4% | 2 | 8.3% | 0 | – | ||||
| Unemployed | 25 | 54.3% | 15 | 62.5% | 10 | 46% | ||||
| Others | 13 | 28.3% | 5 | 20.8% | 8 | 36% | ||||
| Income | 1.649 | 0.648 | ||||||||
| No income | 35 | 76.1% | 19 | 79.2% | 16 | 73% | ||||
| Less than $8K | 7 | 15.2% | 4 | 16.7% | 3 | 14% | ||||
| $8 - 14.9K | 3 | 6.5% | 1 | 4.2% | 2 | 9% | ||||
| $15 – 24.9K | 1 | 2.2% | 0 | – | 1 | 4% | ||||
| Accommodation | 2.348 | 0.672 | ||||||||
| Private housing | 5 | 10.8% | 2 | 8.3% | 3 | 14% | ||||
| Public housing | 13 | 28.3% | 6 | 25% | 7 | 32% | ||||
| Half way home | 1 | 2.2% | 1 | 4.2% | 0 | – | ||||
| Long stay care home | 26 | 56.5% | 14 | 58.3% | 12 | 54% | ||||
| Others | 1 | 2.2% | 1 | 4.2% | 0 | – | ||||
| Living condition | 2.143 | 0.543 | ||||||||
| Alone | 5 | 10.8% | 3 | 12.5% | 2 | 9% | ||||
| With family | 13 | 28.3% | 5 | 20.8% | 8 | 36% | ||||
| In residential hostel | 27 | 58.7% | 15 | 62.5% | 12 | 55% | ||||
| Others | 1 | 2.2% | 1 | 4.2% | 0 | – | ||||
| Duration of illness | −0.889 | 0.374 | ||||||||
| Less than 10 years | 3 | 6.5% | 1 | 4% | 2 | 9% | ||||
| 10 – 19 years | 11 | 23.9% | 10 | 38% | 1 | 4% | ||||
| 20 – 29 years | 20 | 43.5% | 8 | 30% | 14 | 64% | ||||
| 30–39 years | 10 | 21.7% | 7 | 28% | 3 | 14% | ||||
| 40 years or above | 2 | 4.4% | 0 | – | 2 | 9% | ||||
| Psychiatric diagnosis | 1.607 | 0.448 | ||||||||
| Schizophrenia | 38 | 84.5% | 19 | 79.2% | 19 | 90% | ||||
| Paranoid schizophrenia | 2 | 4.4% | 1 | 4.2% | 1 | 5% | ||||
| Brief psychotic disorder | 5 | 11.1% | 4 | 16.7% | 1 | 5% | ||||
| CPZE | 3.061 | 0.382 | ||||||||
| Less than 500 | 20 | 43.5% | 12 | 50% | 8 | 35% | ||||
| 500 – 999 | 17 | 37% | 7 | 29.2% | 10 | 45% | ||||
| 1000–1499 | 5 | 10.8% | 3 | 12.5% | 2 | 10% | ||||
| 1500+ | 4 | 8.7% | 2 | 8.3% | 2 | 10% | ||||
The average number of attendances for each session on average in the MBPP was 6.88 (SD=1.39, range 3–8). Chien et al (2017) defined participants’ attendance of more than or equal to six sessions as satisfactory, while the attendance of fewer than six sessions was defined as low.49 Accordingly, 20 participants (84.6%) attended six sessions or above and were defined as satisfactory attendees, and four participants (8.33%) attended below six sessions and were defined as low attendees. Fourteen out of 24 (58.3%) participants engaged in the homework during the active intervention period, i.e. self-practice at home according to the audio mindfulness guidance. The average duration of the practice was 31 min per week (SD= 17.34, range 0–86.4 mins per week). There was no homework assignment after the active intervention period. Therefore, the self-mindfulness practice after the intervention period was not measured.
The attritions over the intervention and three-month follow-up periods were relatively low. At post-intervention follow-up, one participant from the intervention group was out of contact due to temporarily being out of town, and thus did not receive the first post-test; however, the patient participated at the three-month follow-up. Two participants in the control group did not complete the three-month post-assessment and were treated as dropouts, contributing to the attrition rate of 4.3%.
One participant reported a subjective feeling of terror when practising mindfulness at night-time during the intervention period. She said she avoided practising mindfulness at night-time, and thus all her mindfulness practice was done during the daytime. Another participant had a poor relationship with her family and expressed that her felt irritable when practising mindfulness and thus stopped self-practice over the follow-up period. These psychological discomforts were treated as mild adverse events and were reported to the Institutional Review Board.
Mean (and SD) values of baseline outcome scores and two post-tests for the participants are presented in Table 3. There were no significant differences on the baseline mean scores of all outcomes between groups (P=0.06–0.89).
Table 3.
Mean Scores (Standard Deviation) at Baseline, Post-Assessment (T2) and 3-Month Post-Assessment (T3)
| Mean (SD) | Baseline | p-value | T2 | T3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention Group | Control Group | Mean Diff. | Intervention Group | Control Group | Intervention Group | Control Group | ||||||||
| Primary Outcome | ||||||||||||||
| 1) SRRS | ||||||||||||||
| Total score | 16.83 | (4.59) | 17.00 | (3.84) | −0.17 | 0.89 | 14.78 | (5.65) | 14.19 | (3.37) | 14.83 | (5.25) | 15.55 | (4.49) |
| Brooding | 9.17 | (2.58) | 9.00 | (2.78) | 0.17 | 0.83 | 7.83 | (3.34) | 7.19 | (2.25) | 7.96 | (3.21) | 8.35 | (1.98) |
| Reflection | 7.67 | (2.43) | 8.00 | (2.00) | −0.33 | 0.62 | 6.96 | (2.704) | 7.00 | (2.26) | 6.88 | (2.31) | 7.20 | (3.22) |
| 2) ERQ | ||||||||||||||
| Reappraisal | 18.88 | (9.21) | 22.64 | (7.79) | −3.76 | 0.14 | 24.17 | (7.36) | 25.81 | (8.16) | 26.71 | (5.23) | 23.85 | (6.86) |
| Suppression | 11.96 | (5.88) | 14.50 | (4.62) | −2.54 | 0.11 | 13.78 | (6.84) | 12.14 | (6.55) | 13.08 | (4.54) | 13.50 | (4.93) |
| Secondary outcome | ||||||||||||||
| 3) DASS | ||||||||||||||
| Total score | 16.96 | (9.54) | 17.59 | (11.28) | −0.63 | 0.84 | 14.17 | (11.98) | 10.38 | (7.07) | 13.50 | (9.97) | 14.40 | (11.17) |
| Depression | 5.58 | (3.86) | 4.82 | (3.81) | 0.77 | 0.50 | 3.87 | (4.34) | 1.67 | (2.22) | 3.96 | (3.50) | 3.45 | (3.82) |
| Anxiety | 4.98 | (3.08) | 6.82 | (4.75) | −2.28 | 0.06 | 4.74 | (4.28) | 4.43 | (3.28) | 4.21 | (2.84) | 5.20 | (4.49) |
| Stress | 6.83 | (4.12) | 5.95 | (4.41) | 0.88 | 0.49 | 5.57 | (4.95) | 4.29 | (3.35) | 5.33 | (4.91) | 5.75 | (4.67) |
| 4) FFMQ | ||||||||||||||
| Total score | 56.20 | (7.16) | 59.32 | (10.55) | −3.12 | 0.24 | 58.56 | (7.31) | 58.74 | (7.33) | 60.79 | (5.18) | 58.86 | (7.96) |
| Observing | 9.21 | (2.87) | 10.41 | (3.20) | −1.20 | 0.19 | 10.12 | (2.58) | 9.54 | (3.42) | 11.00 | (2.36) | 9.20 | (3.22) |
| Describing | 9.42 | (3.52) | 10.91 | (3.85) | −1.49 | 0.17 | 9.67 | (3.52) | 9.98 | (3.57) | 10.79 | (3.66) | 11.13 | (3.14) |
| Awareness | 13.54 | (4.51) | 14.18 | (5.38) | −0.64 | 0.66 | 12.73 | (3.97) | 13.47 | (4.27) | 13.13 | (3.44) | 13.85 | (3.41) |
| Non-judging | 13.79 | (4.14) | 13.14 | (3.72) | 0.66 | 0.58 | 14.16 | (2.58) | 14.35 | (2.97) | 14.04 | (2.69) | 13.90 | (2.92) |
| Non-reacting | 10.23 | (3.36) | 10.69 | (3.16) | −0.45 | 0.65 | 11.87 | (3.15) | 11.40 | (2.06) | 11.83 | (2.06) | 10.77 | (3.26) |
| 5) PSYRAT | ||||||||||||||
| Total score | 8.33 | (13.25) | 11.50 | (15.59) | −3.17 | 0.46 | 5.38 | (10.05) | 7.45 | (11.84) | 3.21 | (6.88) | 8.10 | (14.50) |
| Total H score | 5.96 | (11.56) | 9.00 | (11.84) | −3.04 | 0.38 | 4.42 | (9.10) | 5.14 | (8.93) | 2.00 | (5.56) | 5.43 | (10.41) |
| Emotion H | 2.04 | (4.69) | 3.05 | (4.46) | −1.00 | 0.46 | 1.54 | (3.61) | 1.55 | (2.94) | 0.42 | (1.67) | 2.19 | (4.27) |
| Physical H | 1.04 | (1.92) | 1.73 | (2.41) | −0.69 | 0.29 | 0.79 | (1.614) | 1.05 | (1.89) | 0.54 | (1.53) | 1.05 | (2.04) |
| Control H | 1.50 | (2.776) | 2.45 | (3.14) | −0.95 | 0.28 | 1.04 | (2.33) | 1.27 | (2.25) | 0.50 | (1.35) | 1.19 | (2.34) |
| Cognitive H | 1.38 | (2.62) | 1.77 | (2.51) | −0.407 | 0.60 | 1.04 | (2.24) | 1.27 | (2.29) | 0.54 | (1.53) | 1.00 | (1.90) |
| Total D score | 2.38 | (4.80) | 2.50 | (5.83) | −0.13 | 0.94 | 0.96 | (3.33) | 2.32 | (4.90) | 1.21 | (3.48) | 2.67 | (5.74) |
| Cognitive D | 1.38 | (2.79) | 1.32 | (3.06) | 0.06 | 0.95 | 0.58 | (2.00) | 1.09 | (2.45) | 0.71 | (2.05) | 1.38 | (2.97) |
| Emotion D | 1.00 | (2.04) | 1.18 | (2.81) | −0.18 | 0.80 | 0.38 | (1.35) | 1.23 | (2.49) | 0.50 | (1.44) | 1.29 | (2.78) |
| SANS | 56.13 | (24.99) | 59.59 | (22.82) | −3.47 | 0.63 | ||||||||
Primary Outcomes – Emotion Regulation
Group X Time Interaction
GEE indicated that there was a statistically significant group X time interaction in the reappraisal at T3 (β = −6.59, 95% Confidence Interval (CI) = −12.63- −0.54, Wald’s χ2=4.55, p=0.033) of the crude model, with a moderate effect size (d=0.47) (Table 4). There was no group X time interaction in other primary outcomes (rumination and suppression).
Table 4.
Results of the Generalised Linear Model Regarding the Effects of MBPP on Emotion Regulation Outcomes
| Dependent Variable | Crude Model | Adjusted Model | ES Cohen’s d | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | CI | χ2 | p-value | B | CI | χ2 | p-value | |||||
| Upper | Lower | Upper | Lower | |||||||||
| SRRS | (intercept) | 16.83 | 14.98 | 18.68 | 317.59 | 0.000 | 17.43 | 15.31 | 19.54 | 260.67 | 0.000 | |
| Total score | Group | 0.17 | −2.51 | 2.84 | 0.01 | 0.903 | −0.97 | −4.39 | 2.45 | 0.31 | 0.580 | |
| Time (T2) | −2.06 | −4.19 | 0.07 | 3.58 | 0.058 | −2.81 | −5.10 | −0.52 | 5.77 | 0.016* | ||
| Time (T3) | −2.00 | −4.45 | 0.45 | 2.56 | 0.110 | −2.86 | −5.58 | −0.13 | 4.22 | 0.040* | ||
| Group x Time (T2) | −0.83 | −3.92 | 2.26 | 0.28 | 0.597 | 0.73 | −2.97 | 4.44 | 0.15 | 0.698 | 0.13 | |
| Group x Time (T3) | 0.52 | −3.07 | 4.11 | 0.08 | 0.778 | 3.55 | −0.86 | 7.96 | 2.49 | 0.114 | −0.15 | |
| Brooding | (intercept) | 9.17 | 8.06 | 10.27 | 265.18 | 0.000 | 9.52 | 8.29 | 10.75 | 230.06 | 0.000 | |
| Group | −0.17 | −1.76 | 1.43 | 0.04 | 0.838 | −0.83 | −2.82 | 1.16 | 0.67 | 0.413 | ||
| Time (T2) | −1.32 | −2.59 | −0.04 | 4.11 | 0.043* | −1.86 | −3.20 | −0.51 | 7.34 | 0.007** | ||
| Time (T3) | −1.21 | −2.67 | 0.25 | 2.63 | 0.105 | −1.71 | −3.31 | −0.12 | 4.46 | 0.035* | ||
| Group x Time (T2) | −0.53 | −2.37 | 1.31 | 0.32 | 0.574 | 0.24 | −1.93 | 2.41 | 0.05 | 0.827 | 0.22 | |
| Group x Time (T3) | 0.58 | −1.56 | 2.72 | 0.28 | 0.596 | 2.02 | −0.55 | 4.60 | 2.37 | 0.124 | −0.14 | |
| Reflection | (intercept) | 7.67 | 6.67 | 8.67 | 225.09 | 0.000 | 7.90 | 6.76 | 9.05 | 184.34 | 0.000 | |
| Group | 0.33 | −1.11 | 1.78 | 0.20 | 0.652 | −0.14 | −1.98 | 1.71 | 0.02 | 0.886 | ||
| Time (T2) | −0.74 | −1.95 | 0.48 | 1.42 | 0.233 | −0.95 | −2.27 | 0.37 | 2.00 | 0.157 | ||
| Time (T3) | −0.79 | −2.15 | 0.57 | 1.30 | 0.253 | −1.14 | −2.67 | 0.38 | 2.16 | 0.141 | ||
| Group x Time (T2) | −0.30 | −2.06 | 1.46 | 0.11 | 0.737 | 0.49 | −1.64 | 2.63 | 0.20 | 0.652 | −0.02 | |
| Group x Time (T3) | −0.05 | −2.04 | 1.94 | 0.00 | 0.962 | 1.53 | −0.94 | 3.99 | 1.48 | 0.224 | −0.12 | |
| ERQ | ||||||||||||
| Reappraisal | (intercept) | 18.88 | 15.86 | 21.89 | 150.46 | 0.000 | 19.43 | 16.03 | 22.83 | 125.37 | 0.000 | |
| Group | 3.76 | −0.60 | 8.12 | 2.86 | 0.091 | 3.26 | −2.24 | 8.76 | 1.35 | 0.245 | ||
| Time (T2) | 5.27 | 1.53 | 9.01 | 7.64 | 0.006** | 4.43 | 0.50 | 8.36 | 4.88 | 0.027* | ||
| Time (T3) | 7.83 | 3.70 | 11.96 | 13.83 | 0.000*** | 7.14 | 2.61 | 11.68 | 9.53 | 0.002** | ||
| Group x Time (T2) | −2.02 | −7.43 | 3.39 | 0.54 | 0.464 | −3.04 | −9.40 | 3.31 | 0.88 | 0.348 | −0.21 | |
| Group x Time (T3) | −6.59 | −12.63 | −0.54 | 4.55 | 0.033* | −6.30 | −13.63 | 1.04 | 2.83 | 0.093 | 0.47 | |
| Suppression | (intercept) | 11.96 | 9.66 | 14.26 | 103.61 | 0.000 | 12.19 | 9.76 | 14.62 | 96.72 | 0.000 | |
| Group | 2.54 | −0.43 | 5.52 | 2.80 | 0.094 | 2.96 | −0.97 | 6.89 | 2.19 | 0.139 | ||
| Time (T2) | 1.81 | −1.63 | 5.26 | 1.06 | 0.302 | 0.86 | −1.99 | 3.71 | 0.35 | 0.555 | ||
| Time (T3) | 1.13 | −1.53 | 3.78 | 0.69 | 0.406 | 0.43 | −2.84 | 3.69 | 0.07 | 0.797 | ||
| Group x Time (T2) | −4.21 | −9.23 | 0.83 | 2.68 | 0.102 | −3.24 | −7.85 | 1.37 | 1.90 | 0.168 | 0.24 | |
| Group x Time (T3) | −2.12 | −5.93 | 1.69 | 1.20 | 0.274 | −1.35 | −6.63 | 3.93 | 0.25 | 0.616 | −0.08 | |
Notes: Cohen’s d: 0.2 = Small effect size; 0.5 = Medium effect size; 0.8 = Large effect size (Cohen, 1988). *p < 0.05. **p < 0.01. ***p < 0.001. Bold values denote statistical significance at the p < 0.05 level.
Abbreviations: SRRS, Short rumination response scale; ERQ, Emotion regulation questionnaire; ES, Effect size.
Effect for Time
There was statistically significant effects of time in the total SRRS at the post-assessment (T2) (β =−2.81, 95% CI=−5.1–0.52, Wald’s χ2=5.77, p=0.016) and three-month post-assessment (T3) (β =−2.86, 95% CI=−5.58,-0.13, Wald’s χ2=4.22, p=0.40) in the adjusted GEE model (Table 4). There were also statistically significant effects of time in the Brooding sub-scale at T2 (β =−1.86, 95% CI = −3.20,-0.51, Wald’s χ2=7.34, p=0.007) and T3 (β =−1.71, 95% CI=−3.31,-0.12, Wald’s χ2=4.46, p=0.035) in the intervention group and in the adjusted model (Table 4). There was a significant effect of time on the reappraisal at T2 (β =4.43, 95% CI=0.50–8.36, Wald’s χ2=4.88, p=0.027) and T3 (β =7.14, 95% CI=2.61–11.68, Wald’s χ2=9.53, p=0.002) in the intervention group. There were no significant effects of time on the suppression and subscale reflection rumination.
Secondary Outcomes
Group X Time Interaction
The GEE model indicated that there was a statistically significant group X time interaction in FFMQ-Observe at T2 (β =−2.58, 95% CI = −4.99- −0.16, Wald’s χ2=4.37, p=0.037), and T3 (β = −2.81, 95% CI = −5.56- −0.06, Wald’s χ2=4.00, p=0.045), with a small to moderate effect size (d=0.19 at T2 and 0.64 at T3) (Table 5). GEE model indicated no significant group X time interaction in mood symptoms, mindfulness level, and psychotic symptoms.
Table 5.
Results of the Generalised Linear Model Regarding the Effects of MBPP on Secondary Outcomes (Mood Symptoms, Level of Mindfulness, Psychotic Symptoms)
| Dependent Variable | Crude Model | Adjusted Model | ES Cohen’s d | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | CI | χ2 | p-value | B | CI | χ2 | p-value | |||||
| Upper | Lower | Upper | Lower | |||||||||
| DASS | (intercept) | 16.96 | 12.84 | 21.08 | 65.06 | 0.000 | 17.86 | 13.26 | 22.45 | 58.03 | 0.000 | |
| Total score | Group | 0.63 | −5.33 | 6.59 | 0.04 | 0.835 | 0.07 | −7.36 | 7.50 | 0.00 | 0.986 | |
| Time (T2) | −2.85 | −7.37 | 1.67 | 1.53 | 0.216 | −4.29 | −9.15 | 0.57 | 2.99 | 0.084 | ||
| Time (T3) | −3.46 | −8.76 | 1.85 | 1.63 | 0.201 | −5.00 | −10.83 | 0.83 | 2.82 | 0.093 | ||
| Group x Time (T2) | −4.66 | −11.21 | 1.88 | 1.95 | 0.163 | −2.79 | −10.65 | 5.07 | 0.48 | 0.486 | 0.38 | |
| Group x Time (T3) | 0.22 | −7.56 | 7.99 | 0.00 | 0.957 | 4.62 | −4.82 | 14.05 | 0.92 | 0.338 | −0.09 | |
| Depression | (intercept) | 5.58 | 4.12 | 7.05 | 55.73 | 0.000 | 5.90 | 4.26 | 7.55 | 49.51 | 0.000 | |
| Group | −0.77 | −2.88 | 1.35 | 0.50 | 0.479 | −0.90 | −3.56 | 1.76 | 0.44 | 0.505 | ||
| Time (T2) | −1.69 | −3.41 | 0.02 | 3.75 | 0.053 | −2.19 | −4.07 | −0.31 | 5.21 | 0.022* | ||
| Time (T3) | −1.63 | −3.58 | 0.33 | 2.65 | 0.103 | −2.05 | −4.23 | 0.13 | 3.38 | 0.066 | ||
| Group x Time (T2) | −1.53 | −4.02 | 0.95 | 1.46 | 0.227 | −0.81 | −3.85 | 2.23 | 0.27 | 0.602 | 0.63 | |
| Group x Time (T3) | 0.27 | −2.60 | 3.14 | 0.03 | 0.853 | 1.66 | −1.87 | 5.19 | 0.85 | 0.356 | 0.14 | |
| Anxiety | (intercept) | 4.54 | 3.01 | 6.07 | 33.73 | 0.000 | 4.76 | 3.14 | 6.38 | 33.15 | 0.000 | |
| Group | 2.28 | 0.06 | 4.49 | 4.05 | 0.051 | 2.01 | −0.61 | 4.63 | 2.25 | 0.133 | ||
| Time (T2) | 0.10 | −1.60 | 1.79 | 0.01 | 0.912 | −0.38 | −2.09 | 1.33 | 0.19 | 0.662 | ||
| Time (T3) | −0.33 | −2.31 | 1.65 | 0.11 | 0.742 | −0.67 | −2.72 | 1.39 | 0.41 | 0.524 | ||
| Group x Time (T2) | −2.60 | −5.76 | 0.582 | 2.56 | 0.110 | −1.62 | −4.38 | 1.14 | 1.32 | 0.250 | 0.08 | |
| Group x Time (T3) | −1.32 | −4.22 | 1.59 | 0.79 | 0.374 | 0.05 | −3.27 | 3.37 | 0.00 | 0.976 | −0.27 | |
| Stress | (intercept) | 6.83 | 5.05 | 8.61 | 56.62 | 0.000 | 7.19 | 5.16 | 9.22 | 48.36 | 0.000 | |
| Group | −0.88 | −3.45 | 1.69 | 0.45 | 0.503 | −1.04 | −4.31 | 2.24 | 0.38 | 0.535 | ||
| Time (T2) | −1.25 | −3.17 | 0.66 | 1.65 | 0.199 | −1.71 | −3.79 | 0.37 | 2.61 | 0.106 | ||
| Time (T3) | −1.50 | −3.77 | 0.77 | 1.68 | 0.194 | −2.29 | −4.81 | 0.24 | 3.15 | 0.076 | ||
| Group x Time (T2) | −0.52 | −3.29 | 2.26 | 0.13 | 0.715 | −0.36 | −3.73 | 3.00 | 0.04 | 0.833 | 0.3 | |
| Group x Time (T3) | 1.27 | −2.06 | 4.59 | 0.56 | 0.455 | 2.90 | −1.18 | 6.98 | 1.94 | 0.164 | −0.09 | |
| FFMQ | ||||||||||||
| Total score | (intercept) | 56.20 | 53.12 | 59.28 | 1278.75 | 0.000 | 56.15 | 52.67 | 59.64 | 995.53 | 0.000 | |
| Group | 3.12 | −1.33 | 7.58 | 1.89 | 0.169 | 2.08 | −3.56 | 7.72 | 0.52 | 0.469 | ||
| Time (T2) | 2.36 | −1.37 | 6.10 | 1.54 | 0.215 | 2.71 | −1.60 | 7.02 | 1.52 | 0.218 | ||
| Time (T3) | 4.59 | 0.39 | 8.79 | 4.60 | 0.032* | 5.23 | 0.43 | 10.02 | 4.57 | 0.033* | ||
| Group x Time (T2) | −2.94 | −8.34 | 2.46 | 1.14 | 0.286 | −2.86 | −9.83 | 4.10 | 0.65 | 0.421 | −0.02 | |
| Group x Time (T3) | −5.06 | −11.13 | 1.02 | 2.66 | 0.103 | −4.02 | −11.77 | 3.73 | 1.04 | 0.309 | 0.29 | |
| Observing | (intercept) | 9.21 | 8.03 | 10.39 | 233.69 | 0.000 | 9.10 | 7.83 | 10.36 | 199.36 | 0.000 | |
| Group | 1.20 | −0.51 | 2.91 | 1.90 | 0.168 | 0.75 | −1.29 | 2.79 | 0.52 | 0.471 | ||
| Time (T2) | 0.92 | −0.49 | 2.32 | 1.64 | 0.201 | 1.19 | −0.30 | 2.68 | 2.44 | 0.118 | ||
| Time (T3) | 1.79 | 0.20 | 3.39 | 4.84 | 0.028* | 1.81 | 0.11 | 3.51 | 4.34 | 0.037* | ||
| Group x Time (T2) | −1.78 | −3.81 | 0.25 | 2.96 | 0.085 | −2.58 | −4.99 | −0.16 | 4.37 | 0.037* | 0.19 | |
| Group x Time (T3) | −3.00 | −5.30 | −0.69 | 6.48 | 0.011* | −2.81 | −5.56 | −0.06 | 4.00 | 0.045* | 0.64 | |
| Describing | (intercept) | 9.42 | 8.00 | 10.84 | 168.75 | 0.000 | 9.60 | 8.01 | 11.18 | 140.80 | 0.000 | |
| Group | 1.49 | −0.56 | 3.55 | 2.03 | 0.155 | 0.10 | −2.47 | 2.66 | 0.01 | 0.941 | ||
| Time (T2) | 0.25 | −1.40 | 1.91 | 0.09 | 0.763 | −0.07 | −1.83 | 1.69 | 0.01 | 0.937 | ||
| Time (T3) | 1.38 | −0.53 | 3.28 | 2.01 | 0.156 | 1.26 | −0.81 | 3.33 | 1.43 | 0.232 | ||
| Group x Time (T2) | −1.18 | −3.57 | 1.21 | 0.94 | 0.332 | −0.28 | −3.13 | 2.57 | 0.04 | 0.850 | −0.09 | |
| Group x Time (T3) | −1.15 | −3.90 | 1.60 | 0.67 | 0.411 | 0.33 | −3.02 | 3.68 | 0.04 | 0.846 | −0.1 | |
| Awareness | (intercept) | 13.54 | 11.86 | 15.22 | 248.61 | 0.000 | 13.38 | 11.53 | 15.23 | 201.10 | 0.000 | |
| Group | 0.64 | −1.79 | 3.07 | 0.27 | 0.606 | 1.08 | −1.91 | 4.07 | 0.50 | 0.479 | ||
| Time (T2) | −0.81 | −2.69 | 1.07 | 0.71 | 0.401 | −0.43 | −2.41 | 1.55 | 0.18 | 0.672 | ||
| Time (T3) | −0.42 | −2.62 | 1.79 | 0.14 | 0.711 | 0.19 | −2.18 | 2.56 | 0.02 | 0.875 | ||
| Group x Time (T2) | 0.09 | −2.63 | 2.81 | 0.00 | 0.948 | −0.53 | −3.73 | 2.68 | 0.10 | 0.748 | −0.18 | |
| Group x Time (T3) | 0.09 | −3.10 | 3.28 | 0.00 | 0.958 | −0.50 | −4.32 | 3.33 | 0.07 | 0.799 | −0.21 | |
| Non judging | (intercept) | 13.79 | 12.50 | 15.08 | 440.31 | 0.000 | 13.62 | 12.18 | 15.05 | 346.45 | 0.000 | |
| Group | −0.66 | −2.52 | 1.21 | 0.48 | 0.491 | 0.07 | −2.25 | 2.39 | 0.00 | 0.951 | ||
| Time (T2) | 0.37 | −1.11 | 1.84 | 0.24 | 0.626 | 0.81 | −0.88 | 2.49 | 0.89 | 0.346 | ||
| Time (T3) | 0.25 | −1.46 | 1.96 | 0.08 | 0.774 | 0.67 | −1.26 | 2.60 | 0.46 | 0.498 | ||
| Group x Time (T2) | 0.85 | −1.28 | 2.98 | 0.61 | 0.434 | 0.58 | −2.15 | 3.30 | 0.17 | 0.679 | −0.06 | |
| Group x Time (T3) | 0.51 | −1.96 | 2.99 | 0.17 | 0.683 | 0.10 | −3.02 | 3.22 | 0.00 | 0.949 | 0.05 | |
| Non reacting | (intercept) | 10.24 | 9.08 | 11.40 | 300.44 | 0.00 | 10.46 | 9.14 | 11.78 | 241.38 | 0.00 | |
| Group | 0.45 | −1.23 | 2.12 | 0.27 | 0.601 | 0.08 | −2.05 | 2.22 | 0.01 | 0.941 | ||
| Time (T2) | 1.63 | −0.10 | 3.37 | 3.39 | 0.052 | 1.21 | −0.74 | 3.16 | 1.47 | 0.225 | ||
| Time (T3) | 1.59 | −0.03 | 3.22 | 3.70 | 0.049 | 1.30 | −0.56 | 3.16 | 1.87 | 0.171 | ||
| Group x Time (T2) | −0.92 | −3.43 | 1.59 | 0.51 | 0.474 | −0.06 | −3.22 | 3.09 | 0.00 | 0.970 | 0.18 | |
| Group x Time (T3) | −1.51 | −3.86 | 0.84 | 1.58 | 0.209 | −1.15 | −4.16 | 1.86 | 0.56 | 0.453 | 0.39 | |
| PSYRAT | ||||||||||||
| Total score | (intercept) | 8.33 | 3.44 | 13.23 | 11.13 | 0.001 | 8.95 | 3.75 | 14.15 | 11.39 | 0.001 | |
| Group | 3.17 | −3.91 | 10.25 | 0.77 | 0.381 | 3.59 | −4.82 | 11.99 | 0.70 | 0.403 | ||
| Time (T2) | −2.96 | −8.03 | 2.11 | 1.31 | 0.253 | −4.57 | −9.53 | 0.38 | 3.27 | 0.071 | ||
| Time (T3) | −5.13 | −11.26 | 1.01 | 2.68 | 0.102 | −6.86 | −13.02 | −0.70 | 4.76 | 0.029* | ||
| Group x Time (T2) | −1.09 | −8.42 | 6.25 | 0.08 | 0.771 | 4.65 | −3.37 | 12.66 | 1.29 | 0.256 | −0.19 | |
| Group x Time (T3) | 1.35 | −7.52 | 10.22 | 0.09 | 0.765 | 4.70 | −5.26 | 14.67 | 0.86 | 0.355 | −0.44 | |
| Total H score | (intercept) | 5.96 | 2.05 | 9.86 | 8.95 | 0.003 | 6.81 | 2.59 | 11.03 | 10.00 | 0.002 | |
| Group | 3.04 | −2.60 | 8.69 | 1.12 | 0.291 | 2.96 | −3.87 | 9.79 | 0.72 | 0.395 | ||
| Time (T2) | −1.54 | −5.26 | 2.18 | 0.66 | 0.417 | −3.10 | −6.72 | 0.53 | 2.80 | 0.094 | ||
| Time (T3) | −3.96 | −8.58 | 0.67 | 2.81 | 0.094 | −5.38 | −10.01 | −0.75 | 5.19 | 0.023* | ||
| Group x Time (T2) | −2.32 | −7.70 | 3.06 | 0.72 | 0.398 | 2.02 | −3.84 | 7.88 | 0.46 | 0.500 | −0.08 | |
| Group x Time (T3) | 0.25 | −6.48 | 6.98 | 0.01 | 0.941 | 2.92 | −4.57 | 10.41 | 0.58 | 0.445 | −0.42 | |
| Emotion H | (intercept) | 2.04 | 0.55 | 3.54 | 7.15 | 0.007 | 2.33 | 0.71 | 3.96 | 7.91 | 0.005 | |
| Group | 1.00 | −1.16 | 3.17 | 0.83 | 0.363 | 0.90 | −1.73 | 3.53 | 0.45 | 0.504 | ||
| Time (T2) | −0.50 | −2.12 | 1.12 | 0.37 | 0.546 | −1.14 | −2.75 | 0.46 | 1.95 | 0.163 | ||
| Time (T3) | −1.63 | −3.55 | 0.30 | 2.73 | 0.098 | −1.95 | −3.93 | 0.02 | 3.76 | 0.053 | ||
| Group x Time (T2) | −1.00 | −3.34 | 1.34 | 0.70 | 0.403 | 0.53 | −2.07 | 3.12 | 0.16 | 0.691 | 0 | |
| Group x Time (T3) | 0.74 | −2.06 | 3.54 | 0.27 | 0.605 | 1.65 | −1.55 | 4.84 | 1.02 | 0.313 | −0.56 | |
| Physical H | (intercept) | 1.04 | 0.28 | 1.81 | 7.12 | 0.008 | 1.19 | 0.36 | 2.02 | 7.90 | 0.005 | |
| Group | 0.69 | −0.42 | 1.79 | 1.48 | 0.225 | 0.81 | −0.53 | 2.15 | 1.40 | 0.237 | ||
| Time (T2) | −0.25 | −0.91 | 0.41 | 0.55 | 0.458 | −0.48 | −1.12 | 0.16 | 2.13 | 0.144 | ||
| Time (T3) | −0.50 | −1.34 | 0.34 | 1.35 | 0.245 | −0.86 | −1.69 | −0.02 | 4.06 | 0.044* | ||
| Group x Time (T2) | −0.43 | −1.39 | 0.52 | 0.79 | 0.375 | 0.25 | −0.79 | 1.28 | 0.22 | 0.642 | −0.15 | |
| Group x Time (T3) | −0.21 | −1.44 | 1.01 | 0.11 | 0.736 | 0.24 | −1.11 | 1.59 | 0.12 | 0.725 | −0.28 | |
| Control H | (intercept) | 1.50 | 0.53 | 2.47 | 9.23 | 0.002 | 1.71 | 0.66 | 2.76 | 10.25 | 0.001 | |
| Group | 0.95 | −0.44 | 2.35 | 1.79 | 0.181 | 0.75 | −0.95 | 2.44 | 0.74 | 0.388 | ||
| Time (T2) | −0.46 | −1.36 | 0.44 | 0.99 | 0.319 | −0.76 | −1.60 | 0.07 | 3.19 | 0.074 | ||
| Time (T3) | −1.00 | −2.13 | 0.13 | 3.02 | 0.082 | −1.33 | −2.42 | −0.25 | 5.81 | 0.016* | ||
| Group x Time (T2) | −0.72 | −2.03 | 0.58 | 1.18 | 0.277 | 0.45 | −0.90 | 1.81 | 0.43 | 0.510 | −0.1 | |
| Group x Time (T3) | −0.30 | −1.94 | 1.34 | 0.13 | 0.722 | 0.56 | −1.19 | 2.32 | 0.40 | 0.528 | −0.37 | |
| Cognitive H | (intercept) | 1.38 | 0.49 | 2.26 | 9.28 | 0.002 | 1.57 | 0.61 | 2.53 | 10.33 | 0.001 | |
| Group | 0.40 | −0.88 | 1.68 | 0.37 | 0.542 | 0.51 | −1.04 | 2.05 | 0.41 | 0.523 | ||
| Time (T2) | −0.33 | −1.17 | 0.50 | 0.61 | 0.433 | −0.71 | −1.57 | 0.15 | 2.65 | 0.103 | ||
| Time (T3) | −0.83 | −1.87 | 0.21 | 2.47 | 0.116 | −1.24 | −2.32 | −0.15 | 4.99 | 0.026* | ||
| Group x Time (T2) | −0.17 | −1.37 | 1.04 | 0.07 | 0.786 | 0.79 | −0.60 | 2.18 | 1.24 | 0.265 | −0.1 | |
| Group x Time (T3) | 0.03 | −1.49 | 1.54 | 0.00 | 0.972 | 0.47 | −1.29 | 2.23 | 0.27 | 0.601 | −0.27 | |
| Total D score | (intercept) | 2.38 | 0.48 | 4.27 | 6.03 | 0.014 | 2.14 | 0.06 | 4.22 | 4.08 | 0.043 | |
| Group | 0.13 | −2.62 | 2.87 | 0.01 | 0.929 | 0.63 | −2.74 | 3.99 | 0.13 | 0.715 | ||
| Time (T2) | −1.42 | −3.76 | 0.93 | 1.41 | 0.236 | −1.48 | −4.10 | 1.15 | 1.21 | 0.271 | ||
| Time (T3) | −1.17 | −3.77 | 1.44 | 0.77 | 0.380 | −1.48 | −4.36 | 1.40 | 1.01 | 0.315 | ||
| Group x Time (T2) | 1.23 | −2.15 | 4.62 | 0.51 | 0.475 | 2.63 | −1.62 | 6.88 | 1.47 | 0.225 | −0.33 | |
| Group x Time (T3) | 1.31 | −2.48 | 5.10 | 0.46 | 0.499 | 1.78 | −2.87 | 6.44 | 0.56 | 0.453 | −0.31 | |
| Cognitive D | (intercept) | 1.38 | 0.35 | 2.40 | 6.85 | 0.009 | 1.24 | 0.13 | 2.35 | 4.76 | 0.029 | |
| Group | −0.06 | −1.55 | 1.43 | 0.01 | 0.940 | 0.15 | −1.65 | 1.95 | 0.03 | 0.873 | ||
| Time (T2) | −0.79 | −2.06 | 0.48 | 1.49 | 0.222 | −0.86 | −2.29 | 0.58 | 1.37 | 0.241 | ||
| Time (T3) | −0.67 | −2.08 | 0.75 | 0.85 | 0.356 | −0.86 | −2.41 | 0.69 | 1.17 | 0.279 | ||
| Group x Time (T2) | 0.56 | −1.27 | 2.40 | 0.36 | 0.547 | 1.32 | −1.00 | 3.64 | 1.24 | 0.265 | −0.23 | |
| Group x Time (T3) | 0.72 | −1.34 | 2.78 | 0.47 | 0.495 | 1.09 | −1.42 | 3.60 | 0.72 | 0.395 | −0.26 | |
| Emotion D | (intercept) | 1.00 | 0.12 | 1.88 | 4.95 | 0.026 | 0.90 | −0.07 | 1.88 | 3.29 | 0.070 | |
| Group | 0.18 | −1.09 | 1.46 | 0.08 | 0.780 | 0.48 | −1.10 | 2.06 | 0.35 | 0.552 | ||
| Time (T2) | −0.63 | −1.71 | 0.46 | 1.28 | 0.258 | −0.62 | −1.82 | 0.58 | 1.02 | 0.313 | ||
| Time (T3) | −0.50 | −1.71 | 0.71 | 0.66 | 0.417 | −0.62 | −1.96 | 0.72 | 0.82 | 0.366 | ||
| Group x Time (T2) | 0.67 | −0.89 | 2.24 | 0.70 | 0.401 | 1.31 | −0.63 | 3.26 | 1.75 | 0.186 | −0.43 | |
| Group x Time (T3) | 0.59 | −1.17 | 2.35 | 0.43 | 0.511 | 0.70 | −1.47 | 2.86 | 0.40 | 0.529 | −0.36 | |
Notes: Cohen’s d = 0.2 = Small effect size; 0.5 = Medium effect size; 0.8 = Large effect size (Cohen, 1988). *p < 0.05. Bold values denote statistical significance at the p < 0.05 level.
Abbreviations: DASS, Depression Anxiety Stress Scales; FFMQ, Five Facet Mindfulness Questionnaire; PSYRAT, Psychotic Symptoms Rating Scale; Total H score, Total hallucination score; Emotion H, hallucination; Physical H, physical hallucination; Control H, control hallucination; Cognitive H, cognitive hallucination; Total D score, total delusion score; Cognitive D, cognitive delusion; Emotion D, emotion delusion.
Effect for Time
There were statistically significant effects of time on depression subscale, overall mindfulness level, mindfulness subscales, overall psychotic symptoms, and hallucination.
There was a statistically significant reduction in the depression subscale at T2 in the intervention group (β =−2.19, 95% CI=−4.07- −0.31, Wald’s χ2=5.21, p=0.022) and in the adjusted model. Surprisingly, there was also a statistically significant reduction in depression subscale at T2 in the control group (MD=−3.00, 95% CI= 0.61–5.39, P=0.014). This indicates that there was a significant within-group improvement in depressive symptoms at T2 both in the intervention and control groups. There were no significant effects of time on the total DASS and other DASS subscale (anxiety and stress).
In the intervention group, there was a statistically significant effect of time on total FFMQ at T3 (β =5.23, 95% CI = 0.43 −10.02, Wald’s χ2 = 4.57, p=0.033), which was consistent in both adjust and crude model. Besides, There was statistically significant effect of time on mindfulness subscale – observed at T3 (β =1.81, 95% CI = 0.11–3.51, Wald’s χ2 = 4.34, p=0.037) in the adjust model, and a marginal significant effect of time on mindfulness subscale – non-reacting at T3 (β =1.59, 95% CI = −0.03–3.22, Wald’s χ2 = 3.7, p=0.049) in the crude model. There were no statistically significant effects of time on other FFMQ subscale (describing, awareness and non-judging).
Besides, there were statistical significant effects of time on the overall psychotic symptoms (β = −6.86, 95% CI = −13.02 - −0.70, Wald’s χ2 = 4.76, p=0.029), overall hallucinations (β = −5.38, 95% CI = −10.01 - −0.75, Wald’s χ2 = 5.19, p=0.023), physical characteristics (β = −0.86, 95% CI= −1.69- −0.02, Wald’s χ2=4.06, p=0.044), controllability (β = −1.33, 95% CI = −2.42–0.25, Wald’s χ2= 5.81, p=0.016) and cognitive interpretation of hallucinations (β = −1.24, 95% CI = −2.32 - −0.15, Wald’s χ2= 4.99, p=0.026) at T3 in the intervention group (Table 5). There were no significant effects of time on the emotion characteristics of hallucination, and delusion scale.
Pairwise Comparison
The pairwise comparison indicated that the participants in the MBPP group underwent statistically significant improvement in FFMQ-observe at T3 (MD=−1.80, 95% CI=−3.50–0.09, p=0.039), compared with the control group.
The pairwise comparison also indicated that there was a marginal between-group difference in the overall psychotic symptoms at T3 (MD=8.3, 95% CI =0.14 −16.70, p=0.51), with a moderate effect size (d=−0.44 at T3), indicating a marginal difference in the severity of overall psychotic symptoms at T3 in the MBPP group compared to control group. There were no significant differences in the mood symptoms, overall mindfulness level, and psychotic symptoms between the MBPP group and the control group.
Discussion
The current study demonstrates that MBPP is feasible for improving emotion regulation of adult schizophrenic patients in the community setting. The study was feasible, given the low dropout rate (4.3%) and good compliance in the intervention (84.6% attendance ≥6 sessions). Meanwhile, the main difficulty appeared in the recruitment phase. Clients with schizophrenia are difficult to reach in the community because of the social stigma, time constraints and lack of motivation.74–76 Hence the potential candidates for the study were, therefore, less than expected.
The finding indicates that MBPP produced significantly greater improvements in some processes of emotion regulation, such as cognitive reappraisal and rumination, for up to three-month of follow-up. The results also suggested that MBPP might improve mindfulness ability and reduce the symptoms of depression, and the perceived disturbance of hallucinations. Furthermore, it shows that mindfulness psychoeducation might improve a certain degree of emotion regulation ability in schizophrenia. These results are consistent with a non-controlled study that demonstrated that combined compassion, acceptance and mindfulness (CAM) could significantly improve emotional self-regulation, which includes rumination, self-blaming and mood symptoms in people with psychosis at 3 months follow-up.77 The results also echo the findings of Chien et al’s studies,41,49,53 which demonstrated that mindfulness-based intervention promotes significant psychotic reduction. It was however noted that the results might not be able to rule out the improvement in emotion regulation likely contributing by their improvements in symptoms. Further longitudinal studies are needed to confirm the benefits of the MBPP in modulating emotion regulation in schizophrenia.
Contradictory to our hypothesis, MBPP did not effectively improve suppression in the participants. The study suggested that suppression appeared to be the ineffective emotion regulation strategy as individuals had a rebound in target thoughts, which heightened their emotionality after a designated suppression period.78 Mindfulness, which cultivates the acceptance of unwanted experience and thoughts, is suggested to be antithetical to expression suppression.79 Nevertheless, this study result was contradictory to previous studies which demonstrated that mindfulness training reduced expressive suppression in clinical and non-clinical populations.80–82 Meanwhile, recent studies have suggested that emotion regulation practices and the associated psychological impacts are culturally specific.81 Contradictory to the Western context which values emotional expression, the Asian culture considers the expression of the inner self as ego-focused, and a disturbance of social harmony.83 Suppression may function as adaptive self-restraint and interpersonal harmony in the Asian contexts.83–86 Our study revealed that the suppression score was in the unexpected direction, it slightly increased after the MBPP and 3 months follow-up. The use of suppression in emotion regulation may serve the purpose of self-restraint and social attachment in traditional Chinese culture. Meanwhile, Western studies have consistently found that greater use of suppression in patients with schizophrenia is associated with depression, anxiety, and affective blunting, which has been associated with poorer clinical outcomes in psychosis.27,34,37,87 More studies are needed to examine the role of suppression in Chinese patients with schizophrenia, and the effectiveness of mindfulness in modulating the use of suppression and associated emotional response in this population.
In our study, two participants (7.7% of the MBPP participants) reported experiencing unwanted events during the mindfulness practice, which is substantially lower than the occurrence of unwanted events (25.4%) reported by general mindfulness practitioners.88 The common unwanted effects that mindfulness practitioners have experienced include transient anxiety and fear (13.8%), emotional lability (2.3%), and depressive symptoms (2.3%).88 The incidence in this study was lower than that of general practitioners reported by Cebolla et al (2017); and the unwanted effects were mild without the need for medical assistance. Nevertheless, the result informed the consideration of further study for the possible unwanted effects of mindfulness in this population.
This trial has several limitations. First, convenience sampling was adopted for subject recruitment leading to self-selection bias. Secondly, patients were recruited from four mental health centres in two geographical regions (Kowloon and New Territories), which are associated with a high poverty rate, low household income and low social class compared to the overall demographic structure in Hong Kong.89 Thirdly, the participants in this study were dominated by females, aged over 45, married, and with a long duration of illness. The sample bias might limit the generalisation of the findings. Fourth, both participants and clinicians in the ICCMW and LSCH were not blinded, which might produce an expectation, response bias and Hawthorne effect. Fifthly, this study adopts self-reported measurements to measure the outcomes which may induce self-reported/response bias and learning effects. The statistically significant improvement in the reported emotion regulation may not be linked to the clinical improvement and the change of emotional valence in response to the illness experience. Psychophysiological measurements such as neuroimaging or neurobiological responses should be employed in future studies to develop an understanding of the psychophysiological impact of MBPP on the emotion regulation process, and the emotional response for schizophrenia.
Conclusion
This study achieved positive results that strengthened the body of knowledge on the impacts of mindfulness psychoeducation on emotion regulation. The findings suggest that MBPP can be both feasible and acceptable by schizophrenic patients in community settings and improve emotion regulation, in terms of cognitive reappraisal, rumination, reduced depressive symptoms, and hallucination severity. These encouraging results urge further multi-centre randomised controlled trials to examine the treatment effects of using MBPP as an emotion regulation intervention in more diverse patient groups of schizophrenia. It is also important to investigate the comparative effectiveness of other psychosocial interventions and their longer-term effects on schizophrenia.
Acknowledgments
Special thanks to the patients who participated in the study, and the cooperative organisations, the Integrated Community Centre for Mental Wellness (ICCMW) of New Life Association of Hong Kong, and Long Stay Care Home which prefer to remain anonymous.
Data Sharing Statement
The research team could not share the data because both the research team and community centres share held the access right of the data. The community centres had concerns about the confidentiality of identity and data of this sensitive patient population.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Chong HY, Teoh SL, Wu DB, Kotirum S, Chiou CF, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:357–373. doi: 10.2147/NDT.S96649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Schizophrenia. World Health Organization; 2017. Accessed November10, 2019. [Google Scholar]
- 3.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–1131. doi: 10.1001/archpsyc.64.10.1123 [DOI] [PubMed] [Google Scholar]
- 4.Johnson DA. The significance of depression in the prediction of relapse in chronic schizophrenia. Br J Psychiatry. 1988;152:320–323. doi: 10.1192/bjp.152.3.320 [DOI] [PubMed] [Google Scholar]
- 5.Cohen LJ, Test MA, Brown RL. Suicide and schizophrenia: data from a prospective community treatment study. Am J Psychiatry. 1990;147(5):602–607. doi: 10.1176/ajp.147.5.602 [DOI] [PubMed] [Google Scholar]
- 6.Kahn RS, Sommer IE, Murray RM, et al. Schizophrenia. Nat Rev Dis Primers. 2015;1:15067. doi: 10.1038/nrdp.2015.67 [DOI] [PubMed] [Google Scholar]
- 7.Chien WT, Yip ALK. Current approaches to treatments for schizophrenia spectrum disorders, part I: an overview and medical treatments. Neuropsychiatr Dis Treat. 2013;9:1311–1332. doi: 10.2147/NDT [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Psychiatric Association. Practice Guidelines for Treatment of Schizophrenia. 2 ed. Washington, DC: American Psychiatric Association; 2010. [Google Scholar]
- 9.Parikh SV, Quilty LC, Ravitz P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 2. Psychological treatments. Can J Psychiatry. 2016;61(9):524–539. doi: 10.1177/0706743716659418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Collaborating Centre for Mental Health (UK). Psychosis and schizophrenia in adults: treatment and management: updated edition 2014. National Institute for Health and Care Excellence (UK). NICE Clinical Guidelines, No. 178.) 2, Psychosis and Schizophrenia in Adults; 2014. Available from: https://www.ncbi.nlm.nih.gov/books/NBK333029/. Accessed November7, 2018.. [PubMed]
- 11.Álvarez-Jiménez M, Parker AG, Hetrick SE, McGorry PD, Gleeson JF. Preventing the second episode: a systematic review and meta-analysis of psychosocial and pharmacological trials in first-episode psychosis. Schizophr Bull. 2009;37(3):619–630. doi: 10.1093/schbul/sbp129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones C, Hacker D, Meaden A, Cormac I, Irving CB. WITHDRAWN: cognitive behaviour therapy versus other psychosocial treatments for schizophrenia. Cochrane Database Syst Rev. 2011;4:Cd000524. [DOI] [PubMed] [Google Scholar]
- 13.Pilling S, Bebbington P, Kuipers E, et al. Psychological treatments in schizophrenia: I. Meta-analysis of family intervention and cognitive behaviour therapy. Psychol Med. 2002;32(5):763–782. doi: 10.1017/S0033291702005895 [DOI] [PubMed] [Google Scholar]
- 14.Tarrier N, Kinney C, McCarthy E, Humphreys L, Wittkowski A, Morris J. Two-year follow-up of cognitive–behavioral therapy and supportive counseling in the treatment of persistent symptoms in chronic schizophrenia. J Consult Clin Psychol. 2000;68(5):917–922. doi: 10.1037/0022-006X.68.5.917 [DOI] [PubMed] [Google Scholar]
- 15.Almerie MQ, Okba Al Marhi M, Jawoosh M, et al. Social skills programmes for schizophrenia. Cochrane Database Syst Rev. 2015;6:CD009006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chien WT, Leung SF, Yeung FK, Wong WK. Current approaches to treatments for schizophrenia spectrum disorders, part II: psychosocial interventions and patient-focused perspectives in psychiatric care. Neuropsychiatr Dis Treat. 2013;9:1463–1481. doi: 10.2147/NDT [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pfammatter M, Junghan UM, Brenner HD. Efficacy of psychological therapy in schizophrenia: conclusions from meta-analyses. Schizophr Bull. 2006;32(Suppl 1):S64–S80. doi: 10.1093/schbul/sbl030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Livingstone K, Harper S, Gillanders D. An exploration of emotion regulation in psychosis. Clin Psychol Psychother. 2009;16(5):418–430. doi: 10.1002/cpp.v16:5 [DOI] [PubMed] [Google Scholar]
- 19.Kring AM, Sloan DS. Emotion Regulation and Psychopathology. New York: Guilford Press; 2010. [Google Scholar]
- 20.Gross JJ. Antecedent- and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J Pers Soc Psychol. 1998;74(1):224–237. doi: 10.1037/0022-3514.74.1.224 [DOI] [PubMed] [Google Scholar]
- 21.Campbell-Sills L, Barlow DH. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders In: Gross JJ, editor. Handbook of Emotion Regulation. New York: Guilford Press; 2007:542–559. [Google Scholar]
- 22.Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol. 1998;2(3):271–299. doi: 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- 23.van ‘T Wout M, Aleman A, Bermond B, Kahn RS. No words for feelings: alexithymia in schizophrenia patients and first-degree relatives. Compr Psychiatry. 2007;48(1):27–33. doi: 10.1016/j.comppsych.2006.07.003 [DOI] [PubMed] [Google Scholar]
- 24.Visser KF, Esfahlani FZ, Sayama H, Strauss GP. An ecological momentary assessment evaluation of emotion regulation abnormalities in schizophrenia. Psychol Med. 2018;48(14):2337–2345. doi: 10.1017/S0033291717003865 [DOI] [PubMed] [Google Scholar]
- 25.Chadwick P, Taylor KN, Abba N. Mindfulness groups for people with psychosis. Behav Cogn Psychother. 2005;33(3):351–359. doi: 10.1017/S1352465805002158 [DOI] [Google Scholar]
- 26.O’Driscoll C, Laing J, Mason O. Cognitive emotion regulation strategies, alexithymia and dissociation in schizophrenia, a review and meta-analysis. Clin Psychol Rev. 2014;34(6):482–495. doi: 10.1016/j.cpr.2014.07.002 [DOI] [PubMed] [Google Scholar]
- 27.Kimhy D, Vakhrusheva J, Jobson-Ahmed L, Tarrier N, Malaspina D, Gross JJ. Emotion awareness and regulation in individuals with schizophrenia: implications for social functioning. Psychiatry Res. 2012;200(2–3):193–201. doi: 10.1016/j.psychres.2012.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halari R, Premkumar P, Farquharson L, Fannon D, Kuipers E, Kumari V. Rumination and negative symptoms in schizophrenia. J Nerv Ment Dis. 2009;197(9):703–706. doi: 10.1097/NMD.0b013e3181b3af20 [DOI] [PubMed] [Google Scholar]
- 29.Badcock JC, Paulik G, Maybery MT. The role of emotion regulation in auditory hallucinations. Psychiatry Res. 2011;185(3):303–308. doi: 10.1016/j.psychres.2010.07.011 [DOI] [PubMed] [Google Scholar]
- 30.Ricarte JJ, Hernandez JV, Latorre JM, Danion JM, Berna F. Rumination and autobiographical memory impairment in patients with schizophrenia. Schizophr Res. 2014;160(1–3):163–168. doi: 10.1016/j.schres.2014.10.027 [DOI] [PubMed] [Google Scholar]
- 31.Chapman HC, Visser KF, Mittal VA, Gibb BE, Coles ME, Strauss GP. Emotion regulation across the psychosis continuum. Dev Psychopathol. 2019;32(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van der Meer L, Wout M, Aleman A. Emotion regulation strategies in patients with schizophrenia. Psychiatry Res. 2009;170(2):108–113. doi: 10.1016/j.psychres.2009.07.010 [DOI] [PubMed] [Google Scholar]
- 33.Gur RE, Kohler CG, Ragland JD, et al. Flat affect in schizophrenia: relation to emotion processing and neurocognitive measures. Schizophr Bull. 2006;32(2):279–287. doi: 10.1093/schbul/sbj041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Henry J, Rendell P, Green M, McDonald S, O’Donnell M. Emotion regulation in schizophrenia: affective, social, and clinical correlates of suppression and reappraisal. J Abnorm Psychol. 2008;117(2):473–478. doi: 10.1037/0021-843X.117.2.473 [DOI] [PubMed] [Google Scholar]
- 35.Horan WP, Hajcak G, Wynn JK, Green MF. Impaired emotion regulation in schizophrenia: evidence from event-related potentials. Psychol Med. 2013;43(11):2377–2391. doi: 10.1017/S0033291713000019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khoury B, Lecomte T. Emotion regulation and schizophrenia. Int J Cogn Ther. 2012;5(1):67–76. doi: 10.1521/ijct.2012.5.1.67 [DOI] [Google Scholar]
- 37.Perry Y, Henry JD, Grisham JR. The habitual use of emotion regulation strategies in schizophrenia. Br J Soc Clin Psychol. 2011;50(2):217–222. doi: 10.1111/bjc.2011.50.issue-2 [DOI] [PubMed] [Google Scholar]
- 38.Berking M, Wupperman P, Reichardt A, Pejic T, Dippel A, Znoj H. Emotion-regulation skills as a treatment target in psychotherapy. Behav Res Ther. 2008;46(11):1230–1237. doi: 10.1016/j.brat.2008.08.005 [DOI] [PubMed] [Google Scholar]
- 39.Gaudiano BA, Herbert JD. Acute treatment of inpatients with psychotic symptoms using acceptance and commitment therapy: pilot results. Behav Res Ther. 2006;44(3):415–437. doi: 10.1016/j.brat.2005.02.007 [DOI] [PubMed] [Google Scholar]
- 40.Wakefield S, Roebuck S, Boyden P. The evidence base of Acceptance and Commitment Therapy (ACT) in psychosis: a systematic review. J Contextual Behav Sci. 2018;10:1–13. doi: 10.1016/j.jcbs.2018.07.001 [DOI] [Google Scholar]
- 41.Chien WT, Lee IY. The mindfulness-based psychoeducation program for Chinese patients with schizophrenia. Psychiatr Serv. 2013;64(4):376–379. doi: 10.1176/appi.ps.002092012 [DOI] [PubMed] [Google Scholar]
- 42.Kuyken W, Byford S, Taylor RS, et al. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J Consult Clin Psychol. 2008;76(6):966–978. doi: 10.1037/a0013786 [DOI] [PubMed] [Google Scholar]
- 43.Strauss C, Cavanagh K, Oliver A, Pettman D. Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: a meta-analysis of randomised controlled trials. PLoS One. 2014;9(4):e96110. doi: 10.1371/journal.pone.0096110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grow JC, Collins SE, Harrop EN, Marlatt GA. Enactment of home practice following mindfulness-based relapse prevention and its association with substance-use outcomes. Addict Behav. 2015;40:16–20. doi: 10.1016/j.addbeh.2014.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perich T, Manicavasagar V, Mitchell PB, Ball JR. The association between meditation practice and treatment outcome in mindfulness-based cognitive therapy for bipolar disorder. Behav Res Ther. 2013;51(7):338–343. doi: 10.1016/j.brat.2013.03.006 [DOI] [PubMed] [Google Scholar]
- 46.Ledesma D, Kumano H. Mindfulness-based stress reduction and cancer: a meta-analysis. Psychooncology. 2009;18(6):571–579. doi: 10.1002/pon.v18:6 [DOI] [PubMed] [Google Scholar]
- 47.Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med. 2017;51(2):199–213. doi: 10.1007/s12160-016-9844-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lam AHY, Chien WT. The effectiveness of mindfulness-based intervention for people with schizophrenia: a systematic review. Neuropsychiatry (London). 2016;6:208–222. [Google Scholar]
- 49.Chien WT, Bressington D, Yip A, Karatzias T. An international multi-site, randomized controlled trial of a mindfulness-based psychoeducation group programme for people with schizophrenia. Psychol Med. 2017;47(12):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bauml J, Pitschel-Walz G. Psycho Education for Schizophrenia Disorders. Stuttgart: Schattauer; 2003. [Google Scholar]
- 51.Cetin N, Aylaz R. The effect of mindfulness-based psychoeducation on insight and medication adherence of schizophrenia patients. Arch Psychiatr Nurs. 2018;32(5):737–744. doi: 10.1016/j.apnu.2018.04.011 [DOI] [PubMed] [Google Scholar]
- 52.Yilmaz E, Kavak F. Effects of mindfulness-based psychoeducation on the internalized stigmatization level of patients with schizophrenia. Clin Nurs Res. 2018;1054773818797871. [DOI] [PubMed] [Google Scholar]
- 53.Chien WT, Thompson DR. Effects of a mindfulness-based psychoeducation programme for Chinese patients with schizophrenia: 2-year follow-up. Br J Psychiatry. 2014;205(1):52–59. doi: 10.1192/bjp.bp.113.134635 [DOI] [PubMed] [Google Scholar]
- 54.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Vol. 2 Hillsdale N.J: Erlbaum Associates.; 1988. [Google Scholar]
- 55.Whitehead AL, Julious SA, Cooper CL, Campbell MJ. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res. 2016;25(3):1057–1073. doi: 10.1177/0962280215588241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Br Med J. 2016;355:i5239. doi: 10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Urbaniak GC, Plous S Research randomizer (Version 4.0) [Computer software]; 2015. Available from: http://www.randomizer.org/. Accessed November10, 2018.
- 58.Sealed Envelope Ltd. Create a blocked randomisation list. 2016. Available from: https://www.sealedenvelope.com/simple-randomiser/v1/lists. Accessed November10, 2018..
- 59.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149(7):936–943. [DOI] [PubMed] [Google Scholar]
- 60.Zhang C, Chung PK, Si G, Du M, Liu J. Tests of reliability and validity of the Emotion Regulation Questionnaire(ERQ) in Chinese athletes and students. Chin J Sports Med. 2014;9:907–913.:. [Google Scholar]
- 61.Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85(2):348–362. doi: 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- 62.Treynor W. Cognitive therapy and research. Cognit Ther Res. 2003;27(3):247–259. doi: 10.1023/A:1023910315561 [DOI] [Google Scholar]
- 63.Zhang H, Xu Y. Reliability and validity of the Chinese Short Ruminative Responses Scale (SRRS) in Chinese undergraduates. Psychol Res. 2010;4:7. [Google Scholar]
- 64.Norton PJ. Depression Anxiety and Stress Scales (DASS-21): psychometric analysis across four racial groups. Anxiety Stress Coping. 2007;20(3):253–265. doi: 10.1080/10615800701309279 [DOI] [PubMed] [Google Scholar]
- 65.Wang K, Shi HS, Geng FL, et al. Cross-cultural validation of the depression anxiety stress scale-21 in China. Psychol Assess. 2016;28(5):e88–e100. doi: 10.1037/pas0000207 [DOI] [PubMed] [Google Scholar]
- 66.Haddock G, McCarron J, Tarrier N, Faragher EB. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS). Psychol Med. 1999;29(4):879–889. doi: 10.1017/S0033291799008661 [DOI] [PubMed] [Google Scholar]
- 67.Chien WT, Lee IYM, Wang LQ. A Chinese version of the psychotic symptom rating scales: psychometric properties in recent-onset and chronic psychosis. Neuropsychiatr Dis Treat. 2017;13:745–753. doi: 10.2147/NDT.S131174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504 [DOI] [PubMed] [Google Scholar]
- 69.Hou J, Wong SY, Lo HH, Mak WW, Ma HS. Validation of a Chinese version of the five facet mindfulness questionnaire in Hong Kong and development of a short form. Assessment. 2014;21(3):363–371. doi: 10.1177/1073191113485121 [DOI] [PubMed] [Google Scholar]
- 70.Andreasen NC. Negative symptoms in schizophrenia. Definition and reliability. Arch Gen Psychiatry. 1982;39(7):784–788. doi: 10.1001/archpsyc.1982.04290070020005 [DOI] [PubMed] [Google Scholar]
- 71.Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry. 2003;64:663–667. doi: 10.4088/JCP.v64n0607 [DOI] [PubMed] [Google Scholar]
- 72.McCoy CE. Understanding the intention-to-treat principle in randomized controlled trials. West J Emerg Med. 2017;18(6):1075–1078. doi: 10.5811/westjem.2017.8.35985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ballinger GA. Using generalized estimating equations for longitudinal data analysis. Organ Res Methods. 2016;7(2):127–150. doi: 10.1177/1094428104263672 [DOI] [Google Scholar]
- 74.Gard DE, Sanchez AH, Cooper K, Fisher M, Garrett C, Vinogradov S. Do people with schizophrenia have difficulty anticipating pleasure, engaging in effortful behavior, or both? J Abnorm Psychol. 2014;123(4):771–782. doi: 10.1037/abn0000005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ghio L, Natta W, Barbato A, et al. Schizophrenia trial participation: perceived inclusion barriers and beliefs about antipsychotics. Pharmacopsychiatry. 2011;44(4):123–128. doi: 10.1055/s-0031-1277147 [DOI] [PubMed] [Google Scholar]
- 76.Gilbody S, Wahlbeck K, Adams C. Randomized controlled trials in schizophrenia: a critical perspective on the literature. Acta Psychiatr Scand. 2002;105(4):243–251. doi: 10.1034/j.1600-0447.2002.00242.x [DOI] [PubMed] [Google Scholar]
- 77.Khoury B, Lecomte T, Comtois G, Nicole L. Third-wave strategies for emotion regulation in early psychosis: a pilot study. Early Interv Psychiatry. 2015;9(1):76–83. doi: 10.1111/eip.2015.9.issue-1 [DOI] [PubMed] [Google Scholar]
- 78.Richards D, Martin WE. Thought suppression and mindfulness: a randomized controlled study. VISTAS Online. 2013;65:1–10. [Google Scholar]
- 79.Chambers R, Gullone E, Allen NB. Mindful emotion regulation: an integrative review. Clin Psychol Rev. 2009;29(6):560–572. doi: 10.1016/j.cpr.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 80.Jazaieri H, McGonigal K, Jinpa T, Doty JR, Gross JJ, Goldin PR. A randomized controlled trial of compassion cultivation training: effects on mindfulness, affect, and emotion regulation. Motiv Emot. 2014;38(1):23–35. doi: 10.1007/s11031-013-9368-z [DOI] [Google Scholar]
- 81.Fung J, Kim JJ, Jin J, Chen G, Bear L, Lau AS. A randomized trial evaluating school-based mindfulness intervention for ethnic minority youth: exploring mediators and moderators of intervention effects. J Abnorm Child Psychol. 2019;47(1):1–19. doi: 10.1007/s10802-018-0425-7 [DOI] [PubMed] [Google Scholar]
- 82.Robins CJ, Keng SL, Ekblad AG, Brantley JG. Effects of mindfulness-based stress reduction on emotional experience and expression: a randomized controlled trial. J Clin Psychol. 2012;68(1):117–131. doi: 10.1002/jclp.20857 [DOI] [PubMed] [Google Scholar]
- 83.Murata A, Moser JS, Kitayama S. Culture shapes electrocortical responses during emotion suppression. Soc Cogn Affect Neurosci. 2013;8(5):595–601. doi: 10.1093/scan/nss036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yuan J, Long Q, Ding N, Lou Y, Liu Y, Yang J. Suppression dampens unpleasant emotion faster than reappraisal: neural dynamics in a Chinese sample. Sci China Life Sci. 2015;58(5):480–491. doi: 10.1007/s11427-014-4739-6 [DOI] [PubMed] [Google Scholar]
- 85.Keng SL, Tan ELY, Eisenlohr-Moul TA, Smoski MJ. Effects of mindfulness, reappraisal, and suppression on sad mood and cognitive resources. Behav Res Ther. 2017;91:33–42. doi: 10.1016/j.brat.2017.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Butler EA, Lee TL, Gross JJ. Emotion regulation and culture: are the social consequences of emotion suppression culture-specific? Emotion. 2007;7(1):30–48. doi: 10.1037/1528-3542.7.1.30 [DOI] [PubMed] [Google Scholar]
- 87.Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30(2):217–237. doi: 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- 88.Cebolla A, Demarzo M, Martins P, Soler J, Garcia-Campayo J. Unwanted effects: is there a negative side of meditation? A multicentre survey. PLoS One. 2017;12(9):e0183137. doi: 10.1371/journal.pone.0183137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Guo Y, Chang SS, Sha F, Yip PSF. Poverty concentration in an affluent city: geographic variation and correlates of neighborhood poverty rates in Hong Kong. PLoS One. 2018;13(2):e0190566. doi: 10.1371/journal.pone.0190566 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- National Collaborating Centre for Mental Health (UK). Psychosis and schizophrenia in adults: treatment and management: updated edition 2014. National Institute for Health and Care Excellence (UK). NICE Clinical Guidelines, No. 178.) 2, Psychosis and Schizophrenia in Adults; 2014. Available from: https://www.ncbi.nlm.nih.gov/books/NBK333029/. Accessed November7, 2018.. [PubMed]