Abstract
Study Objective:
To characterize hospital admissions for any cause in the 30 days after a significant natural disaster in the United States. The main outcome was all-cause hospital admissions in the 30-days after natural disaster. Separate analyses were conducted to examine all-cause hospital admissions excluding the 72-hours after the disaster, Intensive Care Unit (ICU) admissions, all-cause in-hospital mortality and admissions by state.
Methods:
A self-controlled case series analysis using the 2011 Medicare Provider and Analysis Review File was conducted to examine exposure to natural disaster by elderly adults located in zip codes affected by tornados during the 2011 Southeastern superstorm,
Results:
All-cause hospital admissions increased by 4% in the thirty days after the April 27, 2011 tornadoes (IRR 1.04, 95% CI 1.01–1.07, p=.005). When excluding the first three days after the disaster that may be attributed to immediate injuries, hospitalizations for any cause also remained higher than when compared to the other 11 months of the year (IRR 1.04, 95% CI 1.01–1.07, p=.02). There was no increase in ICU admissions or in-hospital mortality associated with the natural disaster. When examined by individual states, Alabama, which had the highest number of persons affected, had a 9% increase in both hospitalizations and ICU admissions.
Conclusion:
When controlling for all time-invariant characteristics, this natural disaster was associated with a significant increase in all-cause hospitalizations. This analysis quantifies acute care utilization after disasters through examining all-cause hospitalizations and represents an important contribution to building models of resilience—the ability to recover from a disaster—and hospital surge capacity.
Introduction
A recent National Academy of Medicine report on disaster-resilient communities called for identifying gaps in both patient and health care system disaster response,1 to support the development of models of recovery that promote health outcomes in the aftermath of future disasters. However, measuring health outcomes—including acute care utilization such as hospitalizations—after disasters remains difficult largely due to challenges surrounding data collection during and in the immediate aftermath of such incidents. Disaster-related hospitalizations are rarely documented as such. Collecting data during a disaster response therefore requires a unique combination of foresight, planning, and coordination that has proven difficult to implement.2
Nonetheless, there have been attempts to characterize service delivery after disasters. Most studies describe expected increases in emergency department (ED) and primary care visits for disaster-associated injuries and illnesses after a disaster. One study found an increase in hospital length of stay and total charges incurred for non-casualty hospitalized patients in the weeks following a large mass casualty incident in the U.S. at the two main receiving hospitals.3 Psychiatric ED visits remained higher than baseline in the six months after Hurricane Sandy in 2012.4 ED use varied at individual hospitals after Hurricane Sandy, with visits the day of the disaster consistently lower than normal across all studies,5–7 while 30% of dialysis centers experienced some degree of weather-related impact on operations in the aftermath of the June 2012 mid-Atlantic storms in the U.S.8 An increase in all-cause admissions was found in the 30 days after Hurricane Katrina among dialysis patients.9 Yet, evaluating hospitalizations for any cause on a ‘whole disaster’ scale have remained limited in the disaster health literature.
In this study, we pivot from examining the direct sequelae of disasters, including disaster-induced injuries and the immediate surge capacity that accompanies this, to a broader view of the impact of disasters on the total burden of disease and acute care utilization. We sought to determine if hospital admissions for any cause increased in an extended recovery period after disasters. Using the April 27, 2011 Southeastern tornado outbreak as a model system we characterize all-cause hospital admissions in the 30 days after a significant natural disaster in the United States (US). As secondary analyses, we sought to examine the association with all-cause ICU admissions, mortality, and excluding the initial three days of the disaster when admissions for injury may be more likely.10,11
Methods
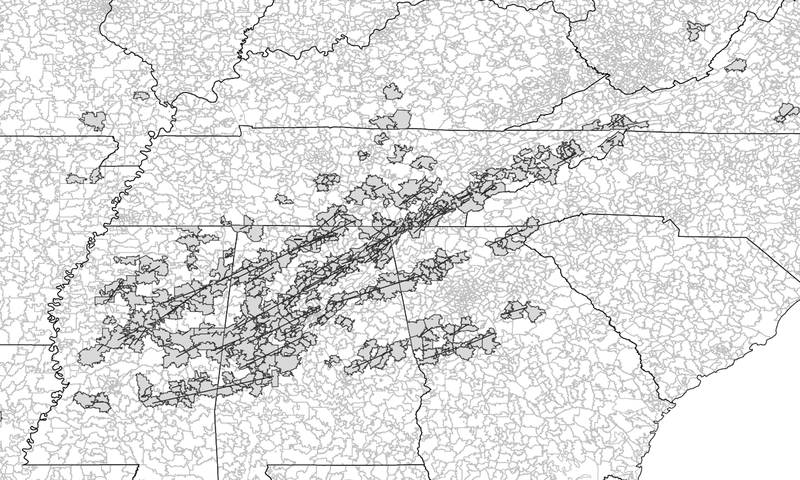
The 2011 Super Outbreak was one of the largest tornado-related natural disasters in US history. During a 24-hour period on April 27, 2011 a reported 218 tornadoes touched down across the Southeastern and Midwestern US, resulting in approximately 317 deaths and an estimated $5 billion in damages.12 Federal Emergency Management Agency (FEMA) disaster declarations were made in ten states.13 Figure 1 depicts a map of EF-4 and 5 tornadic events across Southeastern US. This study was approved by our institution’s Institutional Review Board.
Figure 1:
EF- 4 and 5 Tornado path by affected ZIP code
Data Sources
The 2011 Medicare Provider and Analysis Review File (MedPAR) combined with Medicare beneficiary claims data were used to conduct this analysis. MedPAR contains final action stay records for acute inpatient hospitalizations for individuals aged 65 or older, where we examined one claim per hospitalization. Spatial data of US tornado events was downloaded from the National Oceanic and Atmospheric Administration’s Severe Report database,14 and ZIP code data was obtained from the US Census Bureau.15
Included Population
Our sample included those in the MedPAR database who were hospitalized in areas with ZIP codes that had a confirmed EF-4 or 5 touchdown on April 27, 2011. Affected areas were identified (Figure 1) using ARC-GIS version 10.5 (Environmental Research Systems, Inc.; Redlands, CA). Populations in the affected ZIP code area with EF-4 and 5 tornado paths during the April 2011 Super Outbreak were included in the sample for our primary analysis.16 A population within the same broader geographic area which was confirmed to be unaffected by tornadoes was examined as a negative control.
Primary and Secondary Outcome Variables
All-cause hospital admissions in 2011 were examined as the primary outcome. Secondary analyses examined all-cause ICU admissions, all-cause in-hospital mortality, and all hospital admissions by state.
Statistical Analyses
All-cause hospitalizations after a natural disaster were characterized using self-controlled case series (SCCS) methodology.17 This methodology allows for examination of short-term exposures and acute outcomes. SCCS is a case-crossover method, where individuals serve as their own controls and confounders are controlled for within the modeling, making it an ideal methodology for secondary data analysis where limited information is available on potential confounders.18 Comparisons are made within individuals, where individuals act as their own controls, and are time-limited, requiring clearly defined periods of exposure in which the presence or absence of an event is measured. Since its analysis rests on when an event happened, rather than on who it happened to (e.g., by being ‘within persons’), covariates that would normally have high consideration for inclusion—such as functional status, income or education—are fully controlled for in the analysis without the need to directly measure them. SCCS has been used in the past to study reactions to vaccines where the best control population are the same patients at a different time period (e.g., adverse effects of vaccinations and the role of dysbiosis in rehospitalization for sepsis).17,19 A major limitation of many administrative claims-based analyses is that there are many factors related to hospitalization that are not present in Medicare claims—from functional status to wealth to more detailed information about the burden of comorbid disease-but are relatively stable over the time scale of months.
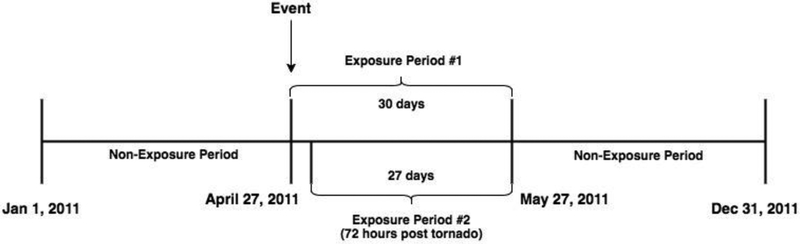
In order to accomplish this analysis, we conducted conditional fixed-effect Poisson regression to measure within-person differences in the rate of all-cause hospitalizations, all-cause ICU admissions, and all-cause in-hospital mortality following exposure to a natural disaster. The primary exposure was defined as 30 days after the tornadic events beginning on April 27, 2011 (Figure 2). This was compared to all other days during the 2011 calendar year. An additional sensitivity analysis was performed for an exposure period of 27 days beginning 3 days after the tornadoes, in order to exclude admissions that were a result of injuries or trauma that were hypothesized to disproportionately account for admissions in the 72-hour period immediately after the disaster.11 Next, analyses were also run individually by the four states most affected; Alabama, Georgia, Mississippi and Tennessee. Finally, a ‘negative control’ model was conducted in order to test the hypothesis that all-cause admissions would not increase in two unaffected locales in the same geographic region (Dothan, Alabama and Thomasville, Georgia) during the defined exposure period.
Figure 2:
Diagram of exposure and comparison periods
Incidence rate ratios (IRR) and 95% confidence intervals (CI) were generated as comparisons. All analyses were run in Stata version 14.0 (College Station, TX). A p-value of .05 was considered statistically significant. Our analytic code is in the Appendix.
Results
Our cohort consisted of 28,475 individuals and 56,857 hospitalizations. All individuals were aged 65 and older, lived in the ZIP codes in Southeastern US immediately affected by tornado touchdowns of EF-4 or greater during the April 27, 2011 Super Outbreak and were admitted to any US hospital during 2011.
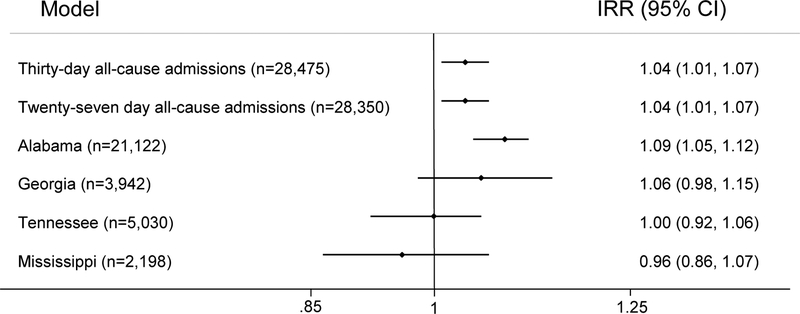
Among those living in the ZIP codes affected by tornadoes, there were 5,028 hospital admissions in the 30 days after the tornadoes, compared to an average of 4,712 hospital admissions per 30 days in this cohort during the rest of the year. Using SCCS analysis, which controlled for all time-invariant characteristics, all-cause hospital admissions increased 4% in this time period, when compared to the other 11 months in 2011 (IRR: 1.04, 95% CI 1.01–1.07, p=.005) (Table 1 and Figure 3).
Table 1:
EF-4 and 5 Tornado Adjusted Models 30-day Model (Exposure Period #1) AND Tornado All-Cause Admission 27-day Model (Exposure Period #2)
| N | Total Hospitalizations | IRR (95%CI) | p-value | |
|---|---|---|---|---|
| Admissions | 28,475 | 56,857 | 1.04(1.01–1.07) | .005 |
| ICU Admissions | 6,813 | 8,163 | 1.01(.93–1.10) | .81 |
| In-Hospital Mortality | 4,787 | n/a | .97(.91–1.04) | .37 |
| Admissions | 28,350 | 56,283 | 1.04(1.01–1.07) | .02 |
| ICU Admissions | 6,753 | 8,081 | 1.00(.92–1.U9) | .98 |
| In-Hospital Mortality | 6,797 | n/a | .94 (.88–1.01) | .09 |
Figure 3:
Forest Plot depicting modelling
We compared these results to two areas in the Southeast US that were unaffected by the Super Outbreak in order to determine if admissions increased independent of the effects of the storm. There were 5,465 individuals with 10,226 hospitalizations in the comparator region of Dothan, Alabama and Thomasville, Georgia. In this negative control cohort, admissions during the exposure period were not significantly different than the rest of the 2011 calendar year (IRR = .98, 95% CI .92–1.05, p=.65) when controlling for all time-invariant characteristics, showing geographic specificity of the association in the disaster cohort.
There were 694 ICU admissions in the 30 days after the tornadoes, compared with an average of 679 ICU admissions per 30 days in this cohort during the rest of the year. In the regression model controlling for all time-invariant characteristics, all-cause ICU admissions did not significantly increase in this time period, when compared to the other 11 months in 2011 (IRR, 1.01, 95% CI .93–1.10, p=.81). There was no increase in in-hospital mortality (IRR = .97, 95% CI .908–1.04, p=.37) from the regression controlling for all time-invariant characteristics.
Subgroup and Sensitivity Analyses
We tested the hypothesis that the apparent increase in hospitalizations was not simply driven by initial injuries during the storms. Excluding hospitalizations in the first 3 calendar days after the storm resulted in a sample of 28,350 individuals who were admitted to the hospital, with a total of 56,283 hospitalizations (Table 1). All-cause admissions increased 4% after regression controls were applied when compared to the rest of the year (IRR 1.04, 95% CI 1.01–1.07, p=.02). Controlling for all time-invariant characteristics, neither ICU admissions nor in-hospital mortality were statistically significant in this sensitivity analysis (IRR = 1.00, 95% CI .92–1.09, p=.98 and IRR = .94, 95% CI .88–1.01, p=.09) as in the primary analysis.
All-cause admissions, all-cause ICU admissions, and in-hospital mortality were also measured in stratified analyses in each of the individual states most severely impacted by the Super Outbreak: Alabama, Georgia, Mississippi and Tennessee, represented in Table 2. Alabama had the highest number of tornado touchdowns and the highest sample size, at 21,122. In examining Alabama separately, increases in all-cause admissions and ICU admissions were significant, representing a 9% increase (IRR 1.09, 95% CI 1.05–1.11, p<.001) in all-cause admissions and a 9% increase (IRR 1.09, 95% CI 1.02–1.20, p=.01) in ICU admissions in the 30 days after the tornado outbreak. In considering the states of Georgia, Mississippi and Tennessee, which had fewer tornadoes, none of the stratified analyses were statistically significant, although the confidence intervals were wide (IRR 1.06, 95% CI 1.98–1.15, p=.20; IRR = .96, 95% CI .86–1.07, p=.44; IRR=1.00, 95%CI .92–1.06, p=.81).
Table 2:
EF-4 and 5 Tornado Adjusted Models by State
| N | Total Hospitalizations | IRR (95%CI) | p-value | |
|---|---|---|---|---|
| Admissions | 21,122 | 42,219 | 1.09(1.05–1.12) | <.001 |
| ICU Admissions | 5,436 | 6,628 | 1.09(1.02–1.20) | .01 |
| In-Hospital Mortality | 5,104 | n/a | 1.00 (.92–1.07) | .90 |
| Admissions | 3,942 | 7,585 | 1.06(.98–1.15) | .15 |
| ICU Admissions | 855 | 1,004 | .93(.74–1.17) | .53 |
| In-Hospital Mortality | 959 | n/a | .796 (.653–.970) | .02 |
| Admissions | 2,198 | 4,435 | .96(.86–1.07) | .44 |
| ICU Admissions | 505 | 580 | .93 (.69–1.26) | .63 |
| In-Hospital Mortality | 406 | --- | .68(.521–.885) | .004 |
| Admissions | 5,030 | 10,096 | 1.00(.92–1.06) | .81 |
| ICU Admissions | 1,344 | 1,586 | .98(.81– 1.17) | .79 |
| In-Hospital Mortality | 1,198 | n/a | 1.13(.974–1.30) | .11 |
Discussion
The April 27 Super Outbreak was associated with a significant increase in all-cause admissions in the 30 days after the disaster, when compared to the rest of the year. This increase was specific to patients who lived in the ZIP codes directly affected by the tornadoes, as no similar increase was seen in comparison with unaffected areas in the same states. Results indicated mixed evidence of increased ICU admissions and in-hospital mortality—this is in line with past work evaluating April 2011 Super Outbreak mortality that found that most deaths occurred at the scene of the tornado rather than in the hospital setting.10
Based on past disasters, we hypothesized that most direct traumatic injuries from the disaster would present in the initial 72 hours after the incident.10,11 Therefore, we conducted analyses that excluded this time period. We found that admissions in the remaining 27 days of the month after the tornadoes still resulted in a significant increase in hospitalizations. This suggests there is a significant burden of excess morbidity and acute care utilization associated with, and likely caused by, the tornadoes that do not present immediately and may not be simply physical trauma-related.20
The significant increase in admissions found in this study and subgroups when compared to the rest of the year calls for a deeper understanding of hospital admissions after disasters. Determining factors that caused the observed increase is essential in building both community and healthcare system resilience—the ability to recover from a disaster—as well as longer-term hospital surge capacity. Current federal policy standards for surge capacity call for immediate availability of 20% of staffed beds within four hours of a declared disaster.21 However, our results support surge planning models based on a multicomponent approach that includes surge planning for longer time-frames post-incident22 as well as considering roles for community-based primary care, homecare, and ED-based interventions in preventing non-injury related hospitalizations.
While the current literature is limited in terms of identification of factors that mediate the effect of disasters on acute care use, specific stressors have been well-studied in individual disasters, such as exacerbation of chronic disease,9,23–25 physical manifestation of disaster-related stress and mental health issues26–28 and delays in access to care.26,29,30 Older adults with chronic disease are particularly at risk, as studies have shown that disaster-related care disruptions lead to chronic disease exacerbations.31,32 Our work builds on these findings by showing increases in acute care use in the form of hospitalizations, while also highlighting the need for further analysis by the specific modifiable factors driving acute care utilization.
While causation cannot be proven based on this study, the temporal and geographic specificity, reproducibility across individual states within this disaster, and plausibility based on body of findings of social epidemiology suggest that a causal interpretation may be possible. It is important to consider that this time-invariant model does control for many confounding factors that might otherwise have affected a traditional regression model. That is, because patients serve as their own control, this approach controls for any potential confounders that were unchanged between the exposure and non-exposure periods. For example, whether a patient’s neighborhood was socially disadvantaged would not be unchanged between the exposure and non-exposure period, and therefore cannot logically explain differences between the exposure and non-exposure periods. Likewise, the time of the year the tornadoes occurred suggests that the increase in admission was not related to seasonal variation. This is supported by the absence of an increase in hospitalizations in the non-exposed region.
A strength of this study is that pre-disaster ZIP codes were used as the baseline for analyses, allowing for inclusion of individuals who leave the area after the disaster, provided that they received care somewhere in the US that was covered by Medicare. This is an important consideration since migration of displaced populations is an expected byproduct after major disasters,33–35 where the disaster-displaced are often lost to follow up.
Quantifying the burden of disease and acute care use after disasters by examining all-cause hospitalizations represents an important contribution to building models of community resilience and hospital surge capacity that can prevent or mitigate disaster sequelae. These sequelae are common and severe.36 Costs associated with disasters in the US in 2011 amounted to $55 billion, with 14 events costing $1 billion or more each,37 not to mention the unquantifiable physical, social and psychological effects on individuals, families, and communities. Multiple initiatives are in place to address community1,37,38 and hospital and health system resilience39–41 on a policy level, from the Office of the Assistant Secretary for Preparedness and Response (ASPR), Department of Health and Human Services (HHS), the United Nations Strategy for Disaster Reduction and the World Health Organization, among others. However, data that supports developing and building resilience remains badly needed.
Limitations
This study was conducted as a test of concept, in an attempt to evaluate our hypothesis that all-cause admissions could be characterized using a large national database when linked to a specific disaster. Also, this study informs the growing body of disaster resilience and hospital surge literature that can be used to support preparedness planning such as building community and healthcare system resilience, resource allocation, and service delivery. However, before that can be done, expanding this study to examine other types of disasters such as terrorist attacks, heat emergencies, and hurricanes, is essential. We have studied only a single cluster of disasters across four states. The generalizability of these findings to other disasters and other settings needs to be further studied. While we report increased all-cause admissions through the use of SCCS modeling, a limitation of using this methodology is that variables of interest, such as differences by age, gender, income, education or racial/ethnic makeup, are not reported here. Further, it is of great interest to understand which populations may be most vulnerable, and which community and healthcare system characteristics may moderate the observed increase in all-cause hospitalizations. This requires an evaluation of a larger sample of disasters.
Conclusion
All-cause hospital admissions increased significantly in the 30 days after the April 27, 2011 Super Outbreak, when compared to the rest of the year. The results of this study point to the need for building community and healthcare system resilience to account for health care needs of older adults after a disaster.
Acknowledgments
Grants: This work was supported by the National Clinicians Scholars Program, and K08 HS020672 to Colin Cooke.
Appendix
Master do-file
use EF45all30d.dta, clear
sum bene_zip
gen keepzip=0
foreach zip in 35966 24361 35643 37325 39169 30741 39756 37153 37409 39767 35744 36279 35771 30178 35773 37421 35757 36738 38962 35548 35571 35740 37411 35480 37339 35083 37406 39152 35988 36776 24211 38827 35755 35019 35127 30205 35214 35401 35984 35975 30183 35746 35217 38929 38944 39358 35749 35750 30258 35244 20735 30285 14821 14838 35554 35552 37323 20136 37328 30725 37329 35980 37419 35981 35986 35989 37128 37343 37347 30734 37416 47882 37331 20190 37359 37360 36912 37353 39739 39743 39776 42151 35810 35811 36732 35958 37742 38580 37753 38588 37760 37777 24236 24340 28741 28775 37934 37920 45344 37681 24597 38471 37711 38506 38547 72404 72437 38928 36786 35406 37311 37336 35207 35950 30240 37690 37332 37034 30217 35633 35905 35758 30545 37341 38838 38563 37046 37412 35463 35550 37302 30663 20181 30216 20744 37352 30056 35806 35601 30125 30124 36855 35224 35016 35971 30256 30171 35477 39752 39356 30752 39751 35111 36271 38828 {
replace keepzip=1 if bene_zip==`zip’
}
tab keepzip
*keep only affected zip
keep if keepzip==1
tab bene_zip
*Keep person id and admission dates
keep bene_id admsn_dt bene_death_dt
egen id=group(bene_id)
codebook id bene_id
sort id admsn_dt bene_death_dt
*Generate exposure time variable
gen whole_year=.
replace whole_year=0 if (admsn_dt>=td(01jan2011))&(admsn_dt<=td(26apr2011))
replace whole_year=1 if (admsn_dt>=td(27apr2011))&(admsn_dt<=td(26may2011))
replace whole_year=0 if (admsn_dt>=td(27may2011))&(admsn_dt<=td(31dec2011))
gen one=1
save EF45all_30dx2, replace
********************************************************
use EF45all_30dx2, clear
codebook id
keep if whole_year <.
*summarize # of people by admission
bysort id: egen n_admission=sum(one)
bysort id: gen firstobs=1 if _n==1
tab n_admission if firstobs==1
keep id bene_death_dt
bysort id: gen firstobs=1 if _n==1
keep if firstobs==1
drop firstobs
save deathdates.dta, replace
use EF45all_30dx2, clear
codebook id
keep if whole_year <.
collapse (count) num_events=one, by(id whole_year)
** to create a balanced sample (each person should have two exposure periods)
reshape wide num_events, i(id) j(whole_year)
reshape long num_events, i(id) j(whole_year)
replace num_events=0 if num_events==.
merge m:1 id using deathdates.dta
gen predx_duration=.
replace predx_duration=bene_death_dt-td(31dec2010) if
(bene_death_dt>=td(01jan2011))&(bene_death_dt<=td(26apr2011))
replace predx_duration=(td(26apr2011)-td(31dec2010)) if (bene_death_dt>=td(27apr2011)) |
missing(bene_death_dt)
gen postdx_duration=.
replace postdx_duration=0 if bene_death_dt<td(27may2011)
replace postdx_duration=bene_death_dt-td(26may2011) if
(bene_death_dt>=td(27may2011))&(bene_death_dt<=td(31dec2011))
replace postdx_duration=(td(31dec2011)-td(26may2011)) if (bene_death_dt>=td(31dec2011)) | missing(bene_death_dt)
gen unexposed_duration=.
replace unexposed_duration= predx_duration + postdx_duration
gen intradx_duration=.
replace intradx_duration=0 if bene_death_dt<td(27apr2011)
replace intradx_duration=bene_death_dt-td(26apr2011) if
(bene_death_dt>=td(27apr2011))&(bene_death_dt<=td(26may2011))
replace intradx_duration=(td(26may2011)-td(27apr2011)) if (bene_death_dt>=td(27may2011)) | missing(bene_death_dt)
tab predx_duration, m
tab postdx_duration, m
tab intradx_duration, m
tab unexposed_duration, m
gen duration=.
replace duration= unexposed_duration if whole_year==0
replace duration= intradx_duration if whole_year==1
tab duration
gen logduration=ln(duration)
xi: xtpoisson num_events i.whole_year, fe i(id) offset(logduration) eform
Footnotes
Meetings: None to declare
Conflicts of Interest: None. No professional writing assistance or others were paid to provide manuscript support.
Contributor Information
Sue Anne Bell, National Clinician Scholars Program, Institute for Health Care Policy and Innovation and School of Nursing, University of Michigan 2800 Plymouth Rd Bldg 14 Rm G100, Ann Arbor, MI 48109.
Mahshid Abir, Department of Emergency Medicine, University of Michigan, Ann Arbor, MI United States.
HwaJung Choi, Department of Internal Medicine, University of Michigan, Ann Arbor, MI United States.
Colin Cooke, Department of Internal Medicine, University of Michigan, Ann Arbor, MI United States.
Theodore Iwashyna, Department of Internal Medicine, University of Michigan, Ann Arbor, MI United States.
References
- 1.Committee on Post-Disaster Recovery of a Community’s Public Health, Medical and SS Healthy, Resilient, and Sustainable Communities after Disasters. Washington, DC; 2015. www.nap.edu. [PubMed] [Google Scholar]
- 2.Morton M, Levy JL. Challenges in Disaster Data Collection during Recent Disasters. Prehosp Disaster Med. 2011;26(3):196–201. doi: 10.1017/S1049023X11006339. [DOI] [PubMed] [Google Scholar]
- 3.Abir M, Choi H, Cooke CR, Wang SC, Davis MM. Effect of a mass casualty incident: clinical outcomes and hospital charges for casualty patients versus concurrent inpatients. Acad Emerg Med. 2012;19(3):280–286. doi: 10.1111/j.1553-2712.2011.01278.x. [DOI] [PubMed] [Google Scholar]
- 4.He FT, Lundy De La Cruz N, Olson D, et al. Temporal and Spatial Patterns in Utilization of Mental Health Services During and After Hurricane Sandy: Emergency Department and Inpatient Hospitalizations in New York City. Disaster Med Public Health Prep. 2016;10(3):512–517. doi: 10.1017/dmp.2016.89. [DOI] [PubMed] [Google Scholar]
- 5.Greenstein J, Chacko J, Ardolic B, Berwald N. Impact of Hurricane Sandy on the Staten Island University Hospital Emergency Department. Prehosp Disaster Med. 2016;31(3):335–339. doi: 10.1017/S1049023X16000261. [DOI] [PubMed] [Google Scholar]
- 6.Gotanda H, Fogel J, Husk G, et al. Hurricane Sandy: Impact on Emergency Department and Hospital Utilization by Older Adults in Lower Manhattan, New York (USA). Prehosp Disaster Med. 2015;30(5):496–502. doi: 10.1017/S1049023X15005087. [DOI] [PubMed] [Google Scholar]
- 7.Kim H, Schwartz RM, Hirsch J, Silverman R, Liu B, Taioli E. Effect of Hurricane Sandy on Long Island Emergency Departments Visits. Disaster Med Public Health Prep. 2016;10(3):344–350. doi: 10.1017/dmp.2015.189. [DOI] [PubMed] [Google Scholar]
- 8.Abir M, Jan S, Jubelt L, Merchant RM, Lurie N. The Impact of a Large-Scale Power Outage on Hemodialysis Center Operations. Prehosp Disaster Med. 2013;28(6):543–546. doi: 10.1017/S1049023X13008844. [DOI] [PubMed] [Google Scholar]
- 9.Howard D, Zhang R, Huang Y, Kutner N. Hospitalization rates among dialysis patients during Hurricane Katrina. Prehosp Disaster Med. 2012;27(4):325–329. doi: 10.1017/S1049023X12000945. [DOI] [PubMed] [Google Scholar]
- 10.Chiu CH, Schnall AH, Mertzlufft CE, et al. Mortality from a tornado outbreak, Alabama, April 27, 2011. Am J Public Health. 2013;103(8):e52–8. doi: 10.2105/AJPH.2013.301291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niederkrotenthaler T, Parker EM, Ovalle F, et al. Injuries and Post-Traumatic Stress following Historic Tornados: Alabama, April 2011. Ramagopalan SV., ed. PLoS One. 2013;8(12):e83038. doi: 10.1371/journal.pone.0083038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NBC News Service. Twister outbreak is second deadliest in U.S. history. http://www.nbcnews.com/id/42834400/ns/weather/#.WJpGGBIrKCQ. Published April 30, 2011.
- 13.Federal Emergency Management Agency. Disaster Declarations by Year. 2015. http://www.fema.gov/disasters/grid/year. Accessed October 16, 2015.
- 14.Storm Prediction Center. SVRGIS. NOAA’s Natl Weather Serv. 2016. http://www.spc.noaa.gov/gis/svrgis/. Accessed February 19, 2017.
- 15.US Census Bureau. Cartographic Boundary Shapefiles - ZIP Code Tabulation Areas (ZCTAs). Geography. 2013. https://www.census.gov/geo/maps-data/data/cbf/cbf_zcta.html. Accessed March 20, 2017. [Google Scholar]
- 16.Storm Prediction Center. Enhanced F Scale for Tornado Damage. Enhanc Fujita Scale Recomm Report, 2006, Revis 2 2006. http://www.spc.noaa.gov/efscale/ef-scale.html. Accessed February 13, 2017. [Google Scholar]
- 17.Petersen I, Douglas I, Whitaker H. Self controlled case series methods: an alternative to standard epidemiological study designs. BMJ. 2016;354:i4515 http://www.ncbi.nlm.nih.gov/pubmed/27618829. Accessed September 15, 2016. [DOI] [PubMed] [Google Scholar]
- 18.Whitaker HJ, Farrington CP, Spiessens B, Musonda P. Tutorial in Biostatistics: The self-controlled case series method. Stat Med Stat Med. 2005;0:1–31. [DOI] [PubMed] [Google Scholar]
- 19.Prescott HC, Dickson RP, Rogers MAM, Langa KM, Iwashyna TJ. Hospitalization Type and Subsequent Severe Sepsis. Am J Respir Crit Care Med. 2015;192(5):581–588. doi: 10.1164/rccm.201503-0483OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brilleman SL, Wolfe R, Moreno-Betancur M, et al. Associations between community-level disaster exposure and individual-level changes in disability and risk of death for older Americans. Soc Sci Med. 2017;173:118–125. doi: 10.1016/j.socscimed.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Assistant Secretary for Preparedness and Response. Hospital Preparedness Program (HPP) Healthcare Preparedness Capability Review National Call Capability 10: Medical Surge and Immediate Bed Availability (IBA) Meeting Summary.; 2013. https://www.phe.gov/Preparedness/planning/hpp/meetings/Documents/capability10.pdf.
- 22.Barbisch DF, Koenig KL. Understanding Surge Capacity: Essential Elements. Acad Emerg Med. 2006;13(11):1098–1102. doi: 10.1197/j.aem.2006.06.041. [DOI] [PubMed] [Google Scholar]
- 23.Lee DC, Gupta VK, Carr BG, et al. Acute post-disaster medical needs of patients with diabetes: emergency department use in New York City by diabetic adults after Hurricane Sandy. BMJ Open Diabetes Res Care. 2016;4(1):e000248. doi: 10.1136/bmjdrc-2016-000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin C, Pierce LC, Roblin PM, Arquilla B. Impact of Hurricane Sandy on Hospital Emergency and Dialysis Services: A Retrospective Survey. Prehosp Disaster Med. 2014;29(4):374–379. doi: 10.1017/S1049023X14000715. [DOI] [PubMed] [Google Scholar]
- 25.Fonseca VA, Smith H, Kuhadiya N, et al. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32(9):1632–1638. doi: 10.2337/dc09-0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sirey JA, Berman J, Halkett A, et al. Storm Impact and Depression Among Older Adults Living in Hurricane Sandy–Affected Areas. Disaster Med Public Health Prep. 2017;11(1):97–109. doi: 10.1017/dmp.2016.189. [DOI] [PubMed] [Google Scholar]
- 27.Bell SA, Folkerth LA. Women’s Mental Health and Intimate Partner Violence Following Natural Disaster: A Scoping Review. Prehosp Disaster Med. 2016:1–10. doi: 10.1017/S1049023X16000911. [DOI] [PubMed] [Google Scholar]
- 28.Lowe SR, Sampson L, Gruebner O, Galea S. Psychological Resilience after Hurricane Sandy: The Influence of Individual- and Community-Level Factors on Mental Health after a Large-Scale Natural Disaster. Chao L, ed. PLoS One. 2015;10(5):e0125761. doi: 10.1371/journal.pone.0125761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abir M, Jan S, Jubelt L, Merchant RM, Lurie N. The Impact of a Large-Scale Power Outage on Hemodialysis Center Operations. Prehosp Disaster Med. 2013;28(6):543–546. doi: 10.1017/S1049023X13008844. [DOI] [PubMed] [Google Scholar]
- 30.Runkle JD, Brock-Martin A, Karmaus W, Svendsen ER. Secondary Surge Capacity: A Framework for Understanding Long-Term Access to Primary Care for Medically Vulnerable Populations in Disaster Recovery. Am J Public Health. 2012;102(12):e24–e32. doi: 10.2105/AJPH.2012.301027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aldrich N, Benson WF. Disaster preparedness and the chronic disease needs of vulnerable older adults. Prev Chronic Dis. 2008;5(1):A27 http://www.ncbi.nlm.nih.gov/pubmed/18082016. Accessed April 5, 2017. [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention (CDC). Rapid assessment of the needs and health status of older adults after Hurricane Charley--Charlotte, DeSoto, and Hardee Counties, Florida, August 27–31, 2004. MMWR Morb Mortal Wkly Rep. 2004;53(36):837–840. http://www.ncbi.nlm.nih.gov/pubmed/15371964. Accessed April 5, 2017. [PubMed] [Google Scholar]
- 33.Sastry N. Tracing the Effects of Hurricane Katrina on the Population of New Orleans: The Displaced New Orleans Residents Pilot Study. Sociol Methods Res. 2009;38(1):171–196. doi: 10.1177/0049124109339370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ridenour ML, Cummings KJ, Sinclair JR, Bixler D. Displacement of the Underserved: Medical Needs of Hurricane Katrina Evacuees in West Virginia. J Health Care Poor Underserved. 2007;18(2):369–381. doi: 10.1353/hpu.2007.0045. [DOI] [PubMed] [Google Scholar]
- 35.Smith M. Katrina revisited: recovery strategies - redevelopment vs. relocation. Int J Emerg Manag. 2014;10(1):91–102. doi: 10.1504/IJEM.2014.061664. [DOI] [Google Scholar]
- 36.NOAA National Centers for Environmental Information (NCEI). Billion-Dollar Weather and Climate Disasters: Summary Stats | National Centers for Environmental Information (NCEI). 2017. https://www.ncdc.noaa.gov/billions/summary-stats. Accessed April 5, 2017.
- 37.The National Academies. Disaster Resilience: A National Imperative. Washington, DC; 2012. https://www.nap.edu/catalog/13457/disaster-resilience-a-national-imperative. [Google Scholar]
- 38.Chandra A, Acosta J, Howard S, et al. Building Community Resilience to Disasters. RAND Corporation; 2011. http://www.rand.org/pubs/technical_reports/TR915.html. Accessed April 3, 2017. [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization; Comprehensive Safe Hospital Framework. Geneva, Switzerland; 2015. http://www.who.int/hac/techguidance/comprehensive_safe_hospital_framework.pdf. [Google Scholar]
- 40.United Nations Office for Disaster Reduction. Hospitals Safe from Disasters. Geneva, Switzerland; 2009. https://www.unisdr.org/2009/campaign/pdf/wdrc-2008-2009-information-kit.pdf. [Google Scholar]
- 41.Assistant Secretary for Preparedness and Response. Hospital Preparedness Program. 2017. https://www.phe.gov/preparedness/planning/hpp/Pages/default.aspx. Accessed February 18, 2017.