Abstract
Background
Urinary tract infections are among the more common types of nosocomial infection in Germany and are associated with catheters in more than 60% of cases. With increasing rates of antibiotic resistance worldwide, it is essential to distinguish catheter-associated asymptomatic bacteriuria from catheter-associated urinary tract infection (CA-UTI).
Methods
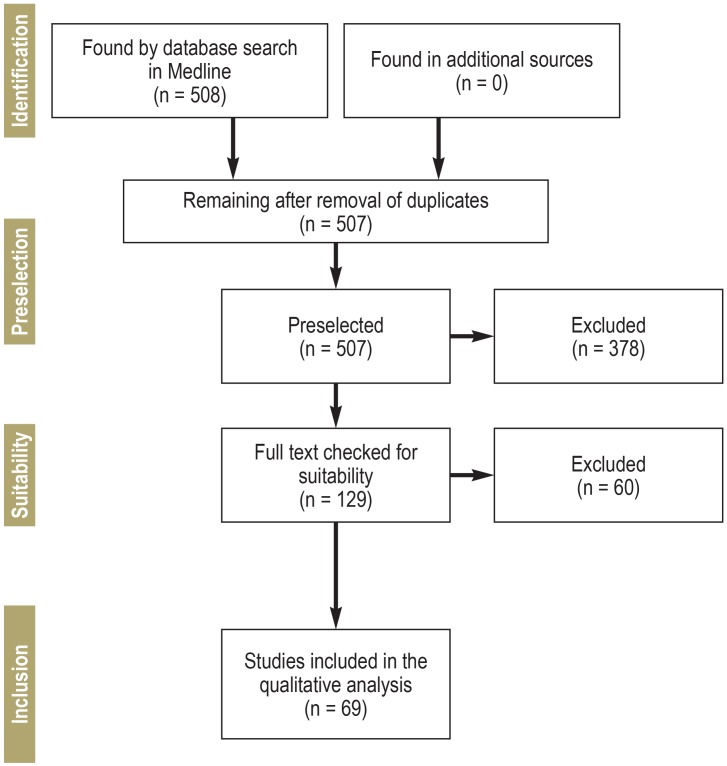
This review is based on publications from January 2000 to March 2019 that were retrieved by a selective search in Medline. Randomized clinical trials and systematic reviews in which the occurrence of CA-UTI in adult patients was a primary or secondary endpoint were included in the analysis. Two authors of this review, working independently, selected the publications and extracted the data.
Results
508 studies were identified and 69 publications were selected for analysis by the prospectively defined criteria. The studies that were included dealt with the following topics: need for catheterization, duration of catheterization, type of catheter, infection prophylaxis, education programs, and multiple interventions. The duration of catheterization is a determinative risk factor for CA-UTI. The indications for catheterization should be carefully considered in each case, and the catheter should be left in place for the shortest possible time. The available data on antibiotic prophylaxis do not permit any definitive conclusion, but they do show a small benefit from antibiotic-impregnated catheters and from systemic antibiotic prophylaxis.
Conclusion
Various measures, including careful consideration of the indication for catheterization, leaving catheters in place for the shortest possible time, and the training of nursing personnel, can effectively lower the incidence of CA-UTI. The available evidence is markedly heterogeneous in some respects, and thus no recommendations can be given on certain questions relevant to CA-UTI.
Klinik für Urologie und Kinderurologie, St. Antonius-Hospital gGmbH, Akademisches Lehrkrankenhaus der RWTH Aachen Dechant-Deckers-Str. 8 52249 Eschweiler, Germany jennifer.kranz@sah-eschweiler.de
Urinary tract infections account for 21.6% of all nosocomial infections in Germany and are thus among the more frequent types of nosocomial infection, along with lower respiratory infections (24%), postoperative wound infections (22.4%), Clostridium difficile infections (10%), and primary sepsis (5.1%) (1, 2).
In more than 60% of cases (407 of 670 patients), nosocomial urinary tract infections are associated with catheters (2, 3). 15–25% of all hospitalized patients are catheterized at some time during their hospital stay (4); among patients in intensive care units, the corresponding percentage has been reported as 18% to 81.7% (5– 7). The incidence of bacteriuria in medical facilities rises by 3–8% per day for each day after catheter insertion; nearly all patients have bacteriuria after 30 days of catheterization (8, 9). Most episodes of catheter-associated bacteriuria are asymptomatic (catheter-associated asymptomatic bacteriuria, CA-ABU), and fewer than 5% of cases lead to bacteremia requiring treatment (10). Overall, catheter-associated bacteremia accounts for 15% of nosocomial bloodstream infections (11) and is associated with 10% mortality (12, 13).
With antibiotic resistance on the rise and presenting major challenges, including increased costs, to health-care systems worldwide (14), it has become essential to distinguish CA-ABU, which needs no treatment, from CA-UTI, which must be treated (15).
The goal of this article is to provide an overview of urinary catheter management and UTI prevention.
Method
A rapid evidence analysis (16) was performed with a literature search in Medline for the period January 2000 to March 2019. Symptomatic CA-UTI in adults was a primary or secondary endpoint of all of the included studies. Only randomized trials and systematic reviews were included in the present analysis. Further information on the methods of this analysis can be found in the supplementary material available over the Internet (ebox).
eBOX. Search strategy.
A literature search was carried out in March 2019 in the Medline biomedical database (via Ovid). The search terms—“urinary tract infections,” “complicated urinary tract infections,” “cystitis,” “pyelonephritis,” “percutaneous nephrostomy,” “catheters,” “pcnl”—were entered as MesH terms and as free text. The search strategy is shown below.
We included only randomized, controlled trials (RCTs) and systematic reviews (SRs). Studies dealing with any type of intervention in catheterized adults in either the inpatient or outpatient setting were included as long as symtpomatic catheter-associated urinary tract infection was a primary or secondary endpoint. Only full-text publications in English or German from the year 2000 or later were included. Studies on catheter-associated bacteriuria were not included.
Two authors of the present review (JK and SS) independently screened the retrieved publications and checked them for suitability for inclusion according to the above criteria. The following study data were extracted by two of the authors (SS, LS): study information and objective, patient population, description of intervention, endpoints, and authors’ conclusions.
Medline Ovid: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily
-
1
exp urinary tract infections/
-
2
exp cystitis/
-
3
exp pyelonephritis/
-
4
exp Percutaneous Nephrostomy/
-
5
cystitis.tw.
-
6
complicated urinary tract infection*.tw.
-
7
urinary tract infection*.tw.
-
8
uti.tw.
-
9
cauti.tw.
-
10
pyelonephriti*.tw.
-
11
exp catheters, indwelling/
-
12
exp urinary catheters/
-
13
urinary catheter*.tw.
-
14
indwelling catheter*.tw.
-
15
permanent catheter*.tw.
-
16
suprapubic catheter*.tw.
-
17
transurethral catheter*.tw.
-
18
Percutaneous Nephrostomy.tw.
-
19
(pcn or pcnl).tw.
-
20
or/1–10
-
21
or/11–17
-
22
18 or 19
-
23
21 or 22
-
24
20 and 23
-
25
Randomized Controlled Trials as Topic/
-
26
randomized controlled trial/
-
27
Random Allocation/
-
28
Double Blind Method/
-
29
Single Blind Method/
-
30
clinical trial/
-
31
clinical trial, phase i.pt.
-
32
clinical trial, phase ii.pt.
-
33
clinical trial, phase iii.pt.
-
34
clinical trial, phase iv.pt.
-
35
controlled clinical trial.pt.
-
36
randomized controlled trial.pt.
-
37
multicenter study.pt.
-
38
clinical trial.pt.
-
39
exp Clinical Trials as topic/
-
40
or/25–39
-
41
(clinical adj trial$).tw.
-
42
((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)).tw.
-
43
PLACEBOS/
-
44
placebo$.tw.
-
45
randomly allocated.tw.
-
46
(allocated adj2 random$).tw.
-
47
or/41–46
-
48
40 or 47
-
49
case report.tw.
-
50
letter/
-
51
historical article/
-
52
or/49–51
-
53
48 not 52
-
54
Meta-Analysis as Topic/
-
55
meta analy$.tw.
-
56
metaanaly$.tw.
-
57
Meta-Analysis/
-
58
(systematic adj (review$1 or overview$1)).tw.
-
59
exp Review Literature as Topic/
-
60
or/54–59
-
61
cochrane.ab.
-
62
embase.ab.
-
63
(psychlit or psyclit).ab.
-
64
(psychinfo or psycinfo).ab.
-
65
(cinahl or cinhal).ab.
-
66
science citation index.ab.
-
67
bids.ab.
-
68
cancerlit.ab.
-
69
or/61–68
-
70
reference list$.ab.
-
71
bibliograph$.ab.
-
72
hand-search$.ab.
-
73
relevant journals.ab.
-
74
manual search$.ab.
-
75
or/70–74
-
76
selection criteria.ab.
-
77
data extraction.ab.
-
78
76 or 77
-
79
Review/
-
80
78 and 79
-
81
Comment/
-
82
Letter/
-
83
Editorial/
-
84
animal/
-
85
human/
-
86
84 not (84 and 85)
-
87
or/81–83,86
-
88
60 or 69 or 75 or 80
-
89
88 not 87
-
90
24 and 53
-
91
24 and 89
-
92
90 or 91
-
93
limit 92 to (english or german)
-
94
limit 93 to yr=”2000 -Current”
-
95
limit 94 to humans
Results
Findings of the literature search
The literature search yielded 508 hits (efigure), of which 69 studies were included in the analysis (eTable). The included studies were thematically clustered: need for catheterization (n = 2), duration of catheterization (n = 11 studies), type of catheter (n = 17), prophylaxis (n = 25), education programs (n = 9), and studies with multiple interventions (n = 5). A total of 28 systematic reviews (including nine Cochrane reviews [6–15]) and 41 randomized, controlled trials (RCTs) were identified.
eFigure.
PRISMA flow diagram for the sequential phases of the systematic review (e37). For further information, see www.prisma-statement.org.
Table 2. Evidence: Catheter-associated UTIs / Updated: 17 July 2019.
|
Study Design Location Dates |
Study aim | Patient information | Information on intervention | Results | Authors' Study conclusion | Comments |
| Studies on duration of catheterization | ||||||
|
Ahmed 2014 RCT Egypt April 2010 to December 2012 |
if immediate (0 h) versus intermediate (6 h) versus delayed (24 h) removal of an indwelling catheter can affect the rate of re-catheterization | Women with uncomplicated abdominal hysterectomy On the morning of surgery, all patients received a single dose of prophylactic antibiotic in the form of ceftriaxone 1 g intramuscularly. |
Group A (73 patients): catheter removal immediately after surgery (0 h) Group B (81 patients): catheter removal 6 h post-OP Group C (67 patients): catheter removal 24 h post-OP size 12 latex Foley's catheter |
Symptomatic UTI, n (%): A: 1 (1,4) B: 3 (3,7) C: 10 (14,9) (p=0.008) |
Removal of urinary catheter 6 h post-OP appears to be more advantageous than early or late removal in cases of uncomplicated total abdominal hysterectomy. | |
|
Alessandri
2006 RCT Italy September 2003 and March 2004 |
comparing immediate versus delayed catheter removal | Women with hysterectomy various benign diseases All patients received a single dose of antibiotic prophylaxis before the operation. |
Group A (32 patients): immediate removal of the catheter in the operating room. 2. Group B (32 patients): removal of catheter at 6 h after the operation. 3. Group C (32 patients): removal of catheter at 12 h after the operation. 16F latex catheters with a 10 ml balloon were used |
Symptomatic urinary infection, n (%): A: 1/32 (3.1) B: 4/30 (13.3) C: 5/32 (15.6) (p NS) |
There could be an association between necessity of recatheterization and the type of surgery (VH) or the type of anesthesia (spinal). Despite recatheterization rate, early removal of in-dwelling catheters immediately after uncomplicated hysterectomy seems to decrease first ambulation time and hospital stay. | |
|
Bray 2017 RCT UK |
to compare immediate removal with the use of an indwelling catheter. | patients admitted for prolapse surgery via the vaginal route one dose of intraoperative prophylactic antibiotics |
Group A (29 patients):
Suprapubic catheter, until day 2 post-OP Group B (31 patients): immediate removal |
Rate of symptomatic bacteriuria (n): A: 15 B: 5 (p<0.01) |
After vaginal surgery for pelvic organ prolapse, the majority of patients do not require extended catheterisation. Early removal of a catheter reduces urinary tract infection and significantly decreases hospital stay | |
|
Chai 2011 RCT Hong Kong November 2007 and September 2009 |
To assess whether early or immediate removal of 12F indwelling Foley catheter after total abdominal hysterectomy affects the level of subjective pain assessment postoperatively | women undergoing total abdominal hysterectomy for various benign gynecological diseases | Group A (35 patients): catheter removal immediately post-OP Group B (35 patients): catheter removal on post-OP day 1, i.e. 24 h latex 12F with a 10ml balloon Foley catheter under aseptic technique Routine prophylactic antibiotics were not given. |
The incidence of symptomatic urinary tract infection did not differ between the two groups UTI, n (%): A: 1 (2.9) B: 3 (8.6) (p NS) |
There are pros and cons regarding the policy of one-day in-dwelling catheterization compared to immediate catheter removal. | |
|
Dunn 2003 RCT USA January 1998 to December 2001 |
whether the immediate removal of indwelling catheters after OP affects the rate of recatheterization, febrile morbidity, UTI, pain. | women with hysterectomy | Group A: immediate catheter removal Group B: catheter removal day 1 post-OP |
UTI: A: 3 B: 3 (p NS) |
Early removal of indwelling catheters after OP no associated with an increased rate of UTIs | |
|
El-Mazny 2014 RCT Egypt November 2012 to March 2014 |
To compare immediate and 12 h postoperative removal of urinary catheter after elective cesarean section. | women admitted for primary or repeat elective cesarean section | Group A (n = 150): catheter removal immediately Group B (n = 150): catheter removal 12 h post-OP Foley urethral catheter (French size 16) all received antibiotic prophylaxis |
Postoperative urinary complications (A, B, p value) number (%): Dysuria: 11 (7.3), 24 (16.0), 0.030 Burning on micturition: 4 (2.7), 15 (10.0), 0.016 Urinary frequency: 3 (2.0), 12 (8.0), 0.031 |
Immediate removal of urinary catheter after elective cesarean section is associated with lower risk of urinary infection and earlier postoperative ambulation. | |
|
Fernandez 2006 SR on RCT and observation al search date July 2004 |
to assess the effect of duration of catheterization on urinary retention. | 8 studies patients of all ages and in any setting (hospital, community, and nursing home) | various durations of catheterization prior to the removal of short-term indwelling urethral catheters | Four trials demonstrated no statistically significant difference in the incidence of urinary tract infection between the groups in patients after TURP (RR 0.55, 95% CI 0.30 to 1.03). However, 1 small trial reported that patients who had their indwelling urethral catheters removed 5 days after rectal resection had a significantly higher incidence of urinary tract infection compared to those who had their indwelling urethral catheters removed 1 day after the surgery (RR 0.48, 95% CI 0.27 to 0.85). | No significant differences in patient outcome were found, but the timing of catheter removal is a balance between avoiding infection by early removal and circumventing voiding dysfunction by later removal. Shorter catheterizations appear to reduce mean length of hospital stay. | |
|
Hakvoort 2004
RCT Netherlands February 2000 and July 2001 |
To determine whether prolonged urinary bladder catheterisation after vaginal prolapse surgery is advantageous. | Patients undergoing anterior colporrhaphy | Group A (45 patients): prolonged catheterization, removal on day 3 Group B (47 patients): not prolonged catheterization, removal in the morning post-OP |
A: 18 (40%) B: 2 (4%) OR = 14,786, 95% CI 3.187–68.595 | The disadvantages of prolonged catheterisation outweigh the advantages, therefore, removal of the catheter on the morning after surgery may be preferable and longer term catheterisation should only be undertaken where there are specific indications. | |
|
Iorio 2000 RCT USA 1993 to 1998 |
to determine which method minimized complications and maximized cost effectiveness. | patients undergoing unilateral total knee arthroplasty | Group A (306 patients):
preoperative insertion of an indwelling bladder catheter for 24 hours Group B (346 patients): catheter inserted postoperatively on an as needed basis only if symptoms of urinary retention developed |
B: 66% (229 of 346) of these patients required catheterization UTI: A: 5 (1.6%) B: 6 (1.7%) |
Routine preoperative insertion of a catheter into the urinary bladder may not be warranted in patients undergoing total knee arthroplasty. It is more cost effective to observe patients for urinary retention and then insert a catheter. If subsequent catheterization is necessary, intermittent straight catheterization should be considered to avoid urinary tract infections. | |
|
Sekhavat 2008 RCT Iran December 2002 to November 2004 |
To assess whether immediate removal of an indwelling catheter after anterior colporrhaphy influences the rate of re-catheterisation and symptomatic urinary tract infections | 90 women who underwent anterior colporrhaphy and aged between 40 and 50 years | A: removal immediately after surgery (n= 45) B: removal at least 24 h after OP (n=45) |
UTI (positive urine culture): A: 4,5% B: 15,5% P= 0,01 |
Early removal of an indwelling catheter immediately after anterior colporrhaphy was not associated with adverse events and increased rate of re-catheterisation. In this group, symptomatic urinary tract infection was significantly lower. Moreover, early removal of indwelling catheters immediately after operation seemed to decrease the ambulation time and hospital stay. | |
|
Weemhoff 2011 RCT, multicenter The Netherlands January 2006 and |
to compare the number of temporary catheter replacements and urinary tract infections after indwelling catheterization for 2 versus 5 days following an anterior colporrhaphy | 246 patients with a cystocele undergoing an anterior colporrhaphy | A: catheter for 2 days B: catheter for 5 days Any kind of urinary catheter |
A: 22% B: 37% OR 0.5 (CI 0.3-0.9, p = 0.02) |
Removal of an indwelling catheter after 2 versus 5 days following anterior colporrhaphy is associated with more temporary catheter replacements, but less urinary tract infections and a shorter hospital stay. | |
| September 2008 | ||||||
| Studies on type of catheter | ||||||
|
Baan 2003 RCT Netherlands |
to compare the risk of urinary tract infections and patient satisfaction among patients with suprapubic and transurethral catheters after laparotomy. | patients who underwent a major abdominal procedure, in particular for gastrointestinal diseases Removal of the catheter was allowed according to the general condition or when the epidural catheter was removed for at least 24 h to prevent urine retention. | Group A (75 patients): suprapubic catheters Group B (71 patients): transurethral catheters |
Urinary tract infection: A: 9/75 (12%) B: 8/71 (11%) (RR = 1.03; 95% CI = 0.64–1.67, p NS) |
The incidence of a urinary tract infection between a suprapubic catheter and a transurethral catheter in patients undergoing major surgery was not different. | |
|
Darouiche
2006
RCT, multicenter |
to assess the impact of using the StatLock securing device on symptomatic UTI | Adult patients with spinal cord injury who were diagnosed with neurogenic bladder and required a longterm indwelling transurethral or suprapubic bladder catheter | Group A (60 patients): indwelling bladder catheters secured in place by using the StatLock device Group B (58 patients): traditional methods that included tape, Velcro strap, Cath-Secure or none. |
UTI: A: 8 (13.3) B: 14 (24.1) (RR 0.55, 95% CI: 0.25-1.22, p NS). |
Although the trial size precluded the demonstration of statistically significant differences, the finding of a 45% reduction in the rate of symptomatic UTI in patients who received the StatLock securing device is clinically relevant | |
|
Dixon 2010 RCT UK |
To compare the use of intermittent urethral catheterization with indwelling suprapubic catheterization | women undergoing surgery for urodynamic stress incontinence or uterovaginal prolapse | Group A (38 patients): suprapubic catheter, 48 hours post-OP Group B (37 patients): urethral catheterization intermittently post-OP |
UTI: A: 9 B: 13 (p NS) |
The use of intermittent catheterization following urogynaecological surgery is associated with a more rapid return to normal micturition and a shorter hospital stay, although the clinical significance of the difference is perhaps limited. | |
|
Fernandez 2005 SR on RCT search date July 2004 |
to determine the effects of clamping short-term indwelling urethral catheters before removal on the incidence of urinary tract infection, time to first void, voiding dysfunction, incidence of recatheterization, and the length of hospital stay | clamping before removal of shortterm indwelling urethral catheters in people of all ages and in any setting (hospital, community, an nursing home) 3 trials included | 1 trial on CA-UTI: Group A: Removal of indwelling catheter within 24 hours after free drainage Group B: Removal of indwelling catheter within 72 hours after Group C: Removal of indwelling catheter within 24 hours + bladder reeducation |
no significant difference in the incidence of UTI (1 trial, 106 women): A: 3/37 (8%) B: 6/36 (17%) C: 3/33 (9%) |
The evidence for clamping indwelling urethral catheters before removal remains equivocal. Given the current state of evidence, procedures relating to clamping of indwelling urinary catheters should not be initiated. Until stronger evidence becomes available, however, practices relating to clamping indwelling urethral catheters will continue to be dictated by local preferences and cost factors. | |
|
Gong 2017 RCT China February 2012–April 2015 |
To determine the effect of clamping the indwelling urinary catheter before its removal on bladder reconditioning | adult patients with cervical cancer after radical hysterectomy | Group A (70 patients): indwelling urinary catheters clamped intermittently for 48 hours before removal Group B (128 patients): indwelling urinary catheters removed without clamping |
incidence of urinary tract infection: A: 22.9% B: 20.3% (p NS) |
Bladder recondition through indwelling urinary catheter clamping may not restore bladder function in patients after radical hysterectomy. | |
|
Hakvoorta 2011 RCT, multicenter Netherlands |
To compare clean intermittent catheterisation with transurethral indwelling catheterisation for the treatment of abnormal post-void residual bladder volume (PVR) following vaginal prolapse surgery. | patients older than
18 years experiencing
abnormal PVR
following vaginal prolapse surgery, with or without the use of mesh. Patients with a PVR of more than 150 ml after their first void were randomised |
Group A (45 patients): clean intermittent catheterisation (CIC) for 3 days Group B (45 patients): transurethral indwelling catheterisation (TIC) for 3 days All patients received prophylactic antibiotics during surgery. Catheter was removed on the first postoperative day. A 14 french silicone transurethral indwelling catheter and a vaginal gauze were inserted directly after surgery. |
UTI: A: 5 (12) B: 13 (33) (p= 0.03) |
Clean intermittent catheterisation is preferable over indwelling catheterisation for 3 days in the treatment of abnormal PVR following vaginal prolapse surgery. | |
|
Halleberg 2013 RCT with costeffectivenes s analysis Sweden September 2009 and May 2011 |
to investigate differences between intermittent and indwelling urinary catheterisation in hip surgery patients in relation to nosocomial UTI and costeffectiveness. | patients undergoing hip fracture surgery or hip replacement surgery that was due to osteoarthritis, aged >50
No antibiotic prophylaxis during surgery: A: 12 (14) B: 8 (10) |
Group A (89 patients): intermittent urinary catheterisation Group B (93 patients): indwelling urinary catheterisation Foley catheter (Charriere 14) was inserted, with aseptic technique, after preoperative antiseptic showering |
UTI: A: 8/85 (9.4) B: 10/85 (11.8) absolute difference 2.4 (-6.9 to 11.6%) |
Both indwelling and intermittent methods could be appropriate in clinical practice. Both methods have advantages and disadvantages but by not using routine indwelling catheterisation, unnecessary catheterisations might be avoided in this patient group. | |
|
Healy 2012 SR on RCT search date March 2012 |
to determine the benefits of suprapubic catheterization compared with urethral catheterization | women
undergoing gynecologic surgery 12 RCTs included |
Group A: suprapubic catheterization Group B: urethral catheterization |
UTI: OR 0.30 (0.18–0.51), favors suprapubic catheterization | Based on the best available evidence, no route for bladder drainage in gynecologic patients is clearly superior. The reduced rate of infective morbidity with suprapubic catheterization is offset by a higher rate of catheter-related complications and crucially does not translate into reduced hospital stay. As yet, there are insufficient data to determine which route is most appropriate for catheterization | |
|
Hunter 2013 Scoping review on all designs Search date May 2011 |
to examine research activity comparing suprapubic catheterization to any other method of chronic bladder emptying such as intermittent and indwelling catheterization | adults | A: Suprapubic catheters B : Urethral Catheters, other methods |
Despite varying definitions and the nonrandomized or retrospective research designs, the clinical evidence on UTI and long-term use of SP catheters provides some evidence of no difference between urethral and SP catheters. | Most studies focused on clinical urologic issues rather than patient understanding of suprapubic catheter management, satisfaction, stoma and skin care, or health related QoL. | |
| Kidd 2015 SR Cochrane of RCT search date January 2015 | To determine the advantages and disadvantages of alternative routes of short-term bladder catheterisation | adults requiring short-term urethral catheterisation in hospital for any reason 42 trials included | Group A: Suprapubic catheterisation
Group B: Indwelling urethral catheterisation we define 'short-term' as intended duration of catheterisation for 14 days or less, |
UTI: RR 1.01 (0.61 to 1.69) based on 575 patients (5 studies) | Suprapubic catheters reduced the number of participants with asymptomatic bacteriuria, recatheterisation and pain compared with indwelling urethral. The evidence for symptomatic urinary tract infection was inconclusive. For indwelling versus intermittent urethral catheterisation, the evidence was inconclusive for symptomatic urinary tract infection and asymptomatic bacteriuria. No trials reported pain. The evidence was inconclusive for suprapubic versus intermittent urethral catheterisation. Trials should use a standardised definition for symptomatic urinary tract infection. Further adequatelypowered trials comparing all catheters are required, particularly suprapubic and intermittent urethral catheterisation. | Niel-Weise 2005_Urinary Ist die Vorgänger Version des Reviews |
| Shepherd 2017 SR Cochrane RCTs and quasi-RCTs Search date May 2016 | To determine if certain washout regimens are better than others in terms of effectiveness, acceptability, complications, quality of life and critically appraise and summarise economic evidence for the management of longterm indwelling urinary catheterisation in adults. | adults (+ 16 years) in any setting with an indwelling urethral or suprapubic catheter for more than 28 days | comparing catheter washout policies (e.g. washout versus no washout, different washout solutions, frequency, duration, volume, concentration, method of administration) | Number of participants with symptomatic UTI: 1. RCT: 1.1. any washout versus no washout: 0.0 [0.0, 0.0] 1.2. saline washout versus no washout: 0.0 [0.0, 0.0] 1.3. citric acid washout versus no washout: 0.0 [0.0, 0.0] | Data from seven trials that compared different washout policies were limited, and generally, of poor methodological quality or were poorly reported. The evidence was not adequate to conclude if washouts were beneficial or harmful. Further rigorous, high quality trials that are adequately powered to detect benefits from washout being performed as opposed to no washout are needed. Trials comparing different washout solutions, washout volumes, and frequencies or timings are also needed. | The high risk of bias of the included studies resulted in the evidence being graded as low or very low quality. //no events were reported |
| Stekkinger 2011 RCT The Netherlands | To compare the effect of suprapubic and transurethral catheterization on postvoid residual volumes (PRVs) after cystocele repair | women who underwent pelvic organ prolapse surgery including cystocele repair | A: suprapubic catheter (n = 64) B: transurethral catheter (n = 62) | Urinary tract infections: A: 9,4% B: 9,7% P=0,93 | Suprapubic catheterization was comparable to transurethral catheterization in the prevention of postoperative voiding dysfunction after vaginal prolapse surgery, but it was associated with a higher rate of complications | |
| Van den Eijkel 2006 SR on RCTs Search date February 2006 | To assess the effects of catheter valves | Adults >16 yrs | A: catheter valve B: catheter bag drainage system | 2 RCTs (only one assessed UTIs: Wilson 1997) | No significant differences for UTIs in the comparison of catheter valve vs standard continuous drainage bag | |
| Wang 2016 SR on RCT Search date prior to May 2016 | to identify the necessity of bladder clamping prior to removal of urinary catheter in patients with short-term indwelling catheter. | Adult inpatient Indwelling urinary catheter up to 14 days | A: Regular clamp on urinary catheter and clamp off before removal B: Keeping the urinary catheter on free draining until removal | All studies on surgical patients. No significant difference between clamping and unclamping group was found (4 studies): OR 0.76, 95% CI (0.33, 1.73) | no significant difference was found between the clamping and unclamping groups in the outcomes of recatheterization, urinary retention, UTI and patients' subjective perceptions of voiding related symptoms. The limited evidence obtained from this review does not provide a robust base to overrule the existing guidelines. | |
| Zhang 2015 SR on RCTs/MA Search date January 2015 | to compare the rates of urinary tract infection (UTI) and postoperative urinary retention (POUR) in patients undergoing lower limb arthroplasty after either indwelling | patients undergoing total joint arthroplasty in the lower limbs | A: indwelling catheterization B: intermittent catheterization | 9 RCTs (on 1771 patients) no significant difference in the rate of UTIs (P>0.05): RR 1.23 (0.85-1.76), favours intermittent catheterization | indwelling urinary catheterization with removal 24 to 48 hours postoperatively did not increase the risk of UTI. | |
| urinary catheterization or intermittent urinary catheterization. | ||||||
| Studies on prophylaxis | ||||||
| Al-Habdan 2003 RCT Arabia | To assess whether catheter type can make a difference in infection rates | patients undergoing orthopedic and trauma surgery requiring post-OP indwelling catheters prophylactic antibiotics were used 30 min preOP and continued for 24 h post-OP | Group A (50 patients): antibiotic-impregnated catheters (nitrofuroxone Foley) Group B (50 patients): nonantibiotic-impregnated catheters (latex Foley) | Number of infections: A: 0 B: 6 (p=0.028) | Use of nitrofuroxone-impregnated cathetets was successful in reducing nosocomial UTIs, the impact of cost containment can be enormous. | |
| Beattie 2011 SR of SR and RCT search date March 2008 | to determine whether there was enough evidence to conclude that silveralloy urinary catheters reduce catheter-associated urinary tract infections compared with silicone or latex urinary catheters in adult inpatients. | short-term hospitalised adult patients with < 2 weeks catheter use | silver-alloy urinary catheters versus standard silicone or latex urinary catheters | primary studies included: 6 SR/MA, 5 RCT No study was able to clearly demonstrate that in short-term hospitalised adult patients, silver-alloy urinary catheters reduce CAUTI compared with standard silicone or latex urinary catheters. included studies with significant heterogeneity or poor-quality. | Owing to the poor quality of some individual studies included in other systematic reviews and the inability to carry out meta-analysis because of significant heterogeneity, definitive conclusions cannot be drawn from the study. | |
| Bonfill 2017 RCT, 14 hospitals, international November 2012 to December 2015 | to assess the efficacy of SAC urinary catheters for preventing catheterassociated urinary tract infections. | Patients with traumatic or medical spinal cord injury (SCI) requiring an indwelling urinary catheter for at least 7 days | Group A (243 patients): Antiseptic silver alloy-coated (SAC) silicone urinary catheters Group B (246 patients): silicone or silicone-latex catheters | UTI:
A: 18/243
B: 19/246
(OR 0.96, 95% CI 0.49–1.87, p NS)
Antibiotic prophylaxis and UTI:
yes: 6/184 no: 31/305 |
The results of this study do not support the routine use of indwelling antiseptic SAC silicone urinary catheters in patients with SCI. However, UTIs associated to longterm urinary catheter use remain a challenge and further investigations are still needed. | |
| Brosnahan 2004 Cochrane SR of RCT search date 2003 | Types of urethral catheters for management of short- term voiding problems in hospitalised adults | Hospitalised adults with an indwelling urethral catheter of short-term duration (less than or equal to fourteen days duration, or other temporary shortterm use as defined by the trialists). | 17 included involving 4237 adults plus one large cluster-
randomised cross-over trial on 27,878 adults.
antiseptic impregnated catheters vs standard catheters (n=11 trials), antibiotic impregnated catheters vs standard catheters (n=1 trial) comparison of different standard catheters (n=6 trials). The antiseptic catheters were either impregnated with silver oxide or silver alloy. |
UTI for ANTISEPTIC CATHETER VERSUS STANDARD CATHETER: RR 0.60 [0.50, 0.73], I2 =49%, based on 7 trials, favours antiseptic alloy UTI for ANTIBIOTIC-IMPREGNATED CATHETER (minocycline + rifampicin) VERSUS STANDARD CATHETER (silicone): RR 0.20 [0.03, 1.63], 1 trial | the use of silver alloy indwelling catheters for catheterising hospitalised adults shortterm reduces the risk of catheter acquired urinary tract infection. Further economic evaluation is required to confirm that the reduction of infection compensates for the increased cost of silver alloy catheters. | |
| Cao 2018 SR and Network MA of RCT search date December 2017 | prevention of CAUTIs through a network metaanalysis of the relevant literature based on the Bayesian method. | Hospitalized patients (>18 years) with indwelling urinary catheters (IDCs) | Group A: an antiseptic such as iodine, chlorhexidine, nitrofurazone, etc. was used to clean the meatal, peri-urethral, or perineal areas before IDC insertion or intermittent catheterization, or during routine meatal care Group B: metal area was cleaned with non-medicated agents such as sterile water, tap water, saline, etc. | 33 trials (6490 patients) with 7 different methods of urethral cleaning versus disinfection were eligible for inclusion no heterogeneity among studies observed no difference in the incidence of CAUTIs when comparing the different urethral cleaning methods versus disinfection (P > 0.05 for all). However, chlorhexidine ranked first in the results of the Bayesian analysis and is recommended for preventing CAUTIs. | Current evidence suggests that there are no significant differences among different urethral cleaning versus disinfection methods with regard to CAUTI incidence rates. | |
| Cardenas 2011 RCT, 15 centers US and Canada April 2006 and July 2009 | To investigate whether intermittent catheterization (IC) with a hydrophiliccoated catheter delays the onset of the first symptomatic urinary tract infection (UTI) and reduces the number of symptomatic UTIs in patients with acute spinal cord injury (SCI) compared with IC with standard, uncoated catheters. | with traumatic SCI of less than 3 months' duration who use intermittent catheterization (IC) The study duration consisted of 2 periods: an institutional period (in acute care or a rehabilitation unit) and a community period (after discharge from the hospital or rehabilitation unit). | Group A (108 patients): catheter (SpeediCath) was a sterile, ready-to-use, hydrophiliccoated, polyurethane Nelaton catheter. The coating consists primarily of polyvinyl-pyrrolidone Group B (116 patients): catheter (Conveen) was a sterile, uncoated, PVC Nelaton catheter | UTIs/ mo*: Group A: 0.479 (99/206.7) Group B: 0.478 (167/349.2) (p NS) | The use of a hydrophilic-coated catheter for IC is associated with a delay in the onset of the first antibiotic-treated symptomatic UTI and with a reduction in the incidence of symptomatic UTI in patients with acute SCI during the acute inpatient rehabilitation. Using a hydrophilic-coated catheter could minimize UTI-related complications, treatment costs, and rehabilitation delays in this group of patients, and reduce the emergence of antibiotic-resistant organisms. | *UTI/mo is a ratio of the total number of UTIs in the group divided by the total number of months in the period in the study group. |
| Cheung 2008 RCT Hong Kong | to compare the risk of acquiring symptomatic UTIs through the conventional practice of using 0.05% chlorhexidine gluconate versus sterile water for periurethral cleansing before insertion of a urinary catheter. | adults receiving community nursing services, requiring long-term indwelling urinary catheter | Group A (12 patients): 0.05% chlorhexidine gluconate Group B (8 patients): sterile water Latex catheters were used in this study. | none of the subjects in the 2 groups developed symptomatic bacteriuria | Using sterile water to clean the periurethral area before catheterization among home care patients will not increase the risk for urinary tract infections. | |
| Chung 2012 RCT Taiwan | to evaluate the effect of rice vinegar administered via nasogastric feeding tube on catheterassociated bacteriuria in patients with longterm urinary catheterization | adult patients from a long-term care facility | Group A (30 patients): vinegar, 100 ml of diluted rice vinegar each day for 4 weeks Group B (30 patients): usual care two-way latex Foley catheter for more than 30 days | UTI: A: 0/25 B: 3/19 | Medicinal use of vinegar may decrease the risk of symptomatic UTI, but further study is needed to determine the effects of ingesting vinegar for a longer period and with a larger sample size. | |
| Dieter 2014 RCT USA August 2011 through February 2013 | To evaluate whether nitrofurantoin prophylaxis prevents postoperative urinary tract infection (UTI) in patients receiving transurethral catheterization after pelvic reconstructive surgery. | participants undergoing pelvic reconstructive surgery | Group A (81 patients): 100 mg nitrofurantoin once daily during catheterization Group B (78 patients): placebo once daily during catheterization | UTI within 3 weeks of surgery: A: 22% B:13% (RR 1.73, 95% CI 0.85–3.52, p NS) | Prophylaxis with daily nitrofurantoin during catheterization does not reduce the risk of postoperative UTI in patients receiving short-term transurethral catheterization after pelvic reconstructive surgery. | |
| Fasugba 2017 SR on RCT search date December 2015 | to assess the effectiveness on antiseptic cleaning before urinary catheter insertion and during catheter use for CAUTI prevention | 14 studies included patients requiring short or long term IDC or intermittent catheterisation in hospital, community settings and long term care facilities | Group A: antiseptic catheter Group B: non-antiseptic catheter | CAUTI: A vs B: OR 0.90 (95% CI 0.73-1.10, p NS) | no benefits of using antiseptic over nonantiseptic for metal cleaning for CAUTI prevention | |
| Foxmann 2015 RCT USA August 2011 and January 2013 | to assess the efficacy of cranberry juice capsules in preventing UTI post surgery. | Women with elective gynecologic surgery | Group A: cranberry capsules two times a day, for 6 weeks post-OP
Group B: placebo
urinary catheter insertion (as per hospital protocol) prophylactic antibiotics pre-OP |
The occurrence of UTI was significantly lower in the cranberry treatment group compared to the placebo group (15/80 (19%) versus 30/80 (38%); OR=0.38; 95% CI: 0.19, 0.79; p=0.008) OR=0.42; 95% CI: 0.18, 0.94 [adjusted] | Among women undergoing elective benign gynecologic surgery involving urinary catheterization, use of cranberry extract tablets during the postoperative period reduced the rate of UTI by half | |
| Gunnarsso n 2017 RCT Sweden July 2009 and June 2013 | to investigate whether intake of cranberry juice concentrate preoperatively decreases the incidence of postoperative UTIs in hip fracture patients that received a urinary catheter. | Female patients, aged 60 years and older, with hip fracture | Group A: two capsules of 550 mg of cranberry powder t.i.d. until 5 days postoperatively. Group B: two capsules of placebo t.i.d. until 5 days postoperatively. | The proportion of patients with positive culture at either day 5 or day 14 postoperatively where 19 of 50 (38%) and 23 of 61 (38%) (p=0.975, RR 0.988, 95% CI 0.457– 2.135) | Cranberry concentrate does not seem to effectively prevent UTIs in female patients with hip fracture and indwelling urinary catheter. | |
| Jahn 2012 SR Cochrane of RCT search date March 2011 | to determine which type of indwelling urinary catheter is best to use for long-term bladder drainage in adults. | Adults with indwelling urethral or suprapubic catheters for more than 30 days, irrespective ofprimary disease and care setting. Three trials were included, involving 102 adults in various settings. | Group A: Silicone catheter Group B: Silver alloyed catheter | UTI:
RR 1 (0.83 to 1.2) based on 20 patients (1 study) |
Very few trials have compared different types of catheter for long-term bladder drainage. All trials were small and showed methodological weaknesses. Therefore, the evidence was not sufficient as a reliable basis for practical conclusions. Further, better quality trials are needed to address the current lack of evidence in this clinically important area | |
| Johnson 2006 SR on RCT | To assess currently marketed antimicrobial urinary catheters for preventing catheterassociated UTI | 12 trials were included (on 13392 patients) | catheters included: silver hydrogel–coated latex, silver hydrogel–coated silicone, silver Foley catheter (silver hydrogel silicone), nitrofurazonecoated silicone | They compared nitrofurazone-coated silicone (n = 3) or silver-coated latex (n = 9) catheters with silicone or latex catheters. No study addressed symptomatic UTI. | According to fair-quality evidence, antimicrobial urinary catheters can prevent bacteriuria in hospitalized patients during short-term catheterization, depending on antimicrobial coating and several other variables. Older data probably lack current relevance. Cost implications and effect on infectious complications remain undefined. | |
| Karchmer 2000 RCT, crossover USA November 1996 to November 1997 | To assess the efficacy of a silver-alloy, hydrogel-coated latex urinary catheter for the prevention of nosocomial catheterassociated UTIs. | hospitalized patients | Group A: silver-alloy, hydrogelcoated latex Foley catheters Group B: silicone-coated (uncoated) latex catheters 1-month washout period during which all wards were stocked with uncoated catheters. In the second 6 months of the study, group 1 wards used uncoated catheters and group 2 wards had silvercoated catheters. | infection per 1000 patient-days: RR 0.79 (95% CI, 0.63-0.99; P=.04) for study wards randomized to silver-coated catheters compared with those randomized to uncoated catheters. RR per 100 silver-coated catheters used on study wards compared with uncoated catheters was 0.68 (95% CI, 0.54-0.86; P=.001). | The risk of infection declined by 21% among study wards randomized to silvercoated catheters and by 32% among patients in whom silver-coated catheters were used on the wards. Use of the more expensive silver-coated catheter appeared to offer cost savings by preventing excess hospital costs from nosocomial UTI associated with catheter use. | |
| Lam 2014 SR Cochrane on RCT | to compare the effectiveness of different types of indwelling urethral catheters in reducing the risk ofUTI and to assess their impact on other outcomes in adults who require short-term urethral catheterisation in hospitals. | hospitalized patients 26 trials included (12,422 patients) |
A: Antiseptic-coated indwelling urethral catheters versus standard indwelling urethral catheters B: Antimicrobial-impregnated indwelling urethral catheters versus standard indwelling urethral catheters C: Antimicrobial-impregnated indwelling urethral catheters versus antiseptic-coated indwelling urethral catheters D: One type of standard indwelling urethral catheter versus another type of standard indwelling urethral catheter | CAUTI: A: RR 0.99, 95% CI 0.85 to 1.16 B: RR0.84, 95%CI 0.71 to 0.99 C: RR 0.84, 95% CI 0.71 to 1.00 D: None of the trials comparing standard catheters versus other types of standard catheters measured symptomatic CAUTI. | Silver alloy-coated catheters were not associated with a statistically significant reduction in symptomatic CAUTI, and are considerably more expensive. Nitrofurazone-impregnated catheters reduced the risk of symptomatic CAUTI and bacteriuria, although the magnitude of reduction was low and hence may not be clinically important. However, they are more expensive than standard catheters. They are also more likely to cause discomfort than standard catheters. | |
| Lusardi 2013 SR Cochrane on RCT | To determine if certain antibiotic prophylaxes are better than others in terms of prevention of urinary tract infections, complications, quality of life and costeffectiveness in shortterm catheterisation in adults. | All adults requiring short-term urinary urethral and supra-pubic catheterisation (up to and including 14 days) in hospital 6 RCT on 789 participants included | The interventions considered were: 1. antibiotic prophylaxis versus no prophylaxis; 2. antibiotic prophylaxis with antibiotic A versus giving antibiotic prophylaxis with antibiotic B; 3. antibiotic prophylaxis at catheterisation only versus antibiotic prophylaxis throughout the catheterisation period. In addition, the route of administration (oral or intravenous, but not topical) was considered. | Antibiotic prophylaxis versus no prophylaxis: UTI: RR 0.20 [0.06, 0.66] (based on 1 trial and 90 patients) | The limited evidence indicated that receiving prophylactic antibiotics reduced the rate of bacteriuria and other signs of infection, such as pyuria, febrile morbidity and gram-negative isolates in patients' urine, in surgical patients who undergo bladder drainage for at least 24 hours postoperatively. There was also limited evidence that prophylactic antibiotics reduced bacteriuria in non-surgical patients. | |
| Marschall 2013 SR and MA RCT and non-RCT | to clarify whether antibiotic prophylaxis at the time of urinary catheter removal confers a benefit in terms of preventing subsequent symptomatic urinary tract infections. | Search date November 2012 All adults requiring short-term urinary urethral and supra-pubic catheterisation (up to and including 14 days) in hospital | A: antibiotic prophylaxis B: no prophylaxis | 6 RCTs and 1 non-randomized controlled intervention study. Studies were heterogeneous in the type and duration of antimicrobial prophylaxis and the period of observation. antibiotic prophylaxis was associated with benefit to the patient (absolute reduction in risk of urinary tract infection 5.8% (RR 0.45 (95% CI 0.28 to 0.72). number needed to treat to prevent one urinary tract infection was 17 (CI 12 to 30). | Patients admitted to hospital who undergo short term urinary catheterization might benefit from antimicrobial prophylaxis when the catheter is removed as they experience fewer subsequent urinary tract infections. Potential disadvantages of more widespread antimicrobial prophylaxis (side effects and cost of antibiotics, development of antimicrobial resistance) might be mitigated by the identification of which patients are most likely to benefit from this approach. | |
| Niel-Weise 2005_Antibt iotic SR Cochrane of RCT and quasi-RCT | To determine if certain antibiotic policies are better than others in terms of prevention of urinary tract infections, complications, quality of life and costeffectiveness in shortterm catheterised adults. | All adults requiring short-term urethral catheterization (up to and including 14 days) in hospital for urine monitoring, investigations, acute retention problems, acute incontinence problems and after surgery. | The interventions considered were: antibiotic prophylaxis (continuous use), use of antibiotics if clinically indicated (e.g. pain, fever) and use of antibiotics if microbiologically indicated (growth of bacteria from a specimen of urine in the absence of clinical symptoms, density of bacteria taken as positive as defined by the trialists). the route of administration (oral or intravenous, but not topical) was considered. | symptomatic urinary tract infection (1 trial): less common in the prophylaxis group (RR 0.20, 95% CI 0.06 to 0.66) | There was weak evidence that antibiotic prophylaxis compared to giving antibiotics when clinically indicated reduced the rate of symptomatic urinary tract infection in female patients with abdominal surgery and a urethral catheter for 24 hours. The limited evidence indicated that receiving antibiotics during the first three postoperative days or from postoperative day two until catheter removal reduced the rate of bacteriuria and other signs of infection such as pyuria and gramnegative isolates in patients urine in surgical patients with bladder drainage for at least 24 hours postoperatively. There was also limited evidence that prophylactic antibiotics reduced bacteriuria in nonsurgical patients. | |
| Pfefferkorn 2009 RCT Switzerland | To assess whether antibiotic prophylaxis at urinary catheter removal reduces the rate of urinary tract infections | patients undergoing elective abdominal surgery | A: With antibiotic prophylaxis (3 doses of trimethoprimsulfamethoxazole at urinary catheter removal) (n =103) B: without antibiotic prophylasis (n= 102) | Symptomatic urinary tract infection: A: 4,9% B: 21,6% (p= < 0.001) | Antibiotic prophylaxis with trimethoprimsulfamethoxazole on urinary catheter removal significantly reduces the rate of symptomatic urinary tract infections and bacteriuria in patients undergoing abdominal surgery with perioperative transurethral urinary catheters. | |
| Pickard 2012 RCT, multicenter, with economic analysis UK | Do antimicrobial catheters reduce the rate of symptomatic urinary tract infection (UTI) during short-term hospital use and is their use cost-effective for the UK NHS? | Adults (≥ 16 years of age) requiring urethral catheterisation (which was expected to be required for a maximum of 14 days), from selected hospital wards with a high volume of shortterm catheterisation. | A: nitrofurazone-impregnated silicone urethral catheter (n = 2153) B: silver alloy-coated latex hydrogel urethral catheter (n = 2097) C polytetrafluoroethylene (PTFE) coated catheter (control group) (n = 2144) | symptomatic antibiotic-treated UTI within 6 weeks of randomization:
Nitrofurazone vs PTFE:
OR 0.81 (0.65 to 1.01); p=0.031 Silver alloy vs PTFE: OR 0.96 (0.78 to 1.19); p=0.69 |
The trial estimate of clinical effectiveness for nitrofurazone-impregnated catheters was less than the pre-specified minimum absolute risk difference that we considered important (-3.3%), and the surrounding CI included zero, indicating that any reduction in catheter-associated UTI was uncertain. Economic analysis, although associated with uncertainty, suggested that nitrofurazone-impregnated catheters may be cost-effective for the NHS. The trial ruled out the possibility that silver alloycoated catheters might reach the pre-set degree of clinical effectiveness and that their use was unlikely to be cost-effective. | |
| Reiche 2000 RCT Denmark | To test the effect on urinary tract infections (UTIs) in patients needing continuous indwelling catheterization, of a newly designed urinecollecting system containing an antibacterial device which slowly releases silver ions onto the inner surface of the system. | 213 adult patients newly catheterized | A: active AB system containing a silver-releasing sodium-calcium phosphate ingot (n=83) B: control (n=87) They were randomized to a urine drainage system (comprising a Unometer 400 metering system or PP 2000N closed urine-bag system, both from Maersk Medical, Denmark) either with or without the antibacterial device | There were fewer UTIs in those using the system containing the antibacterial device (19% vs 24%) HR (the probability of having a UTI using an AB bag compared with a control bag) 0.68 (95% CI 0.33±1.28) | The potential importance of different infection routes were highlighted, suggesting that modifications to Foley catheters and urine-collecting systems attempting to prevent UTIs should focus not only on the intraluminal pathway, but on the internal and external pathways of infection. | |
| Rogers 2004 RCT, multicenter USA | to determine if antibiotic prophylaxis with nitrofurantoin monohydrate macrocrystals (study drug) after pelvic organ prolapse and/or urinary incontinence surgery with suprapubic catheterization (SPC) decreases urinary tract infection (UTI) compared with placebo in a randomized, double- blind, multicenter trial | patients undergoing surgical correction of stress urinary incontinence and/or pelvic organ prolapse |
A: antibiotic prophylaxis with nitrofurantoin (n = 211) Placebo (n = 224) suprapubic catheters |
Antibiotic prophylaxis decreased symptomatic UTI at suprapubic catheters removal (7.2% vs 19.8%, p= 0.001) | Antibiotic prophylaxis with nitrofurantoin monohydrate macrocrystals decreases UTI compared with placebo after pelvic organ prolapse and/or urinary incontinence surgery with suprapubic catheterization. | |
| Stenzilius 2011 RCT Sweden | to compare the incidence of catheterassociated bacteriuria with a noble metal alloy-coated latex catheter or a noncoated silicone catheter in patients undergoing elective orthopaedic surgery with short-term catheterization | adult patients undergoing elective orthopaedic surgery | A: Noble metal alloy-coated latex (n=222) B: silicone Foley catheter (n=217) For both catheter types the size 12 Ch (Charriére) was used | catheter-associated urinary tract symptoms A: 22.1 B: 22.9 P= 0.849 | This study confirmed previous results that the noble metal alloy coating significantly reduces the risk of catheter-associated bacteriuria in short-term catheterization (1- 3 days). Female gender and obesity were significant risk factors for developing bacteriuria, while the use of an open drainage system and insertion of the catheter on the ward were not. owing to the limited numbers the results should be interpreted with caution. | |
| Van Hees 2011 RCT The Netherlands January 2005 until December 2006 | we investigated the effects of a singledose antibiotic regimen, before removing urinary catheters, on the occurrence of significant bacteriuria (SBU) and UTI. | Patients scheduled to undergo major surgery, such as an abdominal operation or hip surgery | A: ciprofloxacin (500 mg)) (n = 43) B: co-trimoxazole (960 mg) (n= 46) C: placebo (n = 51) Antibiotic therapy was administered 2 hours before catheter removal | Symptomatic UTI A: 1/31 (3%) B: 0/24 (0%) C: 1/36 (3%) | our results do not support antibiotic prophylaxis for urinary catheter removal in non-genitourinary surgical patients. | |
| Wazait 2004 RCT UK | to assess if a short course of ciprofloxacin starting at the time of catheter removal reduced the UTI rate after removal. | Patients across specialities with a urethral catheter in situ for ≥ 48 h and ≤ 7 days | A: 48-h course of ciprofloxacin starting 2 h before catheter removal (= 25) B: placebo (n=23) FU was at 7 and 14 days | A: 2 patients had a UTI at the time of catheter removal; both infections was sensitive to ciprofloxacin. Four patients (16%) had a UTI after catheter removal and two of these were symptomatic (8%). | The risk of UTI (both symptomatic and asymptomatic) after removing a urethral catheter is real, even in absence of catheter associated UTI before removal. UTIs occurring after removing a short-term urinary catheter had a high rate of resistance to ciprofloxacin. There was no detectable significant benefit in using prophylactic ciprofloxacin to reduce the UTI rate after catheter removal. | |
| Studies on education programs | ||||||
| Chen 2013 RCT Taiwan April through November 2008 | to evaluate the outcomes of the use of the criteria-based reminder system on the removal of indwelling catheters | patients from 2 respiratory intensive care units with indwelling urinary catheter | Group A (147 patients): use removal criteria Group B (131 patients): Without use of removal criteria | CAUTI: B: 34 (26) A: 20 (14) RR 0.52 ((0.32-0.86), p<0.01) | Use of a criteria-based reminder to remove indwelling urinary catheters can diminish the use of urinary catheterization and reduce the likelihood of catheterassociated urinary infections. | |
| Durant 2017 SR on casecontrol studies | to evaluate nursedriven protocols (NDP) and the prevention of catheter-associated urinary tract infections | 29 studies included studies were conducted primarily in intensive care units and several in academic hospitals | Group A: NDP Group B: prior practice | Several studies reported a reduction in the number of CAUTIs and CAUTI rate | NDPs appear to have a positive impact on the clinical predictors and prevalence of CAUTI; need for improving the study design of quality | |
| Gould 2017 SR on RCT and nonRCT | to help develop an intervention to improve catheter management and reduce CAUTI specifically in the nursing home environment where implementation of infection prevention guidelines is reported to be more challenging than in hospitals | people in nursing homes or longterm care facilities 8 studies included | Implementation of clinical guidelines | Three studies evaluated the impact of implementing a complete clinical guideline. Five additional studies evaluated the impact of implementing individual elements of a clinical guideline. [For detailed CAUTI results of primary studies see Table 2] | There is a need to ensure that evidencebased clinical guidelines to prevent CAUTI in residents catheterized long term are implemented in nursing homes. Before this work can be undertaken, feasibility studies are required to establish what can be achieved in these settings. | |
| Lee 2015 RCT Taiwan | to evaluate the effects of a nurse–family partnership model on the self-efficacy of family caregivers (FCs) and the incidence of CAUTI | patients with an indwelling urinary catheter | Group A (40 patients): nurse attended a 4 h training course Group B (41 patients): routine nursing care | CAUTI: A: 6 (20%) B: 12 (38.8%) (p NS) | Our study considered caregivers as partners in caring for patients with indwelling catheters, and we examined an intervention to enhance the self-efficacy of FCs in urinary catheter-associated care to reduce the occurrence of CAUTIs. The results showed that the effects of the intervention did not differ statistically. The self-efficacy of caregivers and the occurrence of CAUTIs in patients in the two groups were statistically equivalent. | |
| Loeb 2008 RCT Canada January 2004 to June 2006 | To assess whether stop orders for indwelling urinary catheters reduces the duration of inappropriate urinary catheterization and the incidence of urinary tract infections. | hospitalized patients admitted to hospital with indwelling urinary catheters inserted for ≤ 48 h. | Group A (347 patients): Stop order group Group B (345 patients): usual care group | A: 51 (19%)/269 B: 51 (20%)/252 RR 0.94, (95% CI, 0.66 to 1.33, p NS) | Stop orders for urinary catheterization safely reduced duration of inappropriate urinary catheterization in hospitalized patients but did not reduce urinary tract infections. | |
| Meddings 2010 SR and MA on intervention al studies (trials and pre-/post-) Search date August 2008 | to evaluate the effect of interventions that remind clinicians of the presence of urinary catheters to prompt the timely removal of catheters during hospitalization. | catheter removal in hospitalized adults 14 studies included | intervention that functioned to remind physicians or nurses to remove unnecessary urinary catheters Any urinary catheter | The rate of CAUTI (episodes per 1000 catheter-days) was reduced by 52% (P < 0.001) with use of a reminder or stop order (7 studies included in ma): RR 0.48 (0.28-0.68) | Urinary catheter reminders and stop orders appear to reduce the rate of CAUTI and should be strongly considered to enhance the safety of hospitalized patients. | Intervention details varied among studies |
| Meddings 2017 SR on comparison studies Search date June 2015 | To identify strategies to reduce UTIs in nursing home residents. | nursing home residents 20 records describing 19 interventions were included: 8 randomized controlled trials, 10 pre-post nonrandomized interventions, and 1 nonrandomized intervention with concurrent controls. | urinary catheter use such as improving appropriate use, aseptic placement, maintenance care, and prompting removal of unnecessary catheters, single and multiple interventions | The 19 studies reported 12 UTI outcomes, 9 CAUTI outcomes, 4 bacteriuria outcomes, and 5 catheter use outcomes. Five studies showed CAUTI reduction (1 significantly); 9 studies showed UTI reduction (none significantly); 2 studies showed bacteriuria reduction (none significantly). Four studies showed reduced catheter use (1 significantly). | Several practices, often implemented in bundles, such as improving hand hygiene, reducing and improving catheter use, managing incontinence without catheters, and enhanced barrier precautions, appear to reduce UTI or CAUTI in nursing home residents. | Studies were often underpowered to assess statistical significance; none were pooled given variety of interventions and outcomes. The outcome definitions of UTI and CAUTI varied widely: some using definitions specific for nursing home settings such as McGeer's criteria, other reported symptomatic CAUTIs per 1000 catheter-days, others reported symptomatic CAUTIS per 1000 resident-days, others reported symptomatic CAUTIs as counts, or CAUTIs as part of a combined outcome (ie, bacteriuria, CAUTI, or death). |
| Mody 2015 RCT USA May 2010 to April 2013 | To test whether a multimodal targeted infection program reduces the prevalence of multidrug-resistant organisms and incident device-related infections. | high-risk nursing home residents with urinary catheters, feeding tubes, or both (n=418) | A: intervention: Multimodal, including preemptive barrier precautions, active surveillance for multidrug-resistant organisms and infections, and nursing home staff education. B: control | Urinary catheter: A: 59,1 % B: 32,6 % First New CAUTI, All (n = 166 Residents): HR 0.54 (0.30-0.97) All New CAUTI, Includes Recurrent Infection (n = 166 Residents): HR 0.69 (95% CI, 0.49-0.99) | Our multimodal targeted infection program intervention reduced the overall multidrugresistant organisms (MDRO) prevalence density, new methicillin-resistant S aureus acquisitions, and clinically defined catheter-associated urinary tract infection rates in high-risk NH residents with indwelling devices. | subgroup of urinary catheter population included |
| Wilde 2015 RCT USA | to determine effectiveness of a selfmanagement intervention in prevention of adverse outcomes | 202 adult longterm urinary catheter users | A: learning catheter-related selfmonitoring and self- management skills during home visits by a study nurse B: usual care Us of urethral and suprapubic catheters | CAUTI at 12 months: Rate group A: 4,89 (4.12-5.75) Rate group B: 4.12 (3.42-4.91) | A simple-to-use catheter problems calendar and the bimonthly interviews might have functioned as a modest selfmonitoring intervention for persons in both groups. A simplified intervention using a self-monitoring calendar is suggested-with optimal and consistent fluid intake likely to add value. | |
| Catheter vs. no catheter | ||||||
| Li 2011 SR on RCT and abservation als | To assess whether it is necessary to place indwelling urinary catheters routinely in caesarean section, and to determine the effects of this procedure on UTIs, urinary retention, intraoperative difficulties, operative complications, as well as other outcomes. | Three trials (two RCTs and one NRCT) were included (based on 084 participants) | A: Routine catheterisation with indwelling catheter before surgery: the catheterised group (CG). B: No catheterisation before surgery and catheterised only when indicated: the uncatheterised group (UG). | Compared with the use of indwelling urinary catheters, nonuse had a significantly lower incidence: UTIs: [RR 0.08; 95% CI 0.01, 0.64 (study design: RCT); RR 0.10; 95% CI 0.02, 0.57 (study design: NRCT)] | The nonuse of indwelling urinary catheters in caesarean section is associated with less UTIs and no increase in either urinary retention or intra-operative difficulties. Our results suggest that the routine use of indwelling urinary catheters for caesarean delivery in haemodynamically stable patients is not necessary, and can be harmful. However, better and larger randomised trials are needed to confirm these findings. | |
| Nasr 2009 RCT, multicenter Egypt | To prospectively investigate the effects on urinary tract infection (UTI) of indwelling urinary catheter placement during cesarean delivery | Female patients during caesarian delivery | A: Uncatheterized (study) group (n=210) B: Catheterized (control) group (n=210) | the incidence of UTI was significantly greater in the catherization group (P<0.001) | Non-placement of indwelling urinary catheter during cesarean was more convenient to women with no increase in intraoperative complications, or urinary retention. Indwelling catheter placement in hemodynamically stable patients proved not to be beneficial in this study. | Symptoms of UTI are assessed and presented separately (Urinary pain, Burning on urination, Frequency, Urgency, Hematuria (dipstick), Urine nitrate (dipstick) |
| Mixed assessments: | ||||||
| Cooper 2016 SR Cochrane of RCT Search date May 2016 | To determine the effectiveness of different policies for replacing long-term indwelling urinary catheters in adults. | Adults with longterm (> 14 days) indwelling urinary or suprapubic catheters that are anticipated to require replacement. 3 RCTs included (based on 107 patients) | The following types of interventions were compared with each other: 1. One interval versus another interval between catheter replacement 2. Antibiotic prophylaxis versus no prophylaxis at the time of catheter replacement 3. Replacing catheter versus other policy e.g. washouts 4. Replacing in home environment versus clinical environment 5. Clean versus aseptic technique for replacing catheter 6. Cleaning solution A versus cleaning solution B 7. Lubricant A versus lubricant B or no lubricant 8. Catheter users versus carer versus health professional performing the catheter replacement procedure | lower incidence of symptomatic UTI in people whose catheter was changed both monthly and when clinically indicated vs to only when clinically indicated (1 study): RR 0.35, 95%CI 0.13 to 0.95 | There is currently insufficient evidence to assess the value of different policies for replacing long-term urinary catheters on patient outcomes. In particular, there are a number of policies for which there are currently no trial data; and a number of important outcomes which have not been assessed, including patient satisfaction, quality of life, urinary tract trauma, and economic outcomes. | All the included trials were small and underpowered |
| Ercole 2013 integrative review of SR and RCT Search date Nov 2010 | to seek the best evidence available in the literature concerning the knowledge produced and related to the techniques of intermittent and indwelling urinary catheterization | 28 RCT included, 9 SR | different catheters, different removal policies | the infection rate in the urinary tract does not alter whether the perineum is cleaned with sterile water or not, or with the use of povidone-iodine solution or chlorhexidine; or using clean or sterile technique. The use of an intermittent catheter with clean technique results in low rates of complications or infections compared to the use of an indwelling catheter. The removal of the catheter in up to 24 hours after surgery and the use of an antimicrobial-impregnated or hydrophiliccoated catheter reduce urinary tract infection. | there are controversies in relation to periurethral cleansing technique, the type of material the catheter is made of, and some procedures for the maintenance and removal of the catheter. | |
| Kringel 2010 RCT, 3 arm Germany | we analyzed different protocols of postoperative drainage | Patients with an indicated anterior colporrhaphy plus an optional further procedure (i.e., hysterectomy) | Group A (100 patients): urinary catheter for 24 h Group B (100 patients): urinary catheter for 96 h Group C (32 patients): suprapubic urinary catheter for 96 h | UTI: A: 2 B: 6 C: 0 (p=0.155) | The optimal bladder catheter after anterior colporrhaphy was, in our trial, the IUC for 24 h. | |
| Leone 2004 SR on trials Search date 2002 | prevention and management of CAUTI in patients hospitalized in ICU. | 24 trials included The absence of data pertaining to ICU patients led us to include studies involving surgical and/or medical patients | different catheters | There is no consensus on the use of urinary reagent tests for diagnosis. The prevention of CAUTI in ICU patients does not require expensive devices. Neither complex closed drainage systems nor silver-coated urinary catheters have demonstrated efficacy in comparative randomized clinical trials. | The lack of data on CAUTI in ICU patients leads physicians to manage them empirically according to author opinions and personal beliefs. | |
| Liang 2009 RCT, 3 arm Taiwan July 2007 to January 2008 | to assess the impact of bladder catheterization on the incidence of postoperative urinary tract infection (UTI) and urinary retention (PUR) following laparoscopic-assisted vaginal hysterectomy (LAVH) | patients with benign gynecologic disease scheduled for inpatient LAVH | Group A (50 patients): no catheter use Group B (50 patients): indwelling bladder catheter use for 1 day Group 3 (50 patients): indwelling bladder-catheter-use for 2 days | UTI: A: 2 (4) B: 3 (6) C: 9 (18) (p= 0.034) | although the incidence of catheter associated UTI following LAVH was confounded by the use of prophylactic antibiotics in our study, the data suggest that the duration of catheterization was the most important predictor for postoperative adverse urinary events. Short term indwelling catheterization increased the incidence of UTI, but decreased the incidence of PUR among patients undergoing LAVH. | |
| Phipps 2006 SR Cochrane of RCT and quasi-RCT | To establish the optimal way to manage urinary catheters following urogenital surgery in adults | All adults undergoing urogenital surgery. | Any catheter intervention: • urinary catheterisation, by urethral, suprapubic or both routes; • use of PVC, silicone or latex catheters; • use of 2-way or 3-way catheters, all sizes; • use of bladder irrigation and/or wash-out; • use of antibiotic policies regarding catheter manipulation; • use of policies regarding postoperative timing of catheter removal; • use of policies regarding time of day of catheter removal; • use of policies regarding bladder filling prior to catheter removal; • use of clamping of catheter prior to removal; • use of post void residual volume measurement prior to suprapubic catheter removal; • use of policies for assessment following catheter removal. | Urinary tract infection: USING A URINARY CATHETER VS NOT USING A URINARY CATHETER (4 studies): RR 1.35 [0.75, 2.45] (Favours no catheter) URETHRAL CATHETERISATION VS SUPRAPUBIC CATHETERISATION (4 studies): RR 1.16 [0.54, 2.48] (Favours suprapubic) COMPARISON TYPES OF CATHETER: Urethral foley catheter with extra drainage hole VS unmodified foley catheter (1 study): RR 0.40 [0.15, 1.04] (favours foley c.) ONE TYPE OF CATHETERMANAGEMENT IS BETTERTHAN ANOTHER (1 study each): Vaginal cleansing before catheter insertion vs vaginal cleansing after catheter insertion: RR 0.61 [0.33, 1.14] Cefotaxime 1hr prior to catheter removal (versus none: RR 0.08 [0.00, 1.30] Instillation with Neomycin and Sulfamethiozole via urethral catheter following surgery (I) versus placebo: 0.18 [0.06, 0.55] SHORT DURATION CATHETER USE VS LONG DURATION CATHETER USE: Post-op urethral catheter for 1 day versus catheter for 2 days (1 study): RR 0.52 [0.05, 5.40] Post-op urethral catheter for 1 day versus post-op urethral catheter for 3 days (3 studies, not pooled): RRs 0.20 [ 0.03, 1.59]; 0.49 [0.13, 1.80]; 0.60 [ 0.32, 1.13] Post-op catheter for 1 day versus postop catheter for 5 days (2 studies, not pooled): RRs 0.11 [0.03, 0.43]; 0.70 [ 0.29, 1.67] Post-op urethral catheter for 1 day versus post-op catheter for 14 days (1 study): RR 0.21 [0.03, 1.65] CLAMP AND RELEASE POLICIES BEFORE CATHETER REMOVAL VS free IMMEDIATE CATHETER REMOVAL (1 study): RR 4.00 [1.55, 10.29] (Favours free) | Despite reviewing 39 eligible trials, few firm conclusions could be reached because of the multiple comparisons considered, the small size of individual trials, and their low quality. Whether or not to use a particular policy is usually a tradeoff between the risks of morbidity (especially infection) and risks of recatheterisation. | |
| Abbreviations: SR systematic review, MA metaanalysis, h hours, UTI urinary tract infection, n number of patients, RR risk ratio, HR hazard ratio, OR odds ratio, p p-value, CI confidence interval, OP operation, RCT randomized controlled trial | ||||||
Need for catheterization
The authors of a systematic review (SR) concluded that the routine insertion of indwelling catheters in women undergoing cesarean section was associated with more risk than benefit (relative risk [RR] of urinary tract infection in non-catheterized vs. catheterized patients in two RCTs, 0.08, with 95% confidence interval [0.01; 0.64]; RR in a single non-randomized study, 0.10 [0.02, 0.57]) (17).
Duration of catheterization
The time during which a catheter was left in place, after insertion at varying time points associated with gynecological interventions, was studied in nine RCTs (18– 26). The catheters were removed either immediately after surgery or within 24 hours (18, 19, 25, 27). Bray et al. and Hakvoort et al. chose removal after 48 to 72 hours as the condition for the comparison group (20, 24). Weemhoff et al. compared catheterization times of two vs. five days (26). The authors of all of these RCTs concluded that the catheter should be left in place for as short a time as possible to minimize the frequency of urinary tract infection. The rate of CA-UTI was significantly lowered by this strategy in some, but not all studies (18, 20, 23– 26), but no adverse side effects were encountered.
A single systematic review was identified that dealt with the duration of catheterization. This review included data from patients who were catheterized for ambulatory or inpatient surgery, as well as patients in nursing institutions (28). There were a total of 741 included patients from eight separate RCTs. In four of them, no significant differences in CA-UTI rates were found in patients who had undergone either transurethral resection of the prostate (TURP) or gynecological procedures (RR: 0.55; [0.30; 1.03]). In one RCT that compared catheterization for 1 vs. 5 days, a significant difference in the CA-UTI rate was, indeed, demonstrable: the rate was twice as high in the latter group (RR: 0.48; [0.27; 0–85]).
Two Cochrane reviews dealing with transurethral and suprapubic catheterization were included as well (29, 30). Cooper et al. reported that the CA-UTI rate was 65% lower when catheters were regularly changed (monthly and/or when medically indicated, vs. only when medically indicated) (RR: 0.35; [0.13; 0.95]) (29). Phipps et al. studied the following durations of catheterization: one vs. two days (48% fewer CA-UTIs with the shorter interval) (one study: RR: 0.52; [0.05; 5.40]), one vs. three days (three studies, not pooled, constituting one-third of the primary studies with a significant finding [RR: 0.11; (0.03; 0.43)]), one day vs. five days (two studies, not pooled), and one vs. 14 days (one study). Although most of these studies did not show a statistically significant benefit for the shorter interval, the point estimators nonetheless uniformly indicated that the shorter duration was advantageous (30).
Peri- and postoperative catheterization
A single RCT investigated perioperative transurethral catheterization in patients undergoing knee replacement surgery (31). Two different protocols were compared: preoperative catheterization (n = 306) vs. catheterization as needed for postoperative urinary retention (n = 346). The CA-UTI rate was 1.6% (5/306) in the former group and 1.7% (6/346) in the latter.
Type of catheter
Temporary transurethral vs. suprapubic catheterization
Three RCTs (32– 34) and three SRs (35– 37) on this topic were identified, the latter including one Cochrane review (37). Only two publications included urological interventions (33, 34). These studies did not reveal any statistically significant differences in CA-UTI rates. The systematic review by Hunter et al. included both experimental studies and clinical observational studies (36). The authors did not conduct any meta-analysis and did not favor either of the two methods of catheterization over the other on the basis of their findings. In contrast, the meta-analysis by Healy et al., which included twelve RCTs, did show a significantly lower CA-UTI rate with suprapubic catheterization (OR: 0.31; [0.18; 0.51]) (36). The meta-analysis that was part of the Cochrane review by Kidd et al., in which five RTCs with a total of 575 patients were included, did not reveal any difference in CA-UTI rates between the two methods of catheterization (RR: 1.01; [0.61; 1.69]) (37).
Intermittent (self-)catheterization vs. temporary indwelling catheters
Two RCTs (38, 39) and one SR were identified (e1) in which intermittent (self-)catheterization was compared with the use of temporary indwelling catheters. Hakvoort et al. reported a significantly (p = 0.03) lower CA-UTI rate with intermittent catheterization compared to an indwelling catheter left in place for three days (38). Hälleberg Nyman et al. included 182 patients who had undergone hip surgery; they concluded that both approaches are clinically acceptable (39). The absolute risk difference in the group that underwent intermittent catheterization was only 2.4%, a statistically insignificant effect (8 out of 85 patients with CA-UTI in the intermittently catheterized group, vs. 10 out of 85 patients in the group with indwelling catheters). Nor was any statistically significant difference found in the meta-analysis by Zhang et al. (9 RCTs; 1771 patients; RR: 1.23; [0.85; 1.76]) (e1).
Clamping vs. free urinary drainage
Intermittent catheter clamping can be used as a method of training the bladder (the bladder fills while the catheter is clamped and empties during the period of free drainage). One RCT (e2) and two SRs (e3, e4) were identified that dealt with this question. The RCT did not reveal any statistically significant difference between the two groups (210 women who had undergone hysterectomy; CA-UTI in 22.9% vs. 20.3%) (e2). In a systematic review, Fernandez et al. referred to an RCT in which three different modes of catheter management were compared (e3): intermittent clamping for 72 hours (group 1) vs. free drainage and removal after 24 hours (group 2) vs. free drainage and removal after 72 hours (group 3). 106 women who had undergone gynecological surgery were included. No significant differences were found in the rates of CA-UTI with free drainage for 24 hours vs. clamping (RR: 1.12 [0.24; 5.18]) or with free drainage for 72 hours vs. clamping (RR: 0.55; [0.15; 2.01]). Likewise, Wang et al., in a meta-analysis, did not find any statistically significant difference between clamping and free drainage (four RCTs; OR: 0.76; [0.33; 1.73]) (e4). They concluded that the limited available evidence provided no reason to alter the current clinical practice of free drainage.
Irrigation vs. no irrigation
A Cochrane review was devoted to the question whether some catheter irrigation schemes might be better than others with respect to efficacy, acceptability to patients, complication rates, and quality of life (e5). One of the RCTs cited compared irrigation with normal saline to no irrigation at all; in this trial, however, none of the patients in either group developed a CA-UTI.
Stabilization dressings with a catheter attachment or valve
An RCT dating back to 2006 investigated the effect of the StatLock system (e6), a stabilization dressing with a catheter attachment, serving the purpose of securing the catheter and thereby lessening the risk of inadvertent dislocation.
In the intervention group (60 of the 118 patients in the trial), which received a StatLock, the rate of CA-UTI was 45% lower, but this effect did not reach statistical significance (RR: 0.55; [0.25; 1.22]). One SR addressed the question whether a system with a valve was more beneficial than a simple bag to receive the urine (e7). This SR identified two RCTs on the subject, but results relating to the endpoint CA-UTI were only reported in a single RCT dating back to 1997. 30 of the 50 patients in the intervention group with the valve developed CA-UTI, compared to 34 of 50 in the control group. This 8% absolute difference in infection rates was statistically insignificant (p = 0.286).
Prophylaxis
Antibiotic-based prophylaxis strategies
Eleven studies compared the effect of antibiotic catheter impregnation or systemic antibiotic administration with that of no antibiotic prophylaxis at all: five of these were RCTs (e8– e12) and six were SRs (e11, e13– e17), among them four Cochrane reviews (e14– e17). In men who had undergone radical prostatectomy, the use of minocycline combined with rifampicin-impregnated catheters lowered the frequency of CA-UTI (1 in 56, vs. 6 in 68 patients in the control group (single trial, RR: 0.20; [0.03; 1.63]) (e14). A statistically significant difference was likewise found for the use of nitrofural-impregnated catheters compared to standard catheters (single trial; 4297 patients; RR: 0.84; [0.71; 0.99]) (e15), as well as for the systemic intravenous administration of trimethoprim/sulfamethoxazole (single trial; 90 patients; RR: 0.20; [0.06; 0.66]) (e16). The systematic prophylactic administration of antibiotics was also found to be superior to antibiotic administration only when clinically indicated, with respect to the frequency of CA-UTI (single trial; 90 patients; RR: 020; [0.06; 0.66]) (e17).
In their SR, Marschall et al. similarly reported a clinical benefit in the group of patients that received systemic antibiotic prophylaxis (cefotaxime, trimethoprim/sulfamethoxazole, ciprofloxacin, or Nitrofurantoin), with a modest absolute risk reduction of 5.8% (six RCTs, one observational study; RR: 0.45; [0.28; 0.72]). They calculated a number needed to treat (NNT) of 17 (95% confidence interval, 12 to 30) to prevent a single CA-UTI. On the other hand, no benefit was found in the SR by Van Hees et al., which included patients who had undergone surgery and received a single prophylactic antibiotic dose (trimethoprim/sulfamethoxazole [n = 46] or ciprofloxacin [n = 43] vs. placebo [n = 51]) (e18).
Antiseptic-impregnated vs. standard catheters
13 studies compared the effect of antiseptic catheter surfaces vs. catheters that were not antiseptically treated (e12, e19). In one Cochrane review, a statistically significant advantage of silver-coated catheters was reported (seven RCTs; RR: 0.60; [0.50; 0.73]) (e14). Two other Cochrane reviews from 2012 and 2014 did not reveal any advantage of silver-coated catheters (one RCT; 20 patients; RR: 10; [0.83; 1.2]) (e20); nor did a trial involving 4241 patients (RR: 0.99; [0.85; 1.16] [e15]). Jahn et al. concluded that the currently available data are insufficient as a basis for any recommendation for clinical practice (e20).
Antiseptic-impregnated vs. antibiotic-impregnated catheters
A Cochrane review of 2014 compared catheters with an antiseptic-impregnated surface to catheters with an antibiotic-impregnated surface (e15). The findings suggested an advantage of antiseptic-impregnated catheters compared to nitrofural-impregnated catheters (one study; 4250 patients; RR: 0.84; [071; 1.00]).
Cleansing and/or disinfection of the external urethral orifice
The network meta-analysis of 2018 included 36 studies with a total of 6490 patients and analyzed seven different methods of cleansing and/or disinfecting the external urethral orifice (tap water vs. soapy water vs. normal saline vs. mechanical cleaning alone vs. iodine vs. chlorhexidine vs. antibacterial solution) (e21). According to the authors, current data do not show the superiority of any of these methods over the others with respect to the frequency of CA-UTI (e15). Similarly heterogeneous findings were reported in another SR that included 28 RCTs and nine SRs (e22).
Phytotherapy for prophylaxis
It was investigated in two RCTs (e23, e24) whether the preventive administration of cranberry capsules might prevent the occurrence of CA-UTI. In the study by Gunnarson et al., women with hip fractures were divided into two groups: group 1 received 2 capsules containing 550 mg of cranberry powder three times daily until the fifth postoperative day, while group 2 received a placebo. No statistically significant difference was found in the rate of positive urine cultures (p = 0.975): cultures were positive in 19 of 50 patients in the intervention group (38%) and 23 of 61 (38%) in the placebo group (e23). In a study from the USA, the intervention group was given two cranberry capsules twice daily for six weeks after a gynecological procedure, while the control group was given a placebo preparation. The CA-UTI rate was markedly lower in the intervention group: 15 of 80 patients (19%) vs. 30 of 80 patients (38%) with positive urine culture; OR: 0.38; [0.19; 0.79]) (e24).
Education programs
Nine studies were found that dealt with educational approaches, among them five RCTs (17, e25– e28) and four systematic reviews (e29– e32). Education programs in the hospital were systematically assessed by Meddings et al., who pooled the results in a meta-analysis. It was found that the frequency of CA-UTI can be reduced by 52% by a reminder system or a defined catheter removal timepoint, and this effect is highly statistically significant (seven trials; RR: 0.48; [0.28; 0.68]; p = 0.001) (e31). A systematic review including 29 studies likewise showed that protocols for nurses can lower the rate of CA-UTI. In a further SR, the efficacy of the implementation of prevention protocols in nursing institutions was described (e30). The authors concluded that little attention has been paid to CA-UTI prevention until now and that the available evidence is too heterogeneous to derive a coherent synthesis of the results.
Studies involving multiple interventions
Studies involving multiple interventions have shown that transurethral catheters left in for a short period of time (24 hours) are superior to suprapubic catheters left in for a longer period of time (96 hours) (p = 0.034) (e33).
Discussion
Even though our literature search revealed a large number of existing studies on the prevention and management of CA-UTI, the results with respect to duration of catheterization, catheter type, and prophylaxis are highly heterogeneous, and the state of the evidence is still limited. Moreover, the definition of the endpoint and the distinction between CA-UTI and CA-ABU is highly heterogeneous in the primary studies. Some of them use the term CA-UTI to describe catheter-associated asymptomatic bacteriuria or catheter-associated bacteriuria. Many of the relevant studies date back to the 1990s or to the first decade of the present century. The applicability of their findings—in particular, those relating to antibiotic prophylaxis—to the current clinical situation is uncertain, as antibiotic prescribing practices and resistance patterns may well have changed in the meantime.
A study from the USA showed that 41% of treating physicians did not know that the patient under their care was catheterized, and that there was no medical indication for catheterization in 31% of the catheterized (e34). Further studies yielded similar figures (25–63%) with respect to catheterizations that were not medically indicated and/or not ordered by a physician (e35).
Umscheid postulated in 2011 that 65–70% of catheter-associated bloodstream infections and CA-UTI could have been prevented with the (then) current evidence-based strategies (e36). He calculated that the number of preventable infections of these types in the USA lies in the range of 95 483 to 387 550 per year (e36). The costs of preventable CA-UTIs was estimated to be in the range of 115 million to 1.82 billion dollars per year (e36).
Overview
Even though many studies have been published on the questions that are asked in this review, the state of the evidence is highly heterogeneous, and the comparability of the studies is very limited. It is, therefore, difficult to synthesize their results coherently.
Nonetheless, a small number of concise conclusions are stated in detail in the Table, so that physicians will have a few useful recommendations for practice that are based on the scientific literature and thus represent a successful transfer of knowledge from research to everyday clinical routine.
The clinical perspective.
An important distinction is drawn between catheter-associated asymptomatic bacteriuria (CA-ABU), which does not need to be treated, and catheter-associated urinary tract infection (CA-UTI), which needs treatment with antimicrobials.
In choosing the appropriate antibiotic, the physician must considered the local resistance situation, both to optimize the efficacy of treatment and to avoid the further selecting out of resistant organisms.
So-called antibiotic stewardship must be borne in mind whenever antimicrobial drugs are given. This term refers to the rational, responsible use of such drugs, comprising an appropriate choice of drug as well as appropriate dosing, mode of administration, and adaptation of the duration of treatment. The goal is to treat patients optimally while preventing the development of resistance.
The duration of catheterization (i.e., the length of time that a catheter is in place) is a determinative risk factor for CA-UTI. It follows that the indication for catheterization must always be critically considered, and that the catheter should be left in place for the shortest possible time.
Various measures (critical consideration of the indication for, and duration of, catheterization; education of nursing staff, etc.) should be bundled, in order to keep the risk of CA-UTI as low as possible for every patient.
Table. The state of the evidence.
| Question | Best current answer |
| Indication for catheterization | Routine catheterization often has more risks than benefits. The need for catheterization should always be critically considered. |
| Duration of catheterization | CA-UTI is more common when catheters are left in place for longer times. The duration of catheterization should, therefore, be kept as short as possible. |
| Peri- and postoperative catheterization | No randomized trials in urology were carried out on this topic in the period of the publications reviewed here, so no statement for clinical practice can be made. |
| Transurethral vs. suprapubic catheterization | Transurethral catheters probably have no advantage over suprapubic ones. |
| Clamping vs. free urinary drainage | The current evidence does not justify any recommendation. |
| Irrigation vs. no irrigation | The current evidence does not justify any recommendation. |
| Antibiotic prophylaxis | Antibiotic prophylaxis lessens the frequency of CA-UTI. |
| Antiseptic-impregnated catheters | The current evidence does not justify any recommendation. |
| Antiseptic- vs. antibiotic-impregnated catheters | The evidence is limited. Antibiotic-impregnated catheters may be advantageous. |
| Cleansing/disinfection of the urethral orifice | No significant differences have been demonstrated among the various methods of cleansing and/or disinfecting the external urethral orifice. |
| Phytotherapy as prophylaxis | The evidence regarding cranberry products is mixed. |
Key messages.
There is no evidence of any difference between transurethral and suprapubic catheterization with respect to the development of catheter-associated urinary tract infection.
Nor are there any relevant differences among the various types of catheter material (latex vs. silicone vs. polyvinyl chloride vs. polyurethane) with respect to the endpoint “catheter-associated urinary tract infection.”
The putative benefit of antiseptically coated catheters, compared to uncoated standard catheters, is unclear. Antibiotically impregnated catheters seem to be associated with fewer catheter-associated urinary tract infections than antiseptically coated ones.
None of the various methods of cleansing and/or disinfecting the external urethral orifice for transurethral catheterization is better than the others with respect to the development of catheter-associated urinary tract infection.
The current state of the evidence on phytotherapy for the prevention of catheter-associated urinary tract infection does not justify the issuance of any recommendation for clinical practice.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement PD Dr. Kranz has served as a paid consultant for Farco-Pharma.
Dr. Wagenlehner has received third-party research funding from Bionorica, Achaogen, AstraZeneca, Enteris BioPharma, Helpery Therapeutics, Janssen, LeoPharma, MerLion, MSD, OM Pharma/Vifor Pharma, Pfizer, RosenPharma, Shionogi, VenatoRx, and GSK.
The remaining authors state that they have no conflict of interest.
References
- 1.Warren JW, Platt R, Thomas RJ, Rosner B, Kass EH. Antibiotic irrigation and catheter-associated urinary-tract infections. N Engl J Med. 1978;299:570–573. doi: 10.1056/NEJM197809142991103. [DOI] [PubMed] [Google Scholar]
- 2.Nationales Referenzzentrum für Surveillance von nosokomialen Infektionen. Deutsche nationale Punkt-Prävalenzerhebung zu nosokomialen Infektionen und Antibiotika-Anwendung. 2016 Abschlussbericht. www.nrz-hygiene.de/fileadmin/nrz/download/pps2016/PPS_2016_Abschlussbericht_20.07.2017.pdf (last accessed on 14 January 2020) [Google Scholar]
- 3.Saint S, Chenoweth CE. Biofilms and catheter-associated urinary tract infections. Infect Dis Clin North Am. 2003;17:411–432. doi: 10.1016/s0891-5520(03)00011-4. [DOI] [PubMed] [Google Scholar]
- 4.Warren JW. Catheter-associated urinary tract infections. Int J Antimicrob Agents. 2001;17:299–303. doi: 10.1016/s0924-8579(00)00359-9. [DOI] [PubMed] [Google Scholar]
- 5.Bagshaw SM, Laupland KB. Epidemiology of intensive care unit-acquired urinary tract infections. Curr Opin Infect Dis. 2006;19:67–71. doi: 10.1097/01.qco.0000200292.37909.e0. [DOI] [PubMed] [Google Scholar]
- 6.Wagenlehner FM, Loibl E, Vogel H, Naber KG. Incidence of nosocomial urinary tract infections on a surgical intensive care unit and implications for management. Int J Antimicrob Agents. 2006;28(1):S86–S90. doi: 10.1016/j.ijantimicag.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 7.Nationales Referenzzentrum für Surveillance von nosokomialen Infektionen. KISS Krankenhaus-Infektions-Surveillance-System, Infektionssurveillance im Modul ITS-KISS Referenzdaten. www.nrz-hygiene.de/fileadmin/nrz/module/its/201001_201412_ALLE_ITSRef.pdf (last accessed on 14 January 2020) [Google Scholar]
- 8.Warren JW, Damron D, Tenney JH, Hoopes JM, Deforge B, Muncie HL Jr. Fever, bacteremia, and death as complications of bacteriuria in women with long-term urethral catheters. J Infect Dis. 1987;155:1151–1158. doi: 10.1093/infdis/155.6.1151. [DOI] [PubMed] [Google Scholar]
- 9.Garibaldi RA, Burke JP, Dickman ML, Smith CB. Factors predisposing to bacteriuria during indwelling urethral catheterization. N Engl J Med. 1974;291:215–219. doi: 10.1056/NEJM197408012910501. [DOI] [PubMed] [Google Scholar]
- 10.Hartstein AI, Garber SB, Ward TT, Jones SR, Morthland VH. Nosocomial urinary tract infection: a prospective evaluation of 108 catheterized patients. Infect Control. 1981;2:380–386. doi: 10.1017/s0195941700055533. [DOI] [PubMed] [Google Scholar]
- 11.Bryan CS, Reynolds KL. Hospital-acquired bacteremic urinary tract infection: epidemiology and outcome. J Urol. 1984;132:494–498. doi: 10.1016/s0022-5347(17)49707-2. [DOI] [PubMed] [Google Scholar]
- 12.Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31:319–326. doi: 10.1086/651091. [DOI] [PubMed] [Google Scholar]
- 13.Weinstein MP, Towns ML, Quartey SM, et al. The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin Infect Dis. 1997;24:584–602. doi: 10.1093/clind/24.4.584. [DOI] [PubMed] [Google Scholar]
- 14.Kranz J, Schmidt S, Lebert C, Schneidewind L, Schmiemann G, Wagenlehner F. Uncomplicated bacterial community-acquired urinary tract infection in adults. Dtsch Arztebl Int. 2017;114:866–873. doi: 10.3238/arztebl.2017.0866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zowawi HM, Harris PN, Roberts MJ, et al. The emerging threat of multidrug-resistant gram-negative bacteria in urology. Nat Rev Urol. 2015;12:570–584. doi: 10.1038/nrurol.2015.199. [DOI] [PubMed] [Google Scholar]
- 16.Haby MM, Chapman E, Clark R, Barreto J, Reveiz L, Lavis JN. What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice: a rapid review. Health Res Policy Syst. 2016;14 doi: 10.1186/s12961-016-0155-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L, Wen J, Wang L, Li YP, Li Y. Is routine indwelling catheterisation of the bladder for caesarean section necessary? A systematic review. BJOG. 2011;118:400–409. doi: 10.1111/j.1471-0528.2010.02802.x. [DOI] [PubMed] [Google Scholar]
- 18.Ahmed MR, Sayed Ahmed WA, Atwa KA, Metwally L. Timing of urinary catheter removal after uncomplicated total abdominal hysterectomy: a prospective randomized trial. Eur J Obstet Gynecol Reprod Biol. 2014;176:60–63. doi: 10.1016/j.ejogrb.2014.02.038. [DOI] [PubMed] [Google Scholar]
- 19.Alessandri F, Mistrangelo E, Lijoi D, Ferrero S, Ragni N. A prospective, randomized trial comparing immediate versus delayed catheter removal following hysterectomy. Acta Obstet Gynecol Scand. 2006;85:716–720. doi: 10.1080/00016340600606976. [DOI] [PubMed] [Google Scholar]
- 20.Bray R, Cartwright R, Digesu A, Fernando R, Khullar V. A randomised controlled trial comparing immediate versus delayed catheter removal following vaginal prolapse surgery. Eur J Obstet Gynecol Reprod Biol. 2017;210:314–318. doi: 10.1016/j.ejogrb.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Chai J, Pun TC. A prospective randomized trial to compare immediate and 24-hour delayed catheter removal following total abdominal hysterectomy. Acta Obstet Gynecol Scand. 2011;90:478–482. doi: 10.1111/j.1600-0412.2011.01104.x. [DOI] [PubMed] [Google Scholar]
- 22.Dunn TS, Shlay J, Forshner D. Are in-dwelling catheters necessary for 24 hours after hysterectomy? Am J Obstet Gynecol. 2003;189:435–437. doi: 10.1067/s0002-9378(03)00496-4. [DOI] [PubMed] [Google Scholar]
- 23.El-Mazny A, El-Sharkawy M, Hassan A. A prospective randomized clinical trial comparing immediate versus delayed removal of urinary catheter following elective cesarean section. Eur J Obstet Gynecol Reprod Biol. 2014;181:111–114. doi: 10.1016/j.ejogrb.2014.07.034. [DOI] [PubMed] [Google Scholar]
- 24.Hakvoort RA, Elberink R, Vollebregt A, Ploeg T, Emanuel MH. How long should urinary bladder catheterisation be continued after vaginal prolapse surgery? A randomised controlled trial comparing short term versus long term catheterisation after vaginal prolapse surgery. BJOG. 2004;111:828–830. doi: 10.1111/j.1471-0528.2004.00181.x. [DOI] [PubMed] [Google Scholar]
- 25.Sekhavat L, Farajkhoda T, Davar R. The effect of early removal of indwelling urinary catheter on postoperative urinary complications in anterior colporrhaphy surgery. Aust N Z J Obstet Gynaecol. 2008;48:348–352. doi: 10.1111/j.1479-828X.2008.00842.x. [DOI] [PubMed] [Google Scholar]
- 26.Weemhoff M, Wassen MM, Korsten L, Serroyen J, Kampschoer PH, Roumen FJ. Postoperative catheterization after anterior colporrhaphy: 2 versus 5 days A multicentre randomized controlled trial. Int Urogynecol J. 2011;22:477–483. doi: 10.1007/s00192-010-1304-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cai T, Caola I, Tessarolo F, et al. Solidago, orthosiphon, birch and cranberry extracts can decrease microbial colonization and biofilm development in indwelling urinary catheter: a microbiologic and ultrastructural pilot study. World J Urol. 2014;32:1007–1014. doi: 10.1007/s00345-013-1173-5. [DOI] [PubMed] [Google Scholar]
- 28.Fernandez RS, Griffiths RD. Duration of short-term indwelling catheters - a systematic review of the evidence. J Wound Ostomy Continence Nurs. 2006;33:145–153. doi: 10.1097/00152192-200603000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Cooper FP, Alexander CE, Sinha S, Omar MI. Policies for replacing long-term indwelling urinary catheters in adults. Cochrane Database Syst Rev. 2016;7 doi: 10.1002/14651858.CD011115.pub2. CD011115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Phipps S, Lim YN, McClinton S, Barry C, Rane A, N‘Dow J. Short term urinary catheter policies following urogenital surgery in adults. Cochrane Database Syst Rev. 2006 doi: 10.1002/14651858.CD004374.pub2. CD004374. [DOI] [PubMed] [Google Scholar]
- 31.Iorio R, Healy WL, Patch DA, Appleby D. The role of bladder catheterization in total knee arthroplasty. Clin Orthop Relat Res. 2000::80–84. doi: 10.1097/00003086-200011000-00011. [DOI] [PubMed] [Google Scholar]
- 32.Baan AH, Vermeulen H, van der Meulen J, Bossuyt P, Olszyna D, Gouma DJ. The effect of suprapubic catheterization versus transurethral catheterization after abdominal surgery on urinary tract infection: a randomized controlled trial. Dig Surg. 2003;20:290–295. doi: 10.1159/000071693. [DOI] [PubMed] [Google Scholar]
- 33.Dixon L, Dolan LM, Brown K, Hilton P. RCT of urethral versus suprapubic catheterization. Br J Nurs. 2010;19:S7–S13. doi: 10.12968/bjon.2010.19.Sup8.79063. [DOI] [PubMed] [Google Scholar]
- 34.Stekkinger E, van der Linden PJ. A comparison of suprapubic and transurethral catheterization on postoperative urinary retention after vaginal prolapse repair: a randomized controlled trial. Gynecol Obstet Invest. 2011;72:109–116. doi: 10.1159/000323827. [DOI] [PubMed] [Google Scholar]
- 35.Healy EF, Walsh CA, Cotter AM, Walsh SR. Suprapubic compared with transurethral bladder catheterization for gynecologic surgery: a systematic review and meta-analysis. Obstet Gynecol. 2012;120:678–687. doi: 10.1097/AOG.0b013e3182657f0d. [DOI] [PubMed] [Google Scholar]
- 36.Hunter KF, Bharmal A, Moore KN. Long-term bladder drainage: Suprapubic catheter versus other methods: a scoping review. Neurourol Urodyn. 2013;32:944–951. doi: 10.1002/nau.22356. [DOI] [PubMed] [Google Scholar]
- 37.Kidd EA, Stewart F, Kassis NC, Hom E, Omar MI. Urethral (indwelling or intermittent) or suprapubic routes for short-term catheterisation in hospitalised adults. Cochrane Database Syst Rev. 2015;10 doi: 10.1002/14651858.CD004203.pub3. CD004203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hakvoort RA, Thijs SD, Bouwmeester FW, et al. Comparing clean intermittent catheterisation and transurethral indwelling catheterisation for incomplete voiding after vaginal prolapse surgery: a multicentre randomised trial. BJOG. 2011;118:1055–1060. doi: 10.1111/j.1471-0528.2011.02935.x. [DOI] [PubMed] [Google Scholar]
- 39.Hälleberg Nyman M, Gustafsson M, Langius-Eklof A, Johansson JE, Norlin R, Hagberg L. Intermittent versus indwelling urinary catheterisation in hip surgery patients: a randomised controlled trial with cost-effectiveness analysis. Int J Nurs Stud. 2013;50:1589–1598. doi: 10.1016/j.ijnurstu.2013.05.007. [DOI] [PubMed] [Google Scholar]
- E1.Zhang W, Liu A, Hu D, et al. Indwelling versus intermittent urinary catheterization following total joint arthroplasty: A systematic review and meta-analysis. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0130636. e0130636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Gong Y, Zhao L, Wang L, Wang F. The effect of clamping the indwelling urinary catheter before removal in cervical cancer patients after radical hysterectomy. J Clin Nurs. 2017;26:1131–1136. doi: 10.1111/jocn.13579. [DOI] [PubMed] [Google Scholar]
- E3.Fernandez RS, Griffiths RD. Clamping short-term indwelling catheters: a systematic review of the evidence. J Wound Ostomy Continence Nurs. 2005;32:329–336. doi: 10.1097/00152192-200509000-00012. [DOI] [PubMed] [Google Scholar]
- E4.Wang LH, Tsai MF, Han CS, Huang YC, Liu HE. Is bladder training by clamping before removal necessary for short-term indwelling urinary catheter inpatient? A systematic review and meta-analysis. Asian Nurs Res. 2016;10:173–181. doi: 10.1016/j.anr.2016.07.003. [DOI] [PubMed] [Google Scholar]
- E5.Shepherd AJ, Mackay WG, Hagen S. Washout policies in long-term indwelling urinary catheterisation in adults. Cochrane Database Syst Reviews. 2017;3 doi: 10.1002/14651858.CD004012.pub5. CD004012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E6.Darouiche RO, Goetz L, Kaldis T, Cerra-Stewart C, AlSharif A, Priebe M. Impact of StatLock securing device on symptomatic catheter-related urinary tract infection: a prospective, randomized, multicenter clinical trial. Am J Infect Control. 2006;34:555–560. doi: 10.1016/j.ajic.2006.03.010. [DOI] [PubMed] [Google Scholar]
- E7.van den Eijkel E, Griffiths P. Catheter valves for indwelling urinary catheters: a systematic review. Br J Community Nurs. 2006;11:111–114. doi: 10.12968/bjcn.2006.11.3.20586. [DOI] [PubMed] [Google Scholar]
- E8.Al-Habdan I, Sadat-Ali M, Corea JR, Al-Othman A, Kamal BA, Shriyan DS. Assessment of nosocomial urinary tract infections in orthopaedic patients: a prospective and comparative study using two different catheters. Int Surg. 2003;88:152–154. [PubMed] [Google Scholar]
- E9.Dieter AA, Amundsen CL, Edenfield AL, et al. Oral antibiotics to prevent postoperative urinary tract infection: a randomized controlled trial. Obstet Gynecol. 2014;123:96–103. doi: 10.1097/AOG.0000000000000024. [DOI] [PubMed] [Google Scholar]
- E10.Pfefferkorn U, Lea S, Moldenhauer J, Peterli R, von Flue M, Ackermann C. Antibiotic prophylaxis at urinary catheter removal prevents urinary tract infections: a prospective randomized trial. Ann Surg. 2009;249:573–575. doi: 10.1097/SLA.0b013e31819a0315. [DOI] [PubMed] [Google Scholar]
- E11.Rogers RG, Kammerer-Doak D, Olsen A, et al. A randomized, double-blind, placebo-controlled comparison of the effect of nitrofurantoin monohydrate macrocrystals on the development of urinary tract infections after surgery for pelvic organ prolapse and/or stress urinary incontinence with suprapubic catheterization. Am J Obstet Gynecol. 2004;191:182–187. doi: 10.1016/j.ajog.2004.03.088. [DOI] [PubMed] [Google Scholar]
- E12.Pickard R, Lam T, Maclennan G, et al. Types of urethral catheter for reducing symptomatic urinary tract infections in hospitalised adults requiring short-term catheterisation: multicentre randomised controlled trial and economic evaluation of antimicrobial- and antiseptic-impregnated urethral catheters (the CATHETER trial) Health Technol Assess. 2012;16:1–197. doi: 10.3310/hta16470. [DOI] [PubMed] [Google Scholar]
- E13.Marschall J, Carpenter CR, Fowler S, Trautner BW, CDCPE Program. Antibiotic prophylaxis for urinary tract infections after removal of urinary catheter: meta-analysis. BMJ. 2013;346 doi: 10.1136/bmj.f3147. f3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E14.Brosnahan J, Jull A, Tracy C. Types of urethral catheters for management of short-term voiding problems in hospitalised adults. Cochrane Database Syst Rev. 2004;1 doi: 10.1002/14651858.CD004013.pub2. CD004013. [DOI] [PubMed] [Google Scholar]
- E15.Lam TB, Omar MI, Fisher E, Gillies K, MacLennan S. Types of indwelling urethral catheters for short-term catheterisation in hospitalised adults. Cochrane Database Syst Rev. 2014;9 doi: 10.1002/14651858.CD004013.pub4. CD004013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E16.Lusardi G, Lipp A, Shaw C. Antibiotic prophylaxis for short-term catheter bladder drainage in adults. Cochrane Database Syst Rev. 2013;7 doi: 10.1002/14651858.CD005428.pub2. CD005428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E17.Niël-Weise BS, van den Broek PJ. Antibiotic policies for short-term catheter bladder drainage in adults. Cochrane Database Syst Rev. 2005;3 doi: 10.1002/14651858.CD005428. CD005428. [DOI] [PubMed] [Google Scholar]
- E18.van Hees BC, Vijverberg PL, Hoorntje LE, Wiltink EH, Go PM, Tersmette M. Single-dose antibiotic prophylaxis for urinary catheter removal does not reduce the risk of urinary tract infection in surgical patients: a randomized double-blind placebo-controlled trial. Clin Microbiol Infect. 2011;17:1091–1094. doi: 10.1111/j.1469-0691.2010.03447.x. [DOI] [PubMed] [Google Scholar]
- E19.Bonfill X, Rigau D, Esteban-Fuertes M, et al. Efficacy and safety of urinary catheters with silver alloy coating in patients with spinal cord injury: a multicentric pragmatic randomized controlled trial. The ESCALE trial. Spine J. 2017;17:1650–1657. doi: 10.1016/j.spinee.2017.05.025. [DOI] [PubMed] [Google Scholar]
- E20.Jahn P, Beutner K, Langer G. Types of indwelling urinary catheters for long-term bladder drainage in adults. Cochrane Database Syst Rev. 2012;10 doi: 10.1002/14651858.CD004997.pub3. CD004997. [DOI] [PubMed] [Google Scholar]
- E21.Cao Y, Gong Z, Shan J, Gao Y. Comparison of the preventive effect of urethral cleaning versus disinfection for catheter-associated urinary tract infections in adults: A network meta-analysis. Int J Infect Dis. 2018;76:102–108. doi: 10.1016/j.ijid.2018.09.008. [DOI] [PubMed] [Google Scholar]
- E22.Ercole FF, Macieira TG, Wenceslau LC, Martins AR, Campos CC, Chianca TC. Integrative review: evidences on the practice of intermittent/indwelling urinary catheterization. Rev Lat Am Enfermagem. 2013;21:459–468. doi: 10.1590/s0104-11692013000100023. [DOI] [PubMed] [Google Scholar]
- E23.Gunnarsson AK, Gunningberg L, Larsson S, Jonsson KB. Cranberry juice concentrate does not significantly decrease the incidence of acquired bacteriuria in female hip fracture patients receiving urine catheter: a double-blind randomized trial. Clin Interv Aging. 2017;12:137–143. doi: 10.2147/CIA.S113597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E24.Foxman B, Cronenwett AE, Spino C, Berger MB, Morgan DM. Cranberry juice capsules and urinary tract infection after surgery: results of a randomized trial. Am J Obstet Gynecol. 2015;213:194.e1–194.e8. doi: 10.1016/j.ajog.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E25.Chen YY, Chi MM, Chen YC, Chan YJ, Chou SS, Wang FD. Using a criteria-based reminder to reduce use of indwelling urinary catheters and decrease urinary tract infections. Am J Crit Care. 2013;22:105–114. doi: 10.4037/ajcc2013464. [DOI] [PubMed] [Google Scholar]
- E26.Loeb M, Hunt D, O‘Halloran K, Carusone SC, Dafoe N, Walter SD. Stop orders to reduce inappropriate urinary catheterization in hospitalized patients: a controlled trial. J Gen Intern Med. 2008;23:816–820. doi: 10.1007/s11606-008-0620-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E27.Mody L, Krein SL, Saint S, et al. A targeted infection prevention intervention in nursing home residents with indwelling devices: a randomized clinical trial. JAMA Intern Med. 2015;175:714–723. doi: 10.1001/jamainternmed.2015.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E28.Wilde MH, McMahon JM, McDonald MV, et al. Self-management intervention for long-term indwelling urinary catheter users: randomized clinical trial. Nurs Res. 2015;64:24–34. doi: 10.1097/NNR.0000000000000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E29.Durant DJ. Nurse-driven protocols and the prevention of catheter-associated urinary tract infections: a systematic review. Am J Infect Control. 2017;45:1331–1341. doi: 10.1016/j.ajic.2017.07.020. [DOI] [PubMed] [Google Scholar]
- E30.Gould D, Gaze S, Drey N, Cooper T. Implementing clinical guidelines to prevent catheter-associated urinary tract infections and improve catheter care in nursing homes: systematic review. Am J Infect Control. 2017;45:471–476. doi: 10.1016/j.ajic.2016.09.015. [DOI] [PubMed] [Google Scholar]
- E31.Meddings J, Rogers MA, Macy M, Saint S. Systematic review and meta-analysis: reminder systems to reduce catheter-associated urinary tract infections and urinary catheter use in hospitalized patients. Clin Infect Dis. 2010;51:550–560. doi: 10.1086/655133. [DOI] [PubMed] [Google Scholar]
- E32.Meddings J, Saint S, Krein SL, et al. Systematic review of interventions to reduce urinary tract infection in nursing home residents. J Hosp Med. 2017;12:356–368. doi: 10.12788/jhm.2724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E33.Kringel U, Reimer T, Tomczak S, Green S, Kundt G, Gerber B. Postoperative infections due to bladder catheters after anterior colporrhaphy: a prospective, randomized three-arm study. Int Urogynecol J. 2010;21:1499–1504. doi: 10.1007/s00192-010-1221-2. [DOI] [PubMed] [Google Scholar]
- E34.Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control. 2000;28:68–75. doi: 10.1016/s0196-6553(00)90015-4. [DOI] [PubMed] [Google Scholar]
- E35.Fakih MG, Pena ME, Shemes S, et al. Effect of establishing guidelines on appropriate urinary catheter placement. Acad Emerg Med. 2010;17:337–340. doi: 10.1111/j.1553-2712.2009.00677.x. [DOI] [PubMed] [Google Scholar]
- E36.Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32:101–114. doi: 10.1086/657912. [DOI] [PubMed] [Google Scholar]
- E37.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses The PRISMA Statement. PLoS Med. 2009;6 e1000097. [PMC free article] [PubMed] [Google Scholar]