Abstract
Introduction
To improve safe imaging among children, the Image Gently Campaign was launched by several radiologic societies in 2007. A goal of the campaign was to reduce ionizing radiation exposure in children. Given the recurrent nature of their disease, children with kidney stones are at risk of unnecessary ionizing radiation exposure from computed tomography (CT).
We sought to determine whether the campaign caused a decrease in the utilization of computed tomography (CT) for the evaluation of children with nephrolithiasis. We hypothesize that the campaign was the primary cause of a decrease in CT utilization.
Materials and Methods
We analyzed medical claims data (2001–2015), identifying children with nephrolithiasis covered by the same commercial insurance provider. Using a difference-in-differences (DID) design, we estimated changes in CT use among children (<18 years) compared to a control group [i.e., adults (≥18) with nephrolithiasis] after the campaign started.
Results
We identified 12,734 children and 787,720 adults diagnosed with nephrolithiasis. Before 2007, quarterly rates of CT use during a stone episode (per 1000 patients) were increasing at a parallel rate among children and adults (5.1 in children versus 7.2 in adults, p=0.123). After the campaign started, the rate of CT use decreased in both groups, but at a slightly significantly greater rate in adults than children (DID Estimator: 2.96, CI 0.00–5.91, p=0.050).
Conclusions
Although there has been a decrease in the use of CT among children with nephrolithiasis, given a similar trend seen in adults, this change cannot be primarily attributed to the Image Gently Campaign.
Keywords: Ionizing radiation, Nephrolithiasis, Kidney calculi, Diagnostic Imaging, Adverse Effects
Introduction
Over the last several decades, the rapid increase in the utilization of computed tomography (CT) has led to concern about the potential harmful effects of ionizing radiation. This is particularly true for children, who are thought to be particularly susceptible to the ill effects of radiation given the sensitivity of their rapidly dividing tissues and the potential for cumulative lifetime exposure.1–4 Many of these CTs are unnecessary.1,5 These concerns prompted several radiological societies to launch the Image Gently Campaign® in 2007 to “promote safe and effective imaging care of children.”6–7
Cumulative radiation exposure is particularly concerning for the growing number of children with nephrolithiasis. The incidence of stones in children is rising by 6–10% annually and many children experience recurrent stones.2,8,9 Therefore, there are a growing number of children who have substantial lifetime radiation exposure from evaluation of stones. Much of this radiation is potentially preventable. Renal ultrasound (RUS) is recommended for initial evaluation of children with suspected kidney stones, with CT suggested only in the rare case of a nondiagnostic ultrasound with high clinical suspicion.10.11 Nonetheless, 45–79% of children undergo a CT with the majority of CTs performed as the initial imaging modality.12,13 Although these patients could benefit from the advocacy efforts of the campaign, its effect in this population currently remains unknown.
In this context, we sought to determine whether the Image Gently Campaign® caused a decrease in the utilization of CT for evaluation of pediatric kidney stones. Our objective was to evaluate rates of CT utilization before and after the launch of the campaign in children compared to a control group of adults in a national cohort. We hypothesize that CT utilization in children with kidney stones decreased at a greater rate than in adults after the campaign launch.
Materials and Methods:
Study Design and Dataset
We performed a retrospective cohort study of children and adults with kidney stones using a national, private de-identified insurance claims database (Clinformatics® Data Mart Database; OptumInsight, Eden Prarie, MN). This database captures all emergency department (ED), outpatient, and inpatient patient-level encounters of 73 million people commercially insured by a single, large U.S. insurance agency. The study was determined to be exempt by the institutional review board of our institution.
Study Population
Using a code-based algorithm, we identified all children (<18 years) (intervention group) and adults (≥18) (control group) who were evaluated in the ED or an outpatient clinic with the primary diagnosis of nephrolithiasis between August 1, 2001 and July 31, 2015 (Appendix Table 1). To determine whether any changes seen in the utilization of CT was due to the campaign or other independent factors, we used adults as a control group for two reasons: first, they should have been unaffected an exclusively pediatric campaign, and second, imaging recommendations for patients with suspected nephrolithiasis differ between children and adults. For initial imaging, non-contrast CT is recommended for adults and RUS for children.11,14 Therefore, we would expect the use of CT for evaluation of kidney stones in adults to remain stable and could assume no spillover effects.
A stone episode included all visits made within the 7 days prior to and 90 days following the index encounter to allow time for spontaneous stone passage or staged stone removal, while being highly unlikely for new stone development.15 Any visit made for nephrolithiasis after 90 days was assumed to be due to a new stone episode and was also included. Patients were excluded if they did not have continuous enrollment for six months before and 90 days after their first stone visit.
Outcomes
Our primary outcome was the quarterly rate of CT use for the evaluation of nephrolithiasis. We also performed a subgroup analysis to determine whether the use of CT varied for incident versus recurrent stones. For our secondary outcome, we sought to determine if the campaign led to a change in the utilization of other imaging modalities, including renal ultrasound (RUS) and abdominal x-ray (AXR).
To measure the quarterly rate of CT use, we first determined whether a patient underwent a CT of the abdomen and/or pelvis during their stone episode using diagnosis and procedure codes (Appendix Table 1). To enable direct comparison of children and adults, we next calculated the risk-standardized rate of CT utilization per quarter for both groups (Appendix 1 and Appendix Table 2).
For our secondary outcome, we again used a code-based algorithm to determine whether these imaging modalities were used during each stone episode (Appendix Table 1).
Exposure
We compared quarterly utilization of CT before the July 2007 campaign launch (August 2001 – July 2007) to afterwards (August 2007 – July 2015).
Statistical Analysis
We first tested for differences between patients who did or did not undergo a CT during a stone episode. Next, we used a difference-in-differences (DID) approach to evaluate the change in quarterly utilization of CT for evaluation of nephrolithiasis during a stone episode after the launch of the campaign in July 2007. We fitted ordinary least squares regression models to compare trends in quarterly risk-adjusted CT rates between children and adults before and after the campaign launch (Appendix 2).16,17 We confirmed that the parallel trends assumption was met by comparing the trends in CT utilization before the campaign between children and adults.
We next repeated this analysis for two subgroups of patients: first those with incident stones, defined as their first stone during the study period, and second for those with recurrent stones, defined as those who had additional stones during the study period.
A sensitivity analysis was performed to confirm the findings by repeating the DID analysis using several different time frames to ensure the results were not overly influenced by quarters that may have been outliers.
For our secondary analysis, we evaluated the temporal trends of the crude quarterly utilization of all stone imaging procedures (CT, RUS, and AXR).
The analysis was conducted with a combination of SAS 9.4 (SAS Institute Inc., Cary, NC, USA) for extraction, cleaning and descriptive analysis and STATA (Stata 13/SE, College Station, TX, USA) for the DID analysis. All statistical testing was two-tailed and examined at the 0.05 significance level.
Results
We identified a total of 12,734 children and 787,720 adults with kidney stones (Table 1). The proportion of patients who underwent a CT significantly increased after the campaign started for both groups. For children, 48.8% (2,576/5,274) underwent a CT before the campaign started compared to 54.0% (4,029/7,460) after (p<0.001). For adults, 57.8% (153,028/264,793) underwent a CT before the campaign started compared to 66.7% (349,044/522,927) after (p<0.001). For both groups, the majority of patients (72.6–85.5%) who initially presented to an ED underwent a CT, compared to the minority of patients who initially presented to an outpatient clinic (22.4–38.3%) (p<0.001 for all groups) (Table 1).
Table 1.
Demographics of patients with nephrolithiasis before and after the launch of the Image Gently Campaign for a) children and b) adults.
| Pre-Intervention (8/2001–7/2007) | Post-Intervention (8/2007–7/2015) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | No CT | CT | p-value | Overall | No CT | CT | p-value | ||
| Number of Children | 5274 | 2689 | 2576 | 7460 | 3431 | 4029 | |||
| Age (Standard Deviation) | 12.6 (4.5) | 11.1 (5.1) | 14.2 (3.2) | <0.001 | 13.3 (4.3) | 11.5 (5.0) | 14.7 (2.8) | <0.001 | |
| Gender | |||||||||
| Female | 2965 | 1372 (46.3%) | 1593 (53.7%) | <0.001 | 4402 | 1823 (41.4%) | 2579 (58.6%) | <0.001 | |
| Male | 2309 | 1326 (57.4%) | 983 (42.6%) | 3058 | 1608 (52.6%) | 1450 (47.4%) | |||
| Imaging Performed At Index Visit | |||||||||
| Emergency Department | 1962 | 530 (27.0%) | 1432 (73.0%) | <0.001 | 3476 | 951 (27.4%) | 2525 (72.6%) | <0.001 | |
| Outpatient Clinic | 3312 | 2571 (77.6%) | 741(22.4%) | 3984 | 3011 (75.6%) | 973 (24.4%) | |||
| Imaging Performed During Stone Episodea | |||||||||
| Emergency Department | 1962 | 427 (21.8%) | 1535 (78.2%) | <0.001 | 3476 | 801 (23.0%) | 2675 (77.0%) | <0.001 | |
| Outpatient Clinic | 3312 | 2271 (68.5%) | 1041 (31.4%) | 3984 | 2630 (66.0%) | 1354 (34.0%) | |||
| Pre-Intervention (8/2001–7/2007) | Post-Intervention (8/2007–7/2015) | ||||||||
| Overall | No CT | CT | p-value | Overall | No CT | CT | p-value | ||
| Number of Adults | 264793 | 111765 | 153028 | 522927 | 173883 | 349044 | |||
| Age (Standard Deviation) | 47.9 (14.2) | 48.8 (14.3) | 47.2 (14.0) | <0.001 | 53.2 (16.5) | 55.1 (16.6) | 52.3 (16.3) | ||
| Gender | |||||||||
| Female | 110146 | 46733 (42.4%) | 63413 (57.6%) | 0.053 | 229801 | 76762 (33.4%) | 153039 (66.6%) | 0.039 | |
| Male | 154647 | 65032 (42.1%) | 89615 (57.9%) | 293126 | 97121 (33.1%) | 196005 (66.9%) | |||
| Imaging Performed At Index Visit | |||||||||
| Emergency Department | 100820 | 23759 (23.6%) | 77061 (76.4%) | <0.001 | 211787 | 31125 (14.7%) | 180662 (85.3%) | <0.001 | |
| Outpatient Clinic | 163973 | 115024 (70.1%) | 48949 (29.9%) | 311140 | 192069 (61.7%) | 119071 (38.3%) | |||
| Imaging Performed During Stone Episodea | |||||||||
| Emergency Department | 100820 | 18493 (18.3%) | 82327 (81.7%) | >0.001 | 211787 | 22553 (10.6%) | 189234 (89.4%) | <0.001 | |
| Outpatient Clinic | 163973 | 93272 (56.9%) | 70701 (43.1%) | 311140 | 151330 (48.6%) | 159810 (51.4%) | |||
Includes imaging performed during index visit and all subsequent encounters during the stone episode.
Although there was a higher proportion of CTs performed after the campaign launch, this is not reflective of the trend in utilization. Between August 2001 and July 2007, the proportion of children and adults who underwent a CT for evaluation of stones was increasing at a parallel rate (5.07 CTs per 1,000 patients per quarter for children, 7.22 for adults, p-value for difference=0.12) (Table 2 and Figure 1)). Conversely, after the launch of the campaign until August 2015, the proportion of children and adults who underwent a CT each quarter progressively decreased for both groups. The rate of decrease of CT utilization was similar for both groups (−2.82 versus −2.01, p=0.19). However, adults had a higher rate of utilization before the campaign and thus had a marginally significantly greater change in utilization from before the campaign started to after compared to children (DID Estimator: 2.96, CI 0.00–5.91, p=0.050). The results did not change in our sensitivity analysis using different time frames (Appendix Table 3 and Figure 1).
Table 2.
Difference in difference analysis of the proportion of children and adults who underwent a CT for evaluation of nephrolithiasis per quarter for all stone episodes (incident + recurrent stones).
| CT-Rate | Pre-intervention Slope | Post-Intervention Slope | Intervention Differences | Lower Bound 95% CI | Upper Bound 95% CI | p-value |
|---|---|---|---|---|---|---|
| Children | 5.07 | −2.01 | −7.08 | −9.62 | −4.54 | <0.001 |
| Adult | 7.22 | −2.82 | −10.03 | −11.54 | −8.53 | <0.001 |
| Difference | −2.15 | 0.81 | 2.96 | 0.00 | 5.91 | 0.05 |
Figure 1.
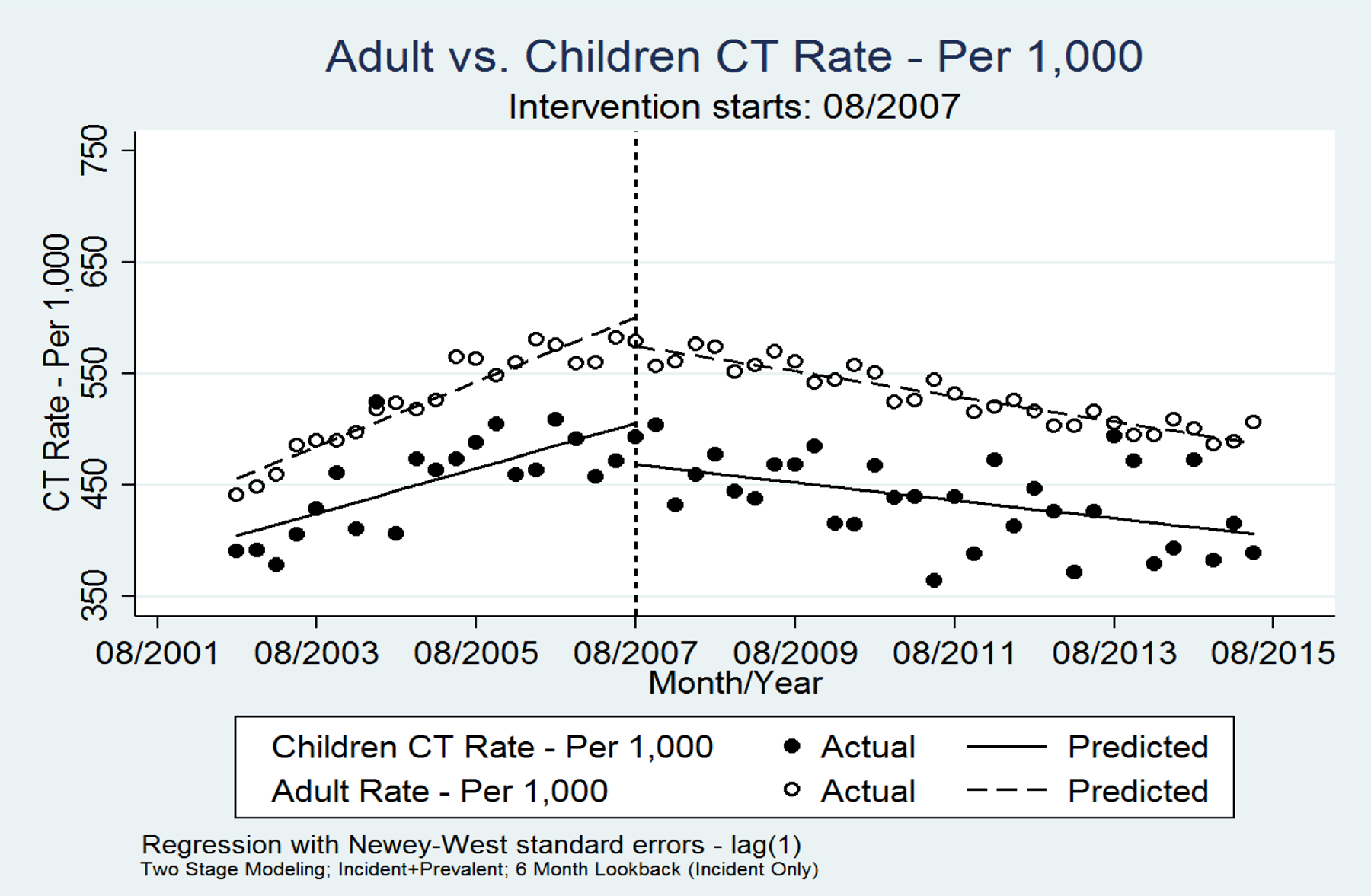
Difference–in-difference analysis of the proportion of children and adults who underwent a CT for evaluation of nephrolithiasis per quarter for all stone episodes (incident + recurrent stones).
A similar trend was noted for patients with incident stones, although the difference between children and adults was not significant (Table 3a and Figure 2a). Although the overall pattern in CT utilization for adults with a recurrent stone episode was also similar (Table 3b and Figure 2b), there were too few children with recurrent stones to allow for comparison.
Table 3.
Difference in difference analysis of the proportion of children and adults who underwent a CT for evaluation of nephrolithiasis per quarter: a) incident stone episodes, b) recurrent stone episodes.
| CT-Rate | Pre-intervention Slope | Post-Intervention Slope | Intervention Differences | Lower Bound 95% CI | Upper Bound 95% CI | p-value |
|---|---|---|---|---|---|---|
| Children | 5.02 | −3.05 | −8.07 | −10.88 | −5.26 | <0.001 |
| Adult | 6.89 | −3.42 | −10.31 | −12.00 | −8.62 | <0.001 |
| Difference | −1.88 | 0.37 | 2.24 | −1.04 | 5.52 | 0.18 |
| CT-Rate | Pre-intervention Slope | Post-Intervention Slope | Intervention Differences | Lower Bound 95% CI | Upper Bound 95% CI | p-value |
| Children | 5.33 | −0.32 | −5.65 | −8.92 | −2.39 | 0.001 |
| Adult | 7.50 | −1.98 | −9.48 | −11.05 | −7.91 | <0.001 |
| Difference | −2.17 | 1.66 | 3.83 | 0.20 | 7.45 | 0.04 |
Figure 2.
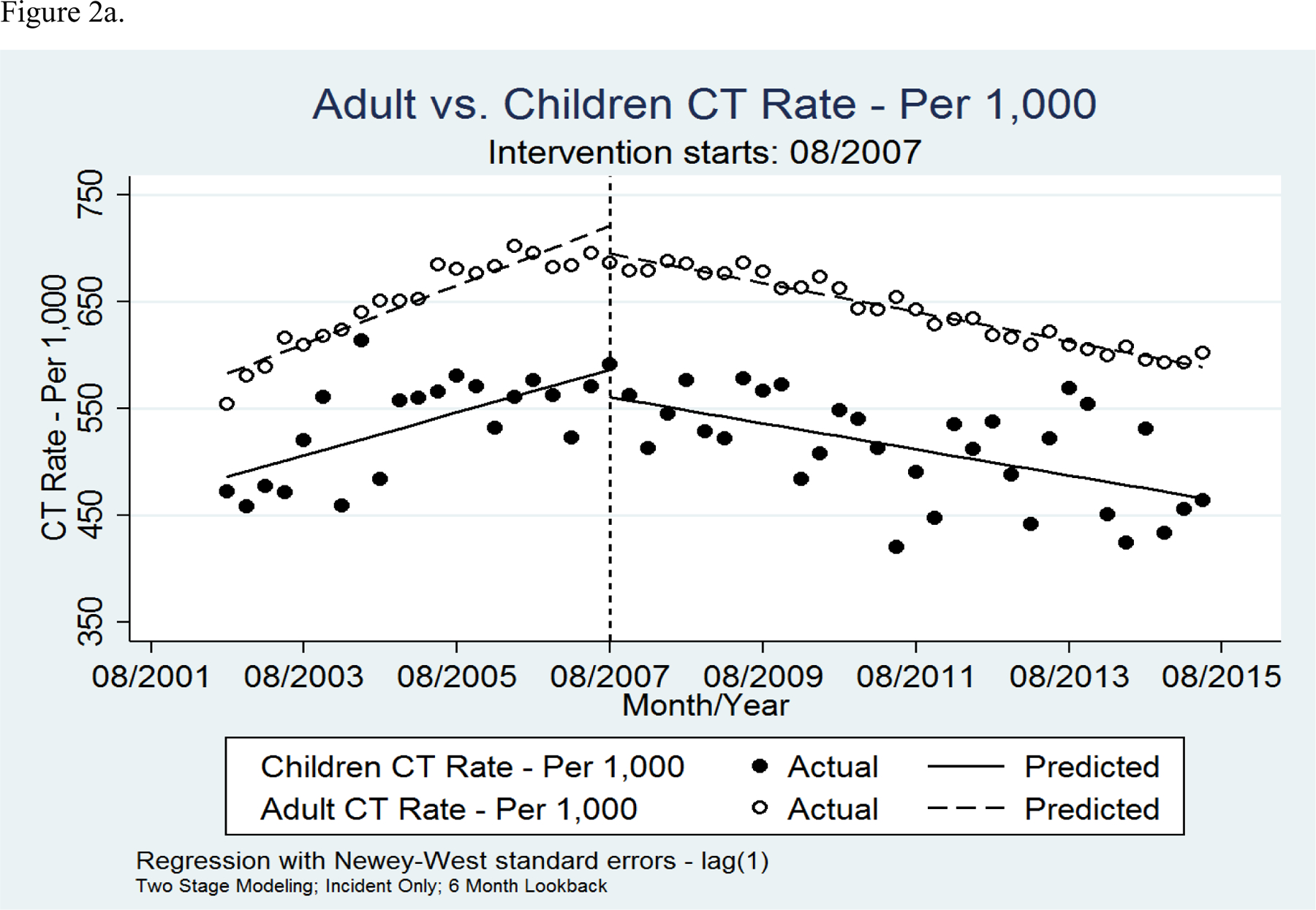
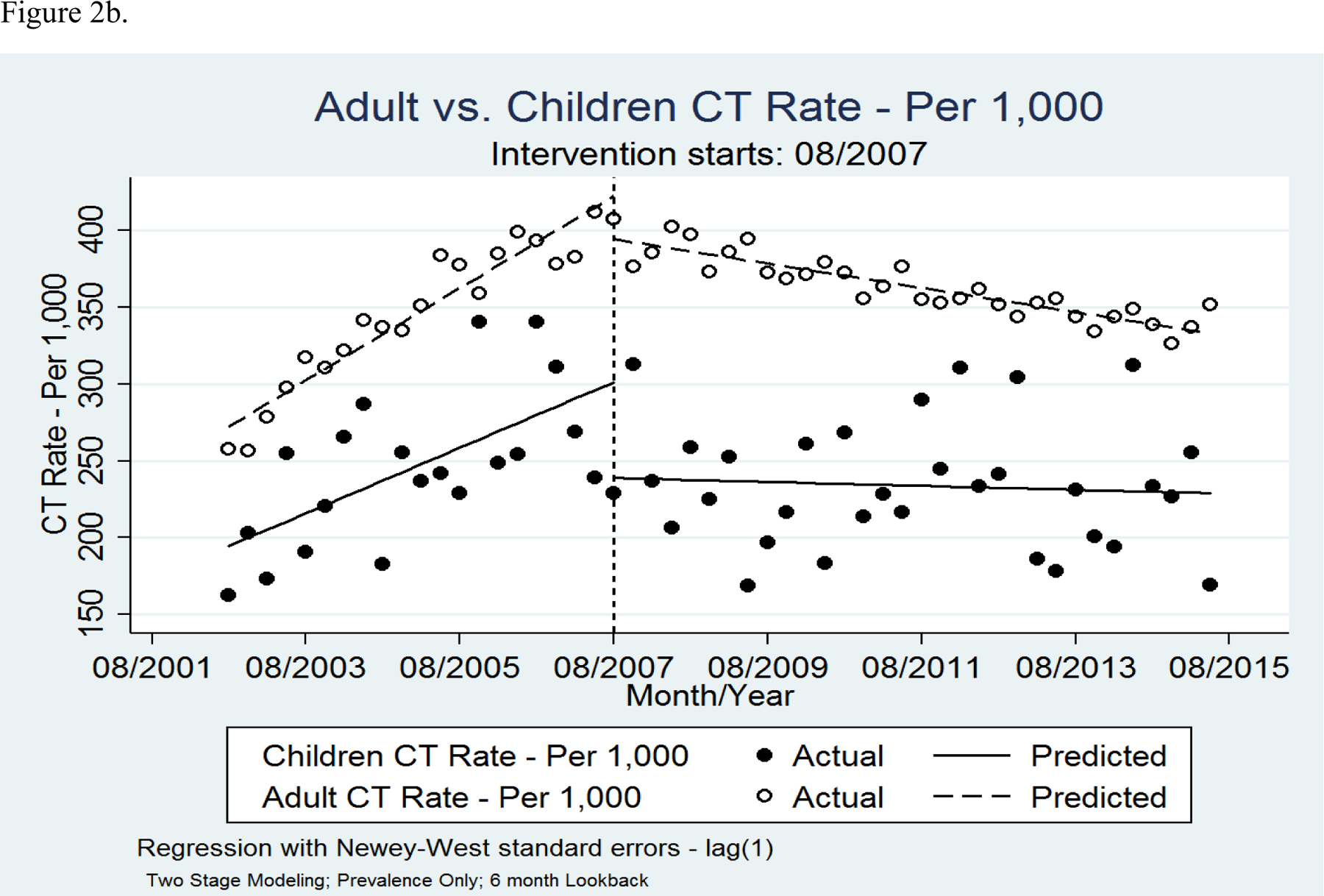
Difference–in-difference analysis of the proportion of children and adults who underwent a CT for evaluation of nephrolithiasis per quarter: a) incident stone episodes b) recurrent stone episodes.
The utilization of the various imaging modalities for evaluation of kidney stones changed over this time period in both children and adults (Figures 3a and 3b). For children, the use of CT has been decreasing since 2007. The use of RUS has been increasing over this time period such that in 2012, it became more frequently utilized than CT. The use of AXR has stayed stable. CT was the sole imaging modality used for 26.2–31.1% of pediatric stone episodes and in addition to other imaging for 24.9–27.8% of pediatric stone episodes (Appendix Table 4). For adults, the use of CT has also been decreasing, but the increase in the use of RUS has been modest and the use of AXR has decreased.
Figure 3.
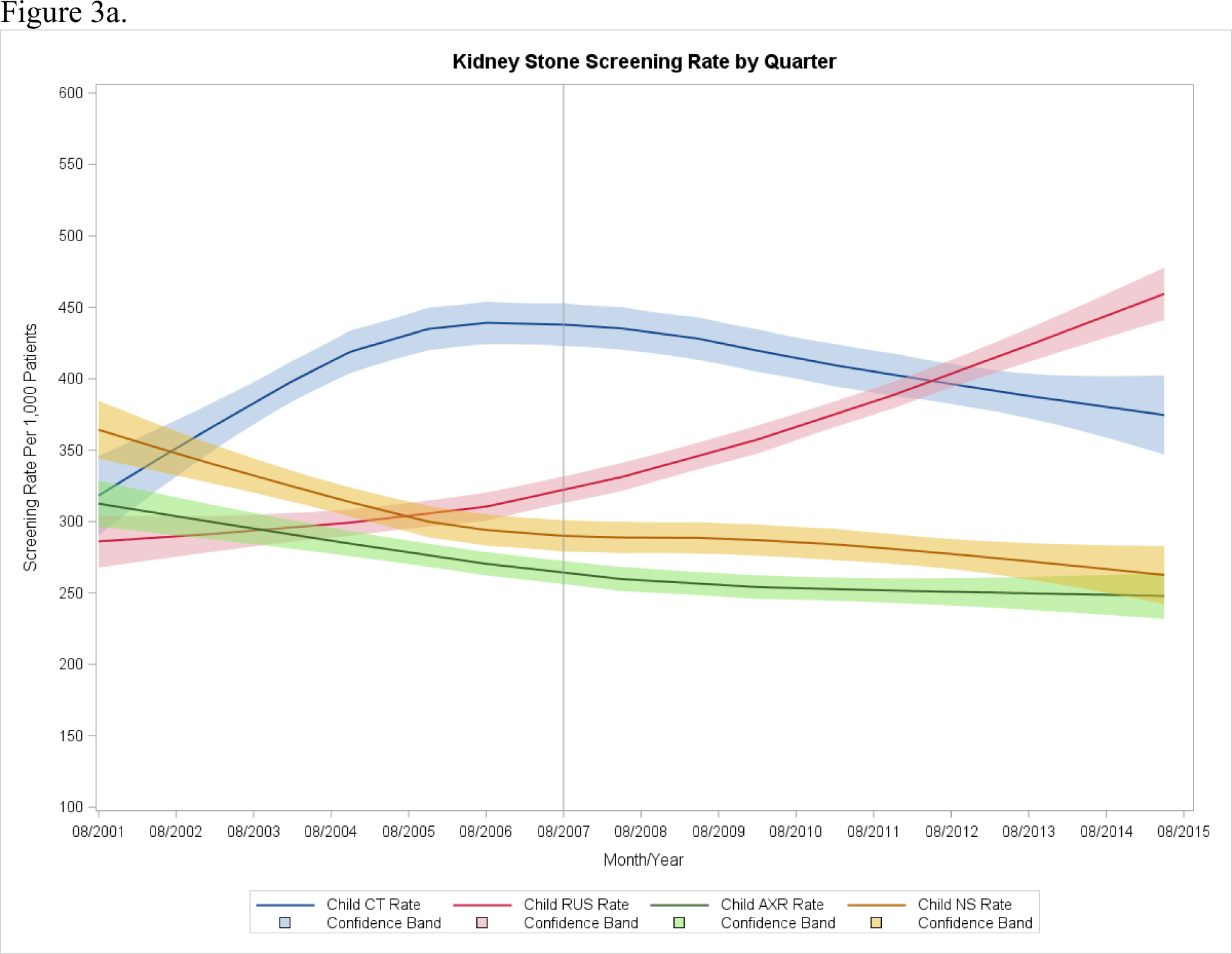
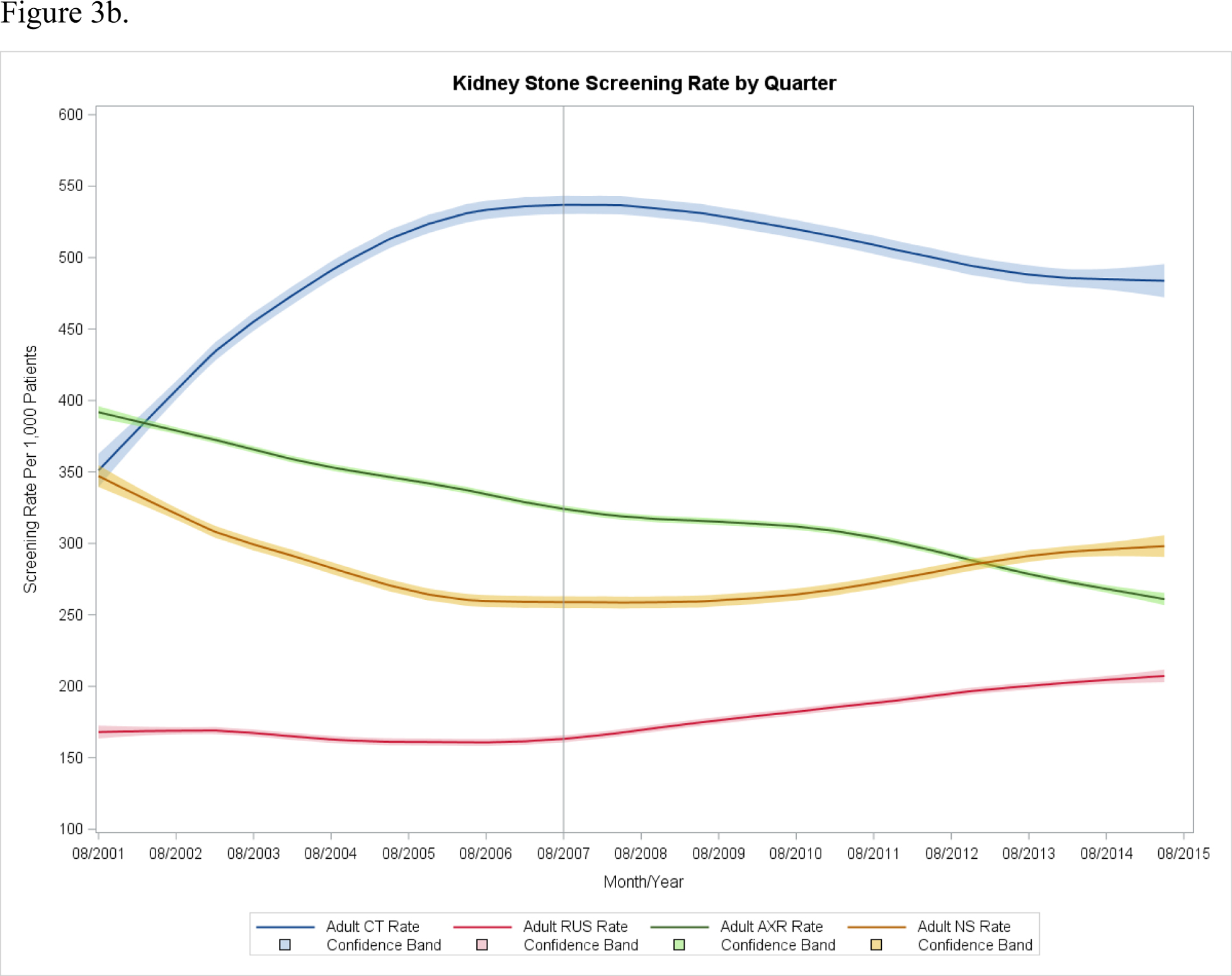
Imaging modalities used to evaluate kidney stones per quarter: a) children b) adults.
Discussion
The use of CT to evaluate kidney stones was increasing at a similar rate for both children and adults prior the launch of the Image Gently Campaign® in 2007. Since that time, it has been decreasing at a similar rate in both groups, although at a slightly greater rate in adults compared to children, suggesting that suggest that the Image Gently Campaign® alone did not lead to the decrease in children’s CT utilization. For children, with the decreased use of CT there has been an increase in the use of RUS such that it is now the most common imaging modality used to evaluate pediatric stones. For adults, the use of RUS has been increasing only modestly and CT remains by far the most commonly used imaging modality. Both pediatric and adult patients seen initially in the ED are most likely to be evaluated with a CT compared to those patients initially seen in an outpatient clinic.
Similar trends of CT utilization for evaluation of nephrolithiasis over this time period have been described. A study using the National Hospital Ambulatory Care Survey demonstrated a 5-fold increase in utilization for both children and adults between 1996 and 2007.18,19 A review of two tertiary EDs demonstrated a peak in CT use in 2008, followed by a decline in 2008–2010.20 A study use the Nationwide Emergency Department also demonstrated a peak in CT use in EDs in 2007 followed by a decline between 2008–2010.21 Finally, a Marketscan study showed an increase in the use of CT for evaluation of pediatric nephrolithiasis between 2003–2006 followed by a decrease in 2007–2011.22
The difference in utilization trends between adults and children differed from our hypothesis. While the use of CT decreased for both adults and children, there was a greater change in the adult cohort. This could be because adults had a higher rate of CT utilization initially and therefore more room for improvement by eliminating unnecessary exams. Interestingly, adults did not see the increase in RUS utilization that children did. This may be due in part to the decreased sensitivity of RUS for detecting stones in adults compared to children.
The growing awareness of the harmful effects of ionizing radiation among providers, patients, and families may have influenced the change in CT utilization. The initial rapid increase in the utilization of CT seen in the late 1990s was met with growing concern about potential harms. By 2005, the World Health Organization, Centers for Disease Prevention and Control, and United States Department of Health and Human Resources had all added x-rays and gamma-rays to their lists of carcinogens and the Food and Drug Administration and National Cancer Institute had started advocating for minimizing radiation exposure from medical imaging in children.23–26 There was also growing research on this subject. Indeed, the number of scientific manuscripts about the harms of radiation on PubMed more than tripled between 1995 and 2015 (Figure 4a). There were several alarming studies published, most famously by Brenner et al estimating that 500 children annually would develop lethal cancer from CT scans (Brenner D 2001).3 Although the validity of the methodology used to obtain these estimates have since been questioned, these warnings and alarming research findings were often prominently publicized in the lay press.27 The trends in publications in the lay press about the harms of medical imaging mirror the trends of the medical literature (Figure 4b), leading to increased public awareness. Therefore, the Image Gently® Campaign, as well as the adult-focused Image Wisely® Campaign it helped launch in 2010, likely served as one voice of many calling on providers to avoid unnecessary radiation.4,28
Figure 4.
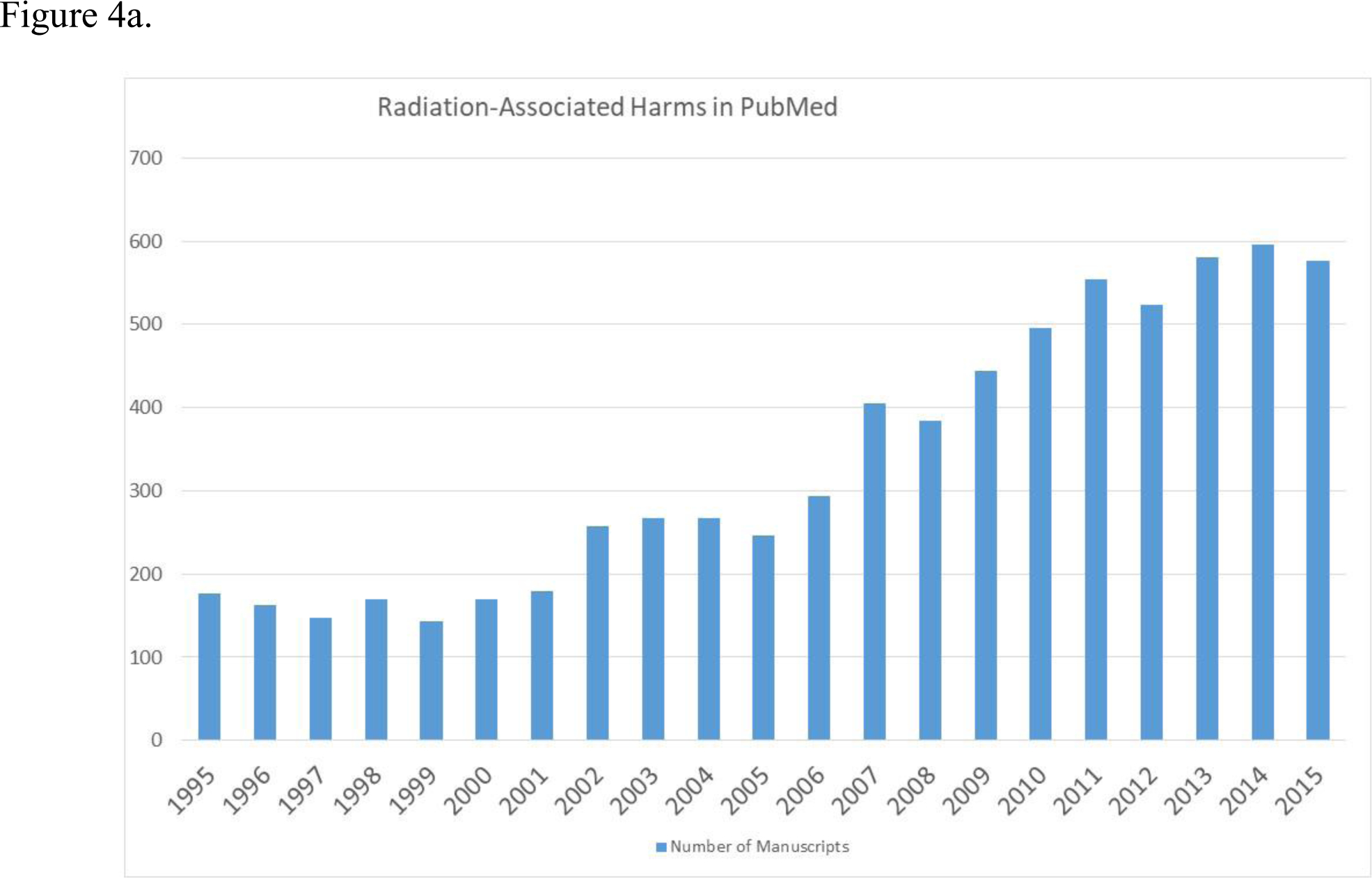
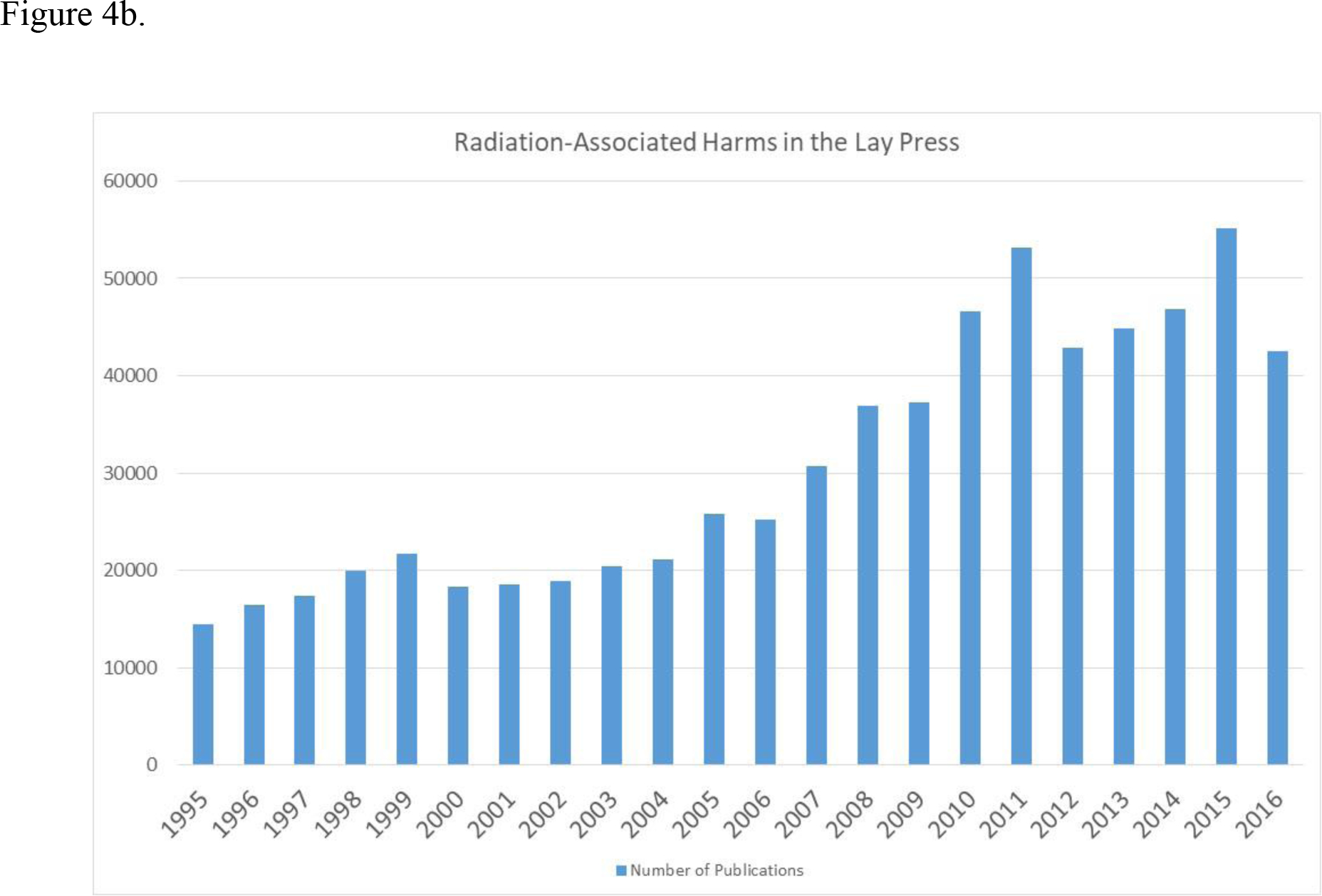
Number of publications published by year on the harms of medical imaging in a) scientific journals (PubMed) b) lay press (ProQuest).
There are several limitations to this study. First, this type of analysis can only determine if the campaign alone led to a decrease in the use of CT, but cannot determine the true underlying cause(s) or the degree to which the campaign may have had some influence. It is possible that although the Image Gently® Campaign was focused on the pediatric population, there were spillover effects on adults by generally raising awareness of imaging utilization and eventually helping to launch the Image Wisely® Campaign in adults. This may have been particularly true at centers who care for both children and adults. However, we would not expect a pediatric-focused campaign to be more efficacious for adults then for children. Therefore, the reason for the change seen is likely multifactorial. As this cohort represents all patients with the same major national insurance provider, it is possible that a different trend exists for patients with public insurance or who are uninsured. Additionally, we are unable to determine what proportion of CTs obtained were clinically indicated, although half of the children in this study underwent a CT only without an initial RUS, which goes against the guidelines. There is also evidence that CTs performed for the evaluation of stones in children are usually not necessary.29 We were unable to account for certain patient and hospital factors that could have influenced whether a CT was performed in our model, such as evaluation at a pediatric versus adult hospital or the stone burden of the patient. It is also unclear how many EDs had regular access to ultrasonography and performed CTs due to a lack of an alternative. Some centers may have chosen to perform low-dose renal colic protocol CT. However, many low-dose CTs are not appropriately dosed.30 There may be additional reasons why a CT was not ordered that cannot be ascertained by this type of study. Finally, this study analyzed only patients with a confirmed diagnosis of nephrolithiasis. It is possible that ultrasound was more frequently used in patients with negative results for stones than those with confirmed stones.
Conclusions
The use of CT for evaluation of kidney stones has been decreasing for both children and adults since 2007. However, it is unlikely this change can be attributed to the Image Gently® Campaign alone. Nonetheless, given the persistent high utilization of CT, the mission of the campaign remains relevant. Future initiatives should focus on educating emergency providers about how kidney stone imaging guidelines differ for children and adults. Additionally, obtaining informed consent for studies involving ionizing radiation could help increase patient, family, and provider awareness.
Supplementary Material
Funding Source:
This research was funded by a T-32 training grant from the National Institute of Health’s National Institute of Diabetes and Digestive and Kidney Diseases (grant number 5T32DK007782-17).
Abbreviations:
- CT
Computed tomography
- DID
difference-in-differences
- RUS
Renal ultrasound
- AXR
Abdominal X-ray
- ED
Emergency Department
References
- 1.Linton OW, Mettler FA Jr., National conference on dose reduction in CT, with an emphasis on pediatric patients. AJR American journal of roentgenology. 2003;181(2):321–329. [DOI] [PubMed] [Google Scholar]
- 2.Tasian GE, Copelovitch L. Evaluation and medical management of kidney stones in children. The Journal of urology. 2014;192(5):1329–1336. [DOI] [PubMed] [Google Scholar]
- 3.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR American journal of roentgenology. 2001;176(2):289–296. [DOI] [PubMed] [Google Scholar]
- 4.Brink JA, Amis ES Jr., Image Wisely: a campaign to increase awareness about adult radiation protection. Radiology. 2010;257(3):601–602. [DOI] [PubMed] [Google Scholar]
- 5.Smith-Bindman R, Bindman AB. Imaging More Wisely. JAMA internal medicine. 2016;176(2):168–170. [DOI] [PubMed] [Google Scholar]
- 6.Alliance IG. Image Gently Mission Statement Update. 2014. https://www.imagegently.org/
- 7.Frush DP, Strauss KJ. Image Gently: Getting It Right. Journal of the American College of Radiology : JACR. 2017;14(4):575–576. [DOI] [PubMed] [Google Scholar]
- 8.Routh JC, Graham DA, Nelson CP. Epidemiological trends in pediatric urolithiasis at United States freestanding pediatric hospitals. The Journal of urology. 2010;184(3):1100–1104. [DOI] [PubMed] [Google Scholar]
- 9.Abhishek, Kumar J, Mandhani A, Srivastava A, Kapoor R, Ansari MS. Pediatric urolithiasis: experience from a tertiary referral center. J Pediatr Urol. 2013;9(6 Pt A):825–830. [DOI] [PubMed] [Google Scholar]
- 10.Riccabona M, Avni FE, Blickman JG, et al. Imaging recommendations in paediatric uroradiology. Minutes of the ESPR uroradiology task force session on childhood obstructive uropathy, high-grade fetal hydronephrosis, childhood haematuria, and urolithiasis in childhood. ESPR Annual Congress, Edinburgh, UK, June 2008. Pediatric radiology. 2009;39(8):891–898. [DOI] [PubMed] [Google Scholar]
- 11.Fulgham PF, Assimos DG, Pearle MS, Preminger GM. Clinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessment. The Journal of urology. 2013;189(4):1203–1213. [DOI] [PubMed] [Google Scholar]
- 12.Tasian GE, Pulido JE, Keren R, et al. Use of and regional variation in initial CT imaging for kidney stones. Pediatrics. 2014;134(5):909–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Routh JC, Graham DA, Nelson CP. Trends in imaging and surgical management of pediatric urolithiasis at American pediatric hospitals. The Journal of urology. 2010;184(4 Suppl):1816–1822. [DOI] [PubMed] [Google Scholar]
- 14.Coursey CA, Casalino DD, Remer EM, et al. ACR Appropriateness Criteria(R) acute onset flank pain--suspicion of stone disease. Ultrasound quarterly. 2012;28(3):227–233. [DOI] [PubMed] [Google Scholar]
- 15.Miller OF, Kane CJ. Time to stone passage for observed ureteral calculi: a guide for patient education. The Journal of urology. 1999;162(3 Pt 1):688–690; discussion 690681. [DOI] [PubMed] [Google Scholar]
- 16.Linden A, Adams JL. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. Journal of evaluation in clinical practice. 2011;17(6):1231–1238. [DOI] [PubMed] [Google Scholar]
- 17.How CMS measures the “30-Day All Cause Rehospitalization Rate” on the Hospital Compare Web Site. Content last reviewed March 2013. Agency for Healthcare Research and Quality, Rockville, MD. [Google Scholar]
- 18.Larson DB, Johnson LW, Schnell BM, Goske MJ, Salisbury SR, Forman HP. Rising use of CT in child visits to the emergency department in the United States, 1995–2008. Radiology. 2011;259(3):793–801. [DOI] [PubMed] [Google Scholar]
- 19.Larson DB, Johnson LW, Schnell BM, Salisbury SR, Forman HP. National trends in CT use in the emergency department: 1995–2007. Radiology. 2011;258(1):164–173. [DOI] [PubMed] [Google Scholar]
- 20.Menoch MJ, Hirsh DA, Khan NS, Simon HK, Sturm JJ. Trends in computed tomography utilization in the pediatric emergency department. Pediatrics. 2012;129(3):e690–697. [DOI] [PubMed] [Google Scholar]
- 21.Johnson EK, Graham DA, Chow JS, Nelson CP. Nationwide emergency department imaging practices for pediatric urolithiasis: room for improvement. The Journal of urology. 2014;192(1):200–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tasian GE, Pulido JE, Keren R, et al. Use of and regional variation in initial CT imaging for kidney stones. Pediatrics. 2014;134(5):909–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.IARC monograms on the evaluation of carcinogenic risks to humans List of classifications, volumes 1–120. World Health Organization. International Agency for Research on Cancer; https://monographs.iarc.fr/list-of-classifications-volumes/ [Google Scholar]
- 24.Public health statement for ionizing radiation. Centers for Disease Control and Prevention. Agency for toxic substances and disease registry; https://www.atsdr.cdc.gov/phs/phs.asp?id=482&tid=86 [Google Scholar]
- 25.Report on carcinogens. Fourteenth edition. U.S. Department of Health and Human Services. National Toxicology Program; https://ntp.niehs.nih.gov/ntp/roc/content/profiles/ionizingradiation.pdf [Google Scholar]
- 26.FDA public health notification: reducing radiation risk from computed tomography for pediatric and small adult patients. Pediatric radiology. 2002;32(4):314–316. [DOI] [PubMed] [Google Scholar]
- 27.Stemberg S. CT scans in children linked to cancer. USA Today 2001. [Google Scholar]
- 28.Mayo-Smith WW, Morin RL. Image Wisely: The Beginning, Current Status, and Future Opportunities. Journal of the American College of Radiology : JACR. 2017;14(3):442–443. [DOI] [PubMed] [Google Scholar]
- 29.Johnson EK, Faerber GJ, Roberts WW, et al. Are stone protocol computed tomography scans mandatory for children with suspected urinary calculi? Urology. 2011;78(3):662–666. [DOI] [PubMed] [Google Scholar]
- 30.Smith-Bindman R, Moghadassi M, Griffey RT, et al. Computed Tomography Radiation Dose in Patients With Suspected Urolithiasis. JAMA internal medicine. 2015;175(8):1413–1416. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


