Abstract
Background
Numerous fixed-stem implants exist for radial head arthroplasty; therefore, we conducted a systematic review to compare the safety and efficacy of different types of fixed-stem implants.
Methods
We conducted a literature search, updated from a previous systematic review, to identify studies evaluating a fixed-stem radial head arthroplasty implant for any indication. We extracted data on revision rates, specific complications, and functional scores. We pooled results across studies using a random-effects method, using proportions for dichotomous data and mean values for functional scores. We analyzed outcomes by indication and specific implant.
Results
We included 31 studies. Studies included patients with radial head fractures only, terrible-triad injuries, or Essex-Lopresti injuries or included a heterogeneous population. We identified 15 different fixed-stem implants. The results of our analysis revealed that patients with terrible-triad injuries may be at an increased risk of revision and instability and patients with Essex-Lopresti injuries may be at an increased risk of arthritis, capitellar erosion, and osteolysis. After removing these outliers and pooling the results by specific device, we observed variability across devices in the rates of revision, arthritis, capitellar erosion, instability, and osteolysis, as well as in functional scores.
Conclusion
Differences were seen across different implants in revision rates, certain complications, and functional scores. This study highlighted that these devices should be evaluated within the context of the patient population under examination, as patients with Essex-Lopresti or terrible-triad injuries may demonstrate worse outcomes relative to those with a fracture only.
Keywords: Radial head fracture, arthroplasty, prosthesis, fixed stem, systematic review, meta-analysis
Radial head fractures account for approximately one-third of all adult elbow fractures.17,36 Under the Mason classification system, radial head fractures are classified as either with displacement or without displacement.19,36 Radial head arthroplasty (RHA) is a surgical option for displaced radial head fractures.1 Current RHA can be classified as unfixed or fixed depending on how rigidly secured the implant is within the radial neck. Unfixed, or loose, implants have smooth shafts and allow for motion to occur within the medullary canal.1 Fixed, or press-fit, implants rigidly secure the implant within the canal of the radial neck.1 The type of implant may influence elbow stability and postoperative outcomes.4
Agyeman et al1 conducted a systematic review to study the differences between the 2 fixation methods of RHA: fixed and unfixed. They concluded that implant fixation type does not appear to affect functional outcomes; however, their results suggested that rigidly fixed implants may increase the risks of revision and overall complications.
Numerous fixed-stem implants exist, with devices being manufactured by various companies. Currently, all fixed-stem RHA implants have been considered equal; therefore, we conducted a systematic review to evaluate the different types of fixed-stem implants in terms of their safety and efficacy. We hypothesized that differences exist between these implants and they should not be considered the same.
Methods
Search strategy
We conducted an updated systematic review using the same methodology reported by Agyeman et al.1 Electronic literature searches were conducted in the MEDLINE and Embase databases using the following search algorithm: radial head AND (arthroplasty OR prosthesis OR replacement). The search was conducted from January 22, 2017—as this was the date reported by Agyeman et al—to November 20, 2018.
Eligibility criteria
We included any clinical study published in English evaluating the use of an RHA device for any indication; however, we only included studies that evaluated a fixed-stem implant.
Data extraction
We collected information from each study including the year of publication, country of publication, study design, follow-up period, patient demographic characteristics, indications, and specific device. We also extracted outcome data to compare revision rates (secondary surgery for implant revision or removal), specific complication rates (arthritis, capitellar erosion, instability, and osteolysis), and functional scores (reported with either the Mayo Elbow Performance Score [MEPS] or Disabilities of the Arm, Shoulder and Hand [DASH] score).
Data analysis
We analyzed the outcome data using Open Meta-analyst software, pooling results across studies for each fixed-stem device using the DerSimonian-Laird random-effects method.38 Dichotomous data (revision and complications) were reported as the proportion of patients experiencing the event, and continuous data (function) were reported as mean scores on the MEPS or DASH questionnaire, with the associated 95% confidence intervals (CIs) for each estimate. For the MEPS, a higher score is indicative of a more favorable outcome, whereas for the DASH questionnaire, a lower score is more favorable. We also analyzed outcomes by injury type (ie, fracture only, heterogeneous population, Essex-Lopresti, or terrible triad) to investigate if certain patient populations demonstrated an increased risk of experiencing an event. If so, we conducted sensitivity analyses removing such outliers to limit the influence of confounding factors when interpreting the results and comparing effect estimates between the different implants. We also performed a subgroup analysis, grouping devices as either bipolar or monopolar implants.
Results
Search results
We screened a total of 117 titles and abstracts (Fig. 1). Of these, 39 were included for full-text review, and a total of 9 studies were deemed eligible.13,14,20,21,27,29,31,34,35 In addition, 22 studies from the publication by Agyeman et al1 were eligible,2,3,5,7, 8, 9, 10, 11, 12,15,16,18,22, 23, 24, 25, 26,28,30,32,33,37 giving a total of 31 studies for the final analysis.
Figure 1.
Flow diagram of included studies. RHA, radial head arthroplasty.
Description of included studies
The included studies were published from 2001 to 2018 and were conducted across 15 different countries (Table I). The study sample sizes for each RHA device ranged from 6 to 63 patients, with an average length of follow-up ranging from 10.5 to 110.4 months (9.2 years). The average age of the patients ranged from 36 to 62 years, and the proportion of male patients ranged from 12.5% to 83.3%. In terms of the indications for surgery, the majority of studies included patients with radial head fractures only (23 studies), whereas the remaining studies included a heterogeneous population (5 studies), patients with a terrible-triad injury (2 studies), or patients with an Essex-Lopresti injury (1 study). Among the 31 included studies, the authors of 24 studies declared no financial conflicts or competing interests, 4 studies were published by authors who received benefits or consulting fees from third parties, and such disclosures were not reported in the remaining 3 studies.
Table I.
Included studies
| Author, year | Country | Design | Patients, n | Average follow-up, mo | Age, yr | Male/female, n | Indication | Device (company) |
|---|---|---|---|---|---|---|---|---|
| Gramlich et al,13 2019 | Germany | Retrospective | 35 | 32.4 | 48 | 22/13 | Fractures only | MoPyC (Tornier) |
| 31 | 53.3 | 47 | 19/12 | Fractures only | rHead (SBi/Stryker) | |||
| Hari Krishnan, and Gupta,14 2019 | India | Prospective | 30 | 24 | 36 | 21/9 | Fractures only | NR (Phoenix Surgical) |
| Laflamme et al,20 2017 | Canada | Retrospective | 36 | 48 | 52.8 | 28/29 | Fractures only | ExploR (Zimmer-Biomet) |
| Laumonerie et al,21 2017 | France | Retrospective | 36 | 110.4 | NR | NR | Fractures only | Guepar (SBi/Stryker) |
| 24 | 36.7 | NR | NR | Fractures only | Evolutive (Aston Medical) | |||
| 10 | 62.8 | NR | NR | Fractures only | rHead RECON (SBi/Stryker) | |||
| 7 | 53.2 | NR | NR | Fractures only | rHead (SBi/Stryker) | |||
| Nestorson et al,27 2017 | Sweden | Retrospective | 8 | 75.1 | 59.1 | NR | Fracture only | rHead (SBi/Stryker) |
| 10 | 56 | 50.2 | NR | Fracture only | Anatomic Radial Head (Acumed) | |||
| Ricon et al,29 2018 | Spain | Retrospective | 18 | 79.8 | 48 | 13/5 | Fractures only | MoPyC (Tornier) |
| Rodriguez-Quintana et al,31 2017 | Puerto Rico | Prospective | 14 | 24 | 54.71 | 6/8 | Terrible-triad injuries | Anatomic Radial Head (Acumed) |
| Sullivan et al,34 2017 | United States | Retrospective | 19 | 10.5 | NR | NR | Fracture only | Radial Head Prosthesis (Synthes) |
| 63 | 19.1 | NR | NR | Fracture only | ExploR (Zimmer-Biomet) | |||
| Tarallo et al,35 2017 | Italy | Retrospective | 31 | 30 | 52 | 21/10 | Fractures only | Anatomic Radial Head (Acumed) |
| Allavena et al,2 2014 | France | Retrospective | 22 | 50 | 44 | 15/7 | Terrible-triad injuries | Guepar (SBi/Stryker) |
| Berschback et al,3 2013 | United States | Retrospective | 13 | 33 | 46 | 8/5 | Essex-Lopresti injuries | Anatomic Radial Head (Acumed) |
| Brinkman et al,5 2005 | Holland | Retrospective | 11 | 24 | 43 | 8/3 | Fractures only | Judet (Tornier) |
| Burkhart et al,7 2010 | Germany | Retrospective | 17 | 106 | 44.1 | 14/3 | Heterogeneous population | Judet (Tornier) |
| Celli et al,8 2010 | Italy | Retrospective | 16 | 41.7 | 46.1 | 11/5 | Fractures only | Judet (Tornier) |
| Chapman et al,9 2006 | United States | Retrospective | 16 | 37 | 50 | 9/7 | Heterogeneous population | Solar (Stryker) |
| Dotzis et al,10 2006 | France | Retrospective | 12 | 63 | 44.8 | 10/4 | Fractures only | Judet (Tornier) |
| El Sallakh,11 2013 | Egypt | Retrospective | 12 | 42 | 39 | 5/7 | Fractures only | Anatomic Radial Head (Acumed) |
| Gauci et al,12 2016 | France | Retrospective | 52 | 46 | 52 | 30/35 | Heterogeneous population | MoPyC (Tornier) |
| Heijink et al,15 2016 | The Netherlands | Retrospective | 25 | 50 | 55 | 7/18 | Fractures only | RHS (Tornier) |
| Katthagen et al,16 2013 | Germany | Retrospective | 29 | 25 | 60 | 8/23 | Heterogeneous population | Corin (Corin Group) |
| Kodde et al,18 2016 | The Netherlands | Retrospective | 30 | 48 | 48 | 9/21 | Fractures only | Judet (Tornier) |
| Levy et al,22 2016 | United States | Retrospective | 15 | 26 | 62 | 9/6 | Fractures only | Anatomic Radial Head (Acumed) |
| Lim and Chan,23 2008 | Singapore | Retrospective | 6 | 29.7 | 53 | 2/4 | Fractures only | Vitallium (Howmedica) |
| Lopiz et al,24 2016 | Spain | Retrospective | 14 | 42 | 54 | 6/8 | Fractures only | MoPyC (Tornier) |
| Moro et al,25 2001 | Canada | Retrospective | 24 (25 elbows) | 39 | 54 | 11/13 | Fractures only | Richards (Smith & Nephew) |
| Mou et al,26 2015 | China | Retrospective | 12 | 60.8 | 41 | 6/6 | Fractures only | Anatomic Radial Head (Acumed) |
| Popovic et al,28 2007 | Belgium | Retrospective | 51 | 101 | 51 | 32/19 | Fractures only | Judet (Tornier) |
| Ricon et al,30 2012 | Spain | Retrospective | 28 | 32 | 54 | 11/17 | Fractures only | MoPyC (Tornier) |
| Rotini et al,32 2012 | Italy | Retrospective | 30 (31 elbows) | 24 | 44 | 19/11 | Heterogeneous population | rHead (SBi/Stryker) |
| Sarris et al,33 2012 | Greece | Retrospective | 32 | 27 | 54 | 20/12 | Fractures only | MoPyC (Tornier) |
| Viveen et al,37 2017 | The Netherlands | Prospective | 16 | 75 | 49 | 2/14 | Fractures only (all revised cases) | Judet (Tornier) |
NR, not reported.
In terms of the specific fixed-stem implants, the studies evaluated devices from Acumed (Anatomical Radial Head [versions not reported; Hillsboro, OR, USA]), Aston Medical (Evolutive; Surrey, UK), Corin Group (Corin; Cirencester, UK), Howmedica (Vitallium; IN, USA), Phoenix Surgical (Cape Town, South Africa), SBi/Stryker (Guepar, rHead, rHead RECON, and Solar; Kalamazoo, MI, USA), Smith & Nephew (Richards; London, UK), Synthes (Radial Head Prosthesis; Warsaw, IN, USA), Tornier (Judet, MoPyC, and RHS; Edina, MN, USA), and Zimmer-Biomet (ExploR; Warsaw, IN, USA).
Revision rates
Figure 2 displays the revision rates by indication. Studies on patients with terrible-triad injuries demonstrated a remarkably higher event rate than studies on the other patient populations and were removed from the analysis of revision rates by specific RHA device (Fig. 3). Relative to the overall revision rate for all fixed-stem devices (11.7%; 95% CI, 8.5%-14.9%), pooled rates were lower, based on the point estimates, for 7 of the 15 different devices, ranging between 4.4% and 10.5%: Anatomical Radial Head (Acumed), ExploR (Zimmer-Biomet), Judet (Tornier), Phoenix Surgical device, Vitallium (Howmedica), Radial Head System (Tornier), and Radial Head Prosthesis (Synthes). The remaining devices demonstrated revision rates ranging between 13.8% and 60%.
Figure 2.
Revision rates (percentages) by indication. LCI, lower limit of confidence interval; UCI, upper limit of confidence interval.
Figure 3.
Revision rates (percentages) by device. Studies on patients with terrible-triad injuries were removed. LCI, lower limit of confidence interval; UCI, upper limit of confidence interval.
Complications
Patients with Essex-Lopresti injuries demonstrated remarkably higher rates of arthritis and were not included in the analysis of arthritis rates by specific RHA device (Fig. 4). Relative to the overall rate of development of arthritis for all fixed-stem devices (34.6%; 95% CI, 18%-51.2%), pooled rates were lower for 5 of the 9 different devices included in the analysis, ranging from 4.5% to 28.2%: Guepar (SBi/Stryker), Anatomic Radial Head (Acumed), Corin (Corin Group), Richards (Smith & Nephew), and rHead (SBi/Stryker). The remaining devices demonstrated arthritis rates ranging between 44% and 61.6%.
Figure 4.
Arthritis rates (percentages) by device. Studies on patients with Essex-Lopresti injuries were removed. LCI, lower limit of confidence interval; UCI, upper limit of confidence interval.
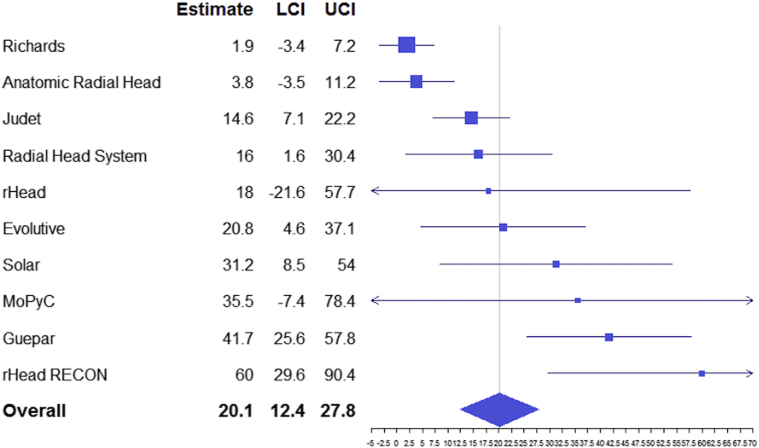
Patients with Essex-Lopresti injuries also showed a markedly increased risk of capitellar erosion and were removed from the analysis by RHA device (Fig. 5). Relative to the overall rate of capitellar erosion for all fixed-stem devices (20.1%; 95% CI, 12.4%-27.8%), pooled rates were lower for 5 of the 10 different devices eligible for the analysis, ranging from 1.9% to 18%: Richards (Smith & Nephew), Anatomic Radial Head (Acumed), Judet (Tornier), Radial Head System (Tornier), and rHead (SBi/Stryker). The remaining devices demonstrated capitellar erosion rates ranging between 20.8% and 60%.
Figure 5.
Capitellar erosion rates (percentages) by device. Studies on patients with Essex-Lopresti injuries were removed. LCI, lower limit of confidence interval; UCI, upper limit of confidence interval.
Patients with terrible-triad injuries showed a substantially higher rate of instability and were removed from the analysis by RHA device (Fig. 6). Relative to the overall rate of instability for all fixed-stem devices (5.7%; 95% CI, 3.1%-8.2%), pooled rates were lower for 4 of the 11 different devices included in the analysis, ranging from 1.7% to 4.4%: Corin (Corin Group), Anatomic Radial Head (Acumed), Solar (Stryker), and Judet (Tornier). The remaining devices demonstrated instability rates ranging between 6.7% and 19.9%.
Figure 6.
Instability rates (percentages) by device. Studies on patients with terrible-triad injuries were removed. LCI, lower limit of confidence interval; UCI, upper limit of confidence interval.
The rate of osteolysis was markedly greater in patients with an Essex-Lopresti injury, and such studies were removed from the analysis by RHA device (Fig. 7). Relative to the overall rate of osteolysis for all fixed-stem implants (40.1%; 95% CI, 27%-53.2%), pooled rates were lower for 6 of the 13 different devices eligible for the analysis, ranging from 1.7% to 39.9%: Corin (Corin Group), Anatomic Radial Head (Acumed), MoPyC (Tornier), Radial Head System (Tornier), Guepar (SBi/Stryker), and rHead (SBi/Stryker). The remaining devices demonstrated osteolysis rates ranging between 43.8% and 94.7%.
Figure 7.
Osteolysis rates (percentages) by device. Studies on patients with Essex-Lopresti injuries were removed. LCI, lower limit of confidence interval; UCI, upper limit of confidence interval.
Function
Figure 8 shows the analysis of function via the MEPS by RHA device. Relative to the overall MEPS for all fixed-stem implants (88.6 points; 95% CI, 86.6-90.5 points), pooled scores were greater for 4 of the 12 different devices eligible for the analysis, ranging from 89.6 to 96.2 points: ExploR (Zimmer-Biomet), Anatomic Radial Head (Acumed), MoPyC (Tornier), and Radial Head System (Tornier). The remaining devices demonstrated MEPS values ranging from 80 to 88 points.
Figure 8.
Mean functional scores by device: Mayo Elbow Performance Score. LCI, lower limit of confidence interval; UCI, upper limit of confidence interval.
Figure 9 shows the analysis of function on the DASH questionnaire by RHA device. Relative to the overall DASH score for all fixed-stem implants (15.2 points; 95% CI, 13.1-17.4 points), pooled scores were more favorable for 5 of the 11 different devices eligible for the analysis, ranging from 8.8 to 13.9 points: ExploR (Zimmer-Biomet), Judet (Tornier), Anatomic Radial Head (Acumed), Vitallium (Howmedica), and Evolutive (Aston Medical). The remaining devices demonstrated DASH scores ranging from 16.1 to 27.5 points.
Figure 9.
Mean functional scores by device: Disabilities of the Arm, Shoulder and Hand score. LCI, lower limit of confidence interval; UCI, upper limit of confidence interval.
Subgroup analysis
Of the 15 devices identified in this review, 9 were monopolar (Anatomic Radial Head, Corin, ExploR, MoPyC, Radial Head Prosthesis, rHead, Richards, Solar, and Vitallium) and 6 were bipolar (Evolutive, Guepar, Judet, Phoenix Surgical, rHead RECON, and RHS). The results of these analyses are summarized in Table II. Overall, monopolar devices demonstrated more favorable results for the majority of outcomes, except for DASH scores, in terms of the pooled point estimates; however, the analyses may be confounded by wide CIs and a high degree of heterogeneity.
Table II.
Subgroup analysis: monopolar vs. bipolar implants
| Outcome | Pooled estimate across monopolar implants | Pooled estimate across bipolar implants |
|---|---|---|
| Revision | ||
| No. of studies | 22 | 13 |
| Estimate (95% CI), % | 10.0 (6.7-13.4) | 14.5 (7.8-21.2) |
| P value for effect estimate | <.001 | <.001 |
| I2 for heterogeneity, % | 44.33 | 78.92 |
| P value for heterogeneity | .014 | <.001 |
| Arthritis | ||
| No. of studies | 10 | 9 |
| Estimate (95% CI), % | 28.3 (13.0-43.5) | 40.8 (12.6-69.0) |
| P value for effect estimate | <.001 | .005 |
| I2 for heterogeneity, % | 89.8 | 97.66 |
| P value for heterogeneity | <.001 | <.001 |
| Capitellar erosion | ||
| No. of studies | 9 | 11 |
| Estimate (95% CI), % | 18.7 (6.8-30.5) | 20.7 (12.5-28.9) |
| P value for effect estimate | .002 | <.001 |
| I2 for heterogeneity, % | 94.61 | 67.57 |
| P value for heterogeneity | <.001 | <.001 |
| Instability | ||
| No. of studies | 10 | 9 |
| Estimate (95% CI), % | 5.6 (1.5-9.6) | 7.0 (3.4-10.7) |
| P value for effect estimate | .007 | <.001 |
| I2 for heterogeneity, % | 46.89 | 0 |
| P value for heterogeneity | .05 | .879 |
| Osteolysis | ||
| No. of studies | 15 | 9 |
| Estimate (95% CI), % | 36.1 (19.1-53.0) | 46.8 (24.0-69.5) |
| P value for effect estimate | <.001 | <.001 |
| I2 for heterogeneity, % | 96.11 | 95.33 |
| P value for heterogeneity | <.001 | <.001 |
| MEPS | ||
| No. of studies | 17 | 10 |
| Estimate (95% CI), points | 89.48 (87.05-91.92) | 87.03 (84.24-89.81) |
| P value for effect estimate | <.001 | <.001 |
| I2 for heterogeneity, % | 73.64 | 50.98 |
| P value for heterogeneity | <.001 | .031 |
| DASH score | ||
| No. of studies | 12 | 7 |
| Estimate (95% CI), points | 16.17 (12.76-19.59) | 14.57 (11.71-17.42) |
| P value for effect estimate | <.001 | <.001 |
| I2 for heterogeneity, % | 24.6 | 35.93 |
| P value for heterogeneity | .202 | .154 |
CI, confidence interval; MEPS, Mayo Elbow Performance Score; DASH, Disabilities of the Arm, Shoulder and Hand.
Discussion
Main findings
This systematic review and meta-analysis provided evidence highlighting that all fixed-stem RHA implants should not be considered equivalent to each other. Differences were seen between different devices (15 in total) across numerous outcomes, which included rates of revision, arthritis, capitellar erosion, instability, and osteolysis, as well as functional scores via either the MEPS or DASH questionnaire. When all evaluated outcomes were considered, the Anatomic Radial Head (Acumed) and ExploR (Zimmer-Biomet) devices generally performed well across most outcomes whereas rHead RECON (SBi/Stryker), Guepar (SBi/Stryker), Solar (SBi/Stryker), and MoPyC (Tornier) devices tended to show less favorable results; however, such conclusions are dependent on which of these outcomes are considered most important.
Agyeman et al1 reported overall revision rates of 7.9% for fixed-stem implants and 3.1% for unfixed stems. We calculated a revision rate of 11.7% for fixed-stem implants, as the additional studies included since the publication by Agyeman et al generally reported revision rates higher than 7.9%13,14,20,21,27,29,31,34; however, when we performed subgroup analysis by the specific RHA devices, revision rates were as low as 4.4% and as high as 60%, demonstrating how problematic it can be to group different devices together based on one similar characteristic. In addition, we noted that outcomes may be influenced by the type of patient receiving an RHA. Specifically, we saw evidence to suggest that patients with Essex-Lopresti or terrible-triad injuries may be at a greater risk of development of certain complications. This finding indicates that we should also evaluate these devices within the context of the patient population. Of note, there is currently no gold standard as to what are clinically important thresholds for revision and complication rates, and what is considered acceptable may vary from surgeon to surgeon. In addition, many of the reported complications may be based purely on radiographic findings within a given study, and it is unclear how many patients experiencing these complications may actually be symptomatic. In terms of the reasons for revision reported in the included literature, the data suggested that the most common reason for revision was to treat elbow joint stiffness and limited range of motion (making up approximately 31% of these revisions), followed by implant loosening, subluxation, and pain unrelated to implant loosening. This finding is consistent with the most commonly reported complications identified in the report by Agyeman et al.1 There may also be inconsistency in the criteria used to define some of the reported complications. For example, most of the studies providing data on the incidence of arthritis stated that they followed the Broberg-Morrey classification to measure the severity of ulnohumeral osteoarthritis6; however, there were still a number of included studies that did not specify their method of measuring arthritis. Standardized definitions and reporting of outcomes would ensure comparability between studies and greater confidence in the pooled estimates.
In a previously published network meta-analysis of randomized controlled trials (RCTs) on displaced radial head fractures, we found that RHA resulted in better function and reduced postoperative complications compared with open reduction–internal fixation.36 Regarding the limited amount of evidence (only 4 RCTs), none of the included RCTs directly compared 2 different fixed-stem implants or compared fixed vs. unfixed stems. Such comparisons are currently limited to either prospective or retrospective cohort studies. In terms of fixed vs. unfixed stems, 1 prospective and 2 retrospective cohort studies found similar pain and functional outcomes with both implant fixation techniques; however, it was reported that fixed-stem implants led to greater osteolysis. It is unclear whether the higher rate of radial neck osteolysis is clinically meaningful and actually compromises pain or functional outcomes.3,20,31 Regarding studies directly comparing fixed-stem devices with each other, they also found differences in outcomes between different devices,13,21,27,34 providing some further support that not all fixed-stem RHA implants are the same.
Limitations
A limitation of this study was the lack of randomized trial evidence. The analysis predominantly comprised data from observational studies (either case series or cohort studies), with variable follow-up lengths and small sample sizes. Higher-quality evidence, with direct comparisons, consistent outcome reporting, and comparable patient populations, would provide greater confidence in estimating the comparative effects between the different devices. In addition, certain devices may have been represented by a small number of studies. For example, the analysis of revision rates included 7 studies that evaluated the Judet (Tornier) device but only 1 study that evaluated the rHead RECON (SBi/Stryker). This may put into question the precision in the estimate for devices similar to the latter (ie, with limited data), and additional evidence on the device may change the observed outcome. Finally, definitions and criteria for an outcome to be considered a “study event” are subjective and may be inconsistent across studies, which could affect the reported estimates. Future researchers in this area should collaborate to standardize, as much as possible, the process of assessing these outcomes.
Conclusion
This systematic review and meta-analysis provided evidence that fixed-stem RHA implants should not be considered equivalent to each other. Differences were seen in revision rates, postoperative complications, and functional scores. This study highlighted that these devices should be evaluated within the context of the patient population under examination, as patients with Essex-Lopresti or terrible-triad injuries may demonstrate worse outcomes relative to patients with isolated fractures only. Additional high-quality evidence is needed to further support these conclusions.
Disclaimer
This study was funded by Acumed.
Christopher Vannabouathong is an employee of OrthoEvidence.
The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this systematic review.
References
- 1.Agyeman K.D., Damodar D., Watkins I., Dodds S.D. Does radial head implant fixation affect functional outcomes? A systematic review and meta-analysis. J Shoulder Elbow Surg. 2019;28:126–130. doi: 10.1016/j.jse.2018.07.032. [DOI] [PubMed] [Google Scholar]
- 2.Allavena C., Delclaux S., Bonnevialle N., Rongieres M., Bonnevialle P., Mansat P. Outcomes of bipolar radial head prosthesis to treat complex radial head fractures in 22 patients with a mean follow-up of 50 months. Orthop Traumatol Surg Res. 2014;100:703–709. doi: 10.1016/j.otsr.2014.06.019. [DOI] [PubMed] [Google Scholar]
- 3.Berschback J.C., Lynch T.S., Kalainov D.M., Wysocki R.W., Merk B.R., Cohen M.S. Clinical and radiographic comparisons of two different radial head implant designs. J Shoulder Elbow Surg. 2013;22:1108–1120. doi: 10.1016/j.jse.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Bonnevialle N. Radial head replacement in adults with recent fractures. Orthop Traumatol Surg Res. 2016;102:S69–S79. doi: 10.1016/j.otsr.2015.06.026. [DOI] [PubMed] [Google Scholar]
- 5.Brinkman J.M., Rahusen F.T.G., De Vos M.J., Eygendaal D. Treatment of sequelae of radial head fractures with a bipolar radial head prosthesis: good outcome after 1-4 years follow-up in 11 patients. Acta Orthop. 2005;76:867–872. doi: 10.1080/17453670510045516. [DOI] [PubMed] [Google Scholar]
- 6.Broberg M.A., Morrey B.F. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res. 1987;216:109–119. [PubMed] [Google Scholar]
- 7.Burkhart K.J., Mattyasovszky S.G., Runkel M., Schwarz C., Kuchle R., Hessmann M.H. Mid- to long-term results after bipolar radial head arthroplasty. J Shoulder Elbow Surg. 2010;19:965–972. doi: 10.1016/j.jse.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 8.Celli A., Modena F., Celli L. The acute bipolar radial head replacement for isolated unreconstructable fractures of the radial head. Musculoskelet Surg. 2010;94(Suppl 1):S3–S9. doi: 10.1007/s12306-010-0062-y. [DOI] [PubMed] [Google Scholar]
- 9.Chapman C.B., Su B.W., Sinicropi S.M., Bruno R., Strauch R.J., Rosenwasser M.P. Vitallium radial head prosthesis for acute and chronic elbow fractures and fracture-dislocations involving the radial head. J Shoulder Elbow Surg. 2006;15:463–473. doi: 10.1016/j.jse.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Dotzis A., Cochu G., Mabit C., Charissoux J.L., Arnaud J.P. Comminuted fractures of the radial head treated by the Judet floating radial head prosthesis. J Bone Joint Surg Br. 2006;88:760–764. doi: 10.1302/0301-620X.88B6.17415. [DOI] [PubMed] [Google Scholar]
- 11.El Sallakh S. Radial head replacement for radial head fractures. J Orthop Trauma. 2013;27:e137–e140. doi: 10.1097/BOT.0b013e318269b7b7. [DOI] [PubMed] [Google Scholar]
- 12.Gauci M.O., Winter M., Dumontier C., Bronsard N., Allieu Y. Clinical and radiologic outcomes of pyrocarbon radial head prosthesis: midterm results. J Shoulder Elbow Surg. 2016;25:98–104. doi: 10.1016/j.jse.2015.08.033. [DOI] [PubMed] [Google Scholar]
- 13.Gramlich Y., Krausch E.L., Klug A., Buckup J., Schmidt-Horlohe K., Hoffmann R. Complications after radial head arthroplasty: a comparison between short-stemmed bipolar and monopolar long-stemmed osteointegrative rigidly fixed prostheses. Int Orthop. 2019;43:1917–1925. doi: 10.1007/s00264-018-4173-7. [DOI] [PubMed] [Google Scholar]
- 14.Hari Krishnan B., Gupta T.P. Bipolar radial head arthroplasty for management of radial head fractures. J Arthrosc Joint Surg. 2019;6:48–52. [Google Scholar]
- 15.Heijink A., Kodde I.F., Mulder P.G.H., Van Dijk C.N., Eygendaal D. Cemented bipolar radial head arthroplasty: midterm follow-up results. J Shoulder Elbow Surg. 2016;25:1829–1838. doi: 10.1016/j.jse.2016.05.017. [DOI] [PubMed] [Google Scholar]
- 16.Katthagen J.C., Jensen G., Lill H., Voigt C. Monobloc radial head prostheses in complex elbow injuries: results after primary and secondary implantation. Int Orthop. 2013;37:631–639. doi: 10.1007/s00264-012-1747-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaur M.N., MacDermid J.C., Grewal R.R., Stratford P.W., Woodhouse L.J. Functional outcomes post-radial head arthroplasty: a systematic review of literature. Shoulder Elbow. 2014;6:108–118. doi: 10.1177/1758573214524934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kodde I.F., Heijink A., Kaas L., Mulder P.G.H., van Dijk C.N., Eygendaal D. Press-fit bipolar radial head arthroplasty, midterm results. J Shoulder Elbow Surg. 2016;25:1235–1242. doi: 10.1016/j.jse.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 19.Kodde I.F., Kaas L., Flipsen M., van den Bekerom M.P., Eygendaal D. Current concepts in the management of radial head fractures. World J Orthop. 2015;6:954–960. doi: 10.5312/wjo.v6.i11.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laflamme M., Grenier-Gauthier P.P., Leclerc A., Antoniades S., Bedard A.M. Retrospective cohort study on radial head replacements comparing results between smooth and porous stem designs. J Shoulder Elbow Surg. 2017;26:1316–1324. doi: 10.1016/j.jse.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 21.Laumonerie P., Reina N., Ancelin D., Delclaux S., Tibbo M.E., Bonnevialle N. Mid-term outcomes of 77 modular radial head prostheses. Bone Joint J. 2017;99-B:1197–1203. doi: 10.1302/0301-620X.99B9.BJJ-2016-1043.R2. [DOI] [PubMed] [Google Scholar]
- 22.Levy J.C., Formaini N.T., Kurowicki J. Outcomes and radiographic findings of anatomic press-fit radial head arthroplasty. J Shoulder Elbow Surg. 2016;25:802–809. doi: 10.1016/j.jse.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 23.Lim Y.J., Chan B.K. Short-term to medium-term outcomes of cemented Vitallium radial head prostheses after early excision for radial head fractures. J Shoulder Elbow Surg. 2008;17:307–312. doi: 10.1016/j.jse.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 24.Lopiz Y., Gonzalez A., Garcia-Fernandez C., Garcia-Coiradas J., Marco F. Comminuted fractures of the radial head: resection or prosthesis? Injury. 2016;47:S29–S34. doi: 10.1016/S0020-1383(16)30603-9. [DOI] [PubMed] [Google Scholar]
- 25.Moro J.K., Werier J., MacDermid J.C., Patterson S.D., King G.J.W. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2001;83:1201–1211. doi: 10.2106/00004623-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Mou Z., Chen M., Xiong Y., Fan Z., Wang A., Wang Z. Comminuted radial head fractures treated by the Acumed anatomic radial head system. Int J Clin Exp Med. 2015;8:6327–6333. [PMC free article] [PubMed] [Google Scholar]
- 27.Nestorson J., Josefsson P.O., Adolfsson L. A radial head prosthesis appears to be unnecessary in Mason-IV fracture dislocation. Acta Orthop. 2017;88:315–319. doi: 10.1080/17453674.2017.1293440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Popovic N., Lemaire R., Georis P., Gillet P. Midterm results with a bipolar radial head prosthesis: radiographic evidence of loosening at the bone-cement interface. J Bone Joint Surg Am. 2007;89:2469–2476. doi: 10.2106/JBJS.F.00723. [DOI] [PubMed] [Google Scholar]
- 29.Ricon F.J., Lajara F., Fuentes A., Aguilar M.L., Boix A., Lozano J.A. Pyrocarbon arthroplasty in acute unreconstructable radial head fractures: mid-term to long term results. J Orthop Traumatol. 2018;19:13. doi: 10.1186/s10195-018-0499-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ricón F.J., Sánchez P., Lajara F., Galán A., Lozano J.A., Guerado E. Result of a pyrocarbon prosthesis after comminuted and unreconstructable radial head fractures. J Shoulder Elbow Surg. 2012;21:82–91. doi: 10.1016/j.jse.2011.01.032. [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez-Quintana D., Comulada D.B., Rodriguez-Quintana N., Lopez-Gonzalez F. Radial head ingrowth anatomic implant versus smooth stem monoblock implant in acute terrible triad injury: a prospective comparative study. J Orthop Trauma. 2017;31:503–509. doi: 10.1097/BOT.0000000000000885. [DOI] [PubMed] [Google Scholar]
- 32.Rotini R., Marinelli A., Guerra E., Bettelli G., Cavaciocchi M. Radial head replacement with unipolar and bipolar SBi system: a clinical and radiographic analysis after a 2-year mean follow-up. Musculoskelet Surg. 2012;96(Suppl 1):S69–S79. doi: 10.1007/s12306-012-0198-z. [DOI] [PubMed] [Google Scholar]
- 33.Sarris I.K., Kyrkos M.J., Galanis N.N., Papavasiliou K.A., Sayegh F.E., Kapetanos G.A. Radial head replacement with the MoPyC pyrocarbon prosthesis. J Shoulder Elbow Surg. 2012;21:1222–1228. doi: 10.1016/j.jse.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 34.Sullivan M.P., Firoozabadi R., Kennedy S.A., Agel J., Magnusson E., Schiffman B. Radial neck dilatory remodeling after radial head arthroplasty with an uncemented, press fit, fully chemically etched stem design. J Orthop Trauma. 2017;31:497–502. doi: 10.1097/BOT.0000000000000876. [DOI] [PubMed] [Google Scholar]
- 35.Tarallo L., Mugnai R., Rocchi M., Capra F., Catani F. Mason type III radial head fractures treated by anatomic radial head arthroplasty: is this a safe treatment option? Orthop Traumatol Surg Res. 2017;103:183–189. doi: 10.1016/j.otsr.2016.10.017. [DOI] [PubMed] [Google Scholar]
- 36.Vannabouathong C., Akhter S., Athwal G.S., Moro J., Bhandari M. Interventions for displaced radial head fractures: network meta-analysis of randomized trials. J Shoulder Elbow Surg. 2019;28:578–586. doi: 10.1016/j.jse.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 37.Viveen J., Kodde I.F., Koenraadt K.L., Beumer A., The B., Eygendaal D. Clinical and radiographic outcome of revision surgery of radial head prostheses: midterm results in 16 patients. J Shoulder Elbow Surg. 2017;26:394–402. doi: 10.1016/j.jse.2016.09.047. [DOI] [PubMed] [Google Scholar]
- 38.Wallace B.C., Dahabreh I.J., Trikalinos T.A., Lau J., Trow P., Schmid C.H. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw. 2012;49:15. [Google Scholar]