Abstract
Background
Stress shielding of the humeral stem is a known complication in press-fit total shoulder arthroplasty (TSA), but there remain limited data on its prevalence and clinical impact in midterm follow-up. The purpose of this study was to determine the prevalence of humeral stem stress shielding and its impact on functional outcomes at minimum 5-year follow-up in standard length press-fit TSA. The hypothesis was that the presence of stress shielding at minimum 5-year follow-up would not affect functional outcome scores or range of motion (ROM).
Methods
A multicenter retrospective review of primary TSAs performed with a press-fit standard length humeral stem. Functional outcome scores, ROM, and radiographs were reviewed at minimum 5-year follow-up. Prevalence of stress shielding was determined by presence of medial calcar osteolysis and adaptive changes. Function was assessed with the visual analog scale (VAS) pain score, Simple Shoulder Test (SST) score, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES) score, and Single Assessment Numeric Evaluation (SANE) score, and ROM.
Results
Forty-seven patients with 47 TSAs were available for follow-up at a mean of 79 months postoperation. Overall, 15 of 47 humeral stems had high adaptive change scores (31.9%), and 20 demonstrated medial calcar osteolysis (42.6%). Stems with evidence of stress shielding showed no significant change in SST, VAS, ASES, or SANE scores and minimal change in ROM measurements at minimum 5-year follow-up.
Conclusion
Stress shielding is common at midterm follow-up in press-fit TSA but does not appear to affect functional outcomes.
Keywords: Total shoulder arthroplasty, stress shielding, standard length, press-fit, midterm, humeral stem
Anatomic total shoulder arthroplasty (TSA) is a reliable treatment for glenohumeral arthritis for most patients with an implant survival rate of 90% or greater at 10 years.4,14 In addition to glenoid loosening, stress shielding of the humeral stem remains a concern.5,6,9 Because TSA is being performed more often and for younger patients, it is important to understand the prevalence of these radiographic changes and whether or not they affect clinical outcomes in the mid- to long term.1,8
Humeral components can be categorized by both method of fixation and stem length. Press-fit stems have replaced cemented stems as the standard of care because of decreased operative time, ease of revision, and preservation of bone stock at time zero. Standard length stems have traditionally been used, but they may have increased stress shielding compared with some newer, short stems.2,10 Although standard length press-fit stems have shown good clinical outcomes in the short term, several studies have demonstrated they have high rates of stress shielding with longer follow-up.6,9,15 However, these changes may vary according to stem design, and there are limited data on the impact of these changes with regard to midterm functional outcome.
The purpose of this study was to evaluate the minimum 5-year stress shielding of a press-fit standard length humeral stem in TSA and determine whether the stress shielding had any impact on the clinical outcomes. The hypothesis is that there would be no significant difference in clinical outcomes based on stress shielding.
Materials and methods
A multicenter retrospective review was performed on a consecutive series of anatomic TSAs performed with a press-fit standard length humeral stem (Univers II; Arthrex Inc, Naples, FL, USA) and a cemented all-polyethylene glenoid from March 2008 to October 2011. Inclusion criteria included (1) primary anatomic TSA performed for glenohumeral arthritis using a press-fit standard length humeral stem; (2) immediate postoperative and minimum 5-year postoperative radiographs; and (3) preoperative and minimum 5-year postoperative range of motion (ROM) and patient-reported outcome scores. Exclusion criteria included revision arthroplasty or a cemented humeral stem. Four hundred sixty-five TSAs were performed during the study period, of which 47 met the study criteria and were included in the analysis.
Surgical technique
TSAs were performed at 3 centers by 3 different surgeons using a consistent technique. The deltopectoral approach was used to access the glenohumeral joint. The subscapularis was detached with the peel technique, and anatomic cut of the humeral head was performed respecting native retroversion and inclination. The humeral canal was opened with a single reamer and then broached to rotational control to accept the press-fit humeral component. All patients received a cemented all-polyethylene glenoid component. Postoperatively, the shoulder was placed in a sling for 4 weeks. Passive ROM was allowed at 2 weeks, and strengthening was allowed at 8 weeks. Full activities were permitted at 4 months postoperation.
Clinical evaluation
Functional outcome and ROM were assessed preoperatively and at a minimum 5-year follow-up by the treating surgeons. Function was determined with the visual analog scale (VAS) pain score, Simple Shoulder Test (SST) score, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES) score, and Single Assessment Numeric Evaluation (SANE) score. ROM measurements were performed by an independent provider at each site using a goniometer to assess forward flexion (FF) and external rotation (ER) at the side; internal rotation (IR) was estimated to the nearest spinal level.
Radiographic evaluation
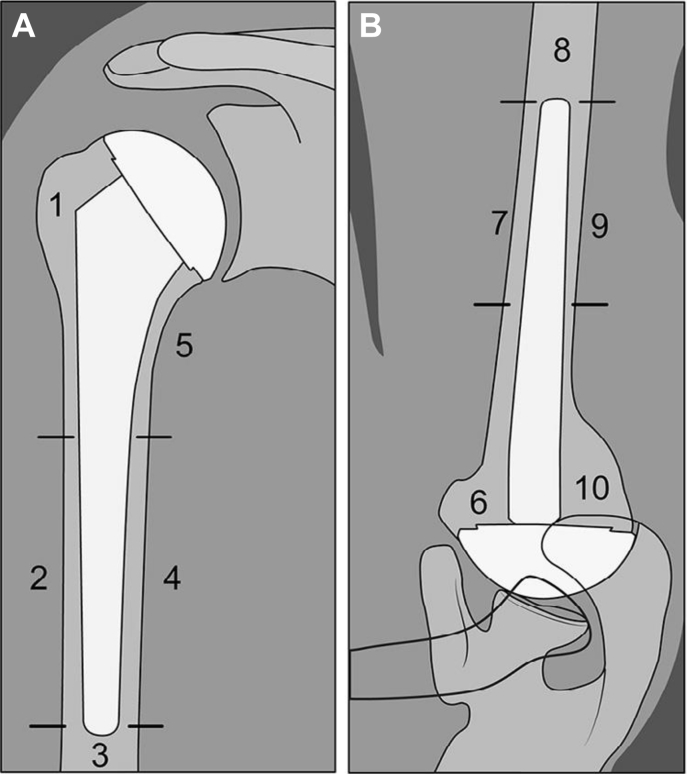
Radiographic changes were determined by comparing immediate postoperative and minimum 5-year postoperative radiographs in 10 humeral zones (5 Grashey anteroposterior, 5 axillary lateral) (Fig. 1).3 Each zone was evaluated by an independent examiner (P.J.D.) for the presence of cortical thinning or osteopenia graded as “yes” or “no,” with 1 point for yes and 0 points for no. A total bony adaptive change score was calculated by summing all zones. Based on previous guidelines, those with 0-3 adaptive changes were considered the “low” adaptive change group, and those with ≥4 adaptive changes were considered the “high” adaptive change group.11 Radiolucent lines in each zone were recorded to the nearest 0.5 mm. A stem was considered to be at risk for loosening if it demonstrated subsidence or shift or had ≥2 mm radiolucent lines in 3 or more zones.12 Medial calcar osteolysis was noted as absent (score = 0), partial (score = 1), or complete (score = 2).
Figure 1.
Zones for radiographic analysis of stress shielding on (A) Grashey anteroposterior and (B) axillary lateral views.
Statistical analysis
Categorical data were described by count and percentage and continuous data by mean and standard deviation. A χ2 test was used to evaluate categorical radiographic data. Differences in preoperative and minimum 5-year postoperative ROM and functional outcome scores were evaluated with a paired t test. A 2-way analysis of variance was conducted to compare the effect of presence of calcar osteolysis (score of 1 or 2) and the amount of adaptive changes (scores ≥4 were considered high) to ROM and patient-reported outcome measures.
Results
A total of 47 patients with 47 TSAs were available for follow-up at a mean of 79 months postoperation (range 60-114). The mean age was 65.3 years (range 46-82). Baseline demographics are summarized in Table I. The group with evidence of calcar osteolysis had significantly decreased ER (P = .002) and lower SST scores (P = .047) preoperatively compared with the group without osteolysis, but there were no other preoperative differences between any of the groups. Comparisons of preoperative ROM and functional outcome scores are listed in Table II.
Table I.
Baseline patient characteristics (N = 47)
| Mean (range) or n (%) | |
|---|---|
| Age, yr | 65.3 (46-82) |
| Follow-up, mo | 78.6 (60-114) |
| Sex | |
| Male | 25 (53.2) |
| Female | 29 (46.8) |
| Side | |
| Right | 29 (61.7) |
| Left | 18 (38.3) |
| Dominant arm | |
| Yes | 29 (61.7) |
| No | 18 (38.3) |
Table II.
Preoperative comparison (N = 47)
| n (%) | Preop. forward flexion | Preop. external rotation | Preop. internal rotation | Preop. VAS pain score | Preop. ASES score | Preop. SST score | Preop. SANE score | |
|---|---|---|---|---|---|---|---|---|
| Adaptive changes | ||||||||
| Low (0-3) | 32 (68.1) | 117° ± 30° | 37° ± 18° | 17.2 ± 1.9 | 6.0 ± 2.4 | 39.5 ± 18.4 | 3.8 ± 2.6 | 33.4 ± 15.5 |
| High (≥4) | 15 (31.9) | 112° ± 34° | 31° ± 15° | 17.9 ± 2.4 | 5.9 ± 2.0 | 36.7 ± 16.6 | 3.2 ± 2.4 | 30.5 ± 15.9 |
| P value | .713 | .278 | .194 | .919 | .607 | .44 | .634 | |
| Calcar osteolysis | ||||||||
| None | 27 (57.4) | 118° ± 29° | 41° ± 17° | 17.4 ± 1.9 | 5.8 ± 2.5 | 42.1 ± 16.7 | 4.3 ± 2.4 | 32.6 ± 16.4 |
| Any | 20 (42.6) | 113° ± 33° | 27° ± 13° | 17.4 ± 2.3 | 6.2 ± 2.1 | 34.0 ± 18.4 | 2.8 ± 2.4 | 32.3 ± 14.5 |
| P value | .609 | .002 | >.999 | .553 | .126 | .047 | .954 |
VAS, visual analog scale; ASES, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form; SST, Simple Shoulder Test; SANE, Single Assessment Numeric Evaluation.
Continuous variables are listed as mean ± standard deviation, and categorical variables, as number (percentage).
Internal rotation was coded as follows: T12 = 12, L2 = 14, L4 = 16, S1 = 18, hip = 20.
Clinical outcomes
Looking at the entire group of TSAs, FF improved from 116° preoperatively to 137° postoperatively (P < .001), ER improved from 35°-50° (P < .001), and IR improved from L5 to L2 (P < .001). VAS pain scores decreased from 5.9-1.3 (P < .001), ASES scores improved from 38.6-81.2 (P < .001), SST scores improved from 3.6-9.2 (P < .001), and SANE scores improved from 32.5-82.5 (P < .001). At final follow-up, 42 of the 47 patients (89.4%) had returned to their usual activity, and 41 were satisfied with their surgical outcome (87.2%) (Table III).
Table III.
Entire cohort outcomes
| Preoperative score | Minimum 5-yr postoperative score | P value | |
|---|---|---|---|
| VAS pain score | 5.9 ± 2.3 | 1.3 ± 2.1 | <.001 |
| ASES score | 38.6 ± 17.7 | 81.2 ± 20.6 | <.001 |
| SST score | 3.6 ± 2.5 | 9.2 ± 2.9 | <.001 |
| SANE score | 32.5 ± 15.4 | 82.5 ± 21.3 | <.001 |
| FF | 116°± 31° | 137°± 25° | <.001 |
| ER | 35°± 17° | 50°± 16° | <.001 |
| IR | L5 | L2 | <.001 |
VAS, visual analog scale; ASES, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form; SST, Simple Shoulder Test; SANE, Single Assessment Numeric Evaluation; FF, forward flexion; ER, external rotation; IR, internal rotation.
Continuous variables are listed as mean ± standard deviation, and IR, as the average level obtained.
Radiographic outcomes
The mean adaptive change score was 2.1 ± 1.8. After review of all humeral stems, 15 of 47 had high adaptive change scores (31.9%) and 32 had low adaptive change scores (68.1%). The presence of high adaptive changes did not have a significant effect on the SST (P = .358), VAS (P = .209), ASES (P = .404), or SANE (P = .873) scores or on FF (P = .615), IR (P = .767), or ER (P = .163). Medial calcar osteolysis was observed in 20 of the 47 cases (42.6%), of which 18 were partial (38.3%) and 2 were complete (4.3%). The group with any medial calcar osteolysis had significantly increased ER (P = .006) from preoperation to minimum 5 years postoperation. However, the presence of osteolysis did not have a significant effect on IR (P = .833) or FF (P = .811), or on the SST (P = .794), VAS (P = .767), ASES (P = .643), or SANE (P = .422) scores (Table IV).
Table IV.
Subgroup outcomes (N = 47)
| n (%) | Δ forward flexion | Δ external rotation | Δ internal rotation | Δ VAS pain score | Δ ASES score | Δ SST score | Δ SANE score | |
|---|---|---|---|---|---|---|---|---|
| Adaptive changes | ||||||||
| Low (0-3) | 32 (68.1) | 23° ± 25° | 13° ± 20° | –2.8 ± 2.5 | –5.1 ± 3.0 | 44.6 ± 24.6 | 5.8 ± 2.6 | 46.7 ± 30.4 |
| High (≥4) | 15 (31.9) | 18° ± 35° | 21° ± 17° | –3.2 ± 3.4 | –3.8 ± 3.1 | 37.9 ± 25.3 | 4.7 ± 4.5 | 48.8 ± 34.8 |
| P value | .615 | .163 | .767 | .209 | .404 | .358 | .873 | |
| Calcar osteolysis | ||||||||
| None | 27 (57.4) | 22° ± 29° | 9° ± 18° | –2.9 ± 2.4 | –4.8 ± 3.0 | 40.9 ± 24.8 | 5.6 ± 2.7 | 50.3 ± 33.2 |
| Any | 20 (42.6) | 20° ± 28° | 24° ± 16° | –3.1 ± 3.2 | –4.5 ± 3.1 | 44.4 ± 25.2 | 5.3 ± 4.1 | 43.4 ± 29.4 |
| P value | .811 | .006 | .833 | .767 | .643 | .794 | .422 |
VAS, visual analog scale; ASES, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form; SST, Simple Shoulder Test; SANE, Single Assessment Numeric Evaluation.
Continuous variables are listed as mean ± standard deviation, and categorical variables as number (percentage).
Only 1 of the 47 humeral stems (2.1%) demonstrated subsidence, and 2 of the stems (4.3%) were determined to be at risk for loosening (1 due to subsidence, 1 due to radiolucent lines) (Table V).
Table V.
Adaptive change prevalence by radiographic zone (N = 47)
| Zone | Adaptation |
|
|---|---|---|
| CNO | RLL ≥2 mm | |
| Z1 | 27 (57.4) | 0 (0) |
| Z2 | 1 (2.1) | 0 (0) |
| Z3 | 1 (2.1) | 1 (2.1) |
| Z4 | 1 (2.1) | 0 (0) |
| Z5 | 24 (51.1) | 0 (0) |
| Z6 | 18 (38.3) | 1 (2.1) |
| Z7 | 0 (0) | 1 (2.1) |
| Z8 | 0 (0) | 0 (0) |
| Z9 | 1 (2.1) | 1 (2.1) |
| Z10 | 24 (51.1) | 0 (0) |
| Total score | 2.1 ± 1.8 | |
Z1, anteroposterior (AP) view: superior lateral half of the stem; Z2, AP view: inferior lateral half of the stem; Z3, AP view: beneath the tip of the stem; Z4, AP view: superior medial half of the stem; Z5, AP view: inferior medial half of the stem; Z6, axillary view: anterosuperior half of the stem; Z7, axillary view: anteroinferior half of the stem; Z8, axillary view: beneath the tip of the stem; Z9, axillary view: posterosuperior half of the stem; Z10, axillary view: posteroinferior half of the stem; CNO, cortical thinning and osteopenia; RLL, radiolucent lines.
Categorical variables are listed as number (percentage).
Complications
Overall, 6 of the 47 patients (12.8%) experienced complications. Two patients experienced pain and stiffness after weight lifting that was attributed to rotator cuff tendonitis, and 1 patient experienced pain and stiffness that was treated with a steroid injection. None of these shoulders were revised. One patient had glenoid component loosening that was treated with glenoid component removal and bone grafting. Two patients had pain and stiffness associated with glenoid component loosening but have not gone on to revision at this time. No humeral stems required revision.
Discussion
The primary finding of this study is that there was a high rate of stress shielding observed at midterm follow-up with a standard length press-fit humeral stem. A significant number of patients demonstrated “high” adaptive changes (32%) and some degree of medial calcar osteolysis (43%). Despite the high incidence of adaptive changes, there was a low risk of humeral stem loosening, and adaptive changes had minimal effect on clinical outcomes. These findings are important as they provide a baseline for comparison with standard length stems as well as short stems that have been commonly used in recent years.
Our rates of stress shielding and medial calcar osteolysis are similar to other studies assessing midterm outcomes with a standard length press-fit TSA. Raiss et al9 assessed the radiographic and clinical outcomes of 67 proximally coated humeral stems (Aequalis; Wright Medical Inc, Memphis, TN, USA) at an average of 5.5 years postoperation. Forty-two percent had osteolysis of the greater tuberosity, 39% had osteolysis of the medial calcar (18% partial, 21% complete), and 63% demonstrated stress shielding at last follow-up. Spormann et al13 reported the 5-year radiographic outcomes of 132 TSAs using a rectangular stem with diaphyseal fixation (Promos; Smith & Nephew, Memphis, TN, USA) and found that 17% had full-thickness proximal bone resorption. By comparison, in our study using a stem designed for proximal fixation we observed calcar osteolysis in 43% and 32% demonstrated “high” adaptive changes at 5-year follow-up, but no cases of proximal tuberosity resorption were observed. This supports the idea that stress shielding is common at midterm follow-up and may vary slightly based on stem design.
Our complication rate of 12.8% (6/47) compares favorably to previously published studies examining midterm TSA outcomes. Three of our patients experienced pain with intact glenoid and humeral components, and were thus only mild complications. Three patients had pain related to loosening of their glenoid component, none of which had been revised at follow-up. Comparable studies assessing midterm TSA outcomes have reported complication and revision rates as high or higher than ours.4,9,15
Overall, adaptive changes in TSA humeral stems have not been shown to affect clinical outcomes at midterm follow-up. Verborgt et al15 found that at an average of 9.2 years postoperatively, an “at risk” humeral component had no effect on absolute Constant score, ROM, postoperative pain, or Neer postoperative satisfaction rating. Nagels et al7 similarly found no difference in Constant scores or ROM at 5-year follow-up in those with and without radiographic evidence of stress shielding. Spormann et al13 showed that at 5-year follow-up, bone resorption did not affect the ASES; Shoulder Pain and Disability Index; or Disability of the Arm, Shoulder, and Hand scores. Our study overall draws a similar conclusion. We found that minimum 5-year postoperative “high” adaptive changes and presence of calcar osteolysis had no significant impact on SST, VAS, ASES, or SANE scores or ROM measurements. The one exception was that the group with calcar osteolysis did show a significant increase in ER compared with the group without, but this is likely explained by the osteolysis group having lower preoperative ER measurements and therefore more room to improve postoperatively.
The study was limited by its retrospective design and small cohort size. Retrospective analysis introduces selection and recall biases that cannot be controlled for. Furthermore, we did not use fluoroscopic controls for the radiographs, which may have affected the review. However, as opposed to most of the previous studies that only analyzed anteroposterior radiographs, we examined both anteroposterior and axillary radiographs in a total of 10 zones. Our study may also lack generalizability to all standard length press-fit humeral stems. The Univers II stem used in our study has a rectangular stem geometry, metaphyseal collar, and proximal coating. There are many stem geometries, collar options, and coating types available in shoulder arthroplasty, and our results may not be applicable to components with different designs. Further study is thus needed to examine the differences in stress shielding based on stem design. For instance, newer, shorter stems may decrease stress shielding, but only short-term follow-up comparative studies are available at this time. We also did not evaluate if nonanatomic alignment (varus and valgus) of the humeral stem was associated with higher rates of stress shielding. However, previous studies have found that nonanatomic alignment in press-fit TSA is rare and does not affect the rate of osteolysis.2
Conclusion
In our review of 47 press-fit TSAs, humeral stem stress shielding was common at midterm follow-up, with 15 demonstrating high adaptive change scores (31.9%) and 20 demonstrating medial calcar osteolysis (42.6%). However, these changes had only a minimal impact on functional outcomes. Although there is limited evidence on the prevalence and clinical importance of humeral stem adaptive changes in TSA midterm follow-up, our outcomes support the idea that humeral stem stress shielding may be common but of little clinical significance in the midterm. Further study is needed to determine if these results are maintained in the long term.
Disclaimer
This study was supported by a grant from Arthrex,Inc.
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was obtained prior to the study (protocol no. 641).
References
- 1.Day J.S., Lau E., Ong K.L., Williams G.R., Ramsey M.L., Kurtz S.M. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010;19:1115–1120. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Denard P.J., Noyes M.P., Walker J.B., Shishani Y., Gobezie R., Romeo A.A. Proximal stress shielding is decreased with a short stem compared with a traditional-length stem in total shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:53–58. doi: 10.1016/j.jse.2017.06.042. [DOI] [PubMed] [Google Scholar]
- 3.Denard P.J., Raiss R., Walker J.B., Gobezie R., Edwards T.B., Lederman E. Stress shielding of the humerus in press-fit anatomic shoulder arthroplasty: review and recommendations for evaluation. J Shoulder Elbow Surg. 2018;27:1139–1147. doi: 10.1016/j.jse.2017.12.020. [DOI] [PubMed] [Google Scholar]
- 4.Deshmukh A.V., Koris M., Zurakowski D., Thornhill T.S. Total shoulder arthroplasty: Long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14:471–479. doi: 10.1016/j.jse.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Fox T.J., Foruria A.M., Klika B.J., Sperling J.W., Schleck C.D., Cofield R.H. Radiographic survival in total shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:1221–1227. doi: 10.1016/j.jse.2012.12.034. [DOI] [PubMed] [Google Scholar]
- 6.Matsen F.A., 3rd, Iannotti J.P., Rockwood C.A., Jr. Humeral fixation by press-fitting of a tapered metaphyseal stem: a prospective radiographic study. J Bone Joint Surg Am. 2003;85:304–308. doi: 10.2106/00004623-200302000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Nagels J., Stokdijk M., Rozing P.M. Stress shielding and bone resorption in shoulder arthroplasty. J Shoulder Elbow Surg. 2003;12:35–39. doi: 10.1067/mse.2003.22. [DOI] [PubMed] [Google Scholar]
- 8.Padegimas E.M., Maltenfort M., Lazarus M.D., Ramsey M.L., Williams G.R., Namdari S. Future patient demand for shoulder arthroplasty by younger patients: national projections. Clin Orthop Relat Res. 2015;473:1860–1867. doi: 10.1007/s11999-015-4231-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raiss P., Edwards T.B., Deutsch A., Shah A., Bruckner T., Loew M. Radiographic changes around humeral components in shoulder arthroplasty. J Bone Joint Surg Am. 2014;96:e54. doi: 10.2106/JBJS.M.00378. [DOI] [PubMed] [Google Scholar]
- 10.Razfar N., Reeves J.M., Langohr D.G., Willing R., Athwal G.S., Johnson J.A. Comparison of proximal humeral bone stresses between stemless, short stem, and standard stem length: a finite element analysis. J Shoulder Elbow Surg. 2016;25:1076–1083. doi: 10.1016/j.jse.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Schnetzke M., Coda S., Raiss P., Walch G., Loew M. Radiologic bone adaptations on a cementless short-stem shoulder prosthesis. J Shoulder Elbow Surg. 2016;25:650–657. doi: 10.1016/j.jse.2015.08.044. [DOI] [PubMed] [Google Scholar]
- 12.Sperling J.W., Cofield R.H., O'Driscoll S.W., Torchia M.E., Rowland C.M. Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elbow Surg. 2000;9:507–513. doi: 10.1067/mse.2000.109384. [DOI] [PubMed] [Google Scholar]
- 13.Spormann C., Durchholz H., Audigé L., Flury M., Schwyzer H.K., Simmen B.R. Patterns of proximal humeral bone resorption after total shoulder arthroplasty with an uncemented rectangular stem. J Shoulder Elbow Surg. 2014;23:1028–1035. doi: 10.1016/j.jse.2014.02.024. [DOI] [PubMed] [Google Scholar]
- 14.Torchia M.E., Cofield R.H., Settergren C.R. Total shoulder arthroplasty with the Neer prosthesis: Long-term results. J Shoulder Elbow Surg. 1997;6:495–505. doi: 10.1016/s1058-2746(97)90081-1. [DOI] [PubMed] [Google Scholar]
- 15.Verborgt O., Abiad R.E., Gazielly D.F. Long-term results of uncemented humeral components in shoulder arthroplasty. J Shoulder Elbow Surg. 2007;16:S13–S18. doi: 10.1016/j.jse.2006.02.003. [DOI] [PubMed] [Google Scholar]