Abstract
Background
This study aimed to determine the toileting ability (TA) of patients undergoing primary reverse total shoulder arthroplasty (RTSA) and identify factors associated with TA postoperatively.
Methods
A questionnaire regarding toileting was administered to 119 patients who underwent primary RTSA with a minimum 1-year follow-up. Patients were separated into 2 groups based on whether the arm that underwent RTSA was the one used for toileting (study group, n = 74) or not (control group, n = 45). Patient-reported TA was calculated both before and after RTSA. Multivariate analysis was performed to identify factors associated with TA postoperatively.
Results
Impairment in TA before RTSA was higher in the study group and affected almost three-quarters of the patients (72%). In the study group, primary RTSA resulted in a statistically significant improvement in TA (P < .001), and no difference in TA was found between groups after RTSA (P = .076). Postoperatively, 92% of the patients in the study group were able to manage toileting with the involved extremity (54% without difficulty and 38% with some degree of difficulty). Only 1 patient (1.3%) was totally unable to manage toileting with either arm postoperatively. The patients at risk of toileting difficulties postoperatively were those who had preoperative toileting difficulties and lower postoperative internal rotation range of motion.
Conclusions
Over 90% of patients can manage toileting after primary RTSA, and total toileting inability is rare after the procedure (1.3%). Patients should be counseled that after primary RTSA, they have a high probability of being able to manage toileting with independence even if it is with some difficulty.
Keywords: Reverse total shoulder arthroplasty, toileting, activities of daily living, shoulder replacement, internal rotation, functional outcomes
Toileting is an important and fundamental activity of daily living that has many implications in patients' independence and quality of life. Loss of internal rotation is often observed in patients requiring shoulder arthroplasty, which may result in variable degrees of impairment in toileting ability. Impairment in toileting ability has been found to be a predictor of patient dissatisfaction after shoulder arthroplasty1,26; therefore, recovery of internal rotation as well as toileting ability is an important goal of the procedure.
However, limited recovery of internal rotation after reverse total shoulder arthroplasty (RTSA) has been reported,11,25,29 and impairment in toileting ability has been reported to be a concern of patients both before and after RTSA.22,37 Little is known about the prevalence of preoperative impairments in toileting ability in patients undergoing RTSA and the effect of the procedure on the patient's ability to perform this task.37 A previous systematic review indicated that only 3% of all published studies of RTSA addressed the issue of toileting.22 In the 6 studies included in that systematic review, most patients (92%; 95% confidence interval, 87%-95%) were able to manage toileting after RTSA, and no significant difference in toileting ability was found after unilateral vs. bilateral RTSA. However, 8% of patients were unable to manage toileting with the involved arm, and 20% of patients reported toileting difficulties after RTSA.
Information on factors associated with toileting ability after RTSA has not been evaluated previously in the literature. To our knowledge, there are no published studies assessing possible factors associated with toileting ability after RTSA. Moreover, although internal rotation may be a fundamental factor of toileting ability after RTSA, the association between clinical measures of internal rotation and toileting ability has not been studied in this population.
Knowledge of the ability of patients undergoing primary RTSA to perform toileting and understanding the factors associated with patients' ability to perform this task after the procedure would be of benefit for patients considering RTSA and for providers who can counsel them on this issue. Therefore, this study aimed to (1) determine the toileting ability and the prevalence of impairment in toileting ability in patients undergoing primary RTSA, (2) identify factors associated with toileting ability after primary RTSA, and (3) describe what modifications or aids patients needed to perform toileting after RTSA.
Materials and methods
Patient selection
From June 2017 to December 2018, a questionnaire regarding toileting (Appendix 1) was administered to 125 consecutive patients who attended our clinic for a routine follow-up visit after primary RTSA. To be included, patients had to have a minimum 1-year follow-up, based on literature that supports significant improvements in pain, function, and ROM within 1 year of RTSA.2,14,24,28 Primary RTSA was defined as the first elective RTSA performed for the diagnosis of cuff tear arthropathy (n = 77) or osteoarthritis with glenoid bone loss and an intact cuff (n = 48). Patients who underwent staged bilateral primary RTSA were included, and all data presented for bilateral cases correspond to the arm used while toileting. Patients who underwent RTSA for other diagnoses such as proximal humeral fractures and those who underwent RTSA as a revision procedure for a previous failed arthroplasty were excluded. Also excluded were patients who had postoperative infections or any other postoperative complication that required reintervention or revision (n = 6), leaving 119 patients for the final analysis.
For analytic purposes and for better assessment of the effect of RTSA on toileting ability, the cohort was separated into 2 groups based on whether the arm that underwent RTSA was the arm that each patient habitually used while toileting (study group, n = 74) or not (control group, n = 45).
Study variables
Preoperative and postoperative data were retrospectively collected from our institution's shoulder arthroplasty database. This database contains data on physical examination measurements and patient-reported outcome measures. Preoperative and postoperative ROM measurements were performed by the senior author or his advanced practice provider. Internal rotation ROM was measured with the arm both behind the back and in 90° of abduction. Internal rotation behind the back was visually estimated by noting the highest vertebral level reached by the patient's extended thumb with the hand up the back.20 Active internal rotation in 90° of abduction was measured with the patient standing without stabilizing the scapula by use of a handheld goniometer. The examiners were blinded to the results of the toileting questionnaire and American Shoulder and Elbow Surgeons (ASES) score at the time of the follow-up examination and for the duration of the study.
The primary outcome was the patient-reported toileting ability using a 4-point Likert scale (0, unable; 1, very difficult; 2, somewhat difficult; and 3, no difficulty). These data were collected preoperatively and postoperatively using the specific question “Is it difficult for you to manage toileting?” from the ASES score.18 The toileting questionnaire (Appendix 1) was designed to identify the arm that patients habitually used while toileting before RTSA and to identify changes patients had to make to manage toileting after RTSA. Patients were asked if they were able to use the same hand while toileting as before surgery, whether the way of wiping had changed after the procedure, and whether they required the use of assistive devices to manage toileting. Impairment in toileting ability was defined as a toileting rating score of less than 3 on the Likert scale. Toileting disability was defined as a toileting rating score of 0 on the Likert scale for both arms or the need for the use of assistive devices.
Surgical technique and postoperative care
All the RTSA procedures were performed through a deltopectoral approach by the senior author. Absence of the subscapularis at the lesser tuberosity footprint was found in 30 patients, whereas the subscapularis in the remaining shoulders was released from the lesser tuberosity using a peel technique.10 The subscapularis was repaired in 27% of cases (24 of 89) in which it was present at the time of the operation. Two different prosthesis systems were used: Encore Reverse Shoulder Prosthesis (DJO Surgical, Vista, CA, USA) in 21 cases from January 2010 to August 2014 and Reunion Reverse Shoulder Arthroplasty (Stryker, Mahwah, NJ, USA) in 98 cases from September 2014 to December 2017. All humeral components regardless of the system used had a 135° neck-shaft angle and were inserted in 30° of retroversion using a standard polyethylene insert. Although these 2 systems are considered lateralized RTSA systems, they differ in the amount of glenoid, humeral, and global lateralization. According to the classification proposed by Werthel et al,36 the DJO Surgical glenohumeral construct is composed of a lateralized glenoid and a medialized humerus that results, on average, in +10 mm of global lateralization, whereas the Stryker construct is composed of a lateralized glenoid and a lateralized humerus that results, on average, in +16.2 mm of global lateralization. In both systems, the amount of glenoid lateralization varies according to the glenosphere size and offset. The distribution of the different glenohumeral constructs used in the study group with the estimated amount of lateralization for each construct is presented in Table I. All patients were allowed motion in flexion after 10 days and were not allowed internal rotation up the back until 3 months postoperatively; unlimited motion was allowed thereafter.
Table I.
Glenoid, humeral, and global lateralization of RTSA constructs used in study group (n = 74)
| Glenosphere size and offset | Glenoid lateralization, mm | Humeral lateralization, mm | Global lateralization, mm | Shoulders, n (%) |
|---|---|---|---|---|
| Encore RTSA system | ||||
| 32 mm neutral | 11.1 | 3.2 | 14.6 | 1 (1.3) |
| 32 mm minus 4 mm | 7.1 | 3.2 | 10.3 | 5 (6.7) |
| 36 mm neutral | 7.1 | 3.2 | 10.3 | 5 (6.7) |
| 36 mm minus 4 mm | 6 | 3.9 | 9.9 | 3 (4) |
| Reunion RTSA system | ||||
| 32 mm plus 2 mm | 3.7 | 11.1 | 14.8 | 32 (43) |
| 36 mm plus 2 mm | 5.1 | 11.1 | 16.2 | 23 (31) |
| 40 mm plus 2 mm | 6.5 | 11.1 | 17.6 | 5 (6.7) |
RTSA, reverse total shoulder arthroplasty.
Statistical analysis
Baseline characteristics were analyzed using the t test for continuous variables and χ2 test for categorical variables. The proportion of patients in each category of toileting ability was calculated and compared between groups. The Wilcoxon signed rank test was conducted to determine if there were differences in toileting ability from preoperatively to postoperatively in the study group. The Mann-Whitney U test was conducted to determine if there were differences in toileting ability between groups. Univariate and multivariate logistic regression analyses were performed in the study group to assess the association between toileting difficulty after RTSA and the following variables: body mass index (BMI), sex, age, length of follow-up, diagnosis leading to RTSA, preoperative toileting ability, subscapularis repair, and postoperative internal rotation ROM both behind the back and in 90° of abduction. Given that different glenohumeral constructs resulting in variable degrees of lateralization were used, we assessed the association between lateralization of the glenohumeral construct (glenoid lateralization, humeral lateralization, and global lateralization) and postoperative toileting ability. Any variable with P < .250 on the univariate analysis was selected as a candidate for multivariate analysis. Covariates were removed from the model if they were not significant (α set at .1) and not confounders (change in any remaining estimate > 15%). The variables included in the multivariate model were sex, BMI, diagnosis leading to RTSA, preoperative toileting ability, and internal rotation behind the back. Marginal predicted probabilities of postoperative toileting ability according to the postoperative level of internal rotation behind the back were calculated and plotted from the multivariate model. All analyses were performed using Stata software (version 14; StataCorp, College Station, TX, USA). P < .05 was considered statistically significant.
Results
Demographic data are presented in Table II. Age, sex, BMI, length of follow-up, diagnosis leading to RTSA, and RTSA system were similar between the study and control groups.
Table II.
Baseline demographic characteristics
| Variable | Total (N = 119) | Study group (n = 74) | Control group (n = 45) | P value |
|---|---|---|---|---|
| Age, yr | 70 ± 10 | 70 ± 10 | 69 ± 11 | .708 |
| Sex | ||||
| Male | 59 (50) | 41 (55) | 18 (40) | .103 |
| Female | 60 (50) | 33 (45) | 27 (60) | |
| BMI | 30.2 ± 6.46 | 29.7 ± 7.5 | 30.9 ± 7.8 | .649 |
| Diagnosis | ||||
| Cuff tear arthropathy | 74 (62) | 44 (60) | 29 (64) | |
| Primary OA with severe bone loss and intact cuff | 45 (38) | 30 (41) | 16 (35) | .342 |
| Dominant side | ||||
| Right | 108 (90) | 3 (2.1) | 139 (97.9) | .354 |
| Left | 12 (10) | 2 (5.9) | 32 (94.1) | |
BMI, body mass index; OA, osteoarthritis.
Data are expressed as number (percentage) or mean ± standard deviation.
Toileting ability before RTSA
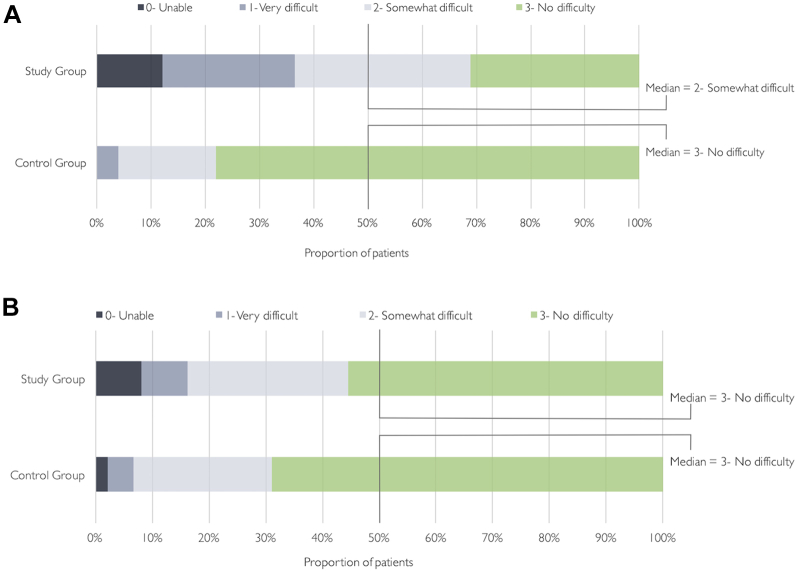
Patients in the study group were more likely to have preoperative impairments in toileting ability than were patients in the control group (Fig. 1, A). Almost three-quarters of the patients in the study group (72%) reported preoperative impairments in toileting ability compared with only 22% of those in the control group (P < .001). Similarly, the median preoperative toileting ability was lower in the study group (score of 2 [somewhat difficult] on Likert scale) than in the control group (score of 3 [no difficulty] on Likert scale) (P < .001) (Fig. 1, A). In the study group, 12% of the patients (8 of 74) reported being unable to manage toileting before RTSA, whereas 24% (18 of 74) reported that the task was very difficult, 35% (26 of 74) reported that the task was somewhat difficult, and 28% (21 of 74) reported no difficulty performing this task before the procedure.
Figure 1.
Patient-reported toileting ability before (A) and after (B) primary reverse total shoulder arthroplasty.
Toileting ability after RTSA
In the study group, toileting ability significantly improved from preoperatively (score of 2 [somewhat difficult] on Likert scale) to postoperatively (score of 3 [no difficulty] on Likert scale) (P < .001). In the study group, 8% of the patients (6 of 74) reported being unable to manage toileting after RTSA, whereas 8% (6 of 74) reported that the task was very difficult, 30% (22 of 74) reported that the task was somewhat difficult, and 54% (40 of 74) reported no difficulty performing this task after the procedure (Fig. 1, B).
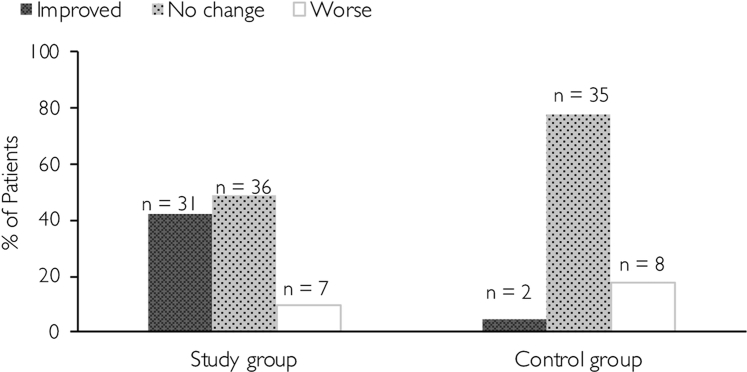
Compared with the control group, the proportion of patients who perceived an improvement in toileting ability after RTSA was significantly higher in the study group (P < .001) (Fig. 2). As a result, no difference in the median toileting ability was found between groups postoperatively (P = .076) (Fig. 1, B). Although the improvement in toileting ability in the study group was statistically significant, most of the patients improved by only 1 point on the Likert scale and some impairment in toileting ability still affected 4 in 10 patients (46%) after RTSA.
Figure 2.
Change in toileting ability after primary reverse total shoulder arthroplasty.
Factors associated with toileting ability after RTSA
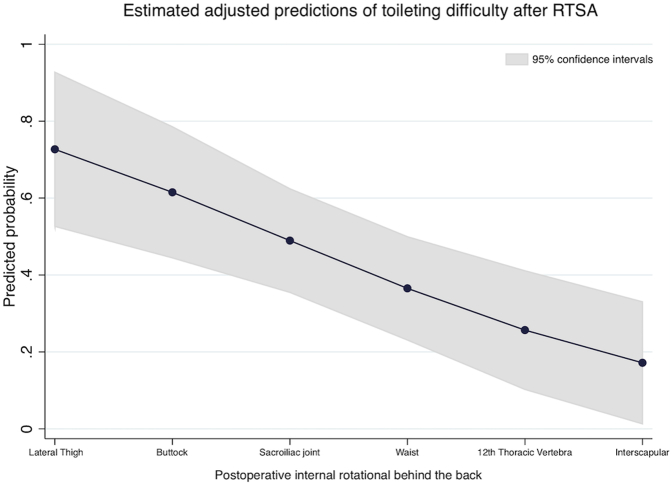
Univariate logistic regression analysis found that of the variables studied, age, sex, BMI, length of follow-up, subscapularis repair, postoperative internal rotation in 90° of abduction, and diagnosis leading to RTSA were not associated with toileting ability after RTSA. The amount of lateralization in either the glenoid, the humerus, or the global glenohumeral construct was not associated with toileting ability after RTSA (Table III). Multivariate logistic regression analysis found that independent factors associated with toileting ability after RTSA were preoperative toileting ability and postoperative internal rotation ROM behind the back (Table IV). According to the multivariate model, the odds of having toileting difficulties after primary RTSA were 4.5 times greater in patients who had toileting difficulties preoperatively than in patients who had a normal toileting ability preoperatively. Predicted probabilities estimated from the multivariate model showed that toileting difficulties after primary RTSA decreased linearly as postoperative internal rotation behind the back increased. For example, a patient who can reach only the lateral thigh postoperatively has a 70% chance of having toileting difficulties after the procedure, whereas a patient who can reach the interscapular level has only a 17% chance of having difficulties performing toileting postoperatively (Fig. 3).
Table III.
Toileting difficulties after RTSA according to glenoid, humeral, and global lateralization of RTSA system
| Variable | Toileting difficulty after RTSA |
P value | |
|---|---|---|---|
| No (n = 40) | Yes (n = 34) | ||
| Glenoid lateralization∗ | .279 | ||
| <5 mm | 15 (47) | 17 (53) | |
| ≥5 mm | 25 (60) | 17 (40) | |
| Humerus lateralization∗ | .394 | ||
| <5 mm | 9 (64) | 5 (36) | |
| ≥5 mm | 31 (52) | 29 (48) | |
| Global lateralization∗ | .273 | ||
| <10 mm | 3 (100) | 0 (0) | |
| 10-15 mm | 21 (49) | 22 (51) | |
| ≥15 mm | 16 (57) | 12 (43) | |
RTSA, reverse total shoulder arthroplasty.
Data are expressed as number (percentage).
Cutoffs were chosen according to the classification proposed by Werthel et al.36
Table IV.
Logistic multivariate analysis of factors associated with toileting ability after primary RTSA
| Variable | OR (95% CI) | P value |
|---|---|---|
| Sex | ||
| Male | Reference | |
| Female | 2.38 (0.76-7.42) | .134 |
| BMI | ||
| <25 kg/m2 (normal weight) | Reference | |
| 25-29.99 kg/m2 (overweight) | 2.42 (0.48-12.09) | .281 |
| ≥30 kg/m2 (obese) | 2.83 (0.62-13.01) | .181 |
| Diagnosis leading to RTSA | ||
| Cuff tear arthropathy | Reference | |
| Primary OA with bone loss and intact cuff | 2.20 (0.55-8.83) | .265 |
| Preoperative toileting difficulty | ||
| No | Reference | |
| Yes | 4.56 (1.28-16.28) | .019∗ |
| Postoperative IR up back (per level) | 0.77 (0.64-0.93) | .007∗ |
RTSA, reverse total shoulder arthroplasty; OR, odds ratio; CI, confidence interval; BMI, body mass index; OA, osteoarthritis; IR, internal rotation.
In this model, an OR greater than 1 represents higher odds and an OR lower than 1 represents lower odds of having toileting difficulties after RTSA.
Statistically significant.
Figure 3.
Predicted probabilities of having toileting difficulties after reverse total shoulder arthroplasty (RTSA) according to level of internal rotation behind back reached postoperatively.
Use of aids or adaptations for toileting
In the study group, 72% of the patients (53 of 74) reported no changes in their toileting habits after primary RTSA, whereas 23% (17 of 74) reported that they changed the hand used while toileting after RTSA and 5% (4 of 74) required an assistive mechanical device. Mechanical devices included toilet water spray devices in 2 patients and bottom wipers in 2 patients. Only 1 patient in the study group (1.3%) was totally unable to manage toileting with either arm postoperatively. This patient underwent staged bilateral RTSA and reported severe impairment in toileting ability with both arms before the second RTSA. As a result, the prevalence of toileting disability (ie, a score of 0 on the Likert score for both arms or the need for mechanical assistance) after primary RTSA was 7% (5 of 74 patients).
Discussion
This study found that among patients who undergo primary RTSA on the side of the extremity used for toileting, a majority (92%) will be able to use the extremity for toileting without difficulty or with some degree of difficulty. If one takes into consideration that patients may use the other, nonoperated extremity to perform toileting after surgery, only 1% could not manage toileting at all after primary RTSA. Finally, this study found that the patients at risk of toileting difficulties after RTSA were those with toileting difficulties preoperatively and those with lower postoperative internal rotation behind the back. This information may be a valuable addition to preoperative counseling, particularly for patients who are undergoing RTSA on the arm habitually used to manage toileting.
The proportion of patients who were able to manage toileting with the involved arm after primary RTSA in this study (92%) was similar to that previously reported in studies that addressed this issue of toileting after RTSA. In a systematic review of the literature that included 6 studies reporting toileting ability after RTSA, Rojas et al22 reported that 92% of the patients were able to manage toileting after RTSA. Similarly, our reported prevalence of impairment in toileting ability after primary RTSA of 46% is comparable to reported rates in the studies included in that systematic review (20%-45%).9,15,17,19,25,29
Our study differs from previous studies on this topic in a few important ways. First, no previous studies have considered in their analysis whether the arm that underwent RTSA was the arm involved in toileting. According to our results, this differentiation is important as preoperative toileting ability was significantly different between these 2 groups of patients. In addition, as may be expected, primary RTSA had minimal to no effect on toileting ability in patients who underwent the procedure on the arm that was not used to perform this task. Second, none of the previous studies reported the change from preoperative to postoperative toileting ability with the operative shoulder. In this study, analysis of toileting ability both preoperatively and postoperatively showed that it is more likely than not that in patients who undergo primary RTSA on the arm used to manage toileting, their toileting ability will improve or be preserved after the procedure.
Despite the finding that primary RTSA resulted in a statistically significant improvement in toileting ability, almost half of the patients continued to have some level of toileting difficulty postoperatively. Our results revealed that preoperative toileting ability and postoperative ROM behind the back are factors associated with toileting difficulties after primary RTSA. The single most important variable associated with toileting difficulties after primary RTSA was the presence of preoperative difficulties in performing this task. Most of the patients improved by only 1 point on the toileting Likert scale postoperatively, and as a result, patients who had severe toileting difficulties preoperatively were more likely to continue to have some level of toileting difficulty after the procedure. Although this is a nonmodifiable variable, it is an important finding for preoperative counseling on this issue.
Our finding that postoperative motion behind the back is strongly related to toileting ability after RTSA confirms this motion as a functional measurement16 and supports its use as an outcome measure despite its questioned validity as a measure of internal rotation glenohumeral motion.6,16 Although this finding may seem obvious, no previous study has formally assessed the nature and magnitude of the association between motion behind the back and toileting ability. We found no association between the degree of internal rotation motion with the arm abducted at 90° and toileting ability. This result suggests than motion behind the back is a better indicator than internal rotation motion at 90° in predicting toileting difficulties in patients undergoing primary RTSA. Motion behind the back is a complex motion that involves not only internal rotation but also a combination of movements between the glenohumeral joint, scapulothoracic articulation, and elbow.16
Postoperative internal rotation behind the back is a variable potentially influenced by the design of the implant system used. Several in vitro biomechanical and computer modeling studies have reported that inferior glenosphere placement,30 glenoid lateralization,12,30,34,35 and lowering of the humeral neck-shaft angle8,35 lead to increased internal rotation after RTSA. In our study, all patients were treated with inferiorly implanted lateralized glenospheres and humeral components with a lower, 135° neck-shaft angle. However, there were differences in the amount of glenoid lateralization and humeral lateralization of the different constructs used. Although lateralization of the more-medialized Grammont-style glenospheres improves internal rotation,12,30,34,35 Tashjian et al,27 in a biomechanical cadaveric study, showed that incremental glenosphere lateralization of lateralized components does not significantly affect passive or active internal rotation. In accordance with this finding, incremental glenosphere lateralization was not associated with improved toileting ability after RTSA in our study. Similarly, although humeral lateralization has been suggested as the most promising parameter to optimize RTSA biomechanics given its decreased muscle force and increased stability profile,13 we did not find any effect of humeral lateralization on toileting ability after RTSA. It may be that this study is underpowered to detect differences in toileting ability due to implant design.
The effect of subscapularis repair on internal rotation after RTSA is controversial. Friedman et al5 compared RTSA outcomes in patients with and without subscapularis repair. They found that the repair group had significantly more internal rotation behind the back than the nonrepair group; however, the difference was so small (ie, 1 vertebral level) that it was unlikely to be clinically meaningful. Other studies have found no effect of subscapularis repair on ROM or functional outcomes after RTSA.4,21,23,31,33 Our results support the findings of these studies as we did not find an association between subscapularis repair and toileting ability after RTSA. In our study, patients' toileting ability improved postoperatively regardless of subscapularis management.
There are several limitations to this study that are important when considering the results. The primary outcome of the study was assessed with a subjective tool using a Likert scale because toileting is an activity that can hardly be evaluated clinically in an objective way. However, the use of patient-reported outcomes and Likert scales in clinical research is well documented. In addition, the question used to collect the data in this study is part of the ASES score, which is a widely validated patient-reported outcome score in shoulder arthroplasty. The diagnosis and indication for RTSA have been shown to affect the final clinical result.32 To minimize variability, we purposefully studied the most homogeneous group of diagnoses possible (ie, only patients with cuff tear arthropathy or with osteoarthritis with glenoid bone) and controlled for this variable during the multivariate analysis. The results for the effect of RTSA on toileting with other diagnoses or for revision cases may not be the same as those seen in this cohort of patients. Even though several studies have found that ROM and function significantly increase within 1 year of RTSA2,14,24,28 and our patients were followed up for a minimum of 1 year, longer-term study is warranted. The surgical procedures in this study were performed by 1 surgeon who is experienced in RTSA, so the results may not be able to be extrapolated to other clinicians. Another limitation of this study was that only 2 examiners performed the internal rotation measurements, and the interobserver and intraobserver reliability of measures of internal rotation up the back has been reported to be poor.3,7 However, minimizing the number of observers performing motion measurements decreases the intraobserver variability.
Conclusion
Although there are concerns about the toileting ability after primary RTSA, this study demonstrates that in most patients, the ability to perform this task is improved or preserved after the procedure. Patients with severe preoperative toileting difficulties should be counseled regarding the risk of continuing to have some impairments in this task after the procedure. Postoperative internal rotation behind the back is highly related to toileting ability, and more studies on factors that may affect this motion after RTSA are required. In this clinical study, incremental glenoid or humeral lateralization did not affect toileting ability after primary RTSA.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
This study received approval from the Johns Hopkins Institutional Review Board (study no. IRB00190134).
Appendix 1. Toileting Questionnaire
We have a few questions about your life with a shoulder replacement. We are trying to develop a better understanding about essential daily activities related to personal hygiene in people with a shoulder replacement.
| Which arm did you habitually used to wipe your bottom before the surgery? | Left | Right |
| Have you had to change the way you wipe your bottom due to your shoulder replacement? | Yes | No |
| Do you still use the same hand as before the surgery when toileting? | Yes | No |
| Do you use any assistive device or aid to wipe yourself after toileting? | Yes | No |
| If yes, please specify: | ||
References
- 1.Chen A.L., Bain E.B., Horan M.P., Hawkins R.J. Determinants of patient satisfaction with outcome after shoulder arthroplasty. J Shoulder Elbow Surg. 2007;16:25–30. doi: 10.1016/j.jse.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 2.Collin P., Matsukawa T., Denard P.J., Gain S., Lädermann A. Pre-operative factors influence the recovery of range of motion following reverse shoulder arthroplasty. Int Orthop. 2017;41:2135–2142. doi: 10.1007/s00264-017-3573-4. [DOI] [PubMed] [Google Scholar]
- 3.Edwards T.B., Bostick R.D., Greene C.C., Baratta R.V., Drez D. Interobserver and intraobserver reliability of the measurement of shoulder internal rotation by vertebral level. J Shoulder Elbow Surg. 2002;11:40–42. doi: 10.1067/mse.2002.119853. [DOI] [PubMed] [Google Scholar]
- 4.Edwards T.B., Williams M.D., Labriola J.E., Elkousy H.A., Gartsman G.M., O'Connor D.P. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:892–896. doi: 10.1016/j.jse.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 5.Friedman R.J., Flurin P.H., Wright T.W., Zuckerman J.D., Roche C.P. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg. 2017;26:662–668. doi: 10.1016/j.jse.2016.09.027. [DOI] [PubMed] [Google Scholar]
- 6.Ginn K.A., Cohen M.L., Herbert R.D. Does hand-behind-back range of motion accurately reflect shoulder internal rotation? J Shoulder Elbow Surg. 2006;15:311–314. doi: 10.1016/j.jse.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Han S.H., Oh K.S., Han K.J., Jo J., Lee D.H. Accuracy of measuring tape and vertebral-level methods to determine shoulder internal rotation. Clin Orthop Relat Res. 2012;470:562–566. doi: 10.1007/s11999-011-2112-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keener J.D., Patterson B.M., Orvets N., Aleem A.W., Chamberlain A.M. Optimizing reverse shoulder arthroplasty component position in the setting of advanced arthritis with posterior glenoid erosion: a computer-enhanced range of motion analysis. J Shoulder Elbow Surg. 2018;27:339–349. doi: 10.1016/j.jse.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 9.Kemp A.L., King J.J., Farmer K.W., Wright T.W. Reverse total shoulder arthroplasty in wheelchair-dependent patients. J Shoulder Elbow Surg. 2016;25:1138–1145. doi: 10.1016/j.jse.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Lapner P.L.C., Sabri E., Rakhra K., Bell K., Athwal G.S. Comparison of lesser tuberosity osteotomy to subscapularis peel in shoulder arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012;94:2239–2246. doi: 10.2106/JBJS.K.01365. [DOI] [PubMed] [Google Scholar]
- 11.Levy J.C., Everding N.G., Gil C.C., Stephens S., Giveans M.R. Speed of recovery after shoulder arthroplasty: a comparison of reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1872–1881. doi: 10.1016/j.jse.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Li X., Knutson Z., Choi D., Lobatto D., Lipman J., Craig E.V. Effects of glenosphere positioning on impingement-free internal and external rotation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:807–813. doi: 10.1016/j.jse.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Liou W., Yang Y., Petersen-Fitts G.R., Lombardo D.J., Stine S., Sabesan V.J. Effect of lateralized design on muscle and joint reaction forces for reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:564–572. doi: 10.1016/j.jse.2016.09.045. [DOI] [PubMed] [Google Scholar]
- 14.Maier M.W., Caspers M., Zeifang F., Dreher T., Klotz M.C., Wolf S.I. How does reverse shoulder replacement change the range of motion in activities of daily living in patients with cuff tear arthropathy? A prospective optical 3D motion analysis study. Arch Orthop Trauma Surg. 2014;134:1065–1071. doi: 10.1007/s00402-014-2015-7. [DOI] [PubMed] [Google Scholar]
- 15.Maier M.W., Zeifang F., Caspers M., Dreher T., Klotz M.C., Rettig O. Can reverse shoulder arthroplasty in post-traumatic revision surgery restore the ability to perform activities of daily living? Orthop Traumatol Surg Res. 2015;101:191–196. doi: 10.1016/j.otsr.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Mallon W.J., Herring C.L., Sallay P.I., Moorman C.T., Crim J.R. Use of vertebral levels to measure presumed internal rotation at the shoulder: a radiographic analysis. J Shoulder Elbow Surg. 1996;5:299–306. doi: 10.1016/s1058-2746(96)80057-7. [DOI] [PubMed] [Google Scholar]
- 17.Mellano C., Kupfer N., Thorsness R. Functional results of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:990–996. doi: 10.1016/j.jse.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 18.Michener L.A., McClure P.W., Sennett B.J. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587–594. doi: 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- 19.Morris B.J., Haigler R.E., O'Connor D.P., Elkousy H.A., Gartsman G.M., Edwards T.B. Outcomes of staged bilateral reverse shoulder arthroplasties for rotator cuff tear arthropathy. J Shoulder Elbow Surg. 2015;24:474–481. doi: 10.1016/j.jse.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 20.Richards R.R., An K.-N., Bigliani L.U., Friedman R.J., Gartsman G.M., Gristina A.G. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 21.Roberson T.A., Shanley E., Griscom J.T., Granade M., Hunt Q., Adams K.J. Subscapularis repair is unnecessary after lateralized reverse shoulder arthroplasty. JBJS Open Access. 2018;3:e0056. doi: 10.2106/JBJS.OA.17.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rojas J., Joseph J., Liu B., Srikumaran U., McFarland E.G. Can patients manage toileting after reverse total shoulder arthroplasty? A systematic review. Int Orthop. 2018;42:2423–2428. doi: 10.1007/s00264-018-3900-4. [DOI] [PubMed] [Google Scholar]
- 23.Routman H.D. The role of subscapularis repair in reverse total shoulder arthroplasty. Bull NYU Hosp Jt Dis (2013) 2013;71(Suppl 2):S108–S112. [PubMed] [Google Scholar]
- 24.Schwartz D.G., Cottrell B.J., Teusink M.J., Clark R.E., Downes K.L., Tannenbaum R.S. Factors that predict postoperative motion in patients treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1289–1295. doi: 10.1016/j.jse.2013.12.032. [DOI] [PubMed] [Google Scholar]
- 25.Stevens C.G., Struk A.M., Wright T.W. The functional impact of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1341–1348. doi: 10.1016/j.jse.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 26.Talley K.M.C., Wyman J.F., Bronas U.G., Olson-Kellogg B.J., McCarthy T.C., Zhao H. Factors associated with toileting disability in older adults without dementia living in residential care facilities. Nurs Res. 2014;63:94–104. doi: 10.1097/NNR.0000000000000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tashjian R.Z., Burks R.T., Zhang Y., Henninger H.B. Reverse total shoulder arthroplasty: a biomechanical evaluation of humeral and glenosphere hardware configuration. J Shoulder Elbow Surg. 2015;24:e68–e77. doi: 10.1016/j.jse.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 28.Tiusanen H., Sarantsin P., Stenholm M., Mattie R., Saltychev M. Ranges of motion after reverse shoulder arthroplasty improve significantly the first year after surgery in patients with rheumatoid arthritis. Eur J Orthop Surg Traumatol. 2016;26:447–452. doi: 10.1007/s00590-016-1795-6. [DOI] [PubMed] [Google Scholar]
- 29.Triplet J.J., Everding N.G., Levy J.C., Moor M.A. Functional internal rotation after shoulder arthroplasty: a comparison of anatomic and reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:867–874. doi: 10.1016/j.jse.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 30.Virani N.A., Cabezas A., Gutierrez S., Santoni B.G., Otto R., Frankle M. Reverse shoulder arthroplasty components and surgical techniques that restore glenohumeral motion. J Shoulder Elbow Surg. 2013;22:179–187. doi: 10.1016/j.jse.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 31.Vourazeris J.D., Wright T.W., Struk A.M., King J.J., Farmer K.W. Primary reverse total shoulder arthroplasty outcomes in patients with subscapularis repair versus tenotomy. J Shoulder Elbow Surg. 2017;26:450–457. doi: 10.1016/j.jse.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 32.Wall B., Nove-Josserand L., O'Connor D.P., Edwards T.B., Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 33.Werner B.C., Wong A.C., Mahony G.T., Craig E.V., Dines D.M., Warren R.F. Clinical outcomes after reverse shoulder arthroplasty with and without subscapularis repair: the importance of considering glenosphere lateralization. J Am Acad Orthop Surg. 2018;26:e114–e119. doi: 10.5435/JAAOS-D-16-00781. [DOI] [PubMed] [Google Scholar]
- 34.Werner B.S., Chaoui J., Walch G. Glenosphere design affects range of movement and risk of friction-type scapular impingement in reverse shoulder arthroplasty. Bone Joint J. 2018;100B:1182–1186. doi: 10.1302/0301-620X.100B9.BJJ-2018-0264.R1. [DOI] [PubMed] [Google Scholar]
- 35.Werner B.S., Chaoui J., Walch G. The influence of humeral neck shaft angle and glenoid lateralization on range of motion in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1726–1731. doi: 10.1016/j.jse.2017.03.032. [DOI] [PubMed] [Google Scholar]
- 36.Werthel J.-D., Walch G., Vegehan E., Deransart P., Sanchez-Sotelo J., Valenti P. Lateralization in reverse shoulder arthroplasty: a descriptive analysis of different implants in current practice. Int Orthop. 2019;43:2349–2360. doi: 10.1007/s00264-019-04365-3. [DOI] [PubMed] [Google Scholar]
- 37.Wiater B.P., Boone C.R., Koueiter D.M., Wiater J.M. Early outcomes of staged bilateral reverse total shoulder arthroplasty: a case-control study. Bone Joint J. 2013;95-B:1232–1238. doi: 10.1302/0301-620X.95B9.31445. [DOI] [PubMed] [Google Scholar]