Abstract
Based on the recent reports of World Health Organization, increased antibiotic resistance prevalence among bacteria represents the greatest challenge to human health. In addition, the poor solubility, stability, and side effects that lead to inefficiency of the current antibacterial therapy prompted the researchers to explore new innovative strategies to overcome such resilient microbes. Hence, novel antibiotic delivery systems are in high demand. Nanotechnology has attracted considerable interest due to their favored physicochemical properties, drug targeting efficiency, enhanced uptake, and biodistribution. The present review focuses on the recent applications of organic (liposomes, lipid-based nanoparticles, polymeric micelles, and polymeric nanoparticles), and inorganic (silver, silica, magnetic, zinc oxide (ZnO), cobalt, selenium, and cadmium) nanosystems in the domain of antibacterial delivery. We provide a concise description of the characteristics of each system that render it suitable as an antibacterial delivery agent. We also highlight the recent promising innovations used to overcome antibacterial resistance, including the use of lipid polymer nanoparticles, nonlamellar liquid crystalline nanoparticles, anti-microbial oligonucleotides, smart responsive materials, cationic peptides, and natural compounds. We further discuss the applications of antimicrobial photodynamic therapy, combination drug therapy, nano antibiotic strategy, and phage therapy, and their impact on evading antibacterial resistance. Finally, we report on the formulations that made their way towards clinical application.
Keywords: nanomedicine, antibacterial resistance, inhibition of antibacterial resistance, anti-biofilm mechanisms, organic nanosystems, inorganic nanosystems
1. Introduction
The resistance to antibiotics is defined as the ability of bacteria causing disease to resist the therapeutic effects of antibacterial drugs. The danger of antibiotic resistance comes from; it resulted in enormous human and economic losses. About 700,000 people have died each year worldwide thanks to the inappropriate antibiotic usage that develops resistance to conventional therapy [1]. For instance, Staphylococcus aureus (MRSA) that resist methicillin was reported to cause almost 120,000 blood-borne infections and 20,000 related deaths in the United States in 2017 [2]. Moreover, carbapenem-resistant Enterobacteriaceae (CRE) has been regarded as a public health threat that requires prompt and invasive actions [3].
Antibiotic-resistant infections were reported to give rise to losses estimated at $55–70 billion annually in USA. In Europe, the losses surpassed €1.5 billion annually [4,5]. The excessive and improper consumption of antibacterials resulted in the emergence of more aggressive strains that do not respond to standard treatments [6]. In addition, there are many concerns related to conventional antibacterial drug usage; such as low water solubility, diminished stability, minimum oral bioavailability, drug targeting complexity, and depressed patient compliance as a result of frequent drug administration and variable toxicity [7]. The disastrous human and economic cost of antibiotic resistance renders the development of newalternative strategies more urgent in order to confront this massive challenge.
To highlight the application of nanosystems as antibacterial delivery agents, it is worth identifying the mechanism by which bacteria form colonies that escape conventional antibiotic therapies. Two forms of bacterial growth exist; the first form is the planktonic growth, which is characterized by a free-swimming unicellular phase existence that is not attached to a surface; while the second form is the biofilm growth phase, which is described as a multicellular sessile state that forms communities [8]. Biofilm represents an evolved system that permits bacteria to be alive in hostile environments, forming permanent colonies, with high ability to dissociate and form new colonies [9,10].
Biofilm bacterial growth is composed of a dense and hydrated group of bacteria attached to each other and to a surface where they are surrounded by an external matrix composed of exo polysaccharide, amino acids, and extracellular deoxyribonucleic acid (DNA) [11]. It is considered to be 1000 times more resilient to conventional antibiotic treatments relative to planktonic bacterial growth [12]. Biofilm is associated with many diseases such as lung, colon, urethra, eye, and ear infections, in addition to infective endocarditis, gum-related infections, and wound-related infections [13]. Biofilm bacteria are liable to cell-density-dependent regulation from its extracellular polymeric substances (EPS) matrix; consequently, they are released into the external environment as free-floating bacteria. Moreover, activation of the normal nonpathogenic commensal bacteria of the human body into virulent forms is facilitated by both biofilms and immune responses of host [14]. Increased genetic mutations rates within biofilms assist the development of survival mechanisms. For example, up-regulation of proteins and expression of particular efflux pumps might diffuse across the biofilm. Moreover, elevated expression of toxin–antitoxin modules stops key cell functions such as translation [15,16]. Due to the diversity and anonymous biofilm-resistant mechanisms, innovative nanosystems should be developed to stop the spread of resistant bacterial infections.
The present review will discuss role of nanosystems in overcoming the bacterial resistance and will outline the various mechanisms of nanosystems as antibacterial drug delivery agents. These nanosystems are classified into two categories; the first one is organic nanosystems such as liposomes, lipid-based nanoparticles, polymeric micelles, and polymeric nanoparticles, and the second one is inorganic nanosystems such as silver, silica, magnetic, zinc oxide (ZnO), cobalt, selenium, and cadmium nanoparticles. Clinical trials and challenges in the clinical translation of nanomedicines will also be discussed.
2. Nanosystems’ Role in Overcoming Antibiotic Resistance
The emergence of aggressive bacteria together with the limited production of new antibacterial drugs has resulted in inefficiency of current antibiotic therapy with relevant risks on human health. The availability of new antibacterial agents appeared to be a very complex process in view of the capability to produce new effective and safe drugs, in addition to the high production costs and the time required for approval of new drugs that takes about 10–15 years [7]. In 2016, many antibiotics were clinically tested for the market in the United States of America [1]. Sadly, however, in the last decades, linezolid was the only approved antibiotic together with the recently discovered teixobactin [17].
Based on the aforementioned facts, the current researches are aimed towards the discovery of novel techniques to overcome these relevant challenges and, hence, the efficiency of conventional antibacterial drugs will be improved. Nanomedicine plays a vital role in enhancing the effectiveness of existent therapeutics, by enhancing the physicochemical properties and stability of antibiotics, offering a chance of biofilm internalization, prolongation of antibiotic release, in addition to the capability of targeted delivery to the site of infection and improved systemic circulation with a consequent reduction of the related side effects compared to the corresponding free drugs [18].
2.1. Mechanism of Nanosystems as Antibacterial Drug Delivery Agents
The physicochemical properties of nanosystems, particle size, surface charge, and solubility, are the key factors that control vital processes for example intracellular uptake, biodistribution, or clearance. Nanometer-sized particles enable better drug loading efficiency of both hydrophilic and lipophilic antibiotics and hence enhanced antibacterial effect [19]. In addition to a more expected cellular internalization of the antibiotics loaded nanosystems was achieved by passing the reticulo-endothelial system [20]. Surface charge and the zeta (ζ)-potential of nanosystems drives interactions with proteins, tissues, or with various components of the tissue, thus affecting cellular biodistribution and uptake. Host cells such as macrophages with anionic nature thus attract positively charged nanosystems compared to uncharged and negatively charged ones [21].
Hydrophobicity of nanosystems plays a great function in targeting of the drug delivery related to interactions with the phospholipid layer of the bacterial membrane [18]. On the contrary, hydrophilic nanosystems interact less with opsonins thus, having longer blood circulation compared with hydrophobic nanosystems [22]. Thus, the enhanced actions of nanosystems as antibacterial drug delivery systems arise from various mechanisms, including their ability to optimize the physicochemical characteristics of entrapped antibacterial drugs, their favored accumulation near the cytoplasm, their electrostatic interactions with bacterial membrane, the high oxidizing power and production of reactive oxygen species, the prevention of unwanted interactions and protection of antibacterials against degradation and the better clinical use of antibacterials through more patient acceptable routes [23].
Interestingly, it was found that nano-sized systems not only improve the therapeutic activity of antibacterial agents but also restrain the stimulation of resistance by overcoming bacteria developed resistance strategies that involve drug decomposition by β-lactamase, efflux pumps, or thickening of bacterial cell walls [24].
2.2. Classification of Nanosystems
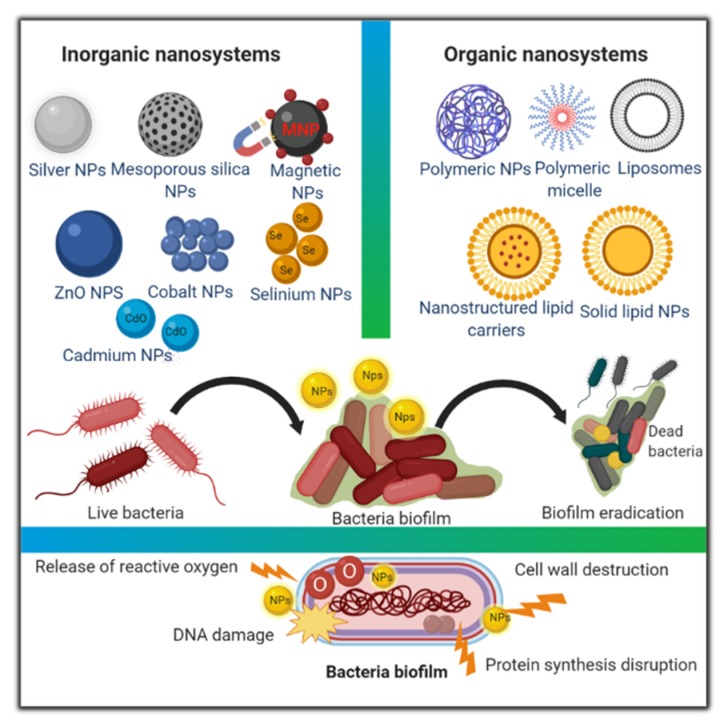
Nanosystems can be categorized based on their matrix properties and the material constituting them into inorganic and organic nanosystems [25], (Figure 1).
Figure 1.
Graphical outline of various classes of nanosystems with illustration of their possible anti-biofilm mechanisms.
Inorganic nanosystems represent a class of nanosystems that originates from inorganic oxides. Their synthesis technique depends on chemical reduction of metallic salts with a reductant. The reaction environmental parameters, for example temperature and pH, play a major function in determining the specificities of these materials, consequently affecting their loading capacity, the in vitro drug release kinetics, aggregation, and hence their antibacterial effect [26].
Furthermore, organic nanosystems such as liposomes, lipid-based nanoparticles, polymeric micelles and polymeric nanoparticles have preferable biodegradability and biocompatibility features, making them suitable candidates for clinical use [27]. Herein, we will report on the recent updates of organic and inorganic nanosystems as antibacterial drug delivery systems with a brief description of each system. Then, we will briefly discuss the recent trends used to overcome antibacterial resistance.
2.2.1. Organic Nanosystems
Liposomes
• Composition and characteristics of liposomes
Liposomes are considered the most extensively evaluated antimicrobial drug delivery nanosystems. They are characterized by spherical structures made up of phospholipid bilayer(s) surrounding an inner aqueous space, ranging in size from 0.02 to 10 µm [28,29,30]. The efficacy of antibacterial-loaded liposomes in biofilm eradication relies on the physicochemical properties of liposomes that control their stability and in vivo interactions [31]. Moreover, liposomes are regarded as inclusive carriers for both hydrophilic and hydrophobic therapeutics. Large unilamellar vesicles including a large volume of aqueous phase are the best carrier for hydrosoluble agents, while hydrophobic compounds can be enclosed in the lipid bilayer of multilamellar or small unilamellar vesicles [32,33].
For antibiotic delivery small unilamellar vesicles of ≃100 nm displayed high capability in the eradication of bacterial strains [34]. Liposomes proved to be useful for the management of topical [35], vaginal [36], pulmonary [37], and ocular [38] bacterial infections.
• Advantages of antibiotics-loaded liposomes as drug delivery agents:
1- Better protection and enhanced antibiotics biodistribution.
Liposomes improved antibiotics pharmacokinetics and pharmacodynamics in a way where inclusion within the liposomal vesicles controls and sustains drug release, maintaining proper antibiotic level for a long enough time, on the contrary to free antibiotics administration that requires several doses per day thus minimizing patient adherence to therapy [39]. In addition, encapsulation of antibiotics within liposomal vesicles safeguards antibiotics against the degradative effect of the defense mechanisms of the body, thus preserving their therapeutic response [40].
In an attempt to enhance the stabilization of orally administered peptide antibiotics, vancomycin was encapsulated within liposomes containing specific tetra ether lipid. The results of in vivo study on Wistar rats expressed a strong enhancement in the oral bioavailability of vancomycin using the liposomal formulation (4.82 ± 0.56%), where the given oral dose of vancomycin reached the blood after one hour, which is considered a very good achievement for the oral administration of peptide antibiotics [41]. Further, administrations of either dicloxacillin-loaded liposomes or dicloxacillin-loaded chitosan-coated liposomes were evaluated against MRSA infections. A significantly wider zone of inhibition of dicloxacillin-loaded liposomes compared to free drug and drug-loaded chitosan-coated liposomes (55.0 ± 1.70, 34.3 ± 0.5, 33.0 ± 0.89 mm, respectively) confirmed the better antibacterial activity of small-sized liposomes as well as better drug biodistribution. Nevertheless, testing formulations in vivo on an MRSA infected animal model is recommended [42].
2- Selective biofilm targeting affinity.
The surface structure of liposomes specifies the type of interaction with the target bacterial biofilm. For nonspecific interactions, the charge of the liposome membrane plays a vital role. Consequently, the liposomes with positive charge showed the strongest interactions with the negatively charged bacterial biofilms. However, for a specific interaction with the target, liposomes are usually equipped with either proteins, antibodies, specific oligosaccharide chains, or immunoglobulin fragments that express an affinity to certain receptors located on the target biofilm, in addition to the possibility of formulating pH-sensitive or thermo-sensitive liposomes vesicles [31].
To improve the gastrointestinal targeting affinity, Wenxi Wang et al. [43] designed S-layer proteins coated positively charged liposomes. S-layer proteins are crystalline arrays of self-assembled protein located on the surface of bacterial cell, that have the ability to bond to cationic liposomes through their carboxyl groups, and then self-reassemble as a functional coat of liposomes. The authors revealed that coating liposomes with S-layer proteins results in significant improvement of the gastrointestinal adhesion property. Wheat germ agglutinin-conjugated liposomes with surface grafted cyclodextrin were developed to overcome oral infections. Two physicochemical variable drugs (ciprofloxacin and betamethasone) were successfully encapsulated and showed a prolonged co-drug release in saliva over a period of 24 h and a significant increase in oral cell survival against Aggregatibacter actinomycetemcomitans biofilm combined with reduced inflammation [44].
Moayad Alhariri et al. [45] tested the targeting efficiency of neutral and negatively charged gentamicin-loaded liposomes towards P. aeruginosa (Pseudomonas aeruginosa) and K. oxytoca (Klebsiella oxytoca) pathogenic strains. Surprisingly, it was found that anionic liposomes improved drug encapsulation and enhanced the targeting affinity of gentamicin to bacterial biofilm better than either neutral antibiotic-loaded liposomes or free gentamicin. This could be better interpreted based on the increased encapsulation efficiency of the positively charged antibiotic (gentamicin) within negatively charged liposomes based on the electrostatic interaction, followed by improved delivery of antibiotic-loaded negatively charged liposomes through a fusion mechanism that allows the direct injection of liposome-entrapped antibiotic into the cytoplasm of bacteria despite the repulsive forces.
3- Improved selectivity towards intracellular and extracellular bacterial strains.
Utilizing liposomes as drug delivery agents showed tremendous results in eradicating intracellular strains via enhancing antibiotic retention in the infected tissues, providing controlled drug release with minimal toxic effects, and maximizing the concentration at the infected area. For targeting macrophage infections, anti-tubercular drugs loaded within stealth liposomes with small interfering ribonucleic acid (RNA) were fabricated [46]. The prepared system successfully inhibited the transforming growth factor-β1, eliminating the infection compared to the free drug.
For extracellularly multiplying bacteria, including Pseudomonas aeruginosa, weakness of inhaled antibiotic for curing P. aeruginosa infection accompanied with cystic fibrosis was reported due to poor drug permeation, inactivation by sputum, reduced efficacy against the protective biofilm, and shortened lung residence. Bilton et al. [47] investigated the potential of inhalation suspension of amikacin-loaded liposome (ALIS) and inhalation solution of tobramycin (TIS) in an open-label, randomized, phase III clinical trial. The findings confirmed the hypothesis that ALIS was similar to TIS for curing chronic P. aeruginosa infection accompanied with cystic fibrosis as shown from the comparable enhancements in forced expiratory volume in 1 s (FEV1%) and reductions in P. aeruginosa sputum density that were identical in the 2 arms.
• Limitations of antibiotics-loaded liposomes as drug delivery agents:
Despite the significant improvements in antibiotics delivery using liposomes, these lipid vesicles also suffer from many drawbacks limiting their efficient usage.
-
1-
Physical and chemical instability problems, that can be minimized by addition of antioxidants and/or freeze-drying [28].
-
2-
The possibility of antibiotic leakage from liposomes under physiological conditions, that can be controlled by adding cholesterol which lead to stabilization of liposomal membrane [48].
-
3-
The low loading capacity of liposomes compromises the liposomal usage as antibiotic delivery agent. This challenge can be solved by maximizing electrostatic attractions between liposomes and oppositely charged antibiotic molecules [49,50].
-
4-
Special sterilization techniques are needed due to the sensitivity of lipids to high temperatures [51].
-
5-
Fabrication techniques are very complex, expensive, and difficult to be scaled up [52].
• Classification of liposomes:
Generally, liposomes have been categorized either based on their composition, vesicle size, bilayers number, and/or technique of preparation. In this context, the classification of liposomes according to their design and physicochemical characteristics into conventional, fusogenic, surface-modified, reactive liposomes encapsulating enzyme(s), antibiotic-metal co-encapsulating, liposomes-in-hydrogel, solid-supported liposomes, liposome-loaded scaffolds, and miscellaneous liposomes will be discussed [31].
1- Conventional Liposomes
Conventional liposomes are regarded as bare liposomes, lacking any surface modulations. They are made up of phospholipids with or without cholesterol addition. Based on the surface charge of the used lipids, they can be grouped into uncharged, negatively charged, or positively charged liposomes of which positively charged liposomes expressed dramatic improvements in biofilm targeting due to the electrostatic attraction with the anionic biofilm surface. Interestingly, Arikace™® and Lipoquin™® are two examples of conventional liposome preparations of amikacin and ciprofloxacin, respectively, which are used for cystic fibrotic patients with P. aeruginosa infections. Arikace™® passed phases II and III of clinical trials and Lipoquin™® passed a 14-day phase II trial, proving their tolerability, safety, improved biologic activity, and restoration of lung function [53,54].
2- Fusogenic Liposomes
Fusogenic liposomes are well famed as Fluidosomes™. They are distinguished by relatively soft lipid bilayers compared to the rigid conventional liposomes. The presence of special lipid (phosphatidyl ethanol amine) that renders the vesicles more fluid encourage the reduction of the membrane transition temperature and destabilize the lipid packing [55]. The enhanced anti biofilm activity of tobramycin Fluidosomes™ against many strains such as B. Cepacia (Burkholderia cepacia), S. maltophilia (Stenotrophomonas maltophilia), P. aeruginosa, E. coli (Escherichia coli), and S. aureus at sub-MIC (minimum inhibitory concentration) levels were reported compared to the corresponding free antibiotic [56]. Furthermore, Beaulac et al. [57] elucidated the superior in vivo bactericidal activity of tobramycin loaded in the negatively charged Fluidosomes™ agianst P. aeruginosa infection.
To realize the mechanism of fluid liposomes interaction with bacteria, Wang et al. [58] realized that the bactericidal effect of tobramycin encapsulated fluid liposomes occur fast when bacteria is co-cultured with liposomes as a result of fusion process between liposomes and bacteria rather than the prolonged residence and release of antibiotic. This fusion process is dependent on degree of fluidity, temperature, pH, and presence of divalent cations as well as the properties of bacterial membranes.
3- Surface-Modified Liposomes
The application of surface-decorated liposomes, for example mannosylated liposomes, immune liposomes, and PEGylated liposomes, is among the proposed strategies for designing long-circulating liposomes to surmount biofilm-related infections. However, the strategy still suffers from many optimization challenges. Tatsuhiro Ishida et al. [59] revealed the loss of long-circulating features of PEGylated liposomes following their intravenous administration to a mice model as evidenced by accelerated blood clearance. Although, polyethylene glycol (PEG) coat prevented this loss to some extent. The observation was attributed to the degree of PEGylation and the amount of lipid. Therefore, further studies will be imperative in order to design effective liposomal preparation suitable for clinical application.
To further examine the effect of the PEG coat on the anti-biofilm activity of liposomes, PEGylated anionic and cationic liposomes were formulated and tested against S. aureus biofilms. Surprisingly, the results revealed the loss of anti-biofilm activity of liposomes after coating with PEG [60]. On the other hand, rifampin-loaded cationic liposomes either with PEG coat or without had the same anti-biofilm activity towards to S. epidermidis biofilm [61]. To explain this, the authors concluded the direct relation between incubation time and the anti-biofilm efficacy.
4- Reactive enzyme(s)-loaded liposomes.
The use of either one or more enzyme(s) loaded within liposomes represents one of the pioneer approaches in the field of anti-biofilm therapy. Moreover, encapsulation of enzymes within liposomes vesicles guarantees their adsorption and stay near to the biofilm surface. The antibacterial activity of reactive-enzyme(s)-loaded liposomes are governed by many factors, such as the enzyme entrapment efficiency, zeta potential, and phospholipid composition of liposomes [62].
For example, endolysins enzymes were successfully encapsulated within cationic liposomes. Contrary to free endolysins that have limited activity, only towards Gm +ve strains, and unable to cross the outer membrane of Gm–ve ones, endolysins entrapped within liposomes could successfully cross bacterial membrane and reach their target peptidoglycan substrate, showing significant reduction in logarithmic growth of live cells of S. Typhimurium and E. coli Gm–ve biofilms [63].
Another approach, which relies on the production of hydrogen peroxide or other oxidizing agents having antimicrobial properties upon contact of enzymes with certain substrate, was discovered. To test this, encapsulation of either a single glucose oxidase (GO) enzyme or coupled glucose oxidase-horse radish peroxidase (GO-HRP) enzymes within DPPC/PI liposomes was performed. The coupling of enzyme with glucose substrate leads to production of hydrogen peroxide, which yields oxy acids that have powerful antibacterial activities against oral Streptococcus gordonii biofilms. In addition, it was concluded that coupled enzymes containing liposomes were more effective than single enzyme formulation [64].
Similarly, Jones et al. [65] encapsulated chloroperoxidase and lactoperoxidase in combination with glucose oxidase enzymes within DPPC/PI liposomes. The reactive liposomes expressed significant antibacterial activity towards Steptococcus gordonii oral biofilm attributed to the reaction of hydrogen peroxide and oxyacids produced with glucose, chloride, or thiocyanate enzyme substrates.
5- Antibiotic-Metal Co-Encapsulating Liposomes
Certain metals, for instance gallium, bismuth, and bismuth-ethanedithiol, have shown promising antibacterial effects. Their activity period comes from affecting iron-metabolism, alginate expression, bacterial adherence, or interference of quorum sensing (QS) signaling and production of virulence factors [66,67,68]. Following this approach, bismuth-ethanedithiol included in a tobramycin-loaded liposome preparation was fabricated by Alhariri and Omri [69]. At sub-minimum inhibitory concentration (MIC), liposomes-loaded metal tobramycin formulation weakens QS signaling and reduces the production of virulence factors such as lipase, chitinase, and protease, compared to both free tobramycin or tobramycin-loaded liposome preparation. In vivo antimicrobial activity of metal-tobramycin incorporated liposome formulation in rats chronically infected with P. aeruginosa showed significant count reduction of P. aeruginosa in lungs.
6- Liposomes-hydrogel system
This policy involves the application of antibacterial-loaded liposomes after being incorporated within a suitable gel base to provide a unique and robust formulation. The hydrogel formulation maintains integrity of the liposomal structure, provides tunable release rate, better bioadhesion, and possibility of surface modification [70]. For the first time, tetracycline HCl and tretinoin-loaded liposomes prepared by the thin film technique were incorporated in carbopol-based gel. The findings revealed enhanced extended release behavior of both drugs with an average 55% release of two drugs up to 24 h. Antibacterial efficacy of the prepared liposome in gel towards S. aureus and Streptococcus epidermidis biofilms has been confirmed. Therefore, it is an effective alternative option for treating Acne vulgaris [71].
Hydrogels also offer capacity for prolonged release of antibiotics for infection control in wounds. Raj Kumar Thapa and colleagues developed collagen mimetic peptide tethered vancomycin-loaded liposomes hybridized to collagen-based hydrogels for the management of MRSA infections. The formulation achieved sustained antibiotic release and enhanced antibacterial efficacy with successful management of wound infection within nine days [72]. In addition, an injectable, antibacterial, and self-healing multifunctional drug delivery system composed of adhesive liposomes loaded with bone morphogenetic protein 2 (BMP-2) incorporated into PEG hydrogels was successfully developed. The system could be used for the treatment of bone cavity damage and reduces the risk of postoperative infections. The presence of silver ions in the adhesive liposome PEG gel system showed effective inhibition of S. aureus and E. coli pathogens [73].
7- Liposomes supporting solid (SSLs) and liposome-loaded scaffolds (LLSs)
Liposome-supporting solid (SSLs) delivery relies on the loading of antibiotic-liposomes on solid particles surfaces. In this regard, the applicability of gentamicin-liposomes loaded onto particles of the calcium sulfate was tested. In vivo antibacterial study revealed the significant improvement of gentamicin SSLs more than gentamicin-loaded calcium sulfate and non-adsorbed liposomal gentamicin due to better targeting ability to the infection site [74].
Targeting bacterial biofilm may be achieved by designing LLSs, whereas antibiotics containing liposomes can be further loaded onto artificial bone scaffolds. To validate this technique, gentamicin-sulfate liposomes have been impregnated onto beta-tri calcium phosphate granules. The in vitro release profile exhibited initial fast release of liposomal gentamicin from the scaffold matrix followed by more prolonged release of the free antibiotic from liposomes. The designed delivery system LLSs displayed significantly elevated anti-biofilm activity compared to free antibiotic [75].
8- Miscellaneous liposomes
Miscellaneous liposomes such as biomineral-binding liposomes (BBLs) were proposed for treating device-associated osteomyelitis and for delivering antimicrobials to the skeletal muscles efficiently [76]. The applicability of liposomes to develop antimicrobial surfaces for construction of efficient medical devices was also explored. Tobramycin-loaded liposomes were immobilized on gold-deposited stainless-steel surfaces and antibacterial efficacy was evaluated against S. epidermidis (Staphylococcus epidermidis) (American type culture collection; ATCC 35984 and ATCC 12228) strains. Antibiotic-liposome coated surfaces were found to possess good antibacterial activity especially for non-biofilm forming strains [77]. Examples on the recent published studies of different types of liposomal preparations used to eradicate bacterial biofilm infections are illustrated in Table 1.
Table 1.
Examples on recently published studies on different types of liposomes used against bacterial biofilm infections.
| Liposome Type | Lipid Composition | Anti-Bacterial Drug/Nutraceutical Agents | Size | Biofilm | Findings | Reference Year |
|---|---|---|---|---|---|---|
| Conventional Liposomes | DPPC (Dipalmitoylphosphatidylcholine) | Calcifediol (25 (OH)D) | 151.2 ± 0.3 nm | P. aeruginosa |
|
2017 [37] |
| Conventional Liposomes | Egg yolk soybean L-α phosphatidyl choline |
|
280 nm–1.76 µm | Ocular post-surgery infections |
|
2018 [78] |
| Conventional Liposomes | pH-sensitive lipids (PSLs):Phosphatidylcholine (PCS 100):Cholesterol (1:3:1 w/w/w) | Vancomycin | 99.38 ± 0.59–105.60 ± 5.38 nm | MRSA |
|
2018 [79] |
|
Lipoid Lipoid + SDch Lipoid + PG DPPCT (Dipalmitoylphosphatidylcholine), DODAB (Dimethyldioctadecylammonium bromide) |
Azithromycin | 132–217 nm | MRSA |
|
2018 [35] |
| Conventional Liposomes | Hydrogenated soy phosphatidylcholine and cholesterol (7:3 w/w) | Ciprofloxacin nanocrystals | ∼130 nm | P. aeruginosa. |
|
2019 [80] |
| Conventional Liposomes | P90 G (Phospholipon 90 G), cholesterol |
|
∼200 nm | K. pneumoniae |
|
2019 [81] |
| Conventional Liposomes | Phospholipon 90 G | Biosurfactants isolated from Lactobacillus gasseri Bc9 | <200 nm | MRSA |
|
2019 [82] |
| Conventional Liposomes | Egg yolk Lecithin | Cinnamaldehyde | 75–92.14 nm | S. aureus |
|
2019 [83] |
| Fusogenic Liposomes | Dope/Dppc/CHe MS (4:2:4 molar ratios) | Fusidic acid | 98.77–99 nm | S. epidermidis (Staphylococcus epidermidis), Acinetobacter baumannii |
|
2015 [84] |
| Surface-Modified Liposomes | PC: DSPE PEG: Chol: SA (6.5:0.5:2:1 mole %) | β-Lapachone | 88.7–112.4 nm | MRSA C. neoformans (Cryptococcus neoformans) |
|
2015 [85] |
| Conventional liposomes Surface-Modified Liposomes Immobilized at surface of chitosan nanofiber mesh |
Dipalmitoylphosphatidylcholine (DPPC)- cholesterol DPPC, cholesterol, DSPE-PEG-Mal and PE-Rho). Mal; (maleimide), Rho; (Rhamnolipids) |
Gentamicin | 126.25–140.26 nm |
E. coli
P. aeruginosa S. aureus |
|
2015 [86] |
| Surface- Modified Liposomes | Phospholipid, cholesterol, tween 80, vitamin E (6:1:1.8:0.12 mass ratios). | Gallic acid | 153.2 ± 1.4 nm |
E. Coli
S. aureus |
|
2019 [87] |
| Surface- Modified Liposomes | Phospholipids + Rhamnolipids (1:0, 10:1, 5:1, 2:1, 1:1 w/w). | Curcumin | 46.4–251 nm | - |
|
2019 [88] |
| Surface-Modified Liposomes |
|
Ciprofloxacin Betamethasone |
∼100 nm | Aggregatibacter actinomycetemcomitans |
|
2020 [44] |
| Liposomes-in-Hydrogel | Phospholipids (PC) | Isoniazide N-Dodecanoyl isonicotinohydrazide (DINH) |
∼130 nm | M. tuberculosis |
|
2019 [89] |
| Reactive Liposomes Encapsulating Enzyme (s) | DPPC, cholesterol, hexadecylamine | Endolysins | 303 nm |
|
|
2019 [63] |
Lipid-Based Nanoparticles
Solid lipid-nanoparticles (SLNs) and nanostructured lipid carriers (NLCs) represent the two main nanoparticles sub-types made up of lipids. SLNs are drug delivery systems in colloid form composed of high melting-stable lipids that were developed to beat the instability problems of liposomes [90]. Techniques for fabrication of SLNs include; solvent emulsification-diffusion, supercritical fluid, microemulsion-based, and film-ultrasound dispersion method [91].
SLNs are characterized by their nanosize range, thus bypassing uptake by reticuloendothelial system; provide high protective effect of incorporated drugs from degradation, offer great targeting, and controlled release opportunity. In addition to their biocompatibility and biodegradability, the possibility of easy scale up may be another advantage. However, their therapeutic application may be hindered by their reduced drug loading potential and possibility of drug ejection during storing [92].
In the war against resistant bacterial infections, researchers explored the idea that the bioavailability of many antibacterial drugs were enhanced upon their incorporation within SLNs, such as clarithromycin, rifampicin, tobramycin, and ciprofloxacin [93,94], in addition to many formulation patents reporting the oral use of SLNs loaded with anti-tubercular drugs [95,96].
Nanostructured lipid carriers (NLCs) are considered as the advanced type of SLNs. NLCs composed of a rigid matrix blended with a liquid oil to form an unstructured matrix. Unlike SLNs, they form an imperfect core and an amorphous matrix for better drug loading ability and minimized drug escape from the matrix during storing [97]. In addition to their high loading capacity for both hydrophilic and lipophilic therapeutics is their capability to pass through multiple biological barriers and efficiently deliver the enclosed therapeutic moieties [98]. Furthermore, NLCs can be fabricated to be stimulated by various parameters such as pH and light for controlling the drug release [99,100]. However, the literature on the usage of NLCs for delivering antibacterial drugs is limited (Table 2). Therefore, there is an imperative requirement to further examine this system for improving antibacterial delivery.
Table 2.
Examples on recent studies on lipid-based nanoparticles against bacterial infections.
| Lipid Composition | Drug | Size | Biofilm | Findings | Reference Year |
|---|---|---|---|---|---|
| SLNs | |||||
| Compritol 888 ATO (a lipid excipient) | Vancomycin- Linoleic acid complex | 102.7 ± 1.01 | S. aureus & MRSA |
|
2014 [101] |
| Compritol 888 ATO | Clotrimazole- silver complex | 124.1 ± 2.5 nm | S. aureus & MRSA |
|
2015 [102] |
| Glyceryl monostearate Precirol Stearylamine |
Rifampin | 101 ± 4.7 nm | S. epidermidis |
|
2016 [103] |
| Stearic acid | Levofloxacin | 237.82 nm |
S. aureus
E. coli |
|
2016 [104] |
| Glyceryl behenate Tripalmitin Stearic acid |
Clarithromycin | 318–526 nm. | S. aureus |
|
2019 [90] |
| Glycerol monostearate | Furosemide-silver complex (Ag-FSE) | 129.8 ± 38.5 nm |
P. aeruginosa
S. aureus |
|
2019 [105] |
| NLCs | |||||
| pH responsive NLC (Stearic acid and oleic acid) | Vancomycin | 225.2 ± 9.1 nm | S. aureus (Resistant and Sensitive) |
|
2019 [106] |
| Cetyl palmitate and caprylic acid | Mupirocin | 99.8–235 nm | MRSA |
|
2019 [107] |
Stearic acid and oleic acid
|
Rifampicin |
|
M. tuberculosis |
|
2019 [108] |
Polymeric Micelles
A typical self-assembled micellization procedure involves the attachment of a hydrophilic block to a lipophilic block resulting in formation of micelles of amphiphilic di-block (or multiple block) copolymers with some characteristic structural properties that differ from either parent. Common polymeric backbones used for constructing micellar systems include chitosan, polyethylene oxide, polypropylene oxide, polybutylene oxide, polystyrene oxide, polyethyleneimine, and polycaprolactone. The size of polymeric micelles is from almost 10 to 100 nm [109].
The polymeric micelles size may be easily controlled by varying the molecular weight and the aggregation number of the amphiphiles, the ratio between hydrophilic and hydrophobic parts, the volume of solvent trapped within the core, and the used technique for preparing [110]. Using polymeric micelles as antibiotic delivery systems can dramatically enhance the pharmacokinetics and biodistribution of entrapped antibiotics. Micellar nanocarriers have the capacity to load poorly water-soluble drugs into their cores [111], better protection of incorporated antibiotics from destructive enzymes, prevention of drug interaction with blood proteins, thus keeping its appropriate plasma concentration.
More recently, for better targeting efficiency, stimuli dual-responsive polymeric micelles have been explored. For instance, poly (N-iso propyl acrylamide) is a commonly used temperature-responsive polymer. However, most studies on dual responsive polymeric micelles were limited to anticancer drugs with very scarce reports on antimicrobials [112,113]. The different pharmaceutical applications of antibacterial polymeric micelles are summarized in Table 3.
Table 3.
Examples on recent studies on polymeric micelles against bacterial infections.
| Composition | Drug | Size | Biofilm | Findings | Reference Year |
|---|---|---|---|---|---|
| Cholesterol conjugated Poly (ethylene glycol) and anchored with transcriptional activator TAT (a trans-activator of transcription) peptide |
Ciprofloxacin | 180 nm |
|
|
2008 [114] |
| Poly (lactic acid-co-glycolic acid)-block-poly (ethylene glycol)-alendronate copolymer | Vancomycin | 39.62–55.08 nm | S. aureus |
|
2015 [115] |
| Mixed-shell-polymeric-micelles consisting of a hydrophilic PEG-shell and pH-responsive poly (β-amino ester) |
Triclosan | 160 nm | S. aureus |
|
2016 [116] |
| Silver decorated amphiphilic diblock copolymers, poly (ε-caprolactone)-block-poly(aspartic acid) | Curcumin | 90–95 nm | P. aeruginosa S. aureus |
|
2017 [117] |
| Ethylene oxide-propylene oxide triblock copolymers, Pluronics® (P84, P85, P103, P105, P123 and F127) | Rifampicin and Isoniazid | - | M. tuberculosis |
|
2018 [118] |
| Amphiphilic poly (ethylene glycol)-poly(ε-caprolactone) copolymers conjugated with vancomycin. | Ciprofloxacin | 77 nm | P. aeruginosa |
|
2018 [119] |
| Fatty acid grafted chitosan conjugates nanomicelles | Ciprofloxacin | 260 nm |
P. aeroginosa
K. pneumoniae S. pneumoniae |
|
2018 [120] |
| Carboxy methyl chitosan hydrophobically modified with stearic acid and conjugated with urea | Clarithromycin | 200 nm | H. pylori |
|
2019 [121] |
| D-α-tocopherol polyethylene glycol 1000 succinate polymeric micelles | Baicalin | 14.05 ± 4.52 nm, | E. coli |
|
2019 [122] |
Polymeric Nanoparticles
Polymer-based nanosystems used against antibacterial resistance can be categorized into polymers that have themselves antibacterial properties and polymeric nanoparticles acting as antibiotic delivery systems [7]. Polymer nanoparticles are among the class of organic macromolecule-based antibacterial drug carriers that have many advantages such as ease of fabrication, physical and chemical stability in physiological environment and under storage conditions, easily controllable physicochemical properties, and prolonged drug release with better targeting efficiency [123].
Chitosan was proved to be the most efficient and versatile polymeric material from a natural source utilized for preparing antibacterial loaded drug carriers. The antibacterial activities of chitosan are dependent on numerous factors such as chitosan deacetylation degree and molecular weight, as well as the chemical structure and functionalization of chitosan molecules [124]. There are variable mechanisms that illustrate the antibacterial activity of chitosan, most commonly depending on the electrostatic attraction between chitosan and anionic surface of bacteria that lead to changing the permeability of cell membrane. Leaking out of the bacterial components results in cell death [125]. Examples of recent innovative studies done on antibiotic loaded chitosan nanoparticles are shown in Table 4.
Table 4.
Examples on recent studies on polymeric nanoparticles against bacterial infections.
| Type of Polymeric Nanoparticles | Drug | Size | Biofilm | Findings | Reference Year |
|---|---|---|---|---|---|
| Natural polymers | |||||
| Chitosan | Ciprofloxacin Chlortetracycline HCL. Gentamycin sulfate. |
S. aureus
E. coli |
|
2015 [131] | |
| pH-responsive chitosan coated iron oxide NPs | Ciprofloxacin | 30–80 nm | urinary tract and intestinal infections |
|
2016 [132] |
| Genipin cross-linked chitosan/heparin NPs | Ciprofloxacin | 250 nm | E. coli MTCC 443 |
|
2016 [133] |
| Chitosan/fucoidan NPs | Gentamicin | 270–300 nm | K. pneumoniae |
|
2016 [134] |
| pH-responsive chitosan nanoparticles with new anionic gemini surfactant (AGS) | Vancomycin | 220.57 ± 5.9 nm | MRSA |
|
2017 [135] |
| Chitosan nanoparticles and fucoidan coated chitosan NPs | Ciprofloxacin | Chitosan NPs: 124 ± 7 nm. Fucoidan coated chitosan CNPs: 320 ± 18 nm. |
Salmonella |
|
2017 [136] |
| Chitosan-Dextran sulphate NPs | Ciprofloxacin | 350 nm | Gm +ve and Gm -ve ophthalmic microorganisms. |
|
2017 [137] |
| Alginate lyase functionalized chitosan NPs | Ciprofloxacin | 205.5 ± 9.0 nm | P. aeruginosa |
|
2019 [138] |
| Synthetic polymers | |||||
| PLGA functionalized with DNase I | Ciprofloxacin | 251.9 nm | P. aeruginosa |
|
2015 [139] |
| PLGA | Amikacin | 447 ± 7 | P. aeruginosa |
|
2016 [140] |
| PLGA | Ciprofloxacin-SDS complex (ciprofloxacin complex loaded PLGA) | 190.4 ± 28.6 nm | P. aeruginosa |
|
2017 [141] |
| PLGA (poly(lactic-co-glycolic acid) | Gentamicin | 227 nm | K. pneumonia |
|
2018 [142] |
| PLGA and PEG-PLGA di-block NPs | Tobramycin | NPs: 225–231 nm MPs: 896–902 nm |
P. aeruginosa and Burkholderia cepacia complex (Bcc) |
|
2018 [143] |
| Polyethylenimine/diazeniumdiolate (PEI/NONOate)-doped PLGA nanoparticles | Nitric oxide (NO) | 240 ± 20 | MRSA |
|
2019 [144] |
| Alginate modified-PLGA nanoparticles | Amikacin and moxifloxacin | Alginate coated PLGA NPs: 640 ± 32 nm Alginate entrapped PLGA NPs: 312–365 nm |
M. tuberculosis (H37Ra) |
|
2019 [145] |
Other examples of natural polymers include dextran sulfate and chondroitin sulfate polysaccharides. Nanoparticles of either chondroitin sulfate or dextran sulfate were formulated with high encapsulation efficiency around 65% and size ranged from 100 to 200 nm. The results indicated that macrophages intracellular uptake of the antibiotic by using antibiotic-loaded dextran sulfate nanoparticles was 4-fold that of the antibiotic-loaded chondroitin sulfate nanoparticles. Further, enhanced anti-microbial activity against intracellular salmonella infections was confirmed [126].
The main merits of natural polymers are being highly biodegradable and biocompatible. On the other hand, aforementioned merits may be originated in synthetic polymers too, for example PLGA (poly (lactic-co-glycolic acid) or PCL) (poly (ε -caprolactone)). PLGA is a commonly used synthetic polymer. Recently, it has been utilized as basic excipient for antibacterial polymeric nanoparticles production [127]. Clarithromycin antibiotic was successfully encapsulated within PLGA particles. The enhanced antibacterial efficacy against H. pylori strains was evidenced from lower MIC values compared to free antibiotic. Although the mechanism remains unclear, it was postulated that PLGA-loaded nanoparticles could carry out either fusion or adsorption [128]. PCL can be utilized for producing good antimicrobial drug delivery nanosystems because of its biocompatibility and biodegradability [129]. For instance, a significant improvement of anti-tubercular rifampicin uptake into macrophages was observed after its encapsulation within PCL nanoparticles compared to free drug, thus improving its antibacterial efficiency towards M. tuberculosis infection [130]. Recent literature on the application of polymeric nanoparticles against bacterial infections is described in Table 4.
2.2.2. Inorganic Nanosystems
Silver NPs (Ag-NPs)
Nano-silver is known to possess a strong bactericidal activity against a variety of bacteria. The remarkable antibacterial action of Ag-NPs is a result of their well-expanded surface that provides the highest contact with the bacterial membrane leading to cellular leakage and cell growth inhibition. In addition to their binding affinity to macromolecules, their contact with the bacterial membrane lead to disintegration of the bacterial cells and death.
Several literatures reported the characteristic antibacterial activity of silver nanoparticles [146]. The activity of silver nanoparticles synthetized from the extract of Corchorus Capsularis leaf was evaluated against coagulase negative staphylococci, P. aeruginosa isolates of post-surgical wound infections, and S. aureus (Staphylococcus aureus) [147]. The results revealed that there was an inverse relationship between the concentration of silver nanoparticles and the number of bacterial cells. In addition, increasing time of bacterial exposure to Ag NPs resulted in lower survival of bacterial cells.
The extract of Trichodesmium erythraeum was utilized for preparing silver nanoparticles [148]. The diameter of prepared nanoparticles was 26.5 nm. The antibacterial findings displayed remarkable inhibition against S. aureus and Proteus mirabilis strains with minimum zone of inhibition 11 mm and 10 mm, respectively, and against antibiotic-resistant strains, for example S. pneumonia (PenicillinR) and S. aureus (TetracyclineR). Another synthesis technique for Ag-NPs by gamma irradiation was also reported by Swaroop et al. [149]. E. coli culture supernatant was also used for biosynthesis of silver nanoparticles. The fabricated particles exhibited a characteristic shape with mean size 33.6 nm. The formulated Ag NPs showed zone of inhibition of 13, 11, 10, and 10 mm, against K. pneumonia, P. aeruginosa, E. coli, and S. aureus, respectively.
Antibacterial activity of Ag-NPs was remarked against E. coli, K. pneumonae, and P. aeruginosa. These findings was also accompanied with decrease concentration of polysaccharides, lipids, proteins, and nucleic acids in biofilm compared with controls [150]. The antimicrobial action resulting from conjugating cationic peptides on the surface of either gold or silver nanoparticles was evaluated [151]. The findings indicated that silver nanoparticles surface decorated with cationic peptide revealed higher antimicrobial efficiency relative to peptide decorated gold nanoparticles as well as undecorated metallic nanoparticles and native peptides. Unfortunately, the use of silver and gold nanoparticles is limited on a large scale because of their high outlay of the production.
Silica Nanoparticles
Mesoporous silica nanoparticles have proven to be the answer in the management of diverse infections, as these nanoparticles have merits at all treatment phases, such as drug release, targeting biofilm, and adjuvant capacity [152]. Levofloxacin enclosed within nanoparticles of mesoporous silica capped with the lectin concanavalin A were formulated for the management of bone infections. The results interestingly showed that samples treated with bare silica nanoparticles presented a little activity towards biofilm. However, after treatment with levofloxacin-loaded silica nanoparticles, the biofilm reduction was more visible, due to the action of antibiotic.
The adsorption of certain biocidal on the surface of silica nanoparticles was evaluated by Jang et al. [153] who reported the fabrication of silica–poly(3-allyl-5,5-dimethylhydantoin-co-methyl methacrylate) (poly(ADMH-coMMA)) core–shell nanoparticles as a biocidal polymeric agent using a seeded polymerization. The produced mixtures (ADMH–MMA) were used to decorate the surface of silica nanoparticles, as a result of their hydrophobic properties, to produce cyclic N-halamines, which are utilized as antimicrobial agents. These N-halamine-decorated silica-nanoparticles showed excellent antibacterial action against both Gram-negative bacteria and Gram-positive bacteria, and their antibacterial actions have been efficiently enhanced compared with their bulk counterparts [154].
Magnetic Nanoparticles, MNPs
Magnetic nanoparticles have received widespread use in the field of biomedical and nanomedicine [155]. The antibacterial activity of MNPs are because of their damaging effect to the bacteria through interfering with the thiol group at the respiratory base of the bacteria [156].
The antibacterial efficacy of biosynthesized MNPs was tested against various drug resistant bacteria, such as E. coli, Shigella, P. aeruginosa, S. aureus, Salmonella typhi, and Pasteurella multocida. Agar-diffusion method confirmed the efficiency of magnetic nanoparticles to suppress the growth of S. aureus and E. coli in a concentration-dependent manner. Moreover, it displayed strong efficacy against all bacteria when compared with the standard drugs [157].
Magnetic nanocomposites were synthetized via sol-gel method. The sizes of the formed nanocomposites were in the range of ~71–91 nm. Antimicrobial activity of nanocomposites was studied against different bacterial and fungal pathogens. Minimum inhibitory concentration and the minimum bactericidal concentration values were observed within the range of 256–2048 µg/mL against E. coli and S. aureus. As expected, they could inhibit the growth of Gram-positive strain more effectively than Gram-negative strain. The existence of additional outer cell membrane renders Gram-negative bacteria more resistant to antimicrobial agents. Metal-ion release, reactive oxygen species generation, outer membrane and cell wall destruction, and particle internalization into microorganisms are the mechanisms of inhibitory action of metal oxide NPs on bacteria and fungi [158].
Zinc Oxide (ZnO) Nanoparticles
The U.S. Food and Drug administration has approved ZnO as a safe material. Many recent researches focus on ZnO, utilizing it as an antibacterial agent [159]. Antibacterial action of zinc oxide nanoparticles against various human pathogens was evaluated. The results revealed that zinc oxide nanoparticles displayed enhanced activity against S. aureus and low efficacy against Mycobacterium bovis-BCG (Bacillus Calmette–Guérin). The mechanism of ZnO-NPs as antibacterials relies on their ability to damage integrity of the cell membrane, diminish hydrophobicity of the cell surface, and down-regulate certain genes in bacteria. Moreover, ZnO-NPs treatment enhanced the intracellular bacterial damage by producing reactive oxygen species. Furthermore, ZnO-NPs prevents biofilm formation and hemolysis by hemolysin toxin that is produced by S. aureus [160].
It is worth to note that the antibacterial action of these metal oxide nanoparticles significantly relies upon their size. The size is important crucial factor because of entrance ease of small-size particles through pores of the bacterial cell surface. These pores in the bacterial cell surface are in nanometer size range. Additionally, ZnO nanoparticles exhibited an anticancer activity as compared with normal cells. Two mechanisms were predicted based on producing reactive oxygen species (ROS), toxicity of ZnO, and inducing apoptosis [161].
Cobalt NPs
Cobalt oxide NPs are receiving wide spread attention lately due to their structural, antibacterial, and biomedical activities [162]. Satpathy et al. [163] evaluated the antibacterial characteristics of cobalt NPs towards isolated E. coli strains. The results confirmed the dependency of antibacterial effect of cobalt nanoparticles on both particle size and cobalt concentration as reflected by the enhanced bactericidal effect of cobalt nanoparticles (35 µg/mL, 200 nm).
These results were contradictory to Khan et al. [164] who examined the anticancer and antibacterial action of cobalt oxide nanoparticles (Co3O4-NPs) on cancerous cells of colon and on bacteria, respectively. The results revealed that Co3O4-NPs displayed anti-cancerous characteristics. However, no antibacterial action was reported. Khalil et al. [165] also evaluated the antibacterial characteristics of Co3O4-NPs either illuminated or without UV illumination. It was found that on UV illumination, antibacterial characteristics of Co3O4-NPs were improved, confirming the antibacterial potential of cobalt oxide NPs against different bacterial strains.
Further, Dogra et al. [166] fabricated nanosuspensions of metallo surfactants-derived cobalt oxide and hydroxide via the microemulsion method. The results revealed that nanosuspension made up of (Bis hexa decyl trimethyl ammonium cobalt tetrachloride) surfactant has maximum antimicrobial activity against multiple-medicine-resistant S. aureus. Cell shrinkage, formation of holes, change of morphology, and cell wall rupturing was observed.
Selenium Nanoparticles (Se-NPs)
Selenium is one of the trace essential elements that recently attracted attention due to its antitumor actions, importance in the immune system, and effect on certain hormones such as thyroid hormones [167,168]. To evaluate the antibacterial activity of selenium, Yazhiniprabha and Vaseeharan evaluated the bacteriostatic and larvicidal efficacy of biosynthesized Se-NPs. The results displayed a significant larvicidal property against the fourth instar larvae of a dengue fever-causing vector Aedes aegypti and anti-bacterial activity against Gram-positive (Enterococcus faecalis and Streptococcus mutans) and Gram-negative (Shigella sonnei and P. aeruginosa) bacteria at 40 and 50 μg/mL. In vitro and in vivo toxicity assessment of nanoparticles showed low cytotoxicity against (RAW 264.7) macrophages and Artemia nauplii. Thus, selenium nanoparticles can be proposed as a biocompatible nano-biomedicine against bacterial infections [169].
Cadmium Nanoparticles (CdO-Nps)
Owing to the ionic nature, stability, biocompatibility, and monodispersity of cadmium nanoparticles (CdO-Nps), all these properties make them good candidates to be used for delivering antibacterial drugs [170]. Zahera et al. [171] synthesized a highly biocompatible, monodispersed, and stable glucose capped CdO-Nps utilizing a sol-gel technique and compared it with naked CdO-Nps. The lowest inhibitory concentrations of glucose-capped CdO-Nps and naked CdO-Nps were 6.42 and 16.29 μg/mL, respectively, against E. coli strain, and 7.5 μg/mL and 11.6 μg/mL, respectively, against S. aureus bacteria. Glucose capping imparted stability and monodispersity to CdO-Nps, in addition to improved biocompatibility and penetrability into the living cells.
Although nanosystems possess immense potential as antibacterial delivery agents, different strains of bacteria display various levels of susceptibilities to different nanosystems. Various formulation factors for example the fabrication technique, particle size, and nanosystems composition, should be optimized in order to get the desired results.
Advantages and Drawbacks of Inorganic Nanoparticles
Inorganic-based nanosystems composed of inorganic metals, among which are silver (Ag), Silica, magnetic metals, selenium (Se), cobalt, and zinc oxide (ZnO), have been demonstrated with pronounced antibacterial activities [160]. However, very limited information is available on the in-vivo antibacterial efficacy of metal oxide NPs, their ability to kill pathogenic strains, and mechanisms of action. In general, metal nanoparticles have some advantages, such as large surface area and multimodal applications. However, toxicity, instability, and storage are major drawbacks of inorganic nanosystems [27].
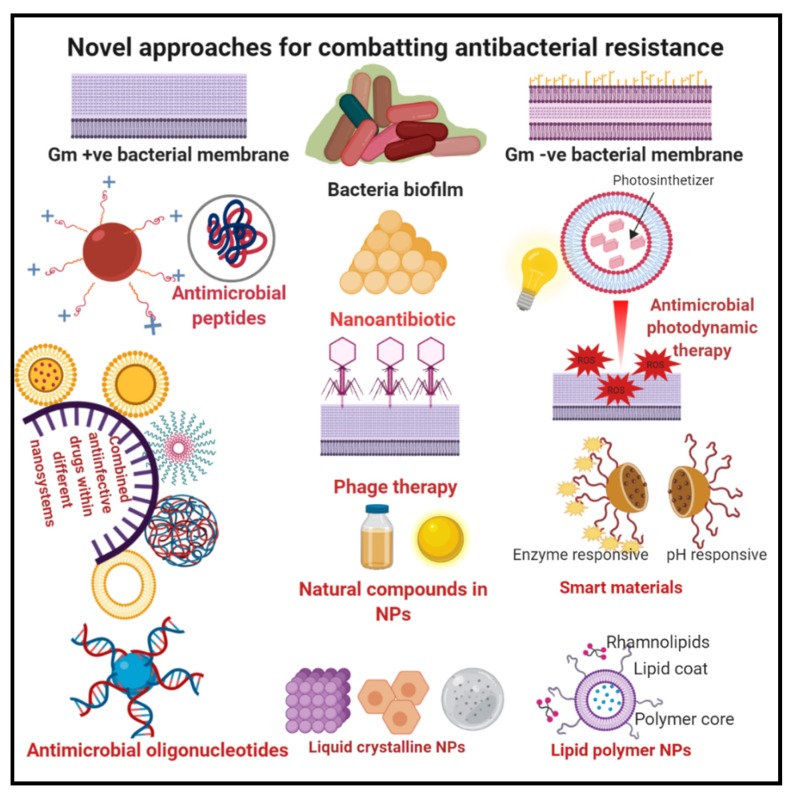
3. Novel Approaches for Combatting Antibacterial Resistance
In light of the abovementioned literature studies, we can conclude that there are many factors contributing to the biofilm resistance to antibiotics; consequently, the management based on only one parameter may not be enough for eradicating biofilm. An illustration of the recent novel approaches used to overcome antibacterial resistance, presented in Figure 2, will be discussed in the following section.
Figure 2.
Diagrammatic illustration of the novel approaches utilized for combating antibacterial resistance.
3.1. Lipid Polymer Nanoparticles (LPNs)
In view of the unique and complex features of biofilm, it was hypothesized that a technique that directly damages the extracellular matrix of biofilm and subsequently causes death of the bacteria could perform an amelioration in biofilm elimination. Disruption of the biofilm matrix leads to release of bacteria that regain their susceptibility to the action of antibiotics. In addition to this is the possibility to inhibit recurrence of infection because planktonic bacteria could not re-adhere to guest cells [172].
Following this principle, the conjugation of rhamnolipid, which is a biosurfactant fundamentally secreted by P. aeruginosa [173], to polymeric nanoparticles was proposed by Li et al. [174] to overcome Helicobacter pylori biofilm resistance. These novel particulate systems are composed of chitosan polymer as the core, encapsulating clarithromycin antibiotic, and the shell is made up of mixed lipids containing (1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[amino(polyethyleneglycol)-2000) DSPE-PEG2000-decoratedrhamnolipids. The fabricated particles have acceptable particle size ranging 148.5–165.2 nm and high clarithromycin encapsulation efficiency (>86%). The eradicating ability was observed to be remarkably enhanced as the lipoidal composition of rhamnolipid increased, which is represented by the considerable reduction of biofilm biomass and viability. These findings can be explained based on the disruptive power of rhamnolipid on biofilm matrix, the characteristic antibacterial properties of clarithromycin and chitosan NPs, the preventive actions of chitosan NPs and rhamnolipids on bacteria adhesion, and biofilm formation. Similarly, rhamnolipid-coated metallic nanoparticles (silver and iron oxide) were fabricated by Khalid et al. [175] and demonstrated excellent anti-biofilm efficacy against S. aureus and P. aeruginosa biofilms.
3.2. Nonlamellar Lyotropic Liquid Crystalline Nanoparticles
Various kinds of self-assembled nonlamellar liquid crystalline nanoparticles have been recently evaluated for their potential as drug delivery systems for antimicrobial molecules [176]. The system consists of amphiphiles that orient themselves into different mesophase structures, for example hexagonal, lamellar, cubic, and the less common sponge structure [177,178]. Advantages of these nanosystems include their amphiphilic nature and their larger interfacial surface areas, which enable them to encapsulate both hydrophilic and hydrophobic drugs, in addition to the ease of production with the ability to scale-up.
To test the antibacterial efficacy of this system, neutral and positively charged monoolein lipid nanoparticles encapsulating rifampicin were prepared by Tran et al. [179]. The results explained the highest potential of cationic nanoparticles reflected by significant reduction of the minimum concentration required to inhibit growth of S. aureus compared to the use of rifampicin alone, suggesting that the bacterial membrane with negative charges are firmly electrostatic and interacted with the lipids with positive charges.
3.3. Anti-Microbial Oligonucleotides
Use of oligonucleotide in antibacterial therapy, for example transcription factor decoys (TFD), is considered as a hopeful policy to overcome antimicrobial resistance. Transcription Factor Decoys (TFD) are short fragments of DNA that act on specific genome by capturing certain regulatory proteins to stop essential genes in the bacterial cells and overcome infection [180]. However, finding a suitable carrier that offer DNA encapsulation and protection against nucleases with efficient targeting to infection site is a challenge. Gonzalez-Paredes et al. [181] investigated the possibility of use of anionic solid lipid nanoparticles that were coated with either the cationic bola amphiphile 12-bis-tetrahydroacridinium or with protamine as a suitable carrier for TFD. Both compounds shifted zeta potential to positive values and demonstrated protective effect of TFD from deoxyribonuclease enzyme and, hence, a preferred accumulation of TFD in bacteria.
Furthermore, in an attempt to solve the challenges of preserving the colloidal stability and transfection efficiency of TFD, Mamusa et al. [182] designed phosphatidylcholine/phosphatidylethanolamine- cationic bolaamphiphile12-bis-THA scaffold to form TFD-loaded cationic liposomes. Although high entrapment efficiency of TFD (about 90%) was achieved with a maximum protection from serum nucleases, further studies towards a pre-clinical preparation against antimicrobial-resistant infections still need to be evaluated. Many authors also reported the possibility of conjugation of oligonucleotide antimicrobials with cationic materials such as peptides for penetrating cell (CPP). However, utilization of CPP is restricted to neutrally charged oligonucleotides, otherwise precipitation will occur [183]. Although these conjugates showed marked performance in an in vivo and in vitro bacterial patterns, the concentration used was relatively high, limiting their application due to cytotoxicity hazards [184].
Recently, strategy of oligonucleotide therapeutics was applied for acting on new therapeutic targets, for instance transcription, however due to undesirable physicochemical characteristics such as size, charge, and hydrophilicity that limit effective permeation across bacterial membranes to reach their target site, new strategies should be developed to solve the problem of efficient delivery of oligonucleotide therapeutics [185].
3.4. Combination of Nanotechnology and Natural Compounds
Inclusion of natural components in nanoparticles fabrication have recently been encouraged to change the carrier matrix and boost the antibiotics efficacy [186].
For instance, Rodenak-Kladniew et al. [187] examined the effect of incorporation of chitosan and eugenol, a natural phenolic compound, into a lipid matrix containing ofloxacin antibiotic by hot homogenization/ultrasonication technique. The results indicated that the developed formulation displayed an improved bactericidal action against P. aeruginosa and S. aureus significantly. Eugenol is known to induce nanostructuration of the matrix, enhance the particles stability, and conflict with bacterial growth, in addition to its high skin penetrability.
3.5. Smart Materials
Among the newly discovered nano antibiotic delivery platforms is the utilization of smart moieties, for example pH [188] and enzyme [189] responsive materials, for targeting bacterial infection tissues. pH-triggered antibiotic release achieves increasing importance nowadays. Designing polymers with pH-responsive materials, for example poly-l-histidine [190], comes with the possibility of pH triggered surface charge switching in acidic medium of the infected bacteria. This specific feature is utilized to maximize the attraction force to the bacterial cell wall having negative charge and hence release the antibacterial drug more precisely in the targeted site.
3.6. Cationic Peptides
One of the hopeful techniques to combat bacterial resistance is the inclusion of cationic peptides as an option to conventional antibiotics [191]. The unique features of cationic peptides include their amphiphilic nature and their cationic charge, which facilitate targeting of negatively charged bacterial membrane leading to escape of intracellular contents and death [192]. Further, due to the impossibility in restoration of the damaged cell structure, this efficient strategy minimizes the emergence of bacterial resistance.
3.7. Antimicrobial Photodynamic Therapy (aPDT)
Utilization of phototherapy for killing microbes is considered as a novel non-invasive treatment of choice to manage infectious diseases. The mechanism of photodynamic therapy depends on the local or systemic use of oxygen, combined with a photosensitizer (PS) and a visible light, producing reactive oxygen species (ROS) upon exposure. Oxygen species cause oxidative stress to ingredients of the bacterial cells such as membranes leading to complete biofilm elimination [193]. The unique advantage of this technique over other conventional ones is the dual selectivity behavior. The photosensitizer only accumulates in the rapidly growing bacterial cells and application of light leads to the photo-destructive effect limited to the area where the light is delivered, criteria that prevent the recurrence of infection [194]. Sanjana Ghosh et al. [195] investigated the loading of ciprofloxacin into photoactivatable liposomes that were made of porphyrin-phospholipid. The authors reported that about 90% of the antibiotic released in less than 30 s. Moreover, with or without laser treatment, ciprofloxacin photoactivatable liposomes inhibited the growth of Bacillus subtilis in liquid media, probably due to the enhanced uptake of liposomes by bacteria. These findings show the feasibility of photoactivatable liposomes to enhance localized antibiotic therapy.
Synergistic antibacterial effect was obtained by coating pullulan (PL)/pheophorbide-A (phA) conjugates (PL/phA) onto erythromycin-loaded liposomes. P. acnes skin infections characterized by secreting lipase enzyme that disrupt erythromycin-loaded liposomes led to the release of encapsulated drug and PhA conjugate. Laser irradiation onto the liberated PhA leads to the maximum P. acnes growth suppression and the curing of P. acnes-infected inflammation [196].
3.8. Nano Systems with Combination Drug Therapy
The gradual back off in mono-drug therapy, due to the resistant strain’s emergence, made the combination drug therapy a first-line option for better outcomes. The principle of combined drug therapy relies on the simultaneous use of multiple therapeutics called a “drug cocktail” to treat bacterial infections with the goal of achieving synergistic drug effects, combating resistance, minimizing side effects, and expanding antimicrobial spectrum [197,198]. Moreover, the co-encapsulation of the combined drugs within nano-systems will offer advances in managing resistant bacterial infections, however the practical application is still in preliminary stages [199]. Fabrication of liposomal formulation co-encapsulated with ciprofloxacin and colistin was done in order to treat P. aeruginosa-induced respiratory tract infections. The in vitro antibacterial findings displayed that the prepared co-loaded liposomes had better anti-P. aeruginosa efficacy than the monotherapies, in addition to improved retention time and prolonged release of the encapsulated drugs at the infection tissues on the lung. However, in vivo evaluations are required to assure the applicability of the system to treat multi resistant respiratory infections [200].
In line with this approach, co-encapsulation of aminoglycoside antibiotic (tobramycin) with macrolide antibiotic (clarithromycin) within proliposomes with the aim of synergistic management of respiratory infections caused by P. aeruginosa was investigated. High entrapment efficiencies of both hydrophobic clarithromycin (89%) and hydrophilic tobramycin (47%) were obtained. The results showed synergistic antimicrobial activity against in vitro P. aeruginosa biofilms compared to either drugs alone [201]. Moreover, the co-encapsulation of LL37 and serpin A1 in solid lipid nanoparticles showed synergistic effect towards E. coli and S. aureus. for treatment of wound infections, although the mechanism of synergism was unknown [202].
3.9. Nano-Antibiotic
Nano-antibiotic is a promising technique where the transformation of the therapeutic agents themselves into nano-sized assemblies can be done, thus considered as carrier-free drug delivery approach. This approach is of great interest due to the fact that it can modify the physical properties of antibiotics, increase their dissolution rate, improve drug bioavailability, reduce side effects, better contact with microorganism, improve interaction and penetration within bacterial membrane, thus perform better against antibiotic-resistant strains [203].
Morakul et al. [204] investigated the potential of clarithromycin nanocrystals towards Helicobacter pylori infections. The formed nanocrystals enhanced the bioavailability and availability of drug at the desired site of action as compared to the lyophilized coarse suspension and the clarithromycin powder. More recently, using hyperbranched polyesters themselves as a new form of nano-grade antibiotics alleviating the complications of antibiotic encapsulation and release was explored [205].
3.10. Phage Therapy
Phage therapy is considered as a safe and effective technique against resilient pathogens. However, up to date, none of the phage therapies have successfully extended its application to the consumers. The major drawbacks that hinder the application of this strategy include high specificity and poor pharmacokinetic properties [206].
In an attempt to overcome the narrow host range and rapid clearance drawbacks, Chadha et al. [207] has demonstrated the potential of phage cocktail loaded-liposomes rather than the monophage therapy and tested it against K. pneumoniae inducing burn wound infections. The findings of the study confirmed the better reduction of bacterial load in main organs and blood of the infected mice treated with liposomal entrapped phage cocktail as compared to non-liposomal free phage cocktail. Additionally, liposomal phage formulation was able to save all the examined animals from death even when there was a slowness of starting the therapy for 24 h. In spite of an increasing number of clinical trials confirming the activity and safety of phage therapy, there are still missing regulatory information that require to be handled before phage therapy can be applied broadly.
4. Clinical Trials
4.1. Current and Future Market of Nanosystem Antibiotics
After these extensive research efforts in developing innovative antibacterial delivery systems to resist the antibiotic resistance crisis, the good news is, there are number of nanosystem-based antibiotics, antitoxin agents, and antimicrobial peptides that have been recently translated to the clinic. However, many are still in different stages of clinical trials (Table 5 and Table 6).
Table 5.
Nanosystem-based antibiotics and anti-toxins in clinical trials different stages.
| Antibiotic | Clinical Trial | Medical Condition/Indication | Trial Phase | Intervention Treatment |
|---|---|---|---|---|
| Ciprofloxacin | Inhaled ciprofloxacin loaded-liposome: Once a day management of respiratory infections [54]. | P. aeruginosa | Phase 1 | Ciprofloxacin |
| Ciprofloxacin | Inhaled ciprofloxacin loaded-liposome: Once a day management of respiratory infections [54]. | P. aeruginosa | Phase 2a | Ciprofloxacin |
| Ciprofloxacin | Inhaled ciprofloxacin loaded-liposome in patients with non-cystic fibrosis bronchiectasis and chronic lung infection with Pseudomonas aeruginosa (ORBIT-3 and ORBIT-4): two phase 3, randomised controlled trials [208]. | Bronchiectasis and Chronic P. Aeruginosa Infection | Phase 3 | Inhaled Liposomal Ciprofloxacin |
| Ciprofloxacin | Phase 3 Study with Ciprofloxacin Dispersion for Inhalation in Non-Cystic Fibrosis Bronchiectasis (ORBIT-3) [209]. | Non-Cystic Fibrosis Bronchiectasis | Phase 3 | Ciprofloxacin dispersion for inhalation (Liquid mixture of liposomally encapsulated and un encapsulated ciprofloxacin) Placebo: Liquid formulation of empty liposomes. |
| Amikacin | Liposomal Amikacin for Inhalation (LAI) for Nontuberculous Mycobacteria [210]. | Mycobacterium Infections, Nontuberculous | Phase 2 | Liposomal amikacin for inhalation (LAI) Drug: placebo |
| Amikacin | Extension Study of Liposomal Amikacin for Inhalation in Cystic Fibrosis (CF) Patients with Chronic Pseudomonas Aeruginosa (Pa) Infection [213]. | Cystic Fibrosis Patients with Chronic Pseudomonas aeruginosa Infection | Phase 3 | Amikacin |
| Amikacin | Inhaled amikacin loaded-liposome for treating Mycobacterium Abscesses Lung Disease [212]. | Mycobacterium Infections, Nontuberculous Mycobacteria, Atypical |
Phase 2 | Liposomal amikacin for inhalation (LAI) plus multi-drug regimen |
| Amikacin | Study to Evaluate Efficacy of inhaled amikacin loaded-liposome combined with multi-drug regimen, Compared to Multi-drug Regimen Alone (CONVERT) [218]. | Mycobacterium Infections, Nontuberculous | Phase 3 | Liposomal Amikacin for Inhalation, 590 mg |
| Amikacin | Study of Dose Escalation of Liposomal Amikacin for Inhalation (ARIKAYCE™)-Extension Phase [211]. | Cystic Fibrosis | Phase 2 | Drug: Arikayce™ |
| Biological: CAL02 | CAL02; a liposomal adjunctive anti-toxin therapy in infections. A new therapeutic approach for severe community-acquired pneumonia [216]. | Severe community-acquired pneumonia | Phase 2 and 3 | CAL02 anti-toxin |
| Biological: GS-CDA1 Biological: MDX-1388 |
Study of the Clinical Effectiveness of a Human Monoclonal Antibody to C. Difficile Toxin A and Toxin B in Patients with Clostridium Difficile Associated Disease [219]. | Clostridium Difficile Associated Disease | Phase 2 | Biological: (GS-CDA1) Biological: MDX-1388 |
Table 6.
Nanosystem-based antimicrobial peptides in clinical trials different stages.
| Antimicrobial Peptides | Medical Condition/Indication | Clinical Trial Phase | Antimicrobial Peptides Source |
|---|---|---|---|
| Mutacin 1140 (MU1140) [220] | Gm +ve bacteria (MRSA, C. difficile (Clostridium difficile)) | Preclinical | Streptococcus mutans |
| lipohexapeptides 1345 (HB1345) [217] | Broad-spectrum antibiotic, acne | Preclinical | Lipopeptide |
| Novarifyn (NP432) [50] | MRSA, P. aeruginosa, C. difficile, A. baumannii, E. coli | Preclinical | Synthetic antimicrobial |
| Arenicin (AP139) [221] | Gm−ve bacteria, UTI | Preclinical | Lugworm Arenicol marina |
| Arenicin (AP138) [217] | MRSA implant infections | Preclinical | Arenicin analog |
| Arenicin (AP114) [217] | C. difficile | Preclinical | Arenicin analog |
| Avidocin and purocin [222] | Gm+ve and Gm−ve bacteria | Preclinical | Modified R-type bacteriocin |
| Novacta biosystems (NVB-302) [223] | C. difficile | Phase 1 | Lantibiotic |
| Human lactoferrin (hlf1-11) [224] | Infection following transplantation | Phase 1 and phase 2 | Lactoferricin analog |
| (a potent cyclic lipodepsipeptides antibiotic) Wap-8294A2 [225] | Gm+ve bacteria (VRE and MRSA) | Phase 1 and phase 2 | Lysobactor spp. |
| The specifically targeted antimicrobial peptide (C16G2) [226] | Prevention of tooth decay caused by Streptococcus mutans | Phase 2 | Synthetic peptide |
| Antimicrobial Peptide (DPK-060) [227] | Acute external otitis | Phase 2 | Human protein kininogen |
| LTX-109 (Lytixar) [228,229] | Nasal decolonization of MRSA Impetigo |
Phase 1 & 2 Phase 2 |
Synthetic peptidomimetic |
| p2TA (AB 103) [230] (A CD28 mimetic peptide) |
Necrotizing soft tissue infections | Phase 3 | Synthetic peptide |
| Surotomycin [231] | C. difficile (diarrhea) | Phase 3 | Cyclic lipopeptide |
| Ramoplanin (NTI-851) [232] | C. difficile | Phase 2 | Actinoplanes spp |
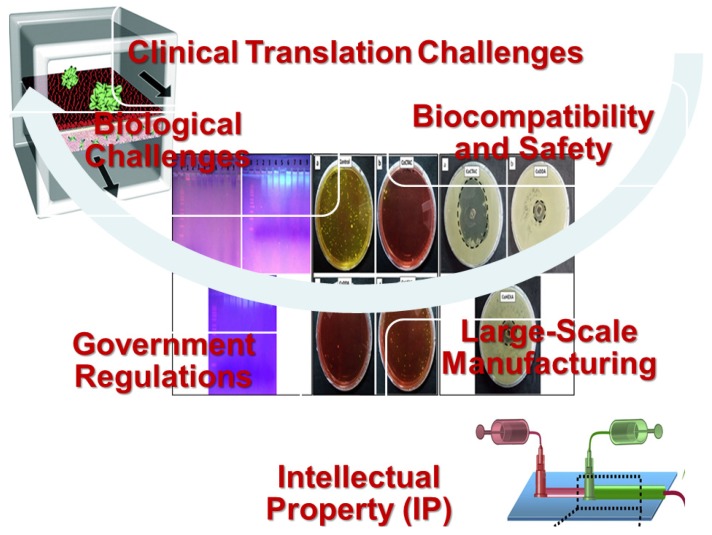
4.1.1. Antibiotic Agents
The first clinical application of inhaled ciprofloxacin-loaded liposome using Lipoquin was a phase 1 trial in certain healthy volunteers [54], as shown in Table 5. Then to evaluate activity, initial safety, and pharmacokinetics of once-daily inhaled ciprofloxacin-loaded liposome (Lipoquin), a Phase 2a multi-center 14-day trial was conducted in 21 adult CF patients. Concurrently, an international, double-blind, randomized, phase 3 trials (ORBIT-3 and ORBIT-4) were run in similar regions to investigate the safety and efficacy of inhaled liposomal ciprofloxacin [208,209]. Moreover, amikacin-loaded liposomes were evaluated in many clinical studies. In a double-blind, phase 2, randomized study, efficacy, safety, and tolerability of once daily dosing of amikacin 590 mg versus placebo for 84 days were explored in subjects with treatment refractory Nontuberculous Mycobacteria lung infection on a stable multidrug regimen [210]. Another study (phase 2) investigated the long-term efficacy, safety and tolerability of once daily 560 mg dose of inhaled amikacin-loaded liposome, administered for six cycles over 18 months, in cystic fibrosis patients with chronic infections caused by Pseudomonas Aeruginosa [211].
A new study of phase 2 trial will assess the efficacy, safety, and tolerability of inhalation liposomal amikacin, once daily dosing for 12 months of 590 mg plus standard-of-care mycobacterial multi-drug regimen, for treatment of mycobacterium abscesses lung disease [212]. In a phase 3 clinical trial, cystic fibrosis patients with chronic infection due to Pseudomonas aeruginosa were included in the study and the long-term tolerability and safety of inhaled amikacin-loaded liposome (590 mg/day) was studied [213]. Various nanosystem-based antibiotics and anti-toxins in clinical trials different stages were listed in Table 5.
4.1.2. Anti-Toxin Agents
New nano-preparation targeting bacterial components responsible for virulence effect of bacteria, such as toxins, may be a promising challenge in the area of antibacterial medications. Bezlotoxumab was the first antitoxin, approved in 2016, as a human monoclonal antibody targeting toxin B of Clostridium difficile [214]. A certain number of anti-toxin agents such as monoclonal antibodies targeting S. aureus’ α-toxin are in the clinical development, in addition to monoclonal antibodies that target type III toxins secretion moiety of P. aeruginosa [215]. A broad-spectrum antitoxin liposomal agent (novel empty liposomes is also in clinical development; CAL02) has resulted in synergistic actions with drugs or antibiotic and also proved the ability to redeem mice from serious infections, for example staphylococci by adsorbing toxins [216].
4.1.3. Antimicrobial Peptides
Antimicrobial peptides exhibit broad-spectrum antibacterial activity with relatively low risk of resistance development due to the rapid onset of killing [217]. The principle target of antimicrobial peptides is the cell membrane of bacteria. Other intracellular targets have been reported including synthesis of cell wall (nisin), synthesis of nucleic acid, synthesis of RNA (e.g., buforin II), enzymatic activity (pyrrhocoricin), protein synthesis (indolicidin), or ATP (Adenosine triphosphate) efflux (histatins) [217]. Many antimicrobial peptides currently undergoing preclinical and clinical trials are listed in Table 6.
5. Challenges in the Clinical Translation of Nanomedicine
Clinical translation of nanomedicine has difficulties, such as being time consuming and expensive. The main challenges related to the clinical translation are biological issues, safety, biocompatibility, intellectual property (IP), laws and regulations, and overall cost-effectiveness compared to traditional therapies [233], (Figure 3). These obstacles limit the usage of nanoparticles in the present markets regardless of their effectiveness [234]. Many issues should be considered during the clinical translation of nanomedicine. The first one is the nanopharmaceutical design that can be enumerated as follows; physical and chemical stability, biodegradability, sophisticated formulation design, and administration route. Efforts should be utilized for resolving obstacles of large-scale production, such as reproducibility and high cost, and also obstacles of quality control assays for characterization such as polydispersity, scalability complexities, incomplete purification from contaminants, consistency and storage stability of the final product, morphology, and charge [235,236]. Preparation techniques are required to consistently produce large scalable quantities of nanoparticulates with high degree of quality and batch-to-batch reproducibility.
Figure 3.
Graphical representation of the challenges in the clinical translation of nanomedicine.
The second issue is preclinical evaluation, such as the need for early detection of the toxicity, in vivo evaluation in appropriate animals, and understanding both pharmacokinetics and pharmacodynamics. Therefore, more advanced toxicological evaluations for nanomedicine should be developed. Moreover, stability of nanoparticulates following administration and interaction of nanoparticulates with tissues should be well understood. The third issue concerns clinical examination for commercialization. Pathways from invention to the markets are complicated, so they should be minimized to save the time and the cost. Additionally, safety/toxicity in humans and therapeutic efficacy in patients should be evaluated using more simple techniques. Specialized toxicology evaluations in animals should be carried out to examine both short-term and long-term toxicity, as biological half-lives are significantly raised with nanoencapsulation.
Clear regulatory guidelines specific for nanoparticulates should be developed for sensitive, validated, and standardizable examinations incorporating protocols to appropriately evaluate the nanotoxicology of nanoparticulates during the early steps of clinical development [237]. Because nanoparticulates represent various types of nanostructures, there are challenges in developing regulatory protocols, techniques, and tools for ensuring standardized good manufacturing practice (GMP) production and characterization, safety, and economic design of clinical trial. Nanoparticulates patents and intellectual properties (IP) are complex and simplification of them is needed to simplify the pathway from invention to commercialization to reduce the time and expense required for negotiating collaboration and licensing agreements [238].
6. Recommendations and Perspectives
As noted, it becomes clear that translation of antibacterial-loaded nanosystems to the clinic is still beyond reach for most approaches, so more research efforts became imperative to solve the massive challenge of antibiotic resistance. The author recommendation is that, presently, the community now has another task, which is to “do more efforts for clinical translation of nanoparticulates and takes their advantages in a more comprehensive way’’. Successful clinical translation firmly demands an interdisciplinary strategy to develop creative protocols, examinations, and infrastructure for large-scale manufacturing of nanoparticulates. Therefore, we invite all academic and pharmaceutical industry experts with specialty in medicine, biology, pharmaceutics, toxicology, and engineering to undertake more efforts to overcome these challenges.
Prospective techniques to fast-track favorable nanoparticulates to clinical applications encompass the coordination of faculties, pharmaceutical factories, and laboratories that have excellent expertise in evaluating nanoparticulates platforms, performing preclinical studies, and designing and carrying out clinical trials of nanoparticulate platforms [239].
7. Concluding Remarks
As defeating bacterial resistance growth is very costly and time consuming, due to high cost of the process of production of new safe and effective antibiotic drugs, new policies for controlling infections became requisite. The recent strategies displayed in this manuscript were based on using nanosystems to surmount antibiotic resistance. In summary, nanosystems are classified based on their matrix composition into organic nanosystems (liposomes, lipid-based nanoparticles, polymeric micelles, and polymeric nanoparticles) and inorganic nanosystems (silver, silica, magnetic, ZnO, cobalt, selenium, and cadmium). The antibacterial activities of either free nanosystems or their synergistic effects when loaded with conventional antibiotic molecules were reported. The physicochemical properties of these nanosystems, for example zeta potential, particle diameter, and solubility, are the important parameters in their employment as antibacterial drug delivery systems. As explained in this context, various mechanisms by which nanosystems were able to overcome antimicrobial resistance were listed, as follows; offer high entrapment efficiency of either hydrophilic or lipophilic drugs, protection of entrapped antibacterial drugs from bacterial enzymatic inactivation, the potential of nanosystems to target the site of infection, increased uptake or decreased efflux, and physical damage of the cell membrane, thus inhibiting re infection.
As reported in the literature, the results of using antibacterial loaded nanosystems against biofilm infections revealed a significant reduction in MIC values compared to their corresponding free unloaded drugs, which have great benefits of delaying or inhibiting the resistance development. More importantly, the review article reported the recently explored innovations used against resilient bacteria. The new approaches were based on the use of lipid polymer nanoparticles, nonlamellar liquid crystalline nanoparticles, oligonucleotides, natural compounds combination, smart materials, cationic peptides, antimicrobial photodynamic therapy, combined antibiotics therapy, nano-antibiotics and phage therapy. However, despite the extensive research done and the promising results of using nanosystems as drug delivery agents in the therapeutic management of infections, very limited formulations have been proposed for clinical trials. Thus, we recommend further steps to be taken in the way of putting such nanosystems formulations on the market.
Author Contributions
N.E.E. conceived the concept of the review article, and prepared the content outline. N.E.E., A.A., S.B.H., and M.M.O. contributed to the review writing for different sections. N.E.E. and M.M.O. supervised the writing and final revision of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Willyard C. The drug-resistant bacteria that pose the greatest health threats. Nature. 2017;543:15. doi: 10.1038/nature.2017.21550. [DOI] [PubMed] [Google Scholar]
- 2.Kourtis A.P., Hatfield K., Baggs J., Mu Y., See I., Epson E., Nadle J., Kainer M.A., Dumyati G., Petit S. Vital Signs: Epidemiology and Recent Trends in Methicillin-Resistant and in Methicillin-Susceptible Staphylococcus aureus Bloodstream Infections—United States. Morb. Mortal. Wkly. Rep. 2019;68:214. doi: 10.15585/mmwr.mm6809e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Livorsi D.J., Chorazy M.L., Schweizer M.L., Balkenende E.C., Blevins A.E., Nair R., Samore M.H., Nelson R.E., Khader K., Perencevich E.N. A systematic review of the epidemiology of carbapenem-resistant Enterobacteriaceae in the United States. Antimicrob. Resist. Infect. Control. 2018;7:55. doi: 10.1186/s13756-018-0346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li B., Webster T.J. Bacteria antibiotic resistance: New challenges and opportunities for implant-associated orthopedic infections. J. Orthop. Res. 2018;36:22–32. doi: 10.1002/jor.23656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blair J.M., Webber M.A., Baylay A.J., Ogbolu D.O., Piddock L.J. Molecular mechanisms of antibiotic resistance. Nat. Rev. Microbiol. 2015;13:42–51. doi: 10.1038/nrmicro3380. [DOI] [PubMed] [Google Scholar]
- 6.Aslam B., Wang W., Arshad M.I., Khurshid M., Muzammil S., Rasool M.H., Nisar M.A., Alvi R.F., Aslam M.A., Usman Q.M. Antibiotic resistance: A rundown of a global crisis. Infect. Drug Resist. 2018;11:1645. doi: 10.2147/IDR.S173867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parisi O.I., Scrivano L., Sinicropi M.S., Puoci F. Polymeric nanoparticle constructs as devices for antibacterial therapy. Curr. Opin. Pharmacol. 2017;36:72–77. doi: 10.1016/j.coph.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Berlanga M., Guerrero R. Living together in biofilms: The microbial cell factory and its biotechnological implications. Microb. Cell Factories. 2016;15:165. doi: 10.1186/s12934-016-0569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rizzato C., Torres J., Kasamatsu E., Camorlinga M., Bravo M.M., Canzian F., Kato I. Potential role of biofilm formation in the development of digestive tract cancer with special reference to Helicobacter pylori infection. Front. Microbiol. 2019;10:846. doi: 10.3389/fmicb.2019.00846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Majumdar S., Pal S. Bacterial intelligence: Imitation games, time-sharing, and long-range quantum coherence. J. Cell Commun. Signal. 2017;11:281–284. doi: 10.1007/s12079-017-0394-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blair K.M., Turner L., Winkelman J.T., Berg H.C., Kearns D.B. A molecular clutch disables flagella in the Bacillus subtilis biofilm. Science. 2008;320:1636–1638. doi: 10.1126/science.1157877. [DOI] [PubMed] [Google Scholar]
- 12.Rossi-Fedele G., Roberts A. A preliminary study investigating the survival of tetracycline resistant Enterococcus faecalis after root canal irrigation with high concentrations of tetracycline. Int. Endod. J. 2007;40:772–777. doi: 10.1111/j.1365-2591.2007.01285.x. [DOI] [PubMed] [Google Scholar]
- 13.Valappil S.P. Drug Delivery Nanosystems for Biomedical Applications. Elsevier; Amsterdam, The Netherlands: 2018. Nanosystems and antibacterial applications; pp. 75–90. [Google Scholar]
- 14.Marsich E., Travan A., Donati I., Turco G., Bellomo F., Paoletti S. Antimicrobial Polymers. John Wiley & Sons, Inc.; Hoboken, NJ, USA: 2012. Tissue-implant antimicrobial interfaces; pp. 379–428. [Google Scholar]
- 15.Zhang L., Mah T.-F. Involvement of a novel efflux system in biofilm-specific resistance to antibiotics. J. Bacteriol. 2008;190:4447–4452. doi: 10.1128/JB.01655-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewis K. Persister cells and the riddle of biofilm survival. Biochemistry. 2005;70:267–274. doi: 10.1007/s10541-005-0111-6. [DOI] [PubMed] [Google Scholar]
- 17.Ling L.L., Schneider T., Peoples A.J., Spoering A.L., Engels I., Conlon B.P., Mueller A., Schäberle T.F., Hughes D.E., Epstein S. A new antibiotic kills pathogens without detectable resistance. Nature. 2015;517:455. doi: 10.1038/nature14098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patra J.K., Das G., Fraceto L.F., Campos E.V.R., del Pilar Rodriguez-Torres M., Acosta-Torres L.S., Diaz-Torres L.A., Grillo R., Swamy M.K., Sharma S. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018;16:71. doi: 10.1186/s12951-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lombardo D., Kiselev M.A., Caccamo M.T. Smart nanoparticles for drug delivery application: Development of versatile nanocarrier platforms in biotechnology and nanomedicine. J. Nanomater. 2019;2019:3702518. doi: 10.1155/2019/3702518. [DOI] [Google Scholar]
- 20.Abed N., Couvreur P. Nanocarriers for antibiotics: A promising solution to treat intracellular bacterial infections. Int. J. Antimicrob. Agents. 2014;43:485–496. doi: 10.1016/j.ijantimicag.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 21.Dacoba T.G., Olivera A., Torres D., Crecente-Campo J., Alonso M.J. Seminars in Immunology. Elsevier; Amsterdam, The Netherlands: 2017. Modulating the immune system through nanotechnology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gustafson H.H., Holt-Casper D., Grainger D.W., Ghandehari H. Nanoparticle uptake: The phagocyte problem. Nano Today. 2015;10:487–510. doi: 10.1016/j.nantod.2015.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vallet-Regí M., González B., Izquierdo-Barba I. Nanomaterials as Promising Alternative in the Infection Treatment. Int. J. Mol. Sci. 2019;20:3806. doi: 10.3390/ijms20153806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baptista P.V., McCusker M.P., Carvalho A., Ferreira D.A., Mohan N.M., Martins M., Fernandes A.R. Nano-strategies to fight multidrug resistant bacteria—“A Battle of the Titans”. Front. Microbiol. 2018;9:1441. doi: 10.3389/fmicb.2018.01441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baranwal A., Srivastava A., Kumar P., Bajpai V.K., Maurya P.K., Chandra P. Prospects of nanostructure materials and their composites as antimicrobial agents. Front. Microbiol. 2018;9:422. doi: 10.3389/fmicb.2018.00422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ashik U.P.M., Kudo S., Hayashi J.-I. Chapter 2—An Overview of Metal Oxide Nanostructures. In: Mohan Bhagyaraj S., Oluwafemi O.S., Kalarikkal N., Thomas S., editors. Synthesis of Inorganic Nanomaterials. Woodhead Publishing; Sawston, UK: 2018. pp. 19–57. [Google Scholar]
- 27.Martin-Serrano Á., Gómez R., Ortega P., de la Mata F.J. Nanosystems as vehicles for the delivery of antimicrobial peptides (AMPs) Pharmaceutics. 2019;11:448. doi: 10.3390/pharmaceutics11090448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Drulis-Kawa Z., Dorotkiewicz-Jach A. Liposomes as delivery systems for antibiotics. Int. J. Pharm. 2010;387:187–198. doi: 10.1016/j.ijpharm.2009.11.033. [DOI] [PubMed] [Google Scholar]
- 29.Omar M.M., Hasan O.A., El Sisi A.M. Preparation and optimization of lidocaine transferosomal gel containing permeation enhancers: A promising approach for enhancement of skin permeation. Int. J. Nanomed. 2019;14:1551–1562. doi: 10.2147/IJN.S201356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Omar M.M., Eleraky N.E., El Sisi A.M., Hasan O.A. Development and Evaluation of in-situ Nasal Gel Formulations of Nanosized Transferosomal Sumatriptan: Design, Optimization, in vitro and in vivo Evaluation. Drug Des. Dev. Ther. 2019;13:4413–4430. doi: 10.2147/DDDT.S235004. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Rukavina Z., Vanić Ž. Current trends in development of liposomes for targeting bacterial biofilms. Pharmaceutics. 2016;8:18. doi: 10.3390/pharmaceutics8020018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sharma A., Sharma U.S. Liposomes in drug delivery: Progress and limitations. Int. J. Pharm. 1997;154:123–140. doi: 10.1016/S0378-5173(97)00135-X. [DOI] [Google Scholar]
- 33.Alavi M., Karimi N., Safaei M. Application of various types of liposomes in drug delivery systems. Adv. Pharm. Bull. 2017;7:3. doi: 10.15171/apb.2017.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Atbiaw N., Aman E., Dessalegn B. Review on targeted drug delivery against intracellular pathogen. Pharm. Pharmacol. Int. J. 2018;6:183–189. doi: 10.15406/ppij.2018.06.00174. [DOI] [Google Scholar]
- 35.Rukavina Z., Klarić M.Š., Filipović-Grčić J., Lovrić J., Vanić Ž. Azithromycin-loaded liposomes for enhanced topical treatment of methicillin-resistant staphyloccocus aureus (mrsa) infections. Int. J. Pharm. 2018;553:109–119. doi: 10.1016/j.ijpharm.2018.10.024. [DOI] [PubMed] [Google Scholar]
- 36.Vanić Ž., Rukavina Z., Manner S., Fallarero A., Uzelac L., Kralj M., Klarić D.A., Bogdanov A., Raffai T., Virok D.P. Azithromycin-liposomes as a novel approach for localized therapy of cervicovaginal bacterial infections. Int. J. Nanomed. 2019;14:5957. doi: 10.2147/IJN.S211691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Castoldi A., Herr C., Niederstraßer J., Labouta H.I., Melero A., Gordon S., Schneider-Daum N., Bals R., Lehr C.M. Calcifediol-loaded liposomes for local treatment of pulmonary bacterial infections. Eur. J. Pharm. Biopharm. 2017;118:62–67. doi: 10.1016/j.ejpb.2016.11.026. [DOI] [PubMed] [Google Scholar]
- 38.Lai S., Wei Y., Wu Q., Zhou K., Liu T., Zhang Y., Jiang N., Xiao W., Chen J., Liu Q. Liposomes for effective drug delivery to the ocular posterior chamber. J. Nanobiotechnol. 2019;17:64. doi: 10.1186/s12951-019-0498-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yadav D., Sandeep K., Pandey D., Dutta R. Liposomes for drug delivery. J. Biotechnol. Biomater. 2017;7:276. doi: 10.4172/2155-952X.1000276. [DOI] [Google Scholar]
- 40.Abed N., Saïd-Hassane F., Zouhiri F., Mougin J., Nicolas V., Desmaële D., Gref R., Couvreur P. An efficient system for intracellular delivery of beta-lactam antibiotics to overcome bacterial resistance. Sci. Rep. 2015;5:13500. doi: 10.1038/srep13500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Uhl P., Pantze S., Storck P., Parmentier J., Witzigmann D., Hofhaus G., Huwyler J., Mier W., Fricker G. Oral delivery of vancomycin by tetraether lipid liposomes. Eur. J. Pharm. Sci. 2017;108:111–118. doi: 10.1016/j.ejps.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 42.Alshamsan A., Aleanizy F.S., Badran M., Alqahtani F.Y., Alfassam H., Almalik A., Alosaimy S. Exploring anti-MRSA activity of chitosan-coated liposomal dicloxacillin. J. Microbiol. Methods. 2019;156:23–28. doi: 10.1016/j.mimet.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 43.Wang W., Shao A., Feng S., Ding M., Luo G. Physicochemical characterization and gastrointestinal adhesion of S-layer proteins-coating liposomes. Int. J. Pharm. 2017;529:227–237. doi: 10.1016/j.ijpharm.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 44.Wijetunge S.S., Wen J., Yeh C.-K., Sun Y. Wheat germ agglutinin liposomes with surface grafted cyclodextrins as bioadhesive dual-drug delivery nanocarriers to treat oral cells. Colloids Surf. B Biointerfaces. 2020;185:110572. doi: 10.1016/j.colsurfb.2019.110572. [DOI] [PubMed] [Google Scholar]
- 45.Alhariri M., Majrashi M.A., Bahkali A.H., Almajed F.S., Azghani A.O., Khiyami M.A., Alyamani E.J., Aljohani S.M., Halwani M.A. Efficacy of neutral and negatively charged liposome-loaded gentamicin on planktonic bacteria and biofilm communities. Int. J. Nanomed. 2017;12:6949–6961. doi: 10.2147/IJN.S141709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Niu N.-K., Yin J.-J., Yang Y.-X., Wang Z.-L., Zhou Z.-W., He Z.-X., Chen X.W., Zhang X., Wei D., Yang T. Novel targeting of PEGylated liposomes for codelivery of TGF-β1 siRNA and four antitubercular drugs to human macrophages for the treatment of mycobacterial infection: A quantitative proteomic study. Drug Des. Dev. Ther. 2015;9:4441. doi: 10.2147/DDDT.S79369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bilton D., Pressler T., Fajac I., Clancy J.P., Sands D., Minic P., Cipolli M., Galeva I., Sole A., Quittner A.L. Amikacin liposome inhalation suspension for chronic Pseudomonas aeruginosa infection in cystic fibrosis. J. Cyst. Fibros. 2019 doi: 10.1016/j.jcf.2019.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ulrich A.S. Biophysical aspects of using liposomes as delivery vehicles. Biosci. Rep. 2002;22:129–150. doi: 10.1023/A:1020178304031. [DOI] [PubMed] [Google Scholar]
- 49.Alhajlan M., Alhariri M., Omri A. Efficacy and safety of liposomal clarithromycin and its effect on Pseudomonas aeruginosa virulence factors. Antimicrob. Agents Chemother. 2013;57:2694–2704. doi: 10.1128/AAC.00235-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moyá M.L., López-López M., Lebrón J.A., Ostos F.J., Pérez D., Camacho V., Beck I., Merino-Bohórquez V., Camean M., Madinabeitia N. Preparation and Characterization of New Liposomes. Bactericidal Activity of Cefepime Encapsulated into Cationic Liposomes. Pharmaceutics. 2019;11:69. doi: 10.3390/pharmaceutics11020069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Toh M.-R., Chiu G.N. Liposomes as sterile preparations and limitations of sterilisation techniques in liposomal manufacturing. Asian J. Pharm. Sci. 2013;8:88–95. doi: 10.1016/j.ajps.2013.07.011. [DOI] [Google Scholar]
- 52.Nkanga C.I., Bapolisi A.M., Okafor N.I., Krause R.W.M. Liposomes-Advances and Perspectives. IntechOpen; London, UK: 2019. General Perception of Liposomes: Formation, Manufacturing and Applications. [Google Scholar]
- 53.Clancy J., Dupont L., Konstan M., Billings J., Fustik S., Goss C., Lymp J., Minic P., Quittner A.L., Rubenstein R.C. Phase II studies of nebulised Arikace in CF patients with Pseudomonas aeruginosa infection. Thorax. 2013;68:818–825. doi: 10.1136/thoraxjnl-2012-202230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bruinenberg P., Blanchard J.D., Cipolla D.C., Dayton F., Mudumba S., Gonda I. Respiratory Drug Delivery. Davis Healthcare International Publishing River Grove; Orlando, FL, USA: 2010. Inhaled liposomal ciprofloxacin: Once a day management of respiratory infections. [Google Scholar]
- 55.Pignatello R., Nicolosi D., Nicolosi V.M. Science against Microbial Pathogens: Communicating Current Research and Technological Advances. Formatex Research Center; Badajoz, Spain: 2011. Fusogenic liposomes as new carriers to enlarge the spectrum of action of antibiotic drugs against Gram-negative bacteria; pp. 52–56. [Google Scholar]
- 56.Beaulac C., Sachetelli S., Lagace J. In vitro bactericidal efficacy of sub-MIC concentrations of liposome-encapsulated antibiotic against gram-negative and gram-positive bacteria. J. Antimicrob. Chemother. 1998;41:35–41. doi: 10.1093/jac/41.1.35. [DOI] [PubMed] [Google Scholar]
- 57.Beaulac C., Sachetelli S., Lagacé J. Aerosolization of low phase transition temperature liposomal tobramycin as a dry powder in an animal model of chronic pulmonary infection caused by Pseudomonas aeruginosa. J. Drug Target. 1999;7:33–41. doi: 10.3109/10611869909085490. [DOI] [PubMed] [Google Scholar]
- 58.Zhao Wang Y.M., Khalil H., Wang R., Lu T., Zhao W., Zhang Y., Chen J., Chen T. Fusion between fluid liposomes and intact bacteria: Study of driving parameters and in vitro bactericidal efficacy. Int. J. Nanomed. 2016;11:4025. doi: 10.2147/IJN.S55807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ishida T., Ichikawa T., Ichihara M., Sadzuka Y., Kiwada H. Effect of the physicochemical properties of initially injected liposomes on the clearance of subsequently injected PEGylated liposomes in mice. J. Control. Release. 2004;95:403–412. doi: 10.1016/j.jconrel.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 60.Ahmed K., Muiruri P.W., Jones G.H., Scott M.J., Jones M.N. The effect of grafted poly (ethylene glycol) on the electrophoretic properties of phospholipid liposomes and their adsorption to bacterial biofilms. Colloids Surf. A Physicochem. Eng. Asp. 2001;194:287–296. doi: 10.1016/S0927-7757(01)00817-2. [DOI] [Google Scholar]
- 61.Moghadas-Sharif N., Fazly Bazzaz B.S., Khameneh B., Malaekeh-Nikouei B. The effect of nanoliposomal formulations on Staphylococcus epidermidis biofilm. Drug Dev. Ind. Pharm. 2015;41:445–450. doi: 10.3109/03639045.2013.877483. [DOI] [PubMed] [Google Scholar]
- 62.Kaszuba M., Jones M.N. Hydrogen peroxide production from reactive liposomes encapsulating enzymes. Biochimica Et Biophysica Acta (BBA) Biomembr. 1999;1419:221–228. doi: 10.1016/S0005-2736(99)00070-X. [DOI] [PubMed] [Google Scholar]
- 63.Bai J., Yang E., Chang P.-S., Ryu S. Preparation and characterization of endolysin-containing liposomes and evaluation of their antimicrobial activities against gram-negative bacteria. Enzym. Microb. Technol. 2019;128:40–48. doi: 10.1016/j.enzmictec.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 64.Hill K.J., Kaszuba M., Creeth J.E., Jones M.N. Reactive liposomes encapsulating a glucose oxidase-peroxidase system with antibacterial activity. Biochimica Et Biophysica Acta (BBA) Biomembr. 1997;1326:37–46. doi: 10.1016/S0005-2736(97)00007-2. [DOI] [PubMed] [Google Scholar]
- 65.Jones M.N., Hill K.J., Kaszuba M., Creeth J.E. Antibacterial reactive liposomes encapsulating coupled enzyme systems. Int. J. Pharm. 1998;162:107–117. doi: 10.1016/S0378-5173(97)00418-3. [DOI] [Google Scholar]
- 66.Goss C.H., Kaneko Y., Khuu L., Anderson G.D., Ravishankar S., Aitken M.L., Lechtzin N., Zhou G., Czyz D.M., McLean K. Gallium disrupts bacterial iron metabolism and has therapeutic effects in mice and humans with lung infections. Sci. Transl. Med. 2018;10:eaat7520. doi: 10.1126/scitranslmed.aat7520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Alipour M., Suntres Z.E., Lafrenie R.M., Omri A. Attenuation of Pseudomonas aeruginosa virulence factors and biofilms by co-encapsulation of bismuth–ethanedithiol with tobramycin in liposomes. J. Antimicrob. Chemother. 2010;65:684–693. doi: 10.1093/jac/dkq036. [DOI] [PubMed] [Google Scholar]
- 68.Halwani M., Yebio B., Suntres Z., Alipour M., Azghani A., Omri A. Co-encapsulation of gallium with gentamicin in liposomes enhances antimicrobial activity of gentamicin against Pseudomonas aeruginosa. J. Antimicrob. Chemother. 2008;62:1291–1297. doi: 10.1093/jac/dkn422. [DOI] [PubMed] [Google Scholar]
- 69.Alhariri M., Omri A. Efficacy of liposomal bismuth-ethanedithiol-loaded tobramycin after intratracheal administration in rats with pulmonary Pseudomonas aeruginosa infection. Antimicrob. Agents Chemother. 2013;57:569–578. doi: 10.1128/AAC.01634-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mokhtar M., Nair A., Al-Dhubiab B., Shehata T. Hydrogels and Their Combination with Liposomes, Niosomes, or Transfersomes for Dermal and Transdermal Drug Delivery. Liposomes. 2017;155:155–186. [Google Scholar]
- 71.Eroğlu İ., Aslan M., Yaman Ü., Gultekinoglu M., Çalamak S., Kart D., Ulubayram K. Liposome Based Combination Therapy for Acne Treatment. J. Liposome Res. 2019 doi: 10.1080/08982104.2019.1630646. [DOI] [PubMed] [Google Scholar]
- 72.Thapa R.K., Kiick K.L., Sullivan M.O. Encapsulation of collagen mimetic peptide-tethered vancomycin liposomes in collagen-based scaffolds for infection control in wounds. Acta Biomater. 2020;103:115–128. doi: 10.1016/j.actbio.2019.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liu L., Xiang Y., Wang Z., Yang X., Yu X., Lu Y., Deng L., Cui W. Adhesive liposomes loaded onto an injectable, self-healing and antibacterial hydrogel for promoting bone reconstruction. NPG Asia Mater. 2019;11:81. doi: 10.1038/s41427-019-0185-z. [DOI] [Google Scholar]
- 74.Hui T., Yongqing X., Tiane Z., Gang L., Yonggang Y., Muyao J., Jun L., Jing D. Treatment of osteomyelitis by liposomal gentamicin-impregnated calcium sulfate. Arch. Orthop. Trauma Surg. 2009;129:1301–1308. doi: 10.1007/s00402-008-0782-8. [DOI] [PubMed] [Google Scholar]
- 75.Zhu C.-T., Xu Y.-Q., Shi J., Li J., Ding J. Liposome combined porous β-TCP scaffold: Preparation, characterization, and anti-biofilm activity. Drug Deliv. 2010;17:391–398. doi: 10.3109/10717541003762870. [DOI] [PubMed] [Google Scholar]
- 76.Liu X.-M., Ren K., Wu G., Wang D. Preparation and Evaluation of Biomineral-Binding Antibiotic Liposomes. Liposome-Based Drug Deliv. Syst. 2018 doi: 10.1007/978-3-662-49231-4_17-1. [DOI] [Google Scholar]
- 77.Mourtas S., Diamanti G., Foka A., Dracopoulos V., Klepetsanis P., Stamouli V., Spiliopoulou I., Antimisiaris S. Inhibition of Bacterial Attachment on Surfaces by Immobilization of Tobramycin-Loaded Liposomes. J. Biomed. Nanotechnol. 2015 doi: 10.1166/jbn.2015.2160. [DOI] [PubMed] [Google Scholar]
- 78.Campardelli R., Trucillo P., Reverchon E. Supercritical assisted process for the efficient production of liposomes containing antibiotics for ocular delivery. J. CO2 Util. 2018;25:235–241. doi: 10.1016/j.jcou.2018.04.006. [DOI] [Google Scholar]
- 79.Jadhav M., Kalhapure R.S., Rambharose S., Mocktar C., Singh S., Kodama T., Govender T. Novel lipids with three C18-fatty acid chains and an amino acid head group for pH-responsive and sustained antibiotic delivery. Chem. Phys. Lipids. 2018;212:12–25. doi: 10.1016/j.chemphyslip.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 80.Khatib I., Khanal D., Ruan J., Cipolla D., Dayton F., Blanchard J.D., Chan H.K. Ciprofloxacin nanocrystals liposomal powders for controlled drug release via inhalation. Int. J. Pharm. 2019 doi: 10.1016/j.ijpharm.2019.05.068. [DOI] [PubMed] [Google Scholar]
- 81.Risaliti L., Kehagia A., Daoultzi E., Lazari D., Bergonzi M.C., Vergkizi-Nikolakaki S., Hadjipavlou-Litina D., Bilia A.R. Liposomes loaded with Salvia triloba and Rosmarinus officinalis essential oils: In vitro assessment of antioxidant, antiinflammatory and antibacterial activities. J. Drug Deliv. Sci. Technol. 2019;51:493–498. doi: 10.1016/j.jddst.2019.03.034. [DOI] [Google Scholar]
- 82.Giordani B., Costantini P.E., Fedi S., Cappelletti M., Abruzzo A., Parolin C., Foschi C., Frisco G., Calonghi N., Cerchiara T. Liposomes containing biosurfactants isolated from Lactobacillus gasseri exert antibiofilm activity against methicillin resistant Staphylococcus aureus strains. Eur. J. Pharm. Biopharm. 2019;139:246–252. doi: 10.1016/j.ejpb.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 83.Chen W., Cheng F., Swing C.J., Xia S., Zhang X. Modulation effect of core-wall ratio on the stability and antibacterial activity of cinnamaldehyde liposomes. Chem. Phys. Lipids. 2019;223:104790. doi: 10.1016/j.chemphyslip.2019.104790. [DOI] [PubMed] [Google Scholar]
- 84.Nicolosi D., Cupri S., Genovese C., Tempera G., Mattina R., Pignatello R. Nanotechnology approaches for antibacterial drug delivery: Preparation and microbiological evaluation of fusogenic liposomes carrying fusidic acid. Int. J. Antimicrob. Agents. 2015;45:622–626. doi: 10.1016/j.ijantimicag.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 85.Cavalcanti I., Pontes-Neto J., Kocerginsky P., Bezerra-Neto A., Lima J., Lira-Nogueira M., Maciel M.A.V., Neves R.P., Pimentel M.F., Santos-Magalhães N.S. Antimicrobial activity of β-lapachone encapsulated into liposomes against meticillin-resistant Staphylococcus aureus and Cryptococcus neoformans clinical strains. J. Glob. Antimicrob. Resist. 2015;3:103–108. doi: 10.1016/j.jgar.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 86.Monteiro N., Martins M., Martins A., Fonseca N.A., Moreira J.N., Reis R.L., Neves N.M. Antibacterial activity of chitosan nanofiber meshes with liposomes immobilized releasing gentamicin. Acta Biomater. 2015;18:196–205. doi: 10.1016/j.actbio.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 87.Zhang Y., Pu C., Tang W., Wang S., Sun Q. Gallic acid liposomes decorated with lactoferrin: Characterization, in vitro digestion and antibacterial activity. Food Chem. 2019;293:315–322. doi: 10.1016/j.foodchem.2019.04.116. [DOI] [PubMed] [Google Scholar]
- 88.Cheng C., Wu Z., McClements D.J., Zou L., Peng S., Zhou W., Liu W. Improvement on stability, loading capacity and sustained release of rhamnolipids modified curcumin liposomes. Colloids Surf. B Biointerfaces. 2019;183:110460. doi: 10.1016/j.colsurfb.2019.110460. [DOI] [PubMed] [Google Scholar]
- 89.Liu P., Guo B., Wang S., Ding J., Zhou W. A thermo-responsive and self-healing liposome-in-hydrogel system as an antitubercular drug carrier for localized bone tuberculosis therapy. Int. J. Pharm. 2019;558:101–109. doi: 10.1016/j.ijpharm.2018.12.083. [DOI] [PubMed] [Google Scholar]
- 90.Öztürk A.A., Aygül A., Şenel B. Influence of glyceryl behenate, tripalmitin and stearic acid on the properties of clarithromycin incorporated solid lipid nanoparticles (SLNs): Formulation, characterization, antibacterial activity and cytotoxicity. J. Drug Deliv. Sci. Technol. 2019;54:101240. doi: 10.1016/j.jddst.2019.101240. [DOI] [Google Scholar]
- 91.Öztürk A.A., Gündüz A.B., Ozisik O. Supervised Machine Learning Algorithms for Evaluation of Solid Lipid Nanoparticles and Particle Size. Comb. Chem. High Throughput Screen. 2018;21:693–699. doi: 10.2174/1386207322666181218160704. [DOI] [PubMed] [Google Scholar]
- 92.Mishra V., Bansal K.K., Verma A., Yadav N., Thakur S., Sudhakar K., Rosenholm J.M. Solid lipid nanoparticles: Emerging colloidal nano drug delivery systems. Pharmaceutics. 2018;10:191. doi: 10.3390/pharmaceutics10040191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sharma M., Gupta N., Gupta S. Implications of designing clarithromycin loaded solid lipid nanoparticles on their pharmacokinetics, antibacterial activity and safety. RSC Adv. 2016;6:76621–76631. doi: 10.1039/C6RA12841F. [DOI] [Google Scholar]
- 94.Mahajan P.S., Mahajan K.B., Darekar A. A review on solid lipid nanoparticle (SLN): An advanced treatment modality. Int. J. Pharmaceut. Sci. Res. 2015 doi: 10.13040/IJPSR.0975-8232.6(9).3698-12. [DOI] [Google Scholar]
- 95.Battaglia L., Ugazio E. Lipid Nano-and Microparticles: An Overview of Patent-Related Research. J. Nanomater. 2019;2019:2834941. doi: 10.1155/2019/2834941. [DOI] [Google Scholar]
- 96.Patravale V., Patel P. Lipidic Nanoparticles Based Composition and Method of Formulation and Use Thereof. IN3329/MUM/2010. Patent. 2010 Dec 7;
- 97.Salvi V.R., Pawar P. Nanostructured lipid carriers (NLC) system: A novel drug targeting carrier. J. Drug Deliv. Sci. Technol. 2019;51:255–267. doi: 10.1016/j.jddst.2019.02.017. [DOI] [Google Scholar]
- 98.Tran T.H., Ramasamy T., Truong D.H., Choi H.-G., Yong C.S., Kim J.O. Preparation and characterization of fenofibrate-loaded nanostructured lipid carriers for oral bioavailability enhancement. AAPS Pharmscitech. 2014;15:1509–1515. doi: 10.1208/s12249-014-0175-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yu Y., Feng R., Yu S., Li J., Wang Y., Song Y., Yang X., Pan W., Li S. Nanostructured lipid carrier-based pH and temperature dual-responsive hydrogel composed of carboxymethyl chitosan and poloxamer for drug delivery. Int. J. Biol. Macromol. 2018;114:462–469. doi: 10.1016/j.ijbiomac.2018.03.117. [DOI] [PubMed] [Google Scholar]
- 100.Yang Y., Yang Y., Xie X., Cai X., Mei X. Preparation and characterization of photo-responsive cell-penetrating peptide-mediated nanostructured lipid carrier. J. Drug Target. 2014;22:891–900. doi: 10.3109/1061186X.2014.940589. [DOI] [PubMed] [Google Scholar]
- 101.Kalhapure R.S., Mocktar C., Sikwal D.R., Sonawane S.J., Kathiravan M.K., Skelton A., Govender T. Ion pairing with linoleic acid simultaneously enhances encapsulation efficiency and antibacterial activity of vancomycin in solid lipid nanoparticles. Colloids Surf. B Biointerfaces. 2014;117:303–311. doi: 10.1016/j.colsurfb.2014.02.045. [DOI] [PubMed] [Google Scholar]
- 102.Kalhapure R.S., Sonawane S.J., Sikwal D.R., Jadhav M., Rambharose S., Mocktar C., Govender T. Solid lipid nanoparticles of clotrimazole silver complex: An efficient nano antibacterial against Staphylococcus aureus and MRSA. Colloids Surf. B Biointerfaces. 2015;136:651–658. doi: 10.1016/j.colsurfb.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 103.Bazzaz B.S.F., Khameneh B., Zarei H., Golmohammadzadeh S. Antibacterial efficacy of rifampin loaded solid lipid nanoparticles against Staphylococcus epidermidis biofilm. Microb. Pathog. 2016;93:137–144. doi: 10.1016/j.micpath.2015.11.031. [DOI] [PubMed] [Google Scholar]
- 104.Baig M.S., Ahad A., Aslam M., Imam S.S., Aqil M., Ali A. Application of Box–Behnken design for preparation of levofloxacin-loaded stearic acid solid lipid nanoparticles for ocular delivery: Optimization, in vitro release, ocular tolerance, and antibacterial activity. Int. J. Biol. Macromol. 2016;85:258–270. doi: 10.1016/j.ijbiomac.2015.12.077. [DOI] [PubMed] [Google Scholar]
- 105.Bolla P.K., Kalhapure R.S., Rodriguez V.A., Ramos D.V., Dahl A., Renukuntla J. Preparation of solid lipid nanoparticles of furosemide-silver complex and evaluation of antibacterial activity. J. Drug Deliv. Sci. Technol. 2019;49:6–13. doi: 10.1016/j.jddst.2018.10.035. [DOI] [Google Scholar]
- 106.Osman N., Omolo C.A., Gannimani R., Waddad A.Y., Rambharose S., Mocktar C., Singh S., Parboosing R., Govender T. Novel fatty acid-based pH-responsive nanostructured lipid carriers for enhancing antibacterial delivery. J. Drug Deliv. Sci. Technol. 2019;53:101125. doi: 10.1016/j.jddst.2019.101125. [DOI] [Google Scholar]
- 107.Alcantara K.P., Zulfakar M.H., Castillo A.L. Development, characterization and pharmacokinetics of mupirocin-loaded nanostructured lipid carriers (NLCs) for intravascular administration. Int. J. Pharm. 2019;571:118705. doi: 10.1016/j.ijpharm.2019.118705. [DOI] [PubMed] [Google Scholar]
- 108.Carneiro S.P., Carvalho K.V., Soares R.D.d.O.A., Carneiro C.M., de Andrade M.H.G., Duarte R.S., David O. Functionalized rifampicin-loaded nanostructured lipid carriers enhance macrophages uptake and antimycobacterial activity. Colloids Surf. B Biointerfaces. 2019;175:306–313. doi: 10.1016/j.colsurfb.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 109.Ding X., Wang A., Tong W., Xu F.J. Biodegradable Antibacterial Polymeric Nanosystems: A New Hope to Cope with Multidrug-Resistant Bacteria. Small. 2019;15:1900999. doi: 10.1002/smll.201900999. [DOI] [PubMed] [Google Scholar]
- 110.Lu Y., Zhang E., Yang J., Cao Z. Strategies to improve micelle stability for drug delivery. Nano Res. 2018;11:4985–4998. doi: 10.1007/s12274-018-2152-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xu W., Ling P., Zhang T. Polymeric micelles, a promising drug delivery system to enhance bioavailability of poorly water-soluble drugs. J. Drug Deliv. 2013;2013:340315. doi: 10.1155/2013/340315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hill L.E., Gomes C.L. Characterization of temperature and pH-responsive poly-N-isopropylacrylamide-co-polymer nanoparticles for the release of antimicrobials. Mater. Res. Express. 2014;1:035405. doi: 10.1088/2053-1591/1/3/035405. [DOI] [Google Scholar]
- 113.Kalhapure R.S., Renukuntla J. Thermo-and pH dual responsive polymeric micelles and nanoparticles. Chem.-Biol. Interact. 2018;295:20–37. doi: 10.1016/j.cbi.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 114.Liu L., Venkatraman S.S., Yang Y.Y., Guo K., Lu J., He B., Moochhala S., Kan L. Polymeric micelles anchored with TAT for delivery of antibiotics across the blood–brain barrier. Pept. Sci. 2008;90:617–623. doi: 10.1002/bip.20998. [DOI] [PubMed] [Google Scholar]
- 115.Cong Y., Quan C., Liu M., Liu J., Huang G., Tong G., Yin Y., Zhang C., Jiang Q. Alendronate-decorated biodegradable polymeric micelles for potential bone-targeted delivery of vancomycin. J. Biomater. Sci. Polym. Ed. 2015;26:629–643. doi: 10.1080/09205063.2015.1053170. [DOI] [PubMed] [Google Scholar]
- 116.Liu Y., Busscher H.J., Zhao B., Li Y., Zhang Z., van der Mei H.C., Ren Y., Shi L. Surface-adaptive, antimicrobially loaded, micellar nanocarriers with enhanced penetration and killing efficiency in staphylococcal biofilms. ACS Nano. 2016;10:4779–4789. doi: 10.1021/acsnano.6b01370. [DOI] [PubMed] [Google Scholar]
- 117.Huang F., Gao Y., Zhang Y., Cheng T., Ou H., Yang L., Liu J., Shi L., Liu J. Silver-decorated polymeric micelles combined with curcumin for enhanced antibacterial activity. ACS Appl. Mater. Interfaces. 2017;9:16880–16889. doi: 10.1021/acsami.7b03347. [DOI] [PubMed] [Google Scholar]
- 118.Sheth U., Tiwari S., Bahadur A. Preparation and characterization of anti-tubercular drugs encapsulated in polymer micelles. J. Drug Deliv. Sci. Technol. 2018;48:422–428. doi: 10.1016/j.jddst.2018.10.021. [DOI] [Google Scholar]
- 119.Chen M., Xie S., Wei J., Song X., Ding Z., Li X. Antibacterial Micelles with Vancomycin-Mediated Targeting and pH/Lipase-Triggered Release of Antibiotics. ACS Appl. Mater. Interfaces. 2018;10:36814–36823. doi: 10.1021/acsami.8b16092. [DOI] [PubMed] [Google Scholar]
- 120.Farhangi M., Kobarfard F., Mahboubi A., Vatanara A., Mortazavi S.A. Preparation of an optimized ciprofloxacin-loaded chitosan nanomicelle with enhanced antibacterial activity. Drug Dev. Ind. Pharm. 2018;44:1273–1284. doi: 10.1080/03639045.2018.1442847. [DOI] [PubMed] [Google Scholar]
- 121.Cong Y., Geng J., Wang H., Su J., Arif M., Dong Q., Chi Z., Liu C. Ureido-modified carboxymethyl chitosan-graft-stearic acid polymeric nano-micelles as a targeted delivering carrier of clarithromycin for Helicobacter pylori: Preparation and in vitro evaluation. Int. J. Biol. Macromol. 2019;129:686–692. doi: 10.1016/j.ijbiomac.2019.01.227. [DOI] [PubMed] [Google Scholar]
- 122.Liu X., Chen Y., Chen X., Su J., Huang C. Enhanced efficacy of baicalin-loaded TPGS polymeric micelles against periodontitis. Mater. Sci. Eng. C. 2019;101:387–395. doi: 10.1016/j.msec.2019.03.103. [DOI] [PubMed] [Google Scholar]
- 123.Sandreschi S., Piras A.M., Batoni G., Chiellini F. Perspectives on polymeric nanostructures for the therapeutic application of antimicrobial peptides. Nanomedicine. 2016;11:1729–1744. doi: 10.2217/nnm-2016-0057. [DOI] [PubMed] [Google Scholar]
- 124.Kravanja G., Primožič M., Knez Ž., Leitgeb M. Chitosan-based (Nano) materials for novel biomedical applications. Molecules. 2019;24:1960. doi: 10.3390/molecules24101960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Li J., Wu Y., Zhao L. Antibacterial activity and mechanism of chitosan with ultra high molecular weight. Carbohydr. Polym. 2016;148:200–205. doi: 10.1016/j.carbpol.2016.04.025. [DOI] [PubMed] [Google Scholar]
- 126.Kiruthika V., Maya S., Suresh M.K., Kumar V.A., Jayakumar R., Biswas R. Comparative efficacy of chloramphenicol loaded chondroitin sulfate and dextran sulfate nanoparticles to treat intracellular Salmonella infections. Colloids Surf. B Biointerfaces. 2015;127:33–40. doi: 10.1016/j.colsurfb.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 127.Gaspar L.M.d.A.C., Dórea A.C.S., Droppa-Almeida D., de Mélo Silva I.S., Montoro F.E., Alves L.L., Macedo M.L.H., Padilha F.F. Development and characterization of PLGA nanoparticles containing antibiotics. J. Nanopart. Res. 2018;20:289. doi: 10.1007/s11051-018-4387-z. [DOI] [Google Scholar]
- 128.Lotfipour F., Valizadeh H., Milani M., Bahrami N., Ghotaslou R. Study of antimicrobial effects of clarithromycin loaded PLGA nanoparticles against clinical strains of Helicobacter pylori. Drug Res. 2016;66:41–45. doi: 10.1055/s-0035-1548910. [DOI] [PubMed] [Google Scholar]
- 129.Malikmammadov E., Tanir T.E., Kiziltay A., Hasirci V., Hasirci N. PCL and PCL-based materials in biomedical applications. J. Biomater. Sci. Polym. Ed. 2018;29:863–893. doi: 10.1080/09205063.2017.1394711. [DOI] [PubMed] [Google Scholar]
- 130.Trousil J., Filippov S.K., Hrubý M., Mazel T., Syrová Z., Cmarko D., Svidenská S., Matějková J., Kováčik L., Porsch B. System with embedded drug release and nanoparticle degradation sensor showing efficient rifampicin delivery into macrophages. Nanomed. Nanotechnol. Biol. Med. 2017;13:307–315. doi: 10.1016/j.nano.2016.08.031. [DOI] [PubMed] [Google Scholar]
- 131.Ibrahim H.M., El-Bisi M.K., Taha G.M., El-Alfy E.A. Chitosan nanoparticles loaded antibiotics as drug delivery biomaterial. J. Appl. Pharm. Sci. 2015;5:85–90. doi: 10.7324/JAPS.2015.501015. [DOI] [Google Scholar]
- 132.Kariminia S., Shamsipur A., Shamsipur M. Analytical characteristics and application of novel chitosan coated magnetic nanoparticles as an efficient drug delivery system for ciprofloxacin. Enhanced drug release kinetics by low-frequency ultrasounds. J. Pharm. Biomed. Anal. 2016;129:450–457. doi: 10.1016/j.jpba.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 133.Kumar G.V., Su C.-H., Velusamy P. Ciprofloxacin loaded genipin cross-linked chitosan/heparin nanoparticles for drug delivery application. Mater. Lett. 2016;180:119–122. doi: 10.1016/j.matlet.2016.05.108. [DOI] [Google Scholar]
- 134.Huang Y.-C., Li R.-Y., Chen J.-Y., Chen J.-K. Biphasic release of gentamicin from chitosan/fucoidan nanoparticles for pulmonary delivery. Carbohydr. Polym. 2016;138:114–122. doi: 10.1016/j.carbpol.2015.11.072. [DOI] [PubMed] [Google Scholar]
- 135.Kalhapure R.S., Jadhav M., Rambharose S., Mocktar C., Singh S., Renukuntla J., Govender T. pH-responsive chitosan nanoparticles from a novel twin-chain anionic amphiphile for controlled and targeted delivery of vancomycin. Colloids Surf. B Biointerfaces. 2017;158:650–657. doi: 10.1016/j.colsurfb.2017.07.049. [DOI] [PubMed] [Google Scholar]
- 136.Elbi S., Nimal T., Rajan V., Baranwal G., Biswas R., Jayakumar R., Sathianarayanan S. Fucoidan coated ciprofloxacin loaded chitosan nanoparticles for the treatment of intracellular and biofilm infections of Salmonella. Colloids Surf. B Biointerfaces. 2017;160:40–47. doi: 10.1016/j.colsurfb.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 137.Chavan C., Bala P., Pal K., Kale S. Cross-linked chitosan-dextran sulphate vehicle system for controlled release of ciprofloxaxin drug: An ophthalmic application. OpenNano. 2017;2:28–36. doi: 10.1016/j.onano.2017.04.002. [DOI] [Google Scholar]
- 138.Patel K.K., Tripathi M., Pandey N., Agrawal A.K., Gade S., Anjum M.M., Tilak R., Singh S. Alginate lyase immobilized chitosan nanoparticles of ciprofloxacin for the improved antimicrobial activity against the biofilm associated mucoid P. aeruginosa infection in cystic fibrosis. Int. J. Pharm. 2019;563:30–42. doi: 10.1016/j.ijpharm.2019.03.051. [DOI] [PubMed] [Google Scholar]
- 139.Baelo A., Levato R., Julián E., Crespo A., Astola J., Gavaldà J., Engel E., Mateos-Timoneda M.A., Torrents E. Disassembling bacterial extracellular matrix with DNase-coated nanoparticles to enhance antibiotic delivery in biofilm infections. J. Control. Release. 2015;209:150–158. doi: 10.1016/j.jconrel.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 140.Sabaeifard P., Abdi-Ali A., Soudi M.R., Gamazo C., Irache J.M. Amikacin loaded PLGA nanoparticles against Pseudomonas aeruginosa. Eur. J. Pharm. Sci. 2016;93:392–398. doi: 10.1016/j.ejps.2016.08.049. [DOI] [PubMed] [Google Scholar]
- 141.Türeli N.G., Torge A., Juntke J., Schwarz B.C., Schneider-Daum N., Türeli A.E., Lehr C.M., Schneider M. Ciprofloxacin-loaded PLGA nanoparticles against cystic fibrosis P. aeruginosa lung infections. Eur. J. Pharm. Biopharm. 2017;117:363–371. doi: 10.1016/j.ejpb.2017.04.032. [DOI] [PubMed] [Google Scholar]
- 142.Jiang L., Greene M.K., Insua J.L., Pessoa J.S., Small D.M., Smyth P., McCann A.P., Cogo F., Bengoechea J.A., Taggart C.C. Clearance of intracellular Klebsiella pneumoniae infection using gentamicin-loaded nanoparticles. J. Control. Release. 2018;279:316–325. doi: 10.1016/j.jconrel.2018.04.040. [DOI] [PubMed] [Google Scholar]
- 143.Ernst J., Klinger-Strobel M., Arnold K., Thamm J., Hartung A., Pletz M.W., Makarewicz O., Fischer D. Polyester-based particles to overcome the obstacles of mucus and biofilms in the lung for tobramycin application under static and dynamic fluidic conditions. Eur. J. Pharm. Biopharm. 2018;131:120–129. doi: 10.1016/j.ejpb.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 144.Hasan N., Cao J., Lee J., Naeem M., Hlaing S.P., Kim J., Jung Y., Lee B.-L., Yoo J.-W. PEI/NONOates-doped PLGA nanoparticles for eradicating methicillin-resistant Staphylococcus aureus biofilm in diabetic wounds via binding to the biofilm matrix. Mater. Sci. Eng. C. 2019;103:109741. doi: 10.1016/j.msec.2019.109741. [DOI] [PubMed] [Google Scholar]
- 145.Abdelghany S., Parumasivam T., Pang A., Roediger B., Tang P., Jahn K., Britton W.J., Chan H.K. Alginate modified-PLGA nanoparticles entrapping amikacin and moxifloxacin as a novel host-directed therapy for multidrug-resistant tuberculosis. J. Drug Deliv. Sci. Technol. 2019;52:642–651. doi: 10.1016/j.jddst.2019.05.025. [DOI] [Google Scholar]
- 146.Mukherjee S., Chowdhury D., Kotcherlakota R., Patra S. Potential theranostics application of bio-synthesized silver nanoparticles (4-in-1 system) Theranostics. 2014;4:316–335. doi: 10.7150/thno.7819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kasithevar M., Periakaruppan P., Muthupandian S., Mohan M. Antibacterial efficacy of silver nanoparticles against multi-drug resistant clinical isolates from post-surgical wound infections. Microb. Pathog. 2017;107:327–334. doi: 10.1016/j.micpath.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 148.Sathishkumar R., Sundaramanickam A., Srinath R., Ramesh T., Saranya K., Meena M., Surya P. Green synthesis of silver nanoparticles by bloom forming marine microalgae Trichodesmium erythraeum and its applications in antioxidant, drug-resistant bacteria, and cytotoxicity activity. J. Saudi Chem. Soc. 2019;23:1180–1191. doi: 10.1016/j.jscs.2019.07.008. [DOI] [Google Scholar]
- 149.Swaroop K., Francis S., Somashekarappa H. Gamma irradiation synthesis of Ag/PVA hydrogels and its antibacterial activity. Mater. Today Proc. 2016;3:1792–1798. doi: 10.1016/j.matpr.2016.04.076. [DOI] [Google Scholar]
- 150.Neihaya H., Zaman H. Investigating the effect of biosynthesized silver nanoparticles as antibiofilm on bacterial clinical isolates. Microb. Pathog. 2018;116:200–208. doi: 10.1016/j.micpath.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 151.Bajaj M., Pandey S.K., Nain T., Brar S.K., Singh P., Singh S., Wangoo N., Sharma R.K. Stabilized cationic dipeptide capped gold/silver nanohybrids: Towards enhanced antibacterial and antifungal efficacy. Colloids Surf. B Biointerfaces. 2017;158:397–407. doi: 10.1016/j.colsurfb.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 152.Martínez-Carmona M., Gun’ko Y.K., Vallet-Regí M. Mesoporous silica materials as drug delivery: “The Nightmare” of bacterial infection. Pharmaceutics. 2018;10:279. doi: 10.3390/pharmaceutics10040279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Jang J., Kim Y. Fabrication of monodisperse silica–polymer core–shell nanoparticles with excellent antimicrobial efficacy. Chem. Commun. 2008:4016–4018. doi: 10.1039/b809137d. [DOI] [PubMed] [Google Scholar]
- 154.Dong A., Huang J., Lan S., Wang T., Xiao L., Wang W., Zhao T., Zheng X., Liu F., Gao G. Synthesis of N-halamine-functionalized silica–polymer core–shell nanoparticles and their enhanced antibacterial activity. Nanotechnology. 2011;22:295602. doi: 10.1088/0957-4484/22/29/295602. [DOI] [PubMed] [Google Scholar]
- 155.Mohammed L., Gomaa H.G., Ragab D., Zhu J. Magnetic nanoparticles for environmental and biomedical applications: A review. Particuology. 2017;30:1–14. doi: 10.1016/j.partic.2016.06.001. [DOI] [Google Scholar]
- 156.Flores-González M., Talavera-Rojas M., Soriano-Vargas E., Rodríguez-González V. Practical mediated-assembly synthesis of silver nanowires using commercial Camellia sinensis extracts and their antibacterial properties. New J. Chem. 2018;42:2133–2139. doi: 10.1039/C7NJ03812G. [DOI] [Google Scholar]
- 157.Madubuonu N., Aisida S.O., Ali A., Ahmad I., Zhao T.-K., Botha S., Maaza M., Ezema F.I. Biosynthesis of iron oxide nanoparticles via a composite of Psidium guavaja-Moringa oleifera and their antibacterial and photocatalytic study. J. Photochem. Photobiol. B Biol. 2019;199:111601. doi: 10.1016/j.jphotobiol.2019.111601. [DOI] [PubMed] [Google Scholar]
- 158.Davarpanah A., Rahdar A., Dastnae M.A., Zeybek O., Beyzaei H. (1−x) BaFe12O19/xCoFe2O4 hard/soft magnetic nanocomposites: Synthesis, physical characterization, and antibacterial activities study. J. Mol. Struct. 2019;1175:445–449. doi: 10.1016/j.molstruc.2018.07.092. [DOI] [Google Scholar]
- 159.Petros R.A., DeSimone J.M. Strategies in the design of nanoparticles for therapeutic applications. Nat. Rev. Drug Discov. 2010;9:615. doi: 10.1038/nrd2591. [DOI] [PubMed] [Google Scholar]
- 160.Pati R., Mehta R.K., Mohanty S., Padhi A., Sengupta M., Vaseeharan B., Goswami C., Sonawane A. Topical application of zinc oxide nanoparticles reduces bacterial skin infection in mice and exhibits antibacterial activity by inducing oxidative stress response and cell membrane disintegration in macrophages. Nanomed. Nanotechnol. Biol. Med. 2014;10:1195–1208. doi: 10.1016/j.nano.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 161.Premanathan M., Karthikeyan K., Jeyasubramanian K., Manivannan G. Selective toxicity of ZnO nanoparticles toward Gram-positive bacteria and cancer cells by apoptosis through lipid peroxidation. Nanomed. Nanotechnol. Biol. Med. 2011;7:184–192. doi: 10.1016/j.nano.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 162.Hoseyni S.J., Manoochehri M., Asli M.D. Synthesis of cobalt nanoparticles by complex demolition method using the reaction between organic ligand Schiff base and cobalt chloride by ultrasonication. Bulletin de la Société Royale des Sciences de Liège. 2017;86:325–331. [Google Scholar]
- 163.Gargibala satpathy E.M. Cobalt Nanoparticle as The Antibacterial Tool: In Vitro. Int. J. Eng. Adv. Technol. 2019;8:3684–3687. [Google Scholar]
- 164.Khan S., Ansari A.A., Khan A.A., Ahmad R., Al-Obaid O., Al-Kattan W. In vitro evaluation of anticancer and antibacterial activities of cobalt oxide nanoparticles. JBIC J. Biol. Inorg. Chem. 2015;20:1319–1326. doi: 10.1007/s00775-015-1310-2. [DOI] [PubMed] [Google Scholar]
- 165.Khalil A.T., Ovais M., Ullah I., Ali M., Shinwari Z.K., Maaza M. Physical properties, biological applications and biocompatibility studies on biosynthesized single phase cobalt oxide (Co3O4) nanoparticles via Sageretia thea (Osbeck.) Arab. J. Chem. 2020;13:606–619. doi: 10.1016/j.arabjc.2017.07.004. [DOI] [Google Scholar]
- 166.Dogra V., Kaur G., Jindal S., Kumar R., Kumar S., Singhal N.K. Bactericidal effects of metallosurfactants based cobalt oxide/hydroxide nanoparticles against Staphylococcus aureus. Sci. Total Environ. 2019;681:350–364. doi: 10.1016/j.scitotenv.2019.05.078. [DOI] [PubMed] [Google Scholar]
- 167.Cui D., Yan C., Miao J., Zhang X., Chen J., Sun L., Meng L., Liang T., Li Q. Synthesis, characterization and antitumor properties of selenium nanoparticles coupling with ferulic acid. Mater. Sci. Eng. C. 2018;90:104–112. doi: 10.1016/j.msec.2018.04.048. [DOI] [PubMed] [Google Scholar]
- 168.Xu C., Qiao L., Guo Y., Ma L., Cheng Y. Preparation, characteristics and antioxidant activity of polysaccharides and proteins-capped selenium nanoparticles synthesized by Lactobacillus casei ATCC 393. Carbohydr. Polym. 2018;195:576–585. doi: 10.1016/j.carbpol.2018.04.110. [DOI] [PubMed] [Google Scholar]
- 169.Yazhiniprabha M., Vaseeharan B. In vitro and in vivo toxicity assessment of selenium nanoparticles with significant larvicidal and bacteriostatic properties. Mater. Sci. Eng. C. 2019;103:109763. doi: 10.1016/j.msec.2019.109763. [DOI] [PubMed] [Google Scholar]
- 170.Ghotekar S. A review on plant extract mediated biogenic synthesis of CdO nanoparticles and their recent applications. Asian J. Green Chem. 2019;3:187–200. [Google Scholar]
- 171.Zahera M., Khan S.A., Khan I.A., Elgorban A.M., Bahkali A.H., Alghamdi S.M., Khan M.S. Enhancing using glucose encapsulation, the efficacy of CdO NPs against multi-drug resistant Escherichia coli. Microb. Pathog. 2018;119:42–48. doi: 10.1016/j.micpath.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 172.Simões M., Simões L.C., Vieira M.J. A review of current and emergent biofilm control strategies. LWT Food Sci. Technol. 2010;43:573–583. doi: 10.1016/j.lwt.2009.12.008. [DOI] [Google Scholar]
- 173.Sood U., Singh D.N., Hira P., Lee J.-K., Kalia V.C., Lal R., Shakarad M. Rapid and solitary production of mono-rhamnolipid biosurfactant and biofilm inhibiting pyocyanin by a taxonomic outlier Pseudomonas aeruginosa strain CR1. J. Biotechnol. 2020;307:98–106. doi: 10.1016/j.jbiotec.2019.11.004. [DOI] [PubMed] [Google Scholar]
- 174.Li P., Chen X., Shen Y., Li H., Zou Y., Yuan G., Hu P., Hu H. Mucus penetration enhanced lipid polymer nanoparticles improve the eradication rate of Helicobacter pylori biofilm. J. Control. Release. 2019;300:52–63. doi: 10.1016/j.jconrel.2019.02.039. [DOI] [PubMed] [Google Scholar]
- 175.Khalid H.F., Tehseen B., Sarwar Y., Hussain S.Z., Khan W.S., Raza Z.A., Bajwa S.Z., Kanaras A.G., Hussain I., Rehman A. Biosurfactant coated silver and iron oxide nanoparticles with enhanced anti-biofilm and anti-adhesive properties. J. Hazard. Mater. 2019;364:441–448. doi: 10.1016/j.jhazmat.2018.10.049. [DOI] [PubMed] [Google Scholar]
- 176.Zhai J., Fong C., Tran N., Drummond C.J. Nonlamellar lyotropic liquid crystalline lipid nanoparticles for the next generation of nanomedicine. ACS Nano. 2019;13:6178–6206. doi: 10.1021/acsnano.8b07961. [DOI] [PubMed] [Google Scholar]
- 177.Boge L., Hallstensson K., Ringstad L., Johansson J., Andersson T., Davoudi M., Larsson P.T., Mahlapuu M., Håkansson J., Andersson M. Cubosomes for topical delivery of the antimicrobial peptide LL-37. Eur. J. Pharm. Biopharm. 2019;134:60–67. doi: 10.1016/j.ejpb.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 178.Mendes C., Meirelles G.C., Barp C.G., Assreuy J., Silva M.A., Ponchel G. Cyclodextrin based nanosponge of norfloxacin: Intestinal permeation enhancement and improved antibacterial activity. Carbohydr. Polym. 2018;195:586–592. doi: 10.1016/j.carbpol.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 179.Tran N., Hocquet M., Eon B., Sangwan P., Ratcliffe J., Hinton T.M., White J., Ozcelik B., Reynolds N.P., Muir B.W. Nonlamellar lyotropic liquid crystalline nanoparticles enhance the antibacterial effects of rifampicin against Staphylococcus aureus. J. Colloid Interface Sci. 2018;519:107–118. doi: 10.1016/j.jcis.2018.02.048. [DOI] [PubMed] [Google Scholar]
- 180.McArthur M. Transcription factor decoys for the treatment and prevention of infections caused by bacteria including clostridium difficile. US20140274800A1. U.S. Patents. 2013 Mar 13;
- 181.González-Paredes A., Sitia L., Ruyra A., Morris C.J., Wheeler G.N., McArthur M., Gasco P. Solid lipid nanoparticles for the delivery of anti-microbial oligonucleotides. Eur. J. Pharm. Biopharm. 2019;134:166–177. doi: 10.1016/j.ejpb.2018.11.017. [DOI] [PubMed] [Google Scholar]
- 182.Mamusa M., Barbero F., Montis C., Cutillo L., Gonzalez-Paredes A., Berti D. Inclusion of oligonucleotide antimicrobials in biocompatible cationic liposomes: A structural study. J. Colloid Interface Sci. 2017;508:476–487. doi: 10.1016/j.jcis.2017.08.080. [DOI] [PubMed] [Google Scholar]
- 183.Bai H., Xue X., Hou Z., Zhou Y., Meng J., Luo X. Antisense antibiotics: A brief review of novel target discovery and delivery. Curr. Drug Discov. Technol. 2010;7:76–85. doi: 10.2174/157016310793180594. [DOI] [PubMed] [Google Scholar]
- 184.Xue X.-Y., Mao X.-G., Zhou Y., Chen Z., Hu Y., Hou Z., Li M.-K., Meng J.-R., Luo X.X. Advances in the delivery of antisense oligonucleotides for combating bacterial infectious diseases. Nanomed. Nanotechnol. Biol. Med. 2018;14:745–758. doi: 10.1016/j.nano.2017.12.026. [DOI] [PubMed] [Google Scholar]
- 185.Hegarty J.P., Stewart D.B. Advances in therapeutic bacterial antisense biotechnology. Appl. Microbiol. Biotechnol. 2018;102:1055–1065. doi: 10.1007/s00253-017-8671-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Rai M., Paralikar P., Jogee P., Agarkar G., Ingle A.P., Derita M., Zacchino S. Synergistic antimicrobial potential of essential oils in combination with nanoparticles: Emerging trends and future perspectives. Int. J. Pharm. 2017;519:67–78. doi: 10.1016/j.ijpharm.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 187.Rodenak-Kladniew B., Montoto S.S., Sbaraglini M., Di Ianni M., Ruiz M., Talevi A., Alvarez V.A., Durán N., Castro G.R., Islan G.A. Hybrid Ofloxacin/eugenol co-loaded solid lipid nanoparticles with enhanced and targetable antimicrobial properties. Int. J. Pharm. 2019;569:118575. doi: 10.1016/j.ijpharm.2019.118575. [DOI] [PubMed] [Google Scholar]
- 188.Gao H., Cheng T., Zhang Y., Liu J., Huang F., Yang C., Shi L., Liu J. A charge-adaptive nanosystem for prolonged and enhanced in vivo antibiotic delivery. Chem. Coummun. 2016;52:6265–6268. doi: 10.1039/c6cc01269h. [DOI] [PubMed] [Google Scholar]
- 189.Li Y., Liu G., Wang X., Hu J., Liu S. Enzyme-Responsive Polymeric Vesicles for Bacterial-Strain-Selective Delivery of Antimicrobial Agents. Angew. Chem. Int. Ed. 2016;55:1760–1764. doi: 10.1002/anie.201509401. [DOI] [PubMed] [Google Scholar]
- 190.Augustine R., Kalva N., Kim H.A., Zhang Y., Kim I. pH-Responsive Polypeptide-Based Smart Nano-Carriers for Theranostic Applications. Molecules. 2019;24:2961. doi: 10.3390/molecules24162961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Zhang Y., Algburi A., Wang N., Kholodovych V., Oh D.O., Chikindas M., Uhrich K.E. Self-assembled cationic amphiphiles as antimicrobial peptides mimics: Role of hydrophobicity, linkage type, and assembly state. Nanomed. Nanotechnol. Biol. Med. 2017;13:343–352. doi: 10.1016/j.nano.2016.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Fillion M., Valois-Paillard G., Lorin A., Noël M., Voyer N., Auger M. Membrane interactions of synthetic peptides with antimicrobial potential: Effect of electrostatic interactions and amphiphilicity. Probiotics Antimicrob. Proteins. 2015;7:66–74. doi: 10.1007/s12602-014-9177-z. [DOI] [PubMed] [Google Scholar]
- 193.Mahmoudi H., Bahador A., Pourhajibagher M., Alikhani M.Y. Antimicrobial photodynamic therapy: An effective alternative approach to control bacterial infections. J. Lasers Med. Sci. 2018;9:154. doi: 10.15171/jlms.2018.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Cieplik F., Deng D., Crielaard W., Buchalla W., Hellwig E., Al-Ahmad A., Maisch T. Antimicrobial photodynamic therapy–what we know and what we don’t. Crit. Rev. Microbiol. 2018;44:571–589. doi: 10.1080/1040841X.2018.1467876. [DOI] [PubMed] [Google Scholar]
- 195.Ghosh S., Qi R., Carter K.A., Zhang G., Pfeifer B.A., Lovell J.F. Loading and releasing ciprofloxacin in photoactivatable liposomes. Biochem. Eng. J. 2019;141:43–48. doi: 10.1016/j.bej.2018.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Jeong S., Lee J., Im B.N., Park H., Na K. Combined photodynamic and antibiotic therapy for skin disorder via lipase-sensitive liposomes with enhanced antimicrobial performance. Biomaterials. 2017;141:243–250. doi: 10.1016/j.biomaterials.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 197.Domalaon R., Ammeter D., Brizuela M., Gorityala B.K., Zhanel G.G., Schweizer F. Repurposed antimicrobial combination therapy: Tobramycin-ciprofloxacin hybrid augments activity of the anticancer drug mitomycin C against multidrug-resistant Gram-negative bacteria. Front. Microbiol. 2019;10:1556. doi: 10.3389/fmicb.2019.01556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Xu X., Xu L., Yuan G., Wang Y., Qu Y., Zhou M. Synergistic combination of two antimicrobial agents closing each other’s mutant selection windows to prevent antimicrobial resistance. Sci. Rep. 2018;8:7237. doi: 10.1038/s41598-018-25714-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Walvekar P., Gannimani R., Govender T. Combination drug therapy via nanocarriers against infectious diseases. Eur. J. Pharm. Sci. 2019;127:121–141. doi: 10.1016/j.ejps.2018.10.017. [DOI] [PubMed] [Google Scholar]
- 200.Chai G., Park H., Yu S., Zhou F., Li J., Xu Q., Zhou Q.T. Evaluation of co-delivery of colistin and ciprofloxacin in liposomes using an in vitro human lung epithelial cell model. Int. J. Pharm. 2019;569:118616. doi: 10.1016/j.ijpharm.2019.118616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ye T., Sun S., Sugianto T.D., Tang P., Parumasivam T., Chang Y.K., Astudillo A., Wang S., Chan H.-K. Novel combination proliposomes containing tobramycin and clarithromycin effective against Pseudomonas aeruginosa biofilms. Int. J. Pharm. 2018;552:130–138. doi: 10.1016/j.ijpharm.2018.09.061. [DOI] [PubMed] [Google Scholar]
- 202.Fumakia M., Ho E.A. Nanoparticles encapsulated with LL37 and serpin A1 promotes wound healing and synergistically enhances antibacterial activity. Mol. Pharm. 2016;13:2318–2331. doi: 10.1021/acs.molpharmaceut.6b00099. [DOI] [PubMed] [Google Scholar]
- 203.Shimanovich U., Lipovsky A., Eliaz D., Zigdon S., Knowles T.P., Nitzan Y., Michaeli S., Gedanken A. Tetracycline Nanoparticles as Antibacterial and Gene-Silencing Agents. Adv. Healthc. Mater. 2015;4:723–728. doi: 10.1002/adhm.201400631. [DOI] [PubMed] [Google Scholar]
- 204.Morakul B., Suksiriworapong J., Chomnawang M.T., Langguth P., Junyaprasert V.B. Dissolution enhancement and in vitro performance of clarithromycin nanocrystals produced by precipitation–lyophilization–homogenization method. Eur. J. Pharm. Biopharm. 2014;88:886–896. doi: 10.1016/j.ejpb.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 205.Havel H.A. Where are the nanodrugs? An industry perspective on development of drug products containing nanomaterials. AAPS J. 2016;18:1351–1353. doi: 10.1208/s12248-016-9970-6. [DOI] [PubMed] [Google Scholar]
- 206.Romero-Calle D., Guimarães Benevides R., Góes-Neto A., Billington C. Bacteriophages as Alternatives to Antibiotics in Clinical Care. Antibiotics. 2019;8:138. doi: 10.3390/antibiotics8030138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Chadha P., Katare O.P., Chhibber S. Liposome loaded phage cocktail: Enhanced therapeutic potential in resolving Klebsiella pneumoniae mediated burn wound infections. Burns. 2017;43:1532–1543. doi: 10.1016/j.burns.2017.03.029. [DOI] [PubMed] [Google Scholar]
- 208.Haworth C.S., Bilton D., Chalmers J.D., Davis A.M., Froehlich J., Gonda I., Thompson B., Wanner A., O’Donnell A.E. Inhaled liposomal ciprofloxacin in patients with non-cystic fibrosis bronchiectasis and chronic lung infection with Pseudomonas aeruginosa (ORBIT-3 and ORBIT-4): Two phase 3, randomised controlled trials. Lancet Respir. Med. 2019;7:213–226. doi: 10.1016/S2213-2600(18)30427-2. [DOI] [PubMed] [Google Scholar]
- 209.ClinicalTrials.gov Phase 3 Study With Ciprofloxacin Dispersion for Inhalation in Non-CF Bronchiectasis (ORBIT-3) [(accessed on 21 November 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01515007.
- 210.ClinicalTrials.gov Liposomal Amikacin for Inhalation (LAI) for Nontuberculous Mycobacteria. [(accessed on 4 November 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01315236.
- 211.ClinicalTrials.gov Study of Dose Escalation of Liposomal Amikacin for Inhalation (ARIKAYCE™)—Extension Phase. [(accessed on 18 November 2019)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT03905642.
- 212.ClinicalTrials.gov Liposomal Amikacin for Inhalation (LAI) in the Treatment of Mycobacterium Abscessus Lung Disease. [(accessed on 4 November 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03038178.
- 213.ClinicalTrials.gov Extension Study of Liposomal Amikacin for Inhalation in Cystic Fibrosis (CF) Patients With Chronic Pseudomonas Aeruginosa (Pa) Infection. [(accessed on 12 November 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01316276.
- 214.Mullard A. FDA approves antitoxin antibody. Nat. Rev. Drug Discov. 2016;15:811. doi: 10.1038/nrd.2016.257. [DOI] [PubMed] [Google Scholar]
- 215.Azeredo da Silveira S., Perez A. Improving the fate of severely infected patients: The promise of anti-toxin treatments and superiority trials. Expert Rev. Anti-Infect. Ther. 2017;15:973–975. doi: 10.1080/14787210.2017.1400908. [DOI] [PubMed] [Google Scholar]
- 216.Laterre P.-F., Colin G., Dequin P.-F., Dugernier T., Boulain T., Azeredo da Silveira S., Lajaunias F.C., Perez A., François B. CAL02, a novel antitoxin liposomal agent, in severe pneumococcal pneumonia: A first-in-human, double-blind, placebo-controlled, randomised trial. Lancet Infect. Dis. 2019;19:620–630. doi: 10.1016/S1473-3099(18)30805-3. [DOI] [PubMed] [Google Scholar]
- 217.Molchanova N., Hansen P.R., Franzyk H. Advances in Development of Antimicrobial Peptidomimetics as Potential Drugs. Molecules. 2017;22:1430. doi: 10.3390/molecules22091430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.ClinicalTrials.gov Study to Evaluate Efficacy of LAI When Added to Multi-drug Regimen Compared to Multi-drug Regimen Alone (CONVERT) [(accessed on 25 October 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02344004.
- 219.ClinicalTrials.gov Study of the Clinical Effectiveness of a Human Monoclonal Antibody to C. Difficile Toxin A and Toxin B in Patients With Clostridium Difficile Associated Disease. [(accessed on 16 November 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT00350298?term=anti+toxin&draw=3&rank=13.
- 220.Ghobrial O.G., Derendorf H., Hillman J.D. Pharmacodynamic activity of the lantibiotic MU1140. Int. J. Antimicrob. Agents. 2009;33:70–74. doi: 10.1016/j.ijantimicag.2008.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Andrä J., Jakovkin I., Grötzinger J., Hecht O., Krasnosdembskaya A.D., Goldmann T., Gutsmann T., Leippe M. Structure and mode of action of the antimicrobial peptide arenicin. Biochem. J. 2008;410:113–122. doi: 10.1042/BJ20071051. [DOI] [PubMed] [Google Scholar]
- 222.Gebhart D., Lok S., Clare S., Tomas M., Stares M., Scholl D., Donskey C., Lawley T., Govoni A. Modified R-Type Bacteriocin Specifically Targeting Clostridium Difficile Prevents Colonization of Mice without Affecting Gut Microbiota Diversity. mBio. 2015;6 doi: 10.1128/mBio.02368-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Crowther G.S., Baines S.D., Todhunter S.L., Freeman J., Chilton C.H., Wilcox M.H. Evaluation of NVB302 versus vancomycin activity in an in vitro human gut model of Clostridium difficile infection. J. Antimicrob. Chemother. 2012;68:168–176. doi: 10.1093/jac/dks359. [DOI] [PubMed] [Google Scholar]
- 224.van der Velden W.J.F.M., van Iersel T.M.P., Blijlevens N.M.A., Donnelly J.P. Safety and tolerability of the antimicrobial peptide human lactoferrin 1-11 (hLF1-11) BMC Med. 2009;7:44. doi: 10.1186/1741-7015-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Zhang W., Li Y., Qian G., Wang Y., Chen H., Wu Z.-H., Liu F., Shen Y., Du L. Identification and Characterization of the Anti-Methicillin-Resistant Staphylococcus aureus WAP-8294A2 Biosynthetic Gene Cluster from Lysobacter enzymogenes OH11. Antimicrob. Agents Chemother. 2011;55:5581–5589. doi: 10.1128/AAC.05370-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Kaplan C., Sim J., Shah K., Kaplan A., Shi W., Eckert R. Selective Membrane Disruption: Mode of Action of C16G2, a Specifically Targeted Antimicrobial Peptide. Antimicrob. Agents Chemother. 2011;55:3446–3452. doi: 10.1128/AAC.00342-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.ClinicalTrials.gov A Study of DPK-060 to Investigate Clinical Safety and Efficacy in Patients With Acute External Otitis. [(accessed on 10 December 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01447017.
- 228.ClinicalTrials.gov A Phase II Study to Evaluate the Efficacy and Safety of Two Doses of LTX-109 in Impetigo. [(accessed on 10 December 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01803035.
- 229.Nilsson A.C., Janson H., Wold H., Fugelli A., Andersson K., Håkangård C., Olsson P., Olsen W.M. LTX-109 is a novel agent for nasal decolonization of methicillin-resistant and -sensitive Staphylococcus aureus. Antimicrob. Agents Chemother. 2015;59:145–151. doi: 10.1128/AAC.03513-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.ClinicalTrials.gov Phase III Efficacy and Safety Study of AB103 in the Treatment of Patients With Necrotizing Soft Tissue Infections (ACCUTE) [(accessed on 11 December 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02469857.
- 231.Knight-Connoni V., Mascio C., Chesnel L., Silverman J. Discovery and development of surotomycin for the treatment of Clostridium difficile. J. Ind. Microbiol. Biotechnol. 2016;43:195–204. doi: 10.1007/s10295-015-1714-6. [DOI] [PubMed] [Google Scholar]
- 232.Stiefel U., Davis N., Helfand M., Donskey C. Efficacy of Oral Ramoplanin for Inhibition of Intestinal Colonization by Vancomycin-Resistant Enterococci in Mice. Antimicrob. Agents Chemother. 2004;48:2144–2148. doi: 10.1128/AAC.48.6.2144-2148.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Narang A., Chang R.-K., Hussain M.A. Pharmaceutical development and regulatory considerations for nanoparticles and nanoparticulate drug delivery systems. J. Pharm. Sci. 2013;102:3867–3882. doi: 10.1002/jps.23691. [DOI] [PubMed] [Google Scholar]
- 234.Hua S., De Matos M.B.C., Metselaar J.M., Storm G. Current trends and challenges in the clinical translation of nanoparticulate nanomedicines: Pathways for translational development and commercialization. Front. Pharmacol. 2018;9:790. doi: 10.3389/fphar.2018.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Tinkle S., McNeil S.E., Mühlebach S., Bawa R., Borchard G., Barenholz Y., Tamarkin L., Desai N. Nanomedicines: Addressing the scientific and regulatory gap. Ann. N. Y. Acad. Sci. 2014;1313:35–56. doi: 10.1111/nyas.12403. [DOI] [PubMed] [Google Scholar]
- 236.Kumar Teli M., Mutalik S., Rajanikant G.K. Nanotechnology and nanomedicine: Going small means aiming big. Curr. Pharm. Des. 2010;16:1882–1892. doi: 10.2174/138161210791208992. [DOI] [PubMed] [Google Scholar]
- 237.Accomasso L., Cristallini C., Giachino C. Risk assessment and risk minimization in nanomedicine: A need for predictive, alternative, and 3Rs strategies. Front. Pharmacol. 2018;9:228. doi: 10.3389/fphar.2018.00228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Murday J.S., Siegel R.W., Stein J., Wright J.F. Translational nanomedicine: Status assessment and opportunities. Nanomed. Nanotechnol. Biol. Med. 2009;5:251–273. doi: 10.1016/j.nano.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 239.Hafner A., Lovric J., Lakos G.P., Pepic I. Nanotherapeutics in the EU: An overview on current state and future directions. Int. J. Nanomed. 2014;9:1005. doi: 10.2147/IJN.S55359. [DOI] [PMC free article] [PubMed] [Google Scholar]