Abstract
Study Design:
Systematic review.
Objective:
To assess the current literature regarding the relationship between the shoulder and the spine with regard to (1) overlapping pain pathways; (2) differentiating history, exam findings, and diagnostic findings; (3) concomitant pathology and optimal treatments; and (4) cervical spine-based etiology for shoulder problems.
Methods:
A systematic literature search was performed according to the guidelines set forth by the Cochrane Collaboration. Studies were included if they examined the clinical, anatomical, or physiological overlap between the shoulder and cervical spine. Two reviewers screened and selected full texts for inclusion according to the objectives of the study. Quality of evidence was graded using OCEBM (Oxford Center for Evidence Based Medicine) and MINORS (Methodological Index for Nonrandomized Studies) scores.
Results:
Out of 477 references screened, 76 articles were included for review and grouped into 4 main sections (overlapping pain pathways, differentiating exam findings, concomitant/masquerading pathology, and cervical spine-based etiology of shoulder pathology). There is evidence to suggest cervical spine pathology may cause shoulder pain and that shoulder pathology may cause neck pain. Specific examination tests used to differentiate shoulder and spine pathology are critical as imaging studies may be misleading. Diagnostic injections can be useful to confirm sources of pain as well as predicting the success of surgery in both the shoulder and the spine. There is limited evidence to suggest alterations in the relationship between the spine and the scapula may predispose to shoulder impingement or rotator cuff tears. Moreover, cervical neurological lesions may predispose patients to developing rotator cuff tears. The decision to proceed with shoulder or spine surgery first should be delineated with careful examination and the use of shoulder and spine diagnostic injections.
Conclusion:
Shoulder and spine pathology commonly overlap. Knowledge of anatomy, pain referral patterns, shoulder kinematics, and examination techniques are invaluable to the clinician in making an appropriate diagnosis and guiding treatment. In this review, we present an algorithm for the identification and treatment of shoulder and cervical spine pathology.
Keywords: cervical spine pain, exam, radiculopathy, rotator cuff tear, shoulder pain, suprascapular neuropathy
Introduction
The etiology of pain arising in either the neck or the shoulder can be difficult for the clinician to isolate. This is because pain may be referred either from the neck to the shoulder or from the shoulder to the neck. In addition, neck and shoulder pathology frequently coexist creating a treatment dilemma of which should be approached first. There have been multiple review articles devoted to the differentiation of shoulder and neck pain based on history and examination.1-3 However, the relationship is more complex than simply understanding overlapping pain patterns and the formation of a differential diagnosis. Recently, Zhang et al showed that degenerative cervical spine pathology may predispose a patient to rotator cuff tears.4 Furthermore, Gumina et al reported that injury to the shoulder can negatively influence neck alignment.5 Not only must the diagnostician understand the differentiation of shoulder and cervical spine pathology but also that these 2 systems closely interact and cannot be viewed independently.
The purpose of this review was to conduct an in-depth exploration of the current evidence regarding the interplay between shoulder and spine pathology. To our knowledge, a systematic review examining the shoulder and the cervical spine together has not been performed. Key questions for this systematic review were the following:
What are the clinical manifestations of shoulder and cervical spine pain referral patterns?
What clinical findings, specifically the results of examination and diagnostic injections, can help differentiate shoulder pathology from cervical spine pathology?
What is the incidence of concomitant (occurring together) or masquerading (isolated pathology mimicking pathology in another area) shoulder and cervical spine disorders? How should they be treated?
Is there evidence that cervical-based pathology can cause shoulder pathology? Can shoulder pathology cause cervical pathology?
Methods
A systematic review was prepared according to the protocol set forth by the Cochrane Collaboration. In November 2017, an electronic search was performed on the Scopus, Cochrane Library, and PubMed databases to identify studies in the English language that contained the following combination of search terms: {“cervical spine” AND “shoulder pathology”}, {“cervical spine” AND “rotator cuff”}, {“cervical spine” AND “adhesive capsulitis”}, {“cervical spine” AND “suprascapular neuropathy”}, and {“cervical spine” AND “shoulder impingement”} within the abstract or title.
Two independent reviewers screened titles and abstracts from which full-length texts were selected. Reference lists contained in the selected texts were also reviewed for possible sources. In addition, major journals were hand searched for recent publications that might not have been included in the initial search.
Studies were included based on the following criteria: (1) described pain referral patterns from various shoulder and spine conditions, (2) explored the use of history and examination to differentiate shoulder from neck pathology, (3) described the coexistence of shoulder and spine problems and optimal treatments strategies for concomitant/masquerading pathology, (4) examined the causative relationship between cervical spine and shoulder pathology.
Studies were excluded when they were (1) focused primarily on isolated pathology to either the shoulder or the spine, (2) review articles, or (3) were not in the English language. An additional section consisting of the basic science of pain transmission and sensory innervation anatomy of the neck was added for completeness and was not part of the original search algorithm. To assess for bias, each study was assigned a Methodological Index for Non-Randomized Studies (MINORS) score.6 Studies were considered to have low bias if their score was greater than 16 for non–comparative studies and 24 for comparative studies. To assess the level of evidence, each study was assigned an Oxford Center for Evidence Based Medicine (OCEBM) score from which grades for recommendations were made.7
Results
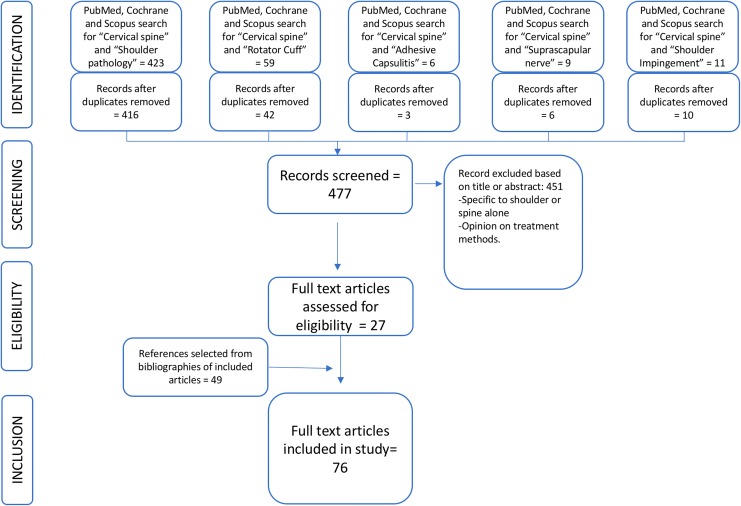
Four hundred seventy-seven references were included for screening after duplicates were removed. Of these articles, 27 were selected for full text review and ultimately included in this study. Based on the broad nature of the topic, a large number of references (49) were also selected for inclusion based on close examination of the bibliographies of the original 27 articles. A flow chart is shown in Figure 1.
Figure 1.
Search strategy and results.
Forty-three clinical articles were graded using the MINORS and OCEBM scores. For the section on pain referral patterns, the average OCEBM score was 2, correlating with a level B recommendation. The MINORS score ranged from 7 to 14, indicating high bias. For the section on clinical assessment of shoulder and spine pathology, the average OCEBM score was 2.5, correlating with a level B recommendation. There was one study with low bias with a MINOR score of 24 by Wainner et al.8 The remainder of the studies were classified as high bias (range 1-21). For the section on concomitant and masquerading neck and shoulder pathology, the average OCEBM score was 3.9, consistent with a level C recommendation. The risk for bias was high in these studies (MINORS score range 1-23). Finally, the average OCEBM score for the section on causative neck and shoulder pathology was 2.8, correlating with a level B recommendation. There were 2 studies with a low risk of bias: Gumina et al5 and Yamamoto et al.9 The remainder of the studies were high bias (MINORS score range 4-21). See Table 1.
Table 1.
Summary of Included Studies with Evidence Grades.
| Author and Year | Study Design (Number of Patients) | Conclusion | OCEBM Score | MINORS Score |
|---|---|---|---|---|
| Pain referral patterns | ||||
| Feinstein et al (1954) | Prospective cohort study (5) | Injection of hypertonic saline into the paravertebral soft tissue at C3-6 produced referred pain to the shoulder. | 1 | 12 |
| Dwyer et al (1990) | Prospective cohort study (5) | Injection of contrast medium into the facet joints (C4-7) caused referred pain to the shoulder. | 1 | 14 |
| Grubb (2000) | Case series (173) | A review of results of a series of cervical discograms showed characteristic pain referred to the shoulder from C4-7. | 4 | 7 |
| Tanaka (2006) | Prospective cohort study (50) | Compression of cervical nerve roots can cause scapular pain particularly at C5-6. | 1 | 14 |
| Gerber (1998) | Prospective cohort study (19) | Hypertonic saline injected into the AC joint that caused referred pain to the lateral neck. | 1 | 13 |
| Gorski (2003) | Case series (34) | Patients with shoulder impingement had relief of neck pain after subacromial injection. | 4 | 8 |
| Clinical assessment | ||||
| Austin (2015) | Case series (54) | Sleep disturbance/pain reported in 86% of patients with rotator cuff tear. After repair only 34% continued to have sleep disturbance/pain. | 4 | 10 |
| Henderson (1983) | Case series (736) | Only 0.6% patients with cervical radiculopathy did not have an instance of arm pain. | 4 | 1 |
| Wainner (2003) | Blinded prospective diagnostic test (82) | Absence of biceps muscle stretch reflex has a sensitivity of 94% for cervical radiculopathy. | 1 | 24 |
| Aktas (2015) | Case report (1) | Lateral pectoral nerve entrapment mimicking C6 radiculopathy. | 4 | 1 |
| Tong (2002) | Cross-sectional study (255) | Spurling’s test has specificity of 93% and sensitivity of 30% for cervical radiculopathy. | 1 | 10 |
| Davidson (1981) | Case series (22) | 15 of 22 patients with cervical radiculopathy had relief of symptoms with abduction of the shoulder. | 4 | 1 |
| Viikari-Juntura (1989) | Case series (43) | The specificity of Spurling’s test, shoulder abduction sign, and the axial manual traction test for radiculopathy were all 100%. However, the sensitivities were low, 28%, 26%, and 31%, respectively. | 4 | 12 |
| Caliş (2000) | Prospective cohort study (120) | Compared patients with impingement to patients without impingement. The tests with the highest specificity were the drop arm test (97.2%) and the painful arc test (80.5). | 2 | 17 |
| Gumina (2013) | Prospective cohort study (1567) | Compared patient with cervical radiculopathy to healthy controls. The arm squeeze test had a specificity of 91% and a sensitivity of 96%. | 1 | 21 |
| Costandi (2015) | Retrospective case series (64) | 92% of patients who reported >50% pain relief after cervical transforaminal epidural steroid injection benefited from cervical surgery. | 4 | 10 |
| Anderberg (2006) | Prospective cohort study (30) | 18 of 22 patients with positive cervical transforaminal epidural steroid injection had good/excellent results with either ACDF or formal series of injections. | 1 | 14 |
| Lim (2005) | Prospective cohort study (101) | Patients with positive diagnostic subacromial injection had better improvement following subacromial decompression compared to those with a negative result. | 1 | 18 |
| Oh (2010) | Prospective cohort study (153) | Positive modified impingement test was associated with significant improvement following rotator cuff repair. | 2 | 13 |
| Concomitant/masquerading shoulder and neck pathology | ||||
| Paul (2007) | Retrospective case-control study (96) | 50% of patient presenting with shoulder pain had MRI abnormality of cervical spine. | 3 | 23 |
| Sembrano (2013) | Case series (694) | 3.6% of patients presenting for shoulder pain will have neck pathology. | 4 | 12 |
| Roberson (2015) | Case series (1169) | 4% of patients with a chief complaint of shoulder pain ended up having isolated cervical radiculopathy. | 4 | 8 |
| Uppal (1995) | Case series (8) | 8 patients with glenoid cysts which presented with symptoms mimicking cervical radiculopathy. | 4 | 1 |
| Pheasant (2016) | Case series (2) | Subacromial impingement resulting from rotator cuff weakness caused by intermittent C5 root compression. | 4 | 1 |
| Cannon (2018) | Case series (191) | The total prevalence of a musculoskeletal disorder is 42% in those undergoing electrodiagnostic studies for suspected cervical radiculopathy. In patients with confirmed radiculopathy it is 29% | 4 | 10 |
| Date (1996) | Case series (33) | 24% of patients with impingement syndrome were positive on EMG/NCS for cervical radiculopathy. | 4 | 10 |
| Hawkins (1988) | Case series (13) | 13 patients treated with anterior cervical decompression and fusion and subacromial decompression. | 4 | 6 |
| Manifold (1999) | Case series (22) | 66% of patients with both rotator cuff tears and confirmed cervical radiculopathy have relief of neck pain. | 4 | 3 |
| Jo (2012) | Case series (96) | 15% cervical spondylosis patients were ultimately diagnosed with shoulder disorders and required treatment. | 4 | 11 |
| Causative neck and shoulder pathology | ||||
| Culham (1993) | Case series (91) | Scapular protraction increased as thoracic kyphosis increased. | 4 | 7 |
| Greenfield (1995) | Case series (60) | Forward head posture was increased in shoulder overuse patient’s vs healthy controls. | 4 | 15 |
| Theisen (2010) | Prospective cohort study (78) | Patients with subacromial outlet syndrome had reduced thoracic motion. | 1 | 21 |
| Kebaetse (1990) | Case series (34) | Thoracic spine position significantly affects scapular kinematics and strength during abduction. | 4 | 14 |
| Yamamoto (2015) | Case series (2015) | Postural abnormality was a significant predictor of asymptomatic and symptomatic rotator cuff tears. | 4 | 24 |
| Kentar (2017) | Ecological study (319) | Kyphotic posture was associated with a high level of rotator cuff tears in wheel chair users. | 4 | 21 |
| Helgadottir (2011) | Prospective cohort study (44) | Symptomatic patients with whiplash had reduced scapular upward rotation compared to healthy controls. | 1 | 19 |
| Gumina (2009) | Prospective cohort study (134) | Type III acromioclavicular joint dislocation predisposes to cervical hyperlordosis when compared to healthy patients. | 1 | 24 |
| Zhang (2015) | Retrospective case-control study (679 112) | The association between cervical spine and rotator cuff pathology is greater than lumbar spine and rotator cuff pathology. | 3 | 9 |
| Ochiai (2017) | Case series (341) | 46% of patients with massive rotator cuff tears have cervical spondylitic amyotrophy | 4 | 4 |
| Campbell (2016) | Case series (24) | Evaluated patients with cervical spinal cord injury. | 4 | 15 |
| Goutallier (1994) | Case series (63) | Fatty atrophy detected in the intact infraspinatus in the face of supraspinatus tears. | 4 | 12 |
| Mallon (2006) | Prospective cohort (8) | 100% of patients with massive rotator cuff tears in this study had evidence of denervation of the supraspinatus muscle. In patients in which repair was performed, there was recovery of the suprascapular nerve. | 1 | 15 |
| Costouros (2007) | Prospective cohort study (26) | 28% of patients with massive rotator cuff repairs had evidence of peripheral nerve injury including suprascapular neuropathy and cervical radiculopathy. | 1 | 9 |
Abbreviations: OCEBM, Oxford Center for Evidence Based Medicine; MINORS, Methodological Index for Nonrandomized Studies; AC, acromioclavicular; ACDF, anterior cervical discectomy and fusion; MRI, magnetic resonance imaging; EMG, electromyography; NCS, nerve conduction studies.
The Basic Science of Shoulder-Spine Pathology
Basic Pain Transmission
The physiology of pain transmission can help in understanding shoulder-spine pain referral patterns. Acute somatic pain transmission occurs via a dual pathway. The “fast” pain pathway is transmitted by myelinated Aδ-fibers and initiated by a mechanical stimulus. The “slow” pain transmission by unmyelinated C-fibers is mediated by chemical signals such as TNF-α (tumor necrosis factor-α) and IL-6 (interleukin-6) released from tissue destruction.10 These first-order fibers terminate in the dorsal root ganglion and are relayed to the brain through second-order neurons of the spinothalamic tract. While Aδ-fibers are excellent at targeted pain perception, C-fibers are carried through the spinal cord via the paleospinothalamamic pathway, which has a diffuse termination in the brain resulting in poor pain localization.11,12 The phenomenon of referred pain occurs when nerve fibers from different locations in the body synapse on the same second-order neurons.11 Pain from the shoulder is relayed through the brachial plexus and into the cervical nerve roots, particularly at the C5-6 level.13 Radicular pain may result from either mechanical compression or inflammation from chemical mediators and thus may be Aδ-fiber and C-fiber mediated and can have a indistinct referral pattern.14
The nervous system not only plays a role in pain but may also contribute to tendon degeneration and inflammation.15,16 An imbalance between vasodilator and vasoconstrictor neurons has been implicated in this pathogenesis.17 Moreover, so-called neuroinflammation may occur where substance-P and calcitonin gene-related peptide, agents responsible for nociception, also cause vasodilation and inflammation resulting in musculotendinous damage.15,18,19
The Anatomy of Neck and Shoulder Pain
The cervical intervertebral disc is innervated by the sinuvertebral nerve, which has both somatic and autonomic input. The autonomic input derives from the vertebral nerve, which is formed from grey rami communicans of the sympathetic trunk and the stellate ganglion, while somatic input comes from the ventral ramus.20 The cervical facets are innervated primarily by the medial branches of the dorsal rami of the cervical vertebral nerve, which contain nociceptive fibers.21-23 The lateral branches of the dorsal rami run superiorly to supply the deep dorsal musculature at a level above (splenius cervicis and longissimus cervicis) and can be involved in referred pain.21
The primary sensory innervation to the shoulder joint is provided by the suprascapular and axillary nerves.13 The course of the suprascapular nerve starts at the superior trunk (C5, C6) of the brachial plexus and travels to the scapular notch running under the transverse scapular ligament. The nerve takes an oblique course across the supraspinatus fossa around the scapular neck and into the infraspinatus fossa. The articular branch supplying sensation to the shoulder joint arises just distal to the transverse scapular ligament in 87% of cases.24 It also provides sensation to the acromioclavicular (AC) joint and subacromial bursa.25 A second sensory branch known as the acromial branch originates just distal to the scapular neck and into the posterior capsule distal to the supraspinatus.24 The inferior capsule of the shoulder is supplied by the axillary nerve, which runs in close proximity to the inferior glenohumeral ligament and gives off branches near the 7 o’clock position of the glenoid rim.26,27 The anterior capsule is innervated by 3 nerves, the lateral pectoral nerve (C5, C6), the subscapular nerve (C5, C6), and the axillary neve.28
Pain Referral Patterns
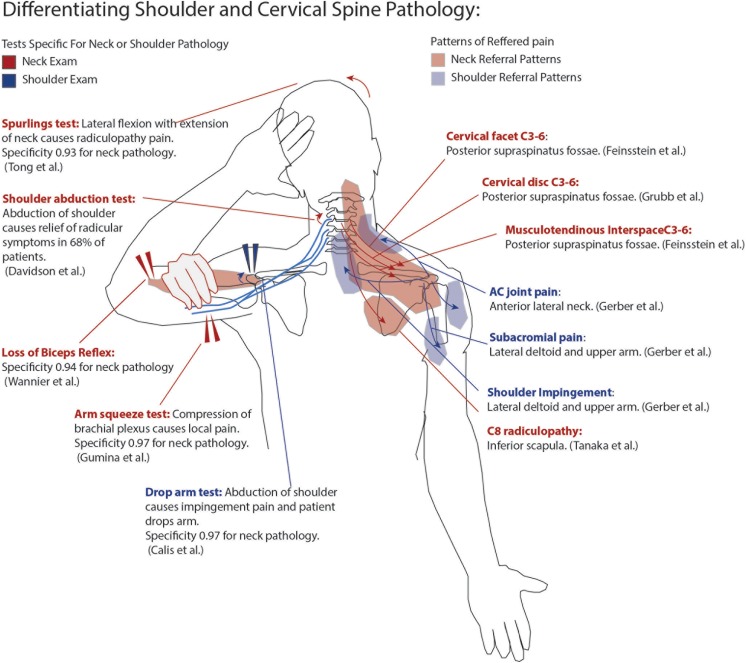
Classic studies have mapped out our understanding of pain referral from the neck to the shoulder. In 1954, Feinstein et al injected volunteers with hypertonic saline at each musculotendinous interspace from C0-1 to the sacrum. They found that stimulation of the paravertebral tissue at C3-6 consistently referred to the shoulder.29 Dwyer et al showed that stimulation of cervical facet joints could produce characteristic posterior shoulder and trapezius pain.30 Moreover, Grubb et al performed cervical discograms demonstrating a similar referral of pain from the discs to the shoulder as that caused by the facet joints.31 Tanaka et al showed that patients with isolated C5 and C6 radiculopathy could have pain referred to the suprascapular shoulder region while C8 nerve root compression can refer to the scapular region.32 Gerber et al demonstrated that AC joint pain stimulation refers to the lateral neck and trapezius while subacromial pain refers to the lateral acromion and deltoid.33 Gorski and Schwartz revealed that referred neck pain from subacromial impingement (in the absence of shoulder pain) could be neutralized with subacromial injections.34
Clinical Assessment
History
There are several key historical factors that may help differentiate shoulder from spine pathology. Timing of symptoms can help differentiate cervical versus shoulder pain. Austin et al reported that approximately 89% of patients with rotator cuff experience nocturnal pain that was relieved by surgical repair in 50% of patients.35 Cervical radiculopathy is most commonly associated with arm pain,36 and arm pain beyond the elbow is the most specific symptom that can differentiate it from a shoulder etiology.8 Finally, peripheral nerve entrapment or injury, such as suprascapular nerve pathology, may mimic both shoulder pathology and cervical radiculopathy.37
In this setting of complex overlapping pain, it may be useful to apply the 3-question framework proposed by Murphy and Hurwitz during patient evaluation.38,39 These questions are as follows: (1) is the pain reflective of a visceral or life-threatening disorder (ie, cancer or cardiac pathology which may refer to the shoulder); (2) where is the origin of the pain (ie, differentiation the character of neuropathic type pain from muscular); (3) what has gone wrong with the person as a whole to allow this problem to develop and persist (ie, assessing other global factors such as posture, repetitive or acute trauma, psychological disorders)?
Examination
Examination of the shoulder is paramount as imaging studies may have false positives in both the cervical and shoulder patient populations.40,41 A description of a complete exam of both the shoulder and cervical spine is beyond the scope of this review. However, the most pertinent aspects of the exam will be discussed in 2 sections. The first describes the basic examination of the shoulder and the cervical spine, while the second describes exam techniques that can be used to differentiate the two.
Conventional Exam
The most critical aspect of the cervical spine exam is the evaluation of the neurologic system supplying the upper extremity. This includes the assessment of strength, sensation, and reflexes of the C5-T1 nerve roots. Manual motor testing is performed on the deltoid (C5), biceps (C6), triceps (C7), abductor pollicis brevis (C8), and dorsal interossei (T1). Strength is graded according to the manual muscle test scale from 0 to 5 (5: antigravity + maximal resistance; 4: antigravity + moderate resistance; 3: antigravity alone; 2: movement with gravity eliminated; 1: trace movement; 0: no movement).8,42 Nonetheless, it is important to note that abduction and biceps strength may be diminished in rotator cuff disease and biceps tendinosis, respectively.43 Sensation to light touch should be tested according to each dermatome (lateral shoulder—C5, thumb—C6, index finger—C7, small finger—C8). Muscle stretch reflexes should be tested bilaterally (Biceps—C5-6, brachioradialis—C5-6, and triceps—C7). Importantly, the examiner must evaluate for signs of myelopathy. This classically manifests with signs of upper motor neuron dysfunction such as hyperreflexia, an inverted radial reflex, and a positive Hoffman’s sign. However, these signs may be absent in up to 21% of patients with myelopathy.44 Ono et al also described the finger escape sign (deficient adduction of the fifth finger with palms facing down) and the grip and release test (patient is unable to grip and release the fingers rapidly), which have a high incidence in spondylotic myelopathy patients and can be used to aid diagnosis.45
There are several common conditions for which the shoulder should be examined. Passive and active motion of the shoulder should be evaluated in forward flexion, abduction, and external rotation to easily rule out motion limiting conditions such as adhesive capsulitis and glenohumeral arthritis. Subacromial impingement occurs when the rotator cuff tendon and subacromial bursa are crushed between the greater tuberosity and the acromial arch during abduction of the shoulder. The most common test used for the diagnosis of impingement is the Hawkins impingement test in which pain occurs when the arm is forward flexed to 90° with maximum internal rotation. However, the Hawkins’s test only has a specificity of 56% and a sensitivity of 80%. SLAP tears (superior labrum anterior to posterior) occur when the superior labrum and biceps anchor are detached from the glenoid. There are many described tests to evaluate for SLAP tears, including the Speed’s, Yergason’s, and Crank tests. Unfortunately, all have a poor sensitivity and specificity.43 Schlechter et al described the passive distraction test for SLAP tears, in which pain is produced when a supine patient forward flexes the arm to 150° and pronates the forearm. They describe a specificity of 80% and a 53% sensitivity.46 The shoulder should also be carefully evaluated for tears of the 4 tendons of the rotator cuff tears, which are common in patients >50 years of age.43 There are many tests to evaluate the rotator cuff; however, a recent review performed by O’Kane and Toresdahl describes 2 tests as having high sensitivity and specificity.43 For the evaluation of subscapularis tears, the belly press test, which is performed by having the patient place their hand on their abdomen, while the examiner moves their elbow forward, is sensitive and specific. The test is considered positive if the patient cannot keep their hand on their abdomen. The infraspinatus and supraspinatus are best evaluated for tears with the external rotation lag sign in which the elbow is flexed to 90° with the shoulder abducted 20° in the scapular plane and maximally externally rotated. The test should be considered positive if the patient is unable to keep the shoulder in external rotation.
Differentiating Exam
Physical examination can help differentiate shoulder from neck pathology although there can be overlap. For identifying a cervical etiology, the absence of biceps muscle stretch reflex is highly specific for cervical radiculopathy.8 Spurling’s test has also been shown to have a high specificity (0.93) for cervical radiculopathy.47 Shoulder abduction plays a key role in the differentiation of shoulder and spine pathology as described above. Davidson et al showed that 68% of patients with cervical radiculopathy had relief with abduction of the arm, which elevates the dorsal root ganglion away from osteophytes and varicosities causing compression.48 In addition, Viikari-Juntura et al showed that Spurling’s test and the shoulder abduction test were both specific for cervical radiculopathy but were not sensitive.49 Caliş et al showed that shoulder abduction pain was highly specific for subacromial impingement, with a drop arm test having a specificity of 0.97 and a painful arc test having a specificity of 0.80.50 Gumina et al proposed the “arm squeeze test,” which hypothesizes that compression of brachial plexus nerves affected by radiculopathy in the middle arm results in increased pain compared with various shoulder pathologies. They showed a 0.96 sensitivity and 0.90 specificity using this test for the detection of cervical radiculopathy.51 A summary of pain referral patterns and differentiating exam findings may be found in Figure 2.
Figure 2.
Pain referral patterns for the shoulder and neck and using examination to differentiate shoulder from neck pathology.
Role of Diagnostic Injections
Diagnostic injections with nerve block agents may be used to differentiate the predominant source of pain as originating from the shoulder or the spine and can be used to help guide surgical treatment.34,52 In a retrospective study, Costandi et al showed that 92% of patients with cervical radiculopathy who experienced pain improvement of >50% with a cervical transforaminal epidural injection (10 mg dexamethasone and 1 mL of 0.5% bupiviacaine) had successful outcomes with cervical decompression surgery.53 Moreover, Anderberg et al reported that 18 of 22 patients with a positive selective transforaminal cervical nerve block (0.5 mL of 1% mepivacaine) had successful treatment at that level with either ACDF (anterior cervical discectomy and fusion) surgery or a formal series of transforaminal steroid injections.54 While cervical injections are generally low risk, complications have been reported and must be considered while counseling patients.55
Similarly, diagnostic injections about the shoulder can be used to predict the success of shoulder surgery.56 Lim et at noted that patients who experienced relief with subacromial local anesthetic had better improvement in constant scores following subacromial decompression compared with those who did not have relief.57 Moreover, Oh et al reported that pain relief with subacromial injection with 8 mL of 1% lidocaine significantly correlated with good outcomes from repair of full-thickness rotator cuff tears.58 Finally, AC joint and bicipital tunnel injections may also be used to confirm pain originating from these areas.56
Diagnostic injections are still invasive procedures with risks. Thus, we suggest that injections be used in cases with equivocal history and exam findings. These injections may either be cervical transforaminal injections to help confirm cervical radiculopathy or injections into the subacromial space to confirm shoulder pathology.
Concomitant/Masquerading Shoulder and Neck Pathology
Shoulder and cervical spine problems may be easily confused for one another and frequently overlap. The overall prevalence of cervical pathology in patients presenting with shoulder pain is high (50%).59 In a large series, 1 of 25 (4%) patients who attended a shoulder or spine clinic for respective shoulder or neck pain were found to have mistaken or overlapping pathology and required the opposite clinic’s service.60 In a similar series, Roberson et al showed again that roughly 4% of patients presenting to a tertiary shoulder referral center for shoulder pain had isolated cervical radiculitis.61 Shoulder problems may also masquerade as radiculopathy. Uppal et al reported on 8 patients who presented for evaluation of cervical radiculopathy who were ultimately diagnosed with cysts of the glenoid labrum.62 All patients presented with vague neck pain but had a positive impingement sign and had relief with intraarticular lidocaine injection. In addition, Pheasant et al published 2 cases of shoulder impingement caused by weakness of the rotator cuff from cervical radiculopathy.63
Tests such as electromyography and nerve conduction studies (EMG-NCS) can help differentiate these entities. In a prospective study, Cannon et al showed that 29% of those who underwent an EMG-NCS for cervical radiculopathy were also positive for a musculoskeletal disorder with shoulder impingement occurring at a rate of 10%.64 In another study examining the EMG-NCS findings in patients with “impingement syndrome,” Date and Gray found that 24% had evidence of a possible cervical radiculopathy and 5.3% had evidence of a C5/6 radiculopathy.65 Three patients of 60 eventually required ACDF (6% of cervical radiculitis cohort).61
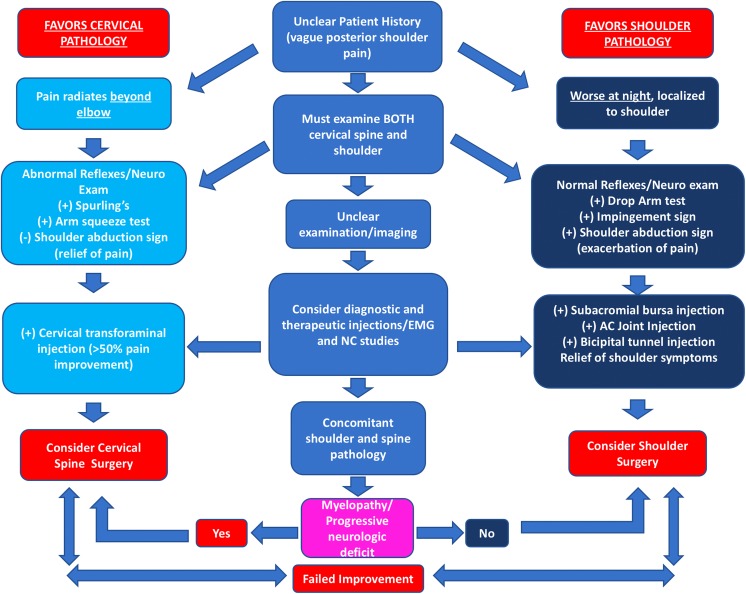
The order of treatment of concomitant shoulder and cervical spine pathology can be difficult to determine, since which pathology should take precedence is not well understood. In a case series of 13 patients with concomitant neck and shoulder pathology, operating on the shoulder first caused resolution of neck pain in 6 patients. In 7 patients who had ACDF operations performed first, all eventually went on to require shoulder surgery in the form of subacromial decompression and/or rotator cuff repair.52 Nonetheless this study was subject to bias as treatments were guided on an individual basis and not standardized. In a separate study, Manifold and McCann showed substantial improvement in both neck and shoulder pain after subacromial decompression and rotator cuff repair in 66% of patients with concomitant shoulder pathology and cervical radiculopathy.66 Again this study suffered from methodological flaws failing to precisely define the cervical spine pathology that was treated. In a series of 96 patients with a diagnosis of cervical spondylosis based on radiographic exam with neck and shoulder pain, it was determined that 15 of the patients’ pain was caused by unrecognized shoulder pathology, which did not resolve with surgical treatment of the neck. In this study, there was a significant difference in the cervical levels involved, with the shoulder cohort having a higher involvement of the C4-5 level (37%) than the C5-6 level (15) (P = .03).67 This result is interesting considering that the most common level for cervical spondylosis is typically C5-C6.68 It should be noted that the studies which examine the treatment of concomitant shoulder and spine pathology are dated, observational, and subject to both bias and diagnostic flaws and thus must be interpreted with care. However, in patients with both shoulder and cervical spine pathology where the origin of pain is unclear despite exhaustive tests, it is reasonable to start with the shoulder. The authors of this study agree with Hawkins and Manifold in that shoulder surgery is typically associated with less risk to the patient and thus may be attempted first. One caveat to this rule is that should the patient exhibit any signs or symptoms of myelopathy (gait, bowel or bladder disturbance, positive Hoffman’s, or hyperreflexia suggesting upper motor neuron lesion) or a progressive motor deficit cervical spine surgery should be prioritized to decompress the spinal canal and prevent further neurologic deteroriation.69 For our suggested treatment algorithm, see Figure 3.
Figure 3.
Algorithm for diagnosis and treatment of shoulder and spine pathology.
Causative Shoulder and Neck Pathology
Spino-Scapular Alignment
The spine and shoulder have an integral biomechanical relationship based on muscular attachments connecting the shoulder girdle to the spine.70,71 These muscular connections consist of the trapezius, levator scapulae, cervical extensors, and flexors. Activation imbalance between these muscle groups can result in neck pain.72,73
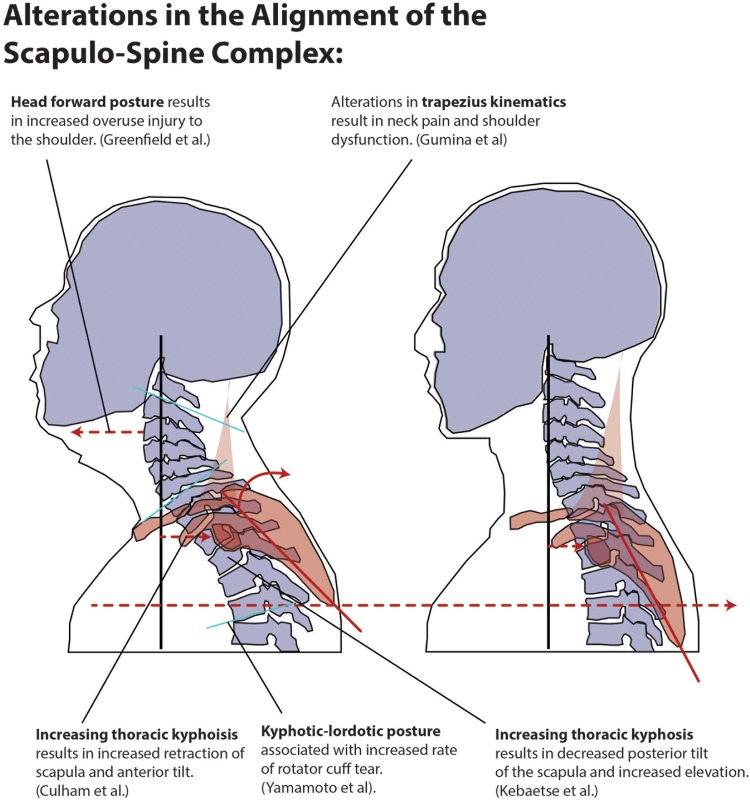
Spinal malalignment specifically in the thoracic region seems to negatively impact the shoulder. Culham and Peat showed that altered cervical and thoracic sagittal alignment changes the kinematics and resting posture of the scapula.74 They reported that with increasing thoracic kyphosis that occurs with aging there is increased anterior tilt and retraction of the scapula.74 Greenfield et al reported that patients with overuse injury to the shoulder were more likely to have a head forward posture that correlates with increasing thoracic kyphosis.75 Theisen et al, in a cohort study comparing patients with subacromial outlet syndrome to healthy subjects showed reduced segmental mobility of the thoracic spine (particularly T5-12) and suggested this may be a contributing factor to the development of outlet impingement syndrome.76 Finally, Kebaetse et al reported that increasing thoracic kyphosis (slouched posture) resulted in altered scapular kinematics, namely, loss of lateral rotation and posterior tilt with abduction and superior translation with abduction. They also reported a decrease in arm abduction strength in this position.70
Muscular forces across the shoulder are altered by changes in spinal alignment. Spinal posture has been shown to affect the rate of rotator cuff tears.9 In the same vein, poor trunk control is linked to rotator cuff pathology.77 Scapular retraction and elevation are reduced in patients with insidious onset neck pain and whiplash-associated disorder, which may result from diminished function of the trapezius.78 Gumina et al reported increased cervical kyphosis and Northwick Park neck pain questionnaire scores in patients with chronic type 3 AC joint dislocations. They hypothesized that this was related to a disturbance in the tensioning of the trapezius.5 In summary, malalignment of the scapula-spine complex alters the kinematics of the trapezius, dysfunction of which has been implicated in the development of impingement syndrome.71,79 These changes are outlined in Figure 4.
Figure 4.
Summary of scapula-spine pathologic changes.
Rotator Cuff Tears
The etiology of rotator cuff tears is poorly understood; however, there is growing evidence that neurologic dysfunction at least plays a partial role. The rotator cuff has been shown to become stiff and inflexible as well as have a decreased force needed to tear in paralysis rodent model proximal to the suprascapular nerve.80 Zhang et al, in a nationwide retrospective review of the Pearldiver database, showed a significant association of rotator cuff tears in patients with cervical spine pathology compared to lumbar spine controls. Not surprisingly, this association increased with the age of the patient, with 25% of patients greater than 60 years of age also having concomitant rotator cuff tears.4 In a large series of massive rotator cuff tears, Ochiai et al showed that 46% coexisted with cervical spondylolytic amotrophy.81 It may be the case that fatty degenerative change resulting from neuropathic lesions preexist tears, rather than result from them.80,82
Animal models have shown that tendon tears and retraction can result in fatty denervation identical to neurological injury.83 Theoretically, neurologic injury results in weakening and decreased amounts of collagen in the rotator cuff.84 Loss of dynamic stabilization due to muscle imbalance in tetraplegic patients with cervical spinal cord injuries has been shown to result in rotator cuff pathology.85-87 Rotator cuff tears are also very prevalent in paraplegic spinal cord patients (as high as 63% vs 15% compared to controls), which may be due to higher reliance on the shoulder for mobilization.88
Goutallier et al noted in their study of 63 patients undergoing repair of rotator cuff tears that muscular atrophy occurred in intact infraspinatus muscles in the face of isolated tears of the supraspinatus.89 Several studies have shown rotator cuff tears can be associated with suprascapular neuropathy, possibly secondary to a significant tethering of the nerve when the supraspinatus retracts.90,91 Moreover, massive rotator cuff tears can have a high prevalence of peripheral nerve injury (28%), including upper trunk brachial plexopathy, suprascapular neuropathy, and cervical radiculopathy. When the rotator cuff is repaired, suprascapular neuropathy tends to resolve, possibly due to a reversal of anatomic derangements.92 The so-called “Double Crush” phenomenon where a C5 radiculopathy predisposed the suprascapular nerve to further injury at the suprascapular notch has been reported sparsely in the literature.93
Overall, little has been written regarding the synergistic effect of shoulder and spine pathology. What has been written is subject to high bias. This review represents an exhaustive collection of relevant articles on the relationship between spinal alignment and denervation via radiculopathy or myelopathy on chronic shoulder problems. However, the selection of articles yielded by this search was small, and consisted mostly retrospective observational evidence (level 4). This is an area in shoulder and spine surgery that would benefit from more focused prospective research. Can we improve shoulder pain by correcting spinal deformity and decompressing the cervical nerve roots? Is it possible for neck pain to be resolved by surgical repair of the rotator cuff or treatment of other shoulder pathology? These questions remain incompletely answered at the current time.
Conclusion
There is considerable overlap between shoulder and spine pain referral patterns. Injury to the nerve, disc, facet complex, or paravertebral soft tissues from C3-7 can refer pain to the posterior shoulder. Moreover, irritation of the AC joint or subacromial space can refer pain to the lateral neck.
History and physical examination can be used to differentiate cervical and shoulder pathology. Rotator cuff pain tends to be more pronounced at night while radicular cervical pain tends to radiate into the arm. Shoulder abduction tends to relieve cervical radicular pain while exacerbating shoulder pain. Spurling’s test and the arm squeeze test can be used to confirm cervical radiculopathy. The drop arm test is highly specific for impingement.
In cases with equivocal history and examination, diagnostic injections can be used to isolate sources of pain and to predict the outcome of both shoulder and spine surgery. Relief of pain following transforaminal epidural injections can help confirm radiculopathy. Subacromial injections help confirm impingement and rotator cuff tears.
Shoulder and cervical spine pathology may coexist creating a treatment dilemma. In patients with concomitant neck and shoulder pathology, treatment of the shoulder before the spine is reasonable as cervical surgery carries higher risks.
Alterations in the alignment of the spine changes the mechanics of the shoulder and can increase the incidence of shoulder dysfunction. In a similar fashion, shoulder injury may also alter the mechanics of the cervical spine resulting in neck pain.
Neurologic disorders of the cervical spine likely predispose the rotator cuff to injury.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Yoshihiro Katsuura, MD  https://orcid.org/0000-0001-7886-4720
https://orcid.org/0000-0001-7886-4720
References
- 1. Bokshan SL, DePasse JM, Eltorai AE, Paxton ES, Green A, Daniels AH. An evidence-based approach to differentiating the cause of shoulder and cervical spine pain. Am J Med. 2016;129:913–918. doi:10.1016/j.amjmed.2016.04.023 [DOI] [PubMed] [Google Scholar]
- 2. Throckmorton TQ, Kraemer P, Kuhn JE, Sasso RC. Differentiating cervical spine and shoulder pathology: common disorders and key points of evaluation and treatment. Instr Course Lect. 2014;63:401–408. [PubMed] [Google Scholar]
- 3. Wilson C. Rotator cuff versus cervical spine: making the diagnosis. Nurse Pract. 2005;30:44–46, 48–50. [DOI] [PubMed] [Google Scholar]
- 4. Zhang AL, Theologis AA, Tay B, Feeley BT. The association between cervical spine pathology and rotator cuff dysfunction. J Spinal Disord Tech. 2015;28:E206–E211. [DOI] [PubMed] [Google Scholar]
- 5. Gumina S, Carbone S, Arceri V, Rita A, Vestri AR, Postacchini F. The relationship between chronic type III acromioclavicular joint dislocation and cervical spine pain. BMC Musculoskelet Disord. 2009;10:157 doi:10.1186/1471-2474-10-157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. [DOI] [PubMed] [Google Scholar]
- 7. Center for Evidence Based Medicine. Oxford Centre for Evidence-Based Medicine—levels of evidence (March 2009). https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/ . Published June 11, 2009. Accessed November 21, 2018.
- 8. Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine (Phila Pa 1976). 2003;28:52–62. [DOI] [PubMed] [Google Scholar]
- 9. Yamamoto A, Takagishi K, Kobayashi T, et al. The impact of faulty posture on rotator cuff tears with and without symptoms. J Shoulder Elbow Surg. 2015;24:446–452. doi:10.1016/j.jse.2014.07.012 [DOI] [PubMed] [Google Scholar]
- 10. Myers RR, Campana WM, Shubayev VI. The role of neuroinflammation in neuropathic pain: mechanisms and therapeutic targets. Drug Discov Today. 2006;11:8–20. doi:10.1016/S1359-6446(05)03637-8 [DOI] [PubMed] [Google Scholar]
- 11. Guyton AC, Hall JE. Textbook of Medical Physiology. 11th ed Philadelphia, PA: Elsevier Saunders; 2006. [Google Scholar]
- 12. Stein C, Kopf A. Anesthesia and treatment of chronic pain. In: Miller RD, Cohen NH, Eriksson LI, Fleisher LA, WienerKronish JP, Young WL, eds. Miller’s Anesthesia. 8th ed Philadelphia, PA: Elsevier/Saunders; 2015:1898–1918.e5. [Google Scholar]
- 13. Ritchie ED, Tong D, Chung F, Norris AM, Miniaci A, Vairavanathan SD. Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: a new modality? Anesth Analg. 1997;84:1306–1312. [DOI] [PubMed] [Google Scholar]
- 14. Abrams B. Patterns of common pain syndromes In: Waldman SD, ed. Pain Management. Philadelphia, PA: Saunders; 2011. [Google Scholar]
- 15. Ackermann PW, Finn A, Ahmed M. Sensory neuropeptidergic pattern in tendon, ligament and joint capsule. A study in the rat. Neuroreport. 1999;10:2055–2060. [DOI] [PubMed] [Google Scholar]
- 16. Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow). Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Boint Joint Surg. 1999;81:259–278. [PubMed] [Google Scholar]
- 17. Ljung BO, Forsgren S, Fridén J. Sympathetic and sensory innervations are heterogeneously distributed in relation to the blood vessels at the extensor carpi radialis brevis muscle origin of man. Cells Tissues Organs. 1999;165:45–54. doi:10.1159/000016673 [DOI] [PubMed] [Google Scholar]
- 18. Berczi I, Chalmers IM, Nagy E, Warrington RJ. The immune effects of neuropeptides. Baillieres Clin Rheumatol. 1996;10:227–257. [DOI] [PubMed] [Google Scholar]
- 19. Brain SD, Williams TJ, Tippins JR, Morris HR, MacIntyre I. Calcitonin gene-related peptide is a potent vasodilator. Nature. 1985;313:54–56. [DOI] [PubMed] [Google Scholar]
- 20. Bogduk N, Windsor M, Inglis A. The innervation of the cervical intervertebral discs. Spine (Phila Pa 1976). 1988;13:2–8. [DOI] [PubMed] [Google Scholar]
- 21. Bogduk N. The clinical anatomy of the cervical dorsal rami. Spine (Phila Pa 1976). 1982;7:319–330. [DOI] [PubMed] [Google Scholar]
- 22. Kallakuri S, Li Y, Chen C, Cavanaugh JM. Innervation of cervical ventral facet joint capsule: histological evidence. World J Orthop. 2012;3:10–14. doi:10.5312/wjo.v3.i2.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kallakuri S, Singh A, Chen C, Cavanaugh JM. Demonstration of substance P, calcitonin gene-related peptide, and protein gene product 9.5 containing nerve fibers in human cervical facet joint capsules. Spine (Phila Pa 1976). 2004;29:1182–1186. [DOI] [PubMed] [Google Scholar]
- 24. Vorster W, Lange CP, Briët RJ, et al. The sensory branch distribution of the suprascapular nerve: an anatomic study. J Shoulder Elbow Surg. 2008;17:500–502. doi:10.1016/j.jse.2007.10.008 [DOI] [PubMed] [Google Scholar]
- 25. Nam YS, Jeong JJ, Han SH, et al. An anatomic and clinical study of the suprascapular and axillary nerve blocks for shoulder arthroscopy. J Shoulder Elbow Surg. 2011;20:1061–1068. doi:10.1016/j.jse.2011.04.022 [DOI] [PubMed] [Google Scholar]
- 26. Ball CM, Steger T, Galatz LM, Yamaguchi K. The posterior branch of the axillary nerve: an anatomic study. J Bone Joint Surg Am. 2003;85-A:1497–1501. [DOI] [PubMed] [Google Scholar]
- 27. Gelber PE, Reina F, Monllau JC, Yema P, Rodriguez A, Caceres E. Innervation patterns of the inferior glenohumeral ligament: anatomical and biomechanical relevance. Clin Anat. 2006;19:304–311. doi:10.1002/ca.20172 [DOI] [PubMed] [Google Scholar]
- 28. Aszmann OC, Dellon AL, Birely BT, McFarland EG. Innervation of the human shoulder joint and its implications for surgery. Clin Orthop Relat Res. 1996;(330):202–207. [DOI] [PubMed] [Google Scholar]
- 29. Feinstein B, Langton JN, Jameson RM, Schiller F. Experiments on pain referred from deep somatic tissues. J Bone Joint Surg Am. 1954;36-A:981–997. [PubMed] [Google Scholar]
- 30. Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: a study in normal volunteers. Spine (Phila Pa 1976). 1990;15:453–457. [DOI] [PubMed] [Google Scholar]
- 31. Grubb SA, Kelly CK, Bgoduk N. Cervical discography: clinical implications from 12 years of experience. Spine (Phila Pa 1976). 2000;25:1382–1389. [DOI] [PubMed] [Google Scholar]
- 32. Tanaka Y, Kokubun S, Sato T, Ozawa H. Cervical roots as origin of pain in the neck or scapular regions. Spine (Phila Pa 1976). 2006;31:E568–E573. doi:10.1097/01.brs.0000229261.02816.48 [DOI] [PubMed] [Google Scholar]
- 33. Gerber C, Galantay RV, Hersche O. The pattern of pain produced by irritation of the acromioclavicular joint and the subacromial space. J Shoulder Elbow Surg. 1998;7:352–355. [DOI] [PubMed] [Google Scholar]
- 34. Gorski JM, Schwartz LH. Shoulder impingement presenting as neck pain. J Bone Joint Surg Am. 2003;85A:635–638. [DOI] [PubMed] [Google Scholar]
- 35. Austin L, Pepe M, Tucker B, et al. Sleep disturbance associated with rotator cuff tear: correction with arthroscopic rotator cuff repair. Am J Sports Med. 2015;43:1455–1459. doi:10.1177/0363546515572769 [DOI] [PubMed] [Google Scholar]
- 36. Henderson CM, Hennessy RG, Shuey HM, Jr, Shackelford EG. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: a review of 846 consecutively operated cases. Neurosurgery. 1983;13:504–512. doi:10.1227/00006123-198311000-00004 [DOI] [PubMed] [Google Scholar]
- 37. Aktas I, Palamar D, Akgun K. Lateral pectoral nerve injury mimicking cervical radiculopathy. Clin J Sport Med. 2015;25:e64–e66. [DOI] [PubMed] [Google Scholar]
- 38. Murphy DR, Hurwitz EL. A theoretical model for the development of a diagnosis-based clinical decision rule for the management of patients with spinal pain. BMC Musculoskelet Disord. 2007;8:75 doi:10.1186/1471-2474-8-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Slaven EJ, Mathers J. Differential diagnosis of shoulder and cervical pain: a case report. J Man Manip Ther. 2010;18:191–196. doi:10.1179/106698110X12804993426884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Okada E, Matsumoto M, Ichihara D, et al. Aging of the cervical spine in healthy volunteers: a 10-year longitudinal magnetic resonance imaging study. Spine (Phila Pa 1976). 2009;34:706–712. [DOI] [PubMed] [Google Scholar]
- 41. Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10–15. [DOI] [PubMed] [Google Scholar]
- 42. Rao R. Neck pain, cervical radiculopathy, and cervical myelopathy: pathophysiology, natural history, and clinical evaluation. J Bone Joint Surg Am. 2002;84:1872–1881. [DOI] [PubMed] [Google Scholar]
- 43. O’Kane JW, Toresdahl BG. The evidenced-based shoulder evaluation. Curr Sports Med Rep. 2014;13:307–313. doi:10.1249/JSR.0000000000000090 [DOI] [PubMed] [Google Scholar]
- 44. Rhee JM, Heflin JA, Hamasaki T, Freedman B. Prevalence of physical signs in cervical myelopathy: a prospective, controlled study. Spine (Phila Pa 1976). 2009;34:890–895. [DOI] [PubMed] [Google Scholar]
- 45. Ono K, Ebara S, Fuji T, Yonenobu K, Fujiwara K, Yamashita K. Myelopathy hand. New clinical signs of cervical cord damage. J Bone Joint J. 1987;69:215–219. [DOI] [PubMed] [Google Scholar]
- 46. Schlechter JA, Summa S, Rubin BD. The passive distraction test: a new diagnostic aid for clinically significant superior labral pathology. Arthroscopy. 2009;25:1374–1379. doi:10.1016/j.arthro.2009.04.070 [DOI] [PubMed] [Google Scholar]
- 47. Tong HC, Haig AJ, Yamakawa K. The Spurling test and cervical radiculopathy. Spine (Phila Pa 1976). 2002;27:156–159. [DOI] [PubMed] [Google Scholar]
- 48. Davidson RI, Dunn EJ, Metzmaker JN. The shoulder abduction test in the diagnosis of radicular pain in cervical extradural compressive monoradiculopathies. Spine (Phila Pa 1976). 1981;6:441–446. [DOI] [PubMed] [Google Scholar]
- 49. Viikari-Juntura E, Porras M, Laasonen EM. Validity of clinical tests in the diagnosis of root compression in cervical disc disease. Spine (Phila Pa 1976). 1989;14:253–257. [DOI] [PubMed] [Google Scholar]
- 50. Caliş M, Akgün K, Birtane M, Karacan I, Caliş H, Tüzün F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis. 2000;59:44–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gumina S, Carbone S, Albino P, Gurzi M, Postacchini F. Arm squeeze test: a new clinical test to distinguish neck from shoulder pain. Eur Spine J. 2013;22:1558–1563. doi:10.1007/s00586-013-2788-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hawkins RJ, Bilco T, Bonutti P. Cervical spine and shoulder pain. Clin Orthop Relat Res. 1990;(258):142–146. [PubMed] [Google Scholar]
- 53. Costandi SJ, Azer G, Eshraghi Y, et al. Cervical transforaminal epidural steroid injections: diagnostic and therapeutic value. Reg Anesth Pain Med. 2015;40:674–680. doi:10.1097/AAP.0000000000000323 [DOI] [PubMed] [Google Scholar]
- 54. Anderberg L, Annertz M, Rydholm U, Brandt L, Säveland H. Selective diagnostic nerve root block for the evaluation of radicular pain in the multilevel degenerated cervical spine. Eur Spine J. 2006;15:794–801. doi:10.1007/s00586-005-0931-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Manchikanti L, Singh V, Boswell MV. Cervical radiculopathy In: Waldman SD, ed. Pain Management. 2nd ed Philadelphia, PA: Elsevier/Saunders; 2011:522–528. [Google Scholar]
- 56. McFarland E, Bernard J, Dein E, Johnson A. Diagnostic injections about the shoulder. J Am Acad Orthop Surg. 2017;25:799–807. doi:10.5435/JAAOS-D-16-00076 [DOI] [PubMed] [Google Scholar]
- 57. Lim JT, Acornley A, Dodenhoff RM. Recovery after arthroscopic subacromial decompression: prognostic value of the subacromial injection test. Arthroscopy. 2005;21:680–683. doi:10.1016/j.arthro.2005.03.015 [DOI] [PubMed] [Google Scholar]
- 58. Oh JH, Kim SH, Kim KH, Oh CH, Gong HS. Modified impingement test can predict the level of pain reduction after rotator cuff repair. Am J Sports Med. 2010;38:1383–1388. doi:10.1177/0363546509359071 [DOI] [PubMed] [Google Scholar]
- 59. Paul A, Lewis M, Saklatvala J, et al. Cervical spine magnetic resonance imaging in primary care consulters with shoulder pain: a case control study. Ann Rheum Dis. 2007;66:1363–1368. doi:10.1136/ard.2006.064881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sembrano JN, Yson SC, Kanu OC, et al. Neck-shoulder crossover: how often do neck and shoulder pathology masquerade as each other? Am J Orthop (Belle Mead NJ). 2013;42:E76–E80. [PubMed] [Google Scholar]
- 61. Roberson TA, Jew NB, Azar FM, Mauck BM, Dockery JD, Throckmorton TW. Cervical radiculitis presenting as shoulder pain: frequency and results of multidisciplinary care. Curr Orthop Pract. 2015;26:521–525. [Google Scholar]
- 62. Uppal GS, Uppal JA, Dwyer AP. Glenoid cysts mimicking cervical radiculopathy. Spine (Phila Pa 1976). 1995;20:2257–2260. [DOI] [PubMed] [Google Scholar]
- 63. Pheasant S. Cervical contribution to functional shoulder impingement: two case reports. Int J Sports Phys Ther. 2016;11:980–991. [PMC free article] [PubMed] [Google Scholar]
- 64. Cannon DE, Dillingham TR, Miao H, Andary MT, Pezzin LE. Musculoskeletal disorders in referrals for suspected cervical radiculopathy. Arch Phys Med Rehabil. 2007;88:1256–1259. doi:10.1016/j.apmr.2007.07.010 [DOI] [PubMed] [Google Scholar]
- 65. Date ES, Gray LA. Electrodiagnostic evidence for cervical radiculopathy and suprascapular neuropathy in shoulder pain. Electromyogr Clin Neurophysiol. 1996;36:333–339. [PubMed] [Google Scholar]
- 66. Manifold SG, McCann PD. Cervical radiculitis and shoulder disorders. Clin Orthop Relat Res. 1999;(368):105–113. [PubMed] [Google Scholar]
- 67. Jo HJ, Shin MH, Hur JW, Kim JS, Ryu KS, Park CK. Unrecognized shoulder disorders in treatment of cervical spondylosis presenting neck and shoulder pain. Korean J Spine. 2012;9:223–226. doi:10.14245/kjs.2012.9.3.223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine (Phila Pa 1976). 2001;26:2463–2466. [DOI] [PubMed] [Google Scholar]
- 69. Fehlings MG, Wilson JR, Kopjar B, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J Bone Joint Surg Am. 2013;95:1651–1658. doi:10.2106/JBJS.L.00589 [DOI] [PubMed] [Google Scholar]
- 70. Kebaetse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80:945–950. [DOI] [PubMed] [Google Scholar]
- 71. Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39:90–104. doi:10.2519/jospt.2009.2808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Falla D, Bilenkij G, Jull G. Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine (Phlia Pa 1976). 2004;29:1436–1440. [DOI] [PubMed] [Google Scholar]
- 73. Johnston V, Jull G, Souvlis T, Jimmieson NL. Neck movement and muscle activity characteristics in female office workers with neck pain. Spine (Phila Pa 1976). 2008;33:555–563. [DOI] [PubMed] [Google Scholar]
- 74. Culham E, Peat M. Functional anatomy of the shoulder complex. J Orthop Sports Phys Ther. 1993;18:342–350. doi:10.2519/jospt.1993.18.1.342 [DOI] [PubMed] [Google Scholar]
- 75. Greenfield B, Catlin PA, Coats PW, Green E, McDonald JJ, North C. Posture in patients with shoulder overuse injuries and healthy individuals. J Orthop Sports Phys Ther. 1995;21:287–295. doi:10.2519/jospt.1995.21.5.287 [DOI] [PubMed] [Google Scholar]
- 76. Theisen C, van Wagensveld A, Timmesfeld N, et al. Co-occurrence of outlet impingement syndrome of the shoulder and restricted range of motion in the thoracic spine—a prospective study with ultrasound-based motion analysis. BMC Musculoskelet Disord. 2010;11:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Kentar Y, Brunner M, Bruckner T, et al. Impact of spine alignment on the rotator cuff in long-term wheelchair users. J Shoulder Elbow Surg. 2018;27:1004–1011. doi:10.1016/j.jse.2017.12.002 [DOI] [PubMed] [Google Scholar]
- 78. Helgadottir H, Kristjansson E, Mottram S, Karduna A, Jonsson H., Jr Altered alignment of the shoulder girdle and cervical spine in patients with insidious onset neck pain and whiplash-associated disorder. J Appl Biomech. 2011;27:181–191. [DOI] [PubMed] [Google Scholar]
- 79. Cools AM, Witvrouw EE, Declercq GA, Danneels LA, Cambier DC. Scapular muscle recruitment patterns: trapezius muscle latency with and without impingement symptoms. Am J Sports Med. 2003;31:542–549. [DOI] [PubMed] [Google Scholar]
- 80. Sasaki Y, Ochiai N, Hashimoto E, et al. Relationship between neuropathy proximal to the suprascapular nerve and rotator cuff tear in a rodent model. J Orthop Sci. 2018;23:414–419. doi:10.1016/j.jos.2017.12.005 [DOI] [PubMed] [Google Scholar]
- 81. Ochiai N, Hashimoto E, Sasaki Y, et al. Prevalence of concomitant neuropathy in large to massive rotator cuff tear using needle electromyography. J Shoulder Elbow Surg. 2017;26:e111 doi:10.1016/j.jse.2016.11.023 [Google Scholar]
- 82. Phelps KD, Hamid N. Spontaneous ruptures of the distal biceps and rotator cuff tendons secondary to syringomyelia: a case report. JBJS Case Connect. 2015;5:e115 doi:10.2106/JBJS.CC.N.00239 [DOI] [PubMed] [Google Scholar]
- 83. Rowshan K, Hadley S, Pham K, Caiozzo V, Lee TQ, Gupta R. Development of fatty atrophy after neurologic and rotator cuff injuries in an animal model of rotator cuff pathology. J Bone Joint Surg Am. 2010;92:2270–2278. doi:10.2106/JBJS.I.00812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Vad VB, Southern D, Warren RF, Altchek DW, Dines D. Prevalence of peripheral neurologic injuries in rotator cuff tears with atrophy. J Shoulder Elbow Surg. 2003;12:333–336. doi:10.1016/S1058-2746(03)00040-5 [DOI] [PubMed] [Google Scholar]
- 85. Campbell CC, Koris MJ. Etiologies of shoulder pain in cervical spinal cord injury. Clin Orthop. 1996;(322):140–145. [PubMed] [Google Scholar]
- 86. Dyson-Hudson TA, Kirshblum SC. Shoulder pain in chronic spinal cord injury, part 1: epidemiology, etiology, and pathomechanics. J Spinal Cord Med. 2004;27:4–17. doi:10.1080/10790268.2004.11753724 [DOI] [PubMed] [Google Scholar]
- 87. Silfverskiold J, Waters RL. Shoulder pain and functional disability in spinal cord injury patients. Clin Orthop Relat Res. 1991;(272):141–145. [PubMed] [Google Scholar]
- 88. Akbar M, Balean G, Brunner M, et al. Prevalence of rotator cuff tear in paraplegic patients compared with controls: J Bone Joint Surg Am. 2010;92:23–30. doi:10.2106/JBJS.H.01373 [DOI] [PubMed] [Google Scholar]
- 89. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;(304):78–83. [PubMed] [Google Scholar]
- 90. Albritton MJ, Graham RD, Richards RS2nd, Basamania CJ. An anatomic study of the effects on the suprascapular nerve due to retraction of the supraspinatus muscle after a rotator cuff tear. J Shoulder Elbow Surg. 2003;12:497–500. doi:10.1016/S1058-2746(03)00182-4 [DOI] [PubMed] [Google Scholar]
- 91. Mallon WJ, Wilson RJ, Basamania CJ. The association of suprascapular neuropathy with massive rotator cuff tears: a preliminary report. J Shoulder Elbow Surg. 2006;15:395–398. doi:10.1016/j.jse.2005.10.019 [DOI] [PubMed] [Google Scholar]
- 92. Costouros JG, Porramatikul M, Lie DT, Warner JJ. Reversal of suprascapular neuropathy following arthroscopic repair of massive supraspinatus and infraspinatus rotator cuff tears. Arthroscopy. 2007;23:1152–1161. doi:10.1016/j.arthro.2007.06.014 [DOI] [PubMed] [Google Scholar]
- 93. Skedros J, Kiser C, Hill B. Florid suprascapular neuropathy after primary rotator cuff repair attributed to suprascapular notch constriction in the setting of double crush syndrome. J Brachial Plex Peripher Nerve Inj. 2015;10:e66–e73. doi:10.1055/s-0035-1567807 [DOI] [PMC free article] [PubMed] [Google Scholar]